6 minute read
Lymphoedema or Lipoedema and what are they?
from Heal Canada Issue 3
by healcanada
by Hazel Bell
My introduction to this “disease” of lymphoedema and lipoedema was to understand just how big my legs were after my heart surgery and the truth to myself that I did not have to accept this. At first, I was told by the Cardiac surgeon and then reaffirmed over the next five years by my GP doctor that I just needed to lose weight andexercisemore.
Well, for five years, I did watch my diet and exercise to the limit of my physiotherapist's advice, but my legs only continued to get larger. My pants became more challenging to get over my knees and thighs, yet the waist was getting too big. I even went so far as to start purchasing wide-leg pants, which were getting tight in theleg.
A friend and doctor saw me walking toward her one day, and she was shocked to see the size of my legs compared to the upper part of my body. “You have done so great with taking care of yourself and getting fit, why are your legs so large?” In response to her shock, I askedthesamequestionmyself.
In self research on the internet (I know, not the place for truthful information), I was able to find some very credible sources and books to read. Plus, I then began talking to others with similar issues, and not just legs, people with one arm enlarged from breast cancer surgery.
I discovered that the lymph system is sadly neglected during medical school for doctors and medicalstaff,onlylearningthebasicknowledgeofanatomyandphysiology.Lymphoedemais animbalanceinthepropermovementanddrainageofthelymphsystem. Becausethelymph system is so close to the vein/artery system of the body, treatment is often misdiagnosed as vascular-related. Patients, mainly cancer-related, who have had lymph node extraction, are very susceptible to developing lymphoedema. Like many others have carried the burden of seeking care outside the current medical system. Oncology-related treatment referrals are oftenavailable,buttheseservicesinsidethecurrenthealthsystemareoverburdenedandhave limitedentry.
Ihavebeenblessedwithacommunitynetworkoffriendswhoreferredmetoalocalclinicfor lymph-balancing treatment. Still, this service is limited to trained therapists, unavailable in everycommunity,and,inmostcases,isanentirelyout-of-pocketcosttotheindividual.
Lymphoedema or Lipoedema and what are they?
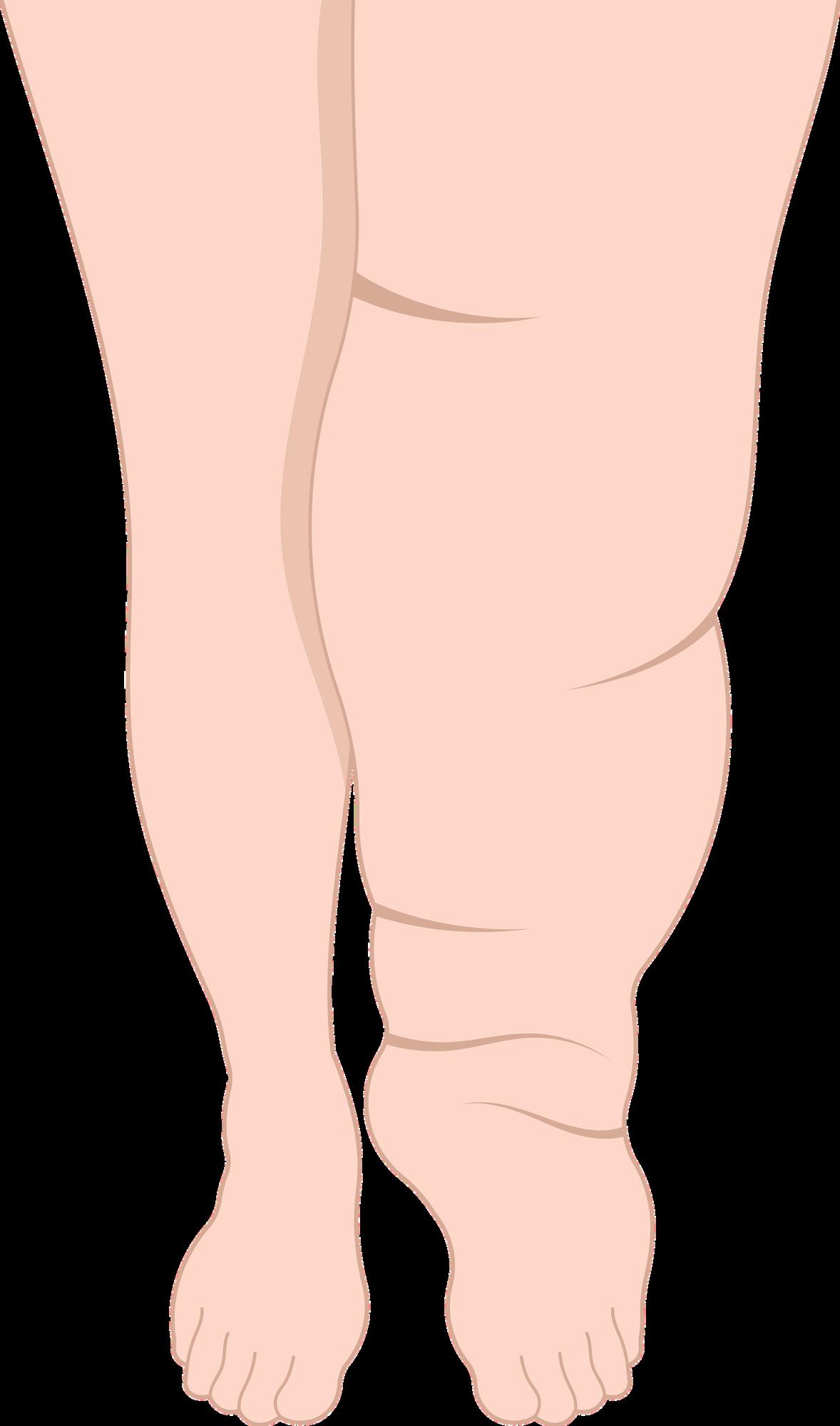
It has helped me understand that the correct term for me is ‘Lipoedema,’ a clinical condition seen in women with a link to obesity and osteoarthritis of the knee when the lymphatic system is out of balance with the lymph nodes' operation. I resemble this definition as my upper body hasremainedslim,withlegsthatresembleridingbreeches.
The swelling extends from the pelvic grill down to the ankle, with a fatty pad in the inner thigh of both thighs at knee level. My ankles will swell to the size of my thigh in a four-hour car ride, whichcanbemistakenfordeepveinthrombosis.
