Why You Should

Of course you should always thank a nurse, but May is a special month. That's when it's celebrated Nurses Week (May 6-12) and Nurses Month.
See releated stories starting on page 11





Of course you should always thank a nurse, but May is a special month. That's when it's celebrated Nurses Week (May 6-12) and Nurses Month.
See releated stories starting on page 11



Cuddly, friendly, fun: Your pet brings so much to your life, but experts warn that, in rare cases, they can also bring illness.
The health benefits of pet ownership are many, noted physician
Stacey Rose, an associate professor of infectious diseases and internal medicine at Baylor College of Medicine in Houston.
For example, the presence of a dog or cat in the home can desensitize a child's developing immune system to certain allergens. Pets are also well-known stress busters, helping to lower risks for high blood pressure and depression, Rose noted in a Baylor news release.
But there are hidden health dangers, especially for pregnant women or anyone with an immune system weakened by illness, organ transplant or infection with HIV.
For those people, there's the risk of toxoplasmosis, caused by the toxoplasma germ that can be found in cat feces, Rose said.
Hookworm — this time found in dog feces — is another infectious agent to be wary of, so always wash your hands after picking up after your dog.
Then there's the danger of getting bitten or scratched by a dog, cat or other pet.
Cats, especially, can transmit a
dangerous organism called Pasteurella multocida through a bite, and dog bites can pass along another hazardous germ called Capnocytophaga canimorsus.
Infections with these germs can be dangerous and even fatal for people with compromised immune systems, Rose said.
Cats and dogs who roam outside can also come into contact with rodents, possums, raccoons and other wild critters. Rose said the main health issue there is the insects that live on these animals, such as fleas and ticks — and the illnesses they carry.
For example, Murine typhus is a flea-borne illness that can bring on rash, fever and other symptoms in humans.
“You don't have to have direct
exposure with a rodent to be at risk; if your pets are gallivanting with those other animals and the fleas are transferred from the rodent to your pet, then your pet can help transmit that disease," Rose explained.
Bartonella henselae illness is another flea-borne bacterium that's so associated with felines that it's been nicknamed "cat scratch" disease. It's most associated with scratches from kittens, Rose said. If the kitten is carrying fleas, the fleas' infected feces can enter your body via a scratch.
According to the Baylor news release, "in kids or adults with a normal immune system, one might develop a big lymph node that will go away on its own," after a scratch, but "with a compromised immune system, that same bug can lead to far-reaching diseases including bloodstream infections or infections of the heart or heart valves, or the eye, liver or spleen."
Then there are illnesses caught from scaly cold-blooded pets such as turtles, lizards or snakes.
The U.S. Centers for Disease Control and Prevention continues to issue alerts about people (often small children) catching salmonella from these animals after handling them.
Elderly people, or those with compromised immune systems, should also avoid handling pet reptiles, or wash their hands thoroughly with soap and water if they do.
“There are plenty of reasons why we can and should have pets, but you just need [to] be aware of your own immune system and the potential risks," Rose said. We have to be conscientious pet owners for our own health and the health of our families and neighbors."


The Community Memorial Hospital (CMH) network is thrilled to unveil the reimagined Center for Orthopedic Services. Nestled within the state-ofthe-art Center for Specialty Services building at 160 Broad Street, this cutting-edge facility promises top-tier care for orthopedic needs.
NEW, EXPANDED MEDICAL OFFICE
As patient demand surged and our exceptional team of providers expanded, it became clear that a larger, more advanced space was essential. The new location ensures unparalleled patient comfort and accommodates our growing roster of experts.
SponsoredContent
REVAMPED SPACE FOR EXCEPTIONAL CARE
Thanks to an extensive renovation, our facility now caters to outpatient care, complete with radiological patient services. Here’s what the new space offers:
• Ten Patient Exam Rooms
• Procedure Room
• Casting Room
• Spacious and Welcoming Waiting Room
With the hospital next door, patient convenience is paramount. Our walk-in clinic, open Monday through Thursday from 9 AM to 1 PM, ensures quick, easy access. Appointments are available promptly after an Emergency Department visit.
ORTHOPEDIC EXCELLENCE
Under the visionary leadership of Jeff Coakley, CMH’s President and CEO, we proudly introduce our Center for Orthopedic Services. The Center is a testament to our commitment to excellence. Let’s meet our remarkable orthopedic specialists:
Dr. Kamaljeet Banga, Orthopedic and Sports Medicine
Dr. Nicholas Qandah, Spine and Neuorsurgery
Dr. Richelle Takemoto, Orthopedic Surgeon
Frank J. Walczak IV, Physician Assistant
Jackie Ireland, Physician Assistant
To learn more about any of the Community Memorial and Hamilton Medical Services, PLLC, visit www.communitymemorial.org or call us at (315) 824.7040.

Along with the Blue Cross Blue Shield Association, we’re committed to reducing racial and ethnic maternal health disparities by 50% in 5 years. Join us and take action today:
Childbirth complications are 46% higher among Black mothers. Anyone can help by learning more about this urgent issue. (Tip: start with our podcast episode)1
Every expecting mother should receive unbiased, high-quality care. Examine your own implicit biases. What might need to change?
Get the facts in our episode “Reducing Racial Disparities in Maternal Health” with Dr. Cuyler at ExcellusBCBS.com/ podcast or wherever you listen to podcasts
Support policies and organizations that increase access to affordable, culturally sensitive maternal healthcare. Let the expecting mothers in your life know they have a voice, are being heard, AND believed.

Medicare spent $57 million to cover the drug in 2017. It spent $4.6 billion in 2022
The catchy tune in the commercial might be referring to its price.
Medicare approved the drug to treat diabetes in 2017. Part D spent a sensible $57 million on it for patients in 2018. But due to increased demand, new uses like weight loss and glaring price gouging by manufacturer Novo Nordisk, Part D spending on Ozempic rose to an astounding $4.6
Not getting much attention, (like the nurse and physician shortage), is the increasing shortage of pharmacists.
In the past 10 years, the number of applicants to pharmacy schools has declined a precipitous 60%. Some of this decline could be self-inflicted as pharmacy schools unilaterally decided to mandate all students must get a Ph.D. starting in 2000. It has gotten so bad that CVS is offering $20,000 scholarships to 21 needy pharmacy students. While laudable, that won’t even make a dent in the shortage. Pharmacy is a great career. Pharmacists work in hospitals, supermarket, community retail stores, primary health centers, nursing facilities and research. Salaries are in the $130,000 to $170,000 range. Pharmacists are increasingly involved in direct patient interaction. The shortage of pharmacists and our dependence on the “goodwill” of corporations like
billion (with the “b”) in 2022.
Medicare has been prevented from using its vast purchasing power to negotiate drug prices literally by an act of Congress under George W. Bush. Recently, Congress has magnanimously allowed Medicare to negotiate 10 - yes, just 10 - drug prices in 2026. This shows how much influence and control the drug lobby exerts over Congress. Maybe one of
CVS to mitigate the shortage is just another example of our fragmented and uncoordinated healthcare system where individual components must fend for themselves because there isn’t a national strategic plan or vision.
In an effort to control unscrupulous private equity firms notorious for realizing profits over patient safety and community welfare, this proposed bill would require medical groups, nursing homes and hospitals to reveal any PE affiliation.
Struggling healthcare organizations, particularly vulnerable rural nursing homes and hospitals, have resorted to partnering with PE for salvation. Typically, the PE firm will quickly turn around the finances of their client by immediately cutting staff and unprofitable services. Before the facility knows what has
contributions and copays are also rising (cost shifting) causing many families to postpone or even avoid seeking care because of high out of pocket expenses. As discussed in previous columns, medical debt is the No. 1 cause of personal bankruptcy. While the goals of the task force are laudable, they should also consider a functioning national healthcare system to replace our enormously expensive, confusing, inequitable, uncoordinated and fragmented healthcare system. Just saying.
the 10 prices Medicare negotiates in 2026 will be Ozempic. This is another example of why our care and drugs cost so much and why we need to seriously consider/ study a national plan. As mentioned last month, total healthcare costs in the US are expected to increase from about $5 trillion last year to around $15 trillion in 2030.
hit them, their fledgling hospital or nursing home has been stripped to bare bones, leaving the remaining employees and the community high and dry.
Once the ephemeral profits are gone, so too is the PE firm. PE firms typically get paid a hefty management fee and then first crack at profits. The Health Over Wealth Act is intended to regulate PE in healthcare and to require healthcare organizations to reveal any PE involvement.
Half of the US population is covered by employer-sponsored healthcare.
The Commonwealth Fund has recently created a task force comprised of representatives from politics, universities and insurers to identify market incentives and regulatory policies that would result in better access, delivery, outcomes and overall population health.
Employers are faced with rising premiums. Consequently, employee
California-based Kaiser has just added Pennsylvania-based Geisinger Health to its vast multi-hospital, multi-system, multi-state healthcare system, Now known as Risant Health, the multifaceted healthcare system boasted revenues more than $100 billion last year. Geisinger brings 10 hospitals (including Guthrie Cortland Medical Center) and 600,000 members to Risant.

