

Australia’s Largest Clinical Consultancy



AN-ACC FUNDING QUALITY INDICATOR REPORTING







COMPLIANCE & ADVISORY
CLINICAL OPERATIONS
KNOWLEDGE
Our team of over 40 aged care experts, including 30 clinical consultants, are dedicated to supporting aged care providers and their residents nationwide.
Genuine Expertise: Our team undergo comprehensive training in their speciality.

Proven Results: Consistently successful outcomes demonstrate our commitment to excellence.
Personalised Engagement: Tailored to our clients’ individual needs and designed to ensure longevity of operations.
Leading Innovation: Utilising the latest systems and processes, we implement effective strategic improvements.







Flexible Hands-On Innovative 1300 909 913
CONNECT WITH



Contact
| team@healthgen.io

Anchor Excellence - Delivering exceptional services and solutions to aged care, home care, retirement living and disability.
Delivering exceptional services and solutions to aged care, home care, retirement living and disability.
Anchor Excellence -
When you partner with Anchor Excellence, you gain access to our wealth of knowledge and expertise. We bring a proven track record of success and increased capability, working hand in hand with providers and operators to achieve exceptional outcomes. Our unwavering commitment to excellence sets us apart as a trusted partner, ready to equip you with the tools and strategies necessary to rise to the challenges across aged care, home care, retirement living and disability.
When you partner with Anchor Excellence, you gain access to our wealth of knowledge and expertise. We bring a proven track record of success and increased capability, working hand in hand with providers and operators to achieve exceptional outcomes. Our unwavering commitment to excellence sets us apart as a trusted partner, ready to equip you with the tools and strategies necessary to rise to the challenges across aged care, home care, retirement living and disability.
Leadership and Governance
Leadership and Governance
Risk governance framework | Full risk and assurance program | Certified chair and advisory body implementation and execution | Strategic transformation project support | Board and key personnel advisory and training | Targeted mentoring and coaching
Business Advisory and Strategy
Business Advisory and Strategy
Board advisory, workshop facilitation and strategy sessions | Sustainability and viability assessments | Financial optimisation and performance | Care, compliance and financial due diligence | M&A | Home closures and AP transfers | Executive recruitment
Board advisory, workshop facilitation and strategy sessions | Sustainability and viability assessments | Financial optimisation and performance | Care, compliance and financial due diligence | M&A | Home closures and AP transfers | Executive recruitment
Quality and Clinical Governance
Quality and Clinical Governance
Certified chair and quality care advisory body implementation and execution | Clinical governance framework development | Model of care development | Quality and compliance reviews, Complete end-to-end policies and processes
Certified chair and quality care advisory body implementation and execution | Clinical governance framework development | Model of care development | Quality and compliance reviews, Complete end-to-end policies and processes




Compliance and Operations Management
Compliance and Operations Management
Eligible advisor appointments | operational, compliance, risk and assurance reviews | additional services programming | nutrition and hospitality reviews, NDIS support | Incident investigations
Eligible advisor appointments | operational, compliance, risk and assurance reviews | additional services programming | nutrition and hospitality reviews, NDIS support | Incident investigations
Education (Anchor Academy - online, on-demand, face to face and bespoke)
Education (Anchor Academy - online, on-demand, face to face and bespoke)


Compliance Essentials for Key Personnel and Board Members | Clinical Management and Governance Essentials | Leadership Sprint | New Graduate Program | Pain Management | End of Life Care | Medication Management | Additional Services
Compliance Essentials for Key Personnel and Board Members | Clinical Management and Governance Essentials | Leadership Sprint | New Graduate Program | Pain Management | End of Life Care | Medication Management | Additional Services


Workforce
Workforce
Workforce analysis and planning | High performing team development workshops | Team management profiling | 360 linking leaders profile | Leadership support programs | AN-ACC strategy and performance review
Workforce analysis and planning | High performing team development workshops | Team management profiling | 360 linking leaders profile | Leadership support programs | AN-ACC strategy and performance review


Consumer Experience and Engagement
Consumer Experience and Engagement
Certified chair and consumer advisory body implementation and execution | Co-design strategy and planning | Customer journey mapping | Stakeholder engagement and mediation | Strategic project marketing | Community consultation and focus groups
Certified chair and consumer advisory body implementation and execution | Co-design strategy and planning | Customer journey mapping | Stakeholder engagement and mediation |


Strategic project marketing | Community consultation and focus groups


(02) 8610 1950
8610 1950
info@anchorexcellence.com
www.anchorexcellence.com
Aged Care Today is the regular publication of Aged & Community Care Providers Association (ACCPA). Unsolicited contributions are welcome but ACCPA reserves the right to edit, abridge, alter or reject material. Opinions expressed in Aged Care Today are not necessarily those of ACCPA and no responsibility is accepted

NOTE
Welcome to our spring issue of AgedCareToday – the magazine of the Aged & Community Care Providers Association (ACCPA).
We’re delighted to present articles from policy makers, leaders, innovators and influencers in aged care, including Minister Anika Wells and Commissioner Janet Anderson.
With ACCPA now into its second year advocating for the aged care sector and older Australians, we’ve had some outstanding wins, including a significant wage increase for aged care workers.
Learn more about that, and get up-to-date with all the latest information, curated exclusively for aged care providers. We hope you enjoy the read.
Linda Baraciolli, Editorby the Association for statements of fact or opinions expressed in signed contributions. Aged Care Today may be copied in whole or distributed among an organisation’s staff. No part of Aged Care Today may be reproduced in any other form without written permission from the article’s author.














A wake-up call for Australia
Why we need to renew the focus on aged care
The Intergenerational Report (IGR) released by the Australian Government last month is a wake-up call, not only for the aged care sector, but the entire Australian population.
It’s sobering reading and highlights what has been predicted for some time. However, it also underscores great opportunities for aged care.
The report forecasts the number of Australians over 85 will triple, and those over 65 will double in the next 40 years, with demand for aged care set to spiral.
At the same time fewer Australians will be working and paying tax, putting a mounting strain on the federal budget.
Life expectancies will also rise in Australia with men living to 87 years of age and women to 89.5.
All this points to a massive surge in demand for aged care.
The IGR forecasts spending on aged care will increase as a proportion of gross domestic product from 1.1 per cent in 2022-23 to around 2.5 per cent in 40 years.
Growth in residential aged care spending will increase the most, but spending on community care is also forecast to rise significantly.
Rather than focus on the doom and gloom, we should be seeing this as a magnificent opportunity for aged care to grow, to employ more Australians, to invest, and to improve the lives of older Australians.
The IGR brings into sharp focus the importance of the national conversation about how Australia can sustainably fund a sector that has already suffered decades of financial pressure, to ensure its readiness to deliver the aged care all Australians deserve as demand grows in coming decades.
These issues are currently being discussed by the Australian Government’s Aged Care Taskforce, chaired by Aged Care Minister Anika Wells. I’m proud to say our very own CEO Tom Symondson is a vital member of this taskforce.
Tom’s inclusion gives ACCPA – the nation’s peak body for aged care providers and our members – a voice on aged care funding. It’s a wonderful opportunity to fix the problems that have plagued the sector for decades. I congratulate Tom for his appointment and wish him all the best in this vital work.
As we understand, nothing is off-the-table when it comes to debate about funding aged care.
The IGR demonstrates just how urgent this work is.
Attracting more workers to the aged care sector is another related and important issue. For too long aged care workers have been undervalued, despite the invaluable work they carry out caring for our most vulnerable.
ACCPA helped bring about a fully funded 15 per cent pay rise for aged care workers from 1 July this year, which still has its challenges. More work is being done with the Fair Work Commission to ensure all workers are paid appropriately. It’s overdue recognition for the workers, who are the backbone of aged care.
Additionally, from 1 July the Government’s mandate to have a nurse on duty 24/7 in aged care facilities kicked in. Although we saw 86 per cent of providers meet the 24/7 RN requirements, we know some providers need further support, particularly those in areas of ongoing workforce shortage and those in regional, rural and remote communities.
ACCPA supports the move to bring more quality care to aged care residents, but we do also need to ensure we have the right supports and the workforce to achieve quality care.
It’s only fitting the theme for ACCPA’s national conference next month is ‘The Age of Change’ and I look forward to seeing all our members there.
On 7 August, ACCPA celebrated the work of all aged care workers with the 5th annual Aged Care Employee Day.
Heartfelt celebrations were held across the country, and ACCPA’s website was bursting with photos, videos and tributes to our dedicated workers.
As the population ages and demand for aged care increases, we need to promote the sector as a career of choice. The role of aged care workers is so important and does so much to improve the lives of older Australians.
The IGR shows just how important that work will be for the future.
Dr Graeme Blackman AO FTSE FAICD Chairman, Aged & Community Care Providers Association













A year of challenges and triumphs
How a shift in advocacy approach led to industry wins

It’s now been more than 12 months since I took over as CEO of ACCPA, so I find myself looking back at the year that was and the challenges facing the aged care sector that lie ahead.
It was certainly a baptism of fire. ACCPA was only a few months old when I started and there was a huge amount of work just to get the new organisation up and running. Aged care was also still reeling after the effects of the COVID-19 pandemic, and the shadow of the Royal Commission into Aged Care Quality and Safety had left the sector’s reputation in tatters.
I had come from the public health sector, which enjoyed a largely positive reputation – something that only grew during the pandemic. It’s fair to say the opposite had happened in aged care, despite the excellent work our members were doing every day.
I also discovered how incredibly resilient our sector is. Our members had faced the toughest challenges on a daily basis and yet they continued to turn up each and every day to meet them head on.
They made my job easier because so many of our members are fantastic leaders.
It still felt like an exciting time to be joining, with so many wonderful people and so much potential to make a difference to the lives of older people. It still does!
One of my first tasks was to change the way we advocated. There was a feeling that the way we had advocated in the past hadn’t always worked to the sector’s advantage and we needed to change direction.
I’ve drawn heavily on my history of representing hospitals and community health services to position us differently.
I’ve made a really conscious effort to change our tone and our approach, to ensure our public commentary is positive and solutions-focused.
I’ve made it my priority to position ACCPA – aged care’s largest industry organisation – as the peak body for reform.
While there are so many fronts to fight on, we’ve had wins along the way as a result of our new approach and the support of our members.
ACCPA worked tirelessly with the Australian Government to ensure that the 15 per cent pay rise for workers from July was fully funded to help alleviate crippling staff shortages, and we will continue to work hard as we enter Stage 3 of the Work Value Case.
We saw the strongest indexation rate for our sector in years included in the May budget, we won an extension to the hours of work for student visa holders, and we were successful in securing a 12-month delay to the implementation of Support at Home, so we can actually get those critical reforms right.
But there is so much more to do, and our next big focus is predictably on funding. More specifically, how aged care is funded now, and in the future.
Over half of residential providers are losing money on each and every resident, and home care is fast approaching a similar situation, which is simply unsustainable.
We can’t just keep slapping on band-aid solutions. Muddling along like we have in the past while the system slowly crumbles just isn’t good enough.
We need to overhaul and improve the sector to help make the lives of residents and consumers better, because that’s what they deserve. Australia deserves a world class aged care sector and older Australians deserve the best we can give them.
Currently Australia spends less than half as much on aged care than other developed countries per head of population –but the clock is ticking with demand set to double as more and more ‘Baby Boomers’ enter aged care.
In June, we hosted an Aged Care Summit at Old Parliament House, bringing together experts, economists and stakeholders to help thrash out a solution to aged care funding.
The Summit produced an issues paper for the Government to consider, which put forward a large range of options,
Join ACCPA - Australia’s national association for aged care.

some more controversial than others. (See the story on page 17.)
It asked questions such as: should those who can afford it contribute more towards their own care, or should government pay the total cost?
Is it fair that someone in a $10 million dollar mansion pays the same as someone with a modest home in the suburbs?
Should a portion of superannuation be used to help older Australians when they need help the most?
Are people willing to forego some of their inheritance to ensure their parents get the best possible care?
Should Australians of all ages pay a Medicare-type levy to fund aged care?

All of this brings us to the Government’s Aged Care Taskforce, which I am pleased to be a part of.
It’s the first real debate on aged care funding in two decades, so we need to get it right. It promises to find a solution to the questions left unanswered by the Royal Commission. There are many factors to consider and ultimately, it will be up to the Australian people to decide.
Tom Symondson Chief Executive Officer Aged & Community Care Providers AssociationAlbanese government drives unprecedented reform
An ambitious journey in partnership with providers
Our ambition for aged care is now becoming reality following reform implementation throughout 2023.
We have more than 100 reform projects currently active. However, we are not on this ambitious journey alone. I commend aged care providers and workers who have taken up this challenge, and are working with the government to lift the standard of care.
Importantly we are acting on the recommendations of the Royal Commission into Aged Care Quality and Safety.
We have funded a 15 per cent pay rise for aged care workers to help attract and retain staff, addressing critical workforce shortages.
We introduced the requirement for a registered nurse to be on-site at all aged care homes from 1 July this year.
The results are:
■ on average, there is a registered nurse onsite in aged care homes 98 per cent of the time
■ on average, there is a registered nurse onsite in aged care homes for 23.5 hours a day
■ 86 per cent of facilities now have a nurse on site 24/7
■ the majority of the remaining homes are very close to 24/7 coverage.
We are also working to make sure residents get better food through a partnership with the Maggie Beer Foundation, instituting a dedicated food and nutrition hotline while we have also introduced six additional Quality Indicators.
Star Ratings, which we launched in December last year and updated quarterly since, show us the sector’s efforts are working.
We’ve seen continuous improvement so that 97 per cent of aged care homes are now meeting or exceeding the level of care expected.
The Serious Incident Response Scheme has been extended to home and community care services.
We’ve ensured accountability at all levels of an organisation, not only with those involved in direct care. Looking forward, the Aged Care Taskforce is reviewing funding arrangements for aged care.
The Government is committed to an aged care system that is fair and equitable both for older people who contribute to the cost of their care and for working people who support aged care through their taxes.

The Albanese Government is the majority funder of aged care, paying an estimated $30 billion in 2022-23. This is expected to increase to $36 billion in 2023-24.
The Royal Commission’s great unanswered question remains – how to make aged care equitable and sustainable into the future.
The Aged Care Taskforce is assessing this question and will provide the Government with options for consideration when it completes its final report in December 2023.
Work is also progressing on the new Aged Care Act, which will put older people front and centre.
I look forward to learning more about the ideas submitted through the consultation process, which closed last week.
We are working our way through the many responses.
We have an ambitious reform agenda and together we will improve care for older people.
The Hon Anika Wells MP Minister for Aged Care
AGED CARE ADVISORY SERVICE HAS A RANGE OF SKILLS AND EXPERTISE TO SUPPORT APPROVED PROVIDERS WHEN THEY NEED IT MOST
ADVISORY SERVICES
• Our experienced Advisory Team has been appointed to multiple aged care providers.

• Extensive experience in consulting and senior operational roles ensures we are well positioned to support residential aged care providers who are required (often at short notice) to appoint an Eligible Advisor and/or Administrator.
• Together with resolving Sanctions and Notices to Agree, we have resolved some of the largest COVID-19 outbreaks in Australia.
• All consultants are experienced and insured as appropriate, are resident focussed, and experienced in mitigating serious risk.
• Consultants and Assessors experienced in both Residential and Home and Community services, can provide Independent Audits against the Aged Care Quality Standards for Residential and Community Care providers.
• Our service is inclusive of upskilling your existing team to create sustainability and develop skills across the team from the board room to the floor.


INTERIM MANAGEMENT – CLINICAL, OPERATIONAL AND SENIOR ROLES

• Aged Care Advisory Service can support aged care providers with unforeseen vacancies. Vacancies often cause significant disruption to business, leaving your home vulnerable to compliance issues, increased unresolved issues including funding gaps, complaints and human resource issues.
• Our interim management and clinical management services provides a solution that allows providers to focus on recruitment without pressure to “fill a role”.
• Care Planning and Assessment services can provide you with experienced RN resources to rectify identified gaps, whilst transferring sustainable skills and processes to your team.
• Additionally, these services can be used to provide coaching, and mentoring should you identify a team member who needs support to step into a more senior role, or who has skills gained in a non-aged care setting.
www.agedcareadvisoryservice.com.au
Strengthening provider governance
Delivering the aged care system that older Australians deserve
Providers are the first to recognise that they need the right mix of people to drive the continuous improvement processes required to deliver highquality care and services.
Amendments made in late 2022 to the Aged Care Act 1997 and Aged Care Quality and Safety Commission Act 2018 strengthened the governance arrangements of approved providers.
The changes provide a clear pathway to securing a better future for older Australians by valuing independence, expertise and diversity in those holding governance roles. This strengthening of governance is being implemented over a 12-month period, with some changes already in effect and more to commence on 1 December 2023.
Currently all approved providers must:
■ assess the suitability of key personnel at least once a year
■ submit material changes, including key personnel notifications, within 14 days, to the Commission
■ submit annual provider operational reports to the Department of Health and Aged Care.
From 1 December 2023, providers approved before 1 December 2022 must also:
■ ensure that their governing body is made up of a majority of independent non-executive members who have a mix of skills and experience, and that at least one member has experience in providing clinical care
■ set up and continue a quality care advisory body
■ annually offer to set up at least one consumer advisory body
■ prioritise older Australians (not the holding company) if the organisation is a wholly owned subsidiary.
Governing bodies have ultimate responsibility for and influence over the care and services provided to older people.
A board member or members with clinical experience will have an important contribution to make to the governing body’s consideration of and decisions about clinical aspects of care.
When appointing someone who meets this requirement, the most important element to consider is whether the individual has clinical qualifications and experience relevant to the types of care and services that a provider delivers.
The legislation does not specify who qualifies as an independent non-executive member. Each organisation needs
to consider the independence of proposed members and whether the person’s interests, positions and relationships enable them to bring independent judgement to issues considered by the governing body.
Providers preparing to fulfil governance obligations that apply to them from December 2023 should be well-progressed in reviewing and amending their policies, procedures and arrangements as appropriate.
These preparations should include development of a communications plan to enable those receiving aged care to understand and participate in what is happening.
This is particularly important in relation to the obligation for providers to offer their consumers the option of establishing a consumer advisory body.
Consumer advisory bodies not only give older Australians a voice in the design of their care, but also provide valuable feedback to governing bodies. Successful providers use this information to implement changes in care arrangements that matter to those receiving it.
To support providers in undertaking work to prepare for the changes, the Commission has made available to all providers, and will continue to build on:
■ online resources such as guidance materials, fact sheets, videos and posters
■ enrolment for senior executives and board members in the Governing for Reform in Aged Care program
■ online learning programs through the Aged Care Learning Information Solution (ALIS)
■ webinars on key reform measures to have their questions answered.
The aged care sector’s reform journey is now well underway. Central to our collective success in translating the new provisions into improved experiences of care will be the close attention we pay to understanding what is required to manage, implement and embed these changes to deliver high quality care and services for every care recipient.
I encourage you to stay in touch with the Commission’s updates on the reforms, including new resources and activities, by regularly visiting our website and subscribing to the monthly Aged Care Quality Bulletin.
Janet Anderson PSM, Commissioner, Aged Care Quality and Safety Commission www.agedcarequality.gov.au


We offer great incentives on top your hourly wage and super, including $150 per working day and a $100 meal allowance per day on placement plus, we arrange and pay for your travel and accommodation.
Rural and remote aged care services need our support, and with your help, we can alleviate workforce shortages and reduce burnout.

+ Registered and enrolled nurses
+ Aged care facility managers
+ Care coordinators + Personal care workers
Funding reform needed
Key outcomes of the ACCPA Financial Sustainability Summit 2023
Australia’s population is ageing. According to the Australian Institute of Health and Welfare, more than 4.2 million Australians are currently aged 65 or over, representing 16 per cent of the population. By 2066, that figure will climb to almost a quarter of the national population.
This inescapable reality means that demand for aged care services will continue to increase, while the proportion of the Australian working population decreases.
At the same time, chronic underfunding for aged care services has resulted in an unsustainable sector – negatively impacting the standard of care older Australians receive.
The Royal Commission into Aged Care Quality and Safety confirmed what has been known to many within the industry for decades: a poorly funded aged care sector compromises service delivery and results in substandard care.
Currently, the long-term financial viability of the sector is at risk with the majority of residential aged care facilities operating at a loss. As highlighted by the StewartBrown report in March, the viability of home and community care providers also continues to trend down, highlighting the unsustainability of current aged care funding. The way Australia funds aged care, which has remained relatively unchanged for decades, needs to be modernised.
The key question is how we balance the fairness of asking older Australians with financial means to make a greater financial contribution to their own care, against the fairness of asking a shrinking percentage of working-age Australians to fund a growing aged care system through their taxes.
To get input from the industry and stakeholders, the Aged and Community Care Providers Association (ACCPA) hosted a Summit at Old Parliament House, Canberra on 1 June 2023, as part of its contribution to the national conversation on the future sustainability of aged care.
Forty-three organisations representing consumers, providers, unions, experts, government bodies and other interest groups, came together in a spirit of cooperation to discuss long-term policy solutions the Australian Government should consider.
Following the views expressed at the Summit, combined with follow-up submissions, a subsequent Issues Paper identified ten principles for consideration in the design of a sustainable aged care system in Australia:
1. Independent and person-centred. Maintaining independence as we age is critical and can be central to a person’s identity and sense of self; many people wish to age in their own homes and community.
2. Efficient. Financing systems should be integrated across health and aged care and should consider efficiency in aged care delivery.
3. Transparent and specific. It should be clear who is paying for what in the aged care system.
4. Equitable. Every person in Australia should have access to high-quality aged care, regardless of their location, income or financial means.
5. Means-tested. Those with financial means should pay for or make a contribution to their accommodation and lifestyle expenses.
6. Flexible design for First Nations aged care. There should be an appropriate and tailored funding system for First Nations aged care.
7. Universal. The Government should continue to be the primary funder of care.
8. Future-focused. The aged care system should aim to support quality into the future, rather than maintaining the status quo
9. Guaranteed. Service levels should be guaranteed, including for thin markets, which requires appropriately skilled and supported aged care workers.
10. Inter-generationally fair. Aged care funding should be designed for the long term, be predictable and be sustainable.
Australia needs to urgently modernise its aged care funding model. This is particularly critical given Australia’s population will progressively age over the next 20 years, and the parallel expectation in the community to improve the quality of care and supports older Australians receive.

While funding alone will not solve all of the problems in aged care, the current financial situation makes solving those problems impossible.
As per Summit participant views, our Issues Paper proposes that the Australian Government continue to be the primary funder of care services – as they are for Australians throughout their lives through the NDIS, Medicare and the public health system.

People should not be treated differently simply because they are over the age of 65, regardless of whether they are still living in the community or in a residential aged care home. However, for those who can afford it, there should be consideration of increased consumer co-contributions in aged care for accommodation and lifestyle expenses, which people have funded throughout their lives.
We can no longer put off the structural reforms needed to ensure older Australians receive the care, dignity and quality of life they need.
Anne Liddell, Head of Policy, Aged & Community Care Providers AssociationTo read the Issues Paper visit: www.accpa.asn.au/mediareleases/financial-sustainability-issues-paper/
The secret to ageing well is simple, eat well.
Developed by dietitians and prepared by chefs, Lite n’ Easy offers more than just a weight loss solution. We also offer nutritious, delicious meals, designed to promote independence, choice & well-being.

• Plenty of variety and choice with over 235 meals designed for weight loss and healthy convenience.
• My Choice range of dinners, soups and desserts designed for older people with smaller appetites.
• Highest quality ingredients.
• Flexible options, no lock-in contracts or subscriptions, and home delivered.
• Approved HCP recipients can take advantage of the government subsidised split payment method, saving up to 70% of the cost.
• Business-to-business commercial opportunities.
Attending ACCPA National Conference in October? Come and visit the My Choice by Lite n’ Easy exhibit for more information and to sample some of our delicious, nutritionally balanced meals from breakfast until close across all three days of the conference.
Tips for avoiding the underpayment and overpayment of staff
During times of significant change and financial stress, the last thing that an aged care provider wants is to accidently underpay or overpay their staff. The following three tips can assist aged care providers to avoid underpaying or overpaying staff.

Be prepared for the next increase in wage rates and allowances
Increases to modern award wage rates and allowances generally happen from the first full pay period on or after 1 July each year and these flow from the Annual Wage Review Decision of the Fair Work Commission (FWC).
The amount of the increase for wages in awards is announced by the FWC in early- to mid-June. It is then approximately two weeks until the new wage rates and allowance rates are published by the FWC.
At this time, Aged & Community Care Providers Association (ACCPA) sends out Information Sheets on the updated award rates, as a service to all members.
It is advisable to mark this period in your calendar as the time to prepare for new pay calculations, ensure that they are entered into the payroll system and run a check prior to the first full pay period (or as close to that time as possible).
If staff are covered by an enterprise agreement, it is good practice to read the agreement and understand when any changes are to occur with its conditions. Increases in rates in an enterprise agreement generally occur at set dates during the life of the agreement, so providers have ample warning for forward planning.
It is also important to ensure that your organisation is paying no less than the higher of the applicable wage rate in the enterprise agreement or the equivalent modern award rate. Given that there have been higher than usual increases from recent Annual Wage Review Decisions that may be higher than increases in enterprise agreements, it is good practice to check the agreement rates versus the comparable award rates after the Annual Wage Review Decision in June.
Consider undertaking a payroll audit
An audit to check that the correct rates and business rules have been entered into the payroll system can be undertaken
at any time to ensure that your organisation is compliant with the applicable award or enterprise agreement. It can be a useful option especially if there has been turnover in the roles at your organisation that have had responsibility for managing or undertaking payroll activities.
A payroll audit is not just about determining whether the correct rates have been paid over a specific period, it should also assess whether the payroll system has the correct business rules entered. It is the business rules in the payroll system that determine, for example, when penalties and overtime are to be paid according to time worked. If these aren’t entered in compliance with the applicable industrial instrument (the award or enterprise agreement) then an underpayment or overpayment will occur.
There are several ACCPA partners that are experienced in payroll audits for aged care providers and these Partners are listed on the ACCPA Partner Directory (www.accpa.asn.au/ partner-directory).
Get reliable advice on wage rates and allowances and how they are to be applied
It is important that providers have access to a reliable source of advice on the application of wage rates and allowances and other employment issues. Staff do not always have the skills and experience necessary to be able to handle these issues by themselves. Even for staff with strong skills in this area, it is helpful for them to be able to have access to someone they can bounce ideas off, to check they are making the right decisions.
There are a number of organisations that offer employment relations advice. It is important to do your homework and make sure you get advice from an organisation that has strong knowledge and experience with employment matters, to get the quality advice that you are paying for.
ACCPA members have access to the ACCPA ER Advisory Service for industry-specific advice on employment matters including pay rates – so if you’re a member and you haven’t made use of this service, reach out today to access the right advice and make the most of your member benefits.
Claire Bailey, Head of Workplace Relations, Aged & Community Care Providers Association www.accpa.asn.au/employment-relationsHow ACCPA lends a helping hand to providers across Australia
Governance is front and centre in aged care reform
Find out how ACCPA can help you remain compliant
Governance is not new; the principles of good governance are well documented and there are many recent examples of failings arising from inadequate corporate oversight.
With its role in delivering quality care highlighted in the Aged Care Royal Commission, strengthening provider governance is central to the Australian Government’s ongoing aged care reform agenda. These reforms introduce measures that aim to build capacity and ensure the consumer and quality of care they receive is at the heart of all governing body decision making.
Good governance in aged care requires a commitment to quality, safety and compassion and is essential for ensuring older people receive the care and support they need to age with dignity and respect.

What does good governance look like?
Today, governance is complex but not necessarily complicated. Providers need to be hyper vigilant not only to remain compliant, but also to fulfil their responsibilities to the consumers who place their trust in them.
Good governance entails:
■ ethical and responsible leadership that promotes the best interests of the older person, community and organisation
■ effective and efficient use of resources to deliver high quality care and services that meet the needs and preferences of the older person
■ open and transparent communication with the older person, families, carers, staff and other stakeholders about the care and services provided and outcomes achieved
■ robust systems and processes for risk management, quality assurance and continuous improvement including regular monitoring, evaluation and reporting
■ adequate training, support and supervision of staff to ensure they have the skills, knowledge and attitudes necessary to provide person-centred care
■ collaboration and partnership with other agencies, governments and communities to address emerging issues and promote the well-being of older people and
■ recognition, respect and protection of the rights and dignity of older people including their autonomy, privacy and cultural diversity.
What is the role of the governing body?
The governing body is accountable for ensuring the organisation meets its responsibilities as an approved provider of aged care therefore, members require honed leadership skills, firm experience across all aspects of aged care operations, and strategic foresight to envision the ongoing delivery of sustainable care into the future.
Members of the governing body must have the knowledge and capacity to challenge thinking and ensure their decisions are informed primarily by a focus on the wellbeing of the consumers in their care.
Reforms have introduced specific requirements regarding the composition of the governing body and suitability of its membership, which means providers should take active measures such as conducting a skills audit of members to confirm capability exists or identify areas where professional development or composition changes may be required to address gaps.
Governance support for aged care providers
Aged & Community Care Providers Association (ACCPA) has developed a Governance Framework which describes contemporary governance in aged care and offers support to providers to achieve good governance regardless of their size, structure and current capability.
The Framework builds on the Strengthening Provider Governance resources available from the Aged Care Quality and Safety Commission and offers providers practical tools, products and services to meet the reform expectations including:
■ free resources for members describing good governance at corporate, operational and clinical levels including manuals covering the function and operations of the governing body and a clinical governance framework
■ discounted subscriptions for members to two quality management platforms, the ACCPA Safety & Quality Management System and ACCPA Quality Portal both of which provide an extensive suite of tools and resources to guide and support good governance (www.accpa.asn.au/ quality-compliance)
■ scheduled and on-demand training and professional development opportunities on leadership, board governance, and clinical governance (www.accpa.asn.au/ professional-development)
■ bespoke consultancy support or coaching to the governing body on their accountabilities and the reform agenda (www. accpa.asn.au/consultancy)
■ discounted subscriptions for members to partner products and services such as the ACCPA Board Management Portal powered by Convene.
A copy of the Framework can be obtained by contacting membersupport@accpa.asn.au and non-members that would like to find governance support through ACCPA are welcome to get in touch to find out more.
Amanda Allen, Head of Services, Aged & Community Care Providers Association www.accpa.asn.au
AGED CARE SUPPORT SPECIALIST

National Care Solutions is ready to work with you to achieve maximum outcomes for your residents and business though contemporary ethical methodologies. We deliver Face to Face & Online Consultancy and training services to meet client specific needs.
National Care Solutions is a professional customer focused aged care specialist company focusing on consultancy management and training for residential and home care providers. We have been working successfully with providers for over 17 years to bring about positive outcomes. NCS specialises in providing assistance for services of all sizes, including rural and regional standalone services.
Specialty areas include:
• Accreditation and remediation issues
• Application writing
• Policy review and management
• Zoom and face to face training
• AN ACC Management and training
Contact Lyn Turner, Director
P: 0418 733 786 E: lyn@nationalcaresolutions.com.au
www.nationalcaresolutions.com.au
Healthier meals, home delivered
You’ll just love the homemade taste
For over 27 years Tender Loving Cuisine has been serving the community with care, compassion and respect. Australian Made and Owned, our health accredited, home delivered meals cater for dietary requirements with all meals developed and supported by independent review. Our extensive menu also includes selections that are Dairy Free, Low Salt, Gluten Free, Heart and Diabetes Friendly. Our purpose is to assist clients to maintain their dignity and independence.
Assured nutrition, great taste, strict dietary controls and dedicated customer service is at the heart of what we do. With a trusted reputation and Industry Recognition, Tender Loving Cuisine sets the standard in quality and reliability. We proudly provide meals in Aged Care Packages, NDIS, CHSP and the general community in areas of QLD, NSW, ACT and VIC. Contact us for brochures or futher information, we’re here to help!

