16 minute read
CPD: Rejuvenating the Neck
Rejuvenating the Neck
Dr Ahmed El Houssieny discusses treatment planning for the ageing neck using non-invasive interventions
Advertisement
Patients requesting non-invasive aesthetic treatment for an ageing neck may report a range of unwanted signs. These include loose or sagging skin, changes in skin colour or texture, accumulation of fat between the chin and the neck, changes to the cervicomental angle, horizontal ‘necklace’ lines or vertical platysmal bands on the neck itself.1,2 It is no longer the case that surgery presents the only option for addressing these signs. Now a growing range of minimally invasive treatment options are available. Injectable agents, such as botulinum toxin and soft-tissue fillers have a key role to play, as do devices and techniques including energy-based treatments.2,3 This article takes a closer look at how to approach rejuvenation of the neck and some of the treatments that are appropriate, as well as the evidence for combinations of treatments in this delicate and complex area.
Anatomy of the neck
Several layers of the superficial anatomy of the skin may be implicated in non-invasive treatment for the effects of ageing.1 Dermal thinning can occur due to ageing or ultraviolet damage.4 Other indications of photodamage on the skin’s surface include lentigines, telangiectasia and dyschromia.5 Below the dermis and epidermis lie the planes of subcutaneous fat, the platysma muscle and the deeper subplatysmal fat with the digastric muscles and the submandibular glands.4,6 Fat may accumulate or be repositioned in the subcutaneous and subplatysmal layers as part of the ageing process (Figure 1).7 The platysma muscle extends from the collar bone to the musculoaponeurotic system of the face and pulls the skin of the neck in downward and lateral directions. 8 It is important, therefore, to include the lower face in the physical examination as it too may
Skin Subcutaneous Tissue require treatment to address signs of ageing in the neck (Figure 2).6 Hyperkinetic activity and loss of muscle Muscle tone with age can result in Fascia the appearance of vertical muscle bands as well as horizontal neck rhytides (necklace lines) and sagging skin.8,9 Interestingly, younger patients are also increasingly experiencing horizontal lines, possibly due to looking down at a computer Figure 1: Cross-section of screen or mobile device for superficial planes in the neck extended periods.10 Injectable treatment options
Botulinum toxin As a neuromodulator, botulinum toxin (BoNT-A) works by blocking the release of the neurotransmitter acetylcholine, which produces a temporary reduction in muscle contractions lasting for three months or more.11 The toxin is the first-line therapy in platysmal banding and is recommended for the prevention of or early intervention in the formation of prominent bands.4 In addition to showing efficacy in treating lines caused by movement of the platysma, BoNT-A has also shown improvement in re-contouring the jaw in a so-called Nefertiti lift.8 Of the 30 patients in a study by Jabbour et al., improvement in the appearance of both the neck and jaw was reported by respondents in 93.3% of patients with both platysmal bands at rest and when contracted, showing statistically significant improvement.8 A subsequent study also showed statistically significant improvement in platysmal banding at contraction, jowls and neck volume in 25 patients who had previously undergone a Nefertiti lift and were subsequently treated with BoNT-A using a microdroplet technique.12 However, in the Jabbour study, significant improvement in platysmal banding occurred at contraction and at rest (p<0.0001 and p = 0.022 respectively) but only at contraction and not at rest in the Awaida study (p<0.0001 and p = 0.6269 respectively), suggesting that the microdroplet technique may be more appropriate to address sagging skin caused by ptosis of the soft tissues.12 When targeting the platysmal bands, BoNT-A should be injected into the platysma intramuscularly or intracutaneously at three to six points in each band with a dose ranging from 6 to 12 units per band, with a maximum total dose of 60 U of onabotulinumtoxin A.13 Dose choice should reflect the requirements of the individual patient. Intracutaneous injection can be used in order to minimise the depth and magnitude of toxin administration.13 Doses greater than 50 U may impede the function of the neck flexor and deglutition muscles.4 Differences in doses between ona- and incobotulinumtoxin A and those for abobotulinumtoxin A should be noted.11 A conversion ratio of 1:2.5 (inco/onabotulinumtoixn A: abobotulinumtoxin A) has been suggested when treating the face based on the literature and clinical experience.14 Treating patients in the sitting position can make the platysmal banding more visible and asking the patient to clench their teeth enables the practitioner to target the bands and inject directly into the muscle.9 Injection deep into the structures of the neck should be avoided.9 Dysphagia, dyspnea, dry mouth and neck weakness are rare adverse effects of BoNT-A when injecting in the platysma.9,13 The risk can be minimised by careful monitoring of doses and avoidance of injection into the thyroid cartilage.9,13
