Genomic Press
Where Breakthrough Science Meets Clinical Impac t
At Genomic Press, we advance the frontiers of neuroscience and psychiatry:
• Multidisciplinary Scope: From molecul ar mechanisms to clinical applications
• Varied Research Welcome: We publish genomic and non-genomic papers
• Exper t Editorial Boards: Led by distinguished researchers
• Rapid Publication: Streamlined review process without sacri cing quality
• Global Visibility: Reaching researchers and clinicians worldwide
Recent publications cover topics such as the economic and public health implications of psychedelic therapies, the e ects of ayahuasca on fear and anxiety, psychedelic treatment for anorexia nervosa and body dysmorphic disorder, and advancements, challenges, and future directions for treating resistant depression with psilocybin-assisted psychotherapy.
EDITORIAL
Countingtheuncountable:Thecriticalquesttoquantifypsychedelicmedicine’sreach
©TheAuthor(s),2025.ThisarticleisunderexclusiveandpermanentlicensetoGenomicPress
Psychedelics March2025;1(2):1–2;doi: https://doi.org/10.61373/pp025d.0005
Inthissecondissueof Psychedelics (1),wefeatureonourcover thethought-provokingstudybyRab,Raison&Marseille(2).Thatpaperpresentsthefirstrigorousestimateofthepotentialdemandfor psilocybin-assistedtherapy(PSIL-AT)intheUnitedStates.Aspsychedelic medicinemovesfromtheperipheryofpsychiatricresearchtowardthe possibility,andnowthereality,ofapprovalbynationaldrugregulatory agencies,1 thisanalysiscouldnotbemoretimely(3, 4).Understandingthe sizeofthepotentialpatientpopulationeligibleforPSIL-ATinformspharmaceuticaldevelopmentandthebroaderhealthcareecosystem,preparingtoaccommodatethisemergingclassoftherapy.
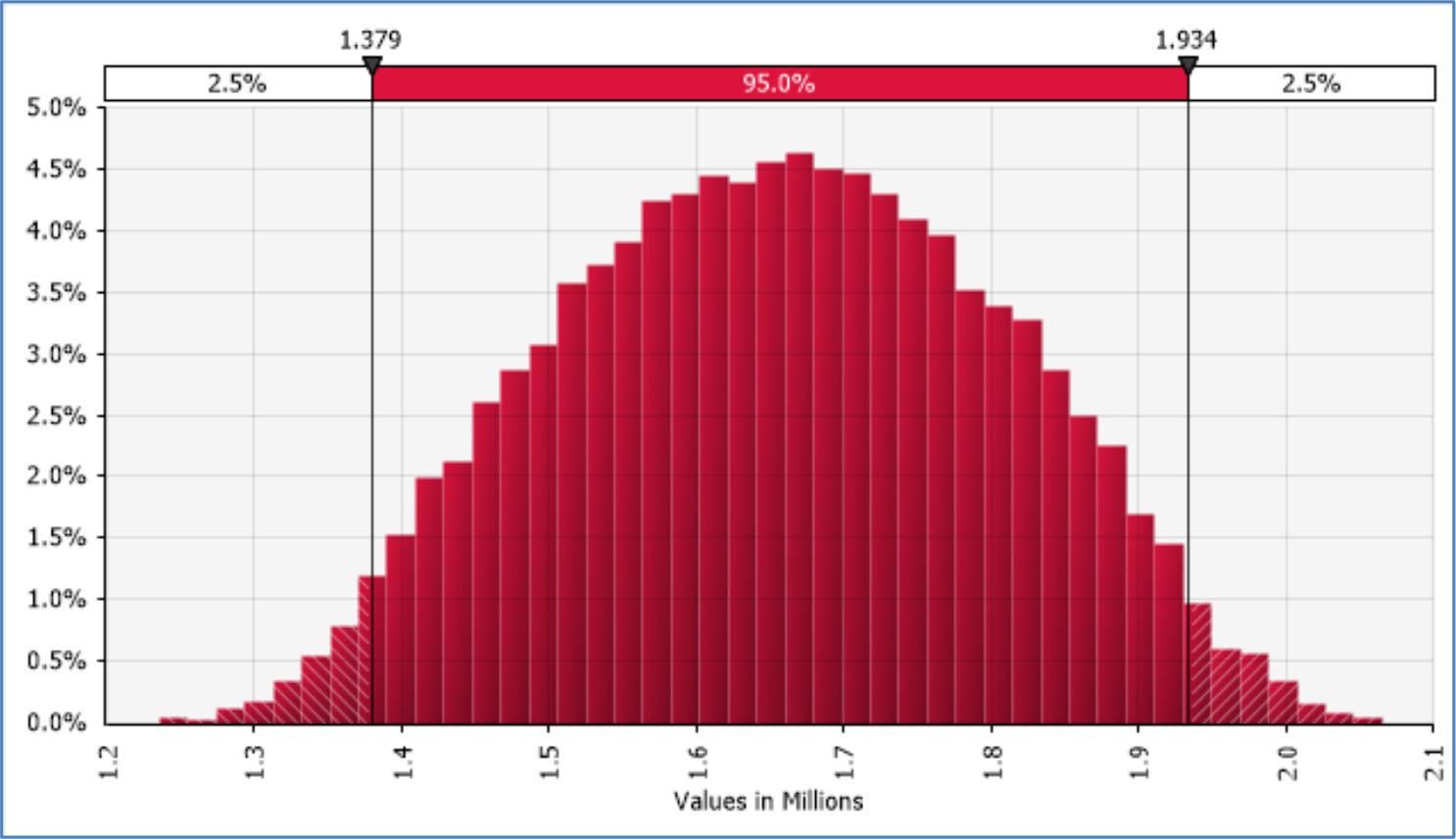
Byestablishingarangeofestimates,theauthorsbringwelcomenuancetotheirmethodology,steeringclearofhyperboleandunduepessimism.Theyavoidoverlybroadassumptionsthatwouldbeimpossible tomeetandexclusioncriteriasoimplausiblynarrowtheyareunlikelyto occurinactualclinicalpopulations.Theirapproachprovidesacredible frameworkforestimatingincidenceinarelativelynarrowyetclinically relevantsetting.Rabandcolleagues’finding—thatbetween24%(using stringentcriteria)and62%(afteradjustmentforcomorbidities)ofindividualswithmajordepressivedisorder(MDD)ortreatment-resistantdepression(TRD)maybeeligibleforPSIL-AT—offersacrucialstartingpoint forhealthcareplanning,onethathasbeensorelyneeded(2).
Thisstudyadvancestheconversationonpsychedelicmedicineinseveralways.First,itacknowledgesthatnoteveryindividualwithadepressiondiagnosisisautomaticallyacandidateforPSIL-AT,pushingback againstoverlyenthusiasticclaimsofpsychedelicsasuniversalremedies. Second,itillustrateshowexclusioncriteriacanactasbarrierstoaccess, highlightingthatdecisionsaboutwhoreceivestreatmentarenotmerely clinical—theyarepublichealthdecisions.Third,itdrawsaclearlinebetweentheoreticalbenefitandpracticalimplementation:thepotentialof atreatmentcannotbeseparatedfromthereal-worldconstraintsonits delivery.
Rabetal.identifyalcoholandsubstanceusedisordersaskeyfactorslimitingeligibilityinclinicaltrials.Theiranalysisisparticularly sharponthispoint.Byshowingthatremovingtheseexclusioncriteriawouldsignificantlyexpandtheeligiblepopulation,theyraiseacriticalquestion:Shouldtheseconditionsautomaticallydisqualifypatients— especiallygivenemergingevidencethatpsychedelicsmayhelpthosewith substanceusedisorders?
Whilemethodologicallystrong,thestudydoeshavelimitationsworth noting.TheassumptionthatdemandwillariseprimarilyfromthosealreadyreceivingcaremayunderrepresentbroaderinterestoncePSIL-AT becomeswidelyaccessible.Additionally,theanalysistreatsexclusioncriteriaasbinary—presentorabsent—whereas,inclinicalpractice,theseare oftensubjecttomorenuancedjudgment.
Theauthorsarecarefultoemphasizethattheyareestimatingpotentialdemand.Butbetweenpotentialandaccessliesacomplexlandscape:
1 TheAustralianTherapeuticGoodsAdministration(TGA)approvedtheuseofpsilocybinfortreatment-resistantdepressionandMDMAforPTSD,effectiveon1July 2023.
Received:7April2025.Accepted:9April2025. Publishedonline:15April2025.
insurancecoverage,providertraining,geography,andculturalattitudes. AsOregonandColoradoleadthewaywithstate-levelframeworksfor psilocybintherapy(5),theseestimatesarenolongerjuststatistics.They areplanningtools,policytriggers,andmoralsignposts.
OregonbecamethefirstU.S.statetolegalizepsilocybinfortherapeuticusethroughMeasure109,whichwaspassedinNovember2020. Thelawestablishedaregulatedsystemforpsilocybinservices,includinglicensedservicecenterswhereindividualsaged21andoldercan accesspsilocybinunderthesupervisionoftrainedfacilitators.Colorado followedin2022bypassingProposition122,whichdecriminalizedthe personaluse,cultivation,possession,andsharingofpsilocybinmushroomsforadults21andover.Italsolegalizedpsilocybin-assistedtherapiesatlicensedhealingcenters.
Yet,historyoffersacautionarynoteasthefieldedgestowardmainstreamlegitimacy.Newtherapies—especiallythoseimbuedwiththeallureofinnovation—tendtoreachtheprivilegedfirst.Inequitiesarenot incidental;theyaresystemic.Equitymustbeengineered,notmerely hopedfor.FutureresearchmustexplorewhoqualifiesforPSIL-ATandwho receivesit.
Thereareurgentnextsteps.Longitudinaltrackingofreal-worldimplementationinOregonandColoradocanhelpvalidateorrefinethese projections.Cost-effectivenessanalysesstratifiedbypatientsubgroups cansupportrationalpolicyandreimbursementdecisions.Clinicaltrials mustevolvetoincludepopulationshistoricallyexcluded—notrecklessly, butwithcarefuloversight—sothat“evidence-based”doesnotbecomea euphemismforexclusion.
Rabetal.havedonemorethanquantifypotentialdemand.Theyhave mappedoutaterrainthatpsychiatrymustnownavigate—notonlywith databutwithconscience.Aswefaceanepidemicofdepressionandacrisisinpsychiatricinnovation,wecannotaffordtomiscalculateeitherour reachorourresolve.
What’satstakeisnotmerelyregulatoryapprovalbutareimagining ofwhatpsychiatriccarecouldbecome—wheninformedbyinnovativescience,shapedbysociety,andgovernedbyethics.
1
Editor-in-Chief,
References
JulioLicinio1
Psychedelics,GenomicPress,NewYork,NewYork10036,USA e-mail: julio.licinio@genomicpress.com
1.LicinioJ.Psychedelics:TheJournalofPsychedelicPharmacology–Chartinganewcourse inpsychedelicscience.Psychedelics.2024:1–2.DOI: 10.61373/pp024d.0007
2.RabSF,RaisonCL,MarseilleE.Anestimateofthenumberofpeoplewithclinicaldepressioneligibleforpsilocybin-assistedtherapyintheUnitedStates.Psychedelics.2024: 1–5.DOI: 10.61373/pp024r.0025
3.NogradyB.Australia’sapprovalofMDMAandpsilocybinforPTSDanddepressionispremature,saycritics.BMJ.2023;382:1599.DOI: 10.1136/bmj.p1599.PMID:37433614
4.NuttDJ,HuntP,SchlagAK,FitzgeraldP.TheAustraliastory:currentstatusandfuturechallengesfortheclinicalapplicationsofpsychedelics.BrJPharmacol.2024.DOI: 10.1111/bph.17398.PMID:39701143
5.XenakisSN,ShannonSM.Whatisneededfortheroll-outofpsychedelictreatments? CurrOpinPsychiatry.2024;37(4):277–81.DOI: 10.1097/YCO.0000000000000946 PMID:38726805
Publisher’snote: GenomicPressmaintainsapositionofimpartialityandneutralityregardingterritorialassertionsrepresentedinpublishedmaterialsandaffiliationsofinstitutionalnature.Assuch,wewillusetheaffiliationsprovidedbytheauthors,withouteditingthem.Suchusesimplyreflectswhattheauthorssubmitted tousanditdoesnotindicatethatGenomicPresssupportsanytypeofterritorial assertions.
OpenAccess. ThisarticleislicensedtoGenomicPressundertheCreativeCommonsAttribution-NonCommercial-NoDerivatives4.0InternationalLicense(CCBY-NC-ND4.0).Thelicensemandates:(1)Attribution:Credit mustbegiventotheoriginalwork,withalinktothelicenseandnotification ofanychanges.Theacknowledgmentshouldnotimplylicensorendorsement.
(2)NonCommercial:Thematerialcannotbeusedforcommercialpurposes.(3) NoDerivatives:Modifiedversionsoftheworkcannotbedistributed.(4)Noadditional legalortechnologicalrestrictionsmaybeappliedbeyondthosestipulatedinthe license.Publicdomainmaterialsorthosecoveredbystatutoryexceptionsareexemptfromtheseterms.Thislicensedoesnotcoverallpotentialrights,suchas publicityorprivacyrights,whichmayrestrictmaterialuse.Third-partycontent inthisarticlefallsunderthearticle’sCreativeCommonslicenseunlessotherwise stated.Ifuseexceedsthelicensescopeorstatutoryregulation,permissionmust beobtainedfromthecopyrightholder.Forcompletelicensedetails,visit https:// creativecommons.org/licenses/by-nc-nd/4.0/.Thelicenseisprovidedwithout warranties.
Psychedelics
INNOVATORS&IDEAS:RISINGSTAR
AlainaM.Jaster:Bridgingthegapacrosspreclinicalandclinicaldisciplinesinthe psychedelicsciences
©GenomicPress,2024.The“GenomicPressInterview”frameworkisprotectedundercopyright.Individualresponsesarepublishedunderexclusive andpermanentlicensetoGenomicPress.
Psychedelics March2025;1(2):3–5;doi: https://doi.org/10.61373/pp024k.0043
Keywords: Psychedelics,serotonin2Areceptor,neuroplasticity, biomarkers,depression,substanceusedisorder,pharmacology, endocannabinoids,fearextinction,endocannabinoids,adolescence
Dr.AlainaM.JasterisapostdoctoralscholarintheDepartmentof PsychiatryandBehavioralNeurosciencesatWayneStateUniversity. Shecurrentlyservesonthetraineeeditorialboardof Psychedelic Medicine,thejournalfortheInternationalSocietyforResearchon Psychedelics(ISRP),andispartoftheSociety’sDiversityEquity InclusionandAccessibilitycommittee.Jasterisalsopartofthe SciencePolicyCommitteeofStudentsforSensibleDrugPolicy(SSDP) andco-foundedascientificcommunicationwebsiteandpodcast, PsychedelicBrainScience. Herresearchaimstounderstandthe underlyingmoleculartargetsandmechanismsofneuropsychiatric disordersandsubstanceusedisorders.HerPhDdissertationfocused ontheserotonin2Areceptor’smodulatoryroleinrewardingaspects ofopioidsandneuroplasticityacrosssexes.Mostofherworkuses translationalmethodologyrelatedtoPavlovianconditioning combinedwithtechniquestomeasureandmanipulate pharmacologicalfactorsinvolvedinthesediseases.Hercurrentwork focusesontheinvolvementofendocannabinoidsinfearextinction, biomarkersoffamilialriskofdepression,andpsychedelicuseamong adolescentpopulations.Dr.JasterisexcitedtoengageintheGenomic PressInterview,lookingdeeperintoherlifeinsideandoutside thelab.
Part1:AlainaM.Jaster–LifeandCareer
Couldyougiveusaglimpseintoyourpersonalhistory,emphasizing thepivotalmomentsthatfirstkindledyourpassionforscience?
ThisquestionisalwaystrickytoanswerbecauseIdidnotrealizethepivotalmomentsuntilIwasalreadydoingscience.Ididnotlinkmypersonal historytomydriveuntilIwaswellintocollege,butitmakessensenow. Ihaveafamilyhistoryofaddictionandhavefirsthandexperiencewith druguse,includingwhatitdoestofamiliesandtopeopleIcareabout. So,whenIwenttocollegeanddecidedtostudyneuroscienceandsubstanceuse,Ididitbecausethat’swhatIknewabout,andIwantedtounderstandwhysomepeoplechoosedrugsoverothervaluesandwhysome peopledon’thaveanyissueswithrecreationaluse.Ilearneditisalotmore complexthanthat,butmyentirelifeledmetothispassionforlearning aboutthemindandprovingthatyourcircumstancesdonothavetobethe end-all-be-all.
Wewouldliketoknowmoreaboutyourcareertrajectoryleadingupto yourcurrentrole.Whatdefiningmomentschanneledyoutowardthis opportunity?
MytrajectoryisalittleinterestingbecauseIdidnotreallyknowIwanted tobeascientist,asIwasneverreallyexposedtothatoption.Iknewabout medicinebecausemymotherwasanurse,butIwantedtobeanartistin highschool.Ihadlittleinterestinsciencesatschool,exceptformyAP
Received:30November2024.Accepted:3December2024. Publishedonline:17December2024.
psychologyclass.So,inmysenioryear,IendeduptouringCentralMichiganUniversity,wheretheyshowedapresentationontheirneuroscience programandtalkedaboutthebrain,whichIthoughtwasinteresting.I toldmyselfIcoulddoitandwantedtoproveIwasnotmyfamilyhistory.Attheendofmyundergraduateexperience,Iwastryingtodecide onbeingacounselororgoingforaPhDinclinicalpsychology.Eventually, IdecidedthroughexperiencesworkingataninpatientpsychiatricfacilitythatIwasnotreadyfordirectpatientcare.However,Istillwantedto helppeoplewhoweresufferingfromthesehorriblepsychiatricillnesses. IendedupwitharesearchassistantjobatWayneStateUniversity,whereI workedwithhumanpostmortemtissueandgeneticsofopioiduse,along withtoxicologyandpharmacologyprojects.Thissolidifiedmyinterestin drugsandhowtheychangethebrain.
Pleasesharewithuswhatinitiallypiquedyourinterestinyour favoriteresearchorprofessionalfocusarea.
Honestly,eversinceIwasinhighschool,Ithoughtpsychedelicdrugs werefascinating.Theclinicaltrialswithsmokingcessationanddecreased drinkingfollowingpsilocybincameoutwhenIwasinmyundergraduate degree,andIwasjustsoexcitedtoseepsychedelicsbeingusedfortreatingsubstanceusedisordersthatIknewIhadtofindawaytostudythis
Figure1. AlainaM.Jaster,PhD,WayneStateUniversity,USA.
Figure2. AlainaJasterexplores“HilltopTrine,”oneofThomasDambo’s“6ForgottenGiants”sculpturesinHvidovre,Denmark(2017).Thephotowastaken duringdowntimefromhersummerneurosciencecourseinCopenhagenwhensheparticipatedinanartistictreasurehunttodiscovertheselarge-scalepublic artinstallationsthroughoutthecity’swesternmunicipalities.ThisimagecapturesoneofAlaina’smanyexplorationsbeyondthelaboratory.
myself.Now,mystudiesarebroader,focusingonthecannabinoidsystem aswell,butitisjustasinterestingbecausecannabishasbeenshownto helpalotoffolkswithneuropsychiatricillnesseslikedepression.
Whatimpactdoyouhopetoachieveinyourfieldbyfocusingon specificresearchtopics?
Ihopetoexpandourcurrentknowledgeofwhyandhowdrugslikepsilocybinorcannabishaveprofoundeffectsonpeople.Itisessentialtodig intothosewhorespondandthosewhodonotrespondandfigureoutif somespecificbiomarkersorpathwaysareinvolvedintheseclinicaloutcomes.Withthisknowledge,wecanbetterinformtreatmentstrategies anddrugpoliciesthatmakesense.
Pleasetellusmoreaboutyourcurrentscholarlyfocalpointswithin yourchosenfieldofscience?
Theuseofmultidisciplinaryapproachestounderstandingdiseasehas onlyrecentlytakenoff,wheremanystudieswithinthefieldofneurosciencefocusedsolelyonbehaviorormolecularpharmacology.However, withmorepeopleinthefieldandnoveltechniques,wecanprobefor thingslikebiomarkers,theinfluenceofspecificcelltypesandtheirprojections,andalterationsinbrainconnectivity—allatonce.Mycurrent focusisonusingtranslationaltechniquesandbridgingthegapbetween preclinicalandclinicalresearchonneuropsychiatricandsubstanceuse disorders.
Whathabitsandvaluesdidyoudevelopduringyouracademicstudies orsubsequentpostdoctoralexperiencesthatyouupholdwithinyour researchenvironment?
Iamcurrentlyinmypostdoctoralposition,whereIamlearningsomuch aboutcoordinatingandleadingclinicaltrials,teamwork,andpositive workenvironments.AcrossmyPhDandnowmycurrentposition,one thingthatIhavefoundmostimportantisallowingmyselftoenjoythe thingsIloveoutsideofscience.AnotherthingIhavefoundacrosspositionsisthatkeepingagreatlabnotebookisaninvaluablehabit.
AtGenomicPress,weprioritizefosteringresearchendeavorsbased solelyontheirinherentmerit,uninfluencedbygeographyorthe researchers’personalordemographictraits.Arethereparticular culturalfacetswithinthescientificcommunitythatwarrant transformativescrutiny,oristhereacausewithinsciencethatdeeply stirsyourpassions?
Ithinkthereisashiftinthecommunitywherepeoplearebecomingmore tolerantandacceptingofallwalksoflife,butthereisstillmuchwork todo.Alotoffolksgointosciencebecausetheyhaveapersonalconnectiontotheirresearchquestions,butalotofpeoplewithlivedexperience(specificallywithsubstanceuseandneuropsychiatricdisorders) areturnedawayfromthefieldordonothaveproperaccesstothetools andhelptheymayneedtothrivewithinthescientificcommunity.Ithink insteadofhidingourpersonalexperiences,weshouldfosteracommunitythatapplaudsopennessandnotrefusestudentsortraineesbecause theywouldbe“difficult”toworkwithbecauseoftheirmentalhealthor disabilities.
Whatdoyoumostenjoyinyourcapacityasanacademicorresearch risingstar?
Thebestpartisalltheopportunitiestomakeadifference.Thereareso manyunansweredquestionsandsomanyopportunitiestocollaborate withothersinsideandoutsidemyspecificexpertisetoanswerthesequestions.Inaddition,theabilitytoinspireothersisalwaysgreat.Itisveryexcitingtohearthatsomeonereadmywork,listenedtomypodcast,orsaw meonapanel,anditgotthemexcitedaboutscience.
Outsideprofessionalconfines,howdoyouprefertoallocateyour leisuremoments,orconversely,inwhatmannerwouldyouenvision spendingthesemomentsgivenachoice?
Ontheday-to-day,afterwork,Ilovecominghometomycatsandputting onsomemusicwhileIcookwithmyfiancé.Ialsolovesittingdownwitha goodbookandacozyblankettospendmyleisuretime.Ialsoreallyenjoy travelingandgoingtoseelivemusic,sowhenIamabletodothesethings, Ialwaystakeuptheopportunityasshownin Figure2
Part2:AlainaM.Jaster–SelectedquestionsfromtheProust Questionnaire1
Whatisyourideaofperfecthappiness? Perfecthappinessdoesnotexist.Lifeisallaboutembracingthingsasthey comeandfindingjoyinthesmallthings.
Whatisyourgreatestfear? Theworldendingduetoclimatedisaster.
Whichlivingpersondoyoumostadmire?
Notasinglepersonbutallthepeoplewhohavebeendealtacrappyhand andkeepongoingdespiteallthethingsmovingagainstthem.
Whatisyourgreatestextravagance?
Idonotfeelquiteextravagant,butIdoenjoyafunstatementpiece fromtimetotime,likeabig,colorfulfuzzycoatorafunhatandgiant sunglasses.
Whatareyoumostproudof? IammostproudofmyselfovercomingalottogetwhereIamtoday.
Whatisyourgreatestregret? IdonotthinkIhaveone.
Whatisthequalityyoumostadmireinpeople? Senseofhumor.
Whatisthetraityoumostdislikeinpeople? Dishonestyandarrogancearetied.
Whatdoyouconsiderthemostoverratedvirtue? Theyallhavevalueandrequirebalanceineveryindividual.
Whatisyourfavoriteoccupation(oractivity)? Myfavoriteactivityisdancingataconcert.
Wherewouldyoumostliketolive?
Iwouldlovetolivesomewherewarmwithmountains.Iwouldalsoenjoy movingaroundEuropeandlivinginanewplaceeveryfewmonths.
Whatisyourmosttreasuredpossession? Mycats.
Whenandwherewereyouhappiest?Andwhyweresohappythen? IamhappiestwheneverIseetheworldandaminnature.Exploringand lettingourcuriosityrunwildiswhatwearemeanttodo.
1 Inthelatenineteenthcentury,variousquestionnaireswereapopulardiversion designedtodiscovernewthingsaboutoldfriends.Whatisnowknownasthe35questionProustQuestionnairebecamefamousafterMarcelProust’sanswersto thesequestionswerefoundandpublishedposthumously.Proustansweredthequestionstwice,atages14and20.In2003Proust’shandwrittenanswerswereauctioned offfor$130,000.Multipleotherhistoricalandcontemporaryfigureshaveanswered theProustQuestionnaire,includingamongothersKarlMarx,OscarWilde,ArthurConanDoyle,FernandoPessoa,StéphaneMallarmé,PaulCézanne,VladimirNabokov, KazuoIshiguro,CatherineDeneuve,SophiaLoren,GinaLollobrigida,GloriaSteinem, Pelé,Valentino,YokoOno,EltonJohn,MartinScorsese,PedroAlmodóvar,Richard Branson,JimmyCarter,DavidChang,SpikeLee,HughJackman,andZendaya.The ProustQuestionnaireisoftenusedtointerviewcelebrities:theideaisthatbyansweringthesequestions,anindividualwillrevealhisorhertruenature.WehavecondensedtheProustQuestionnairebyreducingthenumberofquestionsandslightly rewordingsome.Thesecuratedquestionsprovideinsightsintotheindividual’sinner world,rangingfromnotionsofhappinessandfeartoaspirationsandinspirations.
Whatisyourcurrentstateofmind?
Iamgratefulformyexperiencesandopportunitiesandforthehealthof mylovedones.
Whatisyourmostmarkedcharacteristic? Mydetermination.
Amongyourtalents,whichone(s)give(s)youacompetitiveedge? Iamreallygoodattimemanagement,andthatmakesiteasierformeto getalotdoneinashorttimeframe.
Whatdoyouconsideryourgreatestachievement?
Todate,probablytakingtheUSDrugEnforcementAgencytocourtchallengingtheschedulingofpsychedelicresearchchemicalsDOI/DOC.
Ifyoucouldchangeonethingaboutyourself,whatwoulditbe? Nothing.Peoplearechangingallthetime,everyday.
Whatdoyoumostvalueinyourfriends? Comfortability,knowingyoucanbeyourwholeselfaroundthem.
Whoareyourfavoritewriters?
IamabigfanofCharlesDickens,J.R.RTolkien,Ta-NehisiCoates,andCarl Hart.
Whoareyourheroesoffiction? IdonotthinkIhaveany.
Whoareyourheroesinreallife? Mymomcomestomindfirst;shereallyisa“super-mom.”
Whataphorismormottobestencapsulatesyourlifephilosophy? Inomniaparatus, aLatinphrasethatmeans“preparedforallthings”or “readyforanything.”
Detroit,Michigan,USA 30November2024
AlainaM.Jaster1 1 WayneStateUniversity,Detroit,Michigan48201,USA e-mail: jasteralaina@wayne.edu
Publisher’snote: GenomicPressmaintainsapositionofimpartialityandneutrality regardingterritorialassertionsrepresentedinpublishedmaterialsandaffiliations ofinstitutionalnature.Assuch,wewillusetheaffiliationsprovidedbytheauthors, withouteditingthem.Suchusesimplyreflectswhattheauthorssubmittedtousand itdoesnotindicatethatGenomicPresssupportsanytypeofterritorialassertions.
OpenAccess. The“GenomicPressInterview”frameworkiscopyrightedtoGenomicPress.Theinterviewee’sresponsesarelicensedtoGenomicPressundertheCreativeCommonsAttribution-NonCommercialNoDerivatives4.0InternationalLicense(CCBY-NC-ND4.0).Thelicensemandates: (1)Attribution:Creditmustbegiventotheoriginalwork,withalinktothelicense andnotificationofanychanges.Theacknowledgmentshouldnotimplylicensorendorsement.(2)NonCommercial:Thematerialcannotbeusedforcommercialpurposes.(3)NoDerivatives:Modifiedversionsoftheworkcannotbedistributed.(4) Noadditionallegalortechnologicalrestrictionsmaybeappliedbeyondthosestipulatedinthelicense.Publicdomainmaterialsorthosecoveredbystatutoryexceptionsareexemptfromtheseterms.Thislicensedoesnotcoverallpotential rights,suchaspublicityorprivacyrights,whichmayrestrictmaterialuse.Thirdpartycontentinthisarticlefallsunderthearticle’sCreativeCommonslicenseunless otherwisestated.Ifuseexceedsthelicensescopeorstatutoryregulation,permissionmustbeobtainedfromthecopyrightholder.Forcompletelicensedetails,visit https://creativecommons.org/licenses/by-nc-nd/4.0/.Thelicenseisprovidedwithoutwarranties.

INNOVATORS&IDEAS:RISINGSTAR
FayzanRab:Whataretheeconomicandpublichealthimplicationsof psychedelictherapies?
©GenomicPress,2024.The“GenomicPressInterview”frameworkisprotectedundercopyright.Individualresponsesarepublishedunderexclusive andpermanentlicensetoGenomicPress.
Psychedelics March2025;1(2):6–9;doi: https://doi.org/10.61373/pp024k.0046
Keywords: Psilocybin,FDA,economicdemand,publichealthestimate, exclusioncriteria
Attheintersectionofmedicine,psychedelics,andsocialimpact standsFayzanRab,anMDCandidateatEmoryUniversitySchoolof Medicinewhobringsafascinatingblendofexperiencestohiscurrent roleasaclinicalresearcherattheEmoryCenterforPsychedelicsand Spirituality.Hisresearchexplorescrucialquestionssurroundingthe emergingpsychedelictherapylandscape,fromunderstanding minoritycommunities’perspectivestoexaminingthebroaderpublic healthandeconomicimplicationsofthesegroundbreaking treatments.Beforepursuingmedicine,Fayzancarvedoutadistinctive paththatincludedleadingproductdevelopmentattechgiants GoogleandMindstrongHealth,followedbygrassrootspolitical organizingintheBayArea.Today,alongsidehisresearch,hechannels hisleadershipexperienceintoexecutivecoaching,helping entrepreneursrefinetheircommunicationskillsandpresence.When heisnotexploringthefrontiersofpsychedelicmedicine,Fayzan enjoyslifeinAtlantawithhisfiancéeShuaandtheircatBella,where youmightfindthemhuntingforfreshproduceattheirneighborhood farmer’smarketorhostingspiritedgamenightswithfriends.Inthis GenomicPressInterview,heshareshisinsightsonthetransformative potentialofpsychedelictherapyinmodernhealthcare.
Part1:FayzanRab–LifeandCareer
Couldyougiveusaglimpseintoyourpersonalhistory,emphasizing thepivotalmomentsthatfirstkindledyourpassionforscience? Bothmyparentsarephysiciansandwhileweneverexplicitlydebatedthe meritsofthescientificmethod,itwasbakedintotheDNAofmyupbringing.Afewclassesincollegethatlookedatepistemologyandthehistoryof sciencereinforcedinmethevalueofscienceasaneutralarbiterindecipheringreality.InmyfirstcareerasaproductmanageratGoogle,weused principlesfromscience(breakingproblemsintofirstprinciples,validatingresults,seeingwhatwasreproducible)tobuildtechnologyproducts forusers.BythetimeIstartedmedicalschool,Ihadablendedphilosophyaroundscience.Iwantedtousethescientificmethodtorigorously testandexaminequestionsthatwerepertinentintherealworld.Ihave beensurroundedbymentorswhohaveencouragedthatinquiryindevelopingmyrelationshipwithscienceandusingitasapowerfulinstrument tobringclaritytotopicsthatIfeelareimportanttoanswer.
Wewouldliketoknowmoreaboutyourcareertrajectoryleadingupto yourcurrentrole.Whatdefiningmomentschanneledyoutowardthis opportunity?
Myinterestinpsychedelicsciencebeganduringaseriesofmini-lectures atUCSFdesignedforthepublic.Iwascontemplatingacareerswitchfrom SiliconValleytomedicine,andIwasblownawaybysomeoftheclinical researchonpsychedelictherapiesforhard-to-treatconditionslikePTSD
Received:5December2024.Accepted:9December2024. Publishedonline:24December2024.
anddepression.Thestatisticswerecompelling,butthetransformative, qualitativeaccountsfromparticipantscaptivatedme.
EmoryestablishedaCenterforPsychedelicsandSpiritualityduringmy thirdyearofmedicalschool,whichprovidedanaturalplaygroundtoexploresomeofthequestionsarisingintheburgeoningpsychedelicecosystem.Whilemanyresearchersfocusedonclinicaltrialoutcomes,Isawan unmetneedtoexplorequestionsaroundimplementation—suchaspublic healthneedsandreal-worldoperatingmodels.Thisrealizationledmeto createaresearchteamtoaddressthesecriticalissues.
Pleasesharewithuswhatinitiallypiquedyourinterestinyour favoriteresearchorprofessionalfocusarea.
Sooften,Iwoulddrivehomeattheendofapsychiatricclinicalserviceand besaddenedbythewaythehealthcaresystemtreatssomeofthemost
Figure1. FayzanRab,MDCandidate,EmoryUniversity,USA.
vulnerableandmentallyillinoursociety.Thesearethepatientsthatmany generalprovidersoftenfeelsomeaversiontowantingtotreat.Thecurrenttreatmentswehavedonotseemtoreachthepatientswiththeworst mentalillnessorprovideasustainedimpactthatchangesthetrajectory oftheiroutcomes.
Itwouldbeafool’serrandtosaythatpsychedelictherapies alonewouldchangethat.Treatingmentalillnesswillrequirechanges withinclinicalpracticebutalsoinvestmentsintosocialsafetynets,reemploymentopportunities,andaffordablehousing.
Psychedelictherapiesareoneofmanyingredientsthatcouldmakea significantdifference.Iamfortunatetoseeawholenewfieldofmedicine emergeatthisstageofmyclinicaltraining.Someofthequestionswe gettoaskaboutpsychedelics,suchasreimbursementmodels,diversityandinclusion,andpublichealth,provideentrypointstore-examine manyfundamentalaspectsofthewaymentalhealthcareoccursinthe UnitedStates.
Whatimpactdoyouhopetoachieveinyourfieldbyfocusingon specificresearchtopics?
Manyquestionsarewell-intentionedinacademicresearchformentalillness:howdoweincorporatemoreminorities,whatwouldimproveaccesstoallgroupsofpeople,andhowdowemeasureormakeadentin growingratesofmentalillnessintheUnitedStates?However,manyexistinghealthcaresystemsarestructuredinawaythatmakesithard—if notimpossible—tochangetheseinequities.Myhopeinpsychedelicscienceisthatwegettointegratethosequestionsearlyonwhilepsychedelic therapiesareintheirinfancy.Byaddressingandplanningforthemnow,I believethesetherapiescouldreachandbecomemoreaccessibletothose generallyexcludedfromtreatmentinnovations.
Pleasetellusmoreaboutyourcurrentscholarlyfocalpointswithin yourchosenfieldofscience?
Myresearchwithinpsychedelicscienceencompassesseveralinterconnectedareasoffocus.Iexaminethepublichealthandeconomicimplicationsofpsychedelictherapyapproval,particularlyregardingpatienteligibilityandbroaderhealthoutcomes.Anothercrucialaspectofmywork investigateshowculturalandreligiousminorities,withaspecificfocuson Muslimcommunities,relatetoandmightbenefitfrompsychedelictherapies–thisresearchaimstocreatemoreinclusivetherapeuticframeworks.Iamalsodeeplyinterestedinexpandingtheclinicalapplications ofpsychedelicsbeyondtraditionalmentalhealthconditions.Whilecurrenttrialspredominantlyfocusontreatment-resistantmentalillnesses,I amexploringpotentialapplicationsfordiversepopulations,suchascancerpatientsandthosewithpostpartumconditions,aswellasdifferent therapeutictargets,includingOCDandchronicpain.
Whathabitsandvaluesdidyoudevelopduringyouracademicstudies orsubsequentpostdoctoralexperiencesthatyouupholdwithinyour researchenvironment?
Inleadingmyresearchgroup,Iamguidedbytwofundamentalprinciplesthatshapeourapproach.Thefirstcentersonmaintaininganarrow focuswhileseekingbroaderapplications–eachresearchquestionwe pursuemustconnectspecificinquiriestolargerimplicationswithinthe field.Aprimeexampleisourstudythatestimatedpotentialpatientdemandforpsilocybintherapyindepressiontreatment.Whilewefocusedon determiningeligiblepatientnumbers,thisresearchilluminatedbroader aspectsofmedicaleligibilitycriteria,FDAapprovalprocesses,andpublichealthoutcomes.1 Thesecondprincipleemphasizesvaluingprogress overthepursuitofperfection.Academicworkcanoftenstallwhenresearchersbecomeoverlyfocusedonachievingperfection.Instead,Iencouragemyteamtoviewpeerreviewnotasatestdemandingperfectionbutasacollaborativeopportunitytorefineandenhanceourideas. Asdemonstratedinourrecentpublication(Rab,Raison&Marseille,2024,
1 RabSF,RaisonCL,MarseilleE.Anestimateofthenumberofpeoplewithclinicaldepressioneligibleforpsilocybin-assistedtherapyintheUnitedStates. Psychedelics PublishedonlineSeptember13,2024.doi: 10.61373/pp024r.0025 –inthisissue.
doi: 10.61373/pp024r.0025 –inthisissue),thisapproachhasenabledus tocontributemeaningfulinsightstothefieldwhilemaintainingscientific rigor.
