












Breastcancer researchers and cli nicians have made tremendous progress in reducing death rates in the past three decades, yet a racial gap persists in the United States.
Even with the lower numbers of actual disease compared to white patients, Black women are still much more likely to die from the disease.
The American Cancer Society highlights these disparities in a new report.
“We found that despite contin ued progress in reducing the risk of death from breast cancer, there is an alarming persistent gap for Black women, who have a 40% higher risk of dying from breast cancer than white women despite lower inci dence. This is not new, and it is not explained by more aggressive can cer,” said report co-author Rebecca Siegel, senior scientific director of surveillance research at the American Cancer Society.
“We have been reporting this same disparity year after year for a decade. It is time for health systems to take a hard look at how they are caring differently for Black women,” Siegel said in a cancer society news release.
While Black women have 127.8
cancer cases per 100,000, versus white women with 133.7 cases, they have 40% higher death rates, the report says.
Moreover, for every 19.7 white women per 100,000 who die of breast cancer, 27.6 per 100,000 Black women will die. Among women younger than 50, the death rate is twice as high for Black patients.
Black women remain the least likely of any racial or ethnic group to be diagnosed while their breast cancer is at a localized, more easily treated, stage — at 57% versus 68% in white women, researchers found. They also have the lowest five-year survival rate of any racial or ethnic group for all breast cancer subtypes and stages, except stage 1. The largest gaps were between stage 3 and stage 4.

Gaps also exist for American In dian and Alaska Native women, who are 17% less likely to be diagnosed with breast cancer than white wom en, but 4% more likely to die from the disease.
The U.S. death rate from breast cancer dropped by 43% overall between 1989 and 2020, with 460,000 fewer deaths. The cancer society attributed that to earlier detection
through screening, increased aware ness and advances in treatment.
That pace of decline has slowed. While death rates dropped about 1.9% annually from 2002 to 2011, they dropped 1.3% annually between 2011 and 2020. That may, in part, reflect increased incidence.
“The slow decline in breast can cer mortality during the most recent period partly reflects stagnant screen ing uptake and suboptimal receipt of timely and high-quality treatment,” said study co-author, physician Ahmedin Jemal, senior vice president of surveillance and health equity science for the cancer society.
Jemal called for coordinated and concerted efforts by policymakers, health care systems and providers to
deliver the best breast cancer care to all populations. This includes ex panding Medicaid in the non-expan sion Southern and Midwest states, where Black women are dispropor tionately represented, he said.
“Also, increased investment is needed for improved early detection methods and treatments,” Jemal said in the release.
Cancer advocates called on law makers to provide funding for the National Breast and Cervical Cancer Early Detection Program, a program jointly funded by federal and state governments that helps improve ac cess to lifesaving breast and cervical cancer screenings.
See how Excellus BlueCross BlueShield is bringing Medicare plans with lower costs and better benefits to people throughout our community. That way, everybody benefits.

• Preventive dental +$1,000 on all plans
• PPO plans available in all regions with access to doctors locally and nationwide
• $500 Flex Card on some plans for dental, hearing, and vision expenses
A nonprofit independent licensee of the Blue Cross Blue Shield Association. Excellus BlueCross BlueShield is a PPO and/or an HMO plan with a Medicare contract. Enrollment in Excellus BlueCross BlueShield depends on contract renewal. Our Health Plan complies with applicable Federal civil rights laws and does not discriminate on the basis of race, color, national origin, age, disability, or sex.
ATENCIÓN: si habla español, tiene a su disposición servicios gratuitos de asistencia lingüística. Llame al 1-877-883-9577 (TTY: 711).注 意:如果您使用繁體中文,您可以免費獲得語言援 助服務。請致電 1-877-883-9577 (TTY: 711)














Former TV newswoman and TODAY show anchor Katie Couric has breast cancer.

Couric shared that information late September on Instagram, while also releasing an essay about the experience on her media website.
“Every two minutes, a woman is diagnosed with breast cancer in the United States,” Couric wrote on Instagram. “On June 21st, I became one of them.”
Couric, 65, received her cancer diagnosis in June, had a lumpectomy on July 14 at NewYork-Presbyterian/Weill Cornell Medical Center and then began radiation treatments on Sept. 7, TODAY.com reported.
The anchor’s name is often associated with cancer awareness because her first husband, Jay Monahan, died from colon cancer at 42, when their children were young. Couric has long been a spokeswoman for getting colonoscopies to catch cancer early.
Couric wrote about sharing her cancer news with her daughters, Ellie, now 31, and Carrie, 26.
“Finally, four days after I was diagnosed, I FaceTimed each of them,” she wrote. “I tried to be as reassuring as Dr. Newman. Their faces froze in disbelief. Then shock. Then they began to cry. ‘Don’t worry,’ I told Carrie then Ellie, ‘I’m going to be fine,’ trying to convince myself as well as them.”
“They’d already lost one parent. The idea of losing another was unfathomable,” she wrote.




Although Couric’s family has no history of breast cancer, the family has endured many cancer diagnoses and deaths. In addition to Monahan, Couric’s sister died at age 54 from pancreatic cancer. Her mother-inlaw died from ovarian cancer. Her parents also have a cancer history.
“Please get your annual mammogram,” she wrote. “I was six months late this time. I shudder to think what might have happened if I had put it off longer. But just as importantly, please find out if you need additional screening.”
Q: You’ve recently completed your fellowship at SUNY Upstate Medical Center, correct?
A: Yes, I completed it in the first quarter of this year. I did my internal medicine training at Upstate and then went on to do my fellowship there as well.
Q: What was that experience like?
A: It was a great experience. It’s the only academic center in Central New York. I had good training with great mentors throughout both my residency and fellowship.
Q: And you’re originally from the area?

A: I grew up just north of Syracuse in Cicero.
Q: Was the plan always to stay local or were you looking elsewhere in the country?
A: No, I was always planning to stay local, close to home.
Q: I don’t see the combination of D.O. and oncology that often. It’s mostly in primary care?








A: I think a lot of people are still somewhat confused about what a D.O. is. There are a few of us at Hematology Oncology Associates who are D.O.s [doctor of osteopathic medicine], so it’s not too uncommon. But there aren’t as many of us as M.D.s. Osteopathic schools are pretty much the same as M.D. schools, but the focus is a little more holistic, which may entice someone more toward a primary care path. But I think oncology can be quite a holistic specialty as well. My training
swing me away from oncology and, if anything, I think it helped the foundation of me choosing that specialty.
Q: What would you consider to be a holistic approach to oncology?
A: Basically the holistic approach is mind, body and spirit. I think that’s particularly important for someone who is facing a cancer diagnosis. It’s not just about being diagnosed with a disease and treating it. It’s all-encompassing. There’s a lot of emotional support that’s needed. All of the support services that go along with it. Nutrition is vital. Family support is important as well. So a very well-rounded approach to their care is vital.
Q: You’ve also worked as an internist.
A: I worked as a nocturnist. I always loved internal medicine, but it was always a stepping stone to oncology for me. It was a chance I had to work as internist, and something I thoroughly enjoyed.
Q: What will you be doing at your new position with HOA?

A: I just joined with HOA last month. I’ve known a lot of these providers for many years. It’s a pretty small town, so we interacted with each other a lot during fellowship. I’ve developed relationships with them over the years. I’m a general hematology oncologist so I’ll be seeing patients with a variety of blood disorders as well as cancers. I don’t have a particular sub-specialty. That may change over time, but I’m happy to see any patients in need of my specialty. I truly enjoy seeing all of the potential disease processes and keeping all that knowledge fresh.



Q: Under what conditions might a patient be referred to you?

A: You can think of hematology and oncology as two separate things. There are a lot of benign blood disorders that someone might be referred for. Say if they develop anemia or some other issue with their blood count that their primary care physician has identified. And, of course, there’s the malignant disorders you’d generally associate with cancer. So if the primary care physician ordered a screening test, for example, or they’re sent our way when a patient becomes symptomatic.
Q: How has oncology changed over the course of your training? Has anything
Jill Yeager, a medical oncologist and hematologist, has recently joined Hematology-Oncology Associates of CNY (HOA) in Syracuse. A native of Central New York, she is board-certified in internal medicine, and a graduate of Lake Erie College of Osteopathic Medicine in Erie, Pennsylvania. She completed an internal medicine residency, serving as chief resident, and specialty training (fellowship) in hematology and oncology at SUNY Upstate Medical Center. While completing her training, Yeager also worked as a hospitalist at Crouse Hospital and the VA Medical Center in Syracuse.
surprised you or changed your philosophy?
A: The time I was in training was both exciting and challenging, because it was hard to keep up. So here you are as someone who is training to learn about oncology but it changes day to day almost. So it’s a lot to keep up with, but it’s all good things and advances in the field. Definitely the advances that we’ve made in immunotherapy or molecular targeted treatment have made leaps and bounds over the last decade or so.
Q: Aside from receiving timely treatment, what are the most important factors in cancer survivability?

A: It’s a difficult question to answer because it’s very specific to the disease. We talk about cancer as though it’s a single disease, but it’s really a lot of different similar diseases. But they can be very different in how they behave. Catching them early is the most important thing. That’s why we talk about the importance of screening exams. That’s really the best way to avoid having a cancer that becomes difficult to treat.
Q: What attracted you to HOA in particular?
A: It’s been for a long time. It’s got a really solid foundation with a hardworking staff that are there day in and out taking care of patients. Even though patients are generally coming in for sad reasons, there’s so much camaraderie amongst the staff. I think that’s evident in anyone you speak to at HOA. We’re there to give the best care we can to patients. That’s something I saw before I joined and something I continue to see now that I have.
Q: Have you started seeing patients yet?



A: Yes, I have.

Name: Jill Yeager, D.O.















Position: Hematologist and medical oncologist at Hematology-Oncology Associates of CNY (HOA)







































Hometown: Cicero, New York
Education: Lake Erie College of Osteopathic Medicine







Affiliations: : Crouse Hospital; St. Joseph’s


Organizations: American Society of Clinical Oncology; American Society of Hematology, American College of Physicians

Family: Husband, two sons
Hobbies: Hiking, traveling, cooking, reading
New oncologist and hematologist at Hematology-Oncology Associates, who grew up in Cicero, discusses her training and the importance of a holistic oncology approach to treating cancer
Jill Yeager, D.O.

cerning



U.S.

cials reported in October.

About 2.5 million middle school and high school students reported that they had vaped in the past 30 days in 2022, according to new data from the U.S. Centers for Disease Control and Prevention and the U.S. Food and Drug Administration.



That was 14.1% of high school students and 3.3% of those in middle school.
“This study shows that our nation’s youth continue to be enticed and hooked by an expanding variety of e-cigarette brands delivering flavored nicotine,” said Deirdre Lawrence Kittner, director of the CDC’s Office on Smoking and Health.

“Our work is far from over,” Kittner said in a CDC news release. “It’s critical that we work together to prevent youth from starting to use any tobacco product — including e-cigarettes — and help all youth who do use them to quit.”
The findings are from the National Youth Tobacco Survey, conducted among U.S. students in 6th through 12th grades between Jan. 18 and May 31. They were published Oct. 6 in the CDC publication Morbidity and Mortality Weekly Report.







Among the youth who vape,



about 85% used flavored e-cigarettes. The brands they used were Puff Bar, with 14.5% calling it their usual brand, Vuse at 12.5%, Hyde at 5.5% and SMOK at 4%. More than half used disposable e-cigarettes. Most used flavors were fruit at 69.1%, candy or desserts at 38.3%, mint at 29.4% and menthol at 26.6%.
About 27.6% of youth who vape did so daily. About 42.3% vaped on 20 or more of the past 30 days.
E-cigarettes contain nicotine, which is addictive and can harm the developing adolescent brain, the CDC said. It may also increase risk for future addiction to other drugs. E-cigarettes have been the most popular tobacco product for U.S. youths since 2014.
“Adolescent e-cigarette use in the United States remains at concerning levels, and poses a serious public health risk to our nation’s youth,” said Brian King, director of the FDA’s Center for Tobacco Products.

