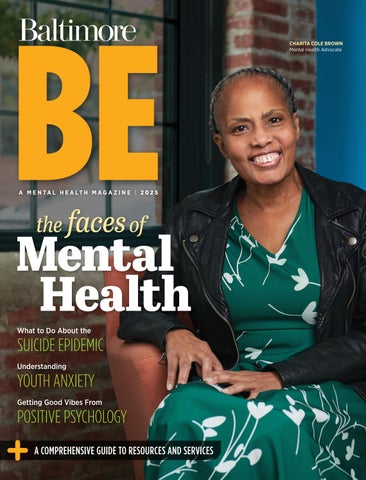
Mental Health the faces of
CHARITA COLE BROWN Mental Health Advocate


Sheppard Pratt is the largest private, nonprofit provider of mental health, substance use, developmental disability, special education, and social services in the country, and is consistently recognized as a top national psychiatric hospital by U.S. News & World Report .
With more than 160 programs, spanning inpatient, outpatient, communities, residential, and schools, Sheppard Pratt is here to help.
























At Hygea Healthcare, we provide innovative addiction treatments that combine traditional methods with cutting-edge technology and alternative healing approaches. Our team of professionals—including doctors, nurses, licensed clinicians, certified therapists, and peer support specialists—offers a comprehensive range of CARF-accredited levels of care. We provide detox, inpatient and outpatient services, and recovery aftercare, meeting clients wherever they are in their recovery journey.
HYGEA


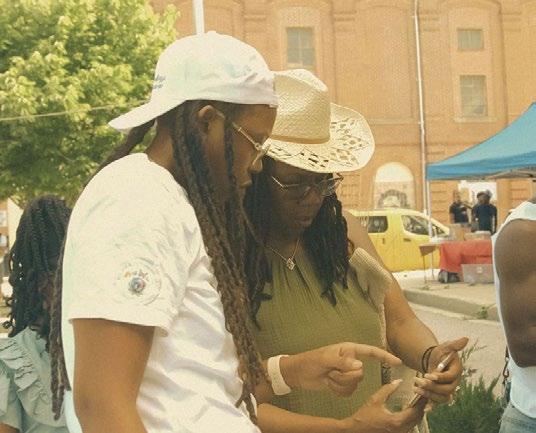
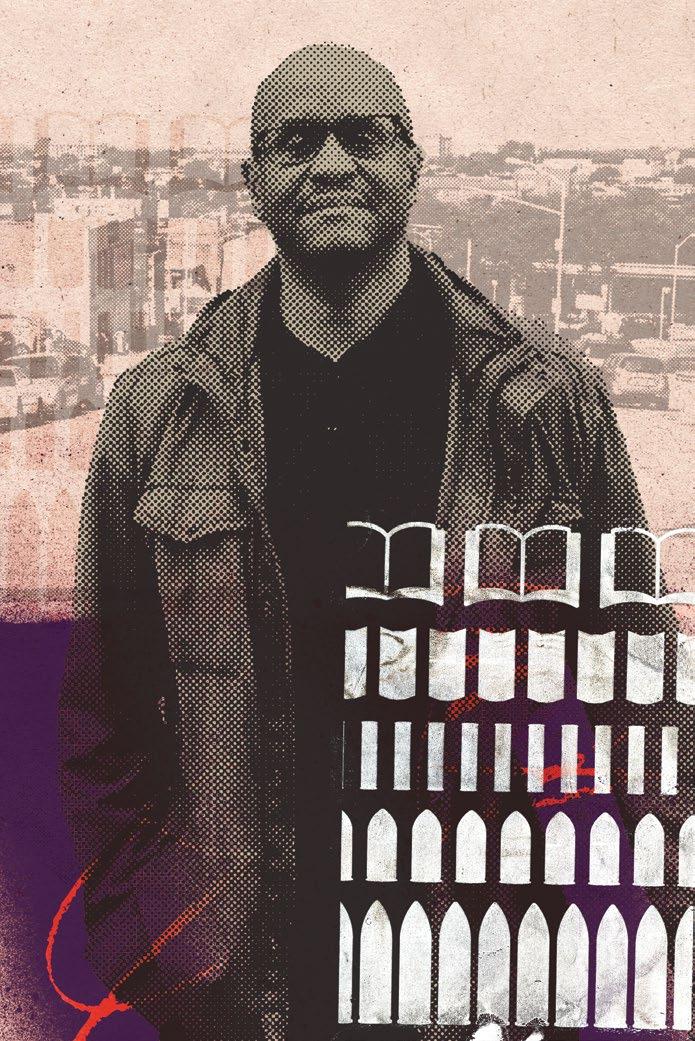
ON THE COVER Author and advocate Charita Cole Brown reflects on living with bipolar disorder in our “Faces of Mental Health” feature. Photography by Joanna Tillman.
32 Lifeline
We look at the rising number of deaths by suicide in the U.S. and how can they be prevented. BY CHRISTIANNA MCCAUSLAND
38 The Faces of Mental Health
Seven Baltimoreans speak out about how mental illness has touched their lives. BY JANE MARION, CHRISTIANNA MCCAUSLAND, AND MAX WEISS
➜ ONLINE EXCLUSIVE: READ OUR COMPLETE CONVERSATION WITH LT. GOV. ARUNA MILLER.

DEPARTMENTS
Kids Are Not Alright
Unpacking the surge in youth anxiety.
BY LAURA FARMER
Good Vibes
How positive psychology uses human strengths to build happiness, gratitude, and resilience.
BY DAN COOK
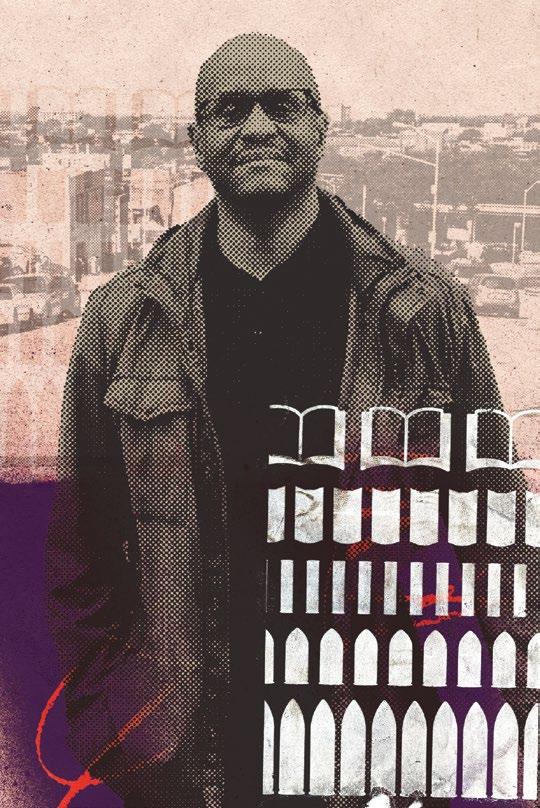
The Journey to Healing
A first-person perspective on trauma in Baltimore and the importance of accessible counseling.
BY KEVIN SHIRD
BLANK CANVAS
Nicole Clark
A local artist finds healing through her practice. BY JANE MARION
ONLINE EXCLUSIVE: SEE THE ARTIST AT WORK.
The
The renowned psychologist and author of An Unquiet Mind speaks out.
BY JANE MARION

How Be Came to Be
The topic of mental health is deeply personal to me and my family. Over 17 years ago, the youngest of my three sons presented with mental health challenges. He was 16 at the time, and until then was a straight-A student, a gifted athlete, talented musician, and had lots of friends. In other words, he was living a good life . . . as were we as a family.
My wife and I were totally caught off-guard, so I can only imagine what my son was going through. We immediately got him the help he needed through therapists and psychiatrists. At the same time, we had to fast-track our learning because we were clueless about his mental health condition. We also realized the need for emotional support, because while our friends had the best of intentions, they couldn’t possibly know what it was like to have a child struggling with a mental health diagnosis. How could they?

In our search for answers, we discovered NAMI (National Alliance on Mental Illness) Baltimore and attended a family support group. From there we learned about NAMI’s Family to Family program and attended their 10-week course. This taught us about the science behind mental health conditions, and the ways to best support our son. Just as importantly, it gave us the tools we needed to cope with his condition.
While much has changed since our son’s diagnosis, a needle that hasn’t moved quite as far as we might like is that of the stigma related to mental health conditions. Individuals with mental health diagnoses still face discrimination; they and their loved ones still deal with shame and blame. The concept of Be is to use storytelling to increase awareness and empathy for those affected by mental illness. In doing so, our aim is to reduce stigma and inspire acceptance and understanding.
NAMI had a profound and positive impact on my family and, 17 years later, I’m honored to continue volunteering as a family support group facilitator and advisory board member following many years of serving as their board chair. That is why, when we decided to move forward with this publication and corresponding event, it was natural to make them our nonprofit partner.
None of this would have happened without the support of CareFirst Blue Cross Blue Shield. From the very beginning, they pledged meaningful support to this ambitious ini tiative, which enabled
We hope you benefit from reading this publication. Our next step is to bring it to life with a storytelling event taking place in collaboration with Stoop Storytelling on March 6. For more information on the event, you can check out
Drawing on his own lived experiences, he supports 12to 18-year-olds facing mental health challenges in an afterschool program. His journey is a reminder of the powerful impact of treatment, empathy, and understanding in mental health recovery.
Michael Teitelbaum President, Baltimore magazine
Sam, here with his father Michael, works as a certified peer recovery specialist.














TRANSFORMING TRAUMA INTO STRENGTH


For over 23 years, the Holistic Life Foundation (HLF)—a Baltimore-based, BIPOC-led nonprofit founded by Ali Smith, Atman Smith, and Andres Gonzalez—has been at the forefront of trauma-informed yoga and mindfulness education. Our groundbreaking programs have empowered over 200,000 students and adults through 100,000+ hours of mindfulness training in schools, detention centers, drug treatment facilities, and underserved communities worldwide.
WHY THIS PROGRAM?
A pilot trial conducted with Johns Hopkins Bloomberg School of Public Health , Penn State , and Baltimore School District found that HLF’s mindfulness programs enhance emotional regulation, reduce stress, and improve resilience—findings published in the Journal of Abnormal Child Psychology Kennedy Krieger studies further recognize their impact in addressing Adverse Childhood Experiences (ACEs) and community trauma healing.
HLF was a driving force behind the trauma informed yoga and mindfulness framework of Baltimore’s Healing Cities Act, helping to establish the nation’s first trauma-informed city. With programs supporting trauma healing across five continents, HLF is recognized as a leader in trauma-informed yoga and mindfulness. As a certified instructor, you’ll gain mentorship, professional development, and access to a global network, expanding your impact and career opportunities.
Our 400-hour training program includes an in-person retreat in Baltimore with interactive online modules, covering yoga, meditation, breathwork, and traumainformed teaching. Gain real-world experience, hands-on mentorship, and the tools to create lasting impact in your community.
Stephen A. Geppi
Vice President Finance and Operations Debbie Darmofal
EDITORIAL, ART & PRODUCTION
Christianna McCausland
Senior Advertising & Marketing Designer Emily
Dan Cook, Laura Farmer,
Contributing Photographers and Artists Tracey Brown, Nicole Clark, Anthony Grant, Joanna Tillman
Vice President of Sales Stephanie Shapiro
Senior Account Executives Michelle A. Coughlan, Danny Glazer, Jodi Hammerschlag, Jennifer Rosenberger
Account Manager Michelle Weinstein
MARKETING
Director of Marketing Lorann Cocca
Content Marketing Manager Kamilia Arroyo
EVENTS
Events Director Jackie Hershfeld
DIGITAL
Digital Senior Editor Lauren Cohen
Digital Operations Manager Megan McGaha
BUSINESS
Finance Consultant Zach Papesh
ADVERTISING/EDITORIAL/BUSINESS OFFICES 10150 York Rd., Suite 300, Cockeysville, MD 21030 443-873-3900 baltimoremagazine.com













HIGHEST SELF
SERVICES WE OFFER:
Individual, Couples and Family Counseling
Medication Management
Psychiatric Rehabilitation Program (PRP)
Respite
Community Housing
Partial Hospitalization
Intensive Outpatient Program (IOP)
Residential Treatment
Community Employment Services
Assertive Community Treatment (ACT)
Day Treatment
Reiki Energy Healing



OUR
D-Dedication
I-Improvement
V-Vulnerability
I-Integrity
N-Neighborly
E-Example
LOCATIONS:
To live in Baltimore is to love it. To love something
is to watch it change and grow.
In a world where mental health care can be challenging to come by – whether due to stigma, providers outside of your insurance plan, or simply the overwhelming lack of available mental health care providers – knowing what resources are available is key. Luckily, Baltimore is famous for being a city of neighborhoods. And as neighbors, we hold an unspoken agreement to show up for one another. Whether it’s at a block party, a front stoop, the neighborhood community center, the corner bar, or a weekly support group, there’s no shortage of people who care.
That’s the thing I’ve always loved best about living here–and the thing I love most about NAMI Metropolitan Baltimore. We’re an organization built by people who, back in 1983, were looking for support and didn’t have somewhere to turn, so they made one. This effort that started as a conversation around a kitchen table has since blossomed into the nation’s largest grassroots mental health organization, made up of real people on the ground, all over the country, who understand their immediate community’s unique needs.


Here are the facts: People in Baltimore experience Adverse Childhood Experiences at a higher rate than the rest of Maryland, the average delay between the onset of mental health symptoms and treatment is 11 years, and one major reason for this delay is stigma. That’s why it matters that over 200 of your neighbors volunteer with NAMI Metro. To help the 1 in 4 of us who will experience a mental health crisis in our lifetime and the people who love them.
How do we do that? By intentionally holding spaces where we can explore our emotions without judgment; by bringing mental health education into where we learn and where we worship and where we work; and by boldly sharing our stories so others can share theirs. Let’s normalize the conversation about mental health and eradicate the stigma that keeps so many of us from seeking help. Mental health isn’t someone else’s problem–it’s yours and mine, and Baltimore’s, together. We can all contribute to making a difference.