AtGenomicPress,weprioritizefosteringresearchendeavorsbased solelyontheirinherentmerit,uninfluencedbygeographyorthe researchers’personalordemographictraits.Arethereparticular culturalfacetswithinthescientificcommunitythatwarrant transformativescrutiny,oristhereacausewithinsciencethatdeeply stirsyourpassions?
Thescientificmethodholdsimmensepotentialtoaddresssociety’smost pressingchallenges,yetscienceisoftenconductedinisolationfromcommunityproviders.Iwouldlovetoseemoredirectcollaborationswith organizationsandproviderstoidentifythemostpertinentreal-world questions.Inoneofmyresearchareas—Muslimsandpsychedelics—the majorityofhypothesesaredevelopedincoordinationwithlocalproviders. Bygroundingresearchquestionsinpartnershipswithon-the-groundorganizations,wecanensurethattheresultsanddiscoveriesarerelevant andmeaningfultothoseinthefield.
Whatdoyoumostenjoyinyourcapacityasanacademicorresearch risingstar?
Atafundamentallevel,itisvalidating.Sometimes,venturingoutsidethe comfortzoneoftheconventionalquestionsbeingstudiedcanfeelrisky. Already,manyclinicalpeersraiseeyebrowswhenImentionIamstudyingpsychedelictherapies.Inaddition,mostresearchersinthepsychedelic spacearenotdivingintothequestionsIamstudying;itcanbealottobe withattimes.Tohaveourpublicationacceptedandthenwidelypublicizedcanbeaffirmingforthatinitialinstinctthathadmeventureinthis direction.
Outsideprofessionalconfines,howdoyouprefertoallocateyour leisuremoments,orconversely,inwhatmannerwouldyouenvision spendingthesemomentsgivenachoice?
Ibelievethatleisureisanimportantpartofanycreativeresearchprocess. Askingunconventionalquestions,gettinginspired,andplayingwithideas wereallmadepossiblebecauseIcreateddedicated,uninterruptedleisure time.Leisure’snon-utilitariannaturetakesthepressureoffforitallto feelusefulandparadoxicallymakestheinquiriesIaskfeelmoreorganic andnatural.
Forme,leisureconsistsofsomestructuredstream-of-consciousness writing(checkoutthemorningpagesconceptfrom TheArtistWay),playingpickleballwithfriendsinmylocalcommunity,andspendingquality timewithmyfiancéeandcat.
Part2:FayzanRab–SelectedquestionsfromtheProust Questionnaire2
Whatisyourideaofperfecthappiness?
Celebratingthemomentsinmylifethatarealreadyjoyfulsuchasmy morningwalk,watchingamoviewithmyfiancée,andrelishingthatIget
2 Inthelatenineteenthcentury,variousquestionnaireswereapopulardiversion designedtodiscovernewthingsaboutoldfriends.Whatisnowknownasthe35questionProustQuestionnairebecamefamousafterMarcelProust’sanswersto thesequestionswerefoundandpublishedposthumously.Proustansweredthequestionstwice,atages14and20.In2003Proust’shandwrittenanswerswereauctioned offfor$130,000.Multipleotherhistoricalandcontemporaryfigureshaveanswered theProustQuestionnaire,includingamongothersKarlMarx,OscarWilde,ArthurConanDoyle,FernandoPessoa,StéphaneMallarmé,PaulCézanne,VladimirNabokov, KazuoIshiguro,CatherineDeneuve,SophiaLoren,GinaLollobrigida,GloriaSteinem, Pelé,Valentino,YokoOno,EltonJohn,MartinScorsese,PedroAlmodóvar,Richard Branson,JimmyCarter,DavidChang,SpikeLee,HughJackman,andZendaya.The ProustQuestionnaireisoftenusedtointerviewcelebrities:theideaisthatbyansweringthesequestions,anindividualwillrevealhisorhertruenature.WehavecondensedtheProustQuestionnairebyreducingthenumberofquestionsandslightly rewordingsome.Thesecuratedquestionsprovideinsightsintotheindividual’sinner world,rangingfromnotionsofhappinessandfeartoaspirationsandinspirations.

toaskthequestionsandworkontheproblemsIorganicallylovetothink about.
Whatisyourgreatestfear?
TolivealifethatisnotauthentictowhoIam.
Whichlivingpersondoyoumostadmire?
BernieSanders.Heiswillingtobemisunderstoodtoservewhathebelieveswillbenefithumanity.
Whatisyourgreatestextravagance?
Iloveagoodspaday.OneofmygoodfriendsandIwillmakeitahabitto visitalocalKoreanspaforawholeevening.
Whatareyoumostproudof?
Imetagreatlifepartnerandhadthecouragetoproposetoher.
Whatisyourgreatestregret?
StayingtoolonginajobwhereIfeltlikemymanagerwaspersonally puttingmedown.
Whatisthequalityyoumostadmireinpeople?
Pioneerswhoareinvestedinbridgingdisparateworlds.
Whatisthetraityoumostdislikeinpeople?
Self-righteousness.
Whatdoyouconsiderthemostoverratedvirtue?
Peoplewhotakemuchprideinsayingtheyarebusy.Busynessdoesnot equatetoprogressorvalue.
Whatisyourfavoriteoccupation(oractivity)?
Ilovecoachingpeoplewhoarefacingpersonallymeaningfulchallenges intheirlife.
Wherewouldyoumostliketolive?
Ahomethatisbasedaroundalotofwildlifeandnaturebutstillclose enoughtoalargeurbancenter.
Whatisyourmosttreasuredpossession? Mygrandfather’sstethoscope.
Whenandwherewereyouhappiest?Andwhyweresohappythen? TheweekendIproposedtomyfiancée:atotalsurprisetoher.Ourclose friendsandfamilycameintotownthefollowingdayandsurprisedus againwithafull-blowncelebration.
Whatisyourcurrentstateofmind?
Iamabitsadaboutcurrenteventsintheworld,butIamalsocalm, present,andgratefulforwhat’snext.
Whatisyourmostmarkedcharacteristic?
Deeplisteningandnotbeingafraidtotaketheconversationonelevel deeper.
Amongyourtalents,whichone(s)give(s)youacompetitiveedge?
Myabilitytodistillmultiple,diverseperspectivesandsynthesizethem intoapathforward.
Whatdoyouconsideryourgreatestachievement?
Cultivatingaclosesetoffriendshipsandmentorswhoserelationships havenotsuccumbedtothebusynessoflife.
Ifyoucouldchangeonethingaboutyourself,whatwoulditbe? IwouldhavemorefaithduringtimesofuncertaintyinthepathIamchartingformyself.
Whatdoyoumostvalueinyourfriends?
Iamluckytohaveanempoweredandaccomplishedsetoffriends.However,noneofthemconflatetheirresumesforwhatismostimportant:relationships.
Whoareyourfavoritewriters?
JohnSteinbeck,HarukiMurakami,andJhumpaLahiri.
Whoareyourheroesoffiction?
IlovethecharacterYusukeUrameshifromthe1990sJapaneseanime Yu YuHakusho.Heisahighschoolstudentwhodiesinacarcrashonlyto beresurrectedtofightinvisiblebattleswithspirits,demons,andvillains. Theshowissurprisinglydeepaboutredemption,rememberingthedayto-dayjoys,andbeingwillingtoputeverythingonthelineforsomething youbelievein.Iregularlywatchclipsfromthatshowforinspirationwhen Iencountersetbacksoruncertainty.
Whoareyourheroesinreallife?
Dr.TomInselforhiswillingnesstoreinvent;BernieSandersforhiscommitmenttoservingthecommonperson,andmygrandfatherforhisability toconnectdeeplywithothersandamazingstorytellingabilities.
Whataphorismormottobestencapsulatesyourlifephilosophy? “AmorFati.”3
Atlanta,Georgia,USA 4December2024
FayzanRab1 1 EmoryUniversitySchoolofMedicine,Atlanta,Georgia30329,USA e-mail: syed.f.rab@emory.edu
3 “AmorFati”isaLatinphrasemeaning“loveoffate”or“loveofone’sfate”thatwas particularlyembracedandpopularizedbyGermanphilosopherFriedrichNietzsche inthe19th century.However,theconcepthasearlierrootsinStoicphilosophy,especiallyinthewritingsofMarcusAureliusandEpictetus.
Figure2. FayzanRabwithhiscat,BellaDonna.
Publisher’snote: GenomicPressmaintainsapositionofimpartialityandneutrality regardingterritorialassertionsrepresentedinpublishedmaterialsandaffiliations ofinstitutionalnature.Assuch,wewillusetheaffiliationsprovidedbytheauthors, withouteditingthem.Suchusesimplyreflectswhattheauthorssubmittedtousand itdoesnotindicatethatGenomicPresssupportsanytypeofterritorialassertions.
OpenAccess. The“GenomicPressInterview”frameworkiscopyrightedtoGenomicPress.Theinterviewee’sresponsesarelicensedtoGenomicPressundertheCreativeCommonsAttribution-NonCommercialNoDerivatives4.0InternationalLicense(CCBY-NC-ND4.0).Thelicensemandates: (1)Attribution:Creditmustbegiventotheoriginalwork,withalinktothelicense
andnotificationofanychanges.Theacknowledgmentshouldnotimplylicensorendorsement.(2)NonCommercial:Thematerialcannotbeusedforcommercialpurposes.(3)NoDerivatives:Modifiedversionsoftheworkcannotbedistributed.(4) Noadditionallegalortechnologicalrestrictionsmaybeappliedbeyondthosestipulatedinthelicense.Publicdomainmaterialsorthosecoveredbystatutoryexceptionsareexemptfromtheseterms.Thislicensedoesnotcoverallpotential rights,suchaspublicityorprivacyrights,whichmayrestrictmaterialuse.Thirdpartycontentinthisarticlefallsunderthearticle’sCreativeCommonslicenseunless otherwisestated.Ifuseexceedsthelicensescopeorstatutoryregulation,permissionmustbeobtainedfromthecopyrightholder.Forcompletelicensedetails,visit https://creativecommons.org/licenses/by-nc-nd/4.0/.Thelicenseisprovidedwithoutwarranties.
Psychedelics
INNOVATORS&IDEAS:RESEARCHLEADER
CharlesL.Raison:Elucidatingtheroleofconsciousexperienceinthetherapeutic effectsofpsychedelicsasameanstooptimizeclinicaloutcomes
©TheAuthor(s),underexclusivelicencetoGenomicPress2024
Psychedelics March2025;1(2):10–12;doi: https://doi.org/10.61373/pp024k.0010
Keywords: psilocybin,psychedelics,consciousness,depression, inflammation
CharlesRaison,MD,isaProfessorofHumanEcologyandPsychiatryin theDepartmentofPsychiatry,SchoolofMedicineandPublicHealth, UniversityofWisconsin-Madison.Dr.RaisonalsoservesasDirectorof ClinicalandTranslationalResearchforUsonaInstitute,asDirectorof theVailHealthBehavioralHealthInnovationCenter,Directorof ResearchonSpiritualHealthforEmoryHealthcare,andasVisiting ProfessorintheCenterfortheStudyofHumanHealthatEmory UniversityinAtlanta,GA.Dr.Raison’sresearchfocusesonthe examinationofnovelmechanismsinvolvedinthedevelopmentand treatmentofmajordepressionandotherstress-relatedemotional andphysicalconditions,aswellashisworkexaminingthephysical andbehavioraleffectsofcompassiontraining.Morerecently, Dr.Raisonhastakenaleadershiproleinthedevelopmentof psychedelicmedicinesaspotentialtreatmentsformajordepression. Hewasnamedoneoftheworld’smostinfluentialresearchersbythe WebofScienceforthedecade2010–2019.WithVladimirMaletic,heis authorof TheNewMind-BodyScienceofDepression publishedby W.W.Nortonin2017.WearehappytoshareDr.Raison’sperspectives onhislifeandcareerwithourreaders.
Part1:CharlesL.Raison–LifeandCareer
Couldyougiveusaglimpseintoyourpersonalhistory,emphasizing thepivotalmomentsthatfirstkindledyourpassionforscience? Mychildhoodwasdominatedbyaloveofscience,especiallyastronomy. Insixthgrade,Istartedmyownstargazingmagazine(withtheprinting helpofmyparents,whoownedasmall-townnewspaper).Myinterestin sciencelapsedinmyteenageyearsandwasreplacedbyasearchforspiritualanswerstolife’smysteries.Myjourneybacktowardsciencebegan notwithsciencebutinthehumanitieswhenIdiscoveredpsychoanalysis notinaclinicalcontextbutwhileworkingonaPh.D.inEnglish.Spurred onbythisandafirstencounterwiththepowerofpsychotherapyinmy ownlife,onChristmasEve1984,Ihada“roadtoDamascus”typeexperienceonaforlornhighwayinSouthTexaswhenIsuddenlydecidedthatI shouldchangemylife’sdirectionandbecomeapsychiatrist.Thisrequired thatIreturntoschooltocompleteallthepre-med-typeclassesIhadstudiouslyavoidedasanundergraduate.Thebeautyofphysicsravishedme, andImighthavesteppedawayfrommymedicalplanshadIthetalent; however,lackingtherequisitemathematicalgifts,Ididbecomeadoctor andapsychiatrist.ButIwasstillawaysawayfromspendingalifeinscienceasmyearlyyearsafterresidencywerespentasafull-timeclinician. Itisinterestinghowlifebringsthingsbackaround.Mylong-terminterestinspiritualtraditionslaunchedmylifeinscience.Inthemid-90s, IhadthegoodfortunetobefriendtheDalaiLama’ssister,who,inturn, introducedmetoseveralbrilliantTibetanBuddhistmonks.Thesegentlementaughtmemuchaboutesotericmeditationpractices,whichfascinatedme.Ibecameobsessedwithunderstandingwhatthesepractices didtothebrainandbodyfromaWesternscientificperspective.Iwas
Received:5March2024.Accepted:6March2024. Publishedonline:8March2024.
CharlesL.Raison,MD,UniversityofWisconsin-Madison,USA. especiallyinterestedintheeffectofthesepracticesonbodytemperature, asraisingbodytemperatureiscentraltothesetechniques,asoddasthat soundsfromourWesternperspective.
Aswonkyastheseconsiderationssound,theymotivatedmetoleavea clinicalfacultypositionatUCLA,throwcautiontothewind,andmoveto EmoryUniversityinAtlantainhopesthatIcouldleveragetheuniversity’s strengthsinTibetanBuddhiststudiesandmind-bodymedicinetopursue thestudiesIwantedtocommence.
Justaslifebringsthingsbackaround,sodoesitmoveforwardin paradoxicalways.IbecamearesearcheratEmoryunderthetutelage ofmyfriendandmentor,AndrewMiller.However,IcouldneverconductthestudiesofadvancedTibetanBuddhistmeditationpracticesthat hadbeenmyinitialimpetusforretoolingmycareertowardresearch. ApivotalmomentcameearlyonatEmorywhenIwasstilltrying—but strugglingtodotheworkIwantedtodo—whenAndysaid,“Whileyou arefiddlingwiththismeditationstuff,howaboutdoingsomerealscienceinthemeantime?”Thiswashisoffertojoinhiminstudyinghow inflammationaffectsthebrainandbodytoproducedepression.Iwas interestedinthermoregulationandbodytemperaturebecauseofmy
Figure1.
Figure2. CharlesL.Raisonvolunteeringto“betatest”anEEGprotocol. interestinameditationtechniquecalledtummo(madesomewhatfamousrecentlybyWimHof).Inflammationincreasesbodytemperature,so Ithought,"Whynot?"andjoinedAndy’sresearchteam.HadIsaid“no”and insistedonmymorenarrowfocus,Iwouldneverhavebeengiftedwitha lifeinscientificresearch.Thisisanimportantpointandaprofoundchallengeforyoungscientists.Ontheonehand,youdonotwanttogosofar awayfromyourintereststhattheworkistedious;however,ifyouaretoo rigid,tremendousopportunitieswillsailpast.
Myexperiencehasbeenthatresearchislikefollowingafascinating trailofbreadcrumbsthroughtheforest.Ifonemaintainsafeltsenseof whatoneislookingfor,thingsoftencircleback.AlthoughIneverdidthe studiesIhadinitiallyhopedtodo,overtheyears,Ihavebeenfortunateto conductmeditationstudiesand,inthelastdecade,studiesthatharken backtomylong-terminterestinbodytemperature/thermoregulation andmood.
Wewouldliketoknowmoreaboutyourcareertrajectoryleadingupto yourmostrelevantleadershiprole.Whatdefiningmoments channeledyoutowardthatleadershipresponsibility?
Myleadershiproles,suchastheyare,weresomethingotherthanwhatI activelypursued.IrealizedmanyyearsagothatIprefertooccupya“vice president”typerole,beingsecondincommandinaresearchgroup.Iwas nevermoreproductivethanwhenIexistedinthistypeofrelationshipat EmoryUniversitywithAndyMiller.Iamanexcellent“wingman”.Butyears pass,oneages,andovertime,oneisfacedwithachoice:toeitherstep intoleadershiporstepaside.Ihavegenerallysteppedin.Ihavehadseveralleadershippositionsoverthelastdecade,butIwillfocusontwohere. In2017,GeorgeGrant,MDiv,PhD,askedmetobecometheDirectorofResearchonSpiritualHealthfortheWoodruffSciencesCenteratEmoryUniversity.Becausemyprimaryacademicpositionis—andwasthen—atthe UniversityofWisconsin-Madison,IrealizedearlyonthatthebestwayI couldleadfromabitofadistancewastobringinasmuchresearchtalentaspossibleandthendisperseleadershipamongsttheseresearchers. IconsiderthisoneofmyprimaryleadershipaccomplishmentsbecauseI havebeenremarkablysuccessful(ifIcanbrag)atbringingremarkable youngerscientiststoEmoryasfacultyworkinginSpiritualHealth.More recently,adefiningmomentinthelastseveralyearsoccurredwhenIwas invitedtotakeontheroleofDirectorofthenewVailHealthBehavioral HealthInnovationCenter,anewinstitutesituatedwithinalargerconsortiumthathasbeenestablishedbetweenUW-MadisonandVailHealth.
Itookthispositionbecauseitpromisestobringmanyofmyresearch interestsandcolleaguestogetherintooneplacetoexploretheimplementationofnoveltreatmentsfordepression,anxiety,andsubstanceuse disorders.
Pleasesharewithuswhatinitiallypiquedyourinterestinyour favoriteresearchorprofessionalfocusarea.
Ihavealwayshadtwodeepintereststhathaveformedanundercurrent inallmywork.Oneoftheseistheabilityofthebodytoinfluencemental states.Theotheristhepotentialofparticularmentalstatestopromote profoundandsustainedwellbeing.Thesetwoare—ofcourse—related: thebodycanbeusedtodrivethemindintocertainmentalstates,and certainmentalstatescanprofoundlyaffectbodilyfunction.AsIdescribed above,IcameintoresearchbecauseIwasfascinatedbythepossibility thatcertainesotericBuddhistmeditationpracticesmightbeequivalent todeepbrainstimulatorstoinduceprofoundlypositivemental/emotional states.Morelately,myworkwithpsychedelicshasinducedinmeaprofoundinterestinthequestionofwhetherconsciousnesshasactualcausal powerintheworld(asopposedtobeingepiphenomenaltomorebasic non-consciousbrainprocesses).
Whatimpactdoyouhopetoachieveinyourfieldbyfocusingon specificresearchtopics?
Onamorefundamentalsciencelevel,Iwouldliketousepsychedelicsto explorethequestionofwhetherconsciousnesshascausalpower.Ona clinicallevel,Ihopetoconductstudiesthatidentifyandoptimizenovel treatmentsfordepressionandanxiety,especiallythosethatbuildupon ancientpracticesthatareoftenalsoadaptivestressors.
Pleasetellusmoreaboutyourcurrentscholarlyfocalpointswithin yourchosenfieldofscience.
IamcurrentlyuptomyeyeballsinfivemajorstudiesforwhichIhave primaryresponsibility.Fourofthesestudiesfocusontryingtounderstandbettertheroleofconsciousexperienceinthetherapeuticeffects ofpsychedelicsand,viathisunderstanding,tooptimizeoutcomes.One ofthestudiesfocusesonwhole-bodyhyperthermia.Thisstudyseeksto understandwhetherthetherapeuticeffectofheatcanbeexpandedby combiningheatwithcoldexposure.Thisstudyalsoseekstofollowupon priorworkthathasidentifiedapotentialimmune-basedantidepressant mechanismofactionofwhole-bodyhyperthermia.
Whathabitsandvaluesdidyoudevelopduringyouracademicstudies orsubsequentpostdoctoralexperiencesthatyouupholdwithinyour researchenvironment?
AprimaryvalueisnevertosetouttoprovewhatIalreadyknowtobe true—atraitthatistoooftenpresentinpeoplewhostudymind-bodytype interventionslikemeditationornoveltreatmentslikepsychedelics.Years ago,Iwastoldbyawiseperson,“Ifyouarescaredofthetruth,getoutof science,”andIhavetakenthattoheart.Istartstudieswithhypothesesbut amalwaysreadytoabandontheseandlistentowhattheworldistrying totellmethroughtheactualresultsofastudy.Themostexcitingstudies Ihavedonehavebeenthosethatdisprovenmyinitialhypotheses.
AtGenomicPress,weprioritizefosteringresearchendeavorsbased solelyontheirinherentmerit,uninfluencedbygeographyorthe researchers’personalordemographictraits.Arethereparticular culturalfacetswithinthescientificcommunitythatwarrant transformativescrutiny,oristhereacausewithinsciencethatdeeply stirsyourpassions?
Ihavebecomeincreasinglyconcernedaboutdatafalsificationwithinscience,asithasbecomesadlyandincreasinglyclearthatthisisarealissue.Asmuchasanyone,Iunderstandtheterriblepressureresearchersare undertoproducepositive“catchy”results.Nevertheless,theentireedificeofscienceisbuiltuponourabilitytotrustresults.Failedstudiesdo notaddmuchtoone’scareerinanystraightforwardsense.However,my bestideasgenerallycomefromresultsthatcontradictedmyeasyinitial hypotheses.
Whatdoyoumostenjoyinyourcapacityasanacademicorresearch leader?
Ienjoytheopportunitytodeviseandimplementstudiesthatattempt toaddressquestionsthatmostinterestmeandareessentialforhuman wellbeing.
Outsideprofessionalconfines,howdoyouprefertoallocateyour leisuremoments,orconversely,inwhatmannerwouldyouenvision spendingthesemomentsgivenachoice?
Itakea“SwissCheese”approachtoworkandleisure.Becauseofmymany responsibilities,Iworkallthetime,meaningIstartthedaywithwork,and lateintotheevening,itisusuallythelastthingIdo.Nevertheless,like SwissCheese,Ileaveholesintheconstantworkstreamtodofunthings withfamilyandfriends.SoIwork,offandonfrom7a.m.to10p.m.,but duringthatperiod,Iwillalsotakeacoupleofwalkswithmypartneror kids.WhenItravelforwork,Ioftentrytoleaveafewextrahoursopenfor whatIhavecalled“targetedtravel,"abriefexcursionthattransformsa worktripintosomethingfunandmemorable.IfIhadmoreofachoicein mytime,Iwouldeliminateemail.Fartoomuchofmytimeisspentjust cullingthroughallthedetailsthatemailingmakesitsoeasytobecome boggeddown.
Part2:CharlesL.Raison–SelectedquestionsfromtheProust Questionnaire1
Whatisyourideaofperfecthappiness?
Iwanttoexploresomewherenewandfascinatingonaperfectsummer’s daywiththepeopleIlove.
Whatisyourgreatestfear? DyingafterthepeopleIlove.
Whichlivingpersondoyoumostadmire? Igreatlyadmiremanypeople.ButIknowmypartnerChristineWhelan bestandadmirehermost.
Whatisyourgreatestextravagance? GreenChartreuse.
Whatareyoumostproudof?
ThewidevarietyofamazingpeopleIhavebeenhonoredtoknowas friends,colleaguesandfamily.
Whatisyourgreatestregret? Notmeetingmypartnersoonerinmylife.
Whatisthequalityyoumostadmireinpeople? Highlycompetent/talentedpeoplewhodon’ttoottheirownhorns.
Whatdoyouconsiderthemostoverratedvirtue?
Overtheyears,peoplehavecomplimentedmeonbeingarisk-taker,which Iappreciatebecause,infact,Iamrathercautiousandconservativeat heart.
1 Inthelatenineteenthcenturyvariousquestionnaireswereapopulardiversiondesignedtodiscovernewthingsaboutoldfriends.Whatisnowknownasthe35questionProustQuestionnairebecamefamousafterMarcelProust’sanswersto thesequestionswerefoundandpublishedposthumously.Proustansweredthequestionstwice,atages14and20.Multipleotherhistoricalandcontemporaryfigures haveansweredtheProustQuestionnaire,suchasOscarWilde,KarlMarx,Arthur ConanDoyle,StéphaneMallarmé,PaulCézanne,MartinBoucher,HughJackman, DavidBowie,andZendaya.TheProustQuestionnaireisoftenusedtointerview celebrities:theideaisthatbyansweringthesequestionsanindividualwillreveal hisorhertruenature.WehavecondensedtheProustQuestionnairebyreducingthe numberofquestionsandslightlyrewordingsome.Thesecuratedquestionsprovide insightsintotheindividual’sinnerworld,rangingfromnotionsofhappinessandfear toaspirationsandinspirations.
Whatisyourfavoriteoccupation(oractivity)?
Walkinginanewandexcitingplacewithmypartner.
Wherewouldyoumostliketolive?
WalnutCreek,CA
Whatisyourmosttreasuredpossession? Mycopyof“TheHandbookoftheYokuts.”
Whenandwherewereyouhappiest?Andwhyweresohappythen? IamthehappiestIhaveeverbeenrightnow.Laterinlife,Imetthelove ofmylife,andwehavefivechildrentogetherwhoarethelightofmylife. Myworkisstressfulbutfascinatingandmeaningful.
Whatisyourmostmarkedcharacteristic?
Wide-rangingcuriosityaboutlifeandtheworldwefindourselvesin.
Amongyourtalents,whichone(s)give(s)youacompetitiveedge? Abilitytopublicspeakandwrite.
Whatdoyouconsideryourgreatestachievement? Raisingmytwoteenageboys.
Ifyoucouldchangeonethingaboutyourself,whatwoulditbe? Iwouldbemoreorganized.
Whatdoyoumostvalueinyourfriends? Kindness,intelligence,passion,andvision.
Whoareyourfavoritewriters?
JohnSpivey(TheCryingDance,TheGreatWesternDivide),Rilke,Whitman, TSEliot(FourQuartets).
Whoareyourheroesinreallife?
FranklinDelanoRoosevelt,EleanorRoosevelt,Buddha,SamuelJohnson.
Whataphorismormottobestencapsulatesyourlifephilosophy?
“Oldmenoughttobeexplorers Hereortheredoesnotmatter Wemustbestillandstillmovingintoanotherintensity Forafurtherunion,adeepercommunion.”
CharlesL.Raison,MD1 1 SchoolofMedicineandPublicHealth,UniversityofWisconsin-Madison, Madison,Wisconsin53719;VailHealthBehavioralHealthInnovationCenter, Edwards,Colorado,UsonaInstitute,Fitchburg,Wisconsin,andWoodruffHealth SciencesCenter,EmoryUniversity,Atlanta,Georgia,USA e-mail: raison@wisc.edu
Publisher’snote: GenomicPressmaintainsapositionofimpartialityandneutrality regardingterritorialassertionsrepresentedinpublishedmaterialsandaffiliations ofinstitutionalnature.Assuch,wewillusetheaffiliationsprovidedbytheauthors, withouteditingthem.Suchusesimplyreflectswhattheauthorssubmittedtousand itdoesnotindicatethatGenomicPresssupportsanytypeofterritorialassertions.
OpenAccess. ThisarticleislicensedundertheCreativeCommons Attribution-NonCommercial-NoDerivatives4.0InternationalLicense (CCBY-NC-ND4.0).Thelicensemandates:(1)Attribution:Creditmustbegiventothe originalwork,withalinktothelicenseandnotificationofanychanges.Theacknowledgmentshouldnotimplylicensorendorsement.(2)NonCommercial:Thematerial cannotbeusedforcommercialpurposes.(3)NoDerivatives:Modifiedversionsofthe workcannotbedistributed.(4)Noadditionallegalortechnologicalrestrictionsmay beappliedbeyondthosestipulatedinthelicense.Publicdomainmaterialsorthose coveredbystatutoryexceptionsareexemptfromtheseterms.Thislicensedoes notcoverallpotentialrights,suchaspublicityorprivacyrights,whichmayrestrict materialuse.Third-partycontentinthisarticlefallsunderthearticle’sCreative Commonslicenseunlessotherwisestated.Ifuseexceedsthelicensescopeor statutoryregulation,permissionmustbeobtainedfromthecopyrightholder.For completelicensedetails,visit https://creativecommons.org/licenses/by-nc-nd/4. 0/.Thelicenseisprovidedwithoutwarranties.
Psychedelics
COMMENTARY
Psilocybin-assistedpsychotherapy:Advancements,challenges,andfuturedirections fortreatingresistantdepression
©TheAuthor(s),2024.ThisarticleisunderexclusiveandpermanentlicensetoGenomicPress
Psychedelics March2025;1(2):13–14;doi: https://doi.org/10.61373/pp024c.0022
Keywords: Psilocybin-assistedpsychotherapy(PAP), treatment-resistantdepression(TRD),psychedelics,psilocybin Depressionisaglobalpublichealthchallengethatrepresentsthe world’slargestcauseofdisability,especiallyinthecontextof traditionaltreatments.Onepotentialsolutionbeingexploredis psilocybinassistedpsychotherapy(PAP)whichshowspromisefor treatingdepression.ArecentstudybyRosenblatetal.exploresthe useofpsilocybininclinicalmentalcarewithpromisingresults(1).
Theincreaseinmajordepressivedisorder(MDD)casesparticularlysince 2005andworsenedbyCOVID-19isalarming(2).Whilemonoaminergic antidepressantshavebeenusedasatreatmentsincethe1980’s,theyoftentaketwotofourweekstoshoweffectsandmaynotworkforuptoonethirdofpatients(2).Additionally,sideeffectsleadupto50%ofpatients tostoptreatment(2, 3).Therefore,thereisagrowingfocusonfinding betterwaystoaddressdepression.
Respondingtotheneedforantidepressantoptions,psychedeliccompoundshavegarneredattentioninrecenttimes.Despitepastdisapproval duetorecreationaldruguse,thereisnowrenewedinterestinexploring psychedelicslikepsilocybinfortheirtherapeuticpotential(2, 4).
Psilocybin,anaturallyoccurringpsychedeliccompoundfoundincertainmushroomspecies,hasbeenfoundtohaveaprofoundimpacton consciousnessbyinteractingwithserotonin5HT2Areceptors(2, 3).Researchonanimalssuggeststhatpsilocybinisassociatedwithanincrease inbrainderivedfactor(BDNF)whichinfluencesplasticity,neurogenesis anddendriticgrowth(5).Interestingly,lowerlevelsofBDNFhavebeen linkedtodepressioninseveralstudies(6).Whiletheexactpathways throughwhichpsilocybinbenefitsconditionsisstillupfordebate,there ispromiseinusingittohelptreattreatment-resistantdepression(TRD) whencombinedwithpsychologicalsupport(3, 7).
TheideaofPAPhasbeengainingtractionasasupportedmethodfor addressingdepressionsymptomsinindividualswithbipolarIIdisorderas notedbyAaronsonandcolleagues(8).However,determiningthecombinationoftherapysessionsanddosagelevelsforeffectivenessremainsan areaofconcern.
Oneimportantareaofconcernisthecriticalissueofadversereactions, whichareparticularlyimportantinthelightofreportsofpsychedelicsinducedmaniathatcouldparadoxicallyindicatetheireffectivenessasantidepressants(9).Averygermanepointisthateffectivenessandsafety mustbewellascertainedinordertoavoidinvestingintherapiesthat maynotwork.Thisisparticularlyrelevantforlong-termpsychotherapyin combinationwithpsychedelics(10).Oneofthefrustrationsexperienced bycliniciansisthatmostoftheevidencesupportingtheuseofpsilocybinfordepressioncomesfromstudieswithverystricteligibilitycriteria, whichmakesitunclearifthefindingsfromthoserigoroustrialsareapplicableinreal-worldsettings,whereconditionslikepersonalitydisorders andsuicidality(whichtendtobeclinicaltrialexclusioncriteria)arehighly prevalent(11).
InaMarch2024articletitled“Psilocybinassistedpsychotherapyfor treatmentdepression:Arandomizedclinicaltrial(RCT)evaluatingrepeateddosesofpsilocybin,”Rosenblatandcolleaguesshedlightonthese issuesinthefieldofPAPresearch(1).ThisnewRCTprovidesevidencesupportingtheuseofpsilocybindosinginapopulationdealingwithcomplex psychiatricissuessuch,asTRDbipolarIIdisorder(BPII)orothercomorbid conditions.
InthestudyconductedbyRosenblatandcolleagues,participantshad anaverageMontgomery-AsbergDepressionRatingScale(MADRS)score of30.5,experiencingdepressionfor18.3years,andhavinggonethrough approximately11.27failedmedicationtrials.Interestingly40%ofthem hadexperiencewithelectroconvulsivetherapyorketamineinfusions.This trialinvolved31individualswithTRD;mostwereinitiallydiagnosedwith MDD(26participants),whileonlyfourwerediagnosedwithBPII.Eachparticipantalsohadatleastanotherco-morbidpsychiatricdiagnosis.One participantwithdrewbeforethestudybegan.Thetrialaimedtoevaluate thefeasibilityofusingpsilocybinincombinationwiththerapytoaddress TRD.Participantsweresplitintotwogroups:onereceivingtreatment (n = 16)andtheotheronawaitlistcontrol(n = 14).Oversixmonthsall treatedparticipantsreceivedonetothreedosesofpsilocybinat25mg eachalongwithpreparatoryandintegrationpsychotherapysessionsover asix-monthperiod.
Resultsshowedsignificantreductionsindepressionseverityinthefull sample,withfurtherMADRSscorereductionsfromrepeateddoses.The resultsshowedareductionindepressionseverityacrossallparticipants afterreceivingrepeateddosesofpsilocybin.Thetreatmentwaswelltoleratedwithoutanyreportedevents.Thehighretentionratesandmanageablesideeffectsemphasizedtheeffectivenessofthisapproachfor individualsstrugglingwithTRD.
TheuniqueaspectoftheresearchstudyconductedbyRosenblatand teamwastheirmethodofdosing,whichinvolvedadministeringpsilocybin basedonrelapseindicators.Thissetsitapartfromstudiesthattypically followedafixedsingledoseprotocol(4, 7, 9, 11, 12).Asacomparison,in astudybyGoodwinetal.,asingledoseapproachwasusedtoevaluatethe effectivenessofpsilocybindosesalongwithsupportforTRD(12).Inthis study,a1mgdoseservedasareferencepointcomparedtodoses.The findingsrevealedthatthe25mgdoseimprovedparticipantssymptoms afterthreeweekswhereasthemedium10mgdosedidnotshowsymptomreduction.Interestinglythecontroldoseof1mgdidnotyieldbenefits.Whilethisresearchemphasizedtheimportanceofdosingstrategies itonlyobservedpatientsfor12weeksindicatingtheneedforlongertrials tofullyunderstandthelastingeffectsofpsilocybintreatment.
Followingtheexaminationofdosingfrequency,theRosenblatetal. studybrokenewgroundbyextendingthefollow-upperiodtosixmonths andallowingforaschedulewithdosesgivenasneeded(1).Evaluating outcomestwoweeksposteachdose,thestudyfoundthattheprimary depressionmeasure,theMADRS,wassignificantlyloweratthelastpostdosefollow-upcomparedwithbaseline.Theauthorsconcludethattheir
Received:1June2024.Revised:16July2024and5August2024.Accepted:7August2024. Publishedonline:12August2024.
resultsindicatethatwhendepressionisrecurrent,asitoftenis,treatingit asonewouldtreattherecurrenceofotherepisodicdisordersmakesmore sensethanstickingwithamorerigidfixed-doseschedulethatmaynotbe personalizedtotheneedsofthepatient.
IfoundthattheapproachtakenintheRosenblatetal.studytodosingwasbetterthanwhatotherstudieshaveshown.However,whilethe researchbyRosenblatandcolleaguesshowspromise,therearesomelimitationstoconsider.Thefactthatitwasanopenlabelstudyhadasamplesize.Usingwaitlistcontrolsinsteadofaplacebogrouparesignificant issuesthatcouldmaketheantidepressanteffectsseemstrongerthan theyactuallyare.Additionally,thisstudydifferedfromonesbyproviding preparatoryandintegrationpsychotherapy,whichmightexplainwhythe antidepressanteffectwasnotasstrongasseeninstudieslikeGoodwin etal.,wheretherewasagreaterreductioninMADRSscores(1, 12).
Instudiesinvolvingpsilocybin,includingtheoneledbyRosenblat etal.,participantsreceivesupportthroughthreephases:preparation, dosingsessionandintegration(1, 13).ForpatientswithTRD,therapyis believedtoenhancetheeffectsofpsilocybinandhelpindividualsprocess theirdosingexperiences(5).Thisdynamicrelationshipmakesitdifficult todeterminewhetherimprovementsinsymptomsareduetopsilocybin itselforthepsychologicalsupportprovidedalongsideit.
TheeffectofpsychotherapiesusedinPAPtrialsontheeffectiveness oftreatingdepressionhasyettobedeterminedbyresearchers.Clinical trialsvaryinthenumberandtypeofpreparationandintegrationsessions provided(14).Aswenotedpreviously,therangeofbackgroundtraining forthetherapistsisequallydiverse(13).ThesePAPtrialshavenottried tostandardizeeitherthepsychotherapiesorthetherapists.