Nonprofit hospitals have had to build large networks and capital in order to compete with well- heeled for-profit providers like Walmart, Amazon and CVS. Size helps Risant effectively negotiate with wealthy commercial insurers like United, Aetna, BCBS, Anthem and Humana. The ultimate goal is to further develop Risant’s own health insurance plan (Kaiser Permanente) by adding members which mitigates risk and keeps their premiums competitive. Profits generated by their proprietary insurance plan are then re-invested in the healthcare system and patient care.
Medicare can’t negotiate prices, but Amazon can. Prime members are eligible for the RxPass which promises not only lower drug prices but drone delivery to your doorstep someday soon. This home delivery presents an existential threat to “mom and pop” pharmacies and huge corporate chains like CVS and Walgreens. Between 2009 and 2015, one of eight brick and mortar pharmacies closed, most in depressed and underserved communities. Innovation is great, but once again our lack of a national gameplan is apparent.

George W. Chapman is a healthcare business consultant who works exclusively with physicians, hospitals and healthcare organizations. He operates GW Chapman Consulting based in Syracuse. Email him at gwc@gwchapmanconsulting.com.
As the world’s population ages, a new report warns that the number of people with cancer could climb 77% by 2050.
In the report, published in April in the journal CA: A Cancer Journal for Clinicians, researchers from the American Cancer Society found there were about 20 million cancer cases and 9.7 million cancer deaths in 2022, the latest year for which data is available.
However, “we think that number will go up to 35 million by 2050, largely due to an increasing population in the aging population,” physician William Dahut, chief scientific officer for the American Cancer Society, told CNN.
“A lot of the drivers for cancer that we’ve traditionally seen in high-income countries, such as tobacco and obesity, these same cancer drivers are now moving into the low-income countries,” Dahut noted. “These are countries that do not have the tools to find cancer early, treat cancer appropriately and prevent it in ways that are often being done in other countries.”
The good news is that those risk factors can be minimized with lifestyle changes, experts said.
“With more than half of cancer deaths worldwide being potentially preventable, prevention offers the most cost-effective and sustainable strategy for cancer control,” senior study author physician Ahmedin Jemal, senior vice president of surveillance & health equity science at the ACS, said in a news release. “Elimination of tobacco use alone could prevent 1 in 4 cancer deaths,
or approximately 2.6 million cancer deaths annually.”
The most common cancer types were lung, breast in women, colon, prostate, stomach, liver, thyroid, cervical, bladder and non-Hodgkin lymphoma, according to the report.
Lung cancer was also the leading cause of cancer deaths, followed by colon, liver, breast in women, stomach, pancreatic, esophagus, prostate, cervical cancer and leukemia.
Tobacco remains “the principal cause of lung cancer,” according to the report.
“While we do see lung cancers that are not related to smoking, the number one cause of lung cancer is smoking. And so obviously, there’s still much work to be done in the U.S. and everywhere to continue to address the epidemic of smoking,” said physician Harold Burstein, an oncologist at Dana-Farber Cancer Institute in Boston.
“Other things that people can do to reduce their cancer mortality include screening for early cancer detection and better outcomes. In the U.S., we have very vigorous opportunities for screening with mammography, colonoscopy and Pap smears, but these are still often under-utilized by many parts of our society,” he said. “In the more advanced economies, like the U.S., we have seen remarkable declines in the rates of mortality from breast cancer and colon cancer, probably about half of that due to early detection.”
In Good Health is published 12 times a year by Local News, Inc. © 2024 by Local News, Inc. All rights reserved. 4 Riverside Drive, Suite 251, Utica, NY 13502 Phone: 315-749-7070 • Email: IGHmohawkvalley@gmail.com A monthly newspaper published by Local News, Inc. 20,000 copies distributed. To request home delivery ($21 per year), call 315-749-7070.
Editor & Publisher: Wagner Dotto • Associate Editor: Stefan Yablonski
Contributing Writers: Barbara Pierce, Deb Dittner, Gwenn Voelckers, David Podos, Deborah Jeanne Sergeant, Anne Palumbo
Advertising: Amy Gagliano: 315-402-3370 • Email: amyIGHmv@gmail.com
Layout & Design: Angel Campos-Toro • Office Manager: Allison Lockwood



Living alone after a divorce or the death of a spouse can be a challenging yet transformative experience.
I know it was for me.
My own path to contentment took some time, some growing pains — setbacks as well as successes — and some aching losses before I could find my way back to my true self.
For many, the transition from married life to being single marks a period of rediscovery and a time to redefine their identity.
After focusing on the needs of a spouse and family, it’s common to feel as if you’ve lost touch with who you are as an individual. However, I’ve come to realize that the key to living alone successfully lies in embracing this opportunity to explore who you really are and who you aspire to be.
My journey began with a set of soul-searching questions to identify and clarify my beliefs, values, likes and dislikes. I was careful to focus on what mattered to me and to steer clear of “shoulds” and other people’s agendas.
This exercise in introspection enabled me to create a life that is authentic, fulfilling and uniquely mine. Contentment followed.
To begin your own journey of self-discovery, you might start by asking yourself some fundamental questions:
1. When have you felt the most fulfilled and alive in your life? What were the circumstances surrounding those moments?
2. What dreams and aspirations did you have when you were younger? Are there any steps you can take now to work toward those dreams?
3. Who are the people in your life that bring out the best in you? What is it about those relationships that are so meaningful to you?
4. What are you curious about? What subjects or topics do you find yourself constantly wanting to learn more about?
5. When do you feel most like your ol’ self again? What are you doing in those moments? (I took up gardening again.)
6. What values are most important to you? Helping the less fortu-
nate? Working toward equal rights? How can you incorporate those values into your daily life?
7. What kind of books, movies or music do you enjoy? Could those subjects hint at a hidden passion or interest?
8. How do you spend your time when no one is watching, when you are just being you? (I like to sing to my cat!)
9. What activities or hobbies did you pursue as a young adult that gave you joy? Are there any ways you can incorporate those activities back into your life now?
10 What are some small, simple pleasures in life that bring you joy? How can you incorporate more of those into your daily routine?
These questions can help you gain a deeper understanding of yourself and your desires. They can also serve as a guide as you navigate this new chapter in your life.
Teresa, a good friend of mine, had spent most of her adult life caring for her family. She wouldn’t have traded that for the world, but after her divorce, she realized that somewhere along the way she had disappeared around the edges. She had lost her own sense of self.
Determined to reconnect with herself, she started exploring her family history through Ancestry.com. As she delved into her roots, she uncovered fascinating stories about her ancestors and their lives. Teresa began to see herself as part of a larger whole, which brought her a deep sense of fulfillment and belonging.
Similarly, Steve, my middle-aged neighbor, found himself at a crossroads after the death of his wife. He had been so aligned with her that he struggled to find his own identity after her passing. Through therapy and self-reflection, Steve recalled his love of travel. On his first solo trip, he discovered a sense of freedom and adventure that he had been missing. It led to many more trips and a newfound appreciation for life’s possibilities.
Teresa and Steve’s stories highlight the transformative power of reconnecting with your true self. By taking the time to understand who you are and what you want out of life, you can create a new and fulfilling existence for yourself.
Remember, this journey is yours and your alone. Embrace it with an open heart and a curious mind, and you will be amazed at what you discover along the way.

Gwenn Voelckers is the author of “Alone and Content: Inspiring, empowering essays to help divorced and widowed women feel whole and complete on their own.” She welcomes your thoughts on this column as well as topic suggestion for future essays at gvoelckers@rochester. rr.com.




ing any new services that you might be offering?

