6 minute read
Sugar: The Link Between Poor Oral Health and Metabolic Disease
The following is a synopsis of the article “The connection between poor oral health and metabolic disease: the sugar link theory,” which appears in the May/June issue of General Dentistry. Read the full article here.
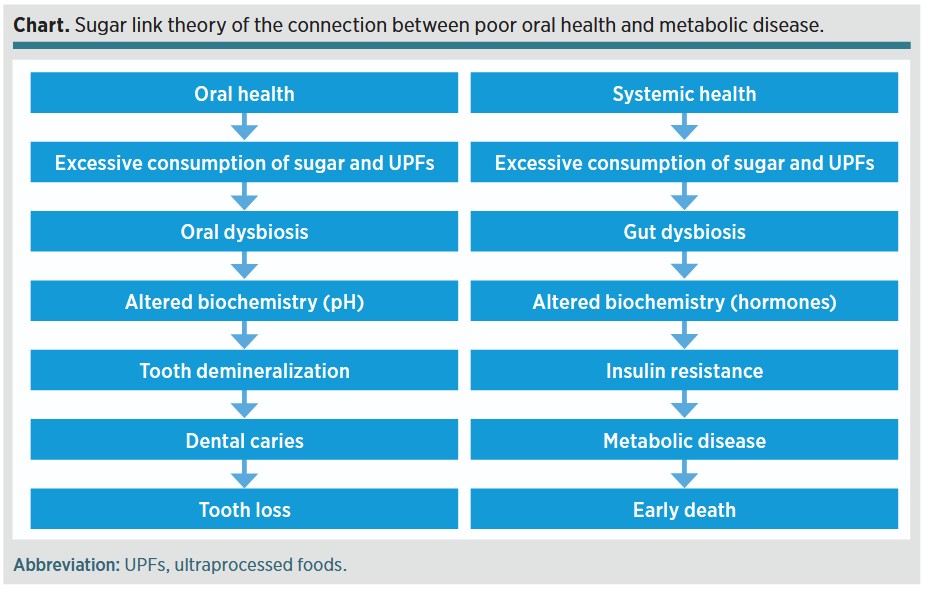
Periodontal disease and tooth loss have been reported to be good predictors of adverse cardiovascular outcomes, and early childhood caries and severe dental caries in adults are associated with obesity and a higher prevalence of metabolic disease.(1-3) While a correlation between poor oral health and metabolic disease has been reported, causality has not been established. The purpose of this narrative review by Dumbrigue is to explore the idea that excessive intake of sugar and ultraprocessed foods (UPFs) may be the link between poor oral health and metabolic disease.
Ultraprocessed Foods and Sugar
UPFs account for nearly 60% to 80% of the calories consumed in the American diet.(4) UPFs are described as items that are created with more than 5 ingredients, often including sugars, and retaining minimal intact food.(5) UPFs are designed to be overconsumed—they are hyperpalatable, nonsatiating, and addictive. Insoluble fiber has been removed, depriving the gut microbiome of food and increasing the absorption of sugar.
Sugar has a detrimental effect on both the oral and gut microbiomes. Sugar (sucrose) contains a single glucose molecule linked to a single fructose molecule. Glucose is essential for life, but dietary glucose is not. Glucose can bind to cellular proteins in vivo, accelerating aging and disrupting organ function.(6) Fructose, which never exists alone in nature, is metabolized in the liver like ethanol, causing nonalcoholic fatty liver disease and metabolic dysfunction.(7)
Decline in Oral Health
The oral microbiome is an assortment of microorganisms organized in an ecologic system that provides important benefits to the host. The oral microbiome efficiently metabolizes sugars into acids, but sugar-rich diets render dental biofilms cariogenic by lowering pH, leading to tooth demineralization.(8) If not interrupted, mineral loss progresses to carious lesion development. Untreated caries will undermine tooth structure, eventually resulting in tooth loss. Tooth loss impairs chewing, nutrition, quality of life, and, it turns out, life expectancy.(9)
Decline in Systemic Health
The gut microbiome is a complex collection of microbes that affect human nutrition, metabolism, physiology, and immune response. UPFs that are high in sugar and lacking in fiber alter the bacterial composition in the gut. Gut dysbiosis has been implicated in obesity, chronic gastrointestinal diseases, colorectal cancer, impaired neurocognitive function, chronic inflammation, hormone imbalance, and metabolic syndrome.(10-12).
Metabolic syndrome is defined as “a cluster of metabolic dysregulations,” including insulin resistance, central obesity, diabetes, hypertension, and cardiovascular disease.(13) The main driver of metabolic syndrome is insulin resistance, which occurs when the body is no longer able to respond appropriately to insulin, and excessive consumption of UPFs is one of the most common causes for the development of insulin resistance.(14) Cell dysfunction from chronically high insulin levels leads to metabolic disease, morbidity, and premature death.(15)
Discussion
The etiology and pathogenesis of dental caries and systemic metabolic disease are multifactorial and complex, as are the possible links between both conditions. The proposed sugar link theory between poor oral health and metabolic disease is intended to highlight the parallel downward declines in oral health and systemic health, with sugar and UPF consumption as a common upstream cause. The lack of dietary fiber in UPFs raises the likelihood for metabolic disease, and excessive consumption of sugar leads to metabolic disease both directly, via impaired regulation of carbohydrate and lipid metabolic processes, and indirectly, via increased adiposity.