For over 200 years, HARTMANN has been at the forefront of medical innovation - improving consumer/ resident outcomes with solutions in advanced wound care, continence promotion and skin care.





Together we shape the future of aged care and deliver person-centred care.

New workshop series for retirement living and seniors housing managers
Building brand reputation through skilled management
Older Australians are living longer, and are increasingly choosing accommodation that provides a low maintenance lifestyle, in a safe and protected environment.
Retirement living villages today are equipped with a range of recreational facilities, which support independence and wellbeing and offer social interaction and connection with others.
For older people desiring to ‘age in place’, these are fundamental drivers, when contemplating alternative accommodation options to traditional suburban home ownership.
Now more than ever before, retirement living and seniors housing settings pose operational and managerial challenges that require skilled, adaptive and resourceful leaders, committed to ensuring that all residents live harmoniously, in well maintained accommodation settings.
Today’s older Australians, dubbed by some as the ‘picky Baby Boomers’, are more discerning regarding their expectations, than previous generations, however the predicted increase in dementia-related illnesses and complexity of chronic health conditions, is creating challenges for those entrusted to manage independent living options.
Designed for people over 55 years of age, the majority of residents entering retirement living villages are aged in their early-to-late 70s, with villages having an average age of 81 years.
At these older ages, the prevalence of dementia will mirror the national rates of disease progression. This will increasingly require linkages between dementia support services to help families with their decision making.
To be successful, managers and front-facing employees working in retirement living and seniors housing will need to be equipped with specific skills and knowledge.
Building on the successful the Aged & Community Care Providers Association (ACCPA) National Retirement Living Virtual Forum in August 2022, ACCPA has developed the Retirement Living & Seniors Housing Operational Managers Program, in response to feedback from operators.

Running from September 2023 to August 2024, the workshop series explores the essential role capabilities that support effective management and the key human skills that support better communication with team members and with older people and their families.
The program is delivered as modules, with three workshops in each module, and aims to build capacity in retirement living and seniors housing operations, with practical strategies and resources to help managers deal with conflicting demands.
Each workshop topic is delivered by industry specialists and has been selected in response to feedback from the sector, and from participants engaging in ACCPA’s events and Member Advisory Groups.
The exclusive program provides an opportunity for networking and the confidential sharing of strategies to address key issues and concerns.
Throughout the program, leaders will:
■ learn the essential tools of management that ease the workload, embrace the freedom that proper planning and execution provides, and explore key asset management principles and practices
■ build resilience by understanding what motivates others, gain awareness of dementia and associated behaviours, and learn how to promote psychological safety and self-care
■ deliver service excellence and memorable customer experience, manage conflict calmly and resolve disputes and complaints with confidence.
To maintain professional currency, increase and broaden knowledge, expertise and competence in the sector, the program offers 22 Continuing Development Points (CPD), endorsed by ACCPA.
Retirement living and seniors housing operators are encouraged to register their leaders for this outstanding program, developed specifically for the sector.
Tegan Roberts, Manager Learning & Professional Development, Aged & Community Care Providers Association www.accpa.asn.au/retirement-living
Future gazing in retirement living
Meeting consumer demands, boomers and beyond
The Australian retirement village sector is experiencing a significant shift in focus as it prepares to meet the demands of the baby boomer generation and beyond. Born between the mid1940s and early 1960s, baby boomers bring with them unique expectations and preferences.
This generation has redefined various life stages throughout their lives, and their approach to retirement living is no exception.
To thrive in the future, the retirement village sector must adapt to the evolving needs and desires of baby boomers, while remaining open to the demands of subsequent generations.
Customise and personalise
Baby boomers are known for their individuality and desire for personalised experiences. As they approach retirement, they seek retirement living options that cater to their unique preferences and needs.
The future of the Australian retirement village sector will likely include a wide range of customisable services and amenities.
Village operators will need to offer a diversity of accommodation styles, such as apartments along with supported and shared living spaces to accommodate various lifestyles and budgets. Stand-alone villas or houses are still very popular but for new developments they are ‘land-hungry’ options.
Additionally, flexible care packages will be essential, allowing residents to tailor their support services according to their specific health and wellness requirements.
Village operators must develop a care strategy, whether that is being co-located with residential aged care, having a relationship with a provider close by or providing Home Care Packages (HCP) to support residents who may need it.
Baby boomers may have grown up in an analog world, but they are increasingly embracing technology in their daily lives. The future of retirement villages in Australia will incorporate innovative technologies to enhance convenience, safety and social connectivity.
Smart home features, wearable health monitors, virtual healthcare consultations and communication platforms will become standard offerings to cater to tech-savvy baby boomers.
Healthy, active and social living
Unlike previous generations, baby boomers are less likely to view retirement as a time of rest and inactivity.
They seek retirement living options that enable an active and socially engaging lifestyle. They will look for a wide array of recreational facilities and community spaces, such as fitness centres, pool, hobby rooms, social lounges, café and communal gardens.
Although we are likely to see the boomers maintain a healthy and independent life for much longer, they will seek out regular social events, group activities and organised outings. These play a vital role in fostering a strong sense of community and companionship.
Most boomers prioritise their health and wellbeing, and retirement villages should reflect this emphasis on holistic care.

Village operators that provide comprehensive health and wellness programs, encompassing physical fitness, mental health support, nutrition guidance, and access to healthcare services, will have a competitive edge.
Embracing alternative therapies such as naturopathy, massage and wellness practices (such as yoga, meditation and mindfulness) will also appeal to the wellness-focused mindset of baby boomers.
Baby boomers are keen on maintaining their independence for as long as possible, and the concept of ‘ageing in place’ is particularly important to them.
Residents will want to transition smoothly between different levels of care within the same community.

Many operators currently run a co-located business model where residential aged care is also available within the same community.
HCPs are also offered to residents of the retirement village to provide support and services to maintain independence within their own apartment.
This flexibility will accommodate changing health needs while preserving the strong social connections forged within the retirement village.
For villages that continue to ignore the need for a care strategy, the end may be nigh.
Sustainable living
As an environmentally conscious generation, baby boomers are increasingly interested in sustainable and eco-friendly living options. Villages of the future will adopt sustainable construction practices, energy-efficient design and renewable energy sources.
Examples may be large underground water tanks connected to garden irrigation and toilets; solar panels on the roof providing free electricity throughout the day to common area lighting cooking and heating; and electric vehicle charging stations in the village car parks. In addition, access to nature, green spaces, and eco-friendly amenities will be attractive to baby boomers seeking a retirement environment that aligns with their values.
The future is bright for our sector if we pay attention to the demands and preferences of those seeking our services. The baby boomer generation seeks personalised, active and socially connected retirement living options.
By embracing technology, customisation and sustainability, and providing comprehensive health and wellness programs and age-in-place solutions, retirement villages will continue to thrive and be in demand for future generations.
Paul Murphy, Member Advisor –Retirement Living & Seniors Housing, Aged & Community Care Providers Association www.accpa.asn.auTransitioning to the new support at home program
Uplifting CHSP provider capability ahead of the aged care reforms
Sector Support and Development (SSD) is a national Australian Government initiative designed to help Commonwealth Home Support Program (CHSP) providers enhance their capability and quality of services in preparation for the transition to the new Support at Home program (SaH).
With the launch date pushed back to 1 July 2025, this has allowed existing grant arrangements for CHSP to be extended by another year (until 30 June 2025).
The SaH program details (now available at health.gov.au/topics/aged-care/ aged-care-reforms-and-reviews/ reforming-in-home-aged-care) include a trial to test products and services for a new assistive technologies loan
program early next year, a study of higher levels of care, refinement of classifications resulting from the Integrated Assessment Tool, and a trial of alternative funding models in CHSP community transport and delivered meals in 2024-25.
Across Australia, SSD teams are working collaboratively to demystify the reform process by ensuring providers have access to key information – and to support them through the reform process.
In New South Wales, the Australian Capital Territory and South Australia, SSD is being delivered by the Aged & Community Care Providers Association (ACCPA), while in other states and territories, CHSP providers can learn more about supports available to assist them through the transition process via their local SSD network.
Ann Mehaffey, ACCPA’s SSD Team Leader in NSW and ACT, says the Australian Government is committed to helping CHSP providers transition smoothly to the SaH program.
“Some CHSP providers may feel lost in this ocean of information, and that is why the SSD program was developed, to provide additional support during the transition period,” she said.
Keeping CHSP providers updated is key. A cascading approach to information sharing sees ACCPA’s policy team sharing a monthly reform update to the National SSD network for distribution regionally and locally.
A national monthly webinar focuses on the reform frameworks plus ‘tips and tricks’ from providers about how to ‘get it right’. Topics have ranged from transition fundamentals, governance, compliance and business practices, to client conversations and expectations.
Our SSD team also recently organised regional face-to-face workshops in NSW and SA, while planning for an online version of these workshops has begun, in order to reach a national CHSP audience and explore the new quality standards in-depth.

“These Aged Care Quality Standards & Quality Review Process workshops demonstrate nice collaborations between ACCPA consulting and local CHSP providers,” says Craig Frost, ACCPA’s SSD Team Leader in SA.
As the changes to in-home aged-care are designed to support older people living in their own home to be safe and well, to choose the services they want, make changes as needed and to understand what their money pays for – SSD activities also focus on how providers can best do this.
ACCPA’s SSD team is a key driver of the annual Support at Home Online National Conference held in November.
This Conference is a unique opportunity to hear the voices of community members, volunteers and staff from diverse communities celebrating how older people do and can live well at home.
In NSW, an SSD partnership has created a set of short amination videos in six different languages to help older people understand the aged care system. Launched in late August, these videos cover My Aged Care, fees, maintaining independence, self-managing packages, wellness and re-ablement, plus an introduction to the new SaH program.
Upskilling CHSP providers is another important element of the SSD program.
In SA for example, the Older Person Mental Health First Aid face-to-face training series is co-delivered with Mental Health First Aid Australia.
Rosie Mangan, from the SA SSD team says, “Under the current mental health situation among older Australians, we feel an urgency to enhance the awareness and response capabilities for CHSP staff in dealing with sudden mental health crises among older people.

“These courses are facilitated by an experienced and knowledgeable mental health training provider through real life cases and examples.”
ACCPA’s SSD team also facilitates the Mental Health Awareness & the Older Person Webinar Series, and the Helping Older People Who Hoard Webinars. These national online series aim to help CHSP providers explore the causes
and symptoms of mental illnesses in an older person and identify the best ways to provide support.
If you are a CHSP provider, be sure to visit the SaH program page on the ACCPA Workforce Hub to check out our ongoing programs and workshops that would benefit your organisation.
Helen Li, Services & Sector Capacity Program Campaign Officer, Aged & Community Care Providers Association www.employment. agedservicesworkforce.com.au/ support-at-home-information-hub
Contact Ann Mehaffey
ann.mehaffey@accpa.asn.au or Craig Frost craig.frost@accpa.asn.au at ACCPA for more information about the SSD program in your state or territory.
• Registered Nurses
• Endorsed Enrolled Nurses
• Assistant in Nursing Cert 3 & 4
• Special Project Coordinators specialising in supporting facilities ready for accreditation
• COVID 19 Support Staff
LOOKING FOR SUPPORT
• Filling last minutes shifts
• Ongoing shifts
• Block bookings
• Contracts
• Part Services
• Permanent Recruitment
• Assessment Centre to cater for your bulk recruitment needs
• “Managed Service Arrangement” –Managing your agency usage
NNPLUS CAN GIVE YOU THE STAFF YOU NEED SPEAK WITH US TODAY FOR MORE INFORMATION
www.nnplus.com.au or call 1300 158 440
Use

Integration with clinical care software completes the puzzle by automating data flow between clinical and catering

Our core product Catering is key to an e cient food service and the heart of the resident dining experien
Survey residents and family members and tailor menus based on true resident preferences
Lead and grow team with best practice ca delivered online
with multi-cultural events, complemented by themed recipes and activities
Plan menus right from the start with fully costed menus, recipes and ingredients

AGED CARE EMPLOYEE DAY 2023
It’sawrap!
AGED CARE EMPLOYEE DAY 2023 It’sawrap!

01 Minister for Aged Care Anika Wells acknowledged the day saying, “I am so grateful for the important work that aged care workers do, day in, day out.”
01 Minister for Aged Care Anika Wells acknowledged the day saying, “I am so grateful for the important work that aged care workers do, day in, day out.”



02 A live cross on the day with Emerald Hill in South Melbourne. Seated at the front are aged care worker Lochlan McLachlan and 92-year-old resident Edith Amy. Lochlan says, “I’m privileged to be able to work for and care for some wonderful people. And to be able to do that every day is a real blessing.”
02 A live cross on the day with Emerald Hill in South Melbourne. Seated at the front are aged care worker Lochlan McLachlan and 92-year-old resident Edith Amy. Lochlan says, “I’m privileged to be able to work for and care for some wonderful people. And to be able to do that every day is a real blessing.”
03 Chef Manager Rachna (Kimi) Power is one of hundreds of VMCH staff and volunteers working within residential, home and community aged care across Victoria. Kimi shows her love through cooking delicious and nutritious food for residents at VMCH’s John R Hannah home. “I feel blessed to have the skill and ability to deliver hearty, homecooked meals for our residents. Seeing their empty plates gives the same joy as feeding my own family,” says Kimi.
03 Chef Manager Rachna (Kimi) Power is one of hundreds of VMCH staff and volunteers working within residential, home and community aged care across Victoria. Kimi shows her love through cooking delicious and nutritious food for residents at VMCH’s John R Hannah home. “I feel blessed to have the skill and ability to deliver hearty, homecooked meals for our residents. Seeing their empty plates gives the same joy as feeding my own family,” says Kimi.


Aged Care Employee Day – held annually on 7 August – has become an important date in our calendar and reminds us of the caring and professional work of our aged care staff. They’re the backbone, the people who support our elders day in and day out. They make the lives of older Australians better.
Aged Care Employee Day – held annually on 7 August – has become an important date in our calendar and reminds us of the caring and professional work of our aged care staff. They’re the backbone, the people who support our elders day in and day out. They make the lives of older Australians better.
Our staff have faced the most challenging of conditions and have been tested to the limit during the COVID-19 pandemic, but they’ve proven to be care ‘superheroes’. They’ve provided essential care to their beloved older residents, while colleagues were struck down with COVID-19 or forced to isolate.
Our staff have faced the most challenging of conditions and have been tested to the limit during the COVID-19 pandemic, but they’ve proven to be care ‘superheroes’. They’ve provided essential care to their beloved older residents, while colleagues were struck down with COVID-19 or forced to isolate.
Be they personal carers, nurses, kitchen and laundry staff, diversion therapy staff, allied health professionals, administrators, gardeners or volunteers, they have all worked above and beyond the call of duty to keep our vulnerable older Australians cared for and safe.
Be they personal carers, nurses, kitchen and laundry staff, diversion therapy staff, allied health professionals, administrators, gardeners or volunteers, they have all worked above and beyond the call of duty to keep our vulnerable older Australians cared for and safe.
Media interest on the day was strong, with coverage on radio and newspapers across the country, plus an inspiring interview on the Seven Network’s Sunrise program, and a heartfelt story on National Nine News.
Media interest on the day was strong, with coverage on radio and newspapers across the country, plus an inspiring interview on the Seven Network’s Sunrise program, and a heartfelt story on National Nine News.
ACCPA has worked tirelessly with the Australian Government to deliver a fully funded 15 per cent increase in the award rates for aged care workers because they deserve it. We’re continuing to advocate for all workers in stage three of the Fair Work Case.
ACCPA has worked tirelessly with the Australian Government to deliver a fully funded 15 per cent increase in the award rates for aged care workers because they deserve it. We’re continuing to advocate for all workers in stage three of the Fair Work Case.
Hosted by the Aged & Community Care Providers Association (ACCPA), Aged Care Employee Day is all about encouraging residents and clients, their families and friends, to join us in saying ‘thank you for a job well done’ and recognise the hard work of aged care staff in caring for our loved ones.
Hosted by the Aged & Community Care Providers Association (ACCPA), Aged Care Employee Day is all about encouraging residents and clients, their families and friends, to join us in saying ‘thank you for a job well done’ and recognise the hard work of aged care staff in caring for our loved ones.
We wanted to keep in mind the almighty effort put in by aged care workers and encourage the public to take a moment and say, ‘thank you for caring’. We also wanted to encourage aged care staff to take a moment for themselves to regroup, take a breath and recharge.
We wanted to keep in mind the almighty effort put in by aged care workers and encourage the public to take a moment and say, ‘thank you for caring’. We also wanted to encourage aged care staff to take a moment for themselves to regroup, take a breath and recharge.


04 To celebrate the day, Peninsula Villages on the NSW Central Coast hosted a BBQ lunch for all staff, cooked by the executives. They also held a raffle, giving staff members an opportunity to win a range of prizes. Residents showed their appreciation by writing messages of gratitude on paper hearts. Pictured are staff members L-R: Samjhana Deuja KC, Leanne McLeod, Belinda Montague and Carolyn McKeon.
05 Clinical Care Coordinator Romina Rios Olivares, from Whiddon Easton Park in Sydney, says, “To work in aged care is a privilege not a burden, because we’re part of the final stages of life, just like a birth is an important stage in life, death is equally as important. Our impact on each individual journey is vital.”

06 Uniting with aged care workers across Australia, staff at Muroona Gardens in sunny North Queensland’s Bowen are in it because they care.
07 Staff from Home Instead – a national provider of relationship-based in-home care for ageing Australians – made a video to acknowledge the day.

08 ACH Group CEO Frank Weits says Aged Care Employee Day is important for the sector and the wider community. The South Australian aged care provider celebrated the day by delivering fresh food hampers to each of its 1,900 employees.
09 Jenny Boettcher, currently an Assistant in Nursing at Carinity Wishart Gardens in Brisbane, has devoted 30 years to aged care and says she is passionate about caring for older people with dementia.

10 Clinical Service Manager Somlata Gautam, who works at Rosewood in West Perth, took the opportunity to thank aged care workers for their “hard work and dedication”. 07



They all deserve our thanks for their professionalism, their warmth and their enthusiasm to help older Australians live comfortably. ACCPA congratulates our aged care heroes for their dedication, their compassion and their hard work.
04 08
Caring for another human being is one of the most important things we can do. We acknowledge the incredible work of every team member involved in the care of more than 1.5 million older Australians receiving home care or residential care services. There are almost 427, 000 people employed in the aged care sector taking care of our parents, grandparents and loved ones every day. The vast majority – over 277,000 people –work in residential aged care.
Care work is hard work. It’s physical work, and its emotional work, but because of this work older Australians can live the lives they deserve.
To all aged care workers across Australia, no matter how you contribute, thanks for caring and thanks for the joy and dignity you bring to so many people, every day of the year.
Tom Symondson, Chief Executive Officer, Aged & Community Care Providers Association
Delivering quality dementia care
Communication is the key
Communication is an intrinsic element in all of our lives. We are surrounded and involved in many forms of communication with people who we connect with every day.
As changes occur for a person living with dementia, it becomes increasingly important to consider all forms of communication. It’s not just a skill or tool that we use, but part of every single engagement we have with others. It’s deeply embedded into our lives, so it can be done subconsciously without consideration, and yet has the ability to deeply impact another person’s wellbeing.
Understanding communication changes
Dementia affects people in different ways. Changes in communication are common and as dementia progresses, communication can become increasingly difficult which can be frustrating and upsetting.
It can include speaking fluently but not coherently, or it may be hard for a person to express themselves clearly or understand what others are saying.
Changes can occur from the physical and social environment, from changes occurring in the brain, and from all of these factors combined to create a challenging and complex communication environment.
Effective communication
There are many communication strategies that can be implemented into everyday life and make a significant difference in the life of a person living with dementia.
Consider verbal language. The words you’re using, the tone and pace at which you’re speaking, and the length of sentences are important considerations.
Be calm, speaking gently and clearly. Keep sentences short and simple. Use words that the person can relate to and give them time to process what you’re saying and to respond. Be respectful and empathetic. If someone is distressed and confused, validate their feelings and take the time to listen to why they’re feeling that way and how you can help.
Consider your body language and how it might be interpreted. Facial expressions, body posture and the personal space you provide all make a difference to a person living with dementia during interactions in everyday settings.
Being aware of how you approach a person and respecting their personal space can reduce confusion, distress and fear. It can help a person feel at ease, build trust and connect.
People living with dementia will interpret body language, facial expressions and tone of voice with greater accuracy than words. Make eye contact, smile and ensure your body language is as positive as possible.
If a person is struggling to understand what you’re saying, consider visual cues that you can respectfully use to support what you’re saying.
Consider the immediate environment. Background noises such as a vacuum cleaner or loud music, which you might not notice in the background, can make all the difference in a person being able to understand what is happening in the foreground.
Understand their story. Who they are, where they are and where they’ve come from, can help inform how to best communicate with a person.
For example, structuring a day in a certain way may not make sense for a person who spent their career life serving in the military. They may be used to a strict schedule, without which could lead to diminished functioning, mood and sense of purpose.
By understanding the person’s story and implementing activities accordingly, you can help them maintain self-worth, positively impacting the person’s health and wellbeing.
Good communication practice is critical in quality dementia care. It’s the small things that make the most difference; the difference between someone feeling distressed, anxious and agitated, or feeling confident, at ease, trusting of those around them and continuing to have a purposeful and dignified life.
It’s important to think about how we’re communicating, not just what we’re saying but how we’re saying it – what words we’re using, how body language might be interpreted, what else is happening in the environment and what might affect how communication is perceived.
To enhance communication practice, care workers can participate in Dementia Australia’s Talk with Ted workshop program. Delivered through an online workshop, Ted is an avatar with symptoms of dementia. By engaging with Ted in a safe setting, workers can build their confidence and skills.

For more information on Dementia Australia’s Centre for Dementia Learning resources, educational tools and programs available for healthcare professionals, please visit our website.
Dr David Sykes, Director, Dementia Australia’s Centre for DementiaLearning www.dementialearning.org.au
Planning for Diversity training series
Who’s missing from your aged care services?
Our free training helps aged care providers to differentiate, address barriers for those who would like to access their services, and demonstrates commitment to Aged Care Quality Standards.
This training includes:

• two face-to-face workshops, delivered by industry specialists
• an online session
• access to a Community of Practice.
I have been to many training sessions in many areas for aged care, but these OPAN sessions have been the best ones I have ever attended.”
-Kim , Clinical ManagerDualPak Ready Meal Trays
Made from pressed paperboard, the DualPak tray features natural insulation properties that will not crack, even when frozen. Perfect for preparing, displaying, storing and heating prepared meals in, the DualPak tray is the go -to choice for makers of good food. DualPak packaging options can be
tailored specifically to your cooking

Request a Demo

A choice of cost effective tray sealing machiner y for DualPak trays is also available, from ergonomic and convenient benchtop sealers to inline automatic models. Contact your Confoil representative today for a demonstration of our tray sealing machiner y options.


The missing piece of aged care funding
Allied health is the elephant in the room
With conversations around crises in the aged care sector, particularly workforce and funding, one key aspect of quality care continues to be largely ignored – allied health.
While the benefits of treatments like physiotherapy are clearly identified –for better mobility and better health generally – many older Australians who are recipients of care are missing out.
At the Royal Commission into Aged Care Quality and Safety, allied health was referred to as a critical part of aged care. The Commissioners agreed that more than the eight minutes of allied health per resident per day was needed because that level was inadequate to prevent older people deteriorating.
The authors of the AN-ACC Anita Westera and Kathy Eagars and the Commissioners called for allied health to be embedded and funded in the aged care reforms at international benchmarks of 22 minutes per resident per day to enable older people to lead their best lives. The then Morrison government partially accepted this recommendation, however only funded $28 million over four years, which clearly wasn’t even close to enough.
Expecting financially at-risk providers to pay for allied health when it isn’t part of star ratings and care minutes, is like a car crash we all saw coming. There was a 37 per cent decrease in allied health jobs and hours in the six weeks after the AN-ACC started on 1 October 2022, and the Aged Care Financial Reports from October to December 2022 also showed an 18 per cent decrease in allied health levels compared to the previous quarter.
We urgently need allied health to have its own transparent and separate funding and to decide where this funding comes from. Allied health must have clear
clinically mandated minimum care levels and scope of practice guidelines to support older people’s needs.
The Australian Government and stakeholders must add allied health to the Aged Care Taskforce meeting agenda and include it in future funding discussions as well.
ACCPA and many professional organisations such as AHPA (Allied Health Professionals), SARRAH (services regional and remote allied health), OT Australia, and the Australian Greens warned what would happen without allied health being funded and mandated at minimum levels and forming part of quality standards and star ratings.
The Aged & Community Care Providers Association, in pre-budget submissions, called for a more sustainable funding model to address financial sustainability issues in the sector. This included putting in place an allied health needs assessment and funding model by July 2024. Petitions by company AAC Allied Aged Care were lodged in the senate, house of reps with over 40,000 signatures of citizens concerned about allied health for older people.
The treasurer Jim Chalmers admitted in May 2023 that allied health levels weren’t good enough, however money wasn’t there in the budget to fund it. Instead, we have continued to hear the same statements that providers are still expected to pay for and provide allied health at clinically needed levels.
These levels are at least four per cent of income, for an average of eight minutes per resident per day, which was confirmed when I asked Dr Nicholas Hartland during a public Q&A session at the ACCPA National Conference in October 2022.
But right now, in August 2023 older people, depending on who you get your
information from are getting around one-quarter of these expected allied health levels.
How can we ensure older people receive the allied health they need, and it is funded in a viable way? We first need to acknowledge, that “Houston (Canberra), we have an allied health problem”. Only then can we work together on financially sustainable models that help consumers, providers and our society benefit from the allied health that older people need.
A user pay model for allied health exists in the US, UK, and New Zealand. Isn’t it time we discussed this seriously as a solution for allied health here as well?
These discussions are vital, because our community needs adequate allied health levels for older people as it takes load off nurses, carers, doctors and hospitals. Allied health prevents falls, pressure injuries, medication side effects, hospital admissions and deaths. Falls alone are the leading cause of preventable death in older people.
Over 5,000 people die from falls each year, impacting quality of life and life expectancy, and cost the health system over $5 billion a year. Physiotherapy alone has been shown to decrease falls by 55 per cent – so the maths is clear.
 Alwyn Blayse, Physiotherapist and CEO, AAC Allied Aged Care www.alliedagedcare.com.au
Alwyn Blayse, Physiotherapist and CEO, AAC Allied Aged Care www.alliedagedcare.com.au
CANBERRA 8-9 NOV 2023
Exhibition Park (Epic)
ADELAIDE 6-7 MARCH 2024

Adelaide Showground
SYDNEY 22-23 MAY 2024
Sydney Showground
BRISBANE 29-30 MAY 2024
Brisbane Convention & Exhibition Centre
FREE
1300 789 845
www.atsaindependentlivingexpo.com.au
Organised by Media Partners

Let’s talk about balance
The key to falls prevention
Balance can be defined as a physical ability to keep the centre of gravity within the base of support by the regulation of postural reactions as required, allowing for body movement and function. Balance is a key component in human ambulation, therefore balance exercises are essential in an exercise routine together with strength, aerobic and flexibility exercises.
Balance control relies on our body’s ability to control posture and the required reactive movements, responding to sensory messages from vision, vestibular and proprioceptive systems, informing us of changes in our surroundings. Poor balance reflects a decreased ability to process this information from these sensory organs, including the slowing down of reaction time and motor responses, as well as decrease of muscle strength.
Physiological ageing is apparent in many ways, including decrease of muscle strength, reaction time and cognition, leading to an impaired balance, and consequently increasing the risk of falling. Indeed, a third of people aged 65 years and more, and half of people aged 80 and over, will experience on average one fall per year.
Appropriate exercise programs are a key aspect of falls prevention. Studies have shown that programs specifically focusing on balance can reduce falls causing injuries by 37 per cent, falls leading to serious injuries by 43 per cent, and broken bones by 61 per cent.
The Sunbeam protocol (2018) – a progressive strength and balance program that provides evidence-based exercise for falls prevention in older people, now being adopted in many residential aged care homes – has been shown to result in a 55 per cent reduction in falls.
The goals of balance training commonly are to improve standing balance and posture, as well as improve postural control during mobility, leading to improvement in physical function, and consequently improved self-efficacy in balance control, feeling of safety and ease of activities of daily living, thus decreasing fear of falling and improving quality of life.
Balance training aims to challenge the balance organs, eyes, muscles, joints and vestibular system. It includes both static (eg. standing on flat and unstable surfaces, standing in different postures and positions while doing tasks) and dynamic (eg. stepping and reaction, changes in the base of support) balance exercises. All exercises should progress in difficulty, and challenge cognition by adding multi-tasking activities.
A research team from the Department of Physiotherapy at Monash University has developed a world first interval rating of balance exercise intensity, the Balance Intensity Scale

(BIS). Balance intensity is defined as ‘the degree of challenge to the balance control system relative to the capacity of the individual to maintain balance’.
The purpose of the BIS is to allow people to assess and train with appropriate intensity, creating an environment where training can be monitored and progressed in a safe, yet progressive manner, allowing both the trainer and the exerciser to rate the intensity.
Monash University, together with lead researcher Dr Mel Farlie, has developed free education and training materials, to promote awareness of the BIS scale and appropriate training. Providers are encouraged to visit their website, where they will find training videos, BIS score sheets and exerciser sheets, which can be accessed here: www.monash.edu/medicine/ balance-intensity-scale
Balance assessment and training efficiency can be objectively monitored by using a force plate, or similar, that records the body’s postural reactions by mapping the trajectory of centre of pressure during standing.
HUR SmartBalance (www.huraustralia.com.au/balance-testing) is an example of a functional platform that allows for both assessment and training in one piece of equipment. The data collected allows for objective analysis of postural sway during testing and monitored progression of exercises.
The importance of balance training is well established in Australia with the support of many world-leading research groups. They are implemented independently, and as part of comprehensive exercise programs. The next step is to focus on the intensity of the balance training, to reach the level where challenge and safety meet appropriately, to allow for required progression, also including multi-tasking, leading to better function and confidence in everyday life.
Dr Tuire Karaharju-Huisman, Physiotherapist, AEP, and Research Lead, HUR Australia www.huraustralia.com.au

NDIS services in aged care
It’s been 10 years since then Prime Minister Julia Gillard and the Federal Labor Government signed the National Disability Insurance Scheme (NDIS) into law in March 2013.
A life-changing piece of legislation for many, the NDIS provides funding to eligible people with disability to gain more time with family and friends, greater independence, access to new skills, jobs, or volunteering in their community, and an improved quality of life.
Currently undergoing reform, services delivered by the NDIS are provided to 592,059 recipients – many of them in aged care – across Australia by 8,659 providers.
It’s important for aged care providers to understand the role of the NDIS, and the need to engage the best possible NDIS services for their residents and clients.
NDIS support for over 65s
While the NDIS supports Australians under the age of 65 with a permanent and significant disability, there are many people who received supports prior to turning 65 whose NDIS plan continues while living in residential aged care homes, supported independent living arrangements or specialist disability accommodation, or with family and caregivers in their home.
Participants can choose whether they want to continue to receive NDIS supports, or whether they’d like to access support through the Commonwealth aged system (e.g. CHSP, HCP and STRC). Today, more than 26,000 participants over the age of 65 continue to receive services under the NDIS.
Allied health & NDIS services
Allied health such as physiotherapy, occupational therapy, speech pathology, dietetics and exercise physiology services can be delivered to NDIS participants across Australia as well
as individuals who formerly received services under the NDIS and have transitioned to receiving support under the Commonwealth’s aged care system.
NDIS services across residential & community
Where possible, the clinician providing services and care to an NDIS participant residing in a residential aged care home should be already working in clinical care within the home, in order to have greater familiarity and a better understanding of client needs and also for continuity of care.
By integrating allied health services within the participant’s place of residence or partnering with on-site care staff at residential aged care homes (eg. nursing staff, GPs, specialists), the level of support a participant receives is better, and more cost-effective.