“Together with the CDC, protecting our nation’s youth from the dangers of tobacco products — including e-cigarettes — remains among the FDA’s highest priorities, and we are committed to combatting this issue with the breadth of our regulatory authorities,” he said in the release.

With the growing popularity of electric scooters, the number of kids injured while riding them has jumped dramatically, a new study finds.
Moreover, those injuries have become more severe: In the past decade, the number of patients admitted to hospitals after an e-scooter accident rose from one in 20 to one in eight.
The findings beg the question of whether young kids should be using e-scooters at all.
Often regulations about their use are left up to local areas and, in many places, no regulations exist and no training on their use is required, the investigators said.
“The regulations surrounding the use of these scooters vary widely across the country,” said lead re-
searcher, physician Harrison Hayward, an emergency medicine fellow at Children’s National Hospital in Washington, D.C.
According to the American Academy of Pediatrics, children under 16 should not operate or ride on e-scooters. Yet, the average age of patients in this study was 11.
For the study, Hayward’s team collected data on nearly 1,500 e-scooter injuries reported to a national database of pediatric injuries from 100 hospitals. The investigators found that over 10% of the patients had a head injury, including concussions, skull fractures and internal bleeding. Broken arms were the most common injury (27%), followed by minor abrasions (22%) and lacerations that needed stitches (17%).
The number of patients admitted
to a hospital jumped from just over 4% in 2011 to nearly 13% in 2020, the researchers noted.
Hayward added that the majority of e-scooter crashes involve running into an object, like a lamppost or hitting a pothole or a pedestrian. But collisions with cars have also been reported, he said.
Often, the youngest kids injured are riding the scooter with an adult, Hayward noted. “We did a study where we looked for levels of injuries among 4-year-olds,” he said. “For a pretty surprising proportion, they were actually on the scooter with another older person.”
Hayward said that only one person should be riding the scooter and they should be wearing a helmet and traveling in a bicycle lane.
Pam Shadel Fischer, senior director of external engagement at the Governors Highway Safety Association, said that “anybody who’s too young to have a driver’s license should not operate or ride on an electric or motorized scooter.”
Helmets are essential when
riding a scooter, she added. “I don’t disagree with those who say, helmets don’t cause crashes,” she said. “But lack of helmets definitely causes some of the injuries that people sustain.”
These scooters were not designed to be ridden on sidewalks, but rather on bike paths and roads. In many places, regulations require that these scooters not be used on sidewalks, Shadel Fischer said.
She believes that state legislatures need to regulate the use of these scooters by setting age limits and putting them in the same class of transportation as bicycles.
It’s also up to parents to ensure that their young kids aren’t using e-scooters.
The findings were presented in October at the American Academy of Pediatrics annual meeting in Anaheim, California. Findings presented at medical meetings are considered preliminary until published in a peer-reviewed journal.
Last year, we spent $603 billion on drugs. That’s about $1,800 per person in the US. Half of the $603 billion was spent on specialty drugs alone. Soaring prices, not increased utilization, drove up the overall drug spending. Specialty drug prices have increased a staggering 43% over the last five years. To reign in drug costs, the Inflation Reduction Act caps all Medicare Part D drug price increases at the inflation rate and out-ofpocket spending for Medicare members is limited to $2,000 annually. This went
The 88 Catholic hospital system lost $1.4 billion in the fiscal year just ended June 30.
St. Joseph’s in Syracuse and St. Peter’s in Albany are local members. Two other national Catholic hospital systems, CommonSpirit and Ascension (Lourdes in Binghamton), lost almost $2 billion each. Deficits were attributable to declining revenues and significant contract labor (mostly nursing) costs. In fairness to hospitals, their fees are either predetermined by Medicare and Medicaid or predetermined with commercial insurers. So, unlike drug manufacturers, they cannot arbitrarily raise prices to increase revenues.
Large national hospital systems have not fared much better than smaller local or regional hospital systems. Industry observers have speculated that the smaller systems (comprised of “across the street mergers”) may be more efficient because their proximity allows them to share clinical staff, consolidate overhead, and merge departments.
Industry experts Kaufman and Hall don’t see things improving for hospitals through next year. If hospitals continue to lose money, they will
into effect Oct. 1, 2022. In addition, Medicare will finally be allowed to negotiate a handful of drug prices — but not until 2026. Seemingly in anticipation of prices being controlled by Medicare, drug manufacturers increased the prices of some 1,200 products an average 31.6% from July 2021 to July 2022. In the meantime, physicians are lobbying Congress not to cut their payments by almost 5% next year. With inflation at 8%, the 5% cut is tantamount to a 13% decrease in reimbursement.
be forced to make painful staff cuts, mostly in non-clinical areas, to keep their doors open.

You are eligible for Medicare the month you turn 65. Open enrollment, which began this Oct. 15, allows people to change their plan for 2023.
Medicare anticipates the trend to enroll in Advantage plans will continue with 32 million seniors, or more than half of all eligible seniors, enrolling. Advantage plans are operated by commercial carries like United, Humana, Aetna, Blues, Cigna and Anthem. As the popularity of Advantage plans grows, so do the markets served by the carriers. These plans offer more services than traditional Medicare, often for no additional cost, such as dental, vision, hearing, transportation and even meals.
Incredibly, Advantage Plan premiums are expected to decrease 8% in 2023. Open enrollment for the Affordable Care Act and most employer plans began Nov. 1. The Kaiser Family Foundation estimates ACA premiums will increase 10% and commercial-employer premiums about 7%.
Prior to the pandemic, 11% of adults suffered from depression and anxiety. Since the pandemic, it is up to 40% of adults.
As the stigmatization associated with mental health declines, more and more people are seeking treatment. But therapists are struggling to keep pace and meet the demand.
Adding to the problem, since 2011, the number of practicing psychiatrists (MDs) has declined 6%. Most don’t accept Medicare and many don’t accept any insurance. Psychiatric nurse practitioners are increasingly critical in providing mental health services. Their numbers have increased 162% since 2011. Since then, NPs have provided 30% of all mental health visits. Start-up companies are assisting these NPs with establishing and running their private practices by lowering overhead and billing costs and contracting with both Medicare and commercial insurers.
Consumer surveys reveal 70% of respondents worry about their mental health coverage. Many plans still restrict coverage or have expensive copays.
A survey of 8,000 adults by the Commonwealth Fund revealed insurance does not provide enough financial protection against rising healthcare costs.
43% of those surveyed were inadequately covered and 9% had no coverage. 29% of those with employer sponsored insurance and 43% of those with individual insurance were underinsured because of high outof-pocket expenses like deductibles and copays. Underinsured is defined as spending more than 10% of your income on out-of-pocket costs. 50% of those surveyed said they could not pay an unexpected medical bill of $1,000 within 30 days. Pollsters West
Health Gallup asked 5,000 adults to grade US healthcare for affordability, equity, accessibility, and quality. 44% of respondents graded US healthcare “F” and 33% graded it “D.” Only 22% of those taking the poll rated US healthcare either “A” or “B.”
Virtual care was growing VERY slowly in the several years prior to the pandemic.
The technology was there, but the acceptance by both providers and consumers was not.
The pandemic caused virtual care, by necessity, to rapidly proliferate. It is now widely accepted by insurers, providers and consumers and it is integral to healthcare access and delivery.
The Massachusetts Blues have teamed up with the Carbon and Firefly healthcare systems to offer their members virtual primary and mental health care by early 2023. The Blues are touting better outcomes, easier access, lower costs, less anxiety and improved outcomes. There will be no copays. You will be able to access your provider via laptop, desktop or phone. In addition to no commuting, waiting times will be minimal. There will be wellness coaching and support and specialists will be engaged, as necessary. The Blues will also provide free medical devices, such as blood pressure monitoring, to its members. United Healthcare, Aetna and Cigna are all considering similar products.
George W. Chapman is a healthcare business consultant who works exclusively with physicians, hospitals and healthcare organizations. He operates GW Chapman Consulting based in Syracuse. Email him at gwc@gwchapmanconsulting.com.









CEO of ICAN discusses how the nonprofit helps families stay together — it works with adults and children who have service needs
By David PodosQ: I understand that ICAN (Integrative Community Alternatives Network) has many programs available. What are some of your main services?
A: The agency presently offers more than 20 programs. One of our flagship services is to offer in-home care through intensive supports to families and their children where the kids are at risk for out-of-home placement because of behavioral and or mental health reasons. So, for example, we wrap services around those families be it mentoring and behavioral health management, psychiatry or individual therapy. We actually provide more than 50 services in just that one program alone to help prevent a family’s child from going out of home care, keeping them home, and to be successful.
Q: Why is it so important to treat a child at home rather than for instance at a child rehab center?




A: All the research shows, from the late 1990s to today, that kids receive the best quality of care and have the best long-term outcomes
when they are being provided services at home and in their community. So, if we as an agency can bring everything to them that they would receive in a residential setting allowing them not only to stay in their homes, but allowing them to stay in their communities, stay in their school system, be on a sports team, be with their peers, that is a win-win situation for them, their families and the community as a whole.
Q: Is this model of home service delivery that you provide for children offered to your adult clientele as well?
A: Actually, yes, we do have a similar model, and that is through our adult health/home care management program. These clients, like our kids we serve at home, are also in need of mental health and behavioral health interventions and treatment.
Q: What other care needs do you see in your adult program that has to be addressed?
A: Many of our adult clients have co-occurring needs such as physical





health issues, as well as support for drug addiction for example. So we seek out and provide the best services for them for those issues. Like our kids’ program, we strive to get our adult clients the best care possible, using wrap-around services this way we can do our best to keep them out of un-necessary psychiatric hospitalizations, and or emergency room usage, basically just allowing them to stay at home with their loved ones during their recovery.
Q: Even though statistics show that teen pregnancy has been on the decline for the past several decades, America still has the highest teen pregnancy rates among all other developed nations. Does ICAN o er any programs that deal directly with this problem?


A: In 2013 the Family Nurturing Center here in Utica was offering phenomenal services including addressing the problems of teen pregnancy. We had the opportunity to bring all their employees as well as their services and programs over to the ICAN umbrella so now we can offer help in that area. One of our programs that works with young mothers is called Healthy Families. We work with the family and the young mother who is either expecting or recently had a newborn. We help them with any skills they might need to assist them to become the most productive parent possible.
In regards to teen pregnancy, we are very proud to have a program called Evelyn’s House. That program is a home for pregnant and or parenting teen moms and their babies. So, we have this wonderful place for young mothers who may not have a place to go to, they may be homeless or on the verge of homelessness, they can come and stay at Evelyn’s house where we will provide a roof over their heads, making sure they are receiving all the needed pre natal care and all the nutrition for their baby.
Q: How many sta does ICAN employ?
A: We currently have 190 staff, which is a mix of full-time as well as part-time employees. In addition, we have a sub-contractor provider network of behavioral health professionals. There are 250 health care professionals in that network which can provide us, (our clients) with direct care.
Q: What is your annual operational budget for 2022?
A: Our budget for 2022 is just over $20 million.
Q: Where does ICAN receive its funding from?
A: We have a number of different revenue sources. First, we are very fortunate to receive funding from each county that we provide our services, which includes Oneida, Herkimer and Otsego counties. We also have state as well as federal dollars that support us, along with Medicaid funded services, and a number of insurance reimbursements.
Q: What has been your biggest challenge?
A: Keeping up with the high demand for our services.

