
8 minute read
Preventing Stillbirths
by RANZCR
$750,000 over two and a half years to the College to improve professional capacity provide stillbirth investigations
Stillbirth is defined in Australia as the birth of an infant after 20 weeks of gestation or weighing at least 400 grams where there are no signs of life at delivery. The World Health Organization defines stillbirth as the birth of an infant at either less than 28 weeks of gestation or weighing less than 1,000g with no signs of life.
Based on the Australian definition, each day six stillbirths occur, with stillbirths accounting for 7.7 of every 1,000 registered Australian births in 2020. Preventing late gestation (after 28 weeks of gestation) stillbirths is a particular focus of the National Stillbirth Action and Implementation Plan; the Plan supports a sustainable reduction in rates of preventable stillbirth after 28 weeks, with a primary goal of 20 per cent or more reduction over five years. 1
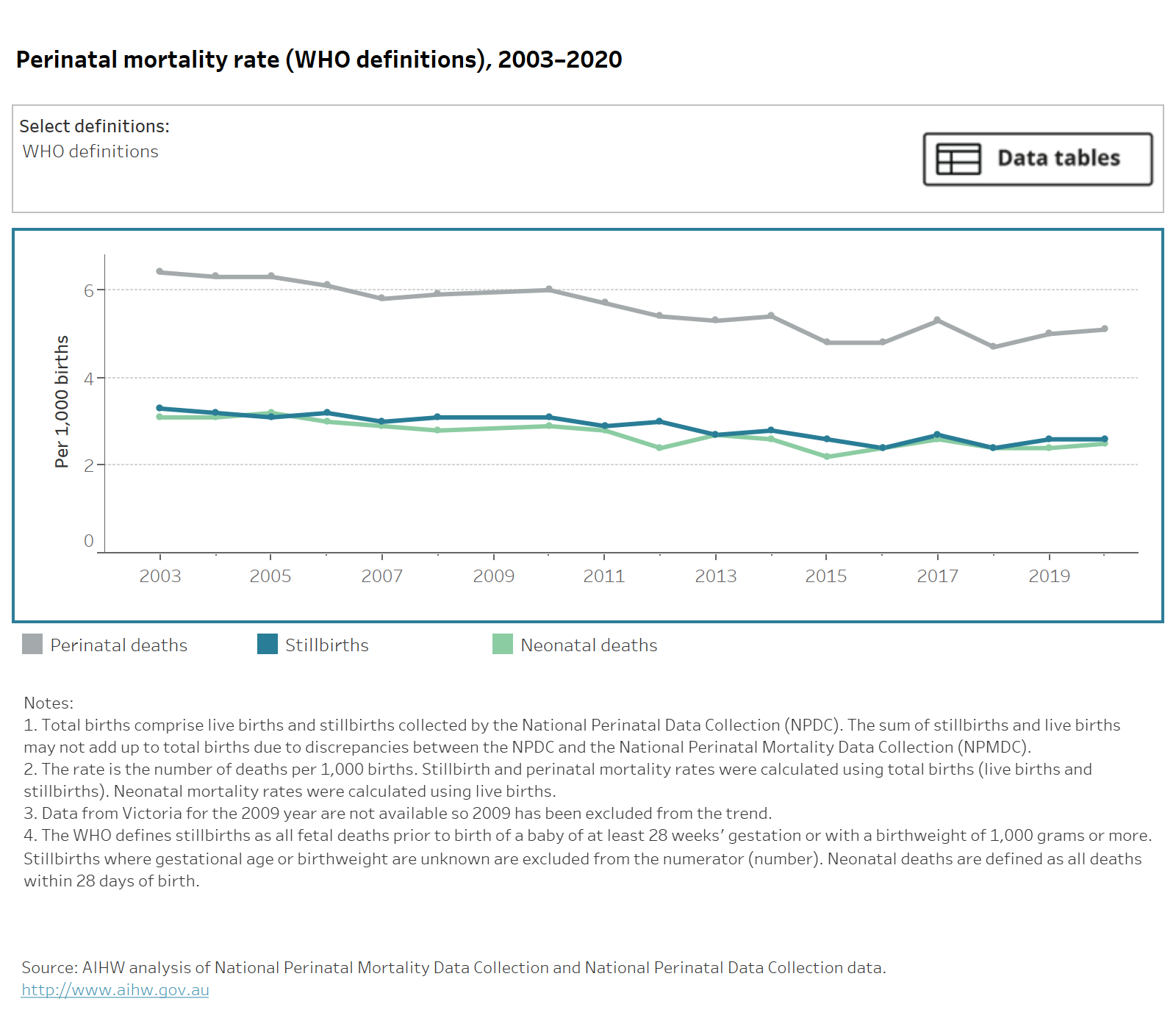
Recent data reported by the Australian Institute of Health and Welfare suggest the rate of preventable stillbirths may be falling. 2 The rate of late gestation stillbirths in Australia (those occurring in the third trimester of pregnancy) has decreased from 3.5 to 2.6 per 1,000 births between 1999 and 2020 (see Figure 1.).
