

















































Physical activity guidelines extended to include pregnant and postpartum women. See page 79.
1 Meet the people behind the HSE library service
2 Spotlight on immunisation
4 My story: Public Health Nurse Audrey Burkley on how sea swimming boosts her wellbeing
8 In focus: Men’s health
11 Meds on time, every time to improve Parkinson’s care; and HSE and NAS collaborate to reduce ED admissions
12 In focus: Children and young people
14 HSE launches Eve’s Protocol to improve diagnosis and care for patients with blood clots in Ireland
15 Let’s talk about… the new law on organ donation
16 Updates from HSE Dublin and South East
22 Digital for Care
26 Updates from HSE South West
32 Spotlight on HSE strategy, people and culture
35 Climate action news
36 Updates from HSE Mid West
42 Spotlight on tobacco, nicotine and other inhaling products
45 Competition: Share a snap of Health Matters and be in with a chance of winning a €100 One4all voucher
46 Updates from HSE Dublin and North East
52 Spotlight on communication
54 Changing the narrative on suicide
55 Ireland shares health system reform insights on international stage
56 Updates from HSE West and North West
62 The HSE cancer survivorship peer support service
64 In focus: Policy and strategy
66 Updates from HSE Dublin and Midlands
72 New surgical hubs begin to roll out across the regions
73 In other news… Updates, events, collaborations, celebrations and milestones
Thank you to everyone who has submitted stories for this edition. If you would like to see your initiative or work featured, you can submit your ideas through our online form at bit.ly/HealthMattersForm
HSE


Welcome to the autumn issue of Health Matters. As we embrace that back-to-school feeling, fill our lungs with that crisp seasonal air, and watch the sun set that little bit earlier each day, we’re reminded about the fleeting nature of time. We therefore invite you to make the most of your free hours to do something beneficial for your physical and mental health. On page 6, Public Health Nurse Audrey Burkley takes a deep dive into how sea swimming can boost your wellbeing, while on page 1 we look at how the HSE library service provides ongoing support for education and lifelong learning.
















In this edition, we also highlight the important campaigns and ongoing efforts to improve the wellbeing of service users nationwide. On page 2, we shine a spotlight on immunisation and what healthcare workers need to do to protect themselves and their patients. Then on page 42, we look at the work being done to tackle the use of tobacco, nicotine and other inhaling products. And as we approach World Suicide Prevention Day on 10 September, we look at how to change the narrative on suicide on page 54.
The last few months have seen great work being done across the health regions. Turn to pages 16, 26, 36, 46, 56 and 66 to catch up on all the news from the six health regions, while on page 72, we take a peek at the new surgical hubs rolling out across the country.
Elsewhere, we focus on men’s health (page 8), children and young people (page 12), organ donation (page 15), HSE strategy, people and culture (page 32), climate action (page 35), communication (page 52), and policy and strategy (page 64). Plus so much more, from Digital for Care news (page 22) to the HSE cancer survivorship peer support service (page 62).
We hope you find inspiration throughout this issue and that you’ll share your feedback with us (check out our reader competition on page 45 and learn how you can be in with a chance to win a €100 One4all voucher). Whether you’re poring over these pages while sipping a hot mug of tea or taking a copy of Health Matters with you on a well-deserved weekend away, we hope this season sees you getting outdoors to enjoy the fresh autumnal air and your days and nights are filled with health, hope and happiness.
Meg Walker Editor
Published by Ashville Media, Unit 55 Park West Road, Park West Industrial Estate, Dublin 12, D12 X9F9. Tel: (01) 432 2200 ISSN: 0332-4400
All rights reserved. Every care has been taken to ensure the information contained in this magazine is accurate. The publishers cannot, however, accept responsibility for errors or omissions. Reproduction by any means in whole or in part without the permission of the publisher is prohibited. © Ashville Media Group 2025.
The HSE library service is a nationwide network of 50 committed information professionals. They are working to support practice, research, education and lifelong learning across our health service. Most of you already benefit from these efforts – in a 2021 independent survey, 92% of respondents said that the library resources help improve patient care, and 94% said the information the service provides was often essential to clinical decisions.
Access to the right information at the right time is key to safe, effective healthcare. Our librarians work closely with clinicians to provide trusted, evidence-based resources that support patient care.
A full range of library services is provided through a dedicated website, hselibrary.ie, offering 24/7 access to highquality electronic resources. This includes prescribing tools such as the British National Formulary and the Maudsley Prescribing Guidelines. You’ll also find mobile-friendly tools like BMJ Best Practice and UpToDate, giving clinicians instant access to the latest guidance. These are supported by a seamlessly integrated collection of databases, journals and e-books, offering a trusted, comprehensive environment for research, learning and decision-making.
Our evidence team offers tailored literature searches to support clinical and policy decisions. Our librarians provide
HSE Library Day – 24 September
vital insights on the availability and trustworthiness of clinical research and evidence, saving clinicians time. For example, our librarians Gethin White and Linda Halton helped develop the National Clinical Guidelines for common cancers with the National Cancer Control Programme earlier this year. Our information skills team offers online training to help staff find and use this information confidently, to support their work and decision-making. The team has run highly successful webinars for health professionals, guiding them through an often complex maze of online information.
Our community outreach team ensures healthcare staff in all community settings, no matter where they work, can access these services equally. In addition, its specialist research bulletins, such as the Nursing in the Community Bulletin and the more recent NCPOP (National Clinical Programme for Older People) Bulletin, provide targeted, relevant information exactly where it’s most needed.
The HSE library staff is the heart of all these services. They locate high-quality information, provide access to key resources, and support clinicians to find, assess and use the evidence needed to treat service users. Their specialist knowledge, initiative and commitment directly support decision-making, patient care and service improvement across the health system.
Join us in celebrating the first-ever HSE Library Day, a national event recognising the impact of library services on patient care and the essential role of our library staff in Irish healthcare. From pop-up events and giveaways to expert advice and interactive sessions, it’s a chance to meet your library team and discover how they support your work, study and service delivery. Contact HSE Library at hselibrary@hse.ie to learn more, or visit hselibrary.ie
On 18 June, Wexford General Hospital hosted the official re-opening of its restored health library, which suffered extensive smoke and water damage during a serious fire in March 2023. Part of the HSE Library Service, the facility is situated on the fourth floor, with spectacular views over the town, Ely Hospital and Raven Point. The newly renovated library offers 24/7 access to dedicated study and ICT spaces and an updated book collection. For the first time, it also offers the services of a newly appointed qualified librarian, Gabriel Graves. Gabriel is on site Tuesdays and Thursdays. The library is open to all hospital and community-based staff, and to students on clinical placement.



Each winter, healthcare workers have a high risk of exposure to respiratory viruses, putting them at risk of illness. This year, the flu vaccine is strongly recommended for all healthcare workers. It provides the best available protection against the serious complications of flu infection.
Based on the advice of the National Immunisation Advisory Committee (NIAC), the recommendations for COVID-19 vaccines for healthcare workers have changed this year. All healthcare workers are no longer routinely recommended to get a COVID-19 vaccine. This is because healthcare workers under the age of 60 with no underlying medical conditions are at low risk of severe infection if they get COVID-19. However, healthcare workers aged 60 years and older, or healthcare workers with medical conditions, including immunocompromise, remain at risk of severe infection and are still recommended to get a COVID-19 vaccine this autumn/winter. Other healthcare workers who choose to receive this vaccine can do so if they wish.

Vaccination Nurse, and Kathleen O’Donoghue, Operations
Lead at Kerry ICPOP proudly supporting the HSE South West’s winter vaccination campaign at Kerry Vaccination Centre, Tralee.



The flu and COVID-19 vaccines can be given together or separately. Flu and COVID-19 vaccines are available free of charge for all healthcare workers as part of the HSE’s 2025/2026 winter vaccination programme. Vaccines may be available at your workplace, and are available from GPs and pharmacies. Clinic details will be listed on hse.ie/staffclinics from October.

1 Flu vaccination matters
Influenza (flu) is a serious viral illness. In 2024/2025, over 6,500 people were admitted to hospital with flu and over 300 people died. Healthcare workers are particularly vulnerable to getting flu, and are 10 times more likely to catch the flu than the general public. Complications of flu can include pneumonia and sepsis. Healthcare workers who are aged 60 and older or who have underlying medical risk factors are particularly at risk of complications, but even if you are otherwise healthy, flu can be serious. Therefore, all healthcare workers are recommended to get a flu vaccine. As well as protecting healthcare workers themselves, vaccination helps to protect others and reduces the chances of spreading flu to family members, colleagues and patients, many of whom may be more vulnerable to serious complications.


2 Vaccination is the best protection
“The flu vaccine provides healthcare workers with the best available protection against the serious complications of flu,” says Dr Louise Marron, Consultant in Public Health Medicine at the National Immunisation Office. “As healthcare workers, we will be exposed to flu this winter. Please take this opportunity to protect yourself, your loved ones and those you care for by getting vaccinated.”
4 Flu vaccines are safe and effective
Five things you should know about this year’s flu vaccine
The HSE only uses vaccines that meet strict standards for safety and effectiveness, and are licensed by the European Medicines Agency. This winter, two flu vaccines will be available for adults: Vaxigrip (Sanofi) and Influvac (Viatris). These target the flu strains that are expected to circulate, as advised by the World Health Organization. It is quick and easy to get vaccinated. Side effects are usually mild; for example, soreness at the injection site, sore muscles or tiredness. The benefits of vaccination far outweigh the risk of side effects.


3 Protecting pregnant healthcare workers and their babies from flu
Flu infection during pregnancy can be more severe and lead to serious complications for mothers and babies. The flu vaccine is strongly recommended for all pregnant healthcare workers, offering protection to both the mother and her newborn during the early months of life. The flu vaccine is very safe in pregnancy.
Learn more about flu at hse.ie/flu
The effectiveness of the flu vaccine can vary between individuals, and depends on the strain of flu that circulates during the flu season. However, if people who have been vaccinated get the flu, their symptoms will be milder and they will have a faster recovery than if they had not been vaccinated.
The flu vaccine is not a live vaccine. It cannot cause flu. However, the vaccine takes two weeks to work, so it should be given early in the flu season to get the best available protection.
5 Stay informed and be part of the solution

Apart from clean water, vaccines have saved more lives than any other public health intervention. Now more than ever, getting vaccinated is a simple but powerful act of care, for yourself and those around you.

Getting vaccinated will reduce your risk of getting flu and of getting seriously unwell with it. However, if you develop flu-like symptoms, you should stay at home, do not go to work, and if you are unwell you should seek advice from your GP.
All healthcare workers across the system, including nurses, doctors, porters, carers and administrative staff are recommended to get the flu vaccine.
“High levels of respiratory illness create additional pressure on our healthcare system,” says Dr Colm Henry, Chief Clinical Officer of the HSE. “Vaccination not only protects you and your family, but also protects your patients.”
You can also complete the 15-minute HSeLanD module: Flu and COVID-19 Vaccines for Healthcare Workers, Protect Yourself, Protect Others at hseland.ie

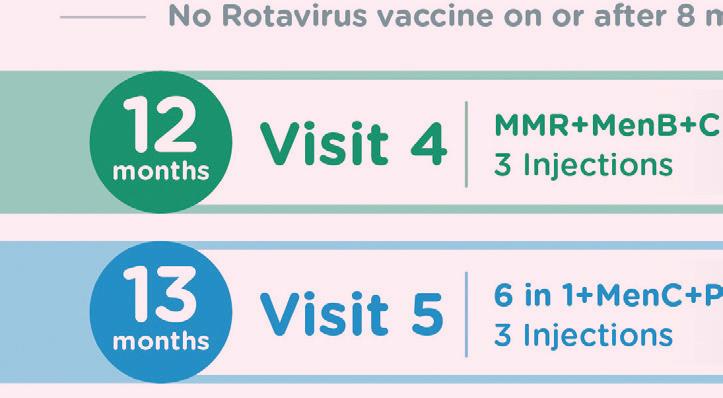
In 2024, the HSE updated the primary childhood immunisation schedule to include the chickenpox (varicella) vaccine for all babies born on or after 1 October 2024. As a result, babies nearing their first birthday will now be due to receive this important vaccine when they turn 1 year of age. This change follows guidance from the National Immunisation Advisory Committee (NIAC) and supports Ireland’s continued commitment to preventing vaccine-preventable disease.
Supporting families through vaccine conversation As healthcare workers, you play a key role in informing families about vaccines and stressing the importance of vaccinating babies on time. While often perceived as a mild illness, chickenpox can cause serious complications both in healthy children and those who are medically vulnerable. In 2023 alone, approximately 170 children were hospitalised in Ireland due to chickenpox, with some experiencing pneumonia, encephalitis or other serious complications.
In 2023 alone, approximately 170 children were hospitalised in Ireland due to chickenpox, with some experiencing pneumonia, encephalitis or other serious complications.
The introduction of the chickenpox vaccine offers early, effective protection. Vaccination has been shown to prevent moderate-to-severe disease in most children and provide long-term immunity.
“We are delighted that the chickenpox vaccine is now part of the routine vaccination schedule for babies,” says Dr Chantal Migone, Consultant in Public Health Medicine, National Immunisation Office. “The vaccine protects babies from chickenpox, which can sometimes lead to serious complications. As healthcare workers, you are highly trusted by parents; your recommendation makes a real difference. By encouraging uptake of the chickenpox vaccine and addressing any questions families may have, you play a vital role in protecting babies and supporting public health.”
Babies born on or after 1 October 2024 will receive the chickenpox vaccine at 12 months of age, free of charge from their general practice. Children born on or before 30 September 2024 are not included in the updated schedule but may be vaccinated privately through their GP, if requested by parents.
Updated immunisation schedule (for babies born on or after 1 October 2024)
Your advice and support are highly trusted by parents. You can continue to recommend vaccination and, if you are a vaccinator, administer vaccines at 2, 4, 6, 12, and 13 months. The chickenpox vaccine is given at the 12-month visit. A second dose of chickenpox vaccine, as well as booster doses of other vaccines, will be due at 4-5 years of age. The updated childhood vaccination schedule is as follows:


Supporting families to stay on track
You can encourage parents to complete the full immunisation schedule on time and openly discuss any questions they may have about vaccines. If you’re working with parents who are unsure about their child’s vaccine status, remind them to check with their GP or local health office.
For more information, visit immunisation.ie or Mychild.ie

Measles is one of the most contagious viral infections in the world, and cases are rising again in Ireland and across Europe. As a healthcare worker, you can play a critical role in both preventing the spread of measles and promoting vaccination among patients and families.


Measles can cause serious complications, including pneumonia, liver inflammation, encephalitis (inflammation of the brain), and in rare cases, death. It spreads quickly through airborne droplets or contact with contaminated surfaces and can remain infectious for several days before symptoms even appear.
The best protection against measles is the MMR (measles, mumps and rubella) vaccine. Two doses are required for full protection. In Ireland, these are routinely given at 12 months of age and again when the child is in junior infants. In some areas, such as Sligo, Leitrim and Donegal, the second dose is administered by GPs at age 4-5.
Healthcare workers are at increased risk of exposure to measles, especially during outbreaks. Verifying your own MMR status helps protect vulnerable patients.
If you are unsure whether you received both doses of the MMR vaccine, you can talk to your GP. The vaccine is free of charge. Infants aged 6 to 12 months travelling abroad are also eligible for an early dose, ideally given at least two weeks before travel. Your voice matters. As a healthcare worker, you can make every contact count by supporting patients to check their MMR vaccination status, recommending vaccination and staying protected yourself.









The HSE is extending last winter’s successful RSV immunisation programme for newborn babies in maternity settings and higher risk babies in the community. It significantly reduced infections, serious illness and hospitalisations.
The RSV immunisation programme will run again for newborns in maternity settings and for higher risk babies at home from September. This will be supplemented with a new catch-up programme for babies born from 1 March 2025.
Before the programme, each winter, four out of 100 infants were hospitalised with RSV, some needing special treatment in intensive care units, says HSE National Director for Health Protection, Dr Éamonn O’Moore. “A further 50 out of every 100 infants got RSV and many needed care from their GP, or A&E. The immunisation is provided for free. It will also help our hospitals by preventing avoidable illness so babies won’t need hospital or medical treatment, which was the case in previous years.”
• Almost 22,500 babies were immunised
• 83% accepted immunisation for their babies
When compared with the same period the year before:
• Cases reduced by 65%
• 57% fewer cases in A&E
• 6% reduction in hospitalised babies
• 65% reduction in babies in ICU




Audrey Burkley, Public Health Nurse in North Lee in the South West, shares how sea swimming has given her the balance she’s long craved
I am a public health nurse specialising in vaccinations. Initially, I was working with an area medical officer, but after the COVID-19 pandemic, more nurses were employed and vaccination teams were established. Between October to December, I vaccinate junior infant schoolchildren, administrating the MMR and 4-in-1 in schools and clinics. Then, from January to the end of May, the first year students are offered the HPV, Tdap and MenACWY vaccines.
In October, I also assist with the flu vaccination clinics. This vaccine is important as it reduces our risk of contracting and spreading influenza, protecting ourselves and the clients we look after. For most influenza seasons, the vaccine provides good protection for 70-90% of people who get the vaccine. For the remainder, it can reduce the severity of illness and make complications from influenza less likely. I strongly recommend everyone to get the vaccine, as complications from influenza – including pneumonia and encephalopathy (inflammation of the brain) – can be life-threatening. It can also cause worsening of chronic medical conditions such as asthma, congestive heart failure, and diabetes.
For most influenza seasons, the vaccine provides good protection for 70-90% of people who get the vaccine.
When I’m not working, I’m often down at the water, sea swimming. I started sea swimming in 2013 when I was advised to do non-weight-bearing activities due to congenital dysplasia of my hips. It quickly became a great passion of mine and, as I became more familiar with the water, I knew I wanted to excel in the area of open water channel swimming. I have completed many relays from the English Channel, the North Channel, the Catalina Channel, the circuit around Jersey, and Jersey to France. My mobility has been decreasing due to my hip problem so my most recent aim was to complete two double relay swims in Ireland that had not been done before, which I achieved last year (see side panel). This September, I’ll be swimming a 36.4km, fourperson relay in Loch Lomond in Scotland.
During the week, I practise in Brookfield Pool in Cork and also with Cork Masters Swimming Club. And at weekends, I swim in Myrtleville Beach in Crosshaven. This schedule can be demanding, but I am my happiest in the water. I enjoy the cold, reaping the benefits of swimming throughout the year.
Swimming is my life. I am so close to nature and love to feel the power of the waves against my arms. It helps me to totally switch off. I think it is so important to have the right balance between work and time off.



My sea swimming achievements in 2024:
• 30 July – Classic Fastnet (Fastnet/Baltimore) – two-way relay; the first time a two-way relay has been completed
• 6 September – Blennerville to Fenit 11km – solo
• 18 September – Classic Galway Bay (Aughinish/Blackrock) –two-way relay
• 21 September – Owenabue Sail Garden Carrigaline to Fountainstown Cork 13.8km; the first time this swim has been done – solo
Sea swimming has brought about many wonderful benefits to my health and wellbeing. And it has connected me with other swimmers and the wider sea swimming community, both nationally and internationally, which has brought me so much joy and friendship.
Whether for fun, connection or to support your physical or mental health, I would highly recommend anyone dip their toe in this wonderful pastime. Autumn is the perfect time to start.

Men’s Health Week (MHW) 2025 focused on the importance of social connection under the theme “Shoulder to shoulder, connecting for health”. Running annually in June ahead of Father’s Day, this campaign is led by HSE Health and Wellbeing in partnership with the Men’s Health Forum in Ireland (MHFI). It aims to raise awareness of how men can improve their health through healthier lifestyle choices and early detection and treatment.
Highlights included:
• HSE Health Promotion and Improvement teams and local partners hosted events in workplaces, agricultural marts and community centres to engage
men in their communities.
• A national webinar featured speakers such as former rugby player Bernard Jackman and former Dublin GAA footballer Michael Darragh MacAuley, alongside Sean Blake, who shared his experience with an eating disorder. BowelScreen promoted its free home screening for those aged 59-70.
• The Irish Men’s Sheds Association encouraged members to walk “shoulder to shoulder” during MHW in various locations through their now annual walks or Slís.
• A special episode of the HSE Talking Health and Wellbeing podcast featured Dr Conor Hammersley discussing healthy masculinity and the challenges men face.
Fergal Fox, Men’s Health Lead in the HSE, highlighted the importance of connection: “Getting involved in some shared activity can help men get vital social support. Talking to another person about your concerns can help a lot. Talking to another man or woman about your health specifically can also help.”
The most shared resource this year was the Action Man booklet, offering practical tools for improving men’s health, which is available on healthpromotion.ie
Men’s Health Week (MHW) was marked in Laois with an event organised by Health Promotion and Improvement in collaboration with Patrick Jones, Resource Officer for Suicide Prevention, and Liam Kelly, Community Sports Development Officer. The theme for MHW 2025 highlights the importance of connectivity and helping each other. This event for HSE staff offered talks on mental health and physical activity, along with a health and wellbeing information stand providing a variety of resources. The purpose of this event was to promote positive lifestyle choices, discuss some of the challenges faced by men, and highlight supports available locally.

From left: Pat Brennan, Patrick Jones, Tom Bourke, Clive Brazil, Martin Gleeson, Ian Dunne, Seamus Murphy, Noel Mooney, Elaine Brennan, Patrick Gallagher, Niall Fitzpatrick, Liam Kelly, and Tom O’Sullivan.

As part of Men’s Health Week, the maintenance teams from St Joseph’s Campus and St Camillus’ Hospital Limerick joined a healthy breakfast live cooking and information session hosted by HSE Mid West Health and Wellbeing. Led by senior dietitians Christine Gurnett and Maria Barrett, along with St Camillus’ Catering Manager, Rory Faye, the session explored the evidence behind nutritious eating, and gave staff a chance to connect and learn together. Participants learned how small changes to their morning routine can significantly improve overall health. Breakfast is the body’s first source of fuel after an overnight fast, helping to regulate energy, hunger and decision-making throughout the day.
Pictured at the healthy breakfast live cooking and information session in St Joseph’s Campus, Limerick were, from left: Beth McDonald, Health Promotion and Improvement Officer, Health and Wellbeing (H&W); Bernadette Mullins, Cancer Prevention lead, H&W; Daniel Butler, Health Promotion and Improvement Officer, H&W; Maria Barrett, Senior Dietitian, H&W; Rory Faye, Catering Manager, St Camillus’ Hospital, Limerick; and Leanne O’Driscoll, Catering Department, St Camillus’ Hospital, Limerick.
As part of Men’s Health Week, the HSE launched a new campaign – “Know the signs” – to raise awareness of the signs and symptoms of penile cancer and urge men to seek medical help early if they notice any changes in their penis. Penile cancer is rare, affecting around 60 men in Ireland each year, mostly those over 50. But early detection significantly improves survival and helps preserve function and appearance.
The campaign featured a video with survivor Cormac France, a father of four from Kildare, who shared his personal journey to encourage early detection. By the time Cormac was diagnosed, the cancer had already spread to his lymph nodes. He underwent urgent surgery at University

Hospital Waterford, under the care of Ivor Cullen, Consultant Urologist at Beaumont Hospital and lead of Ireland’s National Penile Cancer Centre.
“Penile cancer is rare but aggressive once it spreads,” Ivor Cullen explains. “Most cases are preventable, but many men present late due to stigma. Early detection saves lives and quality of life.”
Alison Doran, Clinical Nurse Specialist at Beaumont, highlights key risk factors: “HPV infection, smoking, poor hygiene and conditions like a tight foreskin (phimosis) increase risk. Over half our cases are linked to HPV.”
The campaign ran across HSE social media channels with messaging to encourage early conversations and reduce stigma.
A penile cancer patient guide is available to order for free at healthpromotion.ie Scan the QR code to watch Cormac France share his personal story.