Aswemoveforward,theintegrationofPAPintopracticemaypresent somerealchallenges.Whiletherearethosewhobelievethatpsilocybin therapycouldwellprovidesomelastingbenefitswhencomparedtoketamine,thepotentialcostofthesetherapieshassomeprofessionalsconcerned.Ifthecostofthesetherapiesrises,itbecomesanevenbiggerbarriertoaccess.Rightnow,acoupleofdifferenteffortsareexploringgroup therapyandvirtualtherapyaspotentialalternativesthatcouldsavepeoplemoney,butthesafetyandefficacyofthosetherapiesarenotyetestablished.Anotherthingthatisperhapslessfrequentlydiscussedisthe hugeimportanceofsettinginenhancingtheeffectsofthesetherapies.In short,placesmatter;andyouneedtohaveanaccessiblespaceifyouare goingtohaveapositiveeffect(15).
Tosumup,animportantstepwastakenbyRosenblatandassociates whentheyrecentlyilluminatedthesubjectofpsilocybinanditspossible useasatreatmentfordepression.Whattheydidwasquitedifferentfrom whathasbeendonebeforeinthisarea.Theytookagroupofpeoplewho hadseriousmentalhealthissues(inthisinstance,depression),inreallifesettingsthatincludedmultiplecomorbidities.Futurestudieswillbe requiredtoaddressconstraintslikeanopenlabeldesignsamplesizesand controls.
Onecouldmakethecasethatfutureresearchmustincludelarger, placebo-controlledtrialsoverextendedtimesothatwecanclearlyascertainthelong-termsafetyaspectsofpsilocybinandgeneratetheevidenceneededtooptimizethecombinationofdosingwithpsychotherapy sessions.AddressingvariationsinpsychotherapytechniquesandtherapisttrainingwillplayaroleinenhancingtheeffectivenessandconsistencyofPAP.Moreover,logisticalandfinancialobstaclesneedtobeaddressedsincePAPdemandstherapistengagement,specializedtraining andsuitableclinicalenvironments.Continuousresearchisvitaltorealize thepotentialofpsilocybinasatreatmentfordepressionofferingrenewed optimismforthosestrugglingwithTRD.
RodolfoMyronndeMeloRodrigues1
1 InternalMedicineDepartment,TexasTechUniversityHealthSciencesCenter, ElPaso,Texas79911,USA
e-mail: rdemelor@ttuhsc.edu
References
1.RosenblatJD,MeshkatS,DoyleZ,KaczmarekE,BrudnerRM,KratiukK,etal.Psilocybinassistedpsychotherapyfortreatmentresistantdepression:Arandomizedclinicaltrial evaluatingrepeateddosesofpsilocybin.Med.2024;5(3):190–200.e5.DOI: 10.1016/j. medj.2024.01.005.PMID:3835938
2.PearsonC,SiegelJ,GoldJA.Psilocybin-assistedpsychotherapyfordepression: Emergingresearchonapsychedeliccompoundwitharichhistory.JNeurolSci. 2022;434:120096.DOI: 10.1016/j.jns.2021.120096.PMID:34942586
3.CopaD,ErritzoeD,GiribaldiB,NuttD,Carhart-HarrisR,TagliazucchiE.Predicting theoutcomeofpsilocybintreatmentfordepressionfrombaselinefMRIfunctional connectivity.JAffectDisord.2024;353:60-9.DOI: 10.1016/j.jad.2024.02.089.PMID: 38423367
4.TabaacBJ,ShinozukaK,ArenasA,BeutlerBD,CherianK,EvansVD,etal.Psychedelic therapy:Aprimerforprimarycareclinicians-psilocybin.AmJTher.2024;31(2):e121–32.DOI: 10.1097/MJT.0000000000001724.PMID:38518269
5.ChisamoreN,KaczmarekE,LeGH,WongS,OrsiniDK,MansurR,etal.Neurobiologyof theantidepressanteffectsofserotonergicpsychedelics:Anarrativereview.CurrTreat OptionsPsych.2024;11:90–105.DOI: 10.1007/s40501-024-00319-8
6.SeelamneniV.Peripheralsignals,centralquestions:Examiningtherelationship betweenpsychedelicsandbrain-derivedneurotrophicfactor(BDNF).Psychedelics. 2024;1(1):1-2.DOI: 10.61373/pp024c.0013
7.PerezN,LanglestF,MalletL,DePieriM,SentissiO,ThorensG,etal.Psilocybin-assisted therapyfordepression:Asystematicreviewanddose-responsemeta-analysisofhumanstudies.EurNeuropsychopharmacol.2023;76:61–76.DOI: 10.1016/j.euroneuro. 2023.07.011.PMID:37557019
8.AaronsonST,vanderVaartA,MillerT,LaPrattJ,SwartzK,ShoultzA,etal. Single-dosesyntheticpsilocybinwithpsychotherapyfortreatment-resistantbipolar typeIImajordepressiveepisodes:anonrandomizedcontrolledtrial.JAMAPsychiatry.2024;81(6):555–62.DOI: 10.1001/jamapsychiatry.2023.4685.PMID:38055270; PMCID: PMC10701666
9.BoschOG,HalmS,SeifritzE.Psychedelicsinthetreatmentofunipolarandbipolar depression.IntJBipolarDisord.2022;10(1):18.DOI: 10.1186/s40345-022-00265-5 PMID:35788817;PMCID: PMC9256889
10.AdayJS,HortonD,Fernandes-OsterholdG,O’DonovanA,BradleyER,RosenRC, etal.Psychedelic-assistedpsychotherapy:whereisthepsychotherapyresearch?Psychopharmacology(Berl).2024;241(8):1517–26.DOI: 10.1007/s00213-024-06620-x PMID:38782821
11.GoodwinGM,CroalM,FeifelD,KellyJR,MarwoodL,MistryS,etal.Psilocybinfor treatmentresistantdepressioninpatientstakingaconcomitantSSRImedication. Neuropsychopharmacology.2023;48(10):1492–9.DOI: 10.1038/s41386-023-016487.PMID:37443386;PMCID: PMC10425429
12.GoodwinGM,AaronsonST,AlvarezO,ArdenPC,BakerA,BennettJC,etal.Singledosepsilocybinforatreatment-resistantepisodeofmajordepression.NEnglJMed. 2022;387(18):1637–48.DOI: 10.1056/NEJMoa2206443.PMID:36322843
13.HaikazianS,Chen-LiDCJ,JohnsonDE,FancyF,LevintaA,HusainMI,etal.Psilocybinassistedtherapyfordepression:Asystematicreviewandmeta-analysis.Psychiatry Res.2023;329:115531.DOI: 10.1016/j.psychres.2023.115531.PMID:37844352
14.CroweM,ManuelJ,CarlyleD,LaceyC.Psilocybin-assistedpsychotherapyfor treatment-resistantdepression:Whichpsychotherapy?IntJMentHealthNurs. 2023;32(6):1766–72.DOI: 10.1111/inm.13214.PMID:37589380
15.VargasMV,MeyerR,AvanesAA,RusM,OlsonDE.Psychedelicsandotherpsychoplastogensfortreatingmentalillness.FrontPsychiatry.2021;12:727117.DOI: 10.3389/ fpsyt.2021.727117.PMID:34671279;PMCID: PMC8520991
Publisher’snote: GenomicPressmaintainsapositionofimpartialityandneutrality regardingterritorialassertionsrepresentedinpublishedmaterialsandaffiliations ofinstitutionalnature.Assuch,wewillusetheaffiliationsprovidedbytheauthors, withouteditingthem.Suchusesimplyreflectswhattheauthorssubmittedtousand itdoesnotindicatethatGenomicPresssupportsanytypeofterritorialassertions.
OpenAccess. ThisarticleislicensedtoGenomicPressundertheCreativeCommonsAttribution-NonCommercial-NoDerivatives4.0InternationalLicense(CCBY-NC-ND4.0).Thelicensemandates:(1)Attribution:Credit mustbegiventotheoriginalwork,withalinktothelicenseandnotificationofany changes.Theacknowledgmentshouldnotimplylicensorendorsement.(2)NonCommercial:Thematerialcannotbeusedforcommercialpurposes.(3)NoDerivatives: Modifiedversionsoftheworkcannotbedistributed.(4)Noadditionallegalortechnologicalrestrictionsmaybeappliedbeyondthosestipulatedinthelicense.Public domainmaterialsorthosecoveredbystatutoryexceptionsareexemptfromthese terms.Thislicensedoesnotcoverallpotentialrights,suchaspublicityorprivacy rights,whichmayrestrictmaterialuse.Third-partycontentinthisarticlefallsunderthearticle’sCreativeCommonslicenseunlessotherwisestated.Ifuseexceeds thelicensescopeorstatutoryregulation,permissionmustbeobtainedfromthe copyrightholder.Forcompletelicensedetails,visit https://creativecommons.org/ licenses/by-nc-nd/4.0/.Thelicenseisprovidedwithoutwarranties.
Psychedelics
THOUGHTLEADERSINVITEDREVIEW
Effectsofayahuascaonfearandanxiety:cross-talkbetween5HT1Aand 5HT2Areceptors
LorenaTereneLopesGuerra1 ,RafaelGuimarãesdosSantos1 , 2 ,andJaimeEduardoCecilioHallak1 , 2
Ayahuascaisahallucinogenicsubstancecurrentlybeinginvestigatedforthetreatmentofmood,anxiety,andtrauma-relateddisorders. Evidencefromanimalandhumanstudiessuggestthattheeffectsofayahuascainvolvemodulationofneuralsubstratesrelevantforemotional processing,especiallyinregionsrichinserotonergicreceptors.Moreover,preclinicalstudiesalsoshowthatayahuascahasspecificeffectson fear-relatedmemories.Theserotonergicsystemhasbeenclassicallyassociatedtoanxietyandfearresponses,withselectiveserotonin reuptakeinhibitorsbeingfirst-classmedicationtotreatmood,anxiety,andstress-relateddisorders.Herewereviewcurrentlyavailabledata regardingayahuasca(anditsmaincomponents)behavioralandfunctionaleffectsonanxietyandfear-relatedresponsesthroughits modulationofserotoninergicsignaling.
Psychedelics March2025;1(2):15–25;doi: https://doi.org/10.61373/pp024i.0037
Keywords: Ayahuasca,fear,anxiety,serotonin
Introduction
Ayahuasca(AYA)isahallucinogenicbeveragetraditionallyconsumedby indigenousgroupsfromNorthwesternAmazonand,morerecently,bysyncreticreligiousgroupspresentworldwide.ThemainpsychoactivecompoundinAYAisN,N-dimethyltryptamine(DMT),presentintheleavesof Psychotriaviridis,butthepreparationofAYAalsoinvolvesthe Banisteriopsiscaapi vine,richin β -carbolines(1).The β -carbolinesactasantagonistsondigestivesystemmonoamineoxidaseenzymesthat,otherwise,woulddegradeDMTbeforeitcouldreachthecentralnervous system(2).Harmine,tetrahydroharmine,andharmalinearethemostrelevant β -carbolinesinAYA,whichhavetheirownpharmacologicalproperties,addinganotherlayerofcomplexitytothemechanismsofactionof AYA(3).
AYAcanbedefinedasaclassichallucinogen,sinceithasagonisticeffectsindifferentserotonergicreceptors,especiallythe2Asubtype (5HT2Areceptor)(4).ThesubjectiveandhallucinogeniceffectsofAYA seemtoresultfromitsagonismat5HT2Areceptors;however,itcanalso actondifferentreceptorsubtypes,withthe1Areceptor(5HT1A)being ofspecialinterestforthediscussionproposedbythisreview(5, 6).The effectsofAYAonserotonergicpathwaysmostlyrelyonDMTaction,since β -carbolinespresentlittletonoaffinityformostserotoninergicreceptors,exceptforamodestaffinityforthe5HT2Areceptor(3, 5).
Similarlytowhathavebeenhappeningtootherpsychedelicsubstances,AYApropertieshavebeeninvestigatedastreatmentfornumerouspsychiatricdisorders,suchasdepression,anxiety,andsubstanceuse disorder(7–11).Additionally,preclinicalstudieshavesuggestedapossibleactionofAYAonfearprocessingcircuits,whichcouldsupportpossiblemechanismfortherapeuticeffectsonanxietyandposttraumatic stressdisorder(PTSD)(12, 13).Afewobservationalstudiesandcase reportshavealreadybeenpublishedabouttherapeuticeffectsofAYA ontraumaprocessingandtreatmentofPTSD(14, 15),withpromising results.Nonetheless,untilnow,clinicaltrialsperformedincontrolledsettingsarelacking.
Apartfromserotoninreceptors,AYAalsohaseffectsonglutamatergic, dopaminergic,andendocannabinoidsystems(16–18).Itispossiblethat DMTactsasanagonistof sigma-1 receptors(19),whichwasalreadysuggestedasapossiblemechanismforAYAeffectsonfearprocessing(20).
Moreover,AYAintakecanalterneuroendocrineresponsesaswell(21). Thesecomplexinteractions,however,arebeyondthescopeofthisreview. Here,weaimedtoconcatenateanddiscussdataregardingAYAeffectson fearandanxietyandhowitcanbeassociatedwithitsactionsonserotonin (5HT)receptors.
FearBehaviorandAnxiety
Fearisanevolutivepreservedbehaviorthatactsasadefensemechanism andisusuallytriggeredbythreateninganddangerousstimuli.Somestimulicannaturallyelicitadefensivebehavior,whileotherscanbelearned andassociatedtolifelongresponses.Thisbehavioralplasticityiscrucial foradaptationtoanenvironmentthatcontinuouslychallengesindividualswithnewcontexts(22).Anxiety,ontheotherhand,representsastate ofincreasedarousalandvigilanceevenintheabsenceofanimminent threat,anditcanalsoelicitbehavioraldefensiveresponses(23).
Impairmentsonappropriatefearandanxietyresponsesarethecause ofavarietyofpsychiatricdisorders,suchasPTSD,generalizedanxietyand panicdisorders(24).Effortstodevelopbettertreatmentoptionsforpatientssufferingfromthesedisordersdemandthedevelopmentoftests andparadigmsthatcanassessthebehavioralandneuralalterationsunderlyingthesymptoms.
ParadigmsforAssessingFearandAnxietyResponses
Themorefrequentlyemployedparadigmstoassessfearandanxietyresponsesinpreclinicalstudiesusuallyarerootedoninherentbehavioral characteristicsoftheanimalsoronassociativelearningofconditioned responsestonaturallyaversivestimuli.
Inthefirstcategory,theanimalbehaviorisaffectedbyanapproachavoidanceconflictbetweentheinherenttendencyfortheanimaltoexplorethenewenvironmentversusfear-drivenbehaviors.Theelevated plus-maze(EPM)andtheopenfieldtest(OFT)aretwoofthemostfamoustasksbasedonthispremise.Animalsexpressingincreasedanxietylikebehaviorspendmoretimeontheclosedarms(EPM)orintheedges ofthefield(OFT),respectively.Treatmentwithanxiolyticdrugsincrease entrancesandtimespendontheopenarmsfortheEPM,aswellastime spentinthecenterofthearenafortheOFT(25, 26).
Onthesecondcategory,theclassicalorPavlovianconditioningisthe mostwidelyemployedprotocoltostudyfearbehaviorandmemories.
1 DepartamentodeNeurociênciaseCiênciasdoComportamento,UniversidadedeSãoPaulo,RibeirãoPreto14015-010,Brazil; 2 NationalInstituteofScienceandTechnology TranslationalMedicine(INCT-TM)14015-010,Brazil
CorrespondingAuthor: Prof.RafaelGuimarãesdosSantos,DepartamentodeNeurociênciaseCiênciasdoComportamento,FaculdadedeMedicinadeRibeirãoPreto,UniversidadedeSãoPaulo,HospitaldasClínicas,TerceiroAndar,Av.Bandeirantes,3900,RibeirãoPreto,SãoPaulo,Brazil.Phone: +551636350713.E-mail: banisteria@gmail.com Received:9September2024.Revised:28October2024and12November2024.Accepted:14November2024. Publishedonline:10December2024.
Throughthisparadigm,astimulusonceneutral,thatis,thatdoesnot elicitabehavioralresponse,ispairedtoastimulusthatnaturallyevokes afearresponse.Oncetheanimalistrainedthroughsimultaneouspresentationsofthelatter(thatiscalledtheunconditionedstimulusorUS)togetherwiththeformer(whichwillbecalledtheconditionedstimulusor CS),anassociativememoryisacquiredandtheCSaloneisabletoevoke thebehavioralresponse(27, 28).AlterationsinUSintensityandCScharacteristicscanresultinmemorieswithdifferentcharacteristics,likeduration,intensityofevokedbehavioralresponseandgeneralization(22). Thetwomorefrequentlyemployedfearconditioningparadigmsarethe contextualfearconditioning(CFC)andthetonefearconditioning(TFC). Bothapplyelectricshocksattheanimal’spawastheUS,butthefirstuses thewholecontextwheretheanimalistrainedastheCS,andthelatter usesaspecificsoundastheCS,andtheanimalistestedbeingexposedto thesamesoundbutinadifferentcontextfromtraining(29).
Fearconditioningprotocolshavebeenwidelyemployedbypreclinical researchersasatooltounderstandmemoryformationaswellashowthey canbealteredorforgotten.Repeatedre-exposuretotheCSisthebase forreconsolidationandextinctionprotocols(30).Ifelucidatingthefear memoryformationisrelevant,understandinghowalreadyestablishedresponsescanbealteredcanbeevenmorevaluabletocontributefortreatingdisorderslikePTSD(31).
Inhumans,thebehavioralandsubjectiveconsequencesoffearand anxietyarefrequentlyassessedusingspecificallydevelopedpsychometricinstruments.However,therearemanytasksaswellthatcanbeemployed,beingespeciallyusefulwhenaccessingneuralalterationsunderlyingthebehavioralresponsesthroughneuroimagingtechniques.
Socialcognitiontasksfrequentlyemployemotionalrelevantstimuli. Duringtasksinvolvingtherecognitionofemotionsinfacialexpressions (REFE),subjectsarepresentedtostaticordynamicimagesoffacialexpressionsandaskedtorecognizepicturedemotion.Therearemanyvariationsinthesetasks,butseveralarebasedonEkman’stheoryofbasic universalemotions(32).Performanceinthesetasksseemstobealtered bynumerousconditions,especiallywhenrespondingtonegativevalence emotions,likefear(33–35).AnothertaskexampleistheSimulationof PublicSpeakingTest(SPST),ananxiety-inducedtaskwhereindividuals areaskedtoelaborateaspeechonarandommatterandpresentitinfront ofcamera,mimickingapublicspeaksituation(36).
NeuralSubstratesUnderlyingFearandAnxietyResponses
Multiplebrainregionsareinvolvedonprocessingofemotionallyrelevant stimuli,butasignificantpartoftheavailabledataproducedinthelast decadesfocusesonunderstandingcortical-limbiccircuitsdynamics.In thissection,wewillfocusonprefrontalcortex(PFC),amygdala(AMY), andhippocampus(HPP)influenceonfearandanxietyprocessing.Later (Section2.3),raphenucleiinnervationstothesestructureswillalsobe discussed.
PrefrontalCortex. ThePFCisinvolvedinnumerousexecutiveprocesses. Itreceivesandprojectstostructuresrelevanttoemotional,cognitive, sensory,andmotorfunctioning,resultinginacentralintegrativerolefor behavioralcontrolandflexibility,highlyinfluencedbyexternalcuesand internalcontingencies(37).AlthoughthereisanongoingdebateregardingthehomologiesbetweenrodentandprimatecompositionofthePFC, themedialPFC(mPFC)fromrodentsholdssimilaritiesinthemodulation exertedbyhumandorsolateral,medialandcingulatecorticesovermemory,emotionalregulationandresponsecontrol,amongotherfunctions (38).
TherodentmPFCincludestwomainsubdivisions,theprelimbiccortex(PL),thattogetherwiththeanteriorcingulatecortexconstitutes thedorsalmPFC,andtheinfralimbiccortex(IL),moreventrallylocated. Despitebeingcloselylocatedandintimatelyinterconnected,thesetwo regionshavedifferentprojectingprofiles(37, 39).ThePLhavemore efferentconnectionswiththebasolateralnucleusoftheAMY(BLA),and dorsalandmedianraphenuclei,whiletheILinnervatesnumerousAMY nuclei,butespeciallythecentralAMYnucleus(CeA),andthelateral septum(39).
ThePLprojections,althoughnotnecessaryforfearconditioningacquisition,areneededfortheconsolidationoftheassociativefearmemory
(40).ThePLisalsorelevantforfreezingexpressionafterTFC,sinceCSmodulateddisinhibitionofPLprincipalneurons(PNs)projectionstothe BLAisrelevantforfearexpressionduringtest(41).TheILactivitydoes notinfluencefearacquisitionorconsolidation;however,itisessentialfor fearextinctionretention,suggestingaroleonbehavioralflexibility(42). OptogeneticallysilencingILPNsduringextinctionlearningdoesnotinterferewithfreezingreductionwithinsession,butimpairedextinctionrecall. However,silencingthePNsduringextinctiontestdoesnotimpairextinctionrecall,indicatingthatproperILactivationisnecessaryforconsolidationoftheextinctionmemory(43).
ThemPFCactivityexertsatop-downmodulationofsubcorticalstructuresrelevantforemotionalregulation(37).Consistentwiththat,data fromclinicalandpreclinicalstudiessuggestthatincreasedanxietyresponsesarelinkedtoahypoactivationofthisregion,whichcanalsoresultinimpairedcognitiveflexibility(44–46).Inmice,synchronybetween mPFCandBLAactivityisrelatedtodiscriminationofsafetycontextsduringfearlearningandanxietyprotocols(47).Similarly,whencompared withhealthycontrols,patientswithgeneralizedanxietydisorderhadreducedventromedialPFCactivationwhenprocessingsafetysignals(48).
RegardingPLandIL,theirpreciseroleonmodulationofanxietyresponsesislesswelldefined,withcontrastingresultsontheliterature, thatmayresultfromprojections’functionalheterogeneity(49).
Amygdala. TheAMYisasubcorticalstructurecomprisingdifferentnucleiandlocatedinthemedialtemporallobe.Itreceivesprojections fromcorticalandsubcorticalstructures,essentiallyactingasaninformationprocessinghubthattranslatesensoryinputstootherareasrelevanttobehavioralcontrolandemotionalprocessing,suchasthePFCand HPP(50, 51).
Duringfearconditioning,theCSandUSassociationdependsonanintricatetemporalbalanceofthedifferentAMYnucleiactivation(22).The lateralportionoftheAMYistheinputregionforsensoryinformation,and itisalsowheretheCSandUSstimulirepresentationsareassociated.However,thecommunicationwithotherAMYnucleidependsonglutamatergic projectionsleavingfromthebasalAMY.Sincebothregionsareintimately interconnected,theyareoftenreferredasthebasolateralAMY(BLA)(52). IftheBLAisthemaininputcenter,thecentralAMY(CeA)istheoutput, projectingtostructuresrelevantforfearexpression,suchasthehypothalamusandtheperiaqueductalgray(53).TheBLAPNsinnervatedeCeAdirectly,butalsoregulateitsactivityindirectlythroughprojectionstothe intercalatedcells(ITC),aGABAergiccellmass,thatalsoinnervatesthe CeA(54).AMYactivityisnecessaryforbothCFCandTFC,butontheformer,thecontextrepresentationreliesondorsalHPPactivitywhichthen indirectlycommunicateswiththeAMYthroughventralHPPprojections (29, 55).
AlteredactivityindifferentAMYnucleiisassociatedtoanxietyresponses.InsidetheAMY,activationofprojectionsfromtheBLAtoCeA haveananxiolyticeffect,whileselectiveoptogeneticinhibitionofthese neuronsresultinanincreaseofanxiety-likebehaviorinmice(56).Functionalconnectivitybetweenthesetwosubregionsisalsoimpairedinpatientswithgeneralizedanxietydisorder(57).Whenexposedtoemotional relevantstimuli,patientswithanxietyandtrauma-relateddisorderstend topresentincreasedAMYresponse(58).
Hippocampus. TheHPPislocatedinthetemporallobeandimplicated inmultiplecognitive,memoryandemotionalprocessingfunctions.This structurecanbefunctionallydifferentiatedintotwodistinctareas,the ventralHPPandthedorsalHPP(59).
ThedorsalHPPfunctioningisassociatedtocognitiveperformanceand isresponsibleforencodingtherepresentationofthecontextduringCFC, hencewhythistaskisdescribedasHPP-dependent.Lesionsonthedorsal HPPimpairCFCexpressionwithoutalteringTFC(60).
Additionally,HPPisoneofthefewstructureswherenewneuronscan beborninadultbrains(61),althoughthereisanongoingdebatewhether thispropertyispresentinhumans(61, 62).Impairedneurogenesisseems toberelatedtosymptomatologyofmultiplepsychiatricdisorders,like depressionandPTSD(63).
However,thishippocampalregiondoesnotdirectlyprojecttotheAMY andtheintegrationsofcontextrepresentationtosensoryinputstoAMY
dependsonventralHPPprojections(64).AddedtoitsroleonCFCacquisition,dorsalHPPalsoisrelevantforfearmemoryrecallandextinction (65, 66).
TheventralHPP,ontheotherhand,ismoreassociatedtoemotional processing,beingtheonlyHPPregionprojectingdirectlytoAMY(64). Additionally,theventralHPPalsoseemtoberelevantforexpressionof anxietyresponses.Anxiogenicenvironmentsincreasesynchronizationof mPFCandventralHPP,thesamenotbeingreportedforthedorsalHPP (67).Additionally,lesionsontheventralHPPleadtodecreaseinanxietylikeresponsesintheEPM(68).
Inhumans,PTSDisassociatedwithdecreasedHPPvolumeandimpairedHPPactivationinwomenperformingaverbaldeclarativememory task(69),anditisalsoassociatedwithreducedHPPactivationtotraumarelatedstimuli(70).Inpatientswithgeneralizedanxietydisorder,the anteriorHPP(analogtotheventralHPPinrodents)haddecreasedactivationtorepeatedexposuretothreatcueswhencomparedwithhealthy controls(71).
SerotoninEffectsonFearandAnxietyResponses Studiesonhumanserotoninreceptorsareintimatelylinkedtohallucinogeniccompounds.In1953,Gaddumreportedlysergicaciddiethylamide (LSD)antagonisticeffectover5-HTresponseselicitedinvitro(72, 73) and,sincethen,sevenserotoninreceptorclasseshavebeendescribed, mostlyrepresentedbyG-proteincoupledreceptors(74).Althoughhallucinogeniccompoundscaninteractwithdifferent5HTreceptorclasses, mostoftheavailabledatafocusonthe5HT2and5HT1subtypes,specificallythe2Aand1Asubtypes(75).
The5HT2AsubtypeisGq/11 -coupledandabundantlyexpressedincorticalareas,especiallyonlayerVdendritesofPNs,whicharedenselyinnervatedby5HTaxons(76).Theiractivationmostlyproducesincreased membraneexcitabilitythroughaslowmembranedepolarizationandinhibitionofcalciumactivatedafter-hyperpolarizationcurrents(77).
The5HT1Areceptors,ontheotherhand,arepresynapticallyexpressed on5HTneuronsoftheraphenucleiwheretheyactasautoreceptors andregulate5HTrelease(78).However,theyarealsowidelydistributed throughsubstratesrelevanttomemoryandemotionalprocessing,suchas theHPP,cingulateandentorhinalcorticesandAMY,wheretheyarepostsynapticallyexpressed(79, 80).ThesereceptorsarecoupledtotheGi protein,andtheiractivationinducesmembranehyperpolarizationthrough increaseinrectifyingpotassiumcurrentsandinactivationofcalcium channels(74, 77).
Theseeminglyopposingeffectsof5HT2Aand1Areceptorsonmembranepotentialmayappearcontradictoryastheyareoftenco-expressed oncorticalPNs(81),butthesedifferencesarerelevantforstimuliprocessing.Thehyperpolarizingactionof5HT1Aaltersthesensibilityto input-generatedexcitability,restrainingfiringfrequency,whiletheinhibitionofafter-hyperpolarizationinducedby5HT2Aactivationincreases excitability,modulatingneuronalgain(77).ApartfromPNs,thesereceptorscanbeexpressedoncorticalGABAergicinterneurons(INs)aswell, addinganotherlayerofcomplexitytoserotonergiccontrolovercortical excitatory/inhibitorybalance(76, 81).
Throughthe70sand80smanystudiesexploredhow5HTaffectedpunishmentconditionedbehaviors.Atthetime,5HTsignalingpathwayswere thoughttoregulatethesebehaviorsandpromotepunishment-induced responsesuppression.Althoughfurtherevidenceelucidatedthatthisrelationshipisnotasstraightforwardasinitiallythought,5HTroleonfear andanxietyneurobiologyisstillundeniable,withselective5HTreuptake inhibitors(SSRIs)beingthefirstlineoftreatmentformanystressand anxietydisorders(24).
ThetheoryformulatedbyDeakinsandGraeffproposesthatdistinct fearandanxietybehavioralresponsesarecontrolledbyspecific5HTpathwaysarisingfromtheraphenuclei.Thedorsalraphe(DRN)periventriculartractisresponsibletoreacttoacuteUSexposure,controllingflightor fightresponses,andmostlymodulatingtheperiaqueductalgrayactivity. TheDRNforebrainbundletract(DRD/DRC)isactivatedbyacuteexposure toCSandcontrolsavoidancebehaviorsthroughprojectionstostructures suchastheAMY,ventralHPPandPFC.Andthemedianrapheforebrain bundletract(DRI/MnR)respondstochronicUSand/orCSexposure,being
responsibletopromoteresilienceortolerancetochronicstress,projectingtothedorsalHPPandPLandILcortices,actingmostlythoughpostsynaptic5HT1Aactivation(82, 83).
Knock-outmiceforthe5HT2Areceptorpresentdecreasedanxietylikebehaviors,buthavenormalCFCandTFC,andthereestablishment of5HT2Asignalingincorticalneuronsnormalizedtheanxiety-likeresponses(84).IntheBLA,activationof5HTprojectionsofDRNincreases anxiety-likeresponsesthrough5HT2Aactivation(85).
Pretreatmentwiththe5HT2AagonistTCB-2orantagonistMDL11,939 beforeacquisitionandretrievalofconditionedfearmemorydidnotinterferewithfreezingexpressionofmalemice,whileTCB-2administration posttrainingenhancedfreezingonCFCandTFCtests.Asfortheextinctionlearning,5HT2Aactivationisnotessential,butfacilitatestheprocess (86).Altogether,thesedatasuggestaroleforthe5HT2Areceptoronplasticitymechanismsalteringmemorytracesandbehavioralresponses,but thatroleislimitedtoalreadyacquiredmemoriesanddoesnotseemto influencetheestablishmentofnewassociations.
Activationofpostsynaptic5HT1Areceptors,ontheotherhand,seems todecreaseanxietyandstressresponses.Systemicorintrahippocampal treatmentwith5HT1Aagonist8-OH-DPATbeforeCFCimpairsfearmemoryretrieval,withoutsignificantlyalteringTFCmemoryretrieval.Theimpairmentswerenotobservedwhentreatmentwasadministeredafter training.Additionally,WAY100635,a5HT1Aantagonist,wasnotableto producememoryalterationswhenadministeredalone,butpreventedretrievalimpairmentswhencombinedwith8-OH-DPAT.Opposedtotheoutcomesobservedafter5HT2Amanipulation,5HT1Areceptorsseemtobe relevantformemoryacquisition,especiallyofHPP-dependentmemories, liketheCFC(87).
SerotoninReceptors’RoleonPsychedelicEffects
Thebehavioralandmentalalterationsresultingfrompsychedelicadministrationarefrequentlyassociatedtoitsagonismat5HT2Areceptors.In humans,ketanserin,a5HT2A/2Cantagonist,canbeusedtoreducesubjectiveeffectsinducedbyLSD(100or200 μg)(88, 89).Pretreatmentwith ketanserinalsopreventsthepsilocybin-induced(215 μg/kg)increasein positiveaffectandthedecreaseonrecognitionofnegativefacialexpressions(90).ForDMT(0.7mg/kg,i.m.),pretreatmentwithcyproheptadine,another5HT2A/2Cantagonist,didnotinterferewithsubjective effects(91).Ontheotherhand,pretreatmentwithpindolol,a5HT1A/βadrenergicreceptorsantagonist,intensifiedDMT(0.1mg/kg,i.v.)subjectivereactions,suggestinganattenuationresponseof5HT1Areceptors activationonDMTeffects.Theenhancementofsubjectiveeffectscaused bypindololcouldbearesultofincreased5HT2Asignalingafter5HT1A blockade(5).
RegardingAYA,pretreatmentwithketanserinalteredtheneurophysiologicaloscillatorypatternsinducedbyAYA(doseadjustedtocontain 0.75mg/kgofDMT)intakeandblockedvisualeffectsthroughblocking AYA-induceddecreaseinalphaoscillations(6).
Althoughtheavailableliteraturemostlyattributesthesubjectiveeffectsofpsychedelicstoagonismatthe5HT2Areceptor,someevidence pointsoutthatnoteverythingcanbeexplainedbyit.Inhealthyvolunteers,pretreatmentwithketanserindidnotpreventthereductioninattentionaltrackingabilitycausedbypsilocybin(215 μg/kg),suggesting arolefor5HT1Areceptors(92).Combinedadministrationofbuspirone, 5HT1Aagonist,andpsilocybin(170 μg/kg)reducedtheacutesubjective effectsofpsilocybin(93).Inchronicallystressedmice,treatmentwithketanserindidnotpreventtheantidepressanteffectsofasingledoseof psilocybin(1mg/kg,i.p.)(94).
PreclinicalEvidenceforAyahuasca’EffectsonFearandAnxiety-like Responses
AnimalstudiesevaluatingtheeffectsofAYAadministrationaretryingto decodehowthissubstancecaninterferewithbehavioral,functionaland structuralparametersoffearandanxiety-likeresponses,andhowthis couldbelinkedtothepossibletherapeuticeffects(Table1).
AsingleoraladministrationofAYA(containing9mg/kgofDMT)to femaleratsdecreasedlocomotionontheOFTandEPM,whichcouldbe anindicationofananxiogeniceffect,whilstitalsodecreasedimmobilityonforcedswimtest(FST),anindicationofantidepressanteffect.The
Table1. Fearandanxiety-likeresponsesfrompreclinicalstudies
TrainingTestingReconsolidationExtinction
Fearmemorytests
AYA–ChronicpretreatmentwithAYA(120 mg/kg)increasedfreezingatCFC andTFC(99).
AYAtreatment(60mg/kg) pretreatmentbeforeor afterreconsolidation sessiondecreasesfear expressiononCFCtest(12).
SingleAYA(0.3mg/kg ofDMT)dosereduces freezingduringCFC extinctiontraining, butnottest. However,two treatmentpaired extinctionsessions decreasefreezing duringtest(13).
SingleAYAdose(60 mg/kg)before retrieval,facilitates CFCextinction learningoneday after(12).
DMTAcutetreatmentwithDMT (10mg/kg)increased freezingduringTFC(96).
ChronictreatmentwithDMT (1mg/kg)didnotaffect behaviorduringCFCand TFCtraining(100).
β -carbolinesPre-trainingharmine(10 mg/kg)treatmentdidnot alteredaversiveavoidance learningduringPMDAT training(102).
AcutetreatmentwithDMT (10mg/kg)beforetrainingdid notalterfearresponseduring TFCtest(96).
ChronictreatmentwithDMT(1 mg/kg)didnotaffectbehavior duringCFCandTFCtest(100).
Pre-trainingtreatmentwith harmaline(1mg/kg)impaired fearresponseatthestep-down passiveavoidancetask(101).
Pre-trainingharmine(10mg/kg) treatmentimpairedfearresponse atCFC,butnotTFC(102).
Pre-trainingharmine(10mg/kg) treatmentimpaired aversive-avoidanceduringPMDAT test(102).
–DMTacute(10mg/kg) orchronic(1mg/kg) treatmentfacilitated TFC,butnotCFC, extinction(96, 100).
Anxietytest
AYAAcuteoralAYAdose(9mg/kgofDMT)decreasedlocomotiononOFTandEPM(95).
AcuteoralAYAtreatment(0.1,0.3ofDMT)hadnoeffectontimeintheopenarmsandclosedarmentries,butthehigherAYA dose(1.0mg/kgofDMT)increasedclosedarmentriesandgeneralexploratorybehavior(13).
OralsingledoseofAYA(60mg/kg)didnotalteropenarmandclosedarmentries,anddidnotalterlocomotion(12).
DMTOneDMTdose(10mg/kg,i.p.)reducedexplorationintheOFTandopenarmstimeandentriesonEPM(96). β -carbolinesAcuteharmine(5,10,15mg/kg,i.p.)treatmentdidnotalterbehavioralexpressionontheOFT(98).
AYA:Ayahuasca;CFC:Contextualfearconditioning;DMT:N,N-dimethyltryptamine;EPM:Elevatedplus-maze;OFT:Openfieldtest;PMDAT:Plus-maze discriminativeavoidancetask;TFC:Tonefearconditioning;–:Unavailabledata.
treatmentalsoinducedanincreasein c-fos expressingneuronsinthe DRN,posteriorBLAandHPP(95).Maleratstreatedwithonedoseof DMT(10mg/kg,i.p.)alsopresentedreducedexploratoryandincreased anxiety-likebehaviors,whilethreedoseswereabletoinduceantidepressanteffectsontheFST(96).Psylocibin,another5HT2Apsychedelicagonist,alsoincreasesanxiety-likeresponseswhenadministered15min priortotheOFT,butpromotesanxiolyticeffectswhenanimalsaretested 4haftertheadministration(3mg/kg,i.p.)(97).
Interestingly,acutetreatmentwithharmine(10or15mg/kg,i.p.)also inducedthedecreaseindepressive-likeresponsesonFST,withoutalteringexploratorybehaviors.Additionally,animalstreatedwiththehigher doseofharminealsopresentedincreasedhippocampalbrain-derived neurotrophicfactor(BDNF)expression(98).
