13 minute read
Comparison of Bolton Analysis Between Interproximal Stripping and Mandibular Incisor Extraction to Resolve Lower Anterior Crowding – A Cross-sectional Study
By Dr. Mubassar Fida and Dr. Dr. Kanza Tahir
Dr. Mubassar Fida graduated from Nishtar Medical College: Multan, Punjab, PK. Residency in Orthodontics from Alvi Dental Hospital: Karachi, Sindh, PK.Membership in Orthodontics European Orthodontic Society: London and American Association of Orthodontists: Creve Coeur, Missouri, US, and Fellowship in Orthodontics from College of Physicians. MS in community dentistry. He has authored many indexed original research articles and has also presented his work at various national and international forums. He has received numerous awards for his research presentations both internationally and nationally.
Advertisement
Dr. Kanza Tahir graduated wrom Liaquat University of Medical and Health Sciences, Jamshoro in 2017. After passing her FCPS part-1, her interest in Orthodontics led her to acquire residency in a well-known institution of Pakistan. Currently, she is working on three research work projects related to orthodontics.
Abstract
Background/Objective:
The debate between the two treatments of crowding – whether to extract teeth or use a non-extraction method – has not yet seen a universal winner among modern orthodontists. This study aimed to evaluate the differences in Bolton Ratio (BR) of patients with mild-moderate crowding treated with mandibular incisor extraction or interproximal reduction passing the American Board of Orthodontics – Objective Grading System (ABO-OGS) criteria.
Materials and methods:
A cross-sectional study was conducted in a tertiary care hospital. Preand post-treatment dental casts were utilized to calculate the BR. Posttreatment dental casts and panoramic radiographs were used to determine the ABO-OGS scores of interproximal reduction (IPR) and mandibular incisor extraction (MIE) groups. A total sample size of 40 was required for the study with 20 cases in each group. The Wilcoxon signed-rank test was used to compare pre- and post-treatment Bolton changes. The MannWhitney U test was used for comparison between IPR and MIE group. Linear Regression was used to determine the association among variables.
Results:
In comparison between IPR and MIE groups, statistically significant differences (p ≤ 0.05) were seen in post-treatment anterior Bolton. Statistically significant differences were also reported for alignment, buccolingual inclinations, and occlusal contact scores. On linear regression, the difference in ABO-OGS scores increased by 4.4 units in the IPR group.
Conclusions:
Pre-treatment anterior maxillary excess led to increased overjet scores. Mandibular incisor extraction caused maxillary anterior Bolton excess which raised the overjet scores. Increased ABO-OGS alignment scores were found in the interproximal reduction group.
Keywords:
Mandibular crowding, ABO-OGS, Bolton analysis
Introduction
Correct alignment of teeth is one of the essential goals of orthodontic treatment.1 An attractive smile and accurate alignment of the front teeth are the focal objectives for individuals pursuing orthodontic treatment.2 The anterior region displayed on smile is unique to every individual face and is composed of three components: dental, gingival, and soft tissue components. The dental component comprises the anterior teeth alignment, position, size, shape, and color.3 With an advancing age, soft tissues tend to sag, increasing the lower incisors’ show.4 In adults, the mandibular incisor region is most susceptible to patients’ dissatisfaction and is a cause of concern due to increased exposure of lower incisors on smile.5
The last three decades have revealed that individuals over 20 years mostly exhibit late mandibular crowding.6 Initially, Begg shed some light on the cause of late lower incisor crowding that inadequate interproximal enamel reduction (IPR) may be an element, whereas Müller proposed that crowding may be caused by increased pressure from the buccinator muscle due to inappropriate lowered tongue posture.7 However, Corruccini associated the lack of space with a gradual decrease in the size of the craniofacial structures.8 Different approaches are available to resolve mandibular crowding depending on the severity, which may involve exodontia, interproximal wear, dental expansion and distraction osteogenesis of the mandibular symphysis.9,10
According to Ileri et al,10 a PAR index assessment indicated that malocclusions improved by extracting mandibular incisor where there was mandibular anterior Bolton discrepancy in which the anterior ratio was equal to 81.7 ± 4.5. This suggests that in cases in which there is non-significant mandibular Bolton excess, the best substitute may be interproximal stripping.11,12,13 It is crucial for a satisfactory outcome to establish which method gives a better post-treatment outcome.
By utilizing the American Board of Orthodontics – Objective Grading System (ABO-OGS) discrepancy index and comparing the pre- and post-treatment Bolton ratio (BR), our aim was to establish which method gives better treatment outcomes. Furthermore, this study can help future researchers to derive a range of BR in MIE or congenitally missing lower incisor cases.
