
8 minute read
Eyelid lesions: part two
by TheAOP
Part two in this series of four articles on eyelid lesions continues with a focus on benign eyelid lesions that can present in practice.
Introduction
Advertisement
The first article in this four-part series showcased common eyelid lesions, highlighting that most of these cases are benign in nature. Nevertheless, it is important for practitioners to be alert to indications of suspicious eyelid anomalies during the course of eye examinations, contact lens consultations, the dispensing process, as well as other interactions with patients, such as periodic spectacle adjustments.
Attention should be given to the timeline and evolution of the lesion, such as a change in colour or size, as well as establishing key risk factors, such as personal or family history of skin cancer, solid organ transplantation, immunosuppression and exposure to carcinogenic environmental elements such as ultraviolet (UV) light and radiation.
Part one in the series also demonstrated the need to be aware of key signs that can indicate a malignant presentation. In brief, these include the presence of telangiectasia, disruption of normal eyelid structures, such as obliteration of the lash line or gland orifices, or bleeding. Pearly or irregularly bordered lesions and nonuniform pigmentation should also heighten suspicion of malignancy.
Part two in the series will continue to focus on common benign eyelid lesions that can present in clinical practice.
Seborrhoeic keratosis
Seborrhoeic keratosis (formerly referred to as basal cell papilloma) is the most prevalent benign skin lesion of the elderly.1 It frequently affects the face, trunk and extremities, and appears as a hyperkeratotic, pigmented plaque. On the delicate skin of the eyelid, seborrhoeic keratosis can appear to be ‘stuck on’ with visible excrescences on its surface.2 It may otherwise appear pedunculated or lobulated. Among its distinguishing features, seborrhoeic keratosis frequently occurs in multiples, particularly with increasing age. A soft, oily lesion is a reassuring sign (see Figure 1); it also appears commonly on or below the pretarsal lid margins. Any lesion suspicious of melanoma should be assessed according to the ABCDE criteria outlined in part 1 of this series. Melanoma of the eyelid might be considered if the lesion has irregular borders with intralesion colour variation. If there is diagnostic uncertainty due to the presence of atypical features, a biopsy with histological evaluation will show enlargement of the epidermis owing to basal cell hyperplasia. Sometimes, keratin-filled horns or cystic inclusions may also be present. Most of these lesions, irrespective of their size, remain superficial and can be treated by shave excision at the dermal-epidermal junction. Alternatively, curettage, laser ablation or cryotherapy may be used.

Papilloma
The papilloma family of eyelid lesions is a group of benign epithelial proliferations. Treatment is usually not required except for cosmetic removal where cryotherapy or surgical excision may be offered.
Squamous cell papilloma (SCP) is otherwise known as a skin tag or acrochordon. Once again, it is more prevalent with advancing age. Most arise de novo but UV radiation and infection with human papillomavirus (HPV) are implicated in at least some cases.2 Sessile lesions often have a broad base and a smooth surface whereas pedunculated papillomas are rough in texture.3 They can be solitary, multiple, pigmented or flesh-coloured (see Figure 2). This hyperkeratotic lesion may resemble a squamous cell carcinoma (SCC), and crusting, ulceration and fissuring should warrant further investigation. Despite its many macroscopic appearances, histology of SPCs shows digitated projections of fibrovascular connective tissue encapsulated by irregular hyperkeratotic and acanthotic squamous epithelium.4 Surveillance is sufficient in most cases, although patients may prefer removal using the aforementioned management techniques for benign epithelial hyperplasia.

Verruca vulgaris is another papillomatous lesion colloquially referred to as a wart, affecting approximately 10% of the global population within the first two decades of life.3 It is the result of an epidermal infection with HPV, particularly subtypes six and 11, which usually affect children and swimmers on the soles of their feet. The virus is spread by direct contact and one can selfinoculate the eyelid. Meat handlers and immunosuppressed individuals are also highly susceptible. In the early stages, the lesion appears flesh-coloured or grey and slowly enlarges to become an elevated papule with an irregular, digitated surface, usually on the eyelid margin (see Figure 3). Hyperkeratosis can resemble other benign papillomas, keratoacanthoma or SCC. Crucially, it may be differentiated by the preservation of eyelid architecture and their distinct borders. It is not usual to see ulceration with verruca vulgaris, nor does it bleed or ooze. These lesions rarely require treatment although some patients may seek treatment for cosmesis, or if there is subsequent conjunctivitis due to viral shedding.
