
12 minute read
Fractures of the Pelvic Ring By Mr Nikhil Shah
FRACTURES OF THE PELVIC RING
By Mr Nikhil Shah
Advertisement
Mr Shah is a Trauma and Orthopaedic Surgery Consultant at Wrightington Hospital in Lancashire with special interests including long bone and joint periarticular fractures, pelvic and acetabular fractures, hip and knee replacement. He has extensive medico-legal experience, including multiple/polytrauma accidents and catastrophic injury, clinical negligence, work-related accidents, low velocity impact whiplash and fraud and injury overseas.
The pelvis is the strong and sturdy ring of bones located at the base of the spine. It links the bottom of the spine to the lower limbs. Fractures of the pelvis are relatively uncommon. But they can be life threatening injuries. Management of pelvic ring has evolved and advanced over the last 4-5 decades due to the efforts of many pioneering surgeons, particularly Letournel and Judet in France and Pennal and Tile in North America, to name just a few. Most pelvic fractures are caused by some type of trauma, a high-energy event, such as a car collision or a fall from a height. The pelvis contains and protects major blood vessels, nerves, and important organs, and so pelvic fractures may cause extensive bleeding and other injuries that require urgent treatment. Treatment for a pelvic fracture varies depending on the severity of the injury. While lower-energy fractures can often be managed without surgery, treatment for high-energy pelvic fractures usually involves surgery to reconstruct the pelvis and restore stability of the ring, so that patients can regain the ability for early walking and return to function.
Medico-Legal Relevance
Most pelvic fractures are caused by some type of traumatic, high-energy event, such as a car collision. Some of them occur from crush injuries at work, fall from ladders, fall through a roof, pedestrians hit by vehicles, and hence these injuries give rise to quite a few personal injury claims.
In some cases, a lower-impact event—such as a minor fall—may be enough to cause a pelvic fracture in an older
person who has weaker bones. These too can sometimes form part of a claim, due to the injury having occurred in a public place or after a simple fall due to trips and slips.
It is important to appreciate the features of the injury and arrive at a prompt diagnosis to allow timely appropriate management of the injury. Occasionally the fractures are difficult to spot on simple plain x-rays, particularly undisplaced fractures or sacral fractures, and rarely can be missed at the initial assessment in a busy casualty environment. A high index of suspicion is required for diagnosis. Missed injuries or inappropriate / inadequate treatment can often develop into liability and causation / breach of duty type claims. Whilst the anterior ring lesion- involving the pubic ramus or pubic symphysis is rarely missed, it is the posterior ring lesion in the sacrum or sacro-iliac joint that is not always appreciated by plain x-rays.
Anatomy
The pelvic bones include the following components:
1- Sacrum (the large triangular bone at the base of the spine which forms the sacro-iliac joints). The coccyx (tailbone) joins the lower end of the sacrum. 2- Each hemipelvis or innominate bone contains the
ilium, ischium, and pubis—that are separate during childhood but fuse together as we grow older.
3- These three bones meet to form the acetabulum —the socket for the ball-and-socket hip joint.
There are strong ligaments in the front and rear part which join the pelvis to the sacrum, and the pubic bones to each other, thus providing the pelvis with its uniquely stable ring structure.
Major nerves, blood vessels, and portions of the bowel, bladder, and reproductive organs all pass through and lie within the pelvis which protects these important structures from injury. The pelvis also serves as an attachment for the muscles of the spine, hip, thigh, and abdomen.
Description of the injuries
A ring usually breaks in two places. So a fracture or disruption / dislocation in one part of the ring structure is often accompanied by a fracture or damage to ligaments at another point in the ring. It is important to get appropriate X-rays and sophisticated imaging such as CT scans to ensure that all components of the injury are correctly diagnosed.
Fig 1 showing 3 D CT scans of a pelvic injury Orthopaedic surgeons like to classify injuries to make it easier to describe them, communicate with each other, and help plan treatment. It is important to recognise the common patterns and not underestimate the severity of the injury. Particularly it is important to diagnose the injury at the posterior or rear part of the pelvic ring.
There are many types of pelvic fracture patterns. The specific pattern of the fracture depends upon the direction and the amount of force that caused the injury. Common mechanisms include forces from the front (anteroposterior compression as in a motorcyclist colliding against a wall), from the side (lateral compression as in a side impact collision, or a pedestrian hit from the side) or in a vertical direction (vertical shear as in fall from a height). There can also be combination of these mechanisms (such as being hit and then roll-over). This was described in detail by Young and Burgess.
