
38 minute read
New Frontiers The Potential of AI in Medicine Today
The Potential of AI in Medicine Today
The use of artificial intelligence in healthcare has always been a hot topic, one debated for years due to its ethical, legal and social standpoints. However, while we look at artificial intelligence as a construct of the future, one would be surprised to realise how prevalent it is in the present day and how each individual has most probably engaged with at least one form of medical AI sometime in the past six months! However, don’t be fooled into thinking that we have embraced very much of it, AI holds an enormous amount of potential in the medical field and these possibilities can only unfold with time.
Advertisement
Before we start, let me explain the true nature of the AI I am referring to in this article, and how it is used in this field of practice. Medical AI fundamentally refers to the use of artificial intelligence technology in the healthcare system through automated processes. Essentially, it holds the potential to completely transform the practice of medicine by helping doctors more accurately treat patients, make more precise predictions about a patient's future health and additionally, recommend the most suitable and beneficial treatments through logical constructs. Moreover, it should be noted that studies have shown that an astonishing 50% of practices carried out by medical professionals have the potential to become automated with the use of AI - a rather frightening figure! The question will always be asked - why would we want to use technology instead of humans? And what are some examples of ways that we have already started doing so? Essentially, what issues might arise from these technological advancements in the world of medicine - is technology always better?
There are a myriad of duties that medical professionals face every single day, a large proportion under the umbrella term of ‘patient care. ’ This care consists of gathering data from consultations, processing this data and retrieving results to then generate a diagnosis for the patient by using other sources of data as a reference. Then comes determining the appropriate treatment method, preparing this treatment, monitoring the progress of the patient and finally, ensuring the patient is provided with the correct aftercare through appointments, etc. Yes, it is a lot of work that these healthcare professionals are faced with daily - all for one problem, one patient. A study in 2016 showed that physicians spend a lot more time on entering data and general desk work than actually engaging with their patients! Therefore, I think we’d all be relieved to know that the large majority of the above care has the potential to become automated using AI. Now, what benefits does this hold? Creating automated systems that can carry out these tasks without a human having to do so manually results in more efficient and faster task completion, freeing up a great deal of time for doctors, thus enabling them to focus on other things that cannot be automated.
There will always be certain tasks better done by humans, while others more efficiently done by computers by preventing human calculation errors, saving time, etc. By using AI for certain tasks, the medical system won’t just become more efficient but may also help us move towards more ‘precision medicine’ . If experts are able to find a good balance between the use of AI
and the skills of highly trained medical professionals - healthcare as a whole would benefit and be transformed even further into a highly innovative and successful system. At present, technology has already completely revolutionised the way in which we seek care. It may seem normal to us now, but in the UK most medical records are now digitised. We can schedule appointments online instead of calling in and we can even check into clinics using our own personal mobile phones - all quite modern concepts! Furthermore, programs like Germwatcher designed to detect, track and investigate infections in patients in hospitals, now exist and can help us gain knowledge that otherwise we might have trouble understanding. There exist decision support systems that use inputted symptoms and special algorithms to generate potential diagnoses. Furthermore, a more fascinating, and some might even say frightening, technology is the use of robotic surgical systems like the Da Vinci robot - equipped with robotic arms, precise movement and magnetised vision.
All of these forms of AI seem generally beneficial, so what could possibly go wrong? The relationships built between physicians, nurses and other clinicians with their patients assumes a system built on human care and interaction. However, nowadays electronic health records and data collection in computers seem to be getting the way of this. Doesn’t the idea of talking to a doctor while they type furiously into their computer, trying to keep up with what you are saying as they update your records, seem too familiar an image? Critics may argue that healthcare is slipping into an artificial state and becoming too impersonal. Additionally, the legal issues with sensitive personal data being stored on online databases does make people nervous. Some people do not trust that their data is being stored securely on computers, instead of manually recorded and kept in secure, physical filing systems.
While there are a few issues with the use of AI in the medical system, overall the benefits are astronomical and outweigh the negatives. Personally, I think we should all be excited for what the future holds in the healthcare sector. Furthermore, whilst many believe that doctors could risk being replaced, that will never be the case. We are heading towards evolution not extinction, and while the role of healthcare professionals will most certainly change and adapt, it will ultimately grow alongside technology and shape a brighter future for medicine as a whole.
Ovarian Cancer Detection by Dogs
Nadia Baghai LVI
References:
https://bjgp.org/content/68/668/143
https://healthitanalytics.com/news/arguing-t he-pros-and-cons-of-artificial-intelligence-inhealthcare
Dogs are known to have a highly evolved sense of smell, having up to 300 million olfactory (smell) receptors in their nose compared to just 6 million in humans. Studies have further shown
that their noses function differently to ours. We smell, inhale, and breathe through the same airways within our nose, whereas dogs have a fold of tissue just inside their nostrils that separates the air to perform two different functions: olfaction and respiration. 12% of inspired air diverts to a recessed area in the back of the nose (red), which is dedicated to olfaction.
The rest of the air (blue) continues past this area and performs the expected function and enters the lungs via the pharynx (black).
In addition, dog’s have a part of their brain that is devoted to analysing smells, which is 40 times greater than ours. As a result, their sense of smell is overall 10,000 to 100,000 times more acute.
Have dogs been successful in detecting ovarian cancer?