Vivir Healthcare’s approach in aged care
Vivir Healthcare is proud to deliver allied health services into residential aged care homes, with NDIS and nonNDIS residents, as well as to older clients living independently at home.
Participants in residential aged care homes are referred to Vivir Healthcare for NDIS services through either onsite staff, their support coordinator, a family member or representative, or by themselves independently.
We found integrating our clinical workforce across service lines (residential care, community care and the NDIS) allows us to meet the needs of the care recipients on time at a high level, while also providing a flexible balance to our clinical workforce.
We have also observed that the continuity of care that comes from our clinician providing multiple levels of services within the participant’s home or at a residential aged care home improves the integration of care
across the participant’s supporting domains, and delivers greater humanity, compassion and more cost-effective support for participants.
Vivir making NDIS services accessible
Vivir Healthcare also utilises in-person visits, Telehealth and our Telehealth To You service which requires the assistance of an Allied Health Assistant to support both the participant and the allied health professional with an inperson and in-home assessment. These assessments cover:
■ support with safe handling
■ measuring for home modifications
■ falls prevention
■ mobility equipment
■ nutrition and communication.
Vivir Healthcare’s Telehealth services were introduced with a primary focus on accessibility, particularly for individuals residing outside major cities. In addition to addressing this crucial aspect, the implementation of Telehealth has created new avenues for professional growth and development for Vivir’s clinical workforce, granting them the opportunity to engage in various streams of work.
These virtual services have successfully reached and benefited more than 187,000 participants living outside major cities, to date.
Sustainable care
Vivir Healthcare have found the key to providing effective and sustainable solutions to NDIS participants is by integrating them into all elements of Vivir care. With a dedicated Vivir pathways manager and scheduler to manage each participant’s Service Agreement and unique funding arrangement, participants are quickly allocated to the most appropriate clinician to meet their needs.
If you’re looking for an NDIS allied healthcare provider, doing your research and choosing the right partner will be vital for smooth sailing.
Tyler Burrowes, Osteopath & Project Lead, Vivir Healthcare www.vivir.com.auWhat providers need to know
Empowering seniors for better heart health
How aged care providers can play a role
Heart failure is a pressing concern in the aged care community, with its significant impact often underestimated or overlooked. Aged care providers can play a pivotal role in supporting heart health among seniors by recognising warning signs, understanding risk factors and encouraging individuals to seek medical advice.
The burden of heart failure in seniors
Seniors bear a considerable burden when it comes to heart failure, resulting in over a million days of hospital stays each year for Australians aged 65 and above.
Alarming projections indicate that the absolute number of hospital admissions for heart failure could surge by up to 50 per cent in the next 25 years, owing to population growth, ageing and the rising prevalence of comorbidities.
Regrettably, heart failure does not receive the same attention as other prevalent conditions, despite its profound impact on the aged care community.
Recognising warning signs and risk factors
Early detection is crucial for effective heart failure management among seniors, and familiarising ourselves with warning signs can expedite timely intervention.
Symptoms to watch out for include shortness of breath, swelling of the feet or ankles, irregular heartbeat and fatigue.
Unfortunately, these common indicators are frequently dismissed as unrelated health issues or attributed
to the natural ageing process, leading to delayed diagnoses and impact on quality of life.
Collaborating for positive change
Aged care providers and other stakeholders possess an unparalleled opportunity to make a profound impact on the health of older Australians, by sharing the latest knowledge and information with residents, clients and their loved ones.
Prioritising education, early diagnosis and empowering seniors with knowledge are key factors in reducing the impact of heart failure on individuals and their families, and enhancing overall quality of life.
Free resource available
To combat the pervasive lack of awareness and underdiagnosis of heart failure, Hearts4Heart has produced an invaluable resource Understanding Heart Failure: A Guide for All Australians.

This free guide, available for download from the Hearts4Heart website, was developed in accordance with European and American guidelines, incorporating insights from both clinicians and patients. It offers comprehensive information encompassing prevention, symptom reduction, lifestyle modifications, diagnostic tools and treatment options.
This guide acts as a catalyst for seniors to understand their condition and actively engage in discussions regarding their treatment plans. By empowering them with accessible information, it contributes significantly to reducing the burden of heart failure in the aged care community, fostering early intervention, and promoting patient-centered care.
UnderstandingHeartFailure:AGuideforAll
Hearts4Heart’s commitment to senior heart health
Hearts4Heart takes a proactive approach to address heart failure in seniors. Through awareness initiatives such as Heart Failure Awareness Week, Atrial Fibrillation Week and Heart Valve Awareness Week, they strive to offer unique opportunities for education, support and advocacy. The release of their free guide reinforces their commitment to improving heart health outcomes.
Aged care providers are encouraged to download the guide for their staff, residents, clients and their family members, to help share this vital information and empower older people with the knowledge they need.
Through collective efforts and advocacy, we can lighten the burden of heart failure, fostering improved quality of life for seniors affected by this condition.
Hearts4Heart
www.hearts4heart.org.au




AMH Aged Care Companion






















The AMH Aged Care Companion is a practical reference for health professionals working with older people. It contains evidencebased peer reviewed information on more than 70 speci c conditions that are common in older people, along with general principles when using medicines in this population. It is useful when conducting medication reviews and other activities aimed at improving patient outcomes, eg case conferencing. Available in Book or Online.

When they put their trust in you, it’s vital to have information you can trust )
Mitigating the spread of viruses and pathogens
Within aged care, ensuring the health and safety of residents is of paramount importance – and one critical aspect that directly affects residents’ wellbeing is indoor air quality (IAQ).
Indoor air quality refers to the condition of the air within and around buildings, especially as it relates to the health and comfort of occupants. Aged care homes are particularly susceptible to IAQ issues due to their enclosed nature and the vulnerability of their residents.
Poor IAQ can lead to the spread of viruses and pathogens, causing health issues, particularly for older people who might have weakened immune systems.

Effective heating, ventilation and air conditioning (HVAC) practices play a pivotal role in mitigating these risks – and there is a lot aged care providers can do to prevent the spread of viruses and pathogens.
Impact of poor IAQ
■ Respiratory health. Older people are more prone to respiratory issues, and poor IAQ can exacerbate conditions such as asthma and chronic obstructive pulmonary disease (COPD), or even allergies.
■ Weakened immunity. Ageing often weakens the immune system, making older people more susceptible to infections. Contaminated indoor air can increase the risk of viral infections.
■ Cognitive function. Studies strongly point to a link between IAQ and cognitive function. Good IAQ has been associated with better cognitive performance, which is crucial for aged care residents’ overall quality of life. This is also true for the staff and carers in this environment.
Mitigating the spread of viruses and pathogens
■ Filtration systems. Upgrade HVAC filters to high-efficiency particulate air (HEPA) filters. These filters are capable of capturing tiny particles, including viruses. Also, regularly inspect and replace all filters as per manufacturer recommendations. Clogged filters are less effective and will hamper good airflow.
■ Ventilation. Better cognitive performance, alertness and decision-making is a direct result of monitoring and controlling carbon dioxide levels in the indoor environment. You can help support the right levels by ensuring proper ventilation rates to increase the supply of fresh outdoor
air, which will also reduce the concentration of indoor air pollutants, including viruses. Utilise natural ventilation whenever possible, especially in areas with low population density.
■ Air purification. Consider installing air purifiers with HEPA filters in common areas and residents’ rooms to augment the efficiency of HVAC systems. UV-C germicidal lamps are another option that can be integrated into HVAC systems to neutralise airborne pathogens.
■ Humidity control. Maintain indoor humidity levels between 40 and 60 percent, which is less conducive to the survival and spread of viruses.Humidity control also prevents issues like mould growth, which can further compromise IAQ.
■ Regular maintenance. Establish a comprehensive HVAC maintenance schedule. Regular inspections, cleaning and servicing ensure optimal system performance. Address any leaks, condensation issues, or water damage promptly to prevent mould growth and IAQ deterioration.
■ Sealing and insulation. Ensure proper sealing and insulation of HVAC ducts to prevent the infiltration of pollutants from outside, as leaky ducts can introduce allergens and contaminants, diminishing IAQ.
■ Isolation rooms. Designate isolation or quarantine rooms with enhanced ventilation for residents displaying symptoms of infectious diseases. This prevents the spread of pathogens to other residents
■ Education and training. Train staff on the importance of IAQ and HVAC system management.
Have the right strategy
A well-implemented HVAC system management strategy is an essential part of aged care, and should be high on your list of priorities. By following good practices and incorporating correctly installed equipment, aged care providers can create a healthier and safer environment for their residents, ensuring their comfort and overall quality of life.
This can be quite a complex and detailed undertaking dependant on each individual facility, and requires in-depth understanding. We highly recommend partnering with an experienced and knowledgeable HVAC engineering contractor within the aged care space, so you can achieve the best outcomes for residents and staff.
John Bennett, Director, mechfieldfm www.mechfieldfm.com.auManaging indoor air quality is essential for resident health
Enhancing hygiene, dignity and comfort
The benefits of bidets in residential aged care facilities
As the world’s population continues to age, providing high-quality care and maintaining the dignity of older adults in residential aged care homes becomes an increasingly important challenge. One innovative solution that has gained attention for its potential to improve hygiene, dignity and overall wellbeing is the bidet.

A new approach to personal hygiene
Bidets, commonly associated with improved personal hygiene, have long been utilised in many parts of the world. Their introduction in residential aged care homes brings a new approach to addressing the unique needs of older adults.
Traditional methods of post-voiding cleaning, such as using toilet paper, can be less effective for older individuals who may face mobility limitations, reduced dexterity, or other physical challenges.
Bidets offer a more thorough and comfortable cleansing experience, utilising water jets that can help prevent skin irritation and infections.
Reducing the risk of infections
One significant benefit of bidet use is the potential to reduce the risk of infections, particularly urinary tract infections (UTIs). Older adults are more susceptible to UTIs due to factors such as weakened immune systems, incontinence and reduced bladder control.
Bidets can aid in maintaining proper perineal hygiene, reducing the accumulation of bacteria and decreasing the likelihood of infections. By promoting a cleaner and more sanitary environment, bidets contribute to the overall wellbeing of residents and can lead to fewer instances of UTIs.
Managing incontinence and supporting dignity
With incontinence a common challenge faced by older adults in residential aged care homes, bidets offer an effective solution for managing incontinence-related hygiene. The gentle and efficient cleansing provided by bidets can help residents feel more comfortable and cleaner, enhancing their overall sense of dignity.
Furthermore, bidets may reduce the stigma associated with incontinence, promoting a more open and compassionate atmosphere within the home.
Alleviating constipation
Constipation is another prevalent issue among older adults, often exacerbated by factors such as reduced physical activity, medication side effects and dietary changes. Bidets have been shown to have a positive impact on bowel management by promoting more complete voiding of the bowel.
The warm water stream from the bidet can help relax the anal sphincter muscles and facilitate more regular bowel movements. This can lead to a reduction in constipationrelated discomfort and a potential decrease in the need for laxatives or other interventions.
Easing the workload for caregivers
Bidets not only benefit residents but also ease the workload for caregivers, including staff members and family caregivers. The use of bidets can streamline toileting routines, reducing
the time and effort required for manual cleaning and changing of incontinence products.
Caregivers can allocate more time to providing personalised care and engaging with residents, ultimately improving the quality of their interactions. Moreover, the reduced workload associated with bidets can contribute to staff wellbeing by minimising physical strain and stress.
Promoting sustainability and cost savings
In addition to their direct benefits for residents and caregivers, bidets can contribute to sustainability and operational cost savings within residential aged care homes, by reducing consumption of toilet paper and incontinence products. The decreased paper waste also aligns with environmentally friendly practices – something that can be a competitive point of difference in the marketplace.
Installation tips
To ensure the safety of your water supply when installing smart toilets and bidets, it is crucial for your plumber to consider backflow prevention measures, which help prevent contamination.
Backflow refers to the undesirable flow of contaminated water into the main water supply, and it can occur when
there is a sudden decrease in water pressure externally or when the water pressure within the home exceeds that of the main supply. This can lead to the backflow of water from your toilet or bidet into the main supply, potentially polluting your drinking water.
To prevent such cross-connections and the entry of contaminated water into the main supply, it is essential for your plumber to install a backflow prevention device during the installation of your smart toilet or bidet. These devices typically employ one of the following components to prevent water from flowing backward: a one-way valve, an air gap or a break tank.
A better bidet
Australia’s most advanced bidet system is the InteliClean Air 9000 Series, which includes an Integral High Hazard Backflow Prevention Device complying with the Plumbing code of Australia (PCA). This is one of the only fully certified bidet for installation with no additional backflow required. And, it is packed with features previously not available.
Craig Spence, National Business Development Manager, InteliCorp/The BIDET SHOP
www.thebidetshop.com.au
The Model of Care Holistic
A consumer led model beyond person-centered care

Be ready for the new Aged Care Standards Stay ahead of the Reforms Meet the Babyboomers Expectations
This approach as been developed by the experts from Standards Wise International and Babyboomers who have joined forces to develop a leading model of care for organisations to deliver outstanding outcomes and attract talented staff.
The Holistic Model comes in an easy to implement package which we can deliver over 12 weeks or 12 months to position your organisation to achieve:

• Person Led Solutions
• Inspired staff
• Empowered consumers
• Measured Outcomes
• Compliance
Products and Services
• Comprehensive Onsite and Virtual Audit Service

• Whole Policy and Procedure Suites, Related Documents
• A 16 week Mentorship Program for aspiring aged care clinical leaders

• Preparation for Accreditation Support and Gap Analysis
• Return to Compliance Turn Arounds and General Consultancy
• Education and Training on the new Standards due 1st July 2024
For further information contact: Standards Wise (Australia) 26/44 Market St Sydney, NSW 2000 (02) 9089 8881
admin@standardswise.com.au
www.standardswise.com.au
We can all die better A community approach to end-of-life care
If it takes a village to raise a child – after planning for months for birth – it surely takes a village to ‘die well’. So, why aren’t we investing in the village to ensure we can all die better?
Death in our society is over-medicalised and institutionalised, with dying relegated mostly to medical and residential aged care facilities. It leaves us believing that end-of-life care of a loved one (or ourselves) is best managed by medical experts only. This is not inevitable or the best way to manage end-of-life because death is not just a medical event – it’s so much more.
What would it take to die better?
Death is the one thing that we are all
to die. It’s a uniquely personal and social experience.
New research by the South West Compassionate Communities Network shows that innovative ‘models of death’ or ‘end-of-life care’ where community works in partnership with healthcare services, enable better dying outcomes as well as cost savings to the health system. Known as ‘Compassionate Communities’, this approach encourages communities to use their inherent capability to provide practical and emotional support for those who are caring, dying or grieving within the community.
Preliminary findings of the study on the Compassionate Connectors Program, part of the South West Compassionate Communities Network in Western
approach resulted in 15 per cent fewer hospital admissions.
It also showed that those who were admitted to hospital stayed for 28 per cent less time, and there was 108 per cent more use of community-based services, which are in general cheaper than hospital-based services.
A cost-consequence analysis revealed that using the Compassionate Connectors Program enabled a net saving of $561,256 AUD to the healthcare system over a six-month period (based on hospital admissions of 100 patients during that time).
It’s clear that the community has huge potential to support better dying alongside the status quo of health policy. We do not fairly acknowledge – or harness – the incredible power of involving family, friends and our communities in this process.
Minister for Health and Aged Care, Mark Butler, recently announced $54 million in funding for 14 National Palliative Care

Product training for staff
In addition to initial onsite training, regular reeducation can be provided as well as our online learning platform, excAL. We also provide an invaluable range of resources for you, your staff and your patients as a go to guide for all things medical oxygen and respiratory equipment.
Oxygen therapy products and respiratory devices
We provide a wide range of stationary and portable oxygen concentrators as well as oxygen cylinders, oxygen conserving devices, OPEP devices, suction systems and nebulisers

and access for people with life-limiting illnesses. This is so that people may live longer with symptom management and support for physical, psychological, social, emotional and spiritual needs. This isn’t surprising given that burdened health services are the hungriest mouth in the nest. However, important public health initiatives that focus on community-led end-of-life care, are missing out and struggling to stay afloat.

A Compassionate Communities approach alongside the health system Empowering community as equal partners in end-of-life care would enable better dying outcomes – particularly where there is a wish to die at home.

To support an increase in the number of people dying at home will require a broad set of reforms. A growth in the development of Compassionate Communities across Australia will be an important step in actualising this transformation.

Compassionate Communities raise community awareness of end-of-life

issues, as well as promote participation in the care and support of dying people and their families. Building networks of care, mobilising communities to provide practical and emotional support in skilled and informed ways, and developing resilience, are all elements of a Compassionate Community.
Dying to Know Day, a not-for-profit campaign held on 8 August each year, aims to empower Australians to improve their ‘death literacy’ and start important conversations about end-of-life with their loved ones. The awareness raising event is an initiative of Community Care Northern Beaches (CCNB), a community-led not-for-profit established in 1994, to help people navigate health and social care systems.
Our vision is to have 150,000 endof-life ‘Compassionate Connectors’ across Australia as part of a Connectors Network, which we are hoping to establish nationally. This program has the potential to bring in all the right people, volunteers, coordinators and

caring helpers to inform meaningful change, but it needs funding.




We have an opportunity to advocate for better resources to transform our approach and experience when it comes to death so that you, me and the people we love can die better.
Kaz Dawson, CEO, Community Care Northern Beaches www.comcomnetworksw.com
For a long time, the Aged and Disability Care sector in Australia has been looking for their software providers to offer a fully integrated solution to drive efficiencies by scheduling services, maintain compliance and seamlessly manage payroll, billing, account management and general ledger.
Care Systems ensures
■ Rostering and scheduling is managed efficiently.

■ Overstated KMS (both between and during service delivery) are eliminated.
■ Staff receive the information they need to be effective in their role of delivering quality care.
■ Employees are paid in line with the relevant EA or Award. On time – every time.
■ Clients receive accurate and compliant statements and invoices with no manual data transfer or need for 3rd party integrations.
■ Your organisation maintains compliance while delivering quality services to your clients.
■ Government reporting is generated without the need to import/export data.
Care Systems has listened to what its clients and the market are asking for, and are proud to deliver its suite of fully integrated and cloud-hosted applications that will create efficiency and support compliance for any organisation in the Aged and Disability Care sector.
Ensuring your compliance is maintained
From front-end home and residential client management and service rostering with the support worker mobility app, to resident billing, ACFI calculation, back-end payroll, billing, accounts and government reporting
Using the latest Care Systems cloud technology, payroll and client billing is simple and streamlined. Care Systems’ HomeCare and HomeCare Mobile modules seamlessly integrate to manage your rostering, filling empty shifts quickly and easily, while managing your KMS, worker skills and client preferences.
Once services are completed, real time mobile time and attendance data is matched to rostered shifts and services, enabling swift approval and processing of Payroll.
Want to maximise revenue and ensure effective and compliant Client and Resident Billing?

Care Systems supports providers to maximise their funding entitlements and ensure Clients and Residents are billed correctly. We can manage your Medicare payment statement reconciliation and analysis to ensure you don’t miss out on funding entitlements, payments and supplements.
As clients are billed directly from the system, end of month reconciliation and reporting occurs in parallel.
Have peace of mind knowing your residents are billed correctly, and your staff are paid accurately and on time.
Aboriginal and Torres Strait Islander aged care in Alice Springs
Putting Elders at the heart
Aiming to improve the experience of ageing for Indigenous Australians, the Australian Association of Gerontology (AAG) is highlighting the benefits of a multidisciplinary approach.

Its Aboriginal and Torres Strait Islander Ageing Advisory Group (ATSIAAG) consists entirely of Aboriginal and Torres Strait Islander members of AAG – including researchers, practitioners, carers, Elders and older people committed to addressing and providing advice on all issues related to ageing in Aboriginal and Torres Strait Islander communities.
In May this year, the ATSIAAG held the inaugural two-day forum ‘Ageing at the Centre: Putting Elders and older people at the heart of our work’ – the first time AAG has brought together Elders, service providers and other stakeholders to share their knowledge, experience and insights.

Supported by Tangentyere Council and the National Aboriginal and Torres Strait Islander Ageing and Aged Care Council (NATSIAACC), the aim of the forum was to provide a culturally safe environment for delegates to workshop with peers about issues and strategies relating to Aboriginal ageing and aged care.
Held at Purple Shed, a social enterprise by the Western Desert Nganampa Walytja Palyantjaku Tjutaku Aboriginal Corporation (Purple House) in Mparntwe Alice Springs, participants addressed topics such as advance care planning and end-oflife care, dementia and workforce capacity and skills.
In a message that spanned all topics, forum participants acknowledged ‘real world’ constraints, but reinforced the importance of working with Elders, their family and community to support Elders’ and older people’s choices as they become frailer and need greater care.
It was clear that successful aged care in regional and remote settings with Aboriginal clients and staff depends on community control, collaboration, creativity and compassion. There was strong interest in how to manage the tension between current aged care regulations and legislative expectations, and practical delivery of aged care services in a unique context.
Implementing services according to the aged care standards, for example, does not account for the significant number of clients who have no or limited access to technology, may live in insecure housing and may lack a supportive personal network.
It follows that the assessment of services should allow for an appropriate range of approaches and contexts. Ideally, these assessments would be conducted by assessors who are Aboriginal or Torres Strait Islander people, or others who have undertaken training in cultural safety and trauma-informed approaches.
The long shadow of the COVID-19 pandemic was also a key point. Many services experienced international and interstate staff leaving when COVID-19 travel restrictions and border closures took effect. On a positive note, the required boost to telehealth and online technologies has been beneficial
for many services in the area, while one provider had the opportunity to purchase a series of online courses to train local Aboriginal workers and community members who were interested in gaining aged care skills and knowledge.
Key learnings
For service providers, offering safe, effective and sustainable support within this complex environment involves:
■ Respectful collaboration between Aboriginal and Torres Strait Islander community-controlled organisations and mainstream service providers, clinics and specialists
■ Working together to co-design and deliver care that is authentic, holistic and culturally safe
■ Getting the right people for the job, particularly as the community may not respond to or engage easily with non-Aboriginal aged care staff who lack cultural competence
■ Making provision for government policy frameworks and funding models to accommodate the unique needs of Aboriginal and Torres Strait Elders, their communities and the providers who support them to age well
■ Enabling flexible working conditions for Aboriginal and Torres Strait Islander staff that accommodate, for example, cultural leave and exemptions from duties deemed culturally inappropriate
■ Supporting staff who are caring for clients who have been affected by trauma, and/or have experienced trauma themselves.
Ellen Finlay, First Nations Policy and Aboriginal and Torres Strait Islander Ageing Advisory Group (ATSIAAG) Officer, Australian Association of Gerontology, and Dr Meg Polacsek, Communications, Advocacy and Grants Manager, Australian Association of Gerontology www.aag.asn.au

Serving up food solutions to aged care
Food Solutions is a leading Australian provider of aged care Dietitians and Speech Pathologists.
Our team optimise resident’s nutrition, hydration and safety as well as assisting food services to promote health, wellbeing and quality of life.
How we support aged care staff and their residents:
Dietitians
Up to 60% of aged care residents are likely to be at risk of or experience malnutrition. Our Dietitians will combine clinical and food service expertise to optimise nutrition and good health for these residents.
Mealtime and Dining Experience
Our reviews offer a holistic and independent assessment of the mealtime and dining experience with support programs for improvement.
Speech Pathologists
Approximately 70% of residents in aged care experience dysphagia. Our Speech Pathologists specialise in the assessment and management of swallowing difficulties and can provide support and education to carers and aged care staff.
Education and Training
We are passionate about education. Our online and face-to-face education programs cover a range of nutrition and dysphagia topics suitable for clinical, care and food service staff.
We’d make a great pear! Get in touch today:
Menu Development and Review
Our foodservice programs support the full menu process from design through to review. Dietitian and Speech Pathology intervention tailored to meet your needs.
Telehealth Services
Access quality care, close to home. For your convenience, Food Solutions offers Speech Pathology and Dietetics directly into your facility via Telehealth.
1300 850 246 info@foodsolutions.com.au foodsolutions.com.au
IDDSI Training and Auditing
It is essential to get modified diet and fluids right every time! Our training and auditing programs will ensure your facility is compliant.
Community connections expanded with Elder Rights Advocacy’s Aged Care Volunteer Visitors Scheme

Leading the charge as one of the largest ACVVS services in Victoria
Elder Rights Advocacy (ERA), an organisation which provides information and advocacy support to older people, and their representatives in Victoria, has expanded its Community Visitors Scheme, now known as the Aged Care Volunteer Visitors Scheme (ACVVS), from 1 July 2023, making it one of the largest providers of this invaluable service in the state.
This expansion – made possible through funding from the Department of Health and Ageing – comes as a response to the recommendations put forth by the Royal Commission into Aged Care Quality and Safety.
Megan Collison, Volunteers Coordinator at Elder Rights Advocacy, expressed her enthusiasm for the program’s free statewide implementation, saying, “We are thrilled to be able to extend our reach across Victoria. The Aged Care Volunteer Visitors Scheme allows us to better cater to the needs of older Victorians receiving aged care services, who often face loneliness and social isolation.
“We hope to provide around 785 matches across residential care and for older people living at home receiving aged care services across Victoria. The volunteers will have the opportunity to visit with an older person weekly or fortnightly.
“This program is intimate with a grassroots approach, and we are determined to reach out to all older
people across the state with a focus on those who identify as belonging to a marginalised group or for whom English is a second language.”
The primary objective of the ACVVS is to establish and nurture social connections by providing friendship and companionship through ERA’s dedicated volunteers. This initiative, aims to alleviate the adverse effects of social isolation experienced by older people.
Debra Nicholl, CEO of ERA, emphasised the importance of the program, stating, “Meaningful connections are vital to combatting social isolation among older people. The expanded program ensures that we can match an increased number of volunteers and older people with similar interests, backgrounds and preferences, fostering genuine relationships that improve quality of life.
“There are many reasons why isolation and loneliness occur for older people. They may have limited contact with friends or relatives, lost connections with their culture or heritage, or their health challenges may prevent them from participating in social or leisure activities.
“Therefore, it is fundamental that ERA continues to take a proactive approach in supporting those who need friendship, conversation and connection the most.
“We’re able to provide face-to-face connections, including phone calls, virtual contact, or even sending letters. We can be flexible in our approach to achieve a positive outcome.”
The ACVVS is open to any older person residing in an aged care home or awaiting or receiving support in their own home through a home care package. Aged care providers, as well as family and friends, are encouraged to reach out to Elder Rights Advocacy to learn more about the program and how these valued friendships can positively impact the lives of older individuals, reducing their sense of isolation.
Volunteers are carefully selected and possess a sincere desire to alleviate the social isolation faced by older people and a deep understanding of the complex health challenges they may encounter. Equipped with practical social skills, volunteers will listen, empathise and engage with older people in a way that best suits the older person.
Megan added, “We welcome people who are reliable, confident and caring individuals who seek to make a positive difference in an older person’s life.
If you know someone who might be a good fit, we encourage you to let them know about being a volunteer visitor – a contribution that can bring immense joy and companionship to the volunteer as well as to the older person.”
To learn more about ACVVS and refer an older person for this program, please contact Elder Rights Advocacy at 1800 700 600.
Elder Rights Advocacy
www.elderrights.org.au









Sharing knowledge through reconciliation
Bush tucker garden helps close the gap
Developing a Reconciliation Action Plan, but then also living it, has been an important step for South Australian retirement living and home care service provider ECH in its mission to expand people’s understanding of Aboriginal and Torres Strait Islander cultures.
That’s why when the organisation’s Reconciliation Action Plan (RAP) Working Group created the concept of a Bush Tucker Garden a couple of years ago, it was vital that it was brought to life.
After much planning, the garden was formally opened this year on 1 June at the Encore Apartments Modbury site, to mark National Reconciliation Week.
The event was celebrated with a tour of its edible natives and bush foods hosted by Buandig woman and horticulturalist Leanne Williams, followed by an Indigenous-inspired afternoon tea for ECH residents and clients.
ECH Chief Executive Claire Scapinello is passionate about inclusivity and says engaging clients and team members in its reconciliation journey through a multisensory approach is a priority for the purpose-for-profit organisation.
“Expanding cultural knowledge while learning about the health benefits of native flora really inspired the planting of this new Bush Tucker Garden,” says Claire.
“At ECH, we are a proud and inclusive organisation which encourages residents and clients to embrace cultural diversity and social connections not only through this project at our ECH Encore Apartments, but in all we do.
“We engaged the knowledge and experience of Leanne, and we are so grateful for her generosity of time in developing the
garden. It’s a great way for us to learn from older people and elders within our community about bush tucker and how we can use the flora in our everyday lives.
“The garden has a large range of ornamental plants, fruit trees and native plantings, such as Bush Basil, Native Thyme, Beaded Samphire and Native River Mint, so we encourage residents and clients to take advantage of this opportunity to utilise them in their cooking.”
Leanne, who has a Diploma in Horticulture, Conservation and Land Management, has been presenting workshops to a range of community groups and at the University of South Australia as a guest lecturer in bush food plants, in order to promote their edible and sustainability properties.
“Bush food has sustained generations of Aboriginal peoples, and this event represents a rich and vibrant history in the culture of this land,” she says.

