
27 minute read
SECTION 6 Primary Care
SECTION 6 Primary Care Nurse Practitioner Services
SUMMARY
Effective management of the unique needs of geriatric health requires routine health screenings, medical assessments and evaluation with a primary care provider. The Acts Nurse Practitioners offer primary care services in all its communities to participate in the care of our residents by providing high-quality primary, acute, and specialty senior health care services, helping our residents live longer, healthier, happier lives.
THE ANNUAL WELLNESS EVALUATION
Acts residents are provided with an ANNUAL HEALTH AND WELLNESS EVALUATION (AHWE) each calendar year. The AHWE is a comprehensive medical visit designed to develop and update a personalized prevention plan to help prevent disease and disability, based on the resident’s current health and risk factors. The AHWE includes the following:
✓ Completion of a Health History Assessment and Resident Information Update ✓ Performance of a Comprehensive Medical Evaluation ✓ Performance of Various Health Screenings and Assessments ✓ A Personalized Resident Health Advice and Referral Plan ✓ Review of Medical, Legal and Advance Care Planning
WELLNESS STAFF
The Acts NP Primary Care Practices are located on campus in the Wellness Suites. The Wellness Suites are staffed with Nurse Practitioners, Wellness Office Nurses, Wellness Office Coordinators and (in select communities), a Nurse Navigator. The Wellness staff play an integral role in the AWE and ongoing healthcare needs of the Acts residents.
TECHNOLOGY and EQUIPMENT
• Electronic Health Record System(s) – NextGen Software Solutions (implemented in
July 2022 to the pilot community, St. Andrews Estates)
• Vitals Monitoring – on order • Body Composition Analyzer – equipment to be loaned by the vendor on a trial basis. Arrangements in progress. • Chemical Analyzer/Bloodwork – on order • Urine Analyzer – on order • EKG (electrocardiogram) Machine – standing equipment in all Wellness Suite. Replacement EKG ordered for North campus. • Bladder scanner -- standing equipment in all Wellness Suite • Nebulizer -- standing equipment in all Wellness Suite • Diabetes Management - PT/INR, A1C -- standing equipment in all Wellness Suite
PRIMARY CARE/NP SERVICES ANNUAL HEALTH AND WELLNESS EXAM
PROCESS
Annual Health and Wellness Pre-Visit
1. Resident is scheduled for their pre-annual interview by the Well-Being Coach. The resident reports to the Wellness Office at the time of the appointment. 2. Wellness Office Coordinator reviews and updates (in real time) the resident’s health history and information and documents all changes and updates in the electronic medical record. (Resident is to be provided with a copy of their demographics face sheet. This copy if kept in a plastic container in the resident’s freezer and made available to emergency services if needed). 3. The Mini Nutritional Assessment and height and weight measurements are completed by the Wellness Office Nurse and recorded in the electronic medical record. 4. Blood draw is done for routine blood testing. Processing is completed inhouse and/or sent to an outside lab for processing. 5. Performance of Testing: EKG, Urinalysis, Body Comp Analysis, Bladder Scanning (as indicated)
Annual Health and Wellness Exam with the Nurse Practitioner
Resident reports to the Wellness Suite for their scheduled visit with the Nurse Practitioner