Q: What number can people call to get more information and what is your website?
A: Our phone number is- 315 -792-9039. Website is ICAN.family


Your fondness for midnight snacks has caused you to pack on the pounds over the years, and now researchers have a better understanding of why.

While late-night eating has long been linked with an increased risk for obesity, researchers weren’t sure exactly how it caused weight gain until now.
“When meals are delayed by four hours and everything else stays the same, you burn fewer calories, have an increased drive for food, and experience changes in fat tissue that would promote weight gain,” said study author Frank Scheer. He’s the director of the medical chronobiology program at Brigham and Women’s Hospital in Boston and a professor at Harvard Medical School.
The solution? Eat earlier in the day, he said.
“The new data suggest, together with the literature, eating earlier in the waking day results in changes in physiology that would promote weight loss and limit weight gain,” Scheer said.
For the study, 16 people who were overweight or obese stuck to a strict early and late meal schedule for one day each in a lab. In the weeks before each experiment, folks maintained fixed sleep schedules. They also ate identical diets and stuck to the same meal times at home.
The participants reported on their hunger and appetite, provided blood samples throughout the day, and had their body temperature and calorie use measured. Researchers also collected samples of fat tissue.
Due to the study’s design, researchers were able to tightly control for exercise, sleep and light exposure, which could affect how many calories participants burned.


More research is needed to see if these findings hold in real life, Scheer said.

“In the real world, when people change meal times, they may also change other behaviors such as timing or quality or time of sleep or how much they exercise, which could affect weight,” he said.
The study was published Oct. 4 in the journal Cell Metabolism.

Ifyou are facing Thanksgiving alone for the first time, you may be anticipating a lonely and depressing fourth Thursday of November.

But it doesn’t have to be so.
Whether you’re divorced, widowed or just can’t make it home for Thanksgiving, this family-centered holiday can be an opportunity for personal growth and expression. Plus some fun, too!
Below are some tips and creative ways to manage and embrace what can be a challenging day in the life of those alone this time of year.
• Be thankful — And why not start with yourself? Consider making a list of all the things you are thankful for this year: Your health? Your children? Good friends who have stood by you through thick and thin? A career or volunteer job you love? A beloved pet? Or perhaps even this opportunity now to experiment and learn new things about yourself?
• Take the long view — While you may be alone this year, it doesn’t mean you’ll be dining solo on leftover turkey the rest of your life. This one day doesn’t dictate your destiny.
Who knows what the future holds? Over the next year, you may meet someone special or achieve a measure of inner peace and confidence that enables you to enjoy a holiday on your own or with a “family of friends.”
• Do good — Helping others this time of year can take your mind off
being alone and give you something worthwhile to do. Shelters and food kitchens often welcome volunteers, but, truth is, many of these agencies fill up fast with regular volunteers. You may need to plan and be creative.
As an alternative, many local YMCAs host Turkey Trots and need volunteers to register and cheer on runners of all ages. Instead of serving stuffing at the shelter, you could be serving up smiles at the finish line.
• Throw your own little holiday dinner for fellow “strays” or “untethered” friends — Have some fun! It doesn’t need to be elaborate or even planned far in advance. Sometimes last-minute dinner invitations can turn into the best, most memorable get-togethers.
Chances are you know others who may be alone this Thanksgiving. Extend a warm invitation and invite your guests to bring along a beverage or holiday side-dish to pass. This gives everyone a chance to make a meaningful (and delicious!) contribution.
• Beware of “euphoric recall” — When you are feeling lonely, it can
be easy to glorify the past. Did last year’s Thanksgiving live up to the Norman Rockwell ideal? Or did all the bickering, bad blood, and woozy, overstuffed relatives make you want to run for the hills? Maybe, just maybe, being with your own good company is a blessing.
• Rent a movie and indulge in a tasty guilty pleasure — Oh, why not? Rent a favorite “feel good” film and make a night of it. You might check out “Tootsie” or “On Golden Pond,” two of my favorite oldies, which never fail to warm my heart.

Or find a new movie you haven’t seen and enjoy the novelty of seeing something for the first time. Top it off with a favorite treat. I love everything pumpkin this time of year: pumpkin soup, pie, ice cream and fry cakes!
• Pick up the phone — I’ve modified one of Abe Lincoln’s famous quotes for my own purposes: "Folks are usually about as lonely as they make up their minds to be." The difference between isolation and engagement can be as simple as sending a text or dialing a seven-digit phone number.
My experience happily tells me that most folks welcome a call on Thanksgiving. Why not pick up the phone to connect with out-of-town friends and family members? Catch up and make their day, as well as yours, a little richer.
Or connect locally with a neighbor or friend with an invitation to go for a walk around the block or see a matinee while the turkey is in the oven. Many folks welcome the diversion and chance to get out of the kitchen before or after the big feast.
• Decorate your home inside and out. — Do it for you. It may help put you in the spirit of the holiday. This past weekend, I recreated my annual stacked-pumpkin display for my front porch. It gives me a warm feeling every time I pull up to the house.
Add harvest accents to your

home and feel the essence of Thanksgiving in your heart.
• Nurture yourself — On your own, Thanksgiving can be a great day to do whatever you enjoy doing. Carve out well-deserved time to read, do some early online shopping for the holidays, give yourself a manicure or whatever tickles your fancy.
On Thanksgiving Day, I plan to nurture myself with a solo walk in the woods, where I find peace and feel connected to all living things: trees, birds, critters and insects — even creatures I can’t see within the ponds, underground and in the sky.
I never feel alone when I’m in nature and use the time alone to count my blessings and be grateful.
So pamper yourself for at least 30 minutes and take a mini-vacation from your worries, doubts and fears. Then seize the day with a renewed outlook on life.
• Write “thank you” notes — Now here’s an idea that’s so obvious it often gets overlooked on Thanksgiving. “Build bridges the rest of the year, and cross them during the holidays,” said Craig Ellison, PhD, author of “Saying Goodbye to Loneliness and Finding Intimacy.” If you can’t be with friends or family this holiday, pick up a pen and thank them for their support and friendship.
Who wouldn’t love to receive a hand-written card after Thanksgiving that begins, “I’m sitting here on Thanksgiving morning thinking of you. On this day of thanks, I can’t help but be thankful for our (fill in the blank).”
In preparation for this kind gesture, purchase cards and stamps in advance.
There you have it: Survival tips for a single-serving Turkey Day. The good news? It will be Friday before you know it and you can look back and be proud of yourself for rising to the occasion and treating yourself to big helping of joy and gratitude this Thanksgiving.
Playing sports can benefit children in many ways, but all sports are not equal when it comes to their bones.
New research suggests children will have healthier bones if they participate in multidirectional sports such as soccer or basketball, rather than unidirectional activities such as running.

Mixing it up a bit with a variety of sports instead of focusing on just one is also less likely to lead to overuse injuries, the researchers noted.
“Our data shows that playing multidirectional sports when younger versus specializing in one sport, such as running, decreased a per-
son’s bone injury risk by developing a bigger, stronger skeleton,” said study author Stuart Warden. He is associate dean of research and professor of health and human sciences at Indiana University-Purdue University Indianapolis.

“There is a common misperception that kids need to specialize in a single sport to succeed at higher levels,” Warden said. “However, recent data indicate that athletes who specialize at a young age are at a greater risk of an overuse injury and are less likely to progress to higher levels of competition.”
While researchers have traditionally looked at bone mass to
determine skeleton health, previous studies by Warden’s team have found that bone mass and size are equally important.
For this study, they used high-resolution imaging to examine bones in the shins and feet of women who compete in college cross-country running. These athletes often suffer bone stress injuries, such as stress fractures.
The investigators found that the women who participated in both running and multidirectional sports when younger had 10% to 20% greater bone strength compared to their counterparts who only ran.
In addition, those who had played sports like soccer or basketball when younger had better bone structure and strength than those who solely ran, swam or cycled, the scans revealed.
“We want to ensure people have better, stronger bones as they grow, become adolescents and go through life,” Warden said in a university news release. “Specializing in one sport at too young of an age means they are more likely to get injured and not make it at the collegiate and professional levels.”
Athletes should be given time to allow for proper growth and development, not specializing until at least their freshman year of high school, Warden advised.
Those who already play multiple sports should take time off for rest and recovery during the year, he added. This can improve both bone strength and performance.
The findings were recently published in the journal Medicine and Science in Sports and Exercise.

‘Next to Normal’ is one of these dark rock musicals that show a normal family mentally falling apart after the loss of their son
By Daniel BaldwinNext to Normal” was the first musical that Ilion resident Justin Jones directed and he feels it’s special.
“It’s one of my favorite shows,” Jones said. “It has a beautiful touching (musical) score and beau tiful touching script. It’s a show that audiences are going to be affected by. I think theater is best when people are affected either in a positive way or they learn and feel something by watching the show. I think it’s a show that should be done more often.”
“Next to Normal” is one of these dark rock musicals that show a normal family mentally falling apart after the loss of their son. The moth er of the family (Diana Goodman) cannot move on from her son’s death and has bipolar disorder. The hus band (Dan Goodman) tries to help Diana with her condition, but actual ly worsens it. The daughter (Natalie Goodman) is mad at her parents over this issue and becomes a drug addict.
“Next to Normal” shows how complex the family’s problems are and how one solution, to these is sues, will not fix everything or make everyone happy.

All the treatment, therapies and pills in the world could not erase the memories Diana has of losing her son. These problems take a toll on each family member’s mental health. By no means does this musical end on a happy note. The ending is sad and more grounded in reality.
“Next to Normal” won the 2010
Pulitzer Prize, according to Mu sic Theatre International’s website (Mtishows.com). It also won three Tony Awards in 2009. This musical is based on the book written by Brian Yorkey. The songs were written by Tom Kitt.
Jones was interested in this dark mental health-focused story. The story was what inspired him to direct this play.
“The reason I chose this show is because it does hit a lot of mental health issues,” Jones said. “Even though there are more conversations going on now, there’s not enough real conversation of the situations that people go through. How maybe one way to overcome it, isn’t the best for everybody. The different per spectives in which people can look at a situation. There’s no villain to this storyline. Everyone’s doing the best they can, what they think is the right thing and sometimes that’s not always the best for everyone in this situation.”
Jones directed and worked on this musical last July and August at the Rome Community Theater in Rome. He worked with the local actors and Rome Community Theater members. He helped these actors get into character. He did whatever he could to put on the best musical the Mohawk Valley has ever seen, he said.
The cast got along just fine with Jones and loved working with him.
“Justin Jones has been one of
my best friends for God knows how long,” said Shane Archer Reed, the actor who played Dan Goodman. “I will work with him anytime he asks me to. He’s a visionary. He’s the kind of director who’s willing to take risk and who’s willing to let his actors discover their character in their own way. He made us all come together in the best way possible. I love working with him. I will do it anytime.”
Jessica Sargent-Wilk played Diana. She is another local actor who loved working with Jones.
“I cannot even tell you how well he (Justin Jones) worked with the actors and team here,” Sargent-Wilk said. “Everything he had to get done, along with working full time. Every single ensemble member pulled their weight and was such a huge part of the team. Due to the pandemic, mental illness has gotten worse and worse, so we felt like this was really the best time to tell this story, and we’re so lucky that Justin was there for us and wanted to do that here. I literally can’t wait to do another play with Justin.”
Thesuicide rate in the Unit ed States increased in 2021, following two years of decline, according to preliminary data from the U.S. Centers for Disease Control and Prevention.
The number of suicides increased to 47,646 in 2021, up from 45,979 in 2020, according to researchers at the CDC’s Nation al Center for Health Statistics.
As a result, the U.S. sui cide rate also increased to 14 sui cides for every 100,000 people, up from 13.5 per 100,000 in 2020, according to data published in the CDC’s Vital Statistics Rapid Release.
However, the numbers from 2021 remain lower than the peak set in 2018, suicide preven tion experts noted.
Still, “the uptick is certainly concerning,” said Colleen Carr, director of the National Action Alliance for Suicide Prevention. “It reinforces that we need to continue to invest in suicide prevention and a comprehensive approach to suicide prevention.”
Suicide rates rose by 30% in the United States between 2000 and 2018, before declining in 2019 and 2020.
In July, the U.S. Department of Health and Human Services launched a national crisis line, and the new numbers appear to support the need for it.
People contemplating suicide or suffering a mental health or substance abuse crisis now can call 988 for immediate counseling, much as 911 is now used to report a physical emer gency.
Also putting mental health in the spotlight, the U.S. Preventive Services Task Force recommended last week that screening for anxiety be part of doctor visits.
The COVID-19 pandemic might have played a role in this increase in suicides for a couple of reasons, experts said.
“We have seen during the pandemic increased reports of mental health distress,” Carr said. “Any time that people are feeling more mental health distress, there also is a potential increase for suicide.”

