
7 minute read
RETOOLING THE FUTURE OF HEALTH CARE
Dr. Michael Paul Cary on leveraging AI to achieve better health equity outcomes in the U.S.

Licensed professionals and the organizations that regulate them around the world are finding innovative ways to harness artificial intelligence (AI) to streamline operations and enhance efficiencies.
In North Carolina, Duke University’s School of Nursing is actively exploring AI to enhance patient care and broaden access to health care services.
Dr. Michael Paul Cary, PhD, RN, is a leader in applying AI within health care, focusing on health disparities related to aging and developing strategies to advance health equity. As the inaugural AI Health Equity Scholar at Duke Health, Dr. Cary and his team scrutinize clinical algorithms applications that could perpetuate harm onto diverse communities, while promoting equitable health outcomes for all patients at Duke and beyond.
The Registrar spoke with Dr. Cary about his vision for reducing health care dis- parities through AI innovation and how human-centered AI interfaces can equip health care professionals with skills to use AI effectively.
A veteran of health equity advocacy
Dr. Cary’s appointment as Duke Health’s first AI Health Equity Scholar was just one of many accomplishments in his career grounded in the intersection of social justice and health equity. After earning his master of science in nursing (MSN) at the University of Virginia in 2006, Dr. Cary worked as a registered nurse in postacute care (PAC) facilities and community-based settings before joining Duke University’s faculty in 2016.
“These experiences exposed me to a diverse patient population and highlighted significant health disparities, especially among older adults requiring PAC rehabilitation after an acute illness or injury,” he explains. “Motivated to make a broader impact, I pursued advanced degrees in nursing and health services research [at the University of Virginia]. My focus has always been on improving care delivery and health outcomes for populations susceptible to adverse outcomes, particularly older adults.”
2022 was a year of recognition for Dr. Cary’s professional accomplishments, highlighted by his induction as a Fellow of the American Academy of Nursing for his significant contributions to improve health and health care. His appointment as the inaugural AI Health Equity Scholar in 2024 expanded his work beyond the university, enabling him to address systemic health care challenges.
“As the inaugural AI Health Equity Scholar at Duke AI Health, my primary goal is to evaluate healthcare algorithms and AI-enabled decision tools across the Duke University Health System (DUHS) to identify those that may exacerbate or perpetuate disparities based on race, ethnicity, national origin, age, or disability,” he says.
“By addressing and mitigating biases in these tools, we aim to promote health equity and improve health outcomes for all patients at DUHS.”
Impact across communities
Dr. Cary’s work directly impacts four distinct levels of society, using various AI-influenced models:
• Community level: Redesigning algorithms to include social determinants of health (e.g., housing and food insecurity) to ensure AI addresses marginalized populations' needs, where nurses' involvement helps to build trust and bridge participation gaps.
• State level: Duke’s AI Governance committee sets equitable AI deployment models across North Carolina, reducing rural-urban disparities and ensuring safety, fairness, and compliance.
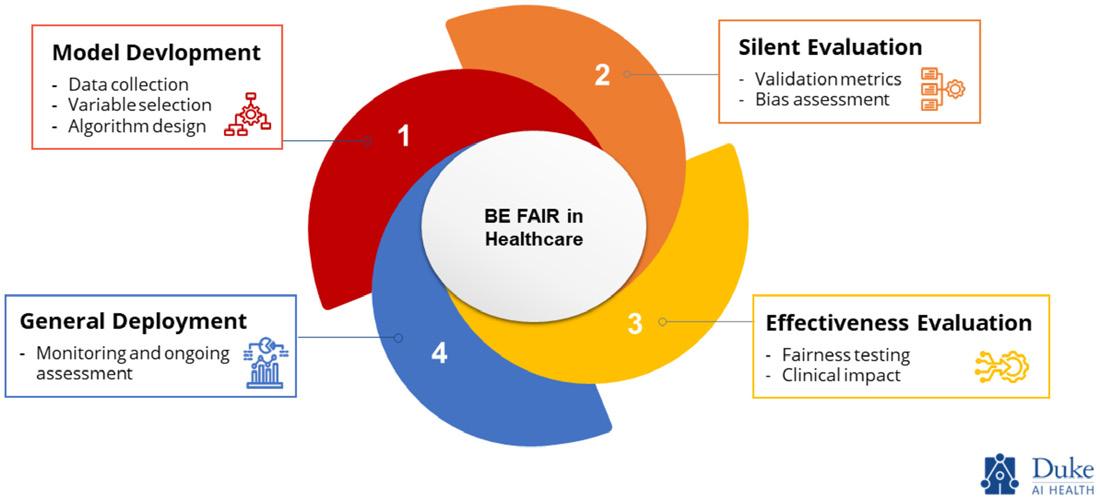
• National level: Empowering nurses to deploy tools like the Bias Elimination for Fair AI in Healthcare (BE FAIR) framework, which mitigates AI bias to align with federal policies, while establishing frameworks for national AI equity standards.
