
13 minute read
From One Killer to Another
from NEXT | Spring 2020
From One Killer
From One Killer to Another
Exploring the Link Between Cancer Treatment and Heart Disease
By Eric Peters
After battling and beating the second leading killer on Earth, what could be more demoralizing and daunting than going right into a fight with the leading killer on Earth? This is the reality for a growing number of people who survive cancer — the No. 2 cause of death on the planet — because, as a result of their treatment, many face cardiovascular disease — the No. 1 cause of death on the planet.
As cancer therapies become much more successful, survivors are experiencing this series of events due in part to traditional chemotherapy, radiation therapy, immunotherapy, transplantation therapy and endocrine modification therapies having adverse effects on the heart and the blood vessels.
One remarkable example that illustrates this phenomenon has to do with women who are battling breast cancer. Studies

now indicate that the leading cause of death among those women is actually not breast cancer. It is heart disease. To address cardiovascular conditions in those being treated for cancer, a relatively new specialty — cardiooncology — has emerged to investigate and preserve heart health among cancer patients. A top researcher in the field is Greg Hundley, M.D., who graduated from the VCU School of Medicine in 1988, went on to the University of Texas Southwestern Medical Center and Wake Forest Baptist Medical Center, then returned to the MCV Campus in 2018 to serve as director of the Pauley Heart Center.
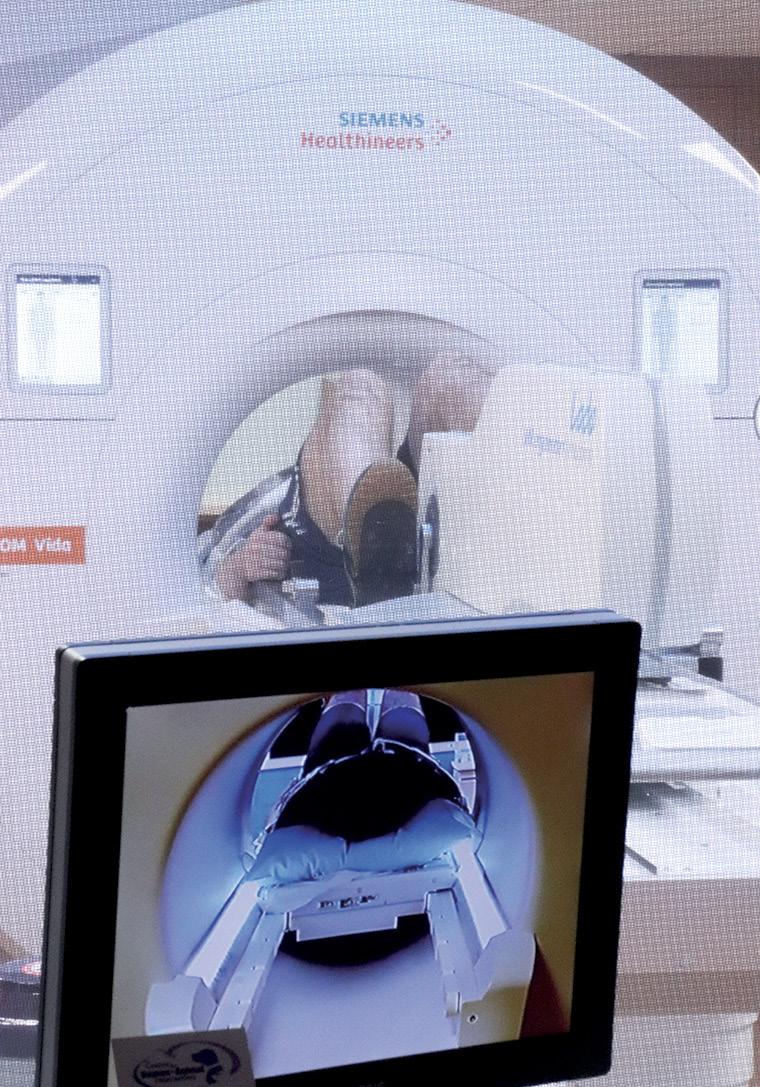
IMAGING IN RESEARCH Dr. Hundley uses magnetic resonance imaging (MRI) in the clinic and in his research. This noninvasive form of imaging, which doesn’t require catheters, surgical
Greg Hundley, M.D., director of the Pauley Heart Center, discusses the advanced imaging capabilities of the MRI system in VCU Health’s Cardiac Imaging Suite, which supports personalized cardiovascular evaluation, diagnosis and treatment for both Pauley Heart Center and Massey Cancer Center patients. Dr. Hundley, a Richmond native and VCU School of Medicine alumnus, is recognized for studying the impact of chemotherapy and radiation therapy on heart health and advancing treatment options for patients in need of cardiovascular and oncology care. Photo: Kevin Morley, VCU University Marketing


