18 minute read
Navigating Implant Success with Photogrammetry
The How, When and Why
By Leila Zadeh, DMD, FAGD
In the United States, more than 36 million people are completely edentulous, and approximately 120 million people are missing at least one tooth.(1) Solutions in the form of fixed-implant prostheses, such as all-on-X hybrids or implant bridges, are invaluable treatment options because they more closely approximate both the function and esthetics of healthy, natural dentition than their removable counterparts. Advances in digital technology and the relatively recent incorporation of photogrammetry — a method of approximating the 3D orientation of objects using 2D images — in dentistry not only improve the accuracy of capturing implant relationships, but they also help streamline the final impression process so that it is significantly faster and easier than traditional analog workflows. This article will explore the how, when and why behind this cutting-edge technology that is revolutionizing implant dentistry and discuss the clinical implications for you and your practice.
A Glance at the Past: The Traditional Analog Approach to Full-Arch Impressions
It was during my advanced education in general dentistry residency when I first realized how time-consuming and technique-sensitive the fabrication of passively-fitting implant prostheses could be. This became evident when I performed my first all-on-X surgery. The implants had great primary stability, so I was comfortable immediately loading the milled acrylic surgical interim. However, the analog interim denture conversion with temporary cylinders and salt and peppering powder acrylic was much more difficult than I had anticipated. I ended up working all through lunch until just after the clinic closed by the time the interim was finally inserted, occlusion double-checked, and the patient’s transformation completed.
Flash forward a few months later, and it was time for the final impression for her zirconia-fixed hybrid denture. Unsurprisingly, the traditional analog workflow we used took an entire morning block and most of lunch, with the not-so-patient patient waiting in the dental chair while I spent the majority of my time doing lab work and running back and forth from the operatory to the lab, pouring up alginate impressions, making and luting together an implant verification jig, making several chairside polyvinyl siloxane impressions, and cross-mounting casts. Adding to the pressure to be both speedy and accurate was the knowledge that the more steps that were needed, the higher the potential for cumulative error.(2)
Although I was a new dentist who had never done this procedure before, I knew from having spoken to my prosthodontist mentors that conventional denture conversions and final impressions for fixed detachable hybrid dentures — even when done in this exact way in their experienced hands — can frequently take up most of a morning or afternoon block. That was, until the incorporation of photogrammetry technology.
Making New Waves in Implant Dentistry: What Is Photogrammetry, and Who Is Using it?
Broadly defined, photogrammetry (PG) is a “method of making precise measurements by using reference points in photographs.”(3) More specifically, it is a “technique for determining the geometrical characteristics of objects and their 3D spatial orientation by recording digital images following a specific protocol,” and it is used in dentistry as a means to digitally transfer intraoral implant locations to computer-aided design (CAD) software.(4) First used in implant dentistry as early as the mid-1990s, PG was proposed as an alternative to conventional full-arch implant-supported impressions by Torsten Jemt et al. in 1999.(3,5-7) Some of the different PG systems currently available on the market include iCam4D (iMetric), MicronMapper (S.I.N. 360), PIC System (PIC Dental), and Blue Sky Bio Grammee (powered by Tupel 3D), and, while each system has its differences, they all aim to better capture the spatial positioning of implants relative to each other by bringing the accuracy of a desktop scanner to the mouth. This is incredibly useful because intraoral scanning alone is currently not accurate enough for the final impressions of edentulous arches for full-arch implantsupported prostheses.(4,5,8,9) Compared with intraoral scanners, PG scanners also do not have the same stitching errors because all of the scan body data is captured at once with each picture; their accuracy is not as influenced by patient movement or by blood, saliva and other residue; and their multiple cameras have a larger scanning range and faster scanning speed.(3,10)
Having only restored all-on-X prostheses the conventional, analog way during residency, I was fortunate to work and train with new digital workflows in private practice, where I experienced firsthand how PG can streamline and simplify the full-arch final impression process chairside to a mere 30 minutes, saving the operator time, money and tremendous headaches. I quickly found that many others felt the same way.
