The State of Dental Medicaid Benefits
Caring for the Patient with PTSD
Leading by Example


Caring for the Patient with PTSD
Leading by Example

Even as some states expand Medicaid, the lack of providers is a major barrier to patients getting the dental care they need. To ensure low-income Americans have access to quality oral healthcare, AGD strongly recommends Medicaid changes that deliver greater benefits for patients and encourage more dentist participation. 14
Self-Instruction article, 1 CE credit
22
Celebrating AGD’s 2023 Fellows and Masters

AGD’s Fellowship and Mastership awards offer general dentists pathways to mastering the art and science of dentistry while also distinguishing themselves among their colleagues as the best of the best. AGD Impact spoke with several of this year’s award recipients about their individual journeys and why they chose to pursue these achievements.
While dental patients experiencing anxiety is common, with up to 75% of adults in the United States experiencing some degree of dental fear, those with post-traumatic stress disorder require a higher level of strategy and intervention from oral healthcare professionals.
Self-Instruction article, 1 CE credit
20 Exercise No. IM147, 1 CE Credit Practice Management and Human Relations
(Subject Code: 550)
29 Exercise No. IM148, 1 CE Credit Special Patient Care
(Subject Code: 750)
Some people view life events as a series of random episodes outside of our control. I, however, choose to view the many situations we face each day as opportunities for positivity. In dentistry, we are fortunate to have many daily opportunities available to us. Some of these can potentially advance our own careers, while others can advance the overall health of our patients.
Each day in my office begins with the morning opportunity meeting (MOM). During these 15 minutes, we have the opportunity to advance someone’s healthcare. We discuss the previous day’s patient encounters and see if any follow-up is necessary — or if any expectations were not met. If so, we’ll assign a team member to resolve any issues. This is an opportunity to show our patients we are devoted to their well-being. We review the day’s schedule to make sure it works and that there are no bottlenecks that would inconvenience patients. Also, we review whom to ask for referrals. (If you know me at all, you know my favorite three-letter word is “ask.”)
goals against what we actually produced and see other key data, including the day’s collection dollars.
We end our MOM with an inspirational story of positivity, which is an opportunity to show gratitude and a means to enlighten the team. Where would we be without our teams?
My team is rewarded well for our area, but it’s not the benefits that count. It is the opportunity to work in a safe environment that offers continual skill improvement. These skills serve the office and increase the team’s stature and ability to interact with people in the community. Talk about a win-win.
Often, when a negative life event or even a bad Google review occurs, you may feel pain, and it extends for an inordinate amount of time. This is the best time to search for an opportunity. We learn from both positive and negative comments, with each being an opportunity to advance our understanding to do better. When you experience a negative life event, reflect appropriately, and look for opportunities to make something good out of the event, whether it be a special remembrance or the opportunity to interact with other similarly affected people. Opportunities abound in family life. Reflect on the times you have made time to help a family member seek something positive. This can be as simple as helping your children make the right decision by listening and then giving your opinion when asked. How about attending a grandchild’s sporting event or even reading a bedtime story?
While it is certainly true that life events shape us into who we are, what we do with our life events in the form of turning them into opportunities is in our control. Don’t get so busy that you forget to take advantage of opportunities that come your way. Writing this Editor’s Note reminds me of the greatest opportunity of all — to interact with my like-minded colleagues to advance our profession and, equally important, to bolster the confidence of my AGD colleagues.
EDITOR
Timothy F. Kosinski, DDS, MAGD
ASSOCIATE EDITOR
Bruce L. Cassis, DDS, MAGD

DIRECTOR, COMMUNICATIONS
Kristin S. Gover, CAE
EXECUTIVE EDITOR
Tiffany Nicole Slade, MFA MANAGING EDITOR
Leland Humbertson, MA
ASSOCIATE EDITOR
Caitlin Davis
MANAGER, PRODUCTION/DESIGN


Tim Henney
GRAPHIC DESIGNERS
Robert Ajami Eric Grawe
Advertising
advertising@agd.org
Reprints scsreprints@sheridan.com
Academy of General Dentistry 560 W. Lake St., Sixth Floor Chicago, IL 60661-6600 agd.org
impact@agd.org
888.243.3368
312.335.3427 (fax)
DISCLAIMER: The Academy of General Dentistry does not necessarily endorse opinions or statements contained in essays or editorials published in AGD Impact. The publication of advertisements in AGD Impact does not indicate endorsement for products and services. AGD approval for continuing education courses or course sponsors will be clearly stated. AGD Impact (ISSN 0194-729X) is published monthly by the Academy of General Dentistry, 560 W. Lake St., Sixth Floor, Chicago, IL 60661-6600. Canadian Mailing Information: IPM Agreement number 40047941. Change of address or undeliverable copies should be sent to: Station A, P.O. Box 54, Windsor, Ontario, N9A 6J5, Canada. Email: impact@agd.org. Periodical postage paid at Chicago, IL and additional mailing office.
*AGD members receive AGD Impact as part of membership; annual subscription rates for nonmembers are $70 to individuals/$90 to institutions (orders to Canada, add $15). Online-only subscriptions available outside U.S./Canada are $75 to individuals/$115 to organizations. Single copy rates are $17.50 to individuals/$20 to institutions (orders to Canada, add $2.50). All orders must be prepaid in U.S. dollars.
POSTMASTER: Send address changes to AGD Impact, 560 W. Lake St., Sixth Floor, Chicago, IL 60661-6600. No portion of AGD Impact may be reproduced in any form without prior written permission from the AGD. Photocopying
Information: The Item-Fee Code for this publication indicates that authorization to photocopy items for internal or personal use is granted by the copyright holder for libraries and other users registered with the Copyright Clearance Center (CCC). The appropriate remittance of $3 per article/10¢ per page is paid directly to the CCC, Inc., 222 Rosewood Drive, Danvers, MA 01923, USA. The copyright owner’s consent does not extend to copying for general distribution, for promotion, for creating new works, or for re-sale. Specific written permission must be obtained from the publisher for such copying. The Item-Fee Code for this publication is 0194-729X.
Printed in U.S.A. © Copyright 2023, Academy of General Dentistry, Chicago, IL.
Next, we look at our most important key performance indicator — production per hour. It is an opportunity to measure our
Bruce L. Cassis, DDS, MAGD Associate Editor
”
“When you experience a negative life event, reflect appropriately, and look for opportunities to make something good out of the event, whether it be a special remembrance or the opportunity to interact with other similarly affected people.
Look for the following article in the July/August 2023 issue of AGD’s peer-reviewed journal, General Dentistry.
This in vitro study aimed to evaluate the acidity and fluoride content of beverages commonly consumed by millennials and the enamelsoftening effect of these drinks on tooth enamel. The study included 13 beverages in 4 categories: energy (sports) drink, flavored sparkling water, kombucha, and other (an unsweetened iced tea, a vegetablefruit juice blend, and a soft drink). The acidity was measured with a pH/ion meter, and the fluoride concentration was measured with a combined fluoride electrode coupled to the meter (n = 10 measurements per beverage). The Vickers hardness number of extracted molars was measured before and after a 30-minute immersion in 4 representative beverages via 2 immersion protocols (n = 10 per beverage per protocol): (1) immersion in the beverage only and (2) immersion alternating between the beverage and artificial saliva every other minute. The pH and fluoride concentrations of the beverages ranged from 2.652 to 4.242 and from 0.0033 to 0.6045 ppm, respectively. One-way analysis of variance (ANOVA) revealed that all differences between beverages in pH values were statistically significant, as were the majority of differences in fluoride concentrations (P < 0.001). The beverages and the 2 immersion methods significantly affected enamel softening (2-way ANOVA, P = 0.0001 to 0.033). The
representative energy drink (pH 2.990; 0.0102 ppm fluoride) caused the greatest enamel softening followed by the representative kombucha (pH 2.820; 0.2036 ppm fluoride). The representative flavored sparkling water (pH 4.066; 0.0098 ppm fluoride) caused significantly less enamel softening than the energy drink and kombucha. A root beer (pH 4.185; 0.6045 ppm fluoride) had the least enamel-softening effect. All tested beverages were acidic and had a pH below 4.5; only some contained fluoride. Flavored sparkling water, likely due to its higher pH, caused less enamel softening than the tested energy drink and kombucha. The fluoride content of kombucha and root beer may lower their enamel-softening effects. It is imperative that consumers be aware of the erosive potential of beverages they consume.
To view past issues, visit agd.org/generaldentistry.
The Daily Grind
AGD’s blog, “The Daily Grind,” offers insight and reflections from dental students and general dentists. Read the beginning of “Balance and Good Health” by AGD Editor Timothy F. Kosinski, DDS, MAGD:
Challenges appear each day. Often, we exaggerate the drama at the moment, whether it be a staff member missing work, a difficult treatment schedule, unruly patients or even a bad test score from one of our children. While each of these situations may be deemed important at the time, the negative energy soon fades, and we move on with life. Health is so important to all of us, but putting family and friends first must be primary.
Visit “The Daily Grind” to read the rest, and also check out the “Moments of Magic” series by Larry Stanleigh, BSc, MSc, DDS, FAGD, FADI, FICD, FACD, FPFA: agd.org/daily-grind
AGD fact sheets provide your patients with all of the information they need to maintain their oral health. Fact sheets on more than 25 oral health topics are available for downloading online and can be customized to include your name and practice information. Download the fact sheet “What to Know About Xerostomia” at agd.org/factsheets
AGD’s Half-Year Dues membership promotion kicks off July 1. This promotion allows dentists who join AGD between July 1 and Sept. 30, 2023, to pay only half the cost of national dues. How does referring colleagues help you? When a referred colleague joins AGD, both the recruit and member who referred them get $50
in AGD Referral Rewards that can be applied toward next year’s membership renewal. There’s no limit to the number of awards that can be earned, so you can spread the word to your fellow dentists looking to save on membership. To qualify, recruits cannot have a membership that expired on Dec. 31, 2022, or be residents or new dentists who graduated in 2022 or 2023.
The Association of Army Dentistry (AAD) dedicated the Army Dentistry Monument on Friday, March 24, 2023, in a ceremony attended by over 300 people at the U.S. Army Medical Department (AMEDD) Museum in San Antonio, Texas. According to retired Col. Ronald Lambert, DDS, MAGD, ABGD (past president of the AAD), “The monument is a lasting tribute to all the soldiers, civilians and spouses who have served and continue to serve in the Army dental care system in support of the U.S. Army and its military mission. The monument recognizes and honors the selfless contributions made by the diverse members of the Army dental care system and its key supporting components in the overall mission of Army medicine.”
about the rich history and important legacy of Army dentistry,” said retired Maj. Gen. M. Ted Wong, DDS, 26th chief of the Army Dental Corps and president of the AAD.
The dedication of the monument marks the culmination of six years of designing, constructing, fundraising, and overcoming mountains of administrative and logistical hurdles. Funding for the design, construction and dedication of the monument came exclusively from private individual and corporate donations secured through the fundraising efforts of the AAD, a nonprofit organization committed to preserving the legacy of Army dentistry. Thanks to donors like the Tennessee AGD, the monument now stands as a permanent reminder of the significant contributions made by those
The monument is composed of three bronze figures partially surrounded by nine granite monoliths. The bronze sculpture depicts a dental officer, dental assistant and patient in a field setting, highlighting the primary mission of Army dentistry — caring for soldiers in any location, at any time. The bronze sculptures are the creations of artisans Stan Watts and Tami Brooks of Atlas Bronze in Kearns, Utah, using an initial design sketched by illustrator Jorden Pao. The individual granite monoliths recognize the various components and aspects of Army dentistry: non-commissioned officers (NCOs) and enlisted soldiers; civilians, spouses and volunteers; dental laboratory services; dental research; education and training; leadership; and U.S. Army dental history. The name plates and the likenesses of the three bronze figures honor the diversity of key personnel that are represented in Army dentistry: the father of Army dentistry, Dr. John S. Marshall; the only Army dentistry Medal of Honor recipient, Capt. Ben Salomon; and African American and female pioneers, Drs. William Birch and Leonie von Zasch, respectively.