procedures or ionizing radiation (X-rays), enables his team to monitor patients frequently or over long periods of time as they receive cancer treatment. This MRI method also enables investigators and clinicians to evaluate the heart and blood vessels in a single examination. Dr. Hundley was the first in the world to demonstrate that MRI stress testing can identify those at risk of heart attack.
“When you have a disease process that is complicated to understand, you need a tool that can look at many different aspects of that disease process in a single setting,” Dr. Hundley said. “We’ve used MRI to identify heart disease in those with and receiving treatment for cancer.”
In addition, a unique feature of the imaging capabilities at VCU Health is the ability to acquire images while patients are lying still and when they are under physiological stress. At the Pauley Heart Center Cardiac Imaging Suite on the MCV Campus, Dr. Hundley’s team can monitor patients after they have been running on a treadmill or while they’re pedaling a stationary bicycle inside a scanner.
Gathering images under these conditions provides investigative teams and clinicians a unique opportunity to better understand disease processes that impact abilities to carry out activities of daily living. “An analogy is when your car has a problem,” Dr. Hundley said. “You don’t take it to a service station and everyone stares at it while it’s off; that would be your condition at rest. You start the car and you push on the accelerator. It is when you start to do things — you grocery shop, you walk down the street or up stairs in a building — that you can experience symptomatology of cardiovascular disease.”
Dr. Hundley is using this technology to help measure outcomes in four ongoing or recently completed studies, described on the following pages, focusing on cardiovascular diseases that are accelerated or newly developed as a result of having cancer or receiving treatment for cancer.
DETECT Dr. Hundley’s Detect study was funded by the NIH and ended last fall. It involved women with breast cancer and both women and men with lymphoma, exploring whether cardiovascular magnetic resonance imaging (CMR) could identify subclinical cardiac disease in patients receiving potentially cardiotoxic cancer treatment regimens.
Subclinical disease is not yet detectable by the usual tests, so diagnosis in this stage is critical for initiation of early treatment to improve quality of life and survival. The study found that utilizing contemporary CMR to accurately define cardiac anatomy, function and tissue characteristics may represent a critical tool to assess patients who have undergone cancer treatment. 1 “To reduce the incidence of cardiovascular events among cancer survivors, there is increasing interest to identify subclinical cardiac abnormalities that portend future cardiovascular events,” Dr. Hundley and his team wrote. “In so doing, one could identify those suitable for cardiovascular interventions to prevent these future untoward cardiovascular events.” 2



