
13 minute read
Treatment of Class II Division I malocclusion with deep bite
Treatment of Class II Division I malocclusion with deep bite in mixed dentition requiring early interceptive orthodontic treatment of arch development and expansion
By Dr How Kim Chuan, Dr Kevin Ng and Dr Manjusri Lim
Advertisement
CASE DESCRIPTION
The male patient was 12 years old at the time of the fi rst presentation and appeared to have delayed dental development. His parents were concerned about his protruding upper incisors.
CLINICAL PRESENTATION
The patient was presented with Class II Division I malocclusion in mid-mixed dentition, moderate deep bite with increased overjet. He appeared to have an increased height in the middle facial one-third, convex profi le, and lips that are incompetent at rest. Gummy smile can also be seen along with a backward and downward jaw rotation with early signs of vertical maxillary excess. There was a deviation of the upper dental midline towards the right and procumbent lips due to proclined incisors.
CLINICAL FINDINGS
• Mixed dentition stage with Class II Division I incisor relationship • Late dental development as multiple deciduous teeth such as 53, 54, 55, 63, 64, 65, 73, 74, 75, and 85 are still present at his age • Complete deep bite to palatal mucosa • Increased anterior overjet of 8mm • Bimaxillary proclination • Gummy smile • Upper dental midline deviation to the right by 1mm and lower dental midline deviation to the right by 3mm • Class I permanent molar relationship on both sides • OPG shown incipient developing crowding on 13, 23, 33, 43, 17, 18, 27, 28, 37, 38, 47, and 48 • Lateral cephalometric analysis showed retrognathic mandible with slight maxillary prognathism • Skeletal Class I tending to Class II relationship • Slightly high mandibular plane angle • LAFH% lesser than the ideal percentage; indicates a discrepancy in the facial proportion • Approximately 90 degrees interincisal angles, with acute nasolabial angle and shallow labiomental fold
TREATMENT GOALS
• Control vertical maxillary growth by arch development • Reverse vertical maxillary excess and facial growth • Arch development and expansion to allow suffi cient space for permanent dentition to erupt in an ideal position • Stimulate mandibular growth • Reduce overbite • Correct Class II incisor relationship • Correct gummy smile
Fig. 1 Fig. 2 Fig. 3 Fig. 4