Pelvic ring injuries are usually described as mechanically "stable" or "unstable," (Pennal and Tile) based on how much damage has occurred to the structural integrity of the bones and ligaments that make the ring stable. In stable patterns, the ring structure is maintained despite the fracture. The broken bones usually remain undisplaced or minimally displaced and well-aligned. The key feature is that the ring is stable.
In unstable fracture patterns, there is often displacement of the broken components, leading to either partial rotational or complete (multidirectional) instability. This type of fracture is more likely to occur due to a highenergy event. A mechanically unstable injury can be lifethreatening and requires urgent surgical treatment to stop internal bleeding.
A pelvic fracture may also occur due to weak or insufficient bone. This is most common in older people whose bones have become weakened by osteoporosis. In these patients, a fracture may occur even after a fall from a standing height, or similar low energy trauma. These injuries are typically stable fractures that do not damage
the structural integrity of the pelvic ring, but may fracture an individual bone. Some sacral insufficiency fractures are only diagnosed after MRI scans
Less commonly, one sees an avulsion fracture where a piece of the pelvic bone attached to a strong muscle such as the anterior inferior iliac spine, or the ischial tuberosity gets pulled away due to sudden muscular contractions. This is most common in young athletes who are still growing. An avulsion fracture does not usually make the pelvic ring unstable or injure internal organs. Many of these may heal without need for surgery, but some displaced fractures may need surgery.
Treatment principles
Patients with high-energy fractures will almost always be brought to a major trauma centre or trauma unit for initial treatment. In the UK trauma system most patients are now brought to the casualty with a pelvic binder applied by ambulance personnel on the scene of injury. This circumferential binder wrapped around the pelvis and hips at the scene of injury, helps to keep the pelvic ring closed and can save lives by controlling internal bleeding.
These patients may also have additional injuries to the head, chest, spine, abdomen, or legs. If their injuries cause significant blood loss, it could lead to shock—a lifethreatening condition that can result in organ failure.
A multidisciplinary approach to their treatment with input from a number of medical specialists is required. Life threatening injuries must be addressed promptly. Airway, breathing, and circulatory problems are treated as a priority. Various specialised x-rays and imaging studies such as CT scans are required to comprehensively analyse the fracture patterns.
In many low energy cases nonsurgical treatment may be appropriate for stable fractures in which the bones are nondisplaced or minimally displaced. This usually involves a short period of rest untill pain can be controlled and gradual supervised mobilisation with the help of walking aids. If there is no risk of serious bleeding, in most cases some form of anti-coagulant, or blood thinning medications are given to reduce the risk of blood clots forming in the veins of the legs and pelvis and travelling to the lungs.
Surgical Treatment is usually required for unstable and displaced pelvic fractures. In the emergency scenario, an external fixator can be used to temporarily stabilise the pelvic ring and control bleeding. In this operation, metal pins or screws, projecting through the skin externally, are inserted into the bones through small incisions on both sides of the pelvis and then connected to connecting bars outside the skin using clamps. In some cases, an external fixator is used as the main definitive method until healing is complete.
Fig 2 external fixator applied to the pelvis In other cases it may have to be combined with skeletal traction to the leg. In this technique a metal pin is inserted through the distal femur (above the knee joint area) or proximal tibia and connected to weight via a system of pulleys. This is used temporarily before surgery, and also during surgery to help realign the pelvic bones.
The definitive treatment of unstable pelvic ring injuries consists of closed, mini-open (percutaneous) or open (making a formal incision) reduction (correct repositioning and realigning of the broken bony fragments) and internal fixation using a combination of different types of plates and screws inserted into the pelvic ring, both in the front and also in the back of the ring, to stabilise it completely.
Fig 3 and 4 showing some of the pelvic fixation techniques There are risks associated with any surgical procedure such as wound healing problems, infection, malalignment, damage to nerves or blood vessels or internal pelvic organs amongst several other risks. These are recognised complications which are explained to the patient before surgery. Medications are administered after pelvic surgery to prevent clots in the legs and lungs.
