
6 minute read
Pushing boundaries
Lecturer Karen Lansdown describes how her research is making a significant impact on the dental hygiene of people of disability, like her own son
Lecturer and PhD candidate in the School of Dentistry, Karen Lansdown, has been awarded $103,000 from the Research Foundation, Cerebral Palsy Alliance PhD Grant to investigate the commonly overlooked condition associated with cerebral palsy and poor oral health.
Cerebral Palsy Alliance PhD research grants are available on a competitive basis to attract new and highly qualified graduates into the field of cerebral palsy research.
As a person with a lived experience of disability, I have attended a range of specialist medical appointments with my 12-year-old son, related to his cerebral palsy (CP). During this process, I started to identify a common theme, no matter what the specialty; no one ever mentioned oral health.
When I raised concerns with a colleague about my son’s migrating central incisor, I was told to wait and see. When I posed the question ‘what about his quality of life?’ the honest response I received, was ‘I had never even considered that’.
Having attended seminars on support and service access within the National Disability Insurance Agency, no one mentioned oral health, let alone had an oral care plan. In fact, when I raised the topic of oral health in a forum, they were dismissive of my ‘radical ideas’. It made me realise that we as dental professionals had failed in making our voices heard to the medical profession and this vulnerable population group. Whilst I can be an advocate for my child, what about those parents and caregivers that are unaware of the importance of oral health to general health?
Research to date identifies that children with CP are at an increased risk for many oral health concerns. The neuromuscular impacts of CP may cause change to the oro-facial structures, negatively impacting nourishment, oral hygiene and resulting in parafunctional habits of the mouth, jaw and tongue. This negatively impacts general health and affects self-esteem and self-confidence, particularly in social situations. There is emerging evidence to suggest that children with CP are at increased risk of developing sleep apnea, drooling, bruxism and pain. However, there are significant gaps in the current literature with regards to oral health, quality of life and oral health recommendations for people with CP, especially in adults.
In both high and low-middle income countries, there is a lack of research conducted on people with CP, 18 years and over. In particular, there is very limited research in this population on oral health-related quality of life, mouth breathing, sleep apnoea, pain, masticatory habits, gastroesophageal reflux disorder, and perceived barriers to dental care.
Findings thus far have shown the majority of research related to oral health for people with CP has been conducted in low-middle income countries. More research in high income countries would provide new opportunities to understand whether the oral health outcomes experienced by both children and adults with CP in these settings are consistent with those in low-middle income countries.
Currently, there are no clear guidelines, frameworks or detailed oral health recommendations for people with CP in Australia or globally. Considering the increased risk of dental disease for people with CP, the dental community needs to support people with CP and their carers to promote good oral health. Interdisciplinary collaboration and preventive strategies are essential to achieve positive outcomes.
My research has found that the major oral health concerns reported as shown in the graphic on this page, were dental caries, occlusion, periodontal diseases and conditions, saliva, dental trauma, tooth wear, soft tissues and tongue, bruxism and oral hygiene. In order to provide appropriate support for people with CP including accessing dental services, my research has identified the need for classification systems that acknowledge functional motor limitations of people with CP such as the Gross Motor Functional Classification System (GMFCS) be documented in patient records. As dental professionals we can exemplify diversity and convey respect for people with a disability such as assimilating disability inclusive language into our practice e.g., ‘people with CP’ or ‘people with a disability’, avoiding the use of language that lacks inclusivity such as the term ‘special care’.
Recommendations arising from my research include the provision of continuing education and training courses for dental professionals, carers and allied health care workers and to employ dental professionals in disability services to:
– Implement targeted dental education for staff, carers and people with CP on the importance of oral health and general health. – Deliver tailored oral health care plans.
The next stage of this body of research is to identify environmental and nonenvironmental barriers experienced by people with CP and their families in accessing dental care to improve oral health disparities. This will provide targeted and specific oral health recommendations, inform policy, and improve the general health of people with CP. Consumer involvement in research is important. Research about us should not be done without us! As such we intend to include people with CP in as many aspects of the development of this body of research as possible.
DHAA members and dental practitioners across Australia will soon be invited to participate in a study to understand the knowledge, attitudes and practices of treating people with CP in Australia. This research will inform our understanding of the experiences of dental professionals treating people with CP in community and private dental settings. This includes an understanding of referral pathways; preparedness of dental practitioners, and barriers and/or enablers to treating people with CP in the dental setting.
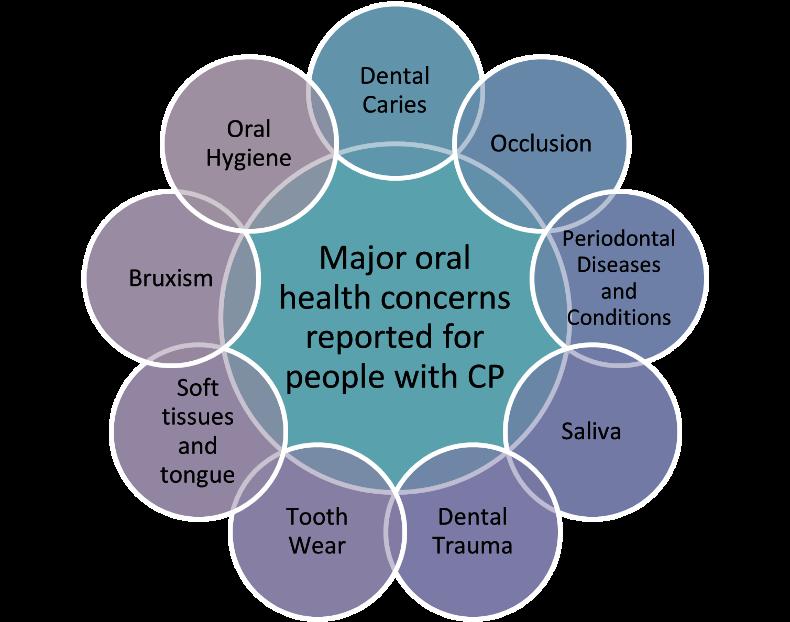
Figure 1
This body of research will help us know what oral conditions are most common for people with CP so we can identify and manage these conditions early and what aspects of the dental and medical system need to be improved so this can be achieved. These findings will help us improve oral health disparities and identify positive strategies, so we as a profession can make a difference in communities.