Executive director of The Utica Center for Development discusses some of the programs it offers to veterans and non-veteran
DavidQ: How long have you been the executive director?
A: Sixteen years. I am also the founder of the organization.
Q: Tell our readers about your business. I believe the center works closely with our veteran population, but I also think you provide services for non veterans as well, is that correct?
A: Yes, we work with both populations. Let me start off first with our services for veterans. So, we have numerous programs, some through the state, others through the county, as well as the Veterans Association. Our main focus where we put most of our effort on is to assist the homeless veteran. Currently, we have 30 units of housing specifically set aside for homeless vets. If for some reason we cannot house the veteran at one of our sites, we have subsidy programs that will house them through private landlords or other nonprofit housing. We also offer peer to peer programs where veterans work together to help one another. We realize that the peer
L. Podos
element is very important for the vets as they oftentimes feel more comfortable talking to another veteran. We also have programs dealing with suicide prevention.
Q: Do you have information on what the national statistics are for homeless vets, as well as suicide statistics?
A: Yes, the national average is one out of every three homeless people are veterans. In regards to suicide, the statistics show that approximately 22 veterans per day will die from suicide. Thankfully we do have a suicide prevention program which includes our case managers along with collaboration with the Oneida County Department of Mental Health.
Q: In regards to homelessness, what are the causes that put people into this situation?
A: When you think about the homeless, there are many issues that lead up to a person and or family facing that situation. It usually takes
A: We are expanding our services to those with developmental disabilities. More info can be found on our website. I also want to make mention that everything that we do for the veteran we also do for their family. You can’t fix an issue unless you are working with the whole family. So, that is very important to us as we work with our veterans. We also own the YWCA building here in Utica and that facility has a pool, so very soon we will be able to offer swimming to our clients.
Q: What number of staff do you presently have?
A: Currently we have 35 staff. Most of them are full-time employees and we also have many amazing volunteers which we rely upon.
Q: Are the services you provide just for Oneida County?
A: Our services reach out to 12 counties throughout New York state.
Q: How are you funded?
A: The majority of our funding comes through the Department of Veteran Affairs. We also receive funding from Oneida County, the city of Utica, Oswego County, fundraising and donations.
Q: In closing, is there anything else you want people to know?
A: They can go to our website to see all our services and any up-coming events. That site:
For more information, visit ucdevelopment.org or call 315-765-0975.





Yesterday I felt really irritable, out of sorts, got mad at my partner for little things I usually can ignore. Got mad at myself because I couldn’t seem to do anything right.
Not a good feeling at all. I wanted to jump out of my skin!
“Let’s get out of here!” I suggested. “I’ve got to get out of here! Now!”
We grabbed our keys and left. Drawn by rock music, we headed over to a nearby concert in the park. “Pink Cadillac!” I heard: “I love you for your pink Cadillac…Cruising down the street…Spending all my money on a Saturday night.”
My mood switched. I felt great as we sat on the wall listening to the music. The last rays of sun flickered through the trees along with a gentle breeze. People milled around as they found a place to sit and set up their chairs. Some joined us on the wall;
some danced on the grass. Suddenly, I felt good; I felt happy. That irritable feeling had been replaced by a feeling of goodwill. The endorphins were flowing through my brain.
What’s making me feel so good, I wondered? You might be saying it’s being outside, in nature. Or the music lifted your spirits. And you wouldn’t be wrong. But I think it’s being around people, even strangers. I love people watching. I love being around people.
That’s why I was so irritable — I’d been cooped up in my apartment for three days or more, not talking to anyone but my partner. Not seeing anyone but him.
Yes, being outdoors, with the trees and the grass, and hearing music with a good beat helped. But I think it was being around people that helped the most.
I definitely have a need to be around people. Doesn’t have to be friends; strangers are just fine. Last night, being around a bunch of strangers filled my heart with joy!
I even talked to strangers. “What a beautiful color that shirt is on you!” I called out to a woman walking by. Her hot yellow shirt was stunning against her olive skin and long dark hair. “Thanks!” she said as she passed. Then I turned to the woman sitting next to me. “What a beautiful woman you are,” I said. Her head was shaved; she’s probably going through chemotherapy, I thought. And she was beautiful, in part because she dared go out in public with a naked head.
One of our basic human needs is for people. We’re wired to connect with others; pathways in our brains are stimulated when we’re around others. When we’re talking with another person, pathways in our brain light up, say scientists. We’re hardwired to interact and connect with others.
That includes strangers. Social connections that fight loneliness don’t have to mean spending time with your best friend. Being around strangers, making small talk, is important also. Talking with strangers is good for your health, say experts.
Isolation kills faster than cigarettes. Faster than Dunkin’ Donuts. Faster than being a couch potato. Even being around strangers is protection against isolation. Experts recommend we connect with others at least once a week.
Studies show that the amount of social interaction a person has in their daily life is one of the most consistent predictors of well-being. One study found that people who had a strong social network were 50% less likely to die during the study period than those with little social support.
I know that’s true of me. Before I lived in my current apartment, I lived in a house in the woods. It was
truly isolated, out of sight of other humans. Bears wandered through every now and then, deer tentatively poked around, raccoons, squirrels, rabbits and birds were plentiful. I loved it there. But I found I got very squirrelly and weird after a few days without people. So I’d hop in my car and drive to the library, or the supermarket. Just hearing the voices of others helped, seeing their faces. Exchanging smiles and greetings with librarians or cashiers made me feel balanced again.
Little things like that can give us immediate relief from loneliness. The U.S. Surgeon General calls loneliness a top public health concern. Experts say it’s a problem more serious than we might realize. Many of us have become more isolated. We can do our banking and satisfy all our shopping needs — groceries, clothing, essentials, hobby supplies and more — online, without a single human interaction. If we need a cup of sugar or a tool, we don’t drop in our neighbor, we have it delivered to our door. Even the library and the supermarket have self-check-out. It’s interaction-free, with no greetings, no eye contact, no smiles, no comments about the weather and no common courtesies exchanged.
Try it! Get out there among people and light up those pathways in your brain!

Barbara Pierce is a retired licensed clinical social worker with many years of experience helping people. If you would like to purchase a copy of her book, “When You Come to the Edge: Aging” or if you have questions for her, contact her at barbarapierce06@yahoo.com.





















Mental health and substance abuse problems often occur together. And they come with an enormous cost to individuals, families, communities and systems.
We asked credentialed alcohol and substance abuse counselor Sarah Decker, director of the Rescue Mission of Utica’s Addiction Stabilization Center, to help us understand this issue.
Q: What are some of the things we should know about people who have substance abuse issues combined with mental health issues?
A: It seems like more people have both issues. It’s difficult to tell which came first, the mental health issues or the substance abuse issues. By the time they start treatment, it’s a dual problem.
This is a difficult population to treat.
The links between mental health and substance abuse issues are complex. Certain substances can cause people with an addiction to experience one or more symptoms of a mental health problem. Also, mental health problems can sometimes lead to alcohol or drug use; some with a mental health problem may misuse these substances as a form of self-medication. Additionally, mental health and substance use disorders share some underlying causes.
People with substance abuse
issues often have feelings of trauma, anxiety or depression.
Also, substance use problems occur more frequently with certain mental health problems, including depression, anxiety, schizophrenia, bipolar disorders, attention-deficit hyperactive disorder and personality disorders.
Q: For many, someone with an addiction looks like they’re repeatedly making bad choices and ignoring reason. Can this be said of those with a combination of mental health and substance abuse issues?
A: It’s not that simple. The newer
drugs, the synthetic drugs people are using now, damage the brain. They amplify the mental health symptoms much more, making it very difficult to treat these people.
When one becomes addicted to a substance, the brain changes; it rewires your brain. Your brain operates differently than the brain of a person who is not addicted. According the National Institute on Drug Abuse, “Addiction is a chronic complex brain disease that is compulsive or difficult to control, despite harmful consequences…Repeated drug use can lead to brain changes that challenge an addicted person’s self-control and interfere with their ability to resist intense urges to take drugs.”
Q: How do you treat people with substance abuse and mental health issues?
A: It’s not very simple. Treating a person takes a long time. And both issues must be treated.
Generally, our facility and most of the facilities in the area have a psychiatric doctor or nurse practitioner on staff. At the Rescue Mission, we have a psychiatric doctor and a licensed social worker. We do counseling and prescribe medication for both issues.
In general, treatment has a low success rate. It’s challenging, but rewarding.
Q: How does one get treatment at the Rescue Mission?
A: Call us or come in. We’ll ask some questions to figure out what’s going on with you, what your crisis might be. If we determine that you’re eligible for our services, we’ll admit you. You’ll stay on site and work on your goals. Housing is a big goal for


many people, also improving social skills, education, family issues and long-term recovery. Everyone admitted has to stay clean for a time to distinguish what are mental health issues and what is drug-induced issues. You have to have a period of time when you’re not using to figure out how to treat your mental health challenges.
The Rescue Mission’s Addiction Stabilization Center is a 25-bed facility for adult men and women with substance use disorder. Stabilization provides a safe environment in which a person may minimize withdrawal symptoms, cravings, psychiatric and medical symptoms before referral or transition to another program or element of structured treatment and recovery.
Q: What else should we know?
A: The new synthetic substances available now are affecting mental health severely. They’re a new trend, not a good trend. These drugs are much different than 15 years ago. In our state, in our county, we try to stay up to par and address this, combat it. Every effort we bring to the table is working towards a better system.
I’d like people to know that there is help. It’s not as simple as ‘go get fixed.’ Long-term, long-term lifestyle changes are necessary. Everyone needs to help. It takes a community to help one person, as there is so much entailed. People with combined substance abuse and mental health issues need a lot of understanding and help.