• Global level: At the International Association of Medical Regulatory Authorities (IAMRA), Dr. Cary emphasized governance, ethics, and strategies for responsible AI integration, proposing global collaboration, accreditation frameworks, and ongoing AI competency in health education.
“I serve as a bridge between clinical practice and technological innovation, a role strengthened by my clinical and research background,” Dr. Cary explains. “My experience as a nurse, health services researcher, and applied data scientist provides a comprehensive understanding of patient care and the systemic challenges within healthcare.”
“Specifically, my research program focuses on developing machine learning models to predict patient outcomes in postacute care (PAC) settings. These models are designed to reduce bias and support data-informed clinical decisions, particularly for older adults who are at risk of adverse outcomes. This allows me to collaborate effectively with data scientists, clinicians, and policymakers, ensuring that AI tools are not only technically robust but also practically applicable.”
Streamlining licensing procedures
Dr. Cary notes that current medical licensing processes in the U.S. involve extensive paperwork and manual credential verification. This is compounded by varying licensing requirements to be fulfilled if the medical professional want to practice across different states. He explains how this all leads to inefficiencies that can be problematic in rural and underserved communities that need health care services. He highlights how AI could be used to streamline these processes but stressed the need to proceed with caution.
“AI has the potential to streamline these processes by automating document verification, using natural language processing to review applications, and standardizing evaluation criteria thereby minimizing redundancies and subjective biases,” he says. “However, as regulators consider new and innovative ways to improve licensing processes, it’s crucial to proceed with the same cautionary principles applied to other AI systems. These tools must undergo rigorous evaluation for bias and discrimination before being deployed. By ensuring equity and accuracy in AI-driven systems, regulators can enhance efficiency while maintaining public trust and fairness in medical licensing practices.”
State-specific licensing requirements enhanced by AI-driven systems can expedite evaluation processes for international medical professionals who aim for quicker licensure without drawbacks, he says.
This, Dr. Cary explains, comes down to the regulator’s ability to track relevant data.
“The Physician Information Exchange (PIE) platform, for example, serves as a critical tool in ensuring transparency and accountability,” Dr. Cary says. “It has facilitated the sharing of information between medical regulatory authorities, allowing agencies to identify doctors with fraudulent applications or those with sanctions who may attempt to practice in another jurisdiction. By leveraging platforms like PIE alongside AI tools, regulatory agencies can maintain robust oversight, track individual progress through the licensure process, and contribute to a safer, more sustainable global health workforce."
Health equity as a foundation
Dr. Cary acknowledges that biases and subjective human judgments, often influenced by unconscious bias, can affect credential assessments. To ensure fairness in the standards used for evaluation, he stresses that AI frameworks must first be developed with health equity at the core.
His team employs the Bias Elimination for Fair AI in Healthcare (BE FAIR) framework, which underpins principles of reducing bias and promoting equity to support the credentialing process. “Although BE FAIR was originally designed to address bias in clinical algorithms, its principles of reducing bias and promoting equity among groups can be adapted to support the credentialing process,” Dr. Cary says. “Applying BE FAIR to credentialing could allow AI systems to:
• Analyze credentialing data to uncover patterns of inequity.
• Adjust algorithms to ensure factors unrelated to professional competence, such as socioeconomic background or place of education (and other factors that potentially discriminate against individuals), do not negatively impact evaluations.
• Provide explanations for credentialing decisions to promote accountability and fairness.
• Regularly review and update algorithms to address emerging biases.
Looking ahead to a future where AI is harnessed by medical professionals with enthusiasm, Dr. Cary underscores the need for strong governance committees to ensure the safe and ethical use of AI tools, including those used in the licensing process. He emphasizes that these tools must undergo rigorous evaluation for bias and discrimination before deployment and be continuously monitored for potentially discriminatory effects, while also ensuring patient health data is managed responsibly.
“Particularly for vulnerable populations, AI tools must incorporate robust encryption methods, strict access controls, and comply with regulations like HIPAA to protect patient information,” Dr. Cary says. “Additionally, these tools should employ data anonymization techniques to safeguard patient identities while allowing for valuable insights. Routine checks and highlighting areas of concern in AI tools will allow regulatory bodies to maintain efficiency without compromising the thoroughness required to ensure patient safety and uphold professional standards.”
Dr. Cary also anticipates more personalized and predictive health care to continually develop. “[The] integration of AI with electronic health records and wearable technology could enable continuous monitoring and early detection of health issues,” Dr. Cary says. “These innovations hold great promise for improving health outcomes and advancing health equity.”






