9 minute read
Innovation Nation
Innovation Nation: Federal funding plays a critical role in empowering researchers at the UIC Retzky College of Pharmacy to tackle biomedical challenges and pursue societal impact.
The U.S. government has long invested in scientific research and development—often, with significant impact to society.
From innovating staples of contemporary life, such as the Internet and GPS, to delivering healthcare advancements like diagnostic tools and novel therapies, investment from the federal government has spurred progress and enhanced lives. The nation’s investment in basic research, in particular, has been critical to laying a foundation for additional inquiry and discoveries benefiting the nation and the world.
In addition, federal funding allows researchers to explore ambitious questions, breeds energizing opportunities for young scientists, and creates new knowledge that fuels understanding and empowers breakthroughs. It is a core ingredient in any research university’s investigative enterprise, including UIC and the Retzky College of Pharmacy.
“It’s rare that any long-term scientific research is done without the involvement of federal research dollars, and that’s especially so in the biomedical space,” says Joanna Burdette, assistant dean for research at the UIC Retzky College of Pharmacy. “No one funds at the level of the federal government, and it's tough to sustain a lively research enterprise without federal funding to support the infrastructure, people, resources, and supplies necessary to carry out ambitious scientific work.”
At UIC, federal funding from the likes of the National Institutes of Health (NIH)—the country’s premier supporter of biomedical research—as well as the Department of Defense’s Congressionally Directed
Medical Research Programs, the National Science Foundation, and the Department of Energy, has spurred a range of compelling, impactful projects over the years.
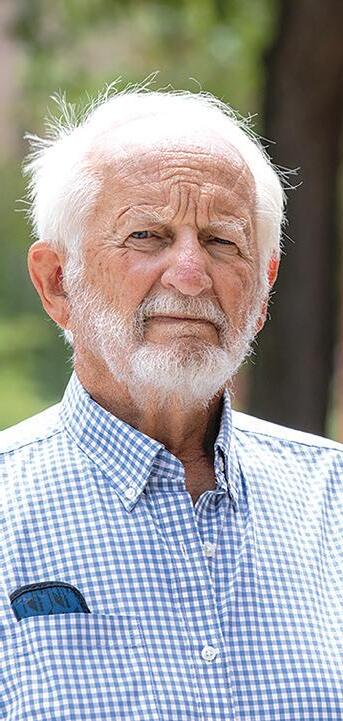
Decades ago, for instance, researchers at the college’s Institute for Tuberculosis Research developed TICE BCG as a vaccine for tuberculosis. It later became a common therapy to treat and prevent certain types of bladder cancer. More recently, Phexxi, has gained widespread use as a Food and Drug Administrationapproved non-hormonal contraceptive agent. Codeveloped by Donald Waller, professor of pharmacology and toxicology, Phexxi is also generating impressive early data as a potential agent to combat sexually transmitted diseases as well.
Today, UIC-based researchers continue their scientific exploration with a high-powered boost from federal agencies. Researchers are examining infectious diseases such as malaria and Ebola, concocting new cancer therapies, uncovering new antibacterial drugs, assessing the therapeutic potential of natural products, creating novel drug delivery methods, and more to advance science and society.
IMPROVING KNOWLEDGE OF DISEASE STATES
In the human body, nitric oxide is an essential cellsignaling molecule. It regulates many physiological responses, such as blood pressure, immune response, and the nervous system. But this short-lived and fastmoving free radical can also have a significant impact on human diseases, reports Douglas Thomas, associate professor of pharmaceutical sciences.

Through its ability to freely diffuse within and between cells and modulate diverse cell-signaling processes, nitric oxide exerts profound and lasting effects on human health and disease, contributing to the pathogenesis of various cancers, cardiovascular disorders, inflammatory conditions, and neurological diseases.
In recent research fueled by funding from the NIH’s National Institute of General Medical Sciences, Thomas and his team discovered an entirely new mechanism of nitric oxide signaling by demonstrating that nitric oxide can regulate gene expression through epigenetic processes, specifically DNA methylation.