The National Stillbirth Centre for Research Excellence (CRE) “Safer Baby” initiatives (including smoking cessation, side sleeping, recognition of reduced fetal movements, decision-making about delivery timing, and monitoring of fetal growth), have likely made a significant contribution to the decline in late stillbirth.
These statistics do not begin to convey the devastation felt by families who experience stillbirth. Grief, guilt and feelings of personal responsibility for the stillbirth, especially when the cause of stillbirth is unknown, can result in relationship breakdown, loss of time at work and loss of employment altogether, and an inability to function fully as parents to other children. Stillbirth can prevent contemplation of future pregnancies, due to fears of losing another baby. The so-called “intangible” economic costs to families and to society in general as a result of stillbirth are poorly quantified and mostly unrecognised. 3
Despite perinatal autopsy, genetic and other testing, and placental analysis, unexplained antepartum death is recorded as the cause of 22 per cent of stillbirths; congenital anomalies account for another 30 per cent of stillbirths; these include pregnancy termination for suspected congenital anomalies following prenatal imaging and other diagnostic testing.
The National Stillbirth Action and Implementation Plan, published in December 2020, recognises stillbirth as a public health issue. The Plan was developed by the Australian Government Department of Health as a result of one of the recommendations of the Report of the Senate Select Committee on Stillbirth Research and Education. The Plan includes short, medium and long-term actions that aim to reduce stillbirth, ensure families affected by stillbirth receive respectful and supportive care and address higher stillbirth rates in disadvantaged communities.
