
5 minute read
Respirasense – digital device transforms care
Innovation a key tool in COVID battle
Respirasense remotely monitors respiration rate to allow for early detection of the deterioration in patient's condition
For Yvonne Whelan and her colleagues on the packed COVID ward of Beaumont Hospital back in March 2020, the new virus taking a foothold was an unpredictable enemy. But an innovative piece of technology gave them a vital boost in their COVID battle.
Respirasense is a monitoring device that measures Respiration Rate (RR) through an electric sensor and allows for early detection of the deterioration in a patient’s condition.
Respirasense sends patient data via
Bluetooth to an iPad on the nurses’ or doctors’ desk. During COVID, patients were placed in isolation rooms and bays, to minimise staff exposure, however this has had the effect of reducing patient visibility.
As an addition to traditional patients monitoring using INEWS, the introduction of Respirascence has allowed for early alert of deteriorating respiratory rate.
Early medical intervention before a patient deteriorates can often mean a greatly improved outcome.
Yvonne, ADON in the Beaumont
Respiratory Service, explained that the 35-bed COVID ward in Beaumont was the first setting to trial the new technology. It has been a major success and is now being used in most hospitals across the country, in both COVID and non-COVID patients.
“We began to use the Respirasense monitors on our COVID patients as they were our highest acuity patients. It is a simple, non-invasive way of monitoring the respiration rate and, from our perspective, it enhances our monitoring of patients and reduces staff exposure to COVID. We were learning so much about the virus all the time and the extra monitoring was a great support,” said Yvonne.
A nurse or doctor can attend to a patient from a safe distance to review RR and trends. This allows for a more rapid intervention. Patients who are physically not close to the desk can be monitored and an alarm will trigger if a patient’s respiratory rate deteriorates. “The device is placed on the patient and we can continuously track the patient’s respiratory rate via the iPad. Any change in respiration rate is immediately flagged and we can respond quickly. It can spot even the most subtle of changes. And in a tracheotomy patient, it can flag early signs of an obstructed airway.”
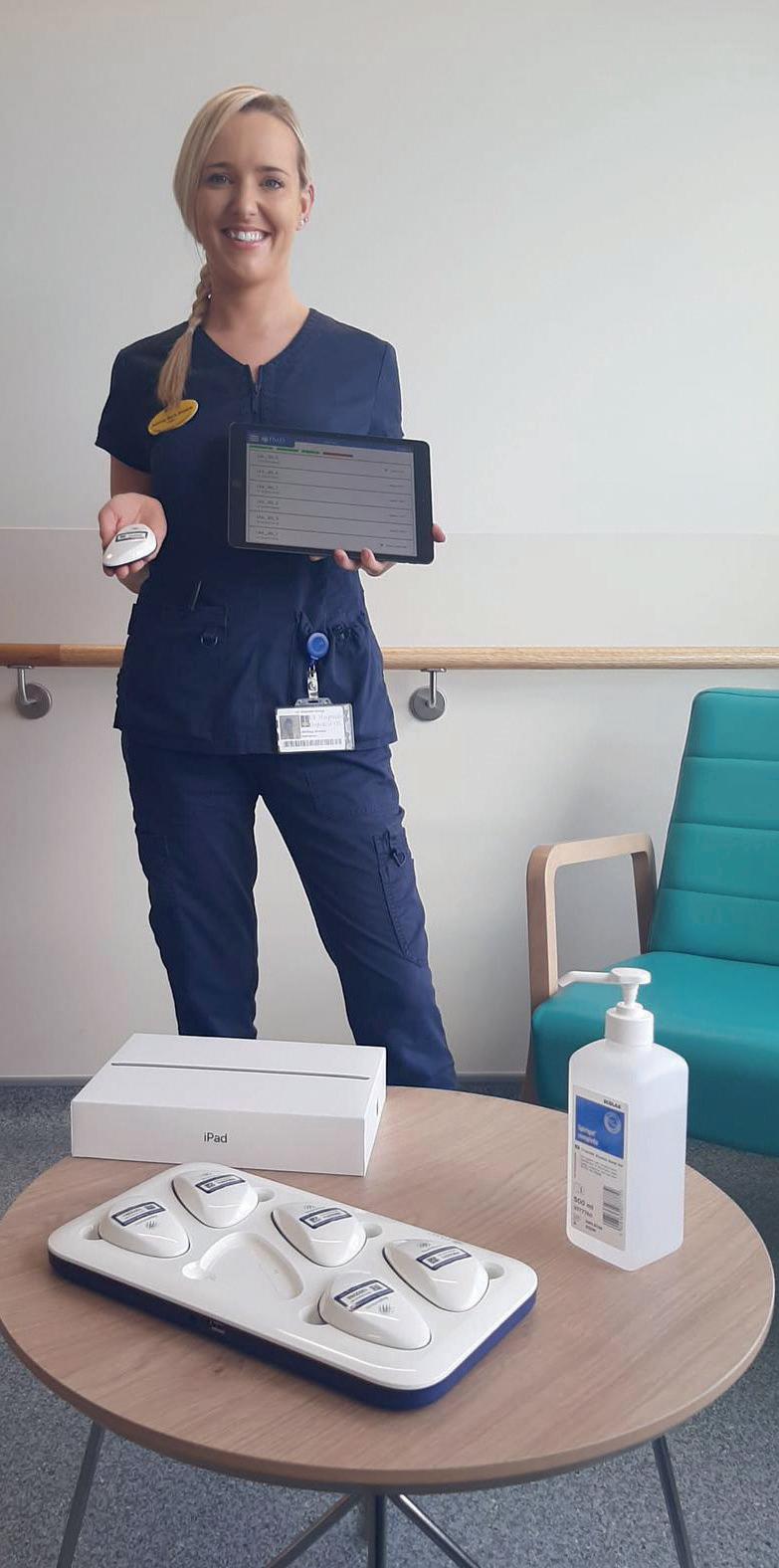
Staff at University Hospital Limerick with the Respirasense devices

She stressed that the new monitoring device does not mean that nursing staff reduce the attention and time given to sick patients.
“This is an additional support but we are still at a patient’s bedside when they need us,” she said.
Respiratory rate is a central part of Early Warning Scoring and is the earliest noninvasive measure of patient deterioration. Traditionally and before this tech solution was used clinical staff manually recorded patients’ breaths which was a less accurate way to record a patient’s respiratory rate.
However, the RR is typically manually counted with more than 80% of measurements being inaccurate leading to over 41% of Early Warning Scores not accurately representing the patient’s true status.