• The NP will review all of the data provided by the Well-Being Coach prior to the resident’s scheduled visit. The NP will conduct a physical exam and complete the assessments listed below. The majority of the assessments are incorporate in an Annual Wellness template that is available in the electronic health record system (NextGen).
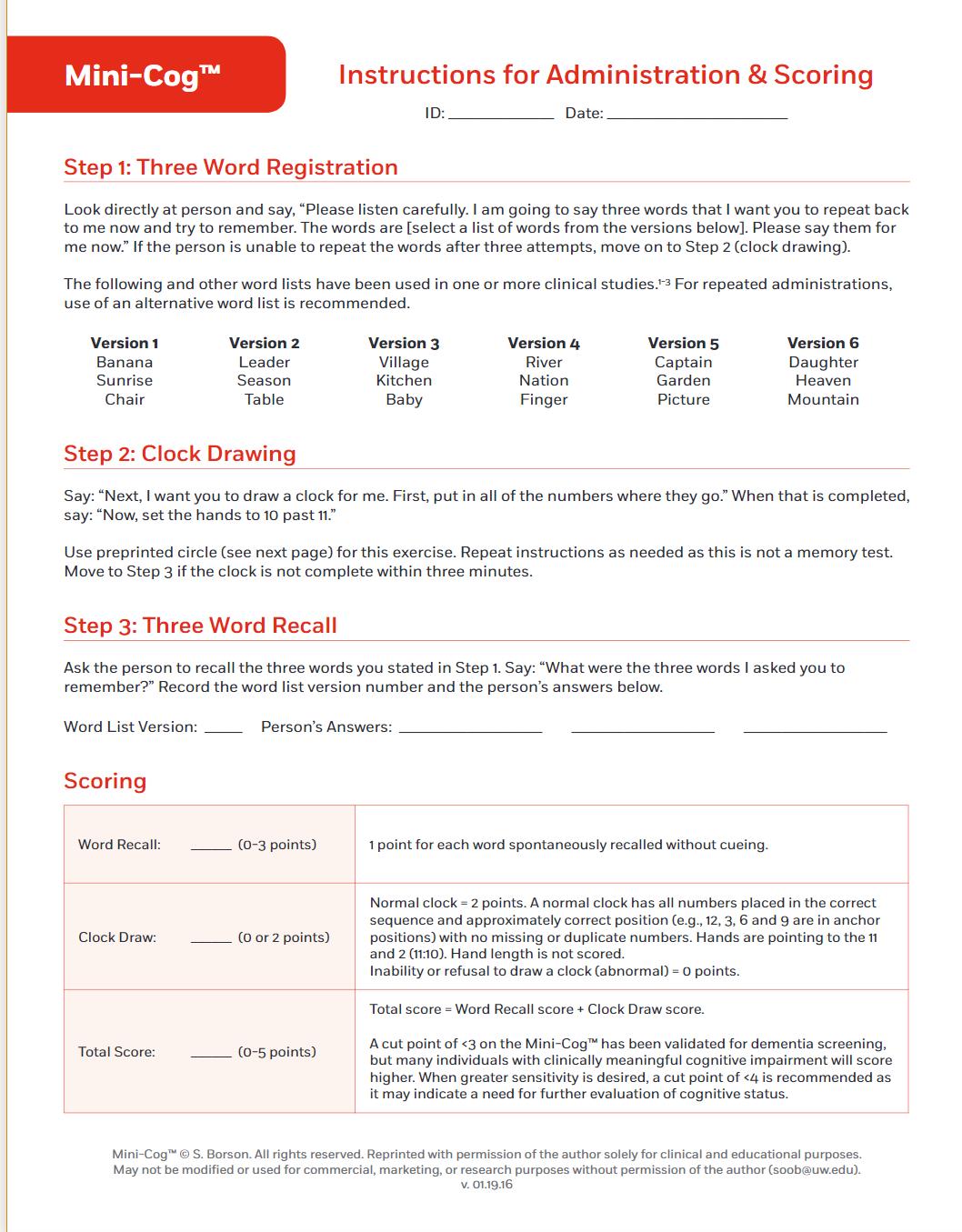
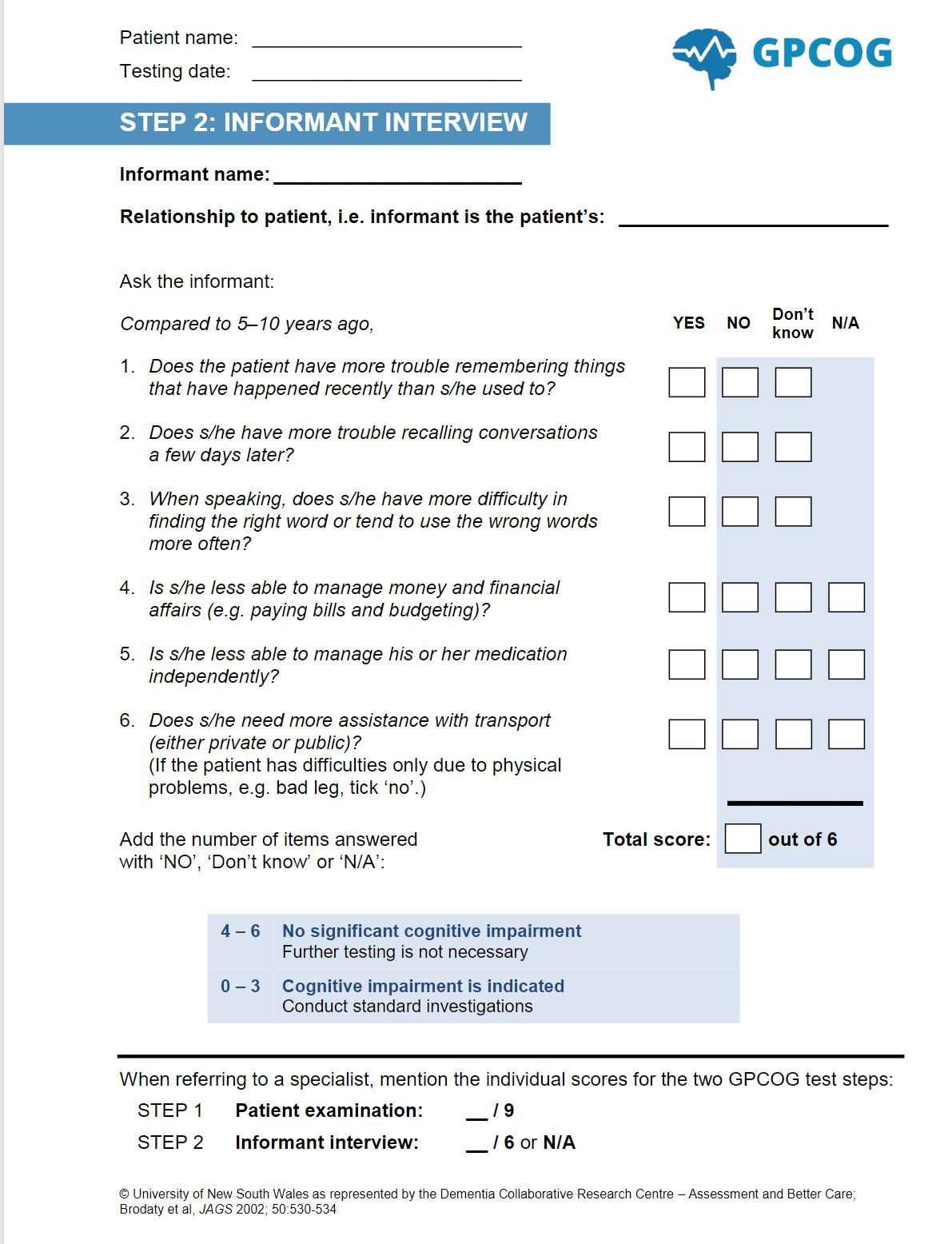
1. High blood pressure screening 2. High cholesterol screening 3. Depression screening 4. Abnormal blood glucose/diabetes screening 5. Stress management assessment 6. Osteoporosis screening 7. Hepatitis C screening 8. Sexually transmitted infections screening 9. Audio screening 10.Visual screening 11.In-Home Risks and Activities of
Daily Living (ADLs) 12.Instrumental ADLs (IADLs) 13.Provide Sleep Assessment 14.Cognitive function test 15.Behavioral risk assessment 16.Psychosocial risk assessment 17.Incontinence assessment 18.Polypharmacy assessment 19.Chronic conditions assessment 20.Signs of elder mistreatment assessment
• A review of medical, legal and advance care planning is completed
• Following the visit, the NP will create a personalized resident health advise and referral plan and provide the completed plan to the Well-Being Coach for insertion to the resident’s
Signature Well-Being Portfolio.
(Medicare) Annual Wellness Visit Providing Personalized Prevention Plan Services
-- Guidelines for the Acts Signature Well-Being Annual Health and Wellness Visit are derived from CMS guidelines for Annual Wellness Visit for Medicare beneficiaries:
(a) Definitions. For purposes of this section -
A review of any current opioid prescriptions means, with respect to the individual determined to have a current prescription for opioids, all of the following: (i) A review of the potential risk factors to the individual for opioid use disorder; (ii) An evaluation of the individual's severity of pain and current treatment plan; (iii) The provision of information on non-opioid treatment options; and (iv) A referral to a specialist, as appropriate.
Detection of any cognitive impairment means assessment of an individual's cognitive function by direct observation, with due consideration of information obtained by way of patient report, concerns raised by family members, friends, caretakers or others.
Eligible beneficiary means an individual who is no longer within 12 months after the effective date of his or her first Medicare Part B coverage period and who has not received either an initial preventive physical examination or an annual wellness visit providing a personalized prevention plan within the past 12 months.
Establishment of, or an update to the individual's medical and family history means, at minimum, the collection and documentation of the following: (i) Past medical and surgical history, including experiences with illnesses, hospital stays, operations, allergies, injuries and treatments. (ii) Use or exposure to medications and supplements, including calcium and vitamins. (iii) Medical events in the beneficiary's parents and any siblings and children, including diseases that may be hereditary or place the individual at increased risk.
