Specialized physical therapy for men and women.
 PG.
PG.













Specialized physical therapy for men and women.
 PG.
PG.












College of Distinction 2022-23

Experience the new vision of nursing education through our innovative partnership with Boone Hospital Center. Earn your Bachelor of Science in Nursing in just three years with early access to clinical experiences. We offer innovative, research-centric degrees in Integrative Human Biology, Health Science, Human Development and Psychology.

We believe that every American veteran deserves our gratitude, respect and support. But we know that women veterans, in particular, often face unique challenges. That’s why we’ve created Mission Promise Kept: to empower women veterans to earn a college degree through a coordinated network of academic, medical, legal, and social services.


Explore all that Stephens has to offer at stephens.edu.

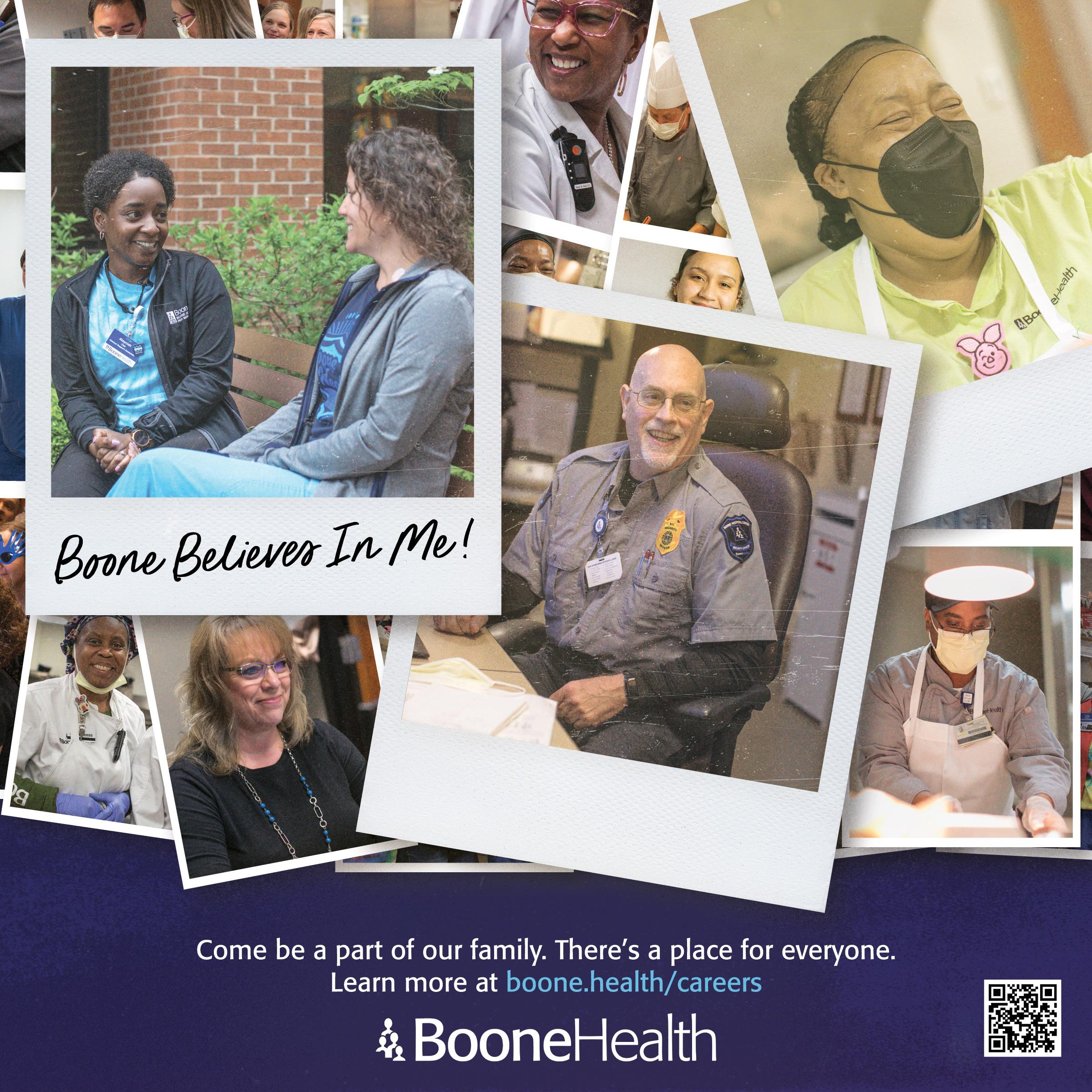
At Boone Health we like to say, “Every employee takes care of our patients,” but what does that mean? I have two outstanding examples.
Ruby Henderson, our 2022 Employee of the Year, has been a part of Boone for over 40 years. As a Physical Activity Tech in our Broadway Outpatient Therapy clinic, hers is the first face our patients see when they arrive – and Ruby is ready for them before they walk through the door. Each afternoon, she reviews tomorrow’s schedule to ensure that our patients’ needs are accommodated before they arrive. She helps new patients get established and stay on course with their treatments. Many patients mention her by name when they tell us about their positive experiences with Boone Therapy.
Ruby is greatly appreciated by her coworkers as well. When she reviews the schedule, she also thinks about what our therapists need so that patients get the most from each appointment. By making it easier for our physical, speech, and occupational therapists to provide exceptional care, Ruby upholds our mission by making Boone an excellent place to work and to receive healthcare.
By now, you may have seen Ruby on TV or online. When she was asked to be featured in our latest ad campaign and learned that we’d be filming in the Boone Therapy clinic, her immediate concern was that the camera crew not take up too much space in the waiting room. Her “patients first” approach reflects the best of Boone – and while her being named our Employee of the Year was a coincidence unrelated to our ad campaign, it makes perfect sense.
Our 2022 Leader of the Year, Security Operations Manager Joe Bayer, manages areas most of us don’t see and may never see. If you’ve ever called our main line, you’ve talked to one of Joe’s teams. He’s active both on our campus and in the community, collaborating with local and regional organizations to keep us prepared for any potential crisis. He held a significant role in our COVID response – including training a team of entrance screeners during the peak of the pandemic – and his commitment to this work helped us keep our patients and staff safe.

Joe takes his responsibilities seriously, but he’s well-known for his friendliness and good sense of humor. He understands the unique needs of promoting security and emergency preparedness in a clinical environment without losing sight of what makes Boone special. His work makes it easier for our employees to focus on delivering high quality care to our patients even under difficult circumstances.
A healthcare organization thrives because of people like Ruby, Joe, and everyone else who’s committed to giving their best. Our patient care staff, medical staff, and support staff share one mission: To improve the health of the people and the communities we serve.

Even if you’ve never thought about working in healthcare, if you take a service-oriented approach to your work, if you strive for excellence, if you enjoy being part of a team and making a difference, we may have a place for you at Boone!
I encourage you to visit www.boone.health/careers and find your opportunity to care for our patients.
 Troy Greer CEO, Boone Hospital Center
Troy Greer CEO, Boone Hospital Center
This January, the Boone Hospital Foundation delivered an Automated External Defibrillator (AED) donation to the historic Village of Arrow Rock, Mo.