Sternocleidomastoid
Depressor anguli oris Trapezius
Platysma
Figure 2: Extent of platysma muscle
Dermal fillers and skin boosters The practitioner has a choice of dermal fillers for use in the rejuvenation of the neck including hyaluronic acid (HA), calcium hydroxylapatite (CaHa), polycaprolactone (PCL) and poly L-lactic acid (PLLA) fillers. Injections of HA fillers at different layers of tissue create volume, whereas biostimulatory fillers such as CaHa, PCL and PLLA fillers induce neocollagenesis, thus increasing volume, tightening the skin and lifting the tissue.3,15,16 While fillers have not been a mainstay treatment in the rejuvenation of the neck, HA fillers have been effective in the treatment of horizontal neck lines or ‘necklace’ lines.17,18 HA filler formulations with and without cross-linking have both shown good results.2,18 In a study of non-cross-linked HA, significantly improved horizontal neck lines (P = 0.000) were reported on follow-up visits up to 10 months in 25 patients who received two to three sessions of an HA compound filling plus mesotherapy when compared with one treatment of BoNT-A.2 Results were graded by blinded evaluators and levels of patient satisfaction were assessed.2 The authors conclude that the effect of the mesotherapy in addressing dryness and fine lines may be complementary to the efficacy of the filler.2 Analysis of a retrospective case series showed that treatment with a cross-linked, cohesive polydensified matrix HA filler with low elastic modulus, low viscous modulus and a high tan delta was also associated with improvement in wrinkle intensity in 64 lateral neck halves (from 32 women), as assessed by Horizontal Neck Wrinkle Severity Scale, from the second week onwards (1.352 ± 0.682, P<0.05).18 Further, diluted CaHa fillers are recommended as a treatment for skin laxity and skin quality without a volumising effect in areas, including the neck, where the skin is thin.4,19,20 Injections of CaHa fillers have shown efficacy in the neck when administered as a single therapy and in combination.21-23 CaHa fillers combined with microfocused ultrasound with visualisation (MFU-V) have been shown to reduce fine lines and improve the texture of the skin in two studies of 20 and 47 participants respectively.22,23 Diluted PLLA fillers have also demonstrated improvements to skin laxity and volume in the neck.24 A combination with microfocused ultrasound has been recommended based on clinical practice.25 The administration of a multi-treatment approach to the rejuvenation of the neck using PCL filler with an HA filler and suspension sutures is suggested based on expert consensus.3 There is a need for further published studies in the use of CaHa, PLLA and PCL fillers alone and in combination with other treatment options in the neck. HA fillers can also be injected more superficially when used as skin boosters in the neck, where the aim is to improve overall skin quality. Dehydration of the skin increases with age, but the injection of a small-particle HA filler in micro-aliquots in the neck in one small study (n=15) has been found to improve hydration levels.26,27 The recommended volume for the neck per injection of the skin boosting HA filler is the smallest injectable aliquot (0.05ml) with a total volume of 1ml, which should be injected into the deep dermis, targeting areas such as horizontal lines as needed.28 Stretching the skin of the neck while administering filler injections can help in identifying the depth of injection as well as reducing discomfort for the patient and minimising bruising.28 The most common adverse events associated with fillers post-injection are transient erythema, pruritus, ecchymosis and localised swelling.18,19
Deoxycholic acid Deoxycholic acid, unlike other treatment options for the neck, is a lipolytic agent that addresses submental fat.5 Approved by the Food and Drug Administration (FDA) in the US in 2015, deoxycholic acid injection (ATX-101) has shown efficacy in significantly reducing submental fat deposits without increasing skin laxity in the area.29,30 Results of the randomised controlled studies showed a ≥1-point improvement in the Clinician-Reported Submental Fat Rating Scale in 62.3% of participants (n=122) receiving 2mg/cm2 of ATX-101 vs 34.5% (n=117) with placebo in the study by Ascher et al. and 65.3% (n=121) vs 23% (n=122) in the study by Rzany et al. (p<0.001 for both studies).29,30 The effects of the treatment are maintained more than five years without the need for maintenance treatments.31 Injections may be performed roughly every six weeks, but due to the fact that post-treatment swelling, erythema and bruising can cause repeated inflammation, they shouldn’t be performed more often than every four weeks.1,25 In most cases, adverse effects are mild and transient.31 Patients who are likely to benefit most from this