After surgery, the aim is to appropriately rehabilitate the patient and help return to as normal a function as possible. This is done by trained physiotherapists by means of specific exercises to help regain flexibility, strength and movement. A period of protected weight bearing is also usually required after surgery in many cases. In many litigated cases, increasingly nowadays a case manager is appointed to oversee and coordinate multidisciplinary rehabilitation requirements.
Pelvic fracture surgery is a specialised branch of orthopaedic trauma surgery performed in regional pelvic trauma centres by trained orthopaedic surgeons and teams who handle a high volume of such cases. Other vital members of such trauma teams include vascular surgeons, plastic surgeons, Urologists, general surgeons,
interventional radiologists, Anaesthetists, pain specialists, and intensive care specialists amongst others.
With correct diagnosis, timely intervention in life threatening injuries, expert definitive management, and active rehabilitation, good functional results can be obtained in these severely injured patients, who are often in the young age group.
However a complete recovery may not necessarily occur in all the patients, particularly after significant injuries. Some may continue to have varying degrees of residual discomfort or pelvic pain or functional problems such as a limp in the long term.
Particularly, injuries to the neurological structures within the pelvis and also urological injuries (the bladder and urinary passage) can be responsible for poor long term results. Many patients also suffer from sexual dysfunction, because of damage to nerves within the pelvis. Most regional centres have specialist urologists who deal with the urological injuries that occur in association with pelvic fractures.
Recent changes to the manner in which trauma services are configured and delivered within the UK, over the last few years, and an emphasis for severely injured patients being promptly taken to regional trauma centres with multidisciplinary trauma teams, has resulted in improved outcomes and reduced mortality from such injuries. Mr Shah can be reached on: Nikhil.shah@consultantcare.com
Fig 1- a 3 D - reformatted CT scan which creates a virtual image of the pelvis and allows accurate assessment of the injury in 3 dimensions to plan treatment. In some cases of difficult fracture patterns, 3 D printed models can be made to help plan the surgical technique. Fig 3 - an unstable type C pelvic ring injury being fixed with plates on the front to the symphysis pubis and percutaneous screws to stabilise the fracture of the sacrum on both sides.

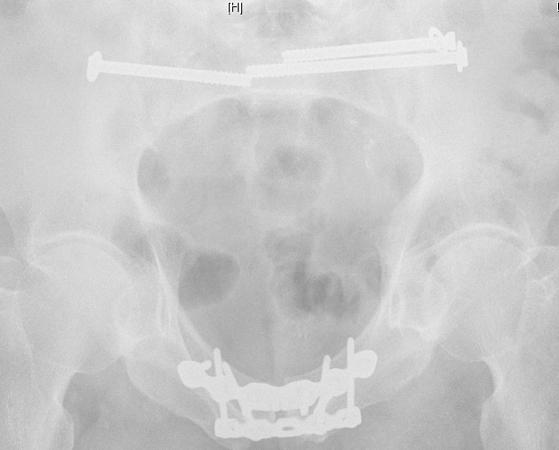

Fig 2 - external fixator applied to the pelvis to try and close the unstable pelvic ring. Fig 4 - an unstable pelvic ring injury treated with symphysis plates and plates to stabilise a right sacro-iliac joint disruption at the back of the ring.

Mediation in uncertain times:
Justice, Fairness and Responsibility
This annual event is a must for mediators of all types and levels, as well as those looking to find out more about this form of dispute resolution. Topics covered will include:
• Carrot and Stick: defining the right role for
mediation in the justice system with Dr Sue Prince
Associate Professor of Law, Exeter University • Insights into implementing mediation schemes with
Karl Cockerill, Health and Wellbeing Practitioner and
Mediation Coordinator ELHT NHS Trust
• Securing your online presence with Charles
Sowden, marketing and branding specialist.
• Parallel Skills Workshops – expanding your mediation practice:
1) Elder and Vulnerable Adult Mediations 2) Women as mediators: Expanding your skills and influence
3) Family Business, Family Battles 4) Crisis Bites: Topical challenges for commercial mediators. How they might be mitigated and resolved.
Running from 9.15am to 5.30pm, the conference will share with you important insights into the various applications of mediation - from the courts, to the office, and to home. Bring a ‘non-mediator’ friend to receive a discount. With a great array of highly experienced speakers this event is not to be missed.
BOOK NOW
Pre-conference Dinner booking:
Places are strictly limited. Please book early to secure your place and avoid disappointment.
BOOK Pre-conference Dinner