Epidermoid and dermoid cysts
Epidermoid cysts are a type of keratinfilled sebaceous cyst lined with epithelium which commonly occur along the face, neck and upper back.5 Dermoid cysts are similarly lined but contain dermal appendages such as teeth, hair, and sebaceous glands. Epidermoid and dermoid cysts are examples of choristomas.6 In contrast to a hamartoma, which is a benign, non-cancerous mass of abnormal cells or tissue that normally occur within the involved site, a choristoma is a proliferation of histologically normal cells or tissue that are not normally found in the involved site. They are congenital cysts, accounting for most orbital tumours of childhood. They usually become symptomatic as they enlarge
WHAT YOU NEED TO KNOW C-105980 LEARNING OUTCOMES
Practitioners will be able to identify the key questions that need to be considered in cases of eyelid abnormalities relative to their scope of practice with age; therefore, those presenting earliest are usually the most superficial. Dermoid cysts are most frequently found at the edge of the lateral brow, followed by the medial upper eyelid. Superficial lesions may also cause some overlying skin discolouration. Several characteristics may suggest their benign nature, such as their smoothness, mobility and slow growth. Posteriorly situated dermoid cysts do not present until adulthood as they become large enough to cause progressive proptosis. Computed tomography (CT) and magnetic resonance imaging (MRI) can help support the clinical diagnosis by determining the contents of the cyst. Small cysts may regress but large symptomatic ones require surgical excision. Rupture and incomplete removal during surgical excision may increase the likelihood of recurrence; therefore, care must be taken by the ophthalmic surgeon to avoid cyst rupture during excision.
Practitioners will consolidate their knowledge on the key features of eyelid lesions and their management.
Epidermal inclusion cysts and milia
Approximately 18% of excised periocular lesions are epidermal cysts, the second most common benign lesion of the area.7 Many of these cysts arise spontaneously from the infundibulum of the hair follicle but may also occur following sunburn or traumatic entrapment of the epidermal layer within the dermis. During the healing process, the ruptured epithelium releases keratin which triggers an inflammatory reaction, and a superimposed infection may occur. These epidermal inclusion cysts present as elevated, smooth papules.
Milia (see Figure 4) is a term used to describe an eruption of multiple epidermal inclusion cysts. Primary milia can present at birth, though it more regularly occurs later in life secondary to local trauma such as sunburn. Additionally, it may appear as a consequence of bullous disease healing. Usually, it self-resolves but patients may seek treatment for improved cosmetic appearance if nonremitting. Management options include needle marsupialisation, cryotherapy, laser resurfacing or dermabrasion. Confluent areas may be treated with a topical retinoid.
Retention cysts
A cyst of Moll, or hydrocystoma, is a retention cyst in the sweat gland of Moll caused by a blockage in the draining duct (see Figure 5).7,8 Either eccrine or apocrine sweat glands are affected. Eccrine hydrocystomas present as small, soft eyelid lesions predominantly affecting the lower eyelid and medial canthus with eyelid margin sparing. Apocrine hydrocystomas characteristically present as firm, transilluminating eyelid margin lesions and may have a bluish colouration with yellow deposits within. They may appear as solitary or multiple lesions. The important malignant differential to consider with these lesions is cystic basal cell carcinoma (BCC), particularly if there is associated telangiectasia and pearliness of the skin.9 Reassuring features of a benign cyst include preservation of the eyelid margin and lash line. Hydrocystomas are typically diagnosed clinically but uncertainty should trigger a biopsy for confirmation. Although benign, ocular pruritus or cosmetic impact may incentivise patients to seek a cure by excision. Similarly, obstruction of ductal outflow of the sebaceous gland of Zeis can lead to cyst formation. The two can be differentiated by the lack of transillumination seen with cysts of Zeis as they are filled with yellow, turbid material. Infection of a cyst of Zeis or Moll results in the formation of an external hordeolum.