Some similar treatments include elevating legs, wearing personally fitted compression garments, and ensuring proper shoes and/or orthotics. It is important to note that any form of vein treatment and sclerosing injections can be potentially dangerous for both lymphoedema andlipoedema(toolateforme!).
Using compression leggings and elevating my feet will generally reduce ankle swelling within 24 hours. However, regular lymph drainage treatments by a registered massage therapist with Dr. Vodder'scertifiedlymphedematraininghavehelpedmeregainmylegs.
I now wear personally fitted compression tights or stockings daily, wear a flat and supportive shoe, continue with proper diet and exercise, and receive regular lymph balance treatments. Each step allows me to walk without feeling like my legs are tree trunks being hauled around. My personal goal is to not need my leggings or stockings every day, especially when the weather is hot, fit back into my dress pants, and wear a healed dress shoe at special occasions.
**Link to include for additional information and resources in your area: https://www.canadalymph.ca/home-of-the-pathways-magazine/

Masen’s Story
by Melanie Colter
My son, Masen, was born on May 25, 2013, in Surrey, British Columbia, Canada, just outside of Vancouver, British Columbia. His newborn screening test came back with no concerns, so we headed home with our happy, and we believed healthy, newborn baby boy
As first-time parents, Masen immediately became our entire world, bringing us happiness. He was a very content baby, always eating and sleeping well and began to smile and giggle early. We never had any serious concerns about his health or well-being. It was February 2021, and Masen was a healthy and active sevenyear-old
My husband Ryan stayed home that morning, and I took Masen appointment. Masen had been wearing glasses since he was about five years old, so this appointment was nothing unusual. During the appointment, our eye doctor did all the usual things, but there was a point where I felt a shift in his demeanour, and he had one of his staff members come and take Masen to look at glasses in another room. The door had barely closed, and I anxiously asked what was happening. The doctor did his best to assure me that his concerns would have to be investigated, but he was clear that the shaking he saw in Masen’s lenses in his eyes was not to be ignored, and he asked me a series of questions about Masen’s overall health. He mentioned something about a possible connective tissue problem and used the term Marfan’s syndrome, which I later learned has been a misdiagnosis for those with HCU in the past, as it mimics many of the symptoms associated with it. He told me he would write to our pediatrician, and we would start investigating. What this eye doctor was doing, I later realized, wastakingtheleadonsavingMasen’slife.

