11 minute read
Hearing Loss and Cognition
DR. JENNIFER STINSON AU.D. STINSON AUDIOLOGY SERVICES LLC
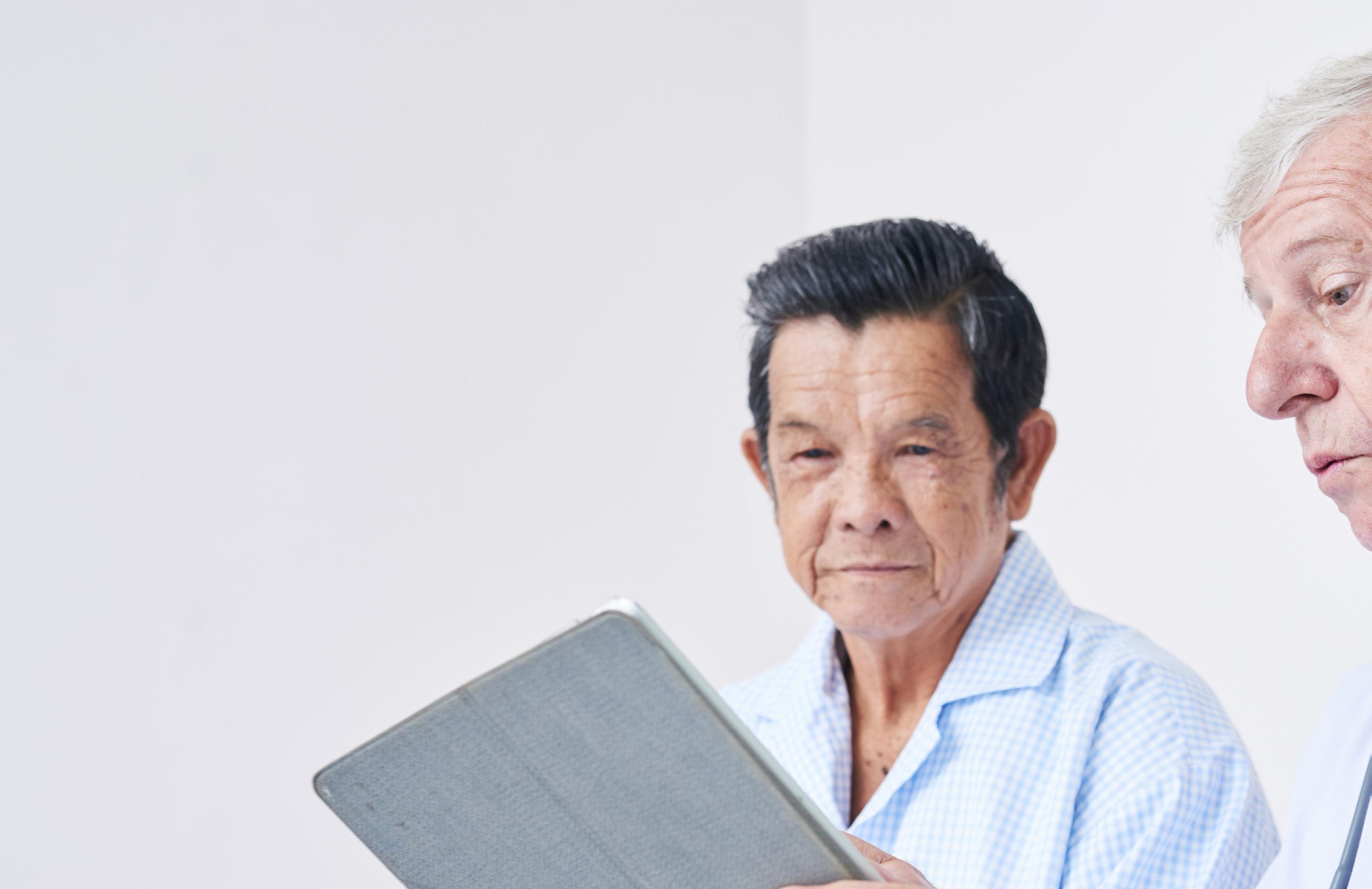
According to the Centers for Disease Control, hearing loss affects about 40 million Americans between the ages of 20-69. It may seem dramatic to say, but this puts hearing loss in the category of a national health crisis. In addition to that, there has been a lot of research connecting hearing loss to cognitive decline or dementia. Dementia is a general term for the cognitive deterioration that includes loss of memory and intellectual function. The exact correlation has been difficult to define

