
17 minute read
AHS responds to COVID-19
Dani Bergey ’19 MS BVIS , David W. Ehlert ’97 MS BVIS and Kristine A. Johnson ’98 MS BVIS are among the team at Cognition Studios in Seattle who are creating visuals to help clinicians, researchers and the general public better understand the novel coronavirus. © 2020, Cognition Studio, Inc. All rights reserved
Our talented alumni, students, faculty and staff are contributing to the efforts to understand the novel Coronavirus Disease 2019 (COVID-19) and its impact on communities. We are proud of their contributions to the collective knowledge about and fight against the pandemic.
Advertisement
Answering the call
When 1,300 members of the Illinois National Guard stepped up to help in the state’s fight against COVID-19, AHS students Cassandra Hall and Akira Tanton were among those who volunteered.

Akira Tanton administers a COVID-19 nasal swab test at a drive-in site. Photo: Brian Cassella / Chicago Tribune
Akira Tanton (AHS Class of 2023) spent most of her spring and summer helping thousands of Chicagoans get tested for COVID-19.
Tanton, airman first class in the 182nd Airlift Wing of the Illinois Air National Guard, was one of about 50 in her medical support unit who volunteered to conduct coronavirus testing at 11 drive-in sites throughout Illinois.
“The uncertainty of it is challenging. This is something we’ve never seen before,” she says. “But we all decided to answer the call.”
Tanton reported for duty March 16 with one day’s notice. Her mission ended July 31 when the National Guard turned over operation of the test sites to civilian contractors.
Tanton completed her spring semester assignments, then her finals, online at night alone in her hotel room.
“School has been hard, but my professors have been accommodating,” she says.
She and her team members shared their meals in a hotel conference room, seated apart for physical distancing. Their vital signs were checked three times a day.
They were transported to the testing site in early morning and stayed until closing mid-afternoon, or when all tests allocated for that day were given. Tanton was stationed at testing sites in Harwood Heights, then Markham and finally, South Holland.
Tanton joined the Air Guard in 2017 to help pay for college and because “I always wanted to do something bigger for myself and to serve others.”
Her unit is headquartered at Peoria Air National Guard Base. As an aerospace medical technician, she’s a certified EMT who spends one weekend a month and two weeks a year training as a medic in hospitals or in the field. Tanton plans a career in the health professions, although she’s not yet certain which field. Last year she went on a MedLife student medical mission to Peru, which inspired her to consider practicing in an underserved country.
When she was called up in March, she didn’t know how long her Guard assignment would extend but, “however long they need us is how long I plan to stay.”
As weeks turned to months, she checked in often with her family in Sterling and Rock Falls, encouraging them to wear masks.
“It could happen to anyone,” she says of COVID-19, adding that some of her friends were asymptomatic but tested positive for the virus.
The reward for her service during the pandemic? “Knowing I’m making an impact,” she says.
"We're part of history."
Read the full story at go.uic.edu/AkiraTanton.

Cassandra Hall inside the McCormick Place Convention Center she helped transform into a temporary hospital for 3,000 COVID-19 patients.
Cassandra Hall (’23 DPT) keeps track of each day’s tasks on Excel spreadsheets. Her closet is organized by color.
So she was not fazed by her National Guard assignment to an 80-person team that transformed McCormick Place Convention Center into a temporary hospital for 3,000 Covid-19 patients.
“It was definitely right up my alley,” says Hall, who was recently promoted from airman first class to senior airman in the Air National Guard.
Hall’s experience helping her father build houses proved useful as Guard members unloaded, unboxed and assembled furniture, including 3,000 chairs and 2,500 beds—some carried upstairs by hand because of building requirements. They placed beds, mattresses, chairs, pillows, trash cans and personal hygiene kits in each section.
They completed one section, then redid it after orders changed. They worked 17-hour days, but they met their deadlines.
Then they were told to take it down.
“We prepared for a worst-case scenario—3,000 people surpassing hospital capacity. Thank goodness we didn’t need to use it,” Hall says.
After her McCormick Center assignment, she was sent to MetroSouth Medical Center in Blue Island to help convert the hospital, which closed last fall, into a 585-bed facility for coronavirus patients. Her deployment, which began April 5, was extended four times—she finally returned home July 15. To protect from the virus, she was confined to hotel and workplace, bringing meals upstairs to dine alone, taking final exams on her laptop and seeing her family on video chat.
The whole experience was intense— but rewarding.
“I learned a ton about how to manage personnel and disseminate information from multiple sources effectively. I also learned the value of hard work, long hours, and effective leadership by seeing the effort and expertise required to manage such a large mission,” she says.
“My experiences will allow me to better recognize when to step up and take charge of a situation, as well as how to communicate effectively in a stressful and at times confusing environment. These are all skills that will help me to be successful in physical therapy school as well as be a successful physical therapist in the future.”
Read the full story at go.uic.edu/CassandraHall.
Helping people breathe