Our primary objective was to study the differences in BR between patients treated by MIE and IPR. The secondary objective of this study was to determine the components of ABO-OGS that led to higher scores in both groups.
Materials and Methods:
After obtaining approval from the departmental ethical review committee (2022-5939-16676), a cross-sectional study was conducted on a sample size of 40 (N) in a tertiary care hospital. Data were collected using the pretreatment and post-treatment dental casts. The mesiodistal widths of each tooth from first molar to the contralateral first molar were obtained using a digital vernier caliper to obtain overall BR. For anterior BR, mesiodistal widths of all teeth from canine to its antimere were obtained. The overall and anterior BR were calculated by the formulas reported in the original Bolton study.14 After calculating the BR, we utilized the post-treatment dental casts and panoramic radiographs to measure the ABO-OGS scores. All the eight criteria were precisely measured by following the guidelines provided by ABO in 1999 using a marking chart provided by Saini P et al.15 in their study. Each component was precisely measured and scored according to the ABO-OGS criteria. The passing criterion was a cumulative score of less than 25. The sample size was calculated with OpenEpi® software v. 3.01, using the findings of Ileri et al.10 who reported a standard deviation of overall ratio for the MIE group to be 2.9 and for non-extraction group 2.0 with a mean difference of 2.5. Keeping α = 0.05 and a power of 80%, at least 16 (n) subjects were required in each group. With 10% inflation, the total sample size for each group was 20. Since we had two groups – Group 1 (IPR) and Group 2 (MIE) – a total sample of 40 (N) was required.
The dental casts included in our study had the following criteria: the casts with a crowding of 2-6 mm, good quality dental casts and radiographs, dental casts that had a complete pre and post-treatment record, nonextraction fixed mechanotherapy cases that followed IPR of both arches and cases with single MIE with no other extractions. The exclusion criteria were cases with crowding of greater than 6 mm, cases with multiple extractions, and any dental model with effects of parafunctional habits on the dentition. Casts of patients with abnormal tooth morphology of the maxillary lateral incisors and lower second premolars or any other teeth were excluded. Dental casts with any missing teeth were also excluded.
Statistical Anaylysis
Data were analyzed using SPSS software (version 23.0). Shapiro-Wilk test was used to determine the normality of the data which showed a non-normal distribution. Frequencies were reported for categorical variables such as gender. Descriptive statistics median and interquartile range (IQR) were reported for age and ABO-OGS scores. Wilcoxon signed-rank test was used to compare pre- and post-treatment Bolton changes within each of the IPR and MIE groups. Spearman’s correlation was used to determine the correlation amongst the variables. Mann-Whitney U test was used for comparison between IPR and MIE groups. Linear regression was carried out to determine the association among variables. Intra-class correlations (ICC) were applied to determine the intra-examiner reliability by measuring the pre- and post-bolton ratios at 2 weeks interval. A p-value < 0.05 was considered statistically significant.
Results:
Demographics:
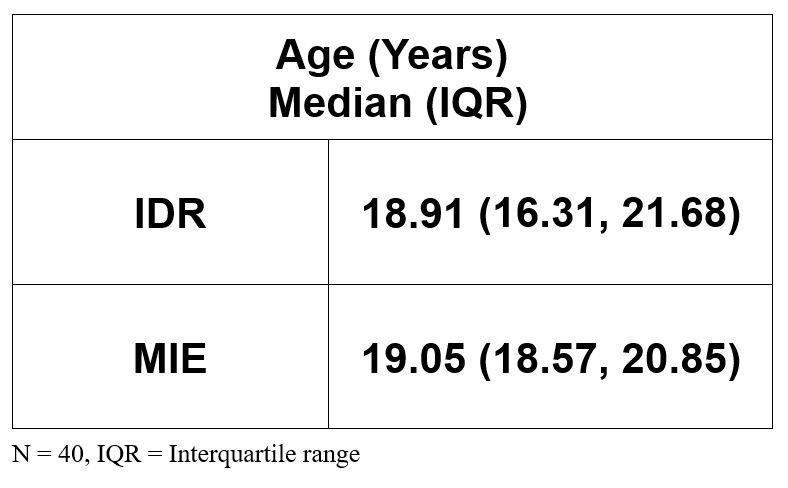
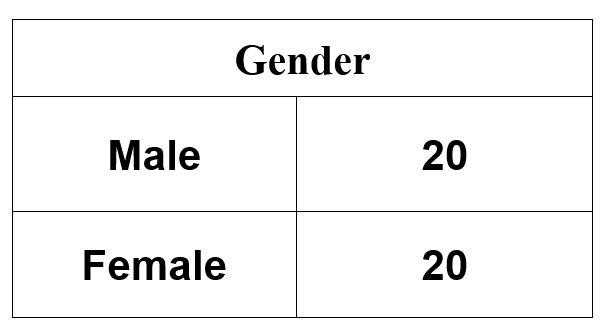
In this study, dental casts of 20 males and 20 females were studied (Table 1). The median ages of IPR and MIE groups were 18.91 years (16.31, 21.68) and 19.05 years (18.57, 20.85), respectively (Table 2). There was a comparable gender distribution between the two groups.
