
9 minute read
Food Allergy in Schools: Strides to Improving Safety and Awareness
by Dr. Ruchi Gupta, MD, MPH

Advertisement
When I began practicing as a pediatrician and researcher over 15 years ago, I met a family committed to improving food allergy (FA) awareness and management. They had two sons with severe food allergies and came to Lurie Children’s for support and to advocate for more research on the condition. As a junior faculty member conducting related research, I was called into the meeting to see if I could help. I instantly connected with the family as their passion to improve children’s lives was contagious, and their support and excitement for our strides in FA research continues to this day.
As I was primarily researching asthma at the time, I was incredibly surprised by the dearth of scientific data on food allergy and recommendations for families like theirs. The only major clinical recommendations in place were to avoid their children’s allergenic foods and carry epinephrine in case of an emergency. There were few (if any) policies or precautions taken in schools and other public places to keep children with FAs safe, and parents were left navigating a brand new lifestyle with this potentially life-threatening condition, mostly on their own. After gathering as much information as I could about the disease, I noticed that even basic prevalence numbers were lacking. I felt that I could contribute to this area of research and help make a difference for affected families, thus began my journey into the food allergy world.
Surprisingly, about three years into my research, my professional and personal worlds collided when my one-year-old daughter had a severe allergic reaction to peanut butter. I experienced firsthand what the families of my allergy patients were feeling. Everything that I learned through my research up to that point could never have prepared me for the daily impact of food allergy. My daily experiences only further cemented my drive to do as much as possible to keep her and all children with food allergies safe at every stage of life.
Therefore, our research team set out to create and distribute a survey to over 40,000 households nationwide to shed some light on the gravity of food allergy in the United States. The data from this study, published in 2011, determined that an estimated 8% of children (1 in 13) in the U.S. were affected by food allergy [1]. As food allergy became a more widely-discussed public health epidemic, we decided to re-distribute this survey to 40,000 children and adults, respectively, and the results were published in 2018 and early 2019 [2]. Our results still found that an estimated 8% of children in the U.S. had a convincing food allergy, though more than 11% reported having one. We also found the most commonly reported allergies in children are to peanuts, milk, shellfish, tree nuts, eggs, fin fish, wheat, soy, and sesame. Among these children with food allergy, 42.3% report a history of severe reactions, and 39.9% have multiple food allergies. Additionally, one in five children have sought emergency care for a food allergic reaction in the past year [3].
Understanding the prevalence and severity of food allergy in the United States has thankfully prompted conversation surrounding prevention strategies, management, treatments, and policies, and we have made major strides in improving safety and awareness. This shift in conversation has been especially important in schools, where children spend so much of their young lives under the care and supervision of their teachers and school staff. As many as a quarter (25%) of first time allergic reactions occur in school due to young children trying foods for the first time or accidental ingestion. The development of inclusive and protective school policies has been critical [4].
About 10 years ago, the Illinois Public Act 96-0349 was passed, and the Illinois State Board of Education (ISBE) and the Illinois Department of Public Health (IDPH) released the guidelines for managing life-threatening food allergies in Illinois schools and required that each school board implement a comprehensive policy based on these guidelines. This prompted Chicago Public Schools’ first draft of their Food Allergy Management Policy which included protections such as requiring parent report of FA and establishing legal documentation such as 504 plans or IEP plans for students to meet their unique needs [5]. Though these policies laid a solid foundation in promoting food allergy awareness and safety in schools, there was still more work to be done. At the time, schools were not authorized to keep an emergency supply of epinephrine for children who did not have a diagnosed food allergy or their own auto-injector, and further, school health personnel were not permitted to administer any lifesaving medication to these children due to fear of liability. With these barriers, schools were instructed to call 911 and wait for help to arrive. In cases of anaphylaxis, this delay in treatment can be fatal.
Unfortunately, a major shift to improve these policies did not come about until 2010 after a 7th grade student passed away from anaphylaxis while attending a Chicago Public School. Following this heartbreaking tragedy, CPS worked tirelessly to ensure all students were completely protected if a sudden anaphylactic reaction occurred on school grounds. I was granted the opportunity to help with this initiative. The amendment to the Administration of Medication policy allowed all schools in the district to stock undesignated epinephrine for nurses to administer to children or staff in case of an emergency. Thankfully, the Illinois Attorney General officially passed the School Access to Emergency Epinephrine Act in 2012 and CPS became the first large urban school district in the country with this life-saving medication widely and readily available for all students and staff [5].