“It opens up a new field and paradigm shift in how we view diseases associated with nitric oxide,” Thomas says.
With a stronger understanding of how nitric oxide controls epigenetic programs and influences how a cell functions and contributes to various disease states, Thomas’ team clears an exciting path to explore potential new treatment mechanisms.
“We do the groundwork to understand the molecular mechanisms, so others can take this knowledge and develop targeted therapies to reverse these negative nitric oxide-associated cell states and slow, if not cure, diseases,” he says.
CONSTRUCTING THE FIRST-EVER BIOMOLECULAR ATLAS
Yu Gao’s UIC-based lab is one of the select academic and institutional research groups participating in the groundbreaking Human BioMolecular Atlas Program (HuBMAP). Funded by the NIH Common Fund, HuBMAP aims to build a comprehensive, open atlas of the healthy human body at the cellular level. The work— understanding how the trillions of cells in the adult human body interact, connect, and arrange into tissues— has profound implications for human health, Gao says.
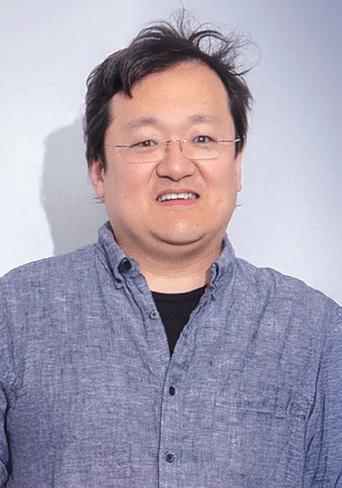
Gao’s lab team became involved with HuBMAP three years ago, teaming with UIC College of Medicine colleague Alexandra Naba to develop the world’s first human extracellular matrix (ECM). A network of molecules surrounding and supporting cells in tissues and organs, ECM has been understudied compared to cells, a trend Gao and his team are actively working to turn with their HuBMAP work.
According to Gao, enhanced knowledge of ECM will improve understanding of countless physiological processes to elevate human health. ECM, for
It’s rare that any longterm scientific research is done without the involvement of federal research dollars, and that’s especially so in the biomedical space.
instance, can provide clues into how cancer tumors migrate, which can help generate therapeutics to prevent or inhibit tumor progression and combat cancer. ECM can also spark more effective ways to address wound healing and tissue regeneration.
“HuBMAP is a cornerstone of future human research,” says Gao, associate professor of pharmaceutical sciences. “It will help us better understand tissue organization and function, which will accelerate biomedical research, stimulate new technologies, deepen knowledge of diseases, and strengthen personalized medicine.”
REDUCING HEALTHCAREASSOCIATED INFECTIONS
In the nation’s hospitals and nursing homes, healthcare-associated infections (HAI) represent an ongoing threat to patient safety and healthcare quality. In hospitals alone, one in 31 patients incur at least one HAI, according to the Centers for Disease Control. These HAIs result in more than 680,000 infections each year, preventable fatalities, billions of dollars in excess costs, and compounded stress to patients and families.