In last month’s issue, we talked about coming to terms with a crappy childhood or an abusive marriage and how to overcome what you survived.
“Changing isn’t like changing clothes,” said one woman who survived an abusive childhood, then married an abusive man. She left him to begin the journey to reclaim her self. “It’s not easy, not easy at all.”
“You’re in a world of pain, but that pain will lessen,” she was quot ed in Ellen Bass’s book, “The Cour age to Heal.” “At the beginning, you can’t see that. You can only see your pain and you think it will never go away. But the nature of pain is that it changes. It changes as you work through it. One day, you wake up and realize that life isn’t just about working through your abuse; it’s about living, too.”
Often, the skills that helped us survive as an abused or neglected child or an abused woman don’t work so well when we’re adults.
From my own experiences and from working as a counselor with people that were hurting, here are a few things others found helpful.
Look it in the face and accept that things happened to you that weren’t OK. You don’t have to forgive anybody, just accept it. These things aren’t forgivable.
“Accept that you were a victim, that the abuse really did take place,” said Bass. “This is often difficult for survivors. When you’ve spent your life denying the reality of your abuse, when you don’t want it to be true, or when your family repeatedly calls you crazy or a liar; it can be hard to remain firm in the knowledge that you were abused.”
Acknowledge your pain, your anger and your grief. Allow yourself to feel. Allow yourself to feel all the feelings. Some days this won’t be easy. All your feelings are valid.
It can help to jot down your feelings; this can provide some sense of release. It can help to get your emotions out on paper.
Recognize how your pain, your anger, and your grief have affected you, affected your behavior and your relationships.
Then change your identity from being a victim to a survivor — one who overcame bad stuff and is now in charge of her life. This can make a huge difference in how you see yourself. See the many ways being a survivor has given you many good qualities.
Begin caring about yourself. Take care of yourself physically and emo tionally. Remind yourself that what happened to you is not your fault.
Treat yourself like you would treat a
is here. More of us will get colds, flu and viruses during winter months.
According to the CDC, viruses like colds, the flu and the highly transmissible coronavirus variant, omicron, start climbing in November and hit their peak between December and February.
Viruses that cause colds and the flu thrive in dry, cold conditions — coupled with the fact that our body’s ability to fight them is decreased.
These viruses tend to enter through our mouth and nose, which usually have strong defenses against viruses. The cold weather slows down these defenses. And, less sunlight and time outside means our bodies get less vitamin D, which is important to battle illnesses.
There’s no data to show that being chilled causes a cold, despite your grandmother’s warnings. Research showed the opposite: when people showered, got their hair wet, then stayed outside in the cold with wet hair, they didn’t get colds. It’s definitely a myth.
The common cold is caused by a viral infection of your nose and
throat, your upper respiratory tract. It’s usually harmless, though it might not feel like that. Many different viruses can cause a common cold.
The flu is caused by a flu virus.
Omicron and other variants of COVID-19 are also caused by viral infection, the coronavirus.
Germs is the catch-all term to describe bacteria or a virus.
Because these illnesses all have similar symptoms, it can be difficult to tell the difference between them. Specific testing is needed to confirm a diagnosis. Having a specific test allows you to get diagnosed and treated for the specific virus you have more quickly.
In general, flu symptoms are worse than the common cold and can include fever or feeling feverish/ chills, cough, sore throat, runny or stuffy nose, muscle or body aches, headaches and fatigue. Flu and COVID-19 can also have serious complications.
You’re leaving yourself open for a cold, flu or other upper respiratory virus if you’re doing any of these things.
good friend. Be gentle with yourself. Talk to yourself like you would talk with a good friend.
Stand up against any more abuse from anyone. Learn to be OK saying no.
I like this fable:
Once upon a time a woman who been a victim all her life moved to a cave to study with a guru. She want ed to learn how not to be a victim. The guru gave her stacks of books and left her alone to study them. Every morning, he came to monitor her progress, carrying a big wood en stick. He’d ask her: “Have you learned what you need to learn yet?” Every morning she answered “No, not yet,” and he struck her over the head with the big wooden stick.
This scenario repeated itself for several weeks. One morning the guru came into the cave and asked her the same question as he raised his stick, ready to strike her. This time, she grabbed the stick from him, stopping his assault in midair.
Relieved to end the daily beat ings but fearing retaliation, she looked at him. To her surprise, the guru smiled.
“Congratulations!” he said. “You now know everything you need to know.”
“How is that?” she asked.
“You’ve learned how to stop the pain,” he replied.
Stop the abuse; stop the pain.
Learning to trust others is another thing that’s hard for many victims. We build walls around our hearts to protect ourselves; we armor ourselves. But then we feel alone,
trapped behind these walls. That can be more painful than taking small risks to trust others.
Seek support from others. Find a support group, activity or hobby. A big part of the healing process is connecting to other people, so make the effort to develop relationships.
It can help to talk to a trusted family member, friend or counselor.
Replace bad habits with good ones. Bad habits can take many forms, like negativity and mistrust ing others, or turning to alcohol or drugs when feelings become too hard to bear. A support group or a therapist can help you learn the right tools. Consider joining a support group for survivors.
Celebrate your progress, no matter how small it may seem. It’s the little victories in your recovery that will eventually help you win the battle of healing your trauma.
• Not washing your hands thoroughly. If you do some kind of quick-splashing thing, followed by an “all done,” you are leaving yourself open for a cold or flu virus. Cold-causing viruses can live on your hands. Regular handwashing can help protect you from getting sick. Frequent, thorough handwash ing protects against a variety of illnesses, including colds, flu and COVID-19 variants.
Thorough means lathering up with running water and soap for at least 20 seconds, long enough to sing “Happy Birthday” twice.
If you’re not near a sink, an alcohol-based hand sanitizer is a runner-up.
• Touching your eyes, nose or mouth. Viruses enter your body when you touch your hands to your face. Your hands touch elevator buttons, door knobs, all the different places you go; viruses jump on your hands, then you touch your face many times a day, giving the viruses a free ticket right in to inflect you.
• Being around people who are sick Germs are how viruses are spread. Sick people can spread virus-contain ing germs when they cough, sneeze or blow their nose. Watch a sneeze in slow motion on YouTube; it gives you a sense of what happens and all the particles that are produced with a sneeze. And, stay home when you are sick.
• You didn’t get the flu shot and
Barbara Pierce is a retired licensed clinical social worker with many years of experience helping people. If you would like to purchase a copy of her book, “When You Come to the Edge: Aging” or if you have questions for her, contact her at barbarapierce06@yahoo.com.

COVID-19 booster.“Everybody, all ages, should get the flu shot,” said Nat Meks, pharmacist at Geneses Street Price Chopper in Utica. “And everybody should get the COVID-19 vaccination and boosters.”
There’s no cure for a cold. To feel better, you should get a lot of rest and drink plenty of fluids.
“We’ve got a variety of over-thecounter medicines for a cold and the flu,” said Meks.
Over-the-counter medicines may give you some relief from your symptoms, will help you feel better, but will not make your cold go away any faster.
If you’ve got the flu or a vari ant of COVID-19, stay home, rest, drink plenty of fluids, use over-thecounter medications to help you feel better and stop your cough. Sit in a steamy bathroom if you’re stuffed up. Antiviral medications will ease your symptoms and make your flu go away faster.
Antiviral medications and anti biotics are not at all the same. They aren’t interchangeable. Antibiotics don’t work for infections caused by a virus, such as colds, flu or variants of COVID-19.
Antibiotics don’t fight viruses; they fight bacteria. Using antibiotics for viruses can put you at risk of getting a bacterial infection that is resistant to antibiotic treatment.
Every early November, my family has the most absurd conversation. We talk about Thanksgiving sides as if they were open for discussion. Who are we trying to kid? Like most Americans, we would never switch up our cherished favorites—our beloved stuffing, mashed potatoes and green bean casserole. Thanksgiving is about peace and togetherness, after all, not acrimony and war!
Green bean casserole is our favorite and that’s because, of all the sides, the nutritional chops of green beans somehow justify all those tempting seconds and thirds.
Green beans pack a decent fiber punch, delivering about a fifth of our daily needs in one cooked cup. Fiber promotes regularity, ferries bad cholesterol out of our bodies and helps to stabilize blood sugars. What’s more, multiple studies suggest that increasing fiber reduces our risk of dying from heart disease, cancer, stroke and diabetes.
On the vitamin front, this tasty legume provides admirable amounts of vitamins K, C, A and folate. While vitamin K helps blood clot properly and maintain strong, healthy bones, vitamins C and A promote healthy immune systems, which is especially
important during flu and cold season. Folate, a critical B vitamin that prevents birth defects in newborns, also contributes to heart health by lowering an amino acid that can lead to hardening of the arteries.
Green beans are a good source of minerals, especially manganese. This essential mineral supports bone health, promotes wound healing, and has antioxidant abilities, much like vitamins C and A, that protect our bodies from disease and accelerated aging by neutralizing toxic free radicals.
A versatile bean that can be eaten raw or cooked, green beans are naturally low in fat, sodium, cholesterol, and calories: only 44 per cooked cup.
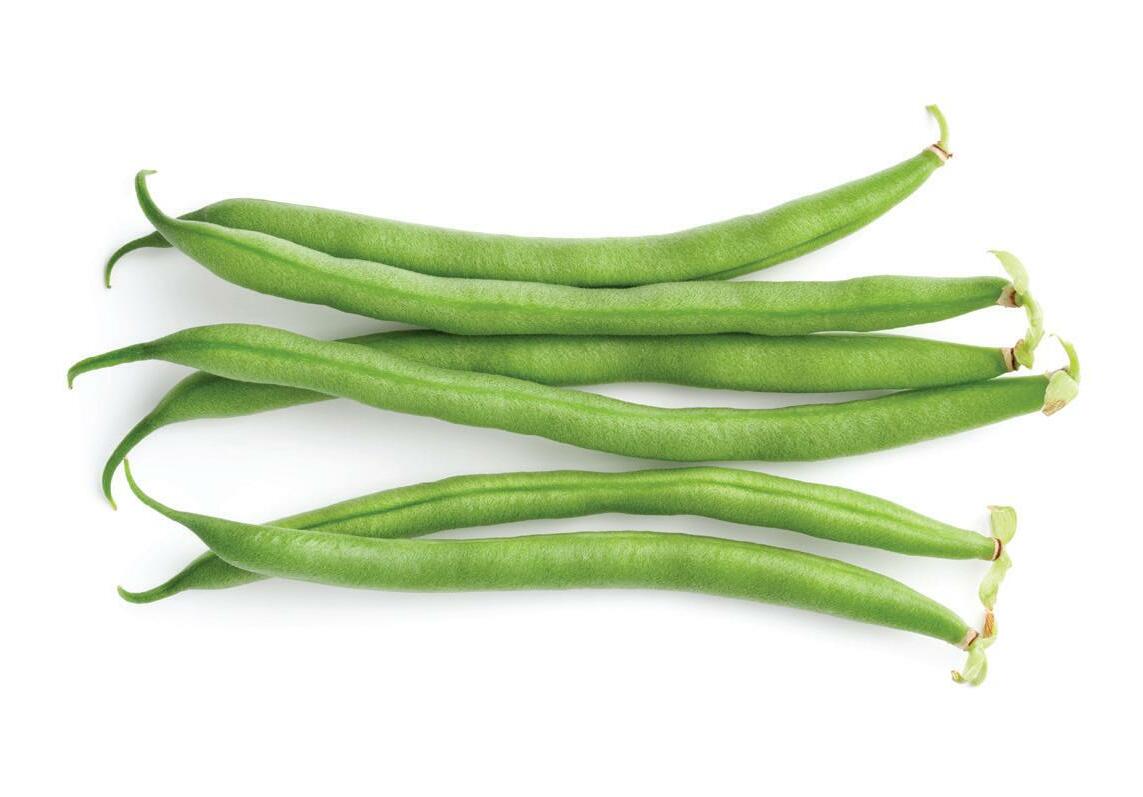
What’s more, fiber-rich beans take longer to digest, which helps us feel full longer, snack less, and maybe, just maybe, reach for only two helpings this Thanksgiving instead of three!
2 pounds fresh green beans
2 tablespoons butter, divided
1 cup shallots or onions, thinly sliced
½ cup whole-wheat panko breadcrumbs