FurthercomprehendinghowAYAcanaffectfearmemoryprocessing mighthelpelucidatehowthissubstancecouldbeusefulfortreatingdisorderssuchasPTSD.Mostpreclinicalstudiesonthisthemefocusonhow
AYAtreatmentcouldalteranalreadyestablishedfearmemory,which makessensewhenconsideredfromatranslationalpointofview.Nevertheless,theresultselicitedbytreatmentwithAYAanditsconstituent compoundspriortofearmemoryformationorduringreconsolidationand extinctionofalreadyestablishedmemoriesseemtodifferentlyaffectbehavioralresponses.
RatschronicallytreatedwithAYA(120mg/kg,oral)for30daysand latersubmittedtoCFCandTFCpresentedenhancedfreezingbehavior duringthetest.OnTFCtest,freezingwasincreasedevenbeforetheCS presentation.Treatmentwithhigherdoses(240and480mg/kg)didnot alterbehavioralexpression(99).DMT(10mg/kg,i.p.)alsoseemstoinfluencefreezingbehaviorwhenadministered1hpriortoTFC,increasing thisbehaviorduringtraining,butnotduringtest(96).Chronictreatment withsmallerdosesofDMT(1mg/kg,i.p.)beforetheconditioningprotocol,ontheotherhand,doesnotincreasefreezingbehavioronCFCandTFC tests(100).
β -carbolines,ontheotherhand,seemtopresentanamnesiceffect whenadministeredtoanimalspriortofearmemorytasks.Harmaline (1mg/kg,i.p.)injectedtomice5minbeforeastep-downpassiveavoidancetasktrainingpreventedincreasedlatencytostepdown24hlater duringtheretentiontest(101).Harmineadministered(10mg/kg,i.p.) torats1hbeforeCFCandTFCconditioningdecreasedfreezingbehavior whenanimalsweretestedforCFC24hlaterbutdidnotaffectfreezing ontheTFCtest48hlater.Ratssubmittedtoaplus-mazediscriminative avoidancetask(PMDAT)alsoweretreatedwithharmine(5,10,15mg/kg, i.p.)beforethetraining.Inthistask,aregularelevatedplusmazeisused, butoneoftheclosedarmswillbeequippedwithvisualandsoundaversivestimuli.Everytimetheanimalenterstheaversivearmduringtraining,thestimuliiscontinuouslypresenteduntiltheanimalleftsthearm. Althoughduringtrainingallanimalslearnedtoavoidtheaversivearm,indicatingmemoryacquisition,24hlaterallharmine-treatedgroupswere notsignificantlyavoidingtheaversivearmwhencomparedwiththeother nonaversivearms(102).
RatstrainedinaCFCprotocolthatreceivedasingledoseofayahuasca (60mg/kg)20minbeforeor3hafterare-exposuresessiontothe conditionedcontextpresentlessfreezingbehaviorwhentestedinthe samecontextonedaylater.Thisdecreaseisnotobservedduringthereexposuresessionitselfnorduringthetestwhentheanimalsaretreated withoutbeingre-exposedtoconditionedcontextpreviouslytotesting.Interestingly,thesameresultsarereproducedevenforremotememories, whentheanimalsaretested22daysafterthere-exposure.Theseresults suggestthatayahuascacouldbeactingonmemoryreconsolidation,reshapingthefearresponseasaconsequenceofthememorytracebecomingmorelabile(12).
Regardingextinctionprotocols,theresultsareconflicting.ThetreatmentwithasingledoseofDMT(10mg/kg,i.p.)1hpriorextinctiontrainingonTFC,aswellaschronictreatmentwithsmallerDMTdoses(1mg/kg, i.p.),seemtofacilitatefearextinction(96, 100).However,intheCFCprotocol,evenmultipletreatment-pairedextinctionsessionswerenotable toextinguishthefearresponse(96).OnmousesubmittedtoTFC,psilocybinadministration(2.5mg/kg,i.p.)priortoextinctiontrainingdecreased fearexpressionduringtrainingandduringextinctiontests1and6days aftertraining(103).
AYA(adjustedtocontain0.3mg/kgofDMT)administrationtorats 1hbeforeaCFCextinctionsessiondecreasesfreezingbehaviorduringthe sessions,butthereductionisnotsustainedonedaylaterontheextinction test.However,whentheanimalissubmittedtotwotreatment-pairedextinctionsessions,theextinctionmemoryisrecalledwhentestedoneday later(13).WhentheAYA(60mg/kg)treatmentwasadministered20min beforeor3hafteraretrievalsession,onedaypriortoextinctiontraining,asingledosewassufficienttofacilitatetheacquisitionofextinction memory(12).ChronicAYAtreatment(120mg/kg,oral)beforeCFCaltered freezingexpression,butdidnotaffectextinctionlearning(99).
Evenafterextinction,re-exposinganimalstotheUScanpromote thereinstatementofthefearresponse.TreatmentwithAYA(60mg/kg) 20minbeforeor3hafteraretrievalsessioncanpreventreinstatement aftertheacquisitionoftheextinctionmemory(12).However,whenthe treatment(adjustedtocontain0.3mg/kgofDMT)iscarriedoutduring theextinctionsession,althoughtheextinctionmemoryisacquired,the reinstatementisnotprevented(13).
ThedifferencesbetweentheresultsobservedfortreatmentwithisolatedcompoundsofAYAsuggestthe β -carbolinescouldbemoreeffectivetargetingHPP-dependentmemories,asisthecaseofCFC,step-down passiveavoidanceandPMDATtasks.Theseamnesiceffectscanbeanindicationthat β -carbolinesarepromotingincreasedneurogenesis,once increasingHPPneurogenesisonHPP-dependenttaskscanpromoteforgetting(104).However,allavailabledatatestthesesubstancesonmemoryacquisitionandearlyconsolidation,whiledataregardingitseffects onalreadyestablishedmemorytracesarestilllacking(101, 102).
DMT,ontheotherhand,doesnotaffectmemoryacquisitionandearly consolidation,althoughitsadministrationbeforeTFCenhancesfreezing responseduringthetraining.However,duringextinctionprotocolsfor TFC,treatingtheanimalwithasingledose1hbeforetheextinctionsessionorachronictreatmentwithsmallerDMTdosescanfacilitatefearex-
tinction,butthesameresultdoesnotoccuronCFCtrainedanimals(96, 100).Theseresultssuggestthat,althoughDMTcaninterferewithfear processing,itisnoteffectivefortargetingHPP-dependentmemories.
WhenAYAitselfisbeingtested,theextinctionandreconsolidation efficacywaslinkedtodurationandfrequencyofexposuretotheconditionedcontext.Extinctionretentionwasdependentonanimalsbeingreexposedtotheconditionedcontextatleasttwotimes(12, 13).Thecurrentmostwidelyacceptedviewonconsolidationofrecentintolong-term memoriespositsthatduringthisprocessthememorytracewillincreasinglyrelymoreoncorticalthanonHPPactivation(105).However,prolongedre-exposuretotheconditioningcontextcanleadtoHPPactivation,whichthencanmakethealreadyestablishedmemoryonceagain susceptibletoneurogenesisinducedforgetting(104, 106).Thesedata arereminiscentofexposuretherapyprotocolscurrentlybeingemployed totreatPTSD(31, 107).TheeffectofAYAonTFCreconsolidationand/or extinctionprotocolsstillneedstobetested.
AlthoughthesestudiessuggestthatAYAanditscomponentsmodulatefearmemoryprocessing,theconditioningprotocolstestedresponses inducedbynonpathologicalfearmemories,sincenoprotocolinduced generalizedfearbehaviorandmosttreatmentsdidnotincreaseanxietylikeresponseswhentestedusingtheEPM(12, 13).Thequestionremains whethertheoutcomeswouldbedifferentwhentestedforpathologicallikememories.
TraumafocusedtherapeuticinterventionsarecurrentlywidelyemployedandadvisedfortreatmentofPTSD(108).Theseinterventions arebasedonthepreviouslydiscussedpremisethatmemoryrecallcan facilitatethealterationofemotionalandbehavioralresponsesassociatedtothememorytrace.However,eventhoughdatasupporting trauma-focusedtherapiesarethemostrobustforallcurrentlyemployedtherapeuticstrategies,theyarenotalwayseffectiveand,inmany cases,theimprovementisnotsufficienttoabolishPTSDdiagnosis(109). Additionally,thereisalsoreportedvariabilityinpharmacologicaltreatmentefficacywhencomparingdifferenttraumaticevents.Forexample,cannabidiol(300mg)iseffectiveinreducinganxietyandcognitiveimpairmenttriggeredbytraumaticmemoryrecallonlyfornonsexual trauma(110).
Amongotherthings,thisvariabilitycanbeaconsequenceofdifferentsymptomatology.ThefiftheditionoftheDiagnosticandStatistical ManualforMentalDisorders(DSM-5)recognizedadissociativePTSDsubtype,characterizedbythepresenceofdepersonalizationandderealizationsymptoms(111).ComparedwithnondissociativePTSD,thissubtype seemstobelinkedtoincreasedcorticalinhibitionoflimbicstructures (112).Inpatientswithborderlinepersonalitydisorder,higherprevalence ofdissociativeexperienceswasapredictorforimpairedacquisitionand extinctionofanAMY-dependentclassicconditioningtask(113).
Althoughanimalmodelscanbeusefultounderstanddifferentinterventionsoutcomesonspecificcircuits,theylackprecisiontoevaluatespecificsymptoms.BroadeningtheunderstandingofhowPTSDcanalterpatients’brainfunctioningisessentialtothedevelopmentofbettermodels.
EvidenceforAyahuasca’EffectsonFearandAnxietyResponsesin Humans
NeuroimagingtechniquesusedtoinvestigatehowAYAintakealtersneuralsubstratessuggestthatitmodulatesstructuresandnetworksrelevant toemotionalprocessing.
Inonestudy,healthymalesubjectswererandomizedtoreceiveAYA (adjustedtocontain1mg/kgofDMT)orplaceboand100–110minafterintakeparticipantsweresubmittedtosinglephotonemissiontomography(SPECT)toassesshowAYAalteredregionalcerebralbloodflow (rCBF).Comparedwithplacebo,AYAbilaterallyincreasedrCBFonanterior insulaandinferiorfrontalgyrus,increasedrCBFontherightanteriorcingulateandfrontomedialcortex,andontheleftAMYandparahippocampalgyrus(114).AnotherSPECTstudy,thistimeevaluatingdepressivepatients,comparedrCBFpriortoand8hafterAYAintake(2.2mL/kg).The treatmentincreasedrCBFonleftnucleusaccumbens,rightinsulaandleft subgenualanteriorcingulatecortex(11).
Functionalmagneticresonanceimaging(fMRI)wasusedtoassess AYAeffectsonthedefaultmodenetwork(DMN)inhealthyvolunteers.
Subjectswereevaluatedbeforeand40minafterAYAintake(2.2mL/kg) whenperformingaverbalfluencytaskorduringrestingstate.Results contrastedDMNsignalduringrestingstateandduringtaskperforming, andadecreaseinsignalwasreportedfortheanteriorandposteriorcingulatecortices,mPFC,precuneusandinferiorparietallobules(115).
Hallucinogenseffectsevaluatedthroughsocialcognitiontaskscan alsobeusefultobettercomprehendhowthesesubstancescanalteremotionalprocessing.Studieswithhealthyandclinicalsampleshavebeen performedtoevaluatehowtheycaninterferewithREFE.
AstudywithhealthyvolunteerscomparedhowdifferentLSDdoses (100or200 μg)couldalterREFEperformancewhencomparedwith placebo.Subjectsweretested5hafterintakeofthelowerdoseand 7hafterintakeofthehigherone,andbothdosesdecreasedaccuracyfor recognitionoffearfulexpressions(116).Anotherstudybythesamegroup usedfMRItocomparehowhealthyindividualsrespondwhenpresented tofearfulorneutralexpressions.Eachsubjectreceived100 μgofLSDor placebo2.5hbeforethescan.Comparedwithplacebo,LSDreducedneuralresponsetofearfulversusneutralfacesonleftAMYandrightmedial frontalgyrus.TheAMYactivationtofearfulfaceswasalsonegativelycorrelatedtoreportedsubjectivedrugeffects(117).Also,administrationof psilocybin(215 μg/kg)tohealthysubjectsdecreasedtherecognitionof negativefacialexpressionswhencomparedwithplacebo(90).
RegardingAYA,healthyvolunteersweresubmittedtofMRIbeforeand afterdrugintake(25–35mL,0.333 ± 0.056mg/kgDMT),andaskedto performataskwithimplicitemotionalstimuli(neutral,disgustedorfearfulfacialexpressions).BeforeAYAintake,reactiontimewaslongerwhen aversivestimuliwerepresented,butduringtheAYAeffects,thereaction timewasnolongerdifferentforneutralandaversivestimuli.Together withthebehavioralalterations,AMYresponsivenesstoaversivestimuli wasattenuatedbyAYA,whiletheanteriorinsulaandthedorsolateral PFCresponsivenessincreased(118).Similarly,increasesinreactiontime inaREFEtaskwereobservedinhealthyvolunteersafterasingleAYA dose(1mL/kg; ±0.72mg/mLDMT)(119).Ontheotherhand,apreviousstudyevaluatingtheeffectsofasingledoseofayahuasca(1mL/kg; ±1.58mg/mLDMT)inhealthyvolunteersdidnotidentifybehavioraldifferencesonREFEperformancewhencomparedwiththeplacebogroup (120).However,thesestudiesdidnotassessparametersregardingneuralactivity,whichcouldbealteredevenintheabsenceofbehavioral outcomes.
AlthoughtheclinicalevidenceassessingtheeffectsofAYAonfear andanxietydisordersisstillscarce,afewobservationalandexperimentalstudieswithhealthysubjectsexploreditseffectsontrauma,memory, anxietyandphobiameasurements.
Long-termmembersofayahuascachurchesinBrazil(over15years), whencomparedwithactivelypracticingreligiousindividualsfrom catholicandprotestantchurches,showedlowerscoresonphobicanxiety availedthroughtheSymptomChecklist90–Revised(SCL-30-R),aselfreportinventorytoassesspsychopathologies(121).Anobservational, naturalisticstudyconductedwithhealthyparticipantstakingpartona AYAtraditionalindigenousretreatinPeruusedtheSentenceCompletionforEventsfromthePastTest(SCEPT)toevaluatehowthehallucinogenicexperiencecouldaltertheirperceptionofautobiographicalmemories,andasignificantreductiononscoresfornegativevalencememories wasobservedwhencomparingthebaselinewithpostretreatmentatthe6 monthsfollow-up.However,itisimportanttopointoutthattheseparticipantsdidnotpresentahighleveloftraumaticchildhoodexperiences,as assessedthroughtheChildhoodTraumaQuestionnairescorescollected onbaseline(14).
Anexperimentaldouble-blindedstudywithexperiencedmembersof anAYAchurchassessedpanicandanxietyoutcomesduringthesubstance peakeffects(1hafteringestion).AYA(3mL)andplaceboscoreswere comparedwithbaseline,andonlyAYAwaseffectiveinreducingpanicrelatedsignsassessedthroughtheAnxietySensitivityIndex.Anxietywas assessedusingtheState-TraitAnxietyInventory(STAI),buttheplacebo andAYAscoresdidnotdifferfrombaseline(122).
AnotherstudyinvestigatedthesubjectiveeffectsofAYA(1mL/kg; ±0.72mg/mLDMT)combinedwithplaceboorcannabidiol(600mg)on healthysubjectsusingtheVisualAnalogueMoodScale(VAMS).During
AYAeffectsparticipantsreportedadecreaseinanxiety,independently fromthepretreatmentgroup(119).
Regardingclinicalpopulations,arecentcaseseriesreportedtheuse ofAYAtotreatPTSDinwarveteranstakingpartinaretreat.ThePosttraumaticStressChecklist(PCL-5)wasusedtoassessPTSDsymptoms andtoevaluateclinicalchangesthroughtheprotocol.Mostparticipants (7outof8)loweredPCL-5scoresaftertheintervention,and5ofthemstill hadlowerscores3monthsaftertheinterventionwhencomparedwith baseline.Morethanhalfoftheparticipantsreportedintenselyexperiencingintrusivememoriesofthetraumaticevent.Aftertheintervention,the largestimprovementswereobservedinClusterEsymptoms,concerning sleepdisturbances,hypervigilance,andconcentrationdifficulties,andalthoughsomeparticipantsreportedareductiononintrusivememories,it wasnotstatisticallysignificant(15).
AYAwasalsotestedinarandomized,placebo-controlledtrialwith subjectsdiagnosedwithsocialanxietydisorder.Participantsreceiveda singledoseofayahuasca(2mL/kg, ±0.68mg/mLDMT)orplaceboand, aftertheacuteeffects(300minafterintake),theyweresubmittedto theSPST.Duringtheprotocol,anxietyandself-perceptionofperformance wereassessedusingtheVAMS,theBeckAnxietyInventoryandtheState VersionoftheSelf-statementsDuringPublicSpeakingScale.Nosignificantdifferenceswerefoundbetweengroupsontheanxietymeasures,but theAYAgroupshowedimprovedperceptionofperformancewhencomparedwithplacebo(7).
Theobservationalandexperimentaldataavailableimplythat ayahuascamightbeapotentialtreatmentforanxietyandstressdisorders;however,thereisalackofstudieswithclinicalpopulationsconductedoncontrolledsettings.SinceAYAisanelementoftraditionalcultures,thereisaninherentchallengeonvariabilitycontrolofAYAstudies. Itcannotbemanufacturedwithcommercialpurposes,andtheabsence ofstandardizedproceduresleadtobrewbatcheswithhighlydiversealkaloidcompositionandconcentration,whichreflectsonthedosagevariabilitypresentinnaturalisticandexperimentalsettings.
Syntheticformulationsarealreadybeingtestedasapossiblealternativetotryimprovingthisvariability,andtotrytodealwithethicalproblemsattachedtotheuseoftraditionalformulations(123).
AyahuascaEffectsonFearandAnxietyResponsesThrough5HT Signaling
ThecurrentlyavailabledatasuggestthatAYAanditsconstituentsubstances,thatis,DMTand β -carbolines,canmodulatefearandanxietyresponses.However,molecularandfunctionaldatasupportingthebehavioralandclinicalobservationsarestillscarce.
Neuronalandsynapticplasticitymechanismsareafundamentalaspectsupportingbehavioralflexibility.Increasingefforthasbeenmade intoelucidatingpsychedelicinducedplasticity,anditispossiblethatthey holdtheanswerforthefast-actingtherapeuticpropertiesthesesubstancesapparentlyhave.
Similarlytootherpsychedelicsubstances,DMTcanpromoteincreased neuritogenesisandsynaptogenesisoncorticalneurons.ThiseffectispossiblymediatedbyBDNFinteractionwithTrkBreceptorsandsubsequent activationofmTORintracellularsignalingpathways(18).Micechronically treatedwithharmine(20mg/kg,i.p.for10days)alsopresentincreased BDNFexpressiononthePFC(124)(Figure1A).Inhumans,healthyanddepressiveparticipantsreceivingasingleAYAdose(1mL/kg)expressedincreasedBDNFserumlevels48hafterintakewhencomparedwithplacebo groups(125).
Oncorticalneurons,DMTplasticityincreasingpropertiesaredependenton5HT2Areceptorsactivation(18).However,injectionofa5HT2A antagonistintotheILdidnotpreventAYAfacilitationofextinctionlearningandrecallonratspreviouslysubmittedtoCFC,eventhoughitincreasedfreezinglevelsduringextinctionsessions(13).Theincreased freezingexpressionmightbeduetoadecreaseintheinhibitorycontrol overcentralAMYprojections,sincetheILPNsinnervatetheITCwhichthen inhibitscentralAMY(126)andthePNsactivationmightberegulatedby the5HT2Areceptor.
IncreasedplasticityattheILisnecessaryforextinctionmemoryretention(127);however,5HT2Aantagonismdidnotimpairextinction
Figure1. Plasticity-promotingmechanismstriggeredbyDMTandBC.(A)DMTandBC-inducedincreaseincorticalplasticityarelinkedtoenhancedBDNFlevels, althoughthismightresultfromactivationofdifferentreceptors.(B)IncreasedhippocampalplasticityandneurogenesisinducedbyDMTandBCrelyondifferent molecularpathways.5HT2A:serotonergicreceptor2Asubtype;BC: β -carboline;BDNF:brain-derivedneurotrophicfactor;DMT:N,N-dimethyltryptamine;SIGMA1: sigmareceptorsubtype1.
learning.Apossibleexplanationisthefactthatextinctionlearningrelies onBDNFincreaseonHPPinputstotheIL(128),soeventhough5HT2A antagonismcouldpreventDMTinducedplasticityattheIL,theextinction memorywasnotaffected.
Ontheotherhand,thesameprotocoltestinga5HT1AantagonistpreventedAYAeffectsonextinctionretentionorrecall,althoughitdidnot alterthedecreaseinfearexpressionduringextinctionlearning(13).IL projectionstoBLAarenecessaryforextinctionretention(129),andthese datasuggestthatthiseffectmightbemediatedby5HT1Aactivity.TheIL projectstoBLAPNsandINs,andduringfearextinctionsynapticefficacy ofPNsinnervationisreducedthroughaprocessthatmightresemblesa long-termdepression(126).Since5HT1Areceptorsarerelevanttomodulateinput-generatedexcitabilityoncorticalPNs,itispossiblethatthey areinvolvedinthesynapticefficacydecrease.AYAandDMTacutetreatmentsinrodentscanleadtoanincreaseinanxiety-likeresponsesonEPM andFST,despitealsoinducinganantidepressanteffectontheFST(95, 96).Thisincreaseinconflictanxietyresponsescouldbeaconsequence of5HT2Areceptoractivationbythesecompounds.Interestingly,different fromwhatisobservedafterAYAandDMTadministration, β -carbolinesdo notinduceanincreaseinanxiety-likeresponsedespitetheirmildaffinity for5HT2Areceptors(98)
Harminechronicadministration(20mg/kg,i.p.for10days)canincreaseHPPneurogenesisinmice(124),whichcouldalsoexplainthe behavioraloutcomesof β -carbolinesadministrationonHPP-dependent tasks(Figure1B).Opposinglytotheeffectsof5HT2Aactivationoncorticalneurons,ontheHPPthisreceptorisnotlinkedtoplasticityincrease. RatstreatedwithDOI,anotherpsychedeliccompound,presentdecreased HPPBDNFmRNAexpression,whilststillhavingincreasedBDNFlevelson corticalareas.Thismodulationwascompletelyblockedbya5HT2Aantagonistadministration.Interestingly,immobilizationstressalsoresults inadecreaseinBDNFmRNAsontheHPPthrough5HT2Aactivation(130). Hence,5HT2AactivationontheHPPpossiblydoesnotcontributeto theantidepressiveandmightberesponsiblefortheanxiogenicDMTef-
fects.Nevertheless,DMTtreatmentcaninduceneurogenesisonHPP,but themechanismseemstoresultfromsigma-1receptorsactivationinstead (131)(Figure1B).
Itispossiblethatthe β -carbolineseffectondepressive-likebehaviorsaswellasinHPP-dependentmemoriescouldrelyonitsantagonism ofmonoamineoxidaseenzymes,thatcouldincreasecirculatinglevelsof 5HT.Additionally,sincetheydonotpresentaffinityfor5HT1Areceptors, theywouldnotactivatetheraphenucleiautoreceptors,preventingthe decreasein5HTreleaseobservedafteracuteadministrationof5HT1A agonists(79, 132).
Possibly, β -carbolinesadministrationcouldsomehowpredominantly activatespecificraphenucleipathways,sincethebehavioralresponses observedafteritsadministrationresemblethemedianrapheforebrain bundletractmediatedresponses.ThispathwaydirectlycontrolsHPPactivity,andincreasedactivityinthiscircuitislinkedtoantidepressantbehavioralresponses(133).Also,thispathwaystimulationcandesynchronizeHPPthetaoscillations,whicharerelevantforassociativememory processing(134).Thiscouldexplainwhy β -carbolinestreatmentseems tobemoreeffectiveoninterferingwithHPP-dependentmemoryprocessing.Theanxiety-likeresponsesevokedbyacutetreatmentwithDMT suggeststhissubstancemightbeactingonsubstratesinnervatedbythe DRD/DRCprojectionsandwouldexplainthelackofeffectsofDMTtreatmentonCFCextinction,sincethistaskisHPP-dependent.Ontheother hand, β -carbolinespreferentialeffectonDRI/MnRpathwaycouldexplain thelackoftreatment-inducedanxiety-likebehaviors,despitetheirmild 5HT2Aaffinity,besidestheantidepressantpropertiesandamnesiceffects onHPP-dependentmemoriesprocessing.
FuturePerspectives
AlthoughAYAhasbeenemployedintherapeuticandreligiouscontextsfor centuries,thereisstillalottobedissectedonitsbiologicalandpsychologicaleffects.Thecomplexnatureofthisbrew,thatcombinesdifferent alkaloids,addsanotherlayerofintricacytoanalreadychallengingtask.
Incurrentlyavailableliterature,DMTisfrequentlymentionedasthe mainpsychoactiveconstituentofAYA,howevermanystudiesdiscussed throughoutthisreviewhighlightrelevantdifferencesonisolatedDMTeffectswhencomparedwithAYAor β -carbolines.Although β -carbolines lackthemind-alteringpropertiesofAYAandDMT,theyseemtohave therapeuticpropertiesaswell.Morestudiesinvestigatingthemolecularpathwayssupportingantidepressantandmemoryeffectselicitedby themcouldimprovecomprehensiononAYA,aswellasindicatecontexts whereisolated β -carbolinescouldbeemployedastreatment.Hereof, differencesonHPPplasticityandneurogenesismolecularpathwaysactivatedbyDMTand β -carbolinescouldclarifythedistinctbehavioral outcomespromotedbythesesubstances.
Regardinghumanstudies,thereisstillalongwaytogo.Theobservationalandexperimentalstudiesinvestigatinghealthypopulationssupporttherelevanceoffurtherinvestigations;however,clinicalstudiesare stilllacking,especiallyincontrolledsettings.Theunknownrisksthat psychedelicintakecanrepresenttospecificclinicalpopulationstogether withtheprejudiceaccumulatedfromyearsofcriminalizationaresome ofthechallengesfacedbytheresearchers.Ontopofthat,theincreasing hypearoundpsychedelictherapeuticeffectscanresultinapositivebias. Controllingthisbiasisalsoadifficulttask,sinceblindingisstillachallengeforthefield.
FinalRemarks
Inanattempttoassociatetheemergingdataonhallucinogenstherapeuticpropertiesfortreatmentofmentaldisordersandtheclassical Deakin/Graefftheorylinkingfearandanxietyresponsesto5HTsignaling,Carhart-HarrisandNutt(2017)proposethathallucinogen-induced 5HT2Aagonism,andthesubsequentactivation-inducedplasticity,mediateactivecopinginasimilarideatotheDRD/DRCprojections.Inthe samereview,theyalsoproposethatpassivecopingwouldbethemechanismsupportingconventionalantidepressantsefficacy,suchasSSRIs, andwouldbemediatedby5HT1Aactivity,similarlytotheDRI/MnR pathway(135).
Throughthatperspective,AYAtherapeuticpropertiescouldbeacombinationofactiveandpassivecopingmechanisms.The β -CarbolinesapparentcapacitytomodulateHPPactivity,inwhattheycallpassivecoping, couldbearelevantfactorbehindAYAeffectsonCFCextinctionthatcould notbereproducedbyDMTtreatment.DMT,ontheotherhand,seemto behavesimilarlytowhatisproposedforotherclassichallucinogens,favoringactivecopingstrategiesandmechanisms.
AuthorContributions
LTLG,MScpreparedtheoriginaldraft.RGDS,PhDintellectualconceptualization,reviewandeditingthemanuscript.JECH,MD,PhDintellectual conceptualization,reviewandeditingthemanuscript.
FundingSources
LTLGreceivedfundingfromCoordenaçãodeAperfeiçoamentodePessoal deNívelSuperior(CAPES,Brazil).JECHisrecipientofCNPq1Aproductivityfellowship.
AuthorDisclosures
Theauthorsdeclarenoconflictsofinterest.Thecorrespondingauthorhad fullaccesstoallthedatainthestudyandhadfinalresponsibilityforthe decisiontosubmitforpublication.Themanuscripthasbeenreadandapprovedbyallauthors.
References
1.Domínguez-ClavéE,SolerJ,ElicesM,PascualJC,ÁlvarezE,delaFuente RevengaM,etal.Ayahuasca:Pharmacology,neuroscienceandtherapeuticpotential.BrainResBull.2016;126:89–101.DOI: 10.1016/j.brainresbull.2016.03. 002.PMID:26976063
2.KimH,SablinSO,RamsayRR.Inhibitionofmonoamineoxidaseabyb-carboline derivatives.ArchBiochemBiophys.1997;337(1):137–42.DOI: 10.1006/abbi. 1996.9771.PMID:8990278
3.GlennonRA,DukatM,GrellaB,HongSS,CostantinoL,TeitlerM,etal.Bindingof β -carbolinesandrelatedagentsatserotonin(5-HT2and5-HT1A),dopamine (D2)andbenzodiazepinereceptors.DrugAlcoholDepend.2000;60(2):121–32. DOI: 10.1016/s0376-8716(99)00148-9.PMID:10940s539
4.VollenweiderFX,SmallridgeJW.Classicpsychedelicdrugs:updateonbiologicalmechanisms.Pharmacopsychiatry.2022;55(03):121–38.DOI: 10.1055/a1721-2914.PMID:35079988;PMCID: PMC9110100
5.StrassmanRJ.HumanpsychopharmacologyofN,N-dimethyltryptamine. BehavBrainRes.1995;73(1):121–4.DOI: 10.1016/0166-4328(96)00081-2 PMID:8788488
6.ValleM,MaquedaAE,RabellaM,Rodríguez-PujadasA,AntonijoanRM,Romero S,etal.Inhibitionofalphaoscillationsthroughserotonin-2Areceptoractivationunderliesthevisualeffectsofayahuascainhumans.EurNeuropsychopharmacol.2016;26(7):1161–75.DOI: 10.1016/j.euroneuro.2016.03.012. PMID:27039035
7.DosSantosRG,OsórioFDL,RochaJM,RossiGN,BousoJC,RodriguesLS, etal.Ayahuascaimprovesself-perceptionofspeechperformanceinsubjects withsocialanxietydisorder:apilot,proof-of-concept,randomized,placebocontrolledtrial.JClinPsychopharmacol.2021;41(5):540–50.DOI: 10.1097/ JCP.0000000000001428.PMID:34166299
8.OsórioFL,SanchesRF,MacedoLR,dosSantosRG,Maia-de-OliveiraJP, Wichert-AnaL,etal.Antidepressanteffectsofasingledoseofayahuascain patientswithrecurrentdepression:apreliminaryreport.BrazJPsychiatry. 2015;37:13–20.DOI: 10.1590/1516-4446-2014-1496.PMID:25806551
9.Palhano-FontesF,BarretoD,OniasH,AndradeKC,NovaesMM,PessoaJA, etal.Rapidantidepressanteffectsofthepsychedelicayahuascaintreatmentresistantdepression:arandomizedplacebo-controlledtrial.PsycholMed. 2019;49(4):655–63.DOI: 10.1017/S0033291718001356.PMID:29903051; PMCID: PMC6378413
10.RodriguesLS,ReisJAS,RossiGN,GuerraLTL,MaekawaRM,DeLima OsórioF,etal.Effectsofasingledoseofayahuascaincollegestudentswith harmfulalcoholuse:asingle-blind,feasibility,proof-of-concepttrial.JClin Psychopharmacol.2024;44(4):402–6.DOI: 10.1097/JCP.0000000000001872 PMID:38820373
11.SanchesRF,deLimaOsórioF,dosSantosRG,MacedoLRH,Maia-de-Oliveira JP,Wichert-AnaL,etal.Antidepressanteffectsofasingledoseofayahuasca inpatientswithrecurrentdepression:aSPECTstudy.JClinPsychopharmacol.2016;36(1):77–81.DOI: 10.1097/JCP.0000000000000436.PMID: 26650973
12.DaneluzDM,SohnJMB,SilveiraGO,YonamineM,SternCA.Evidenceonthe impairingeffectsofAyahuascaonfearmemoryreconsolidation.Psychopharmacology(Berl).2022;239(10):3325–36.DOI: 10.1007/s00213-022-062172.PMID:36069952
13.WerleI,NascimentoLMM,dosSantosALA,SoaresLA,dosSantosRG,Hallak JEC,etal.Ayahuasca-enhancedextinctionoffearbehaviour:Roleofinfralimbic cortex5-HT2Aand5-HT1Areceptors.BrJPharmacol.2024;181(11):1671–89. DOI: 10.1111/bph.16315.PMID:38320596
14.RuffellSGD,NetzbandN,TsangW,DaviesM,InserraA,ButlerM,etal.Ceremonialayahuascainamazonianretreats—mentalhealthandepigeneticoutcomesfromasix-monthnaturalisticstudy.FrontPsychiatry.2021;12:687615. DOI: 10.3389/fpsyt.2021.687615.PMID:34177670;PMCID: PMC8221532
15.WeissB,Dinh-WilliamsLAL,BellerN,RaughIM,StraussGP,CampbellWK. Ayahuascainthetreatmentofposttraumaticstressdisorder:mixed-methods caseseriesevaluationinmilitarycombatveterans.PsycholTrauma.2023.DOI: 10.1037/tra0001625.PMID:38059941
16.BrierleyDI,DavidsonC.Harmineaugmentselectricallyevokeddopamineefflux inthenucleusaccumbensshell.JPsychopharmacol.2013;27(1):98–108.DOI: 10.1177/0269881112463125.PMID:23076833
17.DosSantosRG,RochaJM,RossiGN,OsórioFL,OnaG,BousoJC,etal.Effectsofayahuascaontheendocannabinoidsystemofhealthyvolunteers andinvolunteerswithsocialanxietydisorder:Resultsfromtwopilot,proofof-concept,randomized,placebo-controlledtrials.HumPsychopharmacol. 2022;37(4):e2834.DOI: 10.1002/hup.2834.PMID:35107855
18.LyC,GrebAC,CameronLP,WongJM,BarraganEV,WilsonPC,etal. Psychedelicspromotestructuralandfunctionalneuralplasticity.CellRep. 2018;23(11):3170–82.DOI: 10.1016/j.celrep.2018.05.022.PMID:29898390; PMCID: PMC6082376
19.FontanillaD,JohannessenM,HajipourAR,CozziNV,JacksonMB,RuohoAE. ThehallucinogenN,N-dimethyltryptamine(DMT)isanendogenousSigma1receptorregulator.Science.2009;323(5916):934–7.DOI: 10.1126/science. 1166127.PMID:19213917;PMCID: PMC2947205
20.InserraA.Hypothesis:thepsychedelicayahuascahealstraumaticmemories viaasigma1receptor-mediatedepigenetic-mnemonicprocess.FrontPharmacol.2018;9:330.DOI: 10.3389/fphar.2018.00330.PMID:29674970;PMCID: PMC5895707
21.dosSantosRG,ValleM,BousoJC,NomdedéuJF,Rodríguez-EspinosaJ,McIlhennyEH,etal.Autonomic,neuroendocrine,andimmunologicaleffectsof ayahuasca:acomparativestudywithd-amphetamine.JClinPsychopharmacol. 2011;31(6):717–26.DOI: 10.1097/JCP.0b013e31823607f6.PMID:22005052
22.KimJJ,JungMW.NeuralcircuitsandmechanismsinvolvedinPavlovianfear conditioning:acriticalreview.NeurosciBiobehavRev.2006;30(2):188–202.DOI: 10.1016/j.neubiorev.2005.06.005.PMID:16120461;PMCID: PMC4342048
23.GrillonC.Modelsandmechanismsofanxiety:evidencefromstartlestudies. Psychopharmacology(Berl).2008;199(3):421–37.DOI: 10.1007/s00213-0071019-1.PMID:18058089;PMCID: PMC2711770
24.ZangrossiH,DelBenCM,GraeffFG,GuimarãesFS.Serotonininpanicandanxietydisorders.HandbookofBehavioralNeuroscience.London,UnitedKingdom: Elsevier;2020.p.611–33.
25.PellowS,ChopinP,FileSE,BrileyM.Validationofopen:closedarmentriesinanelevatedplus-mazeasameasureofanxietyintherat.JNeurosci Methods.1985;14(3):149–67.DOI: 10.1016/0165-0270(85)90031-7.PMID: 2864480
26.PrutL,BelzungC.Theopenfieldasaparadigmtomeasuretheeffectsofdrugs onanxiety-likebehaviors:areview.EurJPharmacol.2003;463(1):3–33.DOI: 10.1016/s0014-2999(03)01272-x.PMID:12600700
27.BlanchardRJ,FukunagaKK,BlanchardDC.Environmentalcontrolofdefensive reactionstofootshock.BullPsychonSoc.1976;8(2):129–30.
28.FanselowMS.Conditionalandunconditionalcomponentsofpost-shockfreezing.PavlovJBiolSci.1980;15(4):177–82.DOI: 10.1007/BF03001163.PMID: 7208128
29.CurzonP,RustayNR,BrowmanKE.Cuedandcontextualfearconditioningfor rodents.MethodsofBehaviorAnalysisinNeuroscience.2nded.BocaRaton (FL):CRCPress/Taylor&Francis;2009.
30.KidaS.Interactionbetweenreconsolidationandextinctionoffearmemory.BrainResBull.2023;195:141–4.DOI: 10.1016/j.brainresbull.2023.02.009 PMID:36801360
31.KidaS.Reconsolidation/destabilization,extinctionandforgettingoffear memoryastherapeutictargetsforPTSD.Psychopharmacology(Berl). 2019;236(1):49–57.DOI: 10.1007/s00213-018-5086-2.PMID:30374892; PMCID: PMC6373183
32.EkmanP.Anargumentforbasicemotions.CognEmot.1992;6(3–4):169–200.