Some vegetables need to be tamed, and feisty rhubarb is one of them. It’s barely edible raw, it looks like celery, its leaves are poisonous, it’s beyond tart, and it thinks it’s a fruit!
With such a rebellious personality, is it any wonder rhubarb gets short shrift at the market?
My advice? Give this imposter fruit a chance!
All it takes is a good recipe and a little sugar to open your eyes to rhubarb’s delicious, nutritious side.
Rhubarb, like most fruits and vegetables, benefits heart health in several ways. Its fiber helps lower cholesterol; its diverse antioxidants keep inflammation at bay; and its potassium helps lower blood pressure. Indeed, a trifecta of nutrients to help keep our tickers in tiptop shape.

In addition, rhubarb teems with vitamin K, an essential vitamin for blood clotting, bone building and heart health. Recent studies from the Perth Longitudinal Study of Aging Women revealed that women who ate more vitamin K-rich foods significantly reduced their risk of bone fractures later in life. What’s more, a growing number of studies have demonstrated that vitamin K may play an important role in slowing, and even preventing, the progression of Alzheimer’s disease.
Rhubarb’s fiber benefits our
bodies in ways above and beyond our bowels.
Yes, it promotes regularity and reduces the risk of colon cancer, but it also improves digestion, helps to regulate blood sugar levels, and facilitates weight loss or maintenance because it’s so filling.
On the downside, rhubarb does contain oxalates, which are naturally occurring compounds in plants. Because oxalates can bind to calcium—and to a lesser extent—other minerals in the stomach and intestines, they can reduce the absorption of these beneficial nutrients, as well as increase the risk of kidney stones in some people. What to do? Cook rhubarb to reduce oxalate content; eat in moderation; drink plenty of water to dilute oxalates in urine; and consult your doctor if you have kidney issues.

Anne Palumbo is a lifestyle columnist, food guru, and seasoned cook, who has perfected the art of preparing nutritious, calorie-conscious dishes. She is hungry for your questions and comments about SmartBites, so be in touch with Anne at avpalumbo@aol.com.
Grumbling and grousing to others isn’t an effective way of reducing rage, a new review shows.
Folks who vent about a source of anger might feel better in the moment, but that won’t diminish their ire, researchers found.
Instead, stress-reducing techniques like deep breathing, mindfulness, meditation and yoga are much more effective alternatives than griping, results show.
“I think it’s really important to bust the myth that if you’re angry you should blow off steam -- get it off your chest,” said senior researcher
Brad Bushman, a professor of communication at Ohio State University.
“Venting anger might sound like a good idea, but there’s not a shred of scientific evidence to support catharsis theory.”
For this analysis, researchers reviewed over 150 studies involving more than 10,000 participants. They discovered that turning down the heat through stress-relieving activities is better at reducing anger because it lowers a person’s fight-or-flight response.
On the other hand, venting about anger actually increased a person’s agitation, as did physical activities
Choose firm, crisp stalks with shiny skin. Remove toxic leaves (if present), then wrap rhubarb in plastic wrap and store in fridge for up to a week. Don’t cut the stalks until you are ready to use or the rhubarb will dry out.

Adapted from dishnthekitchen.com 12 standard muffins
FOR THE STREUSEL
3 teaspoons all-purpose flour
2 tablespoons sugar
1 tablespoon brown sugar, packed
1 tablespoon cold butter, cut into pieces pinch salt ¼ cup walnuts
FOR THE MUFFINS
¾ cup + 1 tablespoon white
1. For the streusel topping: Place flour, sugars, butter, and salt into the small bowl of a food processor. Pulse until the mixture resembles coarse crumbs. Add walnuts and pulse until the walnuts are desired size. Set aside.
2. For the muffins: Preheat oven to 425°F and line a standard muffin tin with paper liners.
3. Mix the flours, baking powder, and salt together in a small bowl. Set aside. In the bowl of a stand mixer, cream the butter and sugar together for 3 minutes. Add the eggs one at a time, then add the milk.
whole-wheat flour
½ cup all-purpose flour
1½ teaspoons baking powder
½ teaspoon salt
1 cup sugar
6 tablespoons butter, softened
2 eggs
½ cup 2% milk
½ cup walnuts, chopped
1 cup strawberries, chopped 1 cup rhubarb, chopped
4. Gently add the dry mixture to the bowl until it comes together. Do not overmix.
Fold in the walnuts, strawberries, and rhubarb.
5. Evenly distribute the batter in the muffin cups. Top each muffin with some streusel topping.
6. Bake at 425°F for 15 minutes; then check for doneness with a toothpick. If it doesn’t come out clean, bake a few minutes more until toothpick looks clean. Cool in muffin tin for 10 minutes, then remove and cool muffins on wire rack.