Gillian Corbo
KN clinical instructor Gillian Corbo is working with Ocalink, a Canadian company founded to address the critical shortage of ventilators in the world, to design an emergency ventilator that can be easily built using machined parts sourced from across Canada. Corbo’s expertise in anatomy and training as a physiotherapist give her a critical understanding of the respiratory challenges facing COVID-19 patients. Specifically, Corbo has been reaching out to potential manufacturing, assembly and engineering partners to figure out how they could come together and leverage their expertise to build out a manufacturing and supply chain. The goal? To build 1 million ventilators within 90 days. Fortunately the severity of symptoms for COVID-19 patients has been better than anticipated in North America due to the public health measures implemented, and 1 million emergency ventilators have not been required. However should there be a second wave, the novel supply chain has been established.
Growing closer with distance
AHS physical therapist and client strengthen their relationship while practicing social distancing.
Every week since the state-ordered pandemic restrictions began, physical therapist Deb Davey and her patient, Theresa Harris, have logged on to doxy.me to visit each other’s homes.
They discovered they have the same kind of sofa. Davey has peeked inside Harris’ fridge. They dance to Motown.
Through telehealth, they’ve established a strong level of trust as Davey treats Harris for longtime pain related to two back surgeries.
“I am not a tech-savvy person. I was a little bit worried about how this would go,” says Davey, a clinician and educator at the UIC Physical Therapy Faculty Practice clinic who is seeing seven patients through telehealth. “But it’s been a great experience.”
Harris agrees.

Deb Davey
“At the clinic, there’s interruptions; there’s other people in the room. Doing this online is more personal, because we’re both at home. It’s more undivided attention,” she says.
When the PT clinic temporarily closed March 16 due to the state’s COVID-19 shutdown order, its seven physical therapists offered patients the option to try telehealth. As of July, they had provided nearly 100 telehealth appointments and the experience has been “well-received overall,” says clinic director Aaron Keil.
Davey is a clinical assistant professor who teaches in the post-professional orthopaedic residency and Doctor of Physical Therapy program as well as seeing patients in the clinic.
She specializes in the treatment of chronic pain, which she prefers to call “persistent pain.” She recently completed a European Diploma in Pain Physiotherapy from the European Pain Federation in Leuven, Belgium.
People with chronic pain usually have other health issues too, so Davey makes referrals to the clinic’s nutritionist. Shayna Oshita, as well as social workers and psychologists.
“We give them resources to assist in self-management. We give them a listening ear to hear about their pain experience. It’s about finding a way to create a patient alliance,” Davey says.
And “alliance” is a good description for the bond between Davey and Harris.
After a lifetime of physically demanding jobs—she currently works at UPS— Harris has a long list of health problems. Her back surgeries resulted in complications and infections.
At one point, hospital staff thought she wouldn’t walk again. “They didn’t know I had already made arrangements with Jesus to get up out of that bed,” she says.
Besides persistent pain, Harris has diabetes, high blood pressure and high cholesterol. Last year, she had a heart attack.
“I’ve got a stint in my brain, a stint in my heart and hardware in my back,” she says. “When I get up and start my day and live my life, I don’t look at it as if I have all these chronic illnesses. I don’t make this the end of my story.”
Harris and Davey had several appointments in the clinic before the coronavirus shutdown.