33.BottinelliF,DelvecchioG,MoltrasioC,FerroA,DiwadkarVA,BrambillaP. Facialemotionrecognitioninpanicdisorder:amini-reviewofbehavioural studies.JAffectDisord.2021;282:173–8.DOI: 10.1016/j.jad.2020.12.064 PMID:33418364
34.ReisJAS,RossiGN,OsórioFL,BousoJC,HallakJEC,DosSantosRG.Interventionsfordeficitsinrecognitionofemotionsinfacialexpressionsin majordepressivedisorder:Anupdatedsystematicreviewofclinicaltrials. NeurosciBiobehavRev.2023;153:105367.DOI: 10.1016/j.neubiorev.2023. 105367.PMID:37619644
35.WilliamsCL,MilanakME,JudahMR,BerenbaumH.Theassociationbetween PTSDandfacialaffectrecognition.PsychiatryRes.2018;265:298–302.DOI: 10.1016/j.psychres.2018.04.055.PMID:29778050
36.McNairDM,FrankenthalerLM,CzerlinskyT,WhiteTW,SassonS,FisherS.Simulatedpublicspeakingasamodelofclinicalanxiety.Psychopharmacology (Berl).1982;77(1):7–10.DOI: 10.1007/BF00436092.PMID:6126900
37.JacobsDS,MoghaddamB.Medialprefrontalcortexencodingofstressand anxiety.IntRevNeurobiol.2021;158:29–55.DOI: 10.1016/bs.irn.2020.11.014 PMID:33785149
38.LaubachM,AmaranteLM,SwansonK,WhiteSR.What,ifanything,isrodent prefrontalcortex?eNeuro.2018;5(5):ENEURO.0315-18.2018.DOI: 10.1523/ ENEURO.0315-18.2018.PMID:30406193;PMCID: PMC6220587
39.VertesRP.Differentialprojectionsoftheinfralimbicandprelimbiccortexinthe rat.Synapse.2004;51(1):32–58.DOI: 10.1002/syn.10279.PMID:14579424
40.StevensonCW.Roleofamygdala–prefrontalcortexcircuitryinregulatingthe expressionofcontextualfearmemory.NeurobiolLearnMem.2011;96(2):315–23.DOI: 10.1016/j.nlm.2011.06.005.PMID:21689772
41.CourtinJ,ChaudunF,RozeskeRR,KaralisN,Gonzalez-CampoC,WurtzH,etal. Prefrontalparvalbumininterneuronsshapeneuronalactivitytodrivefear expression.Nature.2014;505(7481):92–6.DOI: 10.1038/nature12755.PMID: 24256726
42.QuirkGJ,RussoGK,BarronJL,LebronK.Theroleofventromedialprefrontal cortexintherecoveryofextinguishedfear.JNeurosci.2000;20(16):6225–31.DOI: 10.1523/JNEUROSCI.20-16-06225.2000.PMID:10934272;PMCID: PMC6772571
43.Do-MonteFH,Manzano-NievesG,Quiñones-LaracuenteK,Ramos-MedinaL, QuirkGJ.Revisitingtheroleofinfralimbiccortexinfearextinctionwithoptogenetics.JNeurosci.2015;35(8):3607–15.DOI: 10.1523/JNEUROSCI.313714.2015.PMID:25716859;PMCID: PMC4339362
44.BishopSJ.Traitanxietyandimpoverishedprefrontalcontrolofattention.Nat Neurosci.2009;12(1):92–8.DOI: 10.1038/nn.2242.PMID:19079249
45.ParkJ,WoodJ,BondiC,DelArcoA,MoghaddamB.Anxietyevokeshypofrontalityanddisruptsrule-relevantencodingbydorsomedialprefrontalcortexneu-
rons.JNeurosci2016;36(11):3322–35.DOI: 10.1523/JNEUROSCI.4250-15. 2016.PMID:26985040;PMCID: PMC4792942
46.ParkJ,MoghaddamB.Impactofanxietyonprefrontalcortexencoding ofcognitiveflexibility.Neuroscience.2017;345:193–202.DOI: 10.1016/j. neuroscience.2016.06.013.PMID:27316551;PMCID: PMC5159328
47.LikhtikE,StujenskeJM,TopiwalaMA,HarrisAZ,GordonJA.Prefrontalentrainmentofamygdalaactivitysignalssafetyinlearnedfearandinnateanxiety.Nat Neurosci.2014;17(1):106–13.DOI: 10.1038/nn.3582.PMID:24241397;PMCID: PMC4035371
48.ViaE,FullanaMA,GoldbergX,Tinoco-GonzálezD,Martínez-ZalacaínI,SorianoMasC,etal.Ventromedialprefrontalcortexactivityandpathologicalworry ingeneralisedanxietydisorder.BrJPsychiatry.2018;213(1):437–43.DOI: 10.1192/bjp.2018.65.PMID:29739481
49.ChenY,HuN,YangJ,GaoT.Prefrontalcorticalcircuitsinanxietyandfear:an overview.FrontMed.2022;16(4):518–39.DOI: 10.1007/s11684-022-0941-2 PMID:35943704
50.JanakPH,TyeKM.Fromcircuitstobehaviourintheamygdala.Nature. 2015;517(7534):284–92.DOI: 10.1038/nature14188.PMID:25592533;PMCID: PMC4565157
51.LeDouxJ.Theamygdala.CurrBiol.2007;17(20):R868–74.DOI: 10.1016/j.cub. 2007.08.005.PMID:17956742
52.GoosensKA,MarenS.NMDAreceptorsareessentialfortheacquisition,but notexpression,ofconditionalfearandassociativespikefiringinthelateralamygdala.EurJNeurosci.2004;20(2):537–48.DOI: 10.1111/j.1460-9568. 2004.03513.x.PMID:15233763
53.VivianiD,CharletA,vandenBurgE,RobinetC,HurniN,AbatisM,etal.Oxytocin selectivelygatesfearresponsesthroughdistinctoutputsfromthecentral amygdala.Science.2011;333(6038):104–7.DOI: 10.1126/science.1201043 PMID:21719680
54.JünglingK,SeidenbecherT,SosulinaL,LestingJ,SanghaS,ClarkSD,etal. NeuropeptideS-mediatedcontroloffearexpressionandextinction:roleofintercalatedGABAergicneuronsintheamygdala.Neuron.2008;59(2):298–310. DOI: 10.1016/j.neuron.2008.07.002.PMID:18667157;PMCID: PMC2610688
55.GoosensKA,MarenS.Contextualandauditoryfearconditioningaremediated bythelateral,basal,andcentralamygdaloidnucleiinrats.LearnMem.2001; 8(3):148–55.DOI: 10.1101/lm.37601.PMID:11390634;PMCID: PMC311374
56.TyeKM,PrakashR,KimSY,FennoLE,GrosenickL,ZarabiH,etal.Amygdalacircuitrymediatingreversibleandbidirectionalcontrolofanxiety.Nature.2011;471(7338):358–62.DOI: 10.1038/nature09820.PMID:21389985; PMCID: PMC3154022
57.EtkinA,PraterKE,SchatzbergAF,MenonV,GreiciusMD.Disruptedamygdalar subregionfunctionalconnectivityandevidenceofacompensatorynetworkin generalizedanxietydisorder.ArchGenPsychiatry.2009;66(12):1361–72.DOI: 10.1001/archgenpsychiatry.2009.104.PMID:19996041
58.ShinLM,LiberzonI.Theneurocircuitryoffear,stress,andanxietydisorders. Neuropsychopharmacology.2010;35(1):169–91.DOI: 10.1038/npp.2009.83 PMID:19625997;PMCID: PMC3055419
59.MoserMB,MoserEI.Functionaldifferentiationinthehippocampus.Hippocampus.1998;8(6):608–19.DOI: 10.1002/(SICI)1098-1063(1998)8:6 608::AIDHIPO3 3.0.CO;2-7.PMID:9882018
60.KimJJ,FanselowMS.Modality-specificretrogradeamnesiaoffear.Science. 1992;256(5057):675–7.DOI: 10.1126/science.1585183.PMID:1585183
61.Terreros-RoncalJ,Flor-GarcíaM,Moreno-JiménezEP,Rodríguez-MorenoCB, Márquez-ValadezB,Gallardo-CaballeroM,etal.Methodstostudyadulthippocampalneurogenesisinhumansandacrossthephylogeny.Hippocampus.2022;33(4):271.DOI: 10.1002/hipo.23474.PMID:36259116;PMCID: PMC7614361
62.GandhiS,GuptaJ,TripathiPP.Thecuriouscaseofhumanhippocampalneurogenesis.ACSChemNeurosci.2019;10(3):1131–2.DOI: 10.1021/acschemneuro. 9b00063.PMID:30724553
63.Tunc-OzcanE,PengCY,ZhuY,DunlopSR,ContractorA,KesslerJA.Activatingnewbornneuronssuppressesdepressionandanxiety-likebehaviors. NatCommun.2019;10(1):3768.DOI: 10.1038/s41467-019-11641-8.PMID: 31434877;PMCID: PMC6704083
64.FanselowMS,DongHW.Arethedorsalandventralhippocampusfunctionally distinctstructures?Neuron.2010;65(1):7–19.DOI: 10.1016/j.neuron.2009.11. 031.PMID:20152109;PMCID: PMC2822727
65.CorcoranKA,MarenS.Hippocampalinactivationdisruptscontextualretrieval offearmemoryafterextinction.JNeurosci.2001;21(5):1720–6.DOI: 10.1523/ JNEUROSCI.21-05-01720.2001.PMID:11222661;PMCID: PMC6762930
66.PereiraLM,deCastroCM,GuerraLTL,QueirozTM,MarquesJT,PereiraGS. Hippocampusandprefrontalcortexmodulationofcontextualfearmemoryisdissociatedbyinhibitingdenovotranscriptionduringlateconsolidation.MolNeurobiol.2019;56(8):5507–19.DOI: 10.1007/s12035-018-1463-4 PMID:30623374
67.AdhikariA,TopiwalaMA,GordonJA.Synchronizedactivitybetweentheventralhippocampusandthemedialprefrontalcortexduringanxiety.Neuron. 2010;65(2):257–69.DOI: 10.1016/j.neuron.2009.12.002.PMID:20152131; PMCID: PMC2822726
68.KjelstrupKG,TuvnesFA,SteffenachHA,MurisonR,MoserEI,MoserMB.Reducedfearexpressionafterlesionsoftheventralhippocampus.ProcNatl AcadSciUSA.2002;99(16):10825–30.DOI: 10.1073/pnas.152112399.PMID: 12149439;PMCID: PMC125057
69.BremnerJD,VythilingamM,VermettenE,SouthwickSM,McGlashanT,Nazeer A,etal.MRIandPETstudyofdeficitsinhippocampalstructureandfunctioninwomenwithchildhoodsexualabuseandposttraumaticstressdisorder. AmJPsychiatry.2003;160(5):924–32.DOI: 10.1176/appi.ajp.160.5.924.PMID: 12727697
70.BremnerJD,OrtegoRV,CampanellaC,NyeJA,DavisLL,FaniN,etal.NeuralcorrelatesofPTSDinwomenwithchildhoodsexualabusewithandwithoutPTSD andresponsetoparoxetinetreatment:aplacebo-controlled,double-blind trial.JAffectDisordRep.2023;14:100615.DOI: 10.1016/j.jadr.2023.100615 PMID:38088987;PMCID: PMC10715797
71.ChaJ,GreenbergT,SongI,SimpsonHB,PosnerJ,Mujica-ParodiLR.Abnormalhippocampalstructureandfunctioninclinicalanxietyandcomorbiddepression.Hippocampus.2016;26(5):545–53.DOI: 10.1002/hipo.22566.PMID: 26743454;PMCID: PMC4837065
72.GaddumJH.Tryptaminereceptors.JPhysiol.1953;119(2–3):363–8.DOI: 10.1113/jphysiol.1953.sp004851.PMID:13035757;PMCID: PMC1392807
73.GaddumJH,PicarelliZP.Twokindsoftryptaminereceptor.BrJPharmacolChemother.1957;12(3):323–8.DOI: 10.1111/j.1476-5381.1957.tb00142. x.PMID:13460238;PMCID: PMC1509685
74.MarinP,BécamelC,Chaumont-DubelS,VandermoereF,BockaertJ,Claeysen S.Classificationandsignalingcharacteristicsof5-HTreceptors:towardthe conceptof5-HTreceptosomes.HandbookofBehavioralNeuroscience.London, UnitedKingdom:Elsevier;2020.p.91–120.
75.HalberstadtAL,NicholsDE.Serotoninandserotoninreceptorsinhallucinogen action.HandbookofBehavioralNeuroscience.London,UnitedKingdom:Elsevier;2020.p.843–63.
76.WeberET,AndradeR.Htr2ageneand5-HT(2A)receptorexpressioninthecerebralcortexstudiedusinggeneticallymodifiedmice.FrontNeurosci.2010;4:36. DOI: 10.3389/fnins.2010.00036.PMID:20802802;PMCID: PMC2928707
77.AndradeR.Serotonergicregulationofneuronalexcitabilityintheprefrontal cortex.Neuropharmacology.2011;61(3):382–6.DOI: 10.1016/j.neuropharm. 2011.01.015.PMID:21251917;PMCID: PMC3110517
78.BlierP,deMontignyC.Electrophysiologicalinvestigationoftheadaptiveresponseofthe5-HTsystemtotheadministrationof5-HT1Areceptoragonists. JCardiovascPharmacol.1990;(15Suppl7):S42–48.PMID:1702486
79.DiGiovanniG,ChagraouiA,BharatiyaR,DeDeurwaerdèreP.Serotonergiccontrolofexcitability:fromneurontonetworks.HandbookofBehavioralNeuroscience.London,UnitedKingdom:Elsevier;2020.p.197–215.
80.KiaHK,MiquelMC,BrisorgueilMJ,DavalG,RiadM,ElMestikawyS,etal.Immunocytochemicallocalizationofserotonin1Areceptorsintheratcentralnervoussystem.JCompNeurol.1996;365(2):289–305.DOI: 10.1002/(SICI)10969861(19960205)365:2 289::AID-CNE7 3.0.CO;2-1.PMID:8822171
81.SantanaN.Expressionofserotonin1aandserotonin2areceptorsinpyramidalandGABAergicneuronsoftheratprefrontalcortex.CerebCortex. 2004;14(10):1100–9.DOI: 10.1093/cercor/bhh070.PMID:15115744
82.DeakinJF,GraeffFG.5-HTandmechanismsofdefence.JPsychopharmacol.1991;5(4):305–15.DOI: 10.1177/026988119100500414.PMID: 22282829
83.PaulED,LowryCA.FunctionaltopographyofserotonergicsystemssupportstheDeakin/Graeffhypothesisofanxietyandaffectivedisorders.JPsychopharmacol.2013;27(12):1090–106.DOI: 10.1177/0269881113490328 PMID:23704363
84.WeisstaubNV,ZhouM,LiraA,LambeE,González-MaesoJ,HornungJP, etal.Cortical5-HT2Areceptorsignalingmodulatesanxiety-likebehaviorsin mice.Science.2006;313(5786):536–40.DOI: 10.1126/science.1123432.PMID: 16873667
85.ChristiansonJP,RagoleT,AmatJ,GreenwoodBN,StrongPV,PaulED,etal. 5-Hydroxytryptamine2Creceptorsinthebasolateralamygdalaareinvolvedin theexpressionofanxietyafteruncontrollabletraumaticstress.BiolPsychiatry. 2010;67(4):339–45.DOI: 10.1016/j.biopsych.2009.09.011.PMID:19914601; PMCID: PMC3278236
86.ZhangG,ÁsgeirsdóttirHN,CohenSJ,MunchowAH,BarreraMP,StackmanRW. Stimulationofserotonin2Areceptorsfacilitatesconsolidationandextinction offearmemoryinC57BL/6Jmice.Neuropharmacology.2013;64:403–13.DOI: 10.1016/j.neuropharm.2012.06.007.PMID:22722027;PMCID: PMC3477617
87.StiedlO,MisaneI,SpiessJ,ÖgrenSO.Involvementofthe5-HT1AreceptorsinclassicalfearconditioninginC57BL/6Jmice.JNeurosci.2000;20(22):
8515–27.DOI: 10.1523/JNEUROSCI.20-22-08515.2000.PMID:11069959; PMCID: PMC6773161
88.HolzeF,VizeliP,LeyL,MüllerF,DolderP,StockerM,etal.Acute dose-dependenteffectsoflysergicaciddiethylamideinadouble-blind placebo-controlledstudyinhealthysubjects.Neuropsychopharmacology. 2021;46(3):537–44.DOI: 10.1038/s41386-020-00883-6.PMID:33059356; PMCID: PMC8027607
89.PrellerKH,BurtJB,JiJL,SchleiferCH,AdkinsonBD,StämpfliP,etal.Changes inglobalandthalamicbrainconnectivityinLSD-inducedalteredstatesofconsciousnessareattributabletothe5-HT2Areceptor.Elife.2018;7:e35082.DOI: 10.7554/eLife.35082.PMID:30355445;PMCID: PMC6202055
90.KometerM,SchmidtA,BachmannR,StuderusE,SeifritzE,VollenweiderFX. Psilocybinbiasesfacialrecognition,goal-directedbehavior,andmoodstate towardpositiverelativetonegativeemotionsthroughdifferentserotonergic subreceptors.BiolPsychiatry.2012;72(11):898–906.DOI: 10.1016/j.biopsych. 2012.04.005.PMID:22578254
91.TuetingPA,MetzJ,RhoadesBK,BoutrosNN.PharmacologicchallengeinERP research.AnnNYAcadSci.1992;658(1):223–55.DOI: 10.1111/j.1749-6632. 1992.tb22847.x.PMID:1497260
92.CarterOL,BurrDC,PettigrewJD,WallisGM,HaslerF,VollenweiderFX.Using psilocybintoinvestigatetherelationshipbetweenattention,workingmemory, andtheserotonin1Aand2Areceptors.JCognNeurosci2005;17(10):1497–508.DOI: 10.1162/089892905774597191.PMID:16269092
93.PokornyT,PrellerKH,KraehenmannR,VollenweiderFX.Modulatoryeffectof the5-HT1Aagonistbuspironeandthemixednon-hallucinogenic5-HT1A/2A agonistergotamineonpsilocybin-inducedpsychedelicexperience.EurNeuropsychopharmacol.2016;26(4):756–66.DOI: 10.1016/j.euroneuro.2016.01. 005.PMID:26875114
94.HesselgraveN,TroppoliTA,WulffAB,ColeAB,ThompsonSM.Harnessingpsilocybin:antidepressant-likebehavioralandsynapticactionsofpsilocybinareindependentof5-HT2Ractivationinmice.ProcNatlAcadSci USA.2021;118(17):e2022489118.DOI: 10.1073/pnas.2022489118.PMID: 33850049;PMCID: PMC8092378
95.Pic-TaylorA,daMottaLG,deMoraisJA,JuniorWM,deFátimaAndrade SantosA,CamposLA,etal.Behaviouralandneurotoxiceffectsofayahuasca infusion(BanisteriopsiscaapiandPsychotriaviridis)infemaleWistarrat.BehavProcesses.2015;118:102–10.DOI: 10.1016/j.beproc.2015.05.004.PMID: 26049017
96.CameronLP,BensonCJ,DunlapLE,OlsonDE.EffectsofN,Ndimethyltryptamineonratbehaviorsrelevanttoanxietyanddepression.ACS ChemNeurosci.2018;9(7):1582–90.DOI: 10.1021/acschemneuro.8b00134 PMID:29664276;PMCID: PMC7196340
97.JonesNT,ZahidZ,GradySM,SultanZW,ZhengZ,RazidloJ,etal.Transient elevationofplasmaglucocorticoidssupportspsilocybin-inducedanxiolysisin mice.ACSPharmacolTranslSci.2023;6(8):1221–31.DOI: 10.1021/acsptsci. 3c00123.PMID:37588757;PMCID: PMC10425994
98.FortunatoJJ,RéusGZ,KirschTR,StringariRB,StertzL,KapczinskiF,etal.Acute harmineadministrationinducesantidepressive-likeeffectsandincreases BDNFlevelsintherathippocampus.ProgNeuropsychopharmacolBiolPsychiatry.2009;33(8):1425–30.DOI: 10.1016/j.pnpbp.2009.07.021.PMID:19632287
99.FavaroVM,YonamineM,SoaresJCK,OliveiraMGM.Effectsoflong-term ayahuascaadministrationonmemoryandanxietyinrats.PLoSOne.2015; 10(12):e0145840.DOI: 10.1371/journal.pone.0145840.PMID:26716991;PMCID: PMC4696664
100.CameronLP,BensonCJ,DeFeliceBC,FiehnO,OlsonDE.Chronic,intermittentmicrodosesofthepsychedelicN,N-Dimethyltryptamine(DMT) producepositiveeffectsonmoodandanxietyinrodents.ACSChem Neurosci.2019;10(7):3261–70.DOI: 10.1021/acschemneuro.8b00692.PMID: 30829033;PMCID: PMC6639775
101.NasehiM,Jamshidi-MehrM,KhakpaiF,ZarrindastMR.Possibleinvolvementof CA15-HT1B/1Dand5-HT2A/2B/2Creceptorsinharmaline-inducedamnesia. PharmacolBiochemBehav.2014;125:70–7.DOI: 10.1016/j.pbb.2014.08.007 PMID:25181578
102.LibânioTC,EufrásioRA,NiigakiSS,PeresFF,SilvaRH,ZuardiAW,etal.Harmine impairsmemoryperformanceoftreatedratsandnontreatedcagemates.Exp ClinPsychopharmacol.2022;30(6):751–9.DOI: 10.1037/pha0000525.PMID: 34735205
103.DuY,LiY,ZhaoX,YaoY,WangB,ZhangL,etal.Psilocybinfacilitates fearextinctioninmicebypromotinghippocampalneuroplasticity.ChinMed J(Engl).2023;136(24):2983.DOI: 10.1097/CM9.0000000000002647.PMID: 37000971;PMCID: PMC10752473
104.IshikawaR,FukushimaH,FranklandPW,KidaS.Hippocampalneurogenesisenhancerspromoteforgettingofremotefearmemoryafterhippocampalreactivationbyretrieval.Elife.2016;5:e17464.DOI: 10.7554/eLife.17464.PMID: 27669409;PMCID: PMC5036964
105.SekeresMJ,WinocurG,MoscovitchM,AndersonJAE,PishdadianS,Wojtowicz JM,etal.Changesinpatternsofneuralactivityunderlieatime-dependent transformationofmemoryinratsandhumans.Hippocampus.2018; 28(10):745–64.DOI: 10.1002/hipo.23009.PMID:29989271
106.SuzukiA,FukushimaH,MukawaT,ToyodaH,WuLJ,ZhaoMG,etal.UpregulationofCREB-mediatedtranscriptionenhancesbothshort-andlong-term memory.JNeurosci.2011;31(24):8786–802.DOI: 10.1523/JNEUROSCI.325710.2011.PMID:21677163;PMCID: PMC6622960
107.McLeanCP,LevyHC,MillerML,TolinDF.ExposuretherapyforPTSD:ametaanalysis.ClinPsycholRev.2022;91:102115.DOI: 10.1016/j.cpr.2021.102115. PMID:34954460
108.BurbackL,Brémault-PhillipsS,NijdamMJ,McFarlaneA,VermettenE.Treatmentofposttraumaticstressdisorder:astate-of-the-artreview.CurrNeuropharmacol.2023;22(4):557.DOI: 10.2174/1570159X21666230428091433 PMID:37132142;PMCID: PMC10845104
109.SmidGE,vanderMeerCAI,OlffM,NijdamMJ.Predictorsofoutcomeand residualsymptomsfollowingtrauma-focusedpsychotherapyinpoliceofficers withposttraumaticstressdisorder.JTraumaStress.2018;31(5):764–74.DOI: 10.1002/jts.22328.PMID:30338583
110.BolsoniLM,CrippaJAS,HallakJEC,GuimarãesFS,ZuardiAW.Theanxiolytic effectofcannabidioldependsonthenatureofthetraumawhenpatients withpost-traumaticstressdisorderrecalltheirtriggerevent.BrazJPsychiatry.2022;44(3):298.DOI: 10.1590/1516-4446-2021-2317.PMID:35293520; PMCID: PMC9169481
111.LaniusRA,BrandB,VermettenE,FrewenPA,SpiegelD.Thedissociativesubtypeofposttraumaticstressdisorder:rationale,clinicalandneurobiologicalevidence,andimplications:dissociativesubtypeofPTSD.DepressAnxiety. 2012;29(8):701–8.DOI: 10.1002/da.21889.PMID:22431063
112.LaniusRA,WilliamsonPC,BluhmRL,DensmoreM,BoksmanK,Neufeld RWJ,etal.Functionalconnectivityofdissociativeresponsesinposttraumatic stressdisorder:afunctionalmagneticresonanceimaginginvestigation.Biol Psychiatry.2005;57(8):873–84.DOI: 10.1016/j.biopsych.2005.01.011.PMID: 15820708
113.Ebner-PriemerUW,MauchnikJ,KleindienstN,SchmahlC,PeperM,Rosenthal MZ,etal.Emotionallearningduringdissociativestatesinborderlinepersonalitydisorder.JPsychiatryNeurosci.2009;34(3):214.PMID:19448852;PMCID: PMC2674975
114.RibaJ,RomeroS,GrasaE,MenaE,CarrióI,BarbanojMJ.Increasedfrontaland paralimbicactivationfollowingayahuasca,thepan-Amazonianinebriant.Psychopharmacology(Berl).2006;186(1):93–8.DOI: 10.1007/s00213-006-03587.PMID:16575552
115.Palhano-FontesF,AndradeKC,TofoliLF,SantosAC,CrippaJAS,HallakJEC, etal.Thepsychedelicstateinducedbyayahuascamodulatestheactivityand connectivityofthedefaultmodenetwork.PLoSOne.2015;10(2):e0118143. DOI: 10.1371/journal.pone.0118143.PMID:25693169;PMCID: PMC4334486
116.DolderPC,SchmidY,MüllerF,BorgwardtS,LiechtiME.LSDacutelyimpairs fearrecognitionandenhancesemotionalempathyandsociality.Neuropsychopharmacology.2016;41(11):2638–46.DOI: 10.1038/npp.2016.82.PMID: 27249781;PMCID: PMC5026740
117.MuellerF,LenzC,DolderPC,HarderS,SchmidY,LangUE,etal.Acuteeffects ofLSDonamygdalaactivityduringprocessingoffearfulstimuliinhealthy subjects.TranslPsychiatry.2017;7(4):e1084.DOI: 10.1038/tp.2017.54.PMID: 28375205;PMCID: PMC5416695
118.SanchezTA,RamosLR,AraujoF,SchenbergEE,YonamineM,LoboI,etal.EmotionregulationeffectsofAyahuascainexperiencedsubjectsduringimplicit aversivestimulation:anfMRIstudy.JEthnopharmacol.2024;320:117430.DOI: 10.1016/j.jep.2023.117430.PMID:37979818
119.RossiGN,RochaJM,OsórioFL,BousoJC,OnaG,SilveiraGDO,etal.Interactive effectsofayahuascaandcannabidiolinsocialcognitioninhealthyvolunteers: apilot,proof-of-concept,feasibility,randomized-controlledtrial.JClinPsychopharmacol.2023;43(4):339–49.DOI: 10.1097/JCP.0000000000001691 PMID:37335211
120.RochaJM,RossiGN,DeLimaOsórioF,BousoJC,DeOliveiraSilveiraG,Yonamine M,etal.Effectsofayahuascaontherecognitionoffacialexpressionsofemotionsinnaivehealthyvolunteers:apilot,proof-of-concept,randomizedcontrolledtrial.JClinPsychopharmacol.2021;41(3):267–74.DOI: 10.1097/JCP. 0000000000001396.PMID:33843820
121.BousoJC,GonzálezD,FondevilaS,CutchetM,FernándezX,BarbosaPCR, etal.Personality,psychopathology,lifeattitudesandneuropsychologicalperformanceamongritualusersofayahuasca:alongitudinalstudy.PLoSOne. 2012;7(8):e42421.DOI: 10.1371/journal.pone.0042421.PMID:22905130; PMCID: PMC3414465
122.SantosRG,Landeira-FernandezJ,StrassmanRJ,MottaV,CruzAPM.Effects ofayahuascaonpsychometricmeasuresofanxiety,panic-likeandhopeless-
nessinSantoDaimemembers.JEthnopharmacol.2007;112(3):507–13.DOI: 10.1016/j.jep.2007.04.012.PMID:17532158
123.AicherHD,MuellerMJ,DornbiererDA,SuayD,ElsnerC,WickiI,etal.Potential therapeuticeffectsofanayahuasca-inspiredN,N-DMTandharmineformulation:acontrolledtrialinhealthysubjects.FrontPsychiatry.2024;14:1302559. DOI: 10.3389/fpsyt.2023.1302559.PMID:38264636;PMCID: PMC10804806
124.LiuF,WuJ,GongY,WangP,ZhuL,TongL,etal.Harmineproduces antidepressant-likeeffectsviarestorationofastrocyticfunctions.ProgNeuropsychopharmacolBiolPsychiatry.2017;79:258–67.DOI: 10.1016/j.pnpbp. 2017.06.012.PMID:28625859
125.deAlmeidaRN,deMenezesGalvãoAC,daSilvaFS,SantosSilvaEAD,PalhanoFontesF,Maia-de-OliveiraJP,etal.Modulationofserumbrain-derivedneurotrophicfactorbyasingledoseofayahuasca:observationfromarandomizedcontrolledtrial.FrontPsychol.2019;10:1234.DOI: 10.3389/fpsyg.2019. 01234.PMID:31231276;PMCID: PMC6558429
126.ChoJH,DeisserothK,BolshakovVY.Synapticencodingoffearextinction inmPFC-amygdalacircuits.Neuron.2013;80(6):1491–507.DOI: 10.1016/j. neuron.2013.09.025.PMID:24290204;PMCID: PMC3872173
127.SantiniE,MullerRU,QuirkGJ.ConsolidationofExtinctionLearningInvolvesTransferfromNMDA-IndependenttoNMDA-DependentMemory.JNeurosci.2001;21(22):9009.DOI: 10.1523/JNEUROSCI.21-22-09009.2001.PMID: 11698611;PMCID: PMC6762277
128.PetersJ,Dieppa-PereaLM,MelendezLM,QuirkGJ.Inductionoffearextinction withhippocampal-infralimbicBDNF.Science.2010;328(5983):1288–90.DOI: 10.1126/science.1186909.PMID:20522777;PMCID: PMC3570764
129.BloodgoodDW,SugamJA,HolmesA,KashTL.Fearextinctionrequiresinfralimbiccortexprojectionstothebasolateralamygdala.TranslPsychiatry. 2018;8(1):1–11.DOI: 10.1038/s41398-018-0106-x.PMID:29507292;PMCID: PMC5838104
130.VaidyaVA,MarekGJ,AghajanianGK,DumanRS.5-HT2Areceptor-mediated regulationofbrain-derivedneurotrophicfactormRNAinthehippocampusand theneocortex.JNeurosci.1997;17(8):2785–95.DOI: 10.1523/JNEUROSCI.1708-02785.1997.PMID:9092600;PMCID: PMC6573109
131.Morales-GarciaJA,Calleja-CondeJ,Lopez-MorenoJA,Alonso-GilS,SanzSanCristobalM,RibaJ,etal.N,N-dimethyltryptaminecompoundfoundinthe hallucinogenicteaayahuasca,regulatesadultneurogenesisinvitroandinvivo. TranslPsychiatry.2020;10(1):331.DOI: 10.1038/s41398-020-01011-0.PMID: 32989216;PMCID: PMC7522265
132.AghajanianGK,FooteWE,SheardMH.Lysergicaciddiethylamide:sensitive neuronalunitsinthemidbrainraphe.Science.1968;161(3842):706–8.DOI: 10.1126/science.161.3842.706.PMID:4874578
133.LowryCA,HollisJH,deVriesA,PanB,BrunetLR,HuntJRF,etal.Identification ofanimmune-responsivemesolimbocorticalserotonergicsystem:potential roleinregulationofemotionalbehavior.Neuroscience.2007;146(2):756–72.DOI: 10.1016/j.neuroscience.2007.01.067.PMID:17367941;PMCID: PMC1868963
134.GraeffFG,QuinteroS,GrayJA.Medianraphestimulation,hippocampalthetarhythmandthreat-inducedbehavioralinhibition.PhysiolBehav. 1980;25(2):253–61.DOI: 10.1016/0031-9384(80)90213-9.PMID:6447883
135.Carhart-HarrisR,NuttD.Serotoninandbrainfunction:ataleoftworeceptors. JPsychopharmacol2017;31(9):1091–120.DOI: 10.1177/0269881117725915 PMID:28858536;PMCID: PMC5606297
Publisher’snote: GenomicPressmaintainsapositionofimpartialityandneutrality regardingterritorialassertionsrepresentedinpublishedmaterialsandaffiliations ofinstitutionalnature.Assuch,wewillusetheaffiliationsprovidedbytheauthors, withouteditingthem.Suchusesimplyreflectswhattheauthorssubmittedtousand itdoesnotindicatethatGenomicPresssupportsanytypeofterritorialassertions.
OpenAccess. ThisarticleislicensedtoGenomicPressundertheCreativeCommonsAttribution-NonCommercial-NoDerivatives4.0InternationalLicense(CCBY-NC-ND4.0).Thelicensemandates:(1)Attribution:Credit mustbegiventotheoriginalwork,withalinktothelicenseandnotificationofany changes.Theacknowledgmentshouldnotimplylicensorendorsement.(2)NonCommercial:Thematerialcannotbeusedforcommercialpurposes.(3)NoDerivatives: Modifiedversionsoftheworkcannotbedistributed.(4)Noadditionallegalortechnologicalrestrictionsmaybeappliedbeyondthosestipulatedinthelicense.Public domainmaterialsorthosecoveredbystatutoryexceptionsareexemptfromthese terms.Thislicensedoesnotcoverallpotentialrights,suchaspublicityorprivacy rights,whichmayrestrictmaterialuse.Third-partycontentinthisarticlefallsunderthearticle’sCreativeCommonslicenseunlessotherwisestated.Ifuseexceeds thelicensescopeorstatutoryregulation,permissionmustbeobtainedfromthe copyrightholder.Forcompletelicensedetails,visit https://creativecommons.org/ licenses/by-nc-nd/4.0/.Thelicenseisprovidedwithoutwarranties.

OPEN RESEARCHREPORT
Anestimateofthenumberofpeople withclinicaldepressioneligiblefor psilocybin-assistedtherapyinthe UnitedStates
SyedF.Rab1 ,CharlesL.Raison2 ,andElliotMarseille3
1 EmoryUniversitySchoolofMedicine,Atlanta,GA30322,USA
2 UniversityofWisconsin-MadisonSchoolofMedicineandPublicHealth, Madison,WI53707,USA
3 UCBerkeley,CollaborativefortheEconomicsofPsychedelics, Berkeley,CA94720,USA
CorrespondingAuthor: SyedFayzanRab,EmoryUniversitySchoolof Medicine,12ExecutiveParkDriveNortheast,Atlanta,GA30329,USA.
Email: Syed.f.rab@emory.edu
Psychedelics March2025;1(2):26–30; doi: https://doi.org/10.61373/pp024r.0025
Thisstudyaimstoestimatethelower,middle,andupperboundsofpotentialdemandforpsilocybin-assistedtherapy(PSIL-AT)formajordepressivedisorder(MDD)andtreatment-resistantdepression(TRD)in theUnitedStates.WecalculatedpotentialPSIL-ATdemandforMDD andTRDbyestimatingthenumberofU.S.patientswithMDD,identifyingthoseintreatment,anddeterminingwhoqualifiesashaving TRD.Weestablishedarangeofestimatesusingtheexclusioncriteria fromthelargesttrialstodateonPSIL-ATforMDDorTRD.Estimates rangedfromlower-boundthroughstringentcriteria,mid-rangebyfocusingonlikelyreal-worldscenarios,toupper-boundbyaccounting fordoublecountingforpatientswithmultiplecomorbidities.AsignificantportionofpatientswithMDDandTRDisineligibleforPSILATduetodisqualifyingconditions.Percentageofpatientswhoare eligibleare24%(lower-bound),56%(mid-range),and62%(upperbound).Variancewaslargelyinfluencedbytheremovalofalcoholand substanceusedisordersasexclusioncriteria,aswellasremovingthe doublecountingfromcomorbidpsychiatricandcardiovascularconditions.Theanalysisoutlinesthepublichealthimplicationsofproviding PSIL-ATforMDDandTRD,emphasizingthattheeffectivedemand willbeshapedbyinsurancecoverage,state-levelregulations,andthe availabilityoftrainedproviders.Thesefindingssuggesttheneedfor carefulpolicyplanningandresourceallocationtoensureequitable accessandeffectiveimplementationofPSIL-ATacrossdiversepopulationsandregions.
Keywords: Psilocybin,depression,exclusioncriteria,psychedelic therapy.
Introduction
Psilocybin-assistedtherapy(PSIL-AT)hasbeendesignatedbytheFood andDrugAdministration(FDA)asbreakthroughtherapyforpatientswith eitheradiagnosisofmajordepressivedisorder(MDD)ortreatmentresistantdepression(TRD)(1).TRDisdefinedashavingatleasttwotreatmentswithantidepressantmedications,atadequatedosesandforan adequatedurationinthecurrentdepressiveepisode,withoutsignificant relieffromsymptomsrelatedtoMDD(2).RecentclinicaltrialshavedefinedinclusionandexclusioncriteriaspecificallyforTRD(3)orMDD(4, 5), thelatterofwhichmayalsoincludepatientswithTRD.AsFDAapproval andsubsequentlegalizationformedicaluseofpsilocybinisnowbeing considered(6),itisimportanttounderstandthepossiblepublichealth
impactfromtheintroductionofPSIL-ATintheUnitedStates.This,inturn, requiresanestimationofthepotentialdemand.Wechosetodefinea clinicallower-bound,mid-range,andupper-boundestimatesofthedemandforPSIL-ATasatreatmentforMDDorTRD.
