4 minute read
Science Update: A Potential Sex difference in Stress Response
Long-term stress is on the rise, thanks to recent crises like the COVID pandemic, rampant inflation, progressive reduction in legally-protected freedoms, and a continuous occurrence of climate disasters. This is particularly concerning because excessive stress can contribute to both mental illness like depression and anxiety, and impairments of physical health, including heart disease and reduced immune function. We face potential stressors on a daily basis, but how individuals respond to stress will vary based on a variety of factors - including, potentially, physiological sex. A study recently published in Neuropsychopharmacology suggests that even when the same stress mechanism is activated in the brain, sex might play a role in how we respond.
When approaching the topic of sex differences, it can be easy to fall victim to gender essentialism—equating gender identities, roles, or presentations & associated cultural beliefs with (biological) sex based attributes—which can cloud our judgement and lead to biased conclusions. However, sex differences in physiology do affect health outcomes. The same disease may tend to have different symptom profiles in people of different sexes. Identifying sex differences in behavioral responses and disorders, including stress-related disorders, can help to better understand & treat them.
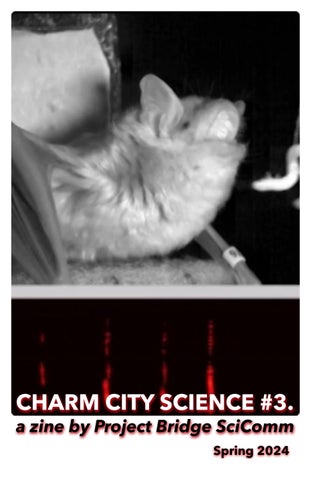
During stressful experiences, various types of neurons in the brain are activated and release stress related hormones. By using experimental tools to selectively activate one such class of neurons - corticotrophin releasing factor neurons - over a period of several weeks, researchers in the Bale Lab at the University of Maryland were able to induce a chronic stress response in mice without any actual stress-inducing experience. The mice exhibited hormonal activity characteristic of a stress response, and were more sensitive to touch, another common indicator of stress.
Crucially, the researchers noticed some differences between how male and female mice responded to activation of the corticotrophin releasing factor neurons. Female mice showed more signaling of a stress hormone called corticosterone. However, male mice were less physiologically resilient to changes in stress hormone levels, experiencing weight loss despite having smaller increases in stress signaling. In contrast, female mice did not experience weight loss, but exhibited more fear-related behaviors in response to stress neuron activation than male mice. Because chronic stress increases risk of neuropsychiatric disease, these results might offer an explanation for why susceptibility to different conditions varies across sex in human. For example, the elevated sensitivity of male mace to changes in stress hormones mirrors the elevated vulnerability of male patients have to schizophrenia, which is triggered by both genetic and environmental risk factors (i.e. stress). Female survivors of traumatic events are more likely to develop PTSD, which may be related to heightened fear response seen in female mice.
As It turns out, sex differences in stress response have been directly observed in humans as well. Like male mice, people assigned male at birth have a greater physiological response to stress. But unlike mice, human males actually have more stress hormone signaling in response to stress than females. Because males experience a higher physiological stress response, stress may also have a more detrimental effect on their immune systems . Being in a state of chronic stress alters the way our body reacts to everyday stressors. With stress consuming a greater portion of the American consciousness, understanding the various factors—including sex—that contribute to our stress response may help us to better manage stress and the toll it takes on our physical and mental health - Mira Swartzlander,PhD Student, JHU-SOM Neuroscience
https://www.apa.org/news/press/releases/stress/2023/collective-trauma-recovery.
Lundberg, U. (2005). Psychoneuroendocrinology. DOI: 10.1016/ j.psyneuen.2005.03.014.
Montgomery, K. R. et al. (2024) Neuropsychopharmacology. DOI: 10.1038/s41386-023-01739-5
Verma, R., Balhara, Y.P. S. & Gupta, C. S. (2011). Ind. Psychiatry J. DOI: 10.4103/0972-6748.98407 5. Li, X., Zhou, W. &Yi, Z. (2022) Gen. Psychiatry. DOI: 10.1136/gpsych-2022-100823
Li, X., Zhou, W. &Yi, Z. (2022) Gen. Psychiatry. DOI: 10.1136/gpsych-2022-100823
Wahbeh, M. H. & Avramopoulos, D. (2021) Genes. DOI: 10.3390/genes12121850
Tolin, D. F. & Foa, E. B. (2006)Psychol. Bull. DOI: 10.1037/0033-2909.132.6.959
Kudielka, B. M. &Kirschbaum. (2005) Biol.Psychol. DOI: 10.1016/ j.biopsycho.2004.11.009
Roelfsema, F. et al. (1993) J. Clin. Endocrinol. Metab. DOI: 10.1210/jcem.77.1.8392084
Segerstrom, S. C. & Miller, G. E. (2004) Psychol. Bull. DOI: 10.1037/0033-2909.130.4.601
Yehuda, R. (2002) Psychiatr. Clin. North Am. DOI: 10.1016/s0193-953x(02)00002-3
Carpenter, L. L. et al. (2007). Biol. Psychiatry. DOI: 10.1016/j.biopsych.2007.05.002