A comparison between IPR and MIE groups was done with a statistically significant difference found in post-treatment anterior BR (Table 3). Statistically significant differences between the IPR and MIE groups were also found for alignment with median scores of 6.00 (3.25, 7.75) and 3.00 (2.00, 5.00) respectively. Statistically significant values were revealed for buccolingual inclinations with median scores of 9.00 (8.00, 10.00) and 6.50 (5.00, 8.75) for the IPR and MIR groups, respectively.
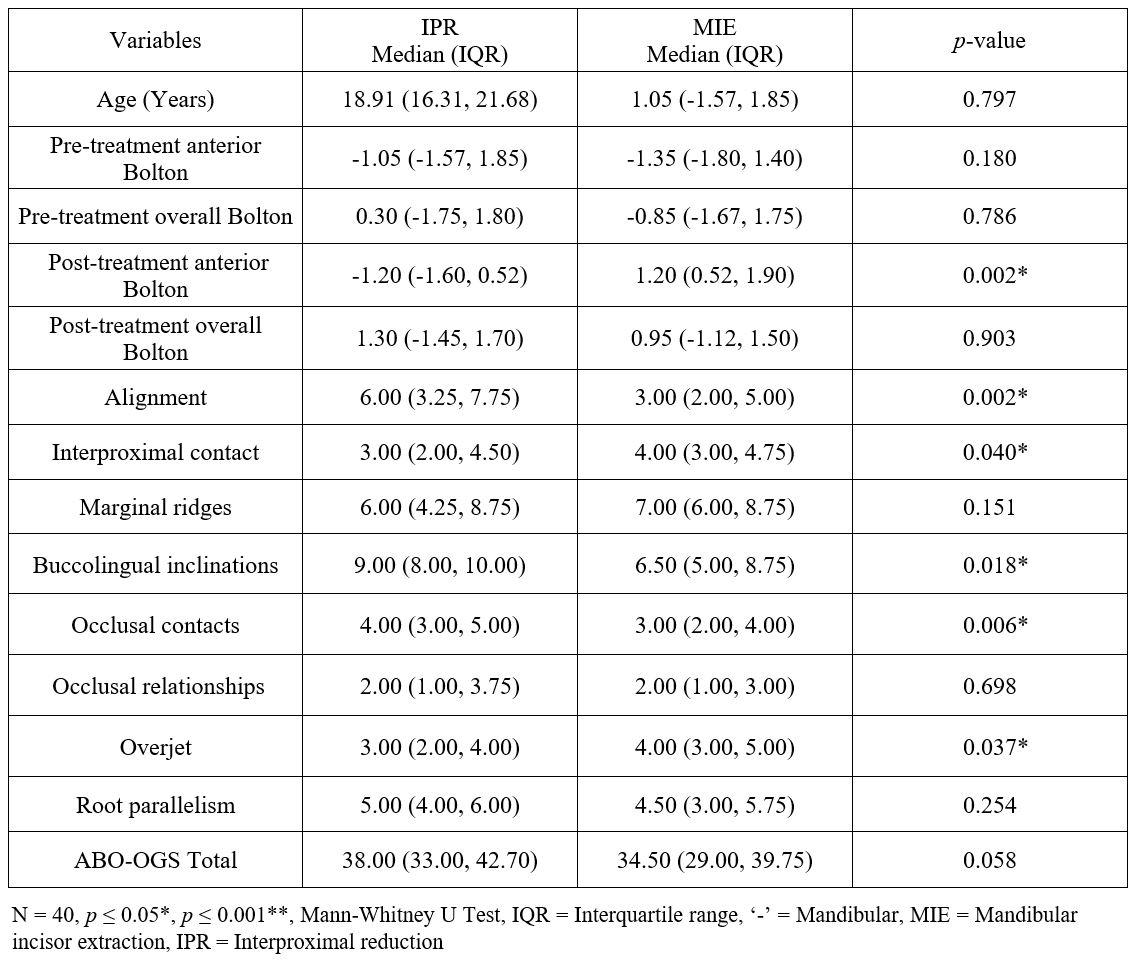
Significant differences were also observed for occlusal contacts (p = 0.006) and interproximal contacts (p = 0.040). The ABO-OGS median scores for the IPR group was 38.00 (33.00, 42.70) and for the MIE group was 34.50 (29.00, 39.75) (p = 0.05). MIE group had better median scores for alignment, occlusal contacts, and buccolingual inclinations. However, the IDR group scored better in interproximal contacts (p = 0.040). The comparison between both groups revealed that the overall ABO-OGS scores were better for the MIE group however, they were statistically non-significant.