Kerry Graves, Executive Director

Mind Matters
BRAIN AIDS
These innovative treatments may offer alternatives to those for whom conventional therapy is not effective.
➜
BY COREY MCLAUGHLIN
NEW FRONTIERS
An estimated 60 million Americans experienced a mental-health related illness in the past year, and some researchers believe roughly half of the U.S. population will encounter one at least some time in their life. For many, traditional front-line treatments like talk therapy and medications such as antidepressants–which have been found to help roughly two-thirds of the population–are effective. But for others, alternative options have been limited until recently.
Some treatments are newer than others. Psychedelics, for example, are ancient but remain taboo in many circles. Much like the brain itself, many are just starting to be understood. “We can take pictures and try to measure some things, but the brain is a little harder to study than other areas of the body, because it’s obviously inside of our skull and it’s hard to access,” says Trish Carlson, a psychiatrist at Sheppard Pratt.
The following innovative treatments, practiced and researched locally, show promise to help meet the challenge.
IT’S ELECTRIC
Transcranial magnetic stimulation is a non-invasive, in-office potential solution for treatment-resistant depression.
Transcranial magnetic stimulation, or TMS, can be a relatively simple, life-changing choice for those with treatment-resistant depression. (Patients who qualify have tried at least two antidepressants that have not proven effective.)
Transcranial means across or through the skull. With TMS, a magnetic coil is positioned over the head that delivers electrical pulses one to two centimeters deep, usually to stimulate a part of the left side of the brain (the dorsal lateral prefrontal cortex) that’s been found to be underactive in people with depression.
So long as patients don’t have epilepsy or seizure disorder or metal in the head or neck, the treatment is considered safe and delivered under the guidance of a doctor, nurse, or trained technician. Patients sit in a chair for roughly 20 minutes a day, five days a week, for five or six weeks, and let the machine work. There’s a three-minute protocol that’s also effective.
Trust the Process
Eye-movement desensitization and reprocessing, or EMDR, can calm the brain to help you make sense of trauma, anxiety, and stress.
A black plastic bar, about to be illuminated with green dots, rests on a tripod a few feet away. You’re handed a pair of mouse-sized buzzers, told to think of your distressing thought and follow a speck of light as it moves from left to right and back again. The buzzers occasionally stimulate your hands.
The sequence moves quickly. It can be difficult to keep up. After 10 seconds or so, a clinician pauses everything, asks you to briefly share what you’re thinking now, if you’re still stressed at a level 10. Repeat. Again. For up to an hour, or maybe even another session, until you report you’re feeling closer to zero—calm—while thinking of what’s been bothering you.
“What it’s thought to do, in the same way that we think oral medications work, is change the neurotransmitter balance in the brain,” says Trish Carlson, a psychiatrist and service chief of the TMS program at Sheppard Pratt in Towson. She notes that everything in our brain works
off electrical energy. “TMS is focusing directly on the area of the brain we think needs to be rebalanced.”
The noninvasive procedure is thought to rebalance neurotransmitters in the brain like serotonin, norepinephrine, and dopamine, that help to regulate mood, and increase blood flow in the targeted area.
The FDA approved TMS as a major depression treatment in 2008 and Carlson says the majority of people will see some improvement. Research shows that roughly one in four patients experience full remission and about half enjoy partial relief, with about two-thirds still feeling better a year later.
Most insurances cover TMS use for depression. In 2018, the FDA also approved it for treating obsessive-compulsive disorder by way of targeting a circuit across both sides of the brain while a patient is asked to think of, or be exposed to, what makes them anxious. More research is being done relative to cognitive disorders, addiction, and PTSD.
This is what eye-movement desensitization and reprocessing, or EMDR, looks like at Bolton Therapy & Wellness in Bolton Hill, one place you can find the mental health treatment technique that can help heal trauma or other troubling experiences. The process, which can include tapping opposite sides of the body or listening to sounds, mimics natural dual attention (or bilateral) stimulation in the body thought to help the brain properly store and process distressing memories.
The eye movement and other stimuli are “calming the right brain that’s feeling the anxiousness and bringing onboard the left brain that’s reasonable,” says Lisa Robinson, the practice director at Bolton. “At the end, you don’t have the same agitation, physical sensations, or arousal due to the memory, and you can move on.”
Developed in the late 1980s by New York-based psychologist Dr. Francine Shapiro, who found that walking paired with moving her eyes back and forth eased her distress, EMDR has since been found to help
Reality Shift
people cope with PTSD, anxiety, stress, phobias, addiction, and to rewire memory networks in adults and children.
“It’s changed my practice,” says Dr. Desyree Dixon, who founded Bolton in 2013, got trained in EMDR in 2019, and now teaches others to use the method. “Sometimes I want to reach out to some of my earlier clients and say, ‘Come back, let’s work on some of these things using this new tool.’”
Psychedelics still have limited legal use for mental health, but that could be changing.
You don’t need to travel far to realize Baltimore is an epicenter of psychedelic research. Johns Hopkins Hospital has a research center that’s been dedicated to psychedelics for the last two decades and at Sheppard Pratt, the Institute for psilocybin has been exploring uses since 2022. And beyond those institutions, there’s a local community exploring the potential mental health benefits of psychedelics’ mindaltering power.
David Jun Selleh, a psychotherapist and licensed clinical professional counselor at Inner Path Wellness in Mt. Washington, for instance, is a part of Maryland Gov. Wes Moore’s task force—established in 2024 as the seventh of its kind in the U.S.—due to deliver policy recommendations for psychedelics from mushrooms and plants to state legislators by the end of July. “Generally, all psychedelics induce neuroplasticity in the brain,” Selleh explains, “the growth of new cells—which allows for new ways of thinking and new perspectives. When you combine that with [talk] therapy, it breaks everything open to possibilities.”
He’s sitting on a couch at Inner Path, alongside University of Maryland, Baltimore alumna Lauren Going, who co-founded the city’s first psychedelicassisted therapy center in 2022. Here patients are given an eye mask, headphones, a mat, and a private room to sustain them on their travels, and as soon as four minutes after receiving
a supervised injection of the psychedelic drug ketamine, they usually experience the peak of what’s typically a 45-minute to hour-long “journey,” says Selleh.
It’s a hallucinogenic trip often described as an out-of-body experience. Ketamine, primarily a synthetic drug used legally for decades as a general anesthetic, creates a surge of the neurotransmitter glutamate in the brain. At Inner Path, ketamine is used off-label for treatment-resistant depression, suicidality, or other mental health disorders. With a low psycholytic dose, people can think and speak clearly while they’re under the influence. With a higher dose, after patients return to reality, a second hour of talk therapy follows, the idea being the trip can spur more lasting change.
Times and tastes have changed since the heyday of the Grateful Dead and in the roughly 50 years since most psychedelics were outlawed by President Richard Nixon in what became known as the War on Drugs. Names like “magic mushrooms,” (psilocybin), LSD, or MDMA still get a bad reputation. Ketamine is also still known as the “Special K” party drug. But psychedelics, which some archeologists say humans may have experienced tens of thousands of years ago, delivered in a supervised clinical setting have shown great promise.
In 2019, the FDA approved a ketamine nasal spray for major depression. The Department of Defense is funding psychedelic research for veterans with PTSD and traumatic brain injury. Additional legal pathways for uses could be coming. The 19-member state task force of which Selleh is a part won’t directly change the regulatory status of any psychedelics, but their recommendations could be a catalyst. “There is rising support,” Selleh says. “People are hearing enough to know there’s something to this.”
Kay Redfield Jamison A CONVERSATION WITH
The renowned psychologist and author of An Unquiet Mind talks about stigma.
BY JANE MARION | PHOTOGRAPHY BY MARLAYNA DEMOND
As a young girl growing up in Virginia, Kay Jamison was intense, curious, and had a keen fascination with science. She volunteered as a nurse’s aide, a candy striper, and even assisted with minor surgical procedures at the hospital at Andrews Air Force Base, where her father was a pilot and meteorologist. At 15, she toured a federal psychiatric hospital, St. Elizabeths in the District of Columbia, for the first time, which she says she found “fascinating and horrifying,” not knowing that she, too, would soon suffer from own mental illness.
And while Jamison had always had a passionate personality, by the time she was a senior at Pacific Palisades High School in suburban Los Angeles, she found her moods shifting between two extremes—exhilarating highs and dark, unyielding lows. That pattern continued for years, though she never sought help or intervention.
It wasn’t until 1974 (just three months after becoming an assistant professor of psychiatry at the University of California, Los Angeles) when she became, in her words, so “ravingly psychotic” that she could no longer ignore the fact that something was terribly wrong. That something was bipolar illness, then known as manic depression. It was, in fact, a disease she was all too familiar with thanks to her patients whom she diagnosed (and her own father who struggled with the
illness). And though she shared her diagnosis with colleagues and close friends, her illness was largely a secret.
After years of serious struggle, a near-lethal suicide attempt, and always a fear of being “discovered,” in 1995, Jamison wrote An Unquiet Mind: A Memoir of Moods and Madness, an astonishing account of what it’s like to live with bipolar illness. As both a student of the disease and someone who struggled with it, the stakes could not have been higher.

immune from detractors. As she writes in a 2011 preface to An Unquiet Mind, 15 years after the book’s first printing, “The kindness and generosity of most people was heartening, the vitriol and irrationality from others disturbing.”
Because she was afraid of the way her work would be perceived, Jamison knew that telling her truth would mean giving up her clinical practice, by then at The Johns Hopkins Hospital. She also feared that publicly sharing her story would lead to losing her hospital privileges or, even worse, her medical license.
It did not. Instead, she revolutionized the field, becoming one of the most famous faces of the illness (along with a long line of luminaries who suffered from bipolar disorder, including writer Sylvia Plath, poet Robert Lowell, and composer Gustav Mahler) and one of the foremost authorities in the world on the disorder, even co-authoring the definitive medical text on the topic.
The acclaim, however, has not made her
Thirty years since the publication of her groundbreaking book, we spoke with Jamison (now professor of psychiatry at The Johns Hopkins School of Medicine and co-director of the Johns Hopkins Mood Disorders Center) about stigma, how to prevent it, and how views about mental illness have changed since she wrote her memoir.
Do you remember the day you were diagnosed with bipolar illness, which was then known as manic depression? I went to a psychiatrist who had been my clinical supervisor when I was an intern and I trusted him implicitly as a doctor. He was the only one I trusted to go see and he just gave me a very thorough psychiatric examination. He said, “It’s unequivocal. You have manicdepressive illness. You are going to need to be








on lithium”—and that was the beginning of struggling with that notion of taking lithium. Overwhelmingly, I was relieved because I knew he was right and I admired him for not mousing around about it and not prettying it up and just saying, “This is going to be really hard.”
Was there a light-bulb moment when you decided to write An Unquiet Mind?
Some of it was that I felt hypocritical treating and studying the illness and not acknowledging that I had it. Also, I got fed up, hurt, and overwhelmed by the lack of information about how many people have bipolar illness and how unaware the world is in general.
When did you start thinking about the impact of sharing your story?
All along, and certainly when I was going to publish a book about my illness, I thought about it endlessly. Would I lose my job?
Would I lose my hospital license? Would I lose my state license? I knew I would lose my privacy and I knew I would lose my ability to see patients.
Was any part of you reluctant to share?
Of course—and I still am. I am trained to be a therapist and I loved it. It was a huge part of my clinical identity. I practiced close to 20 years, including clinical training before giving it up.
Why did you feel you’d lose the privilege of seeing patients for sharing your story?
I had written a very personal book. I had practiced before [the book was written] and had told people about my illness and also colleagues with whom I’d worked to feel free to contact my psychiatrist and chief of my department if there were any concerns whatsoever. Fortunately, that didn’t happen. My book was terribly personal and I think patients have a right to come into your office and talk about their own problems without putting it through the whole kind of strange way of looking at it from someone who has written a book about it.
Where does stigma come from?
“Stigma” is a word I really don’t like, I prefer the word “discrimination,” partly because it has legal implications but one uses stigma because it’s widely used.
So where does discrimination come from?
If you look at the animal world in general, whether you look at a dolphin or a sea lion who is strange to a group, that will be picked up immediately—and the animals will respond accordingly. It’s a natural reaction when things are different. It’s not surprising that when people act in ways that are not usual or ways that make people frightened or hopeless, people are going to distance themselves from it. I feel very strongly where our field [of medicine] has let all of us down is that you can’t just expect people to understand—that is unreasonable. What you can do is give them information with which to possibly change their mind.
How do you prevent discrimination?
The greatest way to destigmatize any illness, and particularly with a psychiatric illness, is with research and good treatment. If you look around you in medicine and you look at epilepsy, for example, it’s not that there’s not still stigma around it but there’s much less stigma than there used to be. And that started when you could begin to control public seizures. And with something like cancer in the ’50s, when it was pretty much a death sentence for many kinds of cancers, people wouldn’t talk about it—and now it’s treatable, so they talk about it much more.
What is the impact of stigma?
The most devasting impact is that people don’t get treatment. They feel alone with their suffering and they feel like they don’t want to reach out and others don’t understand or their licenses are going to be pulled or they are going to lose a job or a relationship—and those are all very legitimate reasons. And then, of course, people stigmatize themselves by saying, “I should be able to pull myself together.” This seems much more a
part of personality than other medical illnesses. It seems like you ought to be able to get over it by dint of will.
When you got sick, was your line of thinking that you should “just be able to handle it”?
At some point it became clear I was ill and that I was not anywhere near myself. It took a while. I was brought up like many people to believe that you could just get a grip—I was brought up Episcopalian and in a military family and in worlds that put a real premium on coping with something yourself and getting on with it. And that’s completely not helpful. It’s a good philosophy of life in general, it’s just not a good philosophy of life when you are ill.
Do you see things changing in terms of discrimination?
I do. The things that have helped psychiatric illnesses is that there are many more treatments available than there used to be. And people are much more aware of it than they used to be. General physicians are more aware of it, too. And people in general are aware that there are antidepressants and you can go to a doctor and maybe get some help. People talk about it more. And thanks to the internet, people can learn much more about it.
People are better informed than they used to be, but I also think there’s a huge amount of misinformation and a lot of terrible attitudes. If you look at the language in the public arena in politics, you can say people are “crazy,” “come from insane asylums,” or are “nutty as a fruitcake.” People can say things about those with mental illness that you could never say about any other large group. That’s painful for people.
How did the pandemic impact people who were struggling?
One of the things that happened during the pandemic is that people became much more aware of the extent of mental illness around them, because they were in day-to-day contact with their kids in a way in which they
are ordinarily not—so they saw the illness. But it has also had a tendency, perhaps, to trivialize—everything is “anxiety” and “depression” in a general, somewhat ill-defined way. There’s all these sloshing around of concepts together that take away from the notion of illness. People say, “mental health issues” instead of mental illness. I suppose it’s meant to be less stigmatizing and more normalizing. But it’s confusing. I just think that the language has gotten mushy.
You were diagnosed as a medical resident. How have you seen attitudes toward seeking help change within the medical community? Residency programs are doing better than they used to and are more aware of depression and stress. It’s up to medical students and medical school faculty to make education about depression a priority so that students recognize symptoms if they get them—or can recognize them in their colleagues. It’s better now than it was, but it’s still pretty minimal.
Your memoir was published 30 years ago. Would you do anything differently now?
Probably not—you have to write what you have in front of you in terms of your life. You are not given the opportunity to go back and change things.
What advice would you give to your younger self and what do wish you knew then?
I went off my medication on and off for the first few years of my illness but that was very costly, there was tremendous loss, and I haven’t stopped my medication for decades, but I regret that hugely.
What personal price did you pay for going off your medication?
Getting manic, getting depressed again, getting suicidal, nearly dying by suicide.
What’s your advice to anyone who is struggling or who loves someone who is? Learn. Read. Be aware that good treatment exists and that the consequences of not getting treatment are pretty awful.







