
14 minute read
Dr. Constance Visovsky first to research exercise
RESEARCH FEATURE
Dr. Constance Visovsky first to research exercise program to help cancer patients suffering from CIPN
Dr. Constance Visovsky remembers the time when
she was a young instructor and doctoral student teaching at Case Western Reserve University and an undergraduate student of hers conducting physical assessments at the VA hospital came to her with a problem.
The student was embarrassed, explaining that he realized he should know how to obtain a patient’s reflexes, but he was having trouble getting a response from one man in particular. Could she help?
Visovsky readily agreed, but when she arrived at the VA to observe the patient she was stunned. Just the semester before, the man—a cancer patient in his sixties—had been walking independently around the unit. After undergoing chemotherapy treatments for lymphoma, he was experiencing horrible neuropathy. Now he could barely walk.
(continued next page)
“The difference was astonishing,” Visovsky recalled. “We saved his life maybe, but we left him with terrible impairment.”
It was a pivotal moment in her career.
“I’m going to study this,” she decided about neuropathy and the neurotoxic and myotoxic effects of chemotherapy. The commitment deepened further a short while later after she graduated from Case Western with her PhD in nursing, and a woman in the community wrote to thank her for her research focus after reading about her in the newspaper.
The woman suffered neuropathy after receiving treatments for breast and lung cancer. She had been an avid gardener and seamstress who made her daughters’ pearllaced wedding gowns by hand, she wrote, sharing the information with Visovsky as if they were old friends. Now she could no longer do either.
“Whenever I got discouraged, I would re-read that letter,” Visovsky said about the 22 years that have passed since receiving it. The letter helped her “understand the importance of the day-to-day things that we take for granted, and the things we can do, and how important it is to a person’s quality of life.”
In those more than two decades, Visovsky, a faculty member at the USF College of Nursing since 2011, has become a renowned researcher and nurse scientist in the area of oncology and exercise.
She is currently in the middle of a five-year study to help cancer survivors improve balance, gait and strength following chemotherapy treatments—part of a $2.2 million grant awarded in 2019 from the NIH’s National Cancer Institute.
The research is the first to test the effects of a home-based exercise intervention for cancer patients suffering from CIPN—chemotherapy-induced peripheral neuropathy.
“There really are no good evidence-based treatments for this problem,” she said. One small past study addressed pain, but not function.
“So we believe that with our interventions, using exercise we are bringing blood flow to the peripheral nerves and oxygen to the peripheral nerves,” she said – in the process, preventing further impairment of the neurons.
The research includes very sophisticated measurements using sensors on a mat as well as on a person’s knees and ankles to record aspects of gait, balance and muscle strength.
While the pandemic slowed the recruitment of participants for the study, Visovsky said, so far more than 40 people had been enrolled by this fall for the 16-week regiment, with the end goal of 312 people. Materials are being translated into Spanish to help recruit non-English speakers as well.
While it’s too soon to draw conclusions, she said, anecdotally patients have told her team that they are enjoying the program and feeling benefits from it.
Visovsky is also working on a study with previous COVID-19 patients, to research people with long-term respiratory effects such as shortness of breath. Her team is designing a pulmonary rehabilitation program that consists of external muscle exercises and pursed-lipped breathing to help expand chests and bring up mucus with the goal of preventing reinfection.

Constance Visovsky, PhD, RN, ACNP, FAAN, Professor and Lewis and Leona Hughes Endowed Chair in Nursing Science, USF Health College of Nursing
For Visovsky, it’s important to practice what she researches —developing a regular exercise routine for herself later in life—from cycling to kayaking to running.
“To stay moving, you have to move,” she said. “I like to do a lot of things, so I want to have the energy to do them.” ■

In the fall of 2020, as the COVID-19 pandemic was raging with no vaccine or effective treatment in sight, Dr. Rayna Letourneau and other leaders at the USF Health College of Nursing asked themselves what they could do for members of their profession in the trenches.
“We have an opportunity to help our nurses in the community who are providing care to these patients on the frontlines,” Letourneau said recalling the conversation. “What resources and experiences do we have to help these nurses?”
Letourneau, an assistant professor at the college for a year by that point specializing in workforce development and safety education, shared with the team reports about nurses in the field enduring burnout, shortages in personal protective equipment, and fears of bringing the virus home to loved ones. Meanwhile, a local philanthropist, David Kotok, approached the dean of the College of Nursing, Dr. Usha Menon, about an idea for a Covid wellness webinar series. The college’s leadership team decided to tackle a needs assessment and then develop an educational webinar program to bring vital support and information to frontline nurses who could also use the series to satisfy continuing education requirements for license renewals. Once the subject concepts were outlined, Letourneau began looking around the country for experts to present the content in the videos.