Theresa Harris
But, to their surprise, the online video appointments made their sessions more personal, more effective— more fun. They don’t have weights, so they use cans of beans or bags of potatoes. They do the exercises together and each session ends with dancing to a Motown playlist.
When Harris’ daughter saw how much her mother gets out of the telehealth appointments, she bought “I never thought I could do something like this in my home and not be bored,” Harris says.
“I never thought I could do something like this in my home and not be bored,” Harris says.
“There’s a vulnerability when you open your home,” Davey says of the telehealth appointments. You feel more comfortable opening up the inner doors of your life, along with the physical doors.
“You don’t get that when people come to the clinic.”
Read the full story at go.uic.edu/CloserWithDistance.
Improving COVID-19 outcomes through healthy living
Ross Arena launches network to support healthy behaviors for improving COVID-19 outcomes.

Ross Arena
In the midst of the biggest global pandemic in living memory, Ross Arena, professor and head of PT, conceived of and launched The Healthy Living for Pandemic Event Protection (HL- PIVOT) network earlier this summer. The overarching goal of this global network is to promote healthy living behaviors that are known to reduce the risk of chronic disease as well as the impact of pandemic diseases such as COVID-19.
“It is well-known that the risk for bad outcomes for people with chronic conditions like diabetes and obesity, which in themselves are considered pandemics, are much higher in pandemic situations like the one we are in right now,” says Arena, who is also interim head of BHIS. “I thought this was an opportune time to launch this global network bringing together researchers, clinicians, educators, policy-makers, fitness professionals and others to help improve awareness of healthy behaviors like eating well and exercising and their protective benefits when it comes to chronic disease.”
The group, which has more than 100 members and is growing, has already published several papers, and is drafting policy statements encouraging the support of healthy living. Members of the group are also working together to develop new global research projects and grant submissions as well as educational programs.
People who are generally healthier to begin with tend to be able to weather illness better than people who are already behind the eight ball in terms of their health. People with heart disease, diabetes or obesity, as well as people who smoke or are sedentary, often have worse health outcomes when they become ill. Keeping healthy – maintaining a healthy weight, not smoking, eating and sleeping well and managing stress – are the cornerstones of good health, Arena explained.
When it comes to COVID-19, a clear pattern has emerged that indicates that people with preexisting conditions, such as obesity, diabetes, hypertension and cardiovascular and respiratory diseases, significantly increase the risk of poor outcomes due to the viral infection, Arena explained. “On the other hand, we have strong evidence that high cardiorespiratory fitness as well as regular physical activity and a healthy diet improve immune function, which helps protect against infection including COVID-19.”
The HL-PIVOT program will include collaborative research, education, policy recommendations and advocacy and programs to support healthy living behaviors around the globe.
Learn more about HL-PIVOT at go.uic.edu/HL-PIVOT.
Health Matters

Beth Marks

Jasmina Sisirak
An AHS research team led by DHD research associate professors Beth Marks and Jasmina Sisirak is examining virtual support for people with intellectual and developmental disabilities (IDD) amid the pandemic. Specifically, the team is examining how community organizations providing services to people with IDD are preparing and responding. The team is also creating a Virtual Coach: HealthMatters Google Classroom to see if the online, on-demand health promotion training program is effective for frontline staff and people with IDD to follow public health guidelines and stay safe and healthy. 18
Solutions expert
Health informatics alumnus uses IT to improve health care.

Raja Talati in his office.
“Technology should translate to better patient care,” insists Raja Talati ’14 MS HI —especially as the world grapples with the COVID-19 pandemic.
And Talati is well-equipped to do it.
He is a physician, teacher, researcher and medical information officer who is also chief of aerospace medicine in the Air Force Reserve at MacDill Air Force Base in Tampa, Florida.
He has a master’s degree in health informatics from UIC and an MBA in health care analytics from University of South Florida.
As a primary care physician, he has practiced in many different settings: urgent care, juvenile detention, multidisciplinary outpatient clinics and now, during the pandemic, in hospitals.
In April, he served a two-month deployment at Jacobi Medical Center in the Bronx, where he and his Air Force team helped care for coronavirus patients. In July, he was granted privileges at a hospital near his practice in Ft. Pierce, Florida, to help with the surge of COVID-19 patients.
Everywhere Talati practices, he sees problems with potential technology solutions.
Although much of his time is spent developing health care technology, Talati is adamant that he continue to see patients.
“I’ve been in practice for 20 years, I don’t want to lose my clinical skills,” he says.
As chief of aerospace medicine at MacDill, he travels to Tampa one weekend a month to conduct health screenings of reserve flight crew members. At the Midway clinic in Fort Pierce, he provides primary care to HIV patients as well as geriatric patients from his previous practice.
When COVID-19 increased dramatically in Florida recently, he began seeing coronavirus patients, sharing with colleagues what he learned during his two-month assignment in New York.
“Our inpatient providers are just exhausted,” he says. “I saw their frustration and saw they needed a bit of help.”
During his time at the Bronx hospital, Talati saw another unmet need: better communication with patients who don’t speak, or understand, English. He started strategizing IT solutions.
“There’s a telephone language line in every room, but what’s lost in translation are the social and cultural nuances of health care,” he says.
“How can we use IT to speak directly with the patient, to combine culture and language to convey the correct meaning?”
Talati has high praise for the UIC health informatics program, with its strong foundation in IT governance and data security. Faculty members Olympia Kalagidis and Eric Swirsky have remained professional contacts over the years, he adds.
In fact, one of his colleagues graduated from the program in December.
The degree has helped expand his career, Talati says.
“I get to see patients, I get to play with computers, I get to create new knowledge. What more could somebody ask for?”
Read the full story at go.uic.edu/RajaTalati.
Safety practices

