TeachingPatientwithVoice the
ACG MAGAZINE MEMBERS. MEDICINE. MEANING. Spring 2023
Call for Abstracts Submission













Dates: March 6 – June 5, 2023











ABSTRACT CATEGORIES
• Biliary/Pancreas
• Colon












• Colorectal
• Endoscopy Video Forum

























• Esophagus
• Functional Bowel Disease
• General Endoscopy
• GI Bleeding
• IBD




• Interventional Endoscopy
• Liver
• Obesity
• Pediatrics

• Practice Management
• Small Intestine
• Stomach
• Clinical Vignettes/ Case Reports
VANCOUVER
Submit Your Abstracts: bit.ly/ACG2023-Abstracts
SubmitAbstract! your

| 1 COVER STORY Teaching With the Patient Voice Patients lend their voice to inform GI fellow training and patient engagement PAGE 18 FEATURED CONTENTS SPRING 2023 // VOLUME 7, NUMBER 1 GETTING IT RIGHT How FDA drug and biologic therapy labels are developed PAGE 15 ACG PERSPECTIVES Dr. Seth Gross discusses GI technological innovations that enhance the field PAGE 36 COVER STORY
ACG POSTGRADUATE COURSE Attend an upcoming
2023
ACG’s Hepatology School & ACG Eastern Regional Postgraduate Course
Renaissance Hotel | Washington, DC
June 2–4, 2023
ACG’s Functional GI and Motility Disorders School & ACG Midwest Regional Postgraduate Course

Radisson Blu Mall of America | Minneapolis, MN
August 25–27, 2023
ACG’s Endoscopy School & ACG/VGS/ODSGNA Regional Postgraduate Course
Williamsburg Lodge | Williamsburg, VA

September 8–10, 2023
ACG’s IBD School & Southern Regional Postgraduate Course
Renaissance Nashville Hotel | Nashville, TN

December 1–3, 2023
2024
ACG Weekly Virtual Grand Rounds
REGISTER NOW: GI.ORG/ACGVGR
ACG VGRs are o ered TWICE each Thursday, with a live broadcast at noon (ET) followed by an 8:00pm (ET) rebroadcast!
ACG Endoscopy School & ACG Board of Governors/ASGE Best Practices Course
Aria Resort | Las Vegas, NV

January 26–28, 2024
MORE INFO: gi.org/acg-course-calendar
"Most trainees, though perhaps less knowledgeable about my illness, have seemed a bit more intent on putting the puzzle together, coming up with new approaches, more open to my suggestions, and willing to learn.”
—
6 // MESSAGE FROM THE PRESIDENT
Dr. Daniel Pambianco on recent efforts to enhance ACG member resources and advocate for physicians and patients
7 // NOVEL & NOTEWORTHY
In Memoriams for Past President Dr. Myron Lewis & Dr. William Y. Chey, recent ACG Institute program developments, podcasts to reach patients & more
15 //
GETTING IT RIGHT
FDA DRUG AND BIOLOGIC THERAPY LABELS
Guidance on FDA clearance and requirements for OTC and Rx medications
with the Patient Voice: Integrating Patient Advocates into GI Fellowship Training” PG 18
18 // COVER STORY
TEACHING WITH THE PATIENT VOICE
Direct insights from patients to inform GI fellow training & patient engagement
31 // ACG PERSPECTIVES
31 CULINARY CONNECTIONS
Fresh perspectives from ACG food enthusiasts
36 INNOVATOR INTERVIEW

Dr. Seth Gross & Dr. Bara El Kurdi on the path to innovation in GI
38 ACG TRAINING GRANT
Dr. Evaristus Sunday Chukwudike shares his experience training at Brown Universaty/ Rhode Island Hospital
39 // INSIDE THE JOURNALS
40 AJG
Two new ACG Guidelines: Celiac Disease by Rubio-Tapia, et al. & GI Subepithelial Lesions by Jacobsen, et al.
40 CTG
Efficacy of a Digital, Personalized Elimination
Diet for the Self-Management of IBS and CoMorbid IBS & IBD by Jactel, et al
40 ACGCRJ
How to Be a a Great Peer Reviewer - Article & Podcast by CRJ Co-EICs Dr. Nicholas McDonald & Dr. Tomoki Sempokuya, MD
42 // REACHING
THE CECUM
ABOUT CELIAC DISEASE
A patient handout about celiac disease from ACG's Patient Care Committee
| 3
SPRING 2023 // VOLUME 7, NUMBER 1
CONTENTS
ABOVE & FEATURED CONTENTS:
Underwater photography at Mikomoto Island, Japan, courtesy of Amy N. Stratton, DO, FACG
Melissa Adams VanHouten, "Teaching
ACG MAGAZINE

CONNECT WITH ACG MAGAZINE STAFF
youtube.com/ACGastroenterology
Executive Director
Bradley C. Stillman, JD
Editor in Chief; Vice President, Communications
Anne-Louise B. Oliphant
Manager, Communications & Member Publications
Becky Abel
Art Director Emily Garel
Senior Graphic Designer
Antonella Iseas
BOARD OF TRUSTEES
President: Daniel J. Pambianco, MD, FACG
President-Elect: Jonathan A. Leighton, MD, FACG
Vice President: Amy S. Oxentenko, MD, FACG
Secretary: Costas H. Kefalas, MD, MMM, FACG
Treasurer: William D. Chey, MD, FACG
Immediate Past President: Samir A. Shah, MD, FACG

Past President: David A. Greenwald, MD, FACG
Director, ACG Institute: Neena S. Abraham, MD, MSc, MACG
Co-Editors, The American Journal of Gastroenterology:
Jasmohan S. Bajaj, MD, MS, FACG
Millie D. Long, MD, MPH, FACG
Chair, Board of Governors: Dayna S. Early, MD, FACG
Vice Chair, Board of Governors: Sita S. Chokhavatia, MD, MACG
Trustee for Administrative Affairs: Irving M. Pike, MD, FACG
TRUSTEES
Jean-Paul Achkar, MD, FACG
Seth A. Gross, MD, FACG
David J. Hass, MD, FACG
Immanuel K. H. Ho, MD, FACG
James C. Hobley, MD, MSc, FACG
Nicholas J. Shaheen, MD, MPH, MACG
Aasma Shaukat, MD, MPH, FACG
Neil H. Stollman, MD, FACG
Renee L. Williams, MD, MHPE, FACG
Patrick E. Young, MD, FACG
facebook.com/AmCollegeGastro
twitter.com/amcollegegastro
instagram.com/amcollegegastro
bit.ly/ACG-Linked-In
CONTACT
IDEAS & FEEDBACK
We'd love to hear from you. Send us your ideas, stories and comments.
ACGMag@gi.org
CONTACT ACG
American College of Gastroenterology 6400 Goldsboro Rd., Suite 200 Bethesda, MD 20817 (301) 263-9000 | gi.org
DIGITAL EDITIONS
GI.ORG/ACGMAGAZINE
American College of Gastroenterology is an international organization with more than 18,000 clinician members representing some 86 countries. The College's vision is to be the pre-eminent professional organization that champions the evolving needs of clinicians in the delivery of high-quality, evidence-based and compassionate health care to gastroenterology patients. The mission of the College is to advance world-class care for patients with gastrointestinal disorders through excellence, innovation and advocacy in the areas of scientific investigation, education, prevention and treatment.
4 | GI.ORG/ACGMAGAZINE
ACG
Leading the Way in Advancing Health Equity ACG MAGAZINE in Advancing Health Equity
MAGAZINE
Sameer K. Berry, MD

Dr. Berry is a gastroenterologist at New York Gastroenterology Associates and Chief Medical Officer of Oshi Health.

CONTRIBUTING WRITERS
Bara El Kurdi, MD
Dr. El Kurdi is a third-year GI fellow at UT Health San Antonio Long School of Medicine and is a member of the ACG Innovation and Technology Committee.
Baha Moshiree, MD, MSc, FACG
Dr. Moshiree is Clinical Professor of Medicine at Wake Forest Medical University and Director of Motility in the Division of Gastroenterology at Atrium Health in Charlotte, NC. She is a member of several ACG committees and previously served as ACG Governor for North Carolina.
James B. Canavan, MD, PhD
Dr. Canavan is a gastroenterologist and a pharmaceutical physician who is a Clinical Trial Lead/IBD Program Lead at Bristol-Myers Squibb. He is a member of ACG’s FDA-Related Matters Committee.

Lawrence Goldkind, MD
Dr. Goldkind is a gastroenterologist at Walter Reed National Military Medical Center in Bethesda, MD, and Assistant Professor of Medicine at the Uniformed Services University of Health Sciences School of Medicine. He is a member of ACG’s FDA-Related Matters Committee.


Amanda K. Cartee, MD
Dr. Cartee is Assistant Professor of Medicine and Associate Scientist in the Center for Clinical and Translational Science at the University of Alabama at Birmingham. She is a member of ACG’s FDA-Related Matters Committee and previously participated in ACG’s FDA Visiting Fellowship Program.
Seth A. Gross, MD, FACG
Dr. Gross is Professor of Medicine at NYU Grossman School of Medicine and Clinical Chief in the Division of Gastroenterology and Hepatology at NYU Langone. He is a Trustee of the College and a member of the ACG Innovation and Technology Committee.

Aasma Shaukat, MD, MPH, FACG


Dr. Shaukat is Director GI Outcomes Research, Robert M. and Mary H. Glickman Professor of Medicine, and Professor of Population Health at NYU Grossman School of Medicine. She is a Trustee of the College and a member of the ACG Innovation and Technology Committee.
Amy N. Stratton, DO, FACG

Dr. Stratton is a gastroenterologist currently on locum tenens service, primarily in Colorado. She previously served on the ACG Women in GI Committee.



Evaristus Sunday Chukwudike, MD
Dr. Chukwudike is a GI fellow at the University of Calabar Teaching Hospital in Nigeria. He is a 2021 recipient of an ACG International Training Grant, gaining clinical experience at Brown University/Rhode Island Hospital.
Emily A. Haller, MS, RDN Emily Haller is Lead GI Dietitian in the Division of Gastroenterology and Hepatology at University of Michigan Health, Michigan Medicine.
Katie A. Dunleavy, MB BCh BAO
Dr. Dunleavy is a second-year GI fellow at Mayo Clinic Rochester and is a member of ACG’s Digital Communications and Publications Committee. She serves as the Editor of ACG MAGAZINE’s Trainee Hub section.
Vivek Kaul, MD, FACG
Dr. Kaul is the Segal-Watson Professor of Medicine and Chief of the Division of Gastroenterology and Hepatology at the University of Rochester Medical Center. He is Chair of the ACG Innovation and Technology Committee and a member of the ACG Educational Affairs Committee.

| 5
INDEFATIGABLE ADVOCACY
By Daniel J. Pambianco, MD, FACG
DEAR COLLEAGUES:
As Spring is upon us, with tulips, kite flying, March Madness, and colorectal cancer awareness, it represents the season of renewal, transformation, and high quality. As your professional home, the ACG embodies these attributes. I begin this missive with our Vision and Mission statements:
“The Vision of the ACG is to be the preeminent professional that champions the prevention, diagnosis, and treatment of digestive disorders, serving as a beacon to guide the delivery of the highest quality, compassionate and evidence-based care. Our Mission is the enhance the ability of our members to provide world class care to patients with digestive disorders and advance the profession through excellence and innovation based upon the pillars of: Patient Care, Education, Scientific Investigation, Advocacy, and Practice Management.”
Through our 24 committees, Board of Governors, ACG Institute, Board of Trustees, executive leadership, administrative staff, and membership, we strive to attain these goals daily.
Regarding the ABIM and MOC, progress is being made, albeit gradually. With the Longitudinal Knowledge Assessment (LKA) for Gastroenterology being online, this year will provide essential and substantial member feedback. We continue to encourage ABIM to expedite practical assessment of our areas of expertise.
The GIOnDEMAND platform pioneered by ACG, whose goal is to bring tertiary multidisciplinary care access to our practices, is growing and bringing our patients genetic testing and virtual counseling if positive for hereditary colon cancer. This should be an integral part of our patient risk assessment, especially with the highest rate of rise of colon cancer in our 20- to 49-year-old patients.
Our Advanced Practice Providers Committee has successfully completed our ACG Universe online teaching module for new APPs in GI, as well as those seeking specialization in IBD and hepatology, with over 50 hours of CME. This is a unique and
vital educational modality to augment onboarding new graduate APPs into our busy practices with a curated curriculum taught by APPs.
The ACG Institute Center for Leadership, Ethics and Equity Vision Council, created under the auspices of Dr. Neena Abraham to vanguard innovative collaborations, had an inaugural meeting with the pharmaceutical industry to discuss advancing clinical research to include a more representative and diverse population to adequately study pharmacologic efficacy in GI and hepatic disorders. This was met enthusiastically and will be instrumental in advancing clinical trial development, recruitment, and conducting more effective drug treatments.
The ACG Board of Governors is unique to the College in that the Governors represent state and local practicing gastroenterologist experiences in a dynamic environment of insurance and political issues with a bilateral conduit of information. Under the leadership of Dr. Dayna Early and Dr. Sita Chokhavatia, our ongoing monitoring system and rapid multi-committee response has never been more astute. One example is a Prior Authorization Task Force, chaired by Dr. Early, collaborating with the ACG Practice Management Committee to develop a suite of template letters for several GI and liver therapies. These letters are a tool to reduce increasing administrative burdens associated with the growing influx of prior authorization requirements. As part of the ACG Practice Management Toolbox and a member benefit, the letters are updated regularly.
The Practice Management Committee under the leadership of Chair Dr. Stephen Amann and Vice Chair, Dr. Sapna Thomas has developed and updated educational materials for the Practice Management section of the ACG website and Education
Universe as resources to enable members to be more effective and efficient in their practices. Most notable is the ACG Practice Management Toolbox, a series of articles by committee members covering issues relevant to private practices and physician-led clinical practices to help optimize their practices. The PMC, in collaboration with the Membership Committee, is developing an Orientation Manual for reference and training of non-medical and endoscopy unit support staff, including basic knowledge of endoscopic procedures, unit flow, and factors affecting procedure timing and scheduling to help office support staff to address basic patient queries and preparation for their endoscopy experience to aid in the unit operating efficiently.
Lastly, the ACG Legislative and Public Policy Council and National Affairs Network, under the leadership of Dr. Louis Wilson and in conjunction with the Board of Governors, has indefatigably advocated for ACG members and patients. Their successes in 2022 included:
• Extending telehealth flexibilities and passing various state laws curbing the use of prior authorization and step therapy
• Eliminating Medicare and patient cost-sharing in CRC screening

• Developing guidance on how to incorporate policy changes in everyday clinical practice
• Working with Congress to prevent unwarranted Medicare reimbursement cuts
Our legislative efforts will continue with the ACG Governors Fly-in and Advocacy Day that will take place in April 2023 in Washington, D.C., to meet with legislators.
In conclusion, Spring will usher in a renewed, continued transformation of the ACG with committee crosspollination and continued creative and innovative educational and information dissemination to you, our colleagues, “advancing gastroenterology, improving patient care.”
6 | GI.ORG/ACGMAGAZINE MESSAGE FROM THE PRESIDENT
—DJP
Note wor thy Note wor thy
WE CELEBRATE THE LIFE of ACG Past President Dr. Myron Lewis with a memorial tribute. In the N&N spotlight are participants in two ACG Institute Programs, the new Clinical Research Leadership Program and the longstanding Edgar Achkar Visiting Professorship.
The ACG Patient Care
Committee has produced a new series of podcasts in partnership with GastroGirl™ and we feature a great conversation with Patient Care Chair Dr. Scott Gabbard on dyspepsia.
Navigating the challenges of prior authorization just got a bit simpler thanks to ACG’s Prior Authorization Task Force, in collaboration with the Practice Management Committee, which introduced a suite of template letters to use with insurers for coverage decisions on a number of GI and liver therapies.
Send your news or story ideas to ACGmag@gi.org
NOVEL & NOTEWORTHY | 7
HARMONY
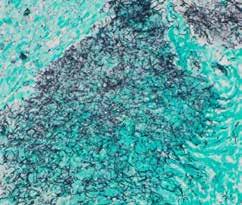
About the Location
This photo was taken at Mikomoto Island. The small island is a 15-minute boat trip southeast of the Izu peninsula in Japan.
What equipment did you use?
The photo was shot using a Sony A1 mirrorless camera with a FE 2860mm F4-5.6 lens. The camera and lens were in a Nauticam underwater housing with a wet wide angle lens/ dome. For lighting, I used two Inon Z330 underwater strobes.
What captured your attention?
The swaying sea anemone tentacles surrounded by an array of colors initially caught my eye. I was then drawn to the domino damselfish protecting the corkscrew tentacle anemone, illustrating their symbiotic relationship.