• A growth or sore on the penis that doesn’t heal within four weeks – it may look like a wart or blister
• Bleeding from the penis or from under the foreskin
• A foul-smelling discharge under the foreskin (not ejaculation)
• Swelling or di iculty pulling back the foreskin (phimosis)
• A change in skin colour on the penis or foreskin to blueish or brown
• A rash or small crusty bumps on the penis
• Lumps under the skin in the groin
For people with Parkinson’s, precise medication timing is essential. Even brief delays or missed doses can worsen symptoms like rigidity, tremors and anxiety, reducing quality of life and increasing risks of falls and extended hospitalisation. Repeated delays may cause permanent decline, making symptoms harder to manage. Consistent timing helps control symptoms, reduce complications and healthcare burdens.
The “On time, every time” campaign by Parkinson’s Ireland is dedicated to ensuring Parkinson’s medications are administered precisely at the prescribed times across all care settings. It aims to raise awareness among healthcare professionals, patients and loved ones about the consequences of timing deviations and providing a suite of tools like the Parkinson’s Passport to support consistent, timely medication delivery.
Developed by Parkinson’s Ireland with support from the Irish Medication Safety Network (IMSN) and the HSE Medication Safety team, the campaign emphasises staff education, accurate medication histories and coordinated care. It also promotes the use of IMSN alerts and planning for circumstances like perioperatively, swallowing difficulties, and out-of-hours medication access.
The primary focus remains maintaining strict medication timing to prevent rapid deterioration. Prioritising timing and coordination helps people with Parkinson’s maintain independence, reduce complications and receive safer, more effective care.
A series of collaborations between the National Ambulance Service (NAS) and HSE Mid West is reducing pressure on the region’s only emergency department (ED) at University Hospital Limerick (UHL). This will maximise operational efficiency of the ambulance service by providing care and support at home or in community settings for lower-acuity patients who did not have to be brought to ED.
During 2024, a total of 838 or 58% of 1,445 patients referred to the Pathfinder and Alternative Prehospital-care Pathway (APP) services received hospital-standard care at home or in their communities.
Pathfinder responds to 999/112 calls from people aged 65 and older who may have fallen at home or become generally unwell. The team supported 329 patients of the 506 calls referred to the team last year – a 65% ED avoidance rate.
The APP service for low-acuity emergency calls received 939 calls in total last year, and supported 505 patients (53.7%), keeping those patients out of the ED while reducing the need for ambulance conveyance and freeing up response vehicles for critically ill and injured patients.
Learn more and access resources at parkinsons.ie

More recently, a pilot triage programme rolled out in 18 Mid West nursing homes in September 2024, has reduced ED admissions from those facilities by an average of 19%. NAS and Older People Services have worked closely to train nursing home staff in the Nursing and Residential Triage (NaRT) tool. This has helped NAS teams to manage a range of treatments within nursing home settings, helping 56 patients avoid ambulance conveyance and ED admission.
A ground-breaking Irish study, led by Professor Jonathan Hourihane (Royal College of Surgeons in Ireland and Children’s Health Ireland) and funded by the Research Ireland Frontiers for the Future Programme (€1.3 million) is examining how the COVID-19 pandemic may have shaped early childhood development.
The original CORAL study (Impact of Coronavirus Pandemic on Allergic and Autoimmune Dysregulation in Infants Born During Lockdown) recruited babies born between March and May 2020, during the first national lockdown. This globally unique study explored how pandemic-related restrictions impacted infant microbiomes, allergy development, diet, and developmental outcomes.
Results to date have been striking. Lockdown babies were breastfed for longer and had fewer courses of antibiotics. These changes were associated with altered gut microbiomes, lower rates of food





Jonathan Hourihane,
with five-year-old Eleanor and



allergy, and reduced exposure to people and environments outside of the home. While there were benefits of lockdown to infants, at two years of age parents of CORAL children were increasingly concerned about their child’s communication and social development – raising important questions about how lockdownrelated factors such as limited social interaction and environment may affect early milestones.
Lockdown babies were breastfed for longer and had fewer courses of antibiotics. These changes were associated with altered gut microbiomes, lower rates of food allergy, and reduced exposure to people and environments outside of the home.



Now, a follow-on study – FLORAL (follow-on to CORAL) – is underway. This new national cohort includes babies born in the same three months of the year, but into a nonpandemic environment in 2025. These babies will undergo the same assessments at 6, 12, and 24 months, with research visits beginning in September. In parallel, the original CORAL cohort, now five years of age, are currently being reassessed to examine the medium-term influences of the COVID-19 pandemic.
FLORAL is the only study worldwide capable of directly comparing child health outcomes between pandemic-born infants and those born post-pandemic. The findings will provide invaluable insights into how global events shape early human development – and how we can better support children’s health during future public health crises.
Children First Awareness Week 2025 takes place 15 to 21 September. This is the third national public campaign to raise awareness about child safeguarding across Ireland.
The HSE Children First National Office is delighted to be supporting this year’s campaign, working with government departments, state agencies and community services.
Within the HSE, safeguarding is part of everything we do. It means making sure children are safe, responding to concerns about their welfare, and creating environments where all children and young people can thrive.
This year’s campaign theme is: We were children once. Now we are Children First.
This message reminds us that we all share the experience of being a child. That memory helps us care more, act responsibly, and understand the importance of putting children first in our work and decisions.
By saying, “We are children first”, we are committing to treating childhood as something precious, something to be protected.
It’s a key part of the HSE’s duty of care, and a responsibility shared by everyone working in our services.
The 2025 campaign places a new focus on reaching parents and responsible adults, expanding the reach of children first principles beyond professional and organisational settings. It recognises that the most powerful safeguarding often begins in everyday spaces, in clubs, schools, and communities, and is enacted by ordinary people who care deeply.
The 2025 campaign encourages all of us, whether working directly with children or not, to think about how children first principles apply in everyday practice. Safeguarding isn’t only about policies or procedures. It’s about the culture of our workplaces, our services, and our conversations. We all have a role, whether we are healthcare professionals, administrators or support staff.
Together, we can make safeguarding stronger by raising awareness and supporting a shared understanding of what it means to put children first.
We are asking all services and staff, including in our funded and contracted services to:
• Share the key messages during the Awareness Week – drive your own campaign using the resources made available.
• Promote understanding of staff responsibilities under children first – reminding staff of what to look out for and how to respond can never be repeated enough.
• Visit hse.ie/childrenfirst for more information, supports, and contact details for your area’s HSE children first training and development officer. Let’s make sure the protection and welfare of children and young people is always at the centre of what we do.
Child safeguarding is everybody’s business. For more information, scan the QR code or visit hse.ie/childrenfirst
The incidence of inflammatory bowel disease (IBD) in Irish children has increased fourfold since 2001, and is among the highest in Europe. Children’s Health Ireland (CHI) is at the international forefront of tackling this debilitating childhood disease. The multidisciplinary IBD team of medical, nursing and health-andsocial care professionals care for over 700 patients aged under 16 years. Regional paediatric centres are pivotal to ensuring timely referrals and delivering care closer to home, through shared-care partnerships with CHI.
Clinical and translational research is embedded within the service,
advancing biomarker-led precision therapies, clinical trials, setting international clinical guidelines, and improving patient outcomes – all stemming from the DOCHAS (Determinants and Outcomes of Children and Adolescents with IBD) Research Group. Recent innovations include National Clinical Programme investments in endoscopy and staffing (gastroenterologists, clinical nurse specialists, advanced nurse practitioners); infusion modifications (biosimilars, off-site infusions, shorter stays, nurse-led admissions, therapeutic drug monitoring), genomic testing, dietary therapies, virtual clinics and

remote disease monitoring. Children and adolescents still face significant challenges: the solitude of chronic disease, stigma, limited supports for those most impacted (financially, educationally, psycho-socially); inequitable access to medical therapies available to Irish adults, or children in other countries; a lack of dedicated psychology and social work supports.
The outlook for paediatric IBD is one of hope and expectation that advances in our diagnosis and treatments will enable young people to do what they want to do, be what they want to be, and manage their IBD, rather than it managing them.
In July, the HSE launched a new national clinical guideline for early diagnosis and management of venous thromboembolism (VTE). The guideline aims to standardise VTE care across Irish hospitals, reduce preventable harm, and ultimately save lives.
VTE affects approximately 5,000 people each year in Ireland, and it is reported that more than 1 in 12 people will experience a VTE event in their lifetime. Risk increases significantly with age, reaching over 5 in 1,000 annually among those aged 80 and older.
The new national clinical guideline, also known as Eve’s Protocol, is designed to improve the prevention, diagnosis and treatment of VTE, including deep vein thrombosis (DVT) and pulmonary embolism (PE). It reflects best international practice as defined by the International Society on Thrombosis and Haemostasis and the European Society of Cardiology.
The guideline is named in memory of Eve Cleary, who tragically died due to VTE.
Speaking after the launch, Eve’s mum Melanie said, “We are so proud to see the implementation of Eve’s guidelines and all that’s been achieved in Eve’s name. These national clinical guidelines will save lives. While you can never stop blood clots, these guidelines will stop the complications attached to VTE. Eve’s legacy will live on.”
Dr Colm Henry, Chief Clinical Officer, HSE added, “Enhanced awareness of VTE is critical to reducing the harm associated with this condition, which can occur in all settings. Eve’s Protocol addresses this need, raising awareness of its signs and symptoms, among both patients and healthcare practitioners. These guidelines are a clear confirmation of the immense value of clinical leadership and the power of multidisciplinary collaboration in shaping our future health service.”
“Many cases of VTE go undiagnosed until serious complications develop,” said Professor Fionnuala Ní Áinle, Consultant Haematologist and Clinical Lead for the National Clinical Programme in VTE (NCP-VTE). “This guideline is designed to change that, ensuring we identify those at risk, raise awareness among patients and staff, and provide a structured approach to care.”
Pathway to recovery: Comprehensive patient education materials
The new guideline is intended for use by all healthcare professionals involved in the prevention, diagnosis and treatment of VTE, including DVT and PE. Under the leadership of Sarah Garvey, Advanced Nurse Practitioner in VTE with the NCP-VTE, a suite of patient education materials is also being co-launched alongside the guideline.
The full set of patient materials is available on the HSE website at bit.ly/VTEResources

is
This is the formation of a clot inside a blood vessel, usually in the leg, which may break off and go to the lungs. This can be fatal. Blood clots can be very serious, but there are effective treatments to deal with them and help prevent them.
Signs and symptoms of a blood clot
• Swelling or pain in one leg or arm
• Warmth or redness in the leg or arm
• Shortness of breath or rapid breathing
• Chest pain (particularly when breathing deeply)
• Coughing or coughing up blood
If you have one or more of these symptoms, you may have a clot and need urgent treatment.
What can I do to help myself?
Ask for your risk of blood clots to be assessed, especially if you are in one of the higher risk groups.
• Walk and move as much as possible
• Drink plenty of fluids
• If directed to use stockings or medication to prevent or treat a clot, follow instructions exactly
A blood clot in the veins is more likely up to 90 days after being in hospital.
If you have any signs or symptoms of a clot, take immediate action to seek medical help.
In June, the Human Tissue Act (Part 2) came into effect to provide a national legislative framework for organ donation and transplant services.
The new law introduced a soft opt-out organ donation system, which means that you agree to be an organ donor when you die, unless you opt out. If you die and are eligible to donate your organs, your next of kin are always consulted before any action is taken, and if they do not give consent, then the donation does not proceed. If you do not want to donate your organs, you can opt out by adding your name to the opt-out register, and in this case your next of kin will not be approached about organ donation. The optout register was developed and is being maintained by the HSE.
Whatever you decide, please let family and friends know your decision, so they can honour it.
The Act also provides a framework for living donation and for the first time provides a way for people to donate a kidney to someone they
LET'S TALK
don’t personally know, called non-directed altruistic donation. The kidney recipient must be someone on a waiting list who needs it, and the Act includes additional protections and safeguards for this.
Speaking in June on the day that the law came into effect, Dr Colm Henry, Chief Clinical Officer said, “The opt-out organ donation system will bring us in line with international best practice. Organ transplantation is one of the great advances in modern medicine. It offers a second chance at life to people with life-threatening illnesses or injuries to their vital organs. Every year, more than 200 people in Ireland have their lives improved or saved by the gift of organ donation.
“At any given time, approximately 600 people in Ireland are on waiting lists for organ transplants,” Dr Henry continued. “I encourage you to have a conversation with your family or next of kin and let them know your wishes around organ donation.”
Dr Brian O’Brien, Clinical Director, HSE Organ Donation Transplant Ireland added, “Not everyone who dies is a potential organ donor. A donor needs to be in hospital and on a life support machine. All organs donated go to people most in need of a transplant. Consent is at the heart of this change. It is important to inform your family and friends about your decision regarding organ donation, as they will always be consulted, and your wishes should be central to any decision.”
To find out more information on organ donation and the opt-out register, visit hse.ie/organdonation or watch the following videos…
• A message from Dr Colm Henry – bit.ly/CCOOrganDonationVideo
• Explainer video in English with Irish sign language – bit.ly/HSEOrganDonation
• Explainer video in Irish with Irish sign language – bit.ly/DeonuOrgan

Regional Executive Officer (REO) Martina Queally and Integrated Healthcare Area (IHA) Manager of Dublin South and Wicklow Aisling Heffernan were delighted to visit disability services in Arklow, Co Wicklow on 10 June. They met with service users and team members from Enable Ireland’s
Adult Day Service, Avoca River House and Rehabcare’s Day Service, Bridge’s Edge. During their visit, the REO and IHA Manager heard about the multidisciplinary and personcentred model at Enable Ireland, and enjoyed a tour of the renovated premises at Bridge’s Edge, including the peaceful and calming space provided by the new sensory garden.

Sinéad Long, Senior Occupational Therapist, Psychiatry of Later Life Team, HSE, with the “Dementia Bus”.
Earlier this year, colleagues from across HSE disciplines participated in a virtual dementia training programme in Kilkenny, in which participants were able to simulate the cognitive and sensory impairments associated with dementia, with the aid of a specially-modified bus. As part of the “Dementia Bus” training, an eight-minute virtual reality immersive experience was followed by a 75-minute comprehensive training session, detailing what was happening in the brain during the virtual tour. It was designed as a first-hand and practical contemplation of the difficulties individuals with dementia face, including disorientation, confusion and memory loss. Two days of training for HSE staff, and some carers and relatives of service users experiencing dementia, were provided. This was organised by the occupational therapy staff in the Psychiatry of Later Life team and the multidisciplinary team in St Gabriel’s Ward (Kilkenny) within the HSE’s Carlow Kilkenny and Tipperary South mental health services. The training took place on the grounds of St Canice’s Hospital in Kilkenny.
Magic Table helping those with dementia

An interactive sensory installation, known as a Magic Table, is proving a popular feature for residents in St John’s Community Hospital in Enniscorthy, Co Wexford.
The Magic Table (or Tovertafel in Dutch) is an award-winning console innovation from the Netherlands that uses specially designed technology to help people with mid-to-late-stage dementia.
The Magic Table consists of a series of colourful and fun, interactive light games projected onto the surface of a table, which respond to hand and arm movements. It is designed to stimulate physical and cognitive activity, as well as encourage social interaction. The Magic Table supports healthcare staff in providing personcentred care at any time of the day and helps to manage behavioural symptoms associated with dementia. The HSE’s Nursing Midwifery Planning and Development Unit supported and funded St John’s Community Hospital in this project.
A new eight-week Bray Outdoor Mobility Programme has been developed collaboratively by the Bray Primary Care Centre physiotherapy team, Health Promotion, and the Physical Activity for Health Officer.
The programme is designed for people who are mildly frail or pre-frail and would benefit from exercise to help prevent further decline. The goal is to improve outdoor mobility, which can support independence, increase opportunities for physical activity, and reduce social isolation. There is huge demand for primary care services like physiotherapy and, as a result, accessing clinic space for group sessions has become more

challenging. This new outdoor programme lessens this challenge. The idea arose from discussions during an older persons integration workshop, where the physiotherapy manager expressed an interest in

Earlier this year, Dungarvan Community Hospital were delighted to be presented by the Waterford County Museum Society with a series of framed photographs, for display in corridors, common areas and foyers in the hospital complex.
The Museum Society runs a museum premises in Dungarvan and also hosts a collection of over 5,000 historical images on their Waterford County Images website. It is from this resource of heritage photographs that a selection, featuring locations and people (some of them well known) from Dungarvan and surrounding areas, was gifted to the hospital to serve as conversation pieces for residents, staff and visitors.
developing a programme similar to the Walk and Talk programme in Churchtown.
Participants received step counters and Healthy Ireland packs with 13 people attending the first walk.

Congratulations to University Hospital Waterford (UHW) who won the Best HSCP Led Project award for Occupational Therapy Led Reablement at the Bright Spark National Innovation Awards 2025 in June. This collaboration between the Acute Occupational Therapy Department at UHW and HSE Older Persons Home Support Services promotes patient flow by providing targeted, home-based rehabilitation for older adults who have been discharged from UHW.
Megan Walsh, Senior Occupational Therapist at UHW (pictured centre) and the team were presented with the award at the Spark Summit in the Dublin Royal Convention Centre on 11 June.

The Royal Victoria Eye and Ear Hospital (RVEEH) is leading the national sustainability drive with Ireland’s first full-cycle sustainable waste solution. On 1 May, the hospital launched its hospital-grade, medicalised, thermophilic biodigester, capable of processing both biodegradable clinical and food waste on site. Developed through a collaboration between HaPPE Earth and Harp Renewables, the biodigester marks a national milestone in sustainable healthcare practice.
As a circular economy innovation, the thermophilic biodigester will transform over 20 tonnes of annual food and compostable clinical waste into reusable compost. It is designed to handle splash aprons, shoe covers, biodegradable PPE, and emerging plastic alternatives. RVEEH currently relies on more than 320 site waste collections annually. The new system reduces this dependence, lowers transport emissions, and enhances local waste management.
Speaking at the official launch, Alan Dillon TD, Minister of State for Small Business and Retail and Circular Economy said, “The Royal Victoria Eye and Ear Hospital is setting a benchmark for sustainability in clinical operations. This project will cut emissions and will lead by example, showing how hospitals can manage waste with environmental responsibility.”
It’s about doing the right thing for the future of sustainability in healthcare in Ireland and about the hospital achieving the goal of a 50% reduction in our carbon footprint by 2030.
Ash Dallsingh, Chair of the Sustainability Committee at RVEEH added, “This project aligns with our strategic pillars. It’s about doing the right thing for the future of sustainability in healthcare in Ireland and about the hospital achieving the goal of a 50% reduction in our carbon footprint by 2030.” The initiative forms part of a two-year research and evaluation partnership to assess biodigestion in clinical environments, including its ability to process additional materials and integrate with nextgeneration thermophilic technologies.
Data gathered during the pilot will inform peer-reviewed findings with academic partners, contributing to future evidence-based waste policy in healthcare. RVEEH is committed to embedding sustainability in patient care and leading by example across the health sector.
On Thursday 22 May, in collaboration with An Garda Síochána, the HSE Dublin South and Wicklow Anti-Human Trafficking team supported a wellpublicised day of action in Dublin Airport.
The event was the first in a planned programme of action to highlight and tackle human trafficking. The team was present to provide advice around how the HSE Anti-Human Trafficking team are supporting identified victims of human trafficking.
There were also other NGOs involved in the event, including Ruhama, an Irish NGO and registered charity that offers nationwide support to women impacted by prostitution, sex trafficking and other forms of commercial sexual exploitation.

Stakeholders taking part in an anti-human trafficking event at Dublin Airport.
On 1 May, following a year of collaboration between the hospital and community, a new improved discharge process was launched. This coincided with the launch of the new Maternity Healthcare Records in Wexford General Hospital and the National Postnatal Maternal Public Health Nurse Record. The initiative was supported by the multidisciplinary team, including the clerical administration in the hospital and the community.
The aim of this initiative was to enhance the information the public health nurse would receive in order to provide a more informed, patient-centred approach at the first visit to mother and child – giving value to the mother’s health as well as the child’s. This consists of a discharge checklist for each mother, which includes information about her own health, including blood pressure, haemoglobin and general wellbeing, alongside a separate discharge checklist for the baby’s health, which includes baby observations, method of feeding and neonatal screening.
On 8 May, this initiative was celebrated at an information-sharing morning in the maternity unit in Wexford General Hospital to celebrate the International Day of the Midwife (5 May) and the Nurse (12 May).

An app specially designed for children due for admission to University Hospital Waterford (UHW) was launched earlier this year. Paediatric and theatre department nurse specialists in UHW worked with a company called Little Journey (UK) to develop this platform for children. The app enables children and their families to view the hospital environment the child will spend time in while they are having elective (planned) surgery or pre-booked blood tests.
Parents and guardians can download Little Journey and it will give a virtual tour of the paediatric ward and the theatre environment at UHW. The aim of the app is to reassure children and help them and their families to prepare and be less worried about their essential “little journey” to UHW. The app also has interactive games that are aimed at distracting children while they are examined or having bloods taken. There will also be lots of helpful information in the app to support parents.
Addressing global health challenges requires collaboration between countries around the globe. I currently work as an epidemiologist in HSE Dublin and South East. In summer 2024, a memo about special leave with pay to volunteer in an exceptional humanitarian crisis for Gaza was circulated in my department. This scheme facilitates the release of public health service staff with specialised skills and expertise to respond to the humanitarian needs of affected countries.
I immediately decided to sign up. Helping people in need and believing in humanitarian principles and ethics were my motivations. The Gaza situation was designated as an exceptional humanitarian crisis. The United Nations Relief and Works Agency for Palestinian Refugees in the Near East (UNRWA) was looking for an epidemiologist to support the surveillance system. UNRWA, as a UN agency, was established after the 1948 conflict to provide relief and work programmes for Palestinian refugees. I joined the UNRWA health department in Amman HQ, Jordan for six weeks.
I supported the surveillance system in
On 12 May, the HSE and the Nursing and Midwifery Planning and Development Unit (NMPDU) proudly celebrated International Nurses Day by honouring the essential contributions of nurses and midwives to evidence-based practice and innovation in healthcare delivery.
Now in its second year, the MENTORR programme – a collaborative initiative between South East Technological University (SETU), the HSE and the NMPDU – has become a cornerstone of research-led professional development. Over a 12-week period, 17 nursing and midwifery professionals were supported through the research cycle, from idea generation to proposal development. The programme culminated in a vibrant regional research showcase at SETU’s

UNRWA during my deployment. Conflict and wartimes create suitable conditions for infectious diseases to emerge and spread. Similarly, the infectious diseases under surveillance increased to alarming levels in Gaza. I could find the chance to experience how the surveillance system could cope with the surging cases in the conflict zones and take necessary actions to control outbreaks and transmission. Moreover, all the work was being conducted under scarce resources and a challenging environment. This was a unique opportunity to expand my knowledge about infectious disease surveillance in humanitarian settings, and my understanding of problemsolving and decision-making, which will have a positive impact on my current role. I would like to express my gratitude and thanks to the UNRWA Health Department in Amman, HSE Global Health department, and the Department of Public Health, HSE Dublin and South East, in particular my colleagues in surveillance.
O’Connell Bianconi building. Participants presented their work through dynamic pitch sessions and academic posters, addressing real-world challenges across acute, community, and integrated care settings. Their research proposals offered practical, patient-centred solutions aimed at improving outcomes and enhancing service delivery. In today’s complex healthcare environment, it is vital that clinical care is informed by robust evidence. Nurses and midwives are not only caregivers – they are educators, innovators and researchers. Through initiatives like MENTORR, the HSE and the NMPDU are fostering a culture of inquiry and continuous improvement, ensuring that clinical decisions are grounded in the latest knowledge and best practices.
As part of ongoing efforts to regionalise and optimise gastrointestinal (GI) endoscopy services, the HSE Dublin and South East service improvement team recently brought together staff from seven hospital sites for a focused improvement event. The aim of the event was to strengthen service delivery, share best practices and ensure more consistent, highquality care for patients.
Key areas of focus:
• Aligning with national protocols
• Making better use of existing resources
• Supporting staff with training and tools
• Enhancing monitoring and oversight
Regional workstreams are now underway to turn ideas into action. This collaborative effort will help ensure more timely, equitable and efficient care for patients needing GI endoscopy services.

HSE Dublin and South East were delighted to welcome Minister for Health Jennifer Carroll MacNeill TD for a number of site visits and openings over recent months.
On 11 June, the Minister officially opened the Dr Kathleen Lynn Cataract Unit at the Royal Victoria Eye and Ear Hospital (RVEEH). The theatre, which will greatly improve access to cataract surgery for patients across Ireland, is named in honour of Dr Kathleen Lynn, a pioneering Irish physician, activist, and the first female doctor on RVEEH’s staff in 1910.
The new facility, which includes the addition of a second theatre, will increase the number of cataract surgeries performed annually from 4,300 to 6,000. This will help the hospital meet the Sláintecare target of 50% of patients waiting less than 12 weeks for their procedure.
On 13 June, the Minister officially turned the sod on the Waterford Surgical Hub, a new state-of-the-art healthcare facility designed to reduce patient waiting times in the South East. The completed development will comprise of four
new theatres, which will deliver additional capacity to support scheduled care for day cases, and allow existing acute capacity to support urgent and more complex procedures at University Hospital Waterford.
During her visit to Waterford, the Minister also officially opened the HSE’s new Integrated Healthcare Hub at St Otteran’s Complex. Specially developed as a facility to accommodate outpatient appointments across three consultant-led disciplines, the Hub will co-locate audiology, orthodontics, and ophthalmology services, which were previously delivered at University Hospital Waterford and other community settings.
including calling to the short and long stay accommodation for older people, to the Waterford Integrated Care for Older Persons (WICOP) Centre and Aidan’s Residential Healthcare Unit (managed by mental health services).
The Minister was accompanied on her Waterford visit by Government Chief Whip and Minister of State for Mental Health Mary Butler TD and Minister of State for Local Government and Planning John Cummins TD.
Then on 27 June, the Minister joined patients and staff at the National Rehabilitation Hospital (NRH) in Dún Laoghaire as they celebrated the success of phase one of the hospital’s major redevelopment project.