The Village of Arrow Rock requested the AED from the Boone Hospital Foundation noting it has more than 120,000 visitors per year and 55 yearround residents.
The AED is installed on the boardwalk which is near the six retail shops and two restaurants. The boardwalk is also where the majority of visitors congregate.
Shop owners, local first responders and several village residents will be trained in the use of the AED.
“The Boone Hospital Foundation supports the mission of Boone Health –improving the health of the people and
communities we serve. AED devices are easy to use and can mean the difference in life and death,” says Barbara Danuser, Boone Hospital Foundation Executive Director.
Sudden Cardiac Arrest is a leading cause of death in the US, accounting for an estimated 325,000 deaths each year.

Boone Health is proud to announce Peter Gloggner, SHRM-SCP as the new Chief People Officer.
Peter has nearly two decades of Human Resources experience including previous service with Boone Hospital Center. Peter has a strong reputation for innovation and cultural development.
Prior to joining Boone, Peter served as the Vice President of Human Resources at Calvert Health in Prince Frederick, Maryland. Prior to his time in Maryland,
For each minute that passes without Defibrillation and CPR, the chance of survival from Sudden Cardiac Arrest decreases by 7-10%. If a cardiac arrest victim is shocked with a defibrillator within the first minute of collapse, the chances for survival are close to 90%.
Peter served as the Chief Human Resource Officer at Jupiter Medical Center in Jupiter, Fl. Peter received his Bachelor of Health Science in Health Services Management from the University of Missouri and his Master’s in Business Administration from William Woods University. Peter started his career as a Communications Supervisor and then Manager of Human Resources & Training at Boone Hospital Center.
“I am excited to return to Columbia and be part of the Boone Health family,” says Peter. “A lot has changed in health care and at Boone since I was last here, but the commitment to quality care and creating an excellent place to work has remained. I am looking forward to doing everything I can to continue that mission.”

Boone Health and Peak Sport and Spine are joining forces at 20 outpatient therapy clinics in mid-Missouri, bringing together two longstanding health care organizations.
The move allows for an elevated coordination of care throughout the patient’s health care journey and accelerates Boone Health’s efforts to expand access to quality care in mid-Missouri.
“We know that Peak Sport and Spine is a strong organization that provides great service to their patients,” says Troy Greer, CEO of Boone Health. “They have established locations throughout our service area in mid-Missouri, including places we currently don’t have a presence. This allows us to continue our focus of bringing Boone care closer to home for our patients.”
The therapy clinics join 9 primary care clinics, 2 convenient care clinics, 10 specialty clinics, and 9 lab services locations in Boone Health’s growing outreach portfolio.
“A lot of our patients have a Boone primary care provider or have surgery at Boone Hospital,” says Phillip Smith, CEO of Peak Sport and Spine. “Now,
those patients have the option to complete their patient journey receiving therapy at a Boone-affiliated Peak Sport and Spine clinic. Our current patients won’t notice a change in the care they receive. It will be the same staff in the same location. But behind the scenes, the coordination of care will be enhanced.”
Peak Sport and Spine locations that will partner with Boone Health include Ashland, Boonville, Camdenton, Centralia, Columbia Berrywood, Columbia South, Columbia West, Fayette, Fulton, Jefferson City South, Jefferson City West, Kirksville, Linn, Marceline, Mexico, Moberly, Milan, Montgomery City, Osage Beach and Owensville.

Boone Health recently donated an ambulance to the Armstrong Fire Department. The vehicle is a 2001 Ford E350 that is low-milage and well maintained but is not compatible with Boone’s current stretcher technology. The Armstrong Fire Department was in need of a more reliable option to replace their current vehicle.
Columbia Family Medical Group’s physicians have joined Boone Health Medical Group. Carolle Silney, MD will now practice at Boone Health Primary Care Nifong, 900 W. Nifong, Columbia. George Prica, MD and Siamac Vahabzadeh, MD will both practice at Boone Health Primary Care Broadway, 1605 E. Broadway, Columbia. Learn more at www.boone.health/primarycare.


Carolle Silney, MD

Boone Health Primary Care Nifong 900 W. Nifong, Columbia George Prica, MD
Boone Health Primary Care Broadway 1605 E. Broadway, Columbia Siamac Vahabzadeh, MD
Boone Health Primary Care Broadway 1605 E. Broadway, Columbia
79 -year-old Betty Hassien is now pain and symptom free after receiving the LINX® Reflux Management System.

Betty suffered for more than 20 years with gastroesophageal reflux disease (GERD). Betty had a hiatal hernia causing her GERD, heartburn, regurgitation, chest pain, coughing, and vomiting. Hiatal hernias are formed when muscle surrounding the esophagus weakens and allows the junction of the esophagus and stomach to bulge up through the diaphragm into the chest cavity. This will often cause GERD symptoms, and the hernia will often gradually worsen over time.
“I tried medication for years, but I was still having problems. It was really interfering with my everyday life. I was constantly having pain and vomiting. I was told that I should possibly do Gastric Bypass, but I really didn’t want to do anything that invasive. That’s when I went to see Dr. Gerber,” says Betty.
Dr. Benjamin Gerber, MD of Boone Health General Surgery specializes in minimally invasive surgeries for acid reflux and hiatal hernia repair. After meeting with Betty, he suggested she repair her hiatal hernia using the LINX® Reflux Management System.
The LINX® system consists of a series of titanium beads, each with a magnetic core that is connected with titanium wires to form a ring shape. The device is surgically implanted around the lower end of the esophagus. It then helps to prevent the
digestive acids of the stomach from backing up into the esophagus (acid reflux) while still allowing for food and drink to flow into the stomach. The procedure is an outpatient procedure and the device is placed as one of the parts of the hiatal hernia repair surgery (an alternative to the Nissen Fundoplication).

“The vast majority of patients who receive the LINX® device will no longer have to take acid reflux medications.

When compared to other acid reflux surgical options, the LINX® has the advantage that the patient may still burp and vomit as normal. Other options that do not allow this can leave the patient feeling bloated and uncomfortable.” says Dr. Gerber.