like jogging.
“To reduce anger, it is better to engage in activities that decrease arousal levels,” Bushman said in a university news release. “Despite
what popular wisdom may suggest, even going for a run is not an effective strategy because it increases arousal levels and ends up being counterproductive.”
In the past decade the number of male nurses increased by 59% but men represent only 125 of
all nursesBy Deborah Jeanne Sergeant
From Florence Nightingale onward, nursing has been a female-dominated career. But more men are earning nursing degrees.
According to the Bureau of Labor Statistics, the percent of male nurses has grown by 59% in the past decade.
However, that still amounts to only 12% of all licensed practical nurses, registered nurses and nurse practitioners.
One of the reasons is the perception that only women work in nursing so that men don’t consider it as a career option.
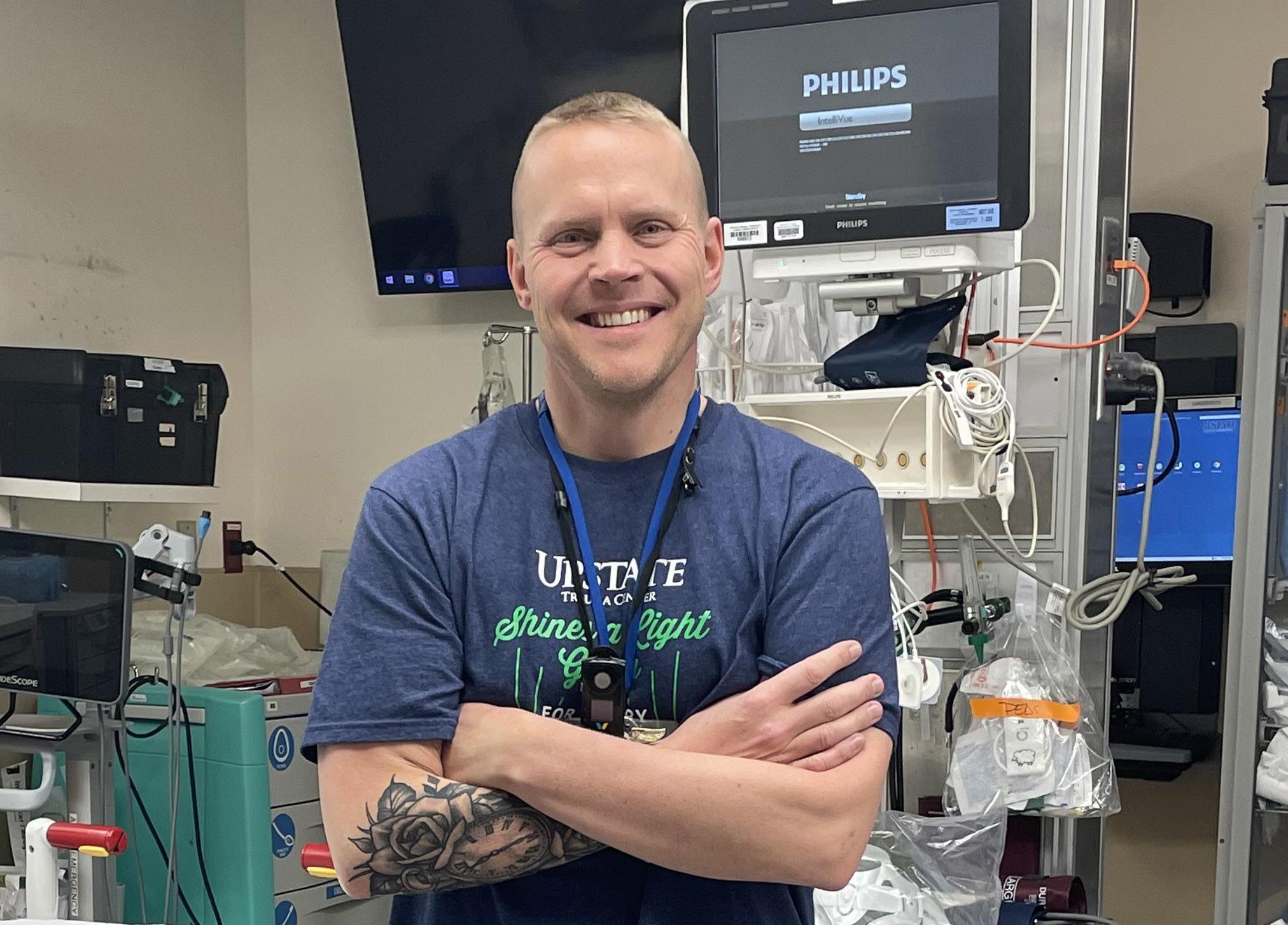
“There still tends to be a stigma and stereotype that exists that labels nursing as a woman’s profession,” said Erik Zeiner, nurse and co-manager of the adult emergency department at Upstate University Hospital. “One such way that nursing programs are trying to overcome this perception is through the use of social media. The goal behind the content is to emphasize the numerous gender-neutral opportunities that are available that include competitive salaries, growth, and even travel.”
By repeatedly showing men in nursing, educators normalize the career. The strategy appears to be working.
Michael Casey, a nurse at Center for Children’s Cancer and Blood Disorders at Upstate Cancer Center, has also observed the “male nurse” stigma while he was in nursing school, but said it wasn’t widespread.
“Since the start of my career in school and professionally, I would say that the culture at both Crouse Hospital and Upstate have been very welcoming of male nurses,” he said. “Obviously, there are the outlying people who do not see things the same way. For example, the nurse who told me that ‘as a male’ it was inappropriate for me to discuss breastfeeding with a new mom who asked me for help after struggling to get the baby to latch on the labor and delivery unit during my clinical experience.
“Luckily, I had an amazing instructor named Shannon who defended me by saying that nurse gender should not affect the fact that I was going to be a nurse and it was my job to help patients and educate them.”
Another of the barriers to seeking an education in nursing is the need to earn while you learn. It’s tough to hit “pause” on work to focus solely on the rigorous studying required to complete a nursing degree. Pew
$30,000 from Excellus
Mohawk Valley Prenatal & Maternal Support (MVPMS) has received a $30,000 Health Equity Innovation Award (HEIA) from Excellus BlueCross BlueShield to support its Sister Circle: Black Birth & Breastfeeding Initiative (SC3BI) program.
The awards program provides financial support to community programs that address racial and ethnic health disparities across Excellus BCBS’s Upstate New York service area.
Sister Circle is a birth and breastfeeding initiative which provides and promotes doula services to women of color, with the goal of improving birth rates, birth outcomes and providing breast feeding and post-partum support.
“We are thankful to Excellus BCBS for providing us with a Health Equity Innovation Award which will strengthen our Sister Circle program and provide vital support to women of color in our community,” said MVPMS Program Director, Ashley
Engram. “Our program will have an impact on birth outcomes and birth rates among black women in our area for years to come because we are focusing on long-term solutions and introducing new doulas into the community.”
As part of the program, MVPMS will provide culturally sensitive doula training to 10 women of color who are passionate about childbirth and breastfeeding. The course, which will be taught by DONA International Certified Doula Trainers, will train the women to be both birth doulas and includes lactation (breastfeeding counselor) support training.
Doulas are non-medical professionals who are trained to provide physical, emotional & informational support to assist and advocate for patients and their families. In the pregnancy setting, doulas provide emotional and informational support. They provide physical support and unbiased, nonjudgmental support during labor/delivery and assist with breastfeeding initiation imme-
Research reveals that women are the primary breadwinner in only 16% of US households and men are the primary or sole breadwinner in 55% of them.
Of course, women who work full time also benefit from hybrid, weekend and online classes. However, the social stigma of quitting work to go to school is less for women than men, as women often take time away from work for family care giving duties. Traditionally, women aren’t expected to serve as the family’s main wage earner.
More nursing schools than ever offer night, weekend, online and hybrid classes to make access to an education easier. Many of the resources and textbooks are also online, which can help people who are working to
fit in study time when they can.
For Jeremy Donohue, registered nurse in the emergency department at Oswego Health, attending nursing school while still working made possible the shift from military medic to civilian nurse. He is still working on his bachelor’s degree while enlisted as a National Guardsman and working as a nurse.
He believes that many men feel drawn to the emerging roles in nursing including leadership positions. Emphasizing the science and technical aspects of nursing also helps draw more men to nursing.
“It’s almost a ‘STEM’ field that’s very science-based with specialized medication and maybe that appeals more to the male side of things,” Donohue said.

diately after delivery. Doulas provide continuity of care by providing emotional and informational support during the post-partum period.
After completing their training, the new doulas will partake in monthly business mentorship sessions for six months and be paired with 10 pregnant women of color.
“The doulas and the expectant mothers will attend Sister Circles hosted by members of MVPMS to discuss issues within pregnancy, fears and concerns about their up-
coming labor/delivery experience and breastfeeding goals,” Engram explained. “The program will then follow up and monitor these women through their post-partum period to gauge the results and provide additional support.”
MVPMS is one of 20 nonprofit, 501(c)(3) organizations from across Excellus BCBS’s Upstate New York service area including the Rochester, Central New York,
Country, and Southern Tier regions who received HEIA funding.

Julie Rose, 46, is a nurse for Bassett Healthcare Network.
Bassett is a health care system offering comprehensive, integrated care. It is comprised of five hospitals, including Bassett Medical Center in Cooperstown and four regional hospitals, including the Little Falls Hospital; one stand-alone emergency department; more than two dozen outpatient clinics, more than 20 school-based health centers, the Bassett Cancer Institute, pharmacies, long-term care facilities, home health and research. It covers an eight-county area.
Rose works part-time in the Co-
bleskill Outpatient Clinic, a specialty unit, and part-time providing nurse orientation and other workshops focusing on the well-being of nurses. She explained what it’s like to be a nurse at Basset.
Q: How did you become interested in a career as a nurse?
A: I went back to school to become a nurse when I was 33 years old. Before then, I worked in marketing, selling condos, etc.
I became interested in becoming a nurse when I cared for grandfather as he died. I noticed that other members of my family couldn’t do some
of the tasks that were necessary, but I didn’t mind these tasks. I like caring for him.
Vermont Technical College in Randolph, Vermont, is where I received my associate RN degree. I never worked in Vermont as a nurse; after school, I moved to New York where I began my nursing career.
Bassett paid for me to get my BA degree and helped me get my master’s degree in nursing education. I’m also a certified holistic nurse. I like working for Bassett.
Q: What do you do in your employment as a nurse?
A: Three days a week, I work in the Cobleskill Outpatient Clinic, with several specialty units. Today I’m working in pediatrics, another day I’ll work in orthopedics, another day in women’s health care. We switch the unit we work in every day. That makes it fun; I like that variety.
One day a week I do education at Cooperstown. I do workshops for nurses, a new nurse orientation and workshops that focus on nurse well-being. Burn-out is a big issue, especially since COVID. Before COVID, I had a yoga studio. Yoga is my passion, but when COVID hit, I had to close it. I do yoga in the workshops I give for the well-being of nurses.
I’m also responsible for Bassett’s DAISY Award program which recognizes nurses for their exceptional care on a quarterly basis.
Q: What are the rewards of your position?
A: I get to do so many different things. I’m working with the things that I’m passionate about. I’m able to bring it all together, combine all my passions. Working here is fun.
I especially like what I do with the DAISY awards. Our nurses here are amazing people; they’re so inspiring; it gives me hope. Basset has the entire network involved in this program.
Q: What are the challenges of your position?
A: The challenge is finding time
to do all the things I have to do. I love the job. Fitting it all in is the most challenging.
Q: What are the things that are especially important for nurses to know?
A: I do presentations on mindfulness and self-care. I encourage nurses to speak up and take care of yourself. It’s also important to recognize how we feel stress in our bodies. Listen to these signs, so before stress overwhelms you, you can do something about it.
With the nurse orientations, I’m dealing with our brand-new nurses, who are new to the field, as well as those who are experienced and are just new to Bassett. I find the new nurses are ‘gung-ho,’ enthusiastic about their careers, eager to sign up for many shifts, taking on additional responsibilities. This will overwhelm them. Many have a fear of saying no. I teach them how to set health boundaries and that it’s OK to say no. Even necessary.
In nursing school, we were taught to celebrate those nurses who don’t take time to eat lunch, who don’t even take time to pee. Instead, we should celebrate those who do take time to care for themselves.
Nurses have an internal caregiver. It is beautiful. In addition to being a nurse, most are dealing with motherhood and a partner; there’s nothing left at the end of the day. This is not OK.
Q: What is the most important thing for a nurse to know?
A: The one thing that I’d like nurses to know: There are so many options. I’m not an adrenaline nurse who likes ICU nursing or med-surg nursing; that’s not for me. I’ve found my passion by trying out different things. So many nurses leave the field. Instead, find something different to do; Basset facilitates that.
There’s an array of nursing careers. If you’re not happy in the one you have, seek another.

