7 minute read
20 key messages from the new ESC HF management guideline
20 key messages the new ESC HF from management guideline
The European Society of Cardiology (ESC) guidelines for the diagnosis and treatment of acute and chronic heart failure (HF) was published online in the European Heart Journal on 27 August.
Advertisement
About 2% of adults worldwide have HF. Prevalence increases with age, from 1% in those under 55 years to more than 10% in people aged 70 and above. In developed countries, the most common causes are coronary artery disease and high blood pressure.
Patients with HF have a poor prognosis and markedly reduced quality of life. The main symptoms are breathlessness, ankle swelling, and tiredness. After diagnosis, patients are hospitalised once every year on average and more than half die within five years.
Chronic HF is a condition where the heart is unable to pump blood around the body properly. It usually occurs because the heart has become too weak or stiff.
Ejection fraction (eg the percentage of the blood within the ventricles that is ejected during the cardiac cycle), is the most important measurement of cardiac function. When the pumping action of the heart is weak it is referred to as HF with reduced ejection fraction (HFrEF) and when it is stiff and does not relax properly, it is referred to as HF with preserved ejection fraction (HFpEF).
Acute HF
Acute HF is a life-threatening condition requiring urgent evaluation and treatment. It may be the first manifestation of HF (new onset) or, more frequently, it is due to an acute deterioration of chronic HF.
Regarding diagnosis, when there is a suspicion of chronic HF, the guidelines recommend measuring the level of hormones produced by the heart (natriuretic peptides). If levels are normal the patient can be reassured that heart failure is very unlikely. If high, this should prompt referral for an echocardiogram to detect the underlying heart problem.
New definition of HF
The HF Society of America, the HF Association of the ESC and the Japanese HF Society recently joined forces to redefine HF: HF is a clinical syndrome with symptoms and/or signs caused by a structural and/or functional cardiac abnormality and corroborated by elevated natriuretic peptide levels and/or objective evidence of pulmonary or systemic congestion.
The new definition also includes a new classification and staging system. The classification includes:
» HFrEF: HF with left ventricular ejection fraction (LVEF) =40%
» HF with mildly reduced ejection fraction (HFmrEF): HF with LVEF 41–49%
» HFpEF: HF with LVEF 50%
» HF with improved ejection fraction: HF with a baseline LVEF = 40%, a 10 point increase from baseline LVEF, and a second measurement of LVEF >40%.
Non-pharmacological treatments
Exercise is recommended for all capable chronic heart patients to improve quality of life and reduce HF hospitalisation. In those with more severe disease, frailty, or comorbidities, a supervised, exercise-based, cardiac rehabilitation programme should be considered.
“The vast majority of drug treatments that improve survival and reduce hospitalisations also have beneficial effects on quality of life and symptoms,” said guidelines task force chairperson Prof Theresa McDonagh of King’s College Hospital, London, (United Kingdom).
“There are some interventions that do not impact survival but do improve quality of life and symptoms – for example exercise rehabilitation – that should also be offered to patients with chronic HF.”
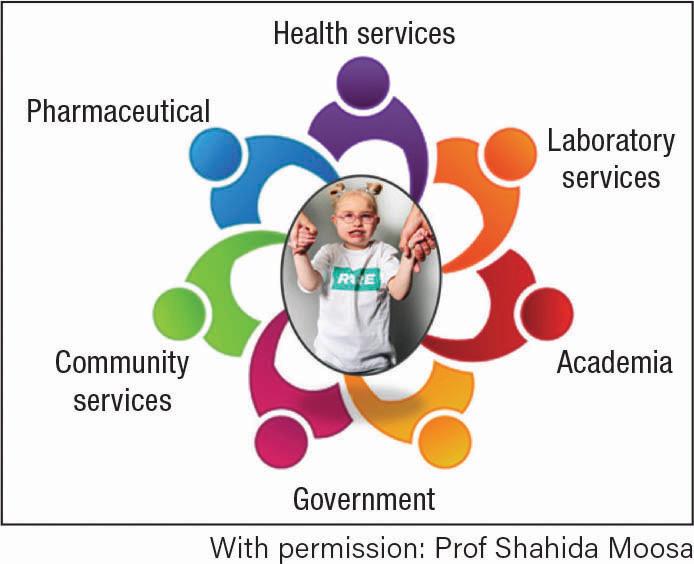
The guidelines recommend that all patients have access to a multi-professional HF disease management programme to ensure that their HF is correctly diagnosed and managed. These programmes have been associated with better care and improved outcomes.
In addition, patients with HF should be encouraged to be actively involved in managing their condition. Self-care includes adopting healthy habits such as physical activity, avoiding excessive salt intake, maintaining a healthy body weight, avoiding excessive alcohol consumption, and not smoking.
