6 minute read
Baptist Health-UAMS Collaboration on Cancer Care Sees Continued Growth
Baptist Health and UAMS continued to collaborate in 2022 on expanding access to essential, innovative cancer care and exploring opportunities to serve additional patients across the state.
In 2021, Baptist Health and UAMS—two of the state’s most-trusted, leading health care organizations—announced that they would be uniting to deliver state-of-the-art cancer treatments with the most innovative technology available in Arkansas.

Knowing that cancer is complicated, the partnership allows both health care systems to operate in an evidence-based environment and to have a high degree of alignment. It also helps to reach more Arkansans and diffuse more knowledge into care pathways for tomorrow.
This year saw even more growth between Baptist Health and UAMS on the cancer front, including physician collaboration to ensure that providers have a clear expectation when it comes to services. Another goal for 2022 was to establish leadership and providers as a means to high-quality, reliable, and safe oncology services.
John Goodman was appointed as Baptist Health’s corporate vice president of oncology, pharmacy, and respiratory services this year. Goodman now steers cancer services for all of Baptist Health and leads development and execution of cancer services in partnership with the Winthrop P. Rockefeller Cancer Institute at UAMS.
Sunny R. K. Singh, M.D., joined the University of Arkansas for Medical Sciences (UAMS) Winthrop P. Rockefeller Cancer Institute this year as a hematologist/oncologist and director of the UAMS Baptist Health Cancer Center in North Little Rock.
Established providers add another level of sophistication, bringing years of focus on specific concerns such as breast, lung, brain, and colorectal cancer.
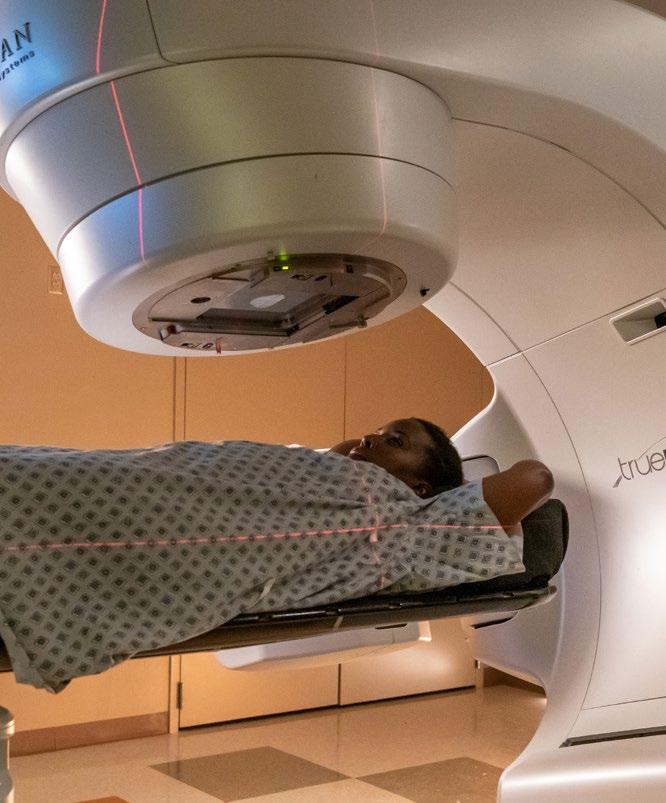
UAMS Baptist Health Cancer Center in North Little Rock on the campus of Baptist Health Medical Center-North Little Rock provides hematology, medical oncology, infusion, and radiation therapy services for most cancer types.
Not only does the center provide these services, but it allows for a more complete continuum of care for cancer patients by allowing specialists to work in coordination with surgical and non-surgical providers on the hospital’s campus.
UAMS Baptist Health Cancer Center in North Little Rock also offers Surface Guided Radiation Therapy (SGRT), which particularly benefits patients with cancer of the left breast, as it can help the radiotherapy team reduce the radiation dose to the heart.
In 2023, Baptist Health and UAMS will open a new medical oncology clinic in the Hickingbotham Outpatient Center on the campus of Baptist Health Medical CenterLittle Rock. The clinic will manage the full spectrum of options for cancer patients such as prescribing the appropriate chemotherapy and leading a multi-discipline approach to address all of a cancer patient’s health needs. A 32bay infusion center is also set to open in the outpatient center.
Work on Arkansas’ first Proton Center— collaboration between Baptist Health, UAMS, Arkansas Children’s, and Proton International— also reached pivotal milestones this year.
A type of particle accelerator that serves as a key piece of the center’s equipment, a cyclotron, was installed in October at its future home on the UAMS campus as part of the $65 million project.
When completed, the Proton Center of Arkansas will offer an advanced form of radiation treatment that uses precisely focused protons to target tumors, rather than photons used in standard X-ray radiation. Proton radiation is more effective in treating some cancers, particularly those in close vicinity of critical organs for which conventional radiation can be too toxic. For patients, that means fewer and less severe side effects, faster recovery time, and an overall better quality of life.
The Proton Center is expected to begin treating patients in September 2023.
Additional opportunities ahead for the Baptist Health-UAMS partnership include UAMSsponsored clinical trials for chemotherapy and radiation therapy.
The center’s opening furthers the partnership’s goal of leveraging Baptist Health facilities across the state to expand cancer care and elevate the level of care that Arkansans have come to expect from both long-standing names in health care.