Betty was able to go home the day of her surgery and says within two weeks of undergoing the procedure, her GERD symptoms were gone.
“I am completely better. No more vomiting or reflux at all. I am also really happy to not have to take medication anymore. I am so grateful for this procedure and Dr. Gerber,” says Betty.
Betty is now enjoying her life pain and symptom free. She stays busy spending time with friends, her husband Joseph, her two children, 10 grandchildren, and 5 great-grandchildren.
By Madison LoethenFIND US AT: 1601 East Broadway Suite 240 Columbia, MO 65201
OFFICE HOURS: Monday-Friday, 8 a.m. - 5 p.m.
PHONE: 573.815.8145
It was the blizzard of 1979. Heavy snow and wind whipped around Sereatha Jean Branham as she trudged up the hill, from her small apartment on Broadway to Boone County Hospital to apply for a job.
Sereatha was hired as a Patient Care Tech (PCT) in the ICU. This year, she is celebrating her 44th anniversary at Boone Health. Planning to retire in 2024 after her 45th anniversary, Sereatha calls herself “The Original”, as there is not another employee who has worked in the ICU as long as she has.
Starting out as a PCT, Sereatha’s responsibilities were patient care. 45 years ago, there were fewer nurses in the unit, which gave the PCTs more responsibilities. Nurses spent more time watching monitors and putting in IVs and lines while PCTs checked patient vitals, suctioned ventilators, gave baths and responded to codes.
“Back then, we didn’t have all of this fancy equipment like they do now,” Sereatha says. “Now, they have a machine to check blood pressure. Back then, we had to do that manually. If the patient was on a dopamine drip, I would sit in a patient’s room taking their blood pressure every 5 minutes. 5 minutes goes fast when you have to take a blood pressure.”
Sereatha loved being a patient care tech. “I was sought after too,” she recalls with a smile. “We gave soap and water baths and I used to shampoo and braid hair.” Sereatha was a PCT for 20 years before her job duties would change.
As machinery evolved and the number of nurses increased, the need for techs decreased and Sereatha’s job moved to a Supply Technician. Her duties included keeping stock of needed items in patient rooms and items needed in each unit.
The ICU used to be separated into 3 units; MICU – Medical Intensive Care Unit, SICU – Surgical Intensive Care Unit and NICU –Neuro Intensive Care Unit. Sereatha had only worked in the MICU, but when the intensive care units combined, Sereatha worked for all 3 units. “It was busy,” Sereatha says, “but I did it.”
Doctors still had written orders and Sereatha would input orders into the patient charts. As she recalls, nurses would then double check that everything was done correctly, which they called "chart checks."
“It was a very busy time,” Sereatha says, “but I loved it.”

After stocking for 15 years, Sereatha became a Unit Secretary and has been doing that ever since. Today, she sits at the front desk and greets everyone with a smile. She’s the first face that family members see when they come into the ICU, and she wants them to feel at ease.
When the ICU moved to its current location and the old MICU was getting remodeled, Sereatha made it a point to visit one final time. It was important to her to remember this space for the nurses and techs who didn’t get to experience how the ICU had grown. When she got there, the rooms were empty and the halls
were quiet. She found a block to sit on and cried. “I could literally see the nurses and doctors running around and I just had to say goodbye,” Sereatha said.
Sereatha has a huge heart for the nurses in the ICU. In 2021, Boone Hospital held a virtual event for Nurses' Week. Hearing how sad the nurses were that there was not a group event planned due to COVID restrictions, Sereatha told her nurses that she would throw them a party.
She opened her home for 2 days for the ICU staff. Turning her garage into a party room, she had lights, couches, pub tables and a bar. “It looked like a little lounge,” Sereatha said. “Over 50 people came, including some doctors. They came before or after their shift and it was just a nice time for everyone.”
Born and raised in Columbia, Mo., Sereatha and her family are connected to Boone Health. Sereatha is a Boone baby herself, as is her daughter Camille, who turned 25 on Valentine’s Day. Sereatha is the youngest of 10 siblings. One of her sisters, Vivian, worked at Boone Health for 14 years on the Psychiatric Floor in the 80’s and one of her brothers was a nurse on the Joint Replacement Unit.

“I’ve always loved nurses and have had admiration for them,” Sereatha says. “When I first started here back in 1979, there were only two African American nurses in the hospital. They were both RNs. There were LPNs, but not RNs. Now there’s a bunch. We’ve come a long way.”
Sereatha was awarded Employee of the Month in 2017.
“I’ve just seen how the hospital has grown over the years. The technology and roles have changed, and it’s just been neat to see the progression,” Sereatha recalls. “Boone has been my family.”
By Erin WegnerMany people struggle with their memory. It’s certainly not uncommon to experience a decline in memory as people age, but how do you know if your memory difficulties are part of the normal aging process or a sign of something more serious?
Alexis Caletka and Sara Beth Kirkweg, Speech-Language Pathologists with Boone Therapy, help physicians answer this question for their patients through a formal cognitive assessment. Whether a patient’s doctor diagnoses a mild impairment or a more severe neurological issue, cognitive therapy may help.
Processes that allow the brain to learn, make judgments, problem-solve, and recall information relate to cognition. With normal aging, mild changes can occur in memory and word finding, such as when what you want to say is right on the tip of your tongue, but you have trouble getting it out. But when memory problems start to interfere with your ability to function independently, a formal assessment of cognitive skills can distinguish normal aging from underlying neurological processes such as dementia or other neurological disorders. The first step to take if you or someone you know is concerned about memory loss is to contact a physician.

“We get referrals from different providers,” says Sara Beth. “They may be from general practitioners whose patient says, ‘I’m having some difficulty with my memory.’ Their first step may be to send them to us to have a cognitive evaluation to determine if there are any cognitive concerns that might need further referrals. Or we might get a referral from a neurologist for a patient with known cognitive concerns to get a baseline measure for how the patient’s performing or to determine if the patient is performing worse than they had been previously.”
Alexis and Sara Beth begin with standardized cognitive assessments, where patients answer questions and perform tasks to assess cognitive abilities. Depending on the results, they may recommend therapy to the patients’ doctor. The strategies they teach patients in therapy focus on what individual patients need to help them in their daily lives. Every case is unique because each
patients’ deficits and requirements to live as independently as possible are different.
“If it’s something they still have to do in daily life, like manage their medications, and they can’t remember what to take and when, that’s where we come in,” says Alexis.
Cognitive therapy is used to treat more than memory. Sara Beth and Alexis treat patients who experience difficulty with problem-solving, reasoning, judgment, maintaining attention, and executive functions, including the ability to plan, organize, and execute tasks. They also treat patients who have language problems, like being unable to find the words to express themselves. Regardless of the deficit, seeking treatment early can help patients with cognitive impairment live more independently for longer.
To help with memory, there are internal strategies like using mnemonic devices such as rhymes, songs, or acronyms. Boone Therapy also teaches external strategies, like using a calendar to
remember appointments or using a pill sorter and setting alarms to remember to take their medication.
Cognitive therapy tends to be more effective when family members are involved.
“We always encourage families to be involved in therapy,” says Alexis. “The more people you have who can help carry over the strategies that you are trying to implement within your therapy session – which is only maybe one hour a week – the better. The family is with them all the time. So, if they can be here for the therapy to help carry over whatever we’re working on, it’s more likely to be effective.”
Alexis adds, “If someone has a bad enough memory impairment, they aren’t going to remember what we’re saying outside of the sessions. Having someone else to help remember information is necessary as well.”
Motivation is an equally important factor in therapy success. If patients are not willing or not interested in participating fully, therapy will be less effective.
Toward the end of the therapy process, Sara Beth and Alexis readminister the cognitive assessment to check for measurable improvements in the targeted deficits. Patients may be discharged from therapy or referred for more if they need more time and support.

By identifying memory decline and providing strategies for patients and their loved ones, Sara Beth and Alexis help people safely and effectively perform the activities of daily living with confidence and lead better, more independent lives.
 By Michelle Terhune
By Michelle Terhune
Early melanoma detection can be as easy as A-B-C-D-E.

For more information on Community Wellness screenings, visit boone.health/community-wellness or call 573-815-3876.
Skin cancer screenings are the best way to detect melanoma and other skin cancers early, when they are easier to treat. If you’re at increased risk for skin cancer, you may need an annual skin cancer screening exam. Even if you have never seen any suspicious moles or spots on your skin, you should still see a dermatologist.