It is also important to avoid drinking large volumes of fluid, recognise sleeping problems, monitor changes in symptoms, and know when to contact a health professional.
Patients with HF are at increased risk of infections, which may worsen symptoms and be a precipitant factor for acute heart failure. The guidelines state that influenza, pneumococcal and Covid-19 vaccination should be considered in patients with HF.
Recommendations are also given on how to manage patients with HF who have co-existing conditions such as atrial fibrillation and valvular heart disease.
“It is crucial to treat the underlying causes of heart failure and its comorbidities,” said cochairperson of the guidelines task force Prof Marco Metra of the University of Brescia (Italy).
“Proper treatment of high blood pressure, diabetes and coronary artery disease can prevent the development of HF. Atrial fibrillation, valvular heart disease, diabetes, chronic kidney disease, iron deficiency and other comorbidities frequently co-exist with HF and the adoption of specific treatments may have a major impact on the clinical course of our patients.”
20 key messages
1. Patients with HF are classified based on their LVEF. Those with a LVEF between 41% and 49% are defined as HFmrEF.
2. Measurement of natriuretic peptide (NP) and echocardiography have key roles in the diagnosis of HF.
3. Angiotensin-converting enzyme inhibitor (ACEi) or angiotensin receptorneprilysin inhibitor (ANRi), beta-blockers, mineralocorticoid receptor antagonist, and sodium-glucose co-transporter 2 inhibitors (SGLT2is) are recommended as cornerstone therapies for patients with HFrEF.
4. Implantable cardioverter-defibrillators are recommended in selected patients with HFrEF of an ischaemic aetiology and should be considered in those with a non-ischaemic aetiology.
5. Cardiac resynchronisation therapy with defibrillator is recommended in those patients with HFrEF, in sinus rhythm, with a left bundle branch block (LBBB) ≥150 ms and should be considered in those with a LBBB ≥130–149 ms or nonLBBB ≥150 ms.
6. Advanced HF strategies (heart transplantation/mechanical circulatory support [MCS]) may be appropriate in selected patients.
7. ACEi/ARNi, beta-blockers, and MRA may be considered in patients with HFmrEF.
8. The diagnosis of HFpEF requires objective evidence of cardiac structural, or functional abnormalities as well as elevated plasma NP concentrations consistent with the presence of LV diastolic dysfunction and raised LV filling pressures. A diastolic stress test is recommended when these markers are equivocal.
9. To date, no treatment has been shown to reduce mortality and morbidity in patients with HFpEF.
10. It is recommended that all patients with HF be enrolled in a multidisciplinary HFmanagement programme.
11. Exercise is recommended for all patients who are able, to improve exercise capacity and quality of life, and reduce HF hospitalisation.
12. Patients with advanced HF refractory to medical/device therapy and who do not have absolute contraindications should be referred for consideration of heart transplantation. MCS should also be considered as a bridge to transplantation or destination therapy in selected patients.
13. Four major clinical presentations of acute HF may occur:
» Acutely decompensated HF
» Acute pulmonary oedema
» RV failure
» Cardiogenic shock.
14. Treatment of acute HF is based on diuretics for congestion, inotropes, and short- term MCS for peripheral hypoperfusion.
15. Patients hospitalised for HF should be carefully evaluated to exclude persistent signs of congestion. Oral treatment should be optimised before discharge.
16. In addition to oral anticoagulation, a strategy of rhythm control including catheter ablation should be considered in patients whose symptoms and/or cardiac dysfunction are associated with atrial fibrillation.
17. Surgical aortic valve replacement or transcatheter aortic valve implantation, as advised by the heart team, are recommended in patients with symptomatic severe aortic valve stenosis.
18. Patients with isolated significant secondary mitral regurgitation and Cardiovascular Outcomes Assessment of the MitraClip Percutaneous Therapy for HF patients with functional mitral regurgitation trial criteria should be considered for percutaneous edgeto-edge repair, whereas those with secondary mitral regurgitation and coronary artery disease, who need revascularisation, should be considered for surgery.
19. It is recommended that patients with type II diabetes are treated with SGLT2is.
20. Patients should be periodically screened for anaemia and iron deficiency and intravenous iron supplementation with ferric carboxymaltose should be considered in symptomatic patients with LVEF <45% and iron deficiency, and in patients recently hospitalised for HF and with LVEF ≤50% and iron deficiency.
References
McDonagh TA, Metra M, Adamo M, et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: Developed by the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) With the special contribution of the Heart Failure Association (HFA) of the ESC. European Heart Journal, 2021.
European Society of Cardiology. ESC Guidelines on heart failure management launched today. News release, 27 August 2021. https://www.eurekalert.org/newsreleases/926357.