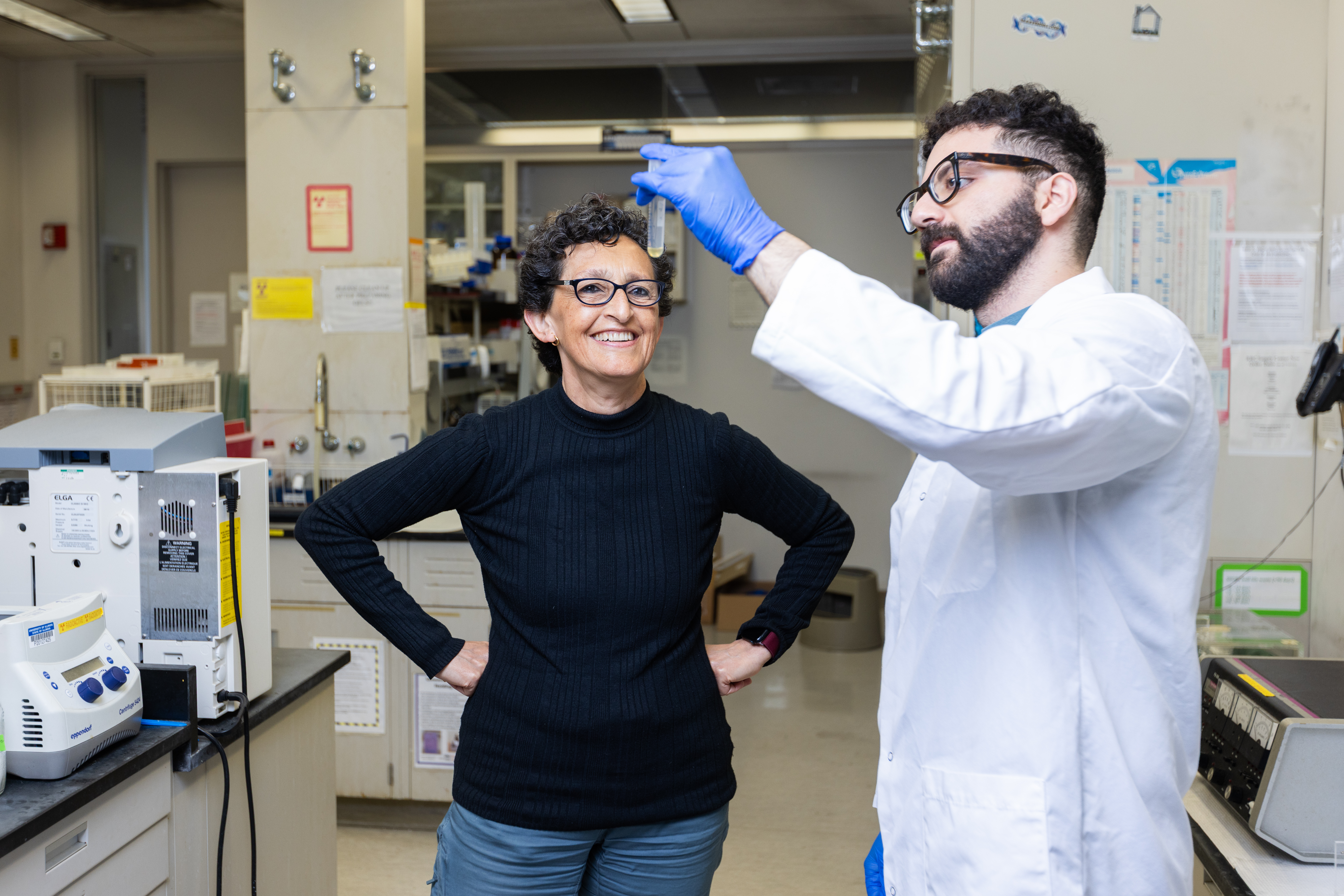
Nancy Freitag, professor and head of the Department of Pharmaceutical Sciences, is battling HAIs with research specifically targeting the mysterious ties between propofol, a commonly used anesthetic, and an increased risk of HAIs.

Powered by a recently concluded two-year grant from the National Institute of Allergy and Infectious Diseases (NIAID), Freitag studied mouse models and discovered even a five-minute sedation period with propofol—an admittedly safe and effective anesthetic—was enough to increase the severity of microbial infection in those already infected or infected within five days of recovery from sedation.
“When confronting hospital-acquired infections, it’s good to know about anything that increases risk of infection to patients,” Freitag says. “If we can understand why these patients are more susceptible to infection when using propofol, then we can then try to counteract the negative effects or issue a different or modified drug without these side effects.”
With her initial two-year NIAID funding complete, Freitag is currently leaning on a modest bank of UIC funding to preserve her team’s research momentum while also preparing a new five-year grant proposal for NIAID’s consideration.
With her initial two-year NIAID funding complete, Freitag is currently leaning on a modest bank of UIC funding to preserve her team’s research momentum while also preparing a new five-year grant proposal for NIAID’s consideration.