PREVENT Prevent is a 24-site placebo-controlled, double-blind clinical trial funded by both the Heart, Lung and Blood Institute and the National Cancer Institute at the NIH. It is examining whether receipt of a statin during breast cancer treatment reduces heart and vascular dysfunction. Statin therapies are used today to lower cholesterol, but they also have pleiotropic effects, meaning they reduce systemic inflammation, a condition that contributes to heart dysfunction after cancer treatment. Participants in the two-year study are those with lymphoma or breast cancer who take anthracycline-based chemotherapy, and the advanced MRI technology at VCU Health is one of the ways outcomes are being measured. Because the study is a double-blind clinical trial, neither the trial investigators nor the patients will know who is taking the placebo until the study has been completed. What investigators can do, though, is look at the data in aggregate to see both placebo and non-placebo groups as a single unidentified sample of 279 patients.
“What we’re seeing is that some patients have more of a decline in heart function, some patients have no decline, and a few patients have an increase,” Dr. Hundley said. “So, the question is, when all of that is unblinded in the next six months, did the statin ingestion promote the preservation of the heart performance?”
Many secondary outcomes are being investigated in this study, including cognition, because some chemotherapies are associated with cognitive decline while statins have been shown to both reduce and preserve cognition. The team will also look at vascular function and the occurrence of heart events like heart attacks and strokes.
UPBEAT Another problem for women who are treated for cancer relates to the development of fatigue, which occurs in about one-third of women undergoing treatment. In one-third of that one-third, women don’t go back to work, and they may experience unwanted changes in their family units, including divorce, as a result.
“It’s unrelenting, it never goes away,” Dr. Hundley said. “And we don’t understand why that fatigue is developing. What better than to perform a noninvasive imaging modality that looks at multiple aspects of your body — your heart function, your blood vessel function, your body composition — to try to gain some understanding about the precipitating factors of that fatigue?”
A research participant rides a stationary bicycle inside an MRI scanner, which plays a major role in cardio-oncology research led by Greg Hundley, M.D., director of the Pauley Heart Center. Gathering images under these conditions provides investigative teams and clinicians a unique opportunity to better understand disease processes that impact abilities to carry out activities of daily living. Photos: Eric Peters
bad disease— breast cancer— for another, which
is unrelenting fatigue related to the development

of heart failure.”
The UPBEAT study also evaluates emotional state, social situation, environmental stress, perceptions of those stressors and cognition. Funded by the NIH through the National Cancer Institute, it is a longitudinal cohort study, or one that follows a group of patients with similar experiences or diagnoses over time. It is another national multicenter study with 24 centers participating. Research participants undergo exercise testing, blood testing, genetic testing and the advanced MRI imaging.
“We want to avoid a situation where we trade one bad disease — breast cancer — for another, which is unrelenting fatigue related to the development of heart failure,” Dr. Hundley said. “You don’t want a woman who is 42, has two young children and undergoes cancer treatment to later not be able to participate in the activities of those children and all the things they need.”
There is also a disparities component to UPBEAT. African American women experience fatigue, heart failure and adverse heart conditions more frequently than those of other races or ethnicities, so there are specific questions in the study that are related to understanding these harmful comorbidities.
PALS The Physical Activity in Lymphoma Study, or PALS, is Dr. Hundley’s newest study, and is the project in which he is approaching cardio-oncology with the most unique lens. As care providers and researchers learn how adverse heart conditions develop during cancer treatment, they’re looking at many ways to approach the issue. The Prevent study, for example, is investigating a statin therapy, and studies around the world are looking at other heart failure therapies in the form of administering pills. PALS is quite different.
“We’ve noticed in cancer survivors, after their treatment, if we can get them exercising, they tend to do better,” Dr. Hundley said. “So, one thing we might consider, which is a total paradigm shift in medicine, is to actually get people to start exercising during their cancer treatment.” Dr. Hundley sees a parallel in this potential shift with one that occurred in a different clinical scenario over the

past half century. “Forty to 50 years ago, when a patient experienced a heart attack, our common thinking was to keep them at bedrest for a month to let them recover,” he said. “Today the paradigm has changed dramatically. We invoke cardiovascular rehabilitation — riding bicycles, walking around tracks under supervision — almost immediately after a heart attack. If you have a heart attack today, provided you don’t have other issues ongoing, the following day we get you up in a chair. On day two, we walk you in the hall. On day three, you’re in a cardiac rehabilitation situation where you’re performing supervised exercise.”
With these things in mind — evidence about the benefits of exercise following cancer treatment and decades of lessons learned from heart attack recovery — the team, led by Dr. Hundley, is examining whether it is beneficial to walk, exercise and strength train in the days between chemotherapy infusions.
“This is no easy task for patients, because cancer treatment is horrible,” Dr. Hundley said. “You lie there in a chair and receive IV therapeutics that are toxic. They make you feel terrible, you experience nausea, vomiting and your hair falls out. About the last thing you want to do is move. There are many aches and pains related to cancer treatment.” PALS will use advanced MRI to measure exercise capacity, questionnaires to evaluate quality of life and fatigue, studies to measure cognitive ability, and blood tests to monitor inflammatory mediators that are associated with adverse cardiovascular effects.
PALS is a multicenter study that began this spring and has five more years to enroll patients. It is a unique, communitywide partnership in Richmond because VCU Health is partnering with Sheltering Arms rehabilitation centers to deliver interventions. “Our partnership with Sheltering Arms is important in providing facilities where patients who are immunocompromised can go and exercise without picking up an infection from someone else who has touched the equipment,” Dr. Hundley said. “We have to do these studies in cardiac rehabilitation facilities.”
These types of partnerships, both within VCU Health and in the wider community, are reasons Dr. Hundley sees
VCU Health and the MCV Campus as such an impactful place to conduct research and deliver care.
“Here at VCU, we’re trying to advance the care of everyone,” he said. “We don’t have the more traditional silos of operation; we’re integrating with a lot of different groups that freely exchange information. VCU Health also has enormous advantages related to technical capabilities. The MRI scanner we’ve discussed, for example, is one in which you can ride a bicycle and gather images simultaneously. There aren’t many places on Earth that can do that. “Applying this technology and interdisciplinary approach, you have Massey and Pauley working together and leveraging the talents of not just a health system,