One of the modules, they decided, had to be about risk mitigation and how nurses could keep themselves safe, beyond behaviors related to hand washing or wearing masks, she said. Another module focused on empowerment and as it relates to working in difficult situations.
One of the experts she contacted was Dr. David Lindquist from Brown University, who specializes in team building and who presented material for a module on debriefing strategies.
Other expert presenters were closer to home, like USF’s Dr. Amber Gum, professor in the Department of Mental Health Law & Policy, and whom Letourneau approached regarding her specializations in mental health and behavioral health interventions in self-care.
“We teach our patients how to stay healthy, but yet nurses don’t practice healthy behaviors,” Letourneau said about extremely stretched personnel who suffer high levels of stress, depression and suicide. “So the pandemic has just really exacerbated the problems of an unhealthy workforce.”
Every single expert jumped at the chance to help, she said.
“Everyone I contacted to present was extremely excited to be able to be a part of the project,” she said. “Everyone made time and made this a priority because nurses need it so much.” After several months of around-the-clock work to produce and edit the videos, the project was launched in January 2021. They called it: Frontline Nursing During COVID-19: A New Paradigm.
It is a four-part educational webinar series in which participants throughout the United States can earn a maximum of 4.0 Continuing Education Units, or CEUs, toward the renewal of their nursing licenses. One track is for novice nurses and a second track is for experienced nurses.
The series is available at no-cost to participants, made possible by Kotok and his partner, Christine Schlesinger.
“Covid proves the importance of dedicated and skilled nurses as a critical component in America’s healthcare,” said Kotok. “An important part of fulfilling the public health of the nation is driven by philanthropy. That’s why we are supporting this initiative.”
Want to learn more?
Scan here to sign up for the education credits and here to listen to the podcast.
For Schlesinger, a retired Advanced Practice Nurse, she has long known that hospitalized patient outcomes improve with optimal nurse-to-patient ratio.
“With increased patient acuity and decreased BSN/RN availability, patient outcomes are severely diminished,” she said. “COVID-19 plus our aging demographic – which naturally will require more nursing care – has brought this reality home like a hammer to a nail.”
Letourneau said that not only are nurses gravitating to the webinar series for accredited CEUs. But she also has been hearing from colleagues at nursing schools around the country who say they want to offer it to their students, especially those getting ready to graduate into the workforce in the middle of the pandemic.
From January through the end of August, more than 780 participants enrolled in the Frontline webinar series for a total of 585 CEUs, she said.
In addition to the webinar series, the team has developed a Frontline Nursing podcast series, too, with a new topic of discussion each month, from self-care to the state of science.
As for what’s next, Letourneau says she and fellow researchers will be seeking grants to study future steps and also looking at larger systemic issues beyond education and ways to address them.
For Letourneau, the feedback on the webinar and podcast series was deeply satisfying. Among the amazing notes she said she has received from around the country, one text in particular from a nurse colleague stood out: “Thank you for supporting us,” it read. “This means more to us than you will ever know.” Letourneau has dreamed of being part of major changes to the health care system all through her career – since acquiring a bachelor’s degree in nursing and a master’s degree in nursing administration from the University of Rhode Island; to obtaining a doctorate in nursing from the University of Massachusetts Dartmouth; to working as an ER nurse; and more recently while as an assistant professor at the University of Massachusetts Dartmouth and now at the University of South Florida.
She feels privileged to be at USF’s College of Nursing at a moment like this and under the vision of Dean Menon.
“This is where I needed to be to do this work,” she said about the college and Menon. “I thank her every day for trusting me to lead this project and for the college’s support.”
Frontline Nursing is all about workforce development, she added, giving nurses the skills to not only enter the field but stay in it safely and then to make systemic changes.
