5 minute read
The Role of Radiation Therapy in Keratinocyte Cancer Management
Prof David Christie MBCHB FRANZCR skin@genesiscare.com
(07) 5598 0366 |
Advertisement
Australia continues to have the unenviable status as the skin cancer capital of the world.1 The incidence of keratinocyte cancers, basal and squamous cell carcinomas (BCCs and SCCs), has increased consistently for the past 30 years, and approximately 70% of Australians will have at least one BCC or SCC excised in their lifetime1, 2. This is an enormous disease and treatment burden, both to patients and the healthcare system, particularly as many patients have multiple lesions. The economic burden is now estimated at $1.2 billion in Australia3. In 2020, there was a significant reduction in skin cancer diagnoses, related to impact of COVID-19, rather than a genuine reduction in skin cancer prevalence4. A rebound in diagnoses is expected, as is identification of more advanced disease. Although treatment success rates for keratinocyte carcinomas is very good in comparison to other cancers, early diagnosis and treatment is important to prevent morbidity,5 and in the setting of SCCs reduce the risk of metastatic spread6
A prior diagnosis increases the risk of future skin cancers as patients age. This is associated with lifestyle patterns and often widespread areas of sun exposure. Extended skin field cancerisation (EFSC) refers to the accumulation of ultra-violet light (UVL)-damage and genetic mutations that heighten the risk of cancerous transformation7 EFSC is frequently associated with widespread areas of pre-cancerous actinic keratoses that also require treatment. Often these patients have a protracted history of multidisciplinary management and combination therapy such as topical antineoplastics, photodynamic therapy (PDT), cryotherapy, curettage & electrodessication, and excisions8. Some patients, with persistent changes despite trialling other therapeutic options, are looking for non-invasive strategies to manage disease.
Radiation therapy is a well-established treatment for skin cancer, with long-term cure rates similar to surgery for certain presentations9-12. It is effective as a non-invasive option for lesions in areas where surgery would result in significant cosmetic imperfections, for patients unsuitable for surgery or in the adjuvant setting for high-risk lesions13-15. Technological advances in radiation therapy, such as volumetric modulated arc therapy (VMAT) allow treatment to be sculpted to large areas of skin affected by pre-cancerous lesions and invasive disease, known as wide field radiotherapy16,17. Recent 12-month follow-up data has revealed promising outcomes for patients with extensive disease who were treated with widefield radiotherapy18. These data underscore some promising advances in the radiation therapy space, particularly how it can be applied to different presentations of skin cancer.
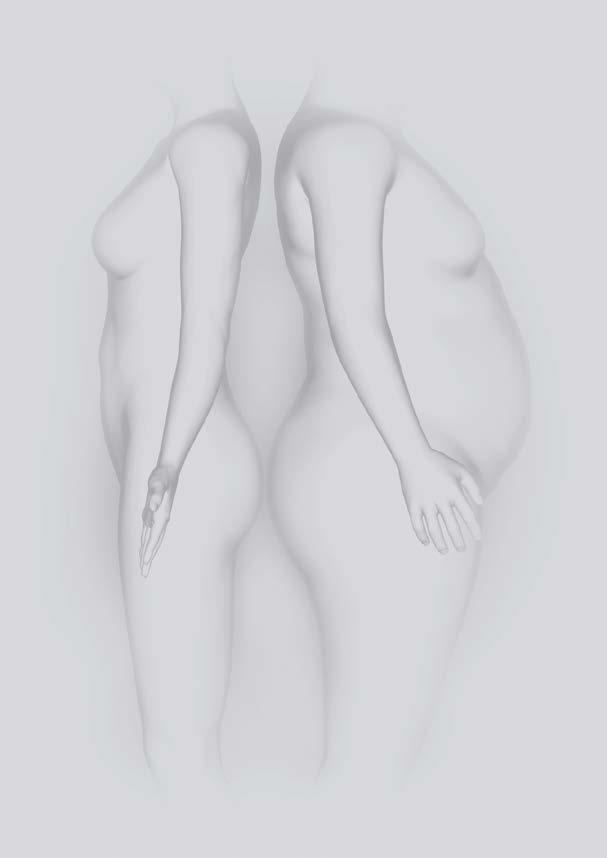
A patient treated with widefield radiation therapy, showing scalp before treatment commenced, and at 24-month follow-up

General Practitioners (GPs) are integral to the diagnosis and treatment of skin cancer, and the longitudinal management of patients with widespread disease. As such, we are pleased to offer a holistic GP-focussed education program on skin cancer and the role of radiation therapy, covering definitive, adjuvant treatment both for local and regional control and widefield interventions.

