
57 minute read
Nursing News
NEWS School to Launch New Acute Care Pediatric NP Program
The UR School of Nursing is set to launch a new Pediatric Nurse Practitioner (PNP) Acute Care program, its latest groundbreaking initiative in a history of transformative nurse practitioner education.
The one-year post-master’s certificate program, slated to begin in the fall of 2021, is the first of its kind in New York State. It focuses on caring for children of all ages with complex, acute, critical and chronic illnesses, disabilities, or injuries, and prepares students to deliver high-quality advanced nursing care that restores health, prevents complications, and assists patients and families in navigating rapidly changing health care environments. Program graduates will be well-prepared to work in a variety of clinical settings, such as pediatric intensive care units, emergency rooms, urgent care departments, trauma centers, and pediatric specialties such as cardiology, pulmonology, and neurology.
The UR PNP acute care post-master’s program is a critical addition to the advanced practice specialties available to nurses, not only in Rochester, but across the region. Nationwide, there are only 42 acute care PNP programs recognized by the Pediatric Nursing Certification Board.
The UR Nursing program was developed by a small group of specialty pediatric faculty, led by Erin Baylor, DNP, RN, PPCNPBC, ONP, who will be the specialty program director. The team also included Elizabeth Cole, MS, RN, ACPNP-BC; Andrew Wolf,
EdD, RN, AGACNP-BC; Craig Sellers, PhD, RN, AGPCNP-BC,
GNP-BC, FAANP; and Margaret Carno, PhD, RN, PPCNP-BC. The program will consist of a mixture of online courses and on-campus intensives. Students will be required to complete two semester-long courses of 6-9 credit hours each, which include a lab and clinical hours.
Requirements for the program include a bachelor’s degree in nursing from an accredited school of nursing, a graduate degree (master’s or doctoral) as a pediatric nurse practitioner, and RN licensure. The application deadline for the program is April 15, and a limited number of students will be accepted into the program each fall. For more information on the program, please visit urson.us/pnp-acute.
Erin Baylor, DNP, RN, PPCNP-BC, ONP, the current director of the Pediatric Nurse Practitioner program, will be the specialty program director of the PNP-Acute Care program. A small group of specialty pediatric faculty, led by Baylor, developed the new program.
UR Nursing in the News
What’s new in the School of Nursing? Here are some recent media reports involving UR Nursing faculty, staff, and students.
Beth Palermo, DNP, RN,
ANP-BC, ACNP-BC, assistant professor of clinical nursing, was quoted in a Futurity article about the history of the ventilator during its peak demand at the beginning of the pandemic.
The Rochester Business Journal profiled Associate Dean Renu Singh, MS, on her success as the CEO of UR Medicine Employee Wellness Program and its nurse-based condition management program.
Dean Kathy Rideout,
EdD, PPCNP-BC, FNAP, made several local Rochester TV and radio appearances during National Nurses Week in May, including teaming up with acute care nurse at Strong Memorial Hospital and alumna
Danette Niles, BSN,
RN-BC, to share how the COVID-19 outbreak had impacted both nursing job responsibilities and education.
Rideout also appeared on Fox’s “Good Day Rochester” in the fall to discuss the UR School of Nursing’s commitment to diversity and its fourth consecutive HEED Award (see story, opposite page).
The stars aligned for UR School of Nursing student Jose Perpignan, RN, when Kelly Ripa and Ryan Seacrest announced he was the winner of the show’s $100,000 Healthcare Hero giveaway. Perpignan is a 2016 graduate of the UR Nursing APNN program and is currently a student in the UR Nursing FNP/DNP program (see story, page 34).
Four-peat
UR School of Nursing Honored with Fourth Consecutive HEED Award
It’s a four-peat for the University of Rochester School of Nursing.
For the fourth straight year, the UR School of Nursing was honored with the Health Professions Higher Education Excellence in Diversity (HEED) Award from INSIGHT Into Diversity magazine.
The UR School of Nursing and the UR School of Medicine and Dentistry were among 46 health professions schools selected to receive the only national honor recognizing U.S. medical, dental, pharmacy, nursing, osteopathic, and allied health schools that demonstrate an outstanding commitment to diversity and inclusion.
The schools were featured in the December 2020 issue of INSIGHT Into Diversity, the oldest and largest diversity-focused publication in higher education. The University of Rochester was previously named a recipient of the HEED Award presented to colleges and universities in November.
The HEED awards were a bright spot in a year where racial tensions ran high and waves of protests raged across the country, including in Rochester, which temporarily became the epicenter of outrage this summer when news emerged of the death of a Black man, Daniel Prude, after being subdued by city police.
On campus, protests and demands for equality also flared, prompting UR Medical Center leadership to take action, such as declaring racism a public health crisis and stripping the name of past leaders whose historical exclusionary practices were well documented from campus buildings. Mark Taubman, MD, dean of the School of Medicine and Dentistry and CEO of the Medical Center, personally led the development of a comprehensive anti-racism action plan, incorporating input from medical students, residents, graduate students, the Black Physicians Network of Greater Rochester, the Rochester Black Nurses Association, and faculty and staff from across the university in an effort to further strengthen the Medical Center’s commitment to diversity and equality.
The UR School of Nursing, which has been at the forefront of diversity, inclusion, and equity issues for nearly two decades, was one of only nine nursing schools to receive the HEED Health Professions Award in 2020. Its academic programs attract scientists, clinicians, researchers, and future nurses of varying ages, backgrounds, and talents, and its incoming fall class of students in the Accelerated Bachelor’s Program for Non-Nurses (ABPNN) included students from across the U.S. and countries such as Nigeria, Mexico, Turkey, Jamaica, and Ghana. Thirty-five percent of the new ABPNN students were from groups underrepresented in nursing, and 25 percent were male, approximately three times higher than the percentage of men in the nursing workforce.
“Receiving the HEED Award is a gratifying acknowledgement of the School of Nursing’s decades of work fostering an environment of diversity, equity, and inclusion,” said Kathy Rideout, EdD, PPCNP-BC, FNAP, dean of the School of Nursing and vice president of the University of Rochester Medical Center. “We’re proud of how much we have accomplished, but we also know there is much work still to do. We will continue to look inward with a critical eye, knowing that our vigilance and persistence is essential to continual growth.” “The HEED Award process consists of a comprehensive and rigorous application that includes questions relating to the recruitment and retention of students and employees – and best practices for both – continued leadership support for diversity, and other aspects of campus diversity and inclusion,” said Lenore Pearlstein, publisher of INSIGHT Into Diversity magazine. “We take a detailed approach to reviewing each application in deciding who will be named a HEED Award recipient. Our standards are high, and we look for institutions where diversity and inclusion are woven into the work being done every day.”

NEWS Employee Wellness Team Honored with Meliora Award
Developed by the University of Rochester School of Nursing, the UR Medicine Employee Wellness program, known internally as the Center for Employee Wellness (CEW), received the 2020 Meliora Award in June.
The award, presented by the University of Rochester, recognizes staff members whose work performance and dedication during the preceding year exemplify the University's motto, Meliora, which translates to “ever better.”
What started as a program for University employees in 2013 is now offered in 55 organizations across the region to more than 47,000 employees.
Akin to a startup company, the Center for Employee Wellness was built from the ground up. With the dedication of a team of over 40 experts that include clinicians, analysts, programmers, and scholars and the leadership of CEO Renu Singh, MS, the CEW developed a game-changing wellness program capable of achieving measurable health improvements in the population they serve.
The team is consistently praised by clients and colleagues as working with clarity, integrity, innovative spirit, and a commitment to wellness.
Rick Amundson, wellness consultant at Smola Consulting said, “The team is driven by a collective commitment to improve health and wellness in our community.”
Team members of the CEW have reached numerous impressive milestones and achievements, including the highest reported engagement rates in condition management coaching programs for individuals with chronic diseases.
Under the direction of Lisa Norsen, PhD, RN, ACNP-BC, the chief wellness officer, the clinical wellness programs have demonstrated measurably improved health for employees that participated in screenings or one-to-one condition management programs. In a large data study published in a peer-reviewed health journal, the CEW demonstrated a significant reduction in cardiovascular health risks in the population they serve.
“For the Center for Employee Wellness, the wellness program is not just a product, it’s their purpose,” UR School of Nursing Dean Kathy Rideout, EdD, PPCNP-BC, FNAP, said in her letter supporting the CEW’s nomination. “Every member of the team is invested in the mission.”
“The most potent differentiator of this program is the outstanding quality and dedication of their clinical team,” said Jason Mull, vice president of employee benefits at Brown and Brown Insurance, in his letter of support. “They are knowledgeable, sincere, and passionate about what they do. The client representatives and the business office are responsive, articulate, and committed to program success and client satisfaction.”