Minister for Health Jennifer Carroll MacNeill TD meeting cataract patients at the Royal Victoria Eye and Ear Hospital.
The new, multi-award-winning rehabilitation hospital is a country first, purpose designed to accommodate the needs of patients requiring complex specialist rehabilitation services. The building was completed and opened on time and within budget in 2020. The move to the new hospital was a momentous occasion for patients and for staff who had worked to accomplish completion of phase one of the project, but were unable to celebrate the opening due to the difficulties of the COVID-19 pandemic at the time.
The Minister also visited Waterford Primary Care Centre, John’s Hill and the Waterford Residential Care Centre campus,
Many retired and former staff who were involved for many years in the planning and design phases of the redevelopment returned to celebrate with current staff and patients on the fifth anniversary of the transition to the new hospital.



Driving safer, connected and patient-centred care, improving healthcare delivery for both staff and patients in Ireland


Thousands of hospital and community appointments are being added in the latest release of the HSE Health App, allowing many more patients to see their health service appointment on their phone.
Over 140,000 people have downloaded and are using the HSE Health App since its launch in February 2025. Hospital appointments for maternity services were available in the first release. We are now adding thousands of additional hospital and community appointments for sites across the country in the latest release.
Features now available include:
• Increased numbers of hospital and community appointments for sites nationwide
• Hospital appointments for maternity
• Digital versions of your European Health Insurance Card, Drug Payment Scheme, long-term illness and medical cards
• List of self-declared and reimbursed medication
• Flu vaccination and COVID-19 records
• Information about urgent and emergency care services
• Health A-Z
• BreastCheck screening appointments


We’re asking staff to download the HSE Health App and encourage patients and the people who use our services to download and use the app, too. The HSE Health App team is working with nominees from each health region to make more appointments available in the app across our acute hospitals and specialities.
Other additional features have been added, including week-by-week healthy pregnancy information and QUIT smoking programme support. Creating a quit plan is a great first step for smokers when they’re preparing to quit.
HSE Live (freephone: 1800 700 700) is there to provide support to people if they need it when using the app. If people don’t want to or can’t use the app, they can still access services and healthcare in the usual way.
Over time, the app will continue to evolve to become the main channel for people to securely access their health information and a range of services online. The HSE Health App is available in Irish and English. Other languages are being explored for future versions. Any member of the public aged 16 and over can use the HSE Health App.
You can find more information on the HSE Health App at hse.ie/health-app
As a number of key digital health programmes gain momentum, we are beginning to see how the vision of the Digital for Care framework can become reality.
Digital for Care is not just about technology and the digitisation of paper records – it embodies so much more. It’s about nationwide transformation that will integrate care across hospitals and communities, empower patients and improve clinical decisionmaking to name but a few benefits. Through the implementation of key
platforms such as Telehealth services, the HSE Health App and many more ongoing infrastructural systems, the foundation is being set for more connected, efficient health services.
This transformation will not come without its challenges. Critical to its success is the process of guiding and including everyone through the changes involved. As we progress plans for a national electronic health record (EHR) and other key programmes, we understand the importance of clinical leadership
The HSE’s Virtual Wards has seen 1,426 patients in their first year of operations, as part of digital innovation at St Vincent’s University Hospital (SVUH) and University Hospital Limerick (UHL). This means patients are treated in the comfort of their own homes and avoid hospital stays.
Additionally, 12,800 patient bed days have been saved, meaning hospitals have freed up 12,800 beds from their physical capacity and can treat more people and reduce trolley numbers. For every one patient on the virtual ward, two patients are affected – the virtual ward patient and the acute patient who got their hospital bed.
Virtual wards support the remote care of patients who would otherwise be in a hospital bed. Currently, there are 22 clinical pathways live, meaning there are 22 entry points across the hospital to the virtual ward. The service may be offered to suitable patients who are admitted to hospital across a range of specialities, including cardiology, respiratory, general medicine, gynaecology, rehab, stroke and orthopaedic specialities.
The national Virtual Wards programme is the empowerment of patients to be active partners in managing their health and wellbeing. Patients remain under the care of the consultant-led team that provided their care in the hospital and will have a dedicated team monitoring their care 24/7, while they are in the comfort of their own homes.
Another programme within Telehealth making steady progress is Attend Anywhere, the online video health appointment. This affords patients and service users the opportunity to attend clinical and healthcare appointments in the comfort of their own homes,
and patient inclusion from the outset. We also understand the requirement to enhance digital health literacy and shifting our culture to that of collaborated and integrated care through transparent communication at every stage.
“While the scale of this ambition is huge, so is the commitment, making for a stronger, smarter health service for the future.”
– Damien McCallion, HSE Chief Technology and Transformation Officer and Deputy CEO.
• HSE’s Virtual Wards saves 12,800 bed days in first year of operations
• 1,426 patients treated in their own homes, avoiding hospital stays

avoiding time and money spent travelling to and from appointments.
Patients can ask their healthcare professional if they do video appointments. These are available across a range of services, where clinically appropriate, including:
• Physiotherapy, dietetics, occupational therapy and speech and language therapy
• Follow-up with a consultant; for example, to get results
• Mental health care
• Chronic disease management
• Maternity care
• Postnatal care such as lactation consultants and more
University Maternity Hospital Limerick (UMHL) has implemented the national Maternal and Newborn Clinical Management System (MNCMS), a digital transformation that marks a major step forward in delivering safer, more coordinated maternity, neonatology and gynaecology care across the region.
The MN-CMS electronic health record (EHR) system went live at UMHL on 5 July, and at the ambulatory gynaecology unit in Nenagh Hospital on 7 July, including menopause and fertility care. UMHL and Nenagh Hospital now join Cork University Maternity Hospital, University Hospital Kerry, the Rotunda Hospital and the National Maternity Hospital in this national initiative.
Replacing traditional paper records, MN-CMS allows doctors, midwives, nurses and allied health professionals to access real-time patient information, improving communication and clinical decision-making across hospital and community settings.
Key benefits of MN-CMS include:
• Enhanced patient safety through instant access to clinical data
• Streamlined, legible documentation that reduces duplication
• Improved multidisciplinary communication
• Support for research, audit and data-driven service planning
• GDPR-compliant, secure information sharing
Dr Mendinaro Imcha, Clinical Director of Maternal and Child Health, HSE Mid West said, “This is a major step forward in delivering safe, evidence-based care. It enhances communication and ensures a more seamless experience for women and families.”
Eileen Ronan, Director of Midwifery at UMHL added, “The system improves access to clear, up-to-date records, making the patient journey safer and more efficient.”
The MN-CMS project began in 2007, with extensive consultation across Ireland’s 19 maternity units. Cerner was appointed as the system vendor in 2014, and phased roll-out began in 2016 under the National Women and Infants Health Programme. The remaining 14 maternity hospitals will adopt the system in future phases.


Top: Pictured at UMHL on Day One of the MN-CMS go live were, from left: Anne Rice, CAE Oracle Cerner; Martina Burns, Delivery Director for Acute Hospitals, Technology and Transformation, HSE; Eileen Bourke, Senior Project Manager, MN-CMS; Eileen Ronan, Director of Midwifery, UMHL; Fran Thompson, CIO, Technology and Transformation, HSE; Liz McInerney, Business Manager, Maternal and Child Health, HSE Mid West; Catherine Jinks, MN-CMS EHR and Women and Infants Health Services Programme Manager; and Eimear Tobin CMM3, Project Manager MN-CMS, HSE Mid West.
Bottom: Pictured after go-live at the ambulatory gynaecology unit in Nenagh Hospital were, from left, Danielle Freeman, Staff Nurse; Aine Brennan, Staff Nurse; Dr Mantas; Aisling Mulcahy, Clinical Nurse Specialist; Sophie Carroll, Admin; Brian Keogh, Chief Pharmacist, MN-CMS NPT; Catherine Henry, Advanced Nurse Practitioner; Amanda Stephens, Admin; and Joan Malone, Gynaecology Workstream Lead MN-CMS NPT.
Fran Thompson, HSE Chief Information Officer praised the “exemplary” work of the Mid West team: “The leadership and dedication shown by the team have ensured a successful go-live. This is a key milestone in delivering digitally enabled, connected care and empowering patients as partners in their healthcare journey.”
The introduction of MN-CMS at UMHL reflects the HSE’s commitment to safe, integrated and person-centred care. As the system expands nationwide, it will continue to support the transformation of maternity services in line with Sláintecare and the Digital for Care strategy.


Unlocking the full power of M365
Many HSE staff first encountered Microsoft Teams through virtual meetings. But Teams is just the beginning – Teams is one of many tools in the Microsoft 365 suite designed to help you work better, faster and more collaboratively.
With Teams, you can create shared workspaces where colleagues across the country can chat, call and collaborate in real time. Everyone sees the same up-to-date version of documents, reducing confusion and duplication.
“Teams with SharePoint has eliminated a lot of duplication for our team. It’s easier to find files, manage emails, and communicate with external stakeholders.”
– Niamh Walker Headon, Library Resources Manager, HSE Library HQ
Where to start
Visit office.com, log in with your HSE email and password and click on “Apps” to explore tools like:
• Planner – for task management
• Forms – for collecting feedback
• OneDrive – for secure file storage
• Teams – for team collaboration
Tackle workload with smart tools
Feeling overwhelmed? M365 can help you stay on top of your tasks:
• Planner lets you organise work into buckets like “To do”, “In progress” and “Done”. Assign tasks, track progress and share visual updates with your team.
• Forms makes it easy to gather feedback or input from HSE colleagues without endless email threads.
One version for all Forget emailing documents back and forth. With M365:
• Store shared files in Teams so everyone can edit and comment on the same version.
• Save drafts to OneDrive for secure access from any HSE location. Share links when ready or move files into a Teams channel for broader collaboration.
“Using MS Teams and SharePoint has improved how I collaborate with dietetic teams across the country. It’s made resource development more efficient and impactful.” – Suzanne Seery, Clinical Specialist Dietitian
Smarter training and scheduling
Delivering training or managing meetings is easier with M365:
• Use Teams webinars to create speaker bios and allow attendees to register in advance.
• Scheduling Assistant helps you find availability without sending multiple emails.
• Attendance tracking and followup tools streamline session management.
“OneDrive makes the day-to-day workings of a multi-site team so much more efficient. Files are always available and up to date.”
– Kate Togher, Clerical Officer, Primary Care, Limerick
Get support and training
The O365 Adoption Team offers live training on Teams, OneDrive, SharePoint and Planner – no registration needed. Find dates and session times at: bit.ly/HSEstafftraining
Need tailored advice? Book a 30-minute clinic for your team by emailing: rosaleen.quinlan@hse.ie, Adoption and Communications Lead, O365 Team.
Hundreds of healthcare staff, patients and communities across Cork and Kerry came together to take part in HSE South West’s 2025 Gathering of Kindness, three heartwarming events focusing on placing kindness at the heart of healthcare.
The events took place at Cork University Hospital (CUH), St Mary’s Healthcare Campus Gurranabraher, and University Hospital Kerry (UHK). As HSE South West transforms to make Cork and Kerry communities proud of their health services, staff learned together how kindness, respect and human connection improve healthcare outcomes. Over three days, people took part in talks, performances and wellness activities – all designed to make kindness an organising principle of healthcare.
“HSE staff across Cork and Kerry came together in a very successful Gathering of Kindness,” says Dr Andy Phillips, Regional Executive Officer, HSE South West. “I have personally benefitted from the kindness of our communities across Cork and Kerry and am humbled by the kindness shown by our healthcare staff, often working in challenging situations. I am very aware that I need to make sure that our health system shows organisational kindness to our staff and to patients, holding myself accountable to the commitments we have made. In this year’s Gathering of Kindness, many people came together with a shared purpose of putting in place health services that, increasingly, have no one waiting on a trolley, or waiting a long time for an appointment.

“I am very grateful to our distinguished presenters, including Dr James Mountford, Editor, BMJ Leader; Professor Brian Dolan, known for his work on valuing patients’ time; and to Professor Cath Crock, who started the kindness movement in health 25 years ago. We all enjoyed the Hush Foundation music played by the Cork Band 1 Brigade and local musicians at CUH, as well as the plays performed by Graffiti Theatre Company at each venue.”

Events over the week included:
• Discussions at CUH on embedding intentional kindness in daily work.
• An outdoor gathering at St Mary’s Healthcare Campus in Gurranabraher, where the local community enjoyed food, wellness sessions, art activities and a tree-planting ceremony, celebrating kindness and wellbeing.
• A Kindness Tent on the UHK campus, which provided a space for creativity and learning, with discussions, theatre performances, music and conversations about kindness in healthcare.
At the Gathering of Kindness, staff shared experiences, stories and inspiring ideas on leadership, workplace culture and the impact of kindness across healthcare settings. Professor Dr Catherine Crock AM, Founder of Hush and Gathering of Kindness says, “Kindness is fundamental to positive relationships in healthcare. HSE South West’s Gathering of Kindness is a reminder that acts of kindness, respect, and human connection ripple outward, improving care for patients, wellbeing for staff and strengthening our communities. Seeing this movement embraced across Cork and Kerry is inspiring. Together we can make kindness a daily reality in every hospital and healthcare setting. Kindness makes healthcare safer for everyone.”

HSE South West has launched a new booklet that supports new mothers to mind their wellbeing during pregnancy and post-birth. Available to all expectant and new mothers across Cork and Kerry, it has useful advice on topics including nutrition, exercise, sleep, and mental health supports.
The booklet is a joint project between staff at Cork University Maternity Hospital (CUMH), University Hospital Kerry (UHK) and HSE South West mental health services. It was funded by HSE South West Connecting for Life (the regional self-harm and suicide reduction plan).
The team involved staff from the Perinatal Mental Health Service in CUMH and UHK including Dr Freda Wynne, Senior Clinical Psychologist; Breda Bird, Clinical Midwife Manager 2 (CMM2); Zodwa Lenihan, Clinical Midwife Specialist (CMS);

and Louise Chawke, CMM2. It also involved Martin Ryan, Resource Officer for Suicide Prevention, Cork; and Donagh Hennebry, Resource Officer for Suicide Prevention, Kerry.
The project team thanked and acknowledged HSE colleagues in HSE Dublin and South East, as this booklet took their work and built on it to make it suitable for families in Cork and Kerry.
“The booklet clearly outlines the fundamental elements of wellbeing: nutrition, exercise, sleep, and the importance of carving out time for oneself,” says Dr Freda Wynne. “It also addresses the mental health
The CUH/UCC Cancer Centre received its gold standard European accreditation in June at a ceremony in Athens and is now a designated Organisation of European Cancer Institutes (OECI) Cancer Centre.
The OECI accreditation certification ceremony took place as part of Oncology Days 2025, an annual conference bringing together cancer experts, clinicians, researchers and healthcare professionals.
This accreditation recognises excellence in cancer care, research, education and training. It marks a significant milestone in the development of the Cancer
Centre – a collaboration between Cork University Hospital and University College Cork – with strong regional support from HSE South West.
“We are working hard to continually improve outcomes for people with cancer and their families,” says Dr Andy Phillips, Regional Executive Officer, HSE South West. “Our accreditation requires us to deliver our Quality Improvement Plan with 25 actions that must be delivered over the next five years. I look forward to working with them to ensure that we do even better for the people we are privileged to serve.”
concerns that new mothers may face and directs them to the appropriate resources for support. Additionally, we have curated a comprehensive list of services, ranging from acute care to community-based family resource centres and online support.”
“This initiative exemplifies successful cross-disciplinary collaboration with the potential to significantly enhance the wellbeing of expecting and new mothers, as well as their support networks, including new dads,” adds Martin Ryan, Resource Officer for Suicide Prevention.

The CUH team celebrate receiving OECI accreditation at the Oncology Days 2025 conference in Athens.
Jane Shanahan, Assistant Director of Nursing, Cancer Centre, Cork University Hospital says the achievement is the result of years of hard work, dedication, and a shared commitment to delivering the highest standards in cancer care.
The Kingdom Dementia Café is a shining example of community collaboration and compassion in action. An initiative of Dementia Friendly Tralee, the café is the result of multiple agencies working together to create a safe, inclusive and welcoming space for individuals living with memory loss and their families.
Held on the first Thursday of every month from 11am to 12.30pm at The Rose Hotel, the café offers a judgement-free environment where attendees can enjoy refreshments, connect with others, and engage with a variety of guest speakers. A special highlight is the regular visits from the Kerry County Museum team, who bring historical artefacts that spark curiosity and conversation.
The café’s purpose is to reduce social isolation and promote community integration. It provides a space where people can speak openly about memory difficulties, fostering understanding, acceptance and a sense of belonging. Healthcare professionals are also available to offer guidance and signpost attendees to additional supports and services.
Regular attendees speak highly of the experience. Sheila shares, “When you attend The Kingdom Dementia Café, no one knows who has memory difficulties – everyone is the same. It’s such an inclusive place.” Ann adds, “It feels like a real treat to attend. Everyone is so lovely, and the staff at The Rose Hotel make us feel so special with the beautiful scones and coffee – they really spoil us.”
This community-driven initiative is more than just a monthly event – it’s a lifeline of connection, joy and dignity for those affected by dementia and memory loss in County Kerry.



“When you attend The Kingdom Dementia Café, no one knows who has memory difficulties – everyone is the same. It’s such an inclusive place.”
The Rose Hotel is a proud and active member of the Dementia Friendly Tralee Interagency Group, playing a vital role in supporting individuals living with dementia and memory loss. Staff members have completed dementia awareness training, which has significantly enhanced their ability to engage with empathy, understanding and compassion. This training is clearly making a difference. Staff have seamlessly put their learning into practice, creating a warm and supportive
environment that attendees of The Kingdom Dementia Café deeply appreciate. People travel from all corners of the county to attend the café, with a dedicated core group of around 25 individuals participating each month.
The Rose Hotel’s commitment to inclusivity and hospitality has helped make the café a safe, welcoming, and stigma-free space – a place where everyone feels valued and supported. Tea and coffee, in good company is guaranteed.
If you are interested in joining, please pop along to the next catch-up or contact Mary Hennessy for more details: mobile: 085 114 9078, landline: 066 717 1177, email: mtrr@bailemhuire.ie.
The aim of breastfeeding support groups is to provide professional and peer support for mothers in the community to initiate and sustain breastfeeding. There are 27 HSE-led support groups across Cork and Kerry. The West Cork breastfeeding support groups operate in Bantry Primary Care Centre (Wednesdays, 10.30-11.30am) and Clonakilty (Tuesdays 10.30-11.30am). They have been working innovatively with Cork County Council to support mums who require hospital-grade breast pumps and positioning pillows to support their journey. These community resources were funded by the council, and public health nurses can access them for mothers in a timely manner.
This is a huge improvement in access and environmental sustainability. A further significant improvement is the development of the advanced nurse practitioner role – Sheila Lucey can diagnose, prescribe and treat breast issues such as mastitis in the community, allowing

mothers to be cared for close to home. Sheila works closely with Cork University Maternity Hospital (CUMH) and the GP network.
National Breastfeeding Week runs 1-7 October and there are many exciting free celebrations and learning
Residents recently moved into the new extension at Millstreet Community Hospital in Co Cork, enjoying 11 single en-suite bedrooms as well as a bright dining room and sitting room. The move is part of an ongoing programme of extension and refurbishment, which is taking place in two phases. The residents’ move from the existing building into new accommodation also allowed phase 2 to commence, which is the refurbishment of the old building.
Acting Director of Nursing Ger Murphy says the team at Millstreet Community Hospital were delighted to welcome residents to their new accommodation, with rooms that offer more privacy and a better standard of accommodation: “Our over-riding aim is to achieve and sustain a high-quality care environment at Millstreet Community Hospital that cares for, supports and values residents in a safe and comfortable environment. These new rooms will help our dedicated team in this aim.”
opportunities planned for professionals and the public in South West. These events are being delivered collaboratively in the community support groups, in CUMH and Kerry General Hospital, in libraries and online.

HSE South West Head of Older Persons Services, Jackie Daly adds: “We thank everyone involved in the project to date, including the residents and staff who have patiently waited for this phase of the development to be ready for occupation. We are delighted to be in a position to move away from shared open wards to single rooms, which offer more privacy and en-suite bathrooms.”

HSE South West proudly held two days of fun while promoting positive mental health over the summer months.
In August, Together at the FairGreen in Midleton launched a vibrant series of community events focused on connection, mental health and wellbeing. The initiative gained further momentum in September with the fourth annual Together at the Castle in Mallow Castle, drawing thousands for an uplifting afternoon of music, dance, food and open conversations around mental health. The events were organised by HSE South West in partnership with Cork County Council, local chambers, HSE colleagues, and over 50 community organisations. Resource Officer for Suicide Prevention, Martin Ryan spoke on the huge success of this year’s events adding that “our events exemplified cross-sector
collaboration, reinforcing the concept that suicide prevention is everyone’s business.”
The festival welcomed families, friends and individuals of all ages to engage in interactive activities and discover the many supports available. Declan Cronin, Head of Mental Health Services called it “a powerful reminder that mental health is a shared journey,” while Mallow Committee representative Sharon Cregg praised the strong community spirit. The events aligned with the See Change Green Ribbon campaign and Connecting for Life Cork, highlighting key messages around stigma reduction and help-seeking. Through inclusive programming and heartfelt dialogue, Together at the Castle demonstrated how shared responsibility, connection and openness foster hope and healing within communities.
HSE South West and local libraries joined together to mark Infant Mental Health Awareness Week 2025. Babies, toddlers and their parents enjoyed a week of free events, including fun activities and information about infant mental health. Throughout the week, parents, expecting parents, carers and families took part in free talks, playgroups and storytelling sessions, all aimed at supporting infants’ emotional and social development. Rachel Knox, Child Health Programme Development Officer, HSE South West says awareness of infant mental health is very important: “A baby’s brain grows quickly in the first three years. Every interaction helps shape their future health and happiness. Relationships in these early years set the groundwork for a baby’s ability to regulate emotions, form secure relationships, and explore their environment.

Ceol, craic and CPR training were all on offer at a free Men’s Health in the Community event at the CYMS Hall in Killorglin in Co Kerry during Men’s Health Week. This annual community event brought together a wide range of HSE South West health professionals to offer advice – including physiotherapists, dietitians, public health nurses, health promotion officers and occupational therapists. Local community groups such as the South Kerry Development Partnership and Local Link Kerry attended, and the Killorglin Men’s Social Club Choir performed. Free blood pressure checks, free CPR and defibrillation workshops, and health checks in local pharmacies were all on offer. Project lead Michelle Foley, Health Promotion and Improvement Officer with HSE South West, says it was a wonderful opportunity for men in Kerry to meet with a range of health and community professionals in a onestop-shop, with a focus on health awareness, prevention and increasing access to services.
The annual event was one of a series planned by HSE South West across Cork and Kerry, with hundreds of men turning out across the two counties at events including farmers’ health checks, staff health checks, free health checks in pharmacies and age-friendly gatherings.