¼ cup sliced almonds
1 pound mushrooms, sliced 3 garlic cloves, minced 2 tablespoons white whole-wheat flour
2 cups reduced-fat milk
2 vegetable bouillon cubes (or chicken)
1 teaspoon dried thyme ½ cup grated Parmesan cheese (optional)
Salt and pepper to taste
Preheat oven to 400 F.
Bring a large pot of water to a boil. Add the green beans and cook 3-4 minutes until bright green and tender crisp. Immediately add to an ice bath to stop the cooking. Strain and dry.
Melt 1 tablespoon of butter in a pan over medium heat. Add the shallots or onions and cook 5-7 minutes until tender. Transfer to a small bowl. Add the breadcrumbs to the
who drink two or three cups of coffee daily appear to live longer than people who don’t care for the beverage, new research shows.

Coffee lovers also seemed to have healthier hearts, which might contribute to the longevity boost, said the team of Australian investigators.
The findings were published Sept. 27 in the European Journal of Preventive Cardiology.

“Ground, instant and decaffeinated coffee were associated with equivalent reductions in the incidence of cardiovascular disease and death from cardiovascular disease or any cause,” study author physician Peter Kistler, of the Baker Heart and Diabetes Research Institute in Melbourne, said in a journal news release.
While other studies have suggested that the coffee habit might be a healthy one, Kistler’s team said there’s not been much investigation into the health effects of various forms of coffee.
To try to find out, they analyzed data from the ongoing UK Biobank database, looking at data on people aged 40 to 69. In this study, the average age was 58 and the Australian researchers focused on levels of daily coffee intake and life span, as well as heart disease, heart failure and stroke.
Overall, data on almost 450,000 Britons was included in the research. Regarding daily coffee intake, participants were divided into six groups: No coffee; less than a cup a day; one cup per day; two to three cups per day; four to five cups per day; and over five cups per day.


Purchase fresh when possible. Look for firm beans that are bright green and free of black spots. Fresh green beans should be refrigerated in a plastic bag and eaten within a week or less, since they lose their fresh flavor quickly. Since cooking green beans may cause a reduction in some nutrients, such as vitamin C, cook them for the least amount of time necessary, whether boiling, steaming, sautéing or roasting. Steaming beans is better than boiling, since it uses less water and prevents the beans from overcooking.
pan, toast for 1-2 minutes until light brown, and transfer to the cooked onions. Stir in the sliced almonds. Set aside.
Wipe out the pan with a paper towel. Add the remaining tablespoon of butter. Once melted, add the mushrooms and cook 6-8 minutes until tender. Add the garlic and cook 1 minute more. Add the flour, along with a splash of water, and stir well. Cook for 1 minute. Add the milk and bouillon cubes. Bring to a simmer and cook for 6-8 minutes, stirring often, until thick and creamy. Turn off the heat and stir in the thyme and Parmesan cheese (if using). Season with salt and pepper to taste.
Lightly oil a 9 x 13 inch baking pan. Add the green beans and mushroom gravy, Stir to combine. Top with the onion mixture.
Bake for 20-25 minutes until browned and bubbly.
Anne Palumbo is a lifestyle columnist, food guru, and seasoned cook, who has perfected the art of preparing nutritious, calorie-conscious dishes. She is hungry for your questions and comments about SmartBites, so be in touch with Anne at avpalumbo@aol.com.

 By Norah Machia
By Norah Machia
During the past year, the Upstate Golisano Children’s Hospital has seen a 17% increase in the number of autism patient appointments, a reflection of a nationwide trend.
In 2021, the Centers for Disease Control estimated that one in 44 children will be diagnosed with an autism spectrum disorder by the age of 8. That represents the highest rate since the federal agency began tracking cases in 2000.
The increasing number of cases is the result of “more awareness of autism spectrum disorder on two fronts,” said Henry Roane, Ph.D., division chief of the Center for Development, Behavior and Genetics at Upstate.
As a society, the discussions surrounding autism spectrum disorder have become more public, helping to reduce the stigma of seeking care and treatment, he said. In fact, “we’ve even had calls from adults who believe they may have gone undiagnosed as a child,” said Roane, who also serves as executive director of the Golisano Center for Special Needs.
Autism, or autism spectrum disorder, refers to a broad range of conditions characterized by challenges with social skills, repetitive behaviors, speech and nonverbal communication, according to the Autism Speaks organization.
“We know that there is not one autism but many subtypes, and each person with autism can have unique strengths and challenges,” the nonprofit agency states. Autism Speaks is both an autism advocacy group and the largest autism research organization in the United States.
“People have become more aware of autism spectrum disorder” as a result of an increasing number of movies and television shows focusing on children with autism and their families, Roane said.
While the increasing number
of autistic children’s portrayals is helping to create a better understanding of the condition, “sometimes those children with the most difficult behaviors are still not as readily accepted,” Roane said. Children with aggressive behavior, for example, are not typically the ones portrayed in the media, he noted.
“That type of awareness is really important for the population, and definitely helps with inclusion and acceptance,” he said. “But there are many children who have severe impairments, including cognitive and language, who also have autism. The media portrayals of these children are lacking.”
Parents of children with more challenging autism disorders, such as those who harm themselves or are not toilet trained “may feel left out of the discussion. That’s not their child on the television,” Roane said.
To help cope, parents of these children have often chosen to form their own support groups to help raise awareness of the “more severely impaired individuals with autism,” he said.
On a local level, the establishment of the Golisano Center for Special Needs in 2021 has also been a major factor contributing to the increase in autism patient appointments, Roane said.
The center provides comprehensive, coordinated and scientifically based medical and behavioral care for children and adolescents with many types of intellectual and developmental disabilities, according to Upstate Medical University. “The center acts as the umbrella, creating a framework to increase collaboration resulting in better patient care,” according to Upstate. “It helps to centralize programs and services available to this population.”
As a result of establishing the Center for Special Needs, which was supported through a major fund-raising campaign by the Upstate Foun-
dation, awareness has increased about the many different treatments and services available to autistic children and their families throughout Central New York, Roane said. It has also resulted in additional referrals from pediatricians in surrounding counties, particularly rural areas.
“The research is clear – the earlier you can start treatment for core symptoms, the better the outcome,” said Roane. “Two years of age is where you want to be for early intervention.”
Advances in medical research have allowed health care professionals to identify children with autism spectrum disorder at an even earlier age. “Now researchers are noticing low muscle control in infancy, how they move their eyes and other characteristics” that could indicate an autism case, he said. There is also experimental saliva testing being conducted as a way to help with diagnosis at an early age, he said.
Roane, a professor of pediatrics, is one of four experts who received grant funding from Autism Speaks to help improve the care provided to those with autism who experience severe behavioral challenges.

The grant funding is designed to collect and compile information nationwide about the current practices in identifying and handling challenging behavior from a wide variety of sources, including pediatric offices and specialized clinics.


The experts plan to analyze the information, including the outcome data, to determine the best care and treatment for these types of problem behaviors. A follow-up clinical trial will later be conducted to determine the success of these care and treatment approaches.
It was also recently announced that Upstate Golisano Children’s Hospital would join the Autism Care Network, a premier network focusing on improving the quality of health care children with autism and
their families.
Upstate will be joining 24 other hospitals nationwide in the network, which is supported by Autism Speaks, Roane said.
The partnership will be a valuable resource in helping to continually improve clinical care and quality of life for children with autism because it will allow health care professionals from throughout the country to share information about “what’s working in their clinics,” he said. “It will help to make our program even better,” Roane said.
• Upstate Golisano Center for Special Needs: 315-464-3555
• CNY chapter of the Autism Society of America: 315-447-4466
• Autism Speaks (Autism Response Team) 1-888-288-4762
Upstate Golisano Children’s Hospital has seen a 17% increase in number of appointments
“I really appreciate whoever’s in charge of this program” is how Gwen Stewart sums up her experience as a foster grandparent at The Neighborhood Center in Utica. “It’s a great program. I’m so glad to be here”
“I love it! I love being around the children,” agrees Cora Ceroc co, another foster grandparent at The Neighborhood Center. “I love helping the children, and seeing their smiles.”
“I like new experiences; I’d be bored at home” added Stewart “I like learning to know each kid each new year. Each one has a different person ality. I get to know all of them.”
“They tell us personal stuff; they know they can trust me,” said Ceroc co. “And they love hugs. One little girl was crying. I just held her and she calmed right down and stopped crying.”
“They’re both amazing” said Karen Kohl, child care supervisor of Stewart and Cerocco. “They come every day. That extra pair of hands assisting the teachers with the kids is so helpful.”
For five years, Cerocco has been a foster grandparent for infants and toddlers at The Neighborhood Cen ter; Stewart for three years, working with preschool children who are transitioning into kindergarten.

They’re in the foster grandparent program of Oneida, Herkimer, and Madison counties. Sponsored by Mohawk Valley Community Action Agency, it’s part of AmeriCorps, a network of national service programs that provide older Americans the opportunity to put their life experi ences to work for local communities. Foster grandparents serve as men
tors, tutors and caregivers for at-risk children and youth with special needs through a variety of commu nity organizations, including local elementary schools, Head Start and day-care centers.
The program gives people older than 55 to opportunity to share of themselves and their caring with special needs kids who face physical, mental social or emotional obstacles to learning. By giving the children one-to-one attention, they help the child overcome those obstacles.
“The foster grandparent program partners with schools, day care cen ters, and Head Start,” said program director Patti Demma, Mohawk Val ley Community Action Agency. “We look for volunteers, 55 and over, who meet eligibility requirements. Once they’re in our program, they start getting benefits, and are assigned to a classroom near their home.”
Benefits include a stipend of $3.15 per hour, paid leave of 78 hours every six months, travel reimburse ment and supplemental insurance. If they don’t have transportation to get to their classroom, we’ll help them get there, she added.
The foster grandparent program is open to people age 55 and older with limited incomes. All applicants undergo a background check and a telephone interview, as well as train ing and ongoing in-service training. Foster grandparents serve 15 to 40 hours a week.
“Each foster grandparent is assigned to a classroom,” explained Demma. “In their classroom, there will be two students they’ve been specifically assigned to, to do cer tain activities with that child. Each grandparent has two kids, though no
one knows this but the teacher and the grandparent. For example, the assignment may to read a book with that child twice a week. As they read, other kids will gather around. And that’s a good thing, so the target child will learn to socialize with others.”
“We have 33 foster grandparents in the Mohawk Valley,” said Dem ma. “We’re always looking for more. We’ll train you.”