Though the pandemic is now endemic, one of its many lasting effects is even worse staffing issues in healthcare than before.
Add to this combative patients, long hours, changing shifts, emotionally stressful work and plenty of physical challenges and it’s little surprise that nurses face high risk for burnout.
“Nurses work in an inherently stressful industry, doing work that is oriented towards caring for others,” said nurse Kerryanna Elhage. “Historically, our nursing education programs haven’t taught us to care for ourselves although fortunately this is slowly improving.”
Elhage, who is the manager of pediatric hematology-oncology and nephrology at Upstate Golisano Children’s Hospital, said she believes that it is “important we learn how to care for ourselves.”
One way is finding harmony between work and home life, along with “nourishing ourselves with healthy activities, nutritious food and engaging in fun social activities are essential elements for balance.
Melissa Gotte, 55, is a nurse in the ICU at Rome Health Hospital. Rome Health Hospital began as a small hospital, serving 19 patients when it opened in 1884. It evolved into Rome Memorial Hospital. In 2021, Rome Memorial Hospital adopted Rome Health as its new name to more accurately reflect the scope of services provided as a health network. It has 129 beds and 80 beds in a skilled nursing facility.
We wondered what it was like to be an ICU nurse at Rome Health and spoke with Gotte.
Q: How did you become interested in a career as a nurse?
A: It evolved. I don’t want to use the word “calling;” my career just evolved. I was always taking care of others: as a big sister, I cared for the younger kids; I was a babysitter.
Then when I was living in Fort Bragg, North Carolina, I decided I wanted to go to college. I came back to New York and became a medical assistant. I worked for an OB-GYN for 10 years. I loved that job. The doctor encouraged me to become a nurse.
I got my two-year nursing degree from MVCC — that was normal in those days; that’s the degree most people got. My goal now is to get my degree as a registered nurse; Rome Health will help with this: I like Rome Health a lot.
Q: How did your nursing career begin?
A: I started at St. Luke’s Hospi-

tal. I began in an intermediate unit where we had four patients to one nurse. When that unit closed, I had to make a decision about where to work. I made the decision to work in the ICU, though I was nervous about working in intensive care when I started.
After 23 years at St. Luke’s, I retired. For 17 of those years, I worked in the ICU.
I started in the Rome Health ICU four or five months ago. When I started working there, I was just overwhelmed because they were all so friendly.
I’m so lucky to be working there in the ICU; I love it here! I’m so happy in my job. We’re like a family in the ICU. Rome Health is growing and I’m happy to see that. They treat employees like family.
(Note: Regarding Rome Health is growing: In November 2023, work began to construct a 30,000-squarefoot, three-floor addition on the north side of the hospital, which will allow the hospital to replace its aging operating rooms and intensive care units.)
Q: What are the rewards?
A: When it’s good, it’s really good; when it’s bad, it’s really bad. There are highs and lows. What I especially like is that you’ve got coworkers; we help each other get through the bad parts. The ICU workers are like a family. I’d never work anywhere else.
Also, l like that every day is different. You never know what to expect each day.


Q: What are the bad parts?
A: It’s especially hard when we have a young person who is dying. Cancer is the worse. You do everything you can, but it’s still gut-wrenching. Sometimes heart breaking.
One thing that helps me get through is what I was told once by a nurse when I worked in the ER. A baby came in as her face had been bitten by a dog. I had to put an IV (intravenous line) in her; she was crying and so distressed. I’m thinking to myself: “I’m causing her pain. I can’t do this.” But a nurse told me “You’ve got to do what you’ve got to do!” I did need to put in an IV so she could get antibiotics or she could get an infection. I was causing her pain, but
ways to cope. To prevent this and the negative outcomes of unhealthy coping, Tracy Carmody, licensed mental health counselor and master credentialed alcohol and substance abuse counselor, encourages engaging in self-care.
“At its core it can be some basic activities like going to the grocery store and making sure you have food for the week,” Carmody said.
She serves as executive director and owns Paths To Recovery Mental Health Counseling, PLLC, in Baldwinsville and Manlius.
“Selfcare is deliberate,” Carmody added. “It’s easy to compromise yourself when you’re giving to others. Compromising self-results in less than exceptional patient care. Drug and alcohol use among nurses can be higher because of that reactive nature.”
it was necessary. It was what I had to do. Ultimately, she was fine.
I often remember what that nurse told me that day: You’ve got to do what you got to do. That’s hard, but you do it because you have to.
Q: What characteristics does it take to do the important job you do?
A: Of course, it takes compassion, caring about people, concern for them. It takes the ability to put yourself in their position, to feel what it’s like for them, to understand what they’re going through. And it takes intelligence.
Being strong is important. You have to be strong. You have to be able to face your fears and do what you’ve got to do for that person. Sometimes that’s rough.
that checking in even once a month can make a big difference in mental health.
While some people may think that self-case is about getting facials and things like that, Carmody said it goes deeper, like getting enough sleep.
“The system is set up to create patient fatigue,” Carmody said. “There’s patient abandonment if a patient needs them. But there are ethical requirements to engage in self-care to provide good care and minimize mistakes.”
She also encourages nurses to exercise to combat stress, as it can help with both physical and mental health.
Some nurses who are starting to feel the effects of stress may not even realize it. Carmody calls it “tunnel vision.”
“Additionally, nurturing positive emotions and a resilient, adaptive mindset can be key to avoiding burnout,” she said. “Happily, we are living at a time where resources such as mindfulness and meditation apps and classes, yoga and other somatic
exercises and in-person or online therapies are easily accessible.”
Elhage noted that nurses at Upstate can access numerous resources to help with self-care and wellness.
Unfortunately, some nurses turn to substance use and other unhealthy
It takes time to work through emotional trauma and nurses use substances to turn off the emotions it stirs up. It’s maladaptive, but it’s faster. Seeking mental healthcare can help deal with workplace trauma in a healthy way. Carmody said
Processing stress with someone else can help ease its effects. Whether a professional therapist or trusted friends, emotional support can assist in diffusing stress.

Tuberculosis cases are on the rise in the United States, with the number of reported infections in 2023 the highest seen in a decade.
Forty states, including New York, logged an increase in tuberculosis (TB) cases, and rates were up among all age groups, the study from the U.S. Centers for Disease Control and Prevention found. More than 9,600 cases were reported, a 16% increase from 2022 and the highest since 2013.
"Although TB incidence in the United States is among the lowest in the world and most U.S. residents are at minimal risk, TB continues to cause substantial global morbidity and mortality," the researchers wrote in the March 28 issue of the CDC publication Morbidity and Mortality Weekly Report.
"This post-pandemic increase in U.S. cases highlights the importance of continuing to engage communities with higher TB rates and their medical providers in TB elimination efforts and strengthening the capacity in public health programs to carry out critical disease control and prevention strategies," they added.
Experts point to a surge in TB cases internationally — the World Health Organization has said TB was behind only COVID-19 in infectious fatal diseases worldwide in 2022, the Associated Press reported. There have also been big spikes in migration and post-pandemic international travel, which likely fueled the spread of TB.
But other factors are at play, including other illnesses that weaken the immune system and allow latent TB infections to surface.
The 2023 count “was a little more than was expected,” physician Philip LoBue, director of the CDC's Division of Tuberculosis Elimination, told the AP.
Tuberculosis is caused by bacteria that attack the lungs, and is spread through the air when an infected person coughs or sneezes. If not treated properly, it can be fatal, according to the CDC.

