
2 minute read
Stem Cell Transplant Success
by Wim Smits
In the Fall of 2018, routine blood work during my annual physical revealed that I had some abnormal blood counts. Repeating the blood tests confirmed the counts. As a result, I was referred to Dr. Nicole Laferriere, hematologist and Chief of Oncology at Thunder Bay (where I live) Regional Health Sciences Centre, for further testing. More detailed blood work was done, along with an abdominal ultrasound, CAT scan, and a bone marrow biopsy. Those tests revealed that I had a rare, terminal blood cancer called Primary Myelofibrosis (PM).
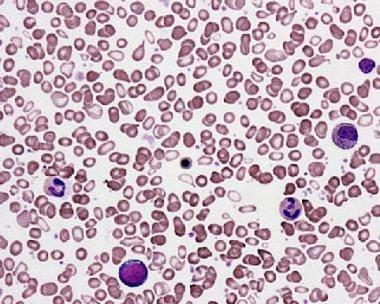
PM belongs to a group of blood cancers called myeloproliferative neoplasms. It is a chronic or slow-growing leukemia in which excessive scar tissue forms in the bone marrow (the soft, spongy tissue inside the bone), making it difficult to produce normal blood cells. This disease affects each person differently. There is no set treatment path for individuals with PM. Some medications may help with some of the symptoms, but currently, the only treatment with the potential to cure PM is a stem cell transplant. However, finding a matching donor is difficult, and the risks associated with the transplant are high.
Dr. Laferriere explained the basics of this disease to me and my wife, Harriet. One significant thing she pointed out was that there was at least a potential cure in a successful bone marrow/stem cell transplant. She also asked if I would like to be referred to Dr. Gupta, a worldrenowned expert in this disease, at Princess Margaret Cancer Centre (PMCC) in Toronto. I agreed without hesitation. We were also offered, and took advantage of, counselling at the Thunder Bay Regional HealthSciencesCentre.
When we got home, we immediately began searching for information on this disease to understand it as best we could. We needed to know what we were dealing with. Among the many sources of information available online, we found the Canadian Myeloproliferative Neoplasm ResearchFoundation(CMNPRF).Wearegladwedid.
During my first visit with Dr. Gupta, he and his team did an extensive background check. They inquired about my family history and asked me about my understanding of the disease, how I wascoping,andmy history of smoking.
They also provided more detailed information on my particular situation. They had the results of genetic testing and could tell me that I did not have the more common JAK2 mutation. I had the less common MPL mutation. At this visit, Dr. Gupta told us that this was a chronic leukemia that could progress slowly or can be aggressive. We discussed the risk factors of this disease, such as anemia, fever, high blood cell counts, leukemic cells, and the patient’s age. At this moment, only one of these was a factor for me (age over 65). He determined that my fibrosis was a grade 1 or 2 and that, at this time, I was classified as an ‘intermediate’ risk. Since I was not statistically likely to die within the next 5 years, bone marrow transplantation was not an option at this time. For now,await-and-watchapproachwaswarranted.