Fig. 5 Fig. 6 Fig. 7


Fig. 8 Fig. 9

Figs. 1-8: Intra and extra oral images before treatment Fig. 9: Panoramic radiograph before treatment Fig. 10: Cephalometric radiograph before treatment Fig. 10
Fig. 11 Fig. 12 Fig. 13 Fig. 14 Fig. 15
Figs. 11-15: Initial ClinCheck treatment plan
TREATMENT APPROACH
The patient was recommended treatment with the Invisalign System (clear aligner therapy) as it can align teeth and allow arch development and expansion for maxillary and mandibular growth to a greater extent than other orthodontic systems.
Phase 1 – Pre-eruptive phase The fi rst phase of treatment involved vertical maxillary control. Both upper and lower arches were expanded by 30% to gain space for permanent dentition eruption to prevent crowding. Intrusion on upper anterior was prescribed to reverse vertical maxillary excess and reduce gummy smile. Extrusion of 4mm on lower posterior teeth would reduce deep overbite and facilitate the spontaneous eruption of permanent succedaneous dentition. Pontics were used to replace missing teeth and to maintain space. Class 2 elastic was used to stimulate mandibular growth through soft tissue stretching of condylar. It also provides reciprocal anchorage to restrain forward maxillary growth. Immediate correction of upper anterior overjet was applied.
For skeletal and teeth relationship analysis, diagnostic orthodontic photographic and radiographic records (panoramic radiograph, lateral cephalogram and PA skull) were collected for the patient. Polyvinyl siloxane (PVS) impressions were taken for the development of the ClinCheck treatment plan. A total of 27 upper and lower aligners were determined to be required for the initial treatment phase. The patient was instructed to wear the aligners for 22 hours daily, change it every 14 days, and to wear Class II elastics. The aligner wear change at 14 days rationale is because tooth exfoliation of permanent teeth and jaw growth is a slow but steady process. The aligners are intended to provide a low but steady force to modify growth directions with a velocity consistent to the bodily growth rate. His progress was reviewed at eight-week intervals.
Phase 2 – Eruption phase We believe that low extrusive force is conducive to stimulate deciduous teeth exfoliation simultaneous to permanent spontaneous tooth eruption. Low expansion force with root control stimulates transverse growth. It broadens the arch form to create space for incipient crowding relief. During the active growth phase, this is eff ective in avoiding extraction by stimulating facial growth. Hence, the second phase of treatment focused on further arch expansion and development to achieve an ideal A-P relationship and to gain space for permanent canines to erupt in position. Mesialisation on the lower arch was done to achieve Class I molar and incisor relationship and encourage mandibular growth. A further 20% expansion was prescribed on both upper and lower arch. The space gained was utilised to fully reduce overjet. A total of 26 upper and lower active aligners were used. The patient was instructed to wear the aligners and continue to wear Class II elastics. His progress was reviewed at eight-week intervals.
Phase 3 – Comprehensive phase The fi nal phase of treatment aimed to further improve the occlusion and smile arc. Intrusion on the upper arch by 3mm progressively was indicated as the patient did not like his gummy smile. The intrusion
was approached from incisor to molars to facilitate lower jaw closure to occlusion by auto-forward jaw rotation. Distalisation on the upper arch was done to achieve ideal Class I molar and incisor relationship. A total of 27 upper and lower active aligners were used. The patient was instructed to wear the aligners and his progress was reviewed at eight-week intervals.
TREATMENT DETAILS
Active treatment time • Phase 1: 11 months • Phase 2: 12 months • Phase 3: 8 months Aligners used • Phase 1: 27 upper and 27 lower aligners • Phase 2: 26 upper and 26 lower aligners • Phase 3: 27 upper and 27 lower aligners
ATTACHMENTS
Phase 1 • Conventional rectangular horizontal attachment (3mm) on teeth 16, 26, 36, 46 and 54, and (4mm) on 55, 65, 75, and 85 • Conventional rectangular vertical attachment (3mm) on tooth 63 • Optimised deep bite extrusion attachment on teeth 64 and 74
Phase 2 • Conventional rectangular horizontal attachment (4mm) on teeth 16, 15, 14, 24, 25, 26, 36, 35, 34, 45, and 46 • Optimised rotation attachment on tooth 44
Phase 3 • Conventional rectangular horizontal attachments (4mm) on teeth 17, 16, 27, 26, 37, 36, 47, and 46 • Conventional rectangular vertical attachment on tooth 23 • Optimised root control attachments on teeth 15, 14, 25, 24, 22, 33 • Optimised rotation attachment on teeth 13, 43, and 45 • Optimised multiplane attachment on tooth 12 • Optimised attachment on teeth 35, 34, and 44
RETENTION
Vivera retainers are currently worn by the patient for both the upper and lower dentitions. He has been instructed to use the retainers permanently at night.
TREATMENT OUTCOME
After treatment, all permanent dentition has erupted in an ideal position and orthodontic treatment was completed without extractions of premolars. Through arch development and expansion, permanent premolars and canines were allowed to erupt into a maintained space. The bimaxillary proclination was subsequently corrected and marked improvement in procumbent facial profi le was seen. Lips are competent at rest. With arch expansion transversely on the upper arch and intrusion on the upper anterior teeth, vertical maxillary growth was reversed and controlled. Vertical dimension was increased by lower posterior extrusion. Jaw position has also improved by auto-jaw rotation (forward and upward). These movement has allowed mandible to grow three-dimensionally, promoting mandibular growth during the growth phase. This can be seen on the patient’s facial profi le, where he has an equal frontal facial third with improvement on chin prominence during treatment.
A Class I incisor canine and molar relationship with maximum intercuspation was achieved by mesialisation of the mandible and

Fig. 16 Fig. 17 Fig. 18 Fig. 19




Fig. 20 Fig. 21 Fig. 22


Fig. 23 Fig. 24

Figs. 16-23: Intra and extra oral images after treatment Fig. 24: Panoramic radiograph after treatment Fig. 25: Cephalometric radiograph after treatment Fig. 25
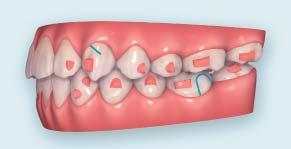

Fig. 26

Fig. 29 Fig. 27 Fig. 28

Fig. 30

Figs. 26-30: Final ClinCheck treatment plan
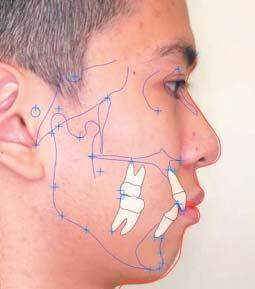
Fig. 31 Fig. 32
Figs. 31-32: Ortho analysis (before and after)
distalisation of the maxilla. Deep bite and increased overjet were resolved. The upper and lower dental midlines coincided with the facial midline. A U-shape arch shape on both upper and lower arches was seen. There was a remarkable improvement in the patient’s gummy smile. A nice smile arc with a posterior curve of spee was achieved. He was happy with his current smile arc and the improvement of his gummy smile as well.
CLINICAL TIPS
• Increased posterior alveolar height result in reverse smile arc appearance and this is a growth precursor indicator of vertical maxillary excess (VME) and increased lower anterior face height • VME would cause downward and backward jaw rotation, which most likely results in severe Class II with retrognathic mandible • Patient with VME tends to have narrow arch mandible, early detection could relieve crowding issues and avoid extraction to gain space • Arch development with expansion is ideal for a patient within the growing phase • The use of the maximum number of horizontal and vertical attachments are able to improve retention on short clinical crowns in mixed dentition • Although tooth movement on deciduous dentition may result in accelerated root resorption, it was necessary to allow early tooth loss and achieve treatment goals • Deep bite extrusive attachment and horizontal extrusive attachment were used on deciduous dentition to allow early exfoliation • Long horizontal attachments were used for extrusion movement on posteriors to increase vertical dimensions • The use of Optimised Root Control Attachment on erupted premolars and canines ensure bodily tooth movement and root

