
7 minute read
Clinical matters
from Vision Now June 2022
by Vision Now
Glaucoma revolution
New trends in glaucoma risk diagnosis and management
By Tom Kersey MBBS (Lond), FRCOphth
Recent advances have seen a surge of new ideas and technologies to aid in the detection, treatment and further understanding of glaucoma. These technologies and advances have led to earlier detection and better treatment options, which can be tailored to individual patients – providing an exciting time for physicians and patients alike and promising much better care on an individual basis.
Glaucoma is a group of conditions characterised by typical changes to the retinal nerve fibre layer and the optic nerve head, resulting in reduced visual field sensitivity. It has an enormous social and economic impact that leads it to remain as a leading cause of blindness worldwide. Not surprisingly, therefore, glaucoma research has attempted to reduce this burden through improved disease detection and more effective treatments. The specific areas of focus include methodologies for earlier diagnosis, elucidating modifiable viable risk factors, and the development of better intraocular pressure (IOP) dependant and non-IOP dependant treatments.
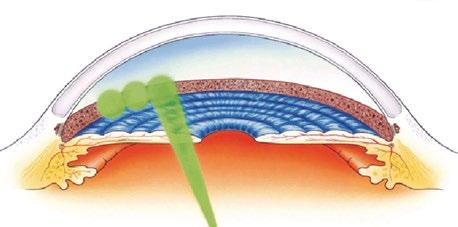
RISK FACTORS The lamina cribrosa provides structural and nutritional support to the retinal ganglion cells, as these pass from the pre-lamina to the post-lamina optic nerve. As glaucoma advances, the lamina cribrosa displays marked posterior bowing in the direction of a pressure differential between the IOP and the cerebrospinal fluid (CSF) pressure.
Although we know much about IOP in glaucoma, our understanding of CSF pressure is gradually emerging. So far, findings suggest that reduced CSF pressure leading to a pathologically enlarged trans cribrosa pressure differential may contribute to glaucoma pathogenesis. Recent studies indicate that CSF pressure may be a risk factor for primary open angle glaucoma. LOWERING IOP AND FLUCTUATIONS The lowering of IOP to prevent progression of glaucoma has now become the backbone of glaucoma management, and is supported by well-designed randomised control trials that have demonstrated that lowering IOP reduces the rate of glaucomatous damage.
These studies have included the ocular hypertension treatment studies (OHTS), which showed that lowering IOP reduces the rate of glaucomatous damage as defined by field loss or optic nerve head damage or both. Treatment by lowering IOP reduced the damage to patients by 10-15 per cent over five years.
Other studies have included the collaborative Normal Tension Glaucoma Study and the Collaborative Initial Glaucoma Treatment Study, as well as the Advanced Glaucoma Intervention Study. All of these studies have given weight and support to the idea that IOP lowering, as well as reducing IOP fluctuations, is a significant way to reduce the risk of glaucoma visual field progression.
Fluctuations in IOP can be thought of as occurring at different frequencies. There is diurnal variation, occurring during a single day, short-term fluctuation occurring over several days and weeks, and long-term fluctuation occurring over months and years. In practice, significant variation is seen over different visits or during phases of out-patients over a single day. Reducing these IOP fluctuations for patients reduces the risk factors for developing visual field progression. DETECTION AND DIAGNOSIS As the anatomical and functional changes from glaucoma are irreversible, early disease detection remains an important strategy to prevent visual impairment. This has been achieved by assessing optic nerve structure and function using optic nerve imagery and perimetry respectively.
Although fundamentally unchanged for several decades, both imaging and perimetric techniques have improved considerably. New strategies have emerged to complement these techniques, and these include retinal nerve fibre layer analysis and detection of retina ganglion cell apoptosis in vivo.
SPECTRAL DOMAIN OCT Spectral domain optical coherence tomography (OCT) in glaucoma patients offers the opportunity to objectively measure the retinal nerve fibre layer and associated change with time. It is an attractive tool in glaucoma assessment due to its ability to take non-contact, objective high resolution measurements.
New generation OCT scanners are able to achieve a resolution of 3-6μm compared with a 10μm resolution from the previous generations.