Make or Break programme supports creativity and wellbeing in the workplace

HSE South West has launched the Make or Break programme, offering workplaces free lunchtime creative workshops. Working with Cork County Council Library and Arts Service,
Kerry County Arts Service, and the Crawford Art Gallery, the workshops offer teams the chance to enjoy creative activities during their lunchbreak, including bookbinding, photography, clay sculpting and printmaking, Designed to be both enjoyable and relaxing, the central focus of the programme is to offer employees the chance to get creative and to promote mental wellbeing, contributing to a positive workplace environment.
The artist-led workshops aim to foster wellbeing and collaboration within workplaces.
Sheelagh Broderick, Arts and Culture Lead for HSE South West says the response has been incredible. HSE South West teams in primary care, older persons services, mental health services and more have taken up the opportunity, proving that creativity is for everybody as a meaningful tool for connection, wellbeing and positive change.
To learn more about the project, visit sample-studios.com/make-or-break
The newly-launched Corporate Plan 2025 to 2027 sets out priorities for change in the health and social care system over the next three years.
“Every step we take together towards achieving our commitments in this Corporate Plan – every new service, every partnership, every innovative solution – is a step towards transforming how health and social care services are experienced by patients and service users in the years to come,” says HSE CEO Bernard Gloster.
The main priorities of the Corporate Plan:
• Partnership-driven, personcentred service delivery
• Improving access to health and social care while focusing on early intervention
• Strengthening the foundations of our health system, including multidisciplinary teamwork and digital health
The introduction of six health regions under Sláintecare will help us transform our services and make sure everyone can access them when they need them.
Life expectancy in Ireland has risen, but there are still health inequalities across the population. Those in disadvantaged areas live, on average, five years less than others. In addition, we also need to address risk factors that lead to preventable diseases like diabetes.
Our plan will:
• Deliver screening programmes for colorectal, breast and cervical cancer, as well as diabetic retinopathy
• Improve the immunisation programme, including flu, COVID-19 and childhood vaccines
• Implement the Women’s Health Action Plan, aiming to eliminate cervical cancer by 2040
• Enhance oral health initiatives, improving emergency and routine dental care access
• Address wider health considerations, such as child poverty and social support gaps
• Promote healthy ageing through local authority age-friendly programmes
• Strengthen health equity initiatives for underserved groups
• Deliver primary prevention strategies under the Healthy Ireland Plan to reduce obesity, smoking and harmful alcohol use
• Develop a new National Suicide Prevention Strategy
The results we aim to achieve include:
• Increased screening participation
• Improved vaccine uptake
• More people engaging in healthier lifestyles
We will make sure that people receive the right care, safely and efficiently. Studies show that up to 30% of health and social care services could be delivered in a better way.
Making sure people receive care in the right setting will help reduce hospital overcrowding and unnecessary emergency department visits. At the moment, up to 30% of emergency visits could be managed elsewhere.
Reducing waiting times for health and social care services is a key priority. In 2024 alone, emergency department visits increased by 8% from the previous year. Nearly 90,000 people, including children, have waited over a year for outpatient appointments. We aim to achieve improved access to disability and mental health services and reduced waiting times in key areas.
Strong foundations
To sustain long-term improvements, we need to invest in our workforce, governance and digital infrastructure.
The Corporate Plan is available to read at the following links: English version – bit.ly/HSECorporatePlan2527 Irish version – bit.ly/PleanCorparaideachFSS2527
We will strengthen our foundations by:
• Carrying out a People Strategy (2025 to 2027) to improve staff training, wellbeing and retention
• Expanding multidisciplinary leadership and professional development programmes
• Collaborating with government departments, educational and regulatory bodies to ensure the appropriate level and mix of health and social care staff
• Strengthening governance through the HSE Performance and Accountability Framework
• Improving decision-making with real-time health data and improved performance tracking
• Rolling out digital tools to modernise healthcare, including electronic health records across acute and community services and a mobile app for patient selfmanagement
We hope to achieve:
• Improved engagement and results in the staff survey
• Reduced staff absence and turnover
• Better cybersecurity and digital health ratings within the EU
Carrying out our Corporate Plan
The HSE Corporate Plan 2025 to 2027 sets out a clear path to improve person-centred care, access, patient experience and health outcomes across our health and social care services.
While this plan covers a three-year period, our goal is to create long-lasting change that benefits future generations.
The plan will be carried out through:
• Annual national service plans
• Funding from our budgetary cycles
• Regional operational plans
• Ongoing monitoring and assessment By working together, we can create a stronger, fairer, more innovative and more efficient healthcare system for everyone.
The newly published People Strategy 2025 to 2027 supports the delivery of the priorities set out in the HSE Corporate Plan 2025 to 2027.
The strategy aims to:
• Support strategic workforce planning and resourcing
• Improve both individual and organisational performance
• Create a diverse and inclusive culture
• Support a safe and healthy workplace
• Encourage open feedback and innovation
The main priorities of the strategy are:
• Strategic workforce planning and resourcing
• Build high-achieving and adaptive teams to enable great performance
• Foster a diverse and inclusive culture
• Support a safe and healthy workplace
• Strengthen the ethos of open feedback and innovation
Our staff are the cornerstone to delivering the right care, in the right place, at the right time. Our shared purpose is to create a workplace where our staff feel better supported, continually valued and proud of the work they do. We want to enable everyone to help create a more sustainable, resilient and adaptable organisation, delivering safer, more effective and more accessible services. This strategy is about creating a culture of growth, innovation, collaboration and inclusivity.
Anne Marie Hoey, Chief People Officer of the HSE, highlights the importance of empowering our staff: “We are confident that working together with respect, we can build a service where we all feel recognised, developed and most importantly, enabled to deliver the best for our service users. Working in partnership to bring our strategy to life will enable us to attract and retain a diverse and talented staff, ensuring we have the right capabilities across the HSE, where everyone has the chance of career development and the opportunity to thrive in their role.”
Read more at bit.ly/HSEPeopleStrategy2527
This autumn, the HSE will publish a new Enabling Framework for Organisational Culture, setting out a strategic foundation for how we shape, support and sustain a culture rooted in compassion, performance, and trust across our health and care services. Organisational culture – defined as the shared assumptions, values and beliefs that influence behaviour within organisations – is a key factor in ensuring both safety and productivity in healthcare settings. Joe Ryan, National Director for Public Involvement, Culture and Risk Management explains, “This Framework will support our leaders and teams to be deliberate about building the culture we want and provides supports that will make it real and sustainable. Culture is shaped as much by everyday interactions as our policies and plans. That’s why this framework is practical, inclusive and rooted in the our values of care, compassion, trust and learning.”
Read more in the winter edition of Health Matters. For more information about the framework, email organisationalculturegroup@hse.ie
The latest HSE Your Opinion Counts staff survey has revealed some consistently strong results. Overall job satisfaction, enthusiasm for our work and a feeling of being trusted to do the job all remain high since the last survey in 2023. Just over 25,000 people took part this year, an increase on the number of responses in 2023. While 9 out of 10 of us feel that our job makes a difference and we are trusted to do our job, the results also highlight areas for consideration.
The survey results highlight staff’s commitment to a high standard of patient care, as well as the personal fulfilment they get from their work.
• 3 out of 4 staff feel patients and service users are the top priority in their service
• 8 out of 10 staff feel a sense of personal fulfilment from their job
Staff’s commitment to patient care has stayed strong during the significant organisational change of the past three years, as we transitioned to the six new health regions.
The relationship between staff and their line managers remains strong. Managers were rated more highly in all areas than comparable public and private sector organisations.
• 7 out of 10 staff feel their line manager listens to their ideas and suggestions
• More staff feel supported by their line managers (up 2.3 points on 2023)
While senior management scores stayed the same or increased on 2023 overall, there are still some areas that need consideration.
• Only 35% of staff feel involved in decisions from senior managers that impact their work
• Only 30% of staff feel supported to learn about and adapt to changes brought about by health regions
Compared to 2023, staff are slightly less satisfied with opportunities to progress their career and use their skills. The survey results show where we can improve support for staff development and make better use of their talents.
• Only 4 out of 10 agree that there are opportunities for career progression
• More staff feel that senior managers act on staff feedback (up 3.2 points on 2023) but this area still needs improvement
The scores for wellbeing in the workplace have stayed the same or slightly improved in most areas since 2023.
• 8 out of 10 staff feel respected by colleagues and patients
• More are satisfied with their physical work environment (up 4.5 points on 2023)
More feel the HSE tries to support a healthy lifestyle among staff (up 1.2 points on 2023). However, a similar number (just under 1 in 2) feel their stress is work related.
The awareness and knowledge of the HSE Dignity at Work policy has stayed the same, though more of us have completed the Dignity at Work training.
• 9 out of 10 staff have completed the Dignity at Work training (up 4.3 points on 2023).
“These results reflect the dedication and resilience of our staff, even during a time of significant change,” says Anne Marie Hoey, Chief People Officer of the HSE. “As we move forward, our focus will be on maintaining strong foundations of engagement, trust and support, while taking meaningful action in areas where improvement is needed. We will prioritise clearer communication around organisational change, expand opportunities for career development, and continue to invest in staff wellbeing.”
Your feedback is invaluable. We are committed to using it to shape a more supportive, inclusive and empowering workplace for all. The survey results for each health region will be shared with REOs and heads of service. The results for Corporate National Services will also be shared with each national director.
The National HR Staff Engagement team can support managers and staff to develop action plans and staff engagement activities. Email staffengagement.hr@hse.ie
As promised, there was a draw for six €300 One4all gift vouchers to thank everyone who participated in the survey. The happy winners have all received their vouchers.
Read the results of the Your Opinion Counts Staff Survey 2025 at bit.ly/StaffSurveyResults2025
University Hospital Kerry (UHK) has officially opened its new staff cycle hub, while marking a significant milestone as the first facility in Co Kerry to achieve the National Transport Authority (NTA) Smarter Travel Mark certification.
The hub, launched during a ribbon-cutting ceremony and plaque presentation, was developed over the past year by the UHK green team with support from the UHK executive management team. The project was put in motion post a 2023 active travel staff survey that identified a strong demand for a secure, accessible bike storage option.
Funded by the NTA and the HSE Climate Action Office, the facility offers secure parking for 40 bikes –including cargo and adaptive options – staff swipe card access, CCTV and weather protection.

Hospital Kerry (UHK) officially opened the UHK staff cycle hub and celebrated its National Transport Authority (NTA) Smarter Travel achievement with Damien Moyles, UHK Operations Manager; Aileen Fitzgerald, HSE Regional Sustainability Officer; Mary Fitzgerald, UHK General Manager; Shane Hayes, NTA Senior Officer Smarter Travel Mark; and Brita Allen, UHK Hygiene and Waste Manager.
Designed to promote sustainable commuting, the hub also supports UHK’s wider goals of reducing carbon emissions, easing parking pressures, and enhancing staff wellbeing. The launch included guided tours of the new cycle hub facility, an active travel information stand, and prize-giving for the national NTA Marchathon-winning UHK team.
HSE Capital and Estates Sustainable Infrastructure Office team and over 400 public sector delegates attended the SEAI annual Public Sector Energy Conference on 15 May at the University of Galway. The conference focused on scaling up the decarbonisation of the public sector building stock to meet public sector climate targets. The Sustainable Infrastructure Office coordinated and hosted the health sector breakout session in the afternoon, which brought HSE and Section 38/39 agencies together for an exchange of learnings, challenges and collaboration opportunities. The session was opened by Brian O’Connell, National Director Head of Strategic Health Infrastructure and Capital Delivery. The HSE Capital and Estates Sustainable Infrastructure Office presented on the HSE approach to achieving energy and GHG emissions reduction targets through improved data collection, the establishment of energy teams and the implementation of energy projects through our partnership with SEAI. The session also included a presentation on the HSE’s journey to achieving ISO 50001, the importance of retro-commissioning to ensure our existing buildings are running at their optimal performance, and the HSE’s Deep Energy Retrofit Pathfinder Project, which is underway across 10 healthcare facilities.
The HSE Capital and Estates Infrastructure Decarbonisation Roadmap outlines HSE Capital and Estates’ approach to meet the public sector targets.
Cork has been awarded the EU Mission Label by the European Commission for its strong leadership and ambitious climate action plans. Niall Gibbons, HSE Capital and Estates Energy Officer was invited to the domestic launch of the EU Mission Label as part of his commitments to the Climate Neutral Public Sector Leadership Group in his role as Energy Officer for the HSE South West. Cork City has been recognised as part of the 100 Climate Neutral and Smart Cities EU initiative and we will promote the potential for Cork to become one of the most resilient, futureproofed and economically successful European cities. However, our success will depend on the actions of everyone who lives or comes to work in Cork; who visit, learn or invest here.

Niamh Keane, Clinical Lead, Health and Wellbeing, HSE Mid West (third from left); with (from left) Yvonne Galvin, Co-CEO/ Early Years Manager, Our Lady of Lourdes Community Services Group (OLOLCSG), Limerick; Niamh Wallace, Head of Service, Health and Wellbeing, HSE Mid West; and Bernie Hannan, Family Resource Worker, OLOLCSG.
Anna Marie Kiernan, Advanced Nurse Practitioner at the Pain Excellence Centre, Croom Orthopaedic Hospital was awarded Best Use of Innovative Technology at the 2025 HSE Spark Summit in Dublin. Her project, Patch Me If You Can/Virtually Pain Free, was one of 12 recognised for addressing healthcare challenges through innovation.
Anna Marie’s project piloted an augmented reality (AR) tool to reduce procedural pain during Qutenza patch treatments. “Distraction techniques can be powerful in easing discomfort,” she explained. “The AR tool has been well received by patients, offering a new, engaging method of pain relief.”
The Spark Summit celebrates frontline healthcare innovation, bringing together professionals, policymakers, and international experts. It highlights how creative use of existing resources can improve care and reduce pressure on services.
Other HSE Mid West winners included Mairead O’Donoghue, RANP Emergency, St John’s Hospital,



Mairead O’Donoghue, ANP, St John’s Hospital and her team celebrate their Best Digital Project Mid West award at the HSE Spark Summit.
Limerick, who won Best Digital Project for Net –Transforming Patient Care through Digital Innovation; and Niamh Keane, Clinical Lead for Health and Wellbeing, Ennis, who received the Best Community Collaboration award for Baby and Me: Baby Bonds and Beyond. These awards reflect the region’s commitment to innovation, patient-centred care, and collaboration across healthcare settings.
To mark World Elder Abuse Awareness Day, the HSE Mid West safeguarding and protection and medical social work teams hosted a series of impactful events. Activities included awareness stands at Nenagh Health Centre and University Hospital Limerick, and an afternoon tea at Thurles Community Hospital. An information day in Moyross brought together community partners like Sage Advocacy, An Garda Síochána, and ALONE.
A special HSE Talking Health and Wellbeing podcast featuring Tim Hanly and Teresa Cronin highlighted the risks of elder abuse and how to recognise and report it. These efforts reflect the HSE’s commitment to safeguarding older people and raising public awareness.

From left: Prof John McManus, NDTP Training Lead, HSE Mid West and Consultant; Dr Emma Kearney, Specialist Registrar, Public Health, HSE Mid West and overall winner of this year’s NCHD Conference for her study on ED attendances; Prof Linda Mulligan, Chief State Pathologist, Department of Justice; and Prof Declan Lyons, Director of Research, HSE Mid West.
The NCHD Research Conference at University Hospital Limerick (UHL) in May showcased record research activity, with 224 abstracts submitted, a 60% increase from last year. Chief State Pathologist Prof Linda Mulligan attended to highlight new national guidelines on improving communication with bereaved families during postmortem exams. She
An innovative two-year project in the Mid West is transforming how professionals support children with concerning behaviour. The CPS Ireland Demonstration Project, involving five children’s disability network teams, focuses on collaborative and proactive solutions (CPS) – a neurodiversity-affirming, trauma-informed approach that replaces traditional behaviour management with problem-solving between children and caregivers. At a recent Day of Sharing in St Gabriel’s Centre, staff shared successes and insights. Over 100 families are now participating in
emphasised the importance of compassionate, family-centred services, reflecting international standards. Dr Emma Kearney won the overall award for research on emergency department (ED) attendance linked to socioeconomic disadvantage, underscoring health inequalities in the Mid West. Sandra Broderick, HSE Mid West Regional Executive Officer, praised the NCHD’s contributions, noting a 60% increase in their numbers and ongoing regional healthcare expansion.

Kate Healy; Aisling Kelliher, Senior Occupational Therapist (SOT); Dr Toby Sachsenmaier, CPS Project Lead; Dr Ailbhe Hogan, Senior Clinical Psychologist; Maya Hamoudah, Psychology Assistant; Bridget Long, SOT; Linda Reen, SOT; and Fiona Hehir, Psychology Assistant.
the final research phase, supported by the University of Limerick and Virginia Tech. Funded under the 2022 National Service Plan, the project is led by Dr Toby Sachsenmaier.
To mark Maternal Mental Health Day on 7 May, healthcare professionals and advocates at University Maternity Hospital Limerick (UMHL) hosted an awareness event highlighting the importance of women prioritising their mental wellbeing during the perinatal period.
Staff from UMHL’s specialist perinatal mental health service and the newly formed Perinatal Mental Health Association Mid West engaged with women, shared resources and offered self-care items. The initiative aimed to reduce stigma and promote equal focus on physical and mental health. With over 265 active cases, UMHL’s multidisciplinary team continues to support women through pregnancy and up to one year postpartum.

UMHL staff Pauline Walsh, Sarah Breen, Fiona Callanan and Aideen Higgins on Maternal Mental Health Day. See livesinthebalance.org

A milestone in the provision of critical care of premature and seriously ill newborns has been reached at University Maternity Hospital Limerick (UMHL) with the refurbishment of the hospital’s neonatal intensive care unit (NICU).
The project, representing an HSE investment of €9.7m, was completed in two phases over the past five years with no interruption to NICU care.
Many non-clinical spaces, including parents’ accommodation, a lactation centre, clinical engineering unit, and support facilities for staff and admin, are now housed in a two-storey extension. This has freed up space for a dramatic refurbishment and
as babies moved in to the newly extended and refurbished
University
expansion of cot space in the intensive care, high dependency, and purpose-built isolation areas. The new unit avoids crowding, enhances opportunities for skin-toskin contact between pre-term infants and parents, improves breastfeeding rates of high-risk neonates, reduces risk of infection outbreaks, and creates in-built
“What impresses me is the fully-breastfed discharge management coordination to ensure all the babies are going home breastfeeding. And I am impressed too by the warm atmosphere and the feeling parents have here of being the main caregivers and truly part of the team.”
provision for surge capacity. New mother-and-baby rooms for family-centred care and floral artwork create calm and comfort for parents and staff.
Managed by HSE Capital and Estates and developed by DK Architects, John Halligan Architects and O’Brien Building and Civil Contractors, the project has been executed to an evidence-based blended design concept, informed by all disciplines at UMHL, and parental input via interactions with the Irish Neonatal Health Alliance (INHA) and the Global Foundation for the Care of Newborn Infants (GFCNI).
Silke Mader, Founder and Chair of the GFCNI, from Germany, who visited the unit soon after the new facility was operational in early June says, “It is a pleasure to see a truly family-centred and familyintegrated approach to care in this newly rebuilt unit. What impresses me is the fully-breastfed discharge management coordination to ensure all the babies are going home breastfeeding. And I am impressed too by the warm atmosphere and the feeling parents have here of being the main caregivers and truly part of the team.”
The project’s Clinical Lead, Consultant Neonatologist Prof Roy Philip said the visit of Ms Mader is an indication of the standards set by the new unit, which he says surpasses UMHL’s aim to develop one of the best neonatal care facilities in the country: “We are thrilled to see the benefits offered by this project to the families of critically ill and premature newborn infants of the Mid West.”
This refurbishment project is among several initiatives being undertaken to improve services at UMHL pending the eventual relocation of the maternity hospital to the University Hospital Limerick campus in Dooradoyle.
HSE Mid West personnel joined colleagues from the department of psychology at Mary Immaculate College Limerick, parents, Tusla and Clarecare to publish a research project exploring the experiences of parents living with mental health challenges.
Over 200 parents across Ireland participated in the anonymous online survey, launched on World Mental Health Day last October. The study, Building Connections, aimed to understand the challenges parents face and the supports – or lack thereof – available.
Some 83% of parents felt their mental health made parenting more difficult. Many reported challenges in accessing support, managing medication while parenting, and discussing their mental health with their children. Notably, 54% said their parenting role wasn’t considered in medication discussions, and 46% didn’t know where to find parenting support.
Representatives from Tusla, the HSE and Clarecare echoed the need for integrated support that considers both parenting and mental health. Martina Kilcommins, Senior Social Work Practitioner, HSE said: “Hearing directly from parents living with mental health challenges
has been a powerful reminder of the importance of truly listening to lived experience in shaping better support. It really helps me to ‘think parent, think family’ in my work with service users.”
The research underscores the urgency of developing targeted, stigma-free services for families navigating these dual challenges.

Social Work
Family
Dr Suzanne Egan, Dept of Psychology, Mary Immaculate College (MIC); Prof Niamh Stack, Dept of Psychology, MIC; Sian Harris, Senior Clinical Psychologist, HSE Primary Care Psychology; Joanne Perill, Team Leader, Family Support Services, Clarecare; Aine Mellett, Senior Manager, Tusla; and Dr Clara Hoyne, Dept of Psychology, MIC.
Recordings from a recent Family Recovery webinar, in partnership with the team behind the research, are available on YouTube, The Wellness Panel podcast on Spotify, Apple and other platforms, and on the Mid West ARIES website, midwestaries.ie/learn/family-recovery
At the World Conference on Tobacco Control in Dublin, HSE Mid West Health Promotion

Officers Mary MacMahon, Beth McDonald and Damien Ahern presented an innovative e-poster showcasing a stop smoking pilot programme tailored for individuals in emergency homeless accommodation through Mid West Simon services.
This collaborative initiative –developed by HSE Mid West Health
and Wellbeing, HSE Social Inclusion (national and regional), QUIT Mid West, the Tobacco Free Ireland Programme, and Mid West Simon – was launched in response to high smoking rates among residents and low engagement with traditional QUIT services.
Key findings revealed that 70% of residents smoked, with over half smoking for more than 20 years. While 63% expressed a desire to quit, only 21% felt confident doing so.
Staff showed strong interest in supporting cessation, with 86% requesting training. Barriers included
smoking as a coping mechanism, medication management, and environmental factors.
Successful strategies included weekly on-site quit clinics, staff training, community outreach, and a literacy-friendly map to the King’s Island quit clinic. Sessions also expanded to cover broader health and wellbeing topics, reflecting residents’ interest in healthier lifestyles.
This pilot has deepened understanding of the unique challenges faced by people experiencing homelessness and laid the foundation for more inclusive, accessible health services. The team is proud to share this work and remains committed to promoting health equity across all communities.
Clinical Nurse Specialist, Integrated Care Chronic Disease Cardiology Service, Limerick
Residents in HSE Mid West’s older persons community nursing units enjoyed front-row access to the 2025 GAA Championship matches, thanks to a renewed partnership with GAA+. All ten residential units received complimentary access, bringing joy to many lifelong Clare hurling fans. GAA+ Marketing Manager Gavin Doyle praised the initiative’s power to unite generations. Aisling Ryan, Head of Service for Older Persons, noted the joy it brought to residents. The partnership highlights the value of sport in enhancing wellbeing and community spirit in care settings. Our photographs show staff and residents at Regina House, Kilrush during one nail-biting clash between Clare and Tipperary.

I work as part of Limerick’s Integrated Care Cardiology team at Croom Primary Care Centre. I love being involved in the delivery of specialist cardiac care in the community, helping patients manage their conditions closer to home. I’ve been in this role for nearly two years and feel privileged to be part of a growing service that’s making a real difference. Our team supports patients with heart failure, hypertension, and atrial fibrillation. My day typically involves taking detailed health histories, performing physical exams,


reviewing blood results, adjusting medications, and working closely with our Consultant Cardiologist, Dr Neasa Starr. I recently qualified as a registered nurse prescriber, allowing me to act as a single point of contact for patients – making their care more holistic and accessible.
I particularly enjoy health promotion and patient education, which empowers people to manage chronic conditions and often avoid hospital admissions. Seeing improvements in patients’ health and receiving positive feedback from families is incredibly rewarding.
Our small but dedicated team includes a consultant cardiologist, three clinical nurse specialists, and a cardiac physiologist. We currently care for over 180 patients and are focused on expanding awareness of our service, gathering feedback, and planning for future growth in cardiac risk prevention.
Limerick City and County Council and HSE Mid West have launched the Limerick Health Equity Region Oversight Group to address health inequalities in the city’s most disadvantaged areas. The group, which had its first meeting on 15 May, aims to create a fairer, healthier Limerick by tackling social determinants of health, such as housing, education and employment. This is Ireland’s first public health-led initiative to adopt the internationally recognised Marmot Principles.
The initial focus is on giving every child the best start in life, targeting North and South Limerick City, where 36.4% of the population is disadvantaged and extreme disadvantage has nearly tripled since 2016.
University Hospital Limerick-based Clinical Placement Coordinators, Geraldine Crilly and Pauline Chapman, have developed a powerful short film, “Great Minds Don’t Think Alike – Neuroinclusive Learning Environments at UHL”, showcasing the voices of neurodivergent students, staff and their supporters.
The film was launched at the multidisciplinary Embedding Inclusion conference in Limerick in the spring, which was attended by more than 150 healthcare professionals from across Ireland. The event focused on lived experience, with speakers including student nurse Rebecca Kearney, dietitian Ruth Reidy, and autistic healthcare professional Florence Horsman Hogan. Their stories highlighted the challenges and strengths of neurodivergent individuals in healthcare.
Marius Zaharia, a mature nursing student from Romania, shared his journey navigating clinical placements.
Keynote speakers Adam Harris (AsIAm) and John Lonergan (former Mountjoy Governor) spoke about the value of diversity in the workforce.
Dr Sadhbh O’Dwyer, Dr Claire O’Donnell, and Caroline Lane also contributed insights on inclusion, reasonable accommodations, and disability support.
The conference received overwhelmingly positive feedback, with attendees praising the depth and impact of the personal stories shared. The event reinforced the importance of inclusive education and support for all students.
Geraldine and Pauline extended thanks to the nursing and midwifery planning and development unit for their support.