The UR Medicine Employee Wellness program started as a pilot in 2013, bringing wellness programs to University of Rochester employees. Several years later, the Employee Wellness team serves 55 organizations and more than 47,000 employees in the Finger Lakes region.
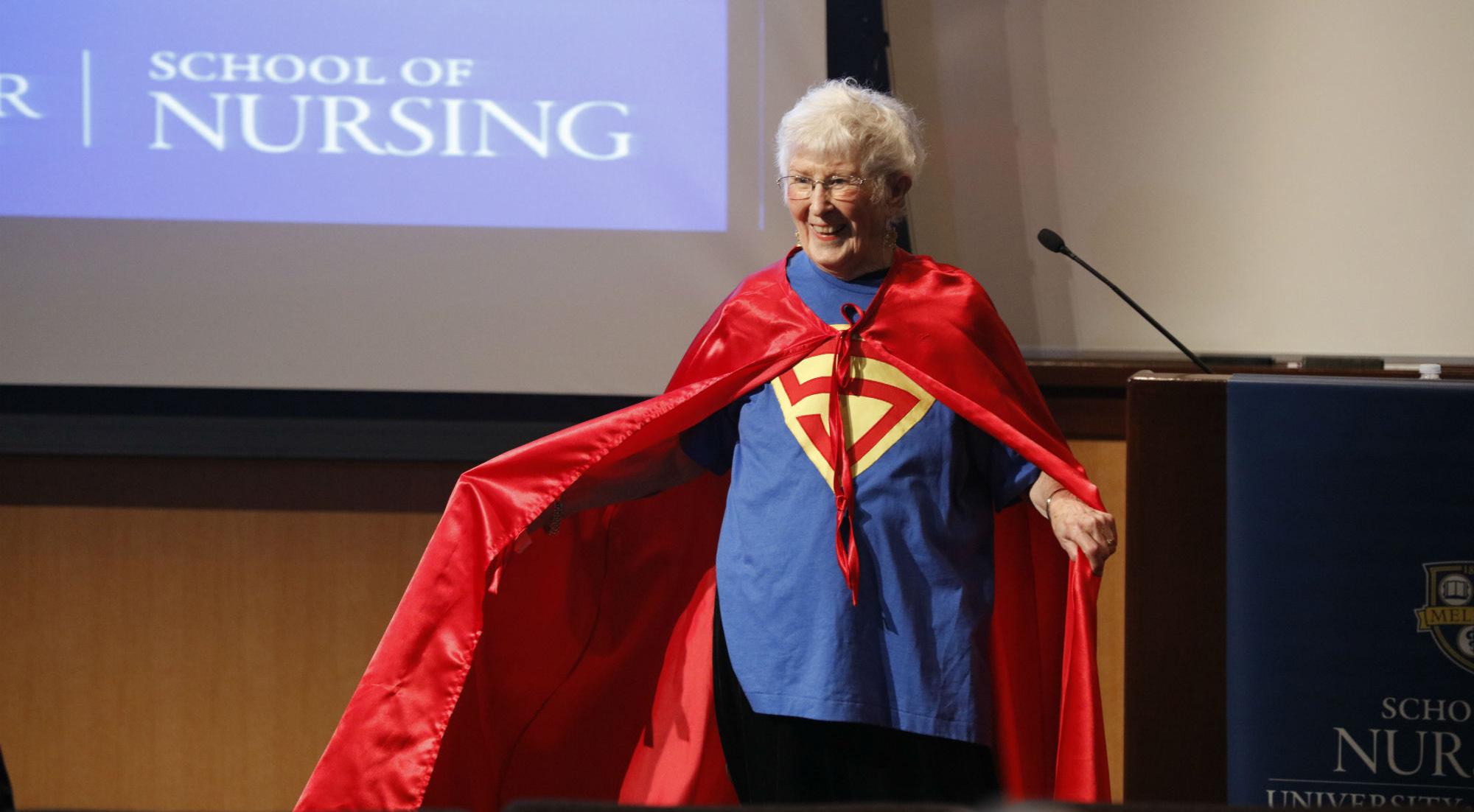
Alumna, Former Faculty Member Elizabeth Kellogg Walker Establishes Endowed Nursing Scholarship with $100K Gift
For more than 60 years, the University of Rochester School of Nursing has been a central influence in the professional life of Elizabeth Kellogg Walker ’62N, ’73N (MS), ’81 (MA), ’86 (PhD). She first came to the University as an undergraduate in 1957 and retired from the nursing faculty in 2016. After so many years being connected to the school, she knew exactly where she would direct the funds if she ever found herself in a position to make a substantial financial gift.
A longtime member of the George Eastman Circle, Walker made a $100,000 gift to the UR School of Nursing in November to establish the Elizabeth Kellogg Walker ‘62N, ‘73N (MS), ’81 (MA), ’86 (PhD) Nursing Scholarship.
“The University has been a very important part of my life, from my days as an undergraduate on River Campus to nursing school and the many degrees I received there,” said Walker. “I was very proud to be a faculty member there, and I believe I contributed to students' growth and the profession of nursing. “I’ve always been proud of the University of Rochester and this is about giving something for future generations. I’m very happy Elizabeth Kellogg Walker with this.” Walker has had a long and distinguished career in nursing and education. She was formerly chair of the UR School of Nursing’s Division of Health Care Systems and was director of the start-up joint MSN/MBA program with Simon School in the late ‘80s and early ‘90s. She went on to serve as dean of nursing at SUNY Institute of Technology, retiring as dean emerita in 2000. She returned to the UR School of Nursing in 2002 as a part-time assistant professor of clinical nursing and mentor for the Center for Academic and Professional Success.
When determining the structure of the scholarship, Walker intentionally left it unrestricted, which will allow the school to annually award funds to students enrolled in any of its academic programs.
“As a former dean, I know that flexibility helps a great deal in offering scholarship support,” Walker said. “I told Kathy Rideout, ‘I want you to be able to use this to go get that star student you want.’”

SON National Council Holds Inaugural Meeting
Members of the new School of Nursing National Council held their inaugural meeting in November.
In their first gathering, held remotely, the council heard updates from around the school, received insight into the next round of strategic planning, and discussed ways they can assist the school moving forward.
Chaired by Sandy Parker, former president and CEO of the Rochester Business Alliance and a member of the University’s Board of Trustees, the council serves as a leadership volunteer advisory group to the dean and a bridge between the school and the greater community. It consists of national thought leaders who bring particular knowledge and experience to help shape plans for the future of the school.
Other members of the National Council, which will meet two times per year, are:
• Rachel Bandych, franchise executive consultant and attorney
• Kamila Barnes, ’11N (MS), ’13N (DNP), assistant professor of nursing at Long Island University - Brooklyn, family nurse practitioner at Northwell Health
• Nancy Dianis, ’85N (MS), vice president and practice director, Westat
• Sergio Esteban, chairman and principal at LaBella Associates
• Marilyn Fiske, ’67N, retired co-founder, OCI
• Arnice Jackson, ’11N, nurse practitioner, adjunct professor,
Long Island University
• Gerri Lamb, ’78N (MS), professor, founding director, Center for Advancing Interprofessional Practice, Education and
Research, Arizona State University
• Susan Parkes McNally, executive vice president, treasurer and human resources director, O’Connell Electric Company
• Jacqueline Nasso, ’95N (MS), ’97N (MS), certified nurse midwife, assistant professor of clinical nursing, UR School of
Nursing
• LaRon E. Nelson, ’02N, ’04N (MS), ’09N (PhD), associate dean of global affairs and planetary health and Independence
Foundation Associate Professor of Nursing, Yale University
• Phyllis Arn Zimmer, ‘72N, NP, president, Nurse Practitioner
Healthcare Foundation; faculty, University of Washington
School of Nursing; president, America’s Nurses, a public benefit corporation
NEWS Helen Wood Hall Expansion Project to Enhance Academic Experience, Accommodate Enrollment Growth
A $15 million expansion project at Helen Wood Hall will enhance the academic environment and allow the UR School of Nursing to better serve its surge in new students.
The project, which adds three floors to the Loretta C. Ford Education Wing, will provide for the continued projected growth of both undergraduate and graduate students and new expanded experiential learning spaces.
Construction of the project began last fall when the School of Nursing welcomed another record-breaking student body. The school’s total enrollment has grown by more than 50 percent since 2016, from 529 to nearly 800 students. The timing of an enrollment boom couldn’t be better since the demand for nurses in the workforce is also at an all-time high.
In response to the workforce needs and health professional education trends over the past decade, 21st-century nurse educators must employ more active learning approaches that ensure graduates are competent clinicians, employ data-driven clinical decision making, demonstrate complex problem-solving skills, and effectively collaborate on inter-professional teams. This requires a dynamic, flexible, and highly individualized learning environment.
Experiential learning labs will support a variety of learning activities, including high-fidelity simulation, standardized patient scenarios, virtual/augmented reality experiences, and task-based education for development of psychomotor skills. This new space will also be used as collaborative spaces for case-based learning, team-based learning, and debriefing activities.
“Year after year, student response to simulated learning opportunities—currently limited due to existing capacity—is overwhelmingly positive with students universally requesting additional simulation experiences,” said Kathy Rideout, EdD, PPCNP-BC, FNAP, dean of the School of Nursing and vice president of the University of Rochester Medical Center. “Therefore, the additional space will not only deepen student learning, but also enhance student engagement and student satisfaction with their educational experience at the School of Nursing.”
Earlier in the year, the UR School of Nursing received a $1 million award from the Higher Education Capital Matching Grant (HECap), part of an apportionment for capital projects at 35 colleges and universities across New York to help campuses modernize facilities, enhance student experiences, and spur economic development.
Helen Wood Hall was originally built in 1925 to house the University of Rochester's nursing program. The building served as a dormitory with classroom learning spaces in its early years. In later years, residential areas were converted to offices, classrooms, and clinical lab spaces. Over time, limitations in classroom and clinical lab space restricted necessary program growth.
The need to incorporate larger and “smarter” classrooms as well as advanced clinical simulation experiences led to the addition of the Loretta C. Ford Education Wing in 2006, a 28,000-square-foot expansion that includes four large classrooms, an auditorium for 170 people, a seminar room and atrium. This current vertical expansion project, expected to be completed by spring of 2022, expands even more the academic programs and instructional capabilities that are critical to student learning in an increasingly complex health care system. It will also allow for renovation of significant square footage on the first floor of Helen Wood Hall due to the relocation of the existing skills and simulation labs to the new addition. This will be completed in a separate phase.

