
36 minute read
Wellness now
Summer self-care
SET ASIDE TIME TO CARE FOR YOURSELF, PHYSICALLY AND SPIRITUALLY
As the summer heats up, calendars fill and backto-school looms large, it’s important to take some time for yourself. Self-care is the time you devote to caring for yourself both physically and spiritually.
SmartHealth is happy to offer no-cost, virtual spiritual care to members and covered dependents. This offering connects you to an Ascension chaplain anytime, anywhere, seven days a week, so it is easy to add to your calendar.
In addition to adding spiritual time to your routine, SmartHealth has developed a list of self-care tasks that can improve any routine so you are feeling your best this season.
FOCUS ON YOUR SKIN CARE
This is a great time to refocus on your skin-care routine. Taking time to wash your face, exfoliate and moisturize can help keep your skin clear and healthy. It’s also good to apply sunscreen daily. According to the American Academy of Dermatology, sunscreen should be used year round, regardless of weather, and should be at least 30 SPF.
SET DAILY QUIET TIME
Another great addition to a daily self-care routine is quiet time. Sectioning off space during the day to reflect, pray, meditate or journal is vital for your mental health. This time could be used for self-reflection or gratitude. If you are looking for a more structured and spiritual setting, this is an excellent opportunity to utilize SmartHealth’s virtual spiritual care service.
GO ON A WALK
With longer days in the summer, you have more time to go outside and enjoy the sunshine (with your sunscreen applied) while getting in some exercise. According to the Centers for Disease Control and Prevention, adults need at least 150 minutes of aerobic exercise weekly to improve health. So, if you are able, scheduling daily times to walk outside can help you stay healthy and is essential to your self-care routine.
Be your best self this summer by focusing on your self-care. The suggestions listed here are just a few examples of focusing on maintaining and improving your health, but find methods that work for you and your lifestyle. With a renewed focus on your health this season, you are on your way to becoming the best version of you.

Experience matters
BEST-IN-CLASS EXPERIENCES WILL HELP DIFFERENTIATE ASCENSION FOR THOSE WE SERVE
With consumers taking more ownership of their healthcare decisions, it’s more important than ever that Ascension focus on providing best-in-class, memorable and shareable experiences grounded in our Mission of serving all.
Ascension already has a strong history of caring about the experience of those we’re privileged to serve, built upon the legacy of the ministry’s historic Sponsors and the commitment of our associates and clinicians. This history provides a solid foundation for revising and renewing our operations and building awareness about how to create truly exceptional experiences — a strategic priority for Ascension.
“Experience is the accumulation of all the interactions a person has with an organization across all touchpoints — human, physical and digital,” said Carol Campbell, Senior Vice President and Chief Experience Officer, Ascension.
Carol notes that best-in-class experiences have two things in common: They consistently deliver on core consumer needs, and they have clearly defined experience differentiators.
“It’s a refinement in the art of listening. Knowing the core behaviors and attitudes of consumers, and what they expect, and then building great experiences that deliver on consumer needs in a way that meets and exceeds those expectations, is what consumer experience, or CX, is all about,” she said.
Elements of this experience include transparency with consumers; providing options to adjust an experience to an individual’s needs and desires; ensuring that people feel that their time is valued; and providing a feeling of being cared for and about — not only in person-to-person encounters, but increasingly in the digital world, a need identified by many associates.
Our digital and technical teams are among several key contributors to this effort. Led by Raj Mohan, Senior Vice President and Chief Digital Officer, Ascension, these teams are working every day to help drive the changes needed to our digital and technical infrastructure as it supports patient encounters such as scheduling appointments, registration across sites of care, billing and other digital experiences that can help demonstrate compassion.
“Our job is to serve those who most directly serve our patients, and while we are deeply focused on improvements to our digital experience and core experience moments, such as access to care, we are also acting upon the feedback we hear from the associates across our ministry, ensuring we’re focusing on the friction points they feel each day so they can better serve our patients,” Raj said.
DELIGHTING CONSUMERS
“The best brands, or organizations, create specific moments that delight the consumer,” Carol said. “These differentiators become a competitive advantage by enhancing the strong base experience they deliver. The most memorable moments come when we can blend human, digital and physical experiences together — they work cohesively and deliver a seamless experience to the consumer.”
In addition to contributions from Ascension Technologies around digital encounters, teams from several disciplines, Ministry Markets and Ministry-wide Functions — including Marketing and Communications, Mission Integration, Human Resources, the Ascension Studio, Finance, Clinical & Network Services, and more — are engaged in efforts across Ascension sites and services to more clearly define what constitutes an exceptional healthcare experience and integrate those concepts into both our human and our digital experiences and dayABOUT CAROL CAMPBELL
Senior Vice President and Chief Experience Officer, Ascension
Carol Campbell has spent more than 25 years in consumer experience (CX), learning as she has led operating teams, development teams and consumer insight teams. She cherishes the diversity of these experiences, and it has allowed her Carol Campbell to build a more structured thought process around CX as a discipline.