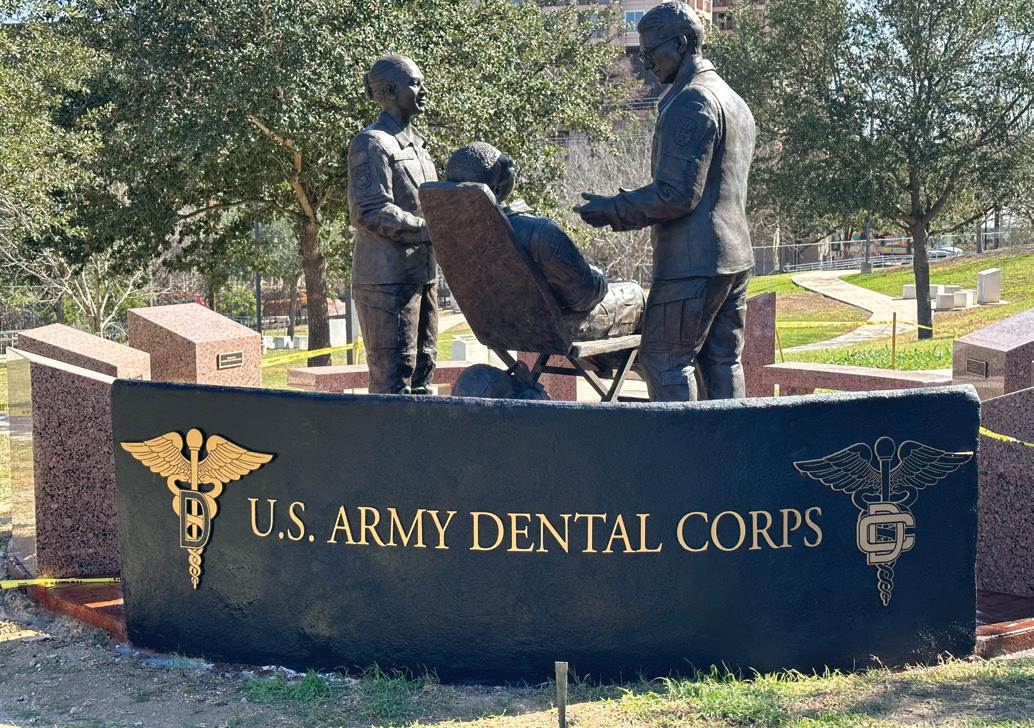
“With the Army Dentistry Monument finally in place, we can more effectively highlight the achievements of, and pay homage to, the multitudes of men and women in the Army dental care system, past, present and future; and inspire visitors to learn more
in uniform and by the dental profession to the Army mission. It was fitting that Lt. Col. James M. Giesen, DDS, FAGD, ABGD, president of the Army constituency, and Lt. Col. Michael A. Hoffman, DDS, FAGD, ABGD, president-elect of the Army constituency, were in attendance representing military service and AGD. Giesen commented, “Attending the Army Dentistry Monument dedication ceremony was like attending a family reunion. It was amazing to come together to celebrate the 112 years of contributions of Army dentistry with active-duty and retired colleagues, our civilian teammates, family members and friends. The monument allows us to revere our history while inspiring us all for the future.”
Founded in March 1911, the Army Dental Corps has a long and distinguished history of providing global dental services to soldiers and ensuring the readiness of the nation’s fighting forces. Even before 1911, the Army contracted dental surgeons to provide dental care to soldiers deployed to the new territories of a growing nation. Since then, Army dentistry has supported the nation’s operational missions, including World War I; World War II; the Korean Conflict; the Vietnam War; operations Desert Shield/Storm, Enduring Freedom and Iraqi Freedom; as well as innumerable humanitarian and training missions. This tradition of providing oral health services to soldiers wherever they are
assigned continues to this day. “The Army Dental Corps is the leader in expeditionary dentistry and sustainment of force readiness. Our Corps’ mission is to have a ready Dental Corps capable of delivering global dental services anytime, anywhere in order to sustain the readiness of the total military force,” said Col. Stephen J. Tanner, DDS, ABGD, chief of the Army Dental Corps.
Some of the skills and competencies to build a ready Dental Corps come from partnership with professional organizations like AGD. According to Hoffman, “Organized dentistry is incredibly important in setting the conditions for military dentists to have success in all phases of their careers.” Army
dentistry has a long history of participation in AGD. The Army constituency — as well as all of Region 17 — steadfastly supports the mission of AGD to advance oral health through quality continuing education. Army constituents actively participate in the governance and committees of AGD and contribute directly to helping AGD achieve its goals and objectives. The educational benefits and awards provided by AGD enhance the professional skills and knowledge of Army constituents, which in turn benefit the mission of Army medicine. This strong relationship between military service and the profession is immortalized in the Army Dentistry Monument.
The Code Maintenance Committee (CMC), a committee of the American Dental Association’s (ADA’s) Council on Dental Benefit Programs (CDBP), met March 9 at ADA Headquarters in Chicago to discuss and vote on proposed changes to the Code on Dental Procedures and Nomenclature (CDT Code).
The CMC’s purview is CDT Code technical content. The group is responsible for maintaining the CDT Code to ensure that it accurately reflects the current practice of dentistry. The CDBP established the CMC and has delegated decision-making authority to the committee. Decisions under the CMC’s purview concern addition of new nomenclatures and descriptors, revision to existing nomenclatures or descriptors, and deletion of full CDT Code entries (nomenclature and descriptor or descriptor only). This technical content will be included in the manual, “CDT 2024 Current Dental Terminology,” which is published by the ADA and also contains other content maintained by ADA staff.
The CMC includes 19 member organizations that have a total of 23 votes among them:
• 5 votes: ADA.
• 1 vote: AGD.
• 11 votes: one for each of the ADA-recognized dental specialty organizations.
• 1 vote: the American Dental Education Association.
• 5 votes: dental benefits (third-party) payer organizations, including the Centers for Medicare & Medicaid Services.
AGD represents the interests of the general dentist in deliberating what coding changes will occur each year, and its efforts are directed by AGD’s Dental Practice Council (DPC).
Two AGD leaders participate in the CMC: Ralph A. Cooley, DDS, FAGD, of the AGD Legislative & Governmental Affairs Council, is AGD’s delegate and voting member to the CMC; and Arlene O’Brien, DMD, FAGD, of the DPC, is AGD’s alternate to the CMC. Both representatives review each suggested code change and offer independent recommendations. The DPC reviews the information and advises how to vote on each proposed change.
This year, the CMC had 31 code submissions to review. One was withdrawn prior to the meeting. During the meeting, the committee approved 14 new codes and revised two codes by adding a descriptor to one and changing nomenclature and descriptor for another.
The American College of Prosthodontists submitted a new code to report when excavation of a tooth is done to determine nonrestorability of the tooth.
The CDBP put forth a new code to report the fabrication of a custom removable clear plastic temporary esthetic appliance, and an additional code was created for the placement of the appliance. Currently, when this procedure is done, it is usually coded with a “by report” code.
The American Academy of Dental Sleep Medicine put forth numerous new codes, including at-home sleep apnea test administration and screening for sleep-related disorders. Additionally, two codes related to oral appliance therapy were approved. One reports a titration visit of the appliance, and the other relates to the fabrication and delivery of a morning reposition device.
Has this happened in your practice? A patient presents with a loose implant crown, and you need to remove material to access the screw, retorque it, and then replace the access material. Any general dentist who has performed this procedure recognizes that it’s not the same procedure as recementing a crown.
Last year, the DPC identified this gap in the current CDT Code and determined that having a CDT Code to report this procedure would benefit general dentists. The DPC collaborated to develop the official code request submission for Retorquing implant screw
per screw and submitted the request to the CMC in October 2022. See “AGD Submits Request for New CDT Code” in the January 2023 issue of AGD Impact for more information.
During the March 9, 2023, CMC meeting, Cooley and O’Brien worked with voting members of the CMC to modify the proposed code’s nomenclature to allow for a successful outcome. Thanks to a broad collaborative effort involving the DPC, AGD’s representatives to the CMC, and voting members of the CMC, the 2024 CDT Code will include a new AGD-sponsored code for Accessing and retorquing implant loose implant screw – per screw
AGD members who identify what they believe are gaps in the CDT Code and who would like AGD to consider sponsoring a request to add or modify the CDT Code on their behalf are encouraged to share that information with the DPC via email to practice.management@agd.org. Members are encouraged to review the ADA website (ada.org) for information about the “CMC Process Document” and “Request a Change to the Code” to ensure they’re providing the necessary information in their initial request to the DPC.

Update on the Work of the ADA’s Enhanced Code Task Force AGD has been closely following the work of the ADA Enhanced CDT Task Force, which was appointed to look at the current coding mechanism and offer changes for consideration by the CDBP. This task force recently concluded an open comment period from Nov. 7, 2022, through March 31, 2023, to gather feedback on examples of a framework for an Enhanced CDT Code. Seven public listening sessions were held during this time. AGD participated in several sessions, and the DPC offered recommendations to AGD President Hans P. Guter, DDS, FAGD, who submitted an official letter to the task force stating AGD’s position and its interests in being the voice of the general dentist in the process. The March 30, 2023, letter can be found at the AGD Advocacy Center under “2023 Activities” (agd.org/advocacy).
The CDT Code’s current architecture has not changed. All comments received will aid the CDBP in determining how the CDT Code should best serve procedure documentation and reporting needs of dentists and the entire dental community in future years. AGD will continue to monitor this closely.
2023 AGD Senior Student Dental Award Winners
AGD is proud to present the 2023 Senior Student Dental Award (SSDA) winners. These senior students throughout the United States and Canada have been recognized by their faculty for maintaining an academic scholastic balance between clinical and didactic basis
courses of study and exhibiting the potential to become outstanding general dentists. Recipients are awarded a complimentary one-year AGD membership and a certificate presented by their dental school’s dean. View the full list of this year’s SSDA winners at agd.org/SSDA.

When I reflect upon my journey in this profession over the last decade, the most fulfilling moments are always the ones that I have spent giving back. Being able to serve others is undoubtedly one of the best abilities we have as dentists. The trait that unites us all is that we prioritize paying our good fortunes forward and using our skills to help others in as many ways as possible. There are a multitude of ways to give back. Some involve helping those in need, and some involve helping the next generation of dentists.
Dental care can be costly. As a result, many people in our communities do not make oral health a priority. Dental insurance is a benefit that has been offered to employees in larger corporations, but it has remained largely unchanged in terms of annual maximums and types of covered procedures since its inception in the 1970s. Even today, a single complex procedure can cause a patient to use all their benefits for an entire calendar year, thus making even preventive visits unaffordable. As a newer graduate, I have seen the impact that this can have personally, professionally and emotionally. Opportunities to give care without staggering costs often fill a gap in the healthcare system and help people who might not have received care otherwise.
I have taken part in volunteer and mission-based work both in the United States and across the world. The first lesson I learned was that charity does not have to exist on a large or grand scale to make a difference. April is Oral Cancer Awareness Month, and the oral cancer walks that I did as a dental student through the streets of Harlem, with survivors and fundraisers walking with us, were my first exposure to this. I have since attended and participated in several community-based oral cancer screening events and am gratified to see that many of them occur in conjunction with health fairs, where attendance is already high. Many of the people I saw had never seen a dentist, and I am confident that the suspicious lesions we noted and referred for examination and treatment would otherwise never have been caught.
I had my first experience with a Mission of Mercy event in Colorado in 2019, where I saw a large school auditorium transformed into a comprehensive dental treatment facility. So many patients needed care that the lines often began in the early morning and stretched around the building. The days we worked were long, and I lost count of the number of people we treated, but it remains to this day one of the best experiences of my dental
career. There are several such programs around the country. National Children’s Dental Health Month occurs in February and corresponds with Give Kids a Smile programs in most states. Even third- and fourth-year dental students can help provide screenings and preventive visits in coordination with local dentists and faculty members. Many of the children I see at such events are at high risk for caries and have no dental homes. The treatments and interventions they receive are the first step toward setting them up for success in their journeys of lifelong oral health. If any of these programs are something that you are interested in, a great place to start is your local dental school or community health clinic.