Any technical challenges?
The biggest challenge to underwater photography is lighting. You start to lose ambient light around 15-20 feet with progressive color loss as you descend further underwater. To add color into the photos, you need to add light, which is accomplished using underwater strobes. You then have to adjust the strength of strobe flash in combination with distance from the subject, which can be difficult, while trying not to overexpose water particulates. Lastly, you have to maintain camera stability to ensure the picture is in focus while moving with the ocean surge.
Share your thoughts on the personal significance of this photo, or photography in general, and why you pursue photography as a hobby and personal passion
I first got into diving thirteen years ago as an activity to do with my husband. I remember being in awe the first time I breathed underwater while looking at the coral reefs and marine life. I started underwater photography as a way to share the beauty of God’s underwater creation with others. I now pursue both underwater and wildlife
photography in search of capturing the whimsical beauty and interactions between wildlife and their environment. I can get lost for hours photographing fauna throughout the world while transcending life’s stressors.
8 | GI.ORG/ACGMAGAZINE N&N GI EYE: ARTWORK FROM ACG MEMBERS
Amy N. Stratton, DO, FACG
Dr. Stratton is a gastroenterologist currently on locum tenens service, primarily in Colorado. She previously served on the ACG Women in GI Committee.
Amy N. Stratton, DO, FACG


NOVEL & NOTEWORTHY | 9
[CONGRATS]
SOPHIE M. BALZORA, MD, FACG was appointed Clinical Professor of Medicine at NYU Grossman School of Medicine. Dr. Balzora is the Chair of ACG’s Committee on Diversity, Equity and Inclusion and co-founder of ACG's #DiversityinGI Social Media Campaign. She serves on the ACG Institute’s Leadership, Ethics and Equity Center (LE&E) Advisory Board.

[CONGRATS]
BRENNAN M. R. SPIEGEL, MD, MSHS, FACG, Director of Health Services Research for Cedars-Sinai and Director of the Cedars-Sinai Master’s Degree Program in Health Delivery Science was named Assistant Dean for Clinical & Translational Sciences at the David Geffen School of Medicine at UCLA. Dr. Spiegel is the ACG Governor for Southern California (Region A) and formerly co-Editor-in-Chief of The American Journal of Gastroenterology.
[CONGRATS]
RENEE L. WILLIAMS, MD, FACG was appointed Professor of Medicine at NYU Grossman School of Medicine. Dr. Williams is a Trustee of the College. She was a member of the College’s Committee on Diversity, Equity & Inclusion from 2011 to 2018 and served as chair from 2016 to 2018.

[TEMPLATES]
A PRIOR AUTHORIZATION
TASK FORCE chaired by Dayna S. Early, MD, FACG collaborated with the ACG Practice Management Committee to develop a suite of template letters for a number of GI and liver therapies. These letters are a tool to reduce the increasing administrative burdens associated with the growing influx of insurer prior authorization requirements. As part of the ACG Practice Management Toolbox, the letters will be updated regularly. The letters are a member benefit. Learn More: gi.org/practice-management/ prior-authorization-template-letters
[ACG AT WCOG]
WGO MASTER
ACG Past President Christina M. Surawicz, MD, MACG, MWGO was among the 2022 Masters of the World Gastroenterology Organisation (WGO) recognized at an awards ceremony that took place during the World Congress of Gastroenterology 2022 (WCOG), in Dubai, United Arab Emirates, in December 2022.

[PATIENT PODCASTS]
WCOG 2022 YOUNG CLINICIAN'S PROGRAM
Several ACG leaders presented at the WCOG in Dubai. Dr. Surawicz on “Effective Leadership,” Aasma Shaukat, MD, MPH, FACG on “How to Build Your Brand,” and Jonathan A. Leighton, MD, FACG on “Negotiation and Interview Skills.”
GASTROGIRL™ AND THE ACG PATIENT CARE COMMITTEE have formed a partnership to produce a series of podcasts for patients and the public on a range of GI and liver topics. Among the latest topics is a conversation with Patient Care Chair Scott L. Gabbard, MD, FACG and GastroGirl’s Jacqueline Gaulin, “Why is My Stomach Always Upset? What Patients Should Know about Functional Dyspepsia.” You can find the series on the ACG website or via GastroGirl’s YouTube channel.
LISTEN: bit.ly/Podcasts-PCC-and-GG
WATCH: bit.ly/GastroGirl-PCC-YouTube
CROHN'S AND COLITIS FOR DUMMIES, SECOND EDITION
 by Tauseef Ali, MD, FACG (Author), David T. Rubin MD, FACG (Foreword)
by Tauseef Ali, MD, FACG (Author), David T. Rubin MD, FACG (Foreword)

Reviewed by Katherine A. Falloon, MD, Cleveland Clinic Foundation



In Crohn’s and Colitis for Dummies, Dr. Tauseef Ali provides a definitive source of patient-centered information on living with inflammatory bowel disease in a format that is both digestible and eminently readable. Split into six parts and further subdivided into eighteen chapters, this book can be read from start to finish or can be consulted as a reliable source when questions regarding specific topics arise (Dr. Ali carefully and concisely defines medical jargon each time it comes up in the text, so any chapter can be read as if it were an isolated article.)
Highlights for me included the overview of how to prepare for a first visit with a gastroenterologist and the chapter discussing alternative and complementary therapies, which provided a data-driven, objective overview of everything from herbal remedies to cognitive behavioral therapy. The must-read section, however,
is the myths about inflammatory bowel disease which explained a lot of the most common misconceptions I encounter with patients in clinic.
This book is targeted to patients and caregivers, but it is also a valuable resource for providers early in their career looking for patient-centered language to be used to educate patients on their disease and how to manage it (keep an eye out for an excellent analogy comparing lymphocytes to hands that can only pick bad apples). Highly recommend.

10 | GI.ORG/ACGMAGAZINE
// N&N
ACG EDGAR ACHKAR VISITING PROFESSORSHIPS
The year ahead promises an inspiring cohort of Edgar Achkar Visiting Professors (EAVP) through the ACG Institute for Clinical Research & Education. EAVP visits bolster the curriculum and inspire fellows-in-training by providing lectures, small group discussions, panel discussions, and one-on-one visits with trainees and faculty. Several visits this year are designated as “ACG Visiting Scholar in Equity, Diversity, and Ethical Care” and feature special lecture topics that aim to create awareness around the issues and challenges related to delivering equitable care, respecting diversity, and instilling ethical decision making.
Bring EAVP to Your GI Program in 2024 The window for applications for 2024 visits will be July 17 to August 18, 2023 for visits starting January 2024. Learn More: gi.org/eavp
2023 EAVP Visiting Professorships
Amy S. Oxentenko, MD, FACG (Mayo Clinic)



To University of Connecticut
March 1
*Sunanda V. Kane, MD, MSPH, FACG (Mayo Clinic)


To University of Nebraska Medical Center
March 2-3
*Christopher D. Vélez, MD (Massachusetts General Hospital)


To Thomas Jefferson University
April 13
*Lauren D. Nephew, MD (Indiana University)
To University of Florida
May 16
David T. Rubin, MD, FACG (University of Chicago)

To University of Massachusetts T.H. Chan School of Medicine
May 18
Francis A. Farraye, MD, MSc, MACG (Mayo Clinic)

To University of Missouri - Kansas City
May 19
*Adjoa N. Anyane-Yeboa, MD, MPH (Massachusetts General Hospital)



To Cooper University Hospital
September 9
*Sonali Paul, MD, MS (University of Chicago)






To NYU Grossman School of Medicine
October 10
*Visits requested an ACG Visiting Scholar in Equity, Diversity, and Ethical Care
[RISING STARS]
ACG’S NEW CLINICAL RESEARCH LEADERSHIP PROGRAM
Introducing the inaugural cohort of the ACG Clinical Research Leadership Program. These emerging leaders will receive training to support skills in clinical research management through The Center for Leadership, Ethics & Equity of ACG Institute for Clinical Research & Education.
Receiving a grant award is a celebratory milestone, inherent with several new responsibilities for the awardee – as a scientific leader, financial administrator, manager, and mentor. This unique interactive program provides funded ACG clinician investigators with the skill set to start, grow and maintain success as research leaders. Participants will learn research leadership skills to maintain a successful independent research program. The cohort is comprised of early to mid-career clinical investigators who are ACG member physicians (between 2-15 years out of fellowship training), are working in the U.S., and who have active or recent funding as a Principal Investigator or Co-Principal Investigator.
Course Directors: Neena S. Abraham, MD, MSc(Epid), MACG, Aasma Shaukat, MD, MPH, FACG, and Rena H. Yadlapati, MD, MSHS, FACG
Patricia Pringle Bloom, MD
Leila Neshatian, MD, MSc
Joy Weiling Chang, MD, MS

Vu Quang Nguyen, MD
Po-Hung (Victor) Chen, MD, FACG

Guru Trikudanathan, MD
Jennifer L. Horsley-Silva, MD

Ravy K. Vajravelu, MD, MSCE


Afrin Nahar Kamal, MD, MS
Christopher Vélez, MD
NOVEL & NOTEWORTHY | 11
[EAVP]
2023 CRLP Participants
Elham Afghani, MD, MPH
Sarah Rosanna Lieber, MD, MSCR
[IN MEMORIAM]
MYRON LEWIS, MD, MACG (1937-2022)
A distinguished past president and champion of the College, Myron Lewis, MD, MACG of Memphis, TN, passed away on April 9, 2022 surrounded by his wife of 58 years, Gail, and his three daughters.
Born in Memphis, TN in 1937 at Baptist Memorial Hospital, Dr. Lewis was a 1959 graduate of Dartmouth College where he received his bachelor's degree Magna Cum Laude and Phi Beta Kappa. Following graduation, he earned his M.D. degree at Columbia University's College of Physicians and Surgeons in New York City in the class of 1963. He did his internship and first year residency at Vanderbilt University Medical Center and completed his residency and gastroenterology training at the Cornell Bellevue Division of Memorial Sloan Kettering. Prior to returning to Memphis, he spent two years in the U.S. Public Health Service stationed in Louisville, Kentucky.
He joined the staff at Baptist Memorial Hospital in 1970 and remained there until he retired. He served as Chief of Staff at Baptist Memorial Hospital in 1985. He was an Associate Professor of Medicine at the University of Tennessee and was Co-Director of the Gastrointestinal Laboratory at Baptist Memorial Hospital.
Dr. Lewis became a Trustee of the College in 1982. His family recalls that he was most proud of his time as President of the American College of Gastroenterology from 1987 to 1988 where he developed close friendships with gastroenterologists from all over the country. His presidential term will be remembered as a critical point in the history of the College when the ACG Board of Trustees engaged Thomas F. Fise, Esq. to serve as ACG’s Executive Director through his firm, Association & Government Relations Management, a role Tom filled until 2005.
Based on Dr. Lewis’ distinguished service to ACG, he became a Master of the American College of Gastroenterology in October of 1992. Dr. Lewis continued to stay active in ACG as a member of the Archives Committee from 2003 to 2009 and the Patient Care Committee from 2006 to 2012.
ACG Past President Chesley Hines, Jr. MD, MACG, who served as ACG President immediately after Dr. Lewis, shared this reflection: “Myron Lewis was the ‘consummate Southern gentleman’ – as those of us who were raised in the Deep South are fond of saying – soft spoken, very polite, and considerate of everyone. Never said anything bad about anyone. Well organized thoughts and decisions. Considerate of other people’s ideas, and supportive of those ideas, if he agreed with them. It was my privilege to work closely with him, before and during his presidency of the American College of Gastroenterology. The ACG is fortunate to have been under his leadership.”
In addition to his professional accomplishments, Dr. Lewis volunteered as a physician at Church Health, which he continued to do even after his retirement. He was also a member of the Germantown Rotary and a former board member of Opera Memphis. He was a devoted husband and father, always putting his family first. He leaves behind his wife Gail, and three daughters, Robin Wallace and her husband Jeff, Tracey Lewis, and Joelle Rogin. He is also survived by his four grandchildren.
[IN MEMORIAM]
WILLIAM Y. CHEY, MD, FACG
ACG was saddened to learn of the death of William Y. Chey, MD, FACG on January 11, 2023. Dr. Chey is the father of ACG Treasurer William D. Chey, MD, FACG.