RESIDENTIAL MENTAL HEALTH TREATMENT PROGRAM FOR YOUNG ADULTS

ClearView Communities is a longer-term (12-18 months on average) residential mental health treatment program located in the suburbs of Frederick, MD treating young adults. Our program incorporates four houses on campus, with eight private bedrooms in each.
PSYCHIATRY & MEDICATION MANAGEMENT
INDIVIDUAL, GROUP & FAMILY THERAPY
4 HOUSES, 32 BEDS STAFFED RESIDENCES
OCCUPATIONAL THERAPY
ART STUDIO & EXPRESSIVE THERAPY
THERAPUTIC NATURE PROGRAM & GREENHOUSE
WELLNESS CENTER
MILIEU THERAPY & SOCIAL SKILLS
INDEPENDENT LIVING & DAILY LIFE SKILLS
COMPREHENSIVE NURSING CARE
COMMUNITY INTEGRATION INCLUDING SUPPORTED EMPLOYMENT, EDUCATION & VOLUNTEERING
The Kids Are Not Alright
What’s behind the surge in youth anxiety?
Lindsey Culli vividly remembers the day in the fall of 2021 when she got a phone call from the counselor at her son’s Baltimore County public school alerting her that he had expressed a desire for self-harm. At the time, Calvin was a six-year-old first grader who was struggling to navigate the post-pandemic world, especially after spending his early education in front of screens.
“Calvin was one of those kids who was in kindergarten when the pandemic started,” Culli recalls. Though her son was academically high achieving, she believes that the social isolation of those years stunted his social and emotional growth.
“He’s an introverted kid. He was feeling all these big feelings [at school] and he didn’t have a way to express it,” says Culli. “He was saying the most outrageous thing he could say, which terrified the guidance counselor because he started talking about self-harm.”
Naturally, this alarmed his school counselor, who took his words seriously. Thankfully, it eventually became clear that Calvin didn’t have plans to actually harm himself.
“He was just kind of grasping at, ‘What is the biggest thing I can say to get somebody to pay attention because I’m not okay. I don’t know the language to talk about what’s wrong. I just know that something is.’”
Eventually, Calvin’s “big feelings” escalated to a point that Culli and Sam, Calvin’s father, decided it was time to seek professional help. Fortunately, Calvin’s school had an arrangement with a private practice therapy group that saw students during the day. His therapist diagnosed him with anxiety and began helping him learn tools to manage it.
“He started seeing a therapist that spring and it was really helpful pretty much right away,” says Culli. “[His therapist] gave him the toolbox that he needed and started putting tools in his toolbox to be able to recognize the emotions he was feeling and name them [and] work through them. That is hard when you’re an adult, but it’s especially hard when you’re only six! He’s come a really long way and it’s a testament to the therapy that he’s gotten and the people that he’s been able to work with.”
Today, Calvin is an active 10-year-old. He still struggles with anxiety—Culli thinks it is likely part of his wiring as someone who strives to be high-achieving. The difference is, when he gets those “big feelings,” he knows how to process them. Best of all, Culli has watched Calvin grow into the creative, empathetic, and thriving kid she always knew him to be.
“We named Calvin after the [comic strip] Calvin and Hobbes,” says Culli. “It turns out he’s actually a lot like the comic book Calvin! He’s very creative. He’s very bright. He’s also a really good friend. He has so much empathy, which probably hinders his mental health a little bit because he takes on other people’s feelings and emotions. I think it’s both a strength and also a challenge to be an empathetic and compassionate person in a world that can be so tough. But now he has the tools to manage it.”
Calvin’s experience with anxiety as a young child is not unique. According to the Centers for Disease Control and Prevention (CDC), about 10 percent of children between the ages of three and 17 have a diagnosed anxiety disorder. Experts contend that it’s normal for kids to experience occasional anxiety about stressful things like academics or social situations. But the National Institutes of Health (NIH) explains that anxiety becomes a disorder when it does not go away and its symptoms interfere with daily activities.
Biologically, the way our bodies experience anxiety is similar to the way we process fear. Fear keeps us safe from danger, preparing our bodies for “fight or flight.” Our heart and breathing quicken to boost oxygen flow to our brain. Our muscles tense up to prepare us to run, fight, or hide. Our minds zoom in with a laser focus on the threat to determine the best plan for safety. Anxiety is the body’s response to a perceived threat. While this heightened state of awareness is helpful for actual danger, living in a state of high alert about unspecific future threats can be overwhelming—especially for children who may not have the tools to manage these feelings.
Krista Dhruv, LCSW-C, is an individual and family therapist and educational consultant based in Baltimore. She has served as a counselor in K-12 schools and higher education settings and has observed how anxiety presents in children of all different ages.
“Starting with our youngest kids, they might experience somatic symptoms, like belly aches, headaches, and disrupted sleep,” explains Dhruv. “It manifests physically because anxiety is in the body. It’s hormonal—cortisol and adrenaline, a hormonal response to perceived fear, metabolizes in the body. [Anxiety] also shows up as worry language: a lot of ‘what ifs’—‘What if you forget to pick me up? What if nobody wants to play with me? What if I eat something and it makes me sick?’”
Research suggests that the causes of childhood anxiety are complex. Some children may be more sensitive to strong emotions or have a biological tendency toward anxiety. For others, anxiety may develop as a reaction to a significant stressful event, like a death in the family. Environmental stressors, such as food insecurity, parents who fight or argue, or experiences of bullying, abuse, and neglect can also cause anxiety in young people.
Further, larger events and issues, such as climate change or global instability, may also impact children’s wellness—especially for older kids who may be more aware. An often-cited study conducted by the Pew Research Center indicates that more than half of teenagers are worried about a shooting happening at their school. Other environmental factors inducing

worry are, well, the environment. A recent survey published in The Lancet polled 10,000 young people across 10 countries, revealing that as many as 84 percent of respondents were worried about climate change, with 45 percent reporting that climate anxiety affected their daily lives.
Regardless of the constellation of causes behind anxiety, it is important to note that it is on the rise. A Department of Health and Human Resources report in 2022 noted that between 2016 and 2020, the number of children ages 3-17 years diagnosed with anxiety grew by 29 percent and those with depression by 27 percent. This is important on many levels, not least of which is that a mental health
“overprotection in the real world and underprotection in the virtual world are the major reasons why children born after 1995 became the anxious generation.”
Kids’ brains are literally being rewired during their crucial early, brain-building years.
“In this new phone-based childhood, free play, attunement, and local models for social learning are replaced by screen time, asynchronous [or non-real-time] interaction, and influencers chosen by algorithms. Children are, in a sense, deprived of childhood,” explains Haidt.
Dhruv agrees and has observed the impact of screen time on today’s youth.
“[Social media] is kind of experience where young people are socializing and interacting,
Anxiety can show up as what ifs: ‘What if you forget to pick me up?’ ‘What if nobody wants to play with me?’
condition is a risk factor for suicide, which is also on the rise among young people. Increasingly, experts point to a growing cause of mental illness in young people: social media and phone use. Jonathan Haidt, a social psychologist and author of The Anxious Generation: How the Great Rewiring of Childhood Is Causing an Epidemic of Mental Illness, claims that what he terms a “phone-based childhood” is to blame for a many of these unsettling youth mental health trends. In fact, so great is the impact of social media that U.S. Surgeon General Dr. Vivek Murthy recently called on Congress to require warning labels on social media sites to communicate their potential harms, especially for the developing adolescent brain. And Australia just passed a groundbreaking ban on a social media for children 16 and under.
Haidt likens young people’s unrestrained exploration of this new virtual frontier to launching our children to the planet Mars without first doing an appropriate amount of research to realize their bodies and minds are not suited to survive this alternate planet. The research he presents in his book posits that
but being that they’re online, the whole body isn’t involved—it’s disembodied. Young children aren’t outside as much playing and climbing trees—maybe even spraining an ankle. Kids aren’t taking healthy risks, which are imperative to healthy development.”
“These are normative life experiences that build our resilience and develop a growth mindset,” Dhruv continues. “When most of our [socializing and recreation] is happening online, whether it is video games or through social influencers, we lose that ability to take risks, social or physical or emotional, and to really experience failure as well as success, which is part of life.” She echoes Haidt’s ideas about asynchronous interactions: “I might text you this morning about a funny thing that my dog did and you might not text me back until 3 o’clock today with a cute little emoji, which feels good.” But something is off: Human beings aren’t meant to communicate via delayed reaction or strictly through our laptops or phones. “We are wired to be in community and in connection,” she says. “We should be able to read body language. If I say something and a friend grimaces, I realize I probably shouldn’t
say that again, or I should check in with her about that. [With online socializing], we lose all that nuance of the human experience.”
There is, however, a silver lining to the over-sharing that is often seen on social media. Experts note that children are increasingly likely to talk about their mental health with transparency, which is steadily chipping away at the stigma of mental illness. There are additional benefits to phone use and social media. For example, many kids who may feel marginalized due to their differences can more easily find their community online. And experts are keen to note that the phone itself is not the enemy: If used responsibly, it’s a valuable tool to help us connect and make life easier. The key is to make sure parents place limits on the amount of time kids spend on screens and the content they view.
“The one positive about social media is that it allows access for a great deal more information,” explains Chad Lennon, MD, a child and adolescent psychiatrist for Sheppard Pratt. “People are communicating more about their mental health.”
Young people are more aware of mental illness—and the resources available to help.
“What has happened over the past 10, maybe 15, years or so is a complete shift. Now what we see that most of the people coming to us for services, whether it’s in a school environment or private practice, are already coming with the diagnostic language. They’re coming with deep attunement to their emotional experience, saying specifically, ‘I have anxiety,’ or ‘I think I’m neurodivergent,’ or ‘I’ve had this many years of treatment,’” shares Dhruv.
And therapy really does help. Calvin is a perfect example. The tools his therapist gave him were the key ingredients for helping him return to the thriving and intelligent kid his parents knew him to be.
“I think therapy is very helpful for everyone, but if you have anxiety, without [therapy], it can be hard to go through daily life and not get overwhelmed or upset,” says Calvin, with a thoughtfulness and maturity that belies his years. “Therapy has helped me to be able to be in certain places or spaces and without feeling afraid or anxious. I have more friends
now and I can do things I think would be fun without being overwhelmed or afraid.”
For parents of children with anxiety, sometimes it’s hard to know what they can do to help. Lennon advises the following game plan: “First, parents really need to know themselves. The best way to help your own child is if you have a sense of your own emotional regulation,” he says.
“Secondly, I’m really big on helping kids develop coping skills—and I use that term very generally because really anything can be a coping skill, as long as you know it helps you reduce your anxiety. Coping skills can be anything from playing a sport, going for a walk, taking a deep breath, reading or drawing, connecting with friends, even video games can be helpful, if used properly.
“[Thirdly,] connect with someone you trust,” shares Lennon, who adds that this doesn’t necessarily need to be a therapist. “This could be a parent, aunt, uncle, or coach. Helping a child connect to someone they trust helps them realize they are not alone, which goes a long way toward reducing anxiety.”
Therapist Krista Dhruv also advises that a great starting point for finding help for school-aged children is the school counselor and/or pediatrician. “The school counselor is a great first place to go,” she says. “They don’t necessarily know your child best, but they know this age range really well and can help you understand this developmental stage and what’s normative, typical, or atypical behavior.”
The family’s pediatrician is also trained to spot an anxiety disorder or help a family understand how to best help a child. Furthermore, they can examine if there is a physical cause for anxiety, especially when a child presents with somatic complaints. Finally, there’s a practical consideration for reaching out to the pediatrician: They can provide a referral for mental health services, which in many cases makes it easier for your health insurance to defray these expenses.
Fortunately, experts agree that most children with anxiety can reduce its impact through a combination of therapy, appropriate medication, and lifestyle changes.


Good Vibes
The practice of positive psychology focuses on growing human strengths to achieve greater levels of happiness, gratitude, and resilience.
Chazz Scott had it all. The successful career as a cybersecurity expert. The six-figure salary. The well-appointed condo overlooking the Potomac River and the high-end luxury car. From the outside, life looked good, but appearances can be deceiving, and they masked Scott’s inner turmoil. He was burned out at work and battled depression. He felt hollow and lacked passion for the things that once fueled his ambition and joy. While searching for ways to shake the malaise, Scott thought back to reading The Power of Positive Thinking by Norman Vincent Peale in college. The self-help book made him realize he could change his current reality simply by changing his mindset.
Scott knew he needed to focus on what was good in his life to create a positive energy that would build momentum toward fulfillment and contentment. It was a straightforward concept, but Scott’s science-based mind craved supporting evidence. He dove into researching neuroscience and discovered the fundamental elements of positive psychology, a relatively new field of study that helps people achieve higher levels of happiness and reach their true potential. Scott was fascinated by the field’s intersection with neuroscience, particularly as it relates to the study of neuroplasticity.
“For many years, it was widely assumed that people were stuck with their current way of thinking,” says Scott, who grew up in Ellicott City. “But we now know that the brain is capable of change through new thoughts and behaviors. With repetition
and consistency, new neuropathways are created and older, less-used pathways become weaker.”
About eight years ago, Scott began to incorporate positive psychology into his life by establishing a morning routine that prioritizes his physical and mental well-being. He wakes up at 5:30 a.m., goes for a brief jog, and completes stretching exercises before meditating for 20 minutes. He then carves out time for reading or listening to a podcast. This combination of movement, mindfulness, and mental growth sets a positive tone for his day and keeps him feeling balanced and productive. The seemingly minor steps resulted in gradual but profound changes to the way Scott viewed and lived his life.
“I feel happier, more resilient and better equipped to handle challenges that come my way,” he says. “Understanding that we all have the innate ability to change our mindset is incredibly empowering. It provides hope for something more.”
The nation’s mental health crisis and corporate burnout epidemic suggest millions of adults and adolescents need help in their
own search for more. That’s where positive psychology comes in. Its empirical study of the factors that allow some of us to thrive while others search endlessly for life’s true meaning helps to define true happiness and how to achieve it.
Positive psychology was popularized by Drs. Martin Seligman and Mihaly Csikszentmihalyi in the late 1990s as a departure from psychology’s traditional disease model, which focuses exclusively on treating mental disorders. Positive psychology does not address behavioral or emotional dysregulation and is not a substitute for treating severe mental illness. Instead, its interventions grow positive emotions and resources that help people maximize their true potential.
Dr. Seligman believes psychology should be just as concerned with human strength as it is with human weakness, and that it should focus on amplifying the best things in life while nurturing people’s innate talents.
“Positive psychology’s traits are skills that can be learned and strengthened, much like any other ability,” says Carly Hunt, who earned her PhD in counseling psychology
from the University of Maryland, where she was the faculty instructor of a course called Living the Good Life: The Psychology of Happiness. “With intentional practice, you can cultivate more gratitude in your life.”
Hunt played collegiate golf as an undergraduate at Georgetown University and as a graduate student at the University of Maryland. What she might have lacked in physical talent she more than made up for with mental toughness. “I’ve always been fascinated with sports psychology, positive self-talk, and the mental resilience athletes need to perform well,” she says.
At Georgetown, Hunt also took a Buddhist studies class. The coursework introduced her to mindfulness, self-compassion, loving kindness, and similar practices that led her to pursue a PhD at Maryland. Over the course of getting her PhD and doing a postdoctoral fellowship in biobehavioral pain research at Johns Hopkins School of Medicine, she studied positive psychology’s impact on physical health and the mindbody connection.
Part of Hunt’s current work as the owner of Present Mind Consulting involves helping driven professionals and high-end talent build the confidence and motivation they need to achieve their goals. She works with performers, sports teams, and artists to address mental health challenges and cultivate personal strengths. She also collaborates with companies to develop strategies that enhance employee well-being and foster a healthier work environment.
Hunt works closely with Christopher Steer, who earned his law degree from the University of Maryland School of Law and now runs a consulting firm that helps companies achieve higher levels of organizational performance. Steer initially grasped the importance of positive leadership as an undergrad captain of the Johns Hopkins lacrosse team. That realization was reinforced by reading the book Man’s Search for Meaning by Viktor Frankl, which introduced him to the idea of stimulus and response, and how the space between them is where growth, joy, happiness, and contentment happen.
“Personal evolution involves focusing on the things we can control rather than
At EviJoy Counseling Center, we understand that life’s challenges can feel overwhelming. Whether you’re an adolescent or an adult, our compassionate team of ten counselors can help you navigate stress, anxiety, depression, mood disorders, trauma and all facets of perinatal mental health. We specialize in providing support that empowers you to process and cope, so you can thrive through life’s toughest moments. Take the first step towards healing and resilience today.