“The Bush Tucker Garden is a testament that ECH is committed to expanding our cultural knowledge and highlighting the significance and versatile qualities of native botanicals.
“It’s great to be part of this project; it means I get to share my culture with the wider community, and the residents of Encore have access to ongoing supplementary flavours they can add to their culinary dishes.
“Reconciliation plans are great, but we can’t just go off what’s on paper, it needs to be put into action. We need things like these gardens to be able to include people in reconciliation, and that’s when we’ll come together more and be able to walk together.”
Madeline Greenfield, Senior Marketing Manager, ECH www.ech.asn.auChanging the cultural narrative for older women
Greater understanding and tailored strategies will lead to better health outcomes
women are provided with the robust supports they need to live and age well. So how can we address and change these ways of thinking, and improve outcomes for older women?
a world accessible to, and inclusive of, older women.
Ageism is not a new concept. In Australia, older people continue to feel the impacts of ageism daily – something we highlighted at the National Ageing Research Institute (NARI) as part of our What Do Older People Want Report, published last year.
For older women in particular, these experiences are pervasive. Often considered an ‘invisible’ cohort, societal views of ageing contribute to women retiring earlier, often leading to lower incomes, assets, superannuation and poorer health, which put women at greater risk of elder abuse and homelessness. And for women with disabilities, First Nations women and other women of colour, these risks are exacerbated.
But women continue to make valuable contributions to our communities as they age – whether that be through work or volunteering.
In fact, 70 per cent of carers are women, which we know comes with its own range of health impacts – both physical and mental. Women continue to give back, even when it may come at a cost. It’s not only time we recognise these contributions, but also ensure older
Step one is to provide a space and platform for the voices of older women. We need to better delve into what older women want and need in order to inform every step we make towards change, rather than society trying to fix the perceived problem of ageing.
At NARI, part of our work is dedicated to understanding the significant health issues experienced by older women, and how changes to policy and practice can improve their ability to age well.

We work with older women to understand their experiences of health and ageing, and take these insights and apply them to our research and the implementation of new practices and strategies in the health and aged care sectors.
Ageing or older age is characterised by heterogeneity – more so than for other age groups. There is no ‘one’ type of older person, which is why co-design of health and aged care programs and policies is so important. The wants and needs of older people must inform us every step of the way, rather than society trying to fix the perceived problem of ageing.
We also need to recognise the importance of environment to create
In Western community-dwelling populations, for example, fall rates are higher in women than in men. What we know is regular physical activity can reduce the risk of falls – which is why dedicated spaces, such as Seniors Exercise Parks, which provide a place for older people to participate safely and freely in physical activity, are increasingly important and becoming more common in states like Victoria.
Intergenerational playgroups are another good example of adapting preexisting systems and environments with evidence showing these programs are beneficial for all involved.
These are ways we can shift our focus to create a world that functions for all ages, including older women.
As I wrote recently in my opinion piece published in the Sydney Morning Herald, when I went and watched the Barbie movie in cinemas, I was struck by the small ways the film celebrated the beauty in ageing.
To grow older wasn’t viewed with the negative stereotypes often attributed by society. But rather, as a triumph of its own – one that not all are lucky enough to experience (even ‘perfect’ Barbie).
Professor Briony Dow, Director, National Ageing Research Institute www.nari.net.auPromoting older women’s health and wellbeing must also include changing the pervasive cultural beliefs regarding the role and value of women as we age.

Sentiolux launches revolutionary nursecall system Acelo to transform the delivery of optimal patient care
As aged care facility managers across Australia face a crippling shortfall of more than 200,000 full-time care workers by 2050, the sector will be looking at new ways to ensure that the shortages don’t negatively impact the wellbeing of valuable – and scarce – colleagues.
Timing their launch to coincide with the Aged and Community Care Providers Association conference in Adelaide, leading care home technology specialist provider Sentiolux is launching a carer call system that can help managers utilise scarce staff and facility resources while ensuring that standards of patient care remain high.
SSG Acelo Nurse Call System is a state-of-the-art, intuitive solution, using fast, two-way local area network communication at the push of a button, with residents connected to staff with voice calls, to attend to their needs and give instant reassurance.

Acelo was designed during the pandemic and aims to reduce in-person staff visits to client rooms. This way, productivity increases while simultaneously ensuring resident safety and reassurance.
More just a way of communicating, Acelo is a way for all care givers, cleaning and catering teams to focus on their specific role and feel more in control, empowered and fulfilled as they deliver optimal service.
Acelo helps to organise workflow for whole facilities, enabling staff to work as efficiently as possible while maintaining resident satisfaction.
Mark Burrell, CEO of Melbourne-based Sentiolux, says “Acelo is a game-changing new technology designed to help care providers in Australia cope with unprecedented
challenges. It provides the ultimate in flexible communications systems – designed around the changing needs of a facility –at the lowest cost.
“With Acelo, residents can easily communicate with staff, alerting them to their needs at the touch of a button. The system is fully customizable, with a range of options for call buttons, in-room displays, and alert notifications, ensuring that even the most vulnerable clients receive the right level of care at the right time, and helping to safeguard their privacy and dignity.
“Acelo future proofs residential care communications’ systems, maximising estate adaptability, reducing capital expenditure and eliminating downtime.
“If you want to move devices from one department to another, or change care protocols, or, as residents change rooms, reconfigure their priorities; it takes seconds. All communications are logged and audited, so Acelo is also a matchless management tool.
“We believe Acelo is a game changing technology for all residential care facilities, which unleashes the potential of linking interoperable IP communications, from connecting in-house staff with health care providers’ smart phones to opening up voice channels in specific rooms – this is exciting and transformative technology for care facilities.”
Acelo also offers analytics figures and data based on monitoring resident call patterns, and staff response times to specific rooms.
Acelo is easy to install, designed as a plug and play system, minimising Total Cost Ownership. Installation time is minimised and requires few changes to existing hospital infrastructure and downtime.
To find out more about Acelo, check out Sentiolux’s website at www. https://sentiolux.com.au/ssg-unveils-acelo/
Making the most of the consumer voice
More than a point in time
The release of the revised Aged Care Quality Standards and Star Rating System recognises the essential role of older Australians and their families as key informants and experts in the design and delivery of the services they receive.
In rising to meet this challenge, aged care providers will require consumer experience systems and processes that go beyond surveys and ratings in order to achieve meaningful engagement, authentic consumer partnering and codesign all year through.
The consumer voice at every touchpoint
Relational feedback collected as narrative stories allows honest observations and feelings from all the touchpoints of a person’s experience to be shared. Stories can be submitted throughout the year, and may only be three sentences long, but provide a powerful mechanism for aged care providers to see their service through the eyes of the resident or client.
This form of de-identified relational engagement is particularly powerful in longer term care settings where care crosses over with daily living and allows for feedback to be shared freely all year through.

A compassionate quality response to feedback shared, particularly where expectations have not been met or things didn’t go right for the older person, offers dignity and validation, creating an environment where experiences and opinions can be shared safely and relationally.
Care Opinion is an online relational feedback platform working in the neutral space between older Australians and their loved ones, and the aged care providers delivering services to them, to support
an improvement and forward-focused dialogue about experiences in care – in a safe, moderated online environment.
Feedback on Care Opinion is shared in de-identified narrative story form about what matters most to an older person and their loved ones. All parties are kept safe throughout supported by strict moderation and publication guidelines, the focus being on feedback, quality improvement and partnership.
Relational engagement through responding
How an aged care provider responds to consumer feedback is one of the many ways they can demonstrate their quality improvement culture in action to their residents, families and workforce.
There is no faster way to convince an older person that an organisation is not listening than to say little more than ‘I’m sorry’ and use blanket statements such as ‘we are committed to person-centred care’.
The devil is in the detail – it’s about being transparent about the actions planned or taken, and use feedback to bring change and seek opportunities for co-design.
Caring for care
The consumer voice can be a powerful influencer of staff morale in a time when workforce retention and attraction are areas of concern for aged care providers. With praise one of the top three reasons why people leave feedback online, there is an opportunity for positive reinforcement for staff.
More than 50 per cent of stories shared on the Care Opinion platform are wholly positive experiences.
Framing to ask
Consumers are more willing to share their feedback when they believe their voice will be heard, valued and applied for improvement or learning purposes. This may be as simple as knowing a
personal ‘thank you’ to a staff member will be heard by that individual, or being reassured not only that concerns have been received but will be discussed and used for continuous improvement. The ability to respond publicly and invite further dialogue demonstrates a commitment not just to the individual but the community as well, that the organisation is listening.
Inviting older Australians to share their feedback year-round, in narrative form about the things that matter most to them complements formal interviews and surveys conducted annually as it:
■ captures the voices of residents experiencing neurological conditions affecting memory loss and cognition to share their story any time, and at the resident’s best time
■ provides a recent holistic view of resident experiences, enabling aged care providers to enact change while issues raised are current and support workers’ day-to-day learning
■ allows for real-time evaluation of improvements, particularly where targeted feedback campaigns are undertaken (eg. food quality and dining).
A year-round relationship through feedback
Relational feedback takes aged care providers on a learning journey of the consumer experience. It is a partnership that explores the power of storytelling, learning and growth through the development of a person-centred culture that looks after the aged care workforce and our older Australians –and it is a highly effective tool for both providers and care recipients.
Alicia Reid, National Operations Manager, Care Opinion Australia and Rebecca Somerville, Client Liaison Lead, Care Opinion Australia www.careopinion.org.auPeninsula Villages’ focus on resident individuality sees introduction of new language classes
Bringing Auslan to aged care
Peninsula Villages, a leading senior living community, is known for its commitment to creating a vibrant and inclusive environment for older aged residents. The organisation continues to set the bar high when it comes to promoting individuality among its residents with a wide array of activities offered catering to diverse interests including music, arts, exercise, gardening, wellbeing and craft classes.
Located in Umina Beach on the NSW Central Coast, Peninsula Villages prides itself on fostering a sense of belonging and community while respecting the unique qualities that each resident brings to the table. Their person-centred approach has garnered praise from residents and family members alike, with a new language class another example of the aged care provider’s dedication to fostering diversity.
Deaf residents, Jan Morley (86) and Maureen Stewart (87) are working with Deaf Connect to introduce a new class to the Village teaching Auslan, the Australian Sign Language, to fellow residents and staff.

Jan and Maureen met at the age of eight and have been close friends ever since. They moved to Peninsula Villages in 2020 and 2023, respectively, to be together and support one another. As active members of the resident community, the ladies participate regularly in bingo, gardening and art activities, but recently asked if they could create an Auslan language class for fellow residents and employees.
Jan and Maureen felt a strong desire to share their passion and language with others. Despite being deaf, they have never let their disabilities hinder their passion for communication and learning. The Auslan classes they offer provide a valuable opportunity for their fellow residents and staff to learn a new language and gain insight into the rich culture of the deaf community.
“We love using Auslan,” said Maureen. “It’s our way of communicating and it’s a beautiful language.”
“We’re so happy that staff and other residents are learning Auslan too,” said Jan. “It means that we can communicate with them better and they can understand us.”
The classes have gained popularity within the community, attracting an enthusiastic group of learners eager to broaden their horizons. Participants have not only been exposed to the basics of Auslan but have also developed a profound appreciation for the challenges and resilience of the deaf community and those hard of hearing.
“We’re so grateful to Maureen and Jan for teaching us,” said Peninsula Villages’ Leisure and Lifestyle Manager Linda Segrott.
“It’s a wonderful way to connect with them and other residents who are hard of hearing or deaf, and to make them feel more at home.”
Peninsula Villages’ commitment to fostering an environment of understanding and empathy has been warmly received by all residents.
“We’ve had nothing but unwavering support for the new Auslan classes and can already see the positive impact these have had on fostering meaningful connections among the residents. As a staff member learning it has really helped us to also communicate with residents who are losing their hearing as they age,” continued Linda.
As the Auslan classes continue to flourish, Peninsula Villages remains committed to promoting diversity, embracing individuality, and creating an inclusive atmosphere that fosters lasting connections among its residents.
“We are grateful to Jan, Maureen and Deaf Connect for their assistance in running the weekly classes, and we are excited to see how this will improve communication between our staff and residents,” said Linda.
Peninsula Villages www.peninsulavillages.com.au








Enabling a personcentred approach in residential aged care
By empowering aged care residents to actively participate in decision-making regarding their care needs, aged care providers can promote independence, dignity and individuality, while ensuring a higher standard of care.
Person-centred care has emerged as a fundamental approach to aged care services, and it can have a profoundly positive impact on the quality of life for older people.
Person-centred care means an individual’s preferences, needs and values are at the heart of their care. Rather than adopting a one-size-fits-all approach, person-centred care acknowledges the uniqueness of each resident, taking into consideration their history, cultural background and personal aspirations.
Effective communication forms the cornerstone of personcentred care, where residential aged care providers strive to create an open and inclusive environment in which residents are encouraged to express their opinions and concerns.
Ensuring resident participation in care planning
Regular meetings and care planning sessions can help ensure residents are actively involved in decision-making regarding their daily routines, activities and care options. Regular care plan reviews and updates help ensure person-centred care continues to be met as the individual’s circumstances and needs change.
Involving the resident’s family in the care planning process can also have a positive impact. By engaging residents’ loved ones in discussions and decision-making, aged care providers can gain valuable insights into a resident’s preferences and history and facilitate activities and social interactions to promote a sense of belonging.

Supporting culturally and linguistically diverse residents
Providers can also enhance person-centred care by respecting the unique backgrounds, languages and traditions of culturally and linguistically diverse (CALD) residents.
To achieve this, aged care facilities can offer multilingual staff and interpreters to facilitate effective communication. They can also provide culturally appropriate meals, activities, and celebrations that reflect the diverse heritage of residents.
Moreover, providers can prioritise staff training on cultural competency, enabling staff to better understand and meet the individual needs of CALD residents.
Transparent care enabled by smart solutions
Effective technology can create efficiencies that allow nursing and care staff to spend more time with residents, while enabling the resident to be actively involved in choices about their care.

When considering which forms of technology could best help your organisation to enhance person-centred care, look for solutions that are user-centred, easy to navigate, and can be learned quickly – even by workers who are less tech-savvy.
Telstra Health designed the award-winning CareKeeper app with illustrative icons to help care staff easily identify the tasks that need completing in required timeframes – a particularly important feature as 36 per cent of Australia’s care workers identify as CALD.
As CareKeeper is a mobile application, care staff can document charts and progress notes at the point of care, allowing for residents to be actively involved in their care documentation and reducing the time staff spend away from residents at the Nurses’ Station.
Telstra Health has also prioritised person-centred care with our award-winning electronic National Residential Medication Chart (eNRMC) conformant module, MedPoint, which connects aged care facilities, prescribers and pharmacies.
MedPoint can help aged care providers and prescribers to deliver informed, dignified care by enabling the capture of informed consent for medications prescribed; either from the resident or their loved one. This includes documenting that a resident or their loved one has understood why a medication has been prescribed or ceased, as well as the benefits versus the side effects of a new medication.
By leveraging cutting-edge technology, residential aged care providers can tailor their care delivery to the unique needs and preferences of each individual resident, while promoting informed and transparent care.
Michael Donnelly, Head of Aged Care, Telstra Health www.telstrahealth.com.auCommunication is key
Driving rural, regional and remote service innovation
Their unique role and the critical factors for success
Research and observation inform us that rural, regional and remote aged care providers are distinctly and uniquely different from metropolitan aged care providers.
Rural, regional and remote aged care providers are an integral part of the health, economic and social fabric of their communities. This makes them extremely well placed to address far more than just aged care or in-home care requirements.

Who are they?
Rural providers are usually small stand-alone aged care notfor-profits or government-funded hospitals, health services or multi-purpose centres in small country towns.
Regional providers are typically medium-sized aged care notfor-profits, privates or government-funded hospitals or health services in large regional towns or cities, with an increasing number being part of a national, multi-state or state-wide notfor-profit or private provider.
Remote providers on the other hand are more likely to be government-funded hospitals, health services or Indigenous aged care and health care organisations, as there are only a few not-for-profits and virtually no private providers. There may also be a few large national, multi-state or state-wide aged care or other human service not-for-profits that service particular remote areas of Australia.
Multi-faceted role
Leading providers in rural, regional and remote areas have a role beyond aged care. Take for example the more than 170
multi-purpose centres and similar providers that service rural and remote communities. These entities, whether not-forprofits or government-run, typically have service, business and financial models that represent an interesting mix of aged care, acute care, primary care and allied health care services, reflecting their communities’ requirements.
Multi-purpose centres are not the only providers of aged care services with diversified service, business and financial models. There are a range of public health services, community health organisations, aged care and Indigenous organisations that have a mix of services beyond traditional Commonwealth-funded aged care.
A few examples are, Sunraysia Community Health, a community health provider; Alpine Health, a public health service; integratedliving Australia, a not-for-profit aged care and healthcare provider; and May Shaw, a not-for-profit aged, allied and primary health care provider. These organisations share the key characteristics of:
■ providing a range of service options and pathways and the provision of care planning and care continuums for clients or residents
■ multi-service, multi-revenue, with a diverse range of aged care, allied health care or primary care practitioners with diverse scopes of practice
■ significant engagement and contributions from their communities, volunteers, local business and local, state and Commonwealth government.
These providers have moved well beyond traditional, programmatic Commonwealth-funded aged care service delivery and the associated aged care standards and quality
framework. They are in essence ‘Rubik’s cubes of care’ re-engineering their service, business and financial models sequentially and logically over time, against an agreed strategy.

Four success factors

integratedliving Australia is one of Australia’s leading rural, regional and remote aged care and healthcare providers. Originally servicing a few communities in the Upper Hunter Valley of New South Wales, it has now expanded to become one of Australia’s largest and most service diverse rural, regional and remote providers, with an increasing focus on healthcare.
Chair Doug Kimberley and Chief Executive Officer Catherine Daley identify four critical success factors that rural, regional and remote providers should understand and address:
1. Ageing clients or residents have emerging or actual chronic health and complex health issues, debilitating accidents or injuries, severe diseases or illness or any combination of these co-morbidities.

2 Any aged care provider’s mandate is to assist in keeping people out of hospital, help people exit hospital earlier, prevent hospital re-admissions and slow client or resident morbidity, that is their rate of decline.
3. A definitive health, wellness and lifestyle philosophy and approach should be adopted to enable a transformation from just aged care services delivery to integrated aged care and health care services delivery.
4. All providers should recognize they are and must increasingly become an integral part of the Australian Health Care System, along with primary care, acute care and allied health.

For boards, CEOs and executives or managers of rural, regional and remote providers, there are significant challenges and risks. However, ideas, innovations, strategies and projects can create new opportunities and developments in the provision of integrated aged care and health care, beyond traditional programmatic aged care.
Is your board and leadership team undertaking this journey? If not get out of the boardroom. Travel, visit and learn from the increasing number of leaders of rural, regional and remote providers who are driving innovation and developing new customer-centric services, business and financial models that are responding to their communities’ changing aged care and healthcare needs.
Michael Goldsworthy, Principal Consultant, Australian Strategic Services www.asspl.com.auNew Memory Lane Café supports LGBTIQ+ community members living with dementia
A first for Victoria is helping to bridge the gap
Research highlights the prevalence and impact of social isolation and stigma experienced by people living with dementia. People living with dementia tell us this is one of the biggest issues they face following a diagnosis of dementia as friends, family and community may struggle to understand how to best support them.
Dementia Australia has been tackling discrimination head on so that no-one with dementia feels isolated. We want to change attitudes to dementia and create greater empathy and acceptance within the wider community.
One of the ways we are working to change this narrative is through the Memory Lane Café program, which has been delivered nationally by Dementia Australia for many years.
Memory Lane Cafés are in-person events that provide an opportunity to meet people in similar situations, create a network of support and connect participants to services as needed. Dementia support specialists from Dementia Australia attend and are available to discuss services to suit their individual needs.
Recently, Dementia Australia, Lifeview, and the Victorian Pride Centre announced the launch of Memory Lane Café - Victorian Pride Centre. This innovative program provides a safe and inclusive space for people from LGBTIQ+ communities living with dementia and their carers.
For many people living with dementia, attending social functions can be challenging. The new Memory Lane Café - Victorian Pride Centre provides a welcoming, relaxing and fun venue for people living with dementia and their carers to meet, interact and foster meaningful connections within their community.
This project addresses the barriers LGBTIQ+ individuals face when accessing mainstream spaces and bridges the gap of social isolation for those living with dementia in LGBTIQ+ communities. There is significant power in creating spaces where people can share their lived experience and build connections in a welcoming and inclusive environment. We know that the impacts of stigma and discrimination can be significant and wide-ranging. Australian and international
studies show that stigma and discrimination associated with a dementia diagnosis can discourage people from seeking health care, including a diagnosis, and reduce social engagement with family, friends and the broader community. This can have serious consequences for the physical, cognitive and psychosocial health of the person living with dementia.
With more than 400,000 Australians living with dementia and the number expected to increase to over 800,000 by 2058, dementia is the chronic disease of the 21st century. We must ensure that all people impacted by dementia have access to appropriate care and support services.
The way we respond, communicate and interact with a person living with dementia has an enormous impact on their day-today life, and we can all do more to make sure people living with dementia remain included and accepted in their own community.
The Memory Lane Café - Victorian Pride Centre launched in September 2023. The events are free to attend, but bookings are essential. Call the National Dementia Helpline on 1800 100 500 or email vic.memorylanecafe@dementia.org.au to find out more.

Currently, this LGBTIQ+ model is currently only available in Victoria, however, Memory Lane Cafés operate in many locations across Australia. To see if there’s a Café available near you, or to learn more about this service or any other support we can help with, we are available 24 hours a day, 7 days per week. Please call us at any time on 1800 100 500.
Maree McCabe AM, CEO, Dementia Australia www.dementia.org.auAll-in-One Care Management Software

Put people first with next generation software designed to create better care outcomes

Aged care wage increase a step in the right direction
Earlier this year, the Australian Government announced a $11.3 billion commitment to fund a 15 per cent pay rise for aged care workers. The increase has been widely welcomed and celebrated by the sector, yet key non-direct care employees working in hospitality, maintenance and administration are excluded from the pay increase.
The intent of the funding increase is valid and finally acknowledges the hard work of the chronically underfunded aged care sector. What cannot be disregarded is the immense importance of non-direct care roles.
While the sector is dealing with the challenges of ongoing shortages and years of systemic underfunding by past governments, these workers make up 20 per cent of the workforce. At Whiddon, this figure is higher with non-direct care roles accounting for 26 per cent of our 2,800-strong workforce.
I have been working in the sector for 15 years and Whiddon pioneered relationship-based care. I have seen the positive impact all employees, regardless of role or position, have on the lives of the people we care for, as well as how valued these people are by our residents.
As someone passionate about improving and innovating the way we care for older Australians, it all starts with our employees and ensuring that we are looking out for them, first and foremost. Without the tireless support of these people, the system collapses.
The exclusion of non-direct care roles from the pay rise fails to celebrate and fairly renumerate care work, going against the grain of incentivising and driving people into the aged care workforce.

At this stage, the roles excluded from the increase will have to wait until next year before the Fair Work Commission hand down a decision. At Whiddon, we have made the decision to fund our own recognition payment for the ‘non-direct’ care workers as we await the outcome of the final hearing.
The Fair Work Value Case hearing
The Fair Work Commission Tribunal has been assessing the Work Value Case in three stages. The first two stages were finalised earlier this year and confirmed the 15 per cent increase for included employees.
Stage 3 to reassesses the excluded employees has been delayed with the decision to be revisited in 2024.
The Australian Government committed to funding the outcomes of the Fair Work Value case and to date have supported the first increase allocated to direct care employees.
The need for clarity
We believe there is a duty to non-direct care employees to set an expedited timing of the Stage 3 Work Value Hearing to provide clarity to all who play a vital role in caring for our senior Australians.
As a regional care provider, Whiddon has witnessed the frustration and feelings of being undervalued expressed by our team members in non-direct care roles. We have visited our team across the state and heard them say again and again how undervalued this makes them feel. A 102-year-old resident recently told me that it’s ‘shameful’ that the workers have had to wait so long.
Why we need a unified workforce
Every employee in aged care plays a vital role in the delivery of a level of quality care that older Australians deserve. Those in non-direct care roles are no exception. They have close working relationships with our residents and provide emotional support and cater for our residents’ needs as much as any other employees.
The sector would like to see the funding increase applied equitably ensuring all aged care workers are included. To continue to provide the level of care that our senior Australian’s deserve, we passionately believe that every worker is entitled to be paid for the incredible work they do, irrespective of how ‘directly’ they are involved in care, on paper.
Chris Mamarelis, CEO, Whiddon www.whiddon.com.auThe wage increase should be applied across the board not just to those in ‘direct care’ rolesA great aged care system starts with taking care of all aged care staff.



Innovative workforce program at Lutheran
Ongoing recruitment initiatives are ensuring quality care and ongoing viability
The Federal Government’s July 1 requirement for 24/7 registered nurses in residential aged care has put into sharp focus the role that innovative recruitment programs can play in attracting staff during critical workforce shortages.
With a 24/7 nursing model in place for some time, Lutheran Services knew the importance of investing in the recruitment and training of nursing staff – but needed to innovate and act quickly as national workforce shortages became increasingly challenging in the lead up to the 24/7 deadline.
This challenge generated two significant programs to super charge the organisation’s recruitment approach to upskill, reward and attract both Registered Nurses (RNs) and Personal Carers (PCs).
Along with the introduction of two innovative recruitment initiatives –Transition to Practice and Grow Your Future – Lutheran Services also invested in regional accommodation support, increased shift allowances, international nurse recruitment and importantly, above Award wages for RNs and PCs.
“We wanted to make sure we left no stone unturned in our approach to attracting staff and ensuring we continued to deliver high quality care and services,” said Lutheran Services CEO Nick Ryan.
“This strategy has required significant investment and an agile recruitment focus to ensure the workforce is fit to meet care minute targets and importantly, a good fit within our caring team culture.”
“We were able to onboard a cohort of new and experienced RNs and PCs ahead of the deadline through our Transition to Practice and Grow Your Future programs. In fact, Transition to Practice has been so successful we plan on expanding it to all of our aged care facilities,” he said.
In June, Lutheran Services’ fourth Grow Your Future program provided 20 trainee PCs with a passion for providing care to older Australians with paid work experience while they attained a Certificate III in Individual Support (Aged Care).
The program has attracted some 60 staff for Lutheran Services across
its aged care homes in Southeast Queensland, showcasing Lutheran Services’ commitment to not just attracting, but also upskilling and nurturing new workers to the industry.

A second recruitment campaign targeting final year university students is Transition to Practice, a collaborative program between Lutheran Services and the University of the Sunshine Coast.
The Transition to Practice program provides a viable pathway to employment in the aged care industry for nursing students in their final year of university. It offers the opportunity to fast-track their transition to work through
an industry placement. Incorporating hands-on learning with targeted education, the students cover critical topics in aged care such as dementia, fall prevention and end-of-life care.
First piloted at Lutheran Services Cooinda Aged Care earlier this year, Transition to Practice has since expanded to three Lutheran Services sites across Queensland, with 52 expressions of interest received for its latest intake.
Ushana Elimelech has been working as an Enrolled Nurse at Lutheran Services St Paul’s Aged Care in Caboolture for the past six years.