First annual wellness visit providing personalized prevention plan services means the following services furnished to an eligible beneficiary by a health professional that include, and take into account the results of, a health risk assessment, as those terms are defined in this section: (i) Review (and administration if needed) of a health risk assessment (as defined in this section). (ii) Establishment of an individual's medical and family history. (iii) Establishment of a list of current providers and suppliers that are regularly involved in providing medical care to the individual. (iv) Measurement of an individual's height, weight, body-mass index (or waist circumference, if appropriate), blood pressure, and other routine measurements as deemed appropriate, based on the beneficiary's medical and family history. (v) Detection of any cognitive impairment that the individual may have, as that term is defined in this section. (vi) Review of the individual's potential (risk factors) for depression, including current or past experiences with depression or other mood disorders, based on the use of an
appropriate screening instrument for persons without a current diagnosis of depression, which the health professional may select from various available standardized screening tests designed for this purpose and recognized by national medical professional organizations. (vii) Review of the individual's functional ability and level of safety, based on direct observation or the use of appropriate screening questions or a screening questionnaire, which the health professional as defined in this section may select from various available screening questions or standardized questionnaires designed for this purpose and recognized by national professional medical organizations. (viii) Establishment of the following: (A) A written screening schedule for the individual such as a checklist for the next 5 to 10 years, as appropriate, based on recommendations of the United States Preventive Services Task Force and the Advisory Committee on Immunization Practices, and the individual's health risk assessment (as that term is defined in this section), health status, screening history, and age-appropriate preventive services covered by Medicare. (B) A list of risk factors and conditions for which primary, secondary or tertiary interventions are recommended or are underway for the individual, including any mental health conditions or any such risk factors or conditions that have been identified through an initial preventive physical examination (as described under § 410.16 of this subpart), and a list of treatment options and their associated risks and benefits. (ix) Furnishing of personalized health advice to the individual and a referral, as appropriate, to health education or preventive counseling services or programs aimed at reducing identified risk factors and improving self management, or community-based lifestyle interventions to reduce health risks and promote self-management and wellness, including weight loss, physical activity, smoking cessation, fall prevention, and nutrition. (x) At the discretion of the beneficiary, furnish advance care planning services to include discussion about future care decisions that may need to be made, how the beneficiary can let others know about care preferences, and explanation of advance directives which may involve the completion of standard forms. (xi) Furnishing of a review of any current opioid prescriptions as that term is defined in this section. (xii) Screening for potential substance use disorders including a review of the individual's potential risk factors for substance use disorder and referral for treatment as appropriate. (xiii) Any other element determined appropriate through the national coverage determination process.