One of these actions is addressing the need to improve investigation of the cause(s) of stillbirth: understanding causation is fundamental to prevention. Traditionally, stillbirths have been investigated with conventional autopsy performed by a perinatal pathologist, supplemented by placental histopathology and testing for intrauterine infection and maternofetal haemorrhage.
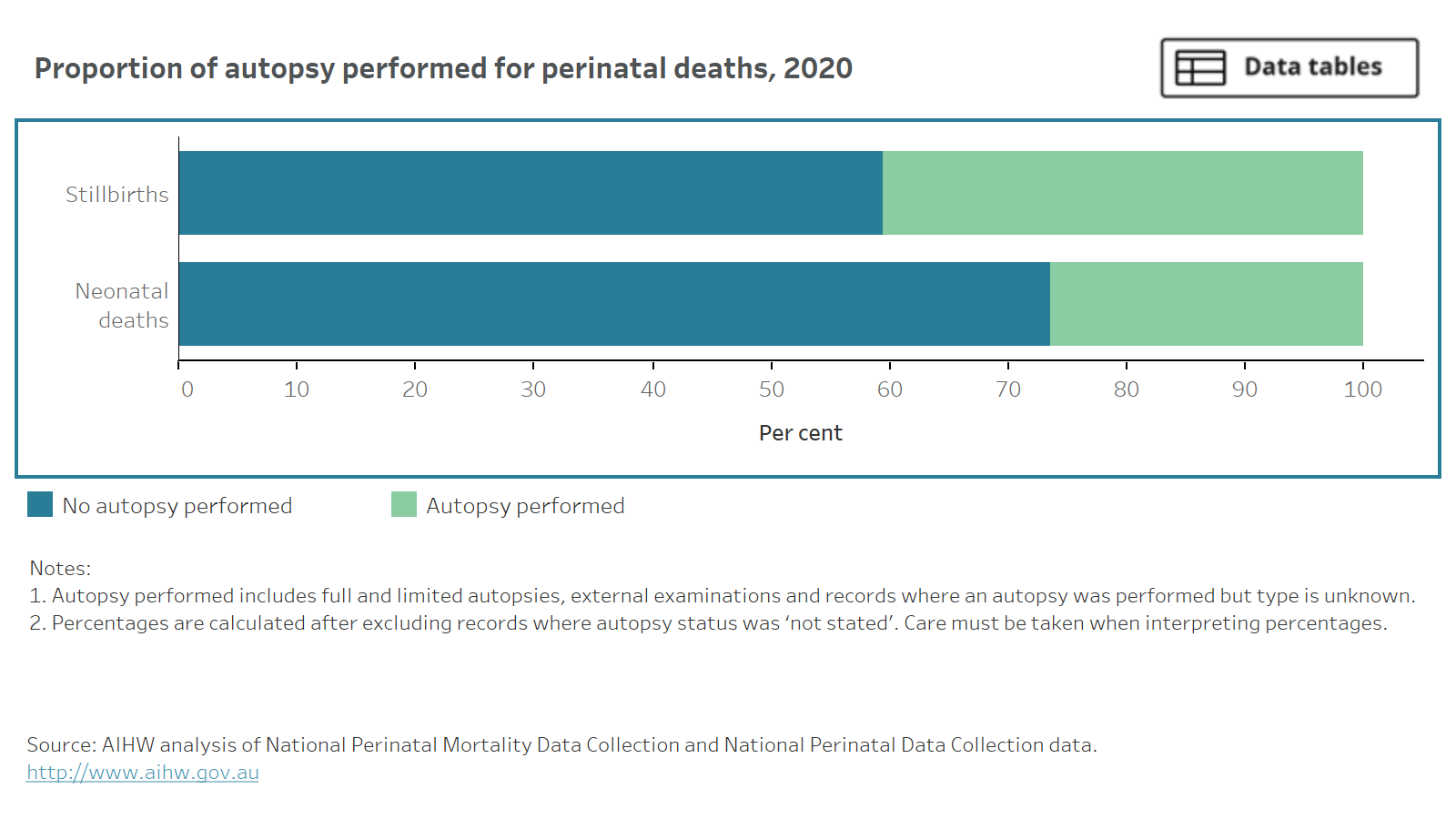
However, only 40 per cent of Australian stillbirths were investigated with any form of autopsy in 2020, down from 52 per cent in 2018. Furthermore, only half of autopsies in 2018 were conventional full autopsies, the remainder being limited to external examination of the fetus; these data are not yet available for 2020.
Autopsy refusal following stillbirth in Australia and internationally has increased for decades. Although it is often assumed that cultural and religious practices are the main reasons for autopsy refusal, surveyed parents often state that it is the thought of having their baby’s body cut that makes them refuse. 4
The Australian Institute of Health and Welfare does not report on rates of indeterminate or failed perinatal autopsy due to post-mortem maceration of the fetus; the published rate is approximately 15 per cent for fetal autopsy performed within one to seven days following death. Failed post-mortem examination of the fetal brain due to maceration is even more frequent.
The national shortage of perinatal pathologists in Australia and long delays in providing autopsy reports to families has received national attention (bit.ly/SMHStillbirthReportBacklog). Such delays were identified in the National Stillbirth Action and Implementation Plan as a major source of distress for bereaved parents. 1
Research over the past decade supports non-invasive or minimally-invasive perinatal post-mortem examination with MRI as a clinically valuable adjunct to fetal autopsy, enabling targeting of biopsies and more limited examination, but also as a substitute for autopsy when this is refused7–13. Radiologists are ideally placed to perform and interpret these studies and to integrate prenatal imaging findings with post-mortem MRI and radiography to create an integrated report and diagnosis.