An architectural rendering of the planned vertical expansion of Helen Wood Hall. The $15M project, which began in October and is expected to be completed by the spring of 2022, adds three floors to the Loretta C. Ford Education Wing.
A Woman for the Ages
Loretta Ford named to USA Today list of most influential women of the last 100 years
2020 was a special year for Loretta Ford, EdD, RN, PNP, FAAN, FAANP.
Not only was she presented with the Surgeon General's Medallion for her extraordinary achievements and contributions to the cause of public health, but December of that year would mark the diminutive trailblazer’s 100th birthday.
Ford, renowned as the co-founder of the nurse practitioner role, was born in New York City in 1920, the same year that women gained the right to vote in the U.S. A century later, when USA Today commemorated the 100th anniversary of the ratification of the 19th Amendment, Ford herself was listed among the period’s most extraordinary and influential women.
USA Today editors compiled a remarkable list of 500 women – living and dead – whose accomplishments and contributions to society over the past century have had an unmistakable impact on American life. Only 10 would be chosen to represent each U.S. state.
Retired and living in central Florida, Ford was selected to represent the Sunshine State, alongside such luminaries as Zora Neale Hurston, Marjory Stoneman Douglas, and Janet Reno, but her time spent in New York and Colorado would have a lasting impact that stretched far beyond any borders.
Ford began her career at age 16 as a nurse’s aide at Middlesex General Hospital in New Brunswick, New Jersey and earned her nursing diploma in 1941. She joined the Visiting Nurse Service, but enlisted in the Air Force after her fiancé was killed in World War II. She spent three years in the military then signed up to attend the University of Colorado on the G.I. Bill, kickstarting a groundbreaking career in nursing practice and education. She received her bachelor’s in nursing in 1949, a master’s in public health in 1951 and a doctorate in education in 1961. She joined the faculty at the University of Colorado School of Nursing, where she famously teamed with pediatrician Henry Silver to create the first pediatric nurse practitioner program in 1965. The move was controversial at the time, and Ford was met with considerable resistance and criticism in the medical community, but she pressed on, seeing how the program could improve patient care for those families most in need.
In 1972, Ford became founding dean of the University of Rochester School of Nursing and director of the nursing service at Strong Memorial Hospital. She bridged these two disciplines to create the “unification model of nursing,” a program that combines education, research, and clinical practice to form a more holistic approach to nursing and health care.
By the time she retired in 1986, Ford had succeeded in establishing the nurse practitioner as an integral part of health care teams and brought greater respect and appreciation to the nursing profession as a whole. Today, there are more than 290,000 practicing nurse practitioners in the U.S. For her work, Ford was inducted into the National Women’s Hall of Fame in 2011.


Few health care providers can boast a legacy equal to that of Loretta Ford. The co-creator of the nurse practitioner role and the unification model of nursing, the UR School of Nursing’s founding dean’s lifetime of work was recognized by USA Today, which named her one of the nation’s most influential women of the past 100 years.
Rochester Academy of Medicine Recognizes Three UR Nursing Faculty Members

Three members of the UR School of Nursing faculty were among a dozen URMC professors honored at the Rochester Academy of Medicine’s annual awards event on Oct. 27.
Marianne Chiafery, DNP, RN, PNP-BC, Elizabeth Palermo, DNP, RN, ANP-
BC, ACNP-BC, and Tobie Olsan, PhD, RN, CNL, FNAP, were each recognized at the academy’s annual meeting for their contributions to health care in the Rochester community.
Chiafery was presented the Individual Distinguished Service in Health Care Award. The academy’s Distinguished Service Awards are given to individuals and teams in recognition of their outstanding service in the health care profession. Chiafery is an associate professor of clinical nursing, a pediatric nurse practitioner, and a member of the Hospital Ethics Committee and the Clinical Ethics Consult Team at Strong Memorial and Golisano Children’s Hospital.
Palermo received the Nurse Practitioner/Physician Assistant Award, which is given to the individual who demonstrates the strongest ability to work collaboratively within a health care team in the delivery of the highest quality, evidence-based care that is patient- or family-focused. In addition to working as a nurse practitioner at Strong Memorial Hospital, Palermo is an assistant professor of clinical nursing and specialty director of the Adult-Gerentology Acute Care Nurse Practitioner program at the UR School of Nursing.
Olsan, professor of nursing emerita, was presented with the Carter & T. Franklin Williams Geriatric Prize Award for her scholarly writing on geriatric health care. Olsan shared the prize with Suzanne Gillespie, MD, RD, a colleague of hers at the Canandaigua Veterans Medical Center and the UR School of Medicine and Dentistry.

Parent Peer Mentor Michelle Morales Honored by NY Office of Mental Health

Michelle Morales was honored by the New York State Office of Mental Health in October for her work mentoring parents of children with eating disorders.
Morales is a parent peer mentor for the Western New York Comprehensive Care Center for Eating Disorders, one of three legislatively mandated comprehensive care centers for eating disorders funded by the New York State Department of Health. In her role, she teaches parents how to offer support to their loved ones in recovery.
She was selected to be the Family/Caregiver honoree at the What’s Great in Our State event, a forum to celebrate children’s mental health awareness, and recognized at the awards ceremony on Oct. 15.
The Western New York Comprehensive Care Center, a partnership between the UR School of Nursing and Golisano Children’s Hospital, is directed by Professor of Clinical Nursing Mary Tantillo, PhD, PMHCNS-BC, FAED, CGP, out of the UR School of Nursing. It serves as a hub for eating disorder services in the 30-county Western New York region, which has an estimated 20,000 to 30,000 individuals with an eating disorder.
Marianne Chiafery, DNP, RN, PNP-BC Elizabeth Palermo, DNP, RN, ANP-BC, ACNP-BC Tobie Olsan, PhD, RN, CNL, FNAP Michelle Morales
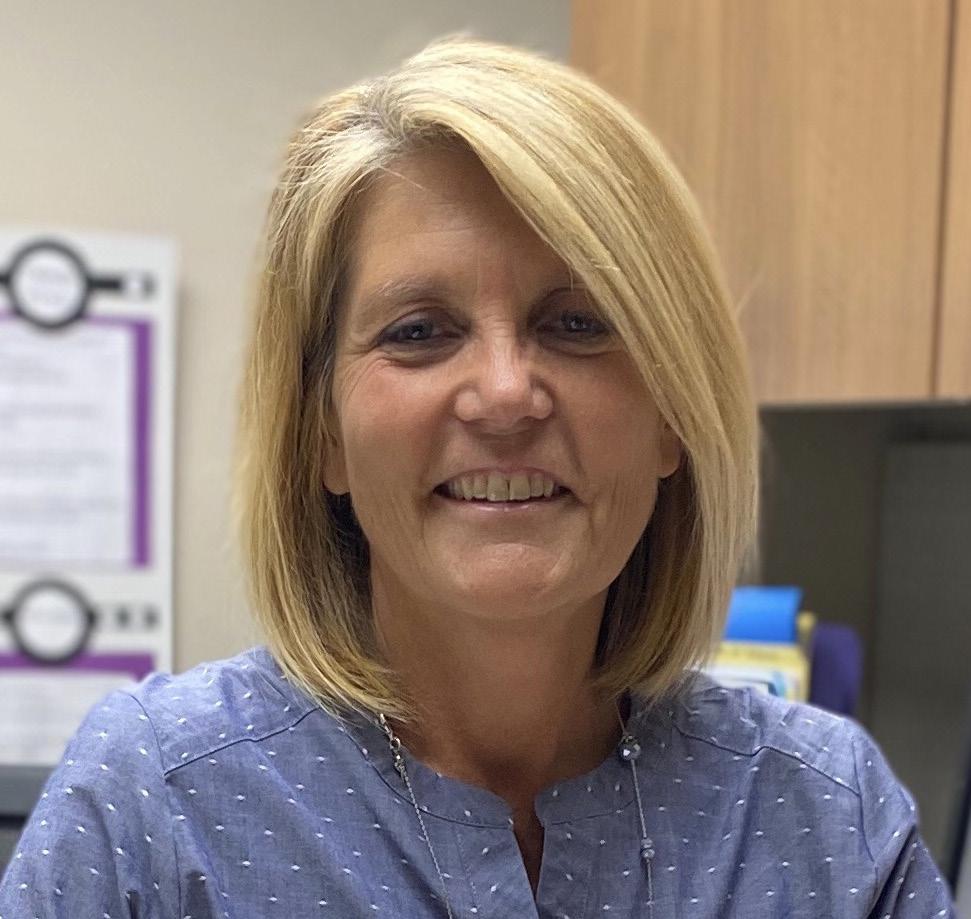
Meet UR Nursing's Director of Student Affairs
Colleen Johnson, MS, joined the UR School of Nursing in July as its new director of student affairs.
Johnson brings a wealth of experience to the role. She worked for seven years at Rochester Institute of Technology, and most recently spent five years at Finger Lakes Community College, where she was director of academic success and access programs.
At the UR School of Nursing, Johnson takes over a newly revamped student affairs office, which formerly was part of the admissions operations, but now reports directly to Lydia Rotondo, DNP, RN, CNS, FNAP, associate dean for education and student affairs. The new student affairs office will focus on all student-facing activities, including advisement and compliance, student support programs, such as the Center for Academic and Professional Success, and student organizations, such as Leading with Integrity For Tomorrow and Street Outreach.
5 Questions with Colleen Johnson:
Where are the places you’ve called home?
Rochester and Greece, NY
Reading, UK
Potter, NY
Fairport, NY
Who are your role models?
The many female leaders, in both my professional and personal life, who’ve taught me to keep learning, ask tough questions, be authentic, and always pay forward what I have been fortunate to receive as a mentee.
Why did you get into higher education/student affairs?
I stumbled into higher education and ultimately, student affairs. As an undergraduate student, I was interested in clinical psychology as well as organizational and industrial (I/O) psychology. After completing my master’s degree in human resource development, I considered doctoral work in I/O psychology, but was discouraged from pursuing the opportunity due to concerns I would be overqualified and under experienced in my late 20’s/ early 30’s. I took a year to focus on my next steps and worked in the Co-op and Career Services Office at RIT, where I started interacting with students preparing for co-op placement. Many years later, I still enjoy the process of building relationships with students, making connections, and guiding them towards completion of their personal and academic goals. I have been fortunate to have experiences where I can combine my love of supporting students, leadership and human resources, and systems design. I think of myself as an architect of the student experience.
What are you currently reading?
I don’t read very much fiction. When I have time and mental bandwidth, I read Outliers, by Malcolm Gladwell and the Handbook of Self-Determination Research by Edward Deci and Richard Ryan.
What might people be surprised to learn about you?
Learning was always difficult for me and it was not until late into my undergraduate experience (just before graduating), where I really understood my own learning preferences, interests, and potential. Ask me about my travels in Europe, it’s all related. The School of Nursing welcomed two faculty members to its academic leadership team this fall.
Linda Schmitt,
MS, RN-BC, CNL, was named co-director of the Health Care Organization Management and Leadership (HCM) program, and Susan Stanek, PhD, MSN/Ed, RN, was named interim director of the Center for Lifelong Learning (CLL).
The school also announced that Yingzi Zhang, PhD, successfully completed her postdoctoral fellowship and accepted an offer to join the school’s tenure track faculty as an assistant professor.
Schmitt, who received her master’s degree in the Clinical Nurse Leader track in 2012, recently joined the faculty as an assistant professor of clinical nursing. Stanek completed her PhD from the UR School of Nursing in 2020. A senior associate, she has been teaching at the school since 2012.