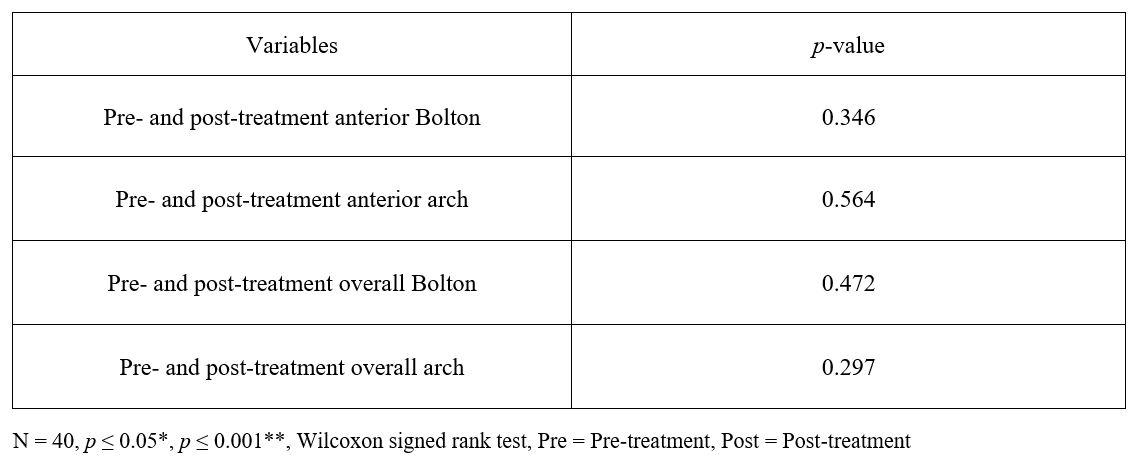
Comparison between the pre-treatment and posttreatment BR showed statistically non-significant differences between the two groups (Table 4).
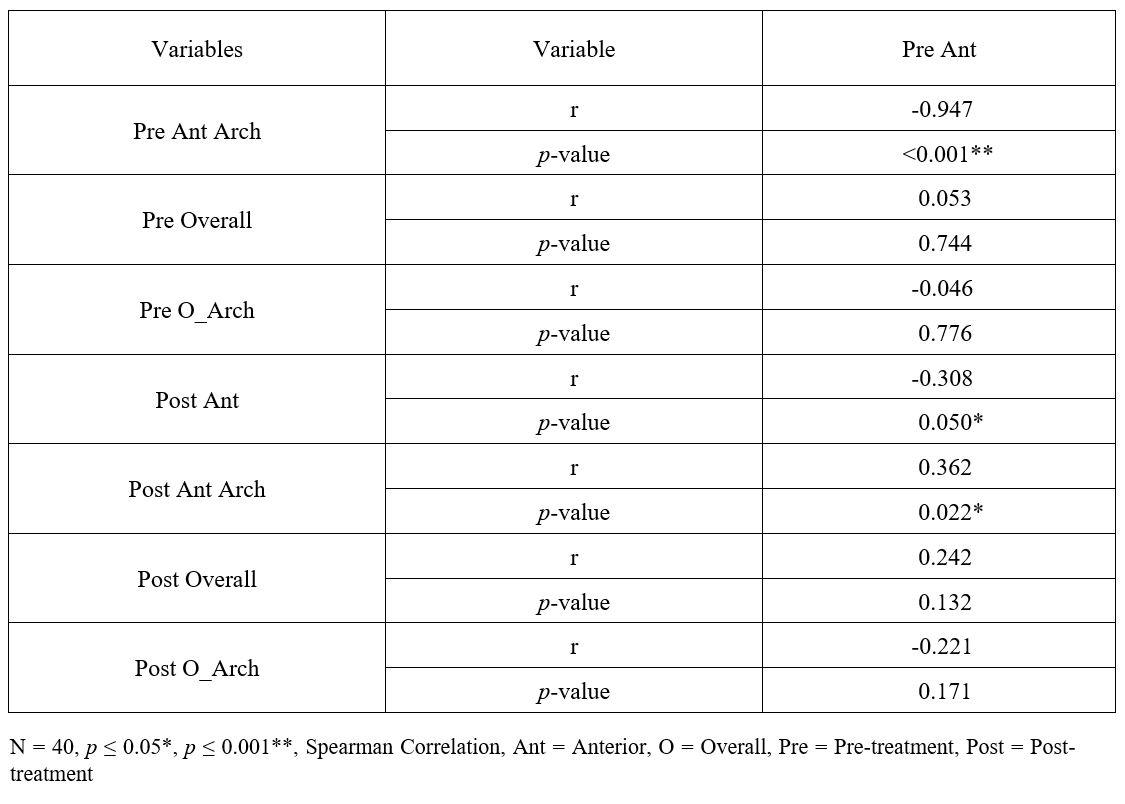
Spearman correlation showed that pre-treatment anterior Bolton had a highly significant (p < 0.001) negative and a very strong correlation with the pretreatment maxillary arch excess (Table 5). Post-treatment anterior Bolton was found to be significantly (p = 0.050) correlated with the pre-treatment anterior Bolton.
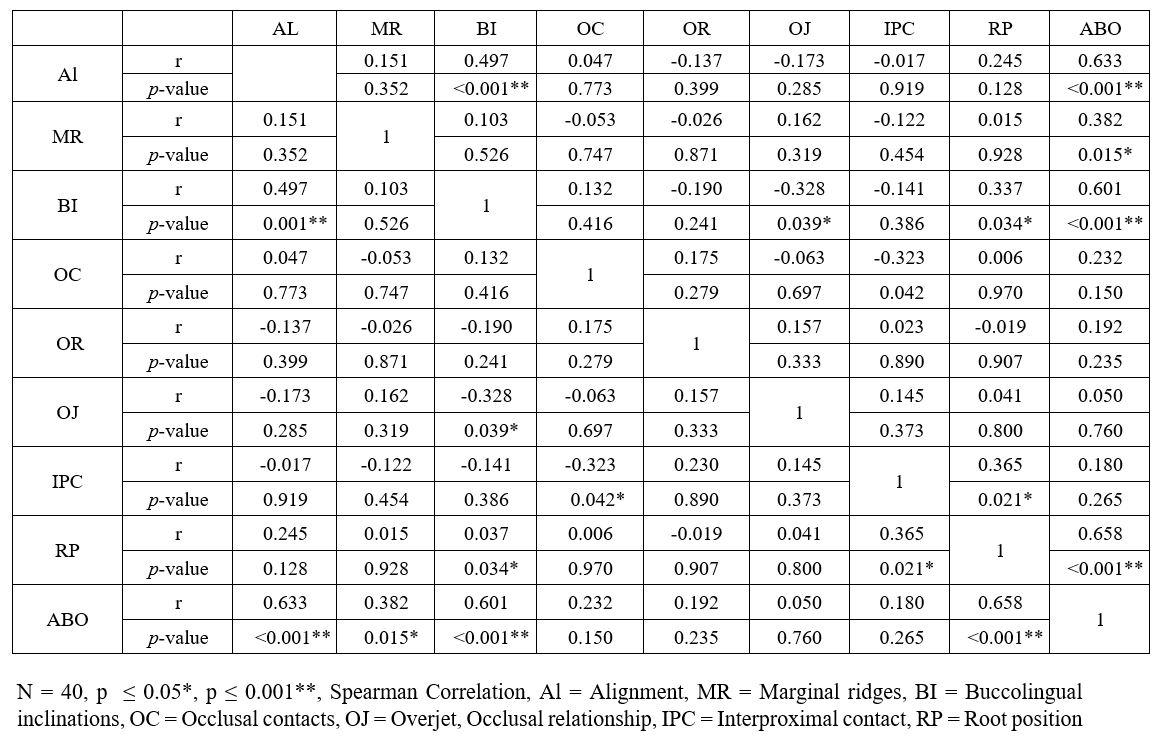
Pre-treatment anterior Bolton had a significant negative and weak correlation with overjet scores (Table 6). Post-treatment anterior Bolton had a significant positive and a weak correlation with marginal ridges scores, indicating that the maxillary excess led to higher marginal ridges scores. Alignment had a highly significant (p ≤ 0.001) positive and a moderate correlation with the buccolingual inclinations (Table 7). Poor alignment scores led to increasing in buccolingual scores. Moreover, the buccolingual scores had a highly significant (p ≤ 0.001) and a positive strong correlation with the ABO-OGS scores. The raised buccolingual scores also led to increased ABO-OGS scores. Interproximal contacts (IPC) had a statistically significant (p = 0.021) positive and a weak correlation with the root position (RP). Increased IPC scores led to higher root positioning scores. Moreover, the RP scores had a significant positive and a very weak correlation with the buccolingual inclinations. Higher RP scores led to increased buccolingual inclination scores. The RP, marginal ridges, and buccolingual scores led to increase in the ABO-OGS scores.