“Positive psychology helps people build on their strengths or resilience resources like mindfulness, rewarding social connections, and compassion toward self and others.”
feeling like life is happening to us,” says Steer. “If you’re not getting the results you want, it’s time to explore a different path.”
Positivity—or good vibes, in the colloquial—is important, and people need to maximize their inner strengths, but Steer believes these feel-good ideas must link to tangible results. He says research reveals that executives and managers who lead with positivity drive better performance among their teams. That’s why high-level executives are increasingly interested in engaging in conversations about psychology, energy, and engagement. They’re realizing it’s not only acceptable but increasingly essential to embrace these concepts.
“Business leaders have started having conversations about emotional intelligence and the principles of positive psychology in the world of organizational development,” says Steer. “Modern neuroscience and psychology have finally converged within long-standing intuitions. Now, we can bring them together in a way that’s more accepted and impactful.”
Steer points to Satya Nadella, chairman and CEO of Microsoft. When Nadella took over the company, he instituted a peoplefocused approach and introduced Carol Dweck’s book Mindset: The New Psychology of Success as required reading. “Microsoft talking about mindset? That’s a gamechanger,” says Steer. “The right influencers, backed by solid research, can shift an organization’s culture.”
Positive psychology is no replacement for competitive salaries, good benefits, and the opportunity for professional growth, but Steer says research now reveals that corporate executives who lead with positivity
drive better performance, retention, and development. “You can’t commoditize dealing with people,” he adds, “but the ability to manage the human variable is becoming the most valuable skill.”
As we all know, life isn’t always easy. Hardships happen. Challenges are inevitable. In that sense, the term “positive psychology” is a bit of a misnomer. The practice is not concerned with papering over negative experiences. It’s more about finding tools to cope with negative experiences and even grow from painful events or adversity.
“Positive psychology helps people build on their strengths or resilience resources like mindfulness, rewarding social connections and compassion toward self and others,” says Hunt. “These resources help us withstand challenges and even thrive when facing them.”
Chazz Scott tuned his passion for positive psychology into the launch of Supra Mentem, a consulting business that specializes in helping executives, entrepreneurs, and professionals improve their overall well-being, reach peak performance, and achieve sustainable success. He emphasizes that embracing gratitude and experiencing positive emotions doesn’t involve ignoring life’s difficulties or being overly optimistic.
“Many of us don’t have effective coping strategies in place, so when stress occurs, we don’t know how to deal with it,” says Scott. “I’m now able to recognize when stress levels rise. I know to begin breathing exercises or meditation to get my body back to a state of balance. Having a set of practices to fall back on is essential for effectively managing life’s ups and downs.”
Scott has coached health care profes-
sionals, particularly during the COVID-19 pandemic, to reduce the negative impact of burnout. He’s also worked with successful professionals who are striving to achieve a better life balance. Many of them are midcareer, feeling disengaged and stressed, and realizing that their current work habits are unsustainable.
“They no longer feel fulfilled and may be contemplating a career change or questioning whether they are on the right path,” says Scott. “They seek guidance to restore balance and find a sense of purpose in their personal and professional lives.”
He knows from experience that positive psychology can help encourage professionals to reconnect with their true selves. “When you align with your personal wellness, even if the job isn’t the right fit, you can still improve your experience,” says Scott. “You can evaluate whether the job is something you still want or confirm that it’s time for a change. Focusing on your wellbeing allows you to make decisions with more clarity and greater confidence.”
Scott is also focused on addressing the youth mental health crisis through Positively Caviar, a grassroots nonprofit he launched to teach positive thinking and optimism to kids in underserved communities throughout Baltimore. Joan Wharton runs a mentorship program in conjunction with the Baltimore City Public Schools and partnered with Scott to lead a series of workshops for the girls at Cherry Hill Middle School.
“Chazz is very impressive and brought an energy that resonated with the girls,” says Wharton. “He met them where they were, and gradually helped raise them to another level. He taught them that the way they think shapes the way they act, and that what they feed their mind, soul, and spirit shows in their actions and attitudes.”
Scott’s workshops discussed personal growth and self-care. “His messaging focused on developing a positive mindset because the way the girls think can influence their behavior and the outcomes they experience,” says Wharton. “Having a positive mindset allows them to grow through empowerment and enlightenment and encourages them to build a strong foundation for
their future.” Weekly workshops aren’t going to solve the world’s problems, but Scott understands the importance of introducing tools to impressionable kids that help them cope with challenging situations. “My goal is to make sure they recognize that they have the agency to control what they think and feel,” he says. “It’s about giving them the ability to respond to their emotions in a healthy way.”
Interest in positive psychology is gaining traction among people who want to perform their best, regardless of their field or profession. But that doesn’t mean positivity can be pursued without consistent and intentional effort. Maximizing one’s potential demands daily focus and work.
“People rarely set aside the time and space in their lives to improve upon their strengths and virtues,” says Hunt. “Cultivating inner strengths and mental qualities that support happiness is something many of us long for and yet we often find ourselves racing toward the future, believing it holds some level of positivity that the present moment lacks.”
Even something as simple as jotting down three good things that happened throughout the day in a gratitude journal can be a powerful practice. Or you can practice “savoring,” which involves intentionally noticing and holding a positive experience in your awareness for 20 to 30 seconds, allowing yourself to fully absorb it. You might even visualize the positive feeling filling you.
The benefits of these practices have been studied extensively, according to Hunt, who says dedicating five to 10 minutes a day to them can be transformative over time.
Our brains naturally focus on the negative. Practices like gratitude, savoring, or acts of kindness help shift this bias, pulling us away from threat-focused thinking and into a mindset of greater positivity and altruism. Meditation and mindfulness, which encourage being fully present in the moment, reinforce these benefits. “What inspires me most is the universal application of positive psychology’s practices,” says Hunt. “We all strive for authentic happiness and fulfillment. At the end of the day, that’s at the core of what we want most in life.”