Schmitt, Stanek take on academic leadership positions
Schmitt
Stanek
NEWS National Nursing Leaders Speak on Caring in Crisis at UR Nursing’s DNP Summit
For the fifth consecutive year, the University of Rochester School of Nursing gathered nursing experts in a national discussion about the value of doctorally prepared nurses in the modern world of health care.
This year’s Doctor of Nursing Practice (DNP) Summit, “DNPs Leading and Caring in Crisis” addressed the need for strong practitioners and nursing professionals to be prepared to meet challenges and enact positive change during a crisis like the COVID-19 pandemic.
The summit began on Friday, Oct. 16, and continued Oct. 23 and Oct. 30. In contrast to previous years and fitting with the event’s theme, the summit was held virtually to maintain COVID-19 safety measures and precautions.
The digital format proved to be a great success, attracting nearly 250 attendees. Alumni, current students, UR School of Nursing and University of Rochester Medical Center (URMC) employees, and individuals from health care institutions in almost every state across the U.S. tuned in to the event.
Presenters included Strong Memorial Hospital’s Director of Adult Critical Care Nursing Kate Valcin, DNP, RN, CCRN-K, NEA-BC, CNL, University of Delaware School of Nursing’s Sharon Dudley-Brown, PhD, FNP-BC, FAAN, FAANP, and Vanderbilt University School of Nursing’s April Kapu, DNP, RN, ACNP-BC, FAANP.
A co-leader of the Highly Infectious Disease Unit, Valcin helped lead Strong’s COVID-19 planning, transforming the Medical Center’s response from reactionary to proactive planning.
In her DNP summit presentation, “Hitting the Ground Running: DNP Preparation Meets Global Pandemic,” Valcin shared stories of nursing innovation, rapid implementation of evidence-based practice, and interprofessional collaboration within URMC. A graduate of UR Nursing’s Clinical Nurse Leader and DNP programs, Valcin also recounted her many “aha” moments where lessons learned in her academic journey aligned with the work being done to combat COVID-19.
Dudley-Brown, who earned her bachelor’s degree from the UR School of Nursing in 1984, was this year’s Clare Dennison Lecturer, a designation that traditionally kicks off the University’s Meliora weekend celebrations. Dudley-Brown, an associate professor and director of the DNP Program at the University of Delaware School of Nursing, shared what every DNP-prepared nurse needs in a time of crisis in her presentation titled, “DNP Toolkit: Critical Competencies for Leading and Caring in Crisis.”
An associate nursing officer at Vanderbilt University Medical Center and professor at Vanderbilt University School of Nursing, Kapu explained how she saw the challenges of COVID-19 as opportunities to innovate and lead.
During her presentation, “Crisis and DNP Opportunity: Practice and Policy during COVID,” Kapu also elaborated on the policy and legislative changes throughout the pandemic that opened doors to demonstrate the impact of increased access to nurse-driven, evidence-based care.

Valcin

Dudley-Brown

Kapu
NEWS UR Nursing Takes New Approach to Traditional Year-End and Convocation Events
In a year that has played havoc with accepted customs and traditions, the University of Rochester School of Nursing continued well-established practices that bookend the school’s academic calendar, albeit in a different format.
When the COVID-19 virus necessitated physical distancing in the midst of the spring semester, the UR School of Nursing, like many institutions, wrestled with how to deal with traditionally in-person academic events. The school not only developed new approaches to handle its graduation and pinning ceremonies (see pages 22-23), but it also retained its year-end award event to honor faculty and staff and launched the 2020-21 academic year with a virtual conovcation ceremony.
Previous convocations featured a packed auditorium with students eager to begin their nursing education. This year, a recordhigh student body of nearly 800 watched the event remotely.
The ceremony began with welcoming remarks from University President Sarah Mangelsdorf, Medical Center CEO Mark B. Taubman, MD, and UR School of Nursing Dean Kathy Rideout, EdD, PPCNP-BC, FNAP. Five UR Nursing students were recognized for their academic achievements in six categories, including:
Clare Dennison Prize
Jassel Glanville, an Accelerated Bachelor’s Program for
Non-Nurses student, was honored for her outstanding proficiency in general nursing care.
Eleanor Hall Award with the Support of the Class of 1965 in Honor of Elsje Planje Higgins
Linzie Marie France, a student in the Family Nurse Practitioner program, demonstrated the ability to work with others, to inspire and listen, and to be a leader with integrity.
Michele Unger Leadership Award and Student Diversity Engagement Award
Lavern Sleigh-Sharpe, a student in the Health Care
Management and Leadership program, received two awards for her ability to establish collaborative relationships with physicians, leaders and staff, and for her commitment to diversity and inclusion.
George Spencer Terry Jr. B’49 Endowed Fund in Nursing
Michele Baker, a Doctor of Nursing Practice student, was honored for being engaged in developing innovative solutions to challenges facing nurses, health care providers, and patients.
Loretta C. Ford Fellowship
Shelby Przybylek, a full-time student in the PhD program, was recognized for demonstrating the highest potential for academic and professional success.
Like the convocation ceremony, the year-end award event was held virtually. Normally held in the spring, it was moved to September and paired with Dean Rideout’s State of the School address.
Among this year’s awardees were:
Dean’s Appreciation Award
Greg Thornton, Claude Goff, John Bauer,
Richard Vangrol, Jham Chhetri,
Environmental Services and Facilities team
Sarah Lesniak, MS, RN-BC, CSPHA, nurse educator, URMC
Nancy Resseguie, RN, MS, nurse recruiter, URMC
Josephine Craytor Nursing Faculty Award
Erin Baylor, DNP, RN, PNP-BC, ONP, assistant professor of clinical nursing, director of simulation, specialty director,
PNP program
Natalie Leblanc, PhD, MPH, RN, BSN, assistant professor, Harriet J. Kitzman Fellow in Health Disparities
Drs. Jeremy A. Klainer and Pamela York Klainer Endowed Dean’s Discretionary Award in Nursing
Joseph Gomulak-Cavicchio, EdD, MSEd;
Tara Serwetnyk, MS, RN, NPD-BC; Kaitlyn Burke, MS,
RN, CCRN, CNE-cl; Nadine Taylor, instructional design team
Outstanding Scholarly Practitioner
Susan Blaakman, PhD, RN, NPP-BC, professor of clinical nursing, director of FPMHNP program
Outstanding Faculty Colleague
Erin Baylor, DNP, RN, PNP-BC, ONP, assistant professor of clinical nursing, director of simulation, specialty director,
PNP program
Mary Dombeck Diversity Enhancement Faculty Award
Mitchell J. Wharton, PhD, RN, FNP-BC, CNS, assistant professor of clinical nursing, faculty diversity officer
Most Promising New Investigator
Natalie Leblanc, PhD, MPH, RN, BSN, assistant professor, Harriet J. Kitzman Fellow in Health Disparities
Professional Advancement Award
Susan Groth, PhD, WHNP-BC, FAANP,
associate professor
Mary Dombeck Diversity Enhancement Staff Award
Helen Arditi, senior software engineer
Outstanding Staff Colleague
Lindsay Kimmerly, staff accountant Outstanding Staff Member of the Year
Patrick Broadwater, senior PR associate, director of strategic communications
NEWS Hyekyun Rhee Named to Strategic Planning Group Advising NINR Leadership
Hyekyun Rhee, PhD, RN, PNP, FAAN, is among a small working group of nurse scientists advising National Institute for Nursing Research (NINR) leadership on its next strategic plan.
This past summer, Rhee, the Endowed Chair of Nursing Science at the University of Rochester School of Nursing, was one of 22 researchers from across the country invited to participate in the process of advising NINR leadership and providing recommendations that will help to identify strengths, limitations, challenges, and opportunities to help determine the future course of federally supported nursing science.
“This is an incredible recognition of the respect for Hyekyun’s work and the role she can play in shaping nursing science for the future,” said Dean Kathy Rideout, EdD, PPCNP-BC, FNAP.
The working group was established under the auspices of the National Advisory Council for Nursing Research, the advisory council to NINR. Group members were chosen as experts in areas of interest central to NINR’s mission. The NINR’s current strategic plan, Advancing Science, Improving Lives: A Vision for Nursing Science, was released in 2016.
Over the past decade, Rhee has established an internationally recognized program of research developing innovative approaches to asthma self-management using technology and peer dynamics to improve asthma outcomes in adolescents. Using these approaches, she developed an award-winning wearable device that monitors symptoms around the clock and can be analyzed for patterns of symptom frequency throughout the day, guiding medication or behavioral adjustments.
Rhee earned her PhD in nursing at the University of North Carolina – Chapel Hill, and joined the UR School of Nursing faculty in 2007.

Tantillo Book Examines Role of Relationships in Eating Disorder Recovery
While there is much more to uncover about eating disorders, considerable progress has been made in understanding how crucial relationships are to treatment and recovery.
In her new book, Multifamily Therapy Group for Young Adults with Anorexia Nervosa: Reconnecting for Recovery, Professor of Clinical Nursing Mary Tantillo, PhD, PMHCNS-BC, FAED, CGP, examines recovery under a relational lens.
Through clinical observations of young adults suffering from anorexia nervosa and their families, Tantillo and her co-researchers developed a family-centered outpatient group therapy called Reconnecting for Recovery (R4R). The new R4R approach is designed to help young adults and their family members learn the emotional and relational skills required to continue collaboration in recovery.
Intended for providers, patients, and their family members, the book acts as a treatment manual that provides a deeper understanding of the nature, purpose, and process that characterizes R4R. It is a product of Tantillo’s extensive expertise in clinical work and research related to the treatment of eating disorders. For over 30 years, she has provided care and support to patients and families coping with eating disorders across a spectrum of clinical settings.
Tantillo is the director of the Western New York Comprehensive Care Center for Eating Disorders, directed out of the UR School of Nursing, that coordinates eating disorder services in the 30-county Western New York region. She is also the founder and former CEO of The Healing Connection, Inc., a non-profit eating disorder partial hospitalization program for adults and adolescents, and a fellow and former board member of the Academy for Eating Disorders.
Multifamily Therapy Group for Young Adults with Anorexia Nervosa: Reconnecting for Recovery is available for purchase on Amazon. The book’s co-authors include Jennifer Sanftner McGraw, PhD, and Daniel Le Grange, PhD.