It is important to become familiar with your skin so you can notice changes, but it’s also a good idea to see a dermatologist for a baseline skin check. Having a physician or trained expert check your skin for subtle changes you may not see is helpful for spotting signs of melanoma and other types of skin cancer early.
Melanoma is the most serious type of skin cancer. It develops in cells called melanocytes that produce melanin, the pigment that gives your skin its color. The exact cause of all melanomas isn’t clear, but exposure to ultraviolet (UV) radiation increases your risk of developing the disease. UV radiation can come from sunlight, tanning lamps, and tanning beds. Genetic factors and skin type can also affect your risks for skin cancer.
Even if you don’t currently have any skin concerns, if you have a family history of melanoma or you use or have used tanning beds, seeing a dermatologist for a baseline skin check can make it easier to look for any changes in the future.
If it’s not checked early, melanoma cells can spread to other areas of your body through the bloodstream and lymphatic system. When it spreads, melanoma can become difficult to treat, but melanoma can be curable if caught early.
When you check your skin, remember the A-B-C-D-Es of skin cancer:
• Asymmetry. Look for moles are markings that are irregularly shaped or where one half looks different from the other.
• Border. Look for moles with uneven, jagged, or scalloped borders.
• Color. If a mole or area of skin changes color or has multiple colors, have it examined by a dermatologist or trained healthcare professional.
• Diameter. If you have a mole larger than one quarter-inch across, have it checked.
• Evolving. If a mole changes in size, shape, or color, or you notice bleeding, itching, or tenderness, have it checked immediately.
A skin check by a dermatologist only takes a few minutes but it’s a critical part of identifying skin cancer early. A dermatologist will also check for basal cell carcinoma and squamous cell carcinoma. These cancers typically look like pink, red, or scaly spots on your skin that don’t go away on their own. They may also bleed and grow in size. Although it is more common to develop new moles during childhood and early adulthood, older people may develop other pigmented spots, such as seborrheic keratosis, that could be mistaken for moles and cause concern. If you’re concerned about any new spots or changes to your skin, consult a dermatologist. You can also help detect and prevent skin cancer by developing healthy skin habits. Get in the habit of checking your skin once a month, and become diligent about protecting your skin. Stay out of the sun during the middle of the day, when UV light is strongest. When you go outdoors, wear protective clothing, including a hat. Use sunscreen in all seasons and all weather. Your sunscreen’s SPF, or sun protection factor, should be at least 30. Look for broad spectrum sunscreen that protects the skin from both UVA and UVB rays. Apply sunscreen generously and reapply frequently to get the full amount of protection.
By Jenny L Workman, Boone Health Community Wellness ManagerA Asymmetry B Border C Color D Diameter E Evolving
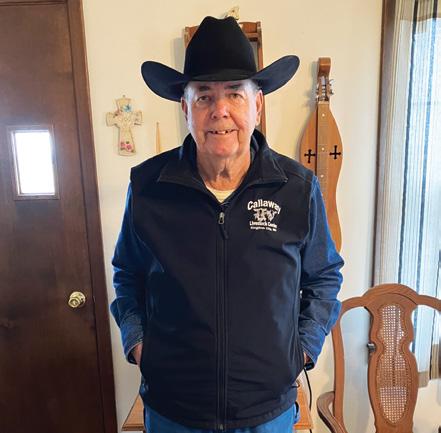
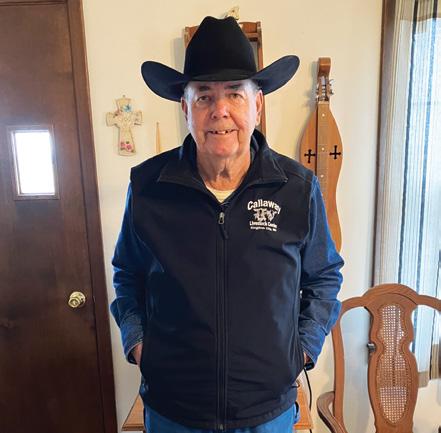
John Brumagin is a mid-Missouri cattle rancher who has now had both knees and hips replaced by Columbia Orthopaedic Group. Although John will tell you all four replacements went smoothly, he was particularly pleased with his most recent joint – a new hip courtesy of COG surgeon Samuel Thompson, MD.

“The knees were the hardest and had the most recovery time,” John says. “But with this hip Dr. Thompson did, I didn’t have much pain at all. I took over-the-counter pills for pain for a couple of days and the therapist had me walking up and down my drive within three or four days.”
Dr. Thompson performed an anterior hip replacement on John in October 2022.
To understand the benefits of anterior hip replacement over more traditional posterior hip replacement, it helps to know how these surgeries work.
In both procedures, the surgeon removes the worn-out parts of the joint – including the ball at the top of the thigh bone, the stem that connects it to the thigh bone, and portions of the interior of the hip bone socket – and replaces them with titanium, ceramic, and plastic equivalents.
During posterior procedures, patients are placed on their sides and the surgeon makes a curved incision on the side and back of the hip. An incision is made in the large muscle in the hip (the gluteus maximus) which is laid open to get access to the joint.
During anterior hip replacement, patients are placed on their backs on a special operating table. The surgeon makes an incision, approximately 5 or 6 inches long, in the skin on the front side of the thigh. The work of removing and replacing worn parts is done between the muscles without cutting them.
To see what he’s doing during the anterior hip procedure, Dr. Thompson uses a small X-ray machine, interfaced with a computer software program called Radlink. This equipment helps him confirm that the stem inserted into the femur, ball, and socket are precisely in the correct position.
According to Dr. Thompson, there are two key reasons why anterior hip replacement may be a better option for some patients. Because the surgeon works between the muscles instead of cutting through them, your muscles don’t have to heal after surgery.

“What’s evident in the literature is that early recovery is easier,” says Dr. Thompson. “Long term, the functional outcomes are similar between both approaches, but patients
can return to their desired activity level sooner after an anterior hip replacement. This is especially attractive to the younger, more active patient.”
Dr. Thompson says the risk of dislocation after posterior or anterior hip replacement is low, but the anterior procedure results in even lower numbers. He explains, “It’s becoming increasingly clear that the risk for hip dislocation after an anterior hip replacement is lower. This is probably due to the fact that we don’t have to cut the muscles around the hip to do the surgery, so the hip is not destabilized. It’s also very easy to use computer-assisted techniques during anterior hip replacements that help us accurately place the implants, reducing the possibility of putting in the parts in a way in which they might be more likely to dislocate.”
Anterior hip replacements can be done outpatient procedures. Once the patient wakes up from the anesthesia, they can usually get up and walk right away.
John did spend the night at Boone Hospital Center just like he did after the posterior hip procedure, but he’ll tell you his recovery was easier with the anterior procedure.
“This worked better. I can’t describe it, but it was better,” John says. “It took longer for my other hip to build back up that muscle they cut.”
Dr. Thompson performed John’s surgery on Thursday and discharged him on Friday. John used a walker for a couple of days but by Monday, the physical therapist had John up and down stairs and the driveway, using only a cane. He was then back on his side-by-side, helping his son and grandson feed cattle.
Not all patients are candidates for anterior hip replacement. Patients with complex problems or existing hip hardware may require the exposure afforded during a posterior hip replacement. Patients who have fat that rests over the front of the thigh are usually not candidates because it hinders proper healing of the incision.
Dr. Thompson learned anterior hip replacement during his orthopedic surgery residency and hip and knee replacement fellowship. Among the hip specialists at Columbia Orthopaedic Group, he is the only one currently performing the anterior procedure. He anticipates that will change as the procedure continues to grow popular.
“At the American Association of Hip and Knee Surgeons annual conference this past year, the percentage of hip surgeons who do anterior hip replacement as their primary approach to the hip has risen to 56 percent,” Dr. Thompson says. “In 2010, it was only 12 percent.”
Although anterior hip replacement may not be for everyone, people like John have experienced the difference.
“Basically, I don’t see how I could have done any better,” John says. “I was very pleased.” By Michelle Terhune

