9 minute read
Palliative Care
focus

Advertisement
Leaving No One

Behind
Dr. Zulkhairi Mohamad & Dr. Asmah Husaini
Living well and being healthy is an aspiration that we all have. In this modern era, we have seen major medical advancements in treating what used to be untreatable. The media often portrays cases of young children with cancer who receive trial treatments and are then declared cancerfree. Television shows such as Grey’s Anatomy portray heroic medical measures to save patients’ lives. In reality, not everyone can be saved. With media coverage focusing only on the positive side of medicine, it is not uncommon for society to have a false perception that medicine can cure all illnesses. The incidences of cancer and other non-communicable diseases such as diabetes and heart failure in Brunei Darussalam have shown an alarming trend.
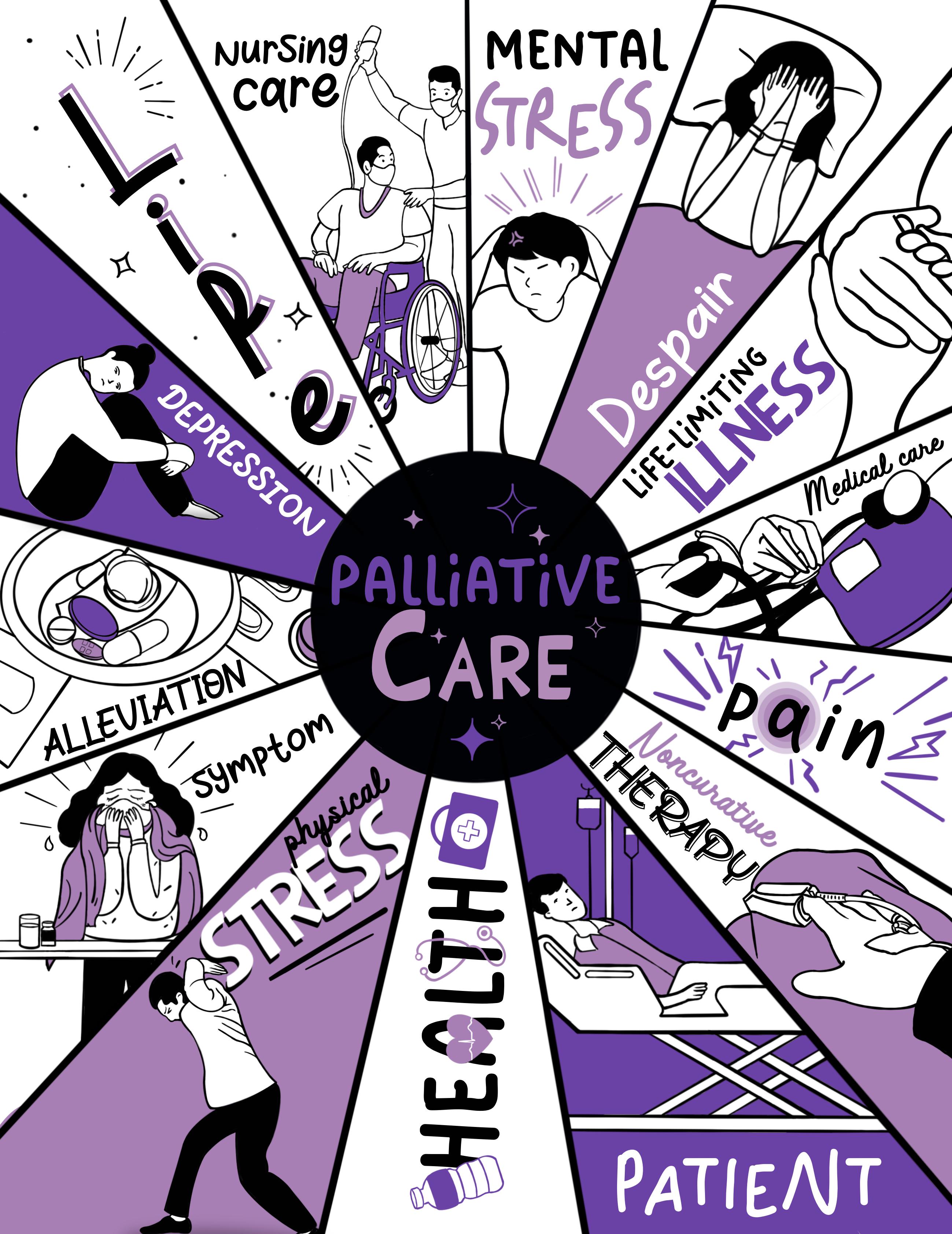
Medicine, according to the Oxford dictionary, is defined as a drug or other preparation for the treatment or prevention of disease, but what is often overlooked is the other side of that definition. Medicine also provides relief from pain and suffering – a specialty known as Palliative Care. The World Health Organization (WHO) defines this as an approach that improves the quality of life of patients and their families facing the problems associated with life-threatening illness, through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other associated problems. The Ministry of Health understands this given our aging population, and cancer being one of the top 5 causes of death in the Sultanate, hence its incorporation into the Brunei
Darussalam Multi-Sectoral
Action Plan for prevention and control of non-communicable diseases (BruMAP NCD).
This field is a specialty that was started in 2009. Our main focus is to relieve pain and control symptoms suffered by people with advanced and chronic illnesses to improve their quality of life and that of their families. In 2010, the RIPAS Palliative Care Unit established the Palliative Care Helpline along with the Geriatrics team. This allows discharged patients and their families to address any concerns directly to doctors or nurses via phone calls or messages without the need to visit clinics or hospitals. Relevant advice is given to reduce unnecessary hospital admissions and allow patients to have more quality time
at home with their loved
ones. World Palliative Day is celebrated annually on the second Saturday of October. This year it fell on October 9th, with the theme of: Leave no one behind - equity in access to palliative care.
What exactly is palliative care & medicine?
In a nutshell, palliative care aims to improve patients’
quality of life by managing
their symptoms. Advanced illnesses such as cancer or multiorgan failure causes pain, breathlessness, and a