Modern Radiation Therapy techniques for the treatment of Keratinocyte Carcinomas (NonMelanoma Skin Cancer).
This program is comprised of 4 modules, each running for 1 - 1.5 hours, covering:
1) keratinocyte cancer incidence, risk factors and treatments
2) radiation therapy advances, its application to skin cancer and treatment guidelines
3) radiation therapy skin reactions, patient management and FAQs
4) interactive case study analysis and referral guidelines.
The first three modules are completed online at the learner’s own pace with incorporated assessment and feedback. The final module is a live, interactive webinar led by a local radiation oncologist, with a focus on real-world case studies. These sessions are small (~10-15 participants) to encourage participation and provide an opportunity to ask direct questions.
This program is accredited as part of the RACGP continuing professional development (CPD) program for six CPD hours (4-education activities;
2 – reviewing performance). It is also eligible for ACRRM and Skin Cancer College CPD hoursbased learning.
To register, visit this website: https:// GenesisCareLearning.litmos.com.au/self-signup/ Please use the code: SKINRT when registering for the online education program.
Once you have registered, log-in to the online education program at: https://genesiscarelearning. litmos.com.au/
References
1) Olsen et al. Keratinocyte cancer incidence in Australia: a review of population-based incidence trends and estimates of lifetime risk. Public Health Research and Practice. 2022; 32:1.
2) Staples et al. Non-melanoma skin cancer in Australia: the 2002 national survey and trends since 1985. Med J Aust 2006 Jan 2;184(1):6-10
3) Gordon et al. ”Estimated Healthcare Costs of Melanoma and Keratinocyte Skin Cancers in Australia and Aotearoa New Zealand in 2021” Int. J. Environ. Res. Public Health 2022, 19(6), 3178
4) Roseleur et al. Skin checks and skin cancer diagnosis in Australian general practice before and during the COVID-19 pandemic, 2011-2020. Br J Dermatol. 2021 Oct;185(4):853-855.
5) Mathias et al. Assessing health-related quality of life for advanced basal cell carcinoma and basal cell carcinoma nevus syndrome: development of the first disease-specific patientreported outcome questionnaires. JAMA Dermatol. 2014 Feb;150(2):169-76.
6) Brougham et al. The incidence of metastasis from cutaneous squamous cell carcinoma and the impact of its risk factors. J Surg Oncol. 2012;106(7):811-5.
7) Willenbrink et al. Field cancerization: Definition, epidemiology, risk factors, and outcomes. J Am Acad Dermatol. 2020 Sep;83(3):709-717.
Bariatric and General Surgeon
8) Cornejo et al. Field cancerization: Treatment. J Am Acad Dermatol. 2020 Sep;83(3):719-730.
9) Hernandex-Machin et al. Office-based radiation therapy for cutaneous carcinoma: evaluation of 710 treatments. Int J Dermatol. 2007. 46:453-459
10) Cognetta et al. Superficial x-ray in the treatment of basal and squamous cell carcinomas: a viable option in select patients. J A Acad Dermatol. 2012. 67:1235-1241
11) Schulte et al Soft x-ray therapy for cutaneous basal cell and squamous cell carcinomas. J Am Acad Dermatol. 2005; 53:9931001
12) Grossi Marconi et al. Head and Neck non-melanoma skin cancer treated by superficial x-ray therapy: An analysis of 1021 cases. PLoS One 2016; 11:e0156544
13) Likhacheva et al., 2020, ‘Definitive and Postoperative Radiation Therapy for Basal and Squamous Cell Cancers of the Skin: Executive Summary of an American Society for Radiation Oncology Clinical Practice Guideline’, Practical Radiation Oncology, vol. 10, no. 1, DOI <https://doi.org/10.1016/j. prro.2019.10.014>.
14) NCCN Clinical Practice Guidelines in Oncology. Basal cell skin cancer. Version 1.2017. Published October 3, 2016. https:// www.nccn.org/professionals/physician_gls/pdf/nmsc.pdf
15) NCCN Clinical Practice Guidelines in Oncology. Squamous cell skin cancer. Version 1.2017. Published October 3, 2016. https://www.nccn.org/professionals/physician_gls/pdf/squamous. pdf
16) Wills et al. Dosimetric comparison of volumetric modulated arc therapy (VMAT) and high-dose-rate brachytherapy (HDR-BT) for superficial skin irradiation with significant curvature in one or more planes. Strahlenther Onkol. 2021 Jun;197(6):547-554.
17) Ostheimer et al. Dosimetric comparison of intensitymodulated radiotherapy (IMRT) and volumetric modulated arc therapy (VMAT) in total scalp irradiation: a single institutional experience. Radiat Oncol J. 2016 Dec;34(4):313-321.
18) Potter et al. Preliminary efficacy and safety analysis: 12-month results in 83 patients using a novel approach of widefield radiation therapy for extensive skin field cancerization with or without keratinocyte cancers. J Dermatol. Treat. 2022 23:1-9
Assoc. Prof Harald Puhalla MD FRACS
An experienced general surgeon with a sub-specialist interest in bariatric and upper gastrointestinal surgery.

Using the latest surgical techniques, including minimally invasive treatment technologies, Harald has helped thousands of people achieve the best health outcomes. Bariatric patients especially benefit from his close partnership with bariatric dietitians, exercise physiologists and psychologists. It is this dedication to holistic care, and Harald’s compassionate manner, that give his patients individual solutions for long-term results.
Bariatric Surgery has substantial health benefits:
No or reduced medication for:
• Type 2 diabetes
• Hypertension
• High cholesterol
• Osteoarthritis / joint pain
• Decreased risk of heart attacks, strokes, blood clots
Decreased risk of developing 13 types of cancer (e.g. large bowel, ovarian)
• Better quality of life and increased physical activity
• Prolonged life expectancy (calculated from the age of 40 years)
• Improved fertility female (polycystic ovarian syndrome) and male








