8 minute read
Environmental factors and auto-immune diseases – a hypothesis / Henrik Nielsen
Environmental factors and autoimmune diseases – a hypothesis
The use of pesticides and chemicals may give us new insights and predictions about the human intestinal virome’s handling of chronic diseases, for example, COVID19, using cytochrome polymorphism as a measurement.
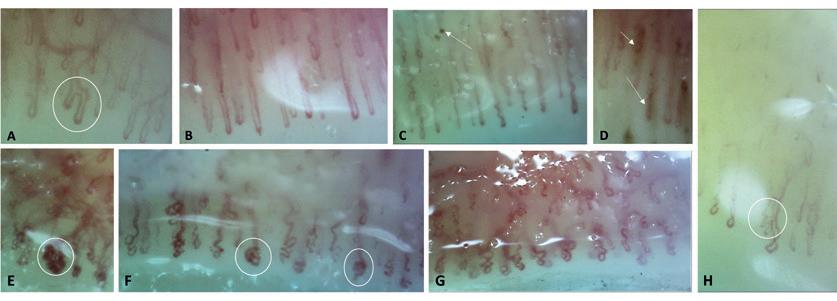
HENRIK NIELSEN is a rheumatologist and specialist in internal medicine and rheumatology. He holds several research and advisory positions in rheumatology. His professional interests cover environmental issues, and he works to promote awareness of the negative impact of pesticide use on autoimmune diseases. MERETE ENGELHART is a specialist in internal medicine and rheumatology at Department of Rheumatology, Gentofte and Center for Rheumatology and Spine Diseases, Rigshospitalet, Denmark. Her research is focused on connective tissue diseases, Raynaud Phenomenon, and connective tissue lung diseases.
For many years, the dialogue involving rheumatic diseases has focused on triggers involving environmental factors combined with viral components in the body; the triggers reactivating the sleeping virus, also called “the human intestinal virome.” But the interplay is poorly understood between environmental factors and possible viral components. The use of pesticides, chemicals, and other factors may give us new insights into chronic diseases, especially if these diseases arise at an earlier living age resulting in new manifestations.
Organophosphate pesticides
Organophosphate pesticides (OPs) are among the most widely used synthetic chemicals for the control of a variety of pests. Reactive oxygen species (ROS) caused by OPs might be involved in one of several toxicities of various pesticides. Previous studies have demonstrated that the reactivation of Epstein-Barr virus (EBV), latent in the human body (>95%), could involve oxidative stress. In one study, OPs were able to reactivate EBV through ROS accumulation. Data showed that OP (chlorpyriphos, abbreviated as CPF) induces oxidative stress, accom-
panied by an increase in ROS production, DNA damage, superoxide dismutase and catalase activity. Moreover, CPF exposure significantly enhances the expression of BZLF-1.1 These results suggest that OPs could contribute to the reactivation of the EBV lytic cycle through ROS induction, a process that may play an important role in the development of EBV-associated diseases as well as other rheumatic diseases.
EBV is a well-known factor in the mechanism in systemic lupus erythematosus (SLE)2, taking part in the crosstalk between the enterovirus. But reactivation of EBV because of pesticide exposure in SLE has not been reported.
A postulate that rheumatoid arthritis could be an occupational disease has been open for discussion in past years3 – but bigger population studies are needed to confirm this hypothesis.
Due to the overuse of pesticides, OP-residues have contaminated drinking water, grains, vegetables, fruits, and other food items, and for many years this has provoked a global health concern about potential neurological disorders.4 These chemicals block the activity of acetylcholine esterase at synapses, leading to a disproportionate accumulation of the neurotransmitter acetylcholine.
Moreover, recent investigations have linked OPs to several biological responses mediating severe toxic outcomes. Studies have suggested OP compounds have an “immunotoxin” potential in human and non-target organisms5, representing an unseen risk of escalating SARS-COV-2 pathology.