She’s in her final year of a Bachelor of Nursing, aiming to graduate as a RN at the end of the year, all while being a single mother to four children.
“All my kids were in primary school when I started studying and got the
job at Lutheran Services. Panic started to set in around how I would get them to school and day care, but it all just happened and fell into place, and I started on the morning shift,” said Ushana.
“I was very nervous going back to aged care because I hadn’t been in the workforce for a long time and was feeling insecure – I’m very grateful for all the support I’ve received,” she said.
Ushana plans on staying in aged care with Lutheran Services, where she’s elected to do her final eight-week placement before becoming an RN.
“I get a lot of satisfaction seeing people thrive and making a difference working,” said Ushana.
“You get to know residents so well and that’s why you care for them so well. In acute care, you might see a person once and never again.”
We’re helping you attract and retain nurses
National programs to support the nurses in your workforce
ACCPA’s Nursing Transition Programs are designed to attract nurses to a career in aged care, and upskill them for residential and community care settings – so your organisation reaps the benefits.
ACCPA offers a 12 month program for Graduate Registered Nurses and Graduate Enrolled Nurses in their first year of practice, and an additional six-month condensed program for experienced Registered Nurses transitioning into aged and community care for the first time.
“I love making connections with people. It’s holistic – emotionally and spiritually and how they function. You get to know their family and their friends, everything about them, and that’s why you can care for them so well,” she added.
Nick says Lutheran Services will always look to evolve its efforts to attract and retain staff.
“We currently employ almost 1,800 valued staff and with ongoing national skills shortages in aged care, we need to continually review and innovate our recruitment and training programs to maintain our valued workforce,” he said.
“In 2023, we plan to enhance our RN development program so we can retain the talented and committed staff who are the heart and soul of Lutheran Services.”
Lutheran Services
www.lutheranservices.org.au
Programs features include:
Online live professional development sessions run by clinical experts

Forums and networking opportunities
Organisation-based mentoring
On-the-job learning
Clinical assessment of competency
The next program intakes are in February and May 2024. Get in touch with us today, to find out how your organisation can benefit.
1300 222 721 accpa.asn.au/nursing accpa.asn.au/nursing
Nurse Educators are available to support the nurse, their mentor and the partnering organisation, for long-term staff retention.
Nurturing leadership in aged care
Inspiring change and combating burnout
In the fast-paced and ever-evolving landscape of aged care, effective leadership plays a crucial role in ensuring the safety, wellbeing and quality of care for older Australians.
Aged care leaders are the driving force behind creating a positive work environment, fostering a culture of compassion, and inspiring their teams to provide exceptional care. However, the demands of this continuing reform and change can often lead to burnout among leaders.
In this article, we will explore the importance of nurturing and fostering leadership in aged care while addressing the issue of burnout and providing strategies for combating it.

Embracing transformational leadership
Effective leadership in aged care involves embracing a transformational leadership style.
Transformational leaders inspire and motivate their teams by setting a clear vision and leading by example. They foster a sense of purpose, encourage innovation, and empower their staff to take ownership of their work.
By fostering a positive environment, leaders can create a ripple effect that extends to the quality of care provided to consumers.
Building strong support systems
Leadership can often be a lonely journey, but it doesn’t have to be.
Building a strong support system is vital to combating burnout. Seeking guidance from mentors, connecting with peers in the industry, and participating in leadership development programs can provide a source of inspiration, encouragement and fresh perspectives.
Additionally, fostering a culture of open communication and collaboration within the organisation encourages leaders to seek support from their teams and promotes a sense of unity.
Promoting continuous learning and development
Leadership in aged care is a dynamic and ever-evolving field. Encouraging leaders to engage in continuous learning and professional development is essential to combat burnout and stay updated with the latest industry practices.
Organisations should invest in leadership training, workshops, and conferences, providing leaders with opportunities to expand their knowledge, enhance their skills and stay motivated in their roles.
Prioritising self-care
Leadership in aged care is demanding, emotionally draining, and downright exhausting. Leaders are expected to serve a
number of roles, all while getting their day-to-day work done. That is why it is vital for leaders to prioritise self-care.
By taking care of their mental and physical wellbeing, leaders can better manage stress, make sound decisions and maintain their resilience. Regular exercise, proper nutrition, sufficient rest, and engaging in activities that bring joy and relaxation are essential self-care practices that can help combat burnout.
Encouraging work-life balance
Maintaining a healthy work-life balance is crucial for leaders in aged care. Encourage leaders to set boundaries and allocate time for personal activities, hobbies and spending quality time with loved ones.
By nurturing a healthy work-life balance, leaders can replenish their energy, reduce stress levels, and approach their responsibilities with renewed vigour and enthusiasm.
Are you doing enough for your leaders?
In aged care, leadership is a challenging yet immensely rewarding endeavour. By nurturing effective leadership and addressing burnout, we can ensure the provision of highquality care to our elders.
Embracing transformational leadership, prioritising selfcare, building strong support systems, encouraging worklife balance and promoting continuous learning are all key strategies to inspire change and combat burnout.
Leadership is always about people, and collectively at Anchor, we are ‘leaders enabling leaders’. Driven by our values, we support the industry with mentoring and development programs for leaders at all levels.
Let us strive to create a culture that fosters resilient, compassionate and motivated leaders who will continue to make a positive impact in the lives of our seniors.
Carla Beheram, COO, Anchor Excellence www.anchorexcellence.com.auYou can’t be what you can’t see Enhancing student nurse education in caring for older Australians
The recent announcement of Commonwealth support for nursing clinical placements in aged care is a welcome investment, but some may be wondering ‘what’s new?’. Maximising mutual benefits for nursing students and industry partners is a critical step in building the nursing aged care workforce required to meet current shortages.
Currently, most nursing students do go on placement to an aged care service, but generally this occurs early in their training and the focus is on fundamental skills such as communication and activities of daily living. Students are often paired with care workers rather than with registered nurses (RNs) on these placements.
This has meant that the work of RNs in aged care has been invisible to the students, including important tasks such as the use of fundamental care to assess and evaluate effectiveness of current treatments and medications; risk assessment; design of complex behaviour assessments and interventions; advance care planning; palliative care; and liaison with family and health professionals.
This lack of engagement between students and RNs leads to misinformation about the complexity of nursing care for older people and influences the students’ perceptions of what aged care work is, and how attractive it is as a future career.
The Clinical Placements with Older People (CPOP) program expands on the successful Gerontological Nursing Competencies project and was developed as part of the Aged Care Nursing Clinical Placements Program, funded by the Australian Government Department of Health and Aged Care.
CPOP will expose students to the role of the RN in aged care. Students will be paired with a RN, and experience the care of an older person through this lens.
Using a structured clinical placement strategy, clinical facilitators are allocated to support students during their placement. These facilitators are uniquely prepared by the UOW Adhere team, grounded in the evidence-based Gerontological Competencies program.
CPOP targets students later in their degree, when they have more knowledge regarding pathophysiology, pharmacology, assertiveness and advocacy communication skills, clinical governance, and evidence-based practice. Students are buddied with an RN, and supported by a clinical facilitator who will work with them for the duration of their placement, over two to four weeks.
The placements are in both residential and non-residential aged care settings, recognising that older person nursing care happens in many locations. The students use a reflective workbook containing a range of activities to helps them examine the role of the RN.
The activities are known as pedagogically rich activities, which support workforce learning by using goal-directed activities that help students see their expanding scope of practice, and facilitate engagement with staff about the complexities behind practice.
The University of Canberra in collaboration with Curtin University, Edith Cowan University and the University of Wollongong will deliver 320 CPOP student places to boost our professional nursing workforce in caring for older people.

CPOP is increasing the accessibility and visibility of expert gerontological nursing care for student nurses, and this is crucial to improving the broader
public understanding and valuing of the RN role.
We are hoping this will attract more graduates to gerontological nursing as a specialty, as they can see the importance in the provision and coordination of care, as well as the value that industry leaders place in the role of the RN to provide a quality service.
These workforce developments are essential to supporting the reforms needed in the sector, and to make RN work visible and admirable.
Right now is the time for universities, residential aged care services and registered nurses to be working together to create high quality clinical placements for nursing students in aged care and other settings providing complex nursing care to older people. Industry partners and interested registered nurses are encouraged to get further information on the program website, and aged care providers are encouraged to get in touch to offer your workplace as a placement opportunity.
Professor
TraceyMoroney OAM. Head, Curtin School of Nursing. Curtin University, Distinguished Professor Diane Gibson, Faculty of Health, University of Canberra, Professor Kasia Bail Faculty of Health, University of Canberra
www.canberra.edu.au/research/ centres/arg/cpop
The Ultimate Client and Care Team Experience
Drive high performing, person centred care teams, and deliver quality care outcomes for NDIS, MAC, HCP, CHSP, DISABILITY, AGED CARE, DVA and RETIREMENT.
• Client & Case Management
• Scheduling & Rostering
• Billing & Claiming
• HR and Compliance
• Award Interpretation & Payroll
• Forms & Workflows
• Collaboration & Communication
• Community Building
• Incident Management
• Policy & Procedure Compliance
• Maintenance Management
• Lifestyle Programs
• Group Program Management
• SIL Household Modules
• Dashboards & Reporting
• Teams and Coordinators App

• Family App

• Smart TV Application
• CareVision Academy
Embracing inclusivity in aged care
Workforce training is vital
As Australian society continues to evolve, lesbian, gay, bisexual, transgender and intersex (LGBTIQ+) older people are entering residential aged care homes and accessing aged care services, and deserve an experience that understand their needs, and respectd the challenges they have faced in the past.
A key way to support the dignity of the LGBTIQ+ community in aged care, is to ensure the aged care workforce is adequately trained.
Silver Rainbow LGBTIQ+ aged care awareness training is funded by the Commonwealth Department of Health and Aged Care, to help aged care workers understand the importance of LGBTIQ+ inclusive care. The training is coordinated nationally by LGBTIQ+ Health Australia (LHA), while in Western Australia, the training is facilitated by GLBTI Rights in Ageing Inc. (GRAI).
According to GRAI Executive Officer, Kedy Kristal, many older LGBTIQ+ people distrust most health and community care services.
“For much of LGBTIQ+ older people’s lives, it was illegal to be who they are. Their sexuality was regarded as a mental health issue, and it resulted in alienation from their family, work colleagues, and friends if they were outed; not to mention being vilified by religious organisations,” Kedy said. The training gives participants a deeper knowledge of the issues LGBTIQ+ older people have faced in their lifetime. They begin to understand the importance of pronouns, and gain insight into how to ask respectful questions, and better connect with LGBTIQ+ communities.
Tasmanian Regional Operations Services Manager at OneCare, George Wilson, has undertaken the training and was surprised by the information that was shared.
“I learned that LGBTIQ+ communities account for around 10 per cent of the broader Australian community – an epiphany for me, having been manager at Bishop Davies Court for going on seven years. It came with the realisation that of the hundreds of residents who have made their home here during my tenure, not one resident has ‘come out’ and declared themselves a part of LBGTI communities,” George said.
Following the training, Bishop Davis Court hosted their first Pride afternoon tea, which was well received by residents and staff. Improvements to admissions and care planning processes have made the aged care home more inclusive and friendly to all residents.

The Silver Rainbow Program aligns with the objectives of the national LGBTIQ+ Ageing and Aged Care Strategy, designed to create a better understanding of diversity and inclusivity across the aged care sector.
According to CEO of LHA Nicky Bath, while Australia was the first country to have a national strategy, which has guided a better understanding of our communities, there is so much more work to be done.
“Our training is available to both frontline staff, and those within leadership and board roles. When only select members of staff undertake the training, it does not always translate to the necessary change in organisational policy and procedures. We need to see increased inclusivity across the sector, which means a whole-of-organisation approach whenever possible,” Nicky said. While 5.9 per cent of LGBTIQ+ people are reported to be 65 years and older, they often do not make their sexual orientation or gender identity known to aged care providers due to past prejudice.
“We know that, overall, older LGBTIQ+ people seeking aged care or home
care are looking for services that are LGBTIQ+ inclusive,” said Kedy.
“We are often asked for recommendations by older LGBTIQ+ people, or by staff looking to be employed by LGBTIQ+ inclusive facilities and services. It is in the best interests of organisations to embrace inclusivity and attract quality staff.”
The aged care sector is going through a period of rapid reform and change following the Aged Care Royal Commission, and the Silver Rainbow Program is here to support aged care providers to meet their requirements and ensure that LGBTIQ+ older people are not left behind.
“We need to see increased uptake by providers of the My Aged Care LGBTIQ+ specialisation verification – a formal Government accreditation process –to ensure that LGBTIQ+ older people have choice and confidence accessing culturally safe aged care,” said Nicky.
LHA coordinates the Silver Rainbow Program nationally through partner organisations in every state and territory. If you would like to find out more about LGBTIQ+ specialisation verification or Silver Rainbow training, visit www.lgbtiqhealth.org.au/silverrainbow-training
LGBTIQ+ Health Australia www.lgbtiqhealth.org.au
The integral role of workforce diversity
Redefining care
As Australia’s population grows older, the demand for high-quality services in healthcare in general and aged care specifically becomes increasingly urgent.
Meeting this growing demand hinges on developing a skilled, diverse workforce in the aged care sector. Equipping our caregivers with a broad range of skills and knowledge is critical, but we also need to remember that fostering an environment of inclusivity in our workforce will help support the unique needs and experiences of our ageing population.
Elevating care through training
Investing in workplace training is paramount in shaping a competent aged care workforce. Such training involves providing comprehensive education to caregivers on critical topics such as dementia care, palliative care, infection control, medication management, fall prevention, nutrition, and more. Workplace training is an avenue for keeping employees up-todate on the latest industry standards and best practices.
Know more than just know-how
Equipping aged care workers with skills goes beyond practical knowledge. Workplace training should also focus on fostering empathy and understanding, arming workers with the emotional intelligence to handle their clients’ complex and diverse needs.
If they’re not doing so already, today’s reputable service providers may want to initiate emotional intelligence training for their staff. Such efforts can increase positive feedback from clients and their families, demonstrating that emotional skills are as valuable as practical knowledge in aged care providers – and healthcare providers as a whole.
Diversity demands diversity
It’s difficult to overstate the importance of a diverse healthcare and aged care workforce, but diversity of knowledge – both practical and emotional – is just the beginning.
A genuinely diverse workforce mirrors the diversity in our aged population. Caregivers from various backgrounds, experiences and cultures can bring unique perspectives, enabling a more personalised approach to aged care.

It also ensures that workers can understand and meet the specific cultural or personal needs of the varied individuals in our ageing population, making for a more inclusive, dignified and respectful care experience.
Diversity pays dividends
The potential benefits of a skilled and diverse workforce in the aged care sector are manifold. Such a workforce leads to a better quality of care and increased patient satisfaction, and by widening the scope of potential employees, providers have access to an expanded workforce.
What’s more, diverse care teams bring together a range of experiences, knowledge, and perspectives, which can lead to out-of-the-box thinking and creative problem-solving. This diversity of thought can likewise introduce fresh insights and ideas, challenging traditional practices and encouraging new, effective approaches in providing care.
Consequently, this helps drive continuous improvement in aged care, enabling the industry to adapt and excel in the face of changing demographics and evolving care needs.
A winning workforce
Through comprehensive workplace training and a commitment to diversity, we can ensure that caregivers in the aged care sector are prepared to provide high-quality, personalised care to all older Australians.
Embracing these practices, we’re not just futureproofing our aged care sector, but also creating an environment where every older Australian feels valued, cared for, and understood.
Kineo Courses www.kineocourses.com.auCelebrating 10 years of providing free dementia education worldwide
Build capacity in your workforce
The University of Tasmania’s Wicking Dementia Research & Education Centre is a global leader in providing accessible, low-barrier, online education. The Wicking Centre offers a wide selection of education programs, designed to provide cohortappropriate modularised content to a broad range of levels and roles in the health and aged care sector.
The Wicking Dementia Centre has two free Massive Open Online Courses (MOOCs), which have been improving dementia literacy worldwide: ‘Understanding Dementia’ and ‘Preventing Dementia’.
The Understanding Dementia and Preventing Dementia MOOCs are world-leading short courses, which to date have attracted 672,728 enrolments – 65 per cent from Australia and the rest from other countries across the globe.
The launch of the initial Understanding Dementia MOOC in 2013 was a key pillar to delivering on our mission – to support dementia knowledge in both families experiencing dementia as well as in the workforce across the aged care and health sectors. In October we will celebrate the 10th anniversary of this course, which is still going strong.
The Director of the Wicking Dementia Centre, James Vickers, said, “I’m very proud that we can continue to offer our free courses on dementia through the MOOCs program.
“Our aim is to offer an educational solution to people seeking to build their knowledge and skills in dementia.
“I’m sure that those who undertake the MOOCs as well as graduates of our degree offerings are agents of change when it comes to impacting the quality of dementia care and enabling our communities to be more inclusive of people with dementia.”
The dementia MOOCs are the leading educational resource on dementia accessed by aged care staff in Australia – and we encourage providers that are unfamiliar with our offerings to take a look.

Participants identifying as nurses and care workers consistently account for 18.4 per cent and 20.2 per cent of the
enrolee cohort respectively. Over the last 10 years, we have had people from a diverse background study our MOOCs, including:
■ health professionals
■ community and residential facility support staff
■ people in the early stages of the disease, their families and caregivers
■ social scientists
■ health policymakers
■ individuals with a general interest in dementia.
The Understanding Dementia MOOC is a leading health online course globally, and in the top 10 MOOCs out of over 15,000 MOOCs internationally, as ranked by independent global MOOC classifier, Class Central.
Participants who have successfully completed the Understanding Dementia MOOC have said that completing the MOOC has improved their confidence in their care approach, increased willingness to try new care approaches, improved communication and practical workplace changes, involved dissemination of knowledge to co-workers and improved working with families.
The format and design of the dementia MOOCs has been intentionally designed with a modularised framework. This enables ‘bite size’ learning opportunities, providing flexible and on-demand learning, across a variety of devices.
It’s important to acknowledge that this free education is government-funded, and the Wicking Centre is proud to deliver quality education to improve the community’s understanding of dementia.
Enrol your team members today in one of our free MOOCs and join the community of learners, to build capacity in your workforce and help improve the quality of care provided to those living with dementia.
Email us at dementia.mooc@utas.edu.au to find out more.
Wicking Dementia Research & Education Centre www.mooc.utas.edu.au
Unlocking the power of candidate profiling
Enhancing safety and efficiency in aged care recruitment
In the dynamic world of aged care, finding the right candidates to join your team can be a challenging task. With a shortage of qualified professionals and an increasing emphasis on safety, organisations are seeking innovative solutions to streamline their recruitment processes and reduce their workplace safety risk.
One such solution that has gained traction is the use of candidate profiling, a powerful tool that enhances safety and efficiency in the hiring process.
Candidate profiling is a comprehensive approach that utilises data-driven insights to assess and predict a candidate’s suitability for a particular role. By analysing various traits, skills and competencies directly related to the advertised position, candidate profiling helps identify the best-fit individuals who are likely to excel in their roles.
This strategic approach ensures a higher level of job satisfaction, productivity and overall success, as well as the opportunity to educate and provide development opportunities during the onboarding process within the aged care industry.
There are many advantages to candidate profiling, as explained in this article.
Streamlining the recruitment process
By leveraging candidate profiling, organisations can efficiently filter and shortlist candidates based on their suitability for the role. This saves valuable time and resources, allowing hiring managers to focus their attention on interviewing the most promising candidates from the onset.
Scientific precision
Candidate profiling employs a scientific approach, measuring and analysing specific traits and competencies that align with the requirements of the role. This data-driven assessment enables organisations to make informed hiring decisions, increasing the likelihood of finding candidates who possess the necessary skills and qualities for success.
Enhanced safety measures
Aged care providers understand the critical importance of safety in their work environments. With candidate profiling, organisations can identify individuals who exhibit a strong safety mindset and demonstrate the necessary skills to mitigate risks. This proactive approach helps minimise workplace injuries, creating a safer environment for both staff and residents or clients.
Improved job matching and productivity
By identifying candidates who possess the right combination of skills, competencies and mindset, candidate profiling improves job matching. When employees are well-suited to their roles, they experience higher job satisfaction, resulting in increased productivity, lower turnover rates, lower workers compensation claims and improved quality of care provided to older people.
Measurable results and return on investment
Implementing candidate profiling leads to measurable results. Organisations that embrace this approach often witness improved job performance, reduced turnover costs, higher employee retention rates, and increased overall return on investment. These benefits contribute to the long-term success and sustainability of aged care providers. For example:
■ 2.3 times fewer workplace injuries
■ 5 times fewer motor vehicle accidents during work-related tasks
■ 2.6 times lower absenteeism
■ 13 per cent stronger performance against quality standards
■ 4 per cent lower staff turnover.
Your hiring solution is clear
Candidate profiling offers a transformative solution for aged care providers seeking to enhance safety and efficiency in their recruitment processes. By leveraging data-driven insights and making informed hiring decisions, organisations can foster a culture of excellence, improve resident care and create a safer working environment.
As the aged services industry continues to evolve, embracing candidate profiling as a fundamental part of the recruitment process will become increasingly important. By understanding the unique traits and competencies required for success, organisations can proactively identify candidates who possess the right skills, mindset and commitment to thrive in the aged care sector.
Candidate profiling will continue to revolutionalise the way we approach recruitment. With a focus on enhancing safety and efficiency, this strategic tool ensures that organisations attract and select the best-fit candidates who will contribute to the wellbeing of residents and clients, and the success of the organisation.
Rod Farrell, Head of Injury Prevention, Prudence Rehab www.prudencerehab.com.auFrom survive to thrive
Financial wellbeing in focus
With financial stress rampant, how can your organisation support the financial wellbeing of your employees?
Workers in aged and community care have unique and sometimes overwhelming physical and psychological pressures to deal with. And with 2023 being marked by economic uncertainty and spiraling cost-of-living pressures, a different but related element has been added to the mix: financial pressures.
The link between mental and financial health can be a vicious cycle – financial stress can lead to poor mental health, which can make taking action to protect financial health more difficult. This is why many employers are taking proactive steps to help their employees navigate through challenging times.
Not surprisingly, poor financial health impacts both employees and employers. For example, Humanforce’s 2022 State of Employee Financial Wellbeing report revealed that almost 30 per cent of Australian employees do not have enough money for food and regular expenses, while 40 per cent struggle to meet bills and commitments. In addition, AMP’s 2022 Financial Wellness report showed financial stress costs Australian organisations $66.8 billion per year in lost productivity through absenteeism and distraction.
For those employees stressed about finances, there are crucial talent management elements to consider as well. PwC’s 2023 Employee Financial Wellness Survey found that 76 per cent would be attracted to another company that cares about their financial wellbeing. Even for employees who said they were not stressed, 57 per cent said they would be attracted to another company that cares.
The key words here are ‘financial wellbeing’; it’s not necessarily about more money but rather providing the tools, resources, confidence and education to help people navigate through tough times.
In aged care in particular, continuity of care is always a priority. Relationship-based care is strengthened by residents being able to forge strong, meaningful and lasting relationships with staff. This is tougher to achieve when there is a heavy reliance on constantly changing agency staff. Hence, employers should be doing whatever they can to retain and attract top quality staff.
A one-size-fits-all approach to financial wellbeing is less effective than empowering workers to pick and choose from a range of benefits that suit their personal circumstances. Employers of shift-based workers, like those in aged care, might consider offering the following benefits:
■ Providing access to an Employee Assistance Program (EAP), which can offer anonymous counselling services for employees at any time
■ Offering financial education including face-to-face sessions, webinars or mobile-based courses, covering a range of topics (eg. sessions on boosting superannuation, saving for a home, clearing student debt or financial budgeting)
■ Partnering with a local financial or tax specialist to offer these services at a discounted rate to employees
■ Helping employees to save on tax with salary sacrifice schemes, whereby they pay for a benefit through their gross salary, which reduces their tax liability
■ Subsidising travel costs to and from the workplace
■ Using benefits to stretch salaries – an employee discount scheme is one way to do this, helping people save money on a range of items, from the weekly supermarket shop to health and travel insurance.
Another popular benefit is providing access to earned wages. This aligns income and expenses by giving employees access to a portion of their accrued wages, in advance of pay day, with the remaining portion paid at the end of the pay period. Unlike salary-based lending or payday loans, on-demand pay does not involve borrowing on the part of the employee, and usually carries little to no cost.
This approach is even more effective if employees can keep track of their spend and are able to pick up extra shifts easily to cover any financial shortfall by using a workforce management software platform that also incorporates a suite of financial wellbeing benefits, such as Humanforce Thrive.
Financial wellbeing is an integral part of one’s overall wellbeing. Aged care providers that can offer benefits and tools that promote financial wellbeing can help them stand out from the competition as employers that genuinely care about their staff during these challenging times.

Humanforce
www.humanforce.com
Workplace culture and person-centred care
Workplace culture can significantly impact the performance of your business, whether it be recruitment, retention, absences, compliance and, importantly, consumer outcomes and satisfaction.
Workplace culture is the way your team interacts with one another and your stakeholders (consumers and their relatives) based on shared values, beliefs, policies and those attitudes and social ‘rules’ that are often implicit.
The people in your team impact your culture, as their personalities, interests and skills can influence the way they communicate and behave. Staff who support each other contribute significantly to a positive workplace culture.
But real success is more than a positive culture; your culture must also support person-centred care.
On a regular basis, management should reflect on:
■ How is person-centred care part of your values and business goals?
■ Does your workforce understand what this means in what they say and do every day?
■ How do you monitor your workforce and the quality of care and services they provide?
Now you’re really able to start looking at continuous improvement for your workforce and consumers, and not just quality assurance.
Recruiting for person-centred care
How do you support a positive workplace, person-centred culture and, consequently, employee retention and wellbeing, consumer health, wellbeing and satisfaction, business viability and compliance?
Recruiting and equipping employees with the skills and resources they need to do their best work based on a personcentred model, is a starting point.
Knowing your consumers’ expectations, whether they fit in with what you can provide, and who they are as individuals, is also critically important. This starts at their first contact with
you and is reviewed throughout their journey in receiving care and services.

To recruit for person-centred care, consider the following questions:
■ Do your position descriptions reflect what person-centred care means for your organisation, in a meaningful way, without the jargon?
■ When recruiting staff, do you ask questions related to your business goals and person-centred care?
■ Does orientation and induction (onboarding) look at your business goals and what person-centred care means for your organisation?
What attitudes and practices do you expect?
■ Is there a relationship with performance development and management?
■ Are your board and executive team driving your business goals and person-centred care?
The importance of monitoring systems
Your audits should not be just about ticking basic audit questions. Rather, use an audit as an opportunity to check what your procedures say and assess the quality of the information and observations that you gather, to improve all aspects of your organisation for consumers, employees and the business itself.
In relation to training, consider whether your organisation offers ongoing training reflect your practices and values, your consumers and the changing regulatory and practice environment.
Meanwhile, your comments and complaints system should reflect your business goals and what person-centred care means for your organisation.
Reflect objectively and see how your organisation fares. Really look at your workforce and continuous improvement as living elements of your culture, and practise improvement for positive consumer, team and business outcomes.
Karen Ross, Erigo M.A.C. and Erigo Training www.erigo.com.auHaving the ‘right’ employees and workplace culture are critical to success
Securing trained aged care workers from kiribati a win-win

Highfields Manor at Port Macquarie is tackling workforce challenges with ease
On a warm and sunny morning in late winter in Port Macquarie, aged care worker Akineti Tearau prepares for a very important day. One of a cohort of 13 care workers from Kiribati, Akineti is graduating with a Certificate III Individual Support (Ageing) and will complete a four year secondment program at Highfields Manor, under the Australian Government’s Aged Care Expansion (ACE) Program.
A new initiative within the broader PALM scheme, ACE supports the growing need for full-time care workers in the Australian aged care sector. Under the scheme, care workers from nine pacific nations and Timor Leste, are carefully selected and trained, initially in their country and then in Australia. They are guaranteed four-year positions in partnering Australian aged care facilities, subject to completion of the final training modules.
As an approved employer of the PALM Scheme, HealthX selected and screened this inaugural cohort through the Kiribati Institute of Technology (KIT) earlier this year. The 12-week in-country training was delivered under the guidance of veteran aged care trainer Sandy O’Brien at KIT.
Kiribati is a tiny island nation with a population of 120,000 people in the Micronesia subregion of Oceania in the central Pacific Ocean, where life is very different to Australia, so part of the preparation is about cultural nuances.
“In addition to delivering the first four aged care training modules, I prepare
the students for a big cultural change,” said Sandy.
“While they all speak excellent English, I spend a lot of time teaching common Australian terms, cultural norms and how to live away from loved ones.
“Australia is a dream destination for them, the money that they will earn over the four years will be enough to support themselves and send back to their families, to educate their children and to secure a better life on their return.
“They have long-term goals and are willing to make personal sacrifices to achieve these.”
The 13 Kiribati workers are lucky to all be placed together at Highfields Manor, a brand new, purpose-built residential aged care home in Port Macquarie, New South Wales. Director of Nursing, Yvonne Tilley spoke to us about the challenges in getting sustainable aged care staff and the positive impact the HealthX care workers have had.
“It’s very hard to get permanent aged care support locally,” said Yvonne. “About 50 per cent of our workforce comes from agencies, which is very expensive, and the lack of consistency of care is disruptive for residents”.
“Having completed the final modules of their Certificate III Individual Support online over 10 weeks while working under supervision in our facility, the HealthX PALM workers will now remain with us as full-time carers for four years.
“They are the most compassionate, beautiful people, who come from a culture where elders are highly respected and cared for. When dealing with irritable or anxious residents,
I often hear them singing to them, which instantly calms the resident down.
“They have integrated perfectly into our team. We have a lot to learn from this culture.”
The graduation ceremony at Highfields Manor included representatives from Department of Foreign Affairs and Trade, the Pacific Labour Facility, The Palladium Group, and HealthX.
Akineti received her certificate and together with her 12 friends and colleagues was gracious and thankful for this life changing opportunity.
“The training with HealthX has been a great opportunity for us because we have learnt how to meet the needs of the residents,” said Akineti.
“I am so grateful that I have the team at HealthX as they not only have supported us to fulfil our dreams but have helped us adapt to the Australian culture.
“We now feel confident and understand the roles that we have been employed for, so we can provide the best care for our residents.”
If you’re interested in finding out more about sustainable aged care solutions, please contact HealthX.
Siobhan Ruri, Director of Strategic Partnerships, HealthX www.healthx.com.auTraining for busy leaders
Would you like to build capacity in your aged care leaders but don’t have the time? Then choose an accelerated learning approach.
The Leadership Accelerator Program can be completed in just three months –with an investment of just 12 hours. For leaders in operational, clinical and corporate roles, this practical program is delivered as two interactive two-hour workshops each month – or you can purchase modules individually.
Upon completion, your leaders will have a deeper knowledge of key criteria and skills outlined in the Australian Aged Care Leadership Capability Framework – along with a renewed mindset and fresh enthusiasm.