Discussion
Orthodontic treatment focuses on providing an aesthetic smile and optimal oral functions by carrying out an individualized treatment plan. Over the years of the orthodontic profession, many different treatment modalities have been put forward, each with its own merits and demerits.16 Two commonly applied methods of gaining space in moderate crowding cases are interproximal reduction and exodontia. The current study aimed to differentiate between the BR after IPR and MIE treatment modalities along with differences in ABO-OGS scores attained posttreatment. We rejected our null hypothesis, as significant differences were observed in the anterior BR after IPR and MIE treatment.
MIE has been a frequently contested treatment modality in orthodontic literature and practices. The controversy lies in the inherent side effects of the treatment modality including but not limited to; increased overjet, increased overbite, decrease in lower intercanine width, class III canines, loss of canine guidance and anterior BR excess in the maxilla at post-treatment.17 Due to these side effects, some practitioners tend to avoid using MIE as a treatment modality. In the current study, a significant difference was observed between the two groups when analyzing the post-treatment anterior BR. IPR group had a minimal mandibular excess, whereas the MIE group had maxillary tooth material excess at posttreatment. These findings are in agreement with Illeri et al.10 who found differences in the anterior BR after nonextraction and MIE treatment.
While there are many side effects to MIE therapy, when used in light of its indications, it has been demonstrated to be an efficient treatment modality in solving mild to moderate anterior mandibular crowding. MIE can be indicated in well balanced soft tissue profiles, interdigitated posterior occlusion, minimal overbite and edge to edge overjet cases.18 In our study, MIE group had better ABO-OGS scores as compared to the IPR group and the statistical difference was found to be nearly significant. This is in agreement with a study conducted by Safavi et al.18 who used PAR improvement percentages to observe the effect of MIE treatment modality. They reported significant improvement with the MIE treatment modality with greatly improved PAR percentages. The reasons cited in their study that led to a decrease in PAR improvement percentages were overjet scores and midline discrepancy scores. When observing the ABO-OGS components used in our study, we also found significant differences in overjet scores between the two treatment modalities with the MIE group having higher scores for this component. However, these findings were in contrast with Maaz and Fida,19 who reported lower PAR and Index of Complexity, Outcome and Need (ICON) scores in MIE when compared to non-extraction. It is important to state that even though lower scores were obtained than non-extraction, the MIE group still had greatly improved PAR percentages and outcomes assessed by ICON.