“I’ve been a foster grandparent for seven years and look forward to continuing year after year,” said Pat Vandeusen, who works in an elementary school near her home in Nampa, Idaho. She’s well known in her community as an enthusiastic spokesperson for the program in her area, also under AmeriCorps.


“Being a foster grandparent is helping kids learn in school,” she added. “Often, they come from homes where the parents aren’t able to help their children with what they’re learning. Or the kids may have a learning disability.”
“As foster grandparents, we go into the classrooms, give individual encouragement, and help children develop the skills needed to learn.
We’re the ones who cheer them on!” she said.
Benefits of being a foster grand parent for her include the challenge of learning new skills, like new math, always helpful to an aging brain and making “precious friends” with other Foster Grandparents.
“We’re always looking for more foster grandparents,” said Kohl. “We value them so much.”
The foster grandparent program joins together two generations, older folks and kids. The program improves the quality of life for se niors, gives them a purpose and the opportunities to make friends. The presence of the foster grandparents gives parents and children an extra sense of security. The kids have a sta ble grandparent figure who mentors and encourages them in both social ization experiences and classroom activities. What a win-win situation for both the kids and their foster grandparents.
For more information on the foster grandparent program in the Mohawk Valley or to apply, call 315624-9930.


“I’m in good health, compared to most people my age. I’m able to keep active,” said 73-year-old Terry Leonard of Ilion. “I know a lot of people who’ve retired, only to sit back in their rocking chairs in front of the TV. I’m glad I’m not one of them. I’m very fortunate.”
Leonard is well-known in the area. In 2014, he became mayor of Ilion after retiring as director of Cath olic Charities of Herkimer County, where he worked for 22 years.
“I only wished I’d waited longer to retire from Catholic Charities. Work is good for older folks,” he added.
He’s absolutely right.
One of the most troubling findings about aging has to do with what happens to your health after you retire. According to the Nation al Institutes of Health, older adults greatly benefit in many ways from engaging in productive activities after retirement, part-time work or volunteer work. Research shows that, of those who retire to their rocking chair, more than 50% experience a significant drop in their health and well-being.
The positive influence of re
maining active as one ages “remains robust,” according to the NIH.gov online. That means the evidence to support these findings is strong and compelling.
ninety five-year-old Elaine Ciroc co of Port Charlotte, Florida, agrees. She has none of the frailties often associated with advanced age; her mind and body are strong.
“It’s because I worked until I was 90!” she claimed. “I owned a catering company in New Hampshire and kept working at it as long as I could. I was a widow and needed the mon ey. But it did benefit me in so many ways.”
As scientists evaluated retirees in terms of what happened to their health after retirement, scientists increasingly focused on social factors. They found that whether one is socially engaged with others or is isolated from others is an import ant factor. When people retire, they often have fewer group activities and fewer friends. And this can have pro found effects on health. Profoundly negative.
Remaining actively engaged with others is shown to be associated with less physical disability and better
 By Jim Miller
By Jim Miller
It definitely pays to know what charges to expect when pre-plan ning a funeral. Most people don’t have a clue and can often be upsold thousands of dollars’ worth of extra services they may not want or need.
Here’s a breakdown of what you can expect.
The first thing you need to be aware of is that funeral costs will vary considerably depending on your geographic location, the funeral home you choose and the funeral choices you make. With that said, here’s a breakdown of what an average funeral costs, nationwide, according to the most recent data from the National Funeral Directors Association.
• Professional services fee: This is a basic non-declinable fee that covers the funeral provider’s time, expertise and overhead: $2,300.
• Transfer of the remains: This is for picking up the body and taking it to the funeral home: $350
• Embalming and body preparation: Embalming is usually mandatory for open-casket viewing, otherwise it’s not required unless the body is going to be transported across state lines. Embalming costs $775. Other body
preparations, which includes hair dressing and cosmetics runs $275.
• Funeral viewing and ceremony: If the viewing and funeral ceremo ny is at the funeral home, you’ll be charged for use of the chapel and any necessary staff. Costs: $450 for view ing, and $515 for funeral ceremony.
• Metal casket: This is a big money maker for funeral homes, with mark ups of up to 300 percent over the wholesale price: $2,500.
• Funeral transportation: Use of hearse and driver; $325 to transport the body to the cemetery. Use of a service car or van: $150.
• Memorial printed package: This includes printed programs and me morial guest book: $183.
In addition to these costs, there are also a number of cemetery costs like the plot or mausoleum fee, the vault or grave liner that most ceme teries require, and the opening and closing of the grave, all of which can run between $2,000 and $3,000; and the gravestone, which typically runs between $1,000 and $3,000.
You’ll also need to budget for related expenses like flowers for the funeral ($200 to $400), the newspaper obituary fee ($100 to $800 or more), the clergy honorarium ($200 to $300) and extra copies of the death certif icate ($5 to $35 per copy depending
overall health. In addition, work is an effective way for older adults to prevent a decline in their cognitive abilities. Studies have shown that work that is complex has an espe cially positive impact, as building a higher level of cognitive reserve can help prevent or slow down the process of dementia and other brain damaging diseases.
For these reasons, many re searchers suggest that those thinking of retiring take time to prepare not only financially but also psycholog ically and socially. Those parts play much larger role in retirement than finances. Parts like how to not be bored out of your head due to lack of challenges. How not to become depressed and deteriorate physically and mentally because of reduced ac tivity, reduced social interaction and lack of a sense of purpose.
Plan what you’ll do with your time before you leave your job. When you’re working full time, there’s not usually time for hobbies or fun activities. Start thinking of what you might do.
“I get real antsy if I just sit around. I can’t do that,” Leonard agreed.
The great challenge is figuring out how to recover some of what you’ve lost in retirement — daily in teractions with colleagues and doing things you’re good at — and combine it with your newfound freedom.
Start by thinking about what you liked most about your job; situations where you felt you were doing well and were completely happy. How
can you begin to duplicate this in retirement? Many retirees work as a consultant, a free-lancer, or are self-employed.
To find well-being in later life, give yourself time to think of new purposes in life. Your hobbies, inter ests and passions are all still there. Embrace them! Instead of commut ing to an office, commute to your workbench or to a class at the local community college. Or join a sports club, religious organization, any kind of a group.
Find something that interests you and pursue it. Give yourself a reason to be eager to get out of bed in the morning. Whatever your interest, there’s probably a group of people with the same interest: historical societies, political groups, arts group and many more.
A significant pathway to a so cially connected, happy and healthy retirement is volunteer work. As a volunteer for Meals on Wheels of Herkimer County, Leonard has found this.
“I deal with people; I interact with the people on my route,” Leon ard said.
He works three hours a day, Monday through Friday.
To keep fit, to keep healthy physically and to keep your brain functioning optimally, it’s essential to keep active.
“I’m very fortunate. I’m able to be active,” is how Leonard summed it up.
on the state).
All told, the average cost of a total U.S. funeral today with view ing and cemetery burial is around $12,000.
If this is more than you’re willing or able to pay, there are ways to save. For starters, you should know that prices can vary significantly by funeral provider, so it’s wise to shop around. If you need some help, there are websites you can turn to like Parting.com that lets you easily compare prices online based on what you want.
When evaluating funeral provid ers, be sure you get an itemized price
list of services and products so you can accurately compare and choose what you want.
The most significant way to save is to request a “direct burial” or “di rect cremation.” With these options the loved one would be buried or cremated shortly after death, which skips the embalming and viewing. If you want a memorial service, you can have it at the graveside or at your place of worship without the body.
These services usually run between $1,000 and $3,000, not counting cem etery charges.
Jim Miller is the author of Savvy Se nior, a column that runs every issue in In Good Health.
Youcannot change the number of years you have been alive.
But you can change and improve upon how your body manages the wear and tear of everyday living.
As you age, you may find yourself slowly declining with the addition of illness or disability. In aging, your body can lose lean muscle mass and be replaced by more body fat.

This process is called sarcopenia. The gradual loss of muscle can contribute to slowing metabolism, decrease in strength, declining aerobic capacity, decreased glucose tolerance and loss of bone density. With the increase in body fat comes the increased risk of disease such as Type 2 diabetes, coronary artery disease and a variety of cancers.
By changing your diet and partaking in regular exercise, you can
become lean and muscular at any age. Your body is designed to move and is necessary to acquire optimal health. The benefits of exercise are many including but not limited to: a reduction in the risk of breast cancer and stroke; maintaining a healthy gut flora; reducing and relieving stress, anxiety and depression; improving the symptoms of asthma; and improving glucose metabolism in diabetics.
Also affected is the lymphatic system which helps to fight illness and infections. Lymph fluid is moved when the body physically moves, circulating immune cells to clear congestion and move fluid through the lymph nodes and vessels. With exercising comes sweating. The sweat glands aid in the removal of waste products and toxins from your




 By Jim Miller
By Jim Miller
There are three different types of senior-specific flu shots (you only need one) that the CDC is now recommending to people age 65 and older. These FDA-approved annual vaccines are designed to offer extra protection beyond what a standard flu shot provides, which is important for older adults who have weaker immune defenses and have a greater risk of developing dangerous flu complications.
Here’s more information on these three vaccines.
• Fluzone High-Dose Quadrivalent: Approved for U.S. use in 2009, the Fluzone High-Dose is a high-potency vaccine that contains four times the amount of antigen as a regular flu shot does, which creates a stronger immune response for better protection. According to a study published in the New England Journal of Medicine, this vaccine was proven 24% more effective than the regular dose shot at preventing flu in seniors.
• Fluad Quadrivalent: First available in the U.S. in 2016, this adjuvanted vaccine contains an added ingredient called adjuvant MF59 that also helps create a stronger immune
response. In a 2013 observational study, Fluad was found 51% more effective in preventing flu-related hospitalizations for older patients than a standard flu shot.
You also need to be aware that both the Fluzone High-Dose and Fluad vaccines can cause more of the mild side effects that can occur with a standard-dose flu shot, like pain or tenderness where you got the shot, muscle aches, headache or fatigue. And neither vaccine is recommended for seniors who are allergic to chicken eggs, or those who have had a severe reaction to a flu vaccine in the past.
Also note that the CDC does not recommend one vaccination over the other.
• FluBlok Quadrivalent: For older adults who are allergic to eggs, FluBlok, which is a recombinant vaccine that does not use chicken eggs in their manufacturing process is your best option. This vaccine is proven to be 30% more effective than a standard-dose influenza vaccine in preventing flu in people age 50 and older.
All of these vaccines are covered
blood which then come to the surface as sweat.
Exercise consists of:
• Aerobic exercise helps the cardiovascular system (heart, lungs and blood vessels) to deliver oxygen to your muscles. Examples of this are jogging, running, swimming and walking, and should be done three to four times per week. If you are new to aerobic exercise, consider starting with a 15 or 30-minute brisk walk.
• Strength training will build muscle mass, increase metabolic rate and help maintain and build bone density. Plan on two to three sessions of strength training per week with two to three days muscle recovery between workouts. It is good do aerobic exercise and strength training on different days to allow for appropriate recovery.
• Stretching will increase the range of motion of your joints and keeping muscles loose and flexible. Examples of this are yoga and pilates approximately one to two times per week. Stretching exercises can also be used as warm-ups and cool-downs.
Your fitness level will help in determining how long to exercise each session. If you are working out with a buddy and are able to talk easily as you both move along, you may not be exercising hard enough. If you are able to talk, but prefer not to because it is more difficult, then you may be achieving a good pace. Conversation should be possible but not so easy to not achieve the benefits.
Over time and as you improve; you will want to increase the intensity and duration of workout sessions. To maintain your current physical
fitness, consider three workout sessions each week. Optimally you want to work out a minimum of four times per week, but five to six sessions weekly will improve your level of fitness. Plan on two to three aerobic workouts alternating with two to three strength training workouts per week incorporating stretching as a warm-up or cool-down.
Keeping motivated can be difficult for some especially if you’ve never exercised before or have physical limitations.
Consider taking your walks or runs in a different place, take a different class, find a workout buddy, or try working out with a personal trainer. Gyms and personal trainers often offer special packages for new clients helping to make it more affordable and provide specialized help in planning your personalized program.
Developing and maintaining an exercise program will improve your strength, health and appearance today and in the future.
Deborah Dittneris a family nurse practitioner and health consultant. Her mission is to transform as many individuals as possible through nutrition and lifestyle changes.