Through her nearly 20 years at The Walt Disney Company and more recently with Delta Air Lines, Carol gained a deep understanding of how to build inclusive, customer- centric organizations and activate robust and nontraditional listening techniques to ensure consumer-centricity and employee-centricity toward experience design.
She served as the global leader for Consumer Insight & Global Customer Experience at Delta. As part of Disney, she held numerous leadership positions, most recently leading experience development for Disney’s hotels and other ancillary experiences worldwide.
Carol received a Master of Business Administration degree from the Crummer Graduate School of Business at Rollins College, Winter Park, Florida, where she earned a Six Sigma Green Belt, and a Bachelor of Arts in Hospitality Administration/Management at Michigan State University, East Lansing, Michigan.
She also has been a core champion in the development of the first master’s degree in CX in North America. The Master of Science in Customer Experience Management is being offered for the first time in August 2022 at the Broad College of Business at Michigan State.
to-day operations, and ultimately exceed patient expectations.
The teams are focusing on the experience a consumer would navigate within each encounter throughout a healthcare journey to ensure greater continuity in handoffs and a more holistic approach — and how that is operationalized in our markets, in our facilities and with all those we serve. Elements include: • Day-to-day engagement through interactions in the marketplace that show consumers that Ascension knows them and their life context.

• Pre-visit experiences across communication channels that are simple, convenient and deliver on core consumer needs, to reduce stress and help people navigate their healthcare journey both in person and online. • The care experience itself, ensuring a frictionless experience where quality and people shine, ultimately driving positive patient outcomes through compassionate, personalized care. • Post-care experience, helping deliver a positive and lasting impression that solidifies Ascension as the consumer’s obvious choice in the future through continued support and resolution of any issues. ”As I joined Ascension, I was moved by the letters and repeated examples our patients shared about our associates really delivering an authentic connection and showing the patient how much we care for them,” Carol said. “This is our opportunity to build on that strength and even further amplify it.”
“Our doctors, nurses and caregivers are going above and beyond to provide extraordinary care; I see it every day,” said Jonathan Nalli, Senior Vice President, Ascension, and Ministry Market Executive, Ascension Indiana. “It’s that vocation, that desire to serve our patients, consumers and each other, that makes our organization a desirable place to work and the best place to receive care in our communities. We are committed to building a next-level care experience. That starts with what matters most to our associates — lifting barriers and providing the ability to solve problems, extend kindness and show compassion to each individual.”
The goal is to design experiences that include both rational and emotional tactics that build and maintain trust, amplify Ascension’s care for all people, create frictionless experiences, and deliver those “moments of delight.”
“Great companies do this in such a way that they deliver a phenomenal, frictionless, competitive experience that also has clearly defined experience differentiators — those hallmarks of the experience that become buzzworthy and help bring our Ascension brand to life in day-to-day conversations between consumers,” Carol said. “At Ascension, listening is at the core of our Mission and what we do each day. Our ability to listen and quickly ‘tune the dials’ to adjust the experience remains a foundational element of our success.”
THE VALUE OF SERVICE RECOVERY
A key aspect in how we elevate the consumer experience is service recovery, our dedication to restoring trust and confidence in our ability as an organization to “get it right.”
“Service recovery is about listening to feedback from those we serve and understanding the full spectrum of experiences consumers, patients and their families have before, during and after care,” said Cindy Adams, PhD, RN, ANP-BC, NEA-BC, Chief Nursing Officer, Ascension St. Vincent, Indianapolis. “Our ability to recover broken moments of trust starts with each of us and how we deliver on our commitments to service, caring for patients and families during some of their most vulnerable moments.”
Ascension Indiana was the first Ministry Market to pilot new service recovery capabilities made available through our Salesforce customer-relationship management software.
Key elements of service recovery are actions such as de-escalation, expressions of empathy and sincere twoway communication. A bundle of resources for associates, linked in the accompanying QR code, provides guidance on how to manage and resolve sometimes-difficult conversations.
AN EVOLVING APPROACH TO LISTENING
“In discussions with many market teams and our ministry-wide teams, a collective need for better understanding of how our patients feel about our experience was a common theme I heard across our ministry,” she said. Traditionally, healthcare providers gather experience insight in a lagging format, generally several weeks after a patient has left care. That information is missing the full context of the patient encounter and may not be linked to a specific care team, making it difficult to recognize great performance and “‘tune the dials” on the experience to address processes and other elements that contribute to patient experience.