After completing medical school at Seoul National University in South Korea and serving as a medical officer in the Korean War, Dr. Chey immigrated to the United States where he completed training in internal medicine and pathology at the City Hospital of NY and Mount Sinai in New York City. He went on to earn a Doctor of Sciences in Medicine from the University of Pennsylvania followed by a fellowship in gastroenterology at Temple University School of Medicine. From 1963 to 1971, he served as a faculty member at Temple where he rose to the rank of Associate Professor of Medicine and Head of GI Research. In 1971, he was recruited to become a Professor of Medicine at the University of Rochester and founding Director of the Isaac Gordon Center of Digestive Diseases and Nutrition at Genesee Hospital.
His groundbreaking patient care and research led to appointment as Director of the Division of Gastroenterology & Hepatology at the University of Rochester in 1992. In this role, he founded and served as Director of the William & Sheila Konar Center for Digestive & Liver Diseases at Strong Memorial Hospital until he retired in 2000. His tenure established Strong Memorial Hospital as the premier GI & Hepatology referral center in upstate NY. In addition to providing life changing patient care and reporting numerous research discoveries, Dr. Chey’s programs trained generations of gastroenterologists from the U.S. and abroad who carry on his legacy to this day. He received numerous professional awards and was invited to lecture about his work all over the world.
He is remembered by his family for an uncanny memory and unique wit which enabled him to share incredibly detailed accounts of his travels and experiences with anyone willing to invest a few minutes. Though his uncompromising standards and strong opinions could be difficult for the uninitiated, his sense of justice, humanity, empathy, generosity and wisdom ultimately won over all those that earned the pleasure of his attention. He was married to his beloved wife Fan K. Tang from 1959 until her passing February 22, 2022.
ACG MAGAZINE published a feature on the remarkable life of Dr. Chey and his biography, “American Dreams, Still Alive: Memoir of an Immigrant Dreamer” in 2021. You can read this remarkable article written by his son Dr. Bill Chey at bit.ly/wm-y-chey-book
12 | GI.ORG/ACGMAGAZINE
// N&N
Dr. William Y. Chey and his sons and grandsons
Where dysbiosis once left the gut microbiome in ruin,
RISE ABOVE RECURRENT C. DIFFICILE INFECTION and

restore hope with REBYOTATM

The first and only FDA-approved microbiota-based live biotherapeutic to prevent recurrence of C. difficile infection starting at first recurrence.1,2,a



aIn the pivotal phase 3 trial, 32.8% of patients were treated at first recurrence of CDI following antibiotic treatment of CDI.1
INDICATION
REBYOTA (fecal microbiota, live - jslm) is indicated for the prevention of recurrence of Clostridioides difficile infection (CDI) in individuals 18 years of age and older, following antibiotic treatment for recurrent CDI.
Limitation of Use
REBYOTA is not indicated for treatment of CDI.
IMPORTANT SAFETY INFORMATION
Contraindications
Do not administer REBYOTA to individuals with a history of a severe allergic reaction (eg, anaphylaxis) to any of the known product components.
Warnings and Precautions
Transmissible infectious agents
Because REBYOTA is manufactured from human fecal matter, it may carry a risk of transmitting infectious agents. Any infection suspected by a physician possibly to have been transmitted by this product should be reported by the physician or other healthcare provider to Ferring Pharmaceuticals Inc.
Management of acute allergic reactions
Appropriate medical treatment must be immediately available in the event an acute anaphylactic reaction occurs following administration of REBYOTA.
Potential presence of food allergens
REBYOTA is manufactured from human fecal material and may contain food allergens. The potential for REBYOTA to cause adverse reactions due to food allergens is unknown.
Adverse Reactions
The most commonly reported (≥3%) adverse reactions occurring in adults following a single dose of REBYOTA were abdominal pain (8.9%), diarrhea (7.2%), abdominal distention (3.9%), flatulence (3.3%), and nausea (3.3%).
Use in Specific Populations
Pediatric Use
Safety and efficacy of REBYOTA in patients below 18 years of age have not been established.
Geriatric Use
Of the 978 adults who received REBYOTA, 48.8% were 65 years of age and over (n=477), and 25.7% were 75 years of age and over (n=251). Data from clinical studies of REBYOTA are not sufficient to determine if adults 65 years of age and older respond differently than younger adults.
You are encouraged to report negative side effects of prescription drugs to FDA. Visit www.FDA.gov/medwatch, or call 1-800-332-1088.
Please see Brief Summary on next page and full Prescribing Information at www.REBYOTAHCP.com.
References
1. REBYOTA. Prescribing Information. Parsippany, NJ: Ferring Pharmaceuticals; 2022. 2. US Food and Drug Administration. FDA Approves First Fecal Microbiota Product. https:// www.fda.gov/news-events/pressannouncements/fda-approves-firstfecal-microbiota-product. Accessed December 1, 2022.
NOVEL & NOTEWORTHY | 13
RESTORE HOPE
Scan to visit website
Ferring and the Ferring Pharmaceuticals logo are registered trademarks of Ferring B.V. REBYOTA is a trademark of Ferring B.V. ©2022 Ferring B.V. All rights reserved. US-REB-2200129 1/23
REBYOTATM (fecal microbiota, live - jslm) suspension, for rectal use
Brief Summary Please consult package insert for full Prescribing Information
INDICATIONS
REBYOTA is indicated for the prevention of recurrence of Clostridioides dif cile infection (CDI) in individuals 18 years of age and older following antibiotic treatment for recurrent CDI. Limitation of Use: REBYOTA is not indicated for treatment of CDI.
CONTRAINDICATIONS
Do not administer REBYOTA to individuals with a history of a severe allergic reaction (e.g. anaphylaxis) to any of the known product components.
Each 150mL dose of REBYOTA contains between 1x108 and 5x1010 colony forming units (CFU) per mL of fecal microbes including >1x105 CFU/mL of Bacteroides, and contains not greater than 5.97 grams of PEG3350 in saline.
WARNINGS AND PRECAUTIONS
Transmissible infectious agents: Because REBYOTA is manufactured from human fecal matter it may carry a risk of transmitting infectious agents. Any infection suspected by a physician possibly to have been transmitted by this product should be reported by the physician or other healthcare provider to Ferring Pharmaceuticals Inc.
Management of acute allergic reactions: Appropriate medical treatment must be immediately available in the event an acute anaphylactic reaction occurs following administration of REBYOTA.
Potential presence of food allergens: REBYOTA is manufactured from human fecal matter and may contain food allergens. The potential for REBYOTA to cause adverse reactions due to food allergens is unknown.
ADVERSE REACTIONS
The most commonly reported (≥ 3%) adverse reactions occurring in adults following a single dose of REBYOTA were abdominal pain, (8.9%), diarrhea (7.2%), abdominal distention (3.9%), atulence (3.3%), and nausea (3.3%).
Clinical Trials Experience: The safety of REBYOTA was evaluated in 2 randomized, double-blind clinical studies (Study 1 and Study 2) and 3 open-label clinical studies conducted in the United States and Canada. A total of 978 adults 18 years of age and older with a history of 1 or more recurrences of Clostridioides dif cile (CDI) infection and whose symptoms were controlled 24 – 72 hours post-antibiotic treatment were enrolled and received 1 or more doses of REBYOTA; 595 of whom received a single dose of REBYOTA.
Adverse Reactions: Across the 5 clinical studies, participants recorded solicited adverse events in a diary for the rst 7 days after each dose of REBYOTA or placebo. Participants were monitored for all other adverse events by queries during scheduled visits, with duration of follow-up ranging from 6 to 24 months after the last dose. In an analysis of solicited and unsolicited adverse events reported in Study 1, the most common adverse reactions (de ned as adverse events assessed as de nitely, possibly, or
probably related to Investigational Product by the investigator) reported by ≥3% of REBYOTA recipients, and at a rate greater than that reported by placebo recipients, were abdominal pain, (8.9%), diarrhea (7.2%), abdominal distention (3.9%), atulence (3.3%), and nausea (3.3%).Most adverse reactions occurred during the rst 2 weeks after treatment. After this, the proportion of patients with adverse reactions declined in subsequent 2-week intervals. Beyond 2 weeks after treatment only a few single adverse reactions were reported. Most adverse drug reactions were mild to moderate in severity. No life-threatening adverse reaction was reported.
Serious Adverse Reactions - In a pooled analysis of the 5 clinical studies, 10.1% (60/595) of REBYOTA recipients (1 dose only) and 7.2% (6/83) of placebo recipients reported a serious adverse event within 6 months post last dose of investigational product. None of these events were considered related to the investigational product.
USE IN SPECIFIC POPULATIONS
Pregnancy: REBYOTA is not absorbed systemically following rectal administration, and maternal use is not expected to result in fetal exposure to the drug.
Lactation: REBYOTA is not absorbed systemically by the mother following rectal administration, and breastfeeding is not expected to result in exposure of the child to REBYOTA.
Pediatric Use: Safety and effectiveness of REBYOTA in individuals younger than 18 years of age have not been established.
Geriatric Use: Of the 978 adults who received REBYOTA, 48.8% were 65 years of age and over (n=477), and 25.7% were 75 years of age and over (n=251). Data from clinical studies of REBYOTA are not suf cient to determine if adults 65 years of age and older respond differently than younger adults
For more information, visit www.REBYOTAHCP.com
You are encouraged to report negative side effects of prescription drugs to FDA. Visit www.FDA.gov/medwatch, or call 1-800-332-1088.
Manufactured for Ferring Pharmaceuticals by Rebiotix, Inc. Roseville, MN 55113
US License No. 2112
9009000002
Rx Only
Ferring and the Ferring Pharmaceuticals logo are registered trademarks of Ferring B.V. REBYOTA is a trademark of Ferring B.V. ©2022 Ferring B.V. This brief summary is based on full Rebyota Prescribing Information which can be found at www.RebyotaHCP.com
US-REB-2200277
GETTING IT
The U.S. Food and Drug Administration (FDA)-approved label, also referred to as the “package insert” or “prescribing information,” provides a comprehensive overview of the efficacy and safety of a medication at the time of approval and provides guidance on its clinical use. Consequently, the FDA-approved label can be considered a “one-stop shop” for information on the efficacy and safety of drug and biologic therapies at the time of approval. Following first approval, additional studies may generate new data on safety and other clinical indications, and the label may be updated accordingly. Such studies may be initiated by the sponsoring pharmaceutical company or may be required by the FDA as a postmarketing commitment. Thus, the label is an asset that informs safe prescribing practices for clinicians. This article will discuss how the label is generated and
By Amanda K. Cartee, MD; Lawrence Goldkind, MD; and James B. Canavan, MD, PhD. Authors are members of the ACG FDA Related Matters Committee
GETTING IT RIGHT | 15
Practice Management Toolbox
How FDA Drug and Biologic Therapy Labels are Developed and How to Optimize Their Use in Clinical Practice
how it can be used by physicians in clinical practice as an efficient source of information meant to enhance patient well-being.
FDA regulations state that the label “must contain a summary of the essential scientific information needed for the safe and effective use of the drug” (21 CFR 201.56). The label must be “informative and accurate” and cannot be promotional in tone. In contrast, publications, promotional material and speakers’ programs educate clinicians about new therapies. These venues generally do not include the broad range of
information provided in an approved label. At the time a drug development program is complete and submitted to the FDA for review, the New Drug Application (NDA) or Biologic Licensing Application (BLA) must contain a proposed label that follows a standard format as described below. The proposed label will be based on the comprehensive characterization of the efficacy, safety, and pharmaceutical properties of a drug or biologic during the clinical development process by the sponsoring pharmaceutical company. The FDA may spend many months reviewing clinical trial
data and primary source documents during the NDA/BLA review period. If the FDA considers the evidence of efficacy and safety adequate to warrant marketing approval, the FDA reviews the proposed label and, after communicating necessary changes to the sponsor, formally approves the label, along with marketing authorization for the drug or biologic. Comprehensive FDA review during the NDA/BLA process provides confidence that the label accurately reflects the profile of a drug or biologic at the time of approval.
The label follows a template, outlined in FDA regulations (21 CFR 201.57), that facilitates an easy review of key prescribing information by clinicians:
1. Highlights of Prescribing Information: This section is generally less than a page long and includes: Boxed Warning, Recent Major Changes, Indications and Usage, Dosage and Administration, Contraindications, Warnings and Precautions, Adverse Reactions, Drug Interactions and Use in Specific Populations
2. Full Prescribing Information: The full prescribing information contains more details about the “short form” highlights section as well as information on use in pregnancy and lactation, females and males of reproductive potential, pediatric use, geriatric use, overdosage, clinical pharmacology, mechanism of action, pharmacodynamics, pharmacokinetics, nonclinical toxicology, carcinogenesis, mutagenesis, impairment of fertility, animal toxicology and/or pharmacology and a clinical studies section. The clinical studies section presents the efficacy data that represents the basis for FDA approval.
The standard format of the first page of a label includes key information in an easy-to-read format and is shown in Figure
1. Subsequent pages in a drug label provide more details. Key clinical components of a drug label include:
• Efficacy Information: Publications of seminal Phase 3 studies contain more details than the label about clinical study design and secondary endpoint information. However, the clinical studies section of the label provides a concise presentation of key outcome measures used in the pivotal studies. Since the FDA has access to the initial protocols, amendments, and study result datasets, the FDA independently analyzes generated data. This provides confidence that the description of efficacy data in the label is accurate and non-promotional in nature.
• New Indication: Post-marketing studies done are added to the label only if they represent a new FDA-approved use, referred to as a new indication. Staying up to date on medical literature is important to keep pace with new
accruing information that may optimize use of approved drugs or biologics. For example, the infliximab label does not contain new data on its alternate dosing regimens and use of therapeutic and antibody level monitoring. Likewise, results of studies comparing drug efficacy for the same indication are unlikely be found in a label unless considered an adequate, well-controlled study by the FDA. Thus, the label provides key prescribing information but is not an exclusive or exhaustive source of information.
• Safety Information: Safety information in the label is primarily derived from Phase 3 pivotal clinical trials and subsequent long-term extension studies since these data represent the longest-term exposures at clinically relevant, approved doses. Most frequent adverse events that differ from rates in the placebo or active comparator arm, as well as serious adverse events, are displayed in the label based on these controlled studies. The results of additional studies that are pertinent to the safe use of a drug or biologic, such as cardiac safety studies (e.g., QT studies), reproductive toxicology studies, and drug-drug interaction studies are also summarized in the label. The FDA may mandate additional post-marketing safety studies as a condition of approval based on characteristics of the drug or biologic, the drug class, or mechanism of action. After approval, post-marketing adverse event reports submitted to the FDA through the MedWatch form 3500 are collected into the FDA adverse event reporting system (FAERS). Individual reports very rarely provide enough evidence to suggest causality. If review of all similar reports provides a reasonable basis to believe that the drug may be causally related, the adverse event is added to the label. It is important for clinicians to submit such reports when they consider a significant drugrelated adverse event to have occurred in their patient. This is particularly important if that event is not already clearly represented in the label.
16 | GI.ORG/ACGMAGAZINE
// GETTING IT RIGHT
Additional data of value to clinicians include:
1. Pharmacokinetics: How the body absorbs, distributes, metabolizes, and excretes the therapy in question. There are times when such knowledge is clinically relevant. Such data may predict when the onset of action may be expected and how comorbid conditions such as renal or liver disease may affect the safety or proper dose of the therapy.
2. Pharmacodynamics: The physiological and biochemical effects of the therapy on the body


3. Drug-Drug Interactions: How the therapy interacts with the effects, particularly the pharmacokinetics of other therapies
4. Special Populations: Information on geriatric age groups, pediatric populations and pregnancy

In summary, the FDA-approved label provides a concise “one-stop shop” for the broad range of information necessary for the safe and effective use of new therapies at approval. The label represents the summary of many months of review of primary source documents by FDA staff and the distillation of important information in a standardized format. New relevant safety information that becomes available with real world use over time in broader populations than those included in clinical trials is added to the label over time. This can include
rare serious adverse reactions, drugdrug interactions, risks in specific vulnerable populations, or events that require longer-term exposure than clinical trials provide. Health care providers and their patients have much to gain through familiarity with the label and have a key role in keeping the label of a drug up to date through the reporting of significant adverse events through the easily accessed MedWatch reporting system.
Lawrence Goldkind, MD is a gastroenterologist at Walter Reed National Military Medical Center in Bethesda, MD and Assistant Professor of Medicine at the Uniformed Services University of Health Sciences School of Medicine. He previously served at the U.S. Food and Drug Administration for five years, including as Acting Director of the Division of Anti-inflammatory, Analgesic, and Ophthalmic Drug Products in the Center for Drug Evaluation and Research.