As an educator, I can confidently say that the interactions I have had with students are some of the more impactful ones I can remember. Academia can be a tough world to navigate, especially for a newcomer like me. There is a definite shortage of instructors and faculty members at predoctoral programs and residency training facilities in most states. Many of these appointments are on a volunteer basis and will allow you to teach for just an afternoon a week in the clinic. If I had to choose an activity in dentistry that I enjoy the most outside of clinical practice, teaching would be it. As technology and methods change, reviewing basic principles and the reasons why our dental systems work the way they do is the best part of my week. As I do this, I find myself remembering lessons from my dental school days (including an instructor who always told us that we make — not take — impressions on patients). Integrating those lessons into the way I teach patient care has enabled me to provide the best educational experiences for my students — and the best care for their patients.
Your skills and your experiences can help a person live a longer and healthier life. There are so many opportunities to give back, and some could be right in your community. Dental schools, charitable drives, national campaigns and hospitals — these are all places where your time is well spent. It is my hope that the next generation of dentists continues to see the good in caring for others in this way. F

This column is a collaboration between AGD and the American College of Dentists.

Since 2001, I have had the honor of being a dental educator with the responsibility of training future dentists. Currently, my time is predominantly spent teaching restorative dentistry preclinically, but I have always had an interest in dental ethics, specifically the American Dental Association (ADA) Principles of Ethics and Code of Professional Conduct. The ADA states: “These high ethical standards should be adopted and practiced throughout the dental school educational process and subsequent professional career.”1 Correspondingly, I believe learning and practicing these principles begins on the first day of dental school — well before entering the clinic.
The five principles that form the code are patient autonomy, nonmaleficence, beneficence, justice and veracity. Although the ADA describes these standards clinically and with a patientoriented perspective, I will discuss elements of these standards from a preclinical perspective. Specifically, I help students learn to adopt and practice these principles from the start of their dental educations. I will focus on the principles of nonmaleficence, beneficence and justice through the unique lens of my role as a preclinical educator, including some of the ways in which I try to model these standards through my approach to teaching.
The principle of nonmaleficence describes the primary obligations of the dentist to include “keeping knowledge and skills current” and “knowing one’s own limitations.”1 Modeling this principle could include seeking to learn about innovations in dental practice and dental education, collaborating with colleagues, and maintaining self-awareness of one’s limitations. For example, I complete required monthly departmental continuing education (CE) on clinical topics and attend CE through my dental school’s CE department. I am an active member of the Consortium of Operative Dentistry Educators, through which I learn what is taught at other dental schools and discuss ideas. In addition, I communicate with clinic faculty to help ensure consistency with what is taught preclinically. Sharing information with each other helps bring the principle of nonmaleficence into practice.
“Knowing yourself is the beginning of all wisdom” is a statement commonly attributed to the philosopher Aristotle. When I am seeking the answer to a question or the best way to approach a topic, I start by researching the answer on my own. Subsequently, I may consult with one or more of my knowledgeable colleagues. Asking someone a question when I do not know the answer, sometimes in front of students and colleagues, models an honest acknowledgment of my limitations. Specifically, this behavior shows that it is OK (even ideal) to admit when you do not know something and then act to find the answer.
The Commission on Dental Accreditation’s accreditation standard 2-11 requires graduating dentists to be able to selfassess, and it offers examples of ways students can demonstrate this, including to “routinely assess their own progress toward overall competency and individual competencies as they progress through the curriculum” and to “identify learning needs and create personal learning plans.”2 In the laboratory courses I teach, students are offered numerous opportunities for self-assessment through daily work and laboratory exam rubrics. Students are invited to discuss their daily work or post-exam attainment of rubric guidelines with faculty. Accordingly, they are encouraged to identify patterns of areas for improvement, develop a strategy to achieve their goals and plan how to practice. Beginning this process and establishing it as a routine habit early in their dental education helps promote a culture of “do no harm.”1
The next principle, beneficence, or doing good, “expresses the concept that professionals have a duty to act for the benefit of others.”1 Moreover, the “most important aspect of this obligation,” as stated by the ADA, “is the competent and timely delivery of
dental care within the bounds of clinical circumstances presented by the patient, with due consideration being given to the needs, desires and values of the patient.”1 My dental school’s technical standards emphasize this as well: “A student must always act in the best interest of the patient and society even when there is a conflict with the student’s personal self-interest,” and “[t]reatment must be completed safely and within an acceptable time.”3 In the preclinical setting, I help students adopt these qualities by teaching indications and contraindications of procedures, reinforcing what is taught regarding material selection, enforcing proper infection control protocol from the very beginning to create lifelong habits, and holding one accountable to due dates and timed exams.
Also falling under the umbrella of beneficence is professional demeanor in the workplace, and that “[d]entists have the obligation to provide a workplace environment that supports respectful and collaborative relationships for all those involved in oral health care.”1 In a study by Nazir et al., “dental students considered the provision of learning resources and the demonstration of honesty/ integrity and respectful/caring attitudes as the most important attributes of effective instructors.”4 Respecting each other’s time, listening to one’s concerns — whether it be through electronic communication, in-person meetings, student evaluations or peer reviews — and making changes for the better wherever possible are good behaviors for faculty to model.
The last principle I will touch upon is justice, also described as “fairness.”1 “The dentist has a duty to treat people fairly. This principle expresses the concept that professionals have a duty to be fair in their dealings with patients, colleagues and society.”1 Application of this principle in the preclinical laboratory setting includes, in part, making sure all of us faculty members are calibrated in our assessments of student work and ensuring that students who need additional help will have it made available through tutoring as well as laboratory help sessions. It means answering the questions, “Is it true, and is it fair?” through my actions. This principle brings to mind what my former dental school roommate said to me when I told her that I was to begin a career as a dental school faculty — “Just be fair, Mary.” I sincerely hope I have, and I hope to continue to do so in my own small way, in my own corner of the world. F
Mary A. Baechle, DDS, is an associate professor in the Department of General Practice at the Virginia Commonwealth University School of Dentistry. To comment on this article, email impact@agd.org.
1. “Principles of Ethics and Code of Professional Conduct.” Council on Ethics, Bylaws and Judicial Affairs, American Dental Association, 2023, ada.org/about/principles/code-of-ethics.
2. “Accreditation Standards for Dental Education Programs.” Commission on Dental Accreditation, 2022, coda.ada.org/standards.
3 School of Dentistry Technical Standards for Dental Education Programs. Virginia Commonwealth University School of Dentistry, 2007.
4. Nazir, M.A., Al-Ansari, A., and Farooqi, F.A. “An Investigation of Dental Students’ Perceptions About the Characteristics of Effective Instructors and Their Related Factors.” European Journal of Dental Education, 2019, vol. 23, pp. 286-294.

When it comes to informed consent, healthcare providers invariably want magic words. What phrase in a consent form will both satisfy the obligation to receive informed consent from the patient and ensure the patient will not bring legal action if they are unhappy with the results of the procedure?
I have good news and bad news. There are no magic words. There are no guarantees that a patient won’t sue a healthcare provider if they are unhappy with the result of the procedure. But, luckily, you can reduce liability risk in the doctor-patient relationship simply by deciding how the dental care will proceed together.
Informed consent is more than just a form to sign. It’s a collaboration between the patient and healthcare provider. As a dentist, you must disclose all necessary information, but you must also ensure that what you have disclosed has been understood by the patient. It is this understanding that creates valid informed consent .
At the heart of informed consent is the belief that every adult of sound mind has the right to bodily autonomy. The legal requirement to obtain informed consent from a patient prior to a medical procedure originated in common law in the criminal law of battery — unwanted touching. Healthcare practitioners were charged with battery when a medical procedure was performed without the patient’s consent. Gradually, informed consent became shaped by the civil law of negligence. From there, the elements of effective informed consent were established.
In a seminal case, the court stated the following definition: “True consent to what happens to one’s self is the informed exercise of a choice, and that entails an opportunity to evaluate knowledgeably the options available and the risks attendant upon each.”1 Today, obtaining valid informed consent is also a process of shared decision-making. 2
It should be well known that for consent to dental treatment, the dentist must:
1. Disclose the dental diagnosis to the patient.
2. Inform the patient of the options for treatment (including the option not to treat).
3. Describe to the patient all risks and benefits of each treatment option.
However, for the consent to be truly informed and effective, the dentist must also confirm that the patient understands all risks and benefits of each of the treatment options. It is in this process that the dentist and patient agree upon the procedure to be performed. The process must be thoroughly documented in writing, and a consent must be signed by the patient.3 The signed consent alone does not document valid informed consent, so the discussion itself should be documented in the dentist’s notes.
Here are some simple steps to follow — and document — that will both assure valid informed consent and that can be used as evidence valid informed consent has been obtained:

• Ask patients to repeat what they heard. Many patients will be uncomfortable asking questions or admitting they didn’t fully comprehend what was said. If the patient can explain what they’ve heard, it’s important evidence that the patient did understand what you said.
• Use procedure-specific consent forms. Be sure the consent form names the diagnosis and the procedure and that the risks of the procedure are included. This serves as a reminder to the patient that, while you may have discussed many things, this is the specific course of action you have agreed upon together.
• Keep narrative notes describing the informed consent process and the goals of care in the patient file. In the absence of filming the exchange, this is the best way to show the elements were met.
• Create decision aids for particularly complex decisions. Patients may need a visual guide to remember how the risks and benefits fit together with a procedure choice and diagnosis. Does obtaining valid informed consent take more time than having an assistant obtain a patient signature on a consent form? Yes, it does. However:
“Time cannot and must not be shorted, as adjuncts such as pamphlets and videos are helpful, but cannot replace a physician taking time with a patient. All true relationships are timedependent. Meaningful shared decisions require time and that time will result in better clinical decisions/outcomes and less potential for liability.”4
Certainly, there will be some patients who do not want to participate in this process. If, after explaining the importance of shared decision-making, the patient does not want to engage in the process, document this in the patient record.
How does shared decision-making reduce the risk of litigation? Very little research has been done on informed consent in dentistry, but the masterful analysis of existing studies by Kevin I. Reid, DMD, MS, MA, 5 concludes in part that:
“Infractions that were emotional and intelligence-related comprised nearly 57% of all disciplinary actions taken by 21 state dental boards. The most frequently observed violation among the four clusters of emotional intelligence-related studied was that of ‘Transparency,’ which refers to maintaining integrity and acting congruently with one’s values. Dentist transparency is perhaps one of the most beneficial virtues in the informed consent process, along with humility, veracity, and compassion.”5
In litigation and in dental board prosecutions, the burden is always on the dentist to prove the patient’s signature was a voluntary choice free of undue influence. It’s also the responsibility of the dentist to show the patient understood the information given by the dentist. Well-documented shared decision-making is the best evidence of valid informed consent and most likely to create a secure patient relationship. The “magic words” are the conversation. F
J. Kathleen Marcus, JD, is compliance regulatory counsel at Everside Health. Formerly general counsel at Strategic Dentistry, she has been a regulatory lawyer concentrating in healthcare for 35 years. To comment on this article, email impact@agd.org.
1. United States Court of Appeals for the District of Columbia Circuit. Canterbury v. Spence, 464 F.2d 772, 1972.
2. Childress, James F., and Marcia Day Childress. “What Does the Evolution From Informed Consent to Shared Decision Making Teach Us About Authority in Health Care?” AMA Journal of Ethics, May 2020, vol. 22, no. 5, pp. E423-E429.
3. Hall, Daniel E., et al. “Informed Consent for Clinical Treatment.” Canadian Medical Association Journal, 2012, vol. 184, no. 5, p. 537.
4. Paterick, Zachary R. “Medical Informed Choice: Understanding the Element of Time to Meet the Standard of Care for Valid Informed Consent.” Postgraduate Medical Journal, 2020, vol. 96, no. 1141, pp. 708-710.
5. Reid, Kevin I. “Informed Consent in Dentistry.” American Society of Law, Medicine & Ethics, 2017, vol. 45, no. 1, pp. 77-94.
Of all the available digital marketing options, which one is the most effective, the most pervasive and the most important? It’s a trick question. Here’s the real question: Is it possible to achieve all of your dental practice’s marketing goals with a single digital marketing channel?