Last spring, a cross-organizational team started testing in Michigan a “real-time net promoter score” tactic, soliciting feedback from patients shortly after their care and working with care teams to celebrate and recognize great performance, and course-correct on opportunities. Plans are underway to roll out this listening approach across Ascension in Fiscal Year 2023.
“This approach provides us the opportunity to recover from any gaps in the experience more quickly — and it has been proven time and again that organizations that recover fast and well build stronger loyalty with that customer, stronger than those who never had an issue at all,” Carol said. This dynamic is called the Service Recovery Paradox.
“Our associates provide great service today because they’ve responded to their calling with a strong desire to serve and a caring heart. Through this work we are developing ways to amplify that even further,” said Craig Cordola, MBA, MHA, FACHE, Executive Vice President and Chief Operating Officer, Ascension. “This will enable our associates to directly hear even more clearly and in real time from our patients, expanding our culture of listening and our larger strategy to ‘ask less, listen more.’”
UNLEASHING AUTHENTIC COMPASSION
Through this strategy, Ascension has an opportunity to lead healthcare with new experiences that resonate with consumers by unleashing the authentic compassion of associates and leveraging technology and consumer-centric data.
“I firmly believe that CX is a ‘team sport’ that involves everyone across our ministry,” Carol said. “In being a team sport, each and every one of us is a steward of Ascension’s CX, and it is the integrated efforts of our entire ministry that will help take us to industry-leading levels across all of our sites of care and patient interactions. My team and I will help architect and orchestrate that experience vision, but it will take each of us to help bring it to life.”
You deserve compassionate care.
Personalized healthcare when you need it most
When you walk through our doors, you deserve to be seen and heard. Your questions matter. That’s why care teams at Ascension sites of care are here to empower you by listening to you, respecting your experiences and creating a care plan that works for you and your family.
ascension.org
© Ascension 2022. All rights reserved.
CARE FOR ALL CAMPAIGN FOCUSES ON EXPERIENCES FOR ALL PERSONS
Fundamental to Ascension’s Mission of caring for all, with special attention to those most vulnerable, is eliminating health disparities. Our ABIDE framework — Appreciation - Belongingness - Inclusivity - Diversity - Equity — is helping further this work and ensure that our efforts to improve the consumer experience extend to all persons.
This summer Ascension launched a Care for All national marketing and brand campaign to raise awareness of our inherent focus on healthcare equity; prioritize the individual needs of the communities we serve; and build trust through a greater commitment to listen and compassionately attend to the unique needs, questions and concerns of everyone.
“Not only do all of our communities need healthcare, but they deserve to have compassionate, personalized care. They deserve to truly be seen and heard,” said Nick Ragone, JD, Executive Vice President and Chief Marketing and Communications Officer, Ascension. “At Ascension, patients will know that their voice is carefully listened to — that the care they need is personalized to fit their specific concerns and we aim to treat their whole self: mind, body and spirit.”
“The Care for All campaign has one simple message: ‘You deserve compassionate care,’” said Tara Raeber Vail, Vice President, Marketing and Consumer Engagement, Ascension. “Care for All is not just a campaign; it is a commitment. If our services and sites of care in our communities are a first choice for all people because they know everyone can always be cared for equally, then that is our measure of success — through the marketing that reaches our community and, most importantly, through our ministry that serves our community.”
The Care for All campaign, which was developed and produced with multicultural marketing firms, provides an exclamation point on Ascension’s Values and our Mission to care for all persons. It demonstrates care both inside and outside of the hospital and how we are connecting with patients in the community and in the home.

Cancer on trial
ASCENSION AIMS TO IMPROVE ONCOLOGY CARE THROUGH A COMMUNITY OF INVESTIGATORS

Physicians at the Ascension Saint Agnes Cancer Institute include, from left, Drs. Saira Ahmed, Abhishek Kalla and Carole Miller. A cross Ascension, clinicians are coming together to establish the organization as a national leader in clinical research. One area of particular focus is research to improve cancer care for those we serve and others across the nation.
According to the latest data from the Centers for Disease Control and Prevention (CDC), more than 1.6 million people are diagnosed with cancer and nearly 600,000 die from it in the United States each year. It’s the nation’s second leading cause of death. Research on how to prevent, detect and treat cancer is imperative to reducing these statistics.
Ascension has established an enterprise-wide clinical research program led by Frederick Masoudi, MD, MSPH, Chief Science Officer and Vice President, Clinical Research and Analytics, Ascension, to unify research efforts across our ministries. The program aims to build a community of investigators by providing a national infrastructure to support and connect researchers across Ministry Markets.
As part of this program, Ascension Clinical Research Institute (ACRI) and Ascension Data Science Institute (ADSI) have partnered with the Oncology Service Line to develop a national research strategy specifically aimed at advancing cancer care.