GETTING IT RIGHT | 17
Amanda K. Cartee, MD is a gastroenterologist and Assistant Professor of Medicine at the University of Alabama at Birmingham where she is also an Associate Scientist in their Center for Clinical and Translational Science.
Figure 1. Standard Format of First Page of Drug Label. Source: U.S. FDA
James B. Canavan, MD, PhD is a gastroenterologist and a pharmaceutical physician who is a Clinical Trial Lead / IBD Program Lead at Bristol-Myers Squibb.
18 | GI.ORG/ACGMAGAZINE // COVER STORY
TeachingPatientwithVoice the
Editor: Katie Dunleavy, MB BCh BAO
Contributors: Tina Aswani-Omprakash, Jessica Caron, Erica Dermer, Ryan Piansky, Jeffrey Roberts, Allison Rosen, Alison Rothbaum, Brad Swiftney, Melissa Adams VanHouten
COVER STORY | 19
Integrating Patient Advocates into GI Fellowship Training
Getting to Know Our Patient Advocates
Tina Aswani Omprakash
Ms. Omprakash is the President & Chair of the Board of South Asian IBD Alliance (SAIA), a global patient-clinician led nonprofit organization for all patients and providers of South Asian descent. She is a Crohn's patient and award-winning health advocate. As a patient with Crohn's disease with a permanent ileostomy due to perianal, fistulizing disease, Tina has maintained her own advocacy platform called Own Your Crohn's (ownyourcrohns.com). Tina’s overarching aim is to normalize the rhetoric around chronic illnesses and disabilities to help diverse groups of patients own their ailments to live fuller, happier lives. She spearheads public health causes, including those proposing research for and creating awareness for IBD, life-saving ostomy surgery, fistulizing disease and initiatives supporting health equity for women and racial & ethnic minorities. Tina is pursuing her Master’s degree in Public Health at Mount Sinai’s Icahn School of Medicine and will be graduating in June. Tina has spoken at many premier GI conferences worldwide and has co-authored 10 research papers in prominent journals (JAMA, Gastroenterology, Clinical Gastroenterology & Hepatology, Crohn’s & Colitis 360), a guidebook on IBD care for the National Alliance for Caregiving and a series of websites on Crohn’s-related ostomy surgery for United Ostomy Associations of America. As a result of her tireless efforts, ACG recognized her in 2022 with the Best Patient Advocacy Award. The Crohn’s & Colitis Foundation recognized Tina in 2021 for her phenomenal leadership and powerful impact on the IBD community with the Above & Beyond Volunteer Award. Tina’s blog was also recognized as a 2020 Best Blog by Healthline, and she was awarded the 2019 Healio Gastroenterology Disruptive Innovator Award for moving the needle on GI care for patients.
Social Media:
Blog: Own Your Crohn's ownyourcrohns.com
Website: South Asian IBD Alliance southasianibd.org
Support Group: IBDesis Facebook Community facebook.com/groups/ibdesis
Facebook, Instagram, Twitter & TikTok: @ownyourcrohns, @southasianibd, @ibdesis
Jessica Caron
Jessica is a healthcare and human services professional currently working as the Senior Director for Engagement Strategy with Snow Companies. Additionally, Jessica is a patient advocate in the IBD community, sharing her experience as a patient living with Crohn’s disease and advocating for a co-facilitated approach to advancing medical care. She blogs and supports patients across the globe through her social media presence and website, Chronically-Jess.com. Jessica has connected with other patients and healthcare professionals through her work with IBDQorus, the IBD Parenthood Project, partnerships with the Crohn’s and Colitis Foundation, and through regular speaking engagements at national events like DDW, AIBD, and The IBD Summit for Fellows. She has a Psychology degree from the University of Maine, a Master of Education in Human Relations from Plymouth State University, and recently earned her master’s in Health Care Delivery Science (MHCDS) from Dartmouth College. Jessica currently lives and works in New Hampshire with her husband and two young sons.
Social Media:
Website: chronically-jess.com
Twitter: @ChronicallyJess @trellushealth
Erica Dermer
Instagram: @Chronicallyjess_
Ms. Dermer is a professional digestive disease patient advocate also known by her blog name, Celiac and the Beast. She’s known for her work covering the trade show floor, searching for the best gluten-free products, finding the newest celiac disease research at national scientific shows and in her role as a patient advocate for digestive health conferences. She’s the former Managing Editor and writer for the largest gluten-free magazine in the U.S. She’s been featured as an on-air personality on Good Day Columbus, Good Day Austin, and online and print ad campaigns for retailers like Sprouts and Schar Gluten Free. She’s been featured in print on The Guardian, Fox News, AdWeek, USA Today and Grocery Headquarters. She was named Spokane’s Top 100 Women in Food Allergies, Best Allergy Blogger nominee from ShiftCon, and Best Allergy Friendly Blog from Healthline. Erica has a B.S. in Marketing and minor in Communications from the Arizona State University W.P. Carey School of Business.
Social Media:
Website: celiacandthebeast.com
Twitter: @CeliacBeast
Ryan Piansky
Instagram: @CeliacandtheBeast
Facebook: facebook.com/ celiacandthebeast
He is a 22-year-old college student at the Georgia Institute of Technology. He has eosinophilic esophagitis, as well as eosinophilic asthma, and follows a restricted diet. Despite health issues, he leads an active life including travel and patient advocacy efforts.

Social Media:
Website: apfed.org
Instagram & Twitter: @APFEDorg
Podcast: Real Talk: Eosinophilic Diseases



20 | GI.ORG/ACGMAGAZINE
// COVER STORY
Jeffrey Roberts
Jeffrey has been an IBS sufferer for 25+ years. He is the Founder and creator of the IBS Patient Support Group (ibspatient. org), creator of World IBS Day held every April 19th (worldibsday.org) and co-creator of TuesdayNightIBS.com. He has testified to the FDA several times on behalf of IBS patients. In 2019, Jeffrey was awarded the inaugural Patient Influencer Travel Award by Digestive Disease Week (DDW). He was also a nominee in 2020, 2021 and 2022 for the Healio Gastroenterology Disruptive Innovators Award. In 2021, Jeffrey was added to the list of Digital Opinion Leaders in Irritable Bowel Syndrome. Jeffrey regularly attends the annual DDW and ACG scientific meetings. He has a Master of Science in Education (MSEd) degree from Medaille College, Buffalo, New York. Jeffrey’s thesis was entitled "Awareness of Childhood Health Issues on Educational Outcome." He also holds a Bachelor of Science (BSc) degree from the University of Toronto and co-authored and published a book entitled IBS Chat: Real Life Stories and Solutions. He lives in Toronto.
Social Media:
Website: ibspatient.org
Twitter & Instagram: @ibspatient
Facebook: facebook.com/groups/ ibspatient
Alison Rothbaum
Allison Rosen
Ms. Rosen has deliberately and consciously chosen to dedicate her life – in and outside of her employment – to use her voice and platform to educate, advocate, and continuously learn how best to represent the collective cancer community. She is a patient, community, policy, and research advocate. She has worked in the world of oncology for over 16 years in cancer research and cancer health disparities. On June 7th, 2012, at the age of 32 after years of struggling with Crohn’s disease, her life was totally disrupted when a colonoscopy revealed Stage 2C colorectal cancer. She has now been cancer free for 10 years and volunteers her time on committees for young adult and colorectal cancer patients, with groups working on effective patient experience, social media, and outreach initiatives. She is a public speaker, board member, and volunteer for local, regional and national organizations and non-profits. Allison has experience on both sides of the fence and works to bridge the gap between the healthcare system and the communities that it serves.
Social Media:
Twitter: @ARosen380
Instagram & Facebook: @alicat380
TikTok: @allisonrosen4
Ms. Rothbaum is a patient advocate with Crohn’s disease since 1994, and ostomy since 2003. She is the program manager/coordinator of multiple social media regularly scheduled events including #MondayNightIBD, #TumorBoardTuesday, #Scrubs&Heels, and #IBDHorizons. Through social media she works to bridge the communication gap between clinicians and patients, in the real world beyond a textbook. Her motto has always been, “advocating to help clarify the healthcare world with you.” Meaning, she helps to present the facts with minimal bias, so patients can make their own informed decision. She is also on the advisory board for IBDSocialCircle since 2015, a Janssen Biotech initiative.


Social Media:
Facebook: facebook. com/PatientAdvocacy
Twitter & Instagram: @Empoweringpts9
Collaborations: Twitter
@MondayNightIBD
@TumorBoardTues
@ScrubsNHeels; ibdhorizons.com
Brad Swiftney
My name is Brad, and I had many diagnoses throughout my GI history. I had my first acute pancreatitis attack in December of 2013 when my lipase was over 66,000. I continued to have several more acute attacks due to gallbladder and biliary dysfunction, and ultimately was diagnosed with chronic pancreatitis. I struggled with pain with food and had many feeding tubes due to weight loss and significant pain/nausea. I then had a total pancreatectomy and auto-islet cell transplantation at Cleveland Clinic in 2020. I had a revision in 2021 (Roux-en-Y) due to excessive bile reflux, and have struggled with pain/nausea since then, which is believed to be due to surgical scar tissue and nerve damage to the biliary system. Due to pain/nausea symptoms, I am no longer a medical social worker (practiced for 7+ years) and I am a stay-at-home father to my two wonderful daughters.


Social Media:
Twitter & Instagram: @bradswiftney
Melissa Adams VanHouten
Ms. VanHouten is a former university political science instructor and corporate trainer who holds a B.S. in Political Science from St. Joseph's College and an M.A. in Political Science from Indiana State University. After being diagnosed with gastroparesis in February of 2014, she founded Gastroparesis: Fighting for Change and became a passionate advocate for those in her community who feel voiceless and ignored. Currently, as the Association of Gastrointestinal Motility Disorders (AGMD) Public Policy and Outreach Director, International Foundation for Gastrointestinal Disorders (IFFGD) Patient Advisory Committee member, co-author of the book, Real Life Diaries: Living with Gastroparesis, and creator and administrator of several online patient support and advocacy groups, she spends her days advancing the cause of those who struggle with the sometimes devastating and life-altering effects of gastroparesis and other chronic illnesses. It is her fondest desire to empower others to advocate for awareness, better treatments, and, ultimately, cures.
Social Media:
Website: curegp.org
Facebook Public Community Page: facebook.com/ GastroparesisFighting4Change
Facebook Gastroparesis Support Group: facebook.com/groups/ GastroparesisSupportGroup
Facebook Advocacy Group: facebook.com/groups/GPMarch
Instagram: @gastroparesisfighting4change
Personal Twitter Account: @melissarvh

COVER STORY | 21
Introduction by Dr. Katie Dunleavy
In December 2022, I attended the IBD Fellows Summit led by course directors Dr. Corey Siegel (Dartmouth-Hitchcock Medical Center) and Dr. David Rubin (University of Chicago) in Orlando, FL. While 10 fellows had the opportunity to convene with leaders of inflammatory bowel disease (IBD) in person, they also hosted more than 100 GI fellows virtually. One of the most poignant moments of this weekend was the discussion led by Jessica Caron, a patient advocate with IBD. Although I had interacted with patient advocates on social media and at conferences, I hadn’t recognized the true value of patient advocates for training GI fellows. Hearing Jessica Caron speak about the impact of IBD on her life including family planning, medication choices, and shared decision making gave me valuable insight into her patient experience. As the saying goes, “what your doctor doesn’t know can hurt you” and learning about the patient experience outside the hospital is essential to becoming a good gastroenterologist.
As the concern for ‘medical gaslighting’ or the experience of having one’s concerns dismissed by a medical professional, has gained national media attention, there is fear that physician bias and improper communication skills can lead to misdiagnoses, treatment delays and unnecessary suffering. Patients –especially women, people of color, geriatric patients and LGBTQ+ people – have voiced valid concerns. There is a critical opportunity for GI fellows to reflect on their biases and communication skills, and learn how to effectively listen, empathize and participate in shared patient decision making. Leveraging this natural collaboration between GI fellows and patient advocates can help to keep the patient voice at the center of our learning.
How do you define your role as a patient advocate? Why did you take on this role and how does it impact your journey as a patient with a gastrointestinal disease?
Melissa Adams VanHouten: Patient advocacy is designed specifically to enhance the interests of patients in all aspects of their care and in any other area which affects their mental, physical, emotional, or spiritual wellbeing. When I was first diagnosed, I was given very little information about gastroparesis. This is a community that has been largely ignored, misunderstood and dismissed – by everyone. So, I made it my mission to share their stories of need and desperation and to gather resources to advocate for proper care.
Ryan Piansky: I’ve been involved with the American Partnership for Eosinophilic Disorders from a very young age. As I grew up, I fell into the role of patient advocate, a role I associate with continuing to grow that community and making sure I can share my experience and connect others to help improve care for all the patients we work with.
Allison Rosen: I was diagnosed with stage 2 colorectal cancer while working in a cancer research lab. Through my experience at surviving cancer, I have knowledge on both sides of the fence, and work to bridge the gap between the healthcare system and the communities that it serves. Becoming a vocal advocate essentially fell into my lap as I was given many opportunities through the hospital to share my story. It was therapeutic to share my story so openly.
Jeffrey Roberts: Patient advocates also assist in recruiting patients for research studies and provide patient testimony so that industry better understands the patient’s perspective.
Erica Dermer: When I was first diagnosed with celiac disease, I didn’t have a lot of resources that really spoke to me about my disease. I started Celiac and the Beast in 2012, when I was still learning about my disease. Over the years, I’ve worked as a medical writer for digestive disease. While I am trained professionally with a certificate from The Academy of Nutrition and Dietetics, I’ve worked really hard and have been really lucky to be involved in the scientific community and I have used my position as an advocate to fight misinformation in the community.