is how many Boone Health pelvic floor therapy patients describe their success. But what is pelvic floor therapy?
Pelvic floor therapy is a specialized kind of rehabilitation that works to lessen the symptoms of pelvic floor dysfunction through a personalized treatment program. It can improve pelvic pain, bladder control, bowel control, pelvic organ prolapse, pain during pregnancy and after childbirth, and pain with sexual intercourse.
The muscles of the pelvic floor sit inside the pelvis and support the internal organs, assist proper bowel and bladder function, contribute to sexual function, and support healthy movement of your hips and core. They are involved in a huge variety of daily activities and can significantly impact quality of life. Boone’s pelvic floor physical and occupational therapists have received specialized training to help you understand your pelvic floor and get back to the activities you love without limitation.
“When I first meet a patient, I spend time understanding their unique limitations and goals. Together, we develop a treatment plan that focuses on retraining the way the body moves and functions to meet those goals,” says Beth Frazier, one of Boone Health’s pelvic floor physical therapists.
Beth Frazier explains the anatomy behind pelvic floor dysfunction.
On the first visit, the therapist assesses movement patterns, posture, breathing mechanics, hip and core strength, and performs any additional specialized tests pertinent to the symptoms. An internal vaginal or rectal examination is often recommended to assess the strength, muscle tension, and motor coordination of the pelvic floor. This exam also allows the therapist to assess for organ prolapse and check for scar tissue if applicable. An internal assessment provides valuable information for the patient and therapist to understand the root cause of the symptoms. However, internal examinations are completely voluntary based on patient comfort. The therapist and patient then develop a treatment plan that is catered to them.
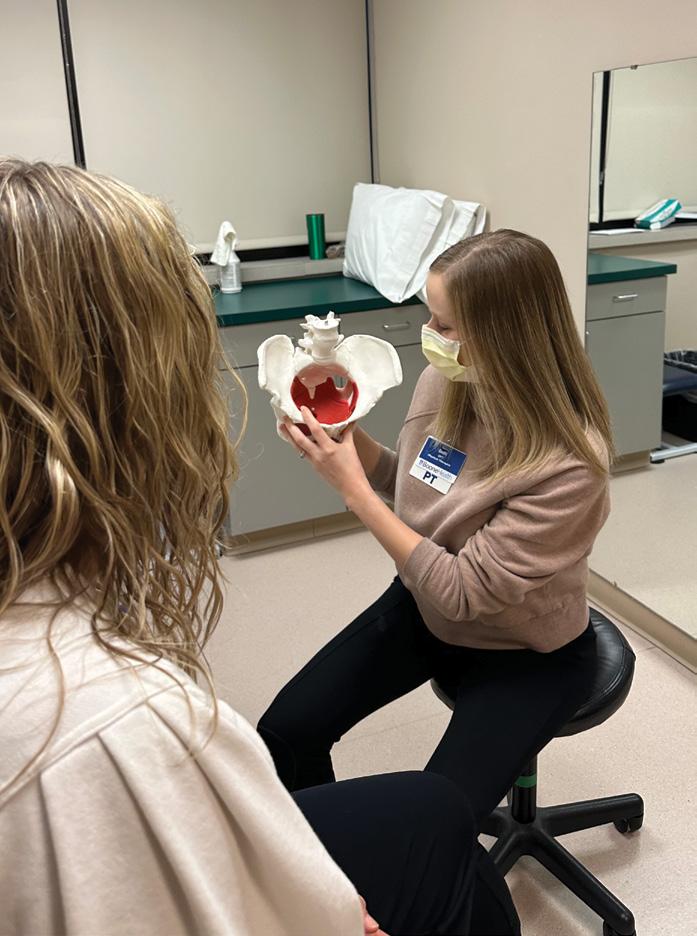
“We may start working on coordination with very basic exercises laying on a mat and then gradually progress to higher level exercises and more functional activities. We use a variety of hands-on manual techniques to address pain, tight muscles, and scar tissue restriction such as massage, manipulation, and dry needling. We also teach patients stretches and breathing techniques to maintain that normal, pain-free muscle tone going forward,” says Beth.
Patient education is also a big part of pelvic floor therapy. Beth shares, “My biggest goal is always to help patients understand what is going on with parts of their body they may not know much about and begin to move in ways that are healthier, so they are able to do what they want to do without pelvic floor dysfunction. We have seen both men and women able to maintain bladder or bowel control after years of struggling. We have seen women return to exercises they thought they’d never be able to do again with prolapse. We have also seen women no longer experience painful sex that had been disturbing their relationship for years.”
Pelvic Pain: Increased tightness in the muscles of the pelvic floor can lead to pelvic pain. This can make pelvic exams, the use of menstrual products, and sexual activity very painful or even impossible. Pelvic floor therapy will guide you in understanding the root causes of your pain and beginning the road to recovery.
Bladder Control: Individuals of all ages deal with urinary leakage during activities like coughing, sneezing, and jumping. The muscles of the pelvic floor support the bladder to sit in the correct position. Bladder control issues may be caused by weakness or tightness of the muscles of the pelvic floor. Pelvic floor therapy will help you understand how your pelvic floor works together with your core.
Bowel Control: Bowel control issues include chronic constipation and fecal leakage. Pelvic floor therapists work as part of a multi-disciplinary team with your physician, dieticians, and gastrointestinal specialists to help you begin regaining bowel control.



Pelvic Organ Prolapse: Often experienced as a sensation of pelvic heaviness, pelvic organ prolapse can occur after childbirth or after repetitive straining during activities like weightlifting or toileting. When one or more organs, including the bladder, uterus, or rectum, have dropped lower than their normal position, this is considered prolapse. A pelvic floor therapist can help you understand if prolapse may be the root cause of your pelvic heaviness and teach you pressure management techniques to manage your symptoms.

Pregnancy and Postpartum Rehabilitation: A variety of aches and pains can arise during pregnancy that suddenly limit your ability to move. Boone’s pelvic floor therapists are specially trained to understand the issues that arise during pregnancy and the postpartum healing phase. They specialize in addressing pubic bone pain, sacroiliac pain, pelvic pain, and diastasis recti (commonly called “ab split”).
By Madison Loethen
Beth says she has seen lives changed by pelvic floor therapy. Ask your doctor for a referral to Boone Therapy if you think pelvic floor therapy may be right for you.
Pelvic floor therapy can help you regain the function you had prior to childbirth and return to movement without limitation.