The Journey to Healing
The author, who survived street violence and prison with the help of therapy, makes the case for recognizing trauma in Baltimore and making counseling more accessible.
One day, I was sitting in my living room eating barbecue Pringles and working on my first book, a memoir of my life as a drug dealer, when a torrent of unexpected emotion rose up. I remember it like it was yesterday. I’d just started recounting the details of a shootout in broad daylight that I’d been involved in with a member of a rival crew decades earlier. As I wrote about the unnerving incident, it struck me, for the first time really, just how incredibly dangerous and reckless that situation had been. Years had passed since that day, but I had buried the memory until I started writing. Putting it on paper ripped open the scab on that old wound and revealed something I hadn’t thought much about.
Our brains have a way of pushing traumatic memories into the deep recesses of our minds, almost as if they never happened. But there I was with tears streaming down my face. Alone, struggling to maintain my composure, I was unsure why this old memory affected me so deeply. Then I realized I was distressed because I could have accidentally harmed an innocent child walking down the street that day—or I could have lost my own life.
After taking some time away from writing, I confided in a friend who worked in mental health services about what had happened. I also told her about my ongoing trouble sleeping and the nightmares. A short time later, I made an appointment with a therapist. That’s where the journey started for me, the journey toward healing.
For decades, I had ignored the traumatic incidents I experienced in the streets of Baltimore. Like when I was 16 years old, and a guy opened fire on me from just six feet away. I still don’t know how he missed but
TRAUMA BY KEVIN SHIRD
thank goodness he did. Or the time a teenage friend and I snuck into a nightclub to hear the tantalizing sounds of the early days of rap music, only to be traumatized when a man was shot and killed inside the club as we danced to the beat. Or the time I was hanging out in Druid Hill Park on a Sunday with some friends, and a man pulled out a handgun, placed it against another man’s head, and pulled the trigger.
Back then, as young men, we didn’t think much of incidents like these. In fact, we had normalized trauma, believing that we could just sleep it off and that it would be gone by morning. We never considered that witnessing these violent acts could affect our mental health decades later and that unresolved trauma could have a significant impact on our lives and decision-making ability. I never understood why I hated the sound of fireworks as a young man and would go out of my way to avoid New Year’s Eve and Fourth of July festivities that included fireworks.
Growing up in Baltimore, I experienced firsthand the challenges of systemic inequality, poverty, and the lure of the underground drug trade, as well as issues related to being the son of an alcoholic father.
These experiences led me into a life of crime, culminating in a federal prison sentence for drug trafficking. However, my incarceration marked a turning point, sparking a quest of self-reflection and redemption. While serving my sentence, I took college courses and began to reimagine my future, using education and personal growth as pathways to transformation.
Over the last 10 years I have authored several books that tackle complex social issues, often drawing from my own life to illuminate broader societal problems. A Life for a Life: Poor Choices and Unresolved Trauma Is Killing America (2025), which comes out this spring, is a true story that examines the intersection of trauma, mental health, and violence. It explores my relationship with
my former cellmate, Damion Neal, who tragically fell into violent crime after struggling with untreated mental health conditions. The book is both a personal reflection and a call to action to address systemic neglect of mental health and trauma. The Colored Waiting Room (2018), which was co-written with civil rights activist Nelson Malden, connects the legacy of the civil rights movement to
this role, I mentor students and continue my advocacy, hopefully inspiring the next generation of leaders and changemakers.
Healing is possible, and every Baltimore resident deserves a quality life.
contemporary struggles for racial and social justice. Uprising in the City (2016) focused on the death of Freddie Gray, the systemic inequalities faced by marginalized communities, and the steps necessary for meaningful rebuilding. My first book, the one that I was writing when the traumatic memory of the shoot-out leapt back into my conscious mind, was Lessons of Redemption (2014), which chronicled my transformation from a life of crime to becoming an advocate for justice and change.
My commitment to advocacy extends beyond writing. In 2014, I worked with the Obama Administration’s Clemency Initiative to address the inequities of the criminal justice system and advocate for fairer drug policies. I have also worked at the Johns Hopkins Center for Medical Humanities & Social Medicine to raise awareness around the public health crises in Baltimore and its effects on individuals and communities.
Currently, I serve as an instructor at Coppin State University, where I educate students about the links between social justice, criminal justice, and public health. Through
But the most significant area of my focus today is mental health. After being diagnosed with Post-Traumatic Stress Disorder (PTSD) as a result of my early life and incarceration, I have become a vocal advocate for mental health awareness. My work highlights the impact of unresolved trauma and the need for compassionate approaches to mental health care. I know firsthand the impacts of trauma and stigma on one’s decision-making and how it has hindered communities of color from seeking treatment and counseling. I want to help tear down those barriers.
My personal story of drug dealing, gun violence, and incarceration may sound dramatic to many, but scores of people in Baltimore are trying to heal from growing up and living in a continuous state of survival. Entire neighborhoods have been subjected to generational poverty due to racist policies, leading to traumas stemming from systemic barriers to education, health care, safe housing, and economic insecurity. These obstacles include underfunded schools, limited access to mental health services, food deserts, inadequate transportation, unaffordable housing, and restricted job opportunities. The COVID-19 pandemic exacerbated these vulnerabilities in communities already facing instability.
In the U.S., high rates of trauma and violence stem, in part, from a lack of coordination and commitment to mental health care. Locally, the homicide rate, though thankfully coming down, nonetheless remains at a very high level. The opioid epidemic in Baltimore City claims even more lives, nearly 6,000 over the past half a dozen years. Meanwhile, nearly one in four high school students across Baltimore seriously considered attempting suicide in the previous year, according to a recent Annie E. Casey Foundation study. And these are not issues that only impact Baltimore. Suicide is
the third leading cause of death for ages 1024 statewide in Maryland.
Inevitably, unresolved trauma becomes a major issue for youth affected by violence and opioid overdoses. Unlike physical wounds, psychological scars can persist indefinitely, often triggered by reminders of the past. These triggers vary widely, from loud noises and flashing lights to crowded spaces or even certain sights or smells. Addressing young people’s mental health needs requires a comprehensive approach that includes prevention and intervention, with therapy and counseling among the most effective tools to help them process experiences, develop coping skills, and gain control over their lives.
“When you live in fight-or-flight mode, it’s a daily reminder of the link between trauma and violence,” says Rev. Kim Lagree, CEO of Healing City Baltimore, a communitydriven organization that emphasizes trauma-informed practices and fosters compassion. One of Healing City Baltimore’s core beliefs is that addressing systemic racism is essential to treating today’s traumas. “A lot of homicides and opioid overdoses are rooted in people hurting and trying to cope. Our youth and communities face challenges with depression and anxiety, and often lack access to quality, culturally relevant services, [which are] typically designed by people who don’t look like those they serve.”
The good news is that Baltimore, with the Healing City initiative headed by Lagree, and Maryland, more broadly, have come to the forefront nationally as leaders in addressing long-ignored issues around trauma and its consequences.
In 2020, then-Mayor Jack Young signed the Elijah Cummings Healing City Act, an initiative pushed by now-City Council President Zeke Cohen, requiring that Baltimore City agencies eliminate policies that cause trauma to citizens and provide traumainformed training to all public-facing staff. In 2021, lawmakers in Annapolis passed the
Healing Maryland Trauma Act, sponsored by Baltimore State Senator Jill Carter and Delegate Robynn Lewis.
Lagree emphasizes that healing is possible, and that every Baltimore resident deserves a quality life. “An Ubuntu quote resonates with me: ‘I am because we are.’ It perfectly captures our belief that ‘if I am not free, then neither are you,’ and vice versa.”
One of Healing City Baltimore’s roles is serving as a hub for collaborators and mental health change agents. They assist organizations in developing solutions and strategies for communities that need access to quality, culturally relevant services.
“We elevate lived experiences as expertise and embrace the voices of youth and community leaders,” Lagree says. “Organizations like We Are Us, which connects directly with men in the streets, and Heart Smiles, a youth-led group training hundreds in trauma-informed care, are making a difference,” she adds.
Research shows that men, in particular, struggle to discuss mental health issues due to societal expectations and stigma. Men are often socialized to express emotions through actions rather than words—I’m no exception here—reinforcing norms of selfreliance and stoicism. Fear of judgment, limited role models who discuss mental health openly, and cultural stigma can make men reluctant to seek help. These factors often prevent them from addressing mental health needs until they become overwhelming.
During my time in prison, I had participated in a reentry program that addressed every issue imaginable, from criminal behavior to gambling and drug and alcohol addiction. The program leaders were strict: If you didn’t speak up and actively participate, you’d be kicked out, which could potentially impact your release date. After my release, I knew I needed to continue working on myself. So, when opportunities for therapy came up, I didn’t hesitate, though finding the right therapist proved to be a challenge.
As I talked with Lagree about the impact of unresolved trauma and recalled some of
my story, she shared what she went through growing up in Edmondson Village and how it informs her understanding today. Raised in a predominantly female-led family, Lagree witnessed the impacts of trauma firsthand. Her grandfather, a combat veteran, returned home with severe mental health issues and eventually became homeless. “He struggled with alcohol addiction and left home before I was born, when my mom was still in middle school,” Lagree says. “We couldn’t locate him for decades, leaving my grandmother to raise the family on her own. She was deeply religious and took me to church with her seven days a week. Despite our challenges, her resilience and faith provided a foundation for our family’s healing.”
Trauma affected multiple generations in Lagree’s family. “My mother and biological father both experienced addiction,” she continues. “My mom would disappear for days— or even months. Years later, when we had the chance to rebuild our relationship, the Black community still wasn’t openly discussing mental health. Growing up, it was expected that we handle family issues privately. For years, I experienced the emotional death of my mother countless times from age five to 20. Filing more than 30 missing persons reports alongside my grandmother had a significant mental impact.”
Along with speaking with Lagree about Healing City Baltimore and efforts to address trauma in the city, I also wanted to talk with Rev. Donte Hickman, whom I’ve actually known since our teenage years. One of the most respected faith and community leaders in the city, he offers a unique perspective on community healing from trauma, which includes having to rebuild a neighborhood senior housing complex that was under construction and destroyed in the Uprising after the death of Freddie Gray. Also, a Baltimore native, he has led the Southern Baptist Church on the east side of town for two decades. A pastor, he nonetheless believes that spirituality and religion should not be the sole tools for healing. He has long talked about the impact of trauma among city residents, youth
Hickman acknowledges that while Baltimore is making economic and infrastructure strides ... people and communities still grapple with trauma ... failure to adequately address these mental health needs will not just hold individuals back but hold the city back as well.
in particular, and the deep need for accessible mental health in Baltimore. “Spirituality should enhance social awareness, not blind us to reality,” he explains. “Some use it to block out real threats [to mental health].”
Hickman acknowledges that while Baltimore is making economic and infrastructure strides with redevelopment underway in many parts of the city, people and communities still grapple with trauma. Ex-offenders, for example, he says, face enormous challenges to healing when they return, and it can be difficult for them to navigate life outside of prison. Failure to adequately address these mental health needs will not just hold individuals back but hold the city back as well, he adds. “Healing can be misunderstood; spirituality is often misused, becoming a shield against pain,” Hickman says. “Karl Marx said, ‘religion is the opiate of the masses.’ Similarly, spirituality can insulate us from violence and trauma, giving a false sense of [physical and psychological] security.”
He believes true healing requires intentional effort. “We must first acknowledge what’s wrong, rather than using spirituality to avoid it. Instead, it should encourage us to confront our realities.”
The mental health impact of violence is profound in the neighborhoods around his church, especially among young people, leading to anxiety, depression, and PTSD. Children shouldn’t live in fear at school, worried about what’s around the corner, Hickman continues. “This contradicts the teachings of Jesus, who said, ‘I came that
they may have life, and have it abundantly.’”
In 2021, Hickman and his congregation faced the personal impact of random community violence when Evelyn Player, a church volunteer, was found dead in the church restroom. Hickman arrived to find police tape surrounding the church, shocked to learn she had been murdered. “I thought, ‘Who would stab a woman in a church?’ It made me realize that not everyone views the church as a sacred space,” he reflects.
After the tragedy, Hickman addressed the congregation about the complicated feeling of being protected by God in such a moment and organized a prayer vigil to honor Player and unite the community in the grieving and healing process. This collective spirit has been evident during past violence, such as the 2015 riots following Freddie Gray’s death. “We went door to door and engaged with seniors to understand their experiences,” he recalls.
The day of Player’s murder was no different. Hickman wanted to bring the community together to affirm their faith and support one another. Gov. Wes Moore, then a church member, attended the vigil, emphasizing the importance of community in the healing process.
Tragedies, such as the murder of a beloved community member like Evelyn Player or the death of an innocent man in police custody, as in the case of Freddie Gray, do have the potential to unite people across boundaries, fostering a shared determination to heal.
For long-overdue healing in Baltimore to occur, the community must show up
for each other, transcending both real and imagined divides, Hickman says. But there must still be broad and affordable access to mental health care as well. “If we ignore the needs of the least and most vulnerable in our communities,” Hickman says, “we will feel the repercussions in all neighborhoods.”
I also know firsthand the impact of trauma and stigma on one’s decision-making and how it has all too often hindered communities of color from seeking treatment and counseling. I want to help tear down those barriers and help communities return to being well again, but it’s also important that if I don’t take care of myself, I won’t be of much service to others.
A therapist once told me I had something called the “Superman Syndrome” or “Superman Complex.” It’s an unhealthy sense of responsibility rooted in the belief that others are incapable of handling even simple tasks on their own. Those with this complex—or its counterpart, Superwoman Syndrome—often see themselves as invincible and incapable of failure. They’re driven by an intense need to fix everyone around them, all while believing they have no issues of their own. She described me to a ‘T’ and that was the day that I started to pay more attention to my own emotions and my own feelings—and take on the problems of others as if they were my own.
At the same time, while writing my first book, Lessons of Redemption, I worried about how people might perceive my story. Gregory Kane, a former columnist for The Baltimore Sun, gave me invaluable advice: “Don’t worry about those fools. Just be honest in your writing.” Which is also good advice for life. I’ll never forget when he said, “Write until your hand falls off, and if it does, learn to write with the other hand.”
At the time, Kane was battling cancer, and his resilience inspired me. If he could fight that battle, I could certainly put words down on paper. Those moments, combined with my conviction to always rise to the occasion when it mattered, played a major role in shaping my journey.
Life
B y CHRISTIANNA MCCAUSLAND
line
WHAT’S BEHIND THE NEARLY 50,000 DEATHS BY SUICIDE IN THE UNITED STATES AND HOW CAN THEY BE PREVENTED?
For much of her 17 years of life, Kristin Rita Strouse was an average kid with an extraordinary gift as an artist. In fact, she’d taken courses at Maryland Institute College of Art (MICA) since she was 12. But in Kristin’s senior year of high school, as she got ready to fulfill her dream of attending art school, her family noticed a change.
“[Kristin] was putting her portfolio together and she was having a hard time doing that,” explains her mother, Sharon Strouse. “As I look back, I can see that something started to unravel.”
In December 2000, Kristin was arrested for shoplifting, which was completely out of character for her and something she could not explain. By January, she was becoming aggressive, though she would also have periods of complete normalcy. Strouse, a licensed art therapist, knew something was wrong. The family took Kristin to a hospital where she was treated for depression and released. (In retrospect, Strouse believes
Kristin, who was having clear manic episodes, may have been misdiagnosed.)
“She started mentioning suicide, but we were told, ‘Don’t pay any attention to that, she’ll never do that,’” says Strouse. “We were told she was just acting out.”
That summer, a calm settled over Kristin. And by fall of 2001, she was attending The Parsons School of Design in New York City. Her parents made sure she had a psychiatrist in the city whom she was seeing regularly. But after the events of 9/11, Kristin’s struggles grew.
She called her mom and told her she wasn’t doing well. “In my head, I heard that social worker saying, ‘Don’t pay attention to that. She’ll never hurt herself,’” recalls Strouse. “I listened to what the experts were telling me instead of acting how I know I should have acted, which was to get in the car, drive up there, and get her home.’”
That night, October 11, Kristin died by suicide. She was just a few weeks from her 18th birthday.
While understanding of both mental illness and suicide risk awareness has improved since Kristin’s death, it has not helped stem the rising tide of suicides. The Centers for Disease Control and Prevention (CDC) now ranks suicide as a leading cause of death in the United States, with one death occurring every 11 minutes. Suicide rates have been increasing for several decades, rising 37 percent between 2000 and 2018, decreasing slightly, then returning to their peak in 2022.
In 2022 there were 1.6 million suicide attempts and just under 50,000 deaths—608 in Maryland alone. Easy access to firearms is making attempts more deadly, with roughly 27,000 of those 50,000 lives taken by a gun. Historically, women were believed to attempt suicide more often than men, though men were more likely to die due to their use of a firearm. Now those numbers are evening out because everyone has easy access to this lethal means.
Perhaps most alarming, the CDC cites that for youth ages 10 to 14, suicide is the second leading cause of death after car accidents. Nearly a quarter of all high school students say they have seriously considered attempting suicide. Research by Johns Hopkins Medicine reports that guns are used in more than half of youth suicides.
“Believe they can and will do it,” says Strouse, if someone you know expresses suicidal thoughts. “If you don’t feel like they’re getting proper treatment, see someone else. Don’t be afraid to go to the school counselor, the pediatrician, a psychiatrist, or psychologist. Don’t be afraid to go to the emergency room. If your gut is saying go— go. Get help.”
Understanding why the suicide rate is rising in the United States is complicated. According to Todd Peters, MD, vice president and chief medical officer at Sheppard Pratt, “This has really been a very difficult last half decade, between the estrangement that people felt during COVID, the disruption in their day-to-day lives, especially for teens, and we know that there’s just a lot of unrest out there in the world, so things like anxiety, depression, and PTSD continue to rise.”
And while social media has its benefits as a place where some people find connection and self-expression, Peters notes it is also a place where bullying can take place 24/7 and one can find nonstop exposure to all the ills of the world. Not to mention the ability to constantly compare and despair while consuming perfectly curated lives online. Research indicates that social media overuse may be linked to increased rates of depression.
But the leading risk factor for suicide is a mental health condition. Jennifer Murphy, area director of the Maryland and Delaware chapters of the American Foundation for Suicide Prevention (AFSP), says an estimated 90 percent of people who died by suicide had a mental health condition—like bipolar disorder or clinical depression—that may or may not have been recognized, diagnosed, or adequately treated. “That said,” she states, “research has also made clear that mental health conditions are not the whole story. One in four people will experience a mental health condition, and most do not go on to die by suicide.”
Murphy outlines other factors, alone or coupled with mental illness, that could put a person at risk for suicide, including a family history of suicide or mental illness; physical health problems and chronic pain; traumatic brain injury; and adverse childhood experiences, including growing up witnessing or experiencing violence, abuse, or neglect, or loss of a family member through divorce, death, or prison. There’s a growing area of research looking specifically at the trickle-down impact the large death toll and family disruption of the opioid epidemic is having on suicide rates, as well as access to deadly fentanyl.
Peters agrees that a mental illness alone is not an indicator, but rather a factor that can destabilize an already-vulnerable person. “When people get to a very low point, when they’re feeling significant emotional pain, they’re feeling really hopeless, they’re feeling really helpless, this can distort their reality and their perception. Coupled with things like social isolation, that opens up the door for suicidal thoughts to creep in.”
OVER 49,000
PEOPLE DIED BY SUICIDE IN 2022
UNDERSTANDING WHY THE SUICIDE RATE IS RISING IN THE UNITED STATES IS COMPLICATED.
All mental health professionals will tell you: If you or someone you know is having suicidal thoughts, get help immediately. (Anyone can call the 988 crisis hotline for help 24/7.) But access to help outside of urgent care can be difficult to find. There are shortages of counselors, psychiatrists, and psychologists—and wait-lists to see a provider are common. Some schools lack a counselor or have too few. Inability to pay for services is another barrier to care. Emergency rooms are overcrowded.
Clinicians have come a long way in their ability to identify and assess someone at risk for suicide. The use of AI-based modeling will further refine that ability. Urgent care centers, like the one at Sheppard Pratt, and crisis hotlines like 988 have gone a long way to bringing care to those who are standing at the precipice. But, says Peters, the question is how to manage people before they get to a crisis point—perhaps through better training for primary care doctors and pediatricians—and then over their lifespan so they don’t get stuck somewhere in the system or fall through its cracks. Assessing that someone is at risk for suicide is simply not enough.
“There still are so many people that just don’t get care,” says Peters. “We would never accept that only 50 percent of people with cancer get treatment, yet here we are in the behavioral health space, recognizing that a significant number of people that have a major mental illness will probably not get care in a timely way—some people wait five to 10 years to get help after their first onset of symptoms.
“While I have a lot of hope and feel very proud to be a psychiatrist working in the behavioral health space,” Peters continues, “we have much more work to do to actually move the needle in getting people better.”
Holly Wilcox, PhD, a mental health researcher and professor at the Johns Hopkins Bloomberg School of Public Health, sees this borne out in her work. “We have data that shows most people who die by suicide do not see a mental health professional before they die,” says Wilcox, who is also
director of Hopkins’ Center for Suicide Prevention, the first of its kind in a school of public health. Wilcox explains that suicide is not just a medical problem, it is a public health issue, one that could be better managed with a systemic approach.
“Part of the problem we see in this field is that we know what works but most people will never get these interventions,” she says. “In an ideal world, everyone in our state would be trained on dialectical therapy, behavioral therapy, and cognitive behavioral therapy, and they would know how to deliver these therapies with high fidelity, quality implementation. Every school, the juvenile justice system, jails—all would have these interventions that we know work so there would be a strong safety net.”
The good news, says Wilcox, is you don’t need a host of skilled psychologists to handle this problem. “People who may not have a PhD or an MD or a lot of initials after their name, but who may have had lived experience or just the right skill set [can] fill the care coordination gap,” she says.
Looking at how to get community health workers trained, into the spaces where they are most needed, and coordinate payment for services through Medicaid is something Wilcox hopes will be taken up in the coming legislative session in Maryland.
For those who are known to be at risk of suicide, a safety plan can be lifesaving. According to the Suicide Prevention Resource Center, a safety plan is a succinct list of coping strategies and supports, written by the at-risk individual, that can be used by that person when they feel a crisis coming on. If someone is concerned that a friend or loved one is in crisis, one of the more effective ways to help prevent a suicide is also the easiest: Talk about it.
The idea that asking someone at risk if they are considering suicide will encour-
FOR YOUTH AGES 10 to 14
SUICIDE IS THE SECOND LEADING CAUSE OF DEATH
BOYS ARE 4x more
LIKELY TO DIE FROM SUICIDE THAN GIRLS
GIRLS ARE MORE likely TO ATTEMPT SUICIDE THAN BOYS
4 in 10
LGBTQ+ STUDENTS SERIOUSLY CONSIDERED ATTEMPTING SUICIDE
MOST PEOPLE WHO DIE BY SUICIDE DO NOT SEE A MENTAL HEALTH PROFESSIONAL BEFORE THEY DIE.
age them to do so has been debunked. “Research shows that it really doesn’t ‘plant’ the idea,” says Wilcox. “It’s more likely that the person, when they receive that question, feels relieved that somebody cares enough to ask.”
Three Warning Signs
Jennifer Murphy, area director, Maryland and Delaware Chapters of the American Foundation for Suicide Prevention, says to think about warning signs in three categories:
TALK
This includes expressing hopelessness, no reason to live, being a burden to others, and comments about ending their lives.
BEHAVIOR
Increased use of alcohol or drugs, withdrawing from activities, and acting recklessly. Also, a person may give away possessions. Teens may withdraw from peers.
MOOD
Moods can vary from depression, irritability, anxiety, and impulsivity. Sudden, unexplained upbeat mood during a period of depression can indicate the individual has decided on a plan and is relieved they will no longer be in pain.
The next step is compassionate, nonjudgemental listening without trying to “fix” the person’s situation. “Sometimes people are afraid to ask and start the conversation, and they tiptoe around it,” says Peters. “Starting that conversation is a really key first step and then trying to listen and not come up with answers or suppositions.”
Finally, make sure to connect the person to professional resources.
Nowhere are these conversations more important than with young people. Karen Swartz, MD, is the Myra S. Meyer Professor in Mood Disorders at Johns Hopkins Medicine and the founder and director of the Adolescent Depression Awareness Program (ADAP). Swartz explains that ADAP’s roots can be traced to the late 1990s, when there was a string of deaths by suicide at a cluster of Baltimore schools. As a mood disorders specialist, she was asked to speak to parents.
“That was a really striking experience for me, because these were parents who clearly wanted to understand, wanted to protect their children, but they had no understanding or knowledge about mood disorders,” she says.
ADAP was the response to this need. A community education program, it focuses on bringing high quality information about depression to high school students, their parents, and teachers so they understand that depression is a treatable medical illness. Over 25 years, the program has reached more than 140,000 students.
One of the central teaching points of ADAP is that if someone is having suicidal thoughts, it’s an emergency to be taken seriously. But, says Swartz, “There’s a challenge with teens, of course, because they want to become more independent. We’ve all heard these stories where someone wasn’t go-
ing to therapy, but was talking to her best friend, and maybe that was a tremendously supportive person, and those conversations were helpful, and for a brief period of time the person felt better because they felt supported, but that’s not going to do anything to address the underlying medical issue of depression, bipolar disorder, severe anxiety, PTSD—the kinds of conditions that would put someone at risk [of suicide].”
A key tenant of the ADAP program is that students leave having made a list of five adults they can speak to if they or someone they know needs help. The program is short, just three hours, yet a study evaluating the program’s effectiveness found that 46 percent of faculty who have led the program say at least one student has come to them with a concern for themself or a friend in the wake of ADAP programming.
Swartz says better access to early diagnosis and evidence-based treatment for youths with mental illness is critical to helping those who are at risk.
“I’ve talked to lots of parent groups after a young person has died, and what I hear repeatedly is the parents in the community trying to come up with an explanation to make sense of what happened,” says Swartz. “The idea that the person had a very serious illness that could cause them to have suicidal thoughts is terrifying. So we all prefer to focus on the story of, ‘Don’t you think it was the breakup?’ or, ‘Do you think it has something to do with the bad grade on that test?’”
These are legitimate challenges all kids go through in adolescence, Swartz notes. But parents must identify if their child has the ability to deal with those challenges at the time they’re happening. “What happens with certain psychiatric conditions is your reactivity and impulsivity increase, so your response to something like a breakup is disproportionately intense,” she explains. “Your response might be severe, like saying, ‘I don’t see the point of being alive,’ whereas if you’re feeling well, you’d have a very different response.”
This is why Swartz underscores that an adolescent talking about suicide must always be taken seriously. Some of the classic red flags that someone is in a crisis—irritability,
mood swings, increased used of substances—can be harder to read with teens. Swartz says to pay attention if a young person is irritable with teachers and peers (not just their parents) and particularly if the person withdraws from friends. “When teenagers don’t want to do things with their friends, that’s really concerning, because that’s their main focus, their social life,” she says.
Awareness programs like ADAP are an important step in suicide prevention. AFSP also has a program called “Talk Saves Lives,” that reviews warning signs, risk factors, and strategies for suicide prevention. That program was presented in 40 diverse settings in 2023, reaching over 1,600 Marylanders. Swartz says if we want to work to prevent deaths, we also need to look at how suicide and violence is glorified in media, as a person with a mental illness may have a different reaction to that violence than someone without. But perhaps the most straightforward way to prevent a suicide is to remove lethal means from an at-risk person.
AFPS notes on its website that, “most people in suicidal crisis who don’t have easy access to a lethal suicide method will not simply find another way to kill themselves.” Safe storage of firearms in particular, as well as gun control, are a large part of this conversation. The organization states that 56 percent of deaths by suicide in the U.S. use a firearm and 90 percent of suicide attempts with a firearm are fatal.
“If you have a [suicidal] thought and you can immediately access a way that you will die, that’s very different than having that thought and then thinking about what you would do,” Swartz says. “And then in that maybe half an hour that you’re trying to figure out what you might do, your brother comes home, or your best friend calls you, or your mom sends you a text. Those kinds of delays can make a big difference.”
When someone dies by suicide, they leave behind survivors who must deal with their own unimaginable grief, a kind of sorrow that is fused with guilt and shame. Sharon Strouse remembers the dark days after her daughter’s death: the parents who didn’t want to get
too close because having a child who dies by suicide is “like a contagion,” and others who told her Kristin would go to hell.
“It’s very different than losing a child who had kidney failure, or a child that was in an accident,” says Strouse. “People look at you like, ‘What did you do wrong?’”
Although trained in art therapy, Strouse was unable to help herself in the aftermath of Kristin’s death and she found conventional talk therapy inadequate. She remembers being in a hopeless place in December of 2002, when a voice in her head said, “Go make a collage.” Strouse heeded that voice, went into the basement and got out Kristin’s art supplies. She proceeded to spend three hours making a collage. That night she slept soundly for the first time in a year. Now she believes that voice in her head was Kristin’s.
The artworks she made that day and in the days that followed are brutal, beautiful, and raw. Through it, Strouse dealt with things she says were unspeakable, even in talk therapy—the vision of her daughter’s body, her own guilt, and the weight of societal shame. Today, she operates a private practice in that same basement that focuses on using art and meditation for healing grief and bereavement and is associate director at the Portland Institute for Loss and Transition. She wrote a memoir, Artful Grief: A Diary of Healing, and conducts numerous art therapy workshops all over the country teaching professionals as well as survivors. The Strouse family turned the tragedy of Kristin’s death into action, creating the Kristin Rita Strouse Foundation to raise funds for suicide prevention. One of the programs they support is ADAP.
Strouse says the recovery from losing someone to suicide takes deep healing over many years. That healing is ongoing; it’s never done. Now, their family is, she says, able to have joyful holidays and happy times. The Strouses’ eldest daughter is soon to be married and their son has given them two grandchildren. “The heartache has gone,” says Strouse, “but Kristin is always with me in the work I do.”

