
4 minute read
Collaboration is key for research impact
Internal and external collaborations are the lifeblood of the applied research program at RaySearch, underpinning sustained product innovation that will ultimately benefit clinical customers and enhance patient outcomes. For Kjell Eriksson, the company’s Chief science officer, the task is to provide oversight and guidance for those diverse research efforts while ensuring alignment versus RaySearch’s long-term commercial and technology strategy.
Front and center among those broader priorities is RaySearch’s vision for comprehensive cancer care – a vision that will manifest through convergence of RayStation ®* and RayCare®* towards a unified system for planning, optimizing and managing patient care across a range of treatment modalities. The first step down this road, moving beyond RaySearch’s traditional core base in radiation oncology, came at the end of 2019 with the release of a dedicated RayStation module for chemotherapy planning. Now, Eriksson and his team are laying the foundations for further diversification with a suite of RayStation tools to support surgeons with the planning of operations for tumor removal. “Ultimately the goal is co-planning of radiotherapy, medical oncology and surgery within the same software platform,” he explains.
CUTTING EDGE A prototype surgery module is already in the works to inform planning and decision-making relating to partial liver resection. “The clinician will be able to visualize the tumor in relation to other substructures and blood vessels in the liver – identifying where to cut and what the remaining liver volume will look like after the tumor is removed,” says Eriksson. That research effort will intensify this summer, with clinical partners helping to evaluate the surgery prototype and further develop its functionality. “The bigger picture is compelling,” Eriksson adds, “with many other organs and disease indications likely to follow after clinical validation of this initial use case in the liver.”
Another headline theme for Eriksson and colleagues is automation of the radiation oncology workflow – including segmentation, treatment planning, as well as clinical decision support for individualized patient treatments. A case study in this regard is RaySearch’s high-profile clinical partnership with MD Anderson Cancer Center in Houston, Texas, where one of several joint projects under way is seeking to develop and validate an automated dose-tracking capability across all of a patient’s treatment fractions. The aim: to harness meaningful clinical results and data-driven insights that will form the basis of adaptive radiation therapy. “We’re working together to build a framework for data anal-
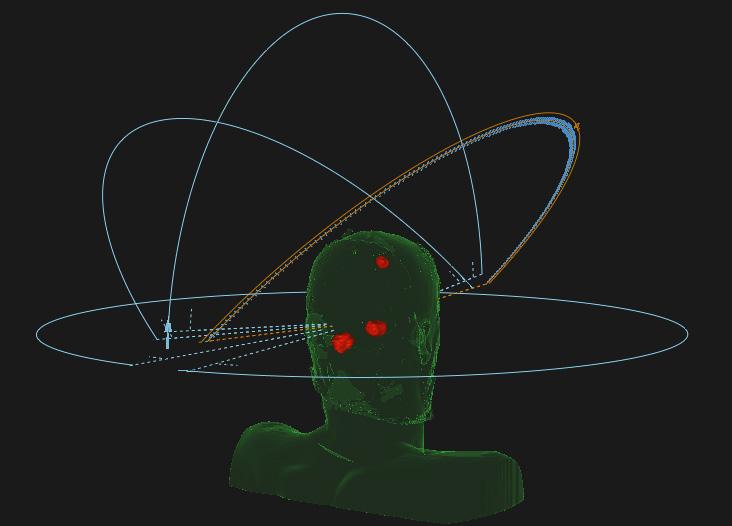
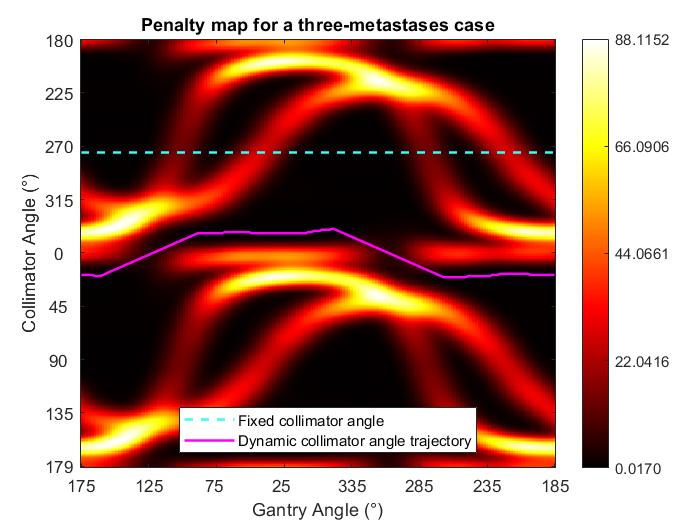
Fig1– Shows a typical beam configuration for SRS case, in particular for a three metastases case. Fig2–Shows a penalty map for a three metastases SRS case. A penalty map indicates areas of high and low penalty for each gantry angle with respect to a certain collimator angle. MACHINE UTILIZATION RaySearch’s sustained investments in R&D are evidenced through formal collaborations with a global network of more than 30 clinical partners. Yet in-house R&D collaboration is no less important, with Eriksson’s 23-strong research team working closely with the RaySearch development department on continuous improvements designed to utilize a range of treatment machines to their full potential. One joint area of focus right now is the use of stereotactic radiosurgery (SRS) to treat multiple metastases in the brain – a complex procedure where intelligent angle selection is critical to avoid unnecessary dose to healthy tissue between the tumor targets.
In a case with many metastases, for example, manual selection of the angles for SRS is a non-trivial task that can take several hours of planning time – even for an experienced medical physicist. “What we have done so far is develop an algorithm that optimizes the collimator angles of arc beams to avoid irradiating healthy brain,” notes Eriksson. “We’ll now continue to add more degrees of freedom with the ultimate goal being to reduce treatment time and planning time, as well as increasing the plan quality.”
ysis and result reporting using the RayAnalytics module within our new RayIntelligence platform,” notes Eriksson. As such, RayAnalytics is effectively “mining” the MD Anderson patient database to identify robust triggers for adaptive replanning based on how the tumor or organs at risk are responding to radiation treatment. A parallel track of the RaySearch/MD Anderson collaboration is seeking to embed automation in the radiation oncology workflow, streamlining and packaging a range of manual procedures into automated routines within a RayStation and RayCare setting. “Ultimately our plan is to provide these workflows as MD Anderson-certified templates to other clinical customers,” Eriksson adds.
FOCUS ON RADIOBIOLOGY Meanwhile, Eriksson’s team is also eyeing longer-term R&D opportunities around the use of radiobiological effects to expand the so-called “therapeutic window”. RaySearch is a partner in the European Union-funded HYPERBOOST consortium, for example, which is evaluating the clinical potential of a process known as hyperthermia – basically the heating of tumors to 40-44 °C as a means of enhancing the effectiveness of radiotherapy or chemotherapy.
Another radiobiology initiative with Lausanne University Hospital (CHUV) in Switzerland is working on FLASH radiotherapy of deep-seated tumor targets using very-high energy electron beams. Here the RaySearch team has developed a prototype Monte Carlo dose computation engine to support ultrafast radiation treatment at dose rates several orders of magnitude beyond current clinical norms while minimizing collateral damage to adjacent healthy tissues. “One thing is certain,” Eriksson concludes. “Clinical research partnerships will remain central to our delivery of advanced software products and innovations shaping the cancer care of tomorrow.”