Arecently released Danish study of 570,000 people over 14 years identified untreated hearing loss as increasing the risk for dementia compared with people with no hearing loss or those with treated hearing loss.
The study doesn’t surprise geriatrician Sharon A. Brangman at Upstate Medical University.
“Alzheimer’s is complex,” said Brangman, who is a distinguished service professor, chairwoman of geriatric medicine and director of the Upstate Center of Excellence for Alzheimer’s Disease and director of the Upstate Center of Excellence for Alzheimer’s Disease.
“It is a neurodegenerative disease. Nerve cells are dying. When you lose hearing, nerve cells are dying. A combination of things is happening that can increase your risk of Alzheimer’s. It’s never just one thing but a combination.”
The correlation between untreated hearing loss and a higher risk of Alzheimer’s has to do with brain changes. Those with untreated hearing loss receive less auditory stimuli than those with good hearing. Brangman said that the center of the brain that helps people interpret sound and connect it to a memory gets less use if the person isn’t hearing as much around them.
“That can increase disassociation with the world around you,” she said. “Research is looking at changes in the retina that may have association with a higher risk of Alzheimer’s. It’s all connected to what’s happening in the brain.”
During the pandemic, many older adults become more isolated as during the quarantine period and following, they stayed away from social gatherings to avoid catching COVID-19. Brangman said that she noted an increase in cases of dementia and cognitive decline as sensory
deprivation and lack of regular socialization were commonplace.
“There are many layers to making a diagnosis of Alzheimer’s and talking with people about their risk of developing Alzheimer’s disease,” Brangman said. “There are things we can do to reduce that risk. If someone has hearing loss, we recommend hearing aids and if they have visual problems to get their eyes checked. Sensory input is so important for brain health.”
Introducing hearing aids earlier can also make their use more effective so that the brain becomes accustomed to their input. For those who would develop cognitive decline, earlier adoption of hearing aids to treat hearing issues can delay onset of dementia by seven years.
Clayton Andrews, board-certified hearing instrument specialist at Upstate Hearing Solutions in Oswego, said that the Danish study draws “a very solid correlation. The latest data coming out of John Hopkins that the more severe your untreated hearing loss is and the longer it goes, the more likely you will be diagnosed with dementia. I see a correlation between dementia and untreated hearing loss.”
He said that many people delay treating their hearing loss because they don’t realize they have a hearing loss. Typically, family members notice before the patient himself.
Some people believe that hearing instruments are too costly for them to afford. Andrew related that most insurance companies offer up to 100% coverage, which wasn’t the case 30 years ago.
“I implore people to get help,” Andrews said. “It will change their life. It breaks my heart when they don’t. God gave us eyes and ears for one reason or another. They’re kind of important.”
Unfortunately, many people wait

Geriatrician Sharon A. Brangman works at Upstate Medical University. “[Alzheimer’s] is a neurodegenerative disease. Nerve cells are dying. When you lose hearing, nerve cells are dying. A combination of things is happening that can increase your risk of Alzheimer’s. It’s never just one thing but a combination.”
eight to 10 years before treating their hearing problem, according to Doug Brown, audiologist and owner of DB Audiology Associates, PC in Syracuse.
By leaving hearing loss untreated, people “tend to withdraw more socially,” Brown said. “It’s a matter of clarity of speech. People have a tendency to withdraw because they don’t want to be put in that position of not understanding. You may make those changes to withdraw unconsciously. As you’re isolated and not interacting with friends and being challenged to think of different things, the cognition does change.” Brown thinks that many people choose to delay treating their hearing loss because of stigma of using hearing aids as something for “old people.” However, hearing aids help improve the lives of people of all ages.
“I’d say that fear of dementia shouldn’t be the reason you get a hearing aid,” Brown said. “It should be so you can participate in those important activities of life that you want to participate in. The other side effects of improved cognition and slowing down of dementia are nice side effects. The reason you get a hearing aid is to hear better.”
Approximately 15% of adults in the U.S. have trouble hearing, according to the National Institute of Health, part of the U.S. Department of Health and Human Services. For those older than 70, 65% have hearing loss. An estimated 12.5% of children have hearing loss.
Hearing loss is frustrating for those who have it and for their loved ones.
It is linked with problems with balance and walking, falls, depression, even dementia.
Mild hearing loss doubles the risk of dementia. Moderate loss triples the risk and people with a severe hearing impairment are five times more likely to develop dementia.
Yet only about one-third of those with hearing loss wear hearing aids, according to JAMA.com (Journal of the American Medical Association). Most wait too long to act, coping as best they can, hoping that their hearing will improve. Sadly, it never does. It just gets worse.
With the rate of hearing loss in the U.S. expected to almost double in the next few decades, we wanted to understand more about hearing loss and what prevents people from seeking treatment. We asked Robert Bishton, board-certified hearing instrument specialist, for answers.
1.What Causes It?
A: In addition to aging, there are several other causes of hearing loss. Hearing does weaken as you grow older. Some illnesses and injuries can cause hearing loss. Earwax buildup can harden and this blockage can affect hearing. Don’t try removing the wax yourself; see your primary care provider. Hearing loss is a side effect of some medications, including certain antibiotics and
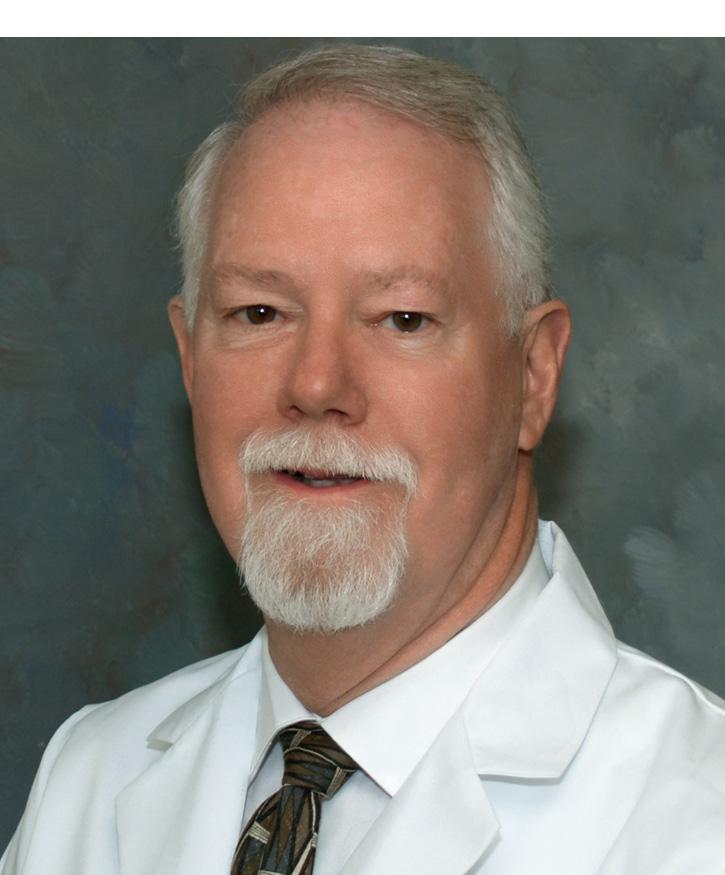
 Robert Bishton, board-certified hearing instrument specialist.
Robert Bishton, board-certified hearing instrument specialist.

