
8 minute read
Ensuring a Safety Net for the Most Vulnerable
Section 2 | How We Give Back to Our Communities
E N S U R I N G A SAFE T Y N E T FO R TH E M OS T V U LN E R AB LE
Advertisement
It is shortsighted to think the successful delivery of healthcare is based solely on results from within the walls of SCL Health hospitals and clinics. We look beyond internal patient care to include coordination and access to external social services for improved health management. Some patients are in vulnerable situations, such as financial insecurity, homelessness, unemployment or exposure to violence. The mission of SCL Health guides us to make sure the most vulnerable are treated with compassion and cared for in ways that meet their individual needs.
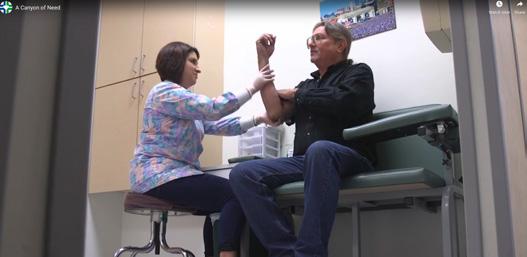
Caritas Clinic patient Monique
When Caritas Clinics first opened its doors more than three decades ago to serve the very low-income, uninsured residents of Leavenworth and Wyandotte Counties in Kansas, most patients needed treatment for their immediate medical needs. Since then, healthcare has changed dramatically; now, 80 percent of patients who visit the St. Vincent Clinic or Duchesne Clinic struggle with at least one chronic disease – meaning a disease that lasts more than a year and that requires ongoing medical treatment – and lack of consistent care prior to coming to one of the clinics.
Caritas Clinic patients come from poor, vulnerable populations and have placed tremendous trust in SCL Health clinics and providers as their medical home, the place where they receive comprehensive and coordinated primary care. Historically, when clinic patients became Medicare/Medicaid eligible, they were forced to move to other providers. In 2019, Caritas Clinics prepared to accept patients insured by Medicare or Medicaid starting in 2020. This is one of the most important ways the clinics can assure continuity of care and well-being for patients.
“We believe our mission, to improve the health of our communities by caring for the poor and vulnerable, and our vision, to exceed our patients’ expectations for health, will be best met by accepting patients covered by Medicare and Medicaid. We want to remain a trusted medical home for all of our patients,” says George M. Noonan, Executive Director of Caritas Clinics.
To prepare, Caritas Clinics partnered with Kansas Healthcare Collaborative, a member of the Practice Transformation Network, to set goals and use data from
2019 STATS | CARITAS CLINICS 1,741 individual patients served 13,108 patient encounters 1,099 patient screenings for social determinants of health and adverse childhood experiences 60 % of patients who required Spanish bilingual interpretation > 500 clinic patients have diabetes 161 bilingual diabetes education sessions held
electronic health records and national benchmarks to further improve quality of care and be ready to accept value-based payment models. The groundwork completed in 2019 will help ensure the success of the program in coming years.
It is a challenge for clinics like Caritas Clinics to afford to operate only based on philanthropy. Accepting Medicaid and Medicare patients will help the clinics build a new revenue stream that is needed to stay open for the long term, while making sure patients continue to receive the excellent medical care they need – and deserve.
Watch an online video about Caritas Clinics. Visit: sclhealthreport.org Getting life saving medications to patients who need them the most
In 2019, the Caritas Pharmacy Assistance Program provided $3.2 million in medications to patients, often with chronic diseases, who could not otherwise afford them. As the most robust program of all safety net clinics serving the Kansas City area, the amount of no-cost medications dispensed represented a 30 percent increase over the previous year.
“We feel that one of the reasons our patients have better than average health outcomes for chronic diseases is because of this program,” Noonan says. “These monthly medications are the backbone of most chronic disease management plans. Now more than ever, we must seek ways of providing these life saving medications, given the rising costs of prescription drugs.”
2019 STATS | PHARMACY ASSISTANCE PROGRAM 617 patients assisted 2,872 medications distributed
Nursing collaboration aims to improve oral health outcomes
Dentistry and medicine, often seen as separate points of care, work best in partnership. Through effective and efficient use of resources and medical expertise, both patients and providers benefit. When oral health and nursing colleagues collaborate, health outcomes improve by having a team of professionals from diverse fields dedicated to care for the whole person.