general weakness, which can cause a great deal of suffering to patients and their family members. When symptoms are appropriately managed, patients can enjoy a good quality of life, while spending their time doing what is important to them.
Social, psychological, and spiritual aspects such as angst are also given equal weight. These aspects of health are assessed and managed at the earliest possible stage to avoid suffering. This is possible because of the multidisciplinary teams involved, which consist of doctors, nurses, medical social workers, physiotherapists, occupational therapists, and an Ustaz/ Ustazah. The approach is a holistic one, as this specialty focusses not just on a diseases’ effect upon a physical body but rather the impact of it on a patient as a whole.
As this specialty recognises that death is part of life. It is important for palliative care teams to ensure patients leave this world with dignity when their time comes. Dignity here means, not being in pain, being calm, in acceptance, and most importantly surrounded by their loved ones. However, one of the challenges of achieving a peaceful end in the hospital setting is the continuous treatment of a disease that can cause additional sources of suffering to the patients. One issue often overlooked by all involved is whether a particular medical intervention is beneficial. Like many things in life, medicine has its limits. To decide to stop a treatment that no longer serves the purpose to cure an illness or disease is one of the most difficult decisions that one would have to make. The dilemma of choosing between quantity and quality of life often leaves patients in a state of receiving treatment just to prolong life despite not curing the illness. Often, this leads to more suffering than wellness.
So, does palliative care mean a person is dying?
Palliative care provides relief from pain and other symptoms of serious illness – at any stage of that illness. It is an
option for a wide variety of illnesses
including Human Immunodeficiency Virus (HIV) or Acquired Immune Deficiency Syndrome (AIDS), Chronic Obstructive Pulmonary Disease (COPD), Parkinson’s Disease, Alzheimer’s Disease, Systemic Lupus, Multiple Sclerosis, Diabetes, and heart disease. Palliative care teams reduce
unnecessary aggressive medical treatment and
hospital admission that increase patients’ suffering. Research shows that reduction of these 2 points leads to extending the life of people with incurable and advanced illnesses. It is a very common misconception that Palliative care starts when treatment stops. In fact, palliative care can begin at the time of diagnosis of a life-limiting illness and can co-exist along with the active treatment that aims to cure the disease. It provides an extra layer of support and care for the patients in question. In the early stages of serious illnesses, patients can continue to pursue aggressive, curative treatment, while receiving palliative care. In fact, palliative care is often used to treat side effects from curative treatments like chemotherapy or radiation, maintaining patients’ good quality of life during treatment.
Dr. Zulkhairi Mohamad
Does palliative care speed up the process of dying?
Another common misconception is that palliative care hastens death via strong medications. In reality, medications are prescribed to provide comfort and the best quality of life from diagnosis of an advanced illness until the end of life. Common medications used by palliative care include opioids like Morphine, sedatives, and other symptomatic medications such as those that control breathlessness, nausea, and vomiting.
Isn’t Morphine addictive?
The mere mention of Morphine can be enough to conjure up all sorts of negative thoughts. Some patients may be afraid of becoming addicted while others may think that only those ready to die should take it. There is a stigma
with the use of opioids
among doctors too, largely due to misinformation and lack of training in this discipline. Morphine is effective and safe for the treatment of pain, which does take a toll on all aspects of a person’s life. Fortunately, almost all pain can be alleviated with the drugs available today.
No one should suffer
because they (or their doctor) are afraid to use Morphine or other opiates. Palliative care doctors have the capacity to manage the type of medication and dosage suitable to control the pain or physical symptoms of individual patients.
Dr. Asmah Husaini