“PG has been a complete gamechanger for my practice,” explained Nate Farley, DDS, MS, FACP, a board-certified prosthodontist, founder of digitalDDS, a continuing education company that teaches dentists digital dentistry and simplifies CAD/CAM (computer-aided design/computer-aided manufacturing) workflows, and co-creator of whatimplantisthat.com. “Before PG, we took 2–3 hours to combine the final impression steps and all the records (e.g., bite, mounting, scanning interims, etc.), all of which was pure ‘doctor-time,’ with technique-sensitive steps that could not be outsourced to anyone else on the team. However, after PG, this same appointment is now down to 1–1.5 hours and is almost completely delegated to our staff, with the total ‘doctor-time’ being only a 15–20-minute sliver of the total appointment. This has greatly improved our chair time, and we — as well as our patients — have really enjoyed how our schedules have opened up as a result.”
Because of its efficiency, this technology is increasingly being used not just by prosthodontists, but also by general dentists who restore a lot of implant prostheses. I’ve noticed an interesting trend in an increased demand for oral surgeons to create and deliver full-arch surgical interims themselves for the general dentists with whom they work.
However, due to the relatively high cost of a PG unit (as of fall 2024, the iCam4D is about $40,000; the Grammee by Blue Sky Bio is about $18,000; the MicronMapper is about $27,000; and PIC ranges from about $33,000 to $40,000), investing in this technology is not practical or cost-effective for practices that do not work frequently with implants. As a result, many dental labs are investing in PG systems and sending technicians chairside to assist dentists with these workflows so that clinicians can get the benefit of this technology without committing to buying a unit. However, according to prosthodontist Kimberly Schlam, DMD, MS, owner of Bend Prosthodontics and a Spear Education faculty member, if utilizing an external lab for its photogrammetry services, it is important to remember that the responsibility ultimately lies with the clinician for the implant position. “This is why I prefer taking my own PG scans,” Schlam said. “As the provider responsible for the prosthesis that will be delivered, I will be the person helping the patient manage the prosthesis into the future, so I do not let any technicians make final impressions of my implants either digitally or conventionally, and I also double-check the passivity of my implant prostheses clinically and radiographically.”
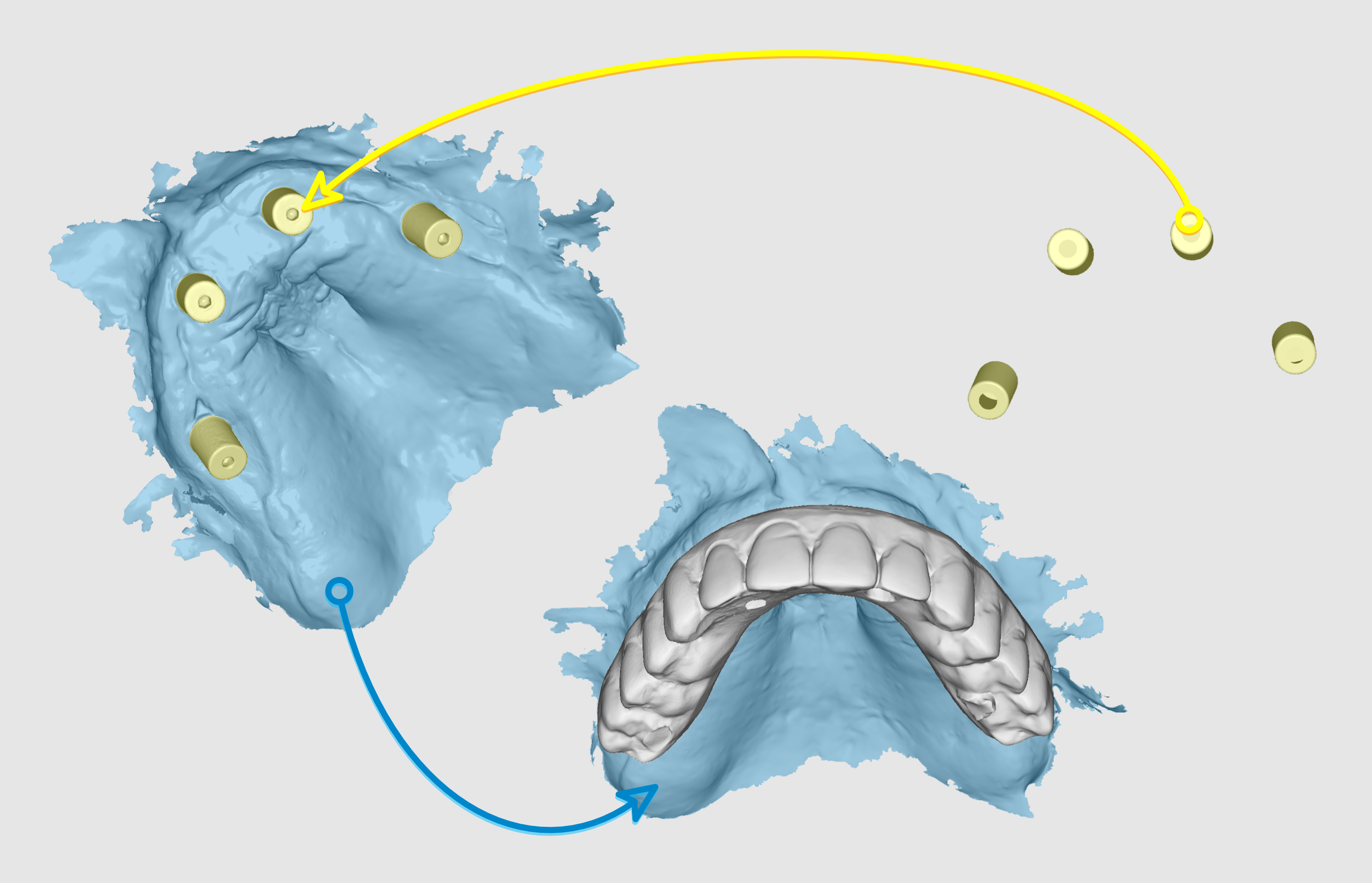
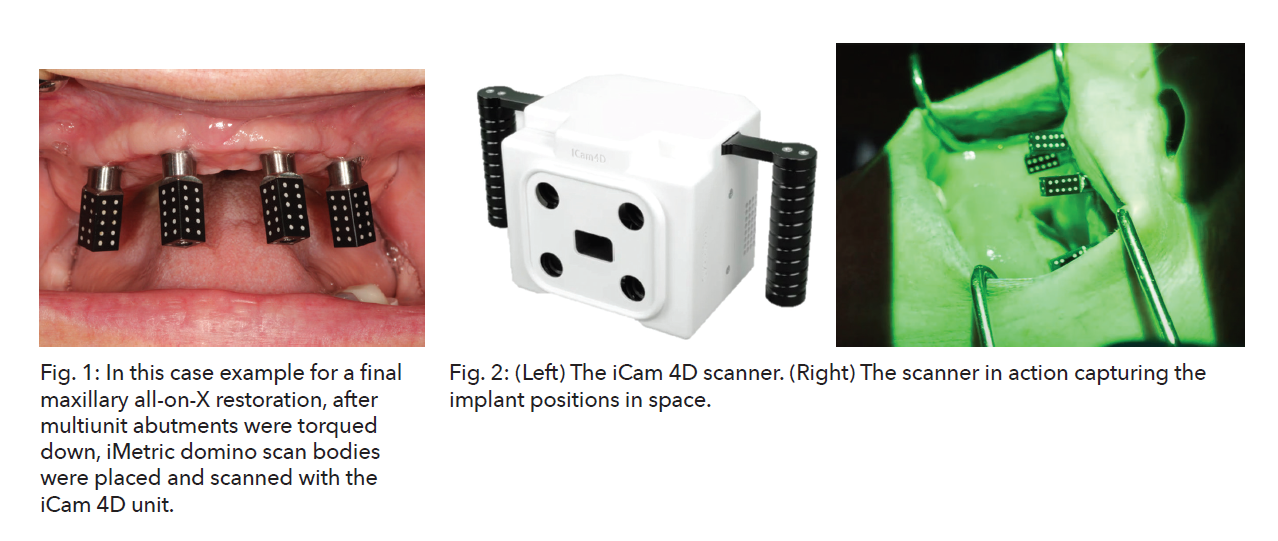
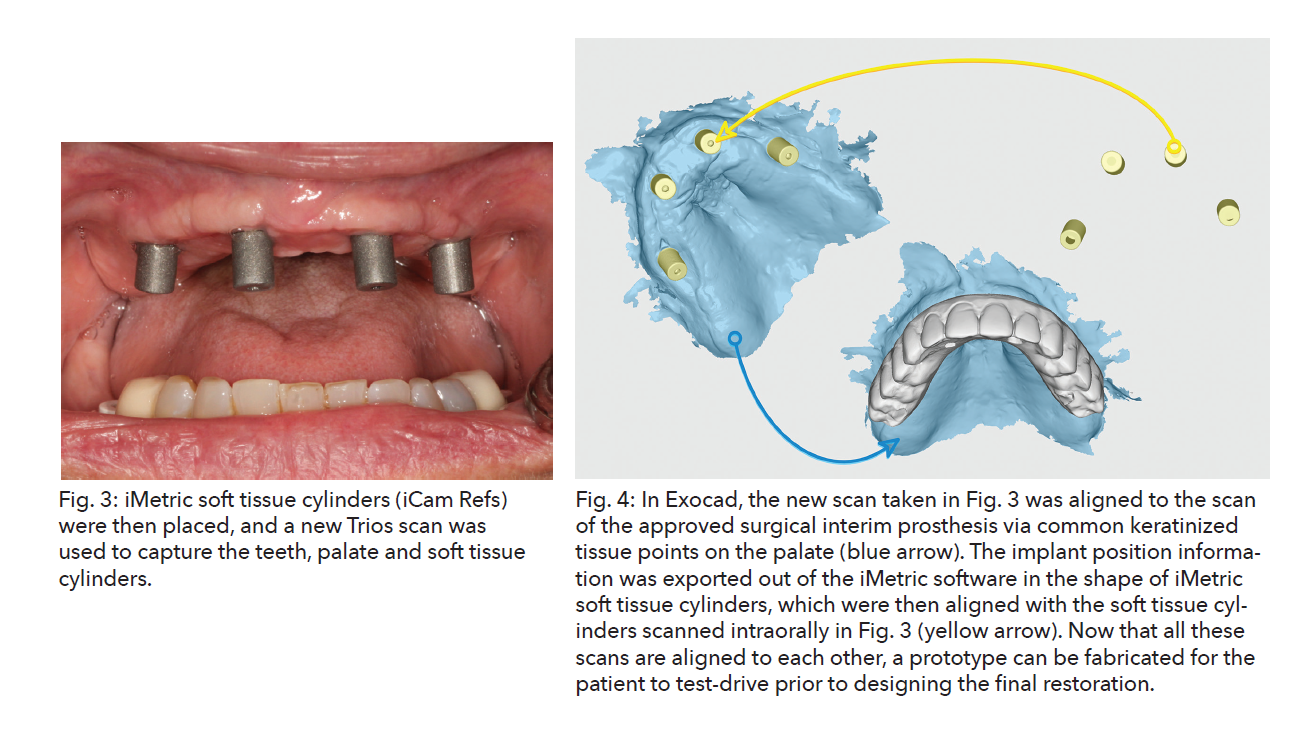
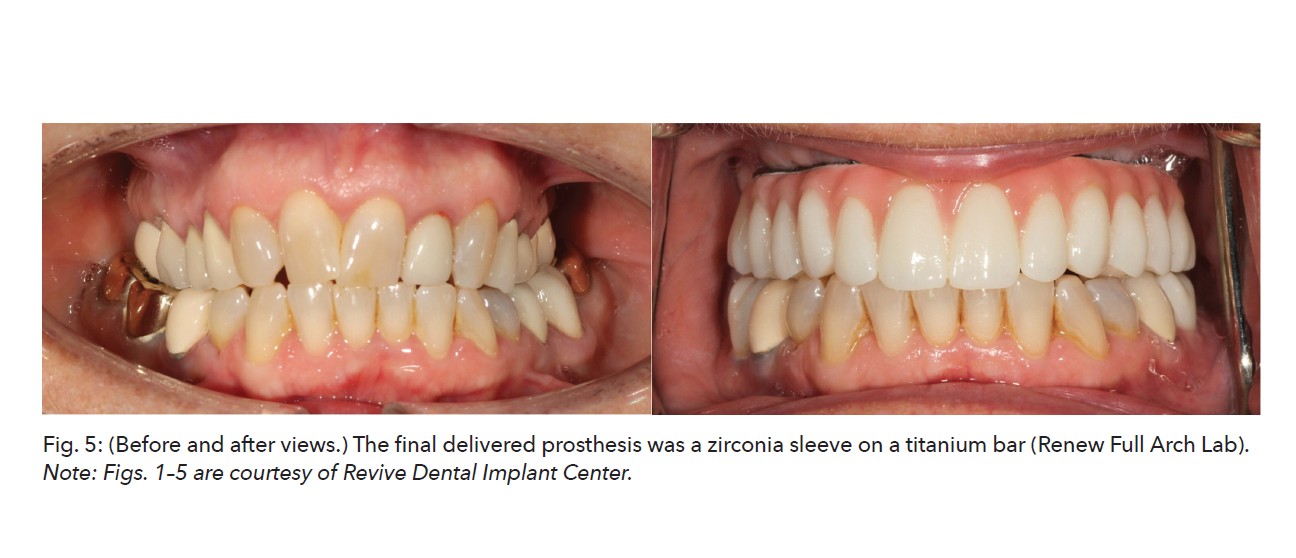
Photogrammetry Unveiled: How to Use This Technology