As babies grow up, the frequency of their doctor visits slows down. By the time most kids are 3 years old, well child checks are recommended annually. Aside from influenza and COVID vaccines, the CDC-recommended immunization series pauses after 4 years old.
But even if your child’s school-age development seems on track, don’t skip regular pediatric visits. Kids benefit from routine well checks, including immunization beyond early childhood, and parents benefit from having a reliable and trusted partner to help them make the best decisions for their children.
There are a few important immunizations for kids entering their teen years. Pediatricians generally follow CDC guidelines for optimal timing to protect patients against vaccine-preventable diseases as early as possible. Of course, recommendations should be tailored based on a child’s individual risk factors.
Meningococcal serogroup
A, C, W, Y vaccination (MCV)
Routinely given at the 11-year well check and boosted at the 16-year visit, this vaccine protects against Neisseria meningitides serogroups, which have historically caused the most cases of disease and death. Meningitis can be neurologically devastating to people who survive infection. This series is required by most school systems.
Meningococcal serogroup
B vaccine (Men B)
This two-shot series is usually given 4 weeks apart between 16 and 18 years. The vaccine provides additional coverage for adolescents at increased risk for infection during an outbreak, especially if they are immune-deficient or reside in close quarters, like a dorm. Although this immunization is considered generally safe, and more cases of meningitis are caused by serogroup B than all other serogroups combined, this vaccine is not mandated by most public-school systems.
This vaccine is routinely given at the 11-year well check and boosted 6 to 12 months later. If the series is started when
the patient is 15 years old, they will need an additional booster 1 month after the first dose. This vaccine is one of very few preventative therapies that can reduce the risk of certain types of cancer. For girls, HPV immunization vastly reduces the risk of cervical cancer and precancer. For boys, the HPV series protects against common causes of some oral and throat cancers. This important vaccine is highly recommended but is not mandated by most school systems in Missouri.
Given at the 11-year well check, the combination Tdap vaccine protects against tetanus, diphtheria, and pertussis. This vaccine is boosted every 10 years for adults. This vaccine protects against several pathogens, including Clostridium tetani, which can cause paralysis; Corynebacterium diphtheriae, a rare infection that can cause severe damage to the throat and respiratory tract; and Bordetella pertussis, or whooping cough, a prevalent disease that can be devastating to infants who cannot yet receive the vaccine. Tdap boosters are recommended for all family members and anyone in a household with a newborn baby. Tdap immunization is required by most school systems.
Well checks for adolescents cover much more than routine immunization – they also review your child’s growth, sleep, diet, academic, and behavioral trends. Regular visits allow your teen’s doctor to monitor their health and detect any changes that may have major medical ramifications.
Being a teenager can be difficult no matter what era they grow up in, and while there are more creature comforts in 2023 than in 1993, adolescents face a growing list of challenges that weren’t
present for older generations. Teens today face increasing incidences of mental health disorders and obesity, and they are exposed to increasing amounts of misinformation.
As a parent, it’s sometimes difficult to spot subtle changes or shifts in attitudes, behaviors, or health habits. For an adolescent, it can be difficult to talk about stressors or health concerns. Well child checks can bridge that gap and present an opportunity to review how your teen is affected by socioemotional and physical stressors, while building trust between patients, parents, and pediatricians.
With countless sources blurring the lines between information and entertainment, it can be difficult to know which sources to trust or who to believe. Misinformation can cause a poor understanding of health or inaccurate explanations of medical conditions, which poses inherent health risks. While a patient may benefit from some publicly shared knowledge, a doctor’s appointment lets them reflect upon their personal health experience and engage with their health in positive, productive ways.
Regular visits with a pediatrician can empower parents and teens. We owe the next generation an honest assessment of their collective and individual health so that, as they enter adulthood, they can take responsibility for their health, maximize their moment to move forward, and thrive despite barriers to success.

We owe the next generation an honest assessment of their collective and individual health so that, as they enter adulthood, they can take responsibility for their health, maximize their moment to move forward, and thrive despite barriers to success.

Iworked my first shift at Boone Hospital’s Emergency Department in December 2003. Since then, my roles have included attending physician in the ER, IRB medical director, Ethics Committee chair, Emergency Department Chief and Facility Medical Director, EMS Medical Director, and I am currently Chief of Staff for Boone Health’s Medical Staff. I am also boardcertified in Family Medicine.
My immediate family includes wife, Zorina – married 24 years and counting –and two sons, Marcus, in sophomore year at Case Western Reserve University in Cleveland, Oh. and Kaden, in senior year at Columbia Independent School and heading to Carleton College in Northfield, Mn. next fall.
I took my first breath in 1959, born of largely Norwegian stock in Minnesota. Despite this, lutefisk, the piece of cod which defies all understanding, simply won’t go down. My education went down better, though, entirely thanks to the encouragement of family and the marvelous generosity of others. Shattuck School in Faribault, Mn. offered secondary school college prep. Yale College in New Haven, Ct. offered liberal arts education and a major in the history of ideas. Harvard Divinity School in Cambridge, Ma. enabled better understanding of compelling religious issues first encountered at home. Columbia College of Physicians and Surgeons and School of Public Health in New York offered initiation in the science and study of health and medicine. An internship in General Surgery and Residency in Family Practice at Montefiore Medical Center in New York helped me hone skills and methods into actual practice. A few years later, a fellowship in Medical Informatics again at Columbia College offered a working education in the uses of information technology in health care.
Why did you get into the health care field? Many people start their way toward a health care career by taking a pre-med track in college. But only after college, several months of wandering, and two years as a Peace Corps volunteer in Botswana from 1982 to 84 did any such path make sense. Training in medicine then seemed a reasonable way to carry on a family tradition of service while cultivating personal interests in science, problem-solving, and exploration. People need doctors everywhere, but they also need good mechanics.
What interested you in your particular specialty? Caring for people, solving interesting medical problems, constant learning, and avoiding boredom.
What is the most rewarding part of your job? To see how, whatever impediments, flaws, fatigue, or trouble arises, we still manage to do our best to care for each other.
What is the most challenging aspect of your job? Dealing with the uncertain and unexpected. But that makes it most interesting, too.
What do you see changing in health care in the next 5 to 10 years? What won’t? One hopes we won’t abandon our commitment to each other’s wellbeing. To pick just three: The tools of care — drugs, instruments, information —
will become more specialized, effective, complicated, and expensive. Physicians will learn what other employees already know, how it feels to be an exchangeable commodity. Dr. ChatGPT will replace Dr. Google and will, in turn, get replaced as well.
What advice would you give someone looking to become a doctor? Remain devoted to your patients and to providing them the best care you can. Remain devoted to your colleagues in this endeavor.
What do you enjoy doing outside of work? Family and friends, ham radio and electronics, reading, travel, astronomy, woodworking, kayaking, biking … oh look, a squirrel!.
What advice would you give to someone who is going to be a patient in a hospital for a period of time? This is more a request than advice — Boone exists to care for you, but with its size and complexity, and with the stress and vulnerability that often goes along with the need for care here, your voice might seem small and insignificant. It’s not. We need your perspective, your advice, your guidance, and your insight so we can do our job as best we can. Please do this for us as we strive to do our best for you.