Many solutions to the drawbacks presented by MIE have been suggested in the literature.20 Studies suggest careful consideration of the pre-treatment condition of malocclusion with a focus on the indications mentioned in the preceding paragraphs. Some studies have suggested the use of the modality only in cases of significant mandibular tooth material excess. A recent study suggested the evaluation of the BR after leveling and alignment have been performed during MIE treatment.21 This analysis allows the quantification of the maxillary excess that has been created by the treatment modality, which leads to an accurate correction of the tooth material excess. Once the tooth material excess has been mitigated, the occlusal relations would be ideal including the overjet and canine relationship.22
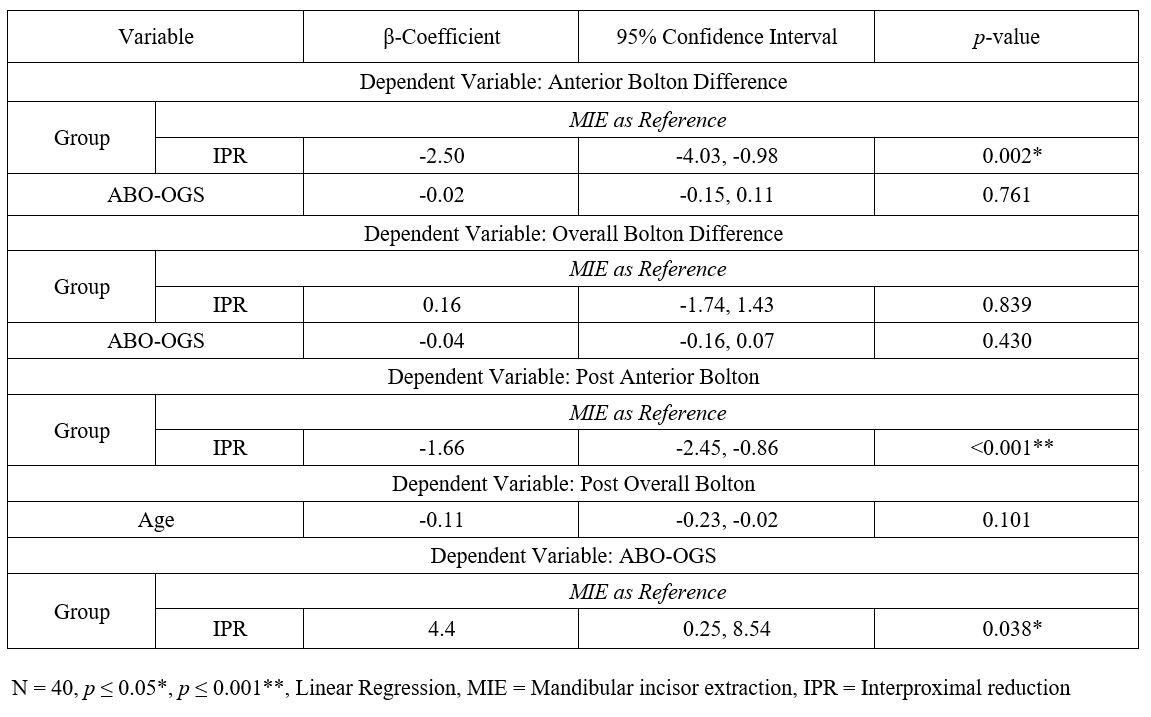
On assessing the linear regression analysis, the relationship between anterior and overall BR was analyzed with the treatment modalities. Anterior BR difference when assessed along with MIE as reference showed significant results in the IPR group. (β = -2.50, 95% C.I: -4.03,-0.98) This signifies the maxillary excess that is observed after MIE treatment and the mandibular excess seen after IPR. Clinicians should evaluate BR both in the anterior and overall, during the finishing stages of treatment so that ideal occlusal relationships can be obtained.
When the relationship of ABO-OGS scores along with the treatment modality was assessed, IPR treatment modality was found to be associated with higher ABOOGS scores when MIE was kept as a reference. (β = 4.4, 95% C.I: 0.25,8.54) These results show that better occlusal and functional results as analyzed using the ABO-OGS index can be obtained with MIE. These differences can be attributed to the amount of space that can be obtained with MIE as compared to IPR which involves judicious removal of 0.25mm of each interproximal surface in the anterior region. These differences can also be attributed to the decreased number of teeth involved in the analysis in the MIE group as one tooth is extracted. This leads to one less tooth analyzed for the overjet, alignment, root parallelism and interproximal space components of the ABOOGS as compared to the IPR group. This may lead to a decreased total ABO-OGS score in the IPR group which might not be attributable to the functional relationships in post-treatment but is instead due to the mismatch in the number of teeth analyzed.
The current manuscript aimed to differentiate between the IPR and MIE treatment modalities in lieu of the BR that is present in pre- and post-treatment.
Certain limitations existed in our study, it being a single center study with a purposive sampling design. The study finds its strength in the sampling; the cases included were treated under two different consultants which helped mitigate operator bias in our study. MIE treatment modality allowed better ABO-OGS scores, but certain limitations exist in its execution which can be managed by careful analysis of the BR. Ideal BR at the end of treatment allows ideal finishing of the occlusion which is functionally stable and aesthetically pleasing.
Conclusions:
1) Pre-treatment anterior Bolton maxillary excess led to increased overjet scores
2) Mandibular incisor extraction caused maxillary anterior Bolton excess which raised the overjet scores.
3) Increased ABO-OGS alignment scores were found in the interproximal reduction group.
References
1. Sabri R. Orthodontic objectives in orthognathic surgery: state of the art today. World J Orthod. 2006;7:177-91.
2. Soh J, Wang ZD, Zhang WB, Kau CH. Smile attractiveness evaluation of patients selected for a U.S.-based board certification examination. Eur J Dent. 2021;15:630-8.