The short answer to this question is yes, and with high rates of success too. A dog’s incredibly strong sense of smell enables them to smell the cancer odour molecules emitted by cancer cells that have been taken from patients. This has led to numerous studies being set up, for example, a study in 2018 worked with dogs from Penn Vet Working Dog Centre, training them to detect malignant ovarian cancer using plasma samples from people at the Perelman School of Medicine. One German Shepherd, Osa, was presented with dishes of blood containing a benign sample, malignant sample, and normal samples, as well as other irrelevant samples to act as “distractors” . Whilst smelling these different samples, Osa suddenly froze and stared at one sample- she had correctly identified the cancer.
Similar research in 2013 has been carried out such as one that aimed to see how well trained dogs could accurately detect cancer odour in the blood of ovarian cancer patients. It also wanted to study whether their ability to detect this smell was affected by treatment to reduce the tumour burden, including surgery and five courses of chemotherapy. This study found that dogs showed high sensitivity (97%) and specificity (99%) in recognizing viable cancer cells thus concluding that canine detection gives a very good assessment of the prognosis of the study patients. However, their reliability did decrease with blood samples that had been through chemotherapy, which is most likely explained by the fact that reducing the number of cancer cells
also reduces the number of odour molecules, making the cancer harder to smell and detect.
How were dogs able to detect these malignant cancer cells?
Through investigating the chemistry of human body odours, it has been found that dogs detect changes in volatile organic compounds (VOC) in plasma. The VOC changes take place in the early stages of ovarian cancer and produce a specific odour.
A further step into these findings.
It is hoped that these ordourants can be collected and/or isolated and are able to be translated into a device and electronic system. The Nano/Bio Interface Centre is creating an electronic nose made of nanosensors that mimic the abilities of a canine nose, producing a tool that could be used in the future for use in ovarian cancer detection.
What is the significance of this research?
Currently, ovarian cancer is easy to treat in its early stages, however, extremely hard to detect due to the ovaries being located deep within the abdominal cavity so patients are unlikely to feel a tumour. At a later stage, when it is eventually easier to detect, it is much harder to treat with there thought to be around 4,200 ovarian cancer deaths in the UK each year (11 per day). Therefore, this research using canine detection could be life-saving as it has the ability to detect cancer reliably and easily at a much earlier stage than before. This should result in lower mortality rates in the treatment of ovarian cancer.
Anneliese Mayer LVI
References
https://www.pbs.org/wgbh/nova/article/dog s-sense-of-smell/
https://www.vet.upenn.edu/about/press-ro om/bellwether/bellwether-magazine/bellwe ther-fall-2018/sniffing-out-ovarian-cancer
https://www.ncbi.nlm.nih.gov/pmc/articles/ uPMC3765942/
https://www.healthline.com/health/cancer/ ovarian-cancer-early-signs#types
https://www.cancerresearchuk.org/health professional/cancer-statistics/statistics-by
Birth and Bacteria
In a world obsessed with hygiene and cleanliness, science and technology have provided us with cleaner alternatives for just about everything. But in the case of childbirth, maybe it wasn’t designed to be pristine.
When women give birth vaginally, their baby is exposed to a vast array of microflora and bacteria, not only during their passage through the birth canal, but also through contact with the mother’s skin and any faeces passed during the birth. While it may seem counterintuitive that evolution and natural selection has facilitated immediate contact with its mother’s excrement, it creates a microbiome of bacteria that helps the baby develop a strong immune system.
However, in the UK, it is estimated that 30% of infants are born via caesarean section, with almost half being elective. In recent years scientists have begun to investigate how different modes of delivery can affect a newborn’s immune system.
A 2011 study found that the mode of newborn delivery contributes not only to variation in the infant microbiome, but also the diversity of bacteria introduced. According to the study, vaginally delivered babies possessed similar microbiomes to the maternal vaginal and fecal flora. The babies’ gut bacteria consisted primarily of lactobacillus and within months showed a strong proportion of bifidobacterium, both of which are considered by biologists to be health promoting bacteria.
The study goes on to demonstrate that the microbiomic composition of caesarean born infants’ had lower distributions of bifidobacterium and alarmingly contained staphylococcus, which is potentially pathogenic. Their bacterial profile also had much higher levels of hospital bacteria, which in some cases made up 30% of their total microbiome.
Several studies have concluded that over time these differences largely disappear, to the extent that caesarean born and vaginally born infants’ microbiomes become indistinguishable by 9 months. However, it appears that by this point each birth type has already acquired certain predispositions.
Low diversity of bacterial microbes in the gut has been linked to an increased risk of several diseases including inflammatory bowel disease, asthma, coeliac disease and obesity. It can also have a lifelong effect on the body’s response to medicinal drugs, and can increase the propensity for allergies by a staggering 800%. Additionally, there is evidence from both human and rodent studies that highlights the key roles played by the gut microbiome in the development of brain functioning, cognition, anxiety and sociability.
In most cases the increased risk posed by these conditions is very minor and the cause may be hard to distinguish from other correlating factors. For instance, diversity of gut flora can be compromised as antibiotics are more frequently used to prevent infection in a caesarean birth. It is more likely (especially in emergency c sections) for caesarean born babies to be separated from their mothers for longer periods which reduces exposure to the maternal skin microbiome, potentially limiting the development of a robust and varied immune
system. When faced with the task of trying to replicate the bacterial exposure during natural births, one of the first methods researchers investigated was ‘vaginal seeding’ by which vaginal swabs from the mother were applied to the infant’s face. Clinical bodies quickly rejected this idea. Rather than just deeming it ineffective, it was concluded that this method was actually harmful.