For more information, check out her website at www.debdittner. com or contact her at 518-596-8565.
100% by Medicare Part B as long as your doctor, health clinic or pharmacy agrees not to charge you more than Medicare pays.
Another important vaccination the CDC recommends to seniors, especially this time of year, are the pneumococcal vaccines for pneumonia. Around 1.5 million Americans visit medical emergency departments each year because of pneumonia, and about 50,000 people die from it.
The CDC recently updated their recommendations for the pneumococcal vaccine and now recommend that everyone 65 and older who has not previously received any pneumococcal vaccine should get either PCV20 (Prevnar 20) or PCV15 (Vaxneuvance). If PCV15 is used, this should be followed by a dose of PPSV23 (Pneumovax23) at least one

year later.
Or, if you’ve previously received a PPSV23 shot, you should get one dose of PCV15 or PCV20 at least one year later.
Medicare Part B also covers two different pneumococcal shots the first shot at any time and a different, second shot if it’s given at least one year after the first shot.
If you haven’t already done so, you should also get a COVID-19 booster shot this fall. Both Moderna and Pfizer have developed new bivalent booster vaccines that adds an Omicron BA 4/5 component to the old formula, which provides better protection.
Jim Miller is the author of Savvy Senior, a column that’s published monthly in In Good Health.

Itcan be hard to talk to your loved ones about moving into assisted living, so don’t push them too hard and make sure they feel safe and comfortable with the idea, one expert advises.

“Start the conversation as early as possible, and focus on what matters,” said Angela Catic. She’s a geriatrician and associate professor in the Roy M. and Phyllis Gough Huffington Center on Aging at Baylor College of Medicine in Houston.
“Think about if an assisted living environment could not just support, but enrich things that really bring joy to that individual’s life,” Catic said in a college news release.
As people age, it gets harder to take care of a house and yard. Adult children often start talking about assisted living when they see their parents are struggling, Catic said. After the death of a partner, a person may feel alone and lose their social connections. This is where transitioning into assisted living could benefit an older person, as such facilities often provide various social activities for their residents.
When starting a conversation with a loved one, consider covering these topics:




• Mention a few facilities you
have already researched prior to the conversation. Whether you visit them in person or do online research, keeping a few facilities in mind can ease any nervous feelings about the process.


• Present a few options close to your loved one’s home or facilities near the home of a family member. This could remind them that they won’t be completely alone and will still have access to their family.
• Stay mindful of their feelings, as they could feel anxious or sad about having such a conversation. These emotions may prompt them to resist the move altogether.
• Mention any of their friends that you have heard from or ask them if they know anyone who has already moved into an assisted living facility, to normalize the idea.

• Make sure they feel involved in the process so they feel like they have control over what happens.
• Encourage them to come with you to tour a few facilities so they can visualize what their stay would be like there.
“Find a place they feel good about, too, and bring some of their belongings,” Catic said. “It’s typically a major downsizing of space, but it is important to bring things that
have meaning to them and make it feel like home as much as possible. This may include items like a favorite chair, items they need to engage in a favorite hobby or family photographs.”
If your loved one says no to the idea of moving to an assisted living facility, don’t keep pushing the idea unless you’re truly worried about their safety. Hospitalization due to an accident or other health issues can also be a good reason to bring up the idea of assisted living again.
If they decline initially, you can always return to the conversation later, as their initial hesitation could be due to other factors that change, Catic said. When bringing the topic up again, ask them if they had time to reconsider the idea. Welcome their thoughts on the subject and offer ways you can make the process more comfortable for them.
Catic advises prioritizing finding








your loved one a place that fits their needs and learning as much about it as you can so you know exactly what you are signing them up for. Even if a place looks nice in the lobby or on the tour, finding out more about what they have to offer can be an important part of finding the best fit for your loved one.
Additionally, learn about the staff and how often people move in and out. On another note, some facilities might have connections to different social groups such as veterans or other interesting people with whom your loved one could socialize.
“Go beyond the beautiful, fresh flower bouquet in the lobby because this is going to be someone’s home, not a hotel they’re staying in for a couple of nights,” Catic said. “You’re looking for a feeling of home and fitting in with other residents and a staff that feel like family.”

– Lisa Clemmons, RN, BSN, OCN
 Dear Savvy Senior,
Dear Savvy Senior,
Can you recommend any good online hearing tests? My husband has hearing loss, but I can’t get him to go in and get his hearing checked, so I thought a simple online test could help him recognize he has a problem. What can you tell me?


There’s actually a growing number of very good online and app-based hearing tests available that will let your husband check his hearing on his own. These tests are a quick and convenient option for the millions of Americans that have mild to moderate hearing loss but often ignore it, or don’t want to go through the hassle or expense of visiting an audiologist for a hearing exam.
Hearing loss for most people develops gradually over many years of wear and tear, which is the reason many people don’t realize they actually have a hearing problem.
Anyone who has difficulty hearing or understanding what people say, especially in noisier environments or over the phone. Or, if you need a higher volume of music or TV than other people, should take a few minutes to test their hearing.
Online and app-based hearing tests can serve as a great screening tool. They are not meant to be a diagnosis, but rather to give you an idea of how bad your hearing loss is and what can be done about it.
For most do-it-yourself hearing tests, you’ll be advised to wear ear headphones or earbuds and sit in a quiet spot.
You also need to know that there are two different types of tests available. One type is known as pure-tone testing, where tones are played in decreasing volumes to determine your specific level of hearing loss. And the other type is known as speech-innoise or digits-in-noise (DIN) where you’ll be asked to identify words, numbers, or phrases amid background noise.
If your husband uses a smartphone or tablet, two of my favorite app-based hearing tests are the hearWHO app created by the World Health Organization, and the Mimi Hearing Test app. Both apps are free to use and are available through the App Store and Google Play.
HearWHO allows users to check their hearing status and monitor it over time using a DIN test, while Mimi uses pure-tone and masked threshold tests to give you a detailed picture of your hearing abilities.
There are also a wide variety of online hearing tests your husband can take on a computer.
Some top online tests — all offered by hearing aid manufacturers — for speech-in-noise or DIN tests can be accessed at ReSound (resound. com/en-us/online-hearing-test) and
Miracle Ear (miracle-ear.com/online-hearing-test).

And some good online hearing tests for pure-tone testing are available by Signia (signia.net/en/ service/hearing-test); Ergo (ergo. com/hearing-health/hearing-check); and MD Hearing Aid (mdhearingaid. com/hearing-test).
All of these hearing tests are completely free to use and take less than five minutes to complete.



If the tests indicate your husband has hearing loss, it’s best to think of that as a starting point. He should take results to his doctor or an audiologist for further evaluation.
Many insurance providers and Medicare Advantage plans cover routine hearing exams, however original Medicare does not.


If his hearing loss is mild to moderate, he should look into the new over-the-counter (OTC) hearing aids, which are available this fall online and at retailers like Best Buy, Walgreens and CVS.
OTC hearing aids don’t require a prescription or medical examination for purchase and they’re much more affordable than traditional hearing aids you buy through an audiologist or a licensed hearing instrument specialist.
Send your senior questions to: Savvy Senior, P.O. Box 5443, Norman, OK 73070, or visit SavvySenior. org. Jim Miller is a contributor to the NBC Today show and author of “The Savvy Senior” book.


Ifyou are eligible at age 65, your initial enrollment period (IEP):
• Begins three months before your 65th birthday.
• Includes the month of your 65th birthday.
• Ends three months after your 65th birthday.
If you are automatically enrolled in Medicare Part B or if you sign up during the first three months of your IEP, your coverage will start the month you’re first eligible. If you sign up the month you turn 65, your coverage will start the first day of the following month. This won’t change with the new rule.
Starting Jan. 1, 2023, your Medicare Part B coverage starts the first
Q.: When a person who has worked and paid Social Security taxes dies, are bene ts payable on that person’s record?


A.: Social Security survivors benefits can be paid to:







• A widow or widower—unreduced benefits at full retirement age, or reduced benefits as early as age 60.
• A disabled widow or widower—as early as age 50.
• A widow or widower at any age if he or she takes care of the deceased’s child who is under age 16 or disabled, and receiving Social Security benefits.
• Unmarried children under 18 or up to age 19 if they are attending high school full time. Under certain circumstances, benefits can be paid to stepchildren, grandchildren, or adopted children.
• Children at any age who were disabled before age 22 and remain disabled.
• Dependent parents age 62 or older.
Even if you are divorced, you still may qualify for survivors benefits. For more information, go to www.ssa.gov.
Q.: I plan to retire soon. When are Social Security bene ts paid?
A.: Social Security benefits are paid each month. Generally, new retirees receive their benefits on either the second, third or fourth Wednesday of each month, depending on the day in the month the retiree was born. If you receive benefits as a spouse, your benefit payment date will be determined by your spouse’s birth date.

Here’s a chart showing how your
day of the month after you sign up if you sign up during the last three months of your IEP.
Before this change, if you signed up during the last three months of your IEP, your Medicare Part B coverage started two to three months after you enrolled.
If you don’t sign up for Medicare Part B during your IEP, you have another chance each year during the general enrollment period (GEP). The GEP lasts from Jan. 1 through March 31. Starting Jan. 1, 2023, your coverage starts the first day of the month after you sign up.
You can learn more about these updates on our Medicare webpage at www.ssa.gov/medicare and our Medicare publication at www.ssa. gov/pubs/EN-05-10043.pdf.
Please pass this information along to someone who may need it.
monthly payment date is determined:
For a calendar showing actual payment dates, see the Schedule of Social Security Benefit Payments at www.ssa.gov/pubs.


Q.: Will my Social Security disability bene t increase if my condition gets worse or I develop additional health problems?

A.: No. We do not base your Social Security benefit amount on the severity of your disability. The amount you are paid is based on your average lifetime earnings before your disability began. If you go back to work after getting disability benefits, you may be able to get a higher benefit based on those earnings. In addition, we have incentives that allow you to work temporarily without losing your disability benefits. For more information about disability benefits, read our publications “Disability Benefits and Working While Disabled — How We Can Help.” Both are available online at www.ssa. gov/pubs.