Don’t wait until your leaders are overwhelmed and exhausted, give them a helping hand today.
The Leadership Accelerator Program has been developed by Aged & Community Care Providers Association specifically for the aged care sector.
Leadership Accelerator Program
Six two-hour workshops
Three months
Optional CILCA360 analysis
Option to ‘pick and pack’ or register for the set
An exclusive program is available for organisations that would like to train groups of 18 or more leaders
Wellness grants to improve the mental fitness of aged care nurses
Altaira’s innovative approach
Through their partnership with wellbeing organisation Healthcare Heartbeat, labour hire agency Altaira have embarked on an innovative approach to support the aged care workforce, by delivering Wellness Grants to aged care nurses, beginning with those based in Victoria and South Australia.
Across Australia, untreated mental health symptoms have led to health professionals having a 30 per cent higher risk of suicide than people in other occupations, while the pressures of aged care are responsible for many people leaving the workforce.

Altaira Director Jelena Giro has first-hand experience managing these challenges, which was the inspiraton for Altaira’s new initiative.
Partnering with Healthcare Heartbeat to deliver Altaira Wellness Grants and other mental fitness initiatives to help aged care nurses learn preventative strategies and tools that will help them long-term.
“At Altaira, we understand the importance of having skilled and compassionate professionals to care for our residents. But the fact of the matter is that aged care nurses dedicate their lives to the wellbeing of our seniors, often at the expense of their own health and the health of their families,” Jelena said.
“Many staff are at breaking point and energy reserves are at an all-time low. This is having a significant impact on the aged care sector.
“By enabling our aged care workers access to Wellness Grants through Healthcare Heartbeat, they can learn how to better recognise signs of stress and ideally put strategies in place to prevent this from progressing to burnout.
“t’s not a quick fix to the many challenges we are all currently facing, however it’s a step in the right direction.”
Recipients of the Altaira Wellness Grants receive a Reflect, Reset & Renew Session, which explores foundational wellbeing practices and enables participants to develop an action plan for integrating three wellbeing habits into their daily experiences. The two-hour online group coaching session focuses on strategies that can be used in the moment to regain a sense of calm, even when healthcare workers are in the midst of a hectic shift.
Grant recipients also receive a delivery of authentically homecooked meals, giving them a chance to have a break from the
stress that can sometimes come with ongoing meal prepping and grocery shopping.
Janice, a Clinical Nurse Educator within the aged care sector, took part in the Reflect, Reset & Renew Session earlier this year. “This coaching experience assisted me with ‘re-tuning’ myself as a healthcare practitioner. It assisted with reflecting on all the enjoyment I have in nursing and caring for the older person, opportunities to reflect and think about how I can best care for myself and those in my community.”
The flow-on effect of strengthening an aged care worker’s mental fitness is that it can also improve the quality of resident care they deliver, boost morale and improve retention rates. Furthermore, research has shown that every dollar spent to improve mental health at work can achieve returns of up to four times, through improved productivity and savings from workers compensation claims.
The Altaira Wellness Grant is open to all aged care nurses in Victoria and South Australia. Encourage your team members to apply today, or apply on their behalf, it’s a wonderful way to acknowledge their hard work and show your appreciation.


Altaira
www.altaira.com.au/apply-for-an-altaira-wellness-grant
Behind the stars
Fresh perspectives on industry comparisons
Australia’s aged care sector is currently undergoing significant reform, driven by recommendations from the Aged Care Royal Commission. These recommendations encompass changes in provider subsidies, ensuring quality of life for participants, and mandating greater transparency for providers.
In December 2022, the Residential Aged Care Star Rating system was launched, with its findings made available on the My Aged Care portal, allowing consumers to compare over 2,500 aged care facilities. However, this system has been criticised for its premature release, lack of context and questionable results specific to facilities.
The Department of Health has given providers a summary of these results, but has not provided detailed metrics or benchmarks for comparison.
Seeing an opportunity, Melbourne’s Blue Bike Solutions, a consulting firm specialising in the community sector, developed ‘Behind the Stars’ to scrutinise and offer insights into the Star Rating data.
This ground-breaking initiative combines the raw Star Rating data with other open data sources to offer previously unseen benchmarks and insights into determinants of Star Rating results and the potential considerations for aged care providers regardless of their for-profit; not-for-profit or government status.

Blue Bike anticipates regular updates to this analysis as more Star Rating data becomes available, enabling performance tracking over time.
In terms of methodology, data was sourced from the My Aged Care portal, and then enriched by drawing from the Gen Aged Care data clearinghouse and the Australian Charities and Not-forProfits Commission.
Blue Bike remains hopeful for easier access to richer and broader data in the future, aligning with the wider industry’s push for transparency and innovation.
The maiden Behind the Stars analysis demanded a fresh approach and experimentation to identify the most effective strategies for meaningful and accurate data evaluation.
By melding the Star Rating outcomes with other datasets, Blue Bike can offer fresh perspectives on comparative measures and insights, fashioning dashboards and metrics that elucidate the story within the data.
It is also possible to ‘zoom’ in and out on the data to see down to the facility level for specific providers or across geographic and organisation dimensions.
One key discovery from the initial analysis suggests that facility size is instrumental in performance; smaller facilities consistently outdo their larger peers. This trend is primarily driven by resident experiences and staffing levels.
Smaller facilities tend to foster a closer bond between carers and residents, perhaps because of their cosier and more familial environments. Moreover, these smaller establishments more consistently achieve the AN-ACC care minutes targets, suggesting their staff aren’t as overwhelmed in terms of workload – or finding a better balance between resident care and experience with the organisation demands for processes to support quality and compliance.
Non-compliance considerably eclipses all other considerations in determining the ratings, stressing the urgency for providers to uphold regulatory standards. Facilities failing to meet compliance standards are restricted in their overall Star Rating, potentially misleading consumers if they don’t delve deeper into the facility’s performance in other areas.
The analysis also suggests that financial motives influence Star Rating outcomes. While it might be an oversimplification to suggest that private providers prioritise profits over care, there’s a marked difference in performance between government and non-government entities.
Recognising that all operating entities need to be fiscally responsible and sustainable, the data shows that government-run facilities, which aren’t driven by managing profitability but rather managing budgets, excel in the ‘Resident Experience’ and ‘Staff Rating’ categories.
This difference raises eyebrows about whether non-government providers operate on a level playing field, especially considering that community services such as residential or in-home care in the local council area might be subsidised by other revenue streams.
Behind the Stars is merely one aspect of the broader SectorFirst portal platform developed by Blue Bike Solutions, which aims to transform the community sector by delivering actionable insights from data – without demanding significant investment in time from care providers or business intelligence capabilities.
Providers can get free access to the Behind the Stars data portal (starratings. sectorfirst.com), by getting in touch with Blue Bike.
Cameron Bedford, Founding Architect, Blue Bike Solutionswww.bluebike.com.au
How is the industry performing under AN-ACC ? Analysis reveals significant under-funding
In this analysis of a sample of industry data we consider how the industry has been performing under AN-ACC during the second quarter of this year – and if we can determine the industry is missing out on funding to which they are entitled.
What’s been happening in My Aged Care (MAC) Data
Considering a sample of 258 facilities, which comprises of 17,821 beds, our analysis identified the following key points.
Requests. In the quarter two of 2023 (April to June), aged care providers made 4,989 requests in MAC, which represents a 13 per cent (4,421) increase compared to quarter one of 2023 (January to March) and represents one request for every four beds in this sample.
To date, 70.2 per cent (3,504) of these requests have been finalised, 20.1 per cent (1,004) are pending and the remaining 9.7 per cent (481) were either recalled or rejected.
Time to complete assessment.
The time to complete a request has been steadily decreasing since the beginning of the year. The average wait time in January 2023 was 20.4 days, which decreased to 19.2 days by May 2023. It seems that despite an increase in workload, the Department of Health is improving their wait time for providers.
We can see a positive trend of requests for assessments increasing, which is extremely important for providers as they need to be correctly funded for the care they are already delivering; and the shorter wait time for assessments is welcomed.
What’s been happening in industry performance data?
In this analysis, we’ve considered a sample of 776 facilities that we are actively monitoring through our management services.
Average AN-ACC. This year, the average daily total AN-ACC funding has increased 3 per cent from $219.83 in January to $226.39 in June. The AN-ACC starting price has also seen an additional 12 per cent increase starting from 1 July 2023.
Occupancy. Over the same period, the industry sample has seen a 2.5 per cent gain in occupancy, where the total occupancy is currently 88.33 per cent. Two thirds of this originated from an increase in permanent occupancy, while the remaining third comes from an increase in respite occupancy.
Reclassification statistics. Investigation into the reclassification statistics of the first half of 2023 indicates there could be unrealised funding in the industry with lower reclassification activity and a decline in results.
The reclassification rate (the percentage of residents in care who have been reclassified) has dropped from 11.6 per cent to 10.3 per cent (the overall number has dropped from 6,423 in quarter one to 5,735 in quarter two). One possible reason for this is the increase in assessment workflow due to the increase in occupancy in the sample. Providers need to make sure they have contingencies in place so reclassification workflows don’t fall behind.
Reclassifications submitted resulted in:
■ Those with no change have increased by 1.0 per cent to 18.6 per cent
■ Those reclassified higher have decreased by 1.3 per cent to 74.9 per cent and the average monetary
increase has also decreased by 50 cents
■ Those reclassified lower have increased 0.4 per cent to 6.5 per cent and the average decrease increased by $3.65.
Are facilities underclaiming AN-ACC funding?
We can categorically say residential aged care providers are underclaiming AN-ACC funding.
Missed funding might happen based on one more of the following:
■ assessments, care delivery or carer knowledge are incongruent
■ care plans are not written well for the AN-ACC tool
■ an increase is not identified
■ a bad outcome isn’t recognised and no reconsideration is pursued – especially where a decrease has occurred.
From the hundreds of AN-ACC Funding Health Checks we’ve completed this quarter, we are finding aged care homes are conservatively missing out on average of between $250,000 to $870,000.
I say ‘conservatively’ as these are clinical documentation audits and only picking up on documented care that is already being delivered – unfunded care. While completing the audits, we also do a quality and compliance review and can also say that due to the quality issues we find, we know we will identify more missed funding when we complete the next stage of our identification.
If you’d like our help to ensure you’re getting the right amount of funding for your operations, we’d be only too happy to assist.
Peter Morley, CEO & Co-owner, Provider Assist




How to ensure quality care while maintaining financial viability
What providers need to consider today
Aged care reforms have brought significant changes to the sector, aiming to improve care outcomes for older people while supporting providers’ financial viability. However, recent findings from Stewart Brown’s sector report indicate that the number of homes operating at a loss has increased from 60% per cent in December 2021 to 63 per cent in December 2022.
It is crucial to recognise that without financial stability, achieving high-quality care becomes unattainable. The industry has been slow to adopt new funding models in the past, directly impacting financial viability.
To ensure older people receive the support and services they need for high-quality care, providers must quickly understand the aged care reforms and their organisational impact.
What does this mean for providers?
To support improvements in risk monitoring, the Australian National Aged Care Classification (AN-ACC) claim data will be shared with the Aged Care Quality and Safety Commission. This data, combined with other regulatory intelligence, will assess providers’ response to minimum care minute targets and the suitability of their skills mix within their services.
Approved providers are also responsible, under the Aged Care Act 1997 for maintaining an adequate number of appropriately skilled staff to meet the care needs of recipients. Failure to meet these requirements puts residential aged care providers at risk of not meeting the Aged Care Quality Standards.
Providers need to align their workforce’s skills mix with the resident case mix to ensure compliance. Various models of care exist within the industry, adaptable to regional availability constraints and the complexity of required care.
Legislation mandates that consumers receive high-quality care based on their individual needs, goals, and preferences. Strategies should not only deliver that level of care but also enhance trust and confidence in the aged care sector’s performance. There is more funding available than ever before to contribute to improving care outcomes and business viability. The introduction of AN-ACC in October 2022 has significantly increased subsidy, surpassing the consumer price index (CPI) and awards.
In July 2023, both the Aged Care Award and subsidy experienced the largest increases in Australian aged care history. Over the past eight years, wages and subsidies have grown by 36 per cent, with subsidies making significant progress in the last year. This affirms the Royal Commission’s recommendation that providers must allocate more funds to clinical and direct care.
How are providers balancing these requirements?
Balancing all these requirements is critical. AN-ACC and Star Ratings now integrate funding, care minutes (rosters) and quality more closely than ever before. With increased activity from the Aged Care Quality and Safety Commission, time is running out to address these issues.
Here is a list of activities providers should prioritise:
■ Enhance management-level reporting to provide oversight on daily

funding and care minutes, including forecasting changes related to new pricing and care minute levels.
■ Improve systems and data capabilities at the resident level to support decision-making on potential reclassification for funding purposes.
■ Establish a new process for reviewing all residents to identify potential AN-ACC changes every two to three months.
■ Streamline care minute reporting for quarterly financial reporting (QFR) and develop the ability to forecast positions within the quarter.
■ Evaluate the efficiency of rosters and determine the optimal balance between funding and care minutes for each site.
■ Implement an efficient rostering system with costed rosters and shift offers, enabling real-time decisions on cost and staff availability to minimise reliance on agency staff.
■ Initiate a review process for the new quality indicators, plan for the new standards, and assess their impact on operations.
■ Understand Star Ratings, how each element is affected by the above initiatives, develop an overall strategy and identify short-term improvements to ratings.
Mirus Australia is currently assisting over a hundred providers each month in addressing these initiatives, lending a helping hand to providers that want to understand how they can maintain financial viability while providing quality care – something that should be a priority for the entire industry.
Katie Airey, Manager –Quality, Risk and Compliance, Mirus Australia www.mirusaustralia.com
How to achieve a successful aged care divestment
Minimise impact, maximise outcomes
Divesting an aged care business is a significant strategic decision which requires proper planning to minimise impact to residents and care recipients while maximising the outcome for the provider.
Providers considering an exit from aged care services can plan for success using a proven framework: agree the transaction objectives, prepare a plan and timeline, get organised and put together a team.
1. Agree the transaction objectives
The provider’s board should agree its current status, future strategic direction and motivation for the sale.
Understanding the objectives for the transaction is an important first step to determining the best approach, including but not limited to:
■ having an informed view of the assets tabled for sale and the relevant market
■ structural impacts of various options on residents, client recipients, employees and other stakeholders such as financiers and the Department of Health and Ageing
■ tax implications of various alternatives.
A measured approach will help to guide the board’s decisionmaking process about whether the divestment will likely achieve its strategic purpose as you begin to engage with interested parties.
The board can then plan for honest communication with government, employees, residents, their families and the community regarding the intention of the provider to exit aged care services and the process. This should aim to inform people about the planned changes to bring them along the journey.
2. Prepare a plan and timeline
To assist with a smooth sale, it is helpful for a provider to set out the series of steps with target dates, which can be used by the board and executive as a roadmap to follow throughout a transaction process.
The use of a roadmap can help clearly inform and communicate the significant effort that is required to effect a sale and target realistic deadlines, acknowledging that once in the market not everything is within your control.
3. Get organised
Not only does presenting the key information in an accurate and easy-to-interpret manner build credibility in the eyes of a potential purchaser, proper preparation will inform the board and management of likely value drivers to maximise value and the key issues that may arise regarding saleability.
We always recommend looking at your business ‘through the eyes of the buyer’ by conducting internal due diligence ahead of time. Issues are then known and quantified before an external party finds these and uses them to negotiate on price, or walks away.
Presenting information to interested parties in an online central location (best done with the use of a virtual dataroom hosted by a specialist provider) can help a provider to manage privacy and facilitate Q&A with multiple interested parties. Importantly, it also keeps a record of the relevant disclosures and negotiations regarding warranties and indemnities provided by sellers.
4. Put together a team
A divestment process will be disruptive to clients and residents and place additional demands on management, so providers should plan to increase management capacity when undertaking a transaction by drawing on external professional advisers to run the transaction process.
Transaction advisors can assist with preparing a transaction roadmap, fact checking information for interested party due diligence, compiling and managing a virtual dataroom, and assisting in negotiations with interested parties. In some jurisdictions where property is involved, a registered real estate agent may also be required.
Once negotiated, a transaction should be documented to give legal effect to the transaction, ideally by lawyers with aged care experience, who understand the unique commercial and regulatory environment.
Increase the chance of a successful transition of the business to an incoming purchaser by setting a clear transaction objective – planning and preparing for the process will mitigate surprises that can disrupt transactions and impact value.
Andrew Fressl and Sam McCombe, McGrathNicol Deals Partners www.mcgrathnicol.com
The significance of cash management
Despite numerous changes in regulations, what is still in the control of operators is how the balance sheet is managed.
Effective financial management is crucial for aged care providers to ensure the sustainability and high-quality delivery of care for older people who access services. Among the various aspects of financial management, managing cash effectively plays a pivotal role – with significant benefits and opportunities for aged care providers.
For the aged care sector, it is not just about the accounting, but about the treasury functions. This refers to the way deposits are placed effectively and cashflow is managed.
Effective cash management is crucial for maintaining financial stability, in relation to analysing cash flows and identifying surplus funds.
This allows providers to invest in infrastructure, enhancing staff training and upgrading equipment.
A proactive approach helps ensure the long-term viability of aged care facilities, enabling them to deliver high-quality care to residents.
Being ‘clever’ doesn’t mean managing an investment portfolio or using overly engineered structured products. Being clever is just about being efficient: earning as much from the banks as possible on any capital and ensuring excess cashflow is not left with banks at little to no interest. Banks call this ‘treasury management’ or ‘balance sheet management’.
The role of the Chief Financial Officer in aged care as we move forward is not just about reporting and managing operational cashflows. They should also ensure that the operating cashflows are highly efficient and that the company has the capital on call to meet the plans of the management and board.
A solution is not sticking with just one bank, and staying up-todate with interest rates, ensuring you get the best deal. Remember, banks only need you as a depositor until they run out of need for that capital. They pay for your deposits until they can’t make any more money lending your capital, so the rates they offer will also decrease accordingly.
The key is always depositing with the banks that want your capital and doing so without taking on extra risk.
Treasury management is not something that an operator can outsource as every operator’s strategy is different to the next.
A tailored approach for aged care
Care360 are partnering with aged care providers to provide a vehicle to benefit from a low cost ‘Treasury Management’ service ensuring that operators maximise deposit rates available.
Care360 is a FinTech (digital technology finance) company that combines transparent information and advice with innovative financial technology solutions to extend providers’ financial resources and reduce the administrative burden. On the flip side, we also help families to enhance their finances in order to secure the best possible support for their loved one.
Care360 is partnering with forward thinking businesses to provide innovation in the aged care sector to deliver real change and innovation for providers in how they can proactively manage their cash flow more productively, to deliver enhanced investment returns.

Our offerings allow portal access to multiple banks, cash on call, and the most competitive deposit rates currently offered in the market.
Whether you choose Care360 or another finance company, it’s important to do your due diligence and ensure you’re getting the most competitive product, with the least amount of burden.
Tim Pritchard, CEO, Care360 www.care360.com.auWhat aged care providers should knowTim Pritchard (far right) with the Care360 team.
Key personnel suitability in aged care
Are you ready for the December deadline?
Providers would now be very aware of the changes to suitability of key personnel requirements which commenced last December. As part of these changes, approved providers are required to undertake an annual assessment of all key personnel, with the first annual assessment to be completed by 1 December this year.
This should be a matter of urgency, because failure to comply with this obligation is an offence which can result in a penalty, and enliven regulatory action which can ultimately result in sanctions (including revocation of approved provider status).
Who are key personnel in aged care?
It is critical providers identify their key personnel, because if you don’t apply the requirements to certain personnel who are in fact key personnel, penalties will apply.
Broadly speaking, the key personnel of an entity are those responsible for key aspects of an approved provider’s operations, which ultimately underpin the quality of care and services provided to care recipients.
According to the Aged Care Quality and Safety Commission Act 2018, key personnel include managers, board members and anyone else with “significant influence over planning, directing or controlling the activities of the approved provider”. At a service level, it also includes managers and senior nurses.
What is required by 1 December 2023?
December 2023 marks the end of the first year of operation of the legislation and subsequently the end of the allocated period to complete the annual review of key personnel.
Under the legislation, approved providers are required to, at least every 12 months:
■ consider all suitability matters (impending, new or historic) in relation to key personnel
■ be reasonably satisfied that key personnel are suitable to be involved in the provision of aged care
■ keep a record of those matters in accordance with Accountability Principles requirements.
Some of the key matters to consider include (but are not limited to):
■ the individual’s experience in providing aged care or other relevant care
■ whether the individual has been convicted of an indictable offence or has been the subject of a civil penalty order
■ whether the individual is or has been the subject of adverse findings or enforcement action by a regulatory body (for example, for key personnel with nursing or allied health qualifications, this would include adverse findings by a tribunal in relation to the person’s conduct as a health professional).
This will require approved providers to undertake and record a comprehensive assessment of suitability for each of their key personnel, which will require contributions from each of these people. As such, we urge providers to start this process immediately if they have not already.
To be clear, if there is a suitability matter identified with someone identified as key personnel, it does not necessarily mean that the person should not be a member of key personnel. Rather, the provider will need to conclude whether it is ‘reasonably satisfied’ that the individual is suitable having regard to all the suitability matters. However, if a suitability concern does arise, providers will need to carefully consider the implications.
What are the other obligations in relation to key personnel?
In addition to the annual assessment, providers must also:
■ consider the new suitability criteria before engaging the person
■ notify the Commission of any changes in key personnel or any suitability matters within 14 days. (This is a shorter timeframe than previously required.)
Failure to notify will result in an offence of strict liability as well as possible sanctions under the Aged Care Quality and Safety Commission Act 2018
Where a provider is a Corporation, its key personnel must also notify the approved provider of any change in circumstances (change in suitability matters) within 14 days of becoming aware of it. Failure to do so will result in a penalty to the key personnel who did not notify the change.
Russell Kennedy key personnel pack
Our team have developed a range of resources that providers can purchase individually or as a pack to assist with your compliance requirements. These include an assessment guide, summary of the requirements, training, policies and clauses for employment agreements. To purchase any of these resources, please get in touch with us.
Victor Harcourt, Principal, Russell Kennedy Lawyers
www.russellkennedy.com.au
Disclaimer: The information contained in this article is intended as general commentary only and should not be regarded as legal advice. Should you require specific advice on the topics discussed, please contact Russell Kennedy Lawyers directly.













Imagine paying for your workers compensation premium twice
Understanding claims and the impact on your operations
Providers’ public liability insurance policies are increasingly being viewed as a source of funds for workers compensation insurers nationwide, with recovery claims being made in two ways, and it’s important to understand the difference, so that you’re not paying for the same compensation claim through different channels.
Recovery claims by workers compensation insurers against the provider as ‘host employer’ for injured contracted labour hire
Labour hire staff are seen as a necessary cost for most aged care providers in the current climate, meaning they are now exposed to the risk of a workers compensation recovery claim for injured contracted workers.
The provider, being the ‘host employer', is legally responsible under WHS legislation for contracted workers and contracted workers have the same protection as employees.

If a contracted worker is injured, the labour hire company’s workers compensation policy will respond, not the policy of the provider or host employer. However, workers compensation insurers are now seeking recovery against the host employer for these costs citing the WHS-regulated responsibility for the safety of the injured contracted worker.
The insurance policy which has been called to respond is the host employer’s public liability insurance policy.
This exposure will continue as a significant risk to providers, as workforce resourcing is currently the single largest challenge faced by the aged care sector. Providers should be seeking to provide contracted labour hire workers with the same training, supervision and support as if the workers are employees.
Recovery claims by workers compensation insurers via the ‘employing entity’ of the injured employee against the ‘earning entity’ of the same organisation
In many provider entity structures:
■ the ‘employing entity’ employs all the staff and arranges the workers compensation policy
■ the ‘earning entity’ (a separate entity) earns the income and manages the care and compliance.
The employing entity’s workers compensation insurance will respond to claims by injured employees. However, workers compensation insurers are now seeking recovery via the earning entity’s public liability policy as the earning
entity is cited as responsible for the WHS obligations of the employees. Despite being in the same group of companies, workers compensation insurers view the earning entity as a separate organisation.
To date, public liability insurers have been responding to these problematic claims, as the workers compensation insurer is considered under current wordings to be an external party and not an insured, not invoking the insured versus insured exclusion under the policy. We anticipate that once public liability insurers understand this exposure, they may introduce exclusions to remove the capacity for these recoveries to continue to take place, or will refuse to provide terms altogether.
There are other implications for providers to consider, however, engaging with legal and tax professionals to seek to remove the difference between earning entities and employing entities within your organisation should be considered.
Public liability premium and deductible implications for providers
The providers’ public liability policy is increasingly being viewed as a source of funds for workers compensation insurers nationwide, and these recoveries have commenced in Victoria and now New South Wales and are being taken up in other states.
As a result, over the last five years, insurers have seen a significant increase in recovery claims being made by workers compensation insurers of injured contracted staff. Increased deductibles (on average minimum $50,000 up to $250,000) are being imposed for contractors and labour hire claims, with some insurers also increasing premiums substantially where providers have a high reliance on labour hire.
It is expected that the ongoing cost of these claims will continue to rise, as it takes two to five years for the full cost of a serious liability claim to come to fruition. This will mean that insurance premiums will continue to rise for this class of cover, and further contract the market available for cover.
Lyle Steffensen, National Manager, Health & Community Services, Lockton-Zenith (Lockton Companies Australia) global.lockton.comThis article has been prepared by Lockton Companies Australia Pty Ltd and is provided for general information only. It is not intended to be interpreted as advice on which you should rely and may not necessarily be suitable for you. You must obtain professional or specialist advice before taking, or refraining from, any action on the basis of the content in this document.
Continuous improvement cultures
Overcoming challenges and meeting regulatory reforms
Continuous improvement is an essential component of modern business and a statutory requirement for aged care providers. According to MOA Benchmarking compliance expert Dr Leith Heyman, however, “embedding continuous improvement in aged care organisations remains a challenge”.
The ACQSC sector performance report consistently highlights requirement 8.3c of the Aged Care Quality Standards (ACQS), which covers governance systems and continuous improvement, as a common area of non-compliance, reaching first and second position in the most recent quarter for home care and residential providers, respectively.
This is concerning given the strengthened commitment to continuous improvement underpinning upcoming regulatory reforms. In addition to maintaining documented plans for continuous improvement, under the Strengthened ACQS, providers must demonstrate that they have a quality management system that is regularly reviewed and improved, foster a culture of continuous improvement, and involve older people in improvement processes.
Involving older people in continuous improvement processes
While involving older people is essential for fostering a culture of improvement, Dr Heyman acknowledges that providers can face challenges getting older people on board. “Many providers are reporting that older people in residential aged care feel over-surveyed,” she said.