3. Sarver DM. The importance of incisor positioning in the esthetic smile: the smile arc. Am J Orthod Dentofacial Orthop. 2001;120:98-111.
4. Drummond S, Capelli J Jr. Incisor display during speech and smile: Age and gender correlations. Angle Orthod. 2016;86:631-7.
5. Aydoğdu E, Özsoy OP. Effects of mandibular incisor intrusion obtained using a conventional utility arch vs bone anchorage. Angle Orthod. 2011;81:767-75.
6. Zigante M, Pavlic A, Morelato L, Vandevska-Radunovic V, Spalj S. Presence and maturation dynamics of mandibular third molars and their influence on late mandibular incisor crowding: A longitudinal study. Int J Environ Res Public Health. 2021;18:100-70.
7. Antoszewska-Smith J, Bohater M, Kawala M, Sarul M, Rzepecka-Skupień M. Treatment of adults with anterior mandibular teeth crowding: reliability of Little’s Irregularity Index. Int J Dent. 2017;17:50-7.
8. Varrela J. Masticatory function and malocclusion: A clinical perspective. Semin Orthod. 2006;12:102-9.
9. Almeida NV, Silveira GS, Pereira DM, Mattos CT, Mucha JN. Interproximal wear versus incisors extraction to solve anterior lower crowding: a systematic review. Dental Press J Orthod. 2015;20:66-73.
10. Ileri Z, Basciftci FA, Malkoc S, Ramoglu SI. Comparison of the outcomes of the lower incisor extraction, premolar extraction, and nonextraction treatments. Eur J Orthod. 2012;34:681-5.
11. Jangra VK, Sharma A, Sharma R, Sharma S. Mandibular expansion in orthodontics: A review. Int Health Res J. 2022;6:6-10.
12. Frindel C. Clear thinking about interproximal stripping. J Dentofacial Anom Orthod 2010;13:187-99.
13. Hariharan A, Arqub SA, Gandhi V, Kuo C, Uribe F. Evaluation of interproximal reduction in individual teeth, and full arch assessment in clear aligner therapy: digital planning versus 3D model analysis after reduction. Prog Orthod. 2022;23:9-15.
14. Bolton WA. The clinical application of a tooth-size analysis. Am J Orthod. 1962;48:504-29.
15. Saini P, Maurya RK, Singh H. Time-saving scoring chart for the American Board of Orthodontics’ objective grading system. APOS Trends Orthod. 2020;10:262-5.
16. Moon S, Mohamed AMA, He Y, Dong W, Yaosen C, Yang Y. Extraction vs. Nonextraction on soft-tissue profile change in patients with malocclusion: A systematic review and meta-analysis. Biomed Res Int. 2021;2021:1-11.
17. Zhylich D, Suri S. Mandibular incisor extraction: a systematic review of an uncommon extraction choice in orthodontic treatment. J Orthod. 2011;38:185-95.
18. Safavi S, Namazi A. Evaluation of mandibular incisor extraction treatment outcome in patients with bolton discrepancy using peer assessment rating index. J Dent. 2012;9:27-34.
19. Maaz M, Fida M. Comparison of treatment outcomes as assessed by 3 indexes in subjects with Class I malocclusion treated by 3 different methods: A cross-sectional study. Am J Orthod Dentofacial Orthop. 2022;161:537-41.
20. Kamal AT, Shaikh A, Fida M. Improvement in peer assessment rating scores after nonextraction, premolar extraction, and mandibular incisor extraction treatments in patients with Class I malocclusion. Am J Or thod Dentofacial Orthop. 2017;151:685-90.
21. Sang SH, Chooryung SA, Yoon J, Woo JC, Kimc J. Long-term follow-up of a patient with deepbite and severely resorbed maxillary central incisors treated by maxillary premolar and mandibular incisor extraction. Am J Orthod Dentofacial Orthop. 2022.
22. Joseph R, Valinoti. Mandibular incisor extraction therapy. Am J Orthod Dentofacial Orthop. 1994;105:107-16.
BR=Bolton ratio
ABO-OGS = American Board of Orthodontics –Objective Grading System
IPR:Interproximal reduction
MIE: Mandibular incisor extraction
IPC: Interproximal contacts
Al = Alignment
MR = Marginal ridges
BI = Buccolingual inclinations
OC = Occlusal contacts
OJ = Overjet
OR = Occlusal relationship
IPC = Interproximal contact, RP = Root position