Health professional means (i) A physician who is a doctor of medicine or osteopathy (as defined in section 1861(r)(1) of the Act); or (ii) A physician assistant, nurse practitioner, or clinical nurse specialist (as defined in section 1861(aa)(5) of the Act); or (iii) A medical professional (including a health educator, a registered dietitian, or nutrition professional, or other licensed practitioner) or a team of such medical professionals, working under the direct supervision (as defined in § 410.32(b)(3)(ii)) of a physician as defined in paragraph (i) of this definition.
Health risk assessment means, for the purposes of this section, an evaluation tool that meets the following criteria: (i) Collects self-reported information about the beneficiary. (ii) Can be administered independently by the beneficiary or administered by a health professional prior to or as part of the AWV encounter. (iii) Is appropriately tailored to and takes into account the communication needs of underserved populations, persons with limited English proficiency, and persons with health literacy needs. (iv) Takes no more than 20 minutes to complete. (v) Addresses, at a minimum, the following topics: (A) Demographic data, including but not limited to age, gender, race, and ethnicity. (B) Self assessment of health status, frailty, and physical functioning. (C) Psychosocial risks, including but not limited to, depression/life satisfaction, stress, anger, loneliness/social isolation, pain, and fatigue. (D) Behavioral risks, including but not limited to, tobacco use, physical activity, nutrition and oral health, alcohol consumption, sexual health, motor vehicle safety (seat belt use), and home safety. (E) Activities of daily living (ADLs), including but not limited to, dressing, feeding, toileting, grooming, physical ambulation (including balance/risk of falls), and bathing. (F) Instrumental activities of daily living (IADLs), including but not limited to, shopping, food preparation, using the telephone, housekeeping, laundry, mode of transportation, responsibility for own medications, and ability to handle finances.
Review of the individual's functional ability and level of safety means, at minimum, assessment of the following topics: (i) Hearing impairment. (ii) Ability to successfully perform activities of daily living. (iii) Fall risk. (iv) Home safety. Subsequent annual wellness visit providing personalized prevention plan services means the following services furnished to an eligible beneficiary by a health professional that include, and take into account the results of an updated health risk assessment, as those terms are defined in this section: (i) Review (and administration, if needed) of an updated health risk assessment (as defined in this section). (ii) An update of the individual's medical and family history. (iii) An update of the list of current providers and suppliers that are regularly involved in providing medical care to the individual as that list was developed for the first annual wellness visit providing personalized prevention plan services or the previous subsequent annual wellness visit providing personalized prevention plan services. (iv) Measurement of an individual's weight (or waist circumference), blood pressure and other routine measurements as deemed appropriate, based on the individual's medical and family history. (v) Detection of any cognitive impairment that the individual may have, as that term is defined in this section. (vi) An update to the following:
(A) The written screening schedule for the individual as that schedule is defined in paragraph (a) of this section for the first annual wellness visit providing personalized prevention plan services. (B) The list of risk factors and conditions for which primary, secondary or tertiary interventions are recommended or are underway for the individual as that list was developed at the first annual wellness visit providing personalized prevention plan services or the previous subsequent annual wellness visit providing personalized prevention plan services. (vii) Furnishing of personalized health advice to the individual and a referral, as appropriate, to health education or preventive counseling services or programs as that advice and related services are defined in paragraph (a) of this section. (viii) At the discretion of the beneficiary, furnish advance care planning services to include discussion about future care decisions that may need to be made, how the beneficiary can let others know about care preferences, and explanation of advance directives which may involve the completion of standard forms. (ix) Furnishing of a review of any current opioid prescriptions as that term is defined in this section. (x) Screening for potential substance use disorders including a review of the individual's potential risk factors for substance use disorder and referral for treatment as appropriate. (xi) Any other element determined appropriate through the national coverage determination process. (b) Conditions for coverage of annual wellness visits providing personalized prevention plan services. Medicare Part B pays for first and subsequent annual wellness visits providing personalized prevention plan services that are furnished to an eligible beneficiary, as described in this section, if they are furnished by a health professional, as defined in this section. (c) Limitations on coverage of an annual wellness visit providing personalized prevention plan services. Payment may not be made for either a first or a subsequent annual wellness visit providing personalized prevention plan services that is performed for an individual who is (1) Not an eligible beneficiary as described in this section. (2) An eligible beneficiary as described in this section and who has had either an initial preventive physical examination as specified in § 410.16 of this subpart or either a first or a subsequent annual wellness visit providing personalized prevention plan services performed within the past 12 months.