NEWS $4.6M Award Extends School’s Deep-Rooted Research on Nurse-Family Partnership
The University of Rochester School of Nursing will receive $4.6 million over the next four years, continuing its three-decade association with the Nurse-Family Partnership.
The UR Nursing award is a sub-grant of a $6.7 million National Institutes of Health study titled "Influence of Prenatal and Early Childhood Home Visiting by Nurses on Development of Chronic Disease: 29-Year Follow-Up of a Randomized Clinical Trial." The latest collaboration between the UR School of Nursing and David Olds of the University of Colorado, the study consists of a follow-up evaluation of participants in the Memphis New Mother’s Study, which was the foundation for the creation of the Nurse-Family Partnership (NFP), a program of prenatal and infancy home visiting by nurses for low-income mothers and their children.
The UR Nursing team, led by Associate Professor Susan Groth, PhD, WHNP-BC, FAANP, oversees the Memphis site and the study’s data collection and data management processes. Mary Carey, PhD, RN, FAHA, FAAN, an associate professor at the School of Nursing, is a co-investigator on the study. Previous studies of NFP participants have supported the hypothesis that early nurse-led interventions lead to reductions in the emergence of cardiovascular disease, type-2 diabetes, and premature mortality among both mothers and their first-born offspring.
The project continues the powerful legacy of Harriet Kitzman, PhD, RN, FAAN, whose work over several decades with young, socioeconomically disadvantaged mothers and children was instrumental in the development and ongoing funding of the NFP. Kitzman herself was the lead principal investigator on at least 14 studies from 1992 through the 2010s, and co-investigator on dozens more, attracting millions of dollars in funding to the school.
The Nurse-Family Partnership, an evidence-based community health program with more than 40 years of evidence showing improvements in the lives of first-time moms and their children living in poverty, was federally funded in 1996 and since then has served more than 330,000 families across 40 states. NFP nurses are charged with improving pregnancy outcomes, children’s health and development, and women’s health and economic self-sufficiency with the goal of reducing health disparities over the lifespan.