The basic idea behind any PG unit is that it uses an external camera to scan intraoral markers and record the spatial position of implants relative to each other in a 3D space, and this information is stored as an STL (standard tessellation language) file, which is a file format for 3D objects (Figs. 1 and 2). Because the PG unit itself does not capture any information about the soft tissue and/or any possible teeth remaining in the arch, a second scan by an intraoral scanner or a digitized conventional analog impression is needed to capture this additional data, which is also stored in STL file format (Fig. 3). These STL files can then not only be aligned to each other, but they can also be aligned to the preoperative scan of the original teeth when making a surgical interim or aligned to the approved surgical interim when designing your final prosthesis (Fig. 4). CAD software such as Exocad can be used to fabricate a prototype or the final implant-supported prosthesis, which can then be printed or milled (Fig. 5). The beauty of this workflow is its flexibility — any portion of the CAD/CAM process can be outsourced to a dental lab or handled in-house.
When Is Photogrammetry Indicated, and How Accurate Is It?
In addition to full-arch cases, PG can also be used to quickly and accurately capture the implant relationships for an implant bridge instead of spending the time to make an implant verification jig and/or luting the implants together chairside. PG can be used to eliminate the need for messy and time-consuming denture conversions on the day of implant placement if the surgical interim prosthesis is designed in advance. PG scans recording the implant positions can be quickly incorporated into this predesign so that the resulting surgical interim can be printed or milled for same-day delivery. This can be coordinated with your local dental lab, or you can incorporate either part or all of this workflow in-house to save on costs. Although two recent systematic reviews published in the Journal of Prosthodontics(10) and the Journal of Prosthetic Dentistry(11) concluded that PG is a reliable tool for recording implant positions, and many studies support the accuracy and/or long-term survivability of prostheses made utilizing PG as being either superior or comparable to analog conventional full-arch implant impressions,(2,3,7,12-16) there are a few studies that have reported the latter to be more accurate.(4,17) Thus, the general consensus is that PG is increasingly showing promise, and more dental research is indicated to establish its reliability in different clinical situations more consistently, as the current scope of research on the subject is relatively limited.(2)
Some important factors to consider when assessing the validity and applicability of these existing studies are:
• The influence of study limitations on the conclusions drawn (i.e., small sample size, whether the study was done in vivo, etc.). We must also recognize that when we practice evidence-based dentistry, systematic reviews and meta-analyses should be given more weight than other study types.