(d) Effective date. Coverage for an annual wellness visit providing personalized prevention plan services is effective for services furnished on or after January 1, 2011.
Source: Code of Federal Regulation, Title 42, Chapter 4, Subchapter B, Part 410, Subpart B
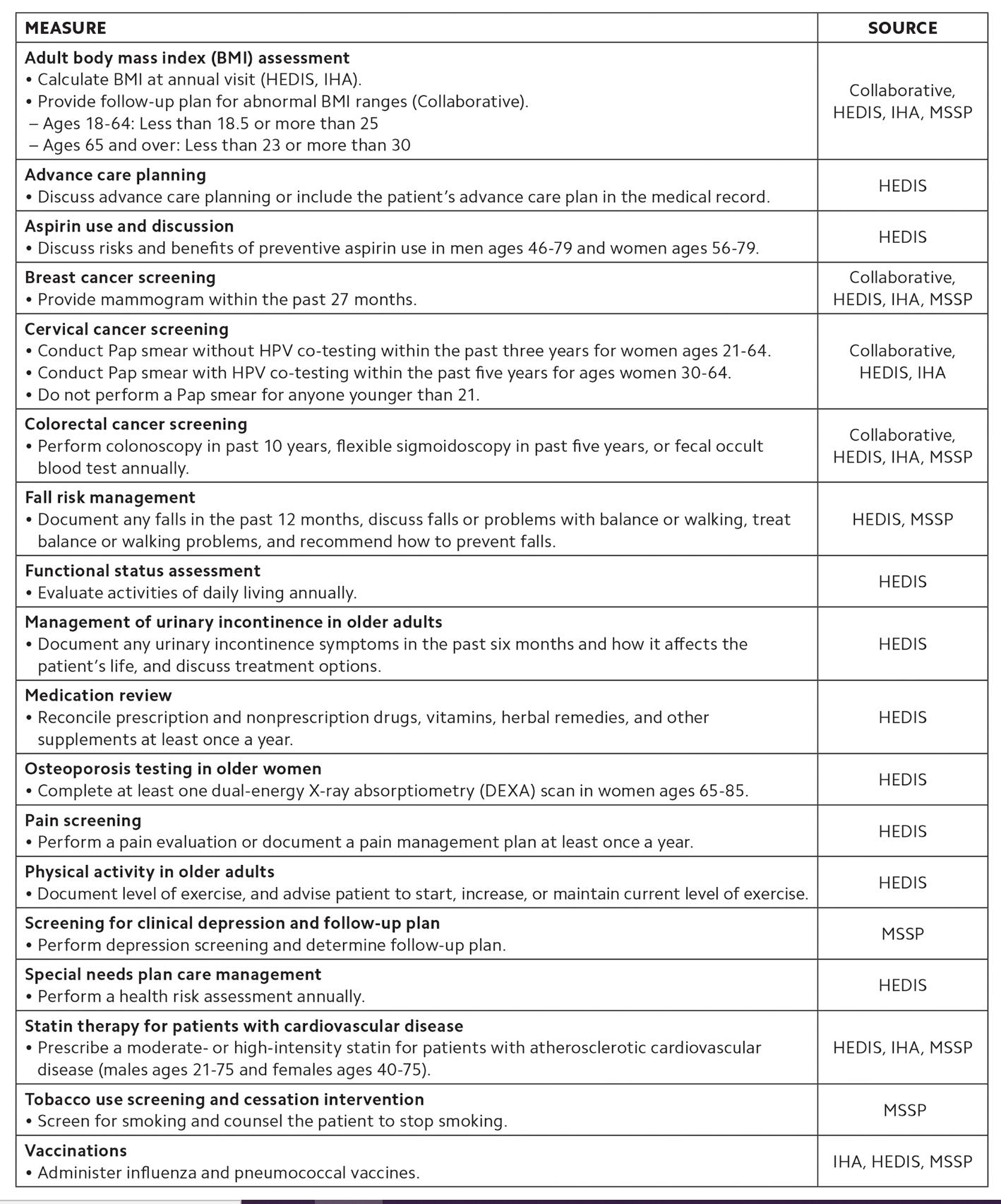
A significant number of the primary care assessments are embedded within one comprehensive Annual Wellness Assessment Template:

The Pittsburgh Sleep Quality Index (PSQI) is an effective instrument used to measure the quality and patterns of sleep in adults. It differentiates “poor” from “good” sleep quality by measuring seven areas (components): subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medications, and daytime dysfunction over the last month.
INSTRUCTIONS :
The following questions relate to your usual sleep habits during the past month only. Your answers should indicate the most accurate reply for the majority of days and nights in the past month. Please answer all questions.
During the past month:
1. When have you usually gone to bed? 2. How long (in minutes) has it taken you to fall asleep each night? 3. What time have you usually gotten up in the morning? 4. How many hours of actual sleep did you get at night? How many hours were you in bed?
5. During the past month, how often have you had trouble sleeping because you
A. Cannot get to sleep within 30 minutes B. Wake up in the middle of the night or early morning C. Have to get up to use the bathroom D. Cannot breathe comfortably
E. Cough or snore loudly
F. Feel too cold
G. Feel too hot
H. Have bad dreams
I. Have pain J. Other reason (s), please describe, including how often you have had trouble sleeping because of this reason (s): Not during the past month (0) Less than once a week (1)
6. During the past month, how often have you taken medicine (prescribed or “over the
counter”) to help you sleep? 7. During the past month, how often have you had trouble staying awake while driving, eating meals, or engaging in social activity? 8. During the past month, how much of a problem has it been for you to keep up enthusiasm to get things done? 9. During the past month, how would you rate your sleep quality overall? Very good (0) Fairly good (1) Fairly bad (2) Very bad (3)
Once or twice a week (2) Three or more times a week (3)
Component 1 #9 Score
Component 2 #2 Score (<15min (0), 16-30min (1), 31-60 min (2), >60min (3)) + #5a Score (if sum is equal 0=0; 1-2=1; 3-4=2; 5-6=3)
Component 3 #4 Score (>7(0), 6-7 (1), 5-6 (2), <5 (3)
Component 4 (total # of hours asleep) / (total # of hours in bed) x 100 >85%=0, 75%-84%=!, 65%-74%=2, <65%=3
Component 5 # sum of scores 5b to 5j (0=0; 1-9=1; 10-18=2; 19-27=3)
Component 6 #6 Score
Component 7 #7 Score + #8 score (0=0; 1-2=1; 3-4=2; 5-6=3) C1
C2
C3
C4
C5
C6
C7
Add the seven component scores together _______________ Global PSQI
A total score of “5” or greater is indicative of poor sleep quality. If you scored “5” or more it is suggested that you discuss your sleep habits with a healthcare provider
• In-Home Risks and Activities of Daily Living (ADLs)
Katz Index of Independence in Activities of Daily Living
Activities
Points (1 or 0) Independence
(1 Point) Dependence
(0 Points)
BATHING
Points:
DRESSING
Points:
TOILETING
Points: NO supervision, direction or personal assistance. WITH supervision, direction, personal assistance or total care.
(1 POINT) Bathes self completely or needs help in bathing only a single part of the body such as the back, genital area or disabled extremity. (0 POINTS) Need help with bathing more than one part of the body, getting in or out of the tub or shower. Requires total bathing
(1 POINT) Get clothes from closets and drawers and puts on clothes and outer garments complete with fasteners. May have help tying shoes. (0 POINTS) Needs help with dressing self or needs to be completely dressed.
(1 POINT) Goes to toilet, gets on and off, arranges clothes, cleans genital area without help. (0 POINTS) Needs help transferring to the toilet, cleaning self or uses bedpan or commode.
TRANSFERRING (1 POINT) Moves in and out of bed or chair unassisted. Mechanical transfer aids are acceptable (0 POINTS) Needs help in moving from bed to chair or requires a complete transfer.
Points:
CONTINENCE (1 POINT) Exercises complete self control over urination and defecation. (0 POINTS) Is partially or totally incontinent of bowel or bladder
Points:
FEEDING
Points: (1 POINT) Gets food from plate into mouth without help. Preparation of food may be done by another person. (0 POINTS) Needs partial or total help with feeding or requires parenteral feeding.
TOTAL POINTS: SCORING: 6 = High (patient independent) 0 = Low (patient very dependent
Source: try this: Best Practices in Nursing
Care to Older Adults, The Hartford Institute for Geriatric Nursing, New York University, College ofNursing, www.hartfordign.org.
What is visual acuity and what does 20/20 vision mean?
Visual acuity (VA) is commonly referred to as the sharpness of vision, measured by the ability to discern letters or numbers at a given distance according to a fixed standard.
20/20 vision is considered "normal" vision, meaning you can read at 20 feet a letter that most people should be able to read at 20 feet.
If a patient reads the 20/200 line that means they can read at 20 feet the letters that people with "normal" vision can read at 200 feet. So at 20/200, your visual acuity is very poor.
Steps to checking vision using Snellen eye chart
1. Have patient stand at appropriate marking on floor. 2. If patient has glasses make sure they are wearing the proper glasses for distance vision. 3. Give patient occluder and have them cover the eye not being tested. 4. Have patient read the smallest line they can see on the chart 5. If patient reads all 5 letters correctly and there are more lines below then ask them to try the next line. 6. Repeat steps for opposite eye.
How to record vision
1. If the patient reads all the letters on the 20/30 line you would record their vision as 20/30. 2. If the patient is reading the 20/30 line and reads 3 out of the 5 letters correctly you would record that vision as 20/30-2. 3. If the patient is reading the 20/30 line and reads all the letters correctly and then reads 2 letters of the next line correct their vision would be 20/30+2. 4. You can use that notation with any line of vision no matter what the number of letters are.
Using a pinhole occluder
1. If the patient can’t see any better than 20/40 try using the pinhole technique. This technique helps to focus the light and removes the effects of refractive errors such as myopia. 2. Using the occluder put the pinhole flap over the opening and have the patient wiggle the occluder back and forth until they find a hold that makes it look clearer for them. 3. Then have the patient read the next clearest line of vision that they can see. 4. Record the vision as PH: 20/___.
Patients with poor vision less than 20/400
WHODAS 2.0
World Health Organization Disability Assessment Schedule 2.0 ( self-administered) This questionnaire asks about difficulties due to health/mental health conditions. Health conditions include diseases or
illnesses, other health problems that may be short or long lasting, injuries, mental or emotional problems, and
problems with alcohol or drugs. Think back over the past 30 days and answer these questions thinking about how much difficulty you had doing the following activities. For each question, please circle only one response.
Clinician Use Only
Numeric scores assigned to each of the items: In the last 30 days, how much difficulty did you have in:
Understanding and communicating
D1.1 Concentrating on doing something for ten minutes?
D1.2 Remembering to do important things?
D1.3 Analyzing and finding solutions to problems in day-to-day life? Learning a new task, for example, learning how
D1.4
to get to a new place? D1.5 Generally understanding what people say?
D1.6 Starting and maintaining a conversation?
Getting around
D2.1 Standing for long periods, such as 30 minutes?
D2.2 Standing up from sitting down?
D2.3 Moving around inside your home?
D2.4 Getting out of your home?
D2.5
Self-care
Walking a long distance, such as a kilometer (or equivalent)?
D3.1 Washing your whole body?
D3.2 Getting dressed?
D3.3 Eating?
D3.4 Staying by yourself for a few days?
Getting along with people
D4.1 Dealing with people you do not know? D4.2 Maintaining a friendship?
Getting along with people who are close to
D4.3
you? D4.4 Making new friends?
D4.5 Sexual activities? 1 2 3 4 5
Raw Item Score Raw Domain Score
Extreme or None Mild Moderate Severe
cannot do
None Mild Moderate Severe Extreme or cannot do
Extreme or None Mild Moderate Severe cannot do
Extreme or None Mild Moderate Severe cannot do
None Mild Moderate Severe Extreme or cannot do
None Mild Moderate Severe Extreme or cannot do 30
Average Domain Score
____ 5
None Mild Moderate Severe Extreme or cannot do
None Mild Moderate Severe Extreme or cannot do
None Mild Moderate Severe Extreme or cannot do
None Mild Moderate Severe Extreme or cannot do
None Mild Moderate Severe Extreme or cannot do ____ 25
None Mild Moderate Severe Extreme or cannot do
None Mild Moderate Severe Extreme or cannot do
None Mild Moderate Severe Extreme or cannot do
None Mild Moderate Severe Extreme or cannot do
None Mild Moderate Severe Extreme or cannot do
None Mild Moderate Severe Extreme or cannot do
Extreme or None Mild Moderate Severe cannot do
None Mild Moderate Severe Extreme or cannot do
None Mild Moderate Severe Extreme or cannot do ____ 20
25
Numeric scores assigned to each of the items: 1 2 3 4 5
In the last 30 days, how much difficulty did you have in:
Life activities—Household
D5.1 Taking care of your household responsibilities? None Mild Moderate Severe
Extreme or cannot do
D5.2 Doing most important household tasks well? None Mild Moderate Severe
Extreme or cannot do
Getting all of the household work done thatD5.3
you needed to do?
Extreme or None Mild Moderate Severe cannot do D5.4 Getting your household work done as quickly as None Mild Moderate Severe Extreme or needed? cannot do
Life activities—School/Work
If you work (paid, non-paid, self-employed) or go to school, complete questions D5.5–D5.8, below. Otherwise, skip to D6.1. Because of your health condition, in the past 30 days, how much difficulty did you have in: D5.5 Your day-to-day work/school? None Mild Moderate Severe
Extreme or cannot do
Doing your most important work/school D5.6 tasks well?
Extreme or None Mild Moderate Severe cannot do D5.7 Getting all of the work done that you need to None Mild Moderate Severe Extreme or cannot dodo? D5.8 Getting your work done as quickly as needed? None Mild Moderate Severe
Extreme or cannot do
Participation in society
In the past 30 days: How much of a problem did you have in joining in community activities (for example, festivities,D6.1 religious, or other activities) in the same way as anyone else can? How much of a problem did you have because D6.2 of barriers or hindrances around you?
Extreme or None Mild Moderate Severe cannot do
None Mild Moderate Severe Extreme or cannot do
D6.3 How much of a problem did you have living with dignity because of the attitudes and actions of others?
Extreme or None Mild Moderate Severe cannot do
D6.4 How much time did you spend on your health condition or its consequences?
Extreme or None Some Moderate A Lot cannot do
D6.5 How much have you been emotionally affected by your health condition?