Sugar and UPFs are ubiquitous in the current food environment. UPFs are delicious, cheap, and addictive, promoting the individual’s urge to consume them for pleasure even in the absence of physical hunger. Consumption of UPFs alters the oral and gut microbiomes to the detriment of the host. A solution to mitigate dental caries and metabolic disease is straightforward but difficult to accomplish: eat real food and avoid UPFs.(16) UPFs and sugary drinks should not be easily accessible at home, school, or the workplace. Instead, home-cooked meals using real food ingredients should be encouraged and promoted.
Summary
Consumption of sugar and UPFs leads to dysbiosis of the oral and gut microbiomes, altering biochemical processes, which in turn produces metabolic changes that damage oral and systemic health. UPFs kill slowly—eroding years from life, and life from years. Living to a ripe old age should not automatically require living with an implant-supported dentition or medication-controlled metabolic disease. Dentists should encourage their patients to avoid excessive consumption of sugar and UPFs and eat real food instead.
Read the full article here.
References
Lee HJ, Choi EK, Park JB, Han KD, Oh S. Tooth loss predicts myocardial infarction, heart failure, stroke, and death. J Dent Res. 2019;98(2):164-170. doi:10.1177/0022034518814829
Cao X, Wang D, Zhou J, Yuan H, Chen Z. Relationship between dental caries and metabolic syndrome among 13998 middle-aged urban Chinese. J Diabetes. 2016;9(4):378-385. doi:10.1111/1753-0407.12424
Sabella FM, Feiria SNB, Ribeiro AA, et al. Exploring the interplay between oral diseases, microbiome, and chronic diseases driven by metabolic dysfunction in childhood. Front Dent Med. 2021;2:718441. doi:10.3389/fdmed.2021.718441
Martínez Steele E, Baraldi LG, Louzada MLDC, Moubarac JC, Mozaffarian D, Monteiro CA. Ultra-processed foods and added sugars in the US diet: evidence from a nationally representative cross-sectional study. BMJ Open. 2016;6(3):e009892. doi:10.1136/bmjopen-2015-009892
Monteiro CA, Cannon G, Levy RB, et al. NOVA. The star shines bright. World Nutr. 2016;7(1-3):28-38.
Dills WL Jr. Protein fructosylation: fructose and the Maillard reaction. Am J Clin Nutr. 1993;58(5 Suppl):779S-787S. doi:10.1093/ajcn/58.5.779S
Jensen T, Abdelmalek MF, Sullivan S, et al. Fructose and sugar: a major mediator of non-alcoholic fatty liver disease. J Hepatol. 2018;68(5):1063-1075. doi:10.1016/j.jhep.2018.01.019
Takahashi N, Nyvad B. Caries ecology revisited: microbial dynamics and the caries process. Caries Res. 2008;42(6):409-418. doi:10.1159/000159604
Friedman PK, Lamster IB. Tooth loss as a predictor of shortened longevity: exploring the hypothesis. Periodontol 2000. 2016;72(1):142-152. doi:10.1111/prd.12128
Valdes AM, Walter J, Segal E, Spector TD. Role of the gut microbiota in nutrition and health. BMJ. 2018;361:k2179. doi:10.1136/bmj.k2179
Kawano Y, Edwards M, Huang Y, et al. Microbiota imbalance induced by dietary sugar disrupts immune-mediated protection from metabolic syndrome. Cell. 2022;185(19):3501-3519.e20. doi:10.1016/j.cell.2022.08.005
Satokari R. High intake of sugar and the balance between pro- and anti-inflammatory gut bacteria. Nutrients. 2020;12(5):1348. doi:10.3390/nu12051348
Fahed G, Aoun L, Zerdan MB, et al. Metabolic syndrome: updates on pathophysiology and management in 2021. Int J Mol Sci. 2022;23(2):786. doi:10.3390/ijms23020786
Lee GY, Lim JH, Joung H, Yoon D. Association between ultraprocessed food consumption and metabolic disorders in children and adolescents with obesity. Nutrients. 2024;16(20):3524. doi:10.3390/nu16203524
Janssen JAMJL. Hyperinsulinemia and its pivotal role in aging, obesity, type 2 diabetes, cardiovascular disease and cancer. Int J Mol Sci. 2021;22(15):7797. doi:10.3390/ijms22157797
Lustig RH. Metabolical: The Lure and the Lies of Processed Food, Nutrition, and Modern Medicine. Harper Collins; 2021:15-25.