• How the results might have been influenced by implant factors, such as whether the impression is implant or abutment level, implant angulation, apico-coronal depth, type of connection, inter-implant distances, intraoral factors (saliva and mucosa movement), the operator’s experience, and different environments (i.e., maxilla or mandible, room temperature or humidity, etc.).(2,12) Additionally, the “design, wear, or torque displacement of the PG markers” could also affect the accuracy.(10)
• The fact that these findings are specific to the particular workflow employed in the study in question (i.e., the specific PG system, intraoral scanner and scan path, scan bodies, and/or implant configurations used).(4)
• Which methods were used to assess accuracy in these studies, as these can influence the accuracy of different impression techniques.(2)
Therefore, future research is indicated to rule out the influence of these variables, and we should always be careful when assessing studies as to whether the conclusions drawn can be generalized to all of PG as a whole. This is important so that we are comparing “apples to apples” when making our own clinical decisions based on the body of dental literature available.
Other Tools in our Toolkit: Photogrammetry Alternatives
As useful as PG can be, it also has some downsides besides high cost. It is a modelless workflow, which makes cementing titanium bases either impossible or a challenge and prevents checking the accuracy and passivity of the implant-supported prosthesis on a verified master cast prior to delivery. Additionally, you still need to use an intraoral scanner to capture the shape of the soft tissue and/or any existing teeth against which the prosthesis will be built.
Trying to find a more cost-effective alternative to PG to get the best of the analog and digital worlds, Russell J. Crockett, DMD, prosthodontist and founder of the company Digital Arches, spent the early COVID-19 pandemic quarantine days developing the Optisplint® (by Digital Arches), which is the first and only scannable full-arch analog and digital verification jig.
“Complexity and cost can be huge barriers for dentists entering the full-arch implant arena, and digital workflows have simplified this procedure significantly,” Crockett said. “The Optisplint is similar to a conventional verification jig, but it uses scan bodies instead of impression copings. They are linked together in the mouth with resin, and an intraoral scanner is then used to capture all necessary scans, such as tissue, interocclusal record and biocopy.”
“The benefit of Optisplint is that it gives clinicians the benefits and advantages of digital scanning, including speed, while also providing the consistency and predictability of conventional records,” Crockett said. “Additionally, since it doubles as a physical jig, it can act as a verification device to confirm passivity on an analog patty cast prior to the delivery appointment, and the linked scan bodies can be scanned extraorally in a desktop scanner for improved accuracy.”
This ability to incorporate a desktop scanner is one of the key differences between the Optisplint and other available intraoral full-arch systems on the market, such as ioConnect™ (TruAbutment), which attempts to reduce stitching errors by shortening the dental arch. Other new products that attempt to improve intraoral scan quality include the Nexus iOS (powered by Osteon), EZ Ref (Evolve), Grammetry ArchBridge™ (Roe Dental), Scan Ladder and TRI® Scanbridge. However, as more studies testing these newer products are performed, we will be able to better gauge their efficacy in our practices for full-arch prostheses.
Clinical and Practice Management Implications
Two of the biggest trends in dentistry are an increase in the number of patients and a simultaneous decrease in the number of dental laboratory technicians. This combination has resulted in an increased burden on dental labs with respect to keeping up with the growing demand and subsequently higher lab bills for the dentist. So, what are some of the ramifications of this newer technology in the dental world?
By making the final impression process for multiunit implant prostheses more efficient by reducing chair time and simplifying the steps needed, PG allows more general dentists to take on a larger number of full-arch implant cases that might have otherwise been referred out to specialists.