“By aligning our research efforts, we have a tremendous opportunity to move the needle on cancer care across our System and even nationally,” said Richard Fogel, MD, FACC, FHRS, Senior Vice President and Chief Clinical Officer, Clinical & Network Services, Ascension. “And, due to our size and expertise, this coordinated approach can make Ascension an attractive research partner for trials and large studies.”
CLINICAL TRIALS INCUBATOR
For several years, Ascension has been laying the groundwork to cultivate and advance cancer clinical trials.
“We are one of the top enrollees for pediatric oncology clinical trials when our Ministry Markets efforts are combined,” said Thomas Aloia, MD, MHCM, FACS, Vice President and Director of Oncology Services, Maternal Health and Perinatal Medicine, Ascension. “Currently, we have four sites participating in research with the Children’s Oncology Group [COG].” The COG is a National Cancer Institute- supported organization that is part of the National Clinical Trials Network and is one of the world’s largest cooperative children’s cancer research entities.
Ascension and affiliated practices also combine to be one of the top research sites enrolling in the Gynecologic Oncology Group (GOG) across the eight participating Ascension sites. The GOG creates the opportunity to participate in the latest clinical trials of novel therapies for gynecologic malignancies such as ovarian and cervical cancers.
“Throughout Ascension, our clinicians are engaging in innovative oncology research,” Dr. Aloia said. “Much of this research focuses on identifying potential opportunities to improve outcomes through precision medicine, which takes into account tumor genetics, patient lifestyle and environmental factors to determine the best treatment options. As we look to the future, we are excited to expand upon these efforts to personalize cancer care.” Thomas Aloia, MD, MHCM, FACS
Susan Kopunek, CRNP, speaks with patient Kellie at the Ascension Saint Agnes Cancer Institute in Baltimore.
BRINGING VALUE
Ascension’s participation in oncology clinical trials also has the opportunity to bring significant value to patients.
“Research plays an integral role in improving the care we deliver to our patients,” Dr. Masoudi said. “By offering clinical trials as an option, we present our patients with a unique opportunity to participate in studies of technologies and treatments that may not yet be widely available. Patients may also feel like they are helping others by participating and contributing to science.
“As we continue to build our clinical research program, we look forward to working alongside our Oncology Service Line colleagues to align Ascension’s research efforts, identify new partnership opportunities and transform cancer care as we know it today,” he added.
BUILDING PARTICIPATION
Looking ahead, Ascension’s research strategy will focus on increasing participation for multisite medical oncology trials across the System.
To help lead these efforts, Douglas Reding, MD, Oncology Service Line Director, Ascension Wisconsin, and Carole Miller, MD, Medical Oncologist and Cancer Institute Director, Ascension Saint Agnes in Baltimore, will be providing their expertise and guidance.
“Dr. Reding and I will be working to help streamline the startup of oncology clinical trials by supporting collaboration across our institutions and partnering with ACRI,” Dr. Miller said. “By supporting our national research infrastructure, we can help streamline the trial startup processes and reduce delays that may occur due to contracting inefficiencies. In turn, by removing these barriers, we hope to encourage more clinicians to lead and participate in research opportunities. We look forward to this exciting work ahead.”
Helping patients feel heard
ASCENSION LANGUAGE SERVICES ALIGNS, CONNECTS, ENHANCES THE EXPERIENCE
Often what matters most to patients and their families is that they feel heard. But what happens when a patient is deaf or hard of hearing, or English is not their preferred language, and as a result the patient-provider relationship is challenging?
For Ascension Language Services, the concerns of these vulnerable populations are a priority.
Through a community of language services leaders who collaborate across our national ministry, Ascension is able to identify and spread best practices that create a safe, inviting environment for our patients and family members who are Limited English Proficient or deaf or hard of hearing.
“Community and connection are foundational to Ascension’s Language Services program, a program that embodies our Mission in action — meeting people where they are,” said Jessica Weber, Senior Director, Patient and Consumer Experience, Ascension. “Language Services can also enhance both our patient and provider experience, as well as play an important role as we strive to address social determinants on Ascension’s path to health equity.”
“Our ABIDE framework calls us to inclusion and equity,” said Pam Mitchell-Boyd, Senior Director, ABIDE (Appreciation - Belongingness - Inclusivity - Diversity - Equity). “There’s such a natural alignment with this important language work, where we walk alongside our patients and their families to ensure they feel welcome and invited into the conversation about their care. This care and attention also impacts and benefits our associates in a meaningful way.”
OUR APPROACH
Ascension Language Services helps associates deliver compassionate,
Phone Interpreting
Video Interpreting personalized care and uses the Ascension Experience Model as its road map to listen with empathy, take meaningful action and learn together. The program is based on five principal pillars:
Data: Working with the Ascension Data Science Institute, Ascension Language Services gathers, analyzes and compares market language services and Ascension-specific REaL (Race, Ethnicity and Language) data sets with existing Ascension Google Cloud content to create a baseline and identify opportunities to reduce health disparities and improve equity of care.