Igrew up in Kansas City, with my mom, dad, sister, and brother. I went to school at Truman State in Kirksville, Mo. Initially I got a Bachelor’s in Health Sciences with an emphasis on public health. Then I completed Truman’s accelerated Bachelor of Science in nursing program. I’ve been with my husband, Taylor, since we were 17, and we’ve been married for 5 years. We don’t have kids, yet, but we do have one dog, Lucy.
Why did you get into the health care field? I’ve always been interested in the healthcare field. Throughout high school I thought I wanted to be a doctor. I was a member of an organization coordinated by Missouri’s AHEC (Area Health education centers) which worked to get high school and undergrad students interested in primary care medicine. So, I had the opportunity to shadow a variety of medical professionals including doctors, nurses, and dentists.
What interested you in your particular specialty?
Most of my career I’ve worked in medical and surgical inpatient nursing. I’ve also worked in the NICU and inpatient psychiatric care. When the weekend house supervisor position opened up at Boone Health, I moved into this role. The house supervisor role is kind of a catch-all position. We coordinate patient transfers from outside hospitals, respond to emergencies throughout the hospital, help coordinate staffing for nurses and techs for inpatient units, and help troubleshoot issues and answer questions for staff, patients, and families.
What is the most rewarding part of your job? I enjoy getting to see all of our different levels of care and interact with different departments at Boone. It’s great getting to work with people all over the hospital.
What is the most challenging aspect of your job? Because I typically work weekends, often there are issues that arise that I’m not familiar with and must figure out how to address or resolve.
What has changed in your field since you started practicing? I became a nurse before the COVID-19 pandemic, so I think the biggest, most obvious change is our response. COVID changed so many things from isolation practices to how nursing programs prepare new nurses.
What do you see changing in the next 5 to 10 years?
I think we’re going to see a lot of innovation in the nursing profession to manage the staffing shortages we’re seeing; however, I have no idea what that may look like!
What do you enjoy doing outside of work? I love spending time with my husband and our dog. We like to go for walks together or hang out at home and watch TV. I also love to spend time with my friends. I love to crochet – I make blankets, scarves, and smaller items. I have also recently started spinning wool into yarn.
What advice would you give someone looking to become a nurse? Be prepared to be flexible and embrace the unexpected. The nursing profession demands flexibility and the ability to adapt our practice and care to changing needs. I don’t think this is emphasized enough in nursing school, but the ability to be flexible and “go with the flow” has been a huge strength for me in my nursing career.
If you’re anything like me, you look back on your lack of proper skin care and regret every minute of it. When we’re young, we think we’re invincible and won’t ever age — until we do. Fortunately, for those of us that are behind the ball, there are a ton of options to reverse the signs of aging. For all my twentysomethings, start taking care of your skin now.
Most signs of aging are a slow and gradual process. For many patients, it feels like it comes out of nowhere. We look in the mirror and our makeup doesn’t go on like it used to, you can point out those fine lines, your makeup creases, or you feel like you’re losing volume. And to add insult to injury, we live in a time where there is so much pressure to look a certain way or to appear young. I live and teach by the rule of five. The five absolute, most important things you should be doing for your skin no matter your age, goals, season, or current condition of the skin. When it comes to skin education, these are the staples for overall skin health and anti-aging.

The. Time.
It is 2023. Skin cancer is becoming more prevalent every year. Skin cancer is the most common cancer in the United States according to the American Academy of Dermatology (2022). Sun exposure is also one of the number one causes of premature aging. Sunscreen should be worn daily, even when it’s cloudy. I recommend SkinBetter Science, Sunbetter Sunscreen to both male and female patients. This is available as a compact (SPF 56-68) or lotion (SPF 7075) and is available in sheer and tinted formulas. They are oil free, fragrance free and protect against UVA and UVB rays. Not only will you reduce your risk of future skin cancer, you’ll also prevent premature skin aging caused by the sun, including hyperpigmentation, fine lines, wrinkles and skin laxity.
Stop sleeping in your makeup. Throughout the day, the skin surface builds up pollutants, dead skin cells, oils, bacteria, and makeup. Lack of bedtime cleansing can result in dryness, breakouts, and aid in early signs of aging. Even better, double cleanse! The first cleanse is used to remove makeup and debris. The second cleanse will provide a deeper cleanse into the pores and ensure your skin absorbs serums and moisturizers to their fullest. No fancy tools or washcloths are required. I am a strong advocate for using clean hands for facial cleansing. In the morning, a single cleanse is ideal.
Hydrated skin is a key element for healthy, glowing skin. This includes both the hydration we consume with our daily water intake and the products we apply topically. A daily moisturizer should be applied, both morning and night. The type of moisturizer you need may vary depending on the season, your age, or your personal skin concerns. Drinking an adequate amount of water every day can make a drastic improvement in the hydration of the skin, improve fine lines and wrinkles and improve suppleness.
This might be the hardest recommendation for patients to follow. Picking at that one irritating blemish can spread further bacteria from your hands to your face, making the problem worse. You’ll also experience more inflammation from picking which can result in scarring and what we term post-inflammatory hyperpigmentation. This form of scarring can last months or longer and can take a multitude of treatments to significantly reduce. Trust me, stop picking.
High quality, medical grade skincare can change your skin dramatically. Medical grade skincare is only available through medical professionals. When it comes to skincare regimens, everyone’s needs are
different. I highly recommend a skincare consultation to discuss your skincare concerns and goals. Together, we will work to start you on a regimen you feel comfortable with to start achieving those goals. Many times, there is a misconception that a regimen includes using 10 products, morning and night. That’s why medical grade skincare is different. Less is more! Many times, patients report significant improvements in their skin with as little as 2-4 products. When we are working to correct, or to prevent signs of aging, the next step includes clinic treatments. Neurotoxin injections, like Botox, are used to reduce and/or stop the formation of fine lines and wrinkles. Dermal fillers are used to replace lost volume in varying areas of the face. Microneedling is used to correct scaring, hyperpigmentation, fine lines, and reduce pore size. Medical grade chemical peels can improve hyperpigmentation, fine lines, active acne, or improve overall texture and glow.
Take care of your skin early on. It won’t stop the hands of time, but it will work in your favor. If you’re past your 30’s and feel behind, it’s never too late to start. There are options available to get your skin back on track. Our office at Boone Health Medical Spa provides free consultations to discuss your options, goals, expectations, and cost. If you’re unsure where to begin, let’s chat!
By Tiffany Carmichael, FNP, Aesthetic
In moderation, chocolate can be a sweet part of a healthy diet.