Brad Swiftney: In my previous career as a social worker, I was constantly a patient advocate. I learned to try and meet the patient/person where they were. I found that this connection through understanding what the patient/family had been through, what they may face on a day-to-day basis, was key to the patient’s care by bringing this perspective to their physician. Over the course of my Master of Social Work program, it helped me to have a perspective beyond my own possibility. As a patient with chronic gastrointestinal conditions, it has helped me to become more honest about my symptoms and the impact of my condition on my daily life. My degree, training and work experience have taught me to be more vulnerable with my physicians.
Tina Aswani Omprakash: There are so many definitions of a patient advocate these days and I want to emphasize the role of ‘selfless service.’ To me, patient advocacy means lending our passion to the patient and clinician community
22 | GI.ORG/ACGMAGAZINE
“There is a critical opportunity for GI fellows to reflect on their biases and communication skills, and learn how to effectively listen, empathize and participate in shared patient decision making. Leveraging this natural collaboration between GI fellows and patient advocates can help to keep the patient voice at the center of our learning.” —Dr. Dunleavy
// COVER STORY
at large and (a) helping patients and caregivers navigate care and understand the ins and outs of IBD, (b) guiding physicians and multidisciplinary staff to understand what our most crucial needs are in a culturally competent manner, and (c) for me personally, advancing research ideas for underserved communities to receive better access to therapies and inclusion in research so phenotypes of disease can be better understood to develop precision medicine are all key.
Q: Tell me about your interactions with trainees/GI fellows. What opportunities are there for improvement in these interactions?
Melissa Adams VanHouten: Most trainees, though perhaps less knowledgeable about my illness, have seemed a bit more intent on putting the puzzle together, coming up with new approaches, more open to my suggestions, and willing to learn. My one major concern is that some fellows are strictly focused on knowledge and procedure, rather than on the patient as a person. It is not enough to get the diagnosis right or choose a good medication; one must demonstrate compassion, empathy, and present a good bedside manner.
Melissa Adams VanHouten: This is not just a training session or learning opportunity; there is a frightened human before you who needs to know you care.

Ryan Piansky: I don’t have too many experiences with trainees in my personal life. My doctors always get excited to teach a trainee about some of my rarer medical issues.
Allison Rosen: One of my most favorite activities is to teach medical students and GI fellows. Every year, I am given the opportunity to tell my story to second year medical students and GI fellows at Baylor College of Medicine. I truly believe every program should allow a patient/survivor to come talk with their medical students and GI fellows to tell their story and share their experiences. I truly think
that hearing my real-life experiences helps GI fellows formulate patient-centered favorable habits well beyond their fellowship years.
Jeffrey Roberts: #GITwitter and #MedTwitter have been excellent vehicles for connecting with trainees and GI fellows. It has created a natural environment for everyone to learn from each other. Earlier introduction to communication techniques with IBS patients would be a beneficial way for trainees to better understand the quality of life issues surrounding a disease or condition.
Erica Dermer: Don’t mistake training with a disease for lived experience with it. Really listen to patients. For many of us, we have had horrible or even traumatic experiences with medical teams. Many people with vague GI symptoms feel like they have been a victim of medical gaslighting. They just don’t feel seen. They don’t feel heard.
Brad Swiftney: I would encourage GI fellows to continue to listen to their patients. Throughout my history with GI care, I’ve come across many physicians who have felt they knew the answer before coming in to meet
COVER STORY | 23
“I was diagnosed with stage 2 colorectal cancer while working in a cancer research lab. Through my experience at surviving cancer, I have experience on both sides of the fence, and work to bridge the gap between the healthcare system and the communities that it serves.”
—Allison Rosen
me as a patient, and with the added level of trainee, I’ve noticed extra detail of care when my history has been fully listened to, especially when seeking care at a new institution.
Jessica Caron: I was shocked to learn how little was being taught to medical students and trainees during their journey to becoming a doctor. I had presumed the psychosocial aspects of our disease was a part of the medical curriculum; I was wrong.
Tina Aswani Omprakash: I have taught medical students, residents and fellows several times. I will still never forget the first time I shared my story to teach a class of medical students at Hunter College in NY. It was a very emotional moment as the students asked about the ins and outs of my Crohn’s disease and also a variety of other diagnoses I had developed over the years and what it felt like to go from a stellar Wall Street career and lose it all to this disease. I told them, “Be humble. We didn’t choose this path. This was the hand that was dealt to us. Show empathy and ask how we are holding up. Encourage us and tell
us how proud you are of us for hanging in there every single day."
Q: What are the most difficult aspects of managing your disease? Do you think these aspects are well known by most physicians?
Melissa Adams VanHouten: There is nothing not difficult about managing my illness. The life I once knew is gone, and (short of a cure for gastroparesis) is never coming back. I get frustrated because people do not understand how my life is affected by this illness – the incredible loss and grief I experience, the isolation, the stress and worry, the desperation for effective treatments or cures, the financial ruin caused by the loss of work, high insurance costs, specialized care and ER visits, and the fear (perhaps realization) that this will never improve, that I will never be normal and carefree again.
Erica Dermer: We have embarrassing symptoms and sometimes we don’t know how to talk about it – so we’d love your help with that.

Ryan Piansky: Spontaneity is difficult with EoE. From a young age, I’ve made sure
to plan my meals, check ingredients, make sure I have my meds, and think through countless other things. There are so many costs to care that physicians don’t acknowledge - time, money, energy.
Allison Rosen: Once a patient is declared ‘cured’ with ‘no evidence of disease,' people assume the survivor’s life will go back to precisely how it was before. However, this is very far from the truth. For example, my treatment left me with a permanent ostomy. Thus, figuring out the best ostomy products for me, an optimum diet, and body image issues all accompany managing the appliance. My treatment also left me incapable of conception. The long-term physical and mental health issues related to cancer are not fully understood by providers. While I would not necessarily expect a GI provider to function as a mental health professional, I would expect him/her to be alert for mental distress and be willing and able to suggest appropriate resources.
Jeffrey Roberts: As we still do not know the cause of IBS, there remains an unmet need for effective treatments which do more than simply manage the symptoms. The integrative model for treatment which touches on medication, diet and therapy offers a more complete option for managing the illness. Still, many patients lack access to healthcare professionals who can offer these types of treatments. Digital therapeutics are now available, which offer better access to the integrative model of care.
Erica Dermer: Every minute of my day is thinking about what I’m going to eat and if it’s safe. I can’t travel for work, I can’t take vacation, I can’t go grocery shopping or go to an amusement park without thinking about glutenfree food and my condition. I think that most doctors probably think it’s a walk in the park to get diagnosed with celiac disease because it’s just controlled by diet – it’s not.
24 | GI.ORG/ACGMAGAZINE
// COVER STORY
“I have used my position as an advocate to fight misinformation in the community.” —Erica Dermer
Brad Swiftney: In the field of GI, there are many symptoms (pain, nausea, fatigue) that not only effect you physically, but also any psychological feelings of depression, guilt, hopelessness, etc. While a GI is no psychologist (and shouldn’t be), I have found there are several medications that can not only treat physical pain, but also support your psychological health as well.
Tina Aswani Omprakash: I want physicians/trainees to know how difficult it is to manage rectovaginal and perianal fistulae. From multiple enemas a day to changing pads round the clock, to having no sex life as a young married woman and crying in pain from the dagger-like feeling in the bottom, this is not a life. We need better interventions and more research funding poured into optimal options to treat fistulae.
Q: How can physicians effectively discuss psychosocial issues, sexual health, and implicit bias with patients during routine care visits?
Melissa Adams VanHouten: The best a physician can do is recognize that biases exist and try to be aware of them should they occur. Physicians

should let the patient lead the discussion and offer a good amount of space and leeway. The safer the patient feels, the better likelihood honest and fruitful discussions can occur.
Ryan Piansky: Building a relationship and rapport with your patient is really important, but it’s also important to remember the patient’s job isn’t to educate the doctor. It’s important the doctor takes the time

COVER STORY | 25
“This is not just a training session or learning opportunity; there is a frightened human before you who needs to know you care.”
—Melissa Adams VanHouten
to understand how the patient wants to be addressed and to make sure the patient feels comfortable.
Allison Rosen: Listening to your patient, having and demonstrating sincere empathy, and asking how you are really doing can foster an amazing doctor-patient relationship. Shared decision making across the cancer continuum is key. Care goes beyond standard cancer care, various topics that can often be considered taboo need to be addressed head on.
Jeffrey Roberts: I hear from patients about their lack of access to physicians. Visible racial minorities have a harder time accessing care and research has shown that patients have better outcomes if seen by someone of the same race.
Ryan Piansky: Healthcare and health insurance is really hard to navigate in the United States. It’s a lot to ask of doctors but helping patients with these issues surrounding access to care can be such a huge help.

Erica Dermer: It’s about being open with your patient. You need to have a relationship where you’re comfortable talking about hard things with your patient. Working with a GI psychotherapist or GI psychologist would be my preference for every GI.
Brad Swiftney: I believe that having a social worker involved in the patient’s care where there may be barriers to care (physical, emotional, financial, etc.) is key to treating the condition, but also the patient. By conversing with the patient’s family and coming to understand their perspective and community, openly discussing the patient’s situation and the physician’s recommendations, and then educating the family on the fundamentals of medications/therapies, there can be a
better understanding. Here the patient feels listened to, not as if a physician is telling them what to do.
Jessica Caron: We don’t want an ‘us versus them’ mentality with our physicians. We don’t want a lose-lose scenario where both the patient and the doctor feel like they have done a disservice. We want our doctors to start to see us as people, and this needs to be role modeled by more senior physicians.
Tina Aswani Omprakash: I would like to see automatic referrals to mental health therapists, dietitians and pelvic floor therapists for patients who are really struggling. There needs to be an algorithm set up, especially at the premier IBD institutions, to make these referrals after the first visit with the physician. It would also help if the physician and their PA or nurse could ask how the patient is managing emotionally and managing diet, as well as pain and defecation mechanics.
Q: What is the biggest pet peeve you have about prior/current care or research relating to your GI disease?
Melissa Adams VanHouten: Reading about an illness in a textbook or hearing lectures is not the same as knowing someone’s personal struggles, feeling their pain, grieving the loss with them. So many physicians downplay, ignore and dismiss the effects of this illness, believing symptoms are exaggerated or invented. This impacts research questions and funding.
Melissa Adams VanHouten: Another pet peeve is regarding language. ‘Functional disorders’ is not a term patients welcome. They likewise do not appreciate brain-gut disorders
26 | GI.ORG/ACGMAGAZINE
“Don’t just talk the talk of inclusion, walk it. If a clinician preaches they’re all about patient-centered care, then they should be providing an opportunity for the patient voice to be heard FROM the patient.”
—Alison Rothbaum
“Building a relationship and rapport with your patient is really important, but it’s also important to remember the patient’s job isn’t to educate the doctor.”
// COVER STORY
—Ryan Piansky
being treated as "all in your head" issues or every symptom being blamed on stress. This language conveys to a patient that they are not being taken seriously, and that the illness is not a big deal. That is simply incorrect.
Ryan Piansky: Early on, I had a lot of my symptoms dismissed outright. Taking the time to listen and believe patients should be a given, but it can be a helpful reminder for doctors. You should NEVER question the patient’s experience.

Allison Rosen: I would love to see more policy initiatives where healthcare workers and the patient/ survivors work together to make changes to the system. My biggest pet peeve about research related to colorectal cancer is that the amount of research dollars does not align with the increasing incidence and associated mortality. Sadly, I have seen many of my own friends literally run out of treatment options and subsequently pass away.
Jeffrey Roberts: My biggest pet peeve about IBS is that physicians often do not follow patients beyond the initial diagnosis. I worry that patients who are initially labeled with IBS might actually have other conditions.
Erica Dermer: If a doctor wants to refer me to a specialist – don’t make me feel like you are just passing me along. I want to feel like you’re equally engaged in my care as I am. I want to feel like you care about every minute you’re talking to me.
Brad Swiftney: My biggest pet peeve is the feeling when a physician has a plan of care before even meeting with the patient and family. It can seem easy to just look at the chart and already have a diagnosis and treatment plan before meeting the patient/family. I urge physicians to take the additional time needed to ask another question or two, as it can reveal so much more for that patient than a medical chart ever could.
Jessica Caron: Unfortunately, when time is tight the first topics of conversation to leave the room are non-life saving topics such as mental health, wellbeing, and chronic disease management.
Q: In the future, if there was an opportunity for patient advocates to participate in GI fellow education how would this work best?
Tina Aswani Omprakash: Trainees must understand the psychosocial impact of a patient’s disease and evaluate how they interact with patients. I believe more training in conversations regarding sexual health, including loss of a sex organ, communication plans, shared decision making, and coordination of care are essential to developing an excellent gastroenterologist. Proactive communication about "who to contact," "how to reach out during a holiday or flare" is how a physician builds trust.
Tina Aswani Omprakash: I would love to see the patient voice celebrated at GI conferences, with in-person or virtual workshops available for GI fellows.
Alison Rothbaum: It is important to guide trainees NOW before they’re in their routine, except they’re also likely being trained by “old school” physicians, so we have to work around that too. Patient inclusion vs. exclusion is imperative. Those that say involving a patient in some areas means the topic dynamic changes just highlights a bias that patient meetings need to be at a lower level of comprehension – which is untrue. This is a missed opportunity for physicians and patients to communicate on research, knowledge gaps, and future opportunities.
Alison Rothbaum: Don’t just talk the talk of inclusion, walk it. If a clinician preaches they’re all about patientcentered care, then they should be providing an opportunity for the patient voice to be heard FROM the patient.
Melissa Adams VanHouten: In-person interactions tend to be the most impactful because you cannot deny there is a person standing before you
COVER STORY | 27
“As we still do not know the cause of IBS, there remains an unmet need for effective treatments which do more than simply manage the symptoms.”
—Jeffrey Roberts
who has individual needs, hopes and desires that must be met. Workshops with role-playing might be valuable as it offers personal interaction (with direct feedback). I plead for genuine patient inclusion and not just tokenism. It needs to matter. Patients will know if it does not.
Ryan Piansky: There are lots of patient experiences highlighted on social media that already exist. I’ve also participated in patient panels (at conferences), and I always enjoy seeing doctors and fellows in the audience. I think these provide a helpful look at patients’ day-to-day lives that allow doctors to better contextualize the illness a patient is facing and the effects of different treatment options.
Allison Rosen: I believe the most important opportunity for patient advocates is to incorporate their detailed, personal stories as a part of formal fellowship curriculum. I sincerely believe every medical education conference


should include the patient voice, and a seasoned advocate should be able to attend at no charge. I do not believe you can create anything useful for the patient without the patient advocate included in every important decision.
Jeffrey Roberts: I have been successful hosting live Twitter chats via @TuesdayNightIBS, podcasts and webinars with trainees that are either conducting research related to IBS or have a desire to care for patients with IBS. Industry also has an interest in both, educating the public about disease. I have brought other patients with me to the FDA to testify at advisory committee meetings. I have tried to bring patients to conferences; however many do not feel that they can leave their homes because of the severity of their IBS. Therefore, social media and remote opportunities seem to work best for the IBS patient community.
Erica Dermer: I am happy to engage with fellows in any way – but as a professional patient advocate I need to be fairly compensated for my time and travel.
Brad Swiftney: I think personal testimonies from patient advocates, medical social workers, etc., would be extremely beneficial to GI trainees. Additionally, having a guest speaker or even an interactive quiz/game to learn some sociological factors that can factor into healthcare would be extremely beneficial. For example,

