4 minute read
better patient outcomes
Surgical professionalism paramount for better patient outcomes
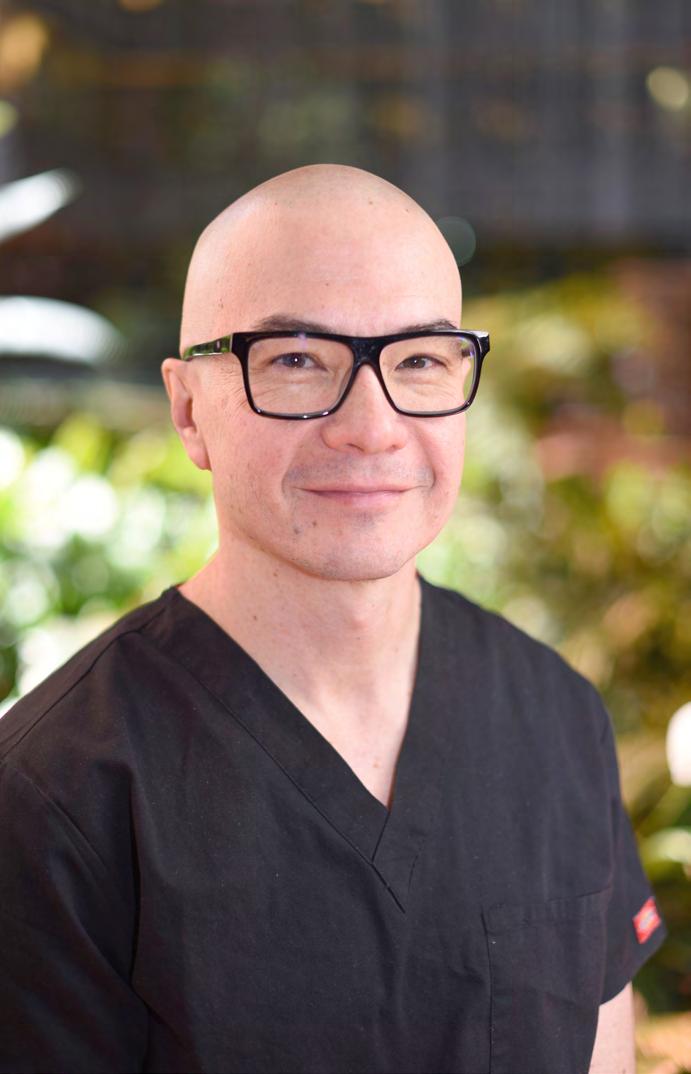
The Royal Australasian College of Surgeons (RACS) is globally recognised for its leadership in implementing a longterm program of work to build respect and increase patient safety in surgery. For a fresh lens on cultural change in the health sector, RACS spoke to closerange observer of health sector culture Dr Mark O’Brien, the medical director of the Cognitive Institute, which operates across Australia, New Zealand, Singapore and the United Kingdom. He is also the international program lead of Risk Prevention for the Medical Protection Society, United Kingdom and a Board Director at St John of God Health Care, Australia. A growing understanding of the link between non-technical performance and patient safety is shifting the culture of medicine and increasing the value placed on professionalism, according to Medical Director of the Cognitive Institute, Dr Mark O’Brien. But he suspects the big drivers of future cultural shifts in Australian health care will be generational change, closer links between funding and patient outcomes and the impacts of COVID-19. “There’s already really great data to show that professionalism matters a lot. There are more infections, more complications and more re-admissions because of the impact of unprofessional behaviour on coordination of care,” he said. Into the future, Dr O’Brien is looking out for the cultural impacts of tighter links between patient outcomes and funding. “Internationally there is a very significant trend among healthcare funders to move the dial on payment for healthcare services away from ‘process’ to ‘outcome’. The drivers and incentives are changing, and the focus is shifting from doing things, to rewarding the results,” Dr O’Brien said. This is where the role of professionalism and a healthy culture comes in. The best patient outcomes result from optimal “communication, coordination, teamwork, professionalism, engagement with your college and professional development – not just whether you did a technically good operation,” he said. Dr O’Brien said COVID-19 will accelerate that trend, with the resulting recession increasing pressures on healthcare funding, possibly reducing rates of private health insurance and patients’ capacity to fund out-of-pocket expenses. “I’m not sure anyone knows exactly how the dust will settle, but I do think there will be significant change in the next 18 months. I suspect these pressures will see a focus by funders on value for money and patient outcomes that we haven’t seen before,” he said. Another emerging aspect of cultural change is generational, with generations X and Y adopting a different model of professionalism. “Younger professionals seem more willing to sacrifice some autonomy in exchange for security, access to leave, lifestyle and work conditions. In general, they don’t want to manage the business of being a doctor and are happier being managed than previous generations,” he said. And then there is the impact of increased procedural complexity. “We are doing things now that we wouldn’t have dreamed of doing 30 years ago, and these advances have increased the pressure and stress on doctors,” he said. But resilience and burnout also affect professionalism, and Dr O’Brien said he wonders if this is another area in which the impact of COVID-19 will be felt. “How can surgeons boost resilience and avoid burnout – for themselves and for their teams? If they’re flagging, there will be poor patient outcomes,” he said. Dr O’Brien’s approach to professionalism is expressed in the ‘Speak Up for Safety’ programs that the Cognitive Institute has developed. This is linked to the Vanderbilt University’s ‘Promoting Professional Accountability’ program of work, which guided RACS’ Action Plan: Building Respect, Improving Patient Safety. RACS’ face-to-face Building Respect training and Speak Up app are specifically designed to support surgeons to speak up for the culture they want to be part of. Dr O’Brien quotes Professor Charles Vincent, “the Oxford guru on patient safety”, and his conviction that a ‘speaking up’ culture is central to patient safety. “If you don’t have a speaking up culture, it will undermine everything else you do,” Dr O’Brien said. “We look at everything through a patient safety lens, rather than a clinician behaviour lens.” When it comes to patient safety and high performance, Dr O’Brien sees bullying and harassment as “a microcosm of a bigger picture”. “Bullying and harassment are a subset of a range of performance-disabling issues that can manifest in a team,” he said. Dr O’Brien is positive about RACS leadership in this area and encourages the College to be “aspirational around high performance” and to continue to prioritise professionalism, emotional intelligence and resilience, as well as technical skills, in selecting surgical leaders.
Advertisement
He asks whether professionalism holds the key to unlocking exceptional performance more widely in health care. “What mindset, emotions and environment do you create for superior performance? It’s not just about intelligence and technical ability, but we have yet to identify the systems, teamwork and processes that will create a high safety, high performance culture,” Dr O’Brien said.