The two-minute film is available to watch on YouTube at bit.ly/GreatMindsDontThinkAlike For more information, contact pauline.chapman@hse.ie or geraldine.crilly@hse.ie
John’s Hospital
St John’s Hospital became the first healthcare facility in the Mid West – and among the first in Ireland – to phase out large-scale use of nitrous oxide gas for anaesthesia. As part of a HSE Mid West pilot project, the hospital decommissioned its nitrous oxide pipework on 16 April, replacing it with mobile equipment that delivers anaesthetic cylinders directly to operating theatres.
Nitrous oxide, once considered harmless, is now recognised as a potent and long-lasting greenhouse gas. Its removal aligns with the HSE’s Climate Action Strategy, which targets a 50% reduction in anaesthetic gas emissions by 2030. Early results from the pilot, now extended to Croom Orthopaedic Hospital, suggest these targets may be exceeded.
Consultant Anaesthetist Dr Hugh O’Callaghan, who led the initiative, praised the hospital’s leadership: “St John’s is now at the forefront of
national efforts to reduce emissions. We must deliver care safely while considering environmental impact. Modern techniques are making nitrous oxide increasingly obsolete.”
Michelle Rogers, Director of Operations at St John’s added, “We’re proud to be on track to meet national climate goals.”
Pending full evaluation, other hospitals in the region are expected to follow suit, marking a significant step toward sustainable healthcare in Ireland.
down on illegal vapes and e-cigarettes and the sale of vapes to under-18s
The HSE National Environmental Health Service (NEHS) staff work with businesses nationwide to ensure tobacco and nicotine inhaling products comply with the law and, where there is a serious risk to health, they issue alerts and take enforcement action. The HSE has the power to seize vapes breaching the legal limits, destroy them and carry out prosecutions.
Dr Maurice Mulcahy, Regional Chief Environmental Health Officer with the HSE’s National Environmental Health Service, says the service strongly recommends that those selling e-cigarettes and vapes get details from their supplier of the products’ origins and confirm that they are legal. Dr Mulcahy adds, “We’re also very concerned about the attraction of vapes to young people and the sale of vapes to under-18s. We undertake an annual programme of test purchases, which includes e-cigarettes. Volunteer children, with parental consent, attempt to buy such products to test whether retailers are asking for proof of age. The worrying thing, given that tobacco and e-cigarettes and vapes contain highly addictive nicotine, is that we are still finding a high proportion of sales to volunteer

If individuals wish to make a complaint in regards to noncompliant electronic cigarettes or vapes, they are asked to contact their local Environmental Health Office; details are available at bit.ly/EnvironmentalHealthOffice
The HSE Health Promotion and Improvement team in the Midlands have been supporting initiatives aimed at creating tobacco- and vape-free environments for children and young people in their counties.
These initiatives, steered by local authorities, represent a partnership approach to working in the Midlands counties. HSE Health Promotion and Improvement have been working in collaboration with other local groups such as Healthy Ireland coordinators, local county councils, Children and Young People’s Services Committees (CYPSCs) and youth groups, Comhairle na nÓg and local gardaí.
The Not Around Us campaign has recently been launched in Longford, Westmeath and Offaly and the Clean Air Around US initiative is in place in playgrounds and play spaces in Laois. HSE health promotion officers also
children. To date this year, we’ve prosecuted 12 businesses with fines up to €2,000.”
The NEHS is charged with the implementation of the Public Health (Tobacco Products and Nicotine Inhaling Products) Act 2023, together with the transposed Tobacco Products Directive.
Environmental health officers undertake inspections of tobacco and nicotine inhaling products at manufacture, import, distribution and retail level as well as test purchase inspections for underage sales. These are some elements of a wider proactive surveillance programme including intelligence gathering, monitoring, sampling, compliance building and enforcement across the whole supply chain under the service’s remit.
Environmental health officers have been very active in terms of enforcement in this area and particularly in relation to products with concentrations of nicotine in



supported these launches by participating in recording promotional videos for social media. The aim of these projects is to protect children and young people from the harms of second-hand smoke exposure. Creating smoke- and vape-free outdoor spaces also helps to de-normalise smoking and vaping for the next generation. These initiatives will hopefully reduce the cost of cleaning discarded tobacco and vape waste while also raising awareness amongst all stakeholders in the Midlands counties of Tobacco and Vape Free Ireland and their role in promoting this strategy. They also provide an invaluable opportunity to signpost the public to HSE Quit services.

excess of the 20mg/ml or 2% permitted and electronic cigarettes with volumes greater than the 2ml permitted.
Ann Marie Part, Assistant National Director for Environmental Health explains, “We take our role very
seriously. It’s the responsibility of the manufacturer and importer of electronic cigarettes, refill containers (e-liquids), tobacco products, novel tobacco products and herbal products for smoking to ensure that they fully comply with all legislative requirements. Retailers must also ensure that all refill containers and electronic cigarettes they place on the market in Ireland comply with the law.”
At retail and distributor level, the NEHS in 2024 successfully prosecuted two businesses for non-compliant nicotine inhaling products. In 2023, eight prohibition orders were served in relation to products where nicotine content and volume exceeded legally permitted levels. In 2024, 14 prohibition orders were served by the NEHS. These 22 prohibition orders led to the destruction of 3,371 non-compliant electronic cigarettes/refill containers that were seized and removed from retail premises.





















The HSE Tobacco Free Ireland Programme has a longstanding programme of work and engagement with the Irish Prison Service. We commenced engagement with the governor of Mountjoy Prison back in 2019 when we first started to support the development of smoke-free wings in the prison and developed stop smoking support for both inmates and prison staff.
Smoking prevalence among prisoners is around 86%, a staggering 3.7 times higher than the general population. There are significant challenges in that there is poor education, high prevalence of homelessness, high prevalence of concurrent drug addiction and mental illness among this population.
The latest development in this partnership has seen the work now extended to a wider network of prisons, and the latest project involves Tobacco Free Ireland stop smoking trainers, delivering peer stop smoking support training to inmates who work as ‘red cross volunteers’ within the prison so that they can further support their own peers in their respective quit attempts.
“Quitting in prison truly tests you … But I am proof that it can happen and would 100% recommend the programme. I think the support group should last longer. I’m so proud.”



Financial incentives to stop smoking (FISS) programmes have been implemented internationally to encourage people who smoke to quit smoking. A Cochrane systematic review and meta-analysis of existing published evidence suggests that financial incentives are 50% more likely to lead to smoking cessation than other types of support. The HSE Tobacco Free Ireland Programme is working with three pilot sites through a Health Research Board-funded study in partnership with the RCSI and has developed a stop smoking gift voucher incentive scheme. This exciting new project commenced at the end of March.
The FISS scheme is a HSE initiative to provide people from disadvantaged areas who smoke with an incentive to make a quit attempt, thereby increasing engagement with stop smoking support and the chances of success. Incentives will be provided in the form of One4all gift vouchers. The maximum amount that someone can avail of is €400 (over a 12-month period) but this is made up of smaller amounts per visit when someone is proven to be off cigarettes by standard clinical testing. For example, if you have quit for one week, you can get €20; quit for 2 weeks, you will get €20, and so on.
Quitting smoking can greatly improve people’s health. Incentives, such as money or vouchers, can be used to encourage smokers to quit, and to reward them if they stay stopped. Such schemes are routine practice in the UK for pregnant women who smoke.

To enter:
1. Email us a photo of yourself reading Health Matters
2. Tell us where you picked up your copy
3. Let us know your favourite article from this issue
You must have all three parts to be entered into the draw.
Congratulations
We love seeing our readers enjoy Health Matters. Now we are giving you the chance to win a €100 voucher just for sharing a snap.

We’re delighted to congratulate Margaret O’Sullivan, a vaccinator on the Health and Wellbeing Vaccination team in Limerick and volunteer with a Dementia Social Club. Margaret enjoys updating herself with the informative articles in Health Matters. She particularly benefits from reading any dementiarelated stories and her favourite pieces in the summer edition were “Dementia Awareness for An Garda Síochána” and “Community Healthcare Collaboration sees Listowel Celebrated as a Dementia Inclusive Town”. Margaret received her online copy of the magazine through the weekly Health Service News email bulletin. Enjoy your One4all voucher, Margaret –and thank you for being a loyal reader.
Send your entry to internalcomms@hse.ie with the subject line ‘Health Matters photo competition’.
The competition closes on Friday, 31 October 2025. One lucky winner will be selected at random. Happy reading and good luck!

and
Clerkin, Integrated Healthcare Area Manager Louth Meath (second from right), Gary Keenan, General Manager (far right), and Gráinne Milne, Director of Midwifery (second from left), parents, children, staff past and present, and representatives from local and national organisations in celebrating the 20th anniversary of the opening of the Midwifery-Led Unit at Our Lady of Lourdes Hospital, Drogheda.
To commemorate the 20th anniversary of the opening of the Midwifery-Led Unit (MLU) at Our Lady of Lourdes Hospital, Drogheda, a special event was held where parents, children, staff past and present, representatives from local and national organisations, and special guest Sabina Higgins, wife of President Michael D Higgins gathered to celebrate this truly
remarkable milestone. MLUs in Drogheda and Cavan opened their doors in July 2004 with a bold and simple vision: to offer womencentred care led by midwives in an environment that is safe, supported and empowering. The ethos of midwifery-led care is about standing together – midwives, doctors, nurses and allied professionals, in strong, respectful communication
Opening of restored Victorian walled garden and orchard in National Forensic Mental Health Service, Portrane
On 20 May, the HSE National Forensic Mental Health Service (NFMHS) officially opened the restored Victorian walled garden and orchard in Portrane, North Dublin. Dating back to the 19th century, it will serve as a therapeutic, recreational space that can be enjoyed by NFMHS patients and staff.
Benefactors and HSE colleagues Dervila Eyres, IHA Manager, HSE Dublin and North East, and Brian Higgins, National Director for Adult Mental Health Services, were given a guided tour of the garden by NFMHS patients and staff members involved in the walled garden project.
and teamwork that places the woman and her family at the centre of everything.
Speaking at the event, Gráinne Milne, Director of Midwifery said, “This 20-year celebration is a testament to the vision, resilience and professionalism of our midwives and staff. Midwifery-led care is about trust, respect, empowering women and the power of collaboration in achieving better outcomes for women and their babies. We are proud of how far we’ve come and excited about the future.”
Sara Long, Regional Executive Officer for HSE Dublin and North East praised the work of midwives and highlighted the importance of delivering care that is respectful, empowering and woman-centred: “It is a great honour to be part of this celebration. The work done here over the past two decades has had a profound impact on so many lives. These units represent the best of what healthcare can be –compassionate, skilled and truly person-focused.”
The event also featured presentations to former service users and displays highlighting two decades of service, stories and success. Special guest Sabina Higgins gave so much of her time to the families, the staff and the unit, stating she thoroughly enjoyed the day.


Cultural Diversity Day was celebrated recently at Connolly Hospital, bringing together over 300 attendees from more than 60 nationalities. The event aimed to promote understanding and appreciation of diverse cultures within the hospital community.
Attendees enjoyed a remarkable array of cuisines, showcasing traditional dishes from various cultures. This culinary diversity not only satisfied tastebuds but also fostered cultural exchange and dialogue among participants.
Engaging competitions were a highlight of the day, including a
TikTok challenge that encouraged participants to creatively showcase their cultural heritage. A best dressed competition featured vibrant traditional attire, allowing participants to display their cultural pride. Spot prizes were awarded throughout the event, adding an element of excitement and encouraging active participation among attendees. The atmosphere was vibrant and festive, characterised by laughter, music, dancing and a strong sense of community. Attendees shared stories, made new friends, and celebrated their unique backgrounds together.
St Joseph’s Community Nursing Unit (CNU), Trim celebrated success at the recent Irish Healthcare Centre Awards 2025 in the Clayton Hotel, Burlington Road, Dublin. Having been shortlisted in three categories, St Joseph’s CNU proudly took home the award for Nursing Home/Residential Centre (Public) of the Year on the night. This marks the second time the centre has been shortlisted and won the award, having been successful in 2022. This recognition is a testament to the commitment and dedication of management, staff and residents, reflecting the high standard of care provided and the extensive redevelopment of the centre over the past decade.
Beaufort House hosts National Arts in Nursing Homes Day
As part of the 30th anniversary of the Bealtaine Festival, residents, families and staff at HSE Navan Community Health Unit, Beaufort House, Co Meath celebrated National Arts in Nursing Homes Day on Friday, 16 May. A vibrant celebration of creativity where attendees share in the power of the arts to foster wellbeing, self-expression and community connection, this annual event is supported by Nursing Homes Ireland and Age and Opportunity. A series of special arts activities and events gave residents the opportunity to showcase their creativity and celebrate the positive impact of the arts on wellbeing. Beaufort House was selected as a recipient of a National Arts in Nursing Homes Day Award this year in recognition of its ongoing commitment to promoting the arts and enhancing the lives of its residents.

To mark Men’s Health Week, the Louth Meath Health Promotion and Improvement team facilitated men’s health training across the two counties, supporting this year’s theme of “Shoulder to Shoulder –Connecting for Health”.
The theme focused on the importance of connection and teamwork in supporting men’s health, reminding everyone that men should not face health issues alone. Supports are available and taking small, realistic steps within a supportive environment can make a big difference.
As part of this initiative, an Engage workshop was held in partnership
with the Healthy Ireland group in Our Lady’s Hospital, Navan. Healthcare staff from both the hospital and community settings attended this practical session, aimed at helping practitioners better engage with men around health and wellbeing issues. One participant said, “…really learned a lot around working with men for their health and wellbeing needs and how to shape resources more effectively to attract men to a healthcare service.”
The National Men’s Health Action Plan 2024–2028 was also highlighted, emphasising the need to empower men to take charge of their own health through supportive
environments and tailored approaches – particularly in the area of mental health.
Another milestone this year was the rollout of the Wellbeing for Men programme to male HSE staff in Louth and Meath. Delivered in the Regional Educational Centre, St Brigid’s Campus Ardee, it received positive feedback. Participants described it as “really enjoyable and beneficial” with many recommending it to colleagues.
Men’s health remains a key focus for healthcare staff in Louth and Meath and the Health Promotion and Improvement team are proud to continue supporting this.
“This has taken me way ahead of where I started. It got me out of myself, out of my house to meet people, and knew I wasn’t alone” – Comhrá partner.
Comhrá café communication training is a training programme developed by speech and language therapists (SLTs) and Comhrá partners (people with communication differences/difficulties) with collaboration from a café manager. It involves 90-minute training delivered by SLTs and Comhrá partners. During the training, Comhrá partners share their personal experiences of communication difficulties and breakdowns, and give advice on how café staff can help to make their café more communication
accessible. The training is usually held in the participating café to allow for real-life examples and suggestions that are specific to the café. At the end of the training, the café staff are supported to write an action plan based on what they learned. Comhrá partner stories are often described as the most impactful part of the training. Their participation is vital for the programme and each partner is offered payment for their time and expenses.
“I loved the stories that were shared. It gave a better insight to those who must live with those difficulties” – café staff member.
To achieve Comhrá certification, the participating café must

Leon Duffy of Leon’s, Navan with the café’s Comhrá certification.
demonstrate followthrough of their action plan and pass a “secret shopper” audit.
The first café to achieve this certification is Leon’s Café, Navan. In June, Leon Duffy was presented with
a certificate and window sticker by Comhrá partner Elaine Morrissey.
Leon’s leads the way for what we hope will be a long list of Comhrácertified businesses in Meath.

Tánaiste and Minister for Foreign Affairs and Trade, Simon Harris TD, accompanied by Niamh Smyth TD, turning the sod at St Christopher’s Hospice.
The Tánaiste and Minister for Foreign Affairs and Trade, Simon Harris TD accompanied by Niamh Smyth TD, Minister of State at the Department of Enterprise, Trade and Employment with special responsibility for Trade Promotion, Artificial Intelligence and Digital Transformation, turned the sod at the St Christopher’s Hospice redevelopment in Cavan.
This specialist palliative care unit will include a 16-bed (single occupancy en-suite) inpatient unit that will cater for patients requiring specialist palliative and end of life
care in Cavan and Monaghan. There will also be a palliative care hub, consisting of an outpatient facility including a rapid access diagnostic and management capacity, a specialist day hospital and a specialist treatment unit with capacity for infusions, transfusions, and a lymphoedema service. It will also contain a physical therapies unit with capacity for prehabilitation and rehabilitation and a creative therapies unit including art, music, creative and complementary therapies.

Kieran O’Donnell TD, Minister for Older People and Housing (pictured), officially opened The Village Residence, Drogheda in May. The Village Residence, renamed and with additional beds, is an expanded residence for people requiring long-term and short-term care. Butterfly Cottage, Red Robin Cottage, and ForgetMe-Not Cottage are each 10-bed homely cottages where people with dementia, in varying degrees of need, are cared for by expert staff. Butterfly Cottage offers a warm and welcoming environment for residents with advanced dementia, providing specialised dementia and palliative care services, tailored to their needs. Red Robin Cottage is a home for individuals experiencing the progressing symptoms of dementia, who may also face frailty and other long-term medical conditions. Forget-Me-Not provides a supportive and nurturing space for residents who now require full-time assistance due to their advancing dementia symptoms. The Village Residence works in an integrated manner with community services, voluntary organisations, and acute services to support people in living as fulfilled lives as possible.
A massive congratulations to the 1,981 HSE staff members from HSE Dublin and North East who stepped up to the challenge and made strides towards a healthier, more active lifestyle. Across 261 teams, participants logged an incredible 618,740,578 steps – an inspiring demonstration of our commitment to healthier, more active lifestyles.
The challenge not only promoted physical activity but also fostered connection and motivation across teams. Team coordinators rated the experience enjoyable and 93% reported they’d volunteer to be team coordinators again. Participants highlighted the strong sense of camaraderie, with many sharing how the challenge brought together colleagues who don’t usually work side by side.
The smooth-running of the challenge was facilitated by local Health Promotion and Improvement teams across Dublin North, Louth, Meath and Cavan. Well done to everyone who took part and a special congratulations to all our weekly competition winners.
Remember, every move counts. Keep going, stay active and continue to boost your health and wellbeing, one step at a time.

St Mary’s Community Residence in Drogheda, Co Louth has become the fourth group in Ireland to receive a prestigious Gold Forum Award for tobaccofree campus efforts.
The award, given by the Global Network for Tobacco-Free Healthcare (GNTH) services, recognises the highest level implementation of tobacco cessation and control measures based on the GNTH service standards – aligned with WHO standards.
To qualify, healthcare services must score at least 126 out of 144 in a self-audit and demonstrate comprehensive tobacco-free initiatives, including systematic cessation and health promotion programmes, a tobacco-free environment, staff engagement, and ongoing evaluation.
Two sites from Louth and Meath were considered for the Gold Awards in 2025, An Draighnéan
The team at St Mary’s Community Residence in Drogheda, Co Louth celebrate their Gold Forum Award for tobacco-free campus efforts.

Disability Site in Navan and Community Mental Rehabilitation Services Louth.
Sharon Crichlow, ADON Community Rehabilitation Service, Louth Meath Mental Health Service, and her team have actively promoted tobacco control over the past four years. All team members completed Making Every Contact Count (MECC) training, and St Mary’s is now a MECC implementation site, engaging with service users on tobacco and other healthrelated behaviours.
St Mary’s Residence received the award at the GNTH conference in Dublin on 26 June – one of three
successful awards given out across Ireland in 2025.
Emer Smyth, Health Promotion and Improvement Manager says, “St Mary’s Residence is so deserving of this award as it is a leading example of how collaboration between mental health services and health promotion and improvement can help improve the health of the population.”
Sharon Crichlow adds, “I personally would like to congratulate all the staff in St Mary’s Residence. This award is testament to the hard work and efforts [staff] make on a daily basis for their residents.”
Jacintha McGahan, Pulmonary Rehabilitation Coordinator, Louth talks about the service
Across Louth and the wider HSE Dublin and North East health region, people living with chronic lung disease are learning to breathe better, move more confidently, and reclaim their health – thanks to a free HSE programme called pulmonary rehabilitation (PR), delivered as part of the respiratory integrated care programme.
PR is a structured programme of exercise, education and support designed to help people manage key symptoms of chronic lung disease. It helps reduce breathlessness, supports airway clearance, lowers the risk of exacerbations and hospital admissions, improves exercise tolerance, and can help reduce fatigue – all essential to improving function and quality of life.
In my role coordinating the PR service in Louth, I see first-hand the
impact it can have. Patients who were once limited by breathlessness or avoiding everyday activities – like walking to the shops or climbing stairs – are now regaining confidence and experiencing relief from the burden of respiratory symptoms.
Recent patient satisfaction questionnaires highlight the programme’s value. Many describe it as “life-changing” – not because it cures their condition, but because it gives them the tools, understanding
Community leaders, health professionals and service users gathered in The Peace Link, Clones to unveil Cavan Monaghan Connects – a new, purpose-built online hub that brings trusted mental health information, services, and training opportunities together in one easily navigated place for the people of Cavan and Monaghan.
Established by HSE Connecting for Life Cavan Monaghan, in partnership with Mental Health Ireland, Cavan and Monaghan County Councils, and a broad network of local community and statutory organisations, the project was developed in response to the growing need for quality-assured and evidence-based information related to mental health and wellbeing, including information on local support and services available. Its mission is to promote positive mental health, reduce stigma, and ensure that everyone in Cavan and Monaghan can quickly find reliable
and confidence to manage it. One participant shared, “By doing the exercises and breathing, I can manage things a lot better now.”
Another said, “The information was excellent – I’ve learned more in these classes than I have anywhere else.”
We marked Pulmonary Rehabilitation Awareness Week (16-20 June) in our health region with a community-focused campaign to raise awareness among both healthcare professionals and the public. With support from Louth County Council and the HSE Health Promotion and Improvement team, we shared educational materials, success stories and videos through internal and digital channels,

From left: Emer Mulligan, HSE Resource Officer for Suicide Prevention, HSE Cavan Monaghan Mental Health Service; Steven Ormsby, Healthy Cavan Co-ordinator, Cavan County Council (CCC); Robert Burns, Chief Executive, Monaghan County Council (MCC); Sinead Tormey, Slaintecare Healthy Communities Cavan, CCC; Cllr PJ O’Hanlon, Cathaoirleach, MCC; Cllr Trevor Smith, CCC; Lisa Cuthbert, CEO, Mental Health Ireland; Su-Zann O’Callaghan, Interim Head of Service, HSE Mental Health Service, Cavan Donegal Leitrim Monaghan Sligo; and Padraig O’Beirne, Area Director of Nursing and Chair of HSE Connecting for Life Cavan Monaghan, HSE Cavan Monaghan Mental Health Service.
local support, training and community connection.
What makes Cavan Monaghan Connects different:
• Local first – all listings are vetted, up to date and tailored to Cavan and Monaghan, reducing the needle-in-a-haystack search through national directories.
• Intuitive filters and search –visitors can sort supports by county, age group, theme or delivery type.
• Built to grow – service providers can submit events or training directly through the site, while a feedback form encourages ongoing community input and quality improvement.
Cavan Monaghan Connects is live at cavanmonaghanconnects.ie with new content added weekly.
highlighting that help is available and that people can feel better and do more, even while living with a long-term condition.
We continue to collaborate with local stop smoking services to promote integrated care and are engaging with GPs and referrers to strengthen access and continuity across the care pathway. Referrals to PR are made by a GP or consultant based on clinical need, and patients can access the programme in a variety of settings.
Raising awareness is crucial. Research shows that PR is one of the most effective nonpharmacological interventions for managing chronic respiratory disease; yet it remains underused, highlighting the need for continued awareness-raising to ensure eligible patients are considered for referral. PR supports the HSE’s broader Sláintecare goals of integrated, community-based, person-centred care – helping people live well with long-term conditions, closer to home.
To learn more, visit the National Clinical Programme for Respiratory at bit.ly/PulmonaryRehabVideos
The HSE Communications and Public Affairs Division has launched new plain language guidance for all HSE staff.
Patients and service users ask us to be clear when we give them information about their health. They also want us to show care and compassion when we talk and write to them.
When we explain things clearly with care and compassion, people have more confidence and trust in us. They are more likely to take our advice and follow medical guidance. This can help improve people’s health outcomes and quality of life.
Why we use plain language We use plain language to make information and services easy to find and understand. This makes it easier for people to make decisions about their health. Accessible information improves the lives of those using our health services and shows that we care about health literacy as an organisation.
Around 1 in 4 adults in Ireland (28%) have limited health literacy (EU health literacy survey 2021, preliminary findings). This means they may have difficulties finding or understanding healthcare information.
Health literacy is about a person’s ability to find, understand and use information to make decisions about their health. Around 1 in 4 adults in Ireland (28%) have limited health literacy (EU health literacy survey 2021, preliminary findings). This means they may have difficulties finding or understanding healthcare information. They may also find it difficult to access or use healthcare services.
People with low levels of health literacy may:
• Have poor general health
• Have longer hospital stays
• Use emergency services more often
• Go to their GP more often
• Have lower life expectancies
Find the new guidance online at hse.ie/plainlanguage or scan the QR code.