Kitzman

Groth
$1.2M HRSA Grant Expands Nurse Practitioner Residency Program
A $1.2 million grant from the Health Resources and Services Administration (HRSA), an agency of the U.S. Department of Health and Human Services, will help expand the Nurse Practitioner (NP) Residency program that is integrated into the University of Rochester/Highland Hospital Family Medicine Residency Program. Funding of $400,000 each year for three years will be used to expand the NP residency program from two residents per year to four residents per year, with a rural medicine component.
The Highland Family Medicine (HFM) Nurse Practitioner Residency program was developed in 2016 as a collaboration between HFM and the UR School of Nursing. It is the first program of its kind in New York state, where residents from all disciplines train together to create an inter-professional collaborative learning environment.
“We are very excited about this opportunity to expand our program and help provide more health care in rural communities,” said director of the program Kristin E. Smith, DNP, FNP-C, AAHIVS.
The HFM clinic is the third oldest physician residency program in the country, internationally recognized for leadership and innovation in the integration of behavioral health into primary care practice. These qualities were instilled into the NP residency program from its inception, leading it to receive accreditation by the National Nurse Practitioner Residency and Fellowship Consortium (NNPRFTC).
Scholarly Publications
The following is a listing of research findings published by School of Nursing faculty from June 2019 to September 2020.
Danielle C. Alcena-Stiner, PhD, RN
Zhang, C., McMahon, J., Leblanc, N., Braksmajer, A., Crean, H.F., & Alcena-Stiner, D. (2020). Association of medical mistrust and poor communication with HIV-related health outcomes and psychosocial wellbeing among heterosexual men living with HIV. AIDS Patient Care and STDs, 34, 27-37.
Elizabeth A. Anson, MS
Olds, D.L., Kitzman, H., Anson, B., Smith, J.A., Knudtson, M.D., Miller, T., Cole, R., Hopfer, C., & Conti, G. (2019). Prenatal and infancy nurse home visiting effects on mothers: 18-Year follow-up of a randomized trial. Pediatrics, 144, e20183889.
Kitzman, H., Olds, D.L., Knudtson, M.D., Cole, R., Anson, E., Smith, J.A., Fishbein, D., DiClemente, R., Wingood, G., Caliendo, A.M., Hopfer, C., Miller, T., & Conti, G. (2019). Prenatal and infancy nurse home visiting and 18-Year outcomes of a randomized trial. Pediatrics, 144, e20183889.
Mary G. Carey, PhD, RN, FAHA, FAAN
Wagner, S.L., White, N., Fyfe, T., Matthews, L.R., Randall, C., Regehr, C., White, M., Alden, L.E., Buys, N., Carey, M.G., Corneil, W., Fraess-Phillips, A., Krutop, E., & Fleischmann, M.H. (2020). Systematic review of posttraumatic stress disorder in police officers following routine work-related critical incident exposure. American Journal of Industrial Medicine, 63, 600-615.
Dzikowicz, D.J., & Carey, M.G. (2020). Exercise-induced premature ventricular contractions are associated with myocardial ischemia among asymptomatic adult male firefighters: Implications for enhanced risk stratification. Biological Research for Nursing, 22, 369-377.
Dzikowicz, D.J. & Carey, M.G. (2020). An incidental finding on a preprocedural electrocardiogram. JNP- Journal for Nurse Practitioners, 16, E49-E52. Dzikowicz, D.J., & Carey, M.G. (2019). Obesity and hypertension contribute to prolong QRS complex duration among middle-aged adults. Annals of Noninvasive Electrocardiology, 24, e12665.
Carey, M.G., Al-Zaiti, S.S., Kozik, T.M., & Pelter, M.M. (2019). Important electrocardiographic changes in the absence of positive cardiac biomarkers. American Journal of Critical Care, 28, 325-326.
Fearrington, M.A., Qualls, B.W., & Carey, M.G. (2019). Essential oils to reduce postoperative nausea and vomiting. Journal of Perianesthesia Nursing, 34, 1047-1053.
Carey, M.G., Trout, D.R., & Qualls, B.W. (2019). Hospital-based research internship for nurses: The value of academic librarians as co-faculty. Journal for Nurses in Professional Development, 35, 344-350.
Carey, M.G., Nowzari, S., & Finnell, D.S. (2019). Brief video intervention to teach firefighters the neurobiological basis of high risk alcohol use: A pilot study. Archives of Psychiatric Nursing, 33, 377-382.
Hugh F. Crean, PhD
Zhang, C., McMahon, J., Leblanc, N., Braksmajer, A., Crean, H.F., & Alcena-Stiner, D. (2020). Association of medical mistrust and poor communication with HIV-related health outcomes and psychosocial wellbeing among heterosexual men living with HIV. AIDS Patient Care and STDs, 34, 27-37.
Braksmajer, A., Walters, S.M., Crean, H.F., Stephenson, R., & McMahon, J.M. (2020). Pre-exposure prophylaxis use among men who have sex with men experiencing partner violence. AIDS and Behavior, 24, 2299-2306.
Arcoleo, K.J., McGovern, C., Kaur, K., Halterman, J.S., Mammen, J., Crean, H., Rastogi, D., & Feldman, J.M. (2019). Longitudinal patterns of Mexican and Puerto Rican children's asthma controller medication adherence and acute healthcare utilization. Annals of the American Thoracic Society, 16, 715-723.
Bishop, T.M., Crean, H.F., Hoff, R.A., & Pigeon, W.R. (2019). Suicidal ideation among recently returned veterans and its relationship to insomnia and depression. Psychiatry Research, 276, 250-261.
Li, Y.I., Cerulli, C., Heffner, K.L., Crean, H.F., Bishop, T.M., & Pigeon, W.R. (2019). Cognitive-Behavioral Therapy for insomnia in PTSD: Differential relationships with symptom clusters. Sleep, 42, A354.
Pigeon, W.R., Funderburk, J., Cross, W.F., Bishop, T.M., & Crean, H.F. (2019). Brief CBT for insomnia delivered in primary care to patients endorsing suicidal ideation: A proof-of-concept randomized clinical trial. Translational Behavioral Medicine, 9, 1169-1177.
Poleshuck, E., Wittink, M., Crean, H.F., Juskiewicz, I., Bell, E., Harrington, A., & Cerulli, C. (2019). A comparative effectiveness trial of two patient-centered interventions for women with unmet social needs: Personalized Support for Progress (PSP) and Enhanced Screening and Referral (ESR). Journal of Women’s Health, 29, 242-252.
Marie A. Flannery, PhD, RN, AOCN
Loh, K.P., Mohile, S.G., & Flannery, M. (2020). Electronic symptom monitoring: Not everyone fits the mold. Annals of Oncology, 31, 13-14.
Loh, K.P., Kleckner, I.R., Lin, P.J., Mohile, S.G., Canin, B.E., Flannery, M.A., … & Mustian, K.M. (2019). Effects of a home-based exercise program on anxiety and mood disturbances in older adults with cancer receiving chemotherapy. Journal of the American Geriatrics Society, 67, 1005-1011.
Loh, K.P., Mohile, S.G., Epstein, R.M., McHugh, C., Flannery, M., Culakova, E., Lei, L., … & Duberstein, P.R. (2019). Willingness to bear adversity and beliefs about the curability of advanced cancer in older adults. Cancer, 125, 2506-2513.
Susan W. Groth, PhD, WHNP-BC, FAANP
Yu, Y., Burke, L.E., Shen, Q.W., Imes, C.C., Sun, R., Groth, S., Zhang, W., & Kalarchian, M.A. (2020). A qualitative exploration of patients' experiences with lifestyle changes after sleeve gastrectomy in China. Obesity Surgery, 30, 3127-3134.
Groth, S.W. (2020). Pregnancy weight: What happens after childbirth matters. Journal of Women's Health, 29, 471-472.
Rhee, H., Love, T., Groth, S.W., Grape, A., Tumiel-Berhalter, L., & Harrington, D. (2019). Associations between overweight and obesity and asthma outcomes in urban adolescents. The Journal of Asthma, 57, 1053-1062.
Kathi L. Heffner, PhD
Li, Y.I., Cerulli, C., Heffner, K.L., Crean, H.F., Bishop, T.M., & Pigeon, W.R. (2019). Cognitive-Behavioral Therapy for insomnia in PTSD: Differential relationships with symptom clusters. Sleep, 42, A354.
Wang, X., Heffner, K.L., Anthony, M., & Lin, F. (2019). Stress adaptation in older adults with and without cognitive impairment: An fMRI pattern-based similarity analysis. Aging, 11, 6792-6804.
Lin, F.V., Tao, Y., Chen, Q.J., Anthony, M., Zhang, Z.W., Tadin, D., & Heffner, K.L.. (2020). Processing speed and attention training modifies autonomic flexibility: A mechanistic intervention study. Neuroimage, 213, 116730.
Harriet J. Kitzman, PhD, RN, FAAN Olds, D.L., Kitzman, H., Anson, B., Smith, J.A., Knudtson, M.D., Miller, T., Cole, R., Hopfer, C., & Conti, G. (2019). Prenatal and infancy nurse home visiting effects on mothers: 18-Year follow-up of a randomized trial. Pediatrics, 144, e20183889.
Kitzman, H., Olds, D.L., Knudtson, M.D., Cole, R., Anson, E., Smith, J.A., Fishbein, D., DiClemente, R., Wingood, G., Caliendo, A.M., Hopfer, C., Miller, T., & Conti, G. (2019). Prenatal and infancy nurse home visiting and 18-Year outcomes of a randomized trial. Pediatrics, 144, e20183889.
Natalie M. Leblanc, PhD, MPH, RN, BSN
Zhang, C., McMahon, J., Leblanc, N., Braksmajer, A., Crean, H.F., & Alcena-Stiner, D. (2020). Association of medical mistrust and poor communication with HIV-related health outcomes and psychosocial wellbeing among heterosexual men living with HIV. AIDS Patient Care and STDs, 34, 27-37.
Harris, O.O., Leblanc, N., McGee, K., Randolph, S., Wharton, M.J., & Relf, M. (2020). Alarm at the gate: Health and social inequalities are comorbid conditions of HIV and COVID-19. Journal of the Association of Nurses in AIDS Care, 31, 367-375.
Braksmajer, A., McMahon, J.M., Leblanc, N., & Urban, M.A. (2019). Feasibility and acceptability of pre-exposure prophylaxis use among women in violent relationships. AIDS Care: Psychological and Socio-Medical Aspects of AIDS/HIV, 31, 475-480.
Zhang, C., McMahon, J., Fiscella, K., Przybyla, S., Braksmajer, A., Leblanc, N., & Liu, Y. (2019). HIV pre-exposure prophylaxis implemen-
tation cascade among health care professionals in the United States: Implications from a systematic review and meta-analysis. AIDS Patient Care and STDs, 33, 507-527.
Ogunbajo, A., Leblanc, N.M., Kushwaha, S., Boakye, F., Hanson, S., Smith, M.D.R., & Nelson, L.E. (2019). Knowledge and acceptability of HIV pre-exposure prophylaxis (PrEP) among men who have sex with men (MSM) in Ghana. AIDS Care-Psychological and Socio-Medical Aspects of AIDS/HIV, 32, 330-336.
McMahon, J.M., Braksmajer, A., Zhang, C., Leblanc, N., Chen, M., Aidala, A., & Simmons, J. (2019). Syndemic factors associated with adherence to antiretroviral therapy among HIV-positive adult heterosexual men. AIDS Research and Therapy, 16, 32.
F. Vankee Lin, PhD, RN
Wang, X., Heffner, K.L., Anthony, M., & Lin, F. (2019). Stress adaptation in older adults with and without cognitive impairment: An fMRI pattern-based similarity analysis. Aging, 11, 6792-6804.
Lin, F.V., Tao, Y., Chen, Q.J., Anthony, M., Zhang, Z.W., Tadin, D., & Heffner, K.L.. (2020). Processing speed and attention training modifies autonomic flexibility: A mechanistic intervention study. Neuroimage, 213, 116730.
Magnuson, A., Lei, L., Gilmore, N., Kleckner, A.S., Lin, F.V., Ferguson, R., Hurria, A., Wittink, M.N., Esparaz, B.T., Giguere, J.K., Misleh, J., Bautista, J., Mohile, S.G., & Janelsins, M.C. (2019). Longitudinal relationship between frailty and cognition in patients 50 years and older with breast cancer. Journal of the American Geriatrics Society, 67, 928-936.
