14 minute read
From the CEO
Spring has sprung.
From the CEO
Advertisement
Welcome to our Spring edition of Pallium! We hope this edition finds all PCNSW members and their families well after what has been a tumultuous few months. We would first and foremost like to acknowledge the amazing job healthcare workers across NSW have done throughout this recent lockdown. Your tireless contributions do not go unnoticed or unappreciated and we are extremely grateful for all that you continue to do. As we move out of lockdown and into a COVIDnormal lifestyle we recognise there will likely be more challenges ahead, and we hope that you will contact us if there is anything we here at PCNSW can do to support you or your service.
Most recently we enjoyed seeing many of you virtually at the Oceanic Palliative Care Conference. There were some wonderful presentations and workshops. Although we missed seeing everyone in-person for a cheeky drink at the end of each day we came away feeling inspired and motivated at the end of the conference. We hope you did too! You can still register at a much reduced rate if you would like to see it all, or you can watch it at any time for 12 months if you are a delegate.
Speaking of conferences, we are excited to remind you all that our Biennial Conference will be going ahead in November 2022 in Terrigal. We are looking forward to reconvening with the Conference Organising Committee on the Central Coast to plan an amazing, in-person learning and networking experience for us all! Stay tuned for more details in the coming months. 3–6 November 2022: Save the date and book your leave now!
Thank you to everyone who has renewed your membership for 2021–22! We have been thrilled to see so many new members join this year and look forward to working together with you all over the next year. We value all of your contributions to Pallium and member emails and can’t wait to see you at future online and in-person education programs and social events that we are hoping will be more frequent moving forward!
As many of you will be aware, Alex Greenwich MP introduced a new Bill into NSW Parliament last week, the Voluntary Assisted Dying Bill 2021. PCNSW has been consulting with various Members of Parliament and others to discuss the importance of supporting and funding palliative care. We continue to have these discussions and advocate on behalf of our members and the general public to ensure everyone in NSW has equitable access to high quality palliative care where and when they need it. If you would like to read more about the PCNSW position statement regarding Voluntary Assisted Dying you can find more information on our website. Go to members area login, click on ‘Let’s Talk About’ and open the VAD link.
Thank you to our members who have contributed to this wonderful edition of Pallium. As a member of PCNSW we encourage you to engage with us throughout the year, feel free to submit research, stories and photos to include in our fortnightly member email as well as the quarterly Pallium editions.
Linda Hansen
PCNSW Chief Executive Officer

Conference wrap up
Over 1000 delegates from across the globe attended the 2021 Virtual Oceanic Palliative Care Conference (21OPCC) on 7–10 September 2021
21OPCC’s theme, Invest Challenge Change, builds on the continuing global push to ensure that we build better, more resilient health systems designed to meet critical health and palliative care needs in normal circumstances, and are sufficiently resourced to meet needs during times of emergency and crisis. Conference delegates identified the priority actions that represent their commitment to ensuring access to quality palliative care for all, across all Oceanic nations. Download Conference Statement. INSPIRING SESSIONS

One of the most inspiring sessions was the opening plenary with a rousing call for palliative care professionals and services to fight racism and other injustices in their sector and the broader health system, and to put equity at the heart of their work. It was delivered by Dr Naheed Dosani, a palliative care physician and health justice advocate, who is the founder of a mobile palliative care service for the homeless in Toronto, Canada. At PCNSW we were particularly interested in Dr Dosani’s presentations as we are currently developing a program for homelessness and equity of access to palliative care support and services. To hear of Dr Dosani’s work and experience in this sector is timely and inspiring for us as we work towards one of our mission goals of improving equity of, and access to, quality care for everyone, regardless of their circumstances. Here is a short excerpt of Dr Dosani’s opening session: “There’s a growing recognition of the limits of how we deliver health care to marginalized populations. From the most superficial level to the deepest roots in society, we can have an impact through the lens of equity, health, and empathy. To what degree we make that change, is up to each one of us.”