Sharon Strouse, who lost her daughter to suicide, finds healing for herself and others through her art therapy practice.








SEVEN BALTIMOREANS SPEAK OUT ABOUT HOW MENTAL ILLNESS HAS TOUCHED THEIR LIVES.
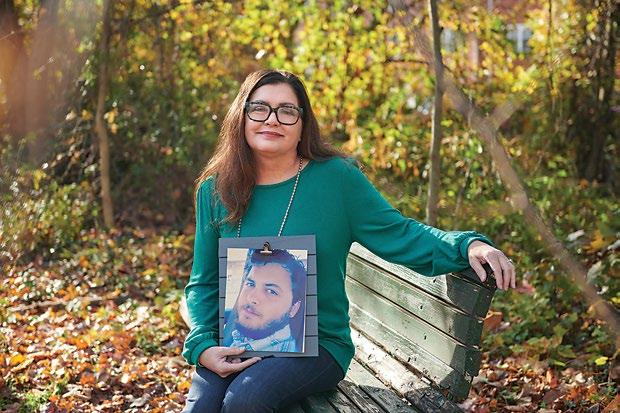
Mental Health the faces of
ACCORDING TO THE National Alliance on Mental Health, one in five adult Americans experiences a mental illness each year. In Maryland, 781,000 people live with a mental health condition and an additional 39 percent of adults in the state report feelings of depression and anxiety, a number that rose after the COVID-19 pandemic. While conversation about mental health has dramatically improved in recent years, stigma remains. Many of those affected suffer in silence and anonymity due to shame, discrimination, and lack of appropriate or accessible care.
Only by looking at those impacted by mental illness and hearing their stories can we, as a community, help heal by seeing it for what it is—an illness that requires treatment so people can live their fullest lives.
On the following pages, we offer the stories of seven individuals in our region who have been touched by mental illness, either their own or through that of a loved one. These are teachers and students, coworkers and parents, writers and activists. They are portraits of what the face of mental health looks like in Maryland today, and they paint a picture of struggle, strength, resilience, and hope.
WRITTEN BY JANE MARION, CHRISTIANNA MCCAUSLAND, AND MAX WEISS
PHOTOGRAPHY BY
JOANNA TILLMAN


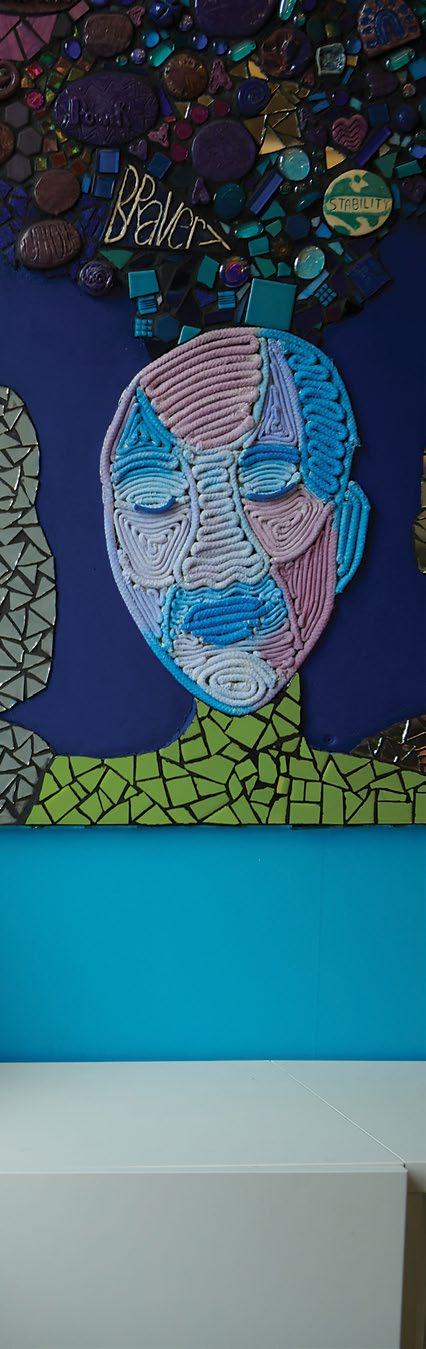

Charita Cole Brown
Author. Mental health advocate. Living with bipolar disorder.
RIGHT AFTER MY 21ST BIRTHDAY, as a student at Wesleyan University, I was diagnosed with bipolar I disorder. My thoughts raced like a ticker tape from the time I woke up until I went to sleep at night. I was thinking, thinking, and the thoughts got faster and faster. During one period of mania, as I trekked outdoors, I believed I was following Harriet Tubman’s tracks on the Underground Railroad. Though depression was horrible and hard, it didn’t scare me. Mania terrified me.
In 1982, my parents took me to see a therapist following a psychotic break. We were told that given the severity and frequency of my episodes, they were looking at a daughter who could eventually need custodial care. Up until that point, everything in my life was about academic achievement. I didn’t have to be pretty or best dressed. Those things didn’t matter to me because I was smart. When I got that news, what I heard was that I was not smart anymore—it was a death knell for me. At this point, I began self-shaming. I didn’t realize the level of shame I was carrying until I wrote my memoir, Defying the Verdict: My Bipolar Life, in 2015. I was ashamed that I was living with an illness I couldn’t control. Black women are expected to “take it on the chin,” in line with the Mammy stereotype. You take care of your kids, her kids, all the kids. You cook, clean, and do all the household chores, and all the while you are smiling—that is society’s expectation.
I am not ashamed anymore since my story became public. The book title was extracted from a quote by writer Norman Cousins. He wrote about cancer, “Don’t defy the diagnosis, try to defy the verdict.” When I read that quote, I thought, “I love this—my life is about defying the verdict.”
I am glad that I am no longer holding my story inside. Someone else can read my book and meet a 21-year-old woman who didn’t know what her quality of life would be—and then they can see this 65-year-old woman who was able to marry and have two children, against doctors’ predictions. I created and managed assisted living-style care for my parents that allowed them to live out their lives in their own home. I have been episode-free for about 30 years. By grace, I am thriving with a serious mental illness diagnosis.
Mary Saha
Mother. Teacher. Author. Living with bipolar disorder.
I WAS FIRST DIAGNOSED WITH major depressive disorder as a sophomore in college. Two years later, a prescription interaction created a manic episode, changing my diagnosis to bipolar disorder. When I was first diagnosed, I was so consumed by shame that I wished my cognitive symptoms were a manifestation of a physical health problem—even if it was life threatening. At the time [the 1990s], many people questioned the abilities of people experiencing mental health conditions. The terms used to describe us were “mentally ill” and “crazy.” After time spent managing major depressive disorder with prescriptions and therapy, I enrolled in community college, studied journalism, and earned an associate degree. Earning that degree proved I could live independently despite my diagnosis, which chipped away at my shame. The more I accomplished, the less shame I felt. When I was diagnosed with bipolar disorder, the shame returned but felt stronger. It’s one thing to tell people you’re depressed and quite another thing to share that you have bipolar disorder. Again, after achieving more goals (college, career, graduate degree), the shame weakened. I could contribute to society in

a meaningful way, something I thought I would never do when first diagnosed.
I went into teaching because I had the desire to do something important. Teaching our future community members to suspend judgment, think critically, and effectively advocate for themselves (and others) was an honor. When students know you genuinely care about them, teaching is quite easy, so it helped me be successful.
I’m currently writing a young adult book about the journey of a high school student experiencing the onset of a mental health condition. It is not a memoir, but I’m hoping my experiences help me write a piece that effectively normalizes the experience and reduces the stigma surrounding mental health. Have I seen the stigma around mental health change? Yes! Improve? Sort of. As a society, we discuss it and address it more. But there are people who don’t think mental health conditions are legitimate or think that they are easy to manage. And it can be easy to only see symptoms and be scared of, or for, your loved one. My hope is we all do a better job of seeing people with mental health conditions first and foremost as people.