LEFT Community Engagement Mary Beth Anderson, Excellus BCBS Regional President Eve Van de Wal, ACR Health Executive Director Lisa D. Alford and ACR Health Prevention CJI Supervisor Wendy Grullon gather together for a check presentation.
RIGHT Excellus BCBS Community Investments and Partnerships Manager Shayna Keller, On Point for College Utica Director Kevin Marken, and Excellus BCBS Regional President Eve Van de Wal meet for a presentation of the Excellus BCBS Community Health Award.
BlueCross BlueShield recently awarded several nonprofit organizations with its Community Health Awards.
They are:
• ACR Health received $2,500 to support its transportation assistance program. The program provides transportation to ACR Health clients who do not qualify for other transportation services. Transportation is provided to medical appointments, pharmacy visits, grocery shopping and social support activities.
“Data shows that lack of transportation is a major barrier to accessing health care and other needed services especially for many low income, racial; ethnic and sexual minority communities,” explained Lisa Alford, ACR Health executive director. “This program will allow our clients to keep medical appointments, pick up medications, and participate in social activities to reduce isolation and improve their mental and physical wellbeing.”
ACR Health is a nonprofit, community-based organization providing an array of support services to individuals affected by a wide range of chronic diseases, including HIVAIDS. The goal of ACR Health is to assist consumers in making informed health decisions so that they may have positive health outcomes. The mission of ACR Health is to create healthy communities by opening doors to services that enhance the
Excellus BlueCross BlueShield has been recognized by Forbes as one of the best employers in New York state.
In New York state, Excellus BCBS was ranked 19th overall. The health plan also finished as the highest ranked insurance company in the state.
“We’re proud to be recognized as a great place to work,” said President and CEO Jim Reed. “As a large Upstate New York employer, we’re committed to engaging and supporting our employees through our strong mission, inclusive culture, flexible work environment and comprehensive employee benefits.”
well-being of all. Their vision is a community in which every person has the opportunity to achieve optimal health and equality.
• Helios Care received $2,000 to support free bereavement counseling for the public. This program provides grief counseling services online and in person through support groups, individual counseling, camps for children, coping kits and presentations to the public. Helios Care social workers have been providing free bereavement counseling for all residents of Delaware and Otsego Counties since the onset of the pandemic and have seen a rise in demand for support groups. The funding provided will allow 12 additional support groups to be added to the program this year.

“Many traditional forms of grieving and commemorative activities of death, such as funerals and memorials, were stifled or stopped during the pandemic.,” explained Kathryn Dailey, Helios Care director of development. “This has left many residents suffering from unresolved grief leading to mental health issues and preventing them from moving on to the next stage of their lives. Support groups, led by our specially trained bereavement counselors, are especially effective since there is the benefit of knowing other people understand what you are going through and can provide mutual support.”
The mission of Helios Care is:
“Last year, we also raised the minimum wage for all employees from $15 to $18 an hour given this commitment to our employees,” he added.
Forbes, and its market research partner Statista, surveyed 70,000 individuals nationwide who worked for companies with at least 500 employees. Forbes divided its list into 51 rankings – one for each of the 50 states and the District of Columbia.
Surveys were conducted anonymously and considered various aspects of the employee experience, including working conditions, salary, potential for growth, and diversity.
Access the full list of rankings at Forbes.com.
Excellus BCBS employs more than 4,000 individuals across 39 counties of upstate New York.
“making life easier for patients and families facing serious illness or end of life by providing choices, dignity and compassionate care”. Helios Care provides hospice and palliative care to manage the symptoms of chronic diseases, as well as social workers to assist with social determinants of health and bereavement counseling. Services are provided in the patient’s home, free of charge or at a nominal cost. Helios Care’s nationally certified staff deliver the best practices of the industry and perform to the highest standards of patient care.
• On Point for College Utica received $4,000 to support it Excellus Scholars Emergency Support Services. This program will provide access and success services to help students enroll in, persist in, and graduate from college.
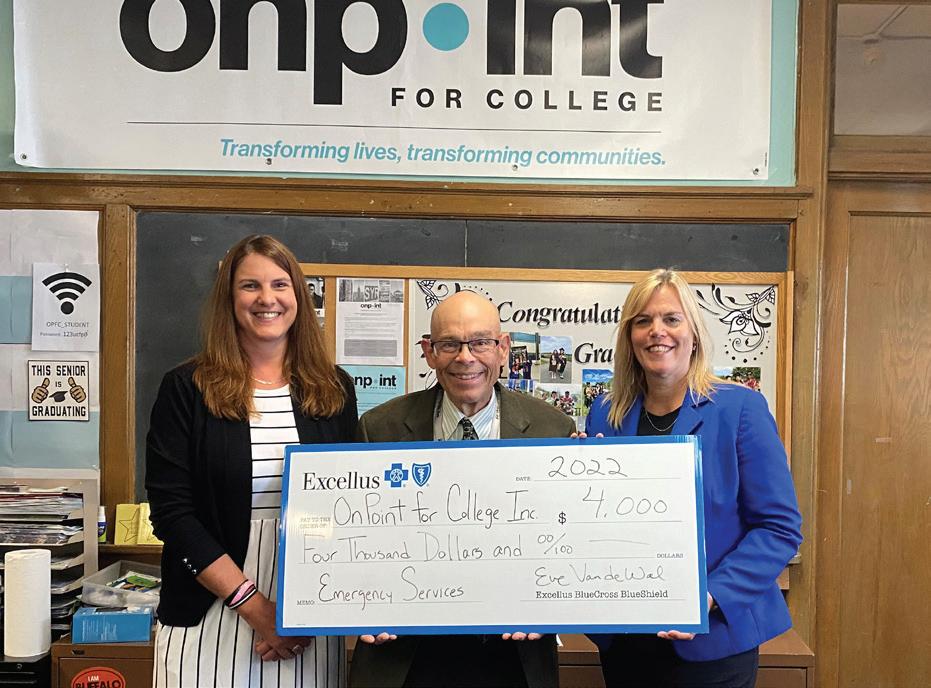
On Point helps students overcome barriers allowing them to pursue higher education and obtain careers as nurses, physicians, CNAs, therapists, medical interpreters, and other healthcare professionals.
“We help lower-income, first generation students believe that college is possible,” said Kevin Marken, On Point for College Utica director. “This funding will allow us to provide 20 On Point students, who are currently enrolled in college and pursuing studies in a healthcare field, the services necessary to persist and graduate. These new healthcare
professionals will have the potential to improve the health and wellbeing of those in our community.”
The mission of On Point for College is to break down barriers that prevent young, under-served individuals from achieving education and career success. On Point for College strives to transform communities by making college, training, and career success a reality for those who face great obstacles. With office in Syracuse and Utica, the organization serves youth in Onondaga, Cayuga, Oswego, Cortland, Madison, Oneida, and Herkimer counties.
Through a competitive application process, Excellus BlueCross BlueShield’s Community Health Awards provide funding to launch, expand, and sustain programs and services that promote health. These investments advance health equity by extending the reach of preventive health services or health-promoting programs to vulnerable populations. The health plan’s corporate giving follows all applicable laws and regulations and does not support funding organizations that conflict with its corporate mission, goals, policies, or products.
“The company’s community health awards demonstrate a corporate commitment to support local organizations that share our mission as a nonprofit health plan,” said Eve Van de Wal, Utica regional president of Excellus BlueCross BlueShield.
Eleven days since Hurricane Ian, a brutal, devasting monster storm hit my town in Charlotte County, Florida.





I stride down the sidewalk, dodging the many downed trees and tree limbs, street signs laying in the grass, shingles from a roof, bits and pieces of plastic and metal I can’t even identify.
Every inch of ground is covered with debris; every yard with big stacks of rubble.
Both sides of the sidewalk used to be green with foliage; it was a tropical jungle. I loved walking un der the canopy of the trees.
Now all is brown; bright sun glaring down.
No canopy of trees; no shade. No leaves left on the trees.
Few trees are intact; most have a limb hanging. No stop lights because there is no power. No power in much of the area.
It’s overwhelming and heart breakingly sad, all this destruction.
When the local weather person said “A massive hurricane is headed toward Florida,” I listened. But I’ve lived in Florida 20 years — I’ve often heard there’s a hurricane that may be headed our way. I didn’t get alarmed. Just another Florida day.
The weather people always make a big deal of it and everyone rush es out and buys tons of water and potato chips and toilet paper. Many evacuate. All sit back and watch the approaching hurricane, but it always turns off course or their predictions were wrong. Time and time again.
So why would this be any dif ferent? I thought. Not a big deal. It
won’t come here.
They warned us this is a bigger, more power hurricane. They weren’t sure where it was headed. They always err on the side of caution, get people all riled up and anxious. Well, not me; I wasn’t going to worry.
The day before, they still weren’t sure where this hurricane would make landfall. We were in the cone. Just to be cautious, I grabbed my toothbrush and favorite pillow and went to stay with my daughter and her family nearby.
The entire country knows what happened the next day, over those eight hours, as Ian’s winds strength ened to 155 mph. The storm sucked water from the Gulf to pour down over us, flooding the streets. It was a category 4 storm; the fifth-strongest hurricane to hit the U.S. Ian will go down in history as one of the most violent hurricanes of all time.
The power went out even before the wind and rain came. The house was cave-like dark because of the hurricane shutters on all the win dows. With the flickering Halloween candles, glow-in-the dark spider webs and menacing skulls, it was creepy.
As the wind and rain started, we hunkered down, shared stories and snacks while monitoring Ian’s prog ress on an iPhone. After a few hours, we couldn’t hear each other over the intensifying cacophony of Ian.
This wasn’t supposed to happen. I was so sure I wasn’t in the path of a hurricane. I was so wrong.
Hour after hour, the constant, loud sound of the wind and the pounding rain, punctuated by
loud hits. The hardest part was not knowing what it was like outside the house. We knew it would be bad from all the noise.
Finally, after a long eight hours, it stopped. We ran out the front door and cheered about how happy we were that we were OK and the house was OK. But outside was a mess. A river instead of the street. Our cars, up in the driveway, under water up to their tires. Before Ian, the lots next door and across the street were for ests, packed with trees and vines.
Now all the green was gone; trees lay on the ground, their roots exposed. Limbs all over the ground. The leaves all gone. Just a few brown tangled branches where it had been a tropical green forest. So sad.
A tree had fallen on the neigh bor’s car. Water was half way up his front door, going into his house; it wasn’t up on a beam like ours.
The backyard shed lost its door. Though filled with stuff and very heavy, the shed had been moved off its foundation by the wind. The huge above-ground pool was destroyed, pieces all over the yard.
As the water in the street less ened, I drove back to my apartment. As my complex has a generator, we had power. My daughter still doesn’t have power in her house, 11 days later. Taking cold showers was the worst of it for her. She’s been scrounging food wherever she can— most restaurants and stores aren’t open. So many people poured into to the county, offering food, helping the cleanup and recovery.
Going through those hours under the hurricane was nothing
compared to the aftermath. You’ve seen it on the news. Much of the fo liage is gone. Many roofs, pool cages and lanai screens stripped. All over, everywhere. Businesses aren’t open.
The landscape has changed; without the signs on buildings, the trees and the street signs, it’s hard to find your way around. It’s heart breaking. People wait in line six hours for gas, or drive hours to get what they need.
Authorities don’t know how many lives were lost; at least 120. My heart goes out to those who lost so much more than I did; two of my friends each lost their homes and are living with friends. A third is in a homeless shelter.
Now, I walk down the sidewalk, sending up thanks it wasn’t worse. A red-headed woodpecker hops up on the tree down in front of me, looks up at me. “Thought you were so smart, did you?” I imagine him say ing. “Next time maybe you’ll listen to them.”
Charlotte County will be OK; I know we’ll come back, better than before. We’re strong; we’re deter mined.
Barbara Pierce is a long-time contributing writer with In Good Health— Mohawk Valley edition.
‘They warned us this is a bigger, more powerful hurricane. They weren’t sure where it was headed. They always err on the side of caution, get people all riled up and anxious. Well, not me; I wasn’t going to worry.’