Results
Asshownin Table1,ofthe14.8millionpeoplewithMDD,9millionare beingtreated,and2.7millionmeetcriteriaforTRD.
Table2 illustratesthepercentageofpatientsdeemedeligiblefor PSIL-AT,accompaniedbycorrespondingestimatesforthenumberofindividualsbeingtreatedforMDDorTRDwhoareeligibleforthistherapeutic approach.
Thelower-boundestimateindicatesonly24%ofpatientswithdepressionwouldmeetstrictclinicaltrialexclusioncriteriaforPSIL-AT.This amountsto2.2millionpatientscurrentlyundergoingtreatmentforMDD or0.6millionpatientswhenconsideringonlythosewithTRD.
Inapplyingexclusioncriterialikelytooperateinreal-worldclinical settings(themid-rangeestimate),weobserveanotableincreaseinthe proportionofincludedpatientsto56%.Applicationofthesemorepermissivecriteriawouldexpandthepoolofeligiblepatientsbeingtreated forMDDorTRDto5.1millionor1.5million,respectively.Theexclusionof alcoholandsubstanceusedisordersaccountsforasignificantportionof thisadjustment,contributingto32%ofthedifference.
Finally,theupper-boundestimate,whichadjustsfordoublecounting betweendifferentmedicalconditions,raisestheestimateto62%ofthe patientpopulationwithdepressionbeingeligibleforPSIL-AT.Thistranslatesto5.6millionindividualsand1.7millioneligibleforPSIL-ATwhen consideringMDDandTRD,respectively.Thisadjustedincreaseisprimarily attributedtotheco-occurrenceofcardiovascularandpsychiatriccomorbidities,witheachcontributingtoa3%–4%increaseineligiblepatients.
Inadditiontoourbaseestimates,weconductedasensitivityanalysistoevaluatetheimpactofvaryingassumptionsontheoveralldemand projectionsforPSIL-AT.Specifically,weassignedbetadistributionswith arangeofplusorminus50%ofthebaselinevaluestoeachofthecomorbidityprevalenceestimatesshownincolumn3of Table2.Using@RISK (PalisadeCorporation,version8.1.1)software,wesimulatedtheoverall uncertaintyinthefinalestimatesofthenumberofpatientseligiblefor PSIL-ATamongthosewithMDDandTRD.
Theresultsofthesensitivityanalysisaredepictedin Figures1 and 2. ForpatientswithMDD,theanalysisproduceda95%confidenceinterval (CI)of4.7millionto6.6millioneligibleindividuals,whileforpatientswith TRD,the95%CIrangedfrom1.4millionto1.9million.Theserangeshighlightthepotentialvariabilityinourestimatesbasedonchangesinthe assumptionsunderlyingcomorbidityprevalence,emphasizingboththe robustnessandtheuncertaintyinherentinourprojections.
Discussion
Thisanalysisoutlinesthedimensionsofthepublichealthimplicationsof providingPSIL-ATforthetreatmentofMDDandTRD.Ourestimatesof
Table1. Estimatesofnumberofpeoplewhowouldqualifyashaving MDD,thoseintreatment,andthosewhohaveTRD
Received:2May2024.Revised:12August2024and27August2024and29August2024.Accepted:29August2024. Publishedonline:13September2024.
Table2. PrevalenceofdisqualifyingcomorbiditiesinthelargestclinicaltrialsutilizingPSIL-ATforMDDorTRDwithnumberofpatientseligible
PrevalenceofdisqualifyingcomorbidityinpatientswithMDDor TRDaccordingto:
Disqualifyingcomorbidities
Trialswith thisexclusion criterion
1.Trialexclusioncriteria1 CI(ConfidenceInterval),OR (OddsRatio),SE(Standard Error) 2.Real-world exclusion criteria
3.Real-world exclusioncriteria adjustedfor comorbid conditions2 , 3
Psychoticormanicdisorder(3–5)19%(8)19%(8)23.2%(9)
Suicideattemptinthepastyear8.0%[95%CI=(3–14%)](10)8.0%(10)
Diabetes,uncontrolled(5)2.9%[OR=1.4(1.4–1.5)](11, 12)2.9%(11, 12)8.0%(13, 14)
Stroke(3–5)1.9%[OR=2.4(2.0–2.8)](11)1.9%(11)
Heartattackinlastyear(3–5)2.7%[OR=0.9(0.8–1.1)](11)2.7%(11)
BP140+/90+,treatment-resistant2.0%[OR=1.4(1.3–1.4)](11, 15)2.0%(11, 15)
Epilepsy3.7%[OR=2.6(2.3–3.0)](11)3.7%(11)3.7%(16)
Personalitydisorder(4)2.2%[SE=.36](16)2.2%(17)2.2%(11)
Hepaticimpairment(Child-Pugh > 7)4 (5)1.8%[SE=.10](18)1.8%(18)1%(17)
Alcoholdependence(3–5)20.0%(19)–Drugdependence12.0%(19)––
Othercardiacconditions(LongQT,cardiac hypertrophy,heartfailure,tachycardiaatrest, atrialfibrillation,prostheticvalve)
Pregnancy UnwillingnesstodiscontinueSSRIs–––
Unwillingorunabletodiscontinueformal psychotherapy
Haveusedpsychedelicsinthepast5years;have usedpsychedelics10+ timesinthepast
Have1stdegreerelativewithpsychoticdisorder orbipolardisorder
ReceivedECTorTMSinthepast90days(5)–––
Percentageofpatientswhowouldbeineligible forPSIL-AT
PercentageandnumberofpatientswithMDDandTRDeligibleforPSIL-AT
PercentageofpatientseligibleforPSIL-AT–24%56%62%
NumberofpatientsbeingtreatedforMDDwho areeligibleforPSIL-AT
NumberofpatientsbeingtreatedforTRDwho areeligibleforPSIL-AT
1 Whereavailable,confidenceintervals,oddsratios,andstandarderrorswerereported.
2 Double-countingcalculationsusedprevalenceestimatesfromthegeneralpopulationandarenotMDD-specific.
3 Forsensitivityanalysis,eachcomorbiditywasassignedabetadistributionwithalphaandbetaparametersof2andmaximum/minimumvaluesof +/ 50%
4 HepaticimpairmentestimatescamefromthegeneralpopulationandarenotMDD-specific.
demandaresubjecttocontingenciespendingFDAdecisionaroundPSILAT.Onepossibilitythatcouldelevatedemandbeyondourprojections involvesoff-labeluseofPSIL-ATforconditionsotherthandepression. Evidencefrompsychiatricprescriptionpracticessuggeststhatpsychiatric medicationsareusedtotreatarangeofconditionsoutsidetheiroriginalFDA-approvedindication.Aretrospectiveanalysis,forexample,revealedthat91%ofpatientscurrentlyprescribedantidepressantswould notmeetrandomizedclinicaltrialseligibilitybasedontheirmedicalstatus(20).ThisdiscrepancysuggeststhattheeligibilityforPSIL-ATmight besignificantlyhigherthanourestimatesifPSIL-ATisusedtotreat othermedicalconditionssuchasanxietydisorders,chronicpain,and otherpsychiatricdisorders,eitheroff-labelorfollowingeventualFDA approvalfortheseconditions.Weareawareofnoreliabledatathat wouldallowustoestimatecurrentandespeciallyfutureprevalenceof treatmentseeking,whichintroducesfurthercomplexityintoourdemand projections.
Conversely,otherpsychedelicsgrantedFDAbreakthroughstatussuch aslysergicaciddiethylamideforgeneralanxietydisorder(21)maybe
usedoff-labelinthefuturetotreatpatientswithMDDorTRDgivenhigh comorbiditybetweentheseconditions(22).Iftheseotherpsychedelics aregivenFDAapprovalinthefuture,thedemandestimatewouldneed tobemodifiedtodistributeacrosstherelativeuptakeofallpsychedelics thathavetherapeuticeffectsondepression.
Additionally,therearecountervailingpracticalconsiderationsfor PSIL-ATwhicharelikelytoconstraineffectivedemandtolevelslowerthan ourestimates.Theseincludetheavailabilityoftrainedproviders,geographicalaccesstotherapy,andpatientpreferencesrelatedtocost,treatmentduration,andculturalacceptability.Forexample,patientslivingin urbancentersarelikelytohavegreateraccesstoPSIL-ATfacilitiesand therapists,whileruralareasmaylacksufficienttrainedprofessionalsand infrastructureforeffectiveadministration.StatesthathavealreadylegalizedpsychedelictherapieslikeOregonandColoradomayasymmetrically dominatedemandintheshort-termwhileotherstatesworkthroughestablishingtheirownregulatoryframeworkforPSIL-AT.
Recentclinicaltrialshaveevaluatedpsilocybin’seffectivenessasboth monotherapyfordepression(3, 4),andasanadjuncttoestablished
Figure1. PatientsbeingtreatedforMDDwhoareeligibleforPSIL-AT.Multivariatesensitivityanalyses,20,0000iterations.
antidepressantregimens(2, 23).Ina2020article,Luo etal. reportedthat 70%ofindividualswithMDDutilizeantidepressants(24).Therefore,if FDAapprovalofPSIL-ATforMDDrestrictsittomonotherapy,itsapplicabilitywouldbesignificantlynarrowed,givenevidencesuggestingthat nearlyhalfofpatientsattemptingtotaperoffpsychotropicdrugsface difficultiesincompletelystoppingtheirmedication(25).
HeterogeneityinthewaysstateschoosetoimplementPSIL-ATwill alsoimpacteffectivedemand.ExistinglegalizationeffortsinColorado andOregonmayserveasamodelforhowPSIL-ATisrolledoutnationwidepost-FDAapproval.Colorado’sNaturalMedicineHealthAct,forexample,mandatesthatlicensedfacilitatorsrefrainfromtreatingpatients withmanyofthecomorbiditiesdiscussedinthispaper(26).However, patientsmaygetclearancefromamedicalprofessionaltoproceedwith psychedelictherapydespiteexclusionaryconditions(26).Whetherstates choosetofollowColoradoorOregon’sexampleorimplementtheirown regulationsisunknownandmakesdemandestimationdifficult.
Perhapsmostimportantly,theprospectivedemandwillbeshapedby theextenttowhichinsurers,bothpublicandprivate,includePSIL-AT intheircoverageschemes.Medicaidisthelargesthealthcarepayerin theUnitedStates.Itcovered85millionlow-incomebeneficiariesin2023 (27)and18%–20%ofitsbeneficiariesarelikelytohaveclinicaldepression(28).Thus,decisionsMedicaidmakesregardingtheconditionsunder whichPSIL-ATservicesaremadeavailableandreimbursedwillbeparticularlyimportantindeterminingeffectivedemand.Ultimately,whether PSIL-AThasasignificantimpactonthementalhealthoftheU.S.populationdependsonthedecisionsofpublicandprivatethird-partypayers, andMedicaidisthesinglemostimportantamongthem.
Therangeofeligibilityestimates(24%–62%)highlightstheneedfor flexiblehealthcareplanningandresourceallocationstrategies.Policymakersandhealthcareprovidersmustprepareforthisvariabilitybyensuringthatsufficientresources—includingtrainedtherapists,facilities,
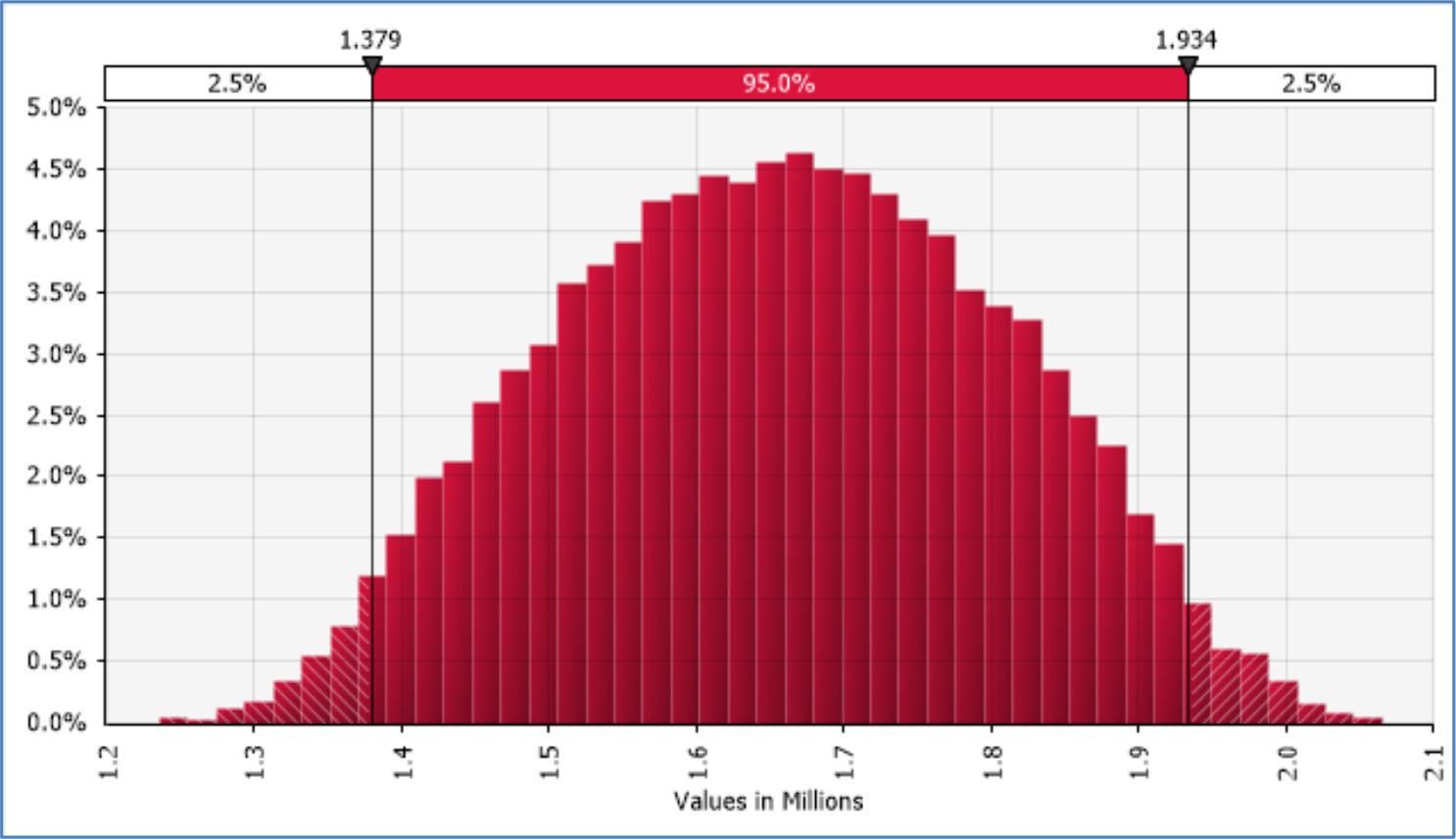
andfinancialsupport—areavailabletomeetdemandundervariousscenarios.ThisflexibilitywillbecrucialasmoredatabecomesavailablepostFDAapproval,allowingforadjustmentsinresourcedistributionandensuringequitableaccesstoPSIL-ATacrossdiversepopulationsandregions. Thisstudyservesasabasisforpolicymakers,healthcarepayers,and pharmaceuticalcompaniestogaugethepotentialpublichealthimpactof PSIL-ATpendingFDAapproval.Asthefieldprogresses,furtherresearchis warrantedtoexplorepsilocybin’stherapeuticrange,includingitsapplicationtoabroaderarrayofmentalhealthconditionsanditsintegration intononclinicalsettings.Futurestudiesshouldfocusonregionalanddemographicvariations,theroleofstateregulations,andculturalattitudes towardpsychedelictherapies.Additionally,longitudinalstudiestracking thereal-worldimplementationofPSIL-ATwillbeessentialforassessing howinitialprojectionsalignwithactualdemand,influencingfuturepolicydecisionsandresourceallocationefforts.Suchanalyseswillrefineour understandingofthepotentialpublichealthimpactofpsychedelictherapiesandhelptoguidepolicyandclinicalpractice.
Methods Overview
TocalculatethepotentialdemandforPSIL-ATforTRDandMDDinthe UnitedStates,weestimatedthenumberofpatientswithMDD,identified howmanyofthesepatientsarecurrentlyundergoingtreatment,andfurtherdefinedwhowouldqualifyashavingTRD.Weestablishedarangeof estimates:alower-boundestimatethroughstringentapplicationofexclusioncriteriausedinclinicaltrials;amid-rangeestimatebyconsideringonlyexclusioncriterialikelytoberelevanttoreal-worldclinicalscenarios;andanupper-boundestimatebyrefiningouranalysistoaccount forpatientswithtwoormorecomorbidconditionsinadditiontoMDD. SinceeachcomorbiditywouldexcludepotentialpatientsfromsafelyaccessingPSIL-AT,weeliminatethedoublecountingthatwouldresultfrom co-occurringdisqualifyingconditions.
WeusedanestimateofMDDcasesintheUnitedStatesbasedonthe 2021NationalSurveyonDrugUseandHealth(6).Wethenfocusedon thesubgroupofindividualswhohadreceivedtreatmentfortheirMDDin thepastyearandfurtheradjustedtoestimatethenumberofindividuals whowouldqualifyashavingTRD(1).
Infocusingonindividualscurrentlyundergoingtreatmentfordepression,ourapproachensuresthatdemandestimatesaregroundedinrealworldclinicalsettings,wherePSIL-ATwilllikelybeadministeredshould theyreceiveFDAapproval.Thisallowsustoworkwithapopulationwhose treatment-seekingbehaviorsandclinicalprofilesarewelldocumented, providingareliablefoundationfordemandestimation.Bychoosingthis baseline,wealsoavoidspeculativeassumptionsaboutthefuturebehaviorofuntreatedindividuals(acknowledgingapotentialinfluxpostFDAapproval),ensuringthatourprojectionsremainconservativeand methodologicallyconsistent.Moreover,thisapproachallowsforflexibility,asfutureresearchanddatacollectioncanexpandupontheseestimatesbyincorporatingthepotentialuptakeofPSIL-ATamongcurrently untreatedindividuals.
Aportionofthispatientpopulationfailstomeetclinicaleligibilityfor PSIL-ATduetoadisqualifyingmedicalcondition.Toestimatetheportion ofsuchdisqualifiedpatients,weidentifiedtheclinicalexclusioncriteria fromthelargestclinicaltrialstodateonPSIL-ATforMDDorTRD(3–5)(see AdditionalMaterials).Whereavailable,weincludedconfidenceintervals anderrormarginsfromprevalencedatalookingatdepressionwithdifferentcomorbidities.WeconstructedthreedifferentestimatesofthepotentialdemandforPSIL-ATbasedonthreerespectivesetsofassumptions regardingeligibilityforPSIL-AT:
1.Allpatientswiththeexclusioncriteriausedinclinicaltrials,assuming nocomorbidmedicalconditions.ThisrepresentsthetheoreticallowerboundofpatientswhowouldbeeligibleforPSIL-ATandisrepresented asthecolumnlabeled“1.Trialexclusioncriteria”in Table2
2.Sameas#1butremovingexclusioncriteriathatwouldberelevantina clinicaltrialsettingbutwouldnotapplyinreal-worldclinicalsettings. Thisrepresentsamid-rangeestimateandislabeled“2.Real-world exclusioncriteria”in Table2
Figure2. PatientsbeingtreatedforTRDwhoareeligibleforPSIL-AT.Multivariatesensitivityanalyses,20,0000iterations.
3.Sameas#2butwithfurtheradjustmentfortheprevalenceofcomorbid medicalconditions(e.g.,psychosisandacutesuiciderisk).Thisrepresentsanupper-boundestimateandisrepresentedas“3.Real-world exclusioncriteriaadjustedforcomorbidconditions”in Table2
Weappliedthesesetsofassumptionstwice,topatientswithMDDand topatientswithTRD.
Acrossallestimates,wedidnotgatherprevalencedataonmedicalconditionsthatweretransient(i.e.,pregnancy),modifiablewitha provider(i.e.,taperingofaSSRI),nichewithlittletonoreliableprevalencedataavailableinpatientswithdepression(i.e.,diagnosedpsychosis infirst-degreefamilymembersorcardiacarrythmias),constructsofeffectivestudydesign(i.e.,discontinueexistingpsychotherapyorprevious psychedelicuse),orexperimental(i.e.,deepbrainstimulationorvagal nervestimulation).
Inevaluating“2.Real-worldexclusioncriteria”,weconsideredboth thepharmacologicalmechanismsofpsychedelicagentsandtheclinical insightsofoneofthepaper’sauthors(Raison).Ourpremiseisthatthe neurobiologicaleffectsofpsilocybinwillbethesameinreal-worldclinicalpracticeastheyareintrials,thuswarrantingourinclusionofconditionsknowntobeaffecteddirectlybytheseneurobiologicalmechanisms inourdemandestimation.Theneurologicalmechanismofpsilocybin(29) isthoughttodestabilizeunderlyingmaniaandpsychosis(30),triggerlatentepilepsy(31),andexacerbateacutesuiciderisk(32).PSIL-ATalsoexhibitsunderlyingserotonergiceffectsonthebody(33),whichareknown tocausecardiovascularstressexacerbatingriskofstroke,heartattack,diabeticcomplication,andothersequelaofhypertension(34).Additionally, severeliverdysfunctionmayalterthemetabolismofpsychotropicmedications,necessitatingitsinclusionasacriterionforexclusioninclinical practice(35).
ThebenefitsofPSIL-ATforthetreatmentofpersonalitydisordershave beendiscussedbutarecurrentlyunsubstantiated(35)andwetherefore retainitasanexclusioncriteriainthisanalysis.Weremovedalcoholuse disorderandsubstanceabusedisorderfromourlistofexclusioncriteriabecauseevidencesuggeststhatPSIL-ATcanbebeneficialforpatients withtheseconditions(31, 36).
Toavoiddoublecounting,wethenrefinedtheresultingestimate basedontheprevalenceofcomorbiditybetweenthedifferentexclusionaryconditions.Thisisrepresentedas“3.Real-worldexclusioncriteriaadjustedforcomorbidconditions”in Table2.Whenavailable,weusedthe prevalenceofcomorbidconditionsamongpeoplewithclinicaldepression. Wherethiswasnotpossible,weusedestimatesoftheprevalenceofcomorbidconditionsinthegeneralpopulation.Forexample,the12-month incidenceofsuicideattemptsamongpatientsreportingpsychosisandany otherpsychiatriccondition,inthiscaseclinicaldepression,was47.4%(9). Utilizingthesedata,weadjustedforthepotentialdoublecountingofpatientsineligibleduetobothpsychosisandacutesuiciderisk,resulting inarevisedcombinedprevalenceof23.2%.Similarly,wefoundhighcomorbiditybetweenuncontrolleddiabetes(13),stroke,heartattack,and treatment-resistanthypertension(14)andformulatedatotalestimateof 8.0%.
AuthorContributions
SFR:Conceptualization,Methodology,Formalanalysis,Investigation, Writing–OriginalDraft,Projectadministration. CLR:Writing–Review&Editing,Supervision. EM:Writing–Review&Editing,Supervision. Allauthorsdiscussedtheresultsandcontributedtothefinalmanuscript.
DesignationofCorrespondingAuthorandLeadContact
SFRisdesignatedasthecorrespondingauthorandleadcontactforthis paper.Hehastakenresponsibilityforcoordinatingtheeffort,overseeing thedataintegrity,handlingthesubmissionprocess,andcommunicating withthejournalpre-andpost-publication.SFRensuresthatallauthors haveapprovedthefinalversionofthemanuscriptandadheretoalleditorialandsubmissionpolicies.
ConflictsofInterest
SFRconfirmsthathewasaconsultantatSunstoneTherapies.EMserves asadjunctfacultyatUCBerkeley’sCollaborativefortheEconomicsof
PsychedelicswhichhasreceivedfinancialsupportfromtheUsonaInstitute.CLRdisclosesthatheservesasaconsultantforUsonaInstitute,Otsuka,andNovartis.Therearenootherconflictsofinterestamongtheauthors,andallauthorshavedisclosedanyrelatedworkunderconsiderationelsewhere.
Allauthorshaveagreedtotheorderofauthorship,affirmingtheir contributionstotheworkasdetailedabove.Incaseofanyauthorship disputes,theauthorswillresolvetheminternallywithoutinvolvingthe journaleditorialprocess.
Acknowledgments
Weextendourgratitudetoparticipantsandresearchersinthepsilocybin clinicalstrialsconductedtodate.
FundingSources
Nonewereutilizedforthisproject.
References
1.HealDJ,SmithSL,BelouinSJ,HenningfieldJE.Psychedelics:thresholdofatherapeutic revolution.Neuropharmacology.2023;236:109610.DOI: 10.1016/j.neuropharm.2023. 109610.PMID:37247807
2.GaynesBN,RushAJ,TrivediMH,WisniewskiSR,SpencerD,FavaM.TheSTAR∗D study:treatingdepressionintherealworld.CleveClinJMed.2008;75(1):57–66. DOI: 10.3949/ccjm.75.1.57.PMID:18236731
3.GoodwinGM,AaronsonST,AlvarezO,ArdenPC,BakerA,BennettJC,etal.Singledosepsilocybinforatreatment-resistantepisodeofmajordepression.NEnglJMed. 2022;387(18):1637–48.DOI: 10.1056/NEJMoa2206443.PMID:36322843
4.Carhart-HarrisR,GiribaldiB,WattsR,Baker-JonesM,Murphy-BeinerA,Murphy R,etal.Trialofpsilocybinversusescitalopramfordepression.NEnglJMed. 2021;384(15):1402–11.DOI: 10.1056/NEJMoa2032994.PMID:33852780
5.RaisonCL,SanacoraG,WoolleyJ,HeinzerlingK,DunlopBW,BrownRT,etal.Singledosepsilocybintreatmentformajordepressivedisorder:arandomizedclinicaltrial. JAMA.2023;330(9):843–53.DOI: 10.1001/jama.2023.14530.PMID:37651119;PMCID: PMC10472268
6.MitchellJM,BogenschutzM,LiliensteinA,HarrisonC,KleimanS,Parker-GuilbertK, etal.MDMA-assistedtherapyforseverePTSD:arandomized,double-blind,placebocontrolledphase3study.NatMed.2023;21(3):315–28.DOI: 10.1176/appi.focus. 23021011.PMID:37404971;PMCID: PMC10316215
7.Majordepression.UpdatedJanuary2022.2022[citedMarch30,2023].Availablefrom: https://www.nimh.nih.gov/health/statistics/major-depression
8.OhayonMM,SchatzbergAF.Prevalenceofdepressiveepisodeswithpsychoticfeatures inthegeneralpopulation.AmJPsychiatry.2002;159(11):1855–61.DOI: 10.1176/appi. ajp.159.11.1855.PMID:12411219
9.DeVylderJE,LukensEP,LinkBG,LiebermanJA.Suicidalideationandsuicideattemptsamongadultswithpsychoticexperiences:datafromthecollaborativepsychiatricepidemiologysurveys.JAMAPsychiatry.2015;72(3):219–25.DOI: 10.1001/ jamapsychiatry.2014.2663.PMID:25715312
10.DongM,ZengL-N,LuL,LiXH,Ungvari,GS,NgCH,etal.Prevalenceofsuicideattemptinindividualswithmajordepressivedisorder:ameta-analysisofobservational surveys.PsycholMed 2019;49(10):1691–704.DOI: 10.1017/S0033291718002301 PMID:30178722
11.SchoepfD,UppalH,PotluriR,ChandranS,HeunR.Comorbidityanditsrelevance ongeneralhospitalbasedmortalityinmajordepressivedisorder:anaturalistic 12-yearfollow-upingeneralhospitaladmissions.JPsychiatrRes.2014;52:28–35. DOI: 10.1016/j.jpsychires.2014.01.010.PMID:24513499
12.LiuL,WangF,GracelyEJ,MooreK,MellyS,ZhangF,SatoPY,EisenHJ.Burdenofuncontrolledhyperglycemiaanditsassociationwithpatientscharacteristicsandsocioeconomicstatusinphiladelphia,USA.HealthEquity.2020;4(1):525–32.DOI: 10.1089/ heq.2020.0076.PMID:34095699;PMCID: PMC8175259
13.EinarsonTR,AcsA,LudwigC,PantonUH.Prevalenceofcardiovasculardiseaseintype2 diabetes:asystematicliteraturereviewofscientificevidencefromacrosstheworldin 2007–2017.CardiovascDiabetol.2018;17(1):83.DOI: 10.1186/s12933-018-0728-6 PMID:29884191;PMCID: PMC5994068
14.CardosoCRL,SallesGF.Refractoryhypertensionandrisksofadversecardiovascular eventsandmortalityinpatientswithresistanthypertension:aprospectivecohort study.JAmHeartAssoc.2020;9(17):e017634.DOI: 10.1161/JAHA.120.017634.PMID: 32851922;PMCID: PMC7660786
15.CareyRM,SakhujaS,CalhounDA,WheltonPK,MuntnerP.Prevalenceofapparenttreatment-resistanthypertensionintheUnitedStates.Hypertension. 2019;73(2):424–31.DOI: 10.1161/HYPERTENSIONAHA.118.12191.PMID:30580690; PMCID: PMC6693520
16.HasinDS,GoodwinRD,StinsonFS,GrantBF.Epidemiologyofmajordepressivedisorder:resultsfromthenationalepidemiologicsurveyonalcoholismandrelatedconditions.ArchGenPsychiatry.2005;62(10):1097–106.DOI: 10.1001/archpsyc.62.10. 1097.PMID:16203955
17.HuangDQ,MathurinP,Cortez-PintoH,LoombaR.GlobalepidemiologyofalcoholassociatedcirrhosisandHCC:trends,projectionsandriskfactors.NatRevGastroenterolHepatol.2023;20(1):37–49.DOI: 10.1038/s41575-022-00688-6.PMID: 36258033;PMCID: PMC9579565
18.NationalCenterforHealthStatistics.SummaryHealthStatistics:NationalHealth InterviewSurvey,2018U.S.DepartmentofHealthandHumanServices,Centersfor DiseaseControlandPrevention;2018.
19.SimonGE,MoiseN,MohrDC.Managementofdepressioninadults:areview.JAMA. 2024;332(2):141–52.DOI: 10.1001/jama.2024.5756.PMID:38856993
20.ZetinM,HoepnerCT.Relevanceofexclusioncriteriainantidepressantclinicaltrials: areplicationstudy.JClinPsychopharmacol.2007;27(3):295–301.DOI: 10.1097/JCP. 0b013e318058263f.PMID:17502778
21.MindMed.MindMedReceivesFDABreakthroughTherapyDesignationandAnnounces Positive12-WeekDurabilityDataFromPhase2BStudyofMM120forGeneralized AnxietyDisorder.2024.
22.ZbozinekTD,RoseRD,Wolitzky-TaylorKB,SherbourneC,SullivanG,SteinMB,etal. Diagnosticoverlapofgeneralizedanxietydisorderandmajordepressivedisorderina primarycaresample.DepressAnxiety.2012;29(12):1065–71.DOI: 10.1002/da.22026 PMID:23184657;PMCID: PMC3629816
23.Cybinannouncespositiveend-of-phase2meetingwithFDAforCYB003inmajordepressivedisorderandphase3programdesign[pressrelease].March14,2024.
24.LuoY,KataokaY,OstinelliEG,CiprianiA,FurukawaTA.Nationalprescriptionpatterns ofantidepressantsinthetreatmentofadultswithmajordepressionintheUSbetween 1996and2015:apopulationrepresentativesurveybasedanalysis.FronPsychiatry. 2020;11:35.DOI: 10.3389/fpsyt.2020.00035.PMID:32116850;PMCID: PMC7033625
25.OstrowL,JessellL,HurdM,DarrowSM,CohenD.Discontinuingpsychiatricmedications:asurveyoflong-termusers.PsychiatrServ.2017;68(12):1232–8.DOI: 10.1176/ appi.ps.201700070.PMID:28712356
26.ColoradoRevisedStatutes,4CCR755-1(2022).
27.CenterforMedicareandMedicaidServices.December2023MedicaidandCHIPEnrollmentTrendSnapshot;2023.
28.ElmarasiM,FuehrleinB.USmedicaidprogram:ananalysisofthespendingand utilizationpatternsforantidepressantsfrom2017to2021.ExplorResClinSoc Pharm.2024;13:100392.DOI: 10.1016/j.rcsop.2023.100392.PMID:38149102;PMCID: PMC10750172
29.GattusoJJ,PerkinsD,RuffellS,LawrenceAJ,HoyerD,JacobsonLH,etal.Default modenetworkmodulationbypsychedelics:asystematicreview.IntJNeuropsychopharmacol.2023;26(3):155–88.DOI: 10.1093/ijnp/pyac074.PMID:36272145; PMCID: PMC10032309
30.ÖngürD,LundyM,GreenhouseI,ShinnAK,MenonV,CohenBM,etal.Defaultmodenetworkabnormalitiesinbipolardisorderandschizophrenia.Psychiatry Res.2010;183(1):59–68.DOI: 10.1016/j.pscychresns.2010.04.008.PMID:20553873; PMCID: PMC2902695
31.DanielsonNB,GuoJN,BlumenfeldH.Thedefaultmodenetworkandalteredconsciousnessinepilepsy.BehavNeurol.2011;24(1):55–65.DOI: 10.3233/BEN-2011-0310 PMID:21447899;PMCID: PMC3150226
32.CaoJ,AiM,ChenX,ChenJ,WangW,KuangL.Alteredresting-statefunctionalnetwork connectivityisassociatedwithsuicideattemptinyoungdepressedpatients.PsychiatryRes.2020;285:112713.DOI: 10.1016/j.psychres.2019.112713.PMID:31810745
33.MadsenMK,FisherPM,BurmesterD,DyssegaardA,StenbækDS,KristiansenS, etal.Psychedeliceffectsofpsilocybincorrelatewithserotonin2Areceptoroccupancyandplasmapsilocinlevels.Neuropsychopharmacology.2019;44(7):1328–34. DOI: 10.1038/s41386-019-0324-9.PMID:30685771;PMCID: PMC6785028
34.FrishmanWH,HuberfeldS,OkinS,WangY-H,KumarA,ShareefB.Serotoninandserotoninantagonismincardiovascularandnon-cardiovasculardisease.JClinPharmacol. 1995;35(6):541–72.DOI: 10.1002/j.1552-4604.1995.tb05013.x.PMID:7665716
35.ZeifmanRJ,WagnerAC.Exploringthecaseforresearchonincorporatingpsychedelics withininterventionsforborderlinepersonalitydisorder.JContextualBehavioral Science.2020;15:1–11.
36.BogenschutzMP,RossS,BhattS,BaronT,ForcehimesAA,LaskaE,etal.Percentageofheavydrinkingdaysfollowingpsilocybin-assistedpsychotherapyvsplacebo inthetreatmentofadultpatientswithalcoholusedisorder:arandomizedclinical trial.JAMAPsychiatry.2022;79(10):953–62.DOI: 10.1001/jamapsychiatry.2022.2096 PMID:36001306;PMCID: PMC9403854
Publisher’snote: GenomicPressmaintainsapositionofimpartialityandneutrality regardingterritorialassertionsrepresentedinpublishedmaterialsandaffiliations ofinstitutionalnature.Assuch,wewillusetheaffiliationsprovidedbytheauthors, withouteditingthem.Suchusesimplyreflectswhattheauthorssubmittedtousand itdoesnotindicatethatGenomicPresssupportsanytypeofterritorialassertions.
OpenAccess. ThisarticleislicensedtoGenomicPressundertheCreativeCommonsAttribution-NonCommercial-NoDerivatives4.0InternationalLicense(CCBY-NC-ND4.0).Thelicensemandates:(1)Attribution:Credit mustbegiventotheoriginalwork,withalinktothelicenseandnotificationofany changes.Theacknowledgmentshouldnotimplylicensorendorsement.(2)NonCommercial:Thematerialcannotbeusedforcommercialpurposes.(3)NoDerivatives: Modifiedversionsoftheworkcannotbedistributed.(4)Noadditionallegalortechnologicalrestrictionsmaybeappliedbeyondthosestipulatedinthelicense.Public domainmaterialsorthosecoveredbystatutoryexceptionsareexemptfromthese terms.Thislicensedoesnotcoverallpotentialrights,suchaspublicityorprivacy rights,whichmayrestrictmaterialuse.Third-partycontentinthisarticlefallsunderthearticle’sCreativeCommonslicenseunlessotherwisestated.Ifuseexceeds thelicensescopeorstatutoryregulation,permissionmustbeobtainedfromthe copyrightholder.Forcompletelicensedetails,visit https://creativecommons.org/ licenses/by-nc-nd/4.0/.Thelicenseisprovidedwithoutwarranties.