Recognising the important role of medical imaging in the twenty-first century stillbirth investigation, the Australian Department of Health and Aged Care (DoHAC) provided funding in the May 2021 Federal Budget of $750,000 over 2.5 years to the College to improve professional capacity provide stillbirth investigations. The RANZCR Stillbirth Investigations Steering Group (Prof Stacy Goergen (chair), Drs Glen Lo, Padma Rao, Nira Borok, and A/Prof Ajay Taranath) provides governance oversight of this project on behalf of the College.

The College has collaborated with the Stillbirth CRE, Red Nose and the Royal College of Pathologists of Australasia to develop and deliver surveys of bereaved parents, obstetricians, radiologists, perinatal pathologists, obstetricians and midwives to evaluate their experience of investigation of stillbirth; more than 120 bereaved parents and more than 60 obstetricians and midwives have responded to the surveys. The College is especially grateful to Red Nose for helping to achieve such a large parent response.
In addition to the surveys, which will inform development of patient and clinician information, consent forms, and practical technical guidance for radiologists, the College is sponsoring a webinar series in collaboration with the European Society of Paediatric Radiology Post-mortem Imaging Taskforce between November 2022 and May 2023.
The series forms the foundational component of the College’s education program for radiologists (bit.ly/ RANZCRTrainingPrograms). The advanced component will be delivered as a face-to-face course and symposium in Melbourne on 4 and 5 August 2023 featuring Prof Owen Arthurs (Great Ormond Street Hospital / University College London), A/Prof Wilhelmijn Klein (Radboud University Medical Centre, The Netherlands), and Prof Teresa Victoria (Massachusetts General Hospital / Harvard Medical School) supported by local experts in stillbirth research, forensic pathology, and post-mortem radiology. Register here: bit.ly/RANZCRSIPWebinars
The grant to the College is a national recognition of the need for a modernised, multidisciplinary and collaborative approach to the investigation of stillbirth. The funding will help to make available stillbirth investigations that are co-ordinated, evidence-based, acceptable, timely and most importantly, that help families understand why their baby died.

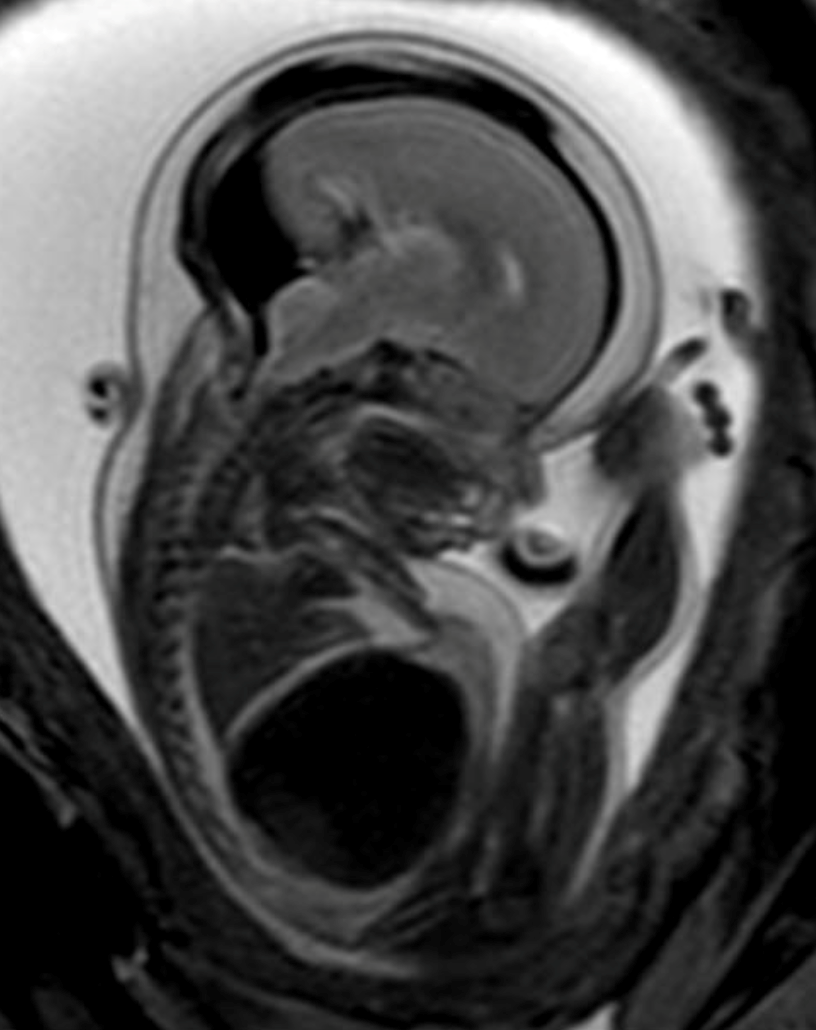
Post-mortem MRI demonstrating multilevel segmental spinal dysraphism in a fetus with rhombencephalosynapsis and VACTERL-R related to poorly controlled maternal diabetes.