Des O’Toole, Digital Clinical Innovation Lead, HSE Digital Transformation and Innovation, highlighted the importance of the respiratory rate as a vital sign.
“It is estimated when calculating a patient’s respiratory rate – where a clinician stands and physically watches the patient breathing, counting the breaths. But, of course, lots of behavioural things can affect how you breathe when you are being assessed so it’s not always accurate. This is how Respirasense can have an immediate impact. It has the potential to detect deterioration in a patient’s condition 10 or 12 hours earlier than traditional monitoring and every second can be vital,” said Des.
Des is part of the Digital Transformation team within the HSE that is responsible for the ‘innovation pipeline’ that has become even more timely with the onset of the pandemic and the need for reduced physical interactions and social distancing. COVID-19 has led to a massive increase in the use of the technology across the health service as in-person appointments and care are replaced by virtual interactions.
Respirasense was just one of the many technologies that the team had been working on. The technology was invented by PMD Solutions, a Cork biomedical company led by Myles Murray. Its potential to help COVID patients meant it was swiftly rolled out to Beaumont in March 2020.
“We approached Beaumont and made the pitch to them about the device. We provided all the devices and provided the training and supports. The staff have been very open and welcoming to the new way of working and have embraced the technological change. They could see the benefits that it was bringing to them and their patients,” said Des.
Since June 2020, Cork University Hospital (CUH) under the direction of Dr Desmond Murphy, National Clinical Lead for Respiratory, began evaluating the technology in applications for non-COVID respiratory-compromised patients in addition to COVID patients there.
The decision to extend the use of Respirasense to three wards in both CUH and Beaumont was based on the positive impressions by consultant and nursing staff alike on ease of use and insight for clinical decision making.
Dr Murphy said the benefits in the third COVID wave were immediate with the decreased need for PPE and the freeing up of nursing time with so much of the clinical staff missing through COVID leave.
“We were under pressure due to the number of our nursing staff who were out on COVID leave so it was helpful in freeing up some nursing time while continuing to monitor the patient’s respiratory rate,” he said.
He said that the data that has been collected since the introduction of Respirasense across the various hospitals will provide invaluable insight into the treatment of respiratory patients.
Research is in progress as part of the Living Lab in CUH, and the clinical feedback to date, reviewed from more than 200 patients, is positive, said Dr Murphy. Research is on-going to evaluate if less Arterial Blood Gas analysis could be done by using Respirasense to indicate, in a non-invasive and patient friendlier way, whether the treatment is effective or not.