and for researchers to document as well as whether follow a conversation is now declining. Thus, making hearing aid use or amplification can reverse the it even more difficult to mentally process the speech decline. There is a lot of speculation both in the mixed in with the background noise. In this scenario, literature and hearing aid advertisements about the person with hearing loss and compounded by this correlation. You may stumble upon some mixed reduced cognition function may start to completely information, so outlined below is a quick and basic remove themselves from conversations that are explanation so that you can make informed decisions difficult to hear. This also introduces the connection regarding your hearing healthcare. between hearing loss and depression or social In simple terms, cognition is defined as mental isolation. processes. When defining cognitive function, you Research conducted by Dr. Frank Lin from Johns must consider the mental processes of how well Hopkins University identifies this as increased you obtain, organize and use knowledge. Hearing is cognitive load. The hearing loss is causing more of how we often obtain information or knowledge. The a challenge in obtaining information or knowledge. connection between what we hear and what we As previously stated, there is no current research do with what we hear is very important. There are stating that wearing hearing aids will prevent further many cognitive processes related to understanding cognitive decline. What we do know is that untreated and comprehending speech sounds. When you have hearing loss can cause social isolation, depression, hearing loss, you are often unable to hear certain and an increased risk of falls. If you have any risk speech sounds. For example, if a person has hearing factors that may increase your chances of having loss, they may often say, "I can hear you, but I can't a hearing loss at a younger age, you should have understand what you are saying." People who have your hearing tested. A few common risk factors for milder hearing loss may communicate 'just fine' hearing loss include a family history of hearing loss, in quiet situations and not even realize they have occupational or recreational noise exposure, balance a hearing loss. This is due to the brain's ability to problems, diabetes, and heart disease. If this is you, use knowledge of language and the content of the have conversations with your primary care doctor conversation to fill in what letters or words may be regarding your hearing care. missing due to hearing loss. Let's consider the same person with the mild hearing loss and put them in a room with ample background noise. The noise further degrades the speech signal, so it is even harder to use knowledge of language to fill in the missing words or sounds. In this case, What? Stop the person with the mild hearing loss must work Procrastinating. even harder to hear or process what is being said. The person with hearing loss can become frustrated and fatigued during the conversation. Now assume this same person, with the hearing loss, is beginning to decline in their cognitive function. The exact cognitive function that was helping to fill in speech sounds and
Hearing Aids. Ear Wax Removal.
FREE CONSULTATIONS
Dr. Jennifer Stinson Doctor of Audiology│(610) 657-1330│stinsonaudiologyservices.com

COVID Vaccines: A Novel Approach to a Novel Virus

GREG LUNDELL, ASSOCIATE DIRECTOR OF EQUIPMENT SERVICES GENESIS AEC
As we're all painfully aware, the global COVID-19 pandemic put a spotlight on the pharmaceutical industry and its ability to develop vaccines at a record pace. Pfizer BioNTech, Johnson and Johnson, and Moderna all have FDA-approved COVID vaccines, while others are in development or close to approval. The process of vaccine development for an infective causing a global pandemic, however, has redefined how pharmaceutical and biotech companies bring a vaccine product to market and how they have positioned their business to support such an endeavor.
Before COVID, the average time to market for a vaccine was 10 to 12 years. This includes the development of novel vaccines for new infectives, as well as the time for generic companies to develop "me-too" vaccines that cause immunity based on the same technology as the original. Yet, the novel vaccines to COVID took a fraction of that time, ~ 1 -1.5 years from the initial reports of widespread infection. The expedited development timeline that played out on the world stage relied heavily on a new technology that has been under development for ~10-15 years and therefore had been in Moderna and Pfizer's "back pocket" for just a crisis that COVID turned into. First, let's take a look at the standard vaccine technology that we're all aware of, if only by having been given our regimen of vaccines as children. Merck's measles, mumps, and rubella, or MMR, vaccine is one of the most widely administered, with over 500 million doses having been given worldwide. Although a novel concept in the 1960s, the action of the vaccine is largely based on the human body's standard response to infection. Basically, the three viruses that cause the three named diseases are artificially weakened in the laboratory, ensuring they do not cause disease when injected. They do, however, cause the immune system to recognize the virus's structure, which leads to the development of antibodies to the virus and further development of memory white blood cells. These cells can cause a future immune response if and when you are exposed to the native, infective virus in the environment. The MMR vaccine is 88-97% effective in preventing disease and has caused a drop in disease-related deaths from ~2.6MM / year to ~100,000 per year. How is the COVID vaccine different? The Moderna and Pfizer vaccines do not use weakened or "killed" viruses. In fact, looking at these 2 COVID vaccines, there is almost no resemblance to the novel coronavirus that causes the disease. Instead, there is only a very small piece of genetic code, called messenger-RNA or mRNA, that is for all intents and purposes the same as what can be found in the viral genetic code itself. The use of mRNA to elicit an immune response is the new technology that is the basis for both the Pfizer and Moderna vaccines.
So what is messenger RNA? mRNA is a piece of genetic code that is translated from our DNA or the RNA in the coronavirus (genetic code contained in the nucleus of the cells of our body or the shell of the virus) into an actionable code, mainly to make proteins. Proteins are the building blocks of cells and also make up that spikey-looking shell that has become the ubiquitous graphic for COVID on the news. The spikes on this shell are the proteins the vaccine mRNA codes for.
These novel vaccines, in simple terms, turns our own cells into little mini-factories. The mRNA that codes for the spike protein of the coronavirus makes its way into our cells once injected. Our cellular organs take that actionable code and start assembling the protein within our cells. Once complete, the protein is forced to the cell's surface, and the immune system can then recognize it and, just like the action of the MMR vaccine, create antibodies to a piece of the coronavirus. All without being infected with the actual virus. It is reported that the mRNA COVID vaccines are >94% effective in preventing the disease. The use of mRNA vaccines is novel in that the coronavirus vaccine is the first to utilize the technology to this magnitude. Due to the speed of development brought on by our advances in genetics, expect this type of technology to become the norm for future vaccine development.