Let’s imagine a scenario where a dental practice is relying on a single digital marketing channel and basically ignoring all the others. What would that look like? It’s actually not hard to imagine because most dental practices that do not utilize a professional marketing agency do exactly that. They usually have a website and not much more, which means that website is being asked to do a lot of heavy lifting, and it’s probably not up for the challenge.
A website is a fundamental digital marketing tool, to be clear. However, if it is your practice’s only one, and especially if it’s not being professionally managed and updated with current information and new content on a regular basis, there is no way it will ever meet all your marketing needs. The same holds true for any digital marketing channel. No matter which marketing channel you choose for your practice, you will always be leaving something on the table. Let’s break it down:
Website. A well-designed, modern website is an excellent starting point. It lays the foundation for your practice’s brand and image and often serves as the point of first contact. It’s also a great place for prospective and existing patients to find basic information about your practice. If actively managed, your practice’s website can stay fresh and relevant with updated information, photos and even videos. However, what a website doesn’t do is actively find people who are interested in your practice. Patients have to search to find it, and there is no guarantee that your website will be seen by anyone, let alone the types of people your practice is looking to attract as patients.
Social media. It’s a hot topic, and anyone who’s anyone is on social media. Using social media is an
excellent way to actively engage existing patients, their friends and their family members, as well as prospective patients who use the same platform. Social media is extremely flexible. You can use it to convey important information, be a little playful, ask questions and show off your successes. You can post as much or as little as you want and be as creative as you like. Where social media falls short, however, is just that — it’s short. The format of most social media platforms is designed to provide information in short bursts, so you have to be very choosy with what you post, and there is no way to really put it all out there in one easy-to-access place (like a website), so there will always be important pieces missing.
Blog. I love blogs because they are great for building a stronger online presence. If you want to take a deeper dive into a specific topic, a blog post is the perfect platform. You can really get into the details and show your target audience that you know your stuff. Having a blog gives your practice instant authority, and a blog is good for adding fresh content to your website on a regular basis, helping the search engines rank your website organically. You can also link to your blog from every other marketing channel. If your practice were to only have a blog, then your patients would have no way to learn the basics about your practice. Even if an enterprising person decided to read every blog your practice ever published, there would still be huge information gaps. Additionally, much like a website, there is no guarantee that anyone will actually see your blog unless you advertise it somehow.
Online business listing. Having an online presence is essential, and an online business listing is the most basic way to accomplish that. With an online business listing, such as a Google My Business listing, when someone in your market area searches for a dentist online, your listing will be included in the search results. Will it be near the top? Perhaps, but maybe not. An online business listing will have very limited information about your practice, so, of course, it cannot convey the full scope of the services you offer. Nor can it adequately show your practice’s personality. Additionally, if you do not stay on top of your online listing, the information can become outdated rather quickly, such as if you make changes to your practice’s hours of operation, contact information, etc. Obviously, an online business listing is important, but it’s really the minimum you can do to establish your practice’s online presence.
Reviews. I think it’s safe to say that everyone looks at reviews when scoping out a new business. Online reviews for healthcare professionals are becoming increasingly important to their marketing. Good reviews inspire confidence.

However, like many of the other digital channels, reviews alone cannot carry your practice. They certainly help to reinforce your other marketing efforts and can even be the deciding factor for some people, but reviews can never include all the information about your practice a person needs to make a truly informed decision.