With a focus on palliative care equity for people experiencing structural vulnerabilities, Dr. Dosani’s inspiring work as founder of Palliative Care and Education for the Homeless (PEACH) a program of the Inner City Health Associates in Toronto, bridges the themes of the Oceanic Palliative Care Conference. PEACH is a mobile, casemanagement, and community-based palliative care approach tailor-made for society’s most marginalized people. This includes individuals experiencing structural vulnerabilities such as homelessness, poverty, substance use, mental illness, and social isolation.
COVID IMPACT
Another area of great interest to PCNSW from the conference was the very strong representation of health professionals all around the world who have used the unanticipated opportunities that the COVID-19 pandemic has presented to drive improvements in care for people nearing end of life. In this issue of Pallium we will hear firsthand from some of our own members in the front-line of care who have been confronted by COVID challenges and how they have rallied to the call. We take inspiration from other countries who are adapting to the changes in our work environments, particularly from the UK, where learning from policy and practice during a pandemic has highlighted the driving need to close the “evidence-policy” gap in striving for improvements in palliative care. Access full session: The future of palliative care in the UK: Learning from policy and practice in a pandemic. And finally, thank you to our own CEO Linda Hansen, who chaired Concurrent Session: Diverse Needs Group on day 4 of the conference. Session topics included the harrowing experience of an asylum seeker dying from cancer, provision of care in prison and understanding the LGBT+ community wishes for palliative care. Access full sessions. Linda was also the driving force behind assembling the virtual choir to sing us out of the conference with a rousing rendition of Queens’ famous rally cry, “We are the champions”. All those working in palliative care during these tough times, indeed you are!
21OPCC ON-DEMAND A reminder that delegates can access conference content over the next 12 months. If you missed the conference, you can still register for 21OPCC post-conference on-demand content.

In their own words
COVID-19 has left no healthcare sector untouched in NSW. It is a subject that is widely discussed about how we have adjusted, reacted to and prepared for this unprecedented health crisis.
We spoke to a few of our frontline health services members to hear in their owns words how they have coped with and adjusted to the impact of a pandemic in their workplace. In the interest of patient privacy and workplace protocol, our contributors will remain anonymous.
B is a Community Palliative Care Nurse who works primarily in South-West Sydney
Covid has meant that there are more patients at home who otherwise would be in hospital or palliative care units. We have had patients taken out of residential aged care facilities because their families could not visit them. Patients are generally worried on top of their usual worries. Trying more than ever to keep people at home. Being in an LGA of concern means that patients and their relatives have to have a swab before every face-to-face appointment at hospital AND if they are coming in to a PCU.
Concern about catching COVID but more concerned about unwittingly giving COVID to a patient or their family at home. Worrying about providing care to patients with COVID at home and if I will use the PPE correctly. COVID seems to have affected every single aspect of the care we provide. Other services are not visiting but we still are.

Be prepared. Read up all your procedures. Have your PPE at the ready. I was a close contact of a positive patient and I wore full PPE because I knew the family would prefer that. He had a terrible cough in his small poorly ventilated bedroom. No one suspected COVID but he tested positive when I sent him to PCU. Poor man died alone in a COVID ward.
We certainly have learned how to use telehealth and have found that it can be quite effective in some cases. I am overwhelmed by the resilience of families who have learnt to facilitate telehealth and provide care at home rather than in hospital. They have been so patient with all the PPE and questions about being in contact with anyone with COVID, every single time.
Is there anything else you would like to share about your experiences?
We are even more short of staff since COVID due to staff attrition to other areas. Some staff have left nursing because of COVID and vaccination requirements. I wish I could retire myself.

C is a Palliative Care Nurse serving the CALD community
COVID has increased the number of virtual and phone consultations. In CALD patients, it means an extra layer of challenge when a CALD patient is unable to navigate the English virtual app. It increased the use of interpreters on phone for the COVID safe questionnaire prior to each home visit.
Zero direct skin contact due to full PPE on each home visit. It was challenging to ask family members and friends who don’t usually live in the same household to withhold or cancel their visit on the same day or leave the room when health professionals arrived. Option of work from home has reduced face to face time with colleagues and reduced informal debrief time. Delayed support from volunteers in CALD charity groups due to restrictions for visits and gatherings. What advice do you have for supporting patients and carers during these challenging times?
There’s help in the hospital and community for them. Don’t delay hospital admission. It will only prolong length of stay. For CALD patients – utilise interpreter services for each health consultation so that they can describe their symptoms and concerns in detail and properly understand our advise. Don’t wait till it is too late when visiting from overseas. A number of patients died when their family members were in quarantine. Conditions can change from stable to terminal for people living at the end of their life within two weeks. Seek and accept emotional support.
Virtual care has it benefits. It is working well for multiple family members to be involve in a teleconference with the multidisciplinary team at the same time. This improves communication and reduces duplication.
R is a Clinical Nurse Consultant/Palliative Care, working in rural and remote areas
We have had to move more towards a telehealth model of care and generally only see patients face to face if they are in the unstable or terminal phase.
Professionally, the most challenging impact has been establishing relationships with patients and carers when you can’t meet them face to face and making and maintaining that connection over time. I think it’s often hard to gauge what is happening for patients in the community when you can’t be in their space and see how they are coping. The need to quickly skill up on the use of telehealth technology at the beginning of the pandemic was a challenge and I know some of our older patients really struggle with the technology and feel disconnected from the staff when we can’t be in the same room. Personally, the most challenging thing has been being separated from family, this is what “fills my cup” so to speak and I have not seen some of them for nearly two years now because of border closures. Seeing patients and families not being able to be together, not able to attend funerals and witnessing the obvious distress this causes as well as sometimes bearing the brunt of their frustrations and grief is hard. Particularly when they don’t understand that we are not the ones making the rules.
I think really learning how to use technology to the best of our advantage particularly in rural and remote settings.
Be kind, be compassionate, we are all tired frustrated and sick of COVID. Nobody was truly prepared for this, and we are learning as we go.