28 | GI.ORG/ACGMAGAZINE
// COVER STORY
“We must find a way to use the patient voice to increase exposure to the physicians who need to hear this message most.” —Jessica Caron
“It can seem easy to just look at the chart and already have a diagnosis and treatment plan before meeting the patient/family. I urge physicians to take the additional time needed to ask another question or two, as it can reveal so much more for that patient than a medical chart ever could.” —Brad Swiftney
when I first started my career in the field of medical social work, I became easily annoyed with the patients who would no-show for their appointments often. I would think to myself: ‘Don’t you want to get better? Why not come to your appointment?’ but I began over time to gain the perspective of my patients and think outside my livelihood. The struggle of the patient who has an unreliable vehicle,
or little finances and family involvement can influence the ability to attend clinic appointments.
Jessica Caron: I’ve had the opportunity to speak at several national GI conferences, but patient advocates are always the least-attended lectures in the room, in the back hallway where no one can find us. To reach the trainees/fellows who need help humanizing their patients, we
Thought s on Future Directions from Dr. Dunleavy
must be standing in front of them, and respected in front of their peers and mentors. We must find a way to use the patient voice to increase exposure to the physicians who need to hear this message most. Often, we are telling the same caring, kind and engaged physicians the same message, but this will not move the needle to improved medical care. We must find the skeptics and engage.
I would like to thank each patient advocate for their participation in this article. It was important to me that their words be heard in their voice, and not mine. These interviews demonstrate the natural collaboration that can occur between patient advocates and GI fellows. I strongly believe the patient voice needs to be celebrated, louder, in more venues, on repeat, for as many trainees and gastroenterologists are willing to listen. Without the patient voice in our training, we cannot address their needs for the present or future. There is a myriad of ways to incorporate the patient advocate voice to significantly improve physician-patient interactions.
• Offer virtual and in-person patient participation in a true hybrid format at major GI conferences. Promote patient advocates on panels center stage, in the main venue to reach more GI fellows.
• Invite patient advocates to share their story when discussing high impact research, industry projects and learning about disease management at the fellowship program level. There are already many engaging patient stories on Twitter, Instagram, Facebook and podcasts organized by patients
• Do not be afraid to listen to the message of support being offered to patients; you can learn from material that was not developed with the doctor in mind.
• Engage patient advocates on social media. For example, @MondayNightIBD on Twitter has created a patient experience day where patients engage with physicians on the topic of the week, creating an open dialogue.
• Create workshops at national conferences to provide an opportunity for GI fellows to practice these skills. Just as we learn procedural skills and receive feedback, the same must apply for communication skills and patient engagement.
How to Build Empathy?
• Invite patient advocates to participate in grand rounds to create an avenue of learning.
• Fairly compensate patient advocates for their time and skills. We must not partake in tokenism when it comes to celebrating the patient voice.
• Meaningfully embed the patient voice formally in GI fellowship curriculum, ensuring our future GI leaders have the tangible skills to care for all patients as a whole person.
As Dr. Corey Siegel says, during his patient visits “there are two experts in the room – the doctor and the patient.” Many of our GI patients have chronic illnesses with waxing and waning disease courses. Between these clinic visits and hospitalizations are first dates, graduations, weddings, world traveling, and countless hours of suffering that we will never see. We must meet our patients where they are and be mindful to not create a burden for either stakeholder.
• Introduce yourself, every single time
• Validate a patient’s fears, desires, and concerns
• Listening means assessing and understanding
• Be accountable: Do what you say you’re going to do, when you say you’re going to do it
• Apologize when mistakes occur
• Always be honest
• Learn about your patient as a person
COVER STORY | 29


30 | GI.ORG/ACGMAGAZINE ACG PRACTICE MANAGEMENT Toolbox Billing & Coding ACG’S FORUM NEW! Members Only ACG members and GI practices continue to face mounting financial and reimbursement pressures. Complex coding and documentation requirements only add to these burdens. The ACG Practice Management Committee is pleased to announce the new member benefit: professional coding and documentation assistance for ACG members, tailored to your individual practice’s questions and needs. gi.org/practice-management Start Building Success Today HAVE A QUESTION? Email coding@gi.org Arlene Morrow, CPC, CMM, CMSCS, is now available to answer your questions! ACG members will receive an answer and guidance within a few business days.
Culinary Connections:
All Things Spring
Editors: Vani Paleti, MD, Alexander Perelman, DO, and Christina Tennyson, MD

SPRING IS FILLED WITH colors, fragrances, chirping birds, promises and celebration of renewed of life from winter slumber.
In this spring edition of #ACGfoodies, we celebrate two gastroenterologists and a registered GI dietitian who share their culinary journeys with their soulful and healthy recipes.
Let’s jump in and enjoy spring contributions from Baha Moshiree, MD, MS-CI, FACG, Clinical Professor of Medicine, Wake Forest Medical University and Director of Motility, in the Division of Gastroenterology at Atrium Health, in Charlotte, NC, Ms. Emily Haller, MS, RDN lead GI dietitian at the Division of Gastroenterology and Hepatology at University of Michigan Health, Michigan Medicine and Sameer K. Berry, MD, MBA, Gastroenterologist, New York Gastroenterology Associates; Chief Medical Officer, Oshi Health.
—The #ACGFoodies (Vani, Alex, Christina)
ACG PERSPECTIVES | 31
BAHA MOSHIREE, MD, MS-CI, FACG
 Clinical Professor of Medicine, Wake Forest Medical University and Director of Motility, Division of Gastroenterology at Atrium Health, Charlotte, NC
Clinical Professor of Medicine, Wake Forest Medical University and Director of Motility, Division of Gastroenterology at Atrium Health, Charlotte, NC
My full first name is Baharak, which means “little spring,” the season in which I was born. Spring has a special meaning in my culture. In addition to signaling the rebirth of nature, it symbolizes a renewal of spirit and recommitment to health, community, and hope. The vernal equinox, or first day of spring, marks the beginning of the Persian New Year, Nowruz (“new day”), which is celebrated by 300 million people worldwide — by Iranians and other Persians of all faiths.
This year, celebrating Nowruz feels especially significant. Today in Iran, women, children, and men are bravely fighting for their basic human rights of self-determination and self-expression against an oppressive regime. The slogan

SABZI-POLO (HERB-RICE)
Ingredients:
• 3 cups long-grain Basmati rice
• 1/2 cup chives, chopped
• 2 cups fresh dill, chopped
• 2 cups fresh parsley, chopped
• 2 cups fresh cilantro, chopped
• 1 Tbsp dried fenugreek
• 1/4 cup vegetable oil




• 1/2 tsp ground saffron dissolved in 4 Tbsp hot water
• 1 tsp rose water (optional)
• 2 Tbsp salt
Steps:


1. Rinse rice in a large bowl until
of their revolution, “Woman, Life, Freedom!” represents an intention and hope for their future rooted in the cultural traditions and proud history of their past. They and all Iranians in the diaspora look forward to a “new day” of freedom, prosperity, and joy.
Growing up, Nowruz was always my favorite time of year. The mark of all good holidays, food plays a vital role in Nowruz and is celebrated not just for its nourishment but for its healing qualities and its ability to bring people together. Each Nowruz, Persians set a “haft-sin” table on which we place items representing rebirth and fertility (sprouts of lentil, sumac, painted eggs), health (apple and garlic), prosperity (coins), joy (candles), love (dry fruit called senjed) and patience (vinegar). Thirteen days of festivities follow and are filled with visits to family and friends. At the center of every table, you will find fruits and nuts in
Saffron is included in most Iranian dishes, including desserts. Some of the digestive health benefits of saffron as an anti-inflammatory agent and antioxidant include its uses in irritable bowel syndrome (IBS).
Persian dishes are also accompanied by a bowl of cultured yogurt combined with either cucumbers and mint or minced shallots. Many ancient civilizations from Persians to Egyptians have lauded the healthy properties of yogurt with links to better skin, longevity, and GI illnesses - a discovery that seems more recent with the microbiome and gut health link.
The main dish for Nowruz is fish and a rice dish called “sabzi-polo.” How Persians prepare rice by rinsing, boiling, then recooking has it own digestive benefits and potentially leads to less bloating. Sabzi polo is also full of nutrient rich herbs. This Nowruz, make this simple sabzi-polo

the water the rice is submerged in is close to clear. (Helps remove starch.)
2. Bring 8 cups of water with 2 Tbsp salt to boil in a large pot. Add rinsed rice and boil for about 6-8 minutes or until the rice grains feel soft.
3. Drain cooked rice in a colander and rinse with 3 cups cold water. Set aside.
4. Combine all freshly chopped herbs and fenugreek in one bowl. Set aside.
5. In a medium bowl, mix vegetable oil, ¼ cup of water, and a few drops of saffron water.
6. Pour in most of the mixture of oil, water and saffron to coat the bottom of the pot used earlier to boil rice. On top of this, layer 2 spatulas of rice followed by 1 spatula of herbs. Repeat until you have a layer of rice at the top. Using the end of a wooden spoon or fork, poke several holes into the rice.
7. Pour the remaining amount of oil, water, and saffron mixture plus 1 tsp rose water over the rice.
8. Place a clean dish towel between the pot and the lid and cover to absorb any condensation. Press the lid firmly on the pot so steam cannot escape. Cook for 10 mins on medium heat and then reduce to low for an additional 30-45 mins. Remove pot from heat and let cool for 5 mins.
9. The crispy rice at the bottom of the pot is called “tadig.” Remove lid, flip the pot onto a large serving dish, and enjoy!
// PERSPECTIVES
EMILY HALLER, MS, RDN
Lead GI Dietitian, Division of Gastroenterology and Hepatology at University of Michigan Health, Michigan Medicine

I pursued a career in dietetics because of my genuine love for food and desire to work in a setting that allowed me to connect with and help others live healthier, happier lives. I appreciate the ability to connect with others through food, whether it be through conversation, experimenting in the kitchen, or sharing a meal.

Two years into working as a dietitian, I attended a presentation at Ann Arbor’s Veg Week on the environmental impacts of animal agriculture. This was my first exposure (that I recall anyway) to learning how factory farming is destroying our ecosystems and it evoked many emotions, including confusion about how this could be true/happening, sadness, and concern. Now, this talk was fortunately not all
CHICKPEA TUNA SALAD
Ingredients: Chickpea Tuna Salad:
• 1 15.5 oz. can of chickpeas, drained* (*Save 1 Tbsp of aquafaba--the chickpea liquid)
• 1 Tbsp aquafaba
• ½ cup celery, diced (~2 stalks)
• ¼ cup red onion, diced (~1/8 of a medium red onion)
• ¼ cup diced dill pickles (~1.5 pickle spears)


• 1/3 cup vegan mayo
• Salt and black pepper, to taste
Sandwich Fixings:
• Whole grain bread of choice, toasted
• Veggies of choice: greens (lettuce, spinach, arugula), tomatoes, thinly sliced radish, cucumbers, shredded cabbage slaw, pickles
and enthusiasm shared around what adopting a plant-based diet can do for our land, air, and water. Shortly after this talk, I decided to do a 30-day vegan challenge to make a positive impact on the environment. During this 30-day challenge I experimented with new recipes, watched a few documentaries like Forks Over Knives and started reading various vegan/vegetarian research articles. I approached the transition with curiosity and flexibility, two things I frequently discuss with patients/ clients when working on habit and behavior change. The more I learned, the more excited I felt about eating a vegan diet and once I reached my 30-day mark I did not want to return to my omnivorous meals. At the time I was training for a half-marathon and felt I was recovering from workouts well so I decided I would stick with it until after my race.
Fast-forward 10 years and I am still
not just for my own health, but for the health of the planet and all its inhabitants. This choice aligns with my morals and values and has helped me become a more empathetic and compassionate person.
While a vegan diet may not be for everyone, the science is clear that eating more nutrient-dense, plant-based meals and decreasing animal products supports human and planetary health. I am fortunate that my job allows me to meet individuals where they are and assist them in adopting a dietary pattern that includes more plants and supports their health.
A key strategy to eating more plantbased meals is to ensure you have a phenomenal replacement for whatever you are taking out. Love eggs? Try making a flavorful tofu scramble and include kala namak (Himalayan black salt) for that sulfur ‘eggy’ flavor. Obsessed with buffalo chicken wraps? Swap in soy curls for chicken and top with your favorite sauce plus toppings.
Steps:




1. Add chickpeas to a medium mixing bowl and mash with potato masher until a flaky texture is achieved. (You can also pulse the chickpeas a few times in a food processor and get the same consistency.)
2. Mix in the rest of the ingredients: diced onion, celery, pickle, vegan mayo, aquafaba
3. Add salt and pepper to taste
4. You can certainly eat this immediately; however, it is best chilled. Recommend transferring to container with a lid and letting chill in the refrigerator.
5. Serve on bread of choice with sliced tomato and fresh greens or whatever toppings your heart desires.
6. The chickpea tuna salad will last for 4 days in the refrigerator and would also be great served on a bed of greens, in a salad, or in a wrap.