Emails to existing patients. I am a huge fan of email. It’s one of the best ways to engage your patient base. A lot of practices are so keen to build revenue through new patients that they neglect the ones they already have. Existing patients are a major source of new business and referrals, and emailing them monthly or even quarterly lets them know you haven’t forgotten about them. Like blogs, emails are great for diving deeper into certain topics, but they are also useful if you want to highlight a specific product or treatment, advertise a special event, offer something new or send a reminder about unaccepted treatment. Like blogs, emails cannot be the only digital channel your practice uses, because an email can never contain enough information to market your practice effectively. Plus, it’s nearly impossible to send your emails to enough people so that you can rely solely on them as your main marketing strategy.
Google Ads. Advertising online is key, and Google Ads makes that relatively easy. Google Ads is a primary driver of new patients who are interested in your practice. If your practice uses Google Ads, it will be prioritized in relevant search results. Google Ads offers flexibility when it comes to expenditure and complexity. There is a Google Ads option to suit any practice. That said, Google Ads alone will not give you the new patient results you want. It’s just one piece of the puzzle.
It may be obvious already, but there is no single online marketing channel that can do it all for your practice. They are all essential if you really consider what each one offers. Fortunately, all the digital marketing channels work well together and play off each other to create and grow your practice’s online presence.
Ideally, you should take advantage of every digital marketing channel you possibly can. However, if you’re not quite ready to do that, start with two channels and make a concrete plan to add more over time. If you stick to your plan, your practice will have a strong, established, engaging online presence and be a digital marketing machine. F
When W. Mark Donald, DMD, MAGD, an AGD past president (2015–16), was in dental school, his philosophy for treating patients came into focus.
“My mission was to help as many people as I could during my career,” Donald said. “I also had a desire to practice in a rural town in Mississippi.”
Donald elected to go back to his hometown and open a solo private practice, which he still runs today in Louisville, Mississippi.
“I studied the demographic, and it was clear that I would be a Medicaid provider,” he said. “Current statistics show that 772,200 Mississippians are Medicaid recipients. In Mississippi, 477,284 children are either on Medicaid or CHIP [Children’s Health Insurance Program]. I saw this as a group of people who needed the treatment I could offer.”
Although accepting Medicaid patients fit his mission, Donald had to accept reimbursement rates at about 40% of his normal fees. He compensated for the reduced rates by increasing volume.
“Many times, I can do multiple procedures in one visit, which makes up for the low reimbursement rates,” Donald said. “Over the years, I have found that parents appreciate it when I can complete much of the child’s treatment in one or two visits. That means fewer missed school days for the child and less time for the parents to spend bringing their child to the office for treatment.”
Donald is in the minority as a Medicaid dentist — only 39% of dentists in the United States accept Medicaid and/or CHIP patients. The ability to use your skills to improve the health of those less fortunate is one that Medicaid, in theory, supports. But dental providers have struggled with the program. Low reimbursement rates, tedious administrative requirements, a trend in no-show appointments and long payment delays have disincentivized dentists from participating in the program.1
Even as some states expand Medicaid, the lack of providers is a major barrier to patients getting the dental care they need. To ensure low-income Americans have access to quality oral
healthcare, AGD strongly recommends Medicaid changes that deliver greater benefits for patients and encourage more dentist participation.
Here’s what dentists face when participating in Medicaid today and how they can contribute to a better future for dentists and patients alike.
Medicaid is a program funded by both the federal and state governments to provide health coverage to eligible adults (based on income level, disability status and age), pregnant women and children. As of January 2023, 85.9 million Americans are covered by Medicaid.2
The requirements for Medicaid dental coverage vary in several ways. The first basis is age. States are required to provide dental benefits to children covered by Medicaid and CHIP. According to a Centers for Medicare & Medicaid Services (CMS) spokesperson, Medicaid covers dental services for all child enrollees as part of a comprehensive set of benefits called the Early and Periodic Screening, Diagnostic and Treatment (EPSDT) benefit. This benefit requires that all covered children be referred to a dentist on a schedule determined by the state, and baseline services include treating pain and oral infections, tooth restoration and dental health maintenance. Any services outside those minimum treatments must be considered “medically necessary,” a designation that is determined by the state. Any conditions found during a preventive visit must be treated, regardless of whether the treatment is covered in the state’s Medicaid plan.3
CMS has recently revised and strengthened the Child Core Set’s dental and oral health measures by including Dental Quality Alliance measures related to Oral Evaluation Dental Services, Topical Fluoride for Children and Sealant Receipt on Permanent First Molars. All three measures will be mandatory for states to report to CMS in 2024, according to a CMS spokesperson.
Medicaid coverage may be separate from CHIP — the Children’s Health Insurance Program. Like Medicaid, CHIP is a partnership between the federal and state governments to offer health coverage to children, but CHIP offers reduced-cost coverage to children (and, in some cases, pregnant women) of families that earn more than the Medicaid income requirements. Some states offer CHIP coverage through a Medicaid expansion program, while others have a separate CHIP program from Medicaid. States have their own rules for determining who qualifies for CHIP and services covered beyond the required comprehensive coverage (such as a preventive exam).3,4
The variances in Medicaid coverage become more stark when adult care is considered. States have more decision-making power when it comes to what dental services to cover for adult Medicaid patients, so the coverage varies by state. Most states provide at least emergency dental services for adult Medicaid patients, but less than half currently provide comprehensive dental care. And, unlike children’s coverage, there are no minimums for adult dental coverage. However, some states are taking steps to expand Medicaid coverage for adults.3
“In the last few years, several states, such as Maryland, Maine, Virginia and Tennessee, have opted to expand adult dental benefits, and New Hampshire plans to launch an expanded adult dental benefit in April 2023,” said a CMS spokesperson. “As of 2022, every state has opted to provide some level of dental coverage to beneficiaries during pregnancy.”
Despite some states taking steps to expand Medicaid dental coverage for adults, other states have kept the scope of adult dental Medicaid care small, covering only emergency dental care or services for women during pregnancy. (See map on page 17.)
Treating the Medicaid population has pros and cons. Donald said a benefit is being able to treat people who desperately need care and seeing them grow during his time as their provider.
“Many of the parents are appreciative of our efforts to create a dental home for their children and their families,” Donald said.
“I have practiced long enough that some of my patients whom I treated as children now have children and grandchildren of their own, and I get the privilege to treat them.”
But treating Medicaid patients also has challenges. Uncooperative children, who are eventually referred to pediatric dentists, and no-show patients decrease production and disrupt the clinic schedule. But Donald’s biggest problem with the program is the administrative burdens from managed care organizations (MCOs).
MCOs are contracted by states to help manage and deliver Medicaid services to enrollees. MCOs are designed to keep costs low while improving healthcare quality and patient health outcomes.5 However, many providers struggle working with MCOs.
“Mississippi has four MCOs, and all four try different ways to make it more difficult to be a participating dentist,” Donald said. “Over the past several years, I have spent more time on the phone with each MCO and our Division of Medicaid than I ever did in the past. The multiple MCOs have only increased the burden on the dentist while denying care to the recipient. It is extremely unfortunate.”
Darren S. Greenwell, DMD, MAGD, who practices in Radcliff, Kentucky, and chairs the AGD Dental Practice Council, shared Donald’s frustrations working with MCOs.
“In Kentucky, Medicaid is run by MCOs that will contract with another company to manage the dental benefits,” Greenwell said. “This has been very burdensome for the dentists taking Medicaid. Patient eligibility must be verified in as many as three different areas to determine eligibility. For example, the office will have to check the state Medicaid website, the MCO website and the dental benefit website. This can create confusion if all sites don’t agree — and can cause an increase in overhead for the dentists.”
Greenwell said he accepted Medicaid patients for 18 years and stopped three years ago due to the overcomplicated administration. His home state of Kentucky’s senate and house legislatures voted to eliminate adult dental Medicaid benefits in April 2023.6
Myron (Mike) Bromberg, DDS, practices in Reseda, California, and chairs AGD’s Legislative and Government Affairs Council. The problem, he said, is that the Medicaid system is so flawed that it disincentivizes dentists from becoming Medicaid providers. He explained that the reasons dentists don’t participate largely fall into two categories. The first reason is the fee structure.
“The fees are so low that, in many cases, they do not even cover the cost of providing the service,” Bromberg said. “In other words, it costs the dentist money to provide the service.”
The second source of complaints are the bureaucratic and administrative issues of dealing with Medicaid. In addition to MCO involvement, Bromberg explained that a developing concern is the Recovery Audit Contractors (RAC) audit, where independent contractors audit Medicaid providers to ensure dentists’ records indicate what and why procedures were performed, according to Medicaid guidelines. If inconsistencies are found, the
People with lower incomes historically avoid going to the dentist due to finances, and Medicaid helps cross that bridge.
— Mike Bromberg, DDS
Adult Medicaid dental benefits are optional for states, so coverage varies from state to state. Below is a look at state Medicaid dental coverage for adults and pregnant women based on data updated in October 2022.
Republished with permission from the Centers for Medicare & Medicaid Services, 2023 Medicaid & CHIP Beneficiaries at a Glance: Oral Health, medicaid.gov/medicaid/benefits/ downloads/2023-oral-health-at-a-glance.pdf. Data originally collected by the National Academy for State Health Policy, nashp.org/state-medicaid-coverage-of-dental-servicesfor-general-adult-and-pregnant-populations/.
penalties can be extrapolated to similar procedures performed by the dentist, and the dentist is billed for a refund.
“The fly in the ointment is that the contractors receive a percentage of what they ‘uncover,’” Bromberg said.
The problems currently faced by Medicaid dental providers and patients are a major challenge for dentistry. Bromberg is helping lead AGD’s effort to promote a better system for adult Medicaid dental benefits because the program is crucial to expanding access to the neediest Americans.
“People with lower incomes historically avoid going to the dentist due to finances, and Medicaid helps cross that bridge,” Bromberg said. “AGD has always encouraged participation in Medicaid, particularly since these people have so few options to maintain oral health.”
Emergency (8 States)
Extensive (25 States + DC)
Limited (14 States)
None (3 States)
AGD recommends the expansion of dental benefits under Medicaid to help address two major challenges facing the field today: underutilization of oral healthcare services and lack of providers in underserved areas.7
Studies link Medicaid dental expansion to increased oral health utilization and improved health outcomes. The early 2000s saw a budget-cutting trend of states reducing or removing adult dental Medicaid coverage, which was linked to a 10% decrease in low-income adult oral healthcare utilization. But after the Affordable Care Act (ACA) expanded Medicaid in 2009, studies showed a correlation to improved oral healthcare among low-income adults. 1,8 A case study in Colorado
General dentists should understand the differences between Medicaid and Medicare, along with AGD’s differing positions on the two programs.
Medicare was signed into law in 1965 and is designed to provide medical benefits to elderly adults in the United States. Over its near 60-year history, Medicare has undergone several changes. From a dental perspective, some groups have encouraged the inclusion of dental benefits into Medicare Part B. This is not an approach that AGD supports. Instead, AGD supports enhanced benefits and reimbursement from private insurance for dental benefits intended for older Americans.13
“The Medicare program is close to insolvency and cannot sustain the addition of dental benefits,” Bromberg said. “It is basically a medical program, and using medical criteria and systems for dentistry would be difficult for dentistry. Physicians who participate in Medicare complain bitterly about the program. I cannot imagine anything worse for the dental profession and our patients than the inclusion of dental benefits in Medicare.”
Effective Jan. 1, 2023, Medicare expanded coverage to select dental services considered “medically necessary,” which include simultaneous reconstruction of a ridge after surgical tumor removal; tooth stabilization when performed with treatment for a jaw fracture; tooth extraction as part of the jaw preparation for radiation therapy; dental splints when used in conjunction with other medically necessary treatment; and dental examination and treatment prior to cardiac valve replacement, valvuloplasty and organ transplant procedures. The rule does not cover dental care for patients with chronic conditions, including diabetes, or dental treatment prior to immunosuppressant therapy or joint replacement surgery.14
This position on dentistry in Medicare is representative of AGD and may not reflect the views of other dental organizations or sources quoted in this article.
illustrated how states saw improved patient dental outcomes and access post-ACA. After Medicaid adult dental services were expanded in the state, the University of Colorado School of Dental Medicine saw its total number of adult Medicaid patients skyrocket by nearly 350%. Additionally, between 2013 and 2016, the school saw a 51% increase in tooth-saving procedures and a 22% decrease in extractions. 9
Although evidence supports Medicaid’s ability to close healthcare gaps faced by low-income Americans, myriad obstacles to dental benefit expansion exist. One such barrier is lack of providers. Only 39% of American dentists accept Medicaid
and/or CHIP patients due to the pitfalls surrounding reimbursement rates, Medicaid population behaviors (e.g., no-shows) and administrative headaches. 1
AGD is recommending an increase in Medicaid funding to help solve the issue of provider participation. In its “White Paper on Increasing Access to and Utilization of Oral Health Care Services,” AGD recommends raising Medicaid fees to at least the 75th percentile of dentists’ regular fees, citing that states that increase Medicaid reimbursement rates see an increase in participating providers. This ultimately leads to more patients in underserved areas receiving care that they wouldn’t otherwise receive.7
Other proposed solutions to improve Medicaid for patients and providers include creating efficiencies around paperwork and e-filing, mandating quicker reimbursement, using case management to ensure patients have transportation to and from their appointments, and increasing education — both to Medicaid representatives about dentistry and to dental clinicians about the unique treatment needs of underserved populations.7
Other dental organizations, including the American Dental Association (ADA), share AGD’s stance on expanding state Medicaid programs’ adult dental coverage to improve oral healthcare among low-income individuals living in rural and underserved areas.10,11 AGD and other dental organizations have lobbied Congress and states to make changes to improve Medicaid dental coverage, but individual general dentists can also take action to support these efforts.
Treating Medicaid patients provides dentists a way to use their skills and expertise to support a demographic in need, but things need to change in order to encourage more providers to participate in Medicaid and ultimately improve patient outcomes.
“Advocacy is the No. 1 way a dentist can make change happen,” Greenwell said.
Medicaid is a partnership between the federal and state governments: The state legislature sets the fees, and the Division of Medicaid administers the program, Donald explained. He has advocated for the expansion of dental Medicaid benefits at both the state and federal levels.
“I have been involved in each step of the process, from talking with the Centers for Medicare & Medicaid Services to lobbying for increased fees and discussing the administrative burdens with the Mississippi Division of Medicaid at all levels,” Donald said. “I believe all Medicaid providers should be involved in the process with the goal of continuing to improve the program.”
Donald has also worked with his legislator on forming a study committee to look at the future of treating Medicaid recipients and to devise a strategic plan to improve the system so that young dentists can participate.
Bromberg highlighted a current piece of legislation called H.R. 1422, the Strengthening Medicaid Incentives for Licensees Enrolled in Dental Act (SMILED Act), sponsored by dentist Rep. Mike Simpson of Idaho, as one that dentists can support.
“Dentists are encouraged to call their congresspeople in support of this bill, which helps to eliminate some of the administrative burdens associated with being a Medicaid provider,” Bromberg said. “It also cuts through the red tape associated with applying to become a Medicaid provider.” Additionally, the legislation may change the RAC Medicaid audits by private contractors, but Bromberg said details on how it would accomplish that aren’t available.
For those general dentists who aren’t Medicaid providers, the passage of H.R. 1422 is designed to make the credentialing process easier. Applying to become a Medicaid provider varies from state to state. If you’re interested in learning more about the process, visit your state’s Medicaid website to learn about the steps to becoming a Medicaid provider.
Medicaid is only one piece of the puzzle in expanding oral healthcare to people in need. Another facet of this effort is boosting oral health education to underserved populations. More knowledge about oral health and its connection to overall health will help individuals recognize the value of oral healthcare and ultimately seek out dental health services.7 Underserved populations also often face struggles like transportation to and from dental appointments, taking unpaid time off work, securing childcare and covering the cost of copayments.1
Another big issue surrounding oral health utilization and access is the lack of providers in rural or low-income areas. Virginia, for example, expanded its adult Medicaid dental coverage in 2021, but only 26.9% of Virginia dentists accepted Medicaid patients in 2022; that number was actually down from 27.4% in 2020, with low reimbursement rates cited as the primary reason dentists don’t participate in the program. Expansion can only do so much when not enough providers accept Medicaid.12
In addition to its general recommendations, which include increasing reimbursement rates, AGD recommends incentivizing dentists to practice in underserved areas by extending the student loan forgiveness period to 10 years with no tax liabilities for the amount forgiven in any year, offering tax credits for practicing in underserved areas, and awarding scholarships to dental students who commit to practice in underserved areas.7
Using student debt relief to address the gaps in oral healthcare of the underserved may be mutually beneficial for both young dentists and patients, but Donald explained that it’s a bit complicated given the state of dental benefits in Medicaid today.
“As my career is winding down, I have great concerns about young practitioners being Medicaid dentists,” Donald said. “With all the administrative burdens, it is harder for the young dentist. The low reimbursement rates, coupled with their dental school debt, make it very difficult for the young dentist to be a Medicaid provider.”
The state of dental Medicaid benefits must be improved because the need it helps address cannot be ignored.
“Most dentists feel an obligation to serve their community,” Greenwell said. “However, a new dentist that is considering joining
the Medicaid system should be aware of the increase in regulation, the no-show rate and the poor reimbursement. Many have found it difficult to maintain a practice. I would encourage them to have good conversations with the Medicaid leadership and local, state and federal governmental agencies to try to improve many of the obstacles that plague the system today.” F
Kelly Rehan is a freelance journalist based in Omaha, Nebraska. To comment on this article, email impact@agd.org
1. “Medicaid Adult Dental Benefits: An Overview.” Center for Health Strategies Inc., Sept. 2019, chcs.org/media/Adult-Oral-Health-Fact-Sheet_091519.pdf.
2. “Medicaid.” Medicaid, Centers for Medicare & Medicaid Services (CMS), medicaid.gov/ medicaid/index.html. Accessed 10 April 2023.
3. “Dental Care.” Medicaid, CMS, medicaid.gov/medicaid/benefits/dental-care/index.html. Accessed 10 April 2023.
4. “State Children’s Health Insurance Program.” Benefits.gov, benefits.gov/benefit/607. Accessed 12 April 2023.
5. “Managed Care.” Medicaid, CMS, medicaid.gov/medicaid/managed-care/index.html. Accessed 15 April 2023.
6. Portalatin, Ariana. “Medicaid Dental Benefits in Kentucky Ended by Veto Override: 5 Notes.” Becker’s Dental Review - DSO + Dental News, Becker’s Healthcare, 3 Apr. 2023, beckersdental.com/revenue-cycle-management/40720-medicaid-dental-benefits-inkentucky-ended-by-veto-override-5-notes.html.
7. “White Paper on Increasing Access to and Utilization of Oral Health Care Services.” Academy of General Dentistry, July 2008, agd.org/docs/default-source/advocacy-papers/agd-whitepaper-increasing-access-to-and-utilization-of-oral-health-care-services.pdf.
8. Elani, Hawazin W., et al. “Dental Outcomes After Medicaid Insurance Coverage Expansion Under the Affordable Care Act.” JAMA Network, 30 Sept. 2021, jamanetwork.com/ journals/jamanetworkopen/fullarticle/2784596.
9. “Expanding Dental Benefits Is Good for States.” CareQuest Institute for Oral Health, carequest. org/resource-library/expanding-dental-benefits-good-states. Accessed 16 April 2023.
10. “Medicaid.” American Dental Association, ada.org/resources/community-initiatives/actionfor-dental-health/medicaid. Accessed 16 April 2023.
11. “Oral Health Leaders Urge Congress to Strengthen Adult Dental Coverage in All State Medicaid Programs.” CareQuest Institute for Oral Health, carequest.org/oral-health-leaders-urgecongress-strengthen-adult-dental-coverage-all-state-medicaid. Accessed 16 April 2023.
12. McIntyre, Meghan. “Virginia Expanded Dental Coverage Under Medicaid — But Not Enough Dentists Accept It.” Virginia Mercury, 17 March 2023, virginiamercury.com/2023/03/17/ virginia-expanded-dental-coverage-under-medicaid-but-not-enough-dentists-accept-it/.
13. “Medicare.” Academy of General Dentistry, agd.org/advocacy/agd-priorities/key-issues/ medicare. Accessed 12 April 2023.
14. Garvin, Jennifer. “CMS Expands Medicare to Cover Medically Necessary Conditions Requiring Dental Services.” American Dental Association, 8 Nov. 2022, ada.org/publications/adanews/2022/november/cms-expands-medicare-to-cover-medically-necessaryconditions-requiring-dental-services.
Recommended Reading
“Medicaid/CHIP Oral Health Services.” Centers for Medicare & Medicaid Services (CMS), Oct. 2010, medicaid.gov/sites/default/files/2019-12/2010-dental-factsheet.pdf.
“Medicaid Adult Dental Benefits Coverage by State.” Center for Health Care Strategies Inc., Sept. 2019, chcs.org/media/Medicaid-Adult-Dental-Benefits-OverviewAppendix_091519.pdf.
“Medicare Dental Coverage.” CMS, 1 Dec. 2021, cms.gov/Medicare/Coverage/ MedicareDentalCoverage.
Subject Code: 550
The 10 questions for this exercise are based on information presented in the article, “The State of Dental Medicaid Benefits” by Kelly Rehan, on pages 14–19. This exercise was developed by members of the AGD editorial team.
Reading the article and successfully completing the exercise will enable you to:
• understand what the Medicaid program is and who it helps;
• understand how dental benefits within Medicaid affect patients and dentists; and
• learn about proposed changes to Medicaid dental benefits to improve patient care and increase provider participation.
This exercise can be purchased and answers submitted online at agd.org/self-instruction
Answers for this exercise must be received by June 30, 2024.
1. Current statistics show that _____ Mississippians are Medicaid recipients. In Mississippi, _____ children are either on Medicaid or CHIP (Children’s Health Insurance Program).
A. 770,000; 479,284
B. 771,000; 478,284
C. 772,200; 477,284
D. 773,000; 476,284
2. Only _____% of dentists in the United States accept Medicaid and/or CHIP patients.
A. 39
B. 40
C. 41
D. 42
3. As of January 2023, _____ million Americans are covered by Medicaid.
A. 85.9
B. 86.9
C. 87.9
D. 88.9
4. Medicaid covers dental services for all child enrollees as part of a comprehensive set of benefits called the _____ Treatment (EPSDT) benefit.
A. Education, Prevention, Screening, Diagnostic, and
B. Early, Preventive, and Supportive Dental
C. Education, Periodic Screening, and Dental
D. Early and Periodic Screening, Diagnostic and
5. _____ organizations (MCOs) are contracted by states to help manage and deliver Medicaid services to enrollees. MCOs are designed to keep costs low while improving healthcare quality and patient health outcomes.
A. Multilevel care
B. Managed care
C. Multilevel collaboration
D. Managed collaboration
6. _____ Audit Contractors (RAC) are independent contractors that audit Medicaid providers to ensure dentists’ records indicate what and why procedures were performed, according to Medicaid guidelines.
A. Records
B. Recovery
C. Rate
D. Reimbursement
7. The early 2000s saw a budget-cutting trend of states reducing or removing adult dental Medicaid coverage, which was linked to a _____% decrease in low-income adult oral healthcare utilization.
A. 10
B. 11
C. 12
D. 13
8. After Medicaid adult dental services were expanded in the state, the University of Colorado School of Dental Medicine saw its total number of adult Medicaid patients skyrocket by nearly _____%. Additionally, between 2013 and 2016, the school saw a _____% increase in tooth-saving procedures and a 22% decrease in extractions.
A. 400; 50
B. 350; 51
C. 300; 52
D. 250; 53
9. H.R. _____, the Strengthening Medicaid Incentives for Licensees Enrolled in Dental Act (SMILED Act), is designed to make the credentialing process easier by eliminating some of the administrative burdens associated with being a Medicaid provider.
A. 502
B. 994
C. 1422
D. 2422
10. Virginia expanded its adult Medicaid dental coverage in 2021, but only 26.9% of Virginia dentists accepted Medicaid patients in 2022; that number was actually down from _____% in 2020.
A. 27.2
B. 27.3
C. 27.4
D. 27.5