El Valor residents participate in a virtual session.
OT students Estefania Garcia and Brielle Seitelman have been offering virtual bilingual sessions for individuals with intellectual and development disabilities who reside in group homes managed by El Valor, a non-profit organization that serves predominantly Black and Latinx populations. The “Staying Safe and Having Fun” sessions teach the importance of wearing a mask, self-care, physical distancing and other safety practices. The students are supervised by Yolanda Suarez-Balcazar, professor and head of OT, and Mansha Mirza, associate professor of OT and DHD.
World renown rendering
BVIS grad’s illustration of COVID-19 is seen around the world.

The C.D.C. scientific/medical visualization experts: (front row, left to right) Stephanie Pfeiffer Rossow, Alissa Hogan Eckert, Jennifer HulseyOosthuizen; (back row, left to right) Dan Higgins, Meredith Boyter Newlove.
Photo: Centers for Disease Control and Prevention
Dan Higgins ’03 MS BVIS may be the only AHS grad to see his work published millions of times around the world, online and in print, on talk shows and network news—even on “Saturday Night Live.”
Higgins is co-creator of an illustration of the COVID-19 virus seen virtually everywhere since it was released by the Centers for Disease Control and Prevention in late January.
"I had no idead that the project was going to take off like it did," says Higgins, a Centers for Disease Control and Prevention visual information specialist since 2002. “We were taken aback when it started showing up on talk shows, major news networks and on the cover of magazines.”
Higgins and colleague Alissa Eckert had about a week to create the illustration that would become the face of the pandemic, working with a team that included epidemiologists and virologists, public health communication specialists and web developers.
“More than just a beauty shot, it had to express the seriousness of the situation but not terrify the public,” he says.
His BVIS studies helped him hit the ground running.
For the COVID-19 project, “I was able to ask the right questions of the virologists at Centers for Disease Control and Prevention, which helped speed up the production process. Once the research had been completed, I was able to apply my knowledge in drawing, 3D art and graphic design to create an image that was both medically accurate and visually appealing,” he says.
Since then, Higgins has been creating additional illustrations and graphics for social media and the Centers for Disease Control and Prevention website to educate the public on the spread of COVID-19.
“It’s been incredible to be a part of Centers for Disease Control and Prevention’s effort in fighting the pandemic,” he says.
He was attracted to the AHS program in biomedical visualization for its prestige as the second-oldest program in the country and its strong focus in digital art, including 3D and virtual reality. He was also impressed with the faculty’s wide range of expertise and skills.
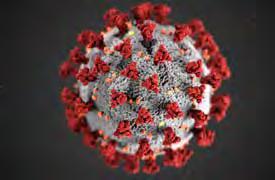
Photo: Centers for Disease Control and Prevention
“This variety opened up many possibilities and helped guide me in the path most suited for me,” he says.
Alice Katz, who was then program director of BVIS, helped him make the connections that led to his first job in the field, at WebMD.
“Many UIC instructors had a huge impact on my career,” Higgins says.
“Attending UIC was an honor and I highly recommend any person interested in medical illustration to look into the biomedical visualization program at UIC.”
Read the full story at go.uic.edu/DanHiggins.