“Our health care system is in crisis. Nurses are the glue holding it together, and nurses need some help to make positive changes,” she said. “I want to be a part of that change.” ■


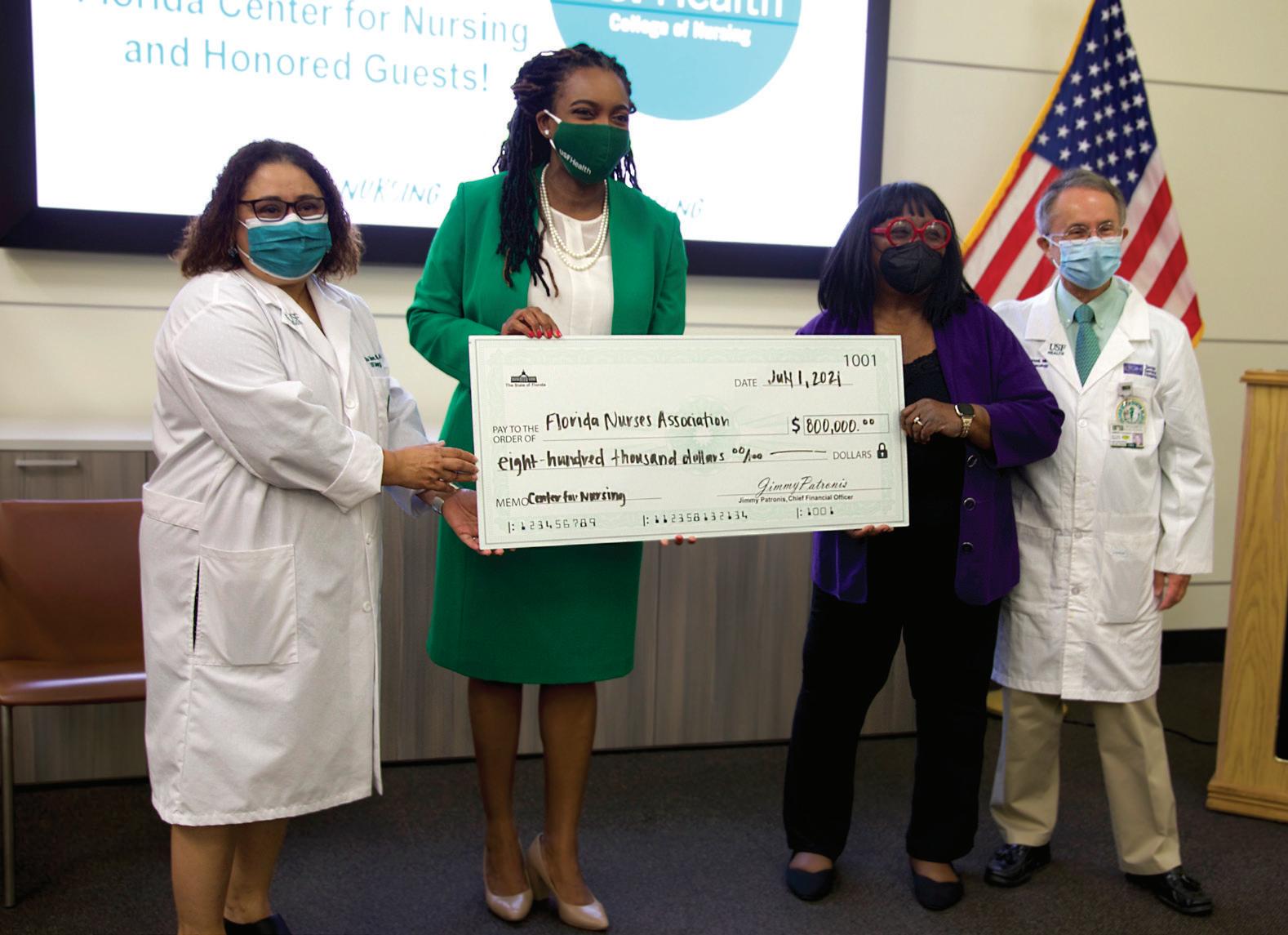

Florida Center for Nursing to be housed at USF College of Nursing
The State of Florida has awarded the Florida Nurses Association with the funding to reestablish the Florida Center for Nursing (FCN) and USF College of Nursing will be the research partner. The FCN was closed in July 2020 because it was vetoed from the state budget and there were no sustainable alternative funds. Reestablishing the FCN comes at a critical time for our state.
The FCN is a State Workforce Center which provides information, analyzes trends, conducts research, and predict nursing needs for the state. State Workforce Centers, as part of the National Forum of Nursing Workforce Centers, address nursing shortages within states and the nation and work to ensure an adequate supply of qualified nurses to meet the health needs of our nation.
During the COVID-19 pandemic, we are seeing nursing leave the bedside and leave the profession at alarming rates. Now more than ever, it is critical to understand the supply and demand of Florida’s nursing workforce. The purpose of the FCN will be to conduct analysis of Licensed Practical Nurses, Registered Nurses, and Advanced Practice Registered Nurse Practitioners every two years to understand the state of the workforce in our Florida. The FCN will collect and analyze data, publish reports and information, and make recommendations to resolve the nursing shortage.