Anderson, A.J. & Lin, F. (2019). How pattern information analyses of semantic brain activity elicited in language comprehension could contribute to the early identification of Alzheimer's disease. NeuroImage: Clinical, 22, 101788.
Yu, F., Mathiason, M., & Lin, F. (2019). Cognitive and physical factors affecting daily function in Alzheimer's disease: A cross-sectional analysis. Nursing Health and Sciences, 21, 14-20.
Anderson, A.J., Ren, P., Baran, T.M., Zhang, Z.W., & Lin, F. (2019). Insula and putamen centered functional connectivity networks reflect healthy agers' subjective experience of cognitive fatigue in multiple tasks. Cortex, 119, 428-440. Ren, P., Anderson, A.J., McDermott, K., Baran, T.M., & Lin, F. (2019). Cognitive fatigue and cortical-striatal network in old age. Aging, 11, 2312-2326.
James M. McMahon, PhD
Zhang, C., McMahon, J., Leblanc, N., Braksmajer, A., Crean, H.F., & Alcena-Stiner, D. (2020). Association of medical mistrust and poor communication with HIV-related health outcomes and psychosocial wellbeing among heterosexual men living with HIV. AIDS Patient Care and STDs, 34, 27-37.
Braksmajer, A., Walters, S.M., Crean, H.F., Stephenson, R., & McMahon, J.M. (2020). Pre-exposure prophylaxis use among men who have sex with men experiencing partner violence. AIDS and Behavior, 24, 2299-2306.
Braksmajer, A., McMahon, J.M., Leblanc, N., & Urban, M.A. (2019). Feasibility and acceptability of pre-exposure prophylaxis use among women in violent relationships. AIDS Care: Psychological and Socio-Medical Aspects of AIDS/ HIV, 31, 475-480.
Zhang, C., McMahon, J., Fiscella, K., Przybyla, S., Braksmajer, A., Leblanc, N., & Liu, Y. (2019). HIV pre-exposure prophylaxis implementation cascade among health care professionals in the United States: Implications from a systematic review and meta-analysis. AIDS Patient Care and STDs, 33, 507-527.
McMahon, J.M., Braksmajer, A., Zhang, C., Leblanc, N., Chen, M., Aidala, A., & Simmons, J. (2019). Syndemic factors associated with adherence to antiretroviral therapy among HIV-positive adult heterosexual men. AIDS Research and Therapy, 16, 32.
Braksmajer, A., Zhang, C., & McMahon, J.M. (2020). Associations between relationship power and pre-exposure prophylaxis (PrEP) use among men who have sex with men. AIDS and Behavior, 24, 1358-1364.
Trabold, N., McMahon, J., Alsobrooks, S., Whitney, S., & Mittal, M. (2020). A systematic review of intimate partner violence interventions: State of the field and implications for practitioners. Trauma Violence & Abuse, 21, 311-325.
Zhang, C., McMahon, J., Simmons, J., Brown, L.L., Nash, R., & Liu, Y. (2019). Suboptimal HIV pre-exposure prophylaxis awareness and willingness to use among women who use drugs in the United States: A systematic review and meta-analysis. AIDS and Behavior, 23, 2641-2653.
Ying Meng, PhD, RN, ACNP
Meng, Y., Wu, T., Billings, R., Kopycka-Kedzierawski, D.T., & Xiao, J. (2019). Human genes influence the interaction between Streptococcus mutans and host caries susceptibility: A genome-wide association study in children with primary dentition. International Journal of Oral Science, 11, 19.
Sally A. Norton, PhD, RN, FNAP, FPCN, FAAN
Duberstein, P.R., Chen, M., Hoerger, M., Epstein, R.M., Perry, L.M., Yilmaz, S., Saeed, F., Mohile, S.G., & Norton, S. (2020). Conceptualizing and counting discretionary utilization in the final 100 days of life: A scoping review. Journal of Pain and Symptom Management, 59, 894-915.
Ingersoll, L.T., Alexander, S.C., Ladwig, S., Anderson, W., Norton, S.A., & Gramling, R. (2019). The contagion of optimism: The relationship between patient optimism and palliative care clinician overestimation of survival among hospitalized patients with advanced cancer. Psycho-oncology, 28, 1286-1292.
Duberstein, P.R., Maciejewski, P.K., Epstein, R.M., Fenton, J.J., Chapman, B., Norton, S.A., Hoerger, M., Wittink, M.N., Tancredi, D.J., Zing, G., Mohile, S., Kravitz, R.L., & Prigerson, H.G. (2019). Effects of the values and options in cancer care communication intervention on personal caregiver experiences of cancer care and bereavement outcomes. Journal of Palliative Medicine, 22, 1394-1400.
Tobie H. Olsan, PhD, RN, CNL, FNAP
Oh, J.H., Shelly, M., Nersinger, S., Cai, X.Y., & Olsan, T. (2020). Implementing clinical practice guidelines for replacing peripheral intravenous catheters. Journal of Nursing Care Quality, 35, 108-114.
Temkin-Greener, H., Szydlowski, J., Intrator, O., Olsan, T., Karuza, J., Cai, X., Gao, S., & Gillespie, S.M. (2019). Perceived effectiveness of home-based primary care teams in veterans health administration. The Gerontologist, 60, 494-502.
Dang, S., Olsan, T., Karuza, J., Cai, X., Gao, S., Intrator, O., Li, J., & Gillespie, S.M. (2019). Telehealth in home-based primary care: Factors and challenges associated with integration into veteran care. Journal of the American Geriatrics Society, 67, 1928-1933. Haverhals, L.M., Manheim, C., Gilman, C., Karuza, J., Olsan, T., Edwards, S.T., Levy, C.R., & Gillespie, S. (2019). Dedicated to the mission: Strategies US Department of Veterans Affairs home-based primary care teams apply to keep veterans at home. Journal of the American Geriatrics Society, 67, 2511-2518.
Hyekyun Rhee, PhD, RN, PNP, FAAN
Rhee, H., Love, T., Groth, S.W., Grape, A., Tumiel-Berhalter, L., & Harrington, D. (2019). Associations between overweight and obesity and asthma outcomes in urban adolescents. The Journal of Asthma, 57, 1053-1062.
Rhee, H., Grape, A., Tumiel-Berhalter, L., Wicks, M., Sloand, E., & Butz, A. (2020). Fidelity of a peer-led asthma self-management intervention and its attention control in a multisite study of urban adolescents. Research in Nursing and Health, 43, 195-205.
Sloand, E., Butz, A., Rhee, H., Walters, L., Breuninger, K., Pozzo, R.A., Barnes, C.M., Wicks, M.N., & Tumiel-Berhalter, L. (2019). Influence of social support on asthma self-management in adolescents. Journal of Asthma, 4, 1-9.
Rhee, H., Love, T., Harrington, D., & Walters, L. (2019). Long-term effects of a peer-led asthma self-management program for adolescents on peer leaders' healthcare utilization. European Respiratory Journal, 54, PA930.
Kathy H. Rideout, EdD, PPCNPBC, FNAP
McCauley, L., Broome, M.E., Frazier, L., Hayes, R., Kurth, A., Musil, C.M., Norman, L.D., Rideout, K.H., & Villarruel, A.M. (2020). Doctor of nursing practice (DNP) degree in the US: Reflecting, readjusting, and getting back on track. Nursing Outlook, 68, 494-503.
Joyce A. Smith, PhD, RN, ANP
Olds, D.L., Kitzman, H., Anson, B., Smith, J.A., Knudtson, M.D., Miller, T., Cole, R., Hopfer, C., & Conti, G. (2019). Prenatal and infancy nurse home visiting effects on mothers: 18-Year follow-up of a randomized trial. Pediatrics, 144, e20183889.
Kitzman, H., Olds, D.L., Knudtson, M.D., Cole, R., Anson, E., Smith, J.A., Fishbein, D., DiClemente, R., Wingood, G., Caliendo, A.M., Hopfer, C., Miller, T., & Conti, G. (2019). Prenatal and infancy nurse home visiting and 18-Year outcomes of a randomized trial. Pediatrics, 144, e20183889.
Karen F. Stein, PhD, RN, FAAN
Stein, K.F., Trabold, N., & Connelly, K. (2019). Unhealthy weight control strategies: An outcome of body image and eating tensions in women of Mexican origin living in rural farming communities. Journal of Health Psychology, 24, 1293-1304.
Stein, K.F., Lee, C.K., Corte, C., & Steffen, A. (2019). The influence of identity on the prevalence and persistence of disordered eating and weight control behaviors in Mexican American college women. Appetite, 140, 180-189.
Lee, C.K., Corte, C., Stein, K.F., Feng, J.Y., & Liao, L.L. (2020). Alcohol-related cognitive mechanisms underlying adolescent alcohol use and alcohol problems: Outcome expectancy, self-schema, and self-efficacy. Addictive Behaviors, 105, 106349.
Mary Tantillo, PhD, PMHCNS-BC, FAED, CGP
Tantillo, M., Starr, T., & Kreipe, R. (2019). The recruitment and acceptability of a Project ECHO(R) eating disorders clinic: A pilot study of telementoring for primary medical and behavioral health care practitioners. Eating Disorders, 28, 230-255.
Megan L. Underhill-Blazey, PhD, APRN, AOCNS
Jabaley, T., Underhill-Blazey, M.L., & Berry, D.L. (2019). Development and testing of a decision aid for unaffected women with a BRCA1 or BRCA2 mutation. Journal of Cancer Education, 35, 339-344.
Berry, D.L., Hong, F., Halpenny, B., Sanda, M., Master, V.A., Filson, C.P., Chang, P., Chien, G.W., Underhill, M., Fox, E., McReynolds, J. & Wolpin, S. (2019). Evaluating clinical implementation approaches for prostate cancer decision support. Urology Practice, 6, 93-99.
Underhill, M., Stopfer, J., Chittenden, A., Nayak, M.M., Lansang, K., Lederman, R., Garber, J., & Gundersen, D.A. (2019). Development and testing of the KnowGene scale to assess general cancer genetic knowledge related to multigene panel testing. Patient Education and Counseling, 102, 1558-1564.
Underhill-Blazey, M., Blonquist, T., Lawrence, J., Hong, F., Yurgelun, M.B., & Syngal, S. (2019). Health behaviours and beliefs in individuals with familial pancreatic cancer. Familial Cancer, 18, 457-464. Underhill, M.L., Pozzar, R., Chung, D., Sawhney, M., & Yurgelun, M. (2020). Health care provider perceptions of caring for individuals with inherited pancreatic cancer risk. Journal of Cancer Education, 35, 194-203.
Jinjiao J. Wang, PhD, RN
Simning, A., Orth, J., Wang, J.J., Caprio, T.V., Li ,Y., & Temkin-Greener, H. (2020). Skilled nursing facility patients discharged to home health agency services spend more days at home. Journal of the American Geriatrics Society, 88, 1573-1578.
Wang, J.J., Caprio, T.V., Simning, A., Shang, J.J., Conwell, Y., Yu, F., & Li, Y. (2020). Association between home health services and facility admission in older adults with and without Alzheimer's disease. Journal of the American Medical Directors Association, 21, 627-633.
Wang, J.J., Kong, D.X., Sun, B.C., & Dong, X.Q. (2020). Health services utilization among Chinese American older adults: Moderation of social support with functional limitation. Journal of Applied Gerontology, 39, 481-489.
Wang, J., Maxwell, C.A., & Fang, Y. (2019). Biological processes and biomarkers related to frailty in older adults: A state-of-the-science literature review. SAGE Journals, 21, 80-106.
Mitchell J. Wharton, PhD, RN, FNP-BC, CNS
Harris, O.O., Leblanc, N., McGee, K., Randolph, S., Wharton, M.J., & Relf, M. (2020). Alarm at the gate: Health and social inequalities are comorbid conditions of HIV and COVID-19. Journal of the Association of Nurses in AIDS Care, 31, 367-375.
Yang Yu, PhDc, MPHc, MSN
Yu, Y., Burke, L.E., Shen, Q.W., Imes, C.C., Sun, R., Groth, S., Zhang, W., & Kalarchian, M.A. (2020). A qualitative exploration of patients' experiences with lifestyle changes after sleeve gastrectomy in China. Obesity Surgery, 30, 3127-3134.
Chen Zhang, PhD, MPH
Zhang, C., McMahon, J., Leblanc, N., Braksmajer, A., Crean, H.F., & Alcena-Stiner, D. (2020). Association of medical mistrust and poor communication with HIV-related health outcomes and psychosocial wellbeing among heterosexual men living with HIV. AIDS Patient Care and STDs, 34, 27-37.