However, trials later undertaken by Willem de Vos and Sture Andersson at the University of Helsinki may have unearthed a promising but unorthodox solution. Their infant group sample each received a dose of their mother’s gut bacteria, delivered via a highly diluted breast milk solution containing traces of carefully screened fecal microbiota from the mother. Amazingly, the cohort went on to develop a bacterial population that resembled that of a vaginally born infant, almost perfectly.
As modern medicine advances and along with it our ever-growing antiseptic capability and desire, it is almost ironic that the introduction of bacteria could be just what we’re looking for. Maybe in this case a little bit of dirt is exactly what we need.
Aimee Wong Rogers LVI
Sources 1.
2. https://www.ncbi.nlm.nih.gov/pmc/a rticles/PMC4681407/#:~:text=Infant s%20born%2 0vaginally%20have%20a,et%20al. %2C%202010).
https://www.newscientist.com/articl e/2216818-c-section-babies-have-a -different-micr obiome-but-not-for-long/
3. https://www.bbc.co.uk/news/health-4974 0735
4.https://digital.nhs.uk/data-and-inform ation/publications/statistical/mater nity-services monthly-statistics/january-2019#ke y-facts
5.https://www.nhs.uk/conditions/caesare an-section/risks/
6.https://pubmed.ncbi.nlm.nih.gov/3300 7265/
7.https://www.economist.com/science-a nd-technology/2020/10/17/how-to-ar m-caesare an-babies-with-the-gut-bacteria-they -need
Biomaterials: Changing the Face of Dentistry
Like in so many fields of science, technological advancements are the reason for improved efficiency and increased opportunities in treatment. Dentistry is no different, and this has brought exciting prospects of utilising biomaterials- a creative regenerative discovery.
Kangaroos, elephants, sharks and alligators- what do they all have in common? Their teeth! Not the shape or quantity, or ease of mutilating their prey, but the ability to regrow. These polyphyodonts are capable of replacing their teeth when tissue that supports them, known as the periodontium, is worn down. This leaves gaps (more scientifically referred to as diastemas) which permit the teeth growing behind the original as a result of their abundance of stem cells to be able to move forwards and take their place. This cycle can continue as there is room at the back for new teeth to grow and so their chewing, which is an imperative part of their digestive process, will never be compromised due to a lack of a full set of robust teeth.
Humans, on the other hand, do not possess this hugely advantageous traitwe are mere diphyodonts. We have just two successive sets of teeth: milk teeth (also known as deciduous teeth) and adult (or permanent) teeth. Though these have evolved to be much more durable so they can last our entire lives and our diet has changed resulting in less strain on our teeth through mechanical breaking down of our food, that is not to say they always do last for that long.
In the case of damaged or missing teeth, there are numerous restorative measures that can be taken: veneers and crowns for the former as well as prosthetics such as implants, dentures and bridges to treat edentulism (toothlessness). Although some provide a more long-term remedy, a permanent solution requiring no further maintenance or replacement is yet to be available. However, biomaterials may be the future of regenerative dentistry. These synthetic substances, alongside stem cells, have the potential to repair and stimulate the growth of pulp and surrounding dentin tissues that make up the central chamber of the tooth as well as the crown and root which form the main structure. Despite being inserted like a dental filling, biomaterials differ from the existing material used to fill cavities in their properties of being compatible with pulp tissue and non-toxic to cells. Using translational therapy, they can modify the behaviour of the stem cells as the cellular microenvironment is imitated to allow optimum conditions for differentiation and so development of these tissues to occur. This, effectively, enables an affected tooth to heal itself or regrow completely. This would prevent the need for extensive drilling to remove decay and insert a filling which is only a temporary solution and, if unsuccessful, would require a root canal causing further impairment of the tooth. Biomaterials offer a significantly more benign treatment plan with longer-lasting results that do not require additional management and support; this ultimately reduces the cost and time of the process.
Although stem cells have already shown huge potential in the field of science,
further research and trialling is needed before this treatment can be clinically approved. Testing on rats has been carried out but humans have yet to be involved in experimentation. However, this biological therapy brings exciting possibilities to restorative dentistry which is so essential in maintaining dental health. Therefore, it is crucial that creativity and innovation continues to grow and be such a prominent aspect of science to allow more incredible and revolutionary advancements in this branch of research.
Dahlia Levin UVI
https://www.ncbi.nlm.nih.gov/pmc/articles/P MC5370483/
https://www.sciencedirect.c
om/science/article/pii/B978
0081024768000013
https://dentistinodenton.co
m/animal-replacement-teet
h/
https://www.labroots.com/trending/plants-an
d-animals/14456/animals-regrow-teeth-hum
ans
https://link.springer.com/chapter/10.1007/97
8-3-319-14845-8 _ 8 https://www.ncbi.nlm.nih.gov/pmc/articles/P MC5126784/
Creativity and Science: How Andrew Pelling’s experimental lab is redefining the limits of medicine
Andrew Pelling is an award winning scientist who runs one of the most experimental labs in the world, based at the University of Ottawa. His goal is nothing short of ambitious: to build novel materials for next generation medical innovations and speculative living technologies of the future. In his lab, this involves making ears out of apples and regenerating spinal chords out of asparagus. Controversial, no?
Now, it might sound ridiculous and impossible, and many more ‘rational' scientists have dismissed his research because of its straight forward of concepts. Yet, sometimes we can solve the biggest problems with the simplest solutions. Maybe the answers have been in front of us the whole time- even as close to us as our kitchens. In the early 1800s, Hungarian physician Ignaz Semmelweis was shunned for his suggestion that a micro biome of microscopic harmful cells lived on our hands and skin, urging other surgeons to wash their hands regularly. For years scientists were certain that the Sun orbited the Earth. History is a reminder that we need to keep an open mind, at the end of the day there is technically no certain known ‘limit’ to the potential of science.