Additionally, this technology can be cost effective for those who perform a high volume of implant restorations (both for provisionals after surgery and for final restorations) or for dentists who want to try to keep more lab work in-house to save on lab fees.
One consequence of PG is that its workflow is model-less, which can be a negative because there is no verified master cast on which titanium bases can be cemented or the passivity of the prostheses checked in advance. As a result, alternative solutions like the Optisplint have become increasingly popular, and more and more full-arch implant prostheses are now being printed or milled directly to the multiunit abutments with special screws that bypass the need for titanium bases. The number and variety of these “direct to multiunit abutment screws” are growing to meet the demand. Some examples of these include the DESS Full Arch Multiunit, Rosen, Vortex, SIN Screws and Powerball screws.
However, “while we routinely use these screws for surgical interims and prototypes, we have seen countless instances in the literature of an increased risk of zirconia being damaged over time when it interfaces directly with metal (i.e., zirconia abutments connected to titanium implants), so we do not like to use these screws for our final implant prostheses,” Farley said. “Instead, we use either titanium bases for a monolithic zirconia prosthesis or, our preference, a titanium bar with a monolithic zirconia sleeve cemented on top.”
Looking Toward the Future: The Digital Advantage
Regardless of the mode of impressionmaking, dentists must go to great lengths to accurately capture implant positions to better ensure the passive fit of implantsupported prostheses. This is because a lack of passive fit can introduce stress into the restoration and surrounding implants, resulting in increased risk for mechanical and biological complications such as bone resorption and screw-loosening, both of which can contribute to prosthetic failure.(3,12) While many studies support the accuracy of PG as a valid method of recording intraoral implant positions, we still need to use our best clinical judgment when evaluating the scope of dental literature as to when it would be fitting to harness this technique for our own cases.
“It is important that people don’t choose all-on-X because it is easier, but rather because it is the best treatment solution for the patient’s specific biology,” Schlam said. “Dentists should be careful not to treatment-plan full-arch implantsupported prostheses based solely off clinician preference but instead decide to do these cases according to what is best for the patient. It is our duty to educate patients about the pros and cons of all treatment options because implants are not without complications.”
If we do decide that implants are indicated, studies have shown that decreasing the number of procedural steps with CAD/CAM technology can increase the precision and survival of the implant prosthesis.(13) By leveraging the digital technology at our fingertips, not only can we be more efficient and profitable chairside, but our patients can be more comfortable, our workflows less complicated and our confidence levels maximized.
Leila Zadeh, DMD, FAGD, is an advanced restorative dentist at digitalDDS and an adjunct assistant professor at NYU Langone Health’s advanced education in general dentistry residency. She also creates educational content for Spear Education.
Zadeh is employed by digitalDDS, a prosthodontic continuing education platform that specializes in digital workflows, including Exocad, Meshmixer and Blue Sky Bio Software instruction. Zadeh reports no conflicts of interest pertaining to this topic. To comment on this article, email impact@agd.org.
References
1. “Facts & Figures.” American College of Prosthodontists, gotoapro.org/facts-figures/. Accessed 4 Sept. 2024.
2. Joensahakij, Nitchakul, et al. “The Accuracy of Conventional Versus Digital (Intraoral Scanner or Photogrammetry) Impression Techniques in Full-Arch Implant-Supported Prostheses: A Systematic Review.” Evidence-Based Dentistry, vol. 25, no. 4, 2024, pp. 216-217.
3. Ma, Bowen, et al. “Accuracy of Photogrammetry, Intraoral Scanning, and Conventional Impression Techniques for Complete-Arch Implant Rehabilitation: An In Vitro Comparative study.” BMC Oral Health, vol. 21, no. 1, 2021, p. 636.
4. Revilla-León, Marta, et al. “Comparison of Conventional, Photogrammetry, and Intraoral Scanning Accuracy of Complete-Arch Implant Impression Procedures Evaluated with a Coordinate Measuring Machine.” The Journal of Prosthetic Dentistry, vol. 125, no. 3, 2021, pp. 470-478.