“The hope is we are pushing this research forward with new funding by early 2026,” she says.
DEVELOPING NEW ANTIBIOTICS TO OUTWIT BACTERIA
Alexander (Shura) Mankin knows bacteria are smart and crafty. When exposed to therapeutics, bacteria adapt and dodge interventions.
“There are more and more bacterial pathogens for which there are almost no treatment, so we’re in an arms race against bacteria,” says Mankin, distinguished professor of pharmaceutical sciences. “We’ve got to stay ahead and create antibiotics that infectious bacteria haven’t seen before.”
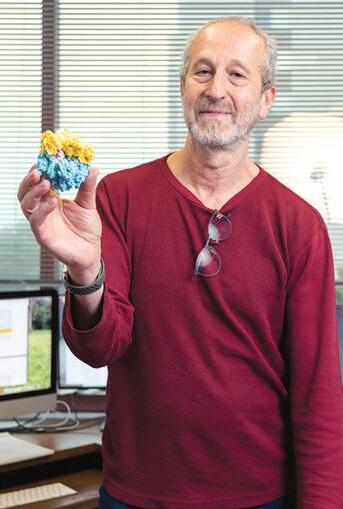
Partnering with scientists from McMaster University in Canada and from UIC Biology, Mankin is doing just that, investigating how three different antibiotics are eliminating pathogenic material.
In a recent study published in Nature, for example, Mankin, his UIC lab co-lead, Nora Vazquez-Laslop, and their Canadian collaborators introduced Lariocidin, a peptide made by bacteria living in soil. Lariocidin proved effective against several different microbes responsible for fatal infections, outsmarting bacteria by binding to a new target site, displaying a novel mechanism of action, and presenting a different structure to bacteria.
“The holy grail of antibiotic research is to find a drug with a new chemical structure, acting upon a new target, and never before seen by pathogenic bacteria,” Mankin says.
Lariocidin represents the Mankin/Vazquez-Laslop lab’s latest promising development in the hunt for new antibiotics, but Mankin teases even more.
“A decade from now, I believe we can have an arsenal of novel antibiotics to treat new bacterial pathogens
as well as old pathogens that have become resistant to existing therapeutics,” he says.
The NIH’s National Institute of General Medical Sciences supports Mankin’s work, and he considers federal funding absolutely essential to antibiotic research.
“This type of forward-looking research is too expensive for small pharma to handle and not profitable enough to stoke large pharma’s interest, so federal funding is critical to advancing science in this important area,” he says.
IDENTIFYING A NEW WAY TO COMBAT OVARIAN CANCER
The American Cancer Society pegs a woman’s risk of getting ovarian cancer at one in 91. The organization also estimates about 21,000 U.S. women will receive a new diagnosis of ovarian cancer this year alone. For another 13,000 women in the U.S., ovarian cancer— among the leading causes of cancer deaths among women around the world—will prove fatal in 2025.
For the last 15 years, Burdette has been leading basic research programs to help transform ovarian cancer treatment and generate improved results.

Empowered by funding from NIH and the Department of Defense, Burdette has found ovarian cancer does not start in the ovaries but rather the fallopian tubes. Slowly, her discovery has ignited changes in clinical action and guidance. Most notably, many clinicians now counsel women deemed high risk of developing ovarian cancer to consider having their fallopian tubes, not their ovaries, removed.
“If we take the wrong tissue out of women who are high risk, we’re not only failing to solve the problem, but we’re having these women endure an unnecessary surgery,” Burdette says, adding that removing a high-risk woman’s ovaries, a oncecommon practice, wholly eliminates her ability to birth children.
While it is too early to discern the impact of proactively removing fallopian tubes on ovarian cancer rates, Burdette points to Canadian studies signaling a slowdown.
“Knowing these concerns arise in certain tissues and showing fallopian tubes as the source of ovarian cancer has supported changes in cancer care and should continue to help women avoid this lifealtering diagnosis,” Burdette says.