Affinity groups: Team members create a common space for cross-market
On-site Interpreting
FTE Interpreters

language services leaders to meet regularly to share ideas, insights, wins, opportunities and lessons learned; and promote key relationships to align, scale and spread evidence-based strategy.
Aligned System approach: Ascension Language Services develops systems, processes and technology for in-market implementation. With market partners, program leaders then personalize shared System goals, create market-specific project plans, and collaborate during monthly one-on-one meetings. Alicia Barlow and daughter Just-in-time consultation: Program Morgan Anderson leaders provide in-house language services-related consultation as needed for developing projects, teamlets and event reporting. Written document translation: The program leverages resources and subject matter experts to provide translation services for patients, associates and communities. Ascension Language Services provides an enterprise model for translation requests and project management with Clinical Professional Development.

Ascension Consumer Experience team members, from left, Jessica Weber, Senior Director, Patient and Consumer Experience; Ibzan Monteagudo, Senior Director, Language Services; and Lesley Herwig, Program Manager, Language Services & Patient/Consumer Education. ATTENTION TO NEW, VULNERABLE POPULATIONS
In 2021, the United States began welcoming the resettlement of Afghan refugees within our borders. The Ascension Consumer Experience team identified an opportunity to implement a System-wide Refugee Response. Ascension’s Language Services and Consumer Education teams engaged with a dozen Ascension functions and workstreams to identify best practices.
“Events in Ukraine and the prospective resettlement of Ukrainian refugees in the United States only validate the value of a proactive response plan. We aim to develop a strategy that not only addresses refugees’ needs, but also those of asylees and migrants,” said Jessica Weber, Senior Director, Patient and Consumer Experience, Ascension. “Language Services isn’t only focused on providing the necessary building blocks to foster communication, but also shaping an agile program, rooted in cultural humility, to address the evolving needs of the unique poor and vulnerable populations we are called to serve.”
Our future in telehealth
MOVING BEYOND VIRTUAL VISITS
As we continue to prioritize equitable access to high-quality care, Ascension is making significant progress in the area of virtual care. We are focused on using technology to bring care to patients anytime, anywhere.
Our telehealth interventions have helped us provide care while managing the physical — and sometimes psychological — challenges facing many of our most vulnerable patients.
Virtual visits now represent 8-10% of all patient visits in Ascension, and over 50% of behavioral health visits. Though important, there is more to telehealth than virtual visits.
EXPANDING THE UNDERSTANDING OF TELEHEALTH
“Some people don’t realize that the definition of telehealth goes far beyond video or telephonic visits [i.e., telemedicine], which is only the tip of the iceberg,” said Tania Elliott, MD, Chief Medical
Officer, Virtual Care and Vice President, Clinical & Network Services, Ascension. “Telehealth, or virtual care, is a broad term that includes a wide spectrum of digital capabilities, including remote monitoring, e-consultations, digital check-ins and digital therapeutics, to name a few. These options should be seen as tools that add to the care of patients — not Tania Elliott, MD as care alternatives or replacements for traditional care delivery. If there was any silver lining to the COVID-19 pandemic, it was that virtual care should now be considered a core component of care delivery — a routine way in which clinicians interact with their patients.”
Ascension’s national remote patient monitoring program continues to expand, as does its e-consult program. e-Consults, also known as interprofessional consultations, enable clinicians to access high-quality specialist opinions electronically for their patients — increasing care coordination and knowledge sharing and improving equity, especially for those living in rural or underserved communities who may not have access to specialty care.
In January, Ascension Indiana launched an interprofessional consultation model between surgeons and cardiologists to ensure that patients were ready for surgery. To date, more than 740 cardiac consultations have been provided, with high levels of clinician and patient satisfaction. Additional use cases are being developed across the organization.

— TANIA ELLIOTT, MD, CHIEF MEDICAL OFFICER, VIRTUAL CARE AND VICE PRESIDENT, CLINICAL &
NETWORK SERVICES, ASCENSION

“To further our progress, we are working to create a model for licensing and credentialing clinicians across state lines and establishing national telehealth programs with our Ascension Medical Group [AMG] clinicians,” Dr. Elliott said. “This approach allows us to expand our reach, especially to those who are underserved — no longer making a person’s access to care determined by their ZIP code.”
During the height of the pandemic, Ascension remote patient monitoring teams cared for more than 13,000 COVID-19 patients across our ministries. Today, these programs continue to demonstrate better outcomes in the care of persons who are enrolled over those not enrolled.
To help reduce disparities and severe maternal morbidities, two important maternal health goals, we have seen significant success with our newest remote patient monitoring program for postpartum hypertension. We know that deliveries involving severe maternal morbidities disproportionately affect minority and low-income pregnant women, especially non-Hispanic Black women and those with Medicaid. The period following birth is a critical time for both woman and infant, and it’s an important time to assess physical, social and psychological well-being.