5. Tohme, Hani, et al. “Accuracy of Implant Level Intraoral Scanning and Photogrammetry Impression Techniques in a Complete Arch with Angled and Parallel Implants: An In Vitro Study.” Applied Sciences, vol. 11, no. 21, 2021, p. 9859.
6. Jemt, Torsten, and Anders Lie. “Accuracy of Implant-Supported Prostheses in the Edentulous Jaw. Analysis of Precision of Fit between Cast Gold-Alloy Frameworks and Master Casts by Means of a Three-Dimensional Photogrammetric Technique.” Clinical Oral Implants Research, vol. 6, no. 3, 1995, pp. 172-180.
7. Jemt, Torsten, et al. “Photogrammetry: An Alternative to Conventional Impressions in Implant Dentistry? A Clinical Pilot Study.” The International Journal of Prosthodontics, vol. 12, no. 4, 1999, pp. 363-368.
8. Iturrate, Mikel, et al. “Accuracy of Digital Impressions for Implant– Supported Complete–Arch Prosthesis, Using an Auxiliary Geometry Part—An In Vitro Study.” Clinical Oral Implants Research, vol. 30, no. 12, 2019, pp. 1250-1258.
9. Pradíes, Guillermo, et al. “Using Stereophotogrammetric Technology for Obtaining Intraoral Digital Impressions of Implants.” The Journal of the American Dental Association, vol. 145, no. 4, 2014, pp. 338-344.
10. Gómez–Polo, Miguel, et al. “Accuracy, Scanning Time, and Patient Satisfaction of Stereophotogrammetry Systems for Acquiring 3D Dental Implant Positions: A Systematic Review.” Journal of Prosthodontics: Official Journal of the American College of Prosthodontists, vol. 32, suppl. 2, 2023, pp. 208-224.
11. Hussein, Mostafa Omran. “Photogrammetry Technology in Implant Dentistry: A Systematic Review.” The Journal of Prosthetic Dentistry, vol. 130, no. 3, 2023, pp. 318-326.
12. Kosago, Pitchaporn, et al. “Comparison of the Accuracy between Conventional and Various Digital Implant Impressions for an Implant– Supported Mandibular Complete Arch–Fixed Prosthesis: An in Vitro Study.” Journal of Prosthodontics: Official Journal of the American College of Prosthodontists, vol. 32, no. 7, 2023, pp. 616-624.
13. Peñarrocha-Diago, María, et al. “A Combined Digital and Stereophotogrammetric Technique for Rehabilitation with Immediate Loading of Complete-Arch, Implant-Supported Prostheses: A Randomized Controlled Pilot Clinical Trial.” The Journal of Prosthetic Dentistry, vol. 118, no. 5, 2017, pp. 596-603.
14. Bergin, Junping Ma, et al. “An in Vitro Comparison of Photogrammetric and Conventional Complete-Arch Implant Impression Techniques.” The Journal of Prosthetic Dentistry, vol. 110, no. 4, 2013, pp. 243-251.
15. Zhang, Yi-Jie, et al. “Accuracy of Photogrammetric Imaging Versus Conventional Impressions for Complete Arch Implant-Supported Fixed Dental Prostheses: A Comparative Clinical Study.” The Journal of Prosthetic Dentistry, vol. 130, no. 2, 2023, pp. 212-218.
16. Tohme, Hani, et al. “Comparison Between Stereophotogrammetric, Digital, and Conventional Impression Techniques in Implant-Supported Fixed Complete Arch Prostheses: An In Vitro Study.” The Journal of Prosthetic Dentistry, vol. 129, no. 2, 2023, pp. 354-362.
17. Revilla-León, Marta, et al. “Trueness and Precision of Complete-Arch Photogrammetry Implant Scanning Assessed with a Coordinate-Measuring Machine.” The Journal of Prosthetic Dentistry, vol. 129, no. 1, 2023, pp. 160-165.