The USF College of Nursing’s faculty experts will collaborate closely with the Florida Nurses Association to guide the FCN’s collection of data, analysis of imbalance between supply and demand, and prediction of needs so that the we can lead efforts that drive nursing workforce development and policy recommendations for the State of Florida. ■
Excellence in Nursing
In collaboration with Sarasota Memorial Hospital (SMH), the College of Nursing is launching a program toaddress the critical shortage of nurses, who are leaving the profession in record numbers.
The Excellence in Nursing During COVID-19 and Beyond program seeks to improve the working environment for nurses facing burnout and stress as the pandemic persists. The program also includes a clinical preceptorship-to-hire program at SMH for nursing students committed to working at that hospital or the new Venice campus after graduation.
“The COVID-19 pandemic has taken a significant toll on nurses, who spend so much time caring for others,” said College of Nursing Dean Usha Menon. “This program will empower the nurses of Sarasota, while also increasing opportunities for our students to work in the region.”Philanthropic support was provided by lead donors David Kotok and Christine Schlesinger, whose $115,000 gift completed funding for the pilot following a match challenge. Additionally, a $25,000 grant from Gulf Coast Community Foundation, as well as private gifts, and grants from the USF Foundation helped fund this pilot program. The program is set to launch in Spring 2022 and will continue for two years.
To learn more about the program, scan this QR code to watch a video.
WIRES™, a new office at the CON, will provide help to
health care workers exacerbated by the pandemic
The USF Health College of Nursing has established a new office dedicated to the health and wellness of nurses and interdisciplinary colleagues. Wellness, Innovation, Resources, Education and Support (WIRES™) for the Health Care Workforce will be recognized at local, state, national and international levels as a resource for the health care workforce. WIRES™ will continuously assess needs of the workforce and develop, implement and test interventions to meet those needs. WIRES™ will also publish reports and make policy recommendations to improve the workforce from the data gathered during assessment. (continued next page)

“We hear you,” said Dr. Rayna Letourneau, founding director of WIRES™.
“We hear our nurses, health care workers and patients telling us about the problems they face in our health care system. We know there is opportunity for improvement,” she added.
Letourneau has more than 20 years of nursing experience. She began her career as a staff nurse in one of the nation’s busiest emergency departments, then moved to hospital-based education and then higher education, where she has been for the past 13 years. Letourneau’s scholarship focuses on nursing workforce development, transition to practice, nurses’ health and wellness, and quality and safety education for nurses. She has numerous peer-reviewed and invited poster and podium presentations, several peer-reviewed publications, and commentary and analysis articles published for the public.
Through WIRES™, Letourneau plans to lead a team of experts at the college to transform the health care industry and ensure a healthy, competent and empowered workforce, ultimately advancing the well-being of communities.
The concept of WIRES™ came to her in 2021 after the College of Nursing launched “Frontline Nursing During COVID-19: A New Paradigm,” an educational webinar and podcast series that provides nurses with tools to navigate the challenges of working the frontlines of a pandemic.
“A tired, sick, burned-out workforce cannot provide the best care,” she explained. “We know the COVID-19 pandemic exacerbated the health and wellness problems of nurses and our interdisciplinary colleagues.”
WIRES™ will provide hands-on assistance to clinicians, faculty and students. Assistance will include webinars, continuing education programs, podcasts, well-being programs and workforce development programs that facilitate students’ transition from academia to professional practice. Additional interventions will be identified as data is gathered.
The vision of WIRES™ is an empowered nursing workforce that will lead health care transformation worldwide. The goals and outcomes of WIRES™ are:
• Promote healthy lifestyle behaviors that have been found to optimize and improve overall health and well-being of ourselves, our patients, our communities, and our fellow clinicians • Deliver transdiscipline, specialized programs and consultation regarding workforce development, leadership, education, and well-being to agencies, clinicians, and other scientists
• Inform and influence policies
• Create a pipeline of healthy clinicians ready to enter the workforce and be known as the national resource for evidence-based retention strategies
• Create academic-practice partnerships that will lead change and advance health through collaboration
The work of WIRES™ aligns with the recently released 2021 National Academy of Medicine’s Future of Nursing 2020-2030 report. WIRES™ key focus areas of wellness, education, and workforce development will promote health and well-being among nurses, health care professionals, individuals, and communities, and address the systematic inequities that cause persistent health disparities.
The WIRES™ office is located at the College of Nursing on the Tampa Campus (MDN 1002L) and can be contacted at healthWIRES@usf.edu. ■
Emerging
NURSE SCIENTISTS
The new Emerging Nurse Scientist Summer Fellowship is made possible thanks to a generous donation from alumnus Carl Goff, PhD, RN, ‘86.