Psychedelics
OPEN RESEARCHREPORT
Whatmotivatesspiritualhealth practitionersinpsychedelic-assisted therapy?Aqualitativestudyand implicationsforfacilitatortraining practices
IshanPasricha1 , 2 ,CarolinePeacock1 , 3 ,RomanPalitsky1 , 3 , 4 , JaimeClark-Soles1 , 5 ,JessicaL.Maples-Keller1 , 4 , GeorgeH.Grant1 , 3 ,andDeannaM.Kaplan1 , 2 , 3
1 EmoryCenterforPsychedelicsandSpirituality,EmoryUniversity, Atlanta,GA30329
2 DepartmentofFamilyandPreventiveMedicine,EmoryUniversity SchoolofMedicine,Atlanta,GA30322
3 DepartmentofSpiritualHealth,WoodruffHealthSciencesCenter, EmoryUniversity,Atlanta,GA30329
4 DepartmentofPsychiatry,EmoryUniversitySchoolofMedicine, Atlanta,GA30322
5 PerkinsSchoolofTheology,SouthernMethodistUniversity,Dallas,TX 75205
CorrespondingAuthor: DeannaM.Kaplan,DepartmentofFamilyand PreventiveMedicineandEmoryCenterforPsychedelicsandSpirituality, EmoryUniversitySchoolofMedicine,Atlanta,GA30322,USA. Phone:(404)727-0839.E-mail: deanna.m.kaplan@emory.edu
Psychedelics March2025;1(2):31–39; doi: https://doi.org/10.61373/pp025r.0008
Spiritualhealthpractitioners(SHPs),alsoknownashealthcarechaplains,areincreasinglyinvolvedinfacilitatingpsychedelic-assisted therapiesinclinicaltrialsandcommunitysettings.Althoughthemotivationsoftherapeuticpractitionersareknowntoimpactclinical decision-makingandtreatmentoutcomes,littleresearchhasinvestigatedwhatdrivesSHPstopursuethiswork.Thisqualitativestudyexamined n = 15SHP’s(60%female; MAge = 46.57)whowereinvolved inlegaladministrationofpsychedelic-assistedtherapy.Aninductivedeductivequalitativeanalysisapproachyieldedtwomajorthemes:(1) InitialMotivationforPracticingPAT,and(2)OngoingSourcesofMeaningandFulfillment.TheSHPsinthisstudyoftencitedpersonalexperiencesaskeymotivationsforenteringthisfield,frequentlylinkedto asignificantpersonalencounterwithpsychedelicuse.ThemostcommonOngoingSourcesofMeaningandFulfillmentincludedwitnessinghealinginothersandexperiencingpositivepersonalimpactsfrom facilitatingpsychedelic-assistedcare.Thisarticleaddressesthesubstantialrolethatpersonalpsychedelicexperiencesappeartoplayin SHPs’motivationstopursuethisareaofpractice.Suchexperiences providevaluablefirst-handknowledgeoftheuniquephenomenology ofpsychedelictreatment,althoughtheycanalsopotentiallyintroduce biasesandreduceobjectivity.Trainingandcertificationguidelinesset bytheAssociationforClinicalPastoralEducation(ACPE)mayhelpaddresstheserisksforSHPsthroughheavyemphasisplacedonselfliteracyandreflectivelearningcomponents.Guidedbythesefindings, weintroduceanovelreflectivelearningexercise,aswellasseveralexistingACPElearningcomponentsthatmaysupportpsychedelicfacilitatorsandfacilitators-in-trainingfromanyprofessionalbackground.
Keywords: Chaplaincy,psychedelic-assistedtherapy,psychedelic facilitation,qualitativemethods,spiritualhealth.
Received:7February2025.Revised:31March2025.Accepted:7April2025. Publishedonline:29April2025.
Introduction
Psychedelic-assistedtherapy(PAT)involvestheadministrationofa psychedeliccompound(e.g.,classicpsychedelicssuchaspsilocybinorlysergicaciddiethylamideaswellasMDMAandothercompounds)together withtherapeuticsupport(1–3).EvidenceforthebenefitsofPATforaddressingseveraldifficult-to-treatconditions(PTSD,treatment-resistant depression,demoralizationamongcancerpatients)ismounting(4–6), andcorrespondingly,theutilizationofPATinterventionsisgrowing.In theUnitedStates,legalframeworksforsuperviseduseofpsilocybinhave beenenactedinOregonandColorado(7, 8),althoughmostpsychedelic compoundsremainfederallyillegal.Recentstate-levellegalchangesand thegrowingmentalhealthcrisishavesparkedburgeoningresearchon thetherapeuticuseofvariouspsychedeliccompounds,aswellasarapid expansionofcertificationandtrainingprogramsforPATfacilitation.
Amongevidence-basedpsychosocialtreatments,adistinctivefeature ofPATisthatitissimultaneouslyapharmacologicalintervention and aclinician-facilitatedtherapy(9).PATfacilitatorsthereforeplayakey roleintheexperiencethatclients’haveduringpreparationfortheir psychedelicdosingsession,duringthedosingsessionitself,andinintegrationoftheexperienceaftertheacuteeffectsofthepsychedelic agentshavewornoff(10, 11).SeveralattributesofPATmakeitaunique treatmenttofacilitate,comparedwithexistingevidence-basedtherapies.Theseincludetheintensephenomenologyofapsychedelicexperience(whichtypicallyinvolvesmarkedperceptual,affective,andcognitivechanges,includinghallucinations);thedurationoftheseexperiences (whichcanlast4–48h);andtheirimmediateandenduringsequelaewhich ofteninvolvechangesinthepatients’worldview(9, 12).ResearchcharacterizingthebesttherapeuticpracticesforPATfacilitationandthetrainingcomponentsthatadequatelypreparefacilitatorstoimplementthem is,therefore,importantfortheoptimizationofPAT.Todate,verylittleresearchhascharacterizedtheattributesofPATfacilitatorsorinvestigated theroleoffacilitatorattributesinprovidingeffectivecare(2).
Spiritualhealthpractitioners(SHPs;i.e.,healthcarechaplains)have increasinglyplayedrolesinPATfacilitationinclinicaltrialsandcommunitypracticecontexts.SHPsarehealthcareprofessionalswhoareemployedinapproximatelytwo-thirdsofallhospitalsintheUnitedStates (13, 14)andtrainedtoworkonintegratedcareteamstorecognizeand respondtoemotional,psychosocial,spiritual,religious,existential,and moralconcerns(15, 16).SHPstraininginvolves1600hoursofclinical traininginanaccredited,year-longclinicalresidency,andadditionalprofessionalcertificationrequirementsincludingpublishedscholarshipand committeeappearances(17).GiventheprevalenceofspiritualandexistentialthemesreportedbythosewhohaveundergonePAT(18, 19),and thepotentialmediatingrolethattheseexperiencesmayplayinPATbenefits(19, 20),thetrainingandprofessionalexpertiseofSHPsisanatural fitforPAT.SHPsareideallyequippedtoengagethespiritualdimensionof biopsychosocial-spiritualmodelsofcare(21, 22)andareuniquelyqualifiedtorespondtospirituallyimpactfulexperiencesthatmayariseforpatients,includingspiritualdistress(19).Inapriorqualitativestudy,these authorsinvestigatedtherolesthatSHPsplayinPATandthecompetencies theyidentifiedwithasmembersofPATtreatmentteams.Resultsindicatedthattrainingandformation(theongoinginternalandcommunally baseddevelopmentofthepersonasaspiritualcareproviderorclergyperson)assistinSHPsbeingabletoholdspace,accompanypersonsinnonordinarystatesofconsciousness,andrespondtospiritual,existential,religiousandtheologicalmaterialthatemergesinPAT.SHPsalsodiscussed howtheycontributetoPATteamsbynoticingandattendingtopowerdynamicsassociatedwithidentitycharacteristicsthatmayconfervulnerabilitiesforpatients(23).
Thepresentstudyismotivatedbyrecentcallstooptimizethe“psychotherapy”componentsofPAT(9, 24–26),aswellaspriorworkindicatingthatclinicians’underlyingmotivationsforpracticeimpacttherapeuticchoicesmadeduringtreatmentand,correspondingly,treatment
outcomes(27).Thisresearchisanovel,secondaryanalysisofqualitativeinterviewspreviouslycompletedwithSHPswhohaveworkedonPAT treatmentteamsinlegalsettings(forfurtherdetailontheprimarystudy, seeref. 23).Thecurrentsecondaryanalysisfocusedonidentifyingthe motivationsthatdrewSHPstothisuniquescopeofpracticeandthefactorsthatsustaintheirmotivationtocontinuetoprovidethismodalityof care.UnderstandingthebackgroundsandmotivationsthatSHPsbringto treatmentteamssupplementsagrowingresearchbaseontheattributes ofPATfacilitatorsandthefacilitator-levelfactorsthatmaycontributeto effectivecare.Methodsaredetailedattheendofthisarticle,afterthe Discussion section.
Results
Twooverarchingthemeswereidentifiedinthisanalysis:“InitialMotivationforPracticingPAT,”whichincludeddescriptionsofwhatinitially drewparticipantsintothisfieldofwork,and“OngoingSourcesofMeaningandFulfillment,”whichincludeddescriptionsofwhatprovidedSHPs withasenseofongoingmeaningorfulfillmentthatmotivatestheirwork presently.InitialMotivationforPracticingPATwasfoundtohavefive subthemes:(1)experiencewithtrauma/adversityandhealingthrough psychedelics,(2)psychedeliccareasacomponentofone’sspiritualvocationalpath,(3)desiretoalleviatesufferinginothers,(4)unplanned exposuretothefield,and(5)multilayeredmotivation.OngoingSourcesof MeaningandFulfillmenthadfoursubthemes:(1)appreciationforthepatternscommonlyassociatedwithpsychedelicexperiences,(2)witnessing thealleviationofsuffering,(3)mutualityofthefacilitationexperience, and(4)personalimpactsoffacilitatingPAT.
Theme1:InitialMotivationforPracticingPAT Subtheme:PersonalExperienceofHealingThroughPsychedelics
ThemostfrequentlyendorsedsubthemeofInitialMotivationforPracticingPATwasparticipants’ownexperienceswithhealingexperienced throughpsychedelics.Someparticipantsspokeof“healing”inbroad terms(i.e.,notassociatedwithaspecifiedailment),whileothersdescribedmorespecifichealingfromphysicalpain,illness,andortraumatic experience.Tenofthe15participantsspokeofthistheme.Asanillustrativeexample,oneparticipantdescribedexperiencingphysicalpainfroma bicycleaccident,eventuallyleadingthemtoseekPAT,whichtheyfoundto providesurprisingrelieffrompainthathadnotbeenresponsivetophysicaltherapy.Inresponsetotheprompt,“Whatledyoutothiswork?”,this individualresponded:
“Well,inoneword,pain…Ihadabikeaccidentafewyearsagoandmultiple breaks.Iwasdealingwithpainanddoingrigorousphysicaltherapy,witha greattherapistforlikeayear.Iwasonhertable,we’redoingdryneedling andmyshoulders,whichiswhereIseemtoholdalot…andfinally,mytherapistsaid,youknowthere’snothingstructurallyproblematicaboutyourbody anymore.Ithinkthatyouhavetrauma.AndI’veworkedwithalotof–Imean, I’vebeenthechaplainatadomesticviolenceshelterandinatrauma1hospital.So,I’mlike,“No.”Outofrespect,IwouldsayI’vehadhardthingshappen tome,butnottrauma.Well,mywholedefinitionofwhatthatmeanshas beencompletelyundone.AndIwenttoseesomeonewhoofferedsomatic therapyand…amplifiedwithpsychedelics,andIbeganaprocessofmyown healing.Andatfirst,IthoughtIwasjustcarryingpain.Ifeltpaininmybody. Ifeltpaininmyheart.Ifeltheavy.Ijustfeltweighted.Andthatwasmybeginning–myownhealing.Istartedtoexperiencethebenefitofwhatwas happening,andmywholeunderstandingopeneduptothefactthatmynervoussystemheldpain,heldstories,heldtraumaticexperiencesevenvicariously.Andthroughthiswork,Iwasabletoreleaseit.Istartedtofeelbetter ineveryway.”
Similarly,anotherparticipantdescribedpersonalexperienceofthe benefitsofpsychedelicsinthemanagementoftheirchronicillnessasmotivatingtheirentrytoworkinthefield:
“SoIhavechronicillness.ChronicLymedisease,Ialsohaveaformofmusculardystrophy,andinmyhealingjourney,Iwasjustintuitivelydrawn.I’d heardaboutatherapistusingspecificallyMDMAandpsilocybinandjust knewthat’swhatIneeded,andithasbeenanincrediblehealingsupport onalllevelsforme.Andso,afterseveralyearsofdoingthatworkformyself andexperiencingincrediblebenefits,IdecidedthatIwantedtogointothe field.”
Otherparticipantsspokeaboutpsychedelicexperiencesthatthey foundtobepersonallytransformative:
“ThebottomlineisthatIhadmyownexperienceswithayahuasca,anditwas deeplyhealingformeinwaysthatIjustcouldn’tevenimagine,andIkindof hadasenseandafeelingthatitwasgoingtobepartofmylifeinsomeway, butIdidn’treallyknowhow.”
Subtheme:AComponentofOne’sSpiritual-VocationalPath
Otherparticipantsdescribedimpactfulspiritualexperiencesfrom psychedelicusethatguidedtheirvocationalpath.Onepersondescribed howanexperiencewithpsychedelicsbecamecentraltotheirspiritual life:
“Twenty-fiveyearsago,IhadtheexperienceofworkingwithbothMDMA andpsilocybininmoreceremonialandhealingcapacities,andonewaswith anativeAmericanChicanomanwhostudiedinMexico,whoalsowascomingoutoftheMazatectraditioninsouthernMexico.Anditwasprofoundfor me…Itwasthethingthathelpedmefocusonmyspiritualpath,whichhas beenBuddhism,formanyyears.IwasstudyingandpracticingBuddhism, workingformanyyearsinend-of-lifecare,spiritualcare,andpalliativecare. Andthenkindofcamebackaroundfullcircletothemedicineagainformy ownhealing.”
Asillustratedbytheabovequote,thisthemesometimesco-occurred withpsychedelicexperiencesthatwerealsodescribedas“healing.”
Subtheme:DesiretoAlleviateSufferinginOthers
Severalparticipantsexpressedadesiretoalleviatethesufferinginothersasaprimarymotivationforenteringthefieldofpsychedeliccare.For example,oneparticipantdescribedthechallengingemotionalexperience ofwitnessingtheirgrandmother’scancerjourneyandsubsequentdeath. Theirfamiliaritywithpsychedelicshelpedthemunderstandthatdifferent experienceswerepossibleforpeoplewhoweresuffering.Theyshared:
“Shewasathome,noteventalkingaboutdyinguntiltwodaysbeforeshe diedandthenwenttothehospitalanddiedtheretwodayslaterandwas fullyalerttothemomentthatherspiritleftherbody,eyeswideopen,sitting upgrippingourhand,justtotallyfightingthisthing.Andthatexperiencereallyiswhatbroughtmeintochaplaincy-experiencingthefeelinglikeIknow there’sabetterwaythatthiscanhappen,andIwanttofindoutwhatthat is.…Itdoesn’tneedtobethatway,butitstillisforsomanypeople…Sofor me,thetoolofpsychedeliccareallowsustosupportpeopleintheirtransformativeprocessatthetimeintheirlivesthatthey’rebeingcalledtoinstead ofwaitingforlifetohappentothemand,likecrossingourfingersthatit’ll begood.Sothat’showIholdit-notinanywaybelievingthatit’sacureallor thatmagicallypeoplearetransformedfromjustoneexperience,butsome peopleare.Andotherpeopleneedahandtoholdforalongtime.Theyneed aparticularformofcareinanexpandedtimelinethatallowsthemtokindof workthroughonepieceatatime,dependingonhowmuchthey’recarrying.”
Subtheme:UnplannedExposuretotheField
SomeparticipantsspokeofanunplannedencounterwiththefieldofPAT thatsparkedtheirinterestinenteringthisareaofpractice.Forsome, theseexperiencescamefromtheirpersonallives;forothers,theywere unexpectedprofessionalexperiences.Oneparticipantdescribedworking asachaplainforaninstitutionthatinitiatedaclinicaltrialofPAT.Inthis context,theywereinvitedtoparticipateinalegalpsychedelicexperience toprepareforbeingafacilitator.Theysharedthefollowing:
“IwouldconsidermyselfasomewhatconservativeevangelicalChristian. Andcertainlythoserootsdon’tnecessarilyoverlapwellwiththehistoryof psychedelicsubstances,whetheritbeinthecontextofastudyorjusttheculturalrevolutionthatweexperiencedinthe50sand60sandthedrugwars inthe70sand80sandkindofwherewearetoday.AndsoIwasreallykind ofuncomfortable,tobehonest.Ididn’tknowifIhadaplaceinthisandI didn’tknowifmorallyIcouldparticipateinsuchastudy,sothisreallytook methroughasoul-searchingprocessonalotoflevels,notthatI’mcompletelydoneprocessingorcompletelydonewiththejourney…Partofthis journeythathasdrawnmeisnotjustintheprocessofhowdoIasachaplain createasafespaceandholdspaceforpeopleundermedicationandtopreparethemandtohelpthemintegratetheseprocesses,butIthinkchaplains alsobringusaparticularangleonthepracticeofmedicineandthestudies thatwehavetooffertothebiggerconversationofwhatexactlyarewedoing withpsychedelicsandwhatexactlyarewemeasuring.”
Anotherparticipantsharedaboutasituationalopportunitytoparticipateinaclinicaltrialthemselves.Theyhadanimpactfulspiritualexperiencewhichultimatelyledthemintotheworkoffacilitation:
“Myintroductiontothisfieldoccurredin(countryelided)whenIwasa23year-oldtheologicalstudent.AndIvolunteeredtohelptestsomenewdrug Ihadneverheardof…derivativesofpsilocybintheywerestudying.Andso,I laythere,openandtrustingandcurious.Andthen,thisincrediblybeautiful transcendentalstateofconsciousnessopenedupinmymind.AndIwasone verystarstruckyoungtheologicalstudent.Andinaway,Icouldsaymylife hasneverbeenthesamesince…inapositiveway…Thisincrediblybeautiful transcendentalstateofconsciousnessopenedupinmymind.InMethodism, there’sanemphasisonconversionexperiences,especiallyinearlyadolescence–givingyourlifetoJesusandbeingsavedinanexperientialsenseof belonging…Ihadalwayshadaprofoundappreciationfornature.ButIhad nevercomeclosetoexperiencingwhathappenedinthatfirstpsilocybinexperience.It’sbeyondwords-basicallyaunity,astateofconsciousness,inner beauty,andmeaningthatfeltmorerealandfundamentalthanthestateof consciousnesswe’rein.Likeahomecomingandawakening.Aremembering ofwhatis.Youknowarealrediscoveryoftheeternaldimensionofconsciousness.”
SeveralparticipantsdescribedexposuretoPATthrougheducational orcontinuingeducationprograms.Forexample,oneparticipantspokeof hearingaresearchertalkaboutthesuitabilityofchaplaincyskillsinPAT, whichwasaninfluencethatledtotheirchoiceofmakingthisafocusof theirscopeofpractice.
“WhenIwasgettingmymastersinpsychologyandreligionat(seminary nameelided)in(cityelided),IwasinthePsychologyandReligionprogram, andwehad[nameelided],who’sdoingthepsilocybinresearchinendoflife contextat(institutionelided),hecameintotalktoaspiringchaplainsatthe seminaryandagainthatjustgotmereallyexcitedinthepossibilityofkindof utilizingmybackgroundandspiritualcare…soIwouldseethosewerekind ofmyintroductionstothefield,sothatwhenopportunitiescameuplater through[companyelided]Iknewthatmyskillswererelevant,Iwasexcited aboutthefield.Ihadalotofjustkindofintellectualknowledgeaboutthe fieldthat’sreallykindofhowImadethetransitionfromchaplaincytocheck itout.”
Subtheme:MultilayeredMotivations
Notably,formostparticipants,motivationstoenterthefieldweremultifaceted.Ratesofco-occurrencebetweentheabovecategorieswere high,withnearlyallparticipantsendorsingmorethanoneoftheabove themes.Whilesomeparticipantswereprimarilydrivenbyonefactor, othersdescribedmoreblendedmotivations.Forexample,oneparticipantsuccinctlydescribedamotivationthatincludedthepromisingresultsofrecentresearch,thehealingtheyhadpersonallyexperiencedfrom psychedelics,andadesiretohelpothersexperiencesimilarhealing.This participantshared:
"Havingwitnessedalotofsufferingfromtraumainpeoplewhoweren’treallyfindingmuchreliefandsupport.Then,intermsofend-of-lifecare… someofthepsilocybinstudiesthathaveshownthatpeoplearereallyable toworkthroughexistentialdistressandotherchallengesoftheendoflife–thatalsoconnectedwithmyvocationalpath.Andthen,onapersonalnote, havinggonethroughsomechildhoodtraumamyself,Ifoundpsychedelic therapytobereallybeneficialformyself.ThosearethemainreasonsthatI startedtolookatthis.Andthenhadsomeopportunitiestobecomeinvolved intheresearch,whichI’mgratefulfor.”
ThisparticipantcametoPATasanareaofpracticeafterencounteringexistingresearchonpsychedelicsandobservingtheirownpositivepsychedelicexperiences.Otherparticipantsshareddifferentconstellationsofprecipitatingfactors.Forexample,oneparticipantidentified challengingordifficultexperienceswithpsychedelics:
"Ithenhadanexperiencethatwasvery,verydifficult,verypainful,verydisorientingduringapsychedelicjourney…thatessentiallysidelinedmeforthe nextdecade.Itscaredmeverybadly.IbelievedthatIwassortofmanifesting somekindofmentalillnessthatIwasgoingtolosemymind–thatmysense ofselfwasgoingtofragment.Thatneverhappenedbutwhatdidhappenis thatoneparticularinstancemanifestedwhatInowknowtobeanxietythat Ihadtodealwithforyearsafterthat.AndthatIstilldealwith.Becauseof thatanxiety,Iwasonthesidelines.Mycommunityandmyfriendscontinued
toexperiment,andIthereforetookonmoreorlessinadvertentlytheroleof babysitteroraguide.”
Anotherparticipantdescribedanexperiencewithpsychedelicsearly inlifethatledtoatransformativespiritualawakening,leadingtheminto chaplaincy.Muchlater,anopportunityarosetotrainasafacilitator.
“Ididalotofpsychedelicsinmyteenageyears.Ihadaverypowerfulexperiencethatwasmorespirituallybasedandhadaverysolidintentionwhen Iwas19.Andthatchangedthecourseofmylifeandhelpedmeexperiencesomethingmuchdeeper–amuchdeeperreality,ifthatmakessense, andIalsoexperiencedalotarounddeathanddying,andfromthatexperience,Iwascalledfirst,intoaspiritualpaththatledmeintomeditation thatthenkindoftookmeintothecallingofordainedministry,aswellas chaplaincywork,specificallywiththosewhoaredying.AndthenIstopped psychedelics;Ididn’tdopsychedelicsfor20years,actually,afterthatreallypowerfulexperience,andIwasapproachingnon-ordinarystatesofconsciousnessmorethroughmeditation,contemplativeprayer,thingslikelong extendedretreats.ButthenIhadanopportunitytogothroughthe(programnameelided)inthefirstcohort,asitwasapilotproject.So,Itook thatopportunity,andthat’skindofwhatthenledmetobeginfacilitating psychedelics.”
Theme2:OngoingSourcesofMeaningandFulfillment
Subtheme:AppreciationforthePatternsCommonlyAssociated withPsychedelicExperiences
Severalparticipantsdescribedderivingongoingappreciationandfulfillmentfromwitnessingcertainexperiencesorthemesthatcommonlyaccompanypsychedelicexperience.Forexample,oneparticipantdescribed aglobalsenseofconnectednessexperiencedbymanywhohavetaken psychedelics:
“Seeingthesimilarexperiencesofparticipantsinstudies…creatingnew storiesbutalsocomingintoasenseofbeingpartofsomethinglarger… thattomeisspiritualhoweveranyonedefinestheirspiritualjourneyor theirreligiouspractices…thefeelingofbeingpartofsomethinglargerthan ourselves.”
Similarly,inanotherparticipant’swords:
“Somethingthatjustseemstoconsistentlyemergewithpsychedelictherapiesandthatseemstobeabeneficialemergenceforthepeoplethatare experiencingit…toseethispatternagainandagainandagainfeelsvery spiritualandveryaffirming.Idon’thavetolabelitorknowexactlywhatit is,orputABCliststoit,butthatthereissomethingthatconnectsusall,connectsustotheplanet,connectsus…whetherwecallthatGod’sspirit,the universe,humanity,earth,whatever,…it’saveryspiritualexperienceforme towitnessagainandagainthesesamepatterns,thesesameexperiencesfor differentpeople.”
WhenSHPsspokeofthepatternsthatemergedacrossfacilitatingpsychedelicexperiences,wordssuchas“connectedness”cameup frequently.SHPsdescribedwitnessingtheseexperiencesaspersonally meaningful,inspiring,andanimportantcontributingfactortotheirmotivationtocontinueinthisfield.
Subtheme:WitnessingtheAlleviationofSuffering ParticipantsalsodescribedthesatisfactiontheyexperiencedinwitnessingthealleviationofsufferingduringPAT.Thisthemecommonlycooccurredwiththe“desiretoalleviatesuffering”subthemeofTheme1 (InitialMotivationforPracticingPAT),aswitnessingthealleviationofsufferingcreatedongoingmotivationforpersonsinitiallydrawntoPATfacilitationwiththisaim.Severalparticipantsdescribedderivingsatisfaction fromseeingothershealandgrowthroughpsychedelicuse.InoneSHP’s words:
“ThedeepestplacewhereIaccessmeaningisthroughbeingofservicetothe healingprocessofothers.Thatcomesthroughinthisworkbecauseit’svery clientcentered.It’sveryfocusedonredirectingindividualstotheirowninner wisdom,innerspiritualvoice…Itfeelslikethatisthegreaterpurpose…It givesmemeaning–thefeelingofbeinginalignmentwithlife’spathhappens whenIamholdingspaceforothersactuallytositwithintheirrelationshipto theirowninnerguide…It’sbeingofservice.It’salsoassistingfolksandmovingintowhatIwouldcalltheirspiritualalignment.Whetherthat’sreligious ornot,orwhetherit’satheist…that’swhatgivesmeaning.”
Otherparticipantsdescribedtherewardingnatureofwitnessingimprovementforclientswhohavehadlimitedsuccesswithotherformsof treatment:
“Alotofthefolksthatarecomingtoourtreatmentmodel,inparticular,have beendealingwithtreatment-resistantdepression,anxiety,orPTSD.They’ve beenhavingreallyseveresymptomsorsymptomsthattheyjusthaven’tbeen abletogetaholdofforareallylongtime.Andjustreallyseeingthisrapidly actingtransformationthatbeginstohappeninjustafewsessions.Ithink it’sjustreallyalwaysexcitingforme…Seeingpeople’shardworkcometo fruition.…beingabletousemychaplainskillsandtoacknowledgehowdifficultitistoopenupatthatmoment.SoIthinkthat’sanotherthingthat’s reallyfulfillingformeisthatalotofpeoplecomeintotreatment,maybealreadyhavingpartiallygivenuporseeingthisistheirlastresort,sotospeak. Sojustbeingabletogrowthatkindofbreakthroughtreatmentforpeople,I think,isexcitingaswell.”
Similarly,anotherparticipantdescribedhopefulnessforPATin addressingconcernstypicallycharacterizedas“subclinical,”suchas burnout.Theyshared:
“Ithinkthere’shopeinit.Othertherapieshaven’tworked.Otherthings haven’tspokentopeople.There’stoomuchthat’sunidentifiedlivinginpeople.Thatyouknowit’siftheyhadaccesstoitorknewwhattodowithit,they wouldhavedoneitalready,itwouldhavebeendealtwith,youknowpeople arenotlazyorstupid,andsotheycan’tgettoit…Iworkedthroughthewhole COVIDintheICU.Welost80nurseswhohaveresignedfromthatunitoverthe courseofthepandemic.AndI’mstilltalkingtothemandhearingthemsay, ‘I’mdeadinside.’That’saquote–‘Iamdead.’We’renotgoingtotalkyouout ofthat.Idon’tthinkwe’regonnabubblebathyououtofthat.”
Participantsalsodiscussedfindingmeaninginhelpingpeopleexperienceaconnectiontothesacred,coupledwiththecapacityofPATtotreat mentalhealthconditions:
“Iwouldn’tbedoingitifitdidn’tgivemesomuchmeaning.Psychedelicsfor meareanextremelypowerfultoolforpeopletoexperiencethesacred,the divineGod,Imeanwhateverlanguage…weknowthat’skindofineffable… alldifferentwordstodescribethat.Also,fromamentalhealthperspective, thedata,thestatisticsthatarecomingout,andtheresultsthatIseeinthe participantsthatIfacilitatecomparedtomoretraditionaltoolsinthementalhealthworldliketalktherapyandpharmaceuticaldrugs…justsuchan amazingsuccessratewiththeuseofpsychedelicsifdonecorrectly,Ireally, reallystronglybelievethat.”
Subtheme:MutualityoftheFacilitationExperience Someparticipantsspokeaboutfindingmeaninginthemutualityofthe facilitationexperience.Participantswhohadtheirown,personallyimpactfullivedexperienceswithpsychedelicsoftendescribedanappreciationfortheaspectsofsharedexperiencethataccompaniedfacilitatingpsychedelicexperiencesforothers.Forexample,asoneparticipant putit:
“…seeingpeopleheal–likereallyseeingpeopleheal–issosatisfying.To havethatandmyownexperience,knowingwhereIaminmyjourneybecause ofthiswork,andIwouldn’tbeherewithoutthisworkandthewaythatIam today,andIseethatitchangespeople’slives.”
Anotherparticipantspokeofasimilarexperienceofmutualityinthe contextofhavingachronicillness:
“AsI’veworkedwithmychronicillnessandasI’vereframedmynarrative,it makesmefeellessisolated,lessalone,partofsociety,partoftheworld.Even ifI’minpain,evenifI’mstillnotfeelingwell,Icanstillbepartofthislarger fabricoftheworldandacceptmylimitations…Psychedelicshavehelped withsymptoms,helpedhealsomeofmychronicillnessesandhelpedme stepmoredeeplyintorelationshipswithothersandwiththiswholeecosystemthatwe’repartofandfeelmoreinconnectionwiththedivine.There’s aplanformylife.There’sareasonIcameinwiththechallenges…ButI’ve gotgroundthatIcansupportotherswithnowbecauseIfoundthisground withinmyself…psychedelictherapiescansupportusalltorecognizethat weareallconnected…canhelpusfindgroundandthenthereforekindof beabletomovefromthatground.EventhoughImaystillhavesymptoms, Imaystillnotfeelgoodsomedays.Istillhavepain,butIcanstillstepinto theworldwithallofmyselfandfindaplacethat’smeaningfulformeand allowsmetohavejoy.”
Notallparticipantsdescribedmutualityintermsofhealing.Otherparticipantsspokeofaspiritualprocessthatbeganwiththeirownexperience oftakingpsychedelicsandisnowenrichedbyfacilitatingpsychedelicexperiencesforothers.Inanotherparticipant’swords:
“Personally,sittingwiththemedicinerequiresadeepcommitmenttomy ownspiritualdevelopment,andmyowninnerhealingwork.Thathasbeen, insomeways,amplifiedand,insomeways,reallydoescometotheforefronttoseeandtobeasclearaspossibleforothers.Toofferthatservice workingwithinthestructureswithinmylifehasbeenextremelyimportant. Encounteringallmybiases,healingmyownstuff,anddoingtheinnerwork. ThemoreIdothat,themoreclarityIhaveandthelessofmyownstuffIbring intotheroomwithothers…Toholdspaceforfolkshavingmysticalexperiences,there’salsobeenachangewithinmetoaccessthosestateswherethe openingisstabilizedbetweensessions.Andalotofmydevelopmentleans intovariousspirituallineagesthatarenotnecessarilyusingmedicinework butareencouragingandareusingancientpracticestoestablishthosesame openingsbutmaybeaccesstheminmoreofastableday-to-dayexpanded way.So,twofold:it’sbeenheavy-dutyspiritualpracticethathasamplifiedit inmylifeandourwork.Ithinkit’stwosidesofthesamecoin.”
Inadditiontomutualitywiththeirclients,participantsalsospoketo impactfulexperiencesofmutualitywithothermembersofclients’care teams.Forexample:
“Personalexperiencewithmedicineworkingintherapeuticandceremonial contextsandhowprofoundlythathasimpactedme,myspirituality,myhealing,mysenseofconnectionintheworld…Imean,relativetootherwork contexts,thisteamhasfeltlikeIhavearealsenseofkinshipandthatwe areinalignmentwiththemodelinamoreholisticapproach.Yeah,andjust howfrommyownexperienceandfromwhatIhearofothershow,potentially, notinevitably,butpotentiallysupportivemedicineworkcanbefornotonly healing,particularlyhealingaroundtrauma,butspiritualgrowthandselfawarenessofconnectionintheworld.”
Subtheme:PersonalImpactsofFacilitatingPAT Thissubthemedescribedexperiencingpersonalimpactfromengaging inPATthatsustainsparticipants’vocationalmotivation.Althoughthis sometimesincludedthepersonalimpactsofthepriortheme,mutuality,participantsalsospoketoseveralpersonalimpactsindependentof sharedexperiences.Oneparticipantdescribedbeinginspiredbythecommonalitiesinpsychedelicexperiencesthattheyhavewitnessedoveryears offacilitation:
“I’vecertainlybeenreinforcedinmyviewoftheworld,inmyspirituallife,in mypsychologicaltheory.I’vehadthegreathonorofbeingwithseveralhundredpeopleintheirpsychedelicsessions,andtome,that’salotofevidence. Peoplefromdifferentraces,differenteducationallevels,differentcareers, differentphysicalhealthsituationsandthehumanmindseemstofunction prettymuchthesamewithallofthem.Andthat’sinspiring…”
Anotherparticipantspokeofthepersonalimpactofworkingina group/peersupportmodelandthepowerofwatchinggroupmembers buildtrustingrelationshipswithoneanother:
“Thisgroupmodelismoreaboutpeersupport,anditismoreaboutcultivatingtoolsforpresence,forgroundedspaciousawareness,forwhatitisthatis emergingwithinusthatwecanaccept,bewith,andpossiblyallowforsome processingsimplybybeingpresenttoitwithcompassion,andthenpeople beingwitnessedbythegroupandfeelingthesenseofsupportandsafety andtrustthatideallyisdeepenedovertheweeksfromthegroup.Seeing peoplewhohave,inthiscase,significanttraumahistories,someofwhom havebeenreallyisolatedeitherforvariousreasons,sociallyorbecauseof thedegreeoftheiranxiety(notcomfortableleavingtheirhouse,especially inthecontextofthelastfewyears)eveninashortperiodoftime,feelinga senseofbondkinship,safety.Feeling‘I’mnotalone’witheachother.Being abletorelaxandfeelinganaturalheartfulness,joyfulness,compassion,and innerhealingwisdomemergewithinthatspace.Thattomeisbeautifulto witness.”
Anotherparticipantdescribedfulfillmentintheintimacyof psychedelic-assistedcare:
“Iwouldsaythingshavekindofchangedmeaboutthiswork….Ithink insomeways,likethepsychiatriccontext,insomeways,likethehospice context,it’saveryintimatesetting.Themedicine,insomeways,really
helpspeopletaketheirdefensesdownandbemoreengagedwiththework, maybetostaypresentwithmoredifficultactivatingmaterial.Ithinkthe sessionsarereallyintimate,andIthinkthere’ssometransformationjust inseeingthiskindofspiritualrevelationsthatpeoplehave.Ithinkjustbeingabletowitnessthat,beingabletoobservethat,supportthat.Ithink itreallyjustopensmyeyestothecomplexityofhumansinourspiritual lives.”
Discussion
AstheevidencebaseforPATscontinuestoexpand,optimizingthefacilitationoftheseuniquetreatmentshasbecomeincreasinglyimportant (25).Inthecontextofthespiritualandexistentialexperiencesthatoften accompanypsychedelicexperiences,SHPsareincreasinglyrecognizedas playingvitalrolesonPATcareteams(19, 23).Understandingtheroles thatSHPscanplayonPATcareteams,andhowtrainingforPATfacilitationcanbeoptimized,requiresanunderstandingofthemotivationsthat drawSHPstoPATfacilitationinthefirstplace,aswellasthefactorsthat sustaintheirongoingworkinthisfield.Themajorthemesidentifiedin thisresearchhighlightthedeeplypersonalnatureofPATfacilitationfor theSHPsinthisstudy,afindingwhichhasvaluableimplicationsforPAT facilitationtraining.
ThisstudyfoundthatpersonalpsychedelicusewasastrongmotivatorforSHPspracticingPAT—afindingconsistentwitharecentinvestigationofpsychedelicuseamongtherapistsfromaphase2clinicaltrialofpsilocybinformajordepressivedisorderthatfoundthatthe majorityoftherapistshadexperiencewithatleastonepsychedelicsubstance,mostcommonlypsilocybin(25).ManySHPsinourstudydescribed theirpsychedelicexperiencesas“healing”;othersdescribedtheirexperiencesasspiritually“transformative,”asopeningnewspiritualawareness,enhancingtheirexistingsenseofspirituality,orincreasingtheir understandingoftheirplaceintheworld.Notably,SHPspredominantly describedpersonalbenefitsassociatedwiththeirpastpsychedelicexperiences,althoughpsychedelicexperiencesarenotexclusivelyexperiencedasbeneficialandaresometimesexperiencedaschallenginginthe generalpopulation(28, 29).
WithrespecttofactorsthatprovideSHPswithongoingsources offulfillmentandmotivationforthiswork,witnessingothersexperiencehealingwasdescribedasparticularlysignificant.Manyparticipantsinthisstudyreportedderivingadeepsenseofmeaningfrom themutualityoftheexperience—thatis,guidingsomeoneelsethrough anexperiencethattheyhadfoundtobesopowerfulandpersonally impactful.Manyparticipantsalsospoketointerconnectednessasa sustainingfactor.Interconnectednesswassometimesdescribedasexperiencedwithclients,sometimesdescribedasexperiencedwithother membersofaPATcareteam,andsometimesdescribedasdrawing fromrepeatedwitnessingofthemesthatcommonlyemergeduringa psychedelicexperience.