Tuna salad sandwich fanatic? Try smashing chickpeas for that flakey, chewy texture and follow my recipe below!
This mouth-watering sandwich is a vegan take on the classic tuna salad sandwich. This chickpea tuna salad recipe is simple to throw together, requires 8 ingredients, and is a great meal prep option. When making this recipe at home, we typically double everything so there are leftovers for the week.
SAMEER K. BERRY, MD, MBA

Like many of us, I live to eat, rather than eat to live. I grew up in a household with two busy working parents, so a complex home-cooked Indian meal was a rare treat. My sister and I both have fond memories of learning to cook Indian recipes with our family elders. I remember how surprised I was to learn how small nuances can have such a significant
impact - the decision to use ground or whole spices, even the order of adding ingredients to the heated pan can change the taste dramatically.
Inadvertently, my medical training continued to remind me of the major impact seemingly trivial changes to one’s diet can have. I spent time as a medical student rounding on the inpatient IBD service with renowned dietitian Kelly Isaacson; and continued to explore the impact of food as medicine during my fellowship with William Chey. These training experiences influenced my choice of clinical practice at New York Gastroenterology Associates, one of the few community practices with three full-time dietitians.
As gastroenterologists, food has a totally new meaning to us. Any gastroenterologist browsing a grocery store aisle will likely see details in food that are unappreciated by most - FODMAPs, gluten, sugar alcohols, and other subtle details which impact nearly all of our patients. Unfortunately, despite the evidence demonstrating improved quality of care when gastroenterologists work alongside dietitians, we have been painfully slow in providing access to dietary interventions
VEGETABLE RAMEN WITH ZUCCHINI NOODLES
Ingredients:
• 1 Tbsp olive oil

• 1 clove garlic, minced
• 1.5 shiitake mushrooms
• 1/2 bell pepper, chopped
• 1 cup spinach, shredded
• 1/2 cup zucchini noodles, frozen
• 1 cup vegetarian broth

• 2 Tbsp coconut amino or soy sauce
• Soft-boiled egg
• 2 Tbsp sauerkraut
• Sriracha hot sauce, to taste
• 2 Tbsp cilantro, chopped
Steps:


1. Heat olive oil in a large pot, add minced ginger and garlic until bubbling.
2. Add shiitake mushroom, cook 1-2 mins.
3. Add green bell pepper and spinach, cook 1 min.
4. Add vegetarian broth and coconut amino (or soy sauce), let simmer.
5. Add frozen zucchini zoodles, let simmer 2 mins.
6. Transfer to bowl and add soft-boiled egg, a drizzle of Sriracha, sauerkraut, and sprinkle with fresh cilantro.
for our patients. This frustration led me to launch a new clinical model at Oshi Health, where we are building a world where all patients can receive access to multidisciplinary care – and understand how connections between food, behavior, and the brain impact their symptoms.
While I do not follow a vegan lifestyle, I try to follow a plant-based diet. I hope you enjoy this healthy, warming vegetable ramen with zucchini noodles and microbiomefriendly sauerkraut. We have overcome so many challenges as physicians and gastroenterologists over the last two years; I look forward to many more delicious meals with my GI mentors and colleagues for decades to come.
We would like to hear from you if you have personal connections with GI & gastronomy. Contact ACG magazine staff by email at acgmag@gi.org to share your story with the ACG community. You can also tweet using #ACGfoodies to connect with the community.
Gastroenterologist, New York Gastroenterology Associates; Chief Medical Officer, Oshi Health
// PERSPECTIVES
Teaching Hospital, Nigeria to Brown University Rhode Island Hospital
 By Evaristus Sunday Chukwudike, MD
By Evaristus Sunday Chukwudike, MD


I, Dr. Evaristus Sunday Chukwudike of the University of Calabar Teaching Hospital, Nigeria, write to express my profound gratitude to the American College of Gastroenterology (ACG) for granting me the privilege to undergo an observership fellowship training for six months as a 2021 ACG International GI Training Grant recipient.

My training at the Brown University/ Rhode Island Hospital in Providence, United States, started on the 4th of January 2021. I was warmly welcomed by my training directors, Dr. Akwi W. Asombang and Dr. Steven F. Moss, and other staff who work at the Rhode Island Hospital endoscopy suite.

After that, my training mentors organized an orientation to enable me to acclimate to the environment and to understand the programs and facilities at the endoscopic suite. During the training, I participated in their general gastroenterology clinic consultations at the specialists' and fellows’ clinics, esophageal motility clinic, Clostridioides difficile clinic, in-patient rounds, and endoscopic procedures. Endoscopic activities comprised basic and advanced procedures emphasizing pre-procedural, intra-procedural, and post-procedural consults. I participated in the following endoscopic procedures, namely; esophagogastroduodenoscopy (EGD), colonoscopy, endoscopic biopsies, endoscopic radiofrequency ablation and
cryoablation for Barrett's, endoscopic esophageal variceal ligation, endoscopic esophageal dilation (balloon and Savary), argon plasma coagulation of AVMs, hemostatic bipolar probe cauterization of bleeding vessels, foreign body retrieval, single balloon/spiral enteroscopy, mapping for intestinal metaplasia, insertion of a wireless catheter for ambulatory pH monitoring, capsule endoscopy, PEG tube insertion, polypectomy techniques for small and large polyps, clip and snare deployment, epinephrine injection, retrieval of large polyps with retrieval nets, deployment of hemo-spray, spyglass cholangioscopy, endoscopic retrograde cholangiopancreatography (ERCP), endoscopic ultrasound (EUS), and manometry.
I also participated in their weekly academic seminars and presented on the topic titled, "Overview of Gastroenterology Program in Nigeria." During my training, I presented my abstract at Digestive Disease Week 2022 titled, “Helicobacter pylori antimicrobial resistance and eradication rates in Africa: A systematic review."
The training offered me the opportunity to interact and network

with the international community of gastroenterologists, courtesy of my training directors' deliberate efforts. I especially thank the American College of Gastroenterology for the opportunity, and my training directors, Dr. Akwi W. Asombang and Dr. Steven F. Moss, for being amazingly supportive. My gratitude also goes to Dr. Rolf Carlson of Brown University. Thanks to Dr. Jean Roye, Dr. Habr Fadlallah, Dr. Sarah Hyder, Dr. Colleen Kelly, Dr. Amanda Pressman, Ablaye Gueye, and all other staff at the Endoscopy Suite of the Rhode Island Hospital.
My training ended on the 30th of June 2022 with a certificate of distinction award and a send-forth/ get-together organized at the endoscopy suite of the Rhode Island Hospital.
ACG PERSPECTIVES | 35
Evaristus Sunday Chukwudike, MD, University of Calabar Teaching Hospital, Nigeria
Evaristus Sunday Chukwudike, MD, University of Calabar
At the endoscopy suite, Rhode Island Hospital. Being guided at the ENDOSIM center by my mentor, Dr. Akwi W Asombang.
transform what we do in day-to-day clinical practice. The current artificial intelligence clinical applications are only the ”tip of the iceberg.” We are going to see the scope of AI expanding into other clinical areas within endoscopy, as well as using big data to help risk stratify patients for various GI diseases.
• I also believe there’s going to be tremendous growth in endosurgery. The current and future endoluminal techniques and devices for procedures, like ESD and endobariatrics, will evolve, allowing more physicians to perform these procedures.
• Lastly, robotics in endoscopy will become an everyday reality.
Innovator Interview by the ACG Innovation & Technology Committee: Dr.
Bara
Kurdi
Seth Gross, MD, FACG Reflects on His Path of Innovation in GI
1 2
What are some of the challenges and hurdles one should expect going down the innovation path and how to best navigate them?
There are many things to consider when going into innovation:

• If it’s your own concept, you must secure the intellectual property rights. If you work for a health system or hospital, you need to make sure you understand your institution’s policies around invention.
What is your experience with GI innovation?
I think everyone’s involvement is different. Initially, I started in fellowship around clinical research. My project was to evaluate narrow band imaging for colon polyp detection. However, my involvement in innovation today has multiple elements. I still do clinical research in up-and-coming areas, most recently it has been with artificial intelligence. I also work closely with the industry to evaluate startup companies by providing guidance on clinical research, pathways to market, and reimbursement strategies. Aside from being involved in clinical research to evaluate/develop devices and techniques, I also work at the society level to help secure reimbursement for new technologies and techniques.
Reimbursement often tends to be the missing link between having access to something beneficial to patients since, without reimbursement, it can be challenging for hospitals and practices to bring on new technology.
How did you get started on this journey? My first exposure to GI innovation was in fellowship. I had the opportunity to work with physicians who loved being at the forefront of our field. This experience inspired me to get involved in innovation after I finished training.
What technologies are you most excited about in the next 3 to 5 years?
4 3 // PERSPECTIVES
There are several areas that are being developed in our field, which I’m very excited about:
• Artificial intelligence, which right now is limited to polyp detection, will ultimately
• The path from developing the idea to having it commercially available is complex and long. You need to navigate early funding to support product development, clinical research, and taking your idea through the regulatory hurdles for FDA approval.
• Lastly, if the plan is for this to get acquired by a larger entity, in most situations you will need clinical data in humans and demonstration of sales.
What is the one hobby/activity that you feel gives you the fuel you need to keep on trailblazing?
For me, trying to improve on my worklife balance is really important. On my personal time, I enjoy being with my family, playing tennis, and navigating the ups and downs on the golf course.
36 | GI.ORG/ACGMAGAZINE
5
El
in Conversation with Dr. Seth Gross
Editors: Aasma Shaukat, MD, MPH, FACG and Vivek Kaul, MD, FACG
What advice do you have for any ACG members interested in getting involved in or started down a path of innovation in the GI space?

• You need to understand the clinical landscape you work in.
• Also being able to recognize the unmet need when you’re asked to evaluate new technologies and procedures. Many times, I see something which is interesting, but at the same time recognize in the current clinical environment it will be difficult to make it to market.
• If you plan to bring an idea of your own to market, you need to commit 100 percent.

• Also, keep in mind there are different ways to be involved with innovation: You can have your own idea, evaluate company concepts, work at the society level on various committees (FDA or Innovation and Technology), or work in the research realm by being a part of clinical trials.
Any final pearls of wisdom or advice based on your experience?
After fellowship training, there are many different paths one could take. If you have interest and desire in innovation, you’ll be joining a community that aims to move medicine forward; it is one of the most rewarding roles in healthcare.
LEARN MORE Robotics in Endoscopy


1. Cui Y, Thompson CC, Chiu PWY, Gross SA. Robotics in therapeutic endoscopy (with video). Gastrointest Endosc. 2022 Sep;96(3):402-410. doi: 10.1016/j.gie.2022.05.019. Epub 2022 Jun 3. PMID: 35667390.

Artificial Intelligence
1. Kröner PT, Engels MM, Glicksberg BS, Johnson KW, Mzaik O, van Hooft JE, Wallace MB, El-Serag HB, Krittanawong C. Artificial intelligence in gastroenterology: A state-of-theart review. World J Gastroenterol 2021 Oct 28;27(40):6794-6824. doi: 10.3748/wjg.v27.i40.6794. PMID: 34790008; PMCID: PMC8567482.
2. Le Berre C, Sandborn WJ, Aridhi S, Devignes MD, Fournier L, Smaïl-Tabbone M, Danese S, Peyrin-Biroulet L. Application of Artificial Intelligence to Gastroenterology and Hepatology. Gastroenterology 2020 Jan;158(1):76-94.e2. doi: 10.1053/j. gastro.2019.08.058. Epub 2019 Oct 5. PMID: 31593701.
ACG PERSPECTIVES | 37 7 6
About Dr. Gross –Seth A. Gross, MD, FACG is Professor of Medicine at NYU Grossman School of Medicine and Clinical Chief, Division of Gastroenterology and Hepatology at NYU Langone. Dr. Gross is a member of the ACG Innovation & Technology Committee.
About Dr. El Kurdi – Bara El Kurdi, MD is a third year GI fellow at UT Health San Antonio Long School of Medicine, Division of Gastroenterology. He is a member of the ACG Innovation & Technology Committee.
EVIDENCE BASED GI JOURNAL REVIEW

Clinical take-aways and evidence-based summaries of articles in GI, Hepatology & Endoscopy.
ACG PUBLICATION EVIDENCE BASED GI (EBGI) evaluates new research articles published across GI and Hepatology journals using evidence-based criteria.
ACG Editors identify the highest quality studies published on important topics and create structured abstracts summarizing the study for quick reference and provide commentary on how the data is applicable to clinical practice.
Editors record audio summaries for easy listening on the go. Listen to individual article summaries or stream the entire issue all at once.
Member benefit!
Watch for the eTOC delivered in your inbox monthly!
Full issue download available as PDF: gi.org/ebgi
38 | GI.ORG/ACGMAGAZINE // PERSPECTIVES
THE RED JOURNAL KICKED OFF THE YEAR with two new ACG clinical guidelines, adding to the catalogue of evidence-based clinical recommendations from the College. Alberto Rubio-Tapia, MD, and colleagues updated the guidelines on Diagnosis and Management of Celiac Disease, and Brian C. Jacobson, MD, MPH, FACG, and co-authors developed a new guideline on Diagnosis and Management of Gastrointestinal Subepithelial Lesions.


In CTG, Jactel, et al., examined the effectiveness of a digital, personalized dietary program in reducing symptoms in patients with comorbid IBS and IBD, using machine learning.
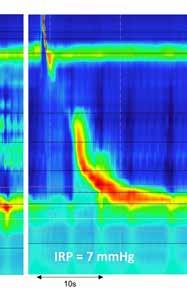





ACG Case Reports Journal Co-Editorsin-Chief Nicholas McDonald, MD, and Tomoki Sempokuya, MD, collaborated with Mohammad Bilal, MD, on an article and podcast, “How to Be a Great Peer Reviewer.”






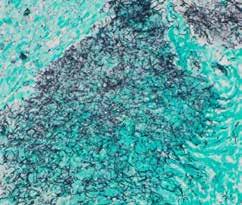
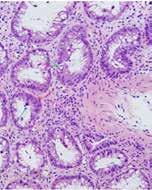

INSIDE THE JOURNALS | 39 Inside
Volume XXX Number X | Month 2023 College of Gastroenterology LIFESPAN OF GI LIFESPAN OF GI CASE REP ACG An Online Journal of Case Reports edited by Gastroenterology& Hepatology Fellows ACGCASEREPORTS.COM ACGREPORTS VOLUME 6 JOURN L
the JOURNALS
AMERICAN JOURNAL OF GASTROENTEROLOGY]
ACG Guidelines Update: Diagnosis and Management of Celiac Disease
Alberto Rubio-Tapia, MD; Ivor D. Hill, MD, FACG; Carol E. Semrad, MD, FACG; Ciarán P. Kelly, MD, FACG; Benjamin Lebwohl, MD, MS. The American Journal of Gastroenterology 118(1):p 59-76, January 2023. | DOI: 10.14309/ajg.0000000000002075
An update to the 2013 ACG Guidelines on Celiac Disease provides evidence-based recommendations derived from clinical findings and advances in our understanding of the disease over the last decade. Using the GRADE methodology, the authors provide eight updated recommendations addressing screening, diagnosis, management strategies including diet and medical device use, preventive care, testing in children, and more. Highlights include recommendations that multiple biopsies of the duodenum are necessary for diagnosis; pneumococcal vaccination is safe, effective, and “widely recommended” for adults 65 and older and smokers aged 19 to 64; and that patients with symptoms suggesting malabsorption, such as chronic diarrhea with weight loss and abdominal pain, should be tested for celiac disease.
READ bit.ly/acg-guidelines-celiac-2023 LISTEN bit.ly/acg-celiac-guideline-podcast
ACG Clinical Guideline: Diagnosis and Management of Gastrointestinal Subepithelial Lesions
118(1):p 59-76, January 2023. | DOI: 10.14309/ajg.0000000000002075
The Gastrointestinal Subepithelial Lesions Guideline is a new ACG guideline and presents 11 preferable approaches to diagnosis and management of a patient with GI subepithelial lesions (SEL). The authors suggest the use of endoscopic ultrasound for the diagnosis of nonlipomatous SEL, that EUS with tissue acquisition may improve diagnostic accuracy for the identification of solid nonlipamatous SEL, and do not suggest one type of endoscopic therapy for the resection of small (<1 cm), low-grade rectal neuroendocrine tumors, among other preferable approaches. The authors note that, “Future studies should clarify the role of primary resection vs. preresection diagnosis, whether there is a diagnostic role for artificial intelligence, and directly compare endoscopic resection methods.”
BASED GI REVIEW evidence-basedsummariesof Endoscopy
READ bit.ly/acg-guideline-sel-2023
BASEDGI(EBGI) evaluates new GI and Hepatology journals using quality studies published on important topics summarizing the study for quick reference and data is applicable to clinical practice. for easy listening on the go. summaries or stream the entire issue all at once.