The National Adult Literacy Association (NALA) recommends healthcare professionals use less medical terminology. For example, use “high blood pressure” instead of “hypertension”. They also recommend that we all use everyday language and take time to explain health advice to people using our services. The new guidance gives many plain language examples, as well as checklists and a range of online tools to help you. Using these guidelines will help us to improve the quality of communications with people who use our services. We have to listen to them; think about how and where they get our information and what they are looking for from us. This helps us decide what kind of information might suit our audience and the most suitable ways to share that information. The new guidance replaces the Communicating Clearly guidelines and accompanying materials developed in 2018.
You can also order copies of the publication and an A3 poster from healthpromotion.ie The ordering code for the publication is HNC01094; the poster is HNC01035. If you have any comments or queries about the new guidance, please contact the HSE Communications and Public Affairs Division at comms.support@hse.ie
Gréasán Gaeilge na hEarnála Poiblí is a new cross-sectoral network for public sector staff who use Irish at work or want to use it more often, whether you’re fluent or just starting out.
With national and regional events, weekend getaways, and hobby-based meet-ups through Irish, it’s a brilliant opportunity to connect with other public servants with similar interests, develop your language skills, and enjoy using Irish in an informal, supportive setting.
For HSE staff, it supports language competence, personal wellbeing and professional development. All levels of ability are welcome and you can sign up for free at greasangaeilge.ie
If you have any questions or want to find out more, feel free to contact the Irish Language Development Team at ato@hse.ie
Is líonra úr trasearnála é Gréasán Gaeilge na hEarnála Poiblí dóibh siúd atá ag obair sa tseirbhís phoiblí agus a úsáideann Gaeilge mar chuid dá post nó ba mhaith leo níos mó Gaeilge a úsáid, cé acu má tá tú líofa nó ag tosú amach ar do thuras teanga.
Eagraítear ócáidí náisiúnta, réigiúnacha, turais deireadh seachtaine agus imeachtaí eile nach iad trí Ghaeilge. Deis iontach é casadh ar dhaoine a bhfuil spéiseanna comhchoiteanna acu leat i gcomhthéacs taitneamhach, sóisialta agus tacúil.
D’fhéadfadh baill foirne FSS tairbhe mhór a bhaint as an líonra seo ó thaobh forbairt teanga, folláine phearsanta agus scileanna gairmiúla de. Tá fáilte roimh gach leibhéal cumais agus is féidir clárú saor in aisce ar greasangaeilge.ie
Téigh i dteagmháil leis an bhFoireann
Forbartha Gaeilge ag ato@hse.ie má tá ceisteanna agat nó tuilleadh eolais uait.
The National Screening Service has produced new videos with Irish sign language (ISL) about our four screening programmes – BowelScreen, BreastCheck, CervicalCheck and Diabetic RetinaScreen. ISL is the primary language of the deaf community in Ireland, and it is estimated that more than 5,000 people use it as their first language. We produced the videos with help from the Irish Deaf Society, which made sure the content was easy to understand and culturally suitable for the deaf community. We recognise the need for inclusive communications that meet the needs of people using screening services, including the deaf community. It is part of our work to improve access to our screening programmes, and to make sure that people who use ISL have the information they need to make informed choices about taking part in screening.
The videos add to the suite of accessible information about screening already available, including easy-to-read and plain English resources, and stories illustrated by photos and videos. They fulfil a goal of our disability needs assessment report – to ensure information about the screening programmes is provided in different formats.
To view the videos, visit screeningservice.ie

Each year on 10 September, we mark World Suicide Prevention Day (WSPD) – an opportunity to raise awareness, reflect and take action to help prevent suicide. The theme for 2025 is “Changing the narrative on suicide” – a call to shift how we talk about and understand suicide and mental health.
Suicide is a complex and deeply personal issue, yet it affects us all. More than 700,000 people die by suicide globally each year, leaving behind families, friends and communities who carry the weight of that loss. But suicide is preventable – and by changing how we talk about it, we can help save lives.
What does it mean to change the narrative?
Changing the narrative means moving away from silence, stigma and misunderstanding. It means creating a culture where people feel safe to talk about their mental health and seek help without fear of judgement. Suicidal thoughts are often a sign of overwhelming pain –not weakness. Talking about suicide does not increase risk. In fact, it can be a powerful step toward healing.
This theme is reflected in Ireland’s national suicide prevention strategy, Connecting for Life, which aims to reduce suicide.
To mark WSPD this year, the HSE National Office for Suicide Prevention (NOSP) is promoting Let’s Talk About Suicide – a free online suicide prevention training programme available to everyone (see traininghub.nosp.ie). The course, which takes 60 minutes to complete, aims to equip individuals with the tools and confidence needed to have open conversations about suicide and provide support to those in need. Let’s Talk About Suicide is designed for a wide audience, including members of the public, healthcare workers, community leaders, and educators.
A day for awareness, support, and change
We recognise that this day can be difficult for those with lived or living experience of suicide. World Suicide Prevention Day is about more than awareness – it’s about fostering understanding, encouraging action, and building a community of support. Together, we can change the narrative.
For more information about WSPD, connect with the HSE National Office for Suicide Prevention on LinkedIn, by email to info@nosp.ie or visit nosp.ie
1. Reach out and check in A simple check-in with someone can bring hope and make a real difference.
2. Your words matter Speak with kindness and empathy. Everyone affected by suicide deserves dignity and respect.
3. Be safe online Share information about suicide responsibly. Help create a safer, more supportive digital space.
4. Let’s talk about suicide Learn how to recognise the signs and support someone in distress. You don’t need to be an expert to help.
5. Know where to get help
Familiarise yourself with local and national supports. Knowing where to turn can be life-saving.
Ireland’s health service featured prominently at the International Forum on Quality and Safety in Healthcare in Utrecht in May. Representing the Organisational Change Unit, Marie O’Haire, General Manager, Organisation Development and Design, and Nuala Scannell, General Manager, Health Regions Programme Team, delivered an engaging session highlighting Ireland’s progress in health system reform. Their presentation demonstrated how integrated care delivery is being enabled through a combined application of design thinking and change methodologies, drawing from the Health Services People’s Needs Defining Change Guide, design principles from the Government of Ireland and aligned with the International Foundation for Integrated Care (IFIC) Principles of Integrated Care. They shared insights on key milestones and lessons learned from delivering large-scale change. They also spoke about the importance of including patients’ and service users’ voices. They used a reflective video to show this. Their session formed part of a full-day workshop led by renowned change experts Helen Bevan and Göran Henriks, exploring the conditions required for deep, systemic transformation in healthcare. The focus was on moving beyond incremental improvements through collective inquiry, shared purpose and distributed leadership.
Speaking with Göran Henriks, Senior Fellow at the Institute for Healthcare Improvement, Marie

captured a critical insight: “Change starts by trying to understand what others understand. Ask questions, be curious, and believe people want good things.”
Professor Jody Hoffer Gittell also introduced Relational Coordination, a research-backed framework for improving interprofessional collaboration and workflow outcomes.
At the All-Ireland Huddle at the BMJ conference, colleagues across the Irish health system came together to share experiences and strengthen connections.
The health and social care system is moving forward with the health regions transformation, as part of the Sláintecare vision. The next big step is putting the Integrated Service Delivery Model into action – this means better joined-up care for patients and service users. Throughout this process, the Organisational Change Unit works in partnership with key stakeholders and leaders. All partners remain committed to supporting change across all levels. To find out more and to access our resources, see linktr.ee/hsechangeguide
Additional change management supports:
• Line manager
• Staff email updates, Health Matters and the HSE staff website: healthservice.hse.ie/staff
• HSE human resources: bit.ly/YourServiceYourSayGuidance
For the latest information on the health regions, visit about.hse.ie/health-regions
If you have a question, please contact the HSE Organisational Change Unit: organisationalchange@hse.ie

Meet Ollie, the therapy dog that brings joy to the paediatric unit at University Hospital
Ollie, an eight-year-old Malshi, visits the paediatric unit at University Hospital Galway (UHG) once a week, where his calming and comforting influence is instantly felt by patients, staff and visitors.
“Dog therapy offers a positive distraction in the unit and helps normalise the setting for children who are away from home,” says Sarah Murphy, Clinical Nurse Manager 3, Paediatric Unit at UHG. “Ollie can be a furry friend and a piece of normalcy in an unfamiliar world for children in hospital.”
Twenty-one men from Marconi Men’s Shed, Clifden recently completed an eightweek tai chi and mindfulness course. The course was organised by the carers department, HSE West and North West, with funding from Galway County Council’s Healthy Galway Fund. Participants were presented with certificates at a ceremony held in Clifden District Hospital.
Peter Jeffries from Clifden, who completed the course shared, “This was my second time doing the course. Every week was fantastic. Tai chi is suitable for people of all ages and fitness levels – at 81 years old, and the oldest participant in the group, I’m living proof. It’s a low-impact exercise with slow, gentle movements combined with mindful breathing.”
Following an evaluation of the course, Michelle Harrison, Manager of the Carers Department, HSE West and North West said, “All participants reported improvements in their overall health and wellbeing after completing the course. They highlighted benefits, including better sleep, improved coordination and flexibility, a greater sense of calm and relaxation, enhanced mood, increased shoulder mobility, reduced joint stiffness and pain, improved fitness, better stress management, more energy, and overall improvements in both physical and mental wellbeing.”
From 9-15 June, communities and organisations across counties Galway, Mayo and Roscommon came together to mark International Men’s Health Week 2025. This year’s theme, “Shoulderto-Shoulder: Connecting for Health” highlighted the importance of community and connection in supporting men’s wellbeing. Across the three counties, a diverse programme of events offered men of all ages the chance to engage, learn and take proactive steps towards better health. This included a free online webinar entitled Shoulder-to-Shoulder: A Conversation on Men’s Health.
Laurence Gaughan, Regional HSE Project Lead for Men’s Health Week commented, “Men’s Health Week provides an important opportunity to raise awareness of preventable health problems, support men and boys to live healthier lives, and encourage them to seek help or treatment at an early stage. In counties Galway, Mayo and Roscommon, a very strong partnership has been established across statutory, community and voluntary organisations, all working together to continue to raise awareness of men’s health generally and promote this annual coordinated focus.”
The bariatric service operating in Galway University Hospitals is only one of two specialist services in the country currently providing specialist multidisciplinary care for people living with obesity. Patients are referred to the service by their GP from counties all across the west.
Once at the clinic, they will be assessed and treated by the multidisciplinary team (MDT). This consists of healthcare professionals and clinicians working in dietetics, physiotherapy, occupational therapy, social work, medicine, nursing, surgery and psychology.
A person-centred, evidence-based care plan is developed in collaboration with the patient and the MDT based on the patient’s unique needs and circumstances. Patient education is an important element of this to help patients manage their condition.
Treatment by the MDT leads to improved patient health. This includes better mood, quality of life, and movement. It also results in
better control of other conditions like diabetes, high blood pressure, and sleep apnoea. It results in reduced hospital admissions, including obesity-related unplanned admissions for diabetes complications or falls and joint issues. It also results in shorter waiting times for surgery, improved patient engagement and retention in service (i.e. lower dropout rates).
The bariatric service includes a psychology team. The team helps adults with obesity who have psychological issues linked to living with the condition. This includes inpatient, outpatient, direct and indirect work as well as work with the MDT, staff consultation and allied agencies that support the person living with obesity.
Patients in the bariatric service attend for psychological assessments and interventions such as compassion focused therapy (CFT) psychology groups for emotional eating and binge eating. Patients who participate in CFT
On 20 May, a celebration was held in Unit 10 Sproai agus Spórt facility in Carndonagh, Co Donegal to mark the official reopening of Carndonagh Day Care Centre services for older persons.
The day service operates two days per week, with up to 20 people attending each day. Those attending benefit from a variety of activities, including music, dancing, card playing, poetry and chair exercises. The service allows people to socialise in their own community.
The celebration was attended by service users of the Carndonagh Day Care Centre, their family and friends, as well as the restoration committee, HSE staff and a number of community representatives. The event was broadcast live by Highland Radio. Entertainment on the day was provided by The Henry Girls, Carndonagh Choir and the Carndonagh Brass Band.
groups show their resilience and courage in developing compassionate insights into their thoughts, feelings, behaviours and life experiences, as they make positive changes for themselves.
Patients attending the bariatric service recently shared their gratitude for the compassionate, multidisciplinary care received from the team. One patient, Elizabeth Coyle, who is three months postgastric-sleeve surgery commented, “My life has changed profoundly and dramatically in the three months since bariatric surgery. I feel like I am taking back control of my health. My life is no longer dictated by an inability to move. I don’t have aches and pains anymore. I feel I have a different confidence about myself now.”
She added, “From the first time you meet [the MDT], they hear you and understand you, and there is no judgement. The support from them was immeasurable. They helped me better understand how certain bodies work and the help we need.”

This initiative marks a major investment in the health and wellbeing of patients across the Galway-Roscommon and Mayo regional health areas.
As part of the implementation of the Integrated Model of Care for Cardiac Rehabilitation, funding has been allocated for 13 whole-time equivalent (WTE) positions. These will include nursing, physiotherapy, dietetics, psychology, and administrative support, ensuring a comprehensive and multidisciplinary approach to cardiac rehabilitation.
This enhanced programme will be delivered through a coordinated model of care, integrating both
hospital and community services under a single governance structure. The end goal is to provide a fully connected, end-to-end cardiac rehabilitation pathway for patients across the region and to reduce waiting times for cardiac rehabilitation, improve patient access and experience and deliver better long-term health outcomes.
Welcoming the initiative, patient Denis Goggin said, “As someone who has directly benefitted from cardiac rehabilitation, I know how vital these services are. Expanding and improving access means more patients will get the support they need to recover and stay well.”
Opening for the first time on 3 June, this day care service operates three days per week and includes dementia-specific day care. Up to 10 people attend each day, benefitting from a variety of activities, including music, dancing, bingo, card playing, poetry, arts and crafts, and chair exercises. Mary Mahon, who attends, says, “It is a great outing. Before this, I might not have seen anybody for days. I have made lots of new friends.”
The integrated specialist continence care service (ISSCS) was recently launched in Donegal. Designed to transform the management of urinary incontinence, the service brings expert care closer to home and offers timely, effective treatment through an integrated approach. With urinary incontinence affecting 1 in 3 women and 1 in 10 men, the need for early intervention and community-based support is greater than ever. The ISSCS is a key component of a new Urology Model of Care, delivering services through local primary care centres and hospitals. This model has developed three pathways: haematuria, lower urinary tract symptoms, and continence management with ISSCS.


The respiratory integrated care team, Galway City Integrated Care Hub, and the HIVE Laboratory at the University of Galway were recently honoured at the Irish Healthcare Centre Awards for their virtual care initiative for COPD patients. The initiative, which leverages remote patient monitoring technology, was recognised with the award for Best Use of Information Technology.
Rather than relying solely on containment products, the ISSCS prioritises identifying and treating the root causes of incontinence. This not only improves quality of life but also helps reduce hospital visits, GP workload, and healthcare costs.
The COPD virtual care pathway, which launched in April 2024, has redefined how care is delivered to patients experiencing a COPD exacerbation. Professor Sinead Walsh, Consultant Respiratory Physician, University Hospital Galway and Respiratory Lead for the Galway City Integrated Care Hub said, “This pathway allows us to detect deterioration earlier, provide timely interventions, and support patients to recover safely in their own homes. The feedback from patients has been overwhelmingly positive – that they feel more in control of their health.”
A newly introduced wellness walkway at Roscommon University Hospital (RUH), designed to promote the health and wellbeing of patients during their recovery from illness and injury, is proving to be a valuable asset in supporting patients.
Located on the first floor of the hospital, the walkway was developed in collaboration with members of the multidisciplinary team, including physiotherapy, occupational therapy, nursing, and the patient advocacy and liaison service (PALS). Each station along the walkway features a range of physical and cognitive exercises, offering patients the opportunity to engage in therapeutic activities tailored to aid both body and mind.
The project was funded by the RUH Healthy Ireland committee, reflecting the hospital’s ongoing commitment to creating a healthpromoting environment for all.
Speaking about the initiative, Marie Doorly, Interim Hospital Manager said, “We are delighted with the
positive impact the wellness walkway is already having on our patients. It offers a supportive space where they can engage in gentle activity and mental stimulation, both of which are key to a holistic recovery.”
Patient Mary Mullally Keane from Lecarrow in Co Roscommon spent four weeks in hospital and described the walkway as an essential part of her recovery journey and daily life: “The wellness walkway has made a tremendous difference to my wellbeing. I use it almost every day, sometimes with my physiotherapist, sometimes with my husband Christopher or my son Enda, and often on my own. It’s a place of stillness, light and warmth. I use it not only for my exercises but also as a space to meditate and reflect. It has truly supported my recovery, and I know it’s having a positive impact on many other patients as well. I’m deeply grateful to my physiotherapist Fionnuala, and to all the doctors and staff at the hospital for their exceptional care and support.”
On 30 May, the Sacred Heart Hospital (SHH) Castlebar, in collaboration with the Mayo Arts Office, hosted an Arts and Health Awareness Day for residents, staff, families and friends as part of Bealtaine –Ireland’s national festival celebrating the arts and creativity as we age.
Helen Walsh, Assistant Director of Nursing at SHH Castlebar said, “We are aware that we have some very talented artists among our residents. This event fosters connection and highlights the benefits of integrating arts into healthcare here in the Sacred Heart Hospital.”
Patient Mary Mullally Keane with Senior Physiotherapist Fionnuala Morrissey at the wellness walkway in Roscommon University Hospital.

Fionnuala Morrissey, Senior Physiotherapist at RUH, also spoke about the impact of the initiative: “The wellness walkway offers patients a safe, accessible and engaging environment to continue their rehabilitation outside of traditional therapy sessions. It encourages independence, improves physical activity levels and confidence, and supports the emotional wellbeing that is so essential to recovery.”

Roscommon University Hospital (RUH) has donated reusable medical equipment valued at €150,000 to Zambia as part of its ongoing commitment to global health equity through the EQUALS initiative.
The EQUALS project, established by the Royal College of Physicians of Ireland and the HSE, aims to reduce global health inequalities and partners with local health services in low-income countries to deliver vital medical equipment and training. This most recent donation from RUH will help further strengthen healthcare infrastructure in Zambia, improve patient care, and support medical staff.
“We are proud to support the EQUALS initiative,” said Marie Doorly, Interim Hospital Manager. “This donation reflects our hospital’s dedication not only to serving our local community, but also to extending care and compassion across borders.”

The 10th annual Research and Academic Awards Day at Galway University Hospitals took place recently to showcase the extraordinary level of talent, innovation and dedication across multiple medical and healthcare disciplines. With 115 abstract submissions and 105 posters exhibited in the Clinical Science Institute building, the event celebrated the remarkable contributions of staff from health and social care professions, nursing and midwifery, and non-consultant hospital doctors.
The afternoon was filled with engaging presentations that covered a wide range of topics, including research, audits, quality improvement, and clinical cases. A total of 26 presenters delivered high-quality talks, highlighting exceptional clinical innovation and excellence.
This year also saw the introduction of two prestigious new awards, the inaugural Florence Nightingale Medal for Nursing and Midwifery and the Surgical Academic Award.

Back row, from left: John Carr, Michael Kilcline and Johnathan Farrell, Maintenance, Roscommon University Hospital (RUH); front row, from left: Marie Doorly, Interim Hospital Manager, and Pauline Conroy, IT Manager, RUH.
A very generous donation of equipment was recently presented to the Patient Comfort Care Treats Fund, Department of Psychiatry in Roscommon University Hospital in memory of the late Seán Donelon, Glenamaddy, Co Galway, who was previously an inpatient in the unit.

From left: Seán Donelon’s sister Claire Dolan; Adrian Tully, Clinical Nurse Manager III, Department of Psychiatry, Roscommon; Paddy Lavin, Assistant Director of Nursing, Department of Psychiatry, Roscommon; and Kate Fahey.
The equipment, including iPads, PlayStations, wireless headphones, Nintendo Switch, seating and furnishings, was presented to the Patient Comfort Care Treats Fund by Seán’s sister, Claire Dolan, and Kate Fahey. The funding for the equipment was raised primarily by the Glenamaddy Truck and Tractor Run. The fundraising was undertaken by the family in appreciation of the care Seán received while he was a patient in the unit.
Adrian Tully, Clinical Nurse Manager III, Department of Psychiatry, Roscommon says, “We are very grateful to Claire, Kate, the Donelon, Dolan and Fahey families for organising the very generous donation of equipment to the Patient Comfort Care Treats Fund in the memory of Seán. These items are and will be extremely beneficial to inpatients in our unit. The memory of Seán will live on through the happiness brought to many during their recovery journey.”


Minister for Health Jennifer Carroll MacNeill recently visited a number of locations across HSE West and North West.
On 1 May, she visited the construction site of the Letterkenny Community Hospital development. The new 110-bed unit is a major enhancement of services for older people in Co Donegal and will provide modern, fit-for-purpose facilities for both short- and long-term care. It will also include a new 10-bed dementia unit.
She then went on to Letterkenny University Hospital where she visited the emergency department and haematology/oncology ward, which has been newly restructured to enhance patient care and experience. She also explored the Errigal Chronic Disease Management Hub, where she was given an update on the Care Virtual Ward programme.
On 2 May, the Minister officially opened new infrastructure developments in Sligo University Hospital (SUH), including 26 beds in the SUH offsite ward located in St John’s Community Hospital. This facility began receiving patients in January and has had a positive
effect on patient flow and overcrowding in SUH.
At SUH, the Minister also turned the sod on the site of the new 42-bed day ward development. This will enable greater quality of service and improved patient outcomes where patients receive care in an appropriate setting in a timelier manner.
A second CT scanner at SUH was also opened by the Minister as part of the visit. This will ensure continuous coverage for trauma, stroke, emergency and inpatient services, improve GP access and provide in-house contingency.
The Minister then visited Carrickon-Shannon where she laid the first brick of the new 90-bed Community Hospital. This will facilitate long-stay, short-stay dementia wards and a designated rehabilitation facility. The design of the Community Hospital aims to create a person-centred approach, which supports the opportunity for older people to continue to direct their own lives in accordance with their cognitive and physical abilities, and in an environment that reflects the comforts of home.
On 15 May, the Minister visited Galway University Hospitals, where
she welcomed the progress in the University Hospital Galway infrastructure masterplan, which will deliver safe, person-centred healthcare into the coming decades. The plan comprises the following major projects, to be delivered in a phased manner, providing meaningful additional capacity in a way that does not disrupt the ongoing operation of the hospital:
• Two new ward blocks, each providing 150 acute beds
• An ambulatory cancer centre
• A new laboratory block
• A new emergency, ICU and surgical block
The works also include a new permanent helipad, which allows the hospital to be future-proofed for the next 40 years.
The final stages of the development control plan includes the following additional accommodation: an enlarged main entrance, an enlarged paediatric and maternity centre, and facilities for staff, research and education. As part of her visit, the Minister went to the Merlin Park campus to view the site of the new surgical hub, the proposed site for the planned new elective hospital and the recently opened outpatient department.