AGD’s Fellowship and Mastership awards offer general dentists pathways to mastering the art and science of dentistry while also distinguishing themselves among their colleagues as the best of the best. By dedicating themselves to continuing education (CE), Fellows and Masters ensure they are able to deliver the most current, cutting-edge care to their patients as they continuously develop their skills and knowledge. Among general dentists, they represent the upper echelon. Meet some of this year’s recipients.
I have many mentors who have earned FAGD and MAGD awards and Lifelong Learning and Service Recognitions (LLSRs). I see that they are lifelong learners who have realized that the second you stop learning in dentistry, you risk becoming obsolete. What we learn in dental school is just the beginning of a career filled with growing and learning from our mistakes and striving to do the best we can for our patients every day. Education allows us to give our patients the most comprehensive care possible.
Having graduated in 2020, my dental education was cut short [by the COVID-19 pandemic], so I felt it was even more important for me to get as much CE as I possibly could after graduation. There is no way I would be able to practice dentistry the way I do now if I did not travel and attend in-person CE courses. In addition to education, the networking aspect of dental meetings has helped me meet new colleagues and mentors, and I have grown tremendously on both personal and professional levels.
I was in a lecture this past weekend (surprise, surprise!), and the speaker was talking about how there is a difference between a dentist who has 10 years of experience learning and growing in their profession and a dentist who repeats the same things 10 years in a row. AGD’s Fellowship and Mastership awards give guidance on how to be a well-rounded and informed dentist who never stops learning and growing in this ever-changing profession.
My advice to other members pursuing these awards would be to make sure you are documenting all of the courses you have attended, and follow up to make sure the correct credits were awarded to you. I made a spreadsheet and tracked when I took CE, then confirmed it had been correctly awarded. It really helped me sort out some courses that were missed and duplicated. I would also target participation hours early if you plan to get your MAGD. The Fellowship Exam is a definite obstacle. It is difficult because there are different schools of thought in dentistry, and it is hard to get inside the brain of the person who wrote the specific question you’re answering.
I did not have an official graduation from dental school, so I didn’t get to fully experience that sense of accomplishment and celebrate with my classmates and faculty members. This summer, I am looking forward to pausing for a moment to appreciate my hard work and celebrate!



When I was completing my general practice residency (GPR), so many of the adjunct faculty members who came and worked with us in clinic were AGD Fellows, Masters and even LLSR recipients. They were all very vocal about how important CE is and how much attaining their Fellowship had done for their careers. These people were my mentors, and I wanted more than anything to have the their knowledge and skill set. So, I joined AGD and started diligently working toward my Fellowship.
The most challenging part for me was probably the Fellowship Exam — it’s definitely not an easy one! With two boys under 6, finding the time to study was definitely the hardest part, but the AGD study materials helped tremendously. Obtaining the CE hours required was relatively easy — a huge number of my hours came from residency and subsequently serving as faculty at the same residency program. The COVID-19 pandemic also made CE more readily accessible and available.
Pursuing my FAGD has changed me as a provider and teacher in more ways than I can count. Dentistry is constantly changing, and you truly have to keep up to date with the latest materials, techniques and equipment, or you can fall behind very quickly. Having new GPR residents rotate through every year, I’ve realized how rapidly undergraduate dental education is changing. Pursuing my FAGD helped me make sure I’m as current as possible on the techniques and technologies my residents are learning in school. It also ensured that I have a wider knowledge base to pass along.
Organizations like AGD and the pursuit of awards like Fellowship and Mastership create a community within dentistry that brings you out of practice isolation and challenges your ways of thinking. You bond with others who are on the same journey or who have been on that journey before. I never want to be static in my way of thinking, and I always have a laundry list of educational goals I want to achieve (PhD? MAGD? Publishing?). On the flip side, there are gold-standard truths in dentistry that will never change, and being a part of a multigenerational group of dentists allows me to learn from others’ wisdom and incorporate new ways of thinking.
If you’re thinking about Fellowship, just go for it! Take as much CE as you can, and soak up every ounce of information presented to
you. Find a mentor in AGD, and ask for advice on what they did and how they achieved success. I did a lot of my AGD coursework and exam preparation with a colleague, and having a friend to bounce ideas and questions off of made the journey more fun. Also, be sure to start logging your CE into the website early on. Once you start with one CE upload, you will become addicted to soaking up and tracking every hour you obtain.
I couldn’t be more proud that I’m now one of “those” AGD dentists whom I looked up to as a resident. I feel elated and very accomplished! Now, my goal is to inspire my current and future residents like my mentors inspired me.
Working toward a future goal has always been something inherent in me. Neither of my parents had more than a two-year degree or equivalent, so even dental school was out of the blue to my family. I was 7 when I wrote in my Dr. Suess book that I wanted to be a dentist, so I don’t remember a time when I didn’t want to do this. I heard about Fellowship and Mastership when my family dentist worked toward hers. So, for me, it was just always next on the list — but first, I had to finish high school! That is how I managed to always push for the next checkpoint.
Within the first year after dental school, I was actively pursuing the CE needed for Fellowship. Unfortunately, I had the same misconception that so many still have — I thought I needed to have my 500 hours of CE before taking the Fellowship Exam. Wrong! I still hear that now and think that is the biggest thing we at AGD need to work on correcting. Taking the exam 10 years out was much more challenging than if I had taken it right away after graduating.
My biggest obstacle was personal; shortly after my 30th birthday, I finalized the details of my business partnership and practice buy-in and lost my father to a massive stroke. Losing my dad was devasting. He was my best friend and mentor. I had just closed on the most significant investment I would likely ever make, and my world had been broken. Fortunately, I dug in and punched through the hurt and worked as hard as possible to be the woman I knew my father expected me to be.
The other obstacles pale in comparison, but completing the CE requirements for specific disciplines for my Mastership award was hard. Trying to do it a la carte without working with an established program adds years to your attempt. In addition, finding suitable courses that fit in the categories you need is challenging. I practice in the Midwest, but I ended up all the way in California twice per year to complete the requirements in a reasonable amount of time. Indirectly, working toward this award gave me confidence that I needed to improve. MAGD presentations were a big part of that. Bringing my cases to share with my peers was frightening but rewarding. Sharing our stories of success and failure reminded me that I was the same as them. Sometimes, despite all your preparation, the case doesn’t go as planned. That’s OK. I have learned from those cases just as much as the others.
Becoming more comfortable and confident grew my practice in ways I couldn’t have imagined.
Convocation was in Nashville the year I received my Fellowship Award, and it was also my first national AGD meeting. I met and connected with involved members at the state and national levels. Those connections primed the path to my volunteering for the organization. I am currently serving as the Michigan AGD president for the second time and continue to be involved nationally. I will receive my Mastership Award this July in Las Vegas. I had initially planned on 2022, but I was a handful of CE credits short of the deadline. It worked out nicely, though; I will be celebrating serving as the Michigan AGD president and being 20 years out of dental school. I received my Fellowship 10 years after dental school, and now Mastership 20 years after. I love the symmetry in that. We are dentists, of course.
To be the best dentists we can be, CE is obvious; we must continue to stay current and be sure we provide the best patient care options. The FAGD and MAGD awards give you a framework to make that happen. Dentists — in a very general sense — are detailoriented, and having a structure to complete a goal works well with our brain chemistry.
My most important advice is take the exam now. Even if you think you will need more time to complete the rest of the CE or need to prepare more, you will regret waiting until next year. Second, find a FellowTrack or MasterTrack program that suits you, which will help make that award achievable in a reasonable time frame.