In American culture, chocolate has become a sweet tradition during certain holidays, such as Valentine’s Day, Easter, and Christmas. But did you know a moderate amount of chocolate can also be part of a healthy lifestyle?
Chocolate is made from cacao pods, which grow in tropical climates around the world. The pods grow on cacao trees and contain seeds called cocoa beans. The pulpy, white center of the pod, also called the baba or mucilage, and cocoa beans are fermented for 5 to 8 days, then dried and roasted. After roasting, the cocoa beans are cracked open to reveal the chocolate nibs inside. Chocolate nibs are melted into chocolate liquor which is mixed with sugar and milk to produce the chocolate we know and love.
There are three main types of chocolate: milk chocolate, dark chocolate, and white chocolate:

• Milk chocolate is the classic combination of chocolate liquor, sugar, and milk.
According to the Food and Drug Administration, milk chocolate must contain at least 10% chocolate liquor and at least 12% milk to legally be defined as milk chocolate.
• Dark chocolate typically has more cacao solids, ranging from 30% to 80% or more. The higher the percentage of cacao in dark chocolate, the more bitter it will taste. Dark chocolate is well-known for its health benefits.
• White chocolate contains no cacao solids, but only cocoa butter, an edible fat derived from the cocoa bean. White chocolate typically has a higher percentage of sugar and milk than other types of chocolate.
Moderate amounts of chocolate – about 1 ounce or 3 squares a day – can also be beneficial to health. Most health benefits from chocolate come from the cacao – the higher the percentage of cacao, the greater the benefits. Cacao has flavanols and antioxidants, which are important for cancer prevention. Cacao has also been known to help with heart health.
Because chocolate contains caffeine and high amounts of phosphorous, it may not be the best treat for some people. If you are sensitive to caffeine, have kidney disease, or are pregnant or breastfeeding, talk to your physician to ensure chocolate is safe for you to enjoy in moderation.
Dark chocolate pairs well with spices like cinnamon and chili powder. This spicy hot chocolate recipe contains both, but feel free to adjust to suit your tastes.
 By Kristen Howard MS, RD, LD, Clinical Dietitian II, Nutrition and Food Service Department
By Kristen Howard MS, RD, LD, Clinical Dietitian II, Nutrition and Food Service Department
INGREDIENTS:
• 2 bars dark (or bittersweet) chocolate
• 1 tsp cinnamon
• 3 tbsp sugar
• 2 cups milk
• 1 cup heavy cream
• ¼ tsp chili powder
• Whipped cream, optional
• Chocolate shavings, optional
DIRECTIONS:
• In a small saucepan over medium heat, combine chocolate, sugar, cinnamon, milk, cream, and chili powder.
• Stir mixture until chocolate is melted.
• Pour mixture in mugs. Top with whipped cream and chocolate shavings, if desired.
Recipe Source: wanderzestblog.com/mexican-hot-chocolate
With its beautiful scenery and perfect outdoor exercise weather, spring is the perfect time to refresh your tness routine.
Exercising outdoors is not only good for your cardiovascular health, but it can also act as a natural antidepressant. Sunshine increases serotonin, a mood-stabilizing neurotransmitter, and exercise produces endorphins, a hormone that boosts your mood. Best of all, outdoor exercise is free!
ese strength-training exercises can be added to your current exercise routine. Start this routine with a 5- to 10-minute warm-up, like a walk through your neighborhood
or favorite park. Do this routine 2 to 3 times a week. Start with 1 or 2 sets of 8 to 10 repetitions and increase as tolerated. Most of these exercises can be done using a stationary object like a park bench, wall, or sturdy chair. Don’t forget to incorporate cardiovascular exercises throughout the week, such as walking, biking, or playing your favorite outdoor sport. By Mackenzie Beck, MHA, ACSM-CEP, Clinical Exercise Physiologist, Cardiopulmonary Rehabilitation, and Matt Pehle, BS, NASM-CPT, Exercise Physiologist, Community Medical Fitness Center
Targets your chest muscles and triceps
Place both hands slightly below shoulder level on a bench or wall. Engage the core by tightening your abdomen and squeezing your glute muscles. Bend the elbows to lower the chest, hips, and head toward your hands. Slowly lower your body until your elbows reach a 90-degree angle. Push your body back to starting position to complete the exercise.
Variation: For a challenge, adjust your hands and body to position yourself more horizontally.
Targets your biceps
Hold a dumbbell or weighted object, like a water bottle, with your arms straight down at your sides and your palms facing outward. Standing tall, slowly raise the weight while keeping your upper arm close to your body. Slowly return the weight to starting position and repeat.



This exercise can be done with one arm at a time or both arms together.



Targets muscles in your outer hip and thigh
Stand near a chair or bench, using one or both hands for support. Slowly raise one leg away from your body until you feel a stretch – but not pain – in your hip. After one set, switch legs and continue until you have done 2 or 3 sets on each leg.






Variation: For a challenge, add resistance with ankle weights or bands.

Targets muscles in your glutes and upper legs
Stand tall with your feet in a comfortable stance, about shoulderwidth apart. Extend your arms in front of your torso as a counterweight, then slowly sit your pelvis straight down. Keep your knees just over your toes as you squat. Slowly return to standing position to finish the movement




Variation: To make this exercise easier, lower yourself onto a chair or bench, which you can use to help you return to a standing position
Targets your oblique muscles
Stand tall and engage your core. Hold both hands overhead to one side, then slightly bend your legs while rotating your torso to the opposite side. Bring your hands down, extending toward your toes in a chopping motion. Repeat on the opposite side.
Variation: Add weight by holding a kettlebell or dumbbell.
Targets muscles in your core
Lie flat on your back on the ground or bench with your knees slightly bent. Cross your arms in front of your chest, placing your fingertips on your shoulders. Point your elbows toward the ceiling and lift your shoulder blades off the mat. Brace your core and hold for one second. Slowly return to start position in a controlled movement.
As proud partners of Boone Health, we’re committed to the community, to hire the best, and provide the best service to the hospital and its patients.


On January 26, 2023, Club Car Wash presented a check to the Boone Hospital Foundation’s NICU fund. Club Car Wash raised $3,034 for the NICU when they held their Grand Re-Opening on Sandman Lane in Columbia, Mo. The check presentation also served as a reunion for the Burgher family and the caregivers who took care of their Boone baby, Landon, when he we was in the NICU for a period of time in 2021. What a reunion it was!

Monday, May 8 at The Club at Old Hawthorne


Gala
Saturday, October 14 at The Country Club of Missouri
Board Members
Leadership
Board President: Betsy Vicente
Board Vice-President: Dr. James Roller
Board Secretary: Sara Jeffrey
Board Treasurer: Paul Mehrle
Representatives
Board of Trustees Representative: Jan Beckett
Board of Trustees Representative: Randy Morrow
On December 19, 2022, Columbia First Nazarene Church presented a generous donation to Harris Breast Center through the Boone Hospital Foundation. The Ladies Ministry organized a “Pink-Out Sunday” event on October 30, 2022. With pledges, donations, and ribbon pins they raised $735 for Harris Breast Center. The Ladies Ministry is led by Boone Health RN Hope Heuer who works in our Post-Anesthesia Care Unit. Hope, who takes care of many patients who battle breast cancer, saw a great opportunity to create awareness for her church family and raise some money for a good cause. Thank you to Hope for all you do for our patients and community – and thank you to Columbia First Nazarene Church!


Boone Health Representative: Drew Wilkinson
Active Boone Physician

Representative: Dr. Joss Fernandez
Community Members
Arlene Heins
Genie Rogers
Jolene Schulz
Larry Swindle
Nancy Thomas
Becky Willard