Thesefindingsarealignedwithpriorresearchonthemotivationsthat drawpractitionerstopsychologicalhealingprofessionsmorebroadly. Studiesexaminingthemotivationsofmentalhealthproviders(includingtherapists,psychologists,andsocialworkers)havefoundthattherapistsfrequentlydescribepersonalexperiencesofadversityandhealingas significantfactorsintheirmotivationfortheirvocation.Specifically,personaladversities,livedexperiencesofsocialandculturalmarginalization, andone’sownexperienceofreceivingtherapyarecommonmotivatorsfor vocation(27, 30, 31).ThelimitedexistingliteraturecharacterizinggeneralvocationalmotivationsofSHPsfinds,similarly,thatmanycometothe professionwithahistoryofpersonaltraumaandadversityintheirfamiliesandcommunities(32, 33).SHPsarealsolikelytocitedisillusionment withreligiousinstitutionsasamotivatorforworkinginchaplaincy(33). Havinglivedexperiencewithsymptomsandexperiencesreportedbypatientshasbeennotedinthepsychotherapeuticliteraturetohavebothadvantagesanddrawbacks.Ithasbeensuggestedthatpersonalexperiences ofadversitymayconferempathyandanenhancedcapacitytounderstand humancomplexities(33),leadingtoagreatercapacityforsittingwith othersintimesofdistress(24, 34).Conversely,personalexperiencescan increasetheriskofinaccurateprojectionofone’sownexperienceontothe patient(24)andmayinterferewithobjectivityinassessmentandtreatmentplanning(35).
Thequestionofwhetherpersonalpsychedelicexperienceshouldbe aprerequisiteforprovidingpsychedelicfacilitationremainsoneofthe mostdebatedtopicsinthefieldofPATfacilitationtraining(24).This studyaddsanadditionaldatapointtoanaccumulatingfindingthat,much likementalandspiritualhealthprofessionalswhoaremotivatedbytheir ownexperiencesofadversityandhealing,psychedelicfacilitatorsarefrequentlymotivatedbypersonalexperienceswithpsychedelicuse.However,ourfindingsalsoraisethepossibilitythatfirsthandpsychedelic experiencemaynot,initself,leadtomoreeffectivecare.Becausepersonalpsychedelicexperienceswerefrequentlydescribedaskeysources ofmotivationtoprovidethiskindofcare,itmaybethatmotivation— ratherthantheexperienceitself—isamoreimmediateandinfluential factorinfacilitatingeffectivetherapy.Whilenoresearchtodatehasexaminedwhetherfacilitatorswithpriorpsychedelicexperiencearemore efficacious,wesuggestthat,evenifsuchanassociationwerefound,it couldbeattributabletoincreasedmotivationratherthananyinherent benefitofthepsychedelicexperience(orotherencounterswithnonordinarystatesofconsciousness)itself.Giventhis,werecommendthat PATfacilitationtrainingprogramsacknowledgepersonalpsychedelicuse asapotentialmotivationalfactorandexplicitlyaddressthisintraining.Regardlessofwhetherprogramschoosetoofferpsychedelicexperiencestotrainees,itisessentialfortraineestorecognizeandthoughtfullyengagewithpriorpsychedelicexperiencesthatarebroughtinto training.
WhentheProfessionalisPersonal:Implicationsfor PATFacilitationTraining
ResultsofthisresearchfoundthatformostSHPs,workinginthefield ofPATisdeeplypersonal.Manyreportedexperiencingtheirowntransformationandhealingthroughpsychedelicuseandnowseektooffer otherssupportthroughsimilarmethods.Ononehand,thislevelofpersonalexperiencecanbebeneficial:experientialknowledgemayequip SHPstoskillfullyrespondtotheuniquephenomenologyassociatedwith psychedelicagents(24, 36).Afacilitator’slivedexperiencewithandbeliefintheeffectivenessofpsychedelicsmayalsoconstitutecommonfactorsoftreatmenteffectiveness.Psychotherapyresearchoncommonfactorshasfoundthattherapistempathyaloneexertslargeeffectsizeson treatmentoutcomes(d > 0.8),andexpectationshavesmallerbutstill significanteffects(d > 0.2),independentofanyspecificcomponentsof treatment(34).
Conversely,personalexperiencescanalsointroducebiasesthat hindertheabilitytoprovideobjectivecare.Facilitatorswhoare stronglymotivatedbypersonalexperienceruntheriskof“experiential encapsulation”—atermweadaptfromculturalencapsulation,whichis usedtodescribeaclinicians’applicationoftheirownculture-boundexperienceandworldviewstothoseofaclientwithoutregardforimportant differences(37, 38).Experientialencapsulationoccurswhenfacilitators assumethattheirownpsychedelicexperiences,thetimelinesoftheseexperiences,andtheirframeworksforinterpretingtheseexperiences,are universallyapplicable.Thiscanleadfacilitatorstooverlooktheunique anddeeplypersonalwaysinwhichdifferentindividualsmayexperience psychedelicsduringPAT.Justasculturallyencapsulatedtherapistsareat riskoffailingtoconsiderculturaldifferencesbetweenthemselvesand theirclientandimposingtheirownvaluesoncare(37, 38),anexperientiallyencapsulatedfacilitatormayfailtorecognizevariationsinhowindividualsexperiencepsychedelicsandthemeaningsthatareascribedto theseexperiences.AnyfacilitatorofPAT(whetheranSHPorfromanother profession)whoseapproachisoverlyshapedbypersonalpsychedelicexperiencerunstheriskofoversightswhenworkingwithsomeonewhohas amarkedlydifferentexperience.Suchoversightscanleadtoineffectiveness,oratworst,treatmentharms(9).
ForSHPs,trainingrequirementssetbytheAssociationforClinicalPastoralEducation(ACPE)mayhelpbufferagainstthisrisk(24).ThepreparatorytrainingtobecomeanSHPthroughACPEplacesaheavyemphasison self-literacy.Self-literacytrainingoccursinthecontextoftheCommon CodeofEthicsforChaplains,PastoralCounselors,PastoralEducatorsand Students,whichsetsforthseveralstandardspertainingtoculturalhumilityandrespectforautonomyintheworldviewandbeliefsofothersinall
Figure1. Self-literacyreflectionexerciseforpsychedelicfacilitators.
professionalactivities(e.g.,Standard1.3:“Demonstraterespectforthe culturalandreligiousvaluesofthosetheyserveandrefrainfromimposingtheirourownvaluesandbeliefsonthoseserved.”)(39).ACPEtraining standardsalsoincludeseveraloutcomesandindicatorsthataskSHPs-intrainingtoreflectupontheirmotivationstoengageintheworkofspiritualcare,theorientingsystembehindtheirspiritualcarechoiceswith clients,andtheirunderstandingofpersonal,social,andculturallocation thatimpactstheirwayofbeingintheworldandwork(39).Forexample, learningoutcomesinclude“Identifyformativeandtransformativeexperiencesinone’snarrativehistoryandtheirsignificancetoone’sspiritual journey”(IA.1)and“Demonstrateanawarenessofimplicitandsystemic biasincludingculturalandvalue/belief-basedprejudiceanditsimpacton spiritualcare”(IA.7).ThisreflectivelearningaimstoaidSHPsinbringing awarenesstofactorsthatmotivatetheiractionsinspiritualcareencounters.InthecontextofPAT,thistrainingmayalsoaidSHPsinsensitively approachingaparticipant’sexperiencewithoutexpectations,regardless oftheSHPs’relationshipwithpsychedelics.Whilethepersonalhistory oftransformationthroughpsychedelicsmaybeasignificantmotivator formanySHPsengagedinthiswork,thelearningoutcomesandethical guardrailsofSHPsmayassistinmaintainingapracticethatcentersthe experienceoftheclient.
Standardssetforthbyprofessionalethicscodesformentalhealth providers(e.g.,theAmericanPsychologicalAssociationEthicsCode;the CodeofEthicsforSocialWork)articulatecomparablepracticestandards withregardstorespectforclients’autonomyandrefrainingfromimposingone’sownvalues(40, 41).However,thesestandardsfortraining andpracticedonotexplicitlyaddressreflectiononone’sownnarrative andpsychospiritualhistory.Intheabsenceofsuchstandards,training programsforclinicalmentalhealthprofessionsoftendedicateminimal timetoexperientialself-literacytrainingasanintegratedcomponentof training.FindingsfromthisresearchsuggestthatwhenitcomestoPAT, trainingcompetenciesassociatedwithself-literacyofone’snarrativeand psychospiritualhistoryandmotivationsmaybeparticularlyimportant.In thecontextofongoingdiscussionsabouttrainingguidelinesandrequirementsforPATthatcutacrossprofessions,wesuggestthatACPE’sreflectivelearningmodelforacquiringself-literacybeconsideredanelement oftrainingthatcanbenefitallPATproviders,regardlessoftheirprofession.Further,aspractitionersengageinPAT,continualreflectiononthese learningoutcomesaspartofcontinuingeducationcanbenefitproviders’ work.
GuidedbyfindingsfromthisstudyandtheACPEreflectivelearningmodel,wesuggestaself-literacyexercisethatcanbecompleted byPATfacilitatorsandfacilitators-in-trainingcomingfromanyprofessionalbackground(Figure1).Thesequestionsaimtobalancethevalue ofpersonalexperiencewiththeneedforclinicalobjectivityandtheimportanceofreflectingonhowpersonalexperiencesandmotivationscan conferbothstrengthsandgapsinawareness.Thenineself-reflection questionsprovidedin Figure1 canbeassignedasawritten,narrativeexerciseduringpsychedelicfacilitationtraining,sothattraineescanpracticereflectivelywithoutbeingrequiredtodiscloseaboutpersonalexperiencebeyondtheircomfortlevel.Practicingfacilitatorsmaybebenefit fromrevisitingthesequestionsannually,asmotivations(andpersonalexperience)maychangeovertime.
LimitationsandResearcherPositionality
Aprimarylimitationofthisworkpertainstorecruitmentandthesampleofparticipantsrepresented.Participantsintheseinterviewswere recruitedthroughanationalprofessionalnetwork(TransformingChaplaincy)thatwasoriginallyco-convenedbythisstudy’sprincipalinvestigator(PI).Thiscouldhaveledtobiassuchthattheviewsofparticipantswere similarinnaturetoeachotherandthePI.Participantsinthisstudyhad avarietyofchaplaincytrainingexperiences,notallthroughACPE.Relatedly,onlythosepracticingPATinlegalsettingswereincluded.Thismeans thatourresultsmaynotgeneralizetothenumerouspractitionersworkinginundergroundsettingsandtraditionalreligious/spiritualsettings. ProviderspracticinginthosesettingshaveuniqueexperiencesfacilitatingPAT,andmayhavedifferentmotivationsandsustainingfactorsfor theirwork.OurresultsalsomaynotgeneralizetolegalPATpractitioners fromnon-SHPtrainingbackgrounds(e.g.,psychiatry,clinicalpsychology, socialwork).Broadlyspeaking,educationalpathwaysandpracticeenvironmentsimpacttheexperiencesandmotivationsofpractitioners.Future researchshouldreachabroadernetworkofproviderstoensuremoregeneralizabilityandunderstandtowhatextentexperiencesmaydiffer.
Additionally,thevastmajorityofparticipantsinthisstudywerewhite (80%)andNorthAmerican(93%).Thisposeslimitationsonthegeneralizabilityofthisworktothepopulationsatlarge.Individualsfromother racial,ethnicandculturalbackgroundsmayapproachpsychedelicexperiencesdifferently,leadingthemtohavedifferentperspectivesthanthose representedhere.Forexample,participantsinthisstudyexpressedanorientationtowardpersonalhealing.Communaldimensionsofhealingare
centraltomanytraditionsofpsychedelicusearoundtheworld(42)and areunder-representedhere.
Thisqualitativestudyshouldalsobeinterpretedinlightofauthorpositionality.AllauthorsofthisstudyresideintheUnitedStatesandwork inprimarilyacademiccontexts,withsettingsspanningalargeacademic medicalcenter,aSchoolofPublicHealth,andaSchoolofTheology.The authorsincludeSHPs(chaplains),clinicalpsychologists,aclinicalsocial worker,andagraduatestudentinpublichealth.AllauthorshaveprofessionalexperiencewithPAT;someauthorshaveprovidedPATfacilitation, whileothershaveservedresearch-focusedrolesonPATtrials(e.g.,investigator,dataanalyst).Ourtrainingbackgroundsinformthelensthrough whichweapproachedtheseanalysesandtheirinterpretation,andindividualswithothertrainingorprofessionalbackgroundsmayhavegenerateddifferentcodingcategoriesordrawndifferentconclusionsthan thoserepresentedhere.Weacknowledgethatourperspectivesdonot representtheperspectivesofallPATfacilitatorsorrecipientsofthese treatments.
ConclusionsandFutureDirections
AsthefieldofPATcontinuestoexpandandthepotentialforFDAapproval ofpsychedelicagent(s)appearsonthehorizon,itisacriticaltimefor professionaldisciplinestosystematicallyevaluatewhatconstitutesappropriatepreparationforthoseworkinginPAT.UnderstandingthemotivatingfactorsforSHPswhoarealreadyengagedinthisworkallows thosewithinandoutsidethefieldofspiritualcaretoconsiderthecomplexdynamicsatplaywithinaPATfacilitationexperiencefromaunique perspective.
Acorefindingfromthisstudywasthatpersonalexperiencessubstantiallyinformedparticipants’initialandongoingmotivationsforworking inthisfield.Wedonotdrawconclusionsregardingwhetherexperience withpsychedelicsisnecessarytobeaneffectivePATfacilitator.However, awarenessofmotivations—whetherrelatedtoone’sownpsychedelicexperiencesornot—canassistthefacilitatorinbringinganobjectiveapproachtotheworkthatiscenteredontheexperienceofthepersonseekingcare.ResultsofthisstudysuggestthattrainingprogramsforPAT wouldbenefitfromcurriculacomponentsthatinvitetraineestoexplore personalmotivatingfactorssothatinsightintothesecanbecultivated andanyresultingbiasescanbeaddressed.Withacarefulandself-aware approach,therapistsofanydisciplinemaybeabletoprovidecarethat issensitivetopowerdynamicsandnon-imposingofpersonalexperience andperspective.
Methods
Thepresentstudyisasecondaryanalysisofaqualitativestudythataimed toidentifytherolethatSHPsplayonPATteams(23).Thissecondaryanalysiswasmotivatedbytheemergenceoftwothemesthatwereinductively identifiedduringouroriginalqualitativeanalysesfortheprimarystudy. Thesethemesfellbeyondthescopeofthatresearch,andthereforewere notexaminedorreported:(1)thefactorsthatinitiallybroughtparticipantstoPATfacilitation,and(2)thefactorsthatmotivatetheircontinued practiceofthisprofession.
Participants
ParticipantsinthisresearchhadexperiencefacilitatingPATandalsomet atleastoneofthefollowingcriteria:(1)oneormoreunitsofClinicalPastoralEducation(ACPE),(2)ordinationorstatusasareligiousleader,(3) aMasterofDivinityorotheradvancedtheologicaldegree,or(4)specific traininginspiritualitywithinpsychedelicwork,aboveandbeyondwhat isofferedinstandardPATcertificationprograms.Recruitmentoccurred betweenMarch2022throughJune2022.“ExperiencewithPAT”wasdefinedasexperiencefacilitatingPATinsettingswhereitwaslegal,includingbothceremonialand/orretreatsettings,aswellasclinicalresearch environments.
Allparticipants(n = 15)intheparentstudyarerepresentedinthe presentstudy.Participantshadanaverageageof46.57(SD = 13.38), identifiedas60%female(40%male),andwere20%Hispanic/Latinxand 80%White.Thevastmajority(93%)wereNorthAmerican,with6.67% beingSouthAmerican.ThemostcommoncontextofPATexperiencewas withinclinicaltrials(46.67%),withthenextmostcommonbeingretreat/
ceremonial(40%),andprivatepractice,clinic,andremote/virtualbeing theleastcommon(6.7%).ThemostcommonlyusedpsychedelicinPAT interventionsreportedbyparticipantswaspsilocybin(66.67%),followed byketamine(46.67%),ayahuascaandMDMA(both13.33%),andLSD, cannabis,andkambo(6.7%).
ProceduresandMeasures
SHPswereinterviewedviatheZoomtelehealthplatform,exceptforone SHP,whowasquestionedviaawrittenemailexchangeduetopoorinternetconnectivityandinabilitytoengageviaZoom.AllSHPswerequeried usingasemistructuredinterviewguideof14standardquestions,reportedintheoriginallypublishedstudy(23).Interviewquestionsincluded itemsaskingSHPstodescribevariousaspectsoftheirprofessionalactivities,theirmotivationsforengaginginPAT,theirviewoftheimportance ofpersonalexperiencewithpsychedelics,ethicalconcernsrelatedtoPAT, spiritualoutcomesofPAT,andviewsofthebuildingfieldofSHPsengaginginPAT.
Twopreviouslyunanalyzedquestionsweretheanalyticfocusforthe presentinvestigation:amotivationquestion,askedtoallparticipants (“Whatmotivatedyoutoworkinthisfield?”),andameaningandfulfillmentprobe(i.e.,“Whatbringsyoumeaningorfulfillmentinthiswork?”). Themeaningandfulfillmentprobewasincludedintheinterviewguideas anoptionalfollow-upprobe,andthereforenotaskedofallparticipants. Informationyieldedinresponsetothisprobe,whenitwasincluded,was relatedtothemotivationthemeandwasthereforeincludedinthepresent analysis.AllinterviewswerevideoandaudiorecordedandtranscribedusingtheautotranscriptionfeatureofZoom.Transcriptsweresubsequently manuallydeidentifiedandcorrectedfollowingtheautomatedtranscriptionforanyerrorsorlackofclarity(viacomparisonwithliverecording) bytworesearchers.
DataAnalysis
Thedataanalyticstrategyfortheprimaryanalysisisdescribedelsewhere (23).Duringthatprocesstwothemesemergedinductively,whichdidnot fallwithinthescopeoftheprimaryanalysis.Thesetwothemeswere(1) participants’descriptionsoftheirinitialmotivationsforfacilitatingPAT, and(2)theircurrentsourcesofongoingmotivationandfulfillmentin theirwork.Thesethemesweredeterminedtobeunrelatedtotheaims oftheprimarystudy,whichweretocharacterizetherolesandactivities ofSHPsonPATtreatmentteams,butofsufficientscientificimportanceto warranttheirowndedicatedsystematicinvestigation.
Thepresentsecondaryanalysesemployedahybridinductivedeductiveapproach(43)torapidqualitativeanalysisofthesetwo themes.Arapidqualitativeapproachwasselectedbecauseoftheshiftingregulatoryenvironmentofpsychedelics,andongoingdiscussions abouttheroleofSHPsinpsychedeliccare,towhichthisanalysismay providedirectlygermane,thoughtime-sensitive,information.Inthe secondaryanalysis,ourfirststepwastogenerateacodebookofsubthemes,whichwascreatedbytwoinvestigatorswithcontentexpertisein chaplaincyandpsychedelicfacilitation.Thecodebookwascreatedbyreviewingalltranscripts,andthenidentifying(1)pre-existingthemesthat weredeemedimportanttoexamineinadeductivestep(e.g.,theexisting unexaminedcategoriesthatemergedintheprioranalysisthatmotivated thepresentinvestigation),and(2)asetofthemesrelevanttothesetwo originalthemes,whichwererecognizedandnotedseparatelybythetwo investigators.Thesewerediscussedandconsolidatedintoonecodebook. Thatcodebookwasthenrefinedbyhavingthetwoexpertcoderscodea subsampleoftranscriptsindependently,andthenresolvedisagreements byconsensus,modifyingandaddingcategoriesasneeded.Theresulting codebookwasthentreatedasafinalizedversion.Thesecodeswere deductivelyappliedbyasinglecoderusingMAXQDAversion22.2.00 qualitativeanalysissoftware.Thismethodofrapidqualitativeanalysis hastheadvantageoftakinglesstimethandouble-codedmethods, andthelimitationthatcodingmaybesubjecttobiaseddetection,with intercoderreliabilityofthefulldatasetnotpossibletoestablish(44). Thislimitationmakesresearcherpositionalityparticularlyimportantto describeandreportaspartofdatainterpretation(see Discussion forthis reporting).
DataAvailability
Datacannotbesharedpubliclybecauseofconcernsaboutidentifiability, andtheneedtopreserveprivacyandconfidentialityofparticipants.Becausethetopicsdiscussedmayincurlegalorsocialsanctionsthedataare heldonprotectedandencrypteduniversityserversatEmoryUniversity. DatamaybemadeavailableforresearcherswhomeetthecriteriaforaccesstoconfidentialdatabycontactingtheEmoryUniversityInstitutional ReviewBoardat irb@emory.edu orthecorrespondingstudyauthor.
Acknowledgments
Theauthorswouldliketothanktheparticipantsinthisresearchforsharingtheirexperiencesandperspectiveswithus.
AuthorContributions
C.P.collectedandanalyzedreporteddata.D.M.K.,I.P.,andC.P.wrotethe firstdraftofthismanuscript,withinputfromR.P.,J.C.S.,J.M.P.,andG.H.G. RevisionstothisarticlewerecompletedbyD.M.K.andI.P.,withinputby C.P.,R.P.,J.C.S.,J.M.P.,andG.H.G.Allauthorsreviewedandapprovedthefinalversionofthismanuscript.Allauthorstakefullresponsibilityfordata andtextandapprovethecontentandsubmissionofthisarticle.Norelatedworkisunderconsiderationelsewhere.
FundingSources
Thisresearchwasnotfundedbyexternalsources.PersonneltimededicatedtopreparationofthisarticlewasgenerouslysupportedbyEmory SpiritualHealth.
AuthorDisclosures
D.M.K.hasservedasaconsultantfortheMindandLifeInstituteandthe OxfordResearchEncyclopediaofGlobalPublicHealth,andhasreceived researchsupportfromtheNIH,theGeorgiaCTSA,theTinyBlueDotFoundation,theSarloFamilyFoundation,andtheVailHealthFoundation.R.P. hasreceivedresearchsupportfromtheTinyBlueDotFoundation,the JimJosephFoundationviaShefaJewishPsychedelicSupport,theSarlo FamilyFoundationandhasconsultedfortheHarvardDivinitySchoolCenterfortheStudyofWorldReligions.J.M.K.hasreceivedconsultingpaymentsfromCOMPASSPathwaysandOstukaandreceivessupportfrom theWoundedWarriorProject(WWP)andMultidisciplinaryAssociationof PsychedelicStudies.
References
1.LuomaJB,PlattMG.Shame,self-criticism,self-stigma,andcompassioninacceptance andcommitmenttherapy.CurrOpinPsychol.2015;2:97–101.
2.SloshowerJ,GussJ,KrauseR,WallaceRM,WilliamsMT,ReedS,etal.PsilocybinassistedtherapyofmajordepressivedisorderusingAcceptanceandCommitment Therapyasatherapeuticframe.JContextBehavSci.2020;15:12–9.DOI: 10.1177/ 02698811231154852.PMID:36938991
3.Denis-LalondeD.(PDF)Emergingpsychedelic-assistedtherapies:Implications fornursingpractice.[Internet].[cited2025Feb4].Availablefrom: https://www. researchgate.net/publication/341583827_Emerging_Psychedelic-Assisted_ Therapies_Implications_for_Nursing_Practice
4.YehudaR,LehrnerA.Psychedelictherapy—anewparadigmofcareformentalhealth. JAMA.2023;330(9):813–4.DOI: 10.1001/jama.2023.12900.PMID:37651148
5.BarberGS,AaronsonST.Theemergingfieldofpsychedelicpsychotherapy.CurrPsychiatryRep.2022;24(10):583–90.DOI: 10.1007/s11920-022-01363-y.PMID:36129571; PMCID: PMC9553847
6.DavisAK,BarrettFS,MayDG,CosimanoMP,SepedaND,JohnsonMW,etal.Effectsof psilocybin-assistedtherapyonmajordepressivedisorder:arandomizedclinicaltrial. JAMAPsychiatry.2021;78(5):481–9.DOI: 10.1001/jamapsychiatry.2020.3285.PMID: 33146667;PMCID: PMC7643046
7.MonteAA,SchowNS,BlackJC,BemisEA,RockhillKM,DartRC.Theriseofpsychedelic druguseassociatedwithlegalization/decriminalization:anassessmentwiththenonmedicaluseofprescriptiondrugssurvey.AnnEmergMed.2024;83(3):283–5.DOI: 10.1016/j.annemergmed.2023.11.003.PMID:38142372
8.XenakisSN,ShannonSM.Whatisneededfortheroll-outofpsychedelictreatments? CurrOpinPsychiatry.2024;37(4):277.DOI: 10.1097/YCO.0000000000000946.PMID: 38726805
9.PalitskyR,KaplanDM,PernaJ,BosshardtZ,Maples-KellerJL,Levin-AspensonHF,etal. Aframeworkforassessmentofadverseeventsoccurringinpsychedelicassistedtherapies.JPsychopharmacol.2024;38(8):690–700.DOI: 10.1177/02698811241265756 PMID:39082259
10.LevinAW,LancelottaR,SepedaND,GukasyanN,NayakS,WagenerTL,etal.Thetherapeuticalliancebetweenstudyparticipantsandinterventionfacilitatorsisassociated withacuteeffectsandclinicaloutcomesinapsilocybin-assistedtherapytrialformajordepressivedisorder.PLoSOne.2024;19(3):e0300501.DOI: 10.1371/journal.pone. 0300501.PMID:38483940;PMCID: PMC10939230
11.ModlinNL,McPheeT,ZazonN,SarangM,HignettR,PickS,etal.Participants’experienceofpsychedelicintegrationgroupsandprocesses:aqualitativethematicanalysis. PsychedelicMed.2025;3(1):19–30.
12.GukasyanN,NayakSM.Psychedelics,placeboeffects,andsetandsetting:insights fromcommonfactorstheoryofpsychotherapy.TranscultPsychiatry.2022;59(5):652–64.DOI: 10.1177/1363461520983684.PMID:33499762
13.CadgeW.PagingGod:religioninthehallsofmedicine[Internet].UniversityofChicago Press;2013[cited2025Feb5].Availablefrom: https://books.google.com/books?hl= en&lr=&id=gFG4jQDufTIC&oi=fnd&pg=PR5&dq=Cadge,+W.+Paging+God:+Religion+ in+the+Halls+of+Medicine%3B+University+of+Chicago+Press:+Chicago,+IL,+USA, +2012&ots=oZ0nv-VWZ5&sig=-hjxumCWOwfaGedVjAy8eRrcam4 14.CadgeW,FreeseJ,ChristakisNA.TheprovisionofhospitalchaplaincyintheUnited States:anationaloverview.2008[cited2025Feb5];Availablefrom: https://books. google.com/books?hl=en&lr=&id=OMpWDwAAQBAJ&oi=fnd&pg=PA36&dq=Cadge, +W.%3B+Freese,+J.%3B+Christakis,+N.A.+The+provision+of+hospital+chaplaincy+ in+the+United+States:+A+national+overview.+South.+Med.+J.&ots=RWY0BTrTOL& sig=iSZWZujJE9siAHzZ93K3OMvOL6o 15.VanderwerkerLC,FlannellyKJ,GalekK,HardingSR,HandzoGF,OettingerSM,etal. Whatdochaplainsreallydo?III.ReferralsintheNewYorkchaplaincystudy.J HealthCareChaplain.2008;14(1):57–73.DOI: 10.1080/08854720802053861.PMID: 18686545
16.PalmerPK,SiddiquiZ,MooreMA,GrantGH,RaisonCL,MascaroJS.Hospitalchaplainburnout,depression,andwell-beingduringtheCOVID-19Pandemic.IntJEnviron ResPublicHealth.2024;21(7):944.DOI: 10.3390/ijerph21070944.PMID:39063520; PMCID: PMC11277059
17. https://www.apchaplains.org/wp-content/uploads/2022/05/2017-Common-Qualifi cations-and-Competenciesfor-Professional-Chaplains.pdf –GoogleSearch[Internet].[cited2025Mar20].Availablefrom: https://www.google.com/search?q=https% 3A%2F%2Fwww.+apchaplains.org%2Fwp-content%2Fuploads%2F2022%2F05%2F+ 2017-Common-Qualifications-and-Competenciesfor-Professional-Chaplains.pdf& oq=https%3A%2F%2Fwww.+apchaplains.org%2Fwp-content%2Fuploads%2F2022% 2F05%2F+2017-Common-Qualifications-and-Competenciesfor-ProfessionalChaplains.pdf&gs_lcrp=EgZjaHJvbWUyBggAEEUYOTIGCAEQRRg60gEHMzMyajBqN6g CALACAA&sourceid=chrome&ie=UTF-8
18.SchuttWA,ExlineJJ,PaitKC,WiltJA.Psychedelicexperiencesandlong-termspiritual growth:asystematicreview.CurrPsychol.2024;43(32):26372–94.
19.PalitskyR,KaplanDM,PeacockC,ZarrabiAJ,Maples-KellerJL,GrantGH,etal.Importanceofintegratingspiritual,existential,religious,andtheologicalcomponents inpsychedelic-assistedtherapies.JAMAPsychiatry.2023;80(7):743–9.DOI: 10.1001/ jamapsychiatry.2023.1554.PMID:37256584
20.HartogsohnI.Themeaning-enhancingpropertiesofpsychedelicsandtheir mediatorroleinpsychedelictherapy,spirituality,andcreativity.FrontNeurosci.2018;12:129.DOI: 10.3389/fnins.2018.00129.PMID:29559884;PMCID: PMC5845636
21.SaadM,DeMedeirosR,MosiniAC.Arewereadyforatruebiopsychosocial–spiritual model?Themanymeaningsof“spiritual.”Medicines(Basel).2017;4(4):79.DOI: 10. 3390/medicines4040079.PMID:29088101;PMCID: PMC5750603
22.SulmasyDP.Abiopsychosocial-spiritualmodelforthecareofpatientsattheend oflife.Gerontologist.2002;42(suppl_3):24–33.DOI: 10.1093/geront/42.suppl_3.24 PMID:12415130
23.PeacockC,MascaroJS,BrauerE,ZarrabiAJ,DunlopBW,Maples-KellerJL,etal.Spiritualhealthpractitioners’contributionstopsychedelicassistedtherapy:aqualitative analysis.PLoSOne.2024;19(1):e0296071.DOI: 10.1371/journal.pone.0296071.PMID: 38166057;PMCID: PMC10760908
24.VilligerD.Howtomakepsychedelic-assistedtherapysafer.CambQHealthcEthics. 2025;1–15.DOI: 10.1017/S0963180124000604.PMID:39618402
25.AdayJS,HortonD,Fernandes-OsterholdG,O’DonovanA,BradleyER,RosenRC, etal.Psychedelic-assistedpsychotherapy:whereisthepsychotherapyresearch?Psychopharmacology(Berl).2024;241(8):1517–26.DOI: 10.1007/s00213-024-06620-x PMID:38782821
26.PalitskyR,Maples-KellerJL,PeacockC,DunlopBW,MletzkoT,GrantGH,etal.A criticalevaluationofpsilocybin-assistedtherapyprotocolcomponentsfromclinical trialpatients,facilitators,andcaregivers.Psychotherapy(Chic).2025.DOI: 10.1037/ pst0000551.PMID:39804360Availablefrom: https://psycnet.apa.org/record/202566803-001
27.McBeathA.Themotivationsofpsychotherapists:anin-depthsurvey.CounsPsychother Res.2019;19(4):377–87.DOI: 10.1037/cou0000596.PMID:34843273
28.SimonssonO,HendricksPS,ChambersR,OsikaW,GoldbergSB.Prevalenceandassociationsofchallenging,difficultordistressingexperiencesusingclassicpsychedelics. JAffectDisord.2023;326:105–10.DOI: 10.1016/j.jad.2023.01.073.PMID:36720405; PMCID: PMC9974873
29.JohnstadPG.Daytriptohell:amixedmethodsstudyofchallengingpsychedelicexperiences.JPsychedelicStud.2021;5(2):114–27
30.FarberBA,ManevichI,MetzgerJ,SaypolE.Choosingpsychotherapyasacareer:why didwecrossthatroad?JClinPsychol.2005;61(8):1009–31.DOI: 10.1002/jclp.20174 PMID:15945066
31.BarnettM.Whatbringsyouhere?Anexplorationoftheunconsciousmotivationsof thosewhochoosetotrainandworkaspsychotherapistsandcounsellors.PsychodynPract.2025;13(3):257–74.Availablefrom: https://www-tandfonline-com.proxy. library.emory.edu/doi/full/10.1080/14753630701455796
32.GubiP,SmartH.Motivationalfactorsinmentalhealthchaplains:practitioners’Perspectives.HealthSocCareChaplain.2014;1
33.KlitzmanR,SinnappanS,GarbuzovaE,Al-HashimiJ,DiSapiaNatarelliG.Becoming chaplains:howandwhychaplainsenterthefield,factorsinvolvedandimplications.
JHealthCareChaplain.2024;30(2):75–88.DOI: 10.1080/08854726.2022.2154108 PMID:36515161
34.WampoldBE.Howimportantarethecommonfactorsinpsychotherapy?Anupdate.WorldPsychiatry.2015;14(3):270–7.DOI: 10.1002/wps.20238.PMID:26407772; PMCID: PMC4592639
35.HecksherD.Formersubstanceusersworkingascounselors.Adualrelationship. SubstUseMisuse.2007;42(8):1253–68.DOI: 10.1080/10826080701446711.PMID: 17674234
36.NielsonEM,GussJ.Theinfluenceoftherapists’first-handexperiencewith psychedelicsonpsychedelic-assistedpsychotherapyresearchandtherapisttraining. JPsychedelicStud.2018;2(2):64–73.DOI: 10.1556/2054.2018.009
37.HeppnerPP,WangKT,HeppnerMJ,WangLF.Fromculturalencapsulationtocultural competence:Thecross-nationalculturalcompetencemodel.In:FouadNA,CarterJA, SubichLM,editors,APAHandbookofCounselingPsychology,Vol.2.Practice,interventions,andapplications,433–471.AmericanPsychologicalAssociation;2012[cited 2025Feb5];Availablefrom: https://psycnet.apa.org/record/2012-03487-018
38.BergkampJ,PonsfordM.Culturalencapsulation.In:CarducciBJ,NaveCS,MioJS,RiggioRE,editors.TheWileyEncyclopediaofPersonalityandIndividualDifferences.1st ed.Wiley;2020[cited2025Feb4].p.239–41.Availablefrom: https://onlinelibrary. wiley.com/doi/10.1002/9781119547181.ch304
39.ACPE[Internet].[cited2025Feb4].CategoryA:SpiritualFormationandIntegration–ACPEManuals–2025.Availablefrom: https://www.manula.com/manuals/acpe/acpemanuals/2016/en/topic/revised-acpe-outcomes-and-indicators-spiritualformation-and-integration
40.Ethicalprinciplesofpsychologistsandcodeofconduct.[cited2025Feb4].Available from: https://www.apa.org/ethics/code
41.Socialworkers’ethicalresponsibilitiestoclients.[cited2025Feb4].Available from: https://www.socialworkers.org/About/Ethics/Code-of-Ethics/Code-of-EthicsEnglish/Social-Workers-Ethical-Responsibilities-to-Clients
42.SanabriaE,TófoliLF.Integrationorcommodification?Acriticalreviewofindividualcenteredapproachesinpsychedelichealing.JPsychedelicStud.2025[cited2025 Mar20];Availablefrom: https://akjournals.com/view/journals/2054/aop/article-10. 1556-2054.2024.00411/article-10.1556-2054.2024.00411.xml
43.LayderD.SociologicalPractice:LinkingTheoryandSocialResearch.SAGEPublications; London(PublisherLocation)1998.
44.CampbellJL,QuincyC,OssermanJ,PedersenOK.Codingin-depthsemistructuredinterviews:problemsofunitizationandintercoderreliabilityandagreement.Sociol MethodsRes.2013;42(3):294–320.DOI: 10.1177/0049124113500475
Publisher’snote: GenomicPressmaintainsapositionofimpartialityandneutralityregardingterritorialassertionsrepresentedinpublishedmaterialsandaffiliationsofinstitutionalnature.Assuch,wewillusetheaffiliationsprovidedbytheauthors,withouteditingthem.Suchusesimplyreflectswhattheauthorssubmitted tousanditdoesnotindicatethatGenomicPresssupportsanytypeofterritorial assertions.
OpenAccess. ThisarticleislicensedtoGenomicPressundertheCreativeCommonsAttribution-NonCommercial-NoDerivatives4.0InternationalLicense(CCBY-NC-ND4.0).Thelicensemandates:(1)Attribution:Credit mustbegiventotheoriginalwork,withalinktothelicenseandnotificationofany changes.Theacknowledgmentshouldnotimplylicensorendorsement.(2)NonCommercial:Thematerialcannotbeusedforcommercialpurposes.(3)NoDerivatives: Modifiedversionsoftheworkcannotbedistributed.(4)Noadditionallegalortechnologicalrestrictionsmaybeappliedbeyondthosestipulatedinthelicense.Public domainmaterialsorthosecoveredbystatutoryexceptionsareexemptfromthese terms.Thislicensedoesnotcoverallpotentialrights,suchaspublicityorprivacy rights,whichmayrestrictmaterialuse.Third-partycontentinthisarticlefallsunderthearticle’sCreativeCommonslicenseunlessotherwisestated.Ifuseexceeds thelicensescopeorstatutoryregulation,permissionmustbeobtainedfromthe copyrightholder.Forcompletelicensedetails,visit https://creativecommons.org/ licenses/by-nc-nd/4.0/.Thelicenseisprovidedwithoutwarranties.


Psychedelics:A dedicated forum for the renaissance in psychedelic research. We publish innovative studies spanning neuroscience and therapeutics, connecting researchers advancing treatment frontiers. Submit your manuscript and become part of the scienti c exploration of consciousness and healing.
Our mission: Transforming scienti c publishing through author- focused suppor t and global dissemination.
Our fair-cost pl atform delivers rapid, rigorous review and uses contemporary tools to amplify research visibility worldwide.
We welcome scientists across disciplines, providing emerging research unprecedented exposure. Our three journals now feature over 100 published papers with extraordinary global reach.
Our innovative distribution strategy has generated 2,500 news stories in 21 l anguages worldwide. Through strategic partnerships with respected science communication pl atforms like EurekAler t! (AA AS) and targeted social media campaigns, we have created unprecedented visibility for our authors' work, connecting cutting-edge research directly with global audiences.
Brain Medicine
Welcome to the future of scienti c publishing!