Dentistry is such a dynamic profession. What you learn in dental school is just a basic foundation of knowledge that you must build upon to make sure you are providing the utmost care to your patients. Knowing what you don’t know is so important. Achieving Mastership has helped me to focus on many different areas in dentistry and pursue more education in areas that I am weakest.
I am so lucky to live in Pennsylvania, which has a MasterTrack program called PEAK. Our PEAK program has been instrumental to me in earning my MAGD. The program meets two times a year, and I had a blast learning from not only the lecturers but also from Pennsylvania AGD dentists. The biggest obstacle was keeping my mommy guilt at bay while spending weekends away from my kiddos and having such a fun time while learning. My advice to others is to find dental friends who support your pursuit — or come join us at the Pennsylvania AGD to enjoy fellowship as well as personal and professional growth!
Awards like Fellowship and Mastership show your patients that you care for them and about them. While patients may not exactly know what the awards mean, I have learned to talk with them and show just how much time and energy I have put into being a knowledgeable dentist. What a distinction to know that I’ve pursued something that only 2% of general dentists achieve. I am proud to have put my education at the forefront in my career. F
Note: This article involves mention of specific types of traumatic events (but not graphic descriptions).
While dental patients experiencing anxiety is common, with up to 75% of adults in the United States experiencing some degree of dental fear, 1 those with post-traumatic stress disorder (PTSD) require a higher level of strategy and intervention from oral healthcare professionals.
PTSD develops in some people “who have experienced a shocking, scary or dangerous event,” according to the National Institute of Mental Health.2
“It happens when there is a perception of death, physical injury or sexual violence,” explained Marhya Kelsch, LCSW, clinical social worker, therapist and owner of Middleway Psychotherapy in Hayward, California. “[The traumatizing event] can be directly experienced or witnessed by you, or it can happen to someone you know very well or hold dear.”
When the body senses severe danger, it will respond with a stress response. Fight, flight and freeze are all common examples of stress, fear or trauma responses. While these responses are natural defense mechanisms, in some people, the physical and emotional response
of traumatic stress due to an event may persist long after the event concludes. When these symptoms are severe and persist for more than one month, even if they arise years after the preceding traumatic event, the person is considered to have PTSD. (Note the “Types of Trauma Responses” and “Diagnostic Criteria for PTSD” sidebars and how the symptoms of PTSD correlate closely with the behaviors exhibited during the common trauma responses.)
PTSD is far more prevalent than most people realize. Most people (70% of adults) will experience at least one traumatic event in their lifetime, and about 20% of people who experience trauma develop PTSD. One in 13 people will develop PTSD at some point in their life. The annual prevalence of PTSD in adults is estimated at 5%; however, PTSD is twice as common in women than in men, at an estimated 8% and 4%, respectively. PTSD among adolescents is estimated at 5%.3 Lifetime prevalence of PTSD in the United States has been estimated in as high as 17% of the population.4 Additionally, when the traumatic stress is related to an event
or period of abuse that occurs over a long period of time (such as long-term child or domestic abuse), the person can develop complex-PTSD (C-PTSD). C-PTSD includes the symptoms of PTSD plus additional symptoms such as dissociation, self-destructive behavior, impulsivity, alcohol and drug misuse, emotional deregulation and depression.
While many people think primarily of combat veterans when discussing PTSD, many types of traumatic events can cause PTSD, and it is important to understand that any dental patient can experience PTSD. Different types of traumatic events correlate with different rates of PTSD development. PTSD develops in:
• 49% of rape victims.
• 32% of victims of severe physical assault.
• 29% of combat veterans. (Note that the statistic for combat veterans does not include veterans who develop PTSD as a result of military sexual trauma. About 1 in 50 male veterans and 1 in 3 female veterans report experiencing this type of trauma.5)
• 16.8% of people involved in serious accidents, such as car accidents.
• 15.4% of shooting and stabbing victims.
• 14.3% of people who experience the sudden, unexpected death of a loved one.
• 10.4% of parents of children with life-threatening illnesses.
• 7.3% of people who witness the murder or serious injury of another person.
• 3.8% of survivors of natural disasters.3,5
While men are more likely to experience a higher number of traumatic events during their lifetime, women are more likely to develop PTSD symptoms; it is conjectured that the types of traumatic events women are more likely to experience are to blame for this increased risk of PTSD.3 Women experience higher rates of sexual trauma and domestic violence than men, as high as 1 in 5 for rape (1 in 71 for men); 1 in 4 for severe physical violence from an intimate partner (1 in 7 for men); and 1 in 7 for injury by an intimate partner (1 in 25 for men).6
While “it seems like PTSD is increasing, that may be because we are much more aware of what trauma is — particularly after the prolonged stress associated with the COVID-19 pandemic — and we are studying and paying more attention to trauma now,” said Sheela Raja, PhD, LCP, University of Illinois at Chicago College of Dentistry associate professor and director of clinical behavioral sciences and the Resilience Center.
“Taking someone off their feet is already disconcerting and gives them the feeling of loss of control,” explained Jason R. Flores, DDS, MHA, BSN-RN, dental anesthesiologist, division chiefdental medicine, University of New Mexico (UNM) Medical Group Ambulatory Surgical Center; and clinical director, director of dental anesthesiology and associate director/associate professor of the UNM advanced education in general dentistry residency program.
“Multiple people stand over them, looking down with masks on, forcing fingers, sharp instruments and noisy suctions into their oral cavity, touching and causing pain to oral mucosa that people
Fight: crying, feelings of anger or rage, jaw tension, tooth grinding, physically or verbally fighting, pushing, struggling. Flight: distancing oneself from danger, including running, hiding or backing away; restlessness; anxiety or shallow breathing; darting eyes.
Freeze: going tense, still and silent; holding breath or restricting breathing; decreased heart rate; sense of stiffness or heaviness; sense of dread; feeling of numbness.
Flop: similar to freezing, except instead of stiffness the muscles become loose and the body floppy; mind may shut down to protect itself.
Fawn or Friend: calling for a friend or bystander for help and/or befriending the person who is dangerous, such as by placating, negotiating, bribing or pleading with them; peoplepleasing in order to avoid or lessen the impact of conflict; neglecting one’s own needs; overapologizing to others.
Sources: “The 5Fs: Fight, Flight, Freeze, Flop and Friend.” Rape Crisis England & Wales, rapecrisis.org.uk/get-help/ tools-for-victims-and-survivors/understanding-your-response/ fight-or-flight/.
“Trauma Response (The 4 Fs – Fight, Flight, Freeze, and Fawn).” Human Relations Institute & Clinic, hricdubai.com/ trauma-response-the-4fs/.
rarely have touched, telling them not to move during the entire event,” Flores added. “Dentistry by its very nature is set up to kick off a PTSD episode.”
“When you have PTSD, you may not be taking care of yourself overall, and you may not be engaging in preventive healthcare treatments, including oral health,” Raja said.
“Such patients push back dealing with their oral health needs as much as they can and avoid going to the dentist,” explained Clement Kairouz, DDS, MPH, a dentist practicing at Apa Aesthetic in New York. “So they become more reactive and end up only coming in when they have pain and need emergency dentistry. Getting them in for routine care is the biggest hurdle.” Many patients with PTSD will wait until they cannot wait any longer.
“Dental patients with PTSD will wait until the infection brings them to death’s door before seeking treatment,” Flores said. “By this time, oral conditions have degraded so much that the patient is now looking at extreme and costly dental repairs.”
In addition to putting off or avoiding care for acute dental needs, patients with PTSD are also more likely to have higher incidences of routine or chronic dental complaints.
To be diagnosed with PTSD, an adult must have all of the following for at least one month:
o At least one re-experiencing symptom.
o At least one avoidance symptom.
o At least two arousal and reactivity symptoms.
o At least two cognition and mood symptoms.
Re-experiencing symptoms include:
o Flashbacks — reliving the trauma over and over, including physical symptoms like a racing heart or sweating.
o Bad dreams.
o Frightening thoughts.
Avoidance symptoms include:
o Staying away from places, events or objects that are reminders of the traumatic experience.
o Avoiding thoughts or feelings related to the traumatic event.
Arousal and reactivity symptoms include:
o Being easily startled.
o Feeling tense or “on edge.”
o Having difficulty sleeping.
o Having angry outbursts.
Cognition and mood symptoms include:
o Trouble remembering key features of the traumatic event.
o Negative thoughts about oneself or the world.
o Distorted feelings like guilt or blame.
o Loss of interest in enjoyable activities.
Symptoms that are unique to children under the age of 6 include wetting the bed after having learned to use the toilet, forgetting how or being unable to talk, acting out the scary event during playtime and being unusually clingy with a parent or other adult.
Source: “Post-Traumatic Stress Disorder.” National Institute of Mental Health, May 2022, nimh.nih.gov/health/topics/ post-traumatic-stress-disorder-ptsd.
What is the best way for clinicians to find out whether patients are affected by PTSD?
“Pre-screening questions about PTSD and abuse should be in the pre-patient questionnaire,” said Flores.
“Ask patients about what they’ve been through,” Raja said.
“If the patient is very stressed about coming in, sometimes we do consults in the comfort of their own home, on the phone or online,” Kairouz said. “Then we bring them in and continue the conversation, but we don’t do any dental work yet. We establish rapport and trust and show that we have their best interests in mind. We alleviate their fear that we’re the bad guys, and then go over a treatment plan and its longevity. We call them up a day or two after, so they have had time to process everything. We don’t bombard them the same day because that only adds to the stress.”
“In appointments, it’s important to give them things to help them feel grounded,” Kelsch said. “Let them grip their keys really hard, encourage them to bring a comfort object to hold, ask them if they want an eye cover, give them a cold sip of water, or coach them on breathing. Use a stop signal. Let the patient know they have some control in the space. PTSD patients want to know where the exit is. Even a skylight or window in the operatory can bring some relief, because it gives the perception of an exit. They also want to know where everyone on the team is and where the sharps are.”
Communicate to the patient “everything you are doing, why and for how long,” Kelsch advised. “What tools are you using? Are there options for using something else? How loud is it going to be? Will it be smelly? Is it going to vibrate or feel hot or cold? Let them know, particularly if the patient can’t see you while you’re working. Let them know, ‘I’m over here mixing this paste to fill your crown.’ Anything that can feel restricting can be triggering, like gauze in the mouth, bite guards or goggles. So, as much as you can narrate and inform, it helps.”
For PTSD sufferers, “it’s hard for them to make decisions,” Kelsch said. “It’s hard for them to pick: ‘Should I get the root canal now, or should I wait?’ It’s important to offer options, and, if there are no options, let them know why.”
“Ask them about triggers or activators — anything that gets them anxious or worried in an oral health environment,” Raja said. “Have a checklist that can indicate things that make them anxious, such as being in a supine position, having a dental dam, radiography, etc. Figure out what you can do to give the patient more shared power and control, such as raising their hand [to signal they need a break] as well as providing more information about the procedure or demonstrating it on a dental model first.”
“There is evidence that people who have a full-blown PTSD diagnosis have higher levels of periodontal disease, are often presenting with more missing and filled surfaces, report higher levels of orofacial pain and also concurrently experience higher levels of dental anxiety,” Raja explained.7
Patients with PTSD also exhibit more bruxism and tooth plaque than patients without PTSD.8
Sedation can be an effective tool.9 “PTSD is one of the most common reasons patients seek anesthesia services for dentistry,” Flores said. Kairouz uses nitrous oxide in his practice.
Kelsch finds that “patients with PTSD have a higher rate of increased symptoms following medical procedures that they often relate to the pain and vulnerable feelings that remind them of past
trauma. However, simply telling the patient those symptoms are possible reduces the impact afterward because they had awareness.”
Raja also warns of emergence agitation. “Patients with PTSD may be at higher risk for emergence agitation,” she said, and suggested informing the entire care team about the risk, use of behavioral strategies, and a pre- and postoperative environment that is “private, quiet and includes bed rails to reduce the likelihood that patients can hurt themselves.”10
In consultation with the patient’s general or mental health practitioner, Kairouz said he may also prescribe alprazolam for the patient to take about an hour before the appointment or CBD (cannabidiol) gummies when the patient is in the chair. “You are not putting them out [of consciousness]; it has more of a calming effect,” Kairouz noted.
Kairouz also uses distraction. “A headset and a TV on the ceiling tune out dental sounds that might elevate their stress level,” he said.
Kelsch uses a similar approach. “If they can hear conversations or drills in other rooms, it doesn’t feel very safe. Use of heat packs also may make them feel better.”
Fear of gagging is common.11 To deal with that fear, “we do scanning rather than taking impressions,” Kairouz explained. “We limit the amount of radiographs that we take. Sometimes we break down the procedures into shorter appointments, and sometimes we bundle them into one longer appointment, depending on how the patient wants to proceed.”
Dentists can also leverage modern technology in innovative ways.
“There is a handheld biofeedback device called a HeartMath that has a light that shows what a person’s pulse is,” Kelsch said. “It coaches them to breathe more slowly.”
“Virtual reality or even something as simple as a video tour of your operatory in advance may help,” Raja said. “If people feel like they’ve seen your operatory before, it isn’t as overwhelming. They know how it is laid out, and that may help people feel more in control.”
Like any chronic physical condition, PTSD necessitates that dentists become part of a patient’s interdisciplinary team of healthcare providers in order to coordinate treatment efforts and minimize harm.
“It takes a village, so we always try to be in touch with the patient’s general provider and/or their psychiatrist to make sure they’re on the right medication and that we’re not stepping out of line by giving them sedatives or anxiety medications,” Kairouz said. “If a patient is under mental health treatment, we always meet with the psychiatrist.”
“Ask the patient, or work with their healthcare provider on what triggers them,” Kelsch said. “Are there sensory things that overwhelm them, like noise or smells? Create a care plan around that. It can even be helpful to talk to or bring in a supportive friend or family member.”
“We’re seeing collaboration more, particularly in pediatric dentistry with social work providers,” Raja noted. “If you’re working with children who have been through the foster care system or with adults who are veterans or refugees, they are at high risk for PTSD,
• “What can I do to make you more comfortable during the procedure or examination today?”
• “Before we proceed, is there anything else you think I should know?”
• “Please feel free to ask me any questions along the way or get my attention by raising your hand if you need a break.”
• “I am going to do a percussion test on your tooth. To do this, I will gently tap on your teeth. Let me show you on my hand, or we can use yours.”
Source: Raja, Sheela, et al. “Treating Patients with Traumatic Life Experiences: Providing TraumaInformed Care.” Journal of the American Dental Association, March 2014, vol. 145, no. 3, pp. 238-245.
• Admits to strange dreams or hallucinations.
• States they feel very uncomfortable when laying recumbent with a dentist standing over them.
• States discomfort or cries when the mouth is probed.
• May only finish half sentences when PTSD questions are asked.
• Overly strong reactions to questioning.
• Overly strong reactions to dental noises.
• Visceral reactions to bright lights being shone in their face.
• Exaggerated signs of paranoia, depression, intimidation behaviors, etc.
Source: Jason R. Flores, DDS, MHA, RN
and it’s important to consider interprofessional teams to work with.
“If your dental practice is embedded in a healthcare setting that has primary care and social work under one umbrella, that might be something that happens more often,” she added.
Sometimes, it is the oral healthcare provider who may find that the patient needs to be referred to general or mental healthcare providers.
“If you feel that somebody is stressed or traumatized — or if they spontaneously disclose something going on in their life — you may want to refer to a mental health provider or primary care physician,” Raja noted.
Oral healthcare practitioners following these strategies can help PTSD sufferers achieve optimum oral health more than ever before. Flores concluded that “now there is more education given to healthcare providers about PTSD, community resources available, insurance and workplace coverage for PTSD, workplace plans focused on wellness, and military awareness and resources for PTSD sufferers.”
Raja also warned that “providers themselves are not insulated. We need to focus on resilient skills for taking care of ourselves as well,” she said.
“Trauma takes away our sense of power and control, so anything we can do to create a more collaborative environment where trust is shared gives back some of that power and control,” Raja concluded. F
William S. Bike is a freelance writer and editor based in Chicago. He is a former director of advancement communications for the University of Illinois at Chicago College of Dentistry. To comment on this article, email impact@ agd.org.
1. Flores, Jason. “Dental Fear in the New Economy,” Dentistry Today, 1 Feb. 2015, dentistrytoday.com/dentalfear-in-the-new-economy/
2. “Post-Traumatic Stress Disorder.” National Institute of Mental Health, May 2022, nimh.nih.gov/health/topics/ post-traumatic-stress-disorderptsd#:~:text=Post%2Dtraumatic%20stress%20disorder%20 (PTSD,danger%20or%20to%20avoid%20it.
3. Carmona, Melissa, and Denise-Marie Griswold. “PTSD Statistics and Facts.” The Recovery Village, 8 May 2023, therecoveryvillage.com/mental-health/ptsd/ptsd-statistics/.
4. Schein, Jeffrey, et al. “Prevalence of Post-Traumatic Stress Disorder in the United States: A Systematic Literature Review.” Current Medical Research and Opinion, Dec. 2021, vol. 37, no. 12, pp. 2151-2161.
5. U.S. Department of Veterans Affairs. “How Common is PTSD in Veterans?” PTSD: National Center for PTSD, ptsd. va.gov/understand/common/common_veterans.asp. Accessed 11 May 2023.
6. “Statistics.” National Coalition Against Domestic Violence, ncadv.org/statistics. Accessed 11 May 2023.
7. Kisely, Steve, et al. “The Oral Health of People with Anxiety and Depressive Disorders – A Systematic Review and Meta-Analysis.” Journal of Affective Disorders, 2016, vol. 200, pp. 119-132.
8. Baker, Lois. “PTSD Patients Damage Teeth Through Involuntary Grinding, Clenching, UB Study Finds.” University at Buffalo News Center, 8 March 2001, buffalo.edu/news/ releases/2001/03/5063.html.
9. Klose, Sara Louise. “Dentists and Sedation.” AGD Impact, Jan. 2022, vol. 50, no. 1, pp. 18-20.
10. Taylor, M., et. al. “A Perioperative Intervention to Prevent and Treat Emergence Delirium at a Veterans Affairs Medical Center.” Patient Safety, vol. 4, no. 4, pp. 26-35.
11. Rehan, Kelly. “Top Patient Phobias and How to Handle Them.” AGD Impact, May 2021, vol. 49, no. 5, pp. 22-25.
Subject Code: 750
The 10 questions for this exercise are based on information presented in the article, “Caring for the Patient with PTSD” by William S. Bike, on pages 24–28. This exercise was developed by members of the AGD editorial team.
Reading the article and successfully completing the exercise will enable you to:
• understand what posttraumatic stress disorder (PTSD) is;
• learn about different traumatic events and risk factors for PTSD such as age, gender and type of event; and
• recognize symptoms of PTSD in your patients and develop accommodations for them.
This exercise can be purchased and answers submitted online at agd.org/selfinstruction
Answers for this exercise must be received by June 30, 2024.
1. While dental patients experiencing anxiety is common, with up to _____% of adults in the United States experiencing some degree of dental fear, those with post-traumatic stress disorder (PTSD) require a higher level of strategy and intervention from oral healthcare professionals.
A. 60
B. 65
C. 70
D. 75
2. All of the following except one are examples of stress, fear or trauma responses. Which is the exception?
A. Flight
B. Flail
C. Fawn
D. Freeze
3. Most people (_____% of adults) will experience at least one traumatic event in their lifetime, and about _____% of people who experience trauma develop PTSD.
A. 75; 15
B. 70; 20
C. 65; 25
D. 50; 30
4. One in _____ people will develop PTSD at some point in their life.
A. 13
B. 14
C. 15
D. 16
5. The annual prevalence of PTSD in adults is the same as among adolescents (5%). PTSD is twice as common in adult men than in women, at an estimated 8% and 4%, respectively.
A. Both statements are true.
B. The first statement is true; the second is false.
C. The first statement is false; the second is true.
D. Both statements are false.
6. Lifetime prevalence of PTSD in the United States has been estimated in as high as _____% of the population.
A. 15
B. 16
C. 17
D. 18
7. When the traumatic stress is related to an event or period of abuse that occurs over a long period of time (such as long-term child or domestic abuse), the person can develop _____PTSD (C-PTSD).
A. Chronic
B. Complex
C. Complicated
D. Compounded
8. Which of the following types of traumatic events correlates with the highest rate of PTSD development?
A. Military combat
B. Car accidents
C. Rape
D. Severe physical assault
9. PTSD develops in _____% of people who experience the sudden, unexpected death of a loved one and _____% of parents of children with life-threatening illnesses.
A. 11.3; 13.4
B. 12.3; 12.4
C. 13.3; 11.4
D. 14.3; 10.4
10. Two patients present to your practice and report symptoms that have lasted longer than a month. Patient A reports frightening thoughts, staying away from the place where they were in a bad car accident, difficulty sleeping, feeling tense, loss of interest in enjoyable activities and negative self-thoughts; Patient B reports being easily startled, difficulty sleeping, feeling tense, angry outbursts, distorted feelings of guilt and negative self-thoughts.
A. Both patients meet the diagnostic criteria for PTSD.
B. Patient A meets the diagnostic criteria for PTSD; Patient B does not.
C. Patient A does not meet the diagnostic criteria for PTSD; Patient B does.
D. Neither patient meets the diagnostic criteria for PTSD.
Filtek™ Supreme Universal Flowable Restorative