Andrew Pelling began to rethink how we use materials to reconstruct damaged or diseased human tissues. His lab stripped plants of their cells and DNA, leaving behind natural fibres that acted as scaffolds for human tissue. He talked about his love of finding broken machine parts and mixing them together to build something new- and his lab did just that.
They took an apple, removed all apple cells and DNA and implanted human cells into the cellular scaffolds which worked very similarly to our organs and tissues. The human cells divide by mitosis and fill the structure, and what fascinated him was when he observed that once implanted, the body treats it like its ownsending cells and blood supply that keeps it alive.
Encouraged by these findings, he asked his wife, a musical instrument carver, to carve human ears out of apples. By treating biology ‘like hardware’ , and using only soap and water, his lab offered an alternative to commercial scaffolds which scientists have been working on for decades which use proprietary products, animals or cadavers. He put his research into an online open research and started a company determined to develop kits so that in the future, we might be able to augment our bodies from our own kitchens.
His next revolutionary idea emerged when he was cutting asparagus in the kitchen, noticing the amazing vascular bundles which reminded him of one of the most spectacular tissues in our bodies- the spinal cord.
There is currently a global bioengineering effort aimed at treating spinal cord injuries as ½ a million a year suffer from pain or numbness to paralysis- a complete and utter loss of motor function.Most research has been using synthetic polymers, animal products or human caradures to solve this
problem.
Pelling’s Lab noticed the asparagus scaffold had microchannels which may guide regenerating neurons like those in our spinal cord. It moves and bends and has the same texture and flexibility as human tissue.
But humans aren’t plants, our cells haven’t evolved to grow on plant tissues and have no business in our spinal cord. At least according to many critics of his research. These guiding structures should disappear over time, but humans lack the enzymes to break these tissues down. However, this proved to be more beneficial than restraining- the inertness of plant tissue made it biocompatible as the body doesn’t detect or reject it, while at the same time cells which are regenerating can benefit from its shape and stability. He became wrapped in doubt - he felt like an outsider, did he have the right to work on such a complex problem? So he surrounded himself with wire neurosurgeons, clinicians, biochemists and bioengineers and began to start planning experiments.
In the experiment which was repeated several times he took a rat and anaesthetised it so they could sever its thoracic region slightly, enough to paralyse its lower body. They then implanted the scaffold between ends of severed spinal cords which acted like a bridge and he began to see that they recovered some mobility. No stem cells, electric stimulation, pharmaceuticals, exoskeletons or physical therapy had been used- and the rats were showing signs of a regenerating spinal cord. This was no easy experiment, it at times felt morally wrong to paralyse the rats, but the team was encouraged by constant positive results. They were still sceptical about them and repeated the experiment until his lab was nearly bankrupt- just to be certain that his findings were true.
This is the start of something extraordinary and they are just beginning to be translated into the clinic, the new technology was designated a breakthrough medical device by the FDA. Human clinical trials are set to begin in two years.
As scientists, we spend our lives living on a knife’s edge, ” he explained, “on the one hand, it’s our job to fundamentally broaden the horizon of human knowledge. But at the same time, we’re trained to doubt: to doubt our data, to doubt our experiments, to doubt our own conclusions. We spend our lives crushed under the weight of constant, unrelenting, never ending anxiety, uncertainty and self doubt. This is something I really struggle with. But I think almost every scientist can tell you about a time they ignored those doubts and did the experiments that would ‘never work’ , and the thing is, every now and then, one of those experiments works out. The challenge we face is that while doubt can be destructive to your mental health it's also the reason why scientific rigour is such a potent tool for discovery. It forces us to ask the difficult questions and repeat experiments, nothing about that is easy. Often it becomes our responsibility to bear the burden of the hard and sometimes heart wrenching experiments. This ultimately leads to the creation of new knowledge, and in some really rare cases
the type of innovation that just might change a person’s life. ” Andrew Pelling’s work has made many scientists reflect on the role of creativity in science as well as bravery it requires to suggest what has never been suggested before. It can be daunting, but thanks to the risk he took humans now have the potential to design the architecture of plant tissues in such a way that they can encourage cell growth, meeting unmet medical needs we face now or in the future.
References:
Ted talks:
https://www.ted.com/talks/andrew _pelling_ t his _ scientist _ makes _ ears _ out _ of _ apples?l angua ge=en
https://www.google.co.uk/url?sa=t&rct=j&q= &esrc=s&source=web&cd=&ved=2ahUKEwj klNS y5JbvAhULHxoKHXh9DeUQtwIwAXoECAU QAw&url=https%3A%2F%2Fwww.ted.com %2Ft alks%2Fandrew _pelling_ could _ we _ treat _ sp inal _ cord _ injuries _ with _ asparagus%2Ftrans cript %3Flanguage%3Den&usg=AOvVaw3MfHlb 3jYvwwr83obk9SLt
Pelling’s Lab website:
https://www.pellinglab.net
Chiara Champeaux Year 11
Obesity: Is it all to do with overconsumption?
Obesity is currently associated with the leading causes of death worldwide including diabetes, ischaemic heart disease and cancer, with at least 2.8 million people dying each year a result of being overweight or obese. It has reached epidemic proportions globally - an increasingly concerning problem for not only high income but also low income country governments to mitigate as food becomes further accessible to citizens. By 2030, more than 2.16 billion individuals are expected to be overweight.