Many health service employees, working in both frontline and supporting roles, are motivated by the desire to offer support, advice and care to the wider population to manage their health and wellbeing. But what happens when an employee themselves is diagnosed with serious illness such as cancer and transitions for a period of time from employee to service user?
The new HSE service, For Survivors, By Survivors is a cancer survivorship peer support service that has been established to fill this gap. It offers one-to-one support to employees from the point of cancer diagnosis, through the treatment phase, on returning to work or considering other options, and in re-establishing life after cancer treatment.
The National Cancer Control Programme states that “one in two
people in Ireland is expected to have cancer in their lifetime”. This stark figure can be tempered with the fact that 4% of the population are cancer survivors and that this survivorship figure is expected to double over the next 25 years. Improved screening programmes, early detection, better treatments and survivorship supports are working together to continuously improve outcomes for people affected by cancer. But a population-wide
From left: Liz Tobin, Bernadette Smith, Niamh O’Leary, Aisling Kenna, Catherine Lynch, Sharon Dowling, Margaret McKenna, John Donoghue, Siobhan Patten, Elaine Carpenter, Helen Forristal, Isabelle McShane, Shirley O’Shea, Marie O’Brien, Paula Gleeson, Susan Wallace, and Ann Marie Kennedy.
What is offered and where does the service fit with other HR services and management support?
The service offered by the peer supporters is informed by their own experiences, and is twofold:
• Signposting to both internal and external services such as the HSE’s rehabilitation policy, advising on the process of seeking reasonable accommodation, local HR contacts, and advising on external services such as those offered by the network of Cancer Care Centres around the country, specialist cancer supports, social protection information and much more.
• Befriending and ‘walking the journey’ with the newly diagnosed staff member. Peer supporters, where appropriate, will share their own experiences of talking to family and friends, supports they availed of during treatment and the supports they availed of on return to work, in situations where it is helpful to the person being supported.
What users of the service, those delivering the service and line managers say about it
A recent evaluation of the service was conducted by researchers in University College Cork. The findings were extremely positive, with 89% of
line managers, 100% of peer supporters and 93% of those supported recommending the service.
The following two comments from service users demonstrate the value of the service:
“It’s such a frightening time being diagnosed, and having a friendly face or voice, a person who has walked in your shoes, showing you there is light at the end of the tunnel… Well, isn’t that what everyone needs?”
“What an amazing service this is. My peer supporter was generous with her time and support and helped me think through my return to work and identify what I needed to help me do so. It was so important to hear from someone who had ‘been there’ and was successfully navigating the world of work again post-treatment.”
How to access the service and get matched with a peer supporter
The HSE has worked closely with the Marie Keating Foundation in the development of this service, and the foundation continues to provide the matching process between peer supporters and those wishing to access the service. Matches are overseen using a set of agreed criteria such as cancer type, age, needs of the person wishing to access the service, and availability of peer supporters.
To access the service, phone 087 334 0235; email hsestaff@mariekeating.ie; or visit mariekeating.ie/hse-for-survivors-by-survivors
statistic also impacts on our workforce, and the increasing numbers of cancer diagnoses are reflected in the health workforce.
A comprehensive literature review by Health Library Ireland established that work is a meaningful aspect of cancer survivors’ lives, and that rebuilding through rehabilitation, and re-establishing self-efficacy are important components of survivorship. Emotional support
is especially beneficial when individuals providing support have lived experience with cancer.
Who are the peer supporters?
The cancer survivorship peer supporters are all health services employees who themselves have had a diagnosis of cancer and now work in a voluntary capacity to partner with employees newly diagnosed to walk the journey of cancer with them.
The peer supporters come from a wide variety of clinical and non-clinical roles and have been through an in-depth selection and training process. The service is strictly non-clinical, and the peer supporters do not give clinical advice.
As one peer supporter puts it: “When they were looking for volunteers, I think for me it jumped out… that is what I wish I would have had before I came back to work.”
Minister for Health, Jennifer Carroll MacNeill, and Minister of State for Public Health, Wellbeing and the National Drugs Strategy, Jennifer Murnane O’Connor, published the National Sexual Health Strategy 2025-2035 in June. The HSE Sexual Health Programme in HSE Health and Wellbeing play an ongoing key role in the implementation of sexual health programmes across the health service.
At the recent National Health Promotion Conference in Galway, Minister Murnane O’Connor and colleagues from the Department of Health and the HSE outlined the background and ambition for the new 10-year strategy. Professor Fiona Lyons, Clinical Lead with the HSE Sexual Health Programme, highlighted the progress and learning made in the decade since the first National Sexual Health Strategy, including the national condom distribution service and the free home STI testing service, and welcomed the focus on equity in the new strategy.
The second sexual health strategy contains a number of commitments designed to support positive sexual health for everyone in Ireland, across all stages of life.
Priorities include:
• Expanding capacity and further developing testing and treatment for sexually transmitted infections (STIs) including the home STI testing service
• Increasing access to contraception by expanding the free contraception service and the free national condom distribution service
• Building capacity to meet demand for HIV prevention and treatment, including preexposure prophylaxis (PrEP) and post-exposure prophylaxis (PEP) and additional supports for
people living with HIV
• Developing a model of care for sexual health services, focusing on prevention, diagnosis, treatment, information and surveillance for STIs and HIV, and improving geographic equity
• Improving access to vaccines that support sexual health, such as the human papilloma virus (HPV) vaccine, and hepatitis A and B vaccines
• Supporting the work of the justice sector and Cuan in domestic, sexual and genderbased violence (DSGBV) prevention
For more information about the work of the HSE Sexual Health Programme, visit sexualwellbeing.ie
On Tuesday 17 June, the HSE launched its updated Open Disclosure Policy 2025. The policy aims to support those involved in incident management and the open disclosure process, in particular patients, relevant persons and staff. Clear information is provided about the important elements of the process and supports available. The HSE is committed to driving a patient safety culture that is open and transparent. Being truthful when an incident occurs is critical when caring for patients and service users or their relevant person. Much insight has been amassed in the six years since the policy was last published. There has been a significant amount of learning since the policy was last published six years ago. The updated policy incorporates this learning to further drive improvements in open disclosure.
The HSE Open Disclosure Policy 2025 also incorporates national developments such as the Patient Safety (Notifiable Incidents and Open Disclosure) Act 2023 and the Department of Health National Open Disclosure Framework, and international developments by the World Health Organization. The revised policy outlines the importance of support for all those impacted by an incident and it identifies steps to take towards the prevention of further harm. It focuses on the importance of supports for service users and their relevant person during the communication that follows a patient safety or notifiable incident. It also identifies the importance of supporting our staff, not only to guide them on the requirements of the policy, but to ensure that they too are supported following an incident. Many incidents span over several teams and services.

We must support one another in open disclosure to provide the service user and their relevant person with the most comprehensive and supportive experience across health and social care services at such difficult times.
For more information visit the dedicated Open Disclosure webpages or contact the National Open Disclosure Office on OpenDisclosore.Office@hse.ie
As part of our commitment to strengthen child protection across the HSE, a new National Policy for Child Safeguarding and Wellbeing within Adult Mental Health Services has been launched.
The policy provides essential guidance for staff working with adult service users who are parents or in close contact with children. It ensures that child safeguarding becomes a routine and visible part of mental health care throughout a service user’s journey – from assessment through to recovery. This policy must now be embraced by all adult mental
health professionals as an essential part of daily practice.
While most adults accessing mental health services do not pose a risk to children, we know that issues such as mental illness, domestic abuse and addiction can sometimes lead to serious harm. This policy acknowledges those risks and supports staff in recognising when a child may be vulnerable – even if signs are not immediately clear.
Importantly, this policy does not replace the HSE’s existing Child Protection and Welfare Policy –both policies must be followed in practice. Where concerns arise, the
HSE Child Protection and Welfare Reporting Procedure must be used.
Key implementation steps for this policy include revising the assessment template to reflect a “Think Family – Think Children” approach, equipping clinicians to be alert to and spot concerns at follow-ups and supporting multidisciplinary work.
This year’s Children First Awareness Week reminds us: “We were children once. Now we are Children First”. Let’s lead by example – protecting children not just through policies, but through culture and commitment.
The summer months have been busy and rewarding. We have pushed forward in our efforts to involve patient and service user voices in the ongoing design of the health regions. We saw some new services introduced and current services being celebrated for the great work they are doing. We also launched the Dublin and Midlands regional news update in June. This is our monthly newsletter, which aims to keep regional staff up to date on important news and events, and share information on some of the wonderful work by staff across our region.
On Friday 4 July, we held the first Regional Patient and Service User Engagement and Partnership Workshop. We aim to ensure that the patient and service user voice is also built into the development of the National Strategy for Patient and Service User Engagement.
With an ambitious agenda, it was an incredibly engaging day, where service users and staff came together to look at what is working well in our health and social care services and what needs improvement. The focus was on real-life changes that will make a real impact on our service users.
We also saw the opening of a 12-bed health and addiction stabilisation service in our region in July, bringing the total number of beds available for treatment to 63. Usher’s Island health and addiction care facility is a collaborative project between the Department of Health, the HSE and Dublin Simon Community to improve access to healthcare services and support the health and addiction care needs of homeless adults.

Regional Executive Officer Kate Killeen White described it as “a very positive development for our service users across Dublin, Kildare and West Wicklow”, adding that “the primary care and social inclusion team continue to work closely with Dublin Simon Community to optimise service user pathways, maximise all
available resources, and plan for future expansion of the facility”.
Minister for Health, Jennifer Carroll MacNeill extended her thanks “to the HSE team working on this vital project, which reflects our commitment to enhancing healthcare services to address the complex health needs of people who are homeless”.
Congratulations were due to various teams across the region following the HSE Spark Summit (11 June). HSE Dublin and Midlands’ winning innovations include:
• CEO Choice Innovation Awards for Best Patient Access awarded to Linda Keogh (Best Patient Access: Community Setting) and Dr Laura Piggott (Best Patient Access: Hospital Setting)
• Best Multi-Disciplinary Team awarded to Dr Aileen McCabe
• Best Design-Led Project awarded to the CHO8 Children’s Services Project Team
• Best Leadership Award given to Edel Carey
• Best Doctor-Led Project awarded to Mairead McNally
• Best Poster awarded to Avril Gannon
These individuals and teams exemplify innovation in action. Congratulations to all our winners – your dedication continues to make a lasting impact across our health service.
Catch up on the latest regional stories at bit.ly/DublinMidlandsHospitalGroupNews
St James’s Hospital became the first acute hospital in Dublin to receive the internationally recognised Green Flag, marking a major milestone in sustainable healthcare. Awarded through the Green Campus Programme by An Taisce, the Green Flag recognises long-term commitment to environmental responsibility. Since 2018, the hospital has implemented a sustainability framework across energy, water, transport and waste. Key achievements include:
• 34% improvement in energy efficiency
• 34% reduction in carbon emissions
• 42% reduction in water usage
• Major improvements in waste management, including a 68% drop in clinical waste

“This Green Flag is more than a symbol, it reflects our deep commitment to greener practices while providing patient care,” says Mary Day, CEO of St James’s Hospital.
Midland Regional Hospital Tullamore (MRHT) is transforming joint replacement surgery with its pioneering day case arthroplasty programme – one of the first of its kind in Ireland. This innovative approach allows selected patients to return home the same day as their hip or knee replacement, promoting faster, more comfortable recovery in familiar surroundings.
The benefits are clear: shorter hospital stays, reduced risk of infection, improved sleep and nutrition, and quicker return to daily life. Early mobilisation is a key feature, helping patients regain strength and independence sooner. At the heart of the programme is a strong focus on patient empowerment. Through preoperative education, including a comprehensive “joint school”, patients are fully prepared for surgery, recovery, and discharge.

“Patients are more motivated, confident, and engaged,” says Dearbhail Foy, Arthroplasty Nurse Specialist. “They know what to expect and feel supported every step of the way.”
Former patient Fiona Brady shares her experience: “Recovering at home was so much better. The preparation beforehand made all the difference. Eight weeks post-op, I’m pain-free and feeling amazing.”
Mr Khalid Merghani, Consultant Orthopaedic Surgeon, highlights the
clinical benefits: “Minimally invasive techniques like the direct anterior approach for hips, and subvastus approach for knees, preserve muscle, reduce pain and enable faster mobilisation. With computer assistance and robotic navigation, we’re achieving greater precision and better outcomes.”
Dr Mugawar Mohan, Consultant Anaesthetist, adds: “Day case arthroplasty is not only safe but also cost-effective. With the right patient selection and enhanced recovery protocols, it’s a win-win for patients and healthcare systems.”
From a hospital perspective, the initiative improves efficiency, reduces bed occupancy, and maintains high-quality care. Every patient’s journey is tracked through the Irish National Orthopaedic Register, ensuring continuous improvement. MRHT’s day case arthroplasty programme is setting a new standard in orthopaedic care –where patients recover faster, feel better, and return to their lives sooner.
The Cellular Pathology Laboratory at Tallaght University Hospital (TUH), responsible for testing patient tissue samples, has just installed a cuttingedge new piece of equipment known as the Axlab AS-410M. This new development will speed up and significantly increase the hospital’s capacity to test patient samples.
TUH is the first site in Ireland to introduce this vital piece of new equipment. The purchase was funded by BowelScreen, a national programme which first began at TUH.
The main benefit of the Axlab AS-410M is that it can automate one of the most time-consuming, manual, and repetitive tasks in the lab. This is a very significant development for TUH as the demand to test patient samples has increased by almost 25% over recent years due to significant service expansion in the hospital.
TUH is currently in an expansion phase, increasing capacity in areas such as dermatology, gynaecology, surgery and endoscopy, all of which directly impact the demand for cellular pathology testing in the hospital laboratory. Additionally, the complexity of testing has increased and is expected to continue rising, putting additional demands on the service.
Sarah Delaney, the Chief Medical Scientist in the Cellular Pathology Laboratory at TUH says, “Our lab receives about 65,000 patient samples per year. One patient sample could need up to 20 blocks, depending on the sample type. Each block could produce 1-20 slides.

Before the arrival of the new technology, our laboratory had a shortfall of 160 blocks a day. We will now be in a position to create 200-300 blocks per day, so we are somewhat future-proofed for increased demand as our services grow.”
Welcoming this new cutting-edge development, Interim CEO of TUH John Kelly says, “The installation of this advanced piece of equipment marks a significant step forward for the service. It will enable us to efficiently handle increased workloads and tackle unexpected challenges, such as busy periods, equipment breakdowns, and staff leave. This technology empowers
our skilled laboratory staff to be freed up from manual tasks to focus on more complex responsibilities while ensuring continued compliance with mandatory training standards.”
With the introduction of this new equipment, the hospital’s Cellular Pathology Lab will now have the increased testing capacity to meet current and future demands and will no longer need to outsource work.
In Ireland, everyone aged 59 to 70 can have free bowel cancer screening. This can help find bowel cancer before symptoms present. If bowel cancer is found early, it’s easier to treat and there’s a better chance of recovery.
To register for your free screening test, visit bowelscreen.ie
On 5 June, HSE Dublin and Midlands officially opened the new Uisneach Integrated Centre for Healthy Ageing at a conference titled Transforming Ageing and Longer Lives – new horizons in the Midlands and beyond, as part of the Integrated Care Programme for Older People (ICPOP).
The centre is situated on the grounds of St Mary’s Hospital, opposite the Regional Hospital Mullingar. The ICPOP community specialist team work together to assess and respond to an older person’s needs, thus helping older people maintain their independence and live well at home.
Kate Killeen White, Regional Executive Officer, HSE Dublin and Midlands welcomed the opening of the facility stating, “The new Uisneach Centre for Healthy Ageing will support older people to maintain their health, independence and wellbeing.”
Officially opening the centre, Dr Donal Fitzsimons, Head of Service for Older Person Services in the Midlands said, “I am delighted to be here today to officially open the

From left: Dr Siobhán Kennelly, Consultant Geriatrician for Integrated Care Service for Older People Westmeath/Longford; Catherine Carragher and Michele Baker, Health Promotion and Improvement, Health and Wellbeing; Breege Doherty, General Manager (Older Persons); Dr Donal Fitzsimons, Head of Service for Older Person Services in the Midlands; Dr Niamh O’Callaghan, Consultant in Public Health Medicine – Health Intelligence; Dr Mary Doolan, Integrated Care Programme for Older Persons (ICPOP) Operational Lead; and Joan Crawford, Health Promotion and Improvement, Health and Wellbeing.
Uisneach Centre. The community specialist team based in the centre will support older people by providing timely access to specialist health services, resulting in a coordinated plan and delivery of care, which leads to better health outcomes for older people in the Midlands.”
Dr Siobhán Kennelly, Consultant Geriatrician for the Integrated Care Service for Older People Westmeath/Longford said, “This specialist service will build on pathways and services, supporting
Maynooth Community Care Unit (MCCU) was the recipient of one of nine awards presented at the Kildare County Council Decarbonising Zone 2025 Climate Champions event in June. They were awarded the top prize, the Oak Award for leadership in driving sustainability, from Kildare County Council and Kildare Climate Action Office.
The HSE-owned Older Persons Service has embraced environmental stewardship by
taking steps to reduce their carbon footprint and implement objectives of the HSE Climate Action Strategy and HSE Capital and Estates Infrastructure Decarbonisation Roadmap. This is made possible by the proactive and engaged MCCU green team that is supported with funding from the HSE Capital and Estates Sustainable Infrastructure Office.
The Oak Award DZ Climate Champion Award for MCCU is a testament to the dedication
the needs of older people in the Longford/Westmeath area, focusing on the integration of care between acute hospital and community services for older people.”
Expert guest speakers in the field of gerontology spoke to the burgeoning research area of healthy ageing. The conference hosted representatives from the Longford/ Westmeath Living Well group, which represents a number of other statutory, voluntary and community agencies, all of whom are integral to the working of the Uisneach Centre.

Members of the Maynooth Community Care Unit receiving the Oak Award for leadership in driving sustainability.
onsite to keep climate action and sustainability high on the agenda and mobilise a coalition of those willing to achieve climate action targets.

family.
Cherry Orchard Hospital (COH) celebrated the retirement of one of its most respected and beloved figures, Dr Seamus O’Dea, on Friday 4 July. The event marked the end of an extraordinary 46-year career in medicine, during which Dr O’Dea served with distinction, compassion and unwavering commitment to patients, staff and the wider community.
From his first day at Cherry Orchard Hospital in 1979, Dr O’Dea dedicated his career to improving the lives of others. He began his journey in medicine and qualified as a doctor in 1976. Following internships at Tullamore and Vincent’s Hospitals, he brought his medical expertise and a remarkable empathy, developed through personal experience, to Cherry Orchard.
Throughout the decades, Dr O’Dea not only witnessed but led transformations in the Irish healthcare landscape. From managing outbreaks such as salmonella in 1982 to supporting psychiatric and older adult care through major national and international crises, his leadership was steadfast and deeply compassionate.
One of Dr O’Dea’s many remarkable contributions came through his specialist training in tropical medicine. As he recounted: “Not long after I started at Cherry Orchard, a young boy admitted with suspected chickenpox didn’t look right… I recognised signs of myiasis from my diploma in tropical medicine. It proved how valuable that training could be.”
Beyond his clinical skills, Dr O’Dea’s mentorship and collaboration with staff across all departments made a profound and lasting impact. He worked alongside former ministers, microbiologists, nurses and residents, many of whom paid tribute to his empathy, integrity and sense of humour.
“There will never be another doctor like you. Your humanity and compassion have left a mark that can never be measured but that will always be felt.”
A message from nursing colleagues stated: “Dr O’Dea… your calm, caring manner alongside your diligent communication skills has rightly earned you the immense respect and affection of staff, residents and families alike. Your absence in COH will be profound, but your legacy of work here should and never will be forgotten.”
Colleague Edel Carey, Advanced Nurse Practitioner said: “There will never be another doctor like you. Your humanity and compassion have left a mark that can never be measured but that will always be felt.”
Residents and their families echoed this sentiment: “Dr O’Dea is always there to help us and make sure that all patients are okay… I wish him all the best in the world.”
– Mary Brennan, resident.
“Our family owes a big depth of gratitude… we have all experienced his kindness and gentleness.” – Dónal and Anne.
In 2007, Dr O’Dea oversaw the opening of new modernised Cherry Orchard Hospital units, a project he championed as a significant step forward in patient dignity and care. Reflecting on his career, he noted: “It’s not just about bricks and mortar, it’s about a complete shift in ethos.”
As Dr O’Dea retires, his influence continues through the values he instilled in others: care, trust, compassion and learning. His story stands as a powerful reminder of what a life of public service can achieve, not only within hospital walls but in the lives of all those he touched.
Staff at Naas General Hospital came together for the multidisciplinary Stroke Education Day. It was a powerful event that placed the patient experience at the heart of learning.
The highlight was a deeply moving session with Paula, a former stroke patient, who bravely shared her personal journey through stroke care. From the moment she arrived in the emergency department to her time in rehabilitation, Paula recounted the emotional and physical challenges she faced. Her story offered invaluable insight into what it truly means to experience a stroke, not just medically, but personally.
She spoke candidly about moments of fear and confusion, the importance of clear communication, and the small acts of kindness from staff that made a lasting impact. Paula also offered constructive feedback, suggesting ways the care experience could be improved for future patients. Her reflections reminded everyone in the room that behind every clinical decision is a person navigating one of the most vulnerable times of their life.
For many staff, Paula’s story brought to life the very treatments and interventions discussed throughout the day. Sessions covered a wide range of topics, including:
• Physiotherapy and mobility after stroke
• Communication and cognitive impairments
• Dysphagia and nutritional care
• Medication management
• Post-stroke support services
Colleagues from physiotherapy and occupational therapy also led hands-on demonstrations, allowing attendees to experience first-hand the complexity of stroke rehabilitation, from upper and lower limb splinting to safe patient transfers and positioning.
The day concluded with emotional reunions between Paula and the staff who had cared for her, a testament to the lasting bonds formed through compassionate care.

Feedback from the event has been overwhelmingly positive, with many attendees expressing gratitude for the opportunity to learn through both clinical expertise and lived experience. As one attendee expressed, “understanding stroke begins with listening to those who’ve lived it”.
We are pleased to announce the appointment of a number of new clinical leads who will report directly to the Office of the Regional Clinical Director:
• Dr Yolande Ferguson, Regional Clinical Lead for Mental Health (commenced in March)
• Dr Eoin Sheehan, Regional Clinical Lead for Perioperative Services (commenced in July)
• Dr Siobhán Ní Bhriain, Regional Clinical Lead for Medicine (commenced in August)
“These roles are key appointments that reflect our commitment to putting clinical leadership at the heart of healthcare delivery,” says Kate Killeen White, Regional Executive Officer for the Dublin and Midlands Region.
We also recently welcomed Lisa O’Farrell to the region as the Head of Quality and Patient Safety in June. As part of her role, Lisa will develop and lead on the implementation of the Quality and Patient Safety Strategy across the region. Lisa has worked for over 20 years in health services with particular expertise in mental health services and the nursing home sector.
World Hand Hygiene Day was celebrated on 5 May and promoted in community services in Dublin South City and West, Dublin South West, Kildare and West Wicklow and focused on improving hand hygiene practices and awareness. Infection Prevention and Control (IPC) link practitioners and hand hygiene trainers led campaigns, education sessions, demonstrations, competitions and activities to promote correct hand hygiene practices among residents, clients, colleagues and visitors. These efforts enhanced knowledge and strengthened a culture of infection prevention best practice. The IPC community team would like to thank all the staff who took part and who have been involved in promoting and advocating good hand hygiene practices across our services, making our facilities and services a safer place for people to live, work and visit.
The HSE plans to open six surgical hubs across Ireland to increase the capacity for day case surgery and minor procedures. Each hub plans to deliver 10,000 day case surgeries and minor procedures, and 18,500 outpatient consultations annually.
“Reducing waiting lists and waiting times for patients is a key priority for the HSE,” says HSE CEO Bernard Gloster. “By moving day case procedures to the surgical hubs, hospitals around the country will have greater capacity for patients who require emergency and more complex care.”
The surgical hub in South Dublin was officially opened in February by Minister for Health Jennifer Carroll MacNeill TD. It consists of four theatres and will deliver additional capacity to support scheduled care for day cases and reduce waiting lists. This will enable the separation of scheduled and unscheduled care and allow existing acute capacity to support urgent and more complex procedures in South Dublin. The hub, under the governance of St James’s Hospital, includes state-of-theart facilities with one of the first green theatres in Ireland.
Construction has commenced on the Limerick surgical hub, a HSE Mid West project that will significantly increase theatre capacity in the region and reduce the times patients currently wait for day surgery.
The €60 million complex will have two operating theatres and two procedure rooms and will be located at the former Scoil Carmel site on O’Connell Avenue in Limerick City. It is scheduled to come into operation before the end of 2026.
Construction of the surgical hub is currently underway on the Merlin Park campus. It is expected that the building infrastructure will be completed in Q4 2025 and the hub will be commissioned soon thereafter. The surgical hub will provide regional capacity and operate under the governance of Galway University Hospitals. The facility will support decongestion on the University Hospital Galway site, where there are significant demands and volumes of scheduled and unscheduled patient services, including many planned and scheduled day case procedures and a very significant unscheduled care stream.
Minister for Health, Jennifer Carroll MacNeill TD officially turned the sod on the Waterford surgical hub on Friday 13 June. The new state-of-the-art healthcare facility is designed to reduce patient waiting times in the South East.
The completed development will comprise of two fully operational theatres and two further theatres that can be fitted out at a later date if needed. The new theatres will deliver additional capacity to support scheduled care for day cases and reduce waiting lists. This will enable the separation of scheduled and unscheduled care and allow existing acute capacity to support urgent and more complex procedures at University Hospital Waterford.
Construction on the surgical hub in Swords is progressing on site with the current projected completion date for the construction element being Q1 2026. Once complete, the building will be handed over to HSE service colleagues, who will take operational control and governance of the facility, complete the clinical commissioning and operationalise the facility.
Exciting developments are underway on the Cork University Hospital campus, where the new Cork surgical hub is taking shape. Designed as a regional centre of excellence, the hub will serve patients not only from Cork but also from Kerry and beyond –bringing high-quality surgical care closer to home for thousands. The facility will support over 90 surgeons and is being delivered on schedule and within budget. It is expected to welcome its first patients in July 2026.
The Cork surgical hub is one of the fastestmoving capital projects in recent memory, and its development marks a significant step forward in addressing waiting lists and improving access to surgical services across the South West.
Staff recruitment has now commenced, with planning underway to ensure the hub delivers a high-performing, patient-centred service. The Cork surgical hub is a key part of the HSE’s broader strategy to enhance regional healthcare infrastructure and improve outcomes for patients through integrated, efficient and accessible care.
Regional Hospital Mullingar Research and Audit Day
The annual Research and Audit Day for the Regional Hospital Mullingar will take place on 8 October. This year’s theme is “Advancing Healthcare: Integrating Research, Clinical Audit and Education for Patient Safety”.
This day recognises and commemorates research and audit projects undertaken by staff in the Regional Hospital Mullingar. The event consists of poster and podium presentations with three prizes in each category; an additional people’s choice prize will also be presented. The day will be opened by Professor Des Toomey, and closing remarks will be given by Mags Kelleher, Hospital Manager. Guest speakers will include Mary Nolan, Nursing and Midwifery Planning and Development Unit.
Scan the QR code to read more on the event