WhileMasenhappilychattedwiththestaffandlookedatglasses,Ididn’twasteamomentandI discretely looked up Marfan’s syndrome and connective tissue disorders on Google on my phone. Let’s say that my need for answers outweighed any logical thinking. I should have waited. Upuntilthatmoment,Iwasoneofthosepeoplewhohadlivedblissfullyandignorantly,unaware of anything that had to do with the rare disease community. My biggest health scare for my child up until then had been a few high fevers. HCU never once showed up on any of my frantic Google searches. For the next three months, the number of questions far outweighed any answers we would get at any time soon. The potential outcome wasn’t clear in any way, and my mindwasaterrifyingplacetobe.
It was Mother’s Day weekend, 2021, when we first heard the word Homocystinuria. Our pediatrician called us after reviewing the most recent bloodwork. From there, we were set up with the metabolic team at BC Children’s Hospital, and on June 25, 2021, we had the official diagnosis.Masenhadjustturnedeightyearsoldthemonthbefore.
Up until this point, Ryan and I had kept the details of everything from Masen because we had no solid information to share. But now, essentially overnight, Masen had to change his diet completely and start drinking the terrible-tasting formula. He had always been such an
Masen’s Story cont'd adventurous eater. He loved all the high-protein foods – eggs, seafood, steak, chicken. We had to explain to him in the most age-appropriate way that we now know these foods aren’t good for his body.
Much of what I mentioned here – months of living in fear, many worst-case scenarios entering your mind on a minute-to-minute basis, having to entertain every parent’s worst nightmare - this all comes from babies being missed at newborn screening. A diagnosis at birth is by no means an easy roadandIwouldneversuggestthat.
For us, with a late diagnosis, we didn’t only grieve the loss of the future we thought we had, the future we thought Masen had, but we had to grieve the type of lifestyle we had been living and just lost We had to tell our eight-year-old that he could not eat most of his favourite foods again, and then we had to enforce that strictly We had to sit with him and watch helplessly as he forced himself to drink the formula We had to start bringing him for blood work regularly so he could be poked and hurt, and there was no end in sight And he felt fine; he wasn’t “sick ” Further, we had some serious investigating to do to find out what damage had been done after going eight years undiagnosed, all while eating a very high protein diet. We felt like our son was a ticking time bomb with all these possible scary outcomes, and to this day, we are infuriated that had this been prevented by being diagnosed at newborn screening, none of this would have happened. We couldbarely comprehendMasen’snextmeal,letalonewhattherestof ourliveswouldlook like.
Here’s what it started to look like Ryan and I spent hours in grocery stores looking at labels We did this alone, and then we did it with Masen and had him help find things that would work We focused on how lucky we were to know and understand his body’ did was get curious and connect with people in similar circumstan tostop resisting theinevitable.Thiswasournewlife,anewreality
And remember that eye doctor? Because of him, we could see a specialist who performed two eye surgeries on Masen, one on each eye, just last year. Those shaking lenses were removed to prevent them from detaching and causing further damage. Masen wears a particular pair of contact lenses to see correctly, and he can see better than ever. Our eye doctor is very humble and says he was doing his job, but I’m sure he saved my son’s life and at least saved him from severe eye damage that would have been much harder to fix had we not known.
Today, Masen is a hard-working, athletic, resilient grade-five student who loves sports, specifically hockey, football and basketball. He loves to make everyone laugh with his quick wit and sarcasm. He is remarkable in every way and more courageous than anyone I know. We are so proud of the person thatheis.
Author Bio and Contact Information

Melanie Colter is mom and advocate for her ten-year-old son, Masen. She loves to connect with others in the rare disease community after experiencing firsthand the challenges, uncertainties and lack of resources faced by those who receive a rare diagnosis. Melanie lives just outside of Vancouver, British Columbia with her husband and son.
Melanie can be reached via email at mcolter82@gmail.com

If you would like to share your story about your journey, as a patient, caregiver, or advocate, send us a short (150 words) description of your journey, for consideration in an upcoming issue! email your submission to: digitalmagazine@healcanada.org