Challenging the Myths about Psych Wards
VANCE P. FARRELL, CPS SUPERVISOR PENNSYLVANIA MENTOR
We've all seen the Hollywood rendition of what a psychiatric unit looks like: large open recreational rooms, often referred to as "rec areas," with people walking around like zombies, others huddled in the corner rocking and/or talking to themselves with random outbursts, menacing-looking staff wearing all white giving medications to the patients, others strapping patients to their bed with a nurse around preparing a cocktail in a syringe to help the patient "calm down" and potentially a doctor as well who is dressed in his white lab coat. It is a scene that is portrayed consistently across television, film, and script and one that everybody can envision when they hear about a psych ward or psych unit at a hospital. However, few have actually seen the inside of, let alone spent a significant amount of time on, a psychiatric unit and know the inner workings that take place in these locations. The first myth that is to be dispelled is the portrayal of the staff, nurses, and doctors that are often displayed through the entertainment industry. The direct care staff in these locations are often college-educated individuals who have knowledge in case management, psychology, sociology, or other related fields of study and are there to gain real experience in the field, which is necessary to continue their education. The nurses and doctors are also not what they are portrayed. The nurses are often as involved as the direct care staff with the patients' daily schedule and activities through educational groups about medication or symptoms associated with common mental illnesses. The doctors are on the units daily but do not have much direct impact on the daily schedule other than their regular discussions with the clients about their medications, symptoms, and diagnoses. The whole goal of the inpatient experience is to provide a safe and monitored place to help the client get back to a baseline level through education, medication adjustment or management, and setting up referrals for support upon discharge designed to maintain their mental health.
Along with the misperception of the staff is the misperceptions about the unit itself and the activities that occur on the unit. The psychiatric unit does typically have a large common area, but they are designed for this location to be central on the unit, with bedrooms lining the hallways extending from this point. This is done to assist staff in having the

ability to monitor the patients consistently and ensure their safety as well as the safety of other patients and other staff on the unit. The activities available are also designed to promote education and care for the individuals. They often consist of multiple group sessions daily that cover a myriad of diverse topics related to medication, coping skills, support development, and self-reflection to help the patients develop a plan that works for them to maintain their wellness upon discharge. Since this is the main focus, there are few "entertaining" items that are allowed on the units because of the danger that these items could pose for the clients and for the staff because of the reasons behind why individuals are on a locked unit. Lastly, the patients on these units can be animated and display behaviors that most people would find disturbing or uncomfortable. The vast majority of what is portrayed by Hollywood are extreme exaggerations and are done for dramatic effect. Typically, patients on these units are there because they are a danger to themselves or others, and often the diagnoses seen and treated are for major mood disorders, schizophrenic disorders, or psychosis that has been induced by drugs or withdrawal from drugs or medications. While all of these disorders can elicit responses that involve symptoms like hallucinations, delusions, paranoia, and mania, the number of patients actively experiencing these symptoms simultaneously on a unit is very low, and rare to have more than a handful at a time.
The portrayal of these locations by the entertainment industry is just that... entertainment. It is not an accurate representation of the unit, the staff, and certainly not the individuals present on the unit. It is important to remember that mental illness can impact anybody.

Cele ate wi Us! Come


Contact Olde Homestead Golf Club or your next Banquet, Holiday Party, Wedding or Golf Tournament!

OldeHomestead