parallelism during space closure and alignment • Facial aesthetics are a key concern for patients when they seek treatment for protrusive lips
IMPACT ON CLINICAL PRACTICE
This case demonstrates that the Invisalign System is eff ective in complex orthodontic cases requiring early interceptive orthodontic. The system allows arch expansion and development without the patient needing to wear additional removable appliances or undergo surgery. Simultaneously, the patient’s deciduous teeth are allowed to exfoliate naturally with the help of Invisalign extrusive attachments placed on them. The use of pontics to maintain space for the eruption of permanent dentition is also possible. Besides, this case provides evidence that with proper treatment planning, the Invisalign System can stimulate mandibular growth and allow auto-forward jaw rotation for the patient to achieve optimum growth within the growing phase. It also provides evidence for the effi cacious use of Invisalign in correcting deep bite and midline shift. Face driven orthodontic philosophy should be a key focus of contemporary orthodontics, particularly in the case of correcting bimaxillary protrusion and gummy smile.
This case also proves that there is a misconception regarding starting orthodontic treatment once all permanent teeth have erupted. In fact, it is best to start early to prevent severe malocclusion happening in the future. A practitioner should be able to identify the problems and foresee potential orthodontic issues when the patient is young, particularly between eight to 10 years old, and if possible, start interceptive orthodontic treatment immediately when the patient is still in the growing phase.
The case provides evidence for the use of the Invisalign System for patients who wish to undergo treatment with an “invisible” aligner system and reluctant to use a conventional fi xed appliance system and removable appliances. We hope to increase the use of the Invisalign System through demonstrating that good results can be obtained with shorter or comparable treatment time to conventional fi xed appliance system. We have developed an aligner changing protocol which enables patients to vary their aligner changing frequency based on the achievable wearing hours with a grading system on the expected outcome (Table 1). Basically, the longer the hours the patient can wear daily, the better the results.
Grade Wearing hours Recommended wearing days A 22 to 24 7
B 20 to 22 10
C 18 to 20 12
D 16 to 18 14 F Less than 16 Bound to have off tracks
Table 1: Aligner changing protocol used by Imperial Dental Specialist Centre showing the recommended wearing days per aligner based on the patient’s wearing hours and the expected outcome
CONCLUSION
This case involved treatment of Class II Division I with deep bite in mid-mixed dentition. The patient presented with procumbent facial profi le, bimaxillary proclination, retrognathic mandible, increased middle facial one-third and a deviated upper dental midline. The treatment plan aimed to control vertical maxillary excess and stimulate mandibular growth in multiple planes. This case has demonstrated that through arch development and expansion, permanent dentition was allowed to erupt in an ideal position. The Class II malocclusion, deep bite, dental midline and gummy smile were corrected. Through this case, the Invisalign System demonstrates its ability to perform interceptive orthodontic treatment during mixed dentition. A nice smile arc and facial profi le were achieved without extractions – the treatment plan that the patient hoped for. DA
About the Authors
Dr How Kim Chuan graduated from the National University of Singapore in 1991. He went on to specialise in orthodontics at the University of London Eastman Dental Institute and obtained his MSc in orthodontics in 1995. He later obtained his MOrth RCS from the Royal College of Surgeons of England as well as Edinburgh in 1996. Dr How is currently the chief consultant at the Imperial Dental Specialist Centre. He is also a speaker for the Invisalign System and has conducted multiple certifi cation courses and study clubs in South East Asia and India. Presently, he is also an examiner for MOrth RCS Edinburgh.
Dr Kevin Ng is a visiting professor at the Ghongzhou Medical University and Hon. Clinical professor at the University of Hong Kong (2017-2019). His post-graduate qualifications include Membership of the Faculty of Dental Surgery (MFDS) of The Royal College of Surgeons of Edinburgh. He runs a private practice in Hong Kong.
Dr Manjusri Lim obtained her Bachelor of Dental Surgery degree from the University of Adelaide, Australia. She has interest in clear aligner therapy and Dr How is one of her mentors in Orthodontics. Dr Lim is currently working in Singapore.