The HSE has expanded its free and confidential home testing service for hepatitis C to include a new rapid oral swab test. This simple, easy-to-use test delivers results in just 20 minutes and can be ordered directly to your home.
The new oral swab test offers people a quick and convenient way to check for hepatitis C without the need to visit a clinic. It complements the existing lab-based home test, which involves a small fingerprick blood sample sent to a laboratory in a prepaid envelope. The lab test has also been updated to offer optional testing for hepatitis B and HIV at no cost.
All tests are available to order online. They are completely free and delivered in discreet packaging. If a test result is reactive, the HSE will support individuals in accessing follow-up testing and free treatment. Treatment is safe, effective and usually involves a short course of tablets taken for 8 to 12 weeks.
Hepatitis C is a virus that affects the liver and can cause serious health problems if left untreated. It is spread through blood-to-blood contact. The HSE’s national hepatitis C treatment programme has already treated more than 7,000 people in Ireland, achieving a 95% cure rate. The programme is working towards eliminating hepatitis C as a public health concern in line with World Health Organization targets.
Order a free home test at hse.ie/hepc
With SAP HR and Payroll now fully rolled out across all HSE statutory sites, the NiSRP programme is moving ahead with Deployment Group 1. This includes Section 38 organisations, PCRS and St Luke’s Radiation Oncology Network.
Chief People Officer Anne Marie Hoey praised the achievement, saying, “Despite challenges such as COVID-19 and the cyber-attack, the programme maintained momentum with all stakeholders and successfully completed delivery across all statutory sites. This is an excellent case study in change management.”
Did you know?
There is a new Parental Leave Quotas tile on HR and Payroll Self Service. Once your quota is approved, use the My Leave Request tile to apply for parental leave.
The NiSRP helpdesk is available to support you. support.nisrp@hse.ie | phone: 0818 300 296
The Patient and Service User Experience Office, in collaboration with each local REO office, delivered a series of Regional Patient and Service User workshops that took place in the month of July. These workshops were independently facilitated, and we had a wide group of people attending. The aim was to gather ideas and look at the practical next steps for the HSE in the establishment of Regional Patient and Service User Partner Participation Councils and connected implementation plans. The workshops generated great ideas and provided an opportunity for each region to look at what partnership initiatives were working well in their local area and how we can build on these together to make partnership
embedded at every level of the HSE. The workshops also provided an opportunity to look at emerging themes for a Patient and Service User Partnership Strategy, which will be further discussed at the Patient Partnership Conference in September.
Anne O’Shea Clarke, Regional Manager South West and Mid West of Sage Advocacy, the national advocacy service for older people, vulnerable adults and healthcare patients, was invited by Sandra Broderick, Regional Executive Officer for HSE Mid West, to the Mid West Regional Patient Partnership Workshop in Limerick on 7 July.
“I attended as a representative from Sage Advocacy,” Ms O’Shea Clarke explains, “as well as a former patient
The National Cancer Control Programme (NCCP) has created two eLearning programmes on cancer on HSeLand: Cancer Risk Reduction, and Early Diagnosis of Cancer. These are available to all health and social care professionals. The Cancer Risk Reduction programme consists of
11 modules, each about 10 minutes long, covering the most common modifiable risk factors for cancer in Ireland. This programme is ICGP-accredited for 3 CPD points and 0.5 days GMS study leave.
The Early Diagnosis of Cancer programme consists of two modules, each about 30 minutes long, covering signs, symptoms
A new nurse-led initiative is enabling more women to access cervical screening at Limerick Prison. Edel Muldowney, the prison’s Nurse Manager, led efforts to address the challenges women in prison face regarding cervical screening.
The initiative saw the prison’s health unit work with the CervicalCheck training unit to establish a trauma-informed, on-site screening service for women in the prison. It set out
to increase the uptake of screening in the prison and ensure women there have timely access to onward care when necessary.
Under the initiative, there were informal “yard sessions” with peer educators about screening, as well as peer-to-peer engagement that was supported by the Red Cross. CervicalCheck provided formal accreditation to participating nurses, and Rape Crisis Centre counsellors offered trauma support.
and service user representative with the National Patient Forum. I joined Sage Advocacy in 2018 following many years as a full-time carer to my late husband, who had Huntington’s disease. It was my lived experience trying to navigate a complex healthcare system and learning the importance of communicating with healthcare professionals with two-way respect and understanding that inspired me to change careers from finance into advocacy.”
She added, “I have been inspired by the changes taking place over recent years within the HSE. I believe there is a real commitment to partnership and I am excited for what is to come with the new Regional Patient and Service User Participation Councils.”
and referral pathways for common cancers in Ireland. The programmes aim to increase healthcare professionals’ knowledge and understanding of risk reduction behaviours and improve early diagnosis of cancer. They can be accessed by logging on to hseland.ie, selecting “clinical skills” and clicking on NCCP.
It is part of the National Screening Service’s work to improve equity in screening and support all eligible people to access screening.
Since the initiative began, 33 women have received cervical screening – a 200% increase on the previous screening uptake. Eight were referred to colposcopy. HPV prevalence in the prison population is double that in the general population, and 88% of HPV-positive women required referral.
Victoria; Maria McEnery, HSE National Cancer Control Programme (NCCP); Dr Helen McAvoy, Institute of Public Health (IPH); Minister of State Jennifer Murnane O’Connor; Dr Ciara Reynolds, IPH; Jane Murray, patient advocate; and Dr Breeda Neville, HSE NCCP.

The HSE’s National Cancer Control Programme (NCCP) and the Institute of Public Health (IPH) held an event for health and social care professionals to discuss sunbed use in Ireland, and the lessons learnt from Australia’s sunbed ban. This event aimed to inform future policy options to reduce skin cancer risk in Ireland.
Speaking at the event, Professor Craig Sinclair, Head of Prevention at Cancer Council Victoria and Director of the World Health Organization Collaborative Centre for UV Radiation, said, “There is a precedent for the successful banning of sunbeds. Australia introduced an outright ban on commercial sunbeds in 2016. The measure has enjoyed strong public support and has undoubtedly prevented thousands of skin cancers and delivered an estimated saving of over AU$64 million to the Australian health system.”
A new report published by the IPH in July 2025 has recommended a ban on sunbeds to reduce the risk of skin cancer in Ireland, which has one of the highest skin cancer rates in the world. The report was developed to support the Department of Health and HSE’s NCCP National Skin Cancer Prevention Plan (2023–2026) and the 2025 Programme for Government commitment to explore a ban on commercial sunbed use.
Clinical Audit Awareness Week 2025, 3-6 June, was a powerful celebration of quality improvement, learning and shared impact across healthcare services. Themed “Clinical Audit, Humans and AI: Smarter Together”, the week brought together clinicians, auditors and healthcare leaders to reflect on innovation in practice and highlighted how clinical audit continues to drive safe, effective and person-centred care.
Nursing and Midwifery Quality Care-Metrics (QC-M) are endorsed by the Office of the Nursing and Midwifery Services Director. Supported by University Hospital Birmingham, the Test Your Care tool captured and monitored QC-M data until March 2025. From 2023 to April 2025, a crossfunctional project team collaborated to deliver a more modern platform capable of enhanced reporting.
MEG-QCM went live across acute, community and integrated care settings on 2 April, supporting 6,000 users across 180 healthcare services to capture their QC-M data. MEG-QCM has been configured to support quality care metrics and indicators across seven care groups – acute care, older persons, mental health, intellectual disability, midwifery, public health nursing and children’s services.
The deployment of the MEG-QCM platform ensures a robust ICT infrastructure, which is critical to long-term quality care. It also enables the quality and safety improvement objectives of the HSE Patient Safety Strategy (2019–2024). Using data to improve patient safety is central to this strategy, and using MEG-QCM as a data source across all clinical services reinforces this commitment.

Minister for Health Jennifer Carroll MacNeill TD with Dr Laura Piggott and Ciara Gormley, Customer Success Manager at myPatientSpace.
On 11 June, nearly 600 healthcare professionals, leaders and innovators gathered at the Dublin Royal Convention Centre for Ireland’s HSE Spark Summit 2025 healthcare innovation conference. The event provided a platform to showcase the ingenuity and dedication of frontline staff transforming health and social care through innovative, practical, patient-centred solutions.
Frontline clinicians shared their experiences from delivering innovative human-centred projects in their area. The summit also featured presentations and panel discussions with key leaders, including Bernard Gloster, HSE CEO; Robert Watt, Secretary General, Department of Health; Jennifer Carroll MacNeill, Minister for Health; Dr Colm Henry, HSE Chief Clinical Officer; and Damien McCallion, HSE Chief Technology and Transformation Officer. These highlighted the importance of staff-led innovation, system-wide collaboration and fostering a culture of continuous improvement. Strategic Designer Paul Taylor shared insights from the UK’s public service and healthcare transformation landscape and Kate Lydon, Director, Big Motive (UK) delivered a keynote on “Field Research and the Front Lines: Designing with Empathy”, emphasising human-centred design in healthcare systems.
The annual Bright Spark Awards honoured frontline teams for their creativity and measurable impact. Twelve projects were recognised for their contribution to improved patient care diagnostics, reduced wait times, and demonstrating scalable models for national adoption.
The Spark Innovation Programme invites new ideas, offering funding, mentorship and support for staff-driven projects. Many showcased innovations are being embedded into everyday practice or explored for national rollout, demonstrating the real and lasting impact of frontline creativity.
For full details of the Bright Spark awardees, visit hse.ie/spark
For information on how to get involved, email spark@hse.ie
Every year, around 7,500 people in Ireland experience a stroke. It’s the third leading cause of death and the single greatest cause of adult neurological disability. About 30,000 people in Ireland live with disabilities as a result of a stroke.
The Irish National Audit of Stroke (INAS) found that in 2014, 73% of stroke patients reached hospital within the vital 4.5-hour window. By 2021, this figure had fallen to just 58%, reducing opportunities for timely, effective treatment.
There is strong evidence of the effectiveness of stroke campaigns, since the first Irish FAST (Face, Arm, Speech, Time) campaign was run by the Irish Heart Foundation in 2010. This September, the HSE will launch a new campaign with a primary objective of increasing the understanding of the importance of acting quickly, as well as reinforcing the knowledge of key symptoms. Look out for the campaign on TV, radio and online, and the key message: The second you suspect a stroke is the second you dial 999.
The National Screening Service has published a guide to screening for carers and the people they support. The guide helps everyone understand what screening programmes are available and who is eligible to take part in them. It also helps carers understand and explain our screening programmes; and supports those being cared for to make their own decisions about taking part in screening. Supporting informed decisionmaking is one of the most important responsibilities for carers, and the guide also highlights this. “A guide to screening for carers and the people they support” is available to download at screeningservice.ie

In February, a Memorandum of Understanding (MoU) was signed between the HSE and the Ministry of Health in Tanzania, marking a strong commitment to continued collaboration. The MoU was signed by Dr Philip Crowley (HSE), Dr Seif A. Shekalaghe (Permanent Secretary, MoH), and Minister Jenista Mhagama, with support from Irish Ambassador Nicola Brennan and Dr David Weakliam, Executive Director of the Global Health Programme. This partnership began in 2022, following an invitation from the Embassy of Ireland to support improvements in primary healthcare (PHC) in Tanzania. Since then, there has been major progress in strategic planning, policy development, leadership strengthening, and building capacity in quality improvement (QI).
A key milestone since the signing of the MoU was the delivery of a purposefully co-designed QI train-the-trainer programme in June. So far, 22 participants have completed the training and are now

prepared to facilitate practice-based QI training and coach QI teams from 15 PHC services. These teams will take part in a four-month pilot programme starting later this year.
The MoU provides a five-year framework to deepen cooperation and expand into new areas such as acute care. Priority areas include:
• Health workforce development – building skills across health professions in both countries
• Quality of health services
This year’s Steps to Health challenge saw 153 teams take part across the Dublin and Midlands region. A total of 1,057 HSE staff took to the streets, highways and byways to reach their goal of 10,000 steps a day, boosting their health and wellbeing.
Teams with names such as “Hungry Gobblers”, “Stepabetes”, “Miles of Smiles”, and “999 Walkers” were led by team co-ordinators, with step totals for each week displayed on the leader board. Participants were reminded each week of the “five ways to wellbeing” – connect, be active, take notice, keep learning and give. The teams within Dublin and Midlands also engaged in a number of local competitions throughout the five weeks, which added a sense of team spirit.
Two key webinars were delivered to engage and support staff. The welcome webinar introduced the refreshed Steps to Health programme and outlined the new regional approach. The celebration webinar marked the end of the challenge, featuring guest speaker Jenny Branigan, Territory Manager for parkrun Ireland, who spoke about the power of volunteering, community spirit and keeping active beyond the Steps to Health challenge. Well done to all who took part.
– including expert exchanges, improved nursing and midwifery care, health system management, and clinical quality monitoring
• Medical research – joint research and capacity building
• Rehabilitation services –strengthening delivery and systems
This agreement reinforces both countries’ commitment to shared learning, stronger systems, and better health outcomes.





The national conference, Shaping the Future (STF) of Intellectual Disability Nursing in Ireland was held on 28 May. It celebrated and highlighted the work of registered nurses in intellectual disability (RNID) in supporting people with an intellectual disability to live ordinary lives in ordinary places.
The conference was hosted by the Office of the Nursing and Midwifery Services Director. Speakers included representation from the Chief Nursing Office, National Clinical Programme for People with Disability, the Irish Prison Service, universities, frontline RNIDs and a student RNID.
The report, “Evidence to inform the development of nursing indicators for intellectual disability, where there is no diagnosis, and nursing knowledge demonstrates grounds for a formal nursing assessment to enable appropriate service access” was also launched.
Mei Lin Yap, Ambassador Liaison Officer at the Trinity Centre for Ageing and Intellectual Disability received a standing ovation for her thought-provoking keynote address. Mei Lin called all those in attendance to be leaders for people with an intellectual disability. The conference offered RNIDs and those working within and on behalf of disability services across Ireland an opportunity to hear about the diverse roles and innovations RNIDs are engaged in.
The HSE Drugs and Alcohol Helpline provides free, confidential support, information, guidance and referral to anyone with questions or concerns related to drug or alcohol use. The recently published 2024 helpline report noted that 96% of people who contacted the helpline were seeking advice or information on treatment and support options. Almost 1 in 3 contacts referenced a mental health issue alongside their substance use issue. The primary substance being discussed in 2024 was alcohol, followed by cocaine and then cannabis. For health service staff, it is of note that:
• Navigating services can be challenging
• Combined cocaine and alcohol use carries extra risks
• 70% of drug debts were due to cocaine use
• Anxiety and depression are often issues for people with drug or alcohol problems
We welcome calls or emails from health service staff to discuss options for people they encounter in their work. Similarly, any member of the public is welcome to contact us to talk through their situation and explore the options.
The HSE Drugs and Alcohol Helpline is open Monday to Friday, 9.30am to 5.30pm; freephone 1800 459 459 or email helpline@hse.ie
Minister for Health Jennifer Carroll MacNeill joined BreastCheck staff, advocacy groups and patient advocate Dympna Cremin at the BreastCheck Eccles Unit in Dublin on 28 May to mark the 25th anniversary of BreastCheck, our national breast screening programme. Since 2000, BreastCheck has performed over 2.6 million mammograms and detected over 18,000 cancers.
The Minister thanked BreastCheck staff for their dedication, highlighting that their contributions are crucial to the programme’s success. She also expressed gratitude to all the women taking part in BreastCheck, noting that their involvement is essential for making this life-saving initiative possible. She encouraged everyone to keep attending their appointments.
Dympna Cremin spoke about her breast cancer journey and the importance of early detection. Dympna was diagnosed with breast cancer after a routine BreastCheck appointment in 2021. She described the kindness and professionalism of the staff who provided her care, from diagnosis to treatment, highlighted the emotional journey and practical supports that helped her through, and expressed gratitude to the BreastCheck programme. Dympna’s story is a powerful reminder of the human impact of screening programmes and the lives they save.

Physical activity guidelines extended to include pregnant/postpartum women and those living with chronic conditions Being physically active is safe and beneficial for pregnant and postpartum women, and those living well with a chronic condition. On 27 June, the HSE and Department of Health launched specific guidance for pregnant and postpartum women and those living with a chronic condition, following an update to the National Physical Activity and Sedentary Behaviour Guidelines for Ireland – “Every Move Counts”. New recommendations for each group include:
Pregnant women:
• Undertake regular physical activity throughout their pregnancy
• Should aim to undertake at least 2 hours and 30 minutes of moderate-intensity aerobic activity distributed throughout the week
• Should incorporate a variety of aerobic and musclestrengthening activities throughout the week
• Should incorporate pelvic floor muscle exercises daily
Postpartum women:
• Can gradually resume physical activity after
childbirth to return to levels similar to those recommended for the general population of at least 2 hours and 30 minutes of moderate-intensity aerobic activity per week
• Should include musclestrengthening exercises that focus on the major muscle groups throughout the week
• Should begin pelvic floor muscle exercises in the early postpartum period
People living with a chronic condition:
• Should aim to undertake between 2 hours and 30 minutes and 5 hours of moderate intensity aerobic physical activity per week; or between 1 hour and 15 minutes and 2 hours and 30 minutes of vigorous intensity aerobic physical activity per week; or a combination of both
• Should undertake muscle strengthening activities at moderate or greater intensity that involve all major muscle groups on 2 or more days per week
• Should undertake multicomponent balance and strength activities on 3 or more days of the week to enhance functional capacity and prevent falls

In response to the COVID-19 pandemic, the National Cancer Control Programme (NCCP) secured 26 acute haematology oncology service (AHOS) nursing posts in cancer units nationwide. The aim was to ensure that cancer patients undergoing treatment who become ill at home could contact a dedicated nurse specialist phone line to discuss their symptoms, rather than having to make a decision whether or not to attend their nearest emergency department.
Five years on, the AHOS nursing service has become an established practice across the country. Triage activity has risen from 1,137 in 2020 to 21,873 calls in 2024. Of those requiring review, 60% were treated and discharged the same day.
For Mary Holden, a terminally ill cancer patient attending St Vincent’s University Hospital in Dublin for ongoing treatment, the service is a godsend: “To know that if I have an unusual symptom, I can pick up the phone and get that symptom checked out, without leaving my home… The AHOS nurse specialist at the end of the phone line uses a traffic light system to assess whether or not treatment is needed. Green light symptoms mean you may be given advice over the phone; amber light symptoms mean your symptoms may need monitoring; and red light symptoms mean you may be advised to come into hospital.”
Unfortunately, the service is currently restricted to business hours, Monday to Friday.
Maria Gillespie, Assistant Director of Nursing of the AHOS in the NCCP is keen to see the service extended: “We are determined to keep pushing ahead, with the ask to build resilience in the service and expand to a 24-hour service across the country because cancer patients on treatment need it and its success proves it is essential.”
Smoking is one of the most common preventable causes of poor pregnancy outcomes. It’s associated with maternal, foetal and neonatal morbidity and mortality. Latest figures show 10–17% of women smoke during pregnancy in Ireland. Maternity services at Midlands Regional Hospital Portlaoise (MRHP) launched a quality improvement (QI) initiative in February aimed at reducing the effects of smoking on the unborn infant. With the support of the midwifery management team and consultant obstetrician, project lead Siobhán Flynn, CMM2 Parentcraft received initial “train the trainer” training from Orla Bowe, CMM2 in smoking cessation in the National Maternity Hospital. The midwives in the antenatal clinics have received relevant training in Making Every Contact Count (MECC), as well as carbon monoxide smokerlyser training. Carbon monoxide (CO) is a colourless, odourless gas present in cigarette smoke and the environment from car fumes, second-hand smoke and solid fuel burners. Exposure to high levels in pregnancy can reduce the amount of oxygen reaching the baby in the womb, potentially affecting its growth and development. Smoking during pregnancy increases the risk of miscarriage, deep vein thrombosis, stillbirth,
neonatal death, sudden infant death syndrome, pre-term birth, low birth weight and cardiac defects in the baby. The National Stop Smoking Guideline (2022) recommends offering CO monitoring to all pregnant women. In response, the maternity services at MRHP introduced routine CO testing for all women attending antenatal appointments.
Key components of the service include:
• Routine CO monitoring at first visit to identify smoking status
• Providing brief smoking cessation interventions through MECC staff training
• Implementing an ‘opt-out’ referral pathway to a dedicated smoking cessation behavioural support service; this applies to women who currently smoke or vape, those who’ve recently quit, and any women with a CO reading of 4 ppm or higher
If a pregnant woman or her support person smokes or vapes, she will be offered a referral to the health promotion officer in her area who will help them to quit. This new service will be offered to all women in line with national recommendations.
In 2018, the World Health Organization (WHO) launched the SAFER initiative, a strategic package of five cost-effective policy actions aimed at reducing alcohol-related harm. Ireland is now bringing this global framework to life at the local level through the Building SAFER Communities project. A national initiative with local impact, led by Alcohol Forum Ireland with research partners Trinity College Dublin, the project is funded by the Drugs Policy Unit in the Department of Health, with a €100,000 investment over three years.
This groundbreaking initiative will support 12 Irish communities to tackle alcohol harm and reduce its impact on children, young people and the wider community, decreasing related health, social and economic consequences. Local steering groups, supported by seven Drug and Alcohol Task Forces, will guide the work in each location, with ongoing input from communities and service partners.
Between 2024 and 2027, the project will be rolled out in Letterkenny, Sligo, Monaghan, Drogheda, Kerry, Cork, Leixlip, Celbridge, Ballymun, Balbriggan, Swords and the Canals Communities.
The SAFER Approach is delivered through the five WHO-endorsed SAFER interventions being implemented, which includes:
S – strengthening restrictions on alcohol availability
A – advancing and enforcing drink-driving countermeasures
F – facilitating access to brief interventions and treatment
E – enforcing bans on alcohol advertising, sponsorship and promotion
R – raising prices through excise taxes and minimum pricing
These evidence-based actions are being adapted into multicomponent, community-focused
solutions for real-world impact. Bringing communities together, the national project launch took place in 2024. Local launches are now taking place across 2025, featuring national and local speakers and partners including An Garda Síochána, the HSE, Tusla, community and voluntary groups, Drug and Alcohol Task Forces, local TDs, councillors and residents. Work is supported nationally through the HSE Alcohol Programme and locally in many areas by Health Promotion and Improvement teams. These events mark a collaborative effort to build healthier, more resilient communities across Ireland.
Safeguarding public health, the initiative also highlights the importance of shielding public health policy from alcohol industry interference and ensuring robust monitoring and evaluation to track progress.
For more information on the project, visit safercommunities.ie













If you work in healthcare, you are at increased risk of being exposed to flu and COVID-19

� Vaccines are safe and effective and provide the best protection from flu and COVID-19.
� All healthcare workers are recommended a flu vaccine.


� Some healthcare workers are recommended a COVID-19 vaccine. Any healthcare worker who wants a COVID-19 vaccine can get one.
� Vaccines may be available at work and are also available free of charge from GPs and Pharmacies.