A major determinant of the biotransformation of OPs and other pesticides is our body’s detoxification system, the cytochrome (CYP) P450 gene families. Genetic polymorphism in CYPs is known to alter metabolic pathways and induce false cellular response. CYP polymorphism has been considered to be an important risk factor for various pathological conditions induced by chronic organochlorine exposure.6 Racial disparity CYP polymorphism and mortality due to COVID-19 have been reported in the United States, where the mortality rate is 3.6 times higher in the African-American population compared to other ethnic individuals.7 The gene/environment interaction between CYPs and OP exposure might induce oxidative stress (OS) and increase the susceptibility to SARS-CoV-2 infection. Pesticides like organochlorines impair cellular and humoral immunity, increasing mortality by infectious diseases8. This represents a new potential trigger with a badly understood mechanism. Contact with environmental chemicals can result in clinical warning signals that arise either later or acutely. For example, exposure to carbamates (OP) is followed by hypersensitivity reactions, inflammatory/chronic manifestations, or cancers. Short-term exposure to atrazine, a widely used herbicide, can persist for a longer duration even after termination of the exposure.9
The agricultural uses of OP pesticides are gaining in popularity, and they account for more than 30% of global insecticide sales. The global market for sales of OP pesticides is expected to grow by a compound annual growth rate of 5.5% during the period 2018–2023.10
Unfortunately, in many developing countries, OPs are being used indiscriminately in ways that could further amplify unintentional exposure to these compounds.
Systemic lupus erythematosus
The etiology of SLE is not well understood, but it is known that certain demographic groups are more affected than others. SLE is significantly more common among women; approximately 90% of patients diagnosed with SLE are women.
The prevalence of SLE is also significantly higher in African Americans compared to West Africans. Previous data has shown a two-fold increase of SLE in the urban population of African American adult women. This suggests that environmental factors in western culture (e.g. OP or other factors) could play a key role in SLE pathogenesis in African Americans.11
As discussed, the decreased anti-viral defense due to CYP polymorphism could further support the hypothesis that external triggers like OP affect different cultures disproportionately. No data however has demonstrated a link with CYP polymorphism indicating a possible genetic factor or COVID-19/EBV prevalence.
Over time, environmental factors that have been implicated in the development of e.g. SLE include crystalline silica, cigarette smok-
CONCLUSION: To summarize, we have limited understanding of whether diseases such as SLE or other manifestations (child adiposity,16 Gulf War illness (GWI),17 chronic fatigue syndrome18 …) present themselves at an earlier living age following exposure to environmental factors. Likewise, our understanding is limited as to whether environmental factors can alter the body’s natural defense mechanism – “the human intestinal virome” – so it will attack the body instead of defending it, thereby escalating SARS-COV-2 – pathogenicity.
ing, environmental pollutants, infections, sex hormones and other factors.12 Studies of (NZB x NZW) F1 lupus-prone mice have pointed to a role of chemicals (silica) in the pathogenesis of SLE13 and human smoking14 although the evidence in human observational studies has been limited until now. Clear evidence has been missing for ethical reasons. Further studies are needed to examine any potential relationship between exposure to pesticides/chemicals via e.g. food intake and CYP polymorphism as exemplified by the SLE model. Whether or not changes in the human intestinal virome result in a defense or attack mechanism is just at the beginning of our understanding.15