“Don’t tell my family about this illness, or else they will lose hope”
It is not uncommon for close family members to protect their ill loved ones from incurable diagnosis due to the fear of them feeling depressed and losing all hope. According to a study conducted by Dr. Asmah
Husaini from the Universiti
Brunei Darussalam, she found that healthcare workers being asked by family members to hide the diagnosis of their sick loved ones, for fearing that it would cause distress and the loss of hope, is a common scenario. This request is often honoured by doctors with some ethical reluctance. We understand families do this with the best of intentions.

Dr. Asmah found that cancer patients who
were accepting of their
illnesses went through a series of spiritual coping mechanisms throughout their journey; from when they were diagnosed, planned and underwent treatment, to when they had to stop treatment and eventually passed. She found that we live in a hopeful society. With this belief, it is important that despite being diagnosed with an incurable illness, to continue seeking treatment for their condition. Palliative care teams treated their patients and families with this exact mindset. They would encourage the patients to seek treatment, but slowly
introduce the concept
of acceptance, to embrace their illness during their consultations. This is to prepare them for the day when their body is no longer able to withstand the medical treatment. These consultations are often done over a period of time, until patients and families develop trusting therapeutic relationships with their caregivers.
When doctors, nurses, patients, and families are on the same page about an illness and treatment plan, it is more likely patients will embrace acceptance of their situation. Feeling spiritually supported has often enabled patients to talk about their wishes and plans before they die. Being able to express this in a safe environment with support and compassion has also become a form of therapy for patients. The study concluded that early referrals to palliative care teams would highly likely enable them to
support patients according
to cultural norms and plan better interventions and care to ensure patients were comfortable right to the end.
A palliative care medical professional by the bedside of an elderly patient
How do I get in touch with palliative care service?
If you feel you need the type of support described above, you can speak to your attending doctor to discuss if a referral to a palliative care team is appropriate. Upon referral, you will be assessed by one of our doctors. This assessment seeks clarification, to offer other potential treatment options and outcomes that the patient may not have considered before. We want and need to know and understand how you are affected by the illness from your point of view. Following the assessment, the team comes up with a treatment plan in which we can bridge the gap between your care and treatment preference and the support we can give. The central aspect of this discipline is to understand the person and their values. We are a family orientated nation. Issues affecting the patient’s loved ones and surrounding caregiving will also be explored.
Is Palliative care only provided in hospitals?
In 2011, our unit extended its service to Palliative Nurse Home Visits. This service is meant to offload the burden of patients whom illnesses have caused them to be bedbound. Palliative nurses have made scheduled home visits to patients, with long-term medications picked up by patients’ relatives at the nearest government healthcare clinic. This service is currently limited to the Brunei-Muara district for the time being but plans are in place to extend the service in other districts. We are still in the continuous stage of improving our service in this specialty and hope to implement more advancements in the near future.