treatment are those with a moderate to large amount of submental fat in the pre-platysmal layer, but with only moderate laxity of the submental skin.32 Injection into the fat of the pre-platysmal fat should be done with care to avoid nearby anatomic structures.32
Energy-based devices
Laser treatment The use of lasers to resurface the skin by removing epidermal and dermal layers has developed greatly over recent decades and now represents an effective and safe method for treating photoaged skin, dyschromia and facial rhytides.33 The advent of CO2 and erbium-doped yttrium aluminium garnet (Er:YAG) lasers has increased the practitioner’s control in targeting specific areas of skin and at different depths.33 Due to the thinness of the skin on the neck, it is suggested that fractionated (targeting a specific fraction of skin) may be preferable to non-fractionated (full-field) laser treatment in the neck and that it should go no deeper than the papillary layer of the dermis.1 This depth is indicated by pinpoint bleeding and a subtle yellowing in the colour of the skin.1 Laser resurfacing has been shown to be a low-risk procedure with possible adverse effects including scarring and dyspigmentation.33 Laser resurfacing is not recommended in patients with darker skin (Fitzpatrick skin types IV to VI), a history of keloidal scarring or prior radiation therapy.33 By emitting energy into the skin, laser resurfacing stimulates neocollagenesis, remodelling and skin tightness.33 A 2014 study with 20 participants of the long-term effects of treatment for the ageing neck with fractional CO2 lasering identified significant (p<0.0001) improvements in skin laxity, jowling and horizontal neck lines after one month that were maintained after one year.7 Improved skin tightness also improved the appearance of fat tissue.7 Some studies of laser treatment in combination with MFU or HA fillers to address skin ageing in the neck are available and have demonstrated that combined treatment is able to address multiple signs of ageing.34-36 A retrospective analysis by Woodward and colleagues of 60 patients from three centres who had undergone treatment to the neck, for example, reported significant improvement in skin laxity and photodamage with combined ablative fractionated laser treatment with micro-focused ultrasound.34
Radiofrequency As with other energy-based devices, radiofrequency (RF) uses thermal energy applied to the dermis to stimulate the generation of new collagen and elastin.37,38 Low fluence, multiple pass treatment is considered to be effective and safe.38,39 RF works in a different way to lasers, allowing epidermal protection while heating the dermal collagen to the optimal level.37 Monopolar and bipolar devices are available, the latter penetrating the skin less deeply, offering more control for the practitioner and less discomfort for patients.37 A study of hybrid bipolar RF in patients with neck and lower face laxity (n = 247) found a statistically significant improvement (P < 0.001) from pre- to post-treatment, and that larger effects were noted in the older patients (mean age 55.1 years).40 The modality is also effective in combination with other treatment modalities, with a significant improvement in a sagging neck shown in 158 patients who were given four sessions of treatment with RF and ultrasound hybrid device at each appointment.38 In RF microneedling, the application of microneedles to different depths of the skin at the same time as the release of RF energy stimulates the production of collagen and elastin. Administered alone or in combination with platelet-rich plasma, RF microneedling demonstrated in a 2022 study with 20 participants that significant improvement in dermal thickness and measurement of cervicomental angle was achieved with both treatment modalities.41 RF is considered to be most effective in patients with mild-to-moderate skin laxity and should not be used in individuals who have or have had a pacemaker or defibrillator, nor in those using oral isotretinoin, with keloids, or hypertrophic scarring.9
Intense pulsed light Intense pulsed light (IPL) is a non-laser, high-intensity light source that uses broad wavelengths to deliver pulses of light to the skin.42 IPL is effective in addressing age-related changes of the dermis.5 It has shown efficacy in disorders of pigmentation and telangiectasias, clearing more than 75% of telangiectasias and hyperpigmentation in a study of 135 participants with poikiloderma of Civatte.43 The thin skin of the neck requires IPL to be administered at lower settings than those used on the face in order to avoid adverse effects or slowing the healing process.5 IPL is reported to have a lower incidence of post-treatment hyperpigmentation in Fitzpatrick skin types IV to VI compared with laser treatment.44 Studies show the efficacy of IPL in combination with laser treatment in the face.45,46 In combination with ablative fractional laser treatment, for example, IPL showed significantly increased skin elasticity, reduced skin wrinkles and improved skin texture in
a population of 28 Chinese women with an average age of 51.4 years.45 However, further studies of IPL in combination with a range of other treatments for rejuvenating the neck are needed.
