3 minute read
INCREASE IN HIV DRUG RESISTANCE
text: Dr Richard Lessells
A new study published in The Lancet Global Health forecasts a significant rise in resistance to dolutegravir, the cornerstone of HIV treatment in South Africa, potentially threatening progress made in controlling the epidemic.
Over 25 million people living with HIV in low- and middle-income countries are receiving dolutegravir (DTG)-based antiretroviral therapy (ART). Most of the 6.2 million people on ART in South Africa now receive DTG-based ART – most commonly in the form of the fixed-dose combination of tenofovir, lamivudine and DTG (known as TLD). This widescale transition to DTG-based ART has been associated with high population levels of viral load suppression. Although DTG resistance is currently rare, it is inevitable that drug resistance will increase over the next few years and this could threaten our efforts to end HIV as a public health threat. What is uncertain is the extent to which DTG resistance will increase, and the speed at which this might occur.
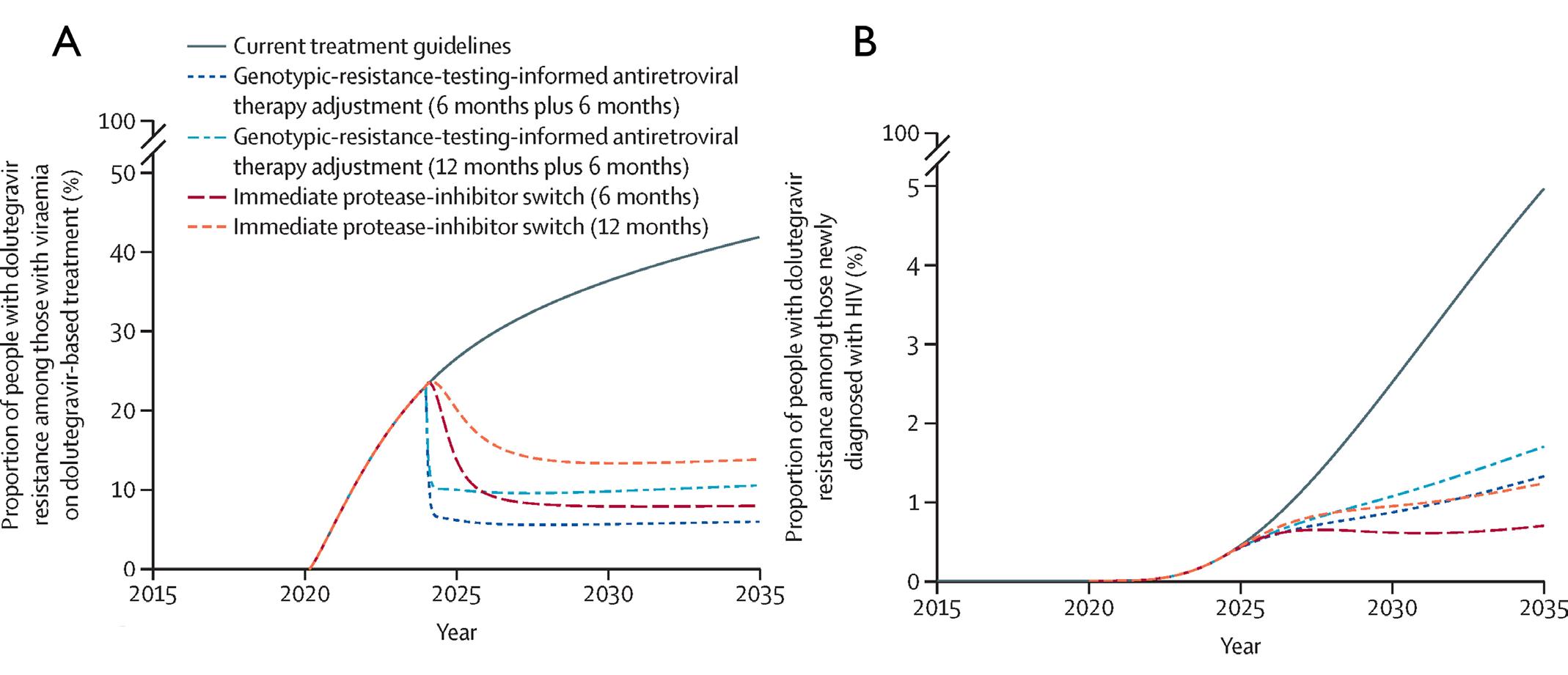
Together with collaborators in Switzerland and other international partners, the researchers used a mathematical modelling framework to predict how DTG resistance might change over time in South Africa, and to identify opportunities for interventions to limit the emergence and spread of drug resistance. Their findings reveal that while dolutegravir-based therapy remains effective for most patients—with viral suppression projected at 93% by 2035—the rate of resistance among those failing treatment could more than double, rising from 18.5% in 2023 to 41.7% by 2035.
The results of the model suggest that, although DTG resistance will increase quite substantially over time in people who do not achieve viral load suppression on ART, levels of transmitted resistance levels will remain at relatively low levels (<5%) up to 2035. Switching people with virological failure to alternative ART regimens (based on protease-inhibitors), with or without genotypic resistance testing to inform the switch, was predicted to significantly limit the increase in drug resistance levels.
“This research provides reassurance that, although dolutegravir resistance will increase, there are things that we can do to limit this and to ensure the long-term sustainability of these highly effective ART regimens. As is often the case with mathematical modelling, there are many uncertainties, as we still have a lot to learn about DTG resistance and about the best approach to managing patients with virological failure on TLD. We hope that our ongoing research with the DTG Resist project and with the RESOLVE trial will help to address some of those knowledge gaps and inform our treatment and monitoring guidelines,” commented Dr Richard Lessells, co-author on the paper.
The study underscores key factors driving resistance, including delayed switching from failing regimens and limited access to genotypic-resistance testing. South Africa’s current guidelines recommend resistance testing only after prolonged viraemia—often too late to prevent mutation development and spread.
However, the research offers hope. Counterfactual modelling scenarios suggest that early intervention—particularly switching patients with failing therapy to protease-inhibitor regimens within six months—could drastically curb resistance.
The study, supported by the US National Institutes of Health and the Swiss National Science Foundation, highlights the critical need for vigilance and adaptability in HIV treatment programs, particularly in resource-limited settings facing high HIV burdens.
Figure Legend:
Effects of the counterfactual scenario and modelled resistance-emergence-mitigation strategies on acquired dolutegravir resistance (A) and transmitted dolutegravir resistance (B).
Link to the Scientific paper:
Predicted dolutegravir resistance in people living with HIV in South Africa during 2020-35: a modelling study. Loosli T, et al. Lancet Glob Health 2025;13(4):e698-e706. doi: 10.1016/s2214-109x(24)00553-9