“They are now participating in quarterly NACMQIP surveys in addition to surveys already run by providers, and as part of the new regulatory model will be further encouraged to participate in consumer advisory bodies and improvement initiatives.”
Some older people may feel over-burdened by these expectations which will make it difficult for providers to meet their obligations. Dr Heyman cautions that “it may also be the case that feedback is predominantly provided by a small subset of older people who may not be representative of the diversity of older people’s experiences”.
With this in mind, providers will need to consider how they can ensure that feedback represents the diverse experiences of older people and not just those who are most vocal.
Barriers and enablers
To better understand barriers and enablers to embedding an improvement culture, MOA surveyed providers from across the sector, and our findings suggest that they are keen to address gaps in their approaches to continuous improvement. The top reason cited for the importance of continuous improvement was ‘maintaining or improving regulatory compliance’, however, Dr Heyman acknowledges that “the ongoing pressure to adapt systems and practices due to ongoing reforms likely influences this response”.
Inadequate staffing numbers and skills were also identified as key barriers, reflecting the workforce crises in the sector. Our survey found ‘adequate workforce skills/education’ to be rated as the second highest enabler for continuous improvement, while ‘inadequate numbers of staff’ and ‘inadequate workforce skills/education level’ took second and third positions as barriers.
Effective leadership also emerged as an important theme, with ‘appropriate prioritisation of improvement initiatives’ receiving the third-highest number of nominations as an enabler, while inappropriate prioritisation narrowly missed the top three barriers list, coming in at fourth place.
Steps for providers
Dr Heyman encourages providers to take proactive steps now to prepare for the strengthened continuous improvement requirements. “Cultivating an open, blame-free culture, where staff and older people feel safe to raise concerns and provide feedback, knowing that their input will be valued and acted on, is an essential first step in building a strong improvement culture”.
Implementing a comprehensive quality management system, such as the MOA platform, can also be beneficial. MOA’s self-assessments and quality indicators flow through to a digital collaborative plan for continuous improvement. By streamlining compliance and improvement processes, the MOA approach to compliance and improvement can help to alleviate pressure on overstretched staff, giving them more time to contribute to the organisation’s improvement culture.
MOA Benchmarking
www.moa.com.au
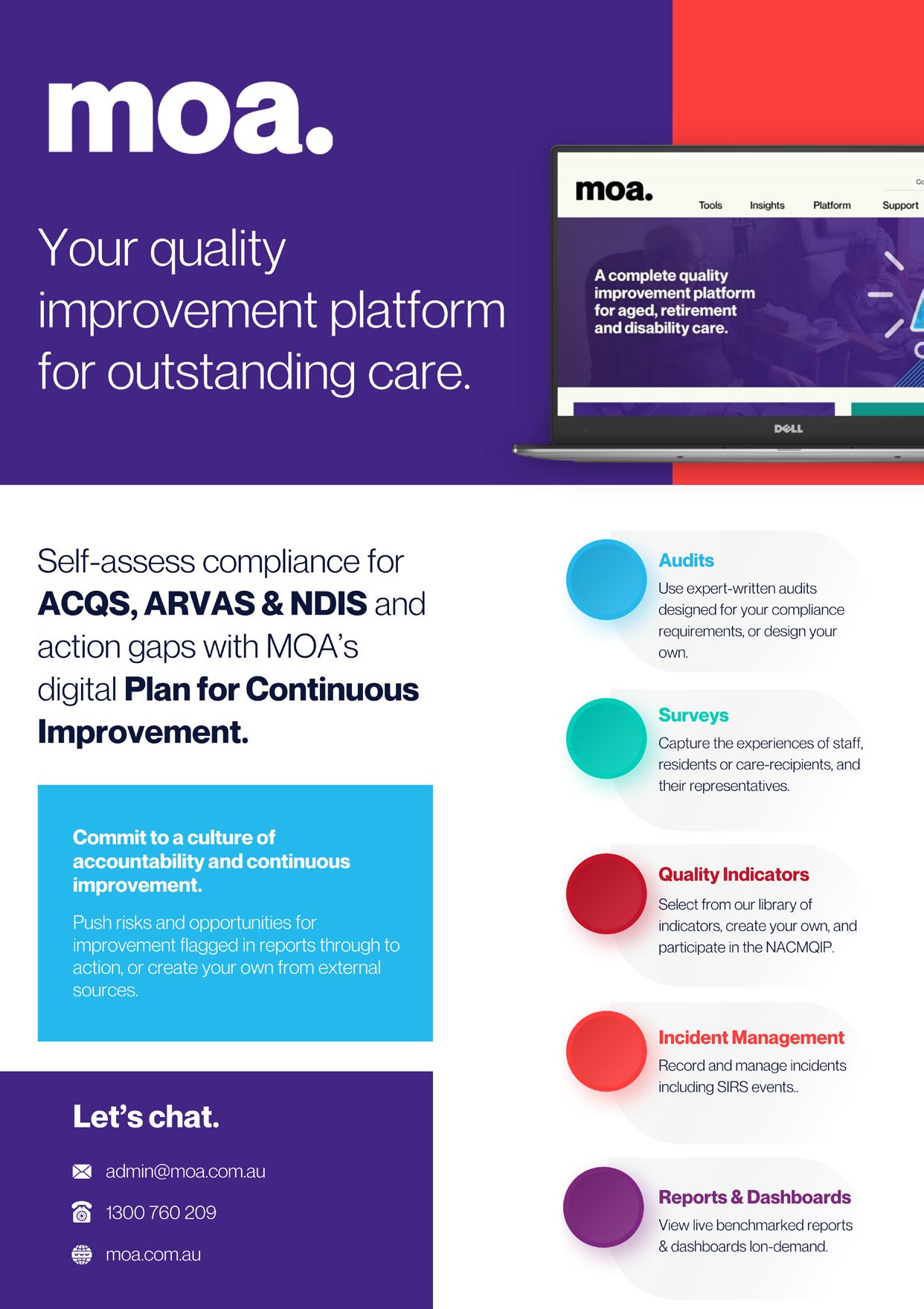
Tough reforms coming to Australia’s privacy act

There’s no ignoring the calculated cyberattacks targeting Optus, Medibank and Latitude Financial over the past year. The ripple effect has caused millions of consumers’ personal information to be compromised. The subsequent public outcry pushed our government to move and introduce privacy framework reforms to catch up with the current global standards.
The Attorney-General’s Department released the Privacy Act Review Report on 16 February 2023, as part of the Australian Government’s review of the Privacy Act 1988 (Cth). Stakeholder feedback was tabled and lodged, which means aged care operators should begin preparing themselves for what will be drastic compliance and regulatory changes on a scale previously not experienced in this country.
Reviewing processes for the protection of personal information
‘Personal information’ is everything that involves the collection, use and disclosure of personal information under ‘fair and reasonable’ circumstances, irrespective of whether consent has been obtained. Business owners will need to:
■ appoint a senior employee who is responsible for privacy
■ keep a record of their handling of personal information (including technical information such as device IDs and IP addresses), the purpose of collection, use and disclosure, secondary uses and disclosures, the sources of information and to whom information is being disclosed
■ include mandatory transparency for specific automated operations, the ability for people to opt out of personal data collection/use, and retention/destruction regulations.
Transparency of handling staff data
Requirements for business owners relating to transparency about informing employees how their information is handled, including its security, destruction and data breach reporting is currently in a consultation process and is still under review. Further detailed information is still to come.
Updating privacy policies, consent forms and collection notices
Privacy policies and collection notices will be required to contain new information. Consents must be voluntary, informed, current, specific and unambiguous. Collection notices must also be clear, up-to-date, concise and easy to understand. Visit www.oaic.gov.au for a list of the current guidelines.
Change to cyber-attacks and data breach reporting structure
Cyber-attacks and data breaches must be reported to the Information Commissioner (IC) within 72 hours. There will now need to be additional information included in breach notices and companies must also be seen to have taken reasonable steps to implement practices that enable them to respond to cyber-attacks.
Statutory tort for serious invasion of privacy
The Report also proposes a statutory tort for serious invasions of privacy, which falls outside the Act. This is not a new
The importance of being proactive
recommendation as it was first proposed by the Australian Law Reform Commission in 2014. The Report acknowledges that existing laws or causes of action, such as breach of confidence or defamation, do not currently provide sufficient redress for a serious invasion of privacy. Further detailed information is still to come.
Role of OAIC enforcement and civil penalties
The Office of the Australian Information Commissioner (OAIC) will be granted additional powers, including undertaking public inquiries and reviews and an expansion of general investigatory powers.
Several tiers of civil penalties will also be introduced. At the top end, maximum penalties will be one of the following:
■ AUD $50 million
■ 3 times the value of any benefit obtained through the misuse of information
■ 30 per cent of a company’s adjusted turnover in the relevant period.
What providers should be doing right now
Aged care providers should be proactively working closely with their IT departments or IT providers to ensure they meet

all the new standards and requirements. To be on the front foot, you need to start:
■ reviewing the Privacy Regulatory Action Policy
■ checking the OAIC’s website for the updated Guide to Privacy Regulatory Action
■ reviewing internal privacy policies and procedures
■ ensuring your organisation has an established cyber-attack and data breach escalation protocol
■ regularly training your staff on privacy and cybersecurity obligations.
A simple way to get an instant ‘snapshot’ of the vulnerability of your organisation’s I.T. Systems, is our T4 Group CyberSCORE assessment (www.t4group.com.au/agedcare). It’s a series of questions you answer online, which instantly provides you with a cyber score. This lets you know how vulnerable you really are.
For a confidential discussion about your company’s IT Cybersecurity and Privacy Framework, T4 Group stands ready to assist you.
Iain Enticott, Managing Director, T4 Group www.t4group.com.au
The value of feedback and complaints
How well do you know your customers?
A key focus of feedback and complaints is continuous improvement. The aim is to seek feedback at every touchpoint with customers, then use that information to continuously improve the customer experience.
Knowing how your customers perceive your company and the services you offer is a fundamental first step to being able to bring about improvements in their overall experience of your brand.
Customer feedback is used to understand how well your business and employees know your customers and to determine if you are successfully addressing their needs and expectations. It also tells you how you’re stacking up against competitors.
Feedback and complaints are also a very important part of the Aged Care Quality Standards, which require providers to have in place a way for your consumers to feel safe, encouraged and supported to give feedback and make complaints. Standard 6 also requires your organisation have an accessible, confidential, prompt and fair system to resolve complaints.
A high-quality feedback and complaints function in an organisation is one where there is understanding and oversight over the two elements to handling feedback and complaints:
■ the system or process for handling feedback
■ the interpersonal skills your people hold to manage the feedback well.
The ‘gift’ of customer feedback
Let’s look at the interpersonal skills your people need to deliver a high-quality outcome. Rather than be considered a problem, customers who provide feedback and complain should be valued and treated with care and respect.
Make sure your team are skilled in being able to manage all feedback including complaints so they can respond to compliments or comments in a timely manner, or calm an angry or upset consumer while working to solve the problem wherever possible.
Customer feedback, whether a compliment or complaint is a ‘gift’ for your organisation and customers should be encouraged and supported to make them. When used well, this information can help your organisation improve your service delivery to better meet the wants and needs of your customers.
Feedback about your performance helps you understand the drivers behind consumer decisions and provides data and insight to design improved experiences and new innovations – while helping you meet your compliance obligations.
Capture ‘passive’ as well as ‘active’ feedback
When considering the feedback system or program, you need to understand how well you are gathering valuable feedback from your customers – and whether you’re gathering feedback using active as well as passive methods.
Many providers employ active feedback methods such as direct questioning via customer surveys, focus groups and customer interviews. But many are not collecting the data from passive feedback methods that occur when the customer initiates an interaction on a variety of channels such as live chat, support calls, social media and online reviews.

Each active or passive interaction with your customer offers you a chance to gain feedback and insight into their habits and behaviours, their satisfaction, and their loyalty to your brand. All you need do is ensure that your feedback program is capturing data systematically with a methodology that best aligns with your business needs, while supporting consumers to make a complaint or give feedback.
Engaging consumers in the feedback process contributes to resolving complaints in a way that is accessible, confidential, prompt and fair – and helps you satisfy your governance obligations.
Christine Davis, Specialist Consultant, Customer Science Group www.customerscience.com.auHR
& the Managers on
& the Managers on
A
A
C C P A _ D I A M
C C P A D I A M
O N D _ S P
O N D
the same W W W . M A R T I A N L
O N
S
O R
S P
O N
C C
C . C
S
planet. O G I
O R
O M
planet. O G I
O M
Innovating at scale Start from the outside in
The Aged Care Royal Commission has called for radical innovation in the aged care sector, with innovation predicted to be a significant driver of growth – and those that learn how to innovate systematically will be more successful than those that don’t.
What does innovation really mean?
Innovation is more than just new technology. It’s the process of taking something that already exists and improving it in a new way. It can be as simple as making a small change to a service or the whole care delivery model such as the ‘Green-house’ model for dementia. Or it can be as complex as completely overhauling an entire system or creating a new market such as platform providers like Mable.
Innovation comes from tapping into people’s creativity and taking a risk to try something new. It can often start with an individual having a good idea, but it’s the willingness of the organisation to pilot or experiment the new idea, get input from others and start to put it into practice that turns it into an innovation.
However, this process does not happen automatically in aged care. It can be challenging for providers in the highly regulated sectors where the idea of ‘experimenting’ is often seen as a risk to compliance. Providers need to look at how they are operating now. Too often we hear about ‘bolted on’ innovation initiatives or ‘ideas’ lists that have not been looked at because the resources are not there to take action.
Harness the power of listening
One of the most powerful ways to start to innovate at scale is to start outside-in: listen to your people to get their ideas.
We all know listening to client voices is crucially important, and many providers are already doing that. However, it can always be done better.
Research shows that 32 per cent of customers will walk away from a brand after a single negative consumer experience. Providers need to pay attention to this even more as the sector moves to a star rating system and funding moves to the client, increasing consumer choice and getting ready to welcome more demanding consumers from the baby-boomer generation.
So how can you improve the way you listen to your consumers? It’s more than addressing complaints or actioning their feedback in a regular customer survey.
Providers need to listen to what is working for their customers and what isn’t, and then get their ideas to improve their experience – starting from the first phone call or email to the ongoing care and lived experience. Plus, the journey often doesn’t end until well after the resident has departed care, it continues with the resident’s loved ones.
It’s just as crucial to listen to your employees. When you listen to your employees, they feel respected. If you engage employees and involve them in co-designing changes, they’ll feel more connected to their purpose and perform better, which ultimately contributes to the overall quality of your consumer experience.
Generating innovation at scale
From our many years of helping care providers setup for success to innovate at scale, we know the following steps work.
1. Continue to improve how you listen to consumers, but find the best way to listen to your employees too.
2. Ensure your leaders role model what they expect. They need to be ready to foster a climate that makes employees feel safe, and are empowered to come up with new ideas and are rewarded for taking risks.
3. Take a look at your organisation’s capabilities to capture new ideas, seize the best ones and capitalise on them:
■ Do you have research partnerships in place to understand the market trends, observe the market and understand what customers want and need?
■ Have you invested in the right governance, processes and capabilities to focus on capturing feedback and prioritising the good ideas, and turning them into opportunities?

■ Do you have the right forums to encourage bringing people together to create solutions that work for your consumers and your people?
4. Finally, it is essential to have a coherent and inspiring strategic vision to encourage a culture of ideas and guide the decision-making that fosters innovation that leads to getting growth and success.
Your next steps
Fire Up Solutions are experts in human-centred change and have strong track record in helping organisations innovate at scale.
Are you set up for success to get ahead of the curve and innovate at scale? If you are, we’d love to hear from you.
Angela Frith, Co-founder, Fire up Solutionswww.fireupsolutions.com
Your helping hand to compliance
ACCPA Safety & Quality Management System (SQMS)
Supports operations through best practice and compliant guidance to all staff
Over 450 aged care specific policies, processes and resource templates that can be tailored to your requirements
Internal audits program with targeted audits focusing on areas of risk
Real time recording and management of incidents, complaints and feedback
Choose a quality system that works for you
Remaining compliant with changing regulations and legislation has become vital for aged care and disability operators, but it’s hard to manage alone.

An easier way is to use an outsourced quality management and compliance system – slashing the time it takes for recording and reporting.
ACCPA has endorsed two reliable, robust and effective quality systems – so your workforce can focus on the caring, not the paperwork.
ACCPA Quality Portal
Management tool for self-assessment against over 100 relevant standards
Over 500 resources and policy templates to assist with compliance
Separate module for governing bodies
Saves 80% of work time on compliance reporting
www.accpa.asn.au/quality-compliance

Choosing the right digital transformation partner
Staffing shortages, limited time and resources and increased compliance requirements –the age care industry is under increasing pressure to do more with less.
Thankfully, modern technology can address a lot of these pain points. There are some great examples of aged care facilities in Australia that have embarked on a digital transformation path are automating manual processes and increasing staff efficiency.
For staff, a lesser focus on administrative tasks ensures they can focus on what they do best – providing better care. For aged care providers, it means doing more without having to hire additional staff. And for residents, it ultimately means better experience.
But working with aged care facilities every day, I am very aware that such digital transformation often includes large-scale changes that many providers simply can’t afford or facilitate all at once. So here are a few things to consider before embarking on such a project.
1. Futureproofing organisation
In a sector impacted by ongoing funding, policy and technology disruption, it is essential for aged care providers to have core systems that are flexible, scalable and future proof.

An investment in digital technology is an opportunity to future proof the organisation to ensure it and adapt to future challenges – be it growth, or policy and legislative changes.
2. Security is non-negotiable
Experts agree recent high-profile cybersecurity attacks are only the tip of
the iceberg. Aged care providers are privileged to be entrusted with incredibly sensitive data about residents and staff, but such privilege comes with a responsibility to invest heavily in security.
Knowing that data security is taken care of by a trusted partner means providers can focus their time and resources on their core business.
At TechnologyOne our global One ERP solution delivers the highest level of security and privacy to ensure our customers are protected by our multitiered security measures and accredited procedures.
3. Consider the pace
With such a large-scale transformation projects, finding a technology solution that can be implemented in stages can be an ideal compromise, moving each facility in the right direction, at their own pace.
A step-by-step solution might be helpful, where aged care providers can take up increasing levels of automation over time, while SaaS will allow work to be done anywhere, at any time and on any device.
For example, our TechnologyOne OneCare solution is a fully integrated ERP solution. This means aged care providers don’t have to undergo their digital transformation in one giant sweep. Instead, they can transition to OneCare in phases and as modules are implemented they will intuitively talk to each other.
4. A tailored solution for aged and community care providers
The aged care industry and its regulatory environment are unique, and facilities need a partner and solution that addresses key challenges across the aged care sector. Having been providing software solutions in Australia
and New Zealand for over 36 years, our OneCare solution has adapted both in technology and functionality to handle the most complex of situations.
Our deep industry expertise means OneCare integrates seamlessly with patients, residents, or client management system, streamlining business processes, and allowing providers to focus on better health outcomes. Our broad enterprise footprint consolidates multiple core systems into one code base and a single source of truth, spanning financial and supply chain management, resident and client billing.
OneCare efficiently automates key tasks, such as auto invoice matching and intelligent transaction processing, resident and client portals, streamlined billing and debt management processes, easy to read statements, out-of-the-box industry reporting, and real-time insights into enterprise-wide information.
The great thing about the transformative power of technology is that it allows facilities to focus more on the people they care for, and elevate the level of care they provide, with many benefits along the way.
Whether it’s finding efficiencies through leveraging new software features or unleashing new data insights and improving security and compliance with privacy requirements, TechnologyOne is proud to be part of the aged and community care sector, and support providers on their digital transformation journeys.
Vanessa Devine, Industry DirectorHealth and Community Services, TechnologyOne www.technologyonecorp.comWhichever technology provider you choose, make sure they’re passionate about helping deliver better care
It’s time to assess your digital health
The aged services industry faces an unprecedented challenge in meeting the growing needs of an ageing population while contending with the aftermath of the COVID-19 pandemic and workforce shortages.
Recognising the seriousness of this challenge, the Australian Government’s 2023 Budget has allocated $101.2 million over five years to support the development and adoption of digital health technologies across various industries.
This significant investment presents a unique opportunity for the aged care sector to leverage data and technology to optimise their operations and deliver the best for aged care clients.
The government’s focus on ‘Data and Digital Capabilities’ in the budget shows that it clearly understands the profound impact these technologies can have on delivering the best for citizens, as well as driving growth and prosperity.
From working from home to online shopping, data-driven technologies have already transformed virtually every aspect of our lives.
But for the aged care sector, there is still much more that can be achieved. By investing in and embracing digital health technologies, aged care services can revolutionise care delivery, making it more efficient and cost-effective for better client outcomes.

The role of integrated data in overcoming blockages
While COVID-19 and staff shortages have undoubtedly contributed to the complexity of the health and aged care crisis, another less-reported cause lies in the disjointed nature of health and care data. The aged care sector is, of course, not alone in facing this challenge.
To address this issue, the government must take the lead in providing integrated solutions that foster better-connected data systems. There are already successful examples of successful B2G integrations, such as the DSS (Department of Social Services) Data Exchange, which has demonstrated the power of two-way information sharing between funding agencies and service providers.
Civica has invested in a real-time approach for providers to ease the burden of reporting manually or bulk file exports. By adopting a similar approach of integrated data, the aged care sector can achieve smarter and more efficient ways of improving service delivery and understanding individual and community outcomes.
Real-time reporting: Every minute counts
In a rapidly evolving healthcare landscape, real-time reporting is no longer a luxury but a necessity. Timely access to
accurate data is crucial for making informed decisions that can significantly impact client outcomes.
Aged care providers should embrace real-time reporting solutions that enable them to monitor and respond to critical information in a proactive and agile manner. By doing so, they can address potential issues before they escalate and ensure a higher quality of care for their clients.
Civica’s Carelink Suite: Pioneering data-driven aged care solutions
As a global provider of GovTech, Civica helps organisations across a range of sectors make smarter use of their own data to deliver more for the people they serve. In the aged care sector, our Carelink Suite is eliminating the reliance on spreadsheets and paper-based forms and empowering care teams to access essential time and attendance schedules, rosters and client information securely from multiple devices. This seamless integration of data and technology streamlines workflows, reduces administrative burden and facilitates more personalised care plans to improve overall efficiency and improving life for clients.
As the aged services industry faces an increasingly complex landscape, the government’s budget commitment to data and digital capabilities is a beacon of hope. By seizing this opportunity, the sector can transform its operations, enhance client outcomes and deliver cost-effective care.
With integrated data systems and real-time reporting, the industry can achieve unprecedented levels of efficiency and quality, making the most of the digital health investment and steering the aged care sector toward a brighter, more sustainable future.
Francis McGahan, Sales Director of Care, Civica APAC www.civica.com.auWhy unlocking data is crucial to delivering smarter care for aged care clients
Alexander aged care’s digital transformation journey
Delivering care more efficiently and improving daily operations
Alexander Aged Care, located in Brookvale, Sydney, is home to 58 residents with many cultural backgrounds and is operated by the Armenian Rest Home Association - a not-for-profit organisation registered as a charity.
In this case study, Mariola Suwart, Director of Nursing at Alexander Aged Care, shares her thoughts about their usage of Centrim Life’s Operations Management Software and their digital journey with Person Centred Software and best-inbreed partners.
How did you embark on your digital journey with Centrim Life?
“We were looking to digitise our maintenance processes as it was all on paper, and it was difficult to keep track of everything, so we desperately needed a system that could help with managing ad-hoc maintenance jobs where staff members could easily create maintenance requests and schedule them monthly or quarterly,” said Mariola.
“At the time, we had a great relationship with Person Centred Software as we had been using its Clinical Care System for many years and heard that they were launching an Operations Management Software powered by Centrim Life that would be able to digitise and streamline our maintenance operations.
“Ultimately, we decided to implement Centrim Life due to the cost and simplicity. The operations management software is so intuitive and easy to navigate, and it isn’t very expensive either. Compared to other systems on the market that are far too complicated, with long, tedious forms and so repetitive, Centrim Life stood out for us due to its simplicity.”
What benefits have
you noticed since implementation?
“We have saved so much time requesting and resolving maintenance jobs at our sites. We have a daily process where we have QR codes at our nursing station, and staff members can easily scan the QR code to view any maintenance requests that need resolving; this has helped us keep track of everything and works very well for us,” said Mariola.
“The feedback and quality management feature has been incredibly useful and is compliant with the aged care quality standards. We have been able to easily create and send surveys to staff, residents, and families to collect their feedback and generate reports. We are also able to record any hazards or accidents that happened on-site and have an overview of that data for our reporting as well.
“There is also a Plan for Continuous Improvement (PCI) section within the system, enabling us to create and manage new PCIs accordingly. Plus, it helped us with reporting during our accreditation.
“Centrim Life has allowed us to see all the important information in one place, making evaluating and actioning tasks much easier. It has enabled us to focus on providing the best care to our residents instead of being bogged down with administrative tasks.”
Since going digital, how has
the experience been?
“Staff members love the Clinical Care System as it is great to be able to evidence care at the point of delivery and have all that information at your fingertips,” said Mariola.
“Another key point is that the Care Delivery App is icon-driven, making it much easier for our non-English speaking staff to enter in progress notes. All they have to do is select the icons, and the system automatically generates the progress notes for them, which has been incredibly valuable.
“Staff don’t have to sit in front of the computer typing in progress notes at the end of their shift; they have the freedom to be with the residents they care for.
“Because of our digital journey with Person Centred Software, we decided to implement other digital solutions like an electronic medication management software from Webstercare and a pain assessment tool from PainChek.

“It was important for us to choose systems that integrated with each other so that our resident information flowed seamlessly through each system, reducing the need for multiple data entries; this has allowed us to create a truly connected care environment in our organisation.”
Person Centred Softwarewww.personcentredsoftware.com

Enhancing cybersecurity posture in the age of AI
A comprehensive approach
In today’s digital landscape, cyber threats continue to evolve at an alarming rate and providers face an unprecedented challenge in safeguarding their sensitive data. The emergence of AI has empowered threat actors with enhanced attack sophistication, necessitating a comprehensive cybersecurity framework.
But there are measures providers can take to bolster their cyber defences while also highlighting the role of AI in combating these threats.
Before diving into advanced cybersecurity measures, it is crucial to get the basics right. Neglecting fundamental security practices can leave vulnerabilities that threat actors can exploit with ease.
Build a strong foundation
Care service providers must start with a solid foundation. This entails implementing essential elements:
■ Infrastructure monitoring and patch management. Ensure that software and hardware remain up to date with the latest security patches, reducing the risk of exploitation.
■ Policies, procedures and access. Robust security policies and procedures are vital for promoting a security-conscious culture. This includes defining strong password requirements, access controls and data handling guidelines.
■ Multi-Factor Authentication (MFA). Add an extra layer of protection to significantly mitigate the risk of unauthorised access, even if passwords are compromised.
■ Cyber phishing training. One of the most common attack vectors is social engineering, accounting for
81 per cent of successful attacks. Regular training programs that educate employees can significantly reduce this risk.
■ Data backup and disaster recovery. Regular backups and robust disaster recovery plans are essential to protect against data loss and minimise downtime in the event of a cyber incident or other disasters.
■ Incident response and recovery plan. Document steps in the event of a security incident including roles and responsibilities, communication protocols, containment measures, and recovery and system restoration procedures.
Understand the threat
As the landscape of cyber threats continues to evolve, threat actors have increasingly turned to AI-powered techniques to amplify the sophistication of their attacks. AI language models have provided threat actors with powerful tools for automating tasks such as crafting convincing phishing emails or generating targeted spearphishing campaigns.
While machine learning algorithms identify vulnerabilities devising more targeted attacks. This rapidly advancing
threat landscape necessitates that organisations consider adopting AI-driven capabilities of their own.
By leveraging AI technologies within their cybersecurity framework, organisations can actively combat threat actors on a level playing field.
AI vs AI
While AI has contributed to the sophistication of cyber threats, it can also be harnessed as a powerful tool to combat them. Providers should consider implementing AI-based solutions to bolster their cybersecurity framework, including:
■ Security Operations Centres (SOC). A SOC enables proactive monitoring and threat detection. AI algorithms analyse vast amounts of data and identify anomalous patterns, allowing 24x7 security teams to respond swiftly to potential threats.
■ Automated incident response. AI-driven automation can streamline high risk incident responsiveness by automatically identifying, containing, and providing remediation recommendations. Minimising response times and mitigating the impact of cyberattacks more effectively.
■ AI-powered threat intelligence. AI can collect and analyse threat intelligence data from various sources, staying ahead of emerging threats. This intelligence can be used to strengthen security controls and enhance incident response strategies.
Develop a scalable cybersecurity framework
A well-rounded cybersecurity framework should support the unique needs of the business. Cybersecurity is an ongoing process, requiring constant monitoring, evaluation and improvement. Providers should regularly assess the effectiveness of their security controls, updating them to adapt to emerging threats.
IT Integrity recommends that any AI offerings should be backed with human rationalisation and be built on a strong cybersecurity foundation.

In an era where AI language models have given rise to more sophisticated cyber threats, providers must protect their sensitive data. By implementing a robust cybersecurity framework, providers can establish a strong foundation advancing to leverage AI-powered technologies to proactively identify and mitigate threats.
At IT Integrity, we have extensive experience in the cybersecurity frameworks and can assist care service providers in building a resilient security posture that aligns with their specific needs, enabling them to navigate the digital landscape confidently and securely.
Steve Iannuzzelli, Head of Sales & Marketing, IT Integrity www.itintegrity.com.auSome time ago, the CEO of a large private aged care operator told us they could not find the right system. “Care systems are a main issue we struggle to nail. We are not just a residential aged care provider, not just a home care operator, nor just a retirement village. There is no right system available to us,” he said.
The CEO was describing a common challenge for operators offering a continuum of care – the bundled care options that follow an individual through time, adapting to their changing needs.
Ryman also couldn’t find what they wanted, so they built it. Ryman is reported as having made a multi-million-dollar investment in creating their own care system. While Ryman is not a partner of eevi, we commend them for their bravery in making that investment. Today Ryman is recognised as an industry leader, having used technology to transform their operations into an efficient and effective execution of the concept of continuum of care.
Can others create systems for continuum of care?
In our view it is possible for any aged care provider to create a system to support continuity of care across their services, tailored to their specific culture and needs, although you don’t need to start from scratch. Partnering with a company like eevi, leveraging our eevi Care technology system and expertise, is a good way to customise a fit-for-purpose solution, while keeping costs down.
There are some serious considerations. It takes real bravery and a long-term commitment, from the highest level to the care staff on the floor. For example, how ready are your care staff to adopt new ways of doing things? If you have high turnover, how committed is your organisation to re-train new entrants to your workforce? How committed are your senior managers to use the data and insights, without fear, to drive performance and change?
Some have said that, in aged care, if you are introducing change, you are the enemy, but we don’t believe that to be the case. We have seen the opposite, with a readiness to adopt proven user-led solutions. They just have to work, and users have to see the benefits – to save carers’ time, or improve residents’ outcomes, or save operators money, or save families the worry.
Where do you start?
It’s important to start by undertaking resident and staff userled research into your pain points and problems. We use an approach called design sprint methodology, borrowed from IDEO, Stanford and Google play books.
The framework offers a compact and robust approach to explore opportunities and to develop and test ideas with actual users. Typically, it operates over four phases, with clients, providers and stakeholders involved throughout the entire process, for co-design and validation.

At its heart, it demands empathetic listening: actively listening without bias, and observing how your residents, carers, care managers and so on interact with their environment and behave. Only then can you analyse recurring themes and insights and start to solve pain points and problems.
There is a warning. The process takes real commitment. The process to develop our eevi Care technology system took over 1,000 interview and script responses, from 37 face-toface interviews across two organisations and four operating sites. A change of management can be enough to abandon the process and revert to traditional ways of care and the systems that support.
In our view, however, the cost of inaction is increasingly high. Faced with consumer and regulator demands for increasing standards of care, declining profitability and workforce shortages that are dire, the sector has little choice but to find new ways of doing things, and technology can and will be a driver of that change.
So, what is the right system today for operators of a continuum of care? Frankly, in our view, it’s a work in progress. We and others continue this work and welcome discussion on opportunities to collaborate widely with others.
David Waldie, Founder & Managing Director, eevi www.eevi.lifeWhat is the ‘right system’ to support a continuum of care?
If you can’t find one, find a proven partner, and collaborate with them.The eevi Design Sprint Methodology Process.
Harnessing clinical data for improved resident outcomes
Analytical dashboards save time and resources
Clinical data is a vital asset for aged care organisations. Although providers collect an abundance of information, assessing all of the data can be labour-intensive and time-consuming.
Providing access to key data points quickly, analytical dashboards eliminate the need for manual data gathering and analysis, saving time and resources.
Harnessing cloud technology with analytical dashboards enables data to be integrated and visually transformed in realtime into actionable information to support evidence-based care. By using live data to inform decision-making, clinical teams can improve the quality of care provided to residents and contribute to the long-term sustainable success of their aged care organisation.
Visualising data via dashboards can benefit and assist clinical managers in identifying patterns and highlighting important issues in multiple ways.
Falls, for example, remain a leading cause of hospitalised injuries and injury deaths among older Australians, making up 77 per cent of all injury hospitalisations and 71 per cent of injury deaths in people aged 65 and over. Residential aged care quality indicator data from 2021-22 shows that almost a third of aged care residents experienced a fall each quarter, with over 2 per cent of falls causing a major injury.
While the approach to falls prevention is multifactorial, dashboards can provide a visual evaluation of the effectiveness of current prevention strategies. By collating and analysing valuable data such as current medications, mobility status, time and location, providers can form the foundation of a trend analysis. By analysing variables, clinical managers can gain a more comprehensive understanding of fall incidents and adjust strategies as required.
Analytical dashboards can also be set up to track Quality Indicators, such as pressure injuries, use of physical restraint, unplanned weight loss and medication management. Managers are able to view how a single facility is tracking or gain a view across multiple sites. By analysing these indicators, clinical managers can identify potential areas for improvement and take steps to enhance the quality of care provided.
Dashboards can also be configured to capture how an organisation is faring in regards to the Quality Standards. For example, feedback and complaints (Standard 6) across multiple
sites can be collated and reviewed via a dashboard, allowing managers to pinpoint areas for possible improvement.
From 1 October 2023, the average of 200 minutes of care will become mandatory for residential aged care homes –and having a clear oversight of staffing ratios and case mix adjusted care minutes targets will be vital for providers.
The star rating system for all residential aged care facilities went live in December 2022. Current awarded star ratings were taken from a time when the sector was not required to meet the 200 minutes of care. In order to retain or boost their rating, providers will need to have ample reporting and tracking mechanisms in place.