Making a treatment plan
In some cases, the ageing neck may be successfully treated with one treatment option.1,10,47 However, given that there are many different factors in the ageing process, age-related changes to the neck may require multiple interventions in combination for optimal improvements.3,4,5 Indeed, many combination treatments in the ageing neck have been shown to be effective and well-tolerated with no increases in the incidence of adverse events.3,4,26,48 It is of note that, to date, the published literature of non-invasive treatments for the ageing neck is largely based on non-randomised control trials and case studies, and further research in this area of the body would be welcome.3,19,49
Conclusion
It has become possible to treat many signs of the ageing neck in a way which is more time-effective and less costly than surgery. The neck needs to be considered in relation to the face – rejuvenating one without the other can look uneven – yet the dermal thinness and the anatomical structure of the neck demand a specific treatment approach. More than one sign of ageing may be present and a combination of treatments may be required. It is an area of aesthetic practice that is developing quickly as technology becomes available and evidence is accrued for more treatment combinations. Non-surgical interventions are not suitable for all patients, and those with severe ageing are likely to require surgery, so practitioners should be doing appropriate assessments/patient selections.
Dr Ahmed El Houssieny is a trained anaesthetist with a passion for aesthetics. He is an honorary lecturer at the University of Chester and an education provider on cosmetic procedures. Dr El Houssieny is an associate member of the British College of Aesthetic Medicine. Qual: MBBCH
VIEW THE REFERENCES ONLINE! AESTHETICSJOURNAL.COM
13 & 14 Oct ExCeL London, UK
Dr El Houssieny will be speaking at CCR on October 14. Turn to p.20 to register for free! Clinical Advisory Board Member Miss Elizabeth Hawkes says...
Dr Ahmed El Houssieny discusses non-surgical neck rejuvenation in this month’s CPD article. The article covers anatomy and the interplay of muscle and fat in the ageing neck. The neck is a challenging area to treat and often a common aesthetic concern, particularly now in the younger patient. The article covers non-surgical options such as botulinum toxin injections to the platysma muscle. There is a thorough discussion on the use of dermal fillers for rejuvenation, cross linked and non-crosslinked hyaluronic acid and the use of biostimulatory fillers. The use of deoxycholic acid to submental fat is briefly covered; this treatment will gain popularity over the next few years as techniques are refined. Finally, the article covers energy-based devices including the use of laser resurfacing, radiofrequency and intense pulsed light.
In clinical practice, a combination approach is required for optimal results and will vary according to the patient’s age and clinical findings. This article provides a foundation for further reading on non-surgical neck rejuvenation.
Test your knowledge! Complete the multiple-choice questions and go online to receive your CPD certificate!
Questions
1. Toxin is recommended for the prevention of, or early intervention in the formation of prominent neck bands. What is the target muscle?
2. Which of the following are options for addressing signs of an ageing neck?
3. Which of these fillers can be used in rejuvenation of the neck?
Possible answers
a. Frontalis b. Zygmaticus major c. Platysma d. Masseter
a. Surgery b. RF c. Microneedling d. All of the above
a. Hyaluronic acid b. CaHa c. PLLA d. All of the above
4. Which lipolytic agent has shown efficiency in reducing submental fat deposits? a. Deoxycholic acid b. Hyaluronic acid c. Hydrochloric acid d. Nitric acid
5. Which treatments have been used in combination to treat the neck? a. Radiofrequency and microneedling b. Hyaluronic acid and toxin c. Laser and RF d. All of the above
Answers: C,D,D,A,D

Discover the Baby Face protocols,
with the world’s most in-demand Laser Facial

20 MINUTES 3 STEPS to meet all needs
Pigmented lesions | Melasma | Radiance | Texture Skin rejuvenation | Active acne | Wrinkles | Large pores

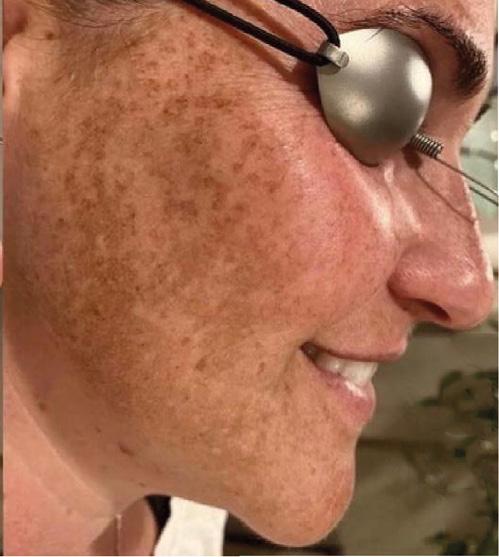
Before After 2 treatments

With the courtesy of Megan Sotiropoulos, (RN, BSN)
Book your Demo to see why LaseMD Ultra™ is revolutionising skin rejuvenation!

For more information, please contact Lutronic PBS UK & Ireland: