CONNECTING

Games as therapy
Hospital at Home
Help for finding hearing aids
Answers about eating disorders
A sweet experiment kids can try
An eye for cool beans
She survived a stroke at 36
Health UPSTATE
YOU TO HEALTH AND MEDICAL EXPERTISE
ISSUE 1 2024
From the experts at
Celebrating Upstate:
The first co-ed medical school in the nation
 BY MANTOSH DEWAN, MD President, SUNY Upstate Medical University
BY MANTOSH DEWAN, MD President, SUNY Upstate Medical University
This year, Upstate Medical University is celebrating 175 years of co-ed medical education. It is one of the many “firsts” at Upstate, and a significant one.
Upstate traces its roots to 1834, when the Geneva Medical College (precursor to today’s Norton College of Medicine) was established to provide doctors to care for the communities that were springing up along the Erie Canal. When Elizabeth Blackwell graduated at the top of her class in 1849, she was the first woman to graduate from a U.S. medical school, and a legacy began.
Elizabeth Blackwell also is a story of persistence. She was inspired to pursue medicine after a dying friend confided that her illness would have been more bearable if she had been treated by a female physician. Blackwell applied to 29 medical schools. Her acceptance to Geneva in 1847 was designed as a joke among the student body. She founded the New York Infirmary for women and, returning to her native England, was the first woman on the British Medical Register.
We are proud of our roots as the first co-ed medical school in the United States and that today, women make up half of the nation’s medical students.

Medical drones take flight
Upstate is using drones through the Medical Autonomous Machines Program, which also includes robots that are used in the hospitals, to ferry medications among its campuses.
The Upstate Outpatient Pharmacy receives medication orders, fills the prescription and secures it in a delivery bag that is placed inside the drone’s cargo hold. The drone flies about 30 miles per hour at 240 feet in the air, bypassing automobile traffic. When the drone arrives at a designated area outside the hospital, it lowers the delivery in a yellow bag that is retrieved by a technician.
It’s one example of the way drones can be used in health care, said hospital Chief Executive Officer Robert Corona, DO. “The hospital already delivers medications to a nearby residence for housing vulnerable individuals, and we look to expand this program, especially as technology advances.”
NEW SPACE OPENS FOR PATIENT CARE
More than a dozen medical services are offered within expansive clinical space at the new Nappi Wellness Institute, a five-story, almost 210,000-squarefoot building across from Upstate University Hospital in downtown Syracuse. It’s named for Sam and Carol Nappi, whose $8 million gift to the Upstate Foundation is the largest monetary gift in the foundation’s history.
Upstate’s drone operator, Causey Aviation Unmanned, is only the fifth operator in the United States to obtain a specialized Part 135 certificate from the Federal Aviation Administration, which allows it to provide deliveries for health care.
machines,

CANCER CARE COMES TO VERONA
The Upstate Cancer Center at Verona is a new, 30,000-square-foot facility that offers expanded diagnostic and treatment services for all cancers.
Located at the intersection of routes 365 and 31, the center
is on Oneida Indian Nation land, a first for the Oneidas and the State of New York. The site provides medical oncology, radiation therapy, surgical subspecialties, radiology, and lab and pharmacy services.

RESPECT FOR HEALTH CARE WORKERS
Leaders from Upstate and other hospitals and health systems across Central New York launched a new collaborative effort called Respect and Heal, aimed at ensuring the safe and respectful treatment of health care workers.
The campaign comes at a time when incidents of violent, disrespectful and disruptive behavior aimed at health care workers is on the rise, even though the vast majority of patients and families are grateful for the care they receive.
Upstate University Hospital’s
chief executive officer, Robert Corona, DO, says Respect and Heal is meant to ensure “that all staff will be treated with respect, that there will be zero tolerance of any threat and that any violence against frontline staff will be met with the full enforcement of the law.”
WHAT’S UP AT UPSTATE
Steve Roberts, Upstate’s director of autonomous
inspects one of the drones. Photo by Darryl Geddes.
2
photo by William Mueller
The presidents of the classes of the Upstate’s Norton College of Medicine gather by the portrait of Elizabeth Blackwell. From left Nathan Ihemeremadu, Gavrielle J. Rood, Katherine Narvaez Mena and Christopher Bushnell.
FIRST AND ONLY UPSTATE HEALTH l issue 1 2024 l upstate.edu
Elizabeth Blackwell applied to 29 medical schools before being accepted. This image is from around the time she applied at age 26.
DIGNIFIED STREET MEDICINE
A Syracuse-based outreach program for the homeless, called In My Father’s Kitchen, has a new Sprinter cargo van to help supply food, clothing and emergency supplies to people living in abandoned buildings, in hidden encampments and under bridges and overpasses.
The van was specially equipped with a medical exam table, lighting, medical supply storage and other amenities to aid in a collaborative partnership with Upstate’s HouseCalls for the Homeless program. This street medicine initiative provides medical, psychiatric and addiction care for men and women experiencing homelessness. “We’ll be able to deliver health care with a greater level of dignity,” said David Lehmann, MD, PharmD, who pioneered the program.
In My Father’s Kitchen, which began in 2011, receives some funding from the city of Syracuse but relies mostly on private donations, local churches and corporate donations.
new In My Father’s

UPSTATE HEALTH
EXECUTIVE
EDITOR-IN-CHIEF
WRITERS
DESIGNER


3 Health CONTENTS UPSTATE ISSUE 1 2024 Upstate Health magazine is a community outreach service of Upstate Medical University in Syracuse, N.Y. Upstate is an academic medical center with four colleges (Medicine, Nursing, Health Professions and Graduate Studies); a robust research enterprise and an extensive clinical health care system that includes Upstate University Hospital, Upstate Community Hospital, the Upstate Cancer Center and the Upstate Golisano Children’s Hospital. Part of the State University of New York, Upstate is Onondaga County’s largest employer.
EDITOR Leah Caldwell Assistant Vice President, Marketing & University Communications
Amber Smith
Jeanne
Albanese
Jim
Charles
Darryl Geddes
Howe
McChesney Amber Smith
Visit us online at www.upstate.edu For corrections, suggestions and submissions, contact Amber Smith at 315-802-9152 or smithamb@upstate.edu Upstate Health offices are located at 750 East Adams St., WH-3168, Syracuse, NY 13210 Need a referral? Contact Upstate Connect at 315-464-8668 or 800-464-8668, day or night, for appointments or referrals to the health care providers on these pages or anywhere at Upstate or for questions on any health topic.
Kathleen Carnes
at Home,
RSV game-changer, page 13 Coffee connoisseur, page 22 On the cover: Photo of stroke survivor Tiffany Henderson by Susan Kahn PATIENTS FIRST A stroke at 36 ......................... 4 An innovative endovascular aortic repair ........................... 6 Hospital care in the home .............. 7 His car was totaled; he survived ........ 8 Twins work together .................. 10 Offering sick kids an escape 11 FROM OUR EXPERTS RSV drug breakthrough ............... 12 Answers about eating disorders ....... 14 12 things to know about vasectomy ... 16 The basics of hearing aids ............. 17 Research roundup .................... 18 Science project: rock candy ............ 19 Science is Art is Science .........back cover IN OUR COMMUNITY This couple became NPs together 21 IN OUR LEISURE Eye doc’s daily grind: Cool beans ....... 22 Roasted acorn squash recipe .......... 23
Hospital
page 7
upstate.edu l issue 1 2024 l UPSTATE HEALTH
The
Kitchen van has space to provide medical care. Photo by Darryl Geddes.
‘Help is on the way’
A hospital worker stricken on the job receives coordinated stroke care
 BY AMBER SMITH
BY AMBER SMITH
Tiffany Henderson-Brown continually picked up extra shifts because of the shortage of workers during the pandemic. She busily checked patients into a medical office one Friday morning in February 2021.
Reaching to open a door, her hand missed the doorknob. Over and over, her hand wouldn’t grasp it. Then Henderson-Brown began to sense that something bad was about to happen. She felt the hospital where she worked was about to blow up. She told her boss.
Her boss escorted her to the nearby emergency department. There, Henderson-Brown watched her arm lift above her head, as if she was trying to wave at someone across the room. She laughed. She remembers the nurse speaking plainly: “You’re having a stroke, and help is on the way.”
Henderson-Brown was 36 and healthy, without the common signs of stroke. Her face did not droop. Her words did not slur. She just had the weirdness in her right arm and the feelings of dread.
A blood clot had lodged in a vessel on the left side of her brain — and it would be years before she felt back to herself.
Doctors at St. Joseph’s Hospital Health Center quickly gave HendersonBrown the clot-busting medication alteplase and transferred her by ambulance to Upstate.
Nurse Jennifer Dennis is the stroke program outreach coordinator at Upstate. She said Henderson-Brown’s story “shows how a primary stroke center such as St. Joe’s and a comprehensive stroke center such as ours, working together, can facilitate great outcomes for stroke patients in our community.” It also serves as a reminder that strokes can happen to anyone, at any age.
Vascular and interventional neurologist Hesham Masoud, MD, was at her side when Henderson-Brown began waking up. He had located and removed the clot. Now he was asking her what day it was and who was president. Henderson-Brown did not know. But she surprised the doctor with her ability to speak. Right away, she noticed her right hand was clenched in a fist she was unable to move.
She said she believes her stroke was caused by job stress. “There was a lot of help that was needed during COVID. I overdid it,” she said.
Four days after her stroke, Henderson-Brown was able to go home. “They told me I would never have the use of my hand again. And I’m righthanded. It was very difficult. I told them I’m not accepting this as my truth.”
She began six months of physical therapy, which ended when the therapists said her deficits would likely no longer improve. “They said, ‘It’s up to you to accept it or try to work around it.’”
4 PATIENTS FIRST
UPSTATE HEALTH l issue 1 2024 l upstate.edu

Henderson-Brown struggled. Her right arm was so weak she couldn’t use it to get out of a chair. She couldn’t feel anything, and her dexterity was missing. Cooking was nearly impossible. She cut herself plenty of times trying to slice vegetables.
Unable to return to work, she found herself sitting at home day after day, drinking.
Her sons, Zacari, 19, and Zuriel, 16, noticed she wasn’t herself. “Ma,” they told her, “we are not going to let this happen.” Her sons and husband, Condrea Brown, motivated her not to fall into an alcoholic depression. They helped her focus on the things she could do, despite the lack of function in her arm. They reminded her she was still important in their lives and the lives of others.
“It’s easier to give up. It’s a lot harder to keep going,” Henderson-Brown said she knows now.
Today she is a switchboard operator at St. Joseph’s. She is sharing her story in two books, one called “Activate Your Faith, Witness Generational Turnaround” about the life-changing experience of surviving a stroke and another called “Stand Up, Vol. 3” about perseverance.
“Now I practice sobriety. I’m very proud of myself,” she said. “The stroke I thought was going to ruin my life has actually saved my life.” u
Understanding intensive care
“Your loved one may seem impossibly ill. But the intensive care unit, or ICU, is designed to take care of the sickest of the sick, bringing all possible expertise and resources to bear — and the large majority of its patients survive and get better.”
Those encouraging words are at the heart of a book by Lara Goitein, MD, who specializes in pulmonology and critical care medicine at Dartmouth Health in New Hampshire. “The ICU Guide for Families — Understanding Intensive Care and How You Can Support Your Loved One” (Rowman & Littlefield Publishers) is 238 pages.
Goitein explains what “stable” means — that oxygen levels in the blood, heart rate and blood pressure are consistently in a safe range. Add she goes into detail about the most common procedures that are done in the ICU, including intubation, insertion of a central line and others.
She also suggests four things loved ones can do to help:
• Alert the patient’s primary care physician, so they know the patient is hospitalized.
• Get a blank notebook; review the events of the days leading up to the ICU admission and write them down to solidify your memory.
• Gather a list of the patient’s medications, their allergies, medical records, test results and advance directives. And let the medical team know if you are their health care proxy.
• Learn who is in charge of your loved one’s care. It could be “the attending physician” or “the ICU doctor,” or in a teaching hospital, this may be a resident or fellow — physicians in specialized training programs. Also get to know the ICU nurse assigned to your relative.
About 4 million people are cared for in an ICU each year. Remember, a large majority survive and get better. u
5
PATIENTS FIRST
upstate.edu l issue 1 2024 l UPSTATE HEALTH
Tiffany Henderson-Brown of Syracuse credits family members with helping her focus on what she is able to do after a stroke. Photo by Susan Kahn.

A novel surgery saved her life
BY DARRYL GEDDES
Avascular surgeon who is the first to perform an innovative thoracic and abdominal aortic repair recently joined the faculty at Upstate Medical University.
Wei Li, MD, joined Upstate from Texas Tech University Health Sciences Center, where he performed the innovative surgery on 58-yearold Susan Benton. At the end of last summer, she traveled from Texas to Syracuse for an appointment with Li.
The surgery, which involved a major arterial reconstruction, saved Benton’s life. Now, more than 2 1/2 years later, she’s back to her activities, including Tae kwon do.
In 2021, Benton was winded and in pain, unable to walk more than 200 feet before tiring, and her skin tone was pale. She saw a cardiologist. Multiple tests determined that Benton, a smoker, suffered extensive and complex blockages of her aorta, from her upper chest to her groin. The aorta is the largest artery in the human body. Undetected and without treatment, aortic blockages can lead to organ failure or death.
Benton had a rare form of aortoiliac occlusive disease, or AIOD, a variant of peripheral artery disease that affects the infrarenal aorta and iliac arteries. The
cardiologist referred Benton to Li.
“He is the absolute best; he is wonderful,” Benton said of Li during her recent visit to Upstate. “When I saw him, he said, ‘You’re in bad condition.’ Then he drew on a paper towel from the sink in my hospital room of how he was going to correct my condition.
“He then turned to me and said, ‘This has never been done, but I can do it,’” Benton recalled.
& Hudgins (Benton’s maiden name) Vascular Surgery Endowment and Fund to spur further advances.
At Upstate, Li does complex and innovative aortic surgeries, new minimally invasive procedures for dialysis access and other routine vascular procedures.
“THIS HAS NEVER BEEN DONE, BUT I CAN DO IT.”
During the nine-hour procedure, Li and his team performed a thoracic and abdominal aortic bypass using a unique transesophageal echocardiogram-guided approach.
Benton’s recovery was aided by occupational and physical therapists who came to her home. Three to four months after surgery, “I felt like I had never felt before,” she said. “I’m so lucky to have found Dr. Li.” Benton plans to continue traveling to Syracuse to see Li for followup care.
The success of the surgery and Benton’s full recovery, after about five months, proved to the physicians that the procedure can be an effective treatment alternative for future cases of AIOD. Benton and her family were so appreciative of Li that they established the Li
— Wei Li, MD
He is one of the physicians who offers fenestrated endovascular aortic repair, or FEVAR, a minimally invasive procedure in which physicians thread a guide wire through the femoral artery to the aneurysm site, so the entire fenestrated stent graft system could be inserted to repair the artery. This preserves blood flow to the kidneys and other organs. Li made headlines as the first physician in the West Texas and Eastern New Mexico region to do this procedure.
Li’s move to Syracuse is a homecoming of sorts, as he served as a general surgery resident at Upstate in 2005 after receiving his medical degree from Tianjin Medical University in China and a Master of Public Health degree from Yale University.
To request an appointment, call 315-464-8272 and then press 1. u
6
UPSTATE HEALTH l issue 1 2024 l upstate.edu PATIENTS FIRST
Susan Benton with vascular surgeon Wei Li, MD, at Upstate. He wrote about her surgery in the international Journal of Vascular Surgery –Cases, Innovations and Techniques. Photo by William Mueller.
Hospital care, but in your home
BY AMBER SMITH
Some Medicare patients at Upstate University Hospital are able to continue receiving hospital care in the comfort of their homes through the aptly named Hospital at Home program.
Patients who want to participate must have stable medical conditions that require hospital care. And they must have a safe home, with support from family or friends. “They meet criteria to be hospitalized but are stable enough to be cared for in the home setting,” describes nurse Diane Nanno. She is the director of nursing for Upstate’s Transitional Care Services, and she helped establish Upstate’s Hospital at Home program.
Suzanne Kline’s husband, Peter, was hospitalized after a fall in February 2023. He was found to have an infection that required intravenous antibiotics. When she heard that he could recover at home but still technically be a hospital patient, she was all for it.
“Nobody wants to be in the hospital,” Kline says. “If they can be in their own home, I would think that mentally it would speed the recovery.”
Since she was retired, she was able to care for him in their home in the hamlet of Lyncourt.
A nurse came every morning between 8 and 9 a.m. “She was punctual,” Kline says. “And between 8 and 9 p.m. the same nurse would
call to check to make sure how everything was going. And I had her cell number.”
Kline says her husband still has some health concerns, but he’s better.
With hospital capacity a critical concern during the pandemic, the federal Centers for Medicare and Medicaid Services encouraged hospitals to apply to begin Hospital at Home programs for certain patients on Medicare, the government health plan for seniors and people with disabilities.
Elsewhere in the country, hospitals already had experience with these programs and reported that 30-day readmission rates were reduced, along with a drop in emergency department utilization. And, patients in the programs were pleased.
The program is not designed to save the hospital money, but it does allow for more patients to receive hospital care, Nanno says. Marjorie “Marge” Kearney spent Christmas Day 2022 with her family in Geddes. Back at her independent-living apartment that evening, she fell, breaking her hip. At the hospital, doctors also discovered a problem with her heart.

A social worker told her family about Hospital at Home. Her daughter-in-law, Kathy Kearney, is a nurse who retired from Upstate before Hospital at Home was offered. “We brought her home. The nurse showed up. Dr. (Timothy) Creamer showed up. The medications showed up. The bed showed up. I couldn’t have asked for a better experience.”
Nurses visited twice a day. She could reach a medical provider via iPad at any time. Kearney, 96, was comfortable. Several days later, she transitioned into hospice care. She died on Jan. 8 2023.
Kathy Kearney says the move from hospital, to home, and then into hospice was seamless. “It was so smooth and coordinated. I was truly impressed.”
She knew Timothy Creamer, MD, when she worked at Upstate. Creamer worked in primary care, making house calls with some regularity, before he launched the hospitalist program in 2001 at what was then Community-General Hospital. Hospitalists are medical providers who focus care on hospitalized patients.
The Community campus is now part of Upstate, and Creamer now oversees the Hospital at Home program. He often visits patients in their homes or talks with them via iPad.
The home care agency Nascentia Health provides care for Upstate’s Hospital at Home patients, and Nunn’s Home Medical Equipment provides the medical equipment.
“This is an incredible, innovative option for those patients who require acute hospital care and are stable enough to be cared for at home,” Nanno says. u
7
upstate.edu l issue 1 2024 l UPSTATE HEALTH PATIENTS FIRST
Peter Kline, seated, with his wife, Suzanne Kline, at home in Lyncourt. Photo by Susan Kahn.
Crash changes perspective
Nurse offers thanks, and a plea, to those who helped him heal after car wreck
 BY JIM HOWE
BY JIM HOWE
After a head-on crash that totaled his car and landed him in the intensive care unit, David E. Cadet wants to share what stands out to him:
• He is grateful for the care he got at Upstate — from the emergency department, or ED, to surgery to the intensive care unit, or ICU, to rehabilitation — as well as to the EMTs, police, family, friends and co-workers who all played a part in his recovery.
• He is giving back to the community to show that gratitude.
• He wants people, especially health care workers, to make self-care a priority, since neglecting his own care likely played a role in his accident.
“Upstate saved my life, from the quick action from the ED, on to the surgical procedures, keeping my family and myself updated with the level of care, what’s next to come, the treatment level. I was very proud.”
Cadet was an ICU/critical care nurse at Upstate for five years.
He singled out the trauma team in the surgical ICU, where more people took care of him than
8 PATIENTS FIRST
UPSTATE HEALTH l issue 1 2024 l upstate.edu



he could keep track of, including former colleagues.
Two years after the accident, his list of people to thank is lengthy, including surgeons who operated on his eye and shattered ankle and family members whose support and medical expertise came in handy, including his younger brother who is also a nurse practitioner; his father, a retired respiratory therapist who was a doctor in Haiti; and his mother, who is a retired nurse.
Cadet was almost home on Syracuse’s East Side when he fell asleep at the wheel in December 2021. He had been doing double duty, returning from a night of travel duty in Rochester. He crashed into an oncoming truck and was rushed to Upstate University Hospital with injuries to his head and chest as well as an eye, an Achilles tendon, and an ankle. He spent about 10 days in the ICU, then another nine days in rehabilitation before leaving the hospital.
It would be another 10 months of rehabilitation before he could go back to work part time, and four more months until he

could go full time. He currently works as a travel nurse in psychiatry in Syracuse, which gives him more free time to provide CPR education and first aid training throughout the community, through #Pump4ABeat and Kontinuity Healthiness and Wellness LLC, both of which he founded.
“That’s my way of giving back, saying my thank-you,” he said.
A lesson his accident and stint as a patient taught him, he says, is the need for people to take better care of themselves, especially those who work in health care.
Do medical professionals neglect their own care?
“At the sacrifice of taking care of others, at times, we do,” he says. “That’s not to say we are doing this purposely, but we just need to remain cognizant of ourselves,” he says, and not neglect things like proper rest and exercise.
His falling asleep while driving showed him that he had overextended himself and did not prioritize his own health. The accident was the consequence, he says.
Cadet’s only visible reminder from that accident is a slight limp. He can’t run yet, but he is upbeat about working at that and at how far he has come.
“Upstate is a great hospital to work in. It’s a great facility. And I want to say that not only as an employee, but as a patient: The care is really next to none. I’m very pleased with the level of care I received.” u
9
Nurse David Cadet is shown recently at his Syracuse home, left; in the surgical intensive care unit at Upstate, top right, after his head-on crash while driving his 2017 Kia Sportage LX, far right; and with fellow nurse Christina Accorso when he returned to light duty after the accident. Accorso had previously worked with Cadet in the medical ICUs and the burn unit.
PATIENTS FIRST upstate.edu l issue 1 2024 l UPSTATE HEALTH
Photo at far left by Susan Kahn; other photos courtesy of David Cadet.
Double duty
Training in funeral service prepared twins for Upstate jobs
BY JIM HOWE
Doing odd jobs for a funeral home across the street from their boyhood home in Red Creek started the Jaeger brothers on the path to their eventual careers at Upstate.
The identical twins work for the autopsy service and the anatomical gift program. For more than two decades, each has covered for the other during a vacation or sick day.
Donald Jaeger is the technical director of the autopsy service, and Daniel Jaeger is the technical director of the anatomy laboratory and the anatomical gift program, which handles the donation of a person’s remains for study by anatomy students.
People frequently mistake one for the other, but there are subtle differences. “He’s a little thinner than I am. I’m the more nourished twin,” Daniel says with a smile.
Each brother had worked as a licensed funeral director before starting at Upstate, and their training impressed on them the importance of professionalism and compassion as they deal with grieving families.
For example, if someone needs to identify a relative who has died in the emergency room, or a family has to travel a long way to Syracuse after a loved one dies, there is a special room for this purpose, so the last goodbye doesn’t take place in a morgue or a busy ER.
That room is the refurbished former autopsy room at Upstate University Hospital; all autopsies are now done at Upstate Community Hospital.
“We both work closely with grieving families, so we have experience dealing with people who have lost a loved one,” Daniel said, noting that Upstate’s spiritual care service offers additional support.
“Part of my responsibilities are preparing the donor, talking to families, getting all the permits filed and helping to organize the annual
memorial service held each year. We teach students how to care for and respect the donor, not just learning the anatomy itself,” Daniel said. Dana Mihaila, MD, PhD, is the program director overseeing the anatomical gift program and the anatomy lab.
Donald, who received autopsy training at the Onondaga County Medical Examiner’s Office, oversees the autopsy service. These autopsies are generally requested by a family to determine the cause of death for a current or recent hospital patient and may add helpful information to a family’s medical history. Donald also teaches the technical parts of an autopsy, such as organ removal, to pathology classes supervised by Robert Stoppacher, MD, the medical director of the autopsy service.
The Jaegers grew up in Red Creek, a 45-minute drive northwest of Syracuse. “There was a funeral home across the street from us, and we started helping out with the yard work,” Daniel recalled. That led to helping with calling hours and funerals and the brothers pursuing a career in funeral service, thinking they might own a funeral home together someday.
Each brother had been working at a private funeral home when they applied for job openings at Upstate. Daniel was hired in 1998, and when Donald was hired in 2002, the running joke was that they could cover for each other, and no one would be able to tell which one was which, Dan recalled, laughing.
As it turned out, the brothers do cover for each other, which means they never have the same time off from work, and between them and Stoppacher, the system can keep going when one brother is absent.
“The dynamics of our positions require us to be on call 24 hours a day, seven days a week. They’re unique positions within the institution,“ Donald noted. “You can’t get just anybody to do what we do, deal with grieving families, facilitate donating to science, those kinds of things.”

Do the brothers have any regrets about not owning a private funeral home together?
“Regrets? No. We’re very passionate about what we do here, both of us,” Donald said. “We’ve dedicated our lives to helping grieving families we devoted a great deal of our time to running these programs and training the next generation of health care professionals. No, we don’t have any regrets at all.” u
10 PATIENTS FIRST
Daniel, left, and Donald Jaeger can cover for each other in their jobs with the anatomy laboratory/ anatomical gift program and the autopsy service. People often mistake one brother for the other.
UPSTATE HEALTH l issue 1 2024 l upstate.edu
Photo by Jim Howe.
Offering an escape
VIDEO GAME SPECIALIST IS PART OF KIDS’ CARE TEAM



As the gaming and technology specialist for Golisano, Taylor’s main job is to play video games with young patients as they await blood draws, an IV insertion, surgery or radiation.
His goal? Normalize the hospital environment, make the patients less afraid, cheer them up, combat their boredom and reduce their pain.
The outcomes of his work show in happy smiles and giant hugs.
“One patient said to me, ‘Every time you’re down here is the best time. I am so happy when you come in to play,’” Taylor said. “The job is fun but hearing that tells me how meaningful it is to patients and families, and how much it impacts them.”
Taylor started in his role in the fall of 2021, thanks to a grant from Child’s Play, a national nonprofit organization that delivers therapeutic
games and technology to pediatric hospitals to improve patients’ lives through the power of play.
Taylor has long been involved in the local board and video game scene. He also has associate’s degrees in computer science and mechanical technology, and a bachelor’s in business management. He was looking for a job with more personal interaction when he saw the Upstate position posted on Facebook and applied.
Now, in addition to gaming with patients, Taylor maintains all of the gaming systems and computers and the iPad that child life specialists use with patients in many different ways. He also uses a 3D printer to make items for the specialists to use when explaining procedures such as IV ports, radiation masks and tracheotomy tubes.
His favorite part of the job is playing games. Every room at Golisano has a PS4, and seven mobile gaming carts feature Xbox and Nintendo Switch games as well as games for mature players.
Taylor checks the list of patients to see who might appreciate a visit from him. He prioritizes patients who can’t eat due to an upcoming procedure, older teen patients and patients who are there alone.
“When kids are unable to eat, I prioritize them more,” he said. “I know if I am gaming, I am no longer hungry and sometimes even forget to eat lunch.”
He says one of the most rewarding parts of the job is making adaptive controllers for patients who have limited use of their hands or arms. Once, Taylor set up a patient with a virtual reality game that was controlled by head movement.
When he arrives at a patient’s room, he introduces himself and assesses the patient’s demeanor and condition.
Then he asks if the child wants to play a game with him. Which game to play depends on the situation. If the child is there a short time or is anxious or bored, Taylor will pick a high-action game like Mario Kart or Super Smash Brothers. For patients with longer stays, he suggests the longer-term building games like Farming Simulator, which is relaxed and slower paced, or Minecraft, where kids can spend days building.
“When you’re playing Mario Kart, it distracts you from why you’re here, and maybe it doesn’t feel like you’re in the hospital,” Taylor said. “You don’t feel the pain as much.” u
11
PATIENTS FIRST
Brad Taylor, a gaming and technology specialist, plays video games with Savannah “Savvy” Spittler, a patient at the Upstate Golisano Children’s Hospital. Provided photo.
upstate.edu l issue 1 2024 l UPSTATE HEALTH

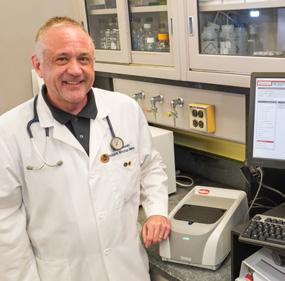
Medical breakthrough
Pediatrician and babies in Syracuse helped develop new RSV drug
BY AMBER SMITH
Babies finally have protection from the leading illness that puts them in the hospital, thanks in part to the tireless work of an Upstate doctor and his team — and three Central New York babies who were the first in the world to receive a shot of this new drug.
“I’m elated,” Joseph Domachowske, MD, said when the FDA announced its approval of nirsevimab this summer. The drug protects newborns from respiratory syncytial virus, or RSV. (Adults 60 and older have another medication to protect them from RSV.)
Domachowske spent more than three decades working on a way to fight RSV. He is a pediatrician at the Upstate Golisano Children’s Hospital specializing in pediatric infectious disease. RSV is the top cause of hospitalizations for babies under 6 months old, and the virus kills about 250,000 infants each year, mostly in developing countries without access to hospital care.
Nearly 5,000 newborns and young infants from all over the world were part of the studies.
The first three received their single shots in Syracuse in January 2015. One was from a family with a history of RSV complications; the other two were twins born prematurely and therefore at increased risk for complications.
Those twins, Cassidy Meany and Stella Meany, were 8 years old when nirsevimab was approved. Their mother, Cheryl Meany, told Syracuse.com, “We feel really blessed we were a part of it. I can’t explain how excited and how happy I am for moms across the world who don’t have to take their babies to the hospital because they can’t breathe.”
Domachowske says nirsevimab consistently was 80 percent effective in preventing RSV hospitalizations and requires just a single dose as the RSV season — from fall to spring — gets started. “At last we can finally reduce the impact of these annual RSV epidemics,” he says. “I’m especially eager to watch RSV fall from its long-held No. 1 cause of hospitalizations among children in their first year of life.”
He predicts that hospitalization numbers could initially be cut in half. As more babies are
protected in subsequent years, Domachowske expects fewer hospitalizations, fewer visits to the emergency department and a major decrease in the number of sick infants who are brought to pediatricians.
Nirsevimab, sold under the brand name Beyfortus, is not a vaccine but rather a monoclonal antibody product that provides a passive immunity.
Vaccines prompt the body to make antibodies to defend against diseases. In contrast, nirsevimab is a ready-made antibody that can bind to the virus and block it from infecting healthy cells.
Babies under 6 months old are at the highest risk for severe infection, so there’s not enough time to deliver a typical vaccine series to allow them to build immunity for the period of time they are most susceptible to severe illness. With this new treatment, the immune system doesn’t have to make anything. u

12
FROM OUR EXPERTS UPSTATE HEALTH l issue 1 2024 l upstate.edu
Cassidy Meany, left, and sister Stella Meany appear in a photo provided by their mother, Cheryl Meany.

Seniors can get RSV protection
The respiratory syncytial virus is also a threat to older people. The rates of hospitalization in people over age 65 from RSV are second only to those for influenza.
The Centers for Disease Control and Prevention recommends a single dose of RSV vaccine for adults 60 and older. The vaccine is also recommended for moms-to-be during weeks 32 to 36 of pregnancy, immediately before or during RSV season.
“With these combinations of prevention options, we’re hoping that we’ll have a less severe RSV season than last year,” said Upstate infectious disease chief Elizabeth Asiago-Reddy, MD. “Last year was a very severe RSV season that was somewhat unprecedented.”
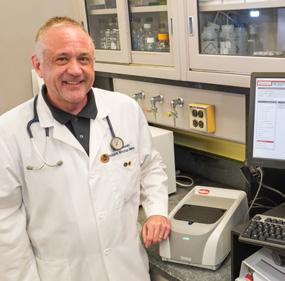
Upstate’s Joseph Domachowske, MD, and other researchers across the globe tried multiple approaches over three decades that did not work against respiratory syncytial virus.
Then, at a conference in Argentina, some of the leading RSV researchers heard a protein chemist describe one of the proteins that sits on the outside of the RSV virus.
“My jaw hit the floor,” Domachowske recalls. Researchers had been focused on the wrong protein.
RSV particles have daggerlike things sticking out of the surface of the virus. As soon as the daggers touch a cell, to try to infect it, the handle of the dagger flips, and the structural component of the protein changes.
Researchers had been working on an antibody that would work after the dagger flipped. But it turns out, they needed an antibody that would be effective prefusion, before the dagger touched the cell. “We’d been working on the confirmation of the wrong protein for decades.”
The second thing that was discovered right around the same time, he said, “was that if we take any antibody, these monoclonal antibodies in particular, and we change the part of the antibody that attaches to the cell — not the part that attaches to the virus, but the part that attaches to the cell — if we change it by just three amino acids, very small changes, it can enhance the half-life of these molecules from 19 days out to more than 120 days. So now we have the potential of making a very high neutralizing antibody against, really, whatever we want, that will last a fairly long time, out to five months, maybe longer. u

Joseph Domachowske, MD, was part of a worldwide team that developed a vaccine for RSV, a respiratory ailment that kills thousands of babies annually and can also threaten senior citizens.
 Upstate’s
Upstate’s
13 upstate.edu l issue 1 2024 l UPSTATE HEALTH FROM OUR EXPERTS
Photo by William Mueller.
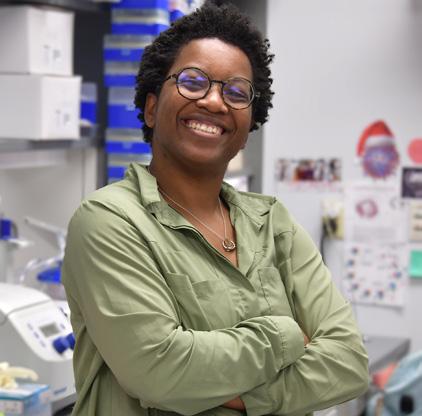
‘Crisis of eating disorders’
Family nurse practitioner explains symptoms, treatment of increasingly common youth problem
 BY AMBER SMITH
BY AMBER SMITH
Agrowing number of adolescents struggle with eating disorders, which are now the third most common chronic health condition in children and adolescents, behind asthma and obesity.
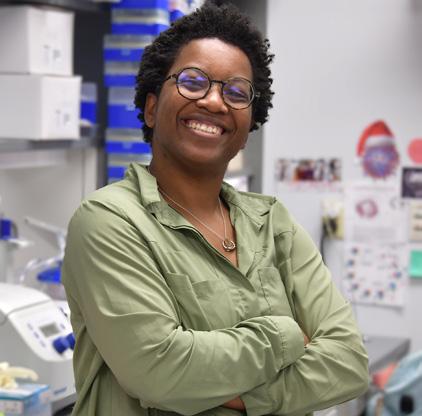
“We are seeing an enormous increase,” said family nurse practitioner Davia Moss, who specializes in adolescent medicine at Upstate.
“The pandemic, combined with social media, combined with our diet culture, has sort of been a perfect storm to create this crisis of eating disorders,” she explained.
Here’s more information, excerpted from a podcast interview with Moss, available at upstate.edu/informed.
HOW DOES THIS BEGIN?
“I hear this a lot from my patients. They will say they were just trying to get healthier, and then somewhere along the line things became out of control.
“I also have a number of patients who were told when they were young that they were so skinny. And the minute they hit adolescence — which is very normal — all of a sudden they stopped hearing that, and that was the trigger. That was all they needed to go down the path of an eating disorder.”
ARE FAD DIETS TO BLAME?
“There’s no reason for any adolescent to be on a ‘diet.’ Their brains are not capable of balance, so it often can get very quickly out of control.
“The other tricky part is, they often get a lot of positive feedback
when their body starts to change. And for an adolescent, they really thrive off that. That’s when things can get very out of control quickly.”
WHAT ARE THE SYMPTOMS?
Significant changes in a child can be a red flag. Is their attention concentration changing? Have they fainted? How is their fatigue level? Are they suddenly wanting to exercise more? Are they isolating themselves more? Eating disorders thrive on isolation.
What medical problems may arise?
• Electrolyte imbalances
• Constipation
• Heartburn or reflux
• Menstrual irregularities
• Cold intolerance
• Brittle hair/nails
• Tooth erosion or cavities
• Anxiety
• Decreased bone density
• Fertility difficulties
WHY DO SOME PEOPLE END UP HOSPITALIZED?
“The patients who are hospitalized are often the ones that are restricting to a very, very significant under-500-calories-a-day and over-exercising. They can have long-term cardiac and gastrointestinal sequelae (consequences). We have patients who abuse laxatives, which can actually impact the ability of your GI (gastrointestinal, or digestive) tract to even function correctly for the rest of your life.”
14 UPSTATE HEALTH l issue 1 2024 l upstate.edu FROM OUR EXPERTS
Symptoms explain condition type
These are four of the most common types of eating disorders:
Someone with anorexia nervosa has restrictive patterns of eating and significant body image concerns.
Those with bulimia nervosa have a pattern of binge eating and intentional vomiting.
A person with a binge eating disorder feels out of control with regard to food.
Someone who restricts his or her eating of certain foods because they create sensory difficulties, but who has no body image concerns, may have avoidant/ restrictive food intake disorder, or ARFID.
The American Psychiatric Association says eating disorders are characterized by severe and persistent disturbances in eating behaviors and associated distressing thoughts and emotions. They can seriously affect physical, psychological and social function.

15
upstate.edu l issue 1 2024 l UPSTATE HEALTH FROM OUR EXPERTS

Vasectomy essentials
KEY THINGS TO KNOW ABOUT MALE STERILIZATION
• A vasectomy is a permanent form of birth control. It is not a quick solution for young men in their 20s who want to have sex without the fear of an unwanted pregnancy, said Upstate urologist Timothy Byler, MD.
A reversal in the future might be possible, but that operation is expensive, may not be covered by health insurers, and may not work.
• The procedure has no physical effect on sexual drive or performance.
• A vasectomy does not protect against sexually transmitted diseases.
• A man can choose a vasectomy on his own, but for most men it’s a joint decision with their partner.
• The first appointment with a urologist typically includes a physical exam and discussion about anesthesia preferences.
A “local” anesthesia will numb the area where the doctor works, and the patient will remain conscious during the procedure. More sedating options mean the patient will be unconscious — and will require a driver after the procedure.
• Most vasectomies are done in the urologist’s office and take about an hour. Byler schedules procedures on Fridays, so patients have the weekend to rest and decide if they’re ready to return to work.
• The surgeon makes one or two tiny incisions in the scrotum to access and divide each of the vas deferens, tubes about the size of spaghetti strands that transport the sperm from the testicle.
The ends of each vas deferens are cauterized and closed with tiny, permanent clips. The incisions are closed with sutures that are absorbed, and scars are usually not visible a couple of months after the procedure.
Some men are able to feel tiny bumps in the scrotum, which are the clips that remain.
• Recovery includes about a week on “light duty,” starting with two days lying flat on a bed or sofa with acetaminophen and/or ice packs as needed. Some men experience temporary bruising or minor pain.
It’s important not to ejaculate for the first week to allow the tissues to heal properly, Byler said.
• A lingering testicular pain may persist for 1% to 2% percent of men, and it is notoriously difficult to treat.
• The failure rate — called spontaneous recanalization — is about 1 in 2,000 men. This risk is minimized by following doctor’s orders during recovery.
• A vasectomy does not take effect immediately. Doctors advise using another form of birth control until subsequent semen analysis shows no sperm in the ejaculate.
• When’s the best time of year for a vasectomy? Byler said some men plan for March Madness, so they have plenty of good basketball to watch during recovery. u
To schedule a consultation with an Upstate urologist, call 315-464-1500.
16 UPSTATE HEALTH l issue 1 2024 l upstate.edu FROM OUR EXPERTS
8 considerations for over-the-counter hearing aids
1 Adults can now buy them over the counter without a prescription or hearing exam, although a hearing exam with an audiologist is usually paid for by health insurance.
2 Neither Medicare, the government health plan for seniors, nor most private health insurers pay for hearing aids, which can cost a few hundred to several thousand dollars, depending on features.
3 Over-the-counter hearing aids are for people with “mild to moderate” hearing loss. Symptoms include speech or other sounds seeming muffled; trouble hearing when you are in a group, in a noisy area, on the phone or when you can’t see who is talking; asking others to speak more slowly or clearly, to talk louder or to repeat what they said; turning the volume higher than other people prefer when watching TV or listening to the radio or music.
4 If you have trouble hearing conversations in quiet settings, or trouble hearing loud sounds like cars or trucks, noisy appliances or loud music, your hearing loss may be more severe — and warrants a consultation with a hearing health professional, such as an audiologist.
5 Hearing aids purchased through audiologists in New York state have a 45-day trial period during which you can return the hearing aids for a refund. Ask about the return policy if you’re buying over the counter.
6 If you choose the right design and they fit properly, hearing aids can be so comfortable that you forget you’re wearing them. (But remember: They are electronic devices and should not be used in a pool or shower.)
7 Understanding the optional features — directional microphones, remote control, wireless connectivity and more — may require a bit of research.
8 The first incarnations of hearing aids in the early 1900s were boxes that people would put in their pockets with wires running up to their ears. Hearing aids grew in popularity after World War II, when many veterans came home with a hearing loss. Since then, the devices have continued to shrink. u
Sources: Upstate audiologist Erin Bagley, the American Academy of Audiology, the American Speech-Language-Hearing Association, and the National Institute on Deafness and Other Communication Disorders.

17 upstate.edu l issue 1 2024 l UPSTATE HEALTH FROM OUR EXPERTS
RESEARCH ROUNDUP
IS HERPESVIRUS CONNECTED TO ALZHEIMER’S DISEASE?
In the ongoing search to understand why someone develops Alzheimer’s disease, scientists have explored many potential causes, including particular genes and a history of head injuries.
There is also thought to be a connection to a herpesvirus.
Nine different herpesviruses spread easily, primarily through saliva or other body fluids. Once infected, a person has that particular herpesvirus forever.
“For the most part, if you have a healthy, competent immune system, the viruses are fairly benign. They don’t cause a lot of issues. It’s only after times of stress or immune suppression that the viruses come back and cause problems,” explained Eain Murphy, PhD, an associate professor of microbiology and immunology at Upstate.
“On a regular basis, anybody walking around is harboring — I believe the current estimates are — 3.2 different herpesviruses,”
Murphy has focused on two types that replicate in nerve cells since 2018, when a flurry of research was published, including one study showing herpesvirus in the areas of the brain where Alzheimer’s was active, but not in the areas where Alzheimer’s was not active.
Three conditions are present in Alzheimer’s. One is inflammation, which Murphy points out can be caused by viral infections. The second is beta-amyloid protein that accumulates outside of the nerve cells, which other researchers have shown increases with herpesvirus infections.
The third condition is the accumulation of tau protein inside the nerve cells.
“That’s where I started research projects saying, ‘Will infection of these neurons cause accumulation of tau inside the cells?’ And, in fact, that is the case,” Murphy said.
“I don’t know if herpes simplex virus infection, alone, is sufficient for promoting the whole disease. I would strongly lay the claim that I think it’s definitely involved,” he said, “but there could easily also be environmental factors or genetic factors we haven’t identified yet.”
STUDY FINDS DAILY CANNABIS USE REDUCES PAIN TOLERANCE
People who use cannabis daily for chronic pain are at risk of addiction, but they may also be lowering their tolerance for pain, according to research published in the American Journal of Addictions by Yanli Zhang-James, MD, PhD, and Brian Johnson, MD, from Upstate’s department of psychiatry and behavioral sciences.
“Reduced tolerance to pain is not new for other drugs like opioids, alcohol and nicotine. But it’s the first time that we reported that this also happens to people who chronically use cannabis,” said Zhang-James, a research associate professor. “This is really important because it’s becoming increasingly widely accepted and considered a relatively safe drug to use for pain, but people should still be aware that it comes with certain risks.”
Assisted by medical student Dennis Grapsas and volunteer Evelyn Wyon, the researchers examined patient medical records from the past 10 years. They compared patients with chronic pain who used cannabis every day with patients who inhaled tobacco and patients who never used cannabis or tobacco.
For an objective measure of pain tolerance, they used the cold pressor time test. “It’s a beer cooler full of ice water, and there’s an aquarium circulating pump,” explained Johnson, a clinical professor emeritus who previously served as director of addiction medicine. “The patient puts their forearm in, and it really hurts. We just time how long the patient is able to keep their arm under the ice.”
Johnson and Zhang-James would like to learn in future research how quickly an increased sensitivity to pain develops, and also whether the sensitivity becomes permanent. “All we can tell you right now is anything that helps with pain short term is going to worsen it long term,” he said.
ALTERNATIVE TREATMENT SHOWS PROMISE AGAINST RISKY INFECTION
Clostridioides difficile, or C. diff, is a potentially life-threatening diarrheal illness. Doctors typically prescribe antibiotics, which are effective but which also increase the person’s risk of a repeated C. diff infection.
“If a person has a C. diff infection for the first time in their life, there’s about a 25% chance that they will have another one. But if they get treated for that other one with antibiotics, the chances of having another one is about 40%. And if you have C. diff two times, the chances of getting a third is about 60%, which is really high,” says Aamer Imdad, MBBS, an Upstate graduate who was a faculty member specializing in nutrition and pediatric gastroenterology. Today he’s an assistant professor of pediatrics at University of Iowa and remains a visiting faculty member at Upstate. “The antibiotics not only help treat, but behind the scenes it may actually exacerbate the problem in the long term.”
The name of the problem is dysbiosis, an imbalance between the good bacteria and the bad bacteria that exist in a person’s gut. Imdad has found a possible solution: stool transplants.
“Fecal microbiota (micro-organisms) transplantation reverses that dysbiosis because we essentially take stool from a healthy person who does not have dysbiosis, and we transplant that to a patient who seems to have dysbiosis and is getting these recurrent C. diff infections because of that,” he explains.
In a study that will inform guidelines from the American Gastroenterology Association, Imdad’s team found that stool transplants helped resolve current C. diff infections more often than antibiotics.
About 75% of patients got better after a single transplant. If they had another recurrence and had a second transplant, the efficacy grew to up to 92%. As Imdad points out, “there are very few interventions in medicine that are as effective as fecal microbiota transplantation for treatment of recurrent C. diff.”
18 UPSTATE HEALTH l issue 1 2024 l upstate.edu FROM OUR EXPERTS

Sweet science
An easy rock candy project for kids
Deanna Clemmer was attracted to science as a child. She loved attending science fairs. “I was always a really big fan of bottle rockets, or the volcanic things with baking soda. As I got older, I just really held onto that childish love for all those things.”
Today, she is a doctoral student in the Upstate laboratory of virologist/ immunologist Harry E. Taylor, PhD.
She shares her love of science with her nephews, with at-home experiments such as making rock candy. This experiment shows how a supersaturated sugar solution creates crystals.
Here’s how:
INGREDIENTS YOU’LL NEED:
2-3 cups of sugar (1 for each stick) plus a few extra tablespoons
2-3 cups of water
2-3 wooden kebab skewers, each about 6 inches in length
2-3 see-through canning jars, about 12- to 16-ounce size
Clothespins
Food coloring, various colors
Candy flavoring or extracts, optional
HOW TO CONDUCT THE EXPERIMENT:
Combine equal parts sugar and water to heat in a saucepan on the stove. This cannot be done in a microwave. Warm the pan until the sugar is dissolved. If you add the sugar to the water slowly, you’ll see it turn cloudy as it dissolves.
If you’re adding a candy flavor, now is the time to stir it in. Then, remove the saturated sugar solution from the heat and allow it to cool a little.
Next, submerge the skewers in plain water. Spread some sugar on a plate, and roll the wet skewers in the sugar. Then set them aside to dry.
Once the skewers are dry, carefully place them in separate jars. Clip each skewer to a clothespin, and lay each clothespin perpendicular across the mouth of a jar. Don’t let the skewers touch the jar’s edges or bottom. Let them hang to about an inch from the bottom of the jar.
“Make sure that the sticks are completely dry before you put them in the jar. That is really important,” Clemmer said. “If it’s wet, it’s not going to grow as well. It might not grow at all. Because the rock candy needs the sugar on the sticks to grow, if it’s not dry, it’s going to dissolve in the water.”
When the sugar solution from the stove has cooled, remove the clothespinned skewers from the jars momentarily. Divide the sugar solution among your jars, filling them to an inch or two below the lip of the jar. Stir your food coloring into each jar.
Choose a spot for your jars where you can watch them for the next week, and place them there before returning the clothespinned skewers to the jars.
You may see crystals form within the first 24 hours, but Clemmer encourages patience. “Some kids get a little antsy, and by day three, they’re like, ‘Oh, there’s enough candy on this; I’m just going to eat it.’ But
I’ve found that once you leave it for a week, you get that whole skewer that’s in the jar. It’s full of candy crystals. It grows in every direction.”
She and her nephews photograph the rock candy progress each day. “They love to see their experiment working throughout time. And I think that’s very important for kids to be seeing that when you’re patient and you wait for things, amazing things can happen.”
Clemmer said she likes this experiment because it illustrates states of matter in a simple way that’s easy to follow. And, dissolving things in water is something she’s used throughout her scientific career.
“What’s cool about it is, we know that it is sugar water. That’s what we dissolved in the saucepan, right? Now that you’ve put the dry sugar in the sugar water, all of the sugar from the sugar water is going to connect to the skewer. It’s basically simple levels of attraction in just normal stuff that we use to cook and eat.
“Essentially, the dried-up sugar will basically draw all of the other sugar particles that are inside the water, that you dissolved, to the skewer. And that’s why it’s so important that the sugar on the skewer is dry. Because if it’s wet, then it’s just going to dissolve. But if it has something to draw it to, almost like a magnet, a sugar magnet, it’s going to draw all of that sugar to the skewer.” u
Deanna Clemmer works in the Upstate lab of Harry E. Taylor, PhD, a virologist and immunologist. Photo by Deborah Rexine.
19 upstate.edu l issue 1 2024 l UPSTATE HEALTH FROM OUR EXPERTS
Young patient inspired her family’s support for others
Brayleigh Mae Scott was a happy patient at Upstate Golisano Children’s Hospital. Her mother recalls her outgoing nature even when her daughter’s health conditions were challenging. With multiple diagnoses, including cerebral palsy, microcephaly and hip dysplasia, Brayleigh had frequent hospital stays.
“The care was above and beyond, and every single person was incredible to our family. They made sure we had everything we needed to feel most at home,” Jessica said. “They did so much for us during Brayleigh’s time in the hospital. One time, a meal from a local restaurant was brought to our room, giving us one less thing to worry about.”
“Being at the hospital is stressful, and nobody wants to be there, especially your child,” she continued. “These small measures add up, making it a little more comfortable for kids and families that have to be there.”
Known for her curly, strawberry-blonde hair, Brayleigh enjoyed crafts, dressing up and being with her grandmother. “Brayleigh Mae was full of sass and life,” recalls Jessica. “She loved art and being outdoors … except in winter.”
To honor Brayleigh’s memory, the family hosted a fundraiser, and they intend to contribute annually to the pediatric intensive care unit and other areas of the hospital.
Jessica also consulted with Upstate’s child life specialists and learned the specific types of donations that would be welcome to share with young patients. She created a hospital-friendly wish list of items Brayleigh enjoyed and promoted it on her social media. On what would have been Brayleigh’s third birthday she brought sticker books, crayons, markers and other art supplies to Upstate Golisano Children’s Hospital.
“Every little bit counts,” she added. “Every smile you put on a child’s face who is in the hospital is 100% worth it.”





F OUNDATION
ARE YOU GRATEFUL? A gift of gratitude is a meaningful way to express appreciation to caregivers and help patients during their time of great need. To donate, contact the Upstate Foundation at 315-464-4416. Impacting patient care, education, research and community health and well-being through charitable giving. Explore health, science and medicine with experts from Central New York’s only The Informed Patient PODCAST Explore health, science and medicine with experts from Central New York’s only academic medical center. Available on a variety of platforms including Spotify, Apple Podcasts and YouTube. Search and listen to topics at upstate.edu/informed The Informed Patient PODCAST UPSTATE HEALTH l issue 1 2024 l upstate.edu 20
Robert, Jessica and Brayleigh Scott of Central Square. Brayleigh’s brother Cooper joined the family soon after this photo was taken.
They made it work
COUPLE BECAME NURSE PRACTITIONERS TOGETHER
BY JEANNE ALBANESE
Adesk calendar in the den of Paige and Mackenzie “Mack” Stanley’s home holds the key to their success as students at Upstate Medical University. For the last three years, they planned out their lives in semester-long chunks.
With that desk pad and a set of colored highlighters, they meticulously recorded their work shifts as nurses at a nearby hospital (yellow); their nursing clinical rotations (purple); in-person classes at Upstate (blue); virtual classes (green); and on top of that, their 4-year-old daughter Finley’s schedule (pink) and anything else (orange).
The two high school sweethearts received their family nurse practitioner degrees from Upstate’s College of Nursing after 10 years of school, sacrifice and scheduling.
Paige knew she wanted to go into nursing since high school at Red Creek Central School. She earned her associate’s degree in nursing two years after graduating high school and immediately began work on her bachelor’s.
“I love helping people,” Paige said. “I love taking care of people. I have a very empathic nature, and I wanted to be able to give back to others.”
Mack wasn’t sure what he wanted to do after high school, and during that time started helping care for his grandfather, Gerald, who was sick. He would visit him and help feed and care for him and noticed the great care he received. That helped Mack decide to join Paige to pursue a career in nursing. Mack earned his licensed practical nursing diploma and then started to work on his bachelor’s.
“I couldn’t imagine doing anything else,” Mack said.
In the middle of all this, the couple got married and had a baby.
They both continued with school, their clinical hours and work. Some days, Paige would meet Mack in the parking lot of Newark-Wayne Community Hospital after he worked the day shift. She would hand off Finley and then go work the night shift.
Paige earned her bachelor’s in 2018; Mack earned his in 2020. Then, together, they
enrolled at Upstate to become family nurse practitioners.
Until they graduated in May 2023, their only real alone time was during their hourlong commute to campus from Wolcott, or when they sat in class together. Paige explained how they made it work: “We lean on each other. We take turns. One night I’ll do bedtime, and he will study, and the next night, we switch.”
After graduation, Paige took a job at Finger Lakes Community Health Center in Sodus. Mack continued to work at Newark-Wayne Community Hospital as a hospitalist.
“I am really glad we chose to go to Upstate,” Mack said. “The professors are really invested in the success of the program and of the students, and that helped us so much. A big part of our success was the true investment the institution had in all the students.” u
Educational options
Upstate’s College of Nursing is the only program in the region that is part of an academic medical center.
Registered nurses can earn a bachelor’s degree in 16 months in a fully online program.
Students with a bachelor’s degree can earn a Doctor of Nursing Practice degree and become a Family, Pediatric, Psychiatric or Adult Geriatric Nurse Practitioner in a program that takes 3 years full-time in a combination of face-to-face and online courses.
Students with a clinical master’s degree from an accredited nursing program can earn advanced certificates (in family, pediatric, geriatric or psychiatric mental health) through a combination of online and face-to-face courses.
Nurse practitioners can earn a doctor of nursing practice degree online, taking courses part time.
Learn details at upstate.edu/con

21
Mackenzie “Mack” Stanley, left, and his wife, Paige Stanley, graduated together from Upstate as nurse practitioners in May 2023. Photo by William Mueller.
IN OUR COMMUNITY upstate.edu l issue 1 2024 l UPSTATE HEALTH

An eye doctor’s daily grind
BY AMBER SMITH
When Robert Fechtner, MD, was in high school, his parents took a trip to Italy, where, as he explained, “they were first exposed to fine Italian espresso.”
Upon return, his father invested in an espresso machine and grinder, and the family began making espressos and cappuccinos at home.
A few years later, his parents began remodeling their kitchen. Fechtner was attending the University of Michigan in Ann Arbor. If they were getting rid of the espresso machine, he asked, could he have it?
Instead, his father found a machine small enough for a dorm room—and a coffee connoisseur was born.
Today, unless he’s operating, he starts each day with some form of coffee, often made at his Fayetteville home. Fechtner is professor and chair of ophthalmology and visual sciences at Upstate.
“I’m an early riser. I’ve been a surgeon my whole life. The first thing I do when I get up is turn on my espresso machine. It takes about 10 minutes to warm up.”
He believes in freshly ground coffee, so he

grinds beans that he buys from a variety of roasters, including Recess Coffee, Freedom of Espresso and Salt City Coffee in the Syracuse area, as well as roasters that ship, including Peet’s Coffee and Blue Bottle Coffee.
Lately, he favors a “flat white.” That is an espresso with a higher proportion of espresso to milk than in a caffe latte, and a thin layer of microfoam — thinner than the usual foamed milk of a cappuccino, and with tinier bubbles.
He used to prefer his coffee black, the blacker the better. “But in the last 10 years I’ve started appreciating the wide range of flavors available,” Fechtner said. “There are all sorts of techniques. It depends on your mood.”
When he travels, he often packs ground coffee and a small AeroPress, a manual device
for making coffee, “for the truly coffee addicted,” he said. He likes to try local coffee shops, but if there aren’t any, he likes to be prepared.
On surgery days, he seeks coffee after he completes his operations. He’s got a soft spot for hospital coffee and notes Upstate University Hospital’s 99-cent special on Thursdays. He typically blends the light roast with the medium roast.
Fechtner limits himself to two a day, and usually not after 4 p.m., so as not to disturb his sleep. But he indulges when he sees affogato on a restaurant menu. This, he explained, is the best way to enjoy espresso — poured like hot fudge over ice cream.
Some espressos are citrusy and bright. Others are more chocolaty and dark, which he drinks more of in the colder months.
“It’s snobby to think that there’s only one way to have coffee,” he said. “Coffee is a flavor. It can be a ritual. It can be a tradition. And it can be enhanced by so many things.” u

22
IN OUR LEISURE UPSTATE HEALTH l issue 1 2024 l upstate.edu
Robert Fechtner, MD, at his home in Fayetteville. Photo by Susan Kahn.
Roasted Acorn Squash
Food that’s good tasting and good for you is a win-win. Try this roasted acorn squash, a recipe that serves four, provided by Daniel Ellithorpe, the senior director of food services at Upstate, and Eric Adams, the system director of food service and hospitality at Upstate.
INGREDIENTS
About 3 pounds acorn squash (2 squashes)
4 teaspoons canola oil, divided 1/4 teaspoon ground black pepper, divided
1/4 teaspoon salt, divided
2 teaspoons pure maple syrup
1/3 cup long-grain wild rice
1/3 cup diced onion
2/3 cup celery, diced small
1 teaspoon minced garlic cloves
1 teaspoon minced garlic cloves
2 teaspoons fresh thyme, minced 1/3 cup dried cranberries
2 teaspoons extra-virgin olive oil
3/4 teaspoon balsamic vinegar
PREPARATION
Use 2 small-to-medium acorn squashes, about 1½ pounds each. Wash and cut them in half. Scoop out and discard the seeds and place the squashes on a sheet pan with the cut side up. Brush the cut sides of the squashes with about 2 teaspoons of the canola oil and the 2 teaspoons of the maple syrup, then sprinkle with about 1/8 teaspoon each of the salt and pepper. Roast in a preheated 350-degree oven until tender, about 20 to 30 minutes.
Place wild rice in a pot of cold water and bring to a boil. Then simmer and cook until 1/3 of the rice opens, about 30 minutes. Drain and set aside.
Heat the 2 remaining teaspoons of the canola oil in a pan and sauté the onion, celery and garlic until tender. Remove from pan and place in a large bowl. Add the remaining ingredients — the thyme, dried cranberries, olive oil, balsamic vinegar, the cooked wild rice and the remaining 1/8 teaspoon each of salt and pepper (or, to taste). Mix to incorporate. Stuff into the cooked acorn squashes. Each will hold about ½ cup of stuffing.
Return stuffed squashes to oven to heat through just prior to serving. Makes 4 servings.
NUTRITIONAL INFORMATION
Each of the 4 servings contains:
Calories: 330
Total fat: 5 grams
Saturated fat: zero grams
Total carbohydrates: 73 grams
Protein: 6 grams
Dietary fiber: 17 grams
Sodium: 190 milligrams

23 A RECIPE
IN OUR LEISURE upstate.edu l issue 1 2024 l UPSTATE HEALTH
SCIENCE IS ART IS SCIENCE IS ART IS SCIENCE




Exploring protein
Actin is a crucial protein involved in various cellular functions that many cell biologists study. They predominantly use actin synthesized from animal muscle cells, but non-muscle actin is called for in some research.
So assistant professor Brian Haarer, PhD, associate professor Jessica Henty-Ridilla, PhD, and professor Dave Amberg, PhD, vice president for research at Upstate, created a tool to purify different forms of actin from humble, budding yeast. Now they can create as much as they need.
Actin from yeast allows for the study of the protein’s role in various cells and diseases.
“How your cells move, grow or reproduce comes down to different forms and styles of actin function,” explains
Henty-Ridilla.“Exactly how actin functions has important implications for a disease like cancer because if you move too fast or to the wrong place, that’s not a good thing most of the time. But at the same time, it’s important for the development of your organs to be in the right place and orientation. Actin is very precisely controlled.”
Pictured are images of actin beneath a microscope, using temporal color coding of the filaments (to show a time sequence). The Journal of Cell Science displayed the colorful strings shown here on its May 2023 cover. Inside, a paper about the process was published by Amberg, Haarer and HentyRidilla and their colleagues, Ebbing De Jong, PhD, and Morgan Pimm, PhD. u
22.277 0323 29.9M KC EL 750 East Adams Street | Syracuse, NY 13210 NON PROFIT ORG. US POSTAGE PAID PERMIT NO. 110 SYRACUSE, NY 23.279 0124 50M ELKC
Jessica Henty-Ridilla, PhD
David Amberg, PhD
Brian Haarer, PhD

 BY MANTOSH DEWAN, MD President, SUNY Upstate Medical University
BY MANTOSH DEWAN, MD President, SUNY Upstate Medical University







 BY AMBER SMITH
BY AMBER SMITH



 BY JIM HOWE
BY JIM HOWE












 Upstate’s
Upstate’s
 BY AMBER SMITH
BY AMBER SMITH