In 2019, the SCL Health Marian Dental Clinic in Topeka,
Kansas, built a relationship with the nursing profession to enhance the quality of patient care. They did so by incorporating a registered nurse and nursing students from Baker University into the dental clinic as an important part of the care team. The nonprofit safety net clinic offers comprehensive, quality dental care to the community.
The clinic is one of only a few in the area providing dental services to 2019 STATS | MARIAN DENTAL CLINIC patients with 137 nursing students in program low income. 360 total nursing hours “Dentistry is no longer 54 health or social services referrals by nursing students just about 7 pre-diabetic referrals by nursing students the mouth. It’s about the whole person. The mouth is the gateway to our entire body and can tell a story about health conditions,” says Barbara
Sollner, RN, MSN, assistant professor at Baker University. ”Nurses are an integral part of the dental team, and this model of care incorporates nurses’ insights and expertise with regard to the health of the patients.”
Baker nursing students participate in eight-week sessions where they volunteer in the clinic twice a week and perform basic physical assessments. The partnership allows students to gain valuable clinical experience while being supervised by Baker nursing faculty. If students discover a possible health issue in a patient, such as high blood pressure or high blood sugar that requires medical follow-up, their findings are shared with clinic staff to assist with the patient’s plan of care.

The nurse clinical care manager in the dental clinic also provides nursing services, care management and care coordination in an effort to improve overall health outcomes. This includes performing patient assessments to identify any economic or social conditions that might lead to health challenges. Referrals to primary care, specialty care and social services are made when needed. The unique collaboration has allowed the clinic to provide expanded services, with the opportunity for additional future growth.
When words aren’t enough: using art therapy as a gateway to healing
Mount Saint Vincent provides mental health treatment, Mount Saint Vincent, helped the mostly nonverbal Kaylee foster care services, preschool through eighth grade work through her feelings. education, and trauma-informed training – all focused on children and their families. At the same time the lengthy court process to terminate Providing psychological parental rights was occurring, treatment in the form of cognitive Kaylee created a complex behavioral therapy for children painting that appeared to be a can often look different than metaphor of what was happening talking to a therapist about with her family. In the painting, thoughts and feelings. If you she depicted objects smashing are a young girl whose ongoing into one another, careening physical abuse began when you were an infant, you may not even “It’s as if she’s a different child.” wildly and breaking apart. have the words or capability to Mount Saint Vincent Art Therapist Lindsay Ritscher “It was a terribly sad but beautiful describe your experiences. That metaphor of what she felt,” is why Mount Saint Vincent’s highly trained therapists use Ritscher recalls. “She processed the loss and pain of many alternative methods, including art therapy, to treat losing her parents using art as a symbolic means of the youngest survivors of trauma. communication.” Kaylee, age 10, arrived at Mount Saint Vincent after three Gradually, Kaylee began to connect with Ritscher as well as years of numerous foster care placements. With a long with her classroom teacher. Strong bonds began to form, history of physical abuse and chronic neglect, she was signifying a turning point. Today, she is a star student and disconnected from life and rarely engaged with others, eager participant in class. The violent behavior is gone, preferring to isolate herself in her imaginary world. 2019 STATS | MOUNT SAINT VINCENT trauma-informed caregiving training and she is happy, smiling and joking with students and staff. During her stay, the parental rights of Kaylee’s parents 44 sessions led by staff and presented throughout Colorado, resulting in 142 total hours training for 708 individuals In large part, Ritscher credits Kaylee’s treatment at were terminated. She became severely depressed, would 16 Front Range school districts served by the K-8 school Mount Saint Vincent for her transformation. have violent outbursts and suffered from uncontrollable bouts of crying. Lindsay 93 95 % % satisfaction rate for Residential Program satisfaction rate by referral sources for educational services their clients received “No matter what Kaylee did, no matter what behaviors she exhibited, she was always Ritscher, Art Therapist at 100 % discharge rate to less-restrictive setting for clients in short-term Stabilization Unit received with kindness, love and compassion.”