SHARE YOUR STORY
We thank our contributors for their time and for expressing their personal experiences in the line of duty. If you would like to share your own experiences, we would love to publish them. Please contact us at: info@palliativecarensw.org.au


Over 1000 delegates attended the 2021 Oceanic Palliative Care Conference (21OPCC) 7–10 September. In his opening address, The Minister for Health and Aged Care, The Hon Greg Hunt MP paid homage to palliative care staff, volunteers, medical professionals, researchers and carers, for their efforts amid the COVID-19 pandemic, praising them for providing care to ‘our most vulnerable Australians at their most vulnerable time.’ One of the conference highlights was the announcement of the National Palliative Care Awards. Congratulations to all the worthy winners.
PROFESSOR MEERA AGAR’S WELCOME

Professor Meera Agar’s welcome to Palliative Care Australia’s 2021 OPCC.


AND THE WINNERS ARE...
NSW WINNERS
Team – Outstanding Teamwork Award
Dungog Shire Palliative Care Volunteers Inc.
Individual – Excellence in Aboriginal or Torres Strait Islander Palliative Care
Cheryl Porter-Pedras, South Western Sydney LHD, Liverpool
Individual – Excellence in Palliative Care – Paediatric Palliative Care
Associate Professor John Collins, The Children’s Hospital at Westmead (Sydney Children’s Hospital Network) Westmead