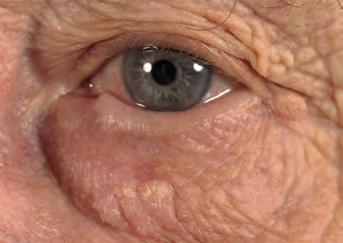
Xanthelasma palpebrarum


Xanthelasma palpebrarum are localised accumulations of lipid-laden macrophages that form in the medial canthus of the eyelids.10 Typically, these lesions are symmetrically distributed around both eyes and may be solitary or multiple (see Figure 6). They are often observed following the fourth decade of life and do not cause ocular symptoms or side effects. Xanthelasma is associated with dyslipidaemia, particularly hypercholesterolaemia, and therefore, may indicate an increased risk of atherosclerotic disease. It is, therefore, prudent to screen patients for lipid disorders and this may result in subsequent diet modification and consideration for lipid-lowering medication. These asymptomatic lesions may be removed by excision, radiofrequency dermabrasion or Argon laser photocoagulation if cosmetically bothersome.11 Following surgical excision, recurrence is common. Radiofrequency abrasion is increasingly used nowadays as it results in less scarring in comparison to other ablative treatments, such as chemical acid peels; however, any form of ablation may also lead to post-treatment hypo- or hyper-pigmentation.
Actinic keratosis
Actinic keratoses are premalignant lesions that typically arise in anatomical areas of high sun exposure, for example, the dorsum of the hand, shoulder and face.12 Around the eyelid, they can appear as solitary or multiple, pigmented, ovoid plaques with overlying scaling and sandpaper-like texture (see Figure 7). Adjacent skin usually shows signs congruent with UV exposure such as telangiectasia and yellow discolouration. They may also give rise to a cutaneous horn. On occasion, actinic keratosis with heavy pigmentation may resemble lentigo maligna. Fewer than 1% of these lesions transform into sebaceous cell carcinoma (SCC) per year.2 When differentiating an actinic keratosis from a malignant lesion, note that they are slow-growing and have distinct borders. They predictably darken with sun exposure and cosmetically improve with sun avoidance.2 Histopathological assessment should be considered if the clinical examination is inconclusive.
Actinic keratosis exhibits cellular atypia resulting in an irregular dysplastic epidermis with hyperkeratosis. Of note, invasion of the stroma would indicate SCC.
They can be treated with ablative therapies such as cryotherapy, curettage, laser or numerous topical agents including 5-fluorouracil (5-FU), diclofenac and imiquimod cream; these are beneficial for patients who have multiple lesions. The advantage of using topical agents is that field-based treatment may also target subclinical actinic keratoses in the area, decreasing their recurrence and opportunity for malignant transformation.13 Topical 5-FU and diclofenac 3% cream have similar dosing regimens, requiring patients to apply the cream to the affected area multiple times a day for one month; this can be rather bothersome for patients and may lead to non-compliance. The latter is not suitable for pregnant women and so diclofenac may be suggested which necessitates concurrent sun protectant use. Imiquimod cream (trade name Aldara) is a good, is a good alternative for the eyelid and is as successful as 5-FU in the long-term at preventing the development of actinic keratoses.13 Dosing is weekly which reduces skin irritation in the area. However, it is usually continued for three to four months. Ophthalmologists will often opt for local excision of small lesions close to the lid margin as topical treatments may cause ocular irritation.14
Nicotinamide is a derivate of vitamin B3 that actively protects cells from UV radiation-induced damage.15,16 It supports deoxyribose nucleic acid (DNA) repair following UV irradiation by ensuring there is sufficient generation of adenosine triphosphate (ATP) to enable the energy-intensive process of DNA repair. Optimising DNA repair processes reduces carcinogenesis. It is obtained exogenously from meat, fish and nuts. Oral nicotinamide, therefore, represents a readily available treatment option for patients at high risk of developing non-melanoma skin cancer and may encourage regression of actinic keratosis.
Conclusion
Practitioners should be reassured that the majority of eyelid lesions seen in clinical practice are benign. Nevertheless, it is essential to remain alert to the characteristic features of malignancies during patient interactions by having awareness of risk factors and potential signs.
To read this article online, access the references and take the exam, visit: www.optometry.co.uk/cpd