3M™
3m.com
Filtek™ Supreme Universal Flowable Restorative is a new take on a longtime product. With a 20-nanometer maximum filler particle size, this material is easy to shine with minimal polishing. What I have enjoyed most about this product is the redesigned handle. Most flowable syringes use a double-wing design, but this handle has a triangular shape that allows for easy gripping from any angle. 3M™ also has redesigned the syringe tip with the goal of eliminating bubbles in the material — although with visual inspection I can’t really see what the company did differently other than adding a few more locking grooves. However, I think it has succeeded because I have noticed zero bubbling, and the static hydraulic pressure makes this a no-drip material. My favorite use for this composite is to line the floors of my Class I and II restorations because it adapts quickly to inconsistent prep surfaces, it is super smooth, and I am not worried about void formation. I don’t personally do composite warming, but that is also a possibility with this product, and it has been shown to maintain its properties when heated up to 158 degrees Fahrenheit for an hour 25 times. Available in all standard shades, Filtek Supreme Universal Flowable handles like a dream and is strong enough to withstand the same forces as enamel without aggressive wear patterns.
Laryngosponge
MillCreek Services
laryngosponge.com
As dentists, we specialize in working with tiny objects in a wet, difficult and unpredictable environment. Losing a tooth down a throat is a real possibility. Devices such as Mr. Thirsty, the Isolite and rubber dams are quite helpful at blocking the throat — but sometimes there is a simpler answer. The Laryngosponge by MillCreek Services is a simple sponge that arrives in a dehydrated form and is easy to store. Upon hydration, it immediately swells to an appropriate size to block the larynx. Since they are not shipped in sterile packaging, the sponges should be run through an autoclave prior to use. They are obviously single-use devices, but they are also inexpensive. The sponge was designed by an oral surgeon to be effective at reducing laryngospasms. It accomplishes this goal by reducing saliva and blood flow into the throat during surgery and keeping the tongue out of the field while working laterally — but especially in the anterior. I have found this to be a helpful shield during sedations, but I don’t use it often because I don’t often sedate my patients beyond anxiolysis. Even though it isn’t rigid, I have found that fully awake patients don’t tolerate a throat pack well, and the same goes for this sponge. However, the sponge is a significant upgrade over using a 4-by-4 gauze or standard throat pack and should replace those in your oral surgery kit.


Artcraft Dental
artcraftdental.com

When performed with purpose and finesse, oral surgery can not only aid someone in pain, but it can also limit trauma and allow for a more successful reconstruction. My goal in the practice of dental surgery is to consistently improve my technique through the acquisition of knowledge and experience and also through the application of an advanced armamentarium. While my initial training was primarily in the use of standard elevators and forceps, I now know that directed force through the use of periodontal ligament knives and intraligamental elevators like the Xpanders™ from Artcraft Dental are more effective ways to quickly and atraumatically extract a tooth. The Xpanders are shaped with a double-pronged tip that allows for a two-point contact on the tooth. With a little twisting and apically aimed pressure, a quick expansion of the socket can loosen ligaments and help teeth jump out. Whether used for extracting a single tooth or multiple, this system works best by angling the curved diamond grip tip into the interproximal area and engaging mesial or distal aspects of the target tooth. The four-piece set includes a straight tip and three angled tips to allow for easy anterior or posterior access. Manufacturer recommendations are that you use a standard 301 elevator forceps first to create some horizontal mobility prior to using the Xpanders. I have tried the instrument after using a 301 forceps and also as just a first elevator. While the tip slides more readily into the ligament space if prior elevation has been completed, there is not a significant change in its ability to engage. From the very first contact, the double prongs on a roughened interior surface create great stability and, when coupled with apical pressure and minor twisting, will lead to a swift result. If you are patient, steady and purposeful with your Xpanders, then you will find that challenging teeth no longer require aggression for removal.
Ross Isbell, DMD, MBA, currently practices in Gadsden, Alabama, with his father, Gordon Isbell, DMD, MAGD. He attended the University of Alabama at Birmingham (UAB) School of Dentistry and completed a general practice residency at UAB Hospital. Isbell has confirmed to AGD that he has not received any remuneration from the manufacturers of the products reviewed or their affiliates for the past three years. All reviews are the opinions of the author and are not shared or endorsed by AGD Impact or AGD. To comment on this article, email impact@agd.org

Now is the time to take advantage of AGD’s Self-Instruction program that includes exercises based on AGD Impact articles. These exercises contain 10 questions and are worth 1 CE credit. It’s the perfect complement to General Dentistry.

AGD Impact General Dentistry

1 exercise = $15
2 exercises = $25 (save $5)
4 exercises = $50 (save $10)
LEARN MORE agd.org/self-instruction
1 exercise = $30
3 exercises = $70 (save $20)
6 exercises = $120 (save $60)
12 exercises = $180 (save $180)
Take advantage of membership tailored to you! For an additional $150 you can receive the following:
• Free Early-Bird Scientific Session Registration
• Free CE Library PLUS 4 On-Demand Webinars of Your Choice
• 20% Fall Fellowship Review Course Discount
• 20% Fellowship Study Guide Discount
• Free Dental Card Services Virtual Terminal Setup
“I wanted to take advantage of all the lectures and classes that the scientific session offers, so, to get the best value, Premium Plus membership was the obvious choice.”
Mohamed H. Attia, DDS, MAGD Member since 2008agd.org/membership




• AGD Supply Discount: Automatically access your membership’s savings benefit of up to 30% off standard industry retail.
• Authorized Access: Order with confidence! No gray market. No fraudulent products.
• FREE Shipping: Consolidate your supply sources and eliminate shipping fees within the continental United States.
• Save Time: Order all of your dental supplies from one easy-to-use online dental supply store.

• Support: Our dedicated account managers review every order for accuracy and apply qualifying manufacturer discounts and deals.