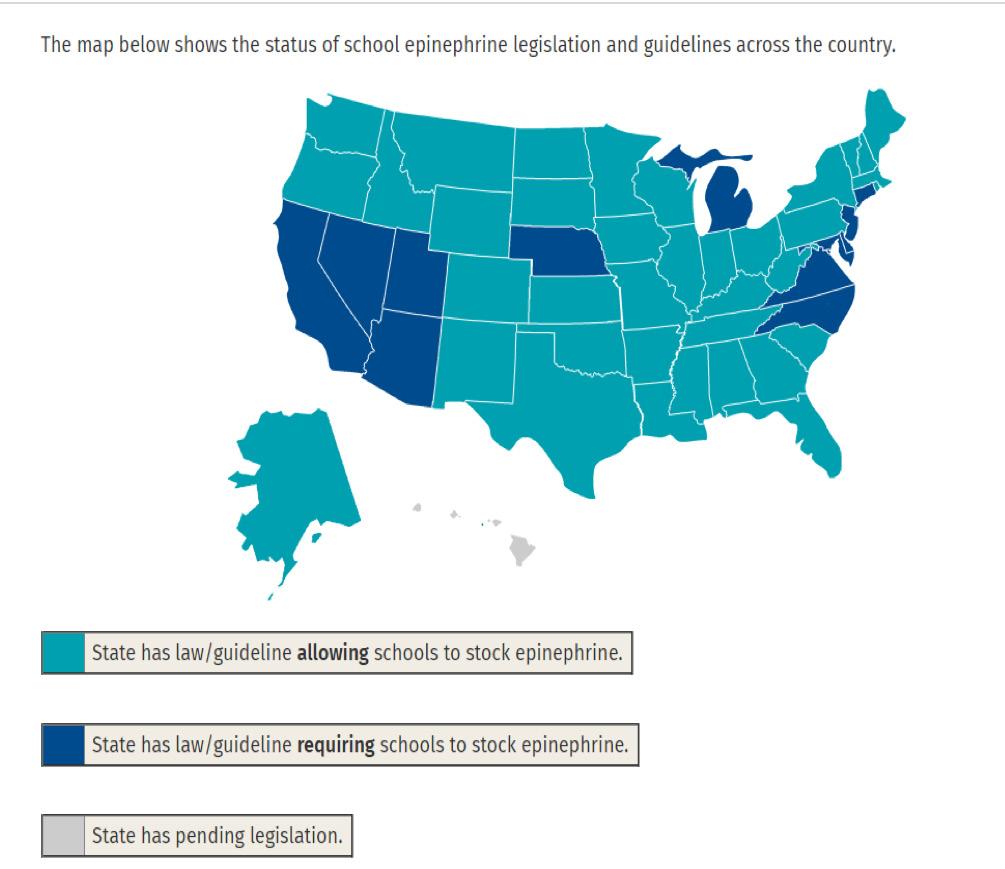
Data from FARE website on school guidelines on stock epinephrine
This victory for CPS was just the first step in protecting all students with food allergy, the next step was to see how this policy was received and utilized. Our research team collaborated with CPS to evaluate the use of this policy during the first year and found that undesignated stock epinephrine auto-injectors were administered about 38 times to students and/ or staff, and more than half of these administrations were to individuals who did not have any previous history of life-threatening food allergies [6]. This data demonstrated the importance of having this life-saving medication available in schools and led to the development of guidelines and policies by school districts nationwide. It was incredible to be part of this experience and today, 49 states either have laws/ guidelines allowing schools to stock epinephrine or actually require schools to stock epinephrine to keep their children safe, and the 50th is on its way [7].
While highlighting the need for life-saving medication in schools, we also wanted to continue to improve safety by assessing how CPS schools reported and managed food allergy in general. As part of the Improving Chronic Disease Verification and Medication Access in the Chicago Public Schools Initiative, our research team collected data on how many children with a documented food allergy had the appropriate health plans (Food Allergy Action Plan) readily available at school. We found that only half of students with a documented food allergy had a health management plan on file with the school, and these numbers were significantly lower among minority and low-income students. These findings paved the way for more education in schools for students and parents about the importance of having an action plan on file with the school for their child’s safety and helped in overcoming the barriers to chronic disease reporting with the CPS administration [8, 9].