Detection of apototic retinal cells (DARC) is the ability to detect glaucoma at the earliest stages before field loss where approximately 40 per cent of retinal ganglion cells have already been lost. This new technique, which utilises the unique optical properties of the eye to directly visualise retinal ganglion cell death, may start to become a realistic option for the first time and give physicians the opportunity to detect glaucoma earlier and monitor the response of treatment in a visual and quantifiable manner.
The technology relies on the unique properties of Annexin V, a protein which has the ability to bind to negatively charged phospholipids in the presence of calcium. Annexin V staining has the ability to identify cells undergoing apoptosis envo using both radiological and macroscopic fluorescent techniques. Although still in its experimental stages, this technology may become widely available in the near future.
IOP TELEMETRY The evidence in support of peak IOP and IOP fluctuation points to the importance of
The Sensimed Triggerfish contact lens sensor transmits information to an antenna connected to a portable recorder (Sensimed AG)


NICE approved trabecular meshwork by-pass Glaukos hydro iStent An increased range of surgical procedures are now available

targeted IOP strategies. This is particularly so given evidence that the timing and type of current IOP lowering techniques can affect IOP fluctuation in different ways. The ability to identify individual differences might allow treatment to be tailored to the individual, and perhaps lead to lower rates of progression.
Our ability to identify patients requiring targeted treatment is improving; an example is the development of a telemetric contact lens with embedded strain gauges called the Sensimed Triggerfish. The device comprises of a disposable silicone contact lens with an embedded micro electro mechanical system and a thin micro fabricated platinum titanium strain gauge that measures the changes in corneal curvature.
It is based on the assumption that a correlation exists between IOP and corneal curvature, with a IOP variation of 1mmHg produces a change of central corneal curvature radius of approximately 3μm. Measurements are taken every five minutes for a duration of 30 seconds giving a total of 228 measurements over a 24-hour period. The results are presented in an arbitrary unit and not mmHg, and the future of this technology relies on translating the arbitrary electrical signal into a meaningful IOP. This is the current focus of many studies.
This technology may provide a paradigm shift, and will inevitably come as physicians will be presented with hundreds of IOP readings over a 24-hour period where previously they were acquainted with a single Goldmann applanation tonometer reading.
NEURO STRATEGIES Glaucoma is a condition characterised by retinal ganglion cell apoptosis and is therefore considered a type of neuro degenerative disorder. Strategies that prevent retinal ganglion cell apoptosis retard the way retinal ganglion cell apoptosis occurs (neuro modulation) or reverse the apoptotic process (neuro recovery). This may be a great benefit in glaucoma management in the future. The potential cellular pathways that contribute to retinal ganglion cell apoptosis are numerous and complex, but this presents many opportunities for therapeutic development.
For many years, animal studies have suggested that Brimonidine may have neuro protective benefits over and above its IOP lowering capability. This and other medications, including Memantine, have been studied in the past but have failed to show statistical significance for primary end points. However, it remains one of the most interesting areas for glaucoma protection development and treatment modalities of the future as it is non-IOP reliant. FUTURE OF TREATMENTS An increased range of surgical procedures dubbed MIGS (minimally invasive glaucoma surgery) are challenging the way we think and plan IOP lowering as glaucoma surgeons. Faster recovery times and safer risk profiles will inevitably be better for our patients. Eye stents, such as the Glaukos iStent inject W, are micro-titanium implants placed into the trabecular meshwork to bypass the fluid obstruction at that level.
Other intraocular stents include the Hydrus, the Xengel stent and Preserflo to name a few that have appeared in the past five years. Inevitably, some of these will prove more successful than others and time will tell which of these procedures remains long term.
Selective laser trabeculoplasty (SLT) has now become a mainstream treatment option, and is indeed the primary option alternative to drops. It is a five-minute outpatient procedure with proven IOP lowering that has been around for many years, making it an attractive and cost-efficient option for this chronic disease.
SUMMARY Glaucoma has never before seen such an advance in research and therapies coming forward to the clinical workplace. It is an exciting time for physicians and researchers alike, and the next decade will certainly see more advances in early detection, efficacious treatments and neuro protection.
Dr Tom Kersey MBBS (Lond), FRCOphth is a consultant ophthalmic surgeon who specialises in micro-invasive glaucoma surgery. He practises in Surrey and Hampshire and is available for NHS and private referrals. www.southeasteyesurgeon.co.uk. ■