References:
1. Zhao L, Xie F, Wang T-T, et al. Chlorpyrifos Induces the Expression of the Epstein-Barr Virus Lytic Cycle Activator BZLF-1 via Reactive Oxygen Species. Oxid Med Cell Longev. 2015;2015: 309125. DOI:10.1155/2015/309125. 2. Blank M, Shoenfeld Y, Perl A. Cross-talk of the environment with the host genome and the immune system through endogenous retroviruses in systemic lupus erythematosus. Lupus. 2009 Nov;18(13): 1136-1143. DOI:10.1177/0961203309345728. 3. Murphy D, Hutchinson D. Is Male Rheumatoid Arthritis an Occupational Disease? A Review. Open Rheumatol J. 2017 Jul 27;11: 88-105. DOI:10.2174/1874312901711010088. 4. Abou-Donia MB. Organophosphorus ester-induced chronic neurotoxicity. Arch Environ Health. 2003 Aug;58(8): 484-497. 5. Rajak P, Ganguly A, Sarkar S, et al. Immunotoxic role of organophosphates: An unseen risk escalating SARSCoV-2 pathogenicity. Food Chem Toxicol. 2021 Mar;149: 112007. DOI:10.1016/j.fct.2021.112007. 6. Docea AO, Vassilopoulou L, Fragou D, et al. CYP polymorphisms and pathological conditions related to chronic exposure to organochlorine pesticides. Toxicol Rep. 2017 May 26;4: 335-341. DOI:10.1016/j. toxrep.2017.05.007. 7. Parpia AS, Martinez I, El-Sayed AM, et al. Racial disparities in COVID-19 mortality across Michigan, United States. EClinicalMedicine. 2021 Feb 26;33: 100761. DOI:10.1016/j.eclinm.2021.100761. 8. Krzystyniak K, Tryphonas H, Fournier M. Approaches to the evaluation of chemical-induced immunotoxicity. Environ Health Perspect. 1995 Dec;103 Suppl 9(Suppl 9): 17-22. DOI:10.1289/ehp.95103s917. 9. Filipov NM, Pinchuk LM, Boyd BL, Crittenden PL. Immunotoxic effects of short-term atrazine exposure in young male C57BL/6 mice. Toxicol Sci. 2005 Aug;86(2): 324-332. DOI:10.1093/toxsci/kfi188. 10. Mordor Intelligence. Global organophosphate pesticide market – segmented by active ingredients, product type, application, and geography – growth, trends, COVID-19 impact, and forecasts (2021-2026). https://www.mordorintelligence.com/industry-reports/organophosphate-pesticides-market [Accessed 15.3.2022]. 11. Williams JN, Chang SC, Sinnette C, et al. Pesticide exposure and risk of systemic lupus erythematosus in an urban population of predominantly African-American women. Lupus. 2018 Nov;27(13): 2129-2134. DOI:10.1177/0961203318805844. 12. Barbhaiya M, Costenbader KH. Environmental exposures and the development of systemic lupus erythematosus. Curr Opin Rheumatol. 2016 Sep;28(5): 497-505. DOI:10.1097/BOR.0000000000000318. 13. Bates MA, Brandenberger C, Langohr I, et al. Silica Triggers Inflammation and Ectopic Lymphoid Neogenesis in the Lungs in Parallel with Accelerated Onset of Systemic Autoimmunity and Glomerulonephritis in the Lupus-Prone NZBWF1 Mouse. PLoS One. 2015 May 15;10(5): e0125481. DOI:10.1371/journal.pone.0125481. 14. Leffers HCB, Troldborg A, Voss A, et al. Smoking associates with distinct clinical phenotypes in patients with systemic lupus erythematosus: a nationwide Danish cross-sectional study. Lupus Sci Med. 2021 Apr;8(1): e000474. DOI:10.1136/lupus-2021-000474. 15. Carding SR, Hoyles ND. The human intestinal virome in health and disease. Aliment Pharmacol Ther. 2017 Nov;46(9): 800-815. DOI:10.1111/apt.14280. 16. Warner M, Ye M, Harley K, Kogut K, Bradman A, Eskenazi B. Prenatal DDT exposure and child adiposity at age 12: The CHAMACOS study. Environ Res. 2017 Nov;159: 606-612. DOI:10.1016/j.envres.2017.08.050. 17. Seth RK, Maqsood R, Mondal A, et al. Gut DNA Virome Diversity and Its Association with Host Bacteria Regulate Inflammatory Phenotype and Neuronal Immunotoxicity in Experimental Gulf War Illness. Viruses. 2019 Oct 21;11(10): 968. DOI:10.3390/v11100968. 18. Naviaux RK, Naviaux JC, Li K, et al. Metabolic features of chronic fatigue syndrome. Proc Natl Acad Sci USA. 2016 Sep 13;113(37): E5472-5480. DOI:10.1073/pnas.1607571113.