The remote patient monitoring program for postpartum hypertension, already active in Texas and Indiana, has a 95% postpartum visit adherence rate for program enrollees compared to 55% for similar patients who were not enrolled and a 50% decrease in emergency department utilization in this high-risk group. The plan is to expand this program across Ascension.
Monica Salinas serves as Supervisor, Consumer and Patient Experience, Ascension Contact Center Operations.
REMOTE MEDICAL ASSISTANTS
Another area where telehealth is making a positive impact is within our care teams. As we continue to foster an environment where Medical Assistants (MAs) can flourish professionally, a unique pilot program in Michigan is showing great promise. The program uses a remote MA position and is intended to not only address retention and recruitment of MAs but also create greater satisfaction among clinicians and patients.
The remote MA helps the care team with such tasks as managing refill messaging and follow-up (scheduling, notification); preparing new patient charts; intake for in-person and virtual visits; communicating between the patient and clinicians and staff; and reviewing care gaps. The program also offers MAs an opportunity to work from home, providing greater flexibility for these often hard-to-fill positions. Working virtually provides MAs much-needed flexibility and balance. They are able to better allocate their time, making it possible to prioritize each patient who calls or sends a message and to complete prior authorizations more efficiently.
Patients are also beneficiaries of the remote MA model.
“Patients have made many comments on how quickly their calls get answered and their messages get a response,” said Carrie Bilek, Practice Manager, Premier Family Medicine/ Howell Family Medicine, Ascension Medical Group. “It has cut down on phone tag. MAs have the ability to also make appointments, so if someone does need to get in and an MA is on the phone with them, the appointment is made right then. Because new patient information is already in the chart, it cuts down on the time the MA in the office is in the room and allows patients to spend more time with the clinician.”
A remote MA can also assist a greater number of clinicians, which allows clinicians to concentrate on spending more time caring for patients.
Plans to scale the remote position in other Ministry Markets are underway, with multiple sites interested in using the program to improve care delivery.
“We will continue to look for opportunities to leverage virtual care solutions that meet shifting consumer preferences and our patients’ needs,” Dr. Elliott said. “It’s so core to our Mission as we seek to break down barriers and ensure that everyone has access to care — wherever they are.”
Well-being Sessions another tool for the journey
myCARE INTRODUCES WEEKLY PROGRAMMING TO HELP ASSOCIATES FOCUS ON THEIR WELL-BEING
Well-being is a lifelong journey toward balance in mind, body and spirit. Recognizing the need for a centralized place to find well-being tools, events and resources, Ascension designed myCare to help associates along the way.
“Self-care is the first step to providing compassionate, personalized care to those we are privileged to serve,” said Herb Vallier, Executive Vice President and Chief Human Resources Officer, Ascension. “We wanted to create a place where associates could find tools to help them find healing, holistic health and resources to support their well-being.”
This year, myCare has become more interactive with the addition of weekly Well-being Sessions. Each Well-being Session addresses a specific aspect of fitness, nutrition, mental health and more. Sessions last 30 minutes and are split between a presentation from an Ascension subject matter expert and a question-and-answer session. Each presentation is recorded and available later on the myCare site for those who are unable to attend a live session.
“We wanted to go beyond a list of resources and begin to engage with co-workers on their well-being journey,” said Sara Campbell, Vice President, Culture and ABIDE, Ascension. “We’ve already witnessed a lot of excitement around the topics, and the meetings often run long due to the rich discussion and interaction with our associates and Ascension subject matter experts.”
“I feel that having all of the information you need from trusted resources is incredibly helpful, so I was happy to present on making fitness simple and sustainable,” said Seth Spicer, Athletic Trainer, Sports Medicine, Lourdes, Binghamton, New York. “Best of all, there was a lot of support and great questions at the end of the presentation, making me feel like the session really helped people.”
“I have really gotten a lot out of the Well-being Sessions,” said Michelle


Athletic Trainer Seth Spicer, MS, ATC, LAT, CSCS, FMSC, Lourdes Hospital, Binghamton, New York, shares tips on keeping exercise simple and sustainable with associates.
Brooks, RN, Nurse Care Manager, Ascension Borgess Hospital, Kalamazoo, Michigan. “I realized how challenging it is trying to get healthy after having kids and being a mom and putting myself last. These Well-being Sessions have kept me motivated to put my health first so I can set an example for my kids and patients.”
“It always helps to know I’m not alone. It helps to know we all have similar issues,” said Chung Massey, RN, Ascension Texas Nursing Practice. “I feel the need to be more mindful of my wellness, so I appreciate Ascension providing the space. It’s helpful that the presentation is only 30 minutes and usually there is time after to stay on and ask questions.”