Zhang, C., McMahon, J., Fiscella, K., Przybyla, S., Braksmajer, A., Leblanc, N., & Liu, Y. (2019). HIV pre-exposure prophylaxis implementation cascade among health care professionals in the United States: Implications from a systematic review and meta-analysis. AIDS Patient Care and STDs, 33, 507-527.
McMahon, J.M., Braksmajer, A., Zhang, C., Leblanc, N., Chen, M., Aidala, A., & Simmons, J. (2019). Syndemic factors associated with adherence to antiretroviral therapy among HIV-positive adult heterosexual men. AIDS Research and Therapy, 16, 32.
Braksmajer, A., Zhang, C., & McMahon, J.M. (2020). Associations between relationship power and pre-exposure prophylaxis (PrEP) use among men who have sex with men. AIDS and Behavior, 24, 1358-1364.
Zhang, C., McMahon, J., Simmons, J., Brown, L.L., Nash, R., & Liu, Y. (2019). Suboptimal HIV pre-exposure prophylaxis awareness and willingness to use among women who use drugs in the United States: A systematic review and meta-analysis. AIDS and Behavior, 23, 2641-2653.
Zhang, C., Qian, H., Liu, Y., & Vermund, S. (2019). Voluntary medical male circumcision and HIV infection among men who have sex with men: Implications from a systematic review. Sage Open Medicine, 7, 2050312119869110.
Zhang, C., Penson, D.F., Qian, H.Z., Webb, G.F., Lou, J., Shepherd, B.E., Liu, Y., Vermund, S.H. (2019). Modeling economic and epidemiological impact of voluntary medical male circumcision among men who have sex with men in Beijing, China. International Journal of STD & AIDS, 30, 630-638.
Zhang, C., Webb, G.F., Lou, J., Shepherd, B.E., Qian, H.Z., Liu, Y., & Vermund, S.H. (2019). Predicting the long-term impact of voluntary medical male circumcision on HIV incidence among men who have sex with men in Beijing, China. AIDS Care-Psychological and Socio-Medical Aspects of AIDS/HIV, 32, 343-353.
Chi, P.L., Zhao, S., Zhang, C., Li, X.M., Guo, Y., Lin, X.Y., & Du, H.F.. (2019). Effects of psychosocial interventions on children affected by parental HIV/AIDS: A meta-analysis on depression and anxiety. BMC Public Health, 19, 1572.
Scholarly Presentations
The following is a listing of presentations by School of Nursing faculty at symposiums, conferences, and meetings from June 2019 to September 2020.
Kaitlyn Burke, MS, RN, CCRN, CNE-cl
Association for the Assessment of Learning in Higher Education Conference. (2019). “Transforming a hybrid health assessment course to an engaged distance learning experience.” St. Paul, MN.
Mary G. Carey, PhD, RN, FAHA, FAAN
ANA-NY Annual Conference. (2020). “Advanced practice providers should interpret 12-lead ECGs.” Virtual.
Margaret A. Carno, PhD, MBA, MJ, RN, CPNP, D,ABSM, FNAP, FAAN
AACN Baccalaureate Conference. (2019). “Trends and emergent solutions for innovation in RN to baccalaureate education.” Orlando, FL.
Susan M. Ciurzynski, PhD, RNBC, PNP, VCE, FNAP
Sigma 45th Biennial Convention and Annual Research Congress. (2019). “Development of a care management curriculum: An academic-practice partner collaboration.” Washington, DC.
Karen K. Davis, PhD, RN, NEA-BC
AACN Doctoral Conference. (2020). “Creating organizational synergy through academic-practice partnerships: Implementation of a DNP Practice Fellow Program.” Naples, FL.
Marie A. Flannery, PhD, RN, AOCN
Council for the Advancement of Nursing Science State of the Science Congress on Nursing Research. (2020). “Patient reported outcome common terminology criteria for adverse events: Free-text symptom responses in older adults.” Virtual.
Irene R. Garrick, PhD, LPC-CT, LMHC-NY, NCC, MBA
World Nursing and Healthcare Congress. (2019). “Dealing with Trauma.” Las Vegas, NV.
Jessica M. Lapinski, MNE, RN
Association for the Assessment of Learning in Higher Education Conference. (2019). “Assessing student knowledge with the use of case studies in clinical post conferences.” St. Paul, MN.
Natalie M. Leblanc, PhD, MPH, RN, BSN
University of Rochester Alumni Lecture. (2020). “The fire this time: Inequalities in the time of COVID-19.” Virtual.
Sigma 45th Biennial Convention and Annual Research Congress. (2019). “Couple-centered HIV prevention and treatment: It’s time for uptake in U.S. health settings.” Washington, DC.
Lisa Norsen, PhD, RN, ACNP-BC
American Public Health Association. (2019). “Reducing cardiovascular disease risk for employees through a comprehensive wellness program.” Philadelphia, PA.
Irena Pesis-Katz, PhD
American Public Health Association. (2019). “Reducing cardiovascular disease risk for employees through a comprehensive wellness program.” Philadelphia, PA.
National Wellness Conference. (2019). “The beat goes on: The comprehensive wellness program that reduces cardiovascular disease risk for employees.” Kissimmee, FL.
Kathy H. Rideout, EdD, PPCNP-BC, FNAP
Rochester Forum. (2019). URSON: Commitment to our community.” Rochester, NY.
Lydia Rotondo, DNP, RN, CNS, FNAP
AACN Doctoral Conference. (2020). “Creating organizational synergy through academic-practice partnerships: Implementation of a DNP Practice Fellow Program.” Naples, FL.
Tara M. Serwetnyk, MS, RN, NPD-BC
Association for the Assessment of Learning in Higher Education Conference. (2019). “Transforming a hybrid health assessment course to an engaged distance learning experience.” St. Paul, MN.
Renu Singh, MS
National Wellness Conference. (2019). “The beat goes on: The comprehensive wellness program that reduces cardiovascular disease risk for employees.” Kissimmee, FL.
Karen F. Stein, PhD, RN, FAAN
Council for the Advancement of Nursing Science State of the Science Congress on Nursing Research. (2020). “State of the science: A review of intuition research in health science.” Virtual.
Andrew Wolf, EdD, MS, RN, ACNP-C
Association for the Assessment of Learning in Higher Education Conference. (2019). “Data-informed curriculum mapping: A four-step approach.” St. Paul, MN. Association for the Assessment of Learning in Higher Education Conference. (2019). “Artificial intelligence to enhance formative assessment of student writing.” St. Paul, MN.
Rebecca R. Wolf, MEd
Association for the Assessment of Learning in Higher Education Conference. (2019). “Data-informed curriculum mapping: A four-step approach.” St. Paul, MN.
Association for the Assessment of Learning in Higher Education Conference. (2019). “Artificial intelligence to enhance formative assessment of student writing.” St. Paul, MN.
Chen Zhang, PhD, MPH
Association in Nurses in AIDS Care. (2019). “Understanding 'Purview Paradox' in the implementation of pre-exposure prophylaxis care in the United States." Portland, OR.
Yingzi Zhang, PhD
Council for the Advancement of Nursing Science State of the Science Congress on Nursing Research. (2020). “Patient reported outcome common terminology criteria for adverse events: Freetext symptom responses in older adults.” Virtual.
Honors and Awards
The following faculty honors were received between June 2019 and September 2020.
Erin S. Baylor, DNP, RN, PNP-BC, ONP
Josephine Craytor Nursing Faculty Award (2020). University of Rochester School of Nursing: Rochester, NY.
Outstanding Faculty Colleague Award (2020). University of Rochester School of Nursing: Rochester, NY.
Susan W. Blaakman, PhD, RN, PMHNP-BC, FNAP
Distinguished Fellow of the National Academies of Practice, Nursing (2020). National Academies of Practice Annual Meeting: San Diego, CA.
Outstanding Scholarly Practitioner Award (2020). University of Rochester School of Nursing: Rochester, NY.
Pamela A. Brady, DNP, RN
Dean’s Excellence in Teaching Award (2020). University of Rochester School of Nursing: Rochester, NY.
Kaitlyn Burke, MS, RN, CCRN, CNE-cl
Drs. Jeremy A. Klainer and Pamela York Klainer Endowed Dean’s Discretionary Award in Nursing (2020). University of Rochester School of Nursing: Rochester, NY.
Mary G. Carey, PhD, RN, FAHA, FAAN RBJ Health Care Heroes Award in Nurse category (2020). Rochester Business Journal: Rochester, NY.
Marianne C. Chiafery, DNP, PNP-BC
Distinguished Service in Health Care Award (2020). Rochester Academy of Medicine: Rochester, NY.
Patricia A. Chiverton, EdD, RN, FNAP
Dean’s Medal (2020). University of Rochester School of Nursing: Rochester, NY.
Loretta C. Ford, EdD, RN, PNP, FAAN, FAANP
Florence Nightingale Award (2019). Center for Nursing at the Foundation of New York State Nurses: Guilderland, NY.
Joseph Gomulak-Cavicchio, EdD, MSEd
Drs. Jeremy A. Klainer and Pamela York Klainer Endowed Dean’s Discretionary Award in Nursing (2020). University of Rochester School of Nursing: Rochester, NY.
Susan W. Groth, PhD, WHNP-BC, FAANP
Professional Advancement Award (2020). University of Rochester School of Nursing: Rochester, NY.
Expert Nurse of the Year (2020). Texas Association of Women’s Health, Obstetric and Neonatal Nurses: Virtual.
Kathi L. Heffner, PhD
Marie C. and Joseph C. Wilson Professorship (2020). University of Rochester: Rochester, NY.
Patrick J. Hopkins, DNP, APRN, C-PNP, NNP
Edward Peck Curtis Award for Excellence in Undergraduate Teaching (2020). University of Rochester: Rochester, NY.
Harriet J. Kitzman, PhD, RN, FAAN
Dean’s Medal (2019). University of Rochester School of Nursing: Rochester, NY.
Rhonda (KC) Knapp-Clevenger, PhD, RN, CPNP, CCRP, FAAN
Distinguished Fellow of the American Academy of Nursing (2019). American Academy of Nursing: Washington, DC.
Natalie M. Leblanc, PhD, MPH, RN, BSN
Josephine Craytor Nursing Faculty Award (2020). University of Rochester School of Nursing: Rochester, NY.
Most Promising New Investigator Award (2020). University of Rochester School of Nursing: Rochester, NY.
Dorothy M. Smith Nursing Leadership Award for Excellence in Diversity (2020). University of Florida School of Nursing: Gainesville, FL.
F. Vankee Lin, PhD, RN
Marie C. and Joseph C. Wilson Professorship (2020). University of Rochester: Rochester, NY.
Lynne Massaro, DNP, RN, FNP-C, ANP-BC, FAANP
Fellow of the American Association of Nurse Practitioners (2019). American Association of Nurse Practitioners Annual Meeting: Indianapolis, IN.
Ying Meng, PhD, RN, ACNP
Early Career Travel Award (2019). Obesity Society: Silver Spring, MD.
Tobie H. Olsan, PhD, RN, CNL, FNAP
Carter & T. Franklin Williams Geriatric Prize Award (2020). Rochester Academy of Medicine: Rochester, NY.
Madeline H. Schmitt Award for Interprofessional Education (2019). Rochester Academy of Medicine: Rochester, NY.
Elizabeth Palermo, DNP, RN, ANP-BC, ACNP-BC
Nurse Practitioner/Physician Assistant Award (2020). Rochester Academy of Medicine: Rochester, NY.
Lydia Rotondo, DNP, RN, CNS, FNAP
Distinguished Fellow of the National Academies of Practice, Nursing (2020). National Academies of Practice Annual Meeting: San Diego, CA.
Tara M. Serwetnyk, MS, RN, NPD-BC
Drs. Jeremy A. Klainer and Pamela York Klainer Endowed Dean’s Discretionary Award in Nursing (2020). University of Rochester School of Nursing: Rochester, NY.
Mitchell J. Wharton, PhD, RN, FNP-BC, CNS
Mary Dombeck Diversity Enhancement Faculty Award (2020). University of Rochester School of Nursing: Rochester, NY.
Ying Xue, DNSc, RN
Loretta C. Ford Endowed Professorship in Primary Care Nursing (2019). University of Rochester School of Nursing: Rochester, NY.