Abner Palencia

I GREW UP IN MONTGOMERY COUNTY. I was poor, a kid of immigrants. I had a bad family situation. Put that together with being a minority and I ran away and joined the Army after just starting community college. Here’s a recruiter offering me a signing bonus and your brain thinks, “I have a golden ticket out of this situation.” I’d had various diagnoses, but never had a good sense of what was wrong with me. [In the Army,] I was a mess. I was drinking and cheating and there was the stress of trying to send money home. They told me I had depression and gave me pills that somewhat stabilized me, but I left the military after two years and I was still drinking. I ended up in my first psych ward in Philly in 2020. There I went to a NA meeting and realized I might have a problem. When I transferred to VA halfway housing, I went to AA. I was homeless for a time. I’ve often had to couch surf. I’m currently about to get evicted because
the VA Section 8 process takes time. The hardest part of [living with mental illness] is lack of resources like TALMAR. TALMAR [a therapeutic farm that runs the Veterans Affairs Farming and Recovery Mental Health Services program] was recommended to me by the VA counselor downtown. She asked if I liked nature and I said, “No way. I came to the city for a reason.” I had to choose between that or cooking and cleaning at the hospital and I didn’t think I needed to be around a lot of emotionally disturbed veterans with addiction. She told me, “It’ll be good for you.” She probably saved my life. Being here makes you human again. You’re forced to face your emotions, like you see the change of seasons and maybe that makes you confront a moment when you lost someone. This is the real America here. This land. It was here before us and hopefully it will be here after we’re gone. As a person, as a soldier, as a human, I feel safe here.
Aruna Miller
Lieutenant governor. Mental health advocate.
THE ONLY DAD I EVER KNEW is the one who came with bipolar illness. I just assumed that’s how all fathers are. My dad would have periods of euphoria where he was high on life. He was articulate and warm and loving and gregarious. Then, he’d have moments of depression where he’d go to bed and didn’t communicate with anyone. He was an engineer who worked for IBM. I remember many occasions where he’d have to go to work, but he couldn’t get himself to go. My mother didn’t know how to speak English all that well, so she would have me call up his employer to say, “My dad isn’t feeling good, he’s not coming to work.” I was probably 11 years old at the time.
As immigrants you don’t talk about it. As children we thought this is just the way everyone acts. When I was a senior in high school, my dad got a job in San Jose, California, and we were going to move from Missouri, but his vice was gambling and he flew to Las Vegas on his way to work one day and for a month no one knew where he was. That was the end of it—they fired him.
When his illness finally came to the surface, I was running for office in 2018 for a congressional seat. I would often, as part of my stump speech, talk about how my father suffered from an illness and I relied on Pell grants to get through college and how, because of that, it led to my journey to be in public service. A media person came up to me and said, “What’s the illness your dad suffered from?” And I said, “It’s just an illness.” He said, “Is it a physical illness or something else?” I said, “I really don’t want to talk about it,” and he said, “Well, maybe you should.” And then I told him, and he said, “You need to tell that story more often because when you do, people will connect with you and they will share their own stories.” I didn’t want to exploit my dad and what he went through as part of a campaign stump speech. I really struggled with that for a while. I thought, “That guy doesn’t know what he’s talking about.” And then, for whatever reason, I shared it several months down the line. Sure enough, people came out of the woodwork in tears and start talking to me.
It isn’t your résumé and all your titles and all that you’ve achieved in life that make people feel connected to you, it’s your vulnerabilities—that’s how you become an authentic person. So, the question we need to ask ourselves is, do we keep that pain to ourselves and just hide it away and go to the grave like that or do we take that pain and try to find light in darkness for other people? I am going to take my vulnerabilities and try to make life a little bit better for people who have been through what I have been through.




Laura Pogliano
Mental health advocate. Educator. Grieving mom.

LOSING ZACCARIA TO SCHIZOPHRENIA was extremely difficult. He was so drastically changed. Some days you see glimmers of your child back, then they have more psychosis and you lose them. Then they are well for a while, then they get sick and you lose them again. It’s literally endless grieving. I did so much crying the first three or four years of his illness that by the time he passed away from heart failure from complications of the disease and the police walked up my steps to tell me that I had lost him, I almost had no reaction. I had had a long, long goodbye. I had already been working with parents doing some advocacy work and when he passed away there was this sense

of, “Now what do I do with the worry and all the work that had gone into caring for him?” I could walk away and say I did my part by taking good care of my own child, but after about a two-week period I realized he doesn’t have to be here for this to be important.
A lot of people with serious mental illness don’t have a voice in the game because they are too sick. I say to myself, “My son couldn’t help families advocate for better services and better laws or help people find good treatment or bring people to Johns Hopkins for a schizophrenia symposium every year. He couldn’t do those things—but I can.”

Trace Terrell
Student, Johns Hopkins University. Mental health advocate.
Living with depression and anxiety.
GROWING UP IN A RURAL COMMUNITY—La Pine, Oregon— was challenging. I began to experience loneliness and isolation in elementary school when I was bullied by other students for my weight, my voice, my personality. By the fifth grade, I realized I was gay, and by age 14, I experienced severe depression, social anxiety, and disordered eating. Nearly every night in middle school, I lay in bed and wished to wake up straight. I thought that if I was “normal,” my problems would vanish.
People in my community didn’t believe that mental health was as important as physical health and whenever the topic was brought up, it was immediately dismissed as simply a “phase.” And whenever I cried or expressed emotion, I was told to “man up” or “get over it” by the men in my life.
Even now, I don’t have a clear answer for why I showed up that day during lunch at school to learn about a volunteer opportunity with a teen-to-teen suicide prevention and mental health crisis hotline. I think it was because I was bored and uninterested in my life and wanted a way to distract myself—a common sign among those considering suicide.

I didn’t realize the impact it would have, but that experience ultimately transformed my life. Each shift, I talked to young people who struggled deeply yet still found the courage to ask for help, which later inspired me to ask my parents if I could see a mental health professional. I truly believe that the peer support I received while volunteering on the hotline saved my life.
Today, I volunteer for the local chapter of NAMI [National Alliance on Mental Illness] and work as an on-campus Peer Health Educator for the PEEP [Preventative Education and Empowerment for Peers]. I am also the founder and president of Active Minds at Johns Hopkins University, which educates and advocates to create better mental health policies on campus. Fortunately, I think we are having more conversations about mental health than ever before. My mental health has never been better. I am surrounded by friends and family who truly understand me and by passionate advocates.
I also feel that I have turned my pain into purpose and action. My goal in life is to ensure no other 12- or 14-year-old feels the same way that I did growing up.
Michael Imai
Research assistant, Kennedy Krieger Institute. Living with depression.
I GREW UP IN SOUTHERN CALIFORNIA in a very supportive, very mentalhealth-aware family, mainly because my mom has major depression, just like I do. And then in 2012, my grandmother passed away very suddenly, and that led my dad into a kind of PTSD-type mental health crisis that lasted for a few years. I don’t want to say that was the thing that sparked my own depression, but it certainly was a contributing factor.
What’s funny is, what I remember most about that time was how it brought my family closer together. I always say that my family is bonded by all of us having things wrong with us simultaneously. It’s not something that is shamed. The family understanding is: Life is hard and it can be stressful and sad sometimes, and we can talk through that and that’s normal.
My depression got worse when I went to UCLA. I have always been a high achiever—and I was constantly blaming myself for having depression, thinking I was lazy.
My mom is my hero. She would always say, ‘If you ever feel like you need to go to the hospital, it’s fine. We’ll pay for anything if your insurance doesn’t cover it.’
The first time I experienced suicidal ideation, I remember the stress and expectations of getting into med school just got to me, and having thoughts of, “Nothing in this world matters, I don’t really matter.” It’s not like I was looking for something to hurt myself, but I kept thinking there’s knives in the kitchen, and I actually kind of had a panic attack, ran into the shower, and just stayed there for an hour because I was so afraid of finding something to hurt myself with. Eventually those thoughts became so pervasive and scary that I walked over to the ER, and told them, I’m having suicidal thoughts, and I’d just like to stay here for my own safety.
[Suicidal ideation] happened twice in my life, and I hope it never happens again, but I know if it does, I can say, “Wait, wait, hold on, your brain is short-circuiting. Let’s get to the emergency room so you don’t hurt yourself.” It’s just like this storm that you have to get through.
I’ve lived in Baltimore for three years and I still think about how far I am from my family, and I do hate that. But I love my job, and I think that helps, actually, almost as like a treatment for depression. It gives me purpose. It gives me something that I look forward to.
Today I have more self-worth, I have more tools to combat my depression, and I have hope.







EVIJOY COUNSELING CENTER
JASMINE SIMMONS, LCPC CLINICAL DIRECTOR
400 Redland Ct., Suite 101
Owings Mills, MD 21117
evijoycounseling.com
info@evijoycounseling.com
EviJoyWhat makes EviJoy Counseling Center stand out?
We have a diverse team of 10 licensed professionals who take a somatic approach that encourages clients to understand where they feel emotions in their body; we are an emotion focused practice.
What inspired you to get in this field?
My own struggle with depression and anxiety as a young child. As I grew up, I realized how much of an impact that made on my life as a young woman and that I wanted to help people.

DIVINE COUNSELING LLC
CARA BALTIMORE, OWNER
90 Painters Mill Road, Suite 136 Owings Mills, MD 21117
443.955.2662
divinecounselingllc.com
referrals@divinecounselingllc.net
Talk about the work you do.
We help individuals reach their highest self by providing quality services that are tailored to each individual’s unique strengths, abilities, preferences, and needs. This was a dream of mine since I was younger. I saw the need in the community, and I wanted to address it.
How do you see the work impacting the community?
The positive feedback we get from those we serve helps evaluate how we are showing up for the community. My goal for the future is to simply help every person I can and to keep expanding on that as the needs of community change.
As a leader, how do you know you’re on the right track?
For me, success is changing the world—or at least our direct community. It’s also important for me to see my employees thriving in their workplace. I help people achieve success by putting them in positions to reach their highest selves.