In addition to Well-being Sessions, Ascension has made several free tools available to associates:
myCARE
On the myCare website, associates can find resources for spiritual, mental, physical, relational, financial and occupational well-being as well as tools to address isolation, stress, empathic leadership and more.
WELL-BEING KUDOBOARD
A special well-being Kudoboard is designed for associates to come together in community to share tips, tricks, pictures, recipes and resources to help each other along the wellness journey.
— SARA CAMPBELL, VICE PRESIDENT, CULTURE AND ABIDE, ASCENSION
eCARDS
Gratitude is an important aspect of well-being. Associates can send co-workers a personalized, digital eCard to show they care.
ASCENSION WYSA
The Wysa app can help reduce stress and anxiety, enhance mood, improve sleep, and encourage mindfulness. It also connects directly to other Ascension-specific offerings.
EMPLOYEE ASSISTANCE PLAN
Counselors help assess issues, refer for follow-on care, identify resources and develop action plans to help associates and family members manage stress, get back on track, get out of debt and more.
VIRTUAL SPIRITUAL CARE
Available anytime, anywhere, Virtual Spiritual Care is staffed by experienced Ascension chaplains committed to supporting associates through listening and compassionate conversation.

INITIATIVES ADDRESS OPIOID OVERUSE AND HELP PEOPLE ON THEIR ROAD TO RECOVERY

For Brandy Ray, it was clear when her addiction began.
As a teenager, she’d gone drinking with friends on weekends. After her marriage to her high school sweetheart ended when she was only 20, she started drinking more to cope. However, she stopped when she became pregnant with her oldest son and, for a time, things seemed to be going well. She got a job, started college and rejoined her church, hoping it would fill the “dark hole” she now realizes had always been inside of her.
In an instant, everything changed.
“I decided to go on a trip with my church’s college youth group, rock climbing in Tennessee. I ended up falling about 60 feet while rappelling down the side of a mountain,” she said. ”I shattered my left ankle and broke my back in two places. This is where my addiction would really start.”
Chronic pain is a major reason Americans access the healthcare system. According to an article by the McGovern Institute at the Massachusetts Institute of Technology, about 50 million Americans suffer from chronic pain, which interferes with their daily life, social interactions and ability to work. Opioid prescriptions for chronic pain are a major contributor to the opioid epidemic.
Like so many others, Brandy received a prescription for oxycodone to treat the pain from her fall.
“I eventually became addicted but was able to be a ‘functioning addict’ for several years,” she said. ”I had my youngest son in 2013 and was so happy to be a mother again, but that wasn’t enough to keep me sober. Eventually, I switched to harder drugs and would lose everything, including my boys. I was in such a dark place and I didn’t think that there was any way out.”
Brandy was only slightly aware of Ascension St. Vincent’s Medical Center Riverside, Jacksonville, Florida, before she overdosed on heroin at age 33. The hospital happened to be the closest facility.
“I remember being in the ambulance that night, on the way to the hospital,” Brandy said, “crying and saying, ‘Please help me. I need help!’”
Fortunately for Brandy, in 2018 Ascension St. Vincent’s had joined a community partnership designed to prevent drug overdose deaths. Working with the city of Jacksonville, Gateway Community Services, Jacksonville Fire and Rescue, and River Region Human Services, the hospital was part of Project Save Lives, Jacksonville’s response to the opioid epidemic.
Overdose deaths had become a big problem in Jacksonville. During the height of the opioid epidemic, the Centers for Disease Control and Prevention estimated that overdoses claimed an average of 275 lives a day.
Ascension St. Vincent’s used to turn patients like Brandy over to drug treatment groups. Addicts would sober up and leave the hospital right away. With Project Save Lives, the strategy was to turn their life around in the hospital bed.
By identifying eligible patients as they overdosed and entered the emergency room, Ascension St. Vincent’s could pair them with peer recovery specialists: people who have battled and survived addiction themselves. These specialists would guide patients through treatment and rehabilitation, and set them on the path of what the hospital team hoped would be their journey to health and recovery.
Help for Brandy came in the form of two key people. The first was a nurse in the emergency department (ED) who listened to her cries for help and immediately offered to call a peer support specialist for her.
“Being offered help at that moment was important,” Brandy said. “If that nurse hadn’t acted so quickly, if it had been a couple of hours later, then I probably would have changed my mind because of fear and that desire to use again being so strong.”
Kristen Nelson, RN, now a nurse in Labor and Delivery at Ascension St. Vincent’s Riverside, was an ED charge nurse when the Project Save Lives pilot began. She remembers when peer support specialists came to the ED to work with patients.
“At that time we had a surge of overdoses with multiple patients being brought in daily,” Kristen said. “Some of them would just take off after we stabilized them, so having the peer support specialists available really helped.”