It was a busy 2022 for Baptist Health’s Population Health Services Organization (PHSO) and value-based care initiatives with the overall goals to lower the cost of care, improve health care quality, and reduce health care disparities making great progress.


The PHSO efforts are highly aligned to Baptist Health’s mission and focused on where the system wants to be in the communities it serves—helping people who are suffering from health issues and improving their health in a proactive way.
One of the biggest accomplishments of 2022 was putting together a care management team to fully guide these efforts. The team involves a collaboration across many disciplines including RNs, LPNs, medical assistance, social navigators, mental health specialists, pharmacists, and pharmacy technicians.
Another big accomplishment of 2022 was redoing contracts with payers to better support population health in a way that sustains the work going into the future.
Additionally, the Accountable Care Organization partnership with UAMS has been paid more than $10 million in the past two years since the PHSO’s start for creating Medicare shared saving, a huge reward for a lot of work in creating quality improvements in diabetes care, blood pressure control, and cancer prevention.
Managing Care and Managing Contracts
Population health efforts can be summarized on two sides—managing care for patients and managing contracts with providers and payers.
During the transition of care from hospital to home, it is easy for the coordination of care to get lost. Patients receive instructions from providers about what to do after discharge, and then they go home and discover they did not understand them or do not remember everything in the midst of being sick and having their life and family’s lives disrupted.
Solving problems that arise during transition of care is one key to improving outcomes after discharge because many adverse health problems can occur if a patient is unable to follow directions from the provider or take the proper medication.
But transition of care is just one issue to be solved. Patients also need help in other areas such as:
Behavioral health integration—There’s more than a small chance that people who have a lot of chronic diseases are going to have depression or anxiety either brought with them to those diseases or created because of those diseases. Behavioral health integration can be a critical component to improving physical health.
Social needs—Some patients don’t have transportation. Some can’t afford the high-cost medicine they were just prescribed. Some are experiencing food insecurity issues. Some don’t have a safe place to walk after being told to exercise. Some don’t have access to a nearby grocery store that has adequate healthy foods. Social navigators are able to help with these needs.
Preventive needs—Patients often have a list of preventive instructions, and home outreach specialists are there to help with those. Pharmacists can help with the medication and determine if there is a way to lessen the number of prescriptions or find a cheaper version of an expensive medication.
Equity issues—If there is a higher mortality rate in certain racial, ethnic, or economic group, it is important to solve those outcome disparities. These efforts can be hard to maintain, however, when there is not a direct financial resource to fund them. However, identifying health equity issues and targeting groups with higher incidence of disease can in the end create revenue within an incentived contract and maintain the resource so that it becomes sustainable for others and can then be replicated to serve more people
Managing patient care on an individual level and getting patients the care they can afford is a big part of the equation in population health. But how providers get paid is another big part.
Contracting goals with the PHSO are different than fee for service because there is an incentive to create value for payers and employers by providing better care and doing a better job managing care for members and employees within the health plan. But those incentives and resources must first be negotiated in a contract, and great strides were made during 2022 in doing so.
Every payer has different focuses, so Baptist Health’s PHSO tries to align the same efforts in each one and then work to create one message that goes out to physician clinics asking them to work on certain measures, Their incentives must be changed from volume to value— provide better outcomes and get rid of waste. Baptist Health is there to meet their needs while simplifying things for the physicians and providers.
The PHSO is looking toward new technology, new analytics, and automated outreach to patients to continue all these efforts in population health. But increasing physician engagement by having quarterly meetings and problem-solving performance issues such as readmissions are equally important. Analytics have proven to be important in helping physicians be engaged in opportunities for improvement.