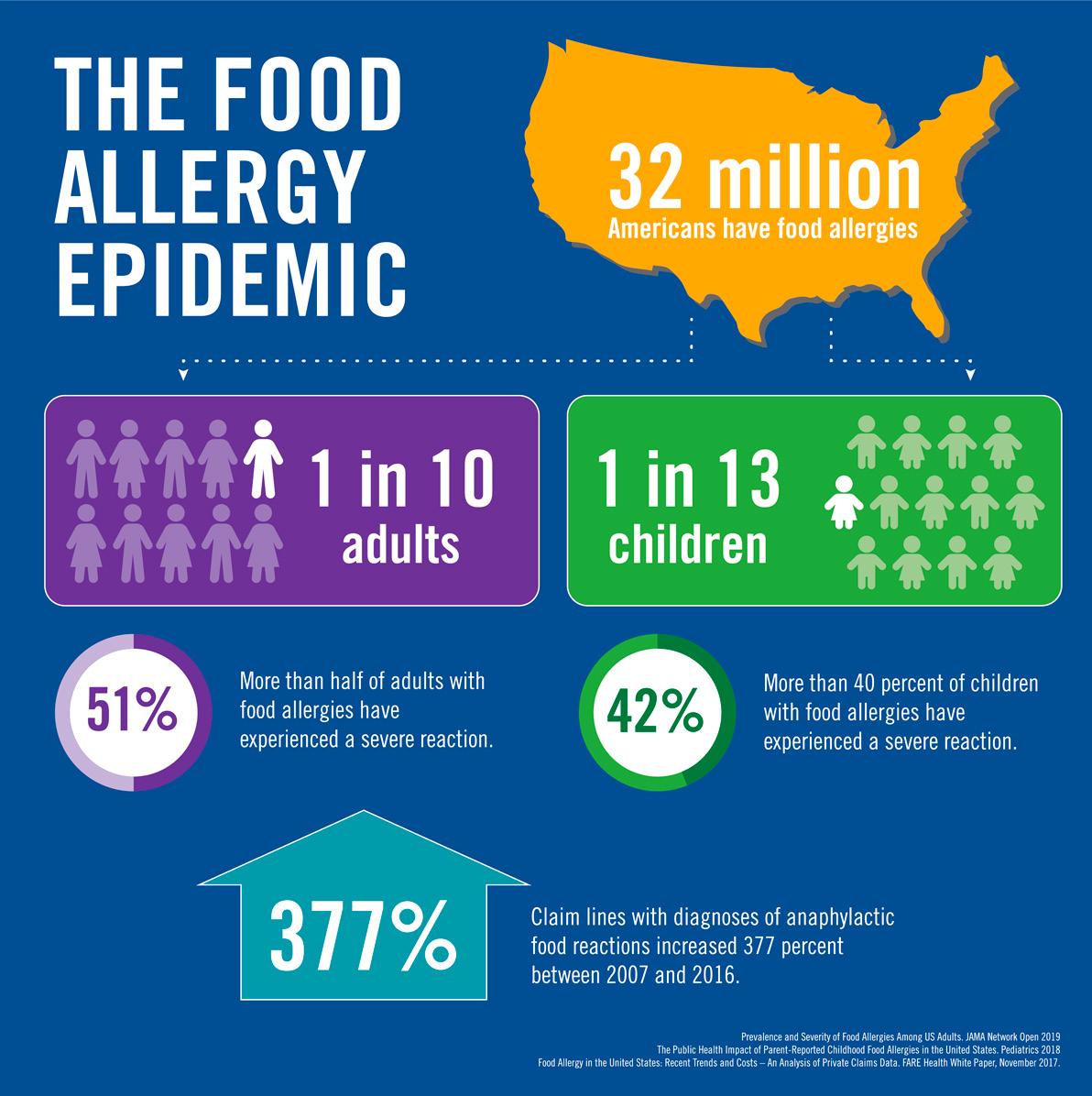
Prevalence data on adulta
Although safety in school has always been the number one priority for children with food allergy, we have also been trying to improve awareness and inclusivity among their classmates to allow these students to feel empowered and connected with one another. Living with a food allergy can be difficult and sometimes scary for children to manage on their own, and many students feel like they always have to educate others and be their own health advocates. Therefore, to help facilitate a more open dialogue and normalize food allergy in schools, we surveyed students on what they would want their peers to know, developed age appropriate videos and teacher guides and conducted pre-post knowledge surveys [10]. The peer-to-peer food allergy educational videos for elementary school, middle school, and high school help peers better understand and support their classmates with food allergies and are available for free on our website or in the form of a USB. They have been distributed nationally to schools and have been incredibly well received by teachers and students alike. While it is abundantly clear that food allergy has become a major public health concern worldwide, the strides to improve policy and care for all children with the condition are unparalleled. Additionally, students living with food allergy are some of the most empowered and resilient children I have ever met, and being a health advocate for them has been nothing but rewarding. I have been so grateful to contribute to the research being done to improve the lives of children and their families and will continue to do my best to spread awareness, eliminate disparities, and find answers until we have a cure!