It was Kristen who heard Brandy’s cry for help and arranged for her to meet her first peer support specialist, Tony. He was kind and listened to her. He drove Brandy to detox and stayed in touch throughout treatment, checking in on her for almost two years to see how she was doing. Brandy worked with a second peer specialist, Heather, during treatment. After completing detox, two weeks in a residential program and 10 months in a women’s sober-living house, Brandy moved out on her own.
“I have been sober now for three years. I am the general manager of a sober-living house in downtown Jacksonville and a certified recovery resident administrator,” Brandy said. “I’ve started school with the goal of obtaining a bachelor’s degree in substance abuse counseling. I’ve rebuilt relationships with my family. And I was able to gain back full custody of both of my boys. Today I am happy and at peace. Life isn’t perfect but it’s good, and I would never in a million years want to go back to the way it was. I’m so grateful to Project Save Lives for being there when I needed it most.”
— RICHARD FOGEL, MD, FACC, FHRS, SENIOR VICE PRESIDENT AND CHIEF CLINICAL OFFICER, CLINICAL &
NETWORK SERVICES, ASCENSION
FROM TREATMENT TO PREVENTION
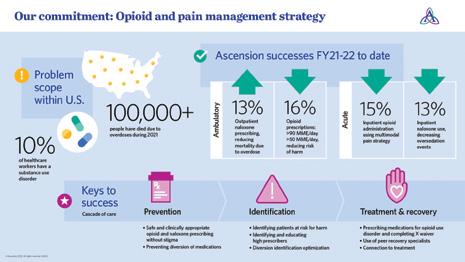
While Project Save Lives holds great promise, treatment programs aren’t enough. Recent data shows that the opioid crisis is not over; in 2021, overall drug overdose deaths increased by 15%.
As far back as 2014, Ascension markets began collaborating on comprehensive pain management programs to minimize opioid use and prevent substance abuse disorder. Today, there are opioid treatment and recovery programs in Ascension’s Alabama, Baltimore, Florida and Gulf Coast, Illinois, Michigan, New York, Tennessee, Texas, and Wisconsin Ministry Markets. These programs have transformed the way we manage pain across Ascension, leading to a variety of improvements in care: reductions in the use of the most potent injectable opioids, in opioid use for patients undergoing knee and hip replacements, and in the number of narcotics prescribed in emergency rooms.
Ascension has put a number of successful interventions in place, including standardized pain assessment tools in the inpatient setting and ambulatory pain management guidelines for cautious and effective treatment of people with chronic pain; updated order sets containing lower doses of opioids that allow the physician to increase the dose based on individual patient needs; and educational tools focusing on use of nonopioid alternatives for various acute pain syndromes and supporting inpatient initiation of medications.
Another tool is medication management software that audits pharmaceutical transactions. Based on information from automated dispensing cabinets, Kronos, PeopleSoft and the electronic health record, it identifies anomalies or deviations in medication handling that require further investigation. Ultimately this new tool will help protect both associates and patients.
In addition, Ascension has introduced comprehensive measures to assess the effectiveness of pain management and opioid stewardship initiatives in both acute and ambulatory settings. And a guide available through Ascension myCare and posted on the Human Resources and SmartHealth member websites helps associates know where to go for substance use disorder resources.
In the near future, Ascension plans to expand these interventions to additional sites of care, such as Ascension Living.
“Against a problem this widespread and complex, only a collaborative approach can possibly provide the compassionate, personalized care that’s needed on the required scale. Ascension is well positioned to lead such collaborative efforts,” said Richard Fogel, MD, FACC, FHRS, Senior Vice President and Chief Clinical Officer, Clinical & Network Services, Ascension. “We must continue to find creative ways to help people manage their pain while minimizing the opportunities for addiction in our communities.”
TREATING SUBSTANCE USE DISORDERS
On a System level, Ascension has proactively assembled dedicated multidisciplinary teams to prevent and confront substance use disorders. The work is overseen by the Opioid and Pain Management Governance Committee, a core team of leaders across Ascension. Together with 13 Ministry Market-level committees headed by designated acute and ambulatory care opioid leads, the committee collaborates closely with Ascension Rx, Associate and Patient Safety, and members of the Behavioral Health Service Line. Their approach to patient care is based on four areas of emphasis:
Prevention: Minimize opioid use when evidence does not support a benefit or if alternatives exist, and prevent harm from opioid use, including overdoses, and opioid misuse and abuse.
Identification: Identify patients at high risk of harm from opioids and clinicians with high opioid prescribing patterns and design ways to deliver appropriate, personalized care.
Treatment: Provide comprehensive holistic treatment options for opioid use disorder in all care settings.
Recovery: Improve access to comprehensive behavioral health services and community resources promoting recovery.