VITA NOVA WELLNESS CLINIC
BRIJEN L. JOSHI, MD, FOUNDER, CEO 513 Bayview Blvd., Suite 513 Baltimore, MD 21224
443.563.1059
vitanovawellnessclinic.com info@vitanovawellnessclinic.com
Can ketamine end the cycle of depression?
For those who’ve tried everything—therapy, medications—ketamine may be the answer.
How does it work?
For many, the change is almost instant. After just one infusion, the heaviness lifts, sleep improves, and life feels possible again.
How does Vita Nova Wellness approach this treatment?
We go beyond simply administering the drug. Our doctors take a science-backed, root-cause approach, delivering real results in over 90 percent of our patients. Seeing lives transformed is what fuels our mission.
RESOURCE GUIDE
ALPAS WELLNESS CENTER
240-342-3240 alpaswellnesscenters.org
CLEARVIEW COMMUNITIES
240-439-4900 clearviewcommunities.org
DIVINE COUNSELING LLC
443-955-2662 divinecounselingllc.com
EVIJOY COUNSELING CENTER
443-364-8099 evijoycounseling.com
HEALING CITIES INC.
202-937-1105 HealingCities.org
HOLISTIC LIFE FOUNDATION INC
410-235-4300 hlfinc.org
HYGEA HEALTH CARE
310-595-5578 hygea.health
JAY CARE MENTAL HEALTH CENTER
1-888-331-3770 jaycarementalhealthcenters.com
KLEIN FAMILY CENTER
1-200-NEXT-STEP umuch.org/Klein
NAMI
METROPOLITAN BALTIMORE
410-435-2600 namibaltimore.org
SHEPPARD PRATT
410-938-3000 sheppardpratt.org
THE MENTAL HEALTH EMERGENCY FUND, INC. 443-436-2636 mentalhealthemergencyfund.org
VITA NOVA WELLNESS
443-563-1059 vitanovawellnessclinic.com THANK YOU TO OUR GENEROUS SPONSORS:
Resource Guide
URGENT CARE
BALTIMORE COUNTY 24-HOUR CRISIS TEAM
410-931-2214
The hotline is available to those in crisis 24/7. Part of the Baltimore County Crisis Response System, it can provide mental health services to persons in mental, behavioral, or emotional crisis via a specially trained police officer paired with a licensed mental health clinician. Once on the scene, emergency responders can assess individuals in need of services, offer resources and referrals, and complete emergency petitions if the individual in crisis needs further care.
BALTIMORE CITY CRISIS, INFORMATION, AND REFERRAL LINE
410-433-5175
Offering 24/7 support for those in mental health or substance use crisis as well as access to information on preventing overdose, finding medical care, and accessing mental health treatment.
MARYLAND CRISIS HOTLINE
800-422-0009
Available for an emergency situation concerning an adult or child’s mental health, 24/7.
MENTAL HEALTH EMERGENCY FUND
mentalhealthemergencyfund.org
The Mental Health Emergency Fund provides mental health stipends up to $1,000 to qualifying marginalized individuals experiencing a crisis.
PSYCHIATRIC URGENT CARE AT SHEPPARD PRATT
sheppardpratt.org/care-finder/psychiatric-urgent-care 410-938-5302
Designed for people who need emergency psychiatric triage, urgent care is available at the Towson and Baltimore/Washington campuses (hours vary).
SUICIDE AND CRISIS LIFELINE
988helpline.org | Dial 988
If you or someone you know is in immediate need of emotional support, this crisis line connects to a live counselor 24/7.
UNIVERSITY OF MARYLAND MEDICAL CENTER
PSYCHIATRIC ER
umms.org/ummc/health-services/emergency/psychiatric 410-328-1219
University of Maryland Medical Center’s 24/7 Psychiatric Emergency Services (PES) program is for people over age 18 who urgently need a psychiatric assessment, evaluation, and referral. Services, provided on a walk-in basis, help people access mental health and addiction recovery resources.
WALK-IN AND URGENT CARE CENTERS
Maryland Department of Health lists county-based walk-in and urgent care centers on its website.
BALTIMORE CITY: 443-438-3509
Walk-ins 24/7/365
BALTIMORE COUNTY: 410-931-2214
Open for urgent care
HARFORD COUNTY: 800-639-8783
Walk-ins 7 days a week, 7 a.m. to 7 p.m.
HOWARD COUNTY: 410-531-6677
Walk-ins 24/7/365
ADDICTION SERVICES
BALTIMORE COUNTY DEPARTMENT OF HEALTH
baltimorecountymd.gov/departments/health/healthservices/substance-use
Substance use hotline: 410-88-REACH (887-3224)
BCDH provides treatment through community providers for substance users and their families and develops, coordinates, and monitors a countywide network of substance use prevention and disorder treatment services. Free screenings and referrals are available as is free language assistance and funding help for the uninsured.
MARYLAND CRISIS STABILIZATION CENTER
443-438-3509
A place to get sober, access support and basic services, be evaluated for medication management, and more. Offered free, 24/7. No insurance required.
REHABS.ORG
rehabs.org/centers/maryland/baltimore | 410-538-2241
Database of accredited drug and alcohol detox, inpatient, and outpatient rehab centers in Baltimore offering free or low-cost services.
UNIVERSITY OF MARYLAND MEDICAL CENTER umms.org/ummc/health-services/addiction UM Addiction Treatment Center 443-462-3400
Center for Addiction Medicine 410-225-8240
UMMC offers numerous addiction services and programs at its downtown and midtown campuses. Individuals can apply for financial assistance.
ADVOCACY
MENTAL HEALTH ASSOCIATION OF MARYLAND mhamd.org | 443-901-1550
MHAM advances mental health in the state through advocacy, training, community outreach/education, and oversight of public mental health services.
NAMI METROPOLITAN BALTIMORE
namibaltimore.org | 410-435-2600
National Alliance on Mental Illness (NAMI) Metropolitan Baltimore supports individuals affected by mental health issues by providing education, support, advocacy, and public awareness surrounding topics of mental health.
ON OUR OWN MARYLAND
onourownmd.org | 410-540-9020
A statewide peer-operated behavioral health advocacy and education organization that promotes equality, justice, autonomy, and choice about life decisions for individuals with mental health and substance use needs.
GENERAL
ALL WALKS OF LIFE
allwalksoflife.org | 410-558-0019
Providing behavioral health care to those in need throughout Baltimore’s schools and communities through their Village-Centered Treatment (VCT) approach. They offer psychiatric rehabilitation services, medication management, a mental health clinic for children and youth grades 1-12, and therapeutic behavioral services.
BEHAVIORAL HEALTH SYSTEM BALTIMORE
bhsbaltimore.org | 410-637-1900 or 988
A nonprofit organization tasked by Baltimore City to manage the system of care that addresses emotional health and well-being and provides services for individuals with substance use and mental health disorders. BHSB helps guide innovative approaches to prevention, early intervention, treatment, and recovery for those who are dealing with mental health and substance use disorders.
BRICK BY BRICK BEHAVIORAL SERVICES
brickbybrickservices.org | 410-616-6333
Organization focused on building stability skills for youth who suffer from trauma. They also engage with family members, aiming to heal the entire family from trauma. They offer high-quality, cost-effective, and evidencebased services tailored to individual needs.
BRIDGING GAPS THROUGH POSITIVE SOLUTIONS
bgtps.com | 443-835-4825
BGTPS is a community-based behavioral health program that offers group, family, or individual therapy sessions. They also offer Psychiatric Rehabilitation Program (PRP) community support through their character and culture program.
CATHOLIC CHARITIES
cc-md.org/our-programs/healing-trauma-addiction
Catholic Charities provides a wide range of mental and behavioral health services for children, adults, and families, including mental health screening, counseling, therapy, psychiatric rehabilitation, substance use disorder treatment, and medication treatment. Multiple locations.
CHANGING TURN COMMUNITY HEALTHCARE SERVICES
changingturn.org
Baltimore City: 443-708-1461
Harford County: 443-402-0172
A licensed community mental health organization, Changing Turn Community Healthcare Services offers an array of services aimed at the management, rehabilitation, and well-being of children, adolescents, adults, and their families.
DIVINE COUNSELING
divinecounselingllc.com | 443-955-2662
A holistic, trauma-informed, outpatient, mental health organization committed to providing compassionate support to individuals, especially BIPOC, seeking guidance on their mental health journeys.
FREE BALTIMORE
freebaltimore.org/mental-health-clinic | 443-759-7075
Free Baltimore aims to educate, heal, and empower LGBTQIA+ and other marginalized people by fostering a safe therapeutic space and providing culturally responsive behavioral health services that center on the patient’s strengths and needs.
HARFORD BELAIR COMMUNITY MENTAL HEALTH CENTER
Serving two communities, the Harford Belair Community Mental Health Center provides the highest quality of psychiatric and mental health services to all persons in the community in need. harfordbelair.org | 410-426-5650
HEALING SELF WELLNESS
thehealingself.com | 443-377-7448
Offers evidence-based approaches for mental health rooted in mindful cognitive behavioral, somatic, natureinformed, and culturally respectful therapies to address the whole person. Work may include verbal processing as well as yoga, and/or informal/formal nature exercises. Sessions can be in-person or virtual sessions for individuals, couples, and groups.
JEWISH COMMUNITY SERVICES
jcsbalt.org/services/emotional-and-behavioral-health
410-466-9200
An agency of The Associated: Jewish Federation of Baltimore offering therapy, psychiatry, a psychiatric rehabilitation program, and critical incident response.
LIVING SPRINGS BEHAVIORAL HEALTH
livingspringsbhc.com | 410-588-9689
Provides caring support to individuals who are struggling with mental health issues with services such as counseling and therapy, support groups, medication management, and crisis intervention.
MIGHTY BEHAVIORAL HEALTH SERVICES
mightybehavioral.net | 667- 260-2933
An integrated mental health service provider where psychiatrists, psychiatric nurse practitioners, psychologists, and psychotherapists collectively treat mental illnesses with complete consideration of your full medical, psychological, social, and family history.
PRO BONO COUNSELING
probonocounseling.org | 410-825-1001
Free mental health care from licensed professionals for families and individuals with no insurance and low incomes.
211 MARYLAND
211md.org/resources/mental-health | Dial 211
This nonprofit is the state’s most comprehensive health and human services information and referral system. With more than 7,500 resources, individuals with essential needs can get connected to local help 24/7/365.
VILLA MARIA BEHAVIORAL HEALTH
cc-md.org/programs/villa-maria-behavioral-health 667-600-2000
A division of Catholic Charities, Villa Marie serves children, teens, families, and adults on Medicaid and Medicare by providing a healthcare environment that is inclusive, compassionate, and free of judgment at its eight clinics, via virtual appointments, and through school programs.
VILLAGE BEHAVIORAL HEALTH CENTER
villagebhcenter.com | 443-759-4184
Expert counseling for both children and adults that aims to enhance each patients’ spiritual, mental, and physical health.
YOUTH & FAMILY
KENNEDY KRIEGER INSTITUTE
CENTER FOR CHILD AND FAMILY TRAUMATIC STRESS
443-923-3213
Provides mental health treatment services to children, adolescents, and families who have experienced or may be at risk for trauma through physical or sexual abuse, neglect, domestic violence, and community violence.
CENTER FOR DEVELOPMENTAL BEHAVIORAL HEALTH
443-923-3234
Brings together psychiatry, psychology, social work, and nursing to provide team-based, patient- and family-centered care.
LIL’ LAUGHS
lillaughs.org
By recognizing the challenges faced by students in schools, such as bullying, Lil’ Laughs seeks to combat the self-esteem issues that plague students every day and build confidence with anti-bullying campaigns fueled by comedy.
MARYLAND COALITION OF FAMILIES
mdcoalition.org | 410-730-8267
Statewide nonprofit that offers family peer support to people and families who have a loved one experiencing mental health, substance use, or problem gambling challenges.
MD YOUNG MINDS
211md.org/about/text-messages/mdyoungminds
Text: 898-211
This text message program connects teens and adolescents with supportive texts focused on adolescent concerns and worries. The program is designed by the Maryland Department of Health, Office of Suicide Prevention, and utilizes 211 Maryland’s texting platform.
MT. WASHINGTON PEDIATRIC HOSPITAL mwph.org | 410-578-8600
Behavioral health services at MWPH are designed to provide high quality mental health assessment and treatment services to children with a wide range of presenting concerns.
WOMEN LEADING BALTIMORE
womenleadingbaltimore.org | 443-789-8378
A nonprofit organization that creates space and opportunities for high school girls to embrace their power and authority through sisterhood, nurturing mentorship, and access to meaningful experiences.
VOCATIONAL TRAINING & SUPPORT
ADVOCATE SUPPORT SERVICES
advocatesupport.com | 866-277-2080
A provider of community-based psychiatric rehabilitation services that educate, advocate, and provide services that maximize personal independence.
B’MORE CLUBHOUSE
Bmoreclubhouse.org | 410-727-2030
Through meaningful, active participation in the maintenance and running of the clubhouse throughout a workordered day, members are given the opportunity to live life on their own terms.
DORS
dors.maryland.gov | 410-554-9442
Maryland State Department of Education’s Division of Rehabilitation Services (DORS) offers supported employment where job seekers with disabilities are given ongoing support after they begin working through training, supervision, and help with adjustment to the work environment.
ROCK CREEK FOUNDATION
rockcreek.org | 301-586-0900
The Foundation’s Mental Health Vocational Program helps individuals find work that aligns with their abilities, interests, and chances for growth.
SHEPPARD PRATT
sheppardpratt.org/care-services/employmentjob-training
Sheppard Pratt provides vocational services and job training, as well as help with job preparedness, like résumé writing, so individuals can find and keep meaningful employment.
TALMAR
talmar.org | 410-825-2020
A vegetable, cut flower, and egg farm with apiary that is designed to provide recreational, therapeutic, and vocational programs for people with disabilities. Licensed OT and supported volunteer opportunities.
HELP BY COUNTY
For information on public mental health services in your county, call your local mental health agency:
ANNE ARUNDEL 410-222-7858
BALTIMORE CITY 410-837-2647
BALTIMORE 410-887-3828
CARROLL 410-876-4800
HARFORD 410-803-8726
HOWARD 410-313-7350
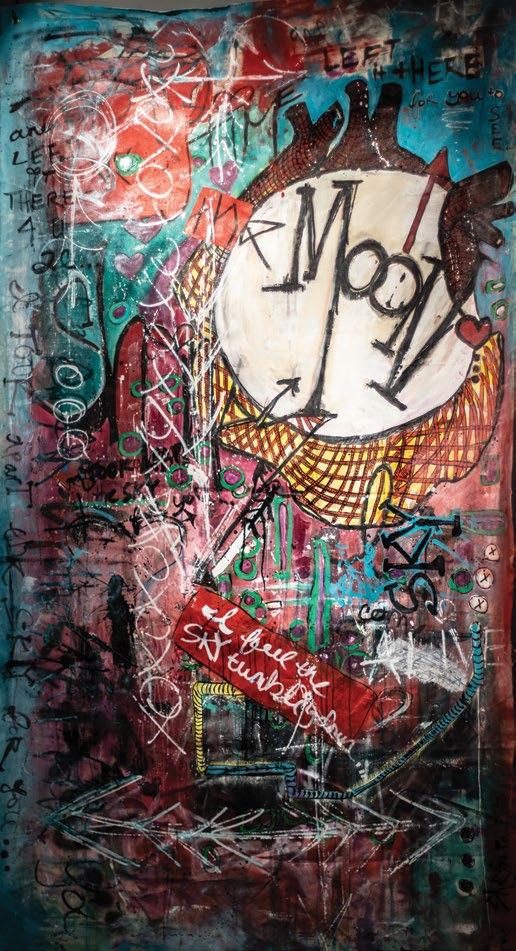
I Took Apart the Sky for You
“My brother, who dabbles in music, had just written these lyrics, ‘I took apart the sky for you and left it there for you to see,’ which became the name of the piece. He was the one I called and who continued to check on me and encouraged me to get help in a really powerful way. He was the one who really helped me in the moment. He was not afraid to ask the hard questions—and when he asked me how I was, he was willing to hear an answer of ‘not that great.’ He went to hell and back to help me understand joy again. For me, ‘I took apart the sky for you’ means showing unconditional love and the lengths that I felt my brother would go to help me.”
King of Sorrow
“I was trying to will a sense of hope into my life and was struggling with suicidal ideation—I was trying to will this female empowerment, this Valkyrie. The piece gave meaning and purpose to this dark time. The title was inspired by a Sade song.”

ARTIST IN RESIDENCE
Nicole Clark
Growing up in Chicago, Nicole Clark was steeped in the visual arts. But by adulthood, she had given up her creative pursuits, except for some occasional writing. “It was a desert of creativity for many years,” says Clark, who moved to Baltimore in 2010 for better job opportunities. But after a divorce at the age of 30, Clark returned to her creative life. “It came out of necessity for my mental health,” she says. “I was not aware that I was in a season of depression.”
One day, Clark found some abandoned wood panels and took them home to use as a canvas for her paint. “I did not have a community in Baltimore at the time,” she says. “I needed artwork for the apartment I moved to after my divorce. I was like, ‘I’ll make art for my walls.’ Initally, in the absence of having a community, it was feeding my soul,” she says. Some 11 years later, it’s taken on an even deeper meaning. “It took me years to understand the creative process and the healing that can bring,” explains Clark. “My work is a lot like writing an essay: You write to answer a question, but sometimes you don’t know what the question is. My paintings are a means for me to understand what’s going on beneath the surface. Once I finish a piece and step back, it’s a reflection of a question that was ruminating. As my creative processes have crystallized, I began to realize my art was like my writing—it was a portal to understand what was happening at a subconscious level.”

We have the privilege of hosting the NAMI Metropolitan Baltimore team for regular discussions about mental health with our colleagues. Here, Brown Advisory’s Joey Martin, Compliance Officer and NAMI Metro Baltimore board member, welcomed Nao Gamo, Ph.D. (center), also a NAMI Metro Baltimore board member, and Julie Funk, director of development at NAMI Metro Baltimore, for a conversation about creating a stigma-free workplace.