In utero post-mortem MRI <24 hours following discovery of fetal death in utero on ultrasound. Arrow points to a large dural sinus malformation potentially causing fetal death by cardiac overload due to A-V shunting through the malformation.
References
1 https://www.health.gov.au/resources/publications/national-stillbirthaction-and-implementation-plan (accessed February 6 2023).
2 AIHW (2021) Stillbirths and neonatal deaths in Australia 2017 and 2018, Perinatal statistics series no. 38. Canberra. p.4.
3 Ogwulu, C.B., Jackson, L.J., Heazell, A.E. et al. Exploring the intangible economic costs of stillbirth. BMC Pregnancy Childbirth 15, 188 (2015).
4 Lewis C, Hill M, Arthurs OJ, Hutchinson C, Chitty LS, Sebire NJ (2018) Factors affecting uptake of post-mortem examination in the prenatal, perinatal and paediatric setting. BJOG 125:172–181
5 Breeze AC, Jessop FA, Set PA, Whitehead AL, Cross JJ, Lomas DJ, Hackett GA, Joubert I, Lees CC. Minimally-invasive fetal autopsy using magnetic resonance imaging and percutaneous organ biopsies: clinical value and comparison to conventional autopsy. Ultrasound Obstet Gynecol. 2011; 37(3):317–23.
6 Thayyil S. Less invasive autopsy: an evidenced based approach. Arch Dis Child. 2011;96(7):681–7.
7 Weustink AC, Hunink MG, van Dijke CF, Renken NS, Krestin GP, Oosterhuis JW. Minimally invasive autopsy: an alternative to conventional autopsy? Radiology. 2009;250(3):897–904.
9 Arthurs OJ, Thayyil S, Owens CM, Olsen OE, Wade A, Addison S, Jones R, Norman W, Scott RJ, Robertson NJ, et al. Diagnostic accuracy of post-mortem MRI for abdominal abnormalities in foetuses and children. Eur J Radiol. 2015;84(3):474–81.
10 Arthurs OJ, Thayyil S, Pauliah SS, Jacques TS, Chong WK, Gunny R, Saunders D, Addison S, Lally P, Cady E, et al. Diagnostic accuracy and limitations of post-mortem MRI for neurological abnormalities in fetuses and children. Clin Radiol. 2015; 70(8):872–80.
11 Taylor AM, Sebire NJ, Ashworth MT, Schievano S, Scott RJ, Wade A, Chitty LS, Robertson N, Thayyil S, Magnetic Resonance Imaging Autopsy Study Collaborative G. Post-mortem cardiovascular magnetic resonance imaging in fetuses and children: a masked comparison study with conventional autopsy. Circulation. 2014;129(19):1937–44.
12 Ben-Sasi K, Chitty LS, Franck LS, Thayyil S, Judge-Kronis L, Taylor AM, Sebire NJ. Acceptability of a minimally invasive perinatal/ paediatric autopsy: healthcare professionals’ views and implications for practice. Prenat Diagn. 2013;33(4):307–12.
13 Persson A, Lindblom M, Jackowski C. A state-of-the-art pipeline for post-mortem CT and MRI visualization: from data acquisition to interactive image interpretation at autopsy. Acta Radiol. 2011;52(5):522–36.