but an entire university to address why we’re facing these problems and what solutions exist.”
If you are interested in helping the Pauley Heart Center continue to utilize the best resources and technology available, which enable preeminent patient care, research and education here in Central Virginia, please contact Carrie Mills, senior major gifts officer at VCU Health, at carrie.r.mills@vcuhealth.org.
1, 2Amitabh Parashar, W. Gregory Hundley. The Role of Cardiovascular Magnetic Resonance for Surveillance of Cardiac Performance upon Receipt of Potentially Cardiotoxic Cancer Therapeutics. Curr Cardiol Rep, 2018;20(12):142. doi:10.1007/s11886-018-1075-7. PMID: 30367282.
A Family Dedicated to Heart Health
Greg Hundley, M.D., graduated from VCU School of Medicine in 1988 and returned in 2018 to serve as director of the VCU Health Pauley Heart Center.
His return to the MCV Campus, and the opening of the Cardiac Imaging Suite where he conducts research, would not have been possible without the generosity of Stan and Dorothy Pauley and the Pauley Family Foundation. In addition to making a generous donation to name the Pauley Heart Center in 2006 and another multimillion-dollar gift in 2013, the family supported Dr. Hundley’s recruitment and funded the suite’s 3T MRI scanner, which is one of the most advanced MRI systems available in the world.
After the 2006 and 2013 gifts, Kenneth Ellenbogen, M.D., the Martha M. and Harold W. Kimmerling, M.D., Chair of

Cardiology, said the Pauley family had transformed VCU Health into a first-tier heart center by helping the health system devote resources toward renovating and improving research and attracting new faculty in cardiology to enable care of the sickest and most complex patients from all over the region. Stan Pauley is one of those patients. “This is a project that is near and dear to my heart,” he said in 2013. “The care these healthcare professionals provide is so genuine and moving that it is an honor to contribute to research that will enable them to learn even more about heart disease.” This February, Stan, Dorothy and the Pauley Family Foundation once again made an investment to fortify VCU Health as a national leader in cardiac care. The foundation donated $5 million to the Pauley Heart Center that will provide resources to research, diagnose and treat atrial fibrillation and ventricular tachycardia, which are two types of irregular heart rhythms. These rhythm disturbances increase mortality, reduce quality of life and limit a person’s ability to perform everyday activities. As the population ages, atrial fibrillation is increasingly common. “With the growing number of patients worldwide who develop atrial fibrillation, the gift from the Pauley family will help us work to develop new and more precise methods of mapping the heart to better identify and destroy the circuits causing atrial fibrillation,” Dr. Ellenbogen said.
Stan Pauley (left) greets Greg Hundley, M.D., director of the Pauley Heart Center, before the ribbon cutting at VCU Health’s new Cardiac Imaging Suite. Kathy Pauley Hickok and Gene Hickok are also pictured as they await the ribbon cutting. In addition to making a generous donation to name the Pauley Heart Center in 2006, the Pauley Family Foundation supported Dr. Hundley’s recruitment and funded a portion of the suite’s equipment. Photo: Kevin Morley, VCU University Marketing