Individual – Excellence in Palliative Care in an Aged Care Setting
Yasothiny Yogarajah, BaptistCare NSW & ACT, Macquarie OTHER WINNERS
Individual – Emerging Leader
Dr Graham Grove
Individual – Emerging Researcher
Dr Claudia Virdun
Individual – Excellence in Generalist Palliative Care
Dr Jonathan Ramachenderan
Individual – Excellence in Palliative Care – Community Based Care
Dr Paula Moffat
Individual – Excellence in Palliative Care – Rural and Remote
Robyn Ellis
Individual – Outstanding Achievement by a Volunteer
Keri Wassenaar
CONGRATULATIONS TO ALL THE WORTHY WINNERS!
Community
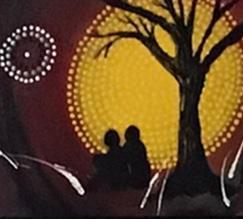
PCA ART COMPETITION
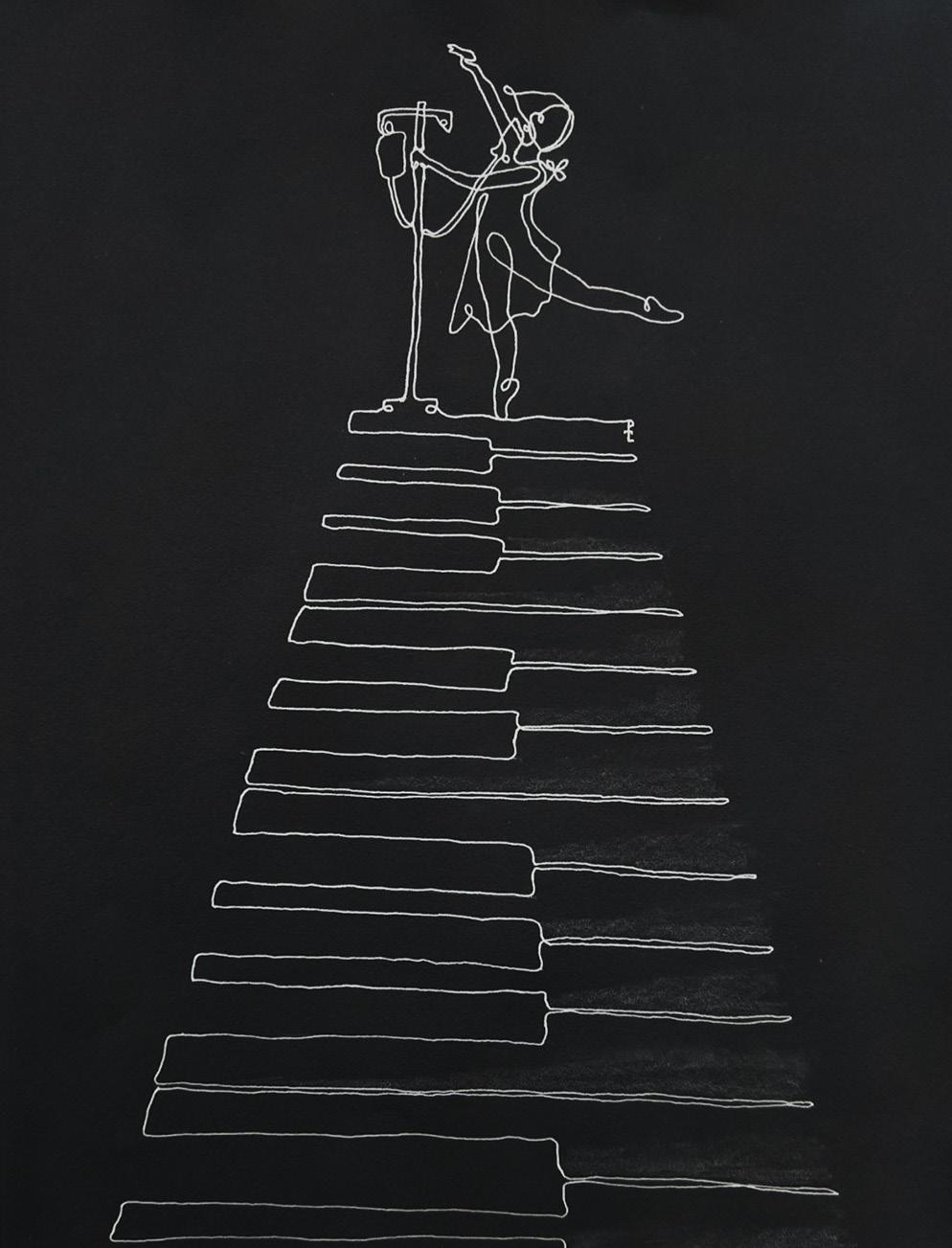
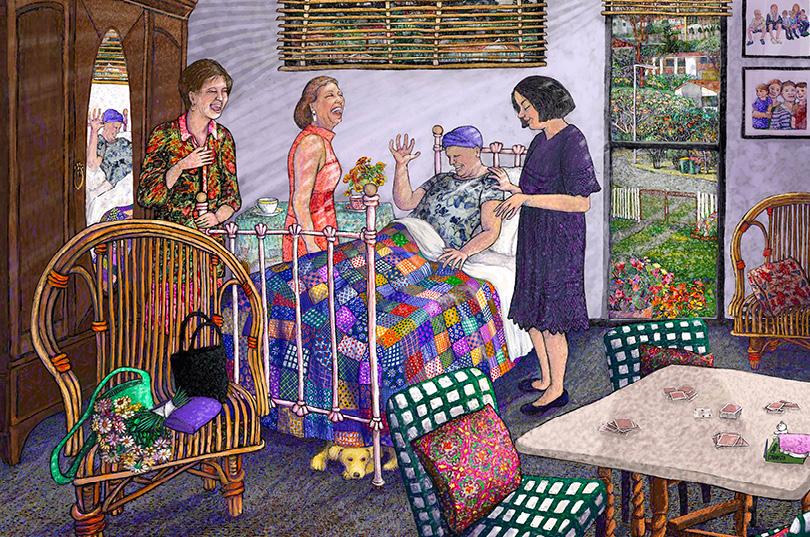
This year’s competition saw over 300 artists of all ages creatively depict the theme ‘Live as well as possible, as long as possible’. The theme explores how palliative care improves quality of life for people with life-limiting conditions, helps people participate in activities that are important to them, and creates opportunities for love, laughter and fulfilment. A big congratulations to the 2021 winners. View the full gallery of entries online. DID YOU SEE ALL KNOW? ENTRIES
First Nations Artist Award: ‘Life Death Life Journey’ by Robyn Chilcott

People’s Choice Award: ‘Not the Last Dance’ by Phyllis Tay. Young Artist Award: ‘Life is Only a Holiday’ by Rebekah Dinning.