Extreme or None Mild Moderate Severe cannot do D6.6 How much has your health been a drain on the financial resources of you or your family? None Mild Moderate Severe Extreme or cannot do D6.7 How much of a problem did your family have because of your health problems? None Mild Moderate Severe Extreme or cannot do D6.8 How much of a problem did you have in doing things by yourself for relaxation or pleasure? None Mild Moderate Severe Extreme or cannot do
Raw Item Score Raw Domain Score Average Domain Score
____ 20 ____ 5
____ 20 ____ 5
____ 40 ____ 5
General Disability Score (Total): ____ 180 ____ 5
© World Health Organization, 2012. All rights reserved. Measuring health and disability: manual for WHO Disability Assessment Schedule (WHODAS 2.0), World Health Organization, 2010, Geneva. The World Health Organization has granted the Publisher permission for the reproduction of this instrument. O.
World Health Organization Disability Assessment Schedule 2.0
36-item version, self-administered
The adult self-administered version of the World Health Organization Disability Assessment Schedule 2.0 (WHODAS 2.0) is a 36-item measure that assesses disability in adults age 18 years and older. It assesses disability across six domains, including understanding and communicating, getting around, self-care, getting along with people, life activities (i.e., household, work, and/or school activities), and participation in society. If the adult individual is of impaired capacity and unable to complete the form (e.g., a patient with dementia), a knowledgeable informant may complete the proxy-administered version of the measure, which is available at www.psychiatry.org/dsm5. Each item on the self-administered version of the WHODAS 2.0 asks the individual to rate how much difficulty he or she has had in specific areas of functioning during the past 30 days.
WHODAS 2.0 Scoring Instructions Provided by World Health Organization
WHODAS 2.0 Summary Scores: There are two basic options for computing the summary scores for the WHODAS 2.0 36-item full version.
Simple: The scores assigned to each of the items—“none” (1), “mild” (2), “moderate” (3), “severe” (4), and “extreme” (5)—are summed. This method is referred to as simple scoring because the scores from each of the items are simply added up without recoding or collapsing of response categories; thus, there is no weighting of individual items. This approach is practical to use as a hand-scoring approach, and may be the method of choice in busy clinical settings or in paper-and-pencil interview situations. As a result, the simple sum of the scores of the items across all domains constitutes a statistic that is sufficient to describe the degree of functional limitations. Complex: The more complex method of scoring is called “item-response-theory” (IRT)–based scoring. It takes into account multiple levels of difficulty for each WHODAS 2.0 item. It takes the coding for each item response as “none,” “mild,” “moderate,” “severe,” and “extreme” separately, and then uses a computer to determine the summary score by differentially weighting the items and the levels of severity. The computer program is available from the WHO Web site. The scoring has three steps:
• Step 1—Summing of recoded item scores within each domain. • Step 2—Summing of all six domain scores. • Step 3—Converting the summary score into a metric ranging from 0 to 100 (where 0 = no disability; 100 = full disability).
WHODAS 2.0 Domain Scores: WHODAS 2.0 produces domain-specific scores for six different functioning domains: cognition, mobility, self-care, getting along, life activities (household and work/school) and participation.
WHODAS 2.0 Population Norms: For the population norms for IRT-based scoring of the WHODAS 2.0 and for the population distribution of IRT-based scores for WHODAS 2.0, please see http://www.who.int/classifications/icf/Pop_norms_distrib_IRT_scores.pdf
Additional Scoring and Interpretation Guidance for DSM-5 Users
The clinician is asked to review the individual’s response on each item on the measure during the clinical interview and to indicate the self-reported score for each item in the section provided for “Clinician Use Only.” However, if the clinician determines that the score on an item should be different based on the clinical interview and other information available, he or she may indicate a corrected score in the raw item score box. Based on findings from the DSM-5 Field Trials in adult patient samples across six sites in the United States and one in Canada, DSM-5 recommends calculation and use of average scores for each domain and for general disability. The average scores are comparable to the WHODAS 5-point scale, which allows the clinician to think of the individual’s disability in terms of none (1), mild (2), moderate (3), severe (4), or extreme (5). The average domain and general disability
scores were found to be reliable, easy to use, and clinically useful to the clinicians in the DSM-5 Field Trials. The average domain score is calculated by dividing the raw domain score by the number of items in the domain (e.g.,
if all the items within the “understanding and communicating” domain are rated as being moderate then the average domain score would be 18/6 = 3, indicating moderate disability). The average general disability score is calculated by dividing the raw overall score by number of items in the measure (i.e., 36). The individual should be encouraged to complete all of the items on the WHODAS 2.0. If no response is given on 10 or more items of the measure (i.e., more than 25% of the 36 total items), calculation of the simple and average general disability scores may not be helpful. If 10 or more of the total items on the measure are missing but the items for some of the domains are 75%–100% complete, the simple or average domain scores may be used for those domains.
Frequency of Use
To track change in the individual’s level of disability over time, the measure may be completed at regular intervals as clinically indicated, depending on the stability of the individual’s symptoms and treatment status. Consistently high scores on a particular domain may indicate significant and problematic areas for the individual that might warrant further assessment and intervention.