Overweight and obesity are defined as abnormal or excessive fat accumulation that presents a risk to health and is prevalent in environments which promote physical inactivity and mass consumption of high calorie foods. However, not all people living in such environments will become obese, nor will all obese people have the same body fat distribution or suffer the same health problems. The link between obesity and genetics is still somewhat debated, the most widely accepted cause of obesity lying in environmental factors. Although genetic changes in humans occur too slowly to be the prime factor in the obesity crisis, the imbalances in how people respond to the same environment implies that genes do in fact play a role in the occurrence of obesity. Other factors that influence the heritability of obesity include epigenetic marks.
Genes code for specific proteins to be made within cells in response to changes in our environment. Studies of resemblances and differences among family members and twins have shed light on evidence that explains the large quantity of the differences in weight among adults. Additional research between obese and non obese people have pinpointed variants in several genes that potentially contribute to obesity by increasing hunger and food intake. In most cases obesity probably results from interaction between a multitude of genes, more than 50 different genes, and environmental factors (multifactorial obesity). Very rarely does obesity occur in families in line with one clear inheritance pattern as a result of changes in a one single gene (monogenic obesity).
But how do genes influence obesity? The brain controls food intake by reacting to signals transmitted from adipose tissue (fat), the pancreas and the digestive tract. These signals are carried by hormones such as insulin (regulates blood glucose concentration) and leptin (controls appetite). The brain then coordinates these signals and responds to the instructions of the body - to eat more and reduce energy or the opposite. Genes are the basis for the signals and responses that control food intake and small changes in these genes can affect their activity. Genes that have been linked to obesity include:
A) FTO GENE - this a protein found on chromosome 16. The presence of this gene has a direct influence on obesity as it promotes food intake; those with this gene have a 30% higher chance of being overweight.
B) MC4R GENE ( melanocortin-4 receptor) - contributes to metabolism. This gene regulates the quantities of energy we use from what we eat and stimulates our appetite. Those with a variant of this gene are likely to be overweight.
C) ADIPOQ GENE - mutations of this gene are associated with adiponectin deficiency which can lead to obesity and insulin resistance (diabetes).
One possible hypothesis to our current obesity epidemic is the prevalence of “energy-thrifty genes” . Energy is vital for survival and human energy regulation is directed towards protecting and preventing weight loss rather than controlling weight gain. The tendency of humans to store energy in the form of fat is more beneficial than storing it in another form as they can hold more energy and are hydrolysed much slower. The storage of energy as fat is hypothesised to result from thousands of years of evolution in environments with limited food supplies. This is where the “energy thrifty gene” comes in. These genes would have helped our ancestors survive famines to much better extent than those who did not have the “thrifty genotype” by storing the energy from food much more efficiently and in greater quantities as fat. These genes are now being challenged by our current environment where food is plentiful and easily accessible all year round.
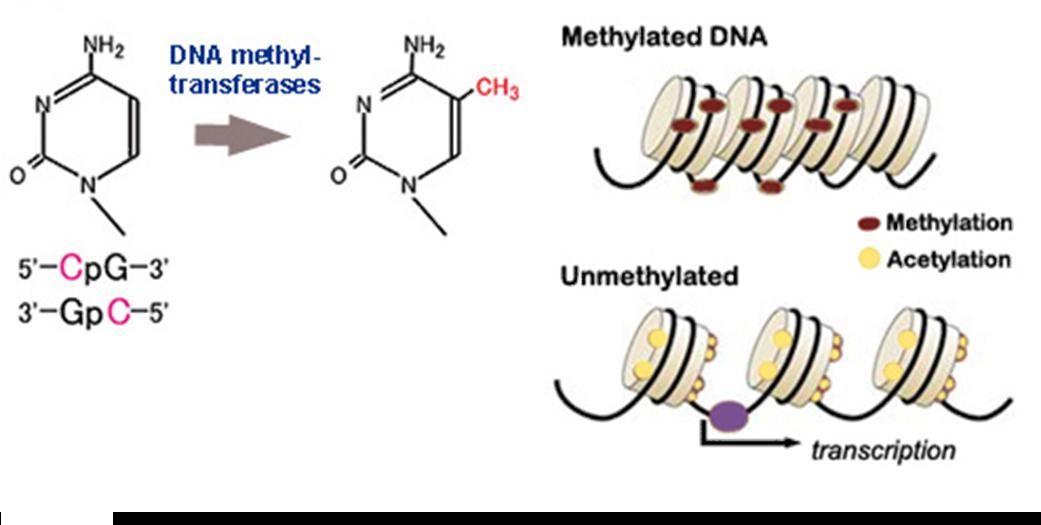
Another proposed hypothesis includes epigenetics. Epigenetic marks or “imprinting” affect gene expression without actually changing the DNA sequence. Changes or failures in imprinting can not only cause extreme forms of obesity but also are associated with human’s susceptibility to obesity. Epigenetic marks are affected by changes in surrounding environments during critical development periods e.g growth of a foetus and are caused by DNA methylation and histone modifications which regulate the imprinting. As many imprinted genes are growth factors, disorders within imprinting often lead to obesity. As well as growth, imprinted genes are involved in differentiation, development and metabolic functions.
Imprinting is regulated by DNA methylation which arises through the addition of a methyl (CH3) group to a cytosine nucleotide. Methylation causes the silencing of gene expression which stops genes from being transcribed during protein synthesis. These methylation patterns can be passed down to children. Histone modifications also control imprinting where the DNA in cells can be packaged as heterochromatin which is tightly stored. This will prevent gene expression as the DNA base sequences are inaccessible to transcription factors. To bring this into perspective, if a mother were to be malnourished during the first half of pregnancy, the child would be more likely to be obese due to inherited epigentic marks from mother to store any food received as fat.
To conclude, it is probable to say that both genetic and environmental effects on epigenetics will in turn be associated with obesity. Clara Gilardi LVI
Current Affairs
Should Vaccines Be Compulsory?
Vaccines are essential in reducing the number of deaths caused by infectious diseases, and are the solution to the current global pandemic. Some of the world’s most major health concerns have been dramatically reduced, almost to the point of eradication, by vaccinations, such as smallpox, polio and measles. However, ever since vaccinations were developed by Edward Jenner in 1796, they have been subject to various ethical debates, the most prevalent being whether vaccinations be a personal choice.
Since the outbreak of smallpox in the early 19th century, vaccination mandates have been established, especially for children, to ensure herd immunity is achieved. Herd (or population) immunity is reached when the majority of the population is vaccinated, which provides indirect protection to individuals who are not vaccinated. With the potential to prevent 6 million deaths worldwide each year, vaccinations are a crucial means of ensuring infectious diseases are prevented from spreading rapidly in populations. In the UK, parents have the choice whether to vaccinate their children, but should vaccinations be made compulsory?
How do vaccines work?
There are various different types of vaccines, however the principle remains the same. Vaccines capitalise on the adaptive immune system, which when exposed to an infection, can respond much more quickly and effectively when exposed to the same pathogen again. By allowing the immune system to recognise something as a threat by mimicking an infection, and safely allowing the immune system to respond, the immune system can then kill the pathogen extremely quickly when exposed to it again. T-lymphocytes are a type of white blood cell which attack pathogens in the body. After the vaccine imitates an infection, the body retains a few T-lymphocytes, called memory cells, which, if exposed to the same pathogen, can kill the cells more quickly and effectively. B-lymphocytes are another type of white blood cell which are responsible for producing antibodies which attack the pathogens. Vaccines are specifically designed to develop immunity by imitating an infection, without causing an illness.
There are five main types of vaccines: live, attenuated vaccines, inactivated vaccines, toxoid vaccines, subunit vaccines, and conjugate vaccines. However, over the last few years, mRNA vaccines have been at the forefront of medical research. The Pfizer-BioNTech vaccine uses this technology, which has been used to vaccinate millions of people in the UK over the last few months. These vaccines work by injecting the nucleic code (mRNA) for the spike protein of SARS-CoV-2 which is contained in a lipid nanoparticle. The nucleic code is incorporated into our cells, which will then begin to produce the spike protein. The body can then recognise this protein as foreign, so amounts an immune response, similarly to the other types of vaccines.

Why are vaccines not compulsory?
By harnessing the power of the immune system, vaccines are able to save millions of lives every year, however some people refuse to be vaccinated, despite the overwhelming evidence about the safety and efficacy of vaccines. These people are commonly referred to as “anti-vaxxers” , and have dramatically risen in prominence since Andrew Wakefield published false claims about the MMR vaccine leading to autism. The World Health Organisation views vaccine hesitancy as one of the top ten global threats, which can be seen when in 2016 there were more than 500 cases of measles reported in England, which was more than five times the number of cases reported in 1996. Another group of people who oppose vaccinations are certain religious groups. For example, some Christians argue that if God has decided that someone will die from smallpox, it would be a sin to stop God’s will by vaccination. Some people are also medically unable to have vaccinations due to compromised immune systems, or allergic reactions in response to certain vaccines. These three groups of people will make it very difficult for vaccines to ever be compulsory, as there will always be people who either strongly oppose vaccinations, or physically cannot be vaccinated due to the health risks.
Should vaccines be compulsory?
Although vaccines provide the solution to infectious disease which can quickly spread across the world, it is not right to impose compulsory vaccinations on a population, as not only will it be very difficult to enforce, but people should be given the choice due to religious or medical reasons. Instead of enforcing vaccinations, the problem of vaccine hesitancy should be solved by educating people on the safety, efficacy and abundant benefits of vaccines, whilst highly recommending that everyone who is offered a vaccine should take this opportunity.

Jess Gilbert LVI6
References
https://www.bbc.com/news/world-48186856 https://www.cdc.gov/vaccines/hcp/conversations/dow nloads/vacsafe-understand-color-office.pdf\\ https://en.wikipedia.org/wiki/Vaccine_hesitancy#Religi onhttps://www.genengnews.com/insights/mrna-addre ssing-the-blind-spot-of-enzyme-replacement-therapy/ https://www.theguardian.com/world/2020/dec/02/howdoes-the-pfizerbiontech-covid-vaccine-work-and-whowill-get-it https://www.bbc.co.uk/news/world-481868
Implications of COVID-19 on the lungs
The coronavirus. A chaotic pandemic that has dominated our lives for nearly a year now. It has been established that COVID-19 is a respiratory disease, and can cause a range of breathing problems- from mild to extremely severe- but as we approach the anniversary of lockdown in the UK, what exactly does this virus do to potentially devastate such a vital organ? How does it even get inside our system? And what makes this disease so spreadable?
The coronavirus enters the body through the nose or mouth via a receptor called ACE2, which is important for controlling blood pressure and electrolyte levels and it is also found in the lungs, the back of the throat, tongue and nose. Researchers have also found a supply of protease in the nose, which chemically removes the top section of the coronavirus spike, allowing it into nasal cells. Because of this splitting off, COVID-19 can bind 10 times more tightly to insert its RNA into the cell, which can explain why the virus spreads so easily around the body. In fact, the viral content in the upper respiratory tract has been found to be at its highest at day one, suggesting that its peak preceded any symptoms and highlights how the virus can be transmitted without the onset of symptoms.
Inside the lung, the ACE2 receptor sits on top of lung cells and are essential for producing surfactant- a compound that coats the alveoli, and plays an important role in gas exchange. Reduced surfactant from the viral destruction of lung cells means it is harder to keep the alveoli open. White blood cells are sent here as an immune response, however blood vessels around these air sacs become leak fluid in response to inflammatory chemicals that the white blood cells release, which puts pressure on the alveoli from outside and, in combination with the lack of surfactant, causes them to collapse, leading to pneumonia and difficulty breathing. While most people fully recover from pneumonia, lung injury associated with COVID-19 may result in long-term breathing problems. More severe inflammation can lead to acute respiratory distress syndrome (ARDS), where patients require a ventilator. Some people also react to the virus’ presence by producing an intense immune response- a cytokine storm. The body replaces damaged cells with scar tissue and potentially leads to pulmonary fibrosis, making people breathless and patients may have long-term pulmonary scarring. What factors increase lung damage? By now it is obvious that age, smoking, and other underlying health conditions play an immense role in the risk of severe infection and how likely a person is to recover. Inhalation of cigarette smoke irritates the lungs, unleashing the immune system to fight said irritation. Adding on a coronavirus infection with that further amplifies the
symptom response, putting smokers at risk
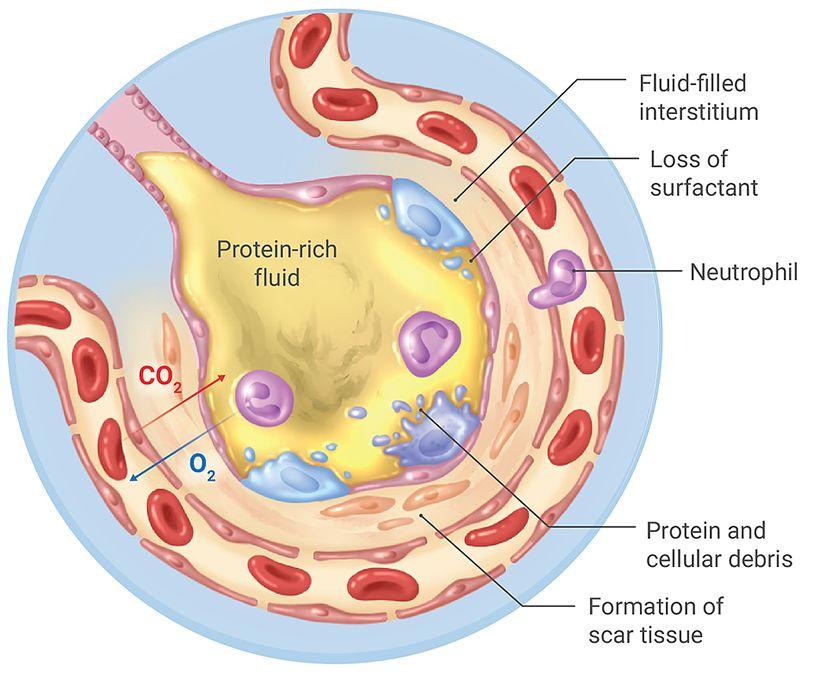
of a more severe case. Older people may have less elastic lung tissues and a weakened immune system that occurs with advanced age. Also, timely support and proper care of patients can massively minimise the long term effects. Lastly, disease severity. This could be down to pure luck whether the person has a mild or a severe case. Milder cases are far less likely to cause lasting scars in the lung tissue. Over time, the tissue will naturally heal, but it can take up to a year for a person’s lung function to return to pre-covid levels and respiratory therapists will be very much needed to help COVID-19 survivors. Unfortunately the virus doesn’t only impact the lungs, researchers and doctors have found there to be other effects on the brain, kidney and liver, to name a few. Even with the development of a vaccine, there is still so much left to discover about this virus
Tabitha Iliffe LVI
References and further reading:
https://www.medicalnewstoday.com/articles/ covid-19-what-happens-inside-the-body#Ph ase4:-Acute-respiratory-distress-syndrome,thecytokine-storm, -and-multiple-organ-failure https://theconversation.com/coronavirus-can -cause-lasting-lung-damage-but-the-effectsmay -ease-over-time-140398 https://www.hopkinsmedicine.org/health/con ditions-and-diseases/coronavirus/what-coro navir us-does-to-the-lungs
https://www.weforum.org/agenda/2020/04/th is-graphic-shows-what-covid-19-does-to-yo ur-b ody/
The Importance of Vaccines in Healthcare
Smallpox, tetanus, diphtheria, meningitis and polio to name but a few are prime examples of the pivotal role vaccinations play in combating the most dangerous diseases not only in childhood, but also in major epidemics and pandemics, like Ebola and, most recently, COVID-19. While vaccines remain “the most effective tool for preventing infectious diseases and improving global health” and are “relevant to people of all ages and in all countries”’ as mentioned in the Vaccine Innovation article within the New England Journal of Medicine in which Professor Chris Witty illustrates how “celebrating vaccines is really celebrating the power of our immune system” . With further research, we are able to see that vaccines do not actively kill or defeat the virus, but instead we do.
I think it is important to begin with analysing why vaccines are actually necessary. While the human anatomy consists of physical barriers such as that of the skin, mucous membranes and expulsive reflexes such as that of coughs and sneezes, we also have the nonspecific immune system. While the non-specific immune response, which includes processes such as phagocytosis, is highly effective, it provides the body with no “memory” of the pathogen and is therefore not what the vaccine seeks to initiate.
Instead, vaccines stimulate the specific or acquired immune system. Acquired immunity is dependent on the specialized white blood cells known as lymphocytes. Lymphocytes originate from stem cells in the bone marrow and divide continuously to release immature lymphocytes into the bloodstream. Some of these travel to the thymus to differentiate into T cells, while others remain in the bone marrow- these are called B cells. Both T and B cells recognize and help eliminate foreign pathogens (with antigens), but do so in very different ways and are essential to the vaccination process. Antigen presenting cells, produced in the non-specific defence system, present the foreign antigen (vaccine antigen) to T Helper cells. The receptors on the T helper cells fit the antigens and become activated to produce interleukins, stimulating T cells to divide rapidly via mitosis, forming clones of activated T cells. These are able to develop into killer T cells which are specific to the presented antigen and destroy infected cells. These interleukins, produced by T cells, are also able to activate B cells which produce specific antibodies to fit the antigens on the surface of the pathogen (acting as opsonins or agglutinins). Some of these B cells, however, develop into memory cells which would be able to wipe out the pathogen rapidly should it ever return. This is known as the secondary immune response.
But, what is the importance of this timeline in vaccination? Well, it allows us to understand why some vaccines require a second or third dose to maintain protection. While the primary vaccination can be likened to a “first infection” , there is a “lag phase” after which B cells and T cells initiate their immune response. The response to the second vaccine, however, is like a “second infection” and is therefore faster. This vaccination schedule leads to longer lasting and more powerful immune responses.
However, in order to appreciate the complexity and application of this immense science, it is vital to look at that of the arguably most notable immunization-related accomplishment- the eradication of smallpox, which was verified by the World Health Organisation in 1980. Edward Jenner, a country doctor (roughly equivalent to a GP) made the intelligent observation that dairymaids, who had cowpox, did not get smallpox. Perhaps this is more clearly highlighted in Jenner’s own small experiment. When Jenner inoculated a small sample of cowpox from Sarah Nelms, who was infected, and transferred it into James Phipps (an eight year old) he showed mild symptoms of the disease and then proceeded to recover. However, when he was soon after infected with smallpox, he showed no symptoms at all. What Jenner took from this was that a milder disease provided immunity to a more severe one. But, Jenners observations did not stop there. He also noticed that in history, and with the smallpox vaccine, that vaccine protection often diminished as time went on.
This knowledge is still extremely relevant today. While vaccines can prevent infection, they are also able to prevent the significance of the disease should someone become infected with the disease. With this, they essentially reduce the severity of the disease and prevent mortality rates worldwide. This knowledge is extremely relevant to the current COVID-19 pandemic and its vaccine- perhaps a revaccination might be necessary?
This contributes greatly to the deployment of a vaccine. For this, there are several “main” strategies. The first was used effectively in smallpox and Ebola outbreaks. For this, a rapid vaccine is used and is initiated by identifying extreme cases and vaccinating their close contacts, and the contacts of the contacts essentially forming a “ring” and the technique is thus titled “ring vaccination” . While this has been proved successful, it is not applicable to the current pandemic as often symptoms are minimal or not present at all. The second, however, might be more relevant. This technique begins by identifying those at high risk of dying, catching and spreading the virus and vaccinating these individuals. These include the elderly, the immunosuppressed or front line workers.
However, it would be inappropriate not to mention how vaccines are dependent on the trust and efficiency of the products themselves. In addition, in the administers and scientists. Failure or mistakes in the vaccination would have “substantial long term public health consequences” according, again, to Vaccination Innovation.
This pattern can be easily seen also from Andrew Wakefield and his colleagues’ now discredited study. Since the 1970s there has been skepticism on the safety of vaccines e.g. against pertussis or whooping cough, however the retracted paper in The Lancet is arguably the most famous. The paper that was built on the work of 12 children promoted the non-existent connection between the MMR vaccine and Autism. This catalysed the anti-vaccine movement for those who are afraid of complications related to the vaccine. With this, people fear their DNA may be altered to produce cancer. To overcome this, education efforts have been put in place and public health experts have focused on
the benefits of mass vaccination to the general population.
In conclusion, incredible progress has been made since Jenner’s smallpox vaccine discovery including the control of childhood diseases (such as measles, mumps, rubella and polio). These scientific breakthroughs have led to the rapid expansion of knowledge of the complex immune system at a molecular level and has allowed for the COVID-19 vaccine to be developed at the fastest rate in history. With this, it can be clearly seen the huge possibility for discovery in controlling pathogens and providing effective vaccines to the pathogens of all nature including cancers. Chris Witty explains that there is “good theoretical reason for thinking that we could use vaccines to help prevent or treat cancers” which is an interesting area for future research.
Nicole Monaghan LVI
References:
https://www.ncbi.nlm.nih.gov/pmc/articles/P MC1200696/
https://www.nejm.org/doi/10.1056/NEJMp20 29466
https://www.gresham.ac.uk/lectures-and-ev ents/vaccination