To watch our student-produced food allergy educational videos, please visit: https://www.feinberg.northwestern.edu/sites/cfaar/education/ video-library.html
Contact our team: cfaar@northwestern.edu
References [1] Gupta, R. S., Springston, E. E., Warrier, M. R., Smith, B., Kumar, R., Pongracic, J., & Holl, J. L. (2011). The prevalence, severity, and distribution of childhood food allergy in the United States. Pediatrics, 128(1), e9-e17. [2] Gupta RS, Warren CM, Smith BM, et al. Prevalence and Severity of Food Allergies Among US Adults. JAMA Netw Open. 2019;2(1):e185630. doi:https:// doi.org/10.1001/jamanetworkopen.2018.5630 [3] Gupta, R. S., Warren, C. M., Smith, B. M., Blumenstock, J. A., Jiang, J., Davis, M. M., & Nadeau, K. C. (2018). The public health impact of parent-reported childhood food allergies in the United States. Pediatrics, 142(6), e20181235. [4] Sicherer, S. H., & Mahr, T. (2010). Management of food allergy in the school setting. Pediatrics, 126(6), 1232-1239. [5]Zadikoff, E. H., Whyte, S. A., DeSantiago‐Cardenas, L., Harvey‐Gintoft, B., & Gupta, R. S. (2014). The development and implementation of the Chicago public schools emergency EpiPen® policy. Journal of School Health, 84(5), 342-347. [6] DeSantiago-Cardenas, L., Rivkina, V., Whyte, S. A., Harvey-Gintoft, B. C., Bunning, B. J., & Gupta, R. S. (2015). Emergency epinephrine use for food allergy reactions in Chicago Public Schools. American journal of preventive medicine, 48(2), 170-173. [7]https://www.foodallergy.org/education-awareness/advocacy-resources/ advocacy-priorities/school-access-to-epinephrine-map [8] Rivkina, V., Tapke, D. E., Cardenas, L. D., Harvey-Gintoft, B., Whyte, S. A., & Gupta, R. S. (2014). Identifying barriers to chronic disease reporting in Chicago Public Schools: a mixed-methods approach. BMC public health, 14(1), 1250. [9] Gupta, R. S., Rivkina, V., DeSantiago-Cardenas, L., Smith, B., HarveyGintoft, B., & Whyte, S. A. (2014). Asthma and food allergy management in Chicago Public Schools. Pediatrics, 134(4), 729-736. [10] Jiang, J., Gallagher, J. L., Szkodon, J. W., Syed, M., Gobin, K. S., Gupta, R. S., & Bilaver, L. A. (2019). The development and evaluation of peer food allergy education videos for school-age youth. Annals of Allergy, Asthma & Immunology.

About the Author
Ruchi Gupta, MD, MPH, has more than 15 years of experience as a board-certified pediatrician and health researcher and currently serves as the director of the Center for Food Allergy and Asthma Research at Northwestern University Feinberg School of Medicine and Ann & Robert H. Lurie Children’s Hospital of Chicago. Dr. Gupta completed her undergraduate and medical education at the University of Louisville and completed her medical residency at Children’s Hospital & Regional Medical Center, University of Washington in Seattle. She completed her pediatric health services research fellowship at Boston Children’s Hospital and Harvard Medical School, and went on to receive her Master of Public Health from the Harvard School of Public Health. Dr. Gupta is nationally recognized for her groundbreaking research in food allergy and asthma epidemiology, specifically for her research on the prevalence of pediatric and adult food allergy in the United States. She is the author of the Food Allergy Experience, has written and co-authored over 100 peer-reviewed research manuscripts, and has had her work featured on major TV networks and in print media. She strives to improve the lives of children and their families through her epidemiological, clinical, and community-based research and hopes to continue finding answers and shaping policies surrounding food allergy and asthma.

About the Artist
Madison Rice is currently a BVIS graduate student at the University of Illinois at Chicago. She is originally from Dallas, Texas, and received a Bachelor of Science in Microbiology from Mississippi State University. Her current work at UIC focuses on cellular and molecular 3D modeling and animation.