LISTEN bit.ly/Jacobson-Podcast
[CLINICAL & TRANSLATIONAL GASTROENTEROLOGY]
download available gi.org/ebgi
Efficacy of a Digital
Personalized
Elimination Diet for the Self-Management of Irritable Bowel Syndrome and Co-Morbid Irritable Bowel Syndrome and Inflammatory Bowel Disease
10.14309/ctg.000000000000049
Patients with comorbid IBS and IBD often report that certain “trigger foods” either initiate or exacerbate symptoms, but there is no consensus on which diet is ideal. This pilot study examined the use of a personalized, digitally delivered elimination diet for patients with comorbid IBS and IBD, using machine learning. The algorithm provided highly customized diets by identifying unique patient-level patterns drawn from large data sets to predict patients’ responses to certain foods. This personalization provided patients with final diets that were less restrictive, as they considered patients’ biological, lifestyle, and clinical profiles.
The authors write, “No two final diets generated by the program were the same, providing further evidence that individuals likely respond to foods heterogeneously and emphasizing the need to personalize nutritional interventions to an individual rather than a group level.”
READ bit.ly/jactel-ibs-ibd-diet
[ACG CASE REPORTS JOURNAL]
ACG Case Reports Co-Editors-in-Chief Nicholas McDonald, MD, and Tomoki Sempokuya, MD, collaborated with Mohammad Bilal, MD, to publish an editorial on How to Be a Great Peer Reviewer. They provide specific tips and recommendations on getting involved in peer review and providing high-quality feedback to authors, which can help build your professional reputation and editorial skills. The EICs also recorded a podcast on the topic with CTG Editor-in-Chief Brian C. Jacobson, MD, MPH, FACG.
READ bit.ly/acgcrj-peer-reviewer
LISTEN bit.ly/acgcrj-peer-reviewer-podcast
You can now follow EBGI on Twitter at its own handle! Follow @ACG_EBGI to keep up with summaries and key takeaways from articles reviewed in EBGI.
40 | GI.ORG/ACGMAGAZINE
Jasmohan S. Bajaj, MD, MS, FACG; Andrew Fagan, BS; Sara McGeorge, BS; Richard K. Sterling, MD, MS, FACG; Shari Rogal, MD; Masoumeh Sikaroodi, PhD; Patrick M. Gillevet, PhD, Clinical and Translational Gastroenterology: June 2022 - Volume 13 - Issue 6 - p e00495 doi:
// INSIDE THE JOURNALS [THE
Brian C. Jacobson, MD, MPH, FACG; Amit MD; Katarina B. Greer, MD, MS; Linda S. Lee, MD; Walter G. Park, MD, MS; Bryan G. Sauer, MD, MSc, FACG; Vanessa M. Shami, MD, FACG. The American Journal of Gastroenterology
EVIDENCE-BASED GI: AN ACG PUBLICATION
delivered monthly!
ACG VIRTUAL GRAND ROUNDS

























Weekly on Thursdays at 12 pm and 8 pm ET















Live Presentation by an ACG Expert Plus Q & A
#GIhomeschooling


Even as all aspects of practice have changed due to COVID-19, your need to stay up to date on clinical GI does not stop. ACG is committed to your professional education. Our goal is to help the GI community embrace #GIhomeschooling with quality speakers and presentations.
ACG has launched Virtual Grand Rounds weekly on Thursdays at 12 pm and 8 pm ET. Each week an expert faculty member will present live on a key topic followed by Q & A.
Learn More and Register: GI.ORG/ACGVGR

INSIDE THE JOURNALS | 41
https://gi.org/acgvgr https://gi.org/acgvg https://gi.org/acgvgr
CELIAC DISEASE
Information for Patients, Parents, and Caregivers: Understanding the ACG Clinical Guidelines Diagnosis and Management of Celiac Disease
What is Celiac Disease?
Celiac disease is one of the most common gastrointestinal disorders. Celiac disease causes damage in the lining of the small intestine when eating gluten (a protein found in wheat, barley, and rye) in persons with a genetic predisposition.
Symptoms can vary greatly, but celiac often causes:
• diarrhea
• fatigue
KEY TAKEAWAYS
• abdominal pain
• anemia
• Be sure to see your doctor before trying a gluten-free diet to avoid incorrect test results.
• The initial test to look for celiac disease is a simple blood test.
• The best way to confirm a diagnosis of celiac disease is with a small tissue sample (“biopsy”) of the small intestine that requires a painless test called endoscopy (a long tube with a tiny camera put into your mouth and passed down to the small intestine under sedation).
• In children, a diagnosis without biopsy is possible under certain circumstances.
• A strict lifelong gluten-free diet is the only treatment. A dietitian can help you with the diet plan.
• Vaccination against Pneumococcus (a common bacteria causing pneumonia and other serious infections) is recommended after your diagnosis.
• Regular visits with the doctor and dietitian for follow-up are needed after starting the diet to make sure your symptoms go away. The doctor will eventually want to confirm the damage in the lining of the small intestine is healed.
• The outlook is excellent in patients who are treated for celiac disease.
• itchy/blistery skin rash
• failure to thrive in children
• loss of bone density (osteoporosis)
Questions You Should ask Your Physician about Gastroparesis Care
• Is my diagnosis confirmed?
• What is the gluten-free diet?
• What are the goals of the treatment?
• What vaccines would you recommend to prevent serious infections?
• What is the recommended follow-up?
• What is the risk in my family?
Warning Signs or Alarm Symptoms
• Celiac disease is a very serious condition, if untreated, it can cause severe malnutrition and even death.
• Consult your doctor immediately if your symptoms are not better despite following a gluten-free diet. You may need additional tests.
42 | GI.ORG/ACGMAGAZINE American College of Gastroenterology | gi.org | Follow ACG on Twitter @AmCollegeGastro
About LEARN MORE ACG Patient Information: Scan QR Code or visit gi.org/topics/celiac-disease Find a gastroenterologist near you: gi.org/FindaGI Read the Celiac Disease Guideline bit.ly/acg-guidelines-celiac-2023
REBYOTATM (fecal microbiota, live - jslm) suspension, for rectal use
Brief Summary Please consult package insert for full Prescribing Information
INDICATIONS
REBYOTA is indicated for the prevention of recurrence of Clostridioides dif cile infection (CDI) in individuals 18 years of age and older following antibiotic treatment for recurrent CDI. Limitation of Use: REBYOTA is not indicated for treatment of CDI.
CONTRAINDICATIONS
Do not administer REBYOTA to individuals with a history of a severe allergic reaction (e.g. anaphylaxis) to any of the known product components.
Each 150mL dose of REBYOTA contains between 1x108 and 5x1010 colony forming units (CFU) per mL of fecal microbes including >1x105 CFU/mL of Bacteroides, and contains not greater than 5.97 grams of PEG3350 in saline.
WARNINGS AND PRECAUTIONS
Transmissible infectious agents: Because REBYOTA is manufactured from human fecal matter it may carry a risk of transmitting infectious agents. Any infection suspected by a physician possibly to have been transmitted by this product should be reported by the physician or other healthcare provider to Ferring Pharmaceuticals Inc.
Management of acute allergic reactions: Appropriate medical treatment must be immediately available in the event an acute anaphylactic reaction occurs following administration of REBYOTA.
Potential presence of food allergens: REBYOTA is manufactured from human fecal matter and may contain food allergens. The potential for REBYOTA to cause adverse reactions due to food allergens is unknown.
ADVERSE REACTIONS
The most commonly reported (≥ 3%) adverse reactions occurring in adults following a single dose of REBYOTA were abdominal pain, (8.9%), diarrhea (7.2%), abdominal distention (3.9%), atulence (3.3%), and nausea (3.3%).
Clinical Trials Experience: The safety of REBYOTA was evaluated in 2 randomized, double-blind clinical studies (Study 1 and Study 2) and 3 open-label clinical studies conducted in the United States and Canada. A total of 978 adults 18 years of age and older with a history of 1 or more recurrences of Clostridioides dif cile (CDI) infection and whose symptoms were controlled 24 – 72 hours post-antibiotic treatment were enrolled and received 1 or more doses of REBYOTA; 595 of whom received a single dose of REBYOTA.
Adverse Reactions: Across the 5 clinical studies, participants recorded solicited adverse events in a diary for the rst 7 days after each dose of REBYOTA or placebo. Participants were monitored for all other adverse events by queries during scheduled visits, with duration of follow-up ranging from 6 to 24 months after the last dose. In an analysis of solicited and unsolicited adverse events reported in Study 1, the most common adverse reactions (de ned as adverse events assessed as de nitely, possibly, or
probably related to Investigational Product by the investigator) reported by ≥3% of REBYOTA recipients, and at a rate greater than that reported by placebo recipients, were abdominal pain, (8.9%), diarrhea (7.2%), abdominal distention (3.9%), atulence (3.3%), and nausea (3.3%).Most adverse reactions occurred during the rst 2 weeks after treatment. After this, the proportion of patients with adverse reactions declined in subsequent 2-week intervals. Beyond 2 weeks after treatment only a few single adverse reactions were reported. Most adverse drug reactions were mild to moderate in severity. No life-threatening adverse reaction was reported.
Serious Adverse Reactions - In a pooled analysis of the 5 clinical studies, 10.1% (60/595) of REBYOTA recipients (1 dose only) and 7.2% (6/83) of placebo recipients reported a serious adverse event within 6 months post last dose of investigational product. None of these events were considered related to the investigational product.
USE IN SPECIFIC POPULATIONS
Pregnancy: REBYOTA is not absorbed systemically following rectal administration, and maternal use is not expected to result in fetal exposure to the drug.
Lactation: REBYOTA is not absorbed systemically by the mother following rectal administration, and breastfeeding is not expected to result in exposure of the child to REBYOTA.
Pediatric Use: Safety and effectiveness of REBYOTA in individuals younger than 18 years of age have not been established.
Geriatric Use: Of the 978 adults who received REBYOTA, 48.8% were 65 years of age and over (n=477), and 25.7% were 75 years of age and over (n=251). Data from clinical studies of REBYOTA are not suf cient to determine if adults 65 years of age and older respond differently than younger adults
For more information, visit www.REBYOTAHCP.com
You are encouraged to report negative side effects of prescription drugs to FDA. Visit www.FDA.gov/medwatch, or call 1-800-332-1088.
Manufactured for Ferring Pharmaceuticals by Rebiotix, Inc. Roseville, MN 55113
US License No. 2112
9009000002
Rx Only
Ferring and the Ferring Pharmaceuticals logo are registered trademarks of Ferring B.V. REBYOTA is a trademark of Ferring B.V. ©2022 Ferring B.V. This brief summary is based on full Rebyota Prescribing Information which can be found at www.RebyotaHCP.com
US-REB-2200277
Where dysbiosis once left the gut microbiome in ruin,


RISE ABOVE RECURRENT C. DIFFICILE INFECTION
and restore hope with REBYOTATM
aIn the pivotal phase 3 trial, 32.8% of patients were treated at first recurrence of CDI following antibiotic treatment of CDI.1
INDICATION
REBYOTA (fecal microbiota, live - jslm) is indicated for the prevention of recurrence of Clostridioides difficile infection (CDI) in individuals 18 years of age and older, following antibiotic treatment for recurrent CDI.


Limitation of Use
REBYOTA is not indicated for treatment of CDI.
IMPORTANT SAFETY INFORMATION
Contraindications
Do not administer REBYOTA to individuals with a history of a severe allergic reaction (eg, anaphylaxis) to any of the known product components.
Warnings and Precautions
Transmissible infectious agents
Because REBYOTA is manufactured from human fecal matter, it may carry a risk of transmitting infectious agents. Any infection suspected by a physician possibly to have been transmitted by this product should be reported by the physician or other healthcare provider to Ferring Pharmaceuticals Inc.
Management of acute allergic reactions
Appropriate medical treatment must be immediately available in the event an acute anaphylactic reaction occurs following administration of REBYOTA.
Potential presence of food allergens
REBYOTA is manufactured from human fecal material and may contain food allergens. The potential for REBYOTA to cause adverse reactions due to food allergens is unknown.
Adverse Reactions
The most commonly reported (≥3%) adverse reactions occurring in adults following a single dose of REBYOTA were abdominal pain (8.9%), diarrhea (7.2%), abdominal distention (3.9%), flatulence (3.3%), and nausea (3.3%).
Use in Specific Populations

Pediatric Use
Safety and efficacy of REBYOTA in patients below 18 years of age have not been established.
Geriatric Use
Of the 978 adults who received REBYOTA, 48.8% were 65 years of age and over (n=477), and 25.7% were 75 years of age and over (n=251). Data from clinical studies of REBYOTA are not sufficient to determine if adults 65 years of age and older respond differently than younger adults.
You are encouraged to report negative side effects of prescription drugs to FDA. Visit www.FDA.gov/medwatch, or call 1-800-332-1088.
Please see Brief Summary on next page and full Prescribing Information at www.REBYOTAHCP.com.
References
1. REBYOTA. Prescribing Information. Parsippany, NJ: Ferring Pharmaceuticals; 2022. 2. US Food and Drug Administration. FDA Approves First Fecal Microbiota Product. https:// www.fda.gov/news-events/pressannouncements/fda-approves-firstfecal-microbiota-product. Accessed December 1, 2022.
RESTORE HOPE
The first and only FDA-approved microbiota-based live biotherapeutic to prevent recurrence of C. difficile infection starting at first recurrence.1,2,a
Scan to visit website
Ferring and the Ferring Pharmaceuticals logo are registered trademarks of Ferring B.V. REBYOTA is a trademark of Ferring B.V. ©2022 Ferring B.V. All rights reserved. US-REB-2200129 1/23


























































































 by Tauseef Ali, MD, FACG (Author), David T. Rubin MD, FACG (Foreword)
by Tauseef Ali, MD, FACG (Author), David T. Rubin MD, FACG (Foreword)























































 Clinical Professor of Medicine, Wake Forest Medical University and Director of Motility, Division of Gastroenterology at Atrium Health, Charlotte, NC
Clinical Professor of Medicine, Wake Forest Medical University and Director of Motility, Division of Gastroenterology at Atrium Health, Charlotte, NC











 By Evaristus Sunday Chukwudike, MD
By Evaristus Sunday Chukwudike, MD