Using a software platform such as eCase, which has been developed by Health Metrics, will allow managers to plan and manage staff levels according to care needs and to predict labour hours required by resident ratios. Managers can then use the eCase dashboards to monitor staffing levels, nurseto-resident ratios and total staffing hours. Facility profiles enable the re-engineering of rosters and the redefining of staff resident ratios, while estimating AN-ACC funding and required care minutes. The eCase dashboard data can easily be exported in a variety of formats for reporting purposes.
Dashboards can enable managers to visualise the performance of single or multiple facilities as measured by the four dimensions that make up the star ratings – resident experience (33 per cent overall rating), compliance (30 per cent), staffing (22 per cent), and quality measures (15 per cent).
By connecting dashboards to these metrics or other key performance indicators (KPIs), managers can gain vital business intelligence along with the ability to dive deep into specific pieces of information to continually monitor success.
Analytical dashboards enhance communication, enabling clinical managers to share key data points and insights with their teams, facilitating greater collaboration and understanding. This can help identify areas for improvement and ensure that all staff are aligned and working towards common goals.
Utilising analytical tools can provide invaluable efficiencies, allowing teams more time to action insights they discover. Used correctly, data can be an empowering way to understand your organisation’s best next steps whilst making informed decisions based on real-time data.
Nina Combe, Chief Product Officer, Health Metrics www.healthmetrics.com.auTechnology: friend or foe for advance care planning?
The digital transformation of aged care
As adoption of technology increases, so too do expectations for it to support and enable the complex human interactions that are so much a part of quality aged care.

Concurrently, advance care planning has become, along with palliative care, a core business of aged care. Recent revisions to the Aged Care Quality Standards and Quality Indicators now require aged care providers delivering clinical care to demonstrate performance in advance care planning.
This has thrown up particular challenges, including:
■ inaccessible advance care plans that provide no meaningful instructions for clinicians and aged care providers
■ conflict occurring among staff and families
■ individuals receiving end-of-life treatment that does not align with their personal values, objectives, or informed decisions.
Providers can look to technology to help overcome these issues, because it can help support the complex human interactions in advance care planning in many ways.
Firstly, it can provide scaffolding to aid decision-making. It can then capture and communicate those choices to the people that matter both legally and emotionally, ahead of time.
This is important because an advance care plan is only used when a person cannot speak for themselves. This may occur slowly over time such as in the cases of dementia or malignancy, or quickly in an accident, a fall, or a cardiac or pulmonary event.
Therefore, advance care plans need to be discussed ahead of time with the families and carers involved in the care planning, and who will be advocating on behalf of the individual who has lost capacity.
Within aged care, staff need access to the advance care plans in emergency situations. Some IT providers include an advance care planning feature in their products, but this may not guarantee real-time access to the many stakeholders who need to access the plan.
Rather than siloed PDFs, of which there could be multiple and outdated copies, advance care plans need to be seamlessly shared beyond just the facility and My Health Record. Families and all emergency responders need 24/7 access including remotely, to the same validated plan.
Technology can support these emergency interactions by providing an interoperable plan in formats that suit emergency use, including via secure QR codes.
Technology can also help support the documented low levels of knowledge and confidence among aged care staff by providing a step-by-step guided process that is easy to use and understand for both staff and clients.
Importantly, individuals deserve a choice about the plan they use – whether that be a common law or statutory directive, voice recordings or other media. Technology helps overcome language, cultural and physical barriers inherent in reading and writing extended documents.
Touchstone Life Care is an Australian-developed software solution that guides staff and clients through a simplified but individualised advance care planning process. The system can be integrated with IT systems, offered as part of a home care package or additional service. It automatically updates and shares edits, includes additional documents, and generates plans that are accessible in real time 24/7, including via a QR code. It also automatically reports measures for the Aged Care Quality Standards and Quality Indicators.
Remember that the technology solution you use for advance care planning needs to be fit-for-purpose for the individual, their provider, their trusted contacts (both formally and informally appointed) and health professionals, all of whom interact in different ways and require access to a plan in a variety of settings with differing time constraints.
Having a tick box solution within a single system risks perpetuating the current problems in advance care planning, but a carefully designed interoperable approach can help support the delivery of person-centred aged and palliative care.
Dr Merran Cooper, Founder and CEO of Touchstone Life Care www.touchstonelifecare.comCalculating your savings
Cater Care’s new aged care catering cost health check
Budgeting catering solutions for residential aged care homes can be an exercise in frustration and unpleasant surprises.
Between staffing, suppliers, and every other potential problem that comes leaping out of the woodwork, there’s a plethora of things that can lead to the final expense figure of your planned catering solution being much higher than expected –with no benefits in relation to quality.
But it doesn’t have to be this way, and technology can lend a helping hand.
The Cater Care team have worked hard to put together a new financial assistance tool – the Catering Cost Health Check – aimed at giving residential aged care providers all the information they need to be forewarned of the general expected costs of establishing a catering solution.
Cater Care’s innovative new software tool means that aged care providers can have a better understanding of potential hidden costs of establishing their catering solution prior to making any commitments, rather than having to rely on hours of guesswork.

The Catering Cost Health Check can shed some light onto the cost and operational implications of hidden factors that may not have been immediately apparent, including:
1. Operational financial implications – an in-depth analysis of both the direct and indirect expenses that may be associated with establishing and maintaining an in-house catering service, such as the costs of acquiring and retaining staff, equipment fitouts, and any other outside contract work that may be required.
2. Menu planning – assessing the cost effectiveness of an in-house menu development strategy, as well as reviewing the potential costs of external dietitian menu reviews and treatment of individual residents.
3. Procurement costs – analysing the efficiencies and inefficiencies of the procurement process, the position of aged care providers giving their relative lack of buying power, and savings that may be made through external procurement providers.
The Catering Cost Health Check’s development and release has come at a critical time for the industry, with many providers across the nation struggling to make ends meet, evidenced by Stuart Brown’s Aged Care Financial Performance Survey (December 2022) that showed 64 per cent of the 1,143 providers surveyed are operating at a loss. With constantly shifting regulations, requirements, and the now skyrocketing cost of doing business, now more than ever it’s crucial for care providers to have a clear understanding of the financial implications of any proposed catering system.
It’s our hope that this tool can make a tangible positive contribution to care providers when planning out their finances to deliver the best possible catering outcomes for their residents.
Cater Care’s software tool allows prospective providers, whether they’re looking to establish an in-house solution, evaluating the cost-effectiveness of outsourcing, or just considering their options, to be forewarned of potential financial snags that could reduce the operational effectiveness of their catering.
If you’re interested in learning more about our Catering Cost Health Check – or trialling it yourself – please can head to Cater Care’s website or get in touch with our aged care expert.
Jonathan Storer, Client Development Manager, Cater Carewww.catercare.com.au/our-markets/retirement-aged-care
Be future-ready with the upcoming aged care reforms
Software systems must adapt and drive change


As the aged services industry in Australia prepares for significant regulatory changes over the next 36 months, providers must adapt swiftly to ensure compliance and the delivery of high-quality care.
In order to succeed, providers will need to focus on a futureready solution that redefines care outcomes, complemented by compliance and revenue improvements, to meet the challenges of the upcoming reforms.
Embracing mandatory care time requirements
New regulations state that providers must ensure a minimum of 200 daily care minutes per recipient, including 40 minutes from registered nurses. Ensuring your technology empowers efficient care time management, real-time performance monitoring and intelligent scheduling, will be a huge help.
With an updated AN-ACC Dashboard, you can also track the ‘target care minutes’ to provide real-time visibility into care minutes allocation, allowing you to effortlessly monitor and ensure that each care recipient receives the appropriate level of care, enhancing their wellbeing and satisfaction.
Adapting to revised Aged Care Quality Standards

The revised Aged Care Quality Standards aim to elevate the quality of care provided to older Australians. Your focus should align seamlessly with these standards, offering comprehensive tools for documentation, care planning, and incident management.
A platform enabling care teams to capture and track data is essential to ensure compliance with the new standards while enhancing transparency, accountability and consumercentric care.
Streamlining governance requirements
To meet the new governance requirements, aged care providers need robust systems in place to manage their operations effectively.
Your care management platform should offer governance tools, including reporting dashboards, analytics, and compliance tracking features.

By leveraging the software’s capabilities, providers can streamline governance processes, monitor performance indicators, and proactively address any gaps to ensure compliance and optimise organisational performance.
Leveraging Star Ratings and Quality Indicators
The introduction of Star Ratings for residential aged care and the expansion of the National Aged Care Quality Indicators Program highlights the government’s commitment to transparency and accountability.
An intelligent care management platform is designed to facilitate the collection and analysis of data necessary for these initiatives, allowing providers to measure their performance against national benchmarks and identify areas for improvement.
Using actionable insights, providers can enhance service delivery, drive continuous quality improvement, and increase the chance of higher ratings.
Integrating with Government Provider Management System
We are working on integrating with the Government Provider Management System (GPMS) to ensure seamless information exchange and compliance with reporting requirements, because this will be of ultimate importance to our clients.
Our platform’s interoperability enables smooth data transmission, reducing administrative burden and ensuring accurate and timely reporting to regulatory bodies.
An intelligent care delivery platform like no other Humanetix is the only Australian care platform that is globally unique and has been independently proven to save time, improve government reporting efficiencies and, most importantly, deliver better care outcomes for aged care recipients.
In a study conducted by the University of Canberra, published by Wiley Journal of Clinical Nursing, Humanetix represents a significant leap forward in the realm of electronic health records, surpassing previous iterations in terms of quality and completeness of documentation.
Unlike earlier electronic-based records that exhibited improved process and structure but lacked the accuracy and
completeness of their paper-based counterparts, Humanetix bridges this gap. According to the study:
“Previous research found that while electronic health records reported better process and documentation structure due to ease of use and omission of illegible handwriting, paper-based records provided more complete and accurate documentation. By contrast, Humanetix has shown to improve both the quality of documentation and the completeness of the records.”
Be future-ready with technology
Humanetix, an intelligent care delivery platform, is designed to help aged and health care providers navigate these changes seamlessly and simplify care. We are happy to guarantee that our platform will be up-to-date with all the required regulatory changes that impact aged care organisations.
Unlike legacy products that can’t customise to local market demands, having technology that has workflow capability or scalability is crucial. Humanetix is designed from the ground up to be the most flexible platform on the market, and with our unique patented technology, we can respond to new regulatory requirements as soon as the government announces them.
Arthur Shih www.humanetix.com.auThe key pinciples of small house design
Research leads to better design at two new sites in South Australia
The ‘small house’ model is gaining traction in Australia’s aged care sector, particularly following the recommendations of the Aged Care Royal Commisssion, and with new village models reaching completion.
The name defines a concept of smaller living groups in a ‘small house’ which is an established priority in dementia design, however further layers influence the delivery and success of the small house model beyond simply the house size.
Brown Falconer design extensively in residential aged care and regularly discuss proprietary care models with our clients. We were particularly keen to distil the key building design moves which lead to better care, health and lifestyle outcomes which are common across models.
Core design elements
In late 2019, Brown Falconer commissioned Dr Fiona Kerr of the Neurotech Institute at the South Australian Health and Medical Research Institute to conduct a scientific literature review of empirical evidence for positive outcomes of established dementia design models.
Brown Falconer were designing Clayton Church Home’s Summerhill home at Uraidla (currently under construction), and Healthia for ACH at Elizabeth (newly completed), and we wanted to maximise support for people with dementia at these South Australian projects.

The research identified a series of commonalities, which we were able to apply in our architectural design and small house approaches in different ways at the sites:
■ small in scale with rooms grouped around a single communal area
■ individual rooms and amenities with enough space for personal belongings
■ intuitive and legible layouts
■ home-like appeal
■ opportunities for engagement and socialising
■ stimulation management
■ ensuring that the model of care matches the design.
In the design approaches for our selected projects Brown Falconer was clear to adopt these core principles, however it was some of the more detailed research observations which led to small but very important design decisions.
Desirable design elements
Other design principles applied to small house dementia design include:
■ furniture not joinery
■ kitchens not serveries
■ resident laundries with standard washers and dryers
■ objects not feature walls or doors
■ free access to outdoors.
Colour versus objects
Colour is often used as a technique for way finding and orientation, but research has identified it has far less impact for residents than using objects as identifiers instead. Objects can be markers for past memories but can simply be items of everyday life. Items can also be part of the technique to make the building home-like and provide the ability to engage.
A simple broom rack directly relates to four of the seven core principles found to be common across all successful dementia-focused design models.
A resident broom cupboard is very seldom provided in an aged care home and yet it provides a recognisable and normalising activity with which some residents may like to engage.



Home-like by nature, it provides an object which is a marker for the resident who knows the broom cupboard is just down the hall from their room. For it to be there, open and accessible, it relies upon a model of care which matches the design intent.

Resident engagement
There are two keys to the success of the design: the care model itself, and resident and family engagement.
Brown Falconer utilise three techniques to ensure alignment: risk management, building user guides and cultural mapping.
Allowing residents to engage requires staff to understand how the design facilitates these outcomes, and for the model of care to allow the activity to occur given an inevitable aspect of risk.
For residents to want to engage they and their families must feel connected, with a sense of ‘belonging to place’. Cultural mapping for a new development uncovers social and historical context which can be used to inform design approaches, art inclusion and future site activities. At Healthia, we used art to define and prompt use of spaces, while at Summerhill a history of Indigenous bread making from Kangaroo grass seeds will be referenced through plantings and resident bread making activities.
In both locations the ability for residents to participate has been discussed and documented and the way in which the design can facilitate life along with mitigating risk has been considered and built into the care model.
The core principles of successful small house and dementiafocused design are common. They are not difficult to build
into the architectural solution, but the skill lies in delivering outcomes simply and authentically, facilitating a process that aligns the model of care with the built opportunities and connection to place.
Mario Dreosti, Managing Director, Brown Falconerwww.brownfalconer.com.au
The first dementia care village for South Australia
Backed by three decades of small household living at HammondCare
Along a busy tree-lined arterial road, the suburban homes of Adelaide’s south are joined by two new additions. Just like the neighbours, their singlestorey brick walls are punctuated by Adelaide bluestone and capped with gabled roofs. But these new homes weren’t bought off the plan – they are the first of their kind in South Australia.
Newly completed, Daw Park Dementia Care Village is the latest iteration of HammondCare’s proven small household living model. Four years in the making, every aspect has been informed by dementia design principles anchored in nearly three decades of dementia-specific care.
At Daw Park, six cottages will be home to 70 residents, with each cottage having a distinct identity: different letterboxes, door panelling, brick and roof colours.
Two cottages face the street, while four surround a central park free from fencing, and dappled with the shade of a towering spotted gum. A hair salon, corner store, and café are dotted around the site, each specifically designed to support varied residents’ needs, and a sense of community.
Adelaide’s first dementia village is informed by HammondCare’s model of care, backed by recent Aged Care Royal Commission recommendations that outline the benefits of smaller, lower density living arrangements for quality aged care, especially for those living with dementia.

While many care homes separate a large building into smaller ‘homes’ internally, Daw Park’s individual cottages promote the small household model in all aspects of the built form.
Three cottages are dementia-specific (acute care to nonambulant) while two cottages will serve to strengthen the state’s specialist dementia care program. These two nine-bed cottages are linked to another 11-place step-down cottage, which provides a gradual transition between services as resident needs change.
To ensure the homes are domestic and familiar to residents, the design invokes elements of the bungalow style, a prominent feature within Adelaide’s garden suburbs such as the adjacent Colonel Light Gardens. Colonel William Light was instrumental in the design of Adelaide and was influenced by the garden city movement and Ebenezer Howard in the late 19th century.
Accordingly, the planning of the Daw Park village was influenced by the principles of the garden suburb philosophy, while recognisable material elements like Adelaide bluestone chimneys add to the sense of familiarity.
At Daw Park, every resident has their own room; to make theirs how they and their loved ones choose. Bedrooms have plate shelves, a memory box, and space for cherished possessions –all to facilitate personalisation and a sense of belonging.
Generous living areas pop with tastefully coloured artwork and furnishings. A variety of tables, chairs and lounges
provide choice and comfort to residents, and contrast their surroundings to support residents with diminished eyesight. Large windows provide views to the garden setting while sheer and block out curtains control natural light and glare. Each cottage provides direct access to safe outdoor spaces, where the planning is intuitive and residents are able to see and sense to get outside with ease. Technology supports resident safety and independence, by alerting staff discreetly when doors are opened and closed. Clinical operations are hidden from the domestic setting, with concealed doors providing discreet access to clinical storage and utilities.
All meals are cooked in the cottage; there is no commercial kitchen. Domestic-style kitchens are positioned in the heart of each home where meals are prepared fresh, often with resident involvement. Residents walk with carers to the on-site general store to collect groceries for the meal ahead.
Around the corner, residents can assist the maintenance manager in the workshop; or mingle with families, staff, and neighbours at the children’s playground and café.
Bickerton Masters is proud of what has been accomplished in partnership with HammondCare. Architecture, interior design and design-phase project management were all completed in-house, with the majority of the design and construction


teams being local to Adelaide – all of whom participated in dementia design schools prior to their involvement.
Now that the rigour of project delivery is complete, the doors are open for those living with dementia to live well in their new homes.
Jonathan Chew, Aged Care & Seniors Living Sector Lead, Bickerton Masters www.bickertonmasters.com.au
Cosy living spaces are designed to support people living with dementia.


Enhancing aged care through innovative furniture solutions

Flexible
and technologically advanced furniture solutions set to revolutionise aged care services
Innovation and technology have become driving forces in various industries, including aged care. With the Australia’s ageing population, there is an increasing demand for high-quality aged care services, creating an opportunity for innovative solutions that can enhance service delivery.
One company leading the way in developing innovative solutions to enhance the interior design of aged care homes, is Workspace Commercial Furniture. Embracing advancements in furniture design, their products help to support the concept of home-style aged care settings, which has been recognised as crucial in providing individuals with a sense of tranquillity and comfort, transitioning from clinical environments to warm and welcoming spaces.
A significant innovation is the introduction of fully customisable furniture, allowing for personalised adjustments to meet individual needs. Recognising that furniture is not merely functional but also an essential component of the care environment, Workspace has invested in research and
development to create furniture that caters to the specific requirements of older adults.
From chair height modifications to facilitate easier sitting motion to fabric options prioritising easy cleaning and extended lifespan, these customisable features enhance both functionality and comfort.
Moreover, the integration of healthcare-treated fabrics ensures cleanliness and hygiene. The inclusion of removable seats with easy clip connectors and fixed or removable cushion options adds to the versatility and adaptability of the furniture.
High-quality foams and webbing ensure durability, while features such as in-built lighting, charging ports and communication devices enhance safety, independence and overall value for the users.
Another notable advancement in furniture design is the development of bariatric chairs. These chairs are designed to offer comfort and support to the user while providing practicality, strength and functionality for caregivers. Featuring
a robust frame with sleek lines, bariatric chairs are suitable for high-level use, incorporating necessary reinforcement to withstand the demands of healthcare environments.
These chairs prioritise the wellbeing of individuals while considering the needs of caregivers, promoting ease of use and efficient care provision. By combining durability, value and aesthetic appeal, bariatric chairs contribute to creating inclusive and supportive spaces in healthcare settings.
Workspace Commercial Furniture collaborates with aged care designers, builders, and facility owners to challenge
the stereotype of aged care and deliver tailored as well as standard product ranges. By embracing innovative functional needs and excelling in aesthetics, they help create inspiring projects that enhance the quality of life as well as quality of care.




Leveraging technology to create functional and adaptable furniture systems, the company assists aged care providers in designing better aged care environments. Additionally, utilising digital technology for furniture asset management enables providers to optimise resources and reduce costs, leading to enhanced care outcomes.
Addressing the challenges posed by the ageing population requires innovative solutions, where technology plays a crucial role. As the aged services industry continues to evolve, we can expect more innovative solutions like those developed by Workspace Commercial Furniture to further elevate the quality of care provided.

Workspace Commercial Furniture www.workspace.com.au
This year, smith+tracey architects celebrate 75 years of practice. During this period we have developed a major presence and awareness within the seniors living, aged care, community and education sectors. We welcome the opportunity to continue our contribution in achieving better designed outcomes for senior living environments.
www.smithtracey.com.au

Powering the future of aged care
Unleashing the potential of sustainable energy technology
In the complex ecosystem of aged care, a profound transformation is underway – one that promises to reshape the landscape of energy consumption and sustainability.
The aged care sector is experiencing a rising demand for sustainable energy solutions, driven by the challenges posed by a volatile and expensive grid electricity market.
Fluctuating energy prices place a significant financial burden on providers, making it imperative to explore alternatives. There is also growing recognition of the need to reduce reliance on fossil-fuelled grid electricity to mitigate environmental impact.
Sustainable energy technology, with its remarkable potential to reduce operational expenses and enhance environmental stewardship, takes centre stage in this narrative.
Diverse sustainable energy technologies
In the pursuit of sustainable energy solutions, a plethora of innovative technologies has emerged to meet the specific needs of aged care facilities.

These include customised solar power systems, battery storage and backup solutions, electric vehicle (EV) charging infrastructure, automated energy management systems, and virtual power plants (VPP).
These technologies, when combined, create a powerful arsenal that can revolutionise the energy landscape of aged care.
Tailoring solutions to aged care homes
The beauty of sustainable energy technologies lies in their adaptability to unique requirements:
■ Customised solar power systems can be designed to harness the optimal amount of sunlight, generating clean energy and reducing reliance on the grid.
■ Battery storage and backup solutions provide a reliable source of power during outages and peak demand periods, ensuring uninterrupted care services.
■ EV charging infrastructure supports the shift towards electric mobility, accommodating the increasing use of electric vehicles.
■ Automated energy management systems optimise energy consumption patterns, enabling precise control and efficient utilisation of resources.
Virtual Power Plants (VPP) enable aged care homes to actively participate in energy markets, contributing to grid stability and potentially generating additional revenue.
Modular solutions for growing energy demand
As the energy demand in aged care facilities continues to escalate, modular solutions offer a flexible approach to meet these evolving needs.
Modular systems can be easily integrated and expanded, accommodating the growing energy demand without disrupting operations. They also enable seamless retrofitting of existing facilities, facilitating a smooth transition towards sustainable energy practices.
By embracing modular solutions, aged care providers can optimise resource allocation, improve energy efficiency and ensure long-term cost-effectiveness.
To retrofit or integrate from scratch?
When considering the implementation of sustainable energy solutions in aged care, providers face a crucial decision:
whether to retrofit existing infrastructure or integrate sustainable energy systems from scratch during new builds or extensions. Each option comes with its own advantages and considerations.
Retrofitting with sustainable energy technologies allows for gradual upgrades, minimising disruption to operations and upfront costs. This approach enables providers to optimise energy efficiency and reduce carbon emissions by integrating solar power systems, battery storage, and other sustainable energy solutions into the current infrastructure.
On the other hand, integrating sustainable energy solutions from scratch during new builds or extensions provides the opportunity to design facilities with sustainability at the core. By incorporating energy-efficient designs, renewable energy systems and advanced energy management systems, providers can achieve higher levels of energy efficiency and operational resilience.
Addressing accessibility and cost barriers

While upfront costs may pose a challenge, it’s important to recognise the long-term benefits and potential cost savings that can be achieved through sustainable energy solutions. By reducing reliance on expensive grid electricity and implementing technologies such as solar power systems and battery storage, there can be significant energy cost savings
over time. Moreover, advancements in technology and market competition have contributed to lower up-front costs than in the past.
To mitigate costs, providers can explore various financing options, grants and government incentives available to support the adoption of sustainable energy technologies. Collaborating with experienced energy solution providers who understand the specific needs of the aged care sector can also be valuable in finding cost-effective tailored solutions. By carefully evaluating the long-term benefits, considering available support mechanisms and working with knowledgeable partners, providers can overcome barriers and leverage the advantages of sustainable energy, fostering a more environmentally friendly and financially sustainable future for the sector.
We encourage readers to explore the potential of sustainable energy options, considering the diverse range of technologies available.
Energis can provide expert guidance to help providers embark on a path towards a greener and more efficient future in aged care – where compassionate care and sustainable energy go hand in hand.
Energis www.energis.com.au
Recognising excellence in retirement living, aged and community care
Are you across everything in your organisation?
We understand the obligations and reporting requirements for aged and home care providers. This process may be difficult when there are constant disruptions and unexpected incidents within the workplace. Whether it’s improving efficiency, implementing new strategies or solving complex problems, consultants play a crucial role in helping organisations achieve their goals and overcome challenges.
Get the right advice and support so you can have the best approach for your core business.
Connect Care Advisory collaborate with your internal team during the consulting process to ensure that the advice provided is practical, feasible, and aligns with your organisation’s capabilities. This will help you identify the specific areas where you require assistance, as well as having a clear understanding of your organisation’s culture, values, and internal dynamics.
Our team will give you a complete insight of your business and work with you to achieve the best outcomes for your consumers and staff.
Visit www.ccadvisory.cc or phone 0410 523 412 for more information.
Industry icon evolves and enters a new era as NeRA Cloud, with features that greatly improve the resident agreement process
NeRA Cloud is the next evolution of resident agreement software, offering providers sophisticated features in a more connected, productive and secure environment.
Introduced in 2006, NeRA software set the industry benchmark by transforming the resident agreement generation process. NeRA still plays a pivotal role in helping hundreds of providers produce compliant legal agreements successfully.

The move to cloud technology marks the start of a new era. Providers can access data securely from anywhere, using either a smart device or computer. Combined with advanced functions powered by cloud technology, NeRA Cloud will have a positive impact on workplace efficiency, outcomes for residents and the provider’s bottom line.
To look at how you can keep your aged service moving forward using NeRA Cloud, visit www.e-tools.com.au or contact e-Tools Software to schedule a free online demonstration on 03 9573-3277.
Healthy community and holistic wellbeing at Carinya Home
As exercise is a key aspect in improving the quality of life in the ageing population via prevention of diseases, reduction of falls risk, improvement of overall mental health and cognition, as well as social well-being, Carinya opened of a purposebuilt gym, equipped with HUR Australia products that allow for for individually tailored exercise programmes that also track the progress.
The allied health team is rapidly seeing the positive effects of the gym – only two months after the opening 30% of the residents are actively using the gym, with numbers continuously growing. Residents are demonstrating enhanced independence, elevated moods, and reduced agitation, as well as Improvements in balance, strength, flexibility, and mobility.

“Our goal is to keep promoting a holistic approach to maintain the wellbeing of individuals, promoting participation in a healthy community and support spiritual and emotional wellbeing. Purchase of HUR gym was the right decision and considered a real asset to us” says CEO David Osborne.
For more information visit: www.carinyahome.org.au
Core Capabilities Unify Home care and Residential Care

The Aged Care Reform train keeps chugging in terms of consultation and laying out the roadmap. To thrive in the next wave, Providers must get five things front and centre when it comes to consumer-facing risk.
1. Understand clearly which consumers experience the greatest degree of risk (harm-inducing) and build these into your business systems and people awareness systems. This means being able to determine consumer vulnerability.
a. Living on their own
b. Rural and remote with limited-service options
c. Few or no family or friends
d. Cognitive impairment and are unable to problem solve or ‘speak up’ for themselves
e. Have responsive behaviours which may impact on are provision (e.g. aggression, sexual disinhibition, purposeless wandering)
f. Links to any of the nine Special Needs groups as outlined in the Aged Care Act 1997
2. Understand the foundations of ‘capacity and substitute decision making’ for each consumer. No health and aged care system will ever support ‘consenting to neglect’. Providers will need to ramp up consumer health literacy and awareness and shift to a rights-based approach built around consumer needs, goals and preferences.
Soodox™ Soothe & Protect Barrier Cream

3. Have solid processes for clinical risk (High impact/ High Prevalent risk) – the main focus ones include (irrelevant of program type);
a. Pain Management
b. Falls prevention and management
c. Skin Integrity and pressure injury prevention and management
d. Complex care risks including (not limited to) diabetes, chronic disease, dementia affecting the ability to navigate dignity of risk decision making
e. Nutrition and hydration
4. Consumer deterioration recognition and response systems – very clear clinical pathways which are easy to follow and execute
5. Policy and practices that enable the entire workforce to recognise risks of neglect, abuse and exploitation and have clear processes for the escalation of those risks which include appropriate control measures.

Maintaining healthy skin is crucial for overall health and well-being. Soodox™ Soothe & Protect Barrier Cream is an excellent preventive measure against skin irritation caused by occupational exposure to irritants. This is where barrier creams are effective, now available is Soodox™ Soothe & Protect Barrier Cream which is Australian made, 100% natural, paraffin and fragrance free. It is gentle enough to use on the most sensitive areas - incontinence rash, skin folds, under breasts, bedsores, and chafing. This cream is highly recommended for use before and during work, as it forms a lubricating film on the skin, preventing water depletion in the skin’s outermost layer.
This protective effect may help prevent irritant contact dermatitis and allergic contact dermatitis, which are common conditions that often result from moisture depletion. It is essential to choose a product that is suitable for your skin type and needs, Soodox™ Soothe & Protect Barrier Cream is the perfect choice!
www.aussiepharmadirect.com.au
Health Staffing Australia
Before Labor came into power back in late May, they made some big promises about the aged care industry, and what they intended to do to improve it. Since being elected they have introduced a number of changes, many of which directly affect aged care providers. While the changes - including the introduction of the Star Rating System and a cap on home care charges - are beneficial to older Australians and their families, they do put more pressure on providers at a time
when many are already operating at a loss. The introduction of the Australian National Aged Care Classification (AN-ACC) funding model has not satisfactorily addressed this. However, it’s important to remember that fixing our aged care system is going to require long-term planning, and providers must continue to be part of the conversation in order to advocate for their own requirements and to help transform the industry into one that is sustainable for everyone.
Visit www.healthstaffingaustralia.com.au or phone 1300 132 595 for more information.