cancer drugs. Regular use of aspirin, ibuprofen and acetaminophen may increase the risk of hearing loss.
Long-term exposure to continuous loud noise can cause lasting hearing loss. If you work in a loud environment, use power tools or a motorcycle, wear earplugs.
A: Most people don’t know when they need hearing aids. Studies have shown it takes seven to 10 years for someone to even consider hearing aids. More often than not, it’s a spouse, family or friends complaining to them that drives them to first look into hearing aids. People often don’t realize how poor their hearing was until they hear again.
3.Why Are People So Hesitant to Get Hearing Aids?
A: I’ve found that people today are far less hesitant than they
were 20-25 years ago. It used to be we didn’t see anyone considering hearing aids until they were in their late 60s or early 70s, but today we’re seeing people in their 40s stepping up and doing something about their hearing loss.
The old age stigma isn’t the big deal it used to be and people are far more educated about hearing loss today, especially the connection between untreated hearing loss and cognitive decline.
Hearing aids today are fantastic; they’re small. Nobody even notices or cares. A person would rather have a face-to-face conversation with you when you’re not going ‘Huh?’ or asking you to repeat yourself.
4.Why Should I See a Hearing Professional?
A: There’s so much more to just buying a pair of hearing aids. If someone is looking for cheap, they
Six out of every 10 stroke survivors wind up struggling with depression later in their lives, a new study says.
That compares to the 22% depression rate of the general population, results show.
Further, nine of 10 stroke-related depression cases occur within five years of surviving a stroke, researchers found.
“Depression is common in stroke survivors but our research shows it persists for much longer than previously thought,” researcher Yanzhong Wang, a professor of statistics in population health at King's College London, said in a news release.
Biochemical changes in the brain caused by stroke injury can contribute to depression by interfering with a person's ability to feel positive emotions, according to the American Stroke Association.
For the study, researchers reviewed the cases of 6,600 stroke survivors whose data appears in a South London stroke registry.
Results showed that severe depression tended to occur earlier after stroke, lasted longer than expected, and was quicker to recur than cases of mild depression.
Depression among stroke survivors can affect their mobility, hampering simple tasks like walking
buy an OTC, which is typically just an amplifier found in drugstores or Walmart, but the success rate is very low. Don’t be fooled by purchasing online.
Purchasing online can be better than an OTC but not as inexpensive as you might think. In fact, you can pay nearly as much as you would visiting an audiologist or hearing professional. An audiologist or hearing professional offers the counseling and instruction that is vitally important to success.
In a one-to-one office visit, we provide an accurate hearing test (audiogram), a precision fit with the correct domes or molds to match the hearing loss and precise adjustment.
Additionally, the number one reason for hearing aid failure is wax buildup in the receiver. Without a professional to assist you in how to clean, service and change wax guards, the hearing aids will fail and you’ll give up wearing them. Even with proper instruction, people are hesitant to change these out on their own.
A: Simply put… if you have to yell to converse, your hearing is in danger. Anytime you are using a lawnmower, a chainsaw or attending loud concerts the potential to exposure for hearing loss is there. Wearing hearing protection is a must.
If you have hearing loss, don’t accept it! If you’re losing your hearing, get it diagnosed and treated. Get treated and live life to the fullest.
Experts recommend that everyone have their hearing tested once a year, to identify issues early on and treat them before they become a severe problem.
and holding objects, Wang said. It also can increase their overall risk of death.
“Quality of life is important for stroke survivors as there is evidence depressed survivors have a reduced survival rate,” researcher Lu Liu, a doctoral candidate at King's College London, said in a news release.
“There are many reasons why this could be, including disruptions to the survivor's social life, reduced physical ability and inflammatory disorders observed in depressed patients,” Liu added.
Doctors need to pay particular attention to stroke survivors who have depression that lasts longer than one year, “because of the high risks of experiencing persistent depression,” Liu said.
If any of you are “Outlander” fans, you will remember these words as part of the quote of the Celtic wedding vows.
I use this quote not only as an “Outlander” fan but also because our bones are the support of our bodies. Much like the foundations of a marriage, paying attention to your bodily structure requires much consideration.
To return to today’s discussion of “bone of my bone,” you need to look at your body and the best ways to care for your bones. It is never too late to be diligent and work to improve your bodily structure reducing the risk of falls and fractures. With aging, you want your bones to be as strong as possible. If you haven’t been kind to your body, it is never too late to begin. Osteoporosis, a condition in which bones become weak and brittle, can be prevented keeping you strong and self-reliant.
Physical movement is a must. Exercise and physical movement are an important lifestyle change and a necessary one in taking care of you in the best way possible.
Do establish achievable goals and be realistic. A fitness assessment can help determine your goals after examining the results.
Speak with your healthcare provider or physical therapist or personal trainer to point you in the direction of a good assessment tool, and follow through with the results and necessary changes.
For seniors (and actually everyone), exercise is anti-aging. Exercise will help lubricate joints, increase
By Deborah Dittnermobility and decrease overall inflammation.
Resistance training and strength training boosts the growth of new bone tissue. By adding 30 minutes three or four times a week of simple movements such as squats and pushups (using your own body weight) and bicep curls (using weights starting with filled water bottles or soup cans and progress to other handheld weights), you will improve not only bone but overall health as well.
Working with a trained professional, especially if you have osteoporosis or other bone disease, is a must. Modifications can always be made and will help strengthen you as you move forward. Cardio activity such as brisk walking and hiking can also support the building of new bone growth.
Throughout physical movement you want to also work on maintaining good balance and proper posture.
Yoga comes in a variety of styles and one pose that assists in balance is tree pose. Holding tree pose for two minutes on each side daily is helpful. A good time to do tree pose is while brushing your teeth — one side in the morning and the other in the evening. Plank is another movement increasing core strength (abs, back, hips and butt), lower back strength and encourages good posture.
Of course, you can’t talk about bone health without eating whole nutrient-dense foods. Bone building nutrients needed every day consist of vegetables, fruits, whole grains, healthy fats and protein.
Some examples: dark leafy greens, beans and canned fatty fish

such as salmon (high in calcium); eggs and other fatty fish (high in vitamin D — don’t forget to get out in the sun, too!); nuts, seeds, dark leafy greens and fatty fish (great sources of magnesium). Eating a variety of plant foods also aids in good gut bacteria. Eating anti-inflammatory foods such as berries helps in supporting bone heath as well. If you’re eating enough food, you are more than likely getting enough protein. To make sure of your nutritional needs, consult with a health coach or nutritionist to discuss what you eat daily and what you can add to make your nutrition top notch in supporting your bone health.
Maintaining physical activity and eating whole nutrient-dense foods

Adaily multivitamin could help people keep their brains healthy as they age, a new trial finds. Results suggest taking multivitamins could help prevent memory loss and slow cognitive aging among older adults, researchers report in the Jan. 18 issue of the American Journal of Clinical Nutrition.
The effect was measurable: A
daily multivitamin slowed brain aging by the equivalent of two years compared to placebo.
Still, experts expressed some skepticism, and wondered if simply eating healthy might not bring about the same results.
“Taking a multivitamin supplement is probably good for you, but we don’t know if it’s likely to have a big impact in people who have
a healthy diet,” physician Richard Caselli, a professor emeritus of neurology at the Mayo Clinic in Arizona, told NBC News.
“I still maintain a bit of skepticism as far as what magnitude of impact this makes,” he added. “I’m doubtful the difference would be really big.”
The new study was led by physician Chirag Vyas, an instructor in investigation at Massachusetts General Hospital’s department of psychiatry.
“Cognitive decline is among the top health concerns for most older adults, and a daily supplement of multivitamins has the potential as an
will provide you with the assurance to do everything you want to do for your long life ahead.
Be patient with yourself as results don’t happen overnight. Encourage a buddy to join with you — the more the merrier!

Deborah Dittner is a family nurse practitioner and health consultant. Her mission is to transform as many individuals as possible through nutrition and lifestyle changes. www. debdittner.com
appealing and accessible approach to slow cognitive aging,” he said.
The Cocoa Supplement and Multivitamin Outcomes Study (COSMOS) is a large-scale, randomized trial performed in collaboration by Massachusetts General Hospital (MGH), Brigham and Women’s Hospital, Columbia University and Wake Forest University. It looked at whether a special cocoa extract supplement, a daily multivitamin (in this case Centrum Silver) or both might help boost health.
The clinical trials were funded by the National Institutes of Health and candy and snack manufacturer Mars Inc. Pfizer donated both the multivitamins and placebo tables used in the trials. Neither company had any role in the design of the trials.
Analysis of more than 5,000 participants in three separate, but related, COSMOS clinical trials found strong evidence of benefits for both brain function and memory from taking daily multivitamins for two to three years, researchers said.
“The meta-analysis of three separate cognition studies provides strong and consistent evidence that taking a daily multivitamin, containing more than 20 essential micronutrients, helps prevent memory loss and slow down cognitive aging,” Yvas said in a MGH news release.
Dear Savvy Senior,
Can you help me identify some good senior living communities that offers all levels of housing and care from independent living to nursing home care? I am in my late 70s and know I need to downsize from my current house, but I want my next move to be my last.
One Move Mary
Dear Mary,
If you want your next move to be your last, an all-inclusive retirement community — also known as a continuing-care retirement community (or CCRC) — is a great option to consider.
Here’s what you should know, along with some tips to help you locate one.
CCRCs are different from other types of senior housing because they provide all levels of housing, services and care in one convenient location.
While the appearance and services of CCRCs can vary greatly, most provide apartments or sometimes single-family homes for active independent seniors. In addition, they also offer onsite assisted living for seniors who require help with basic living tasks like bathing, dressing or going to the bathroom, and nursing home care for residents when their health declines.
CCRCs also provide a variety of resort-style amenities and services that include community dining halls, exercise facilities, housekeeping and transportation, as well as many social and recreational activities.
But be aware that all these services come at a hefty price. Most communities have entry fees that range from less the $100,000 to more than $1 million, plus ongoing monthly fees that generally range from $2,000 to $5,000 for singles ($3,000 to $6,000 for couples) depending on the facility, services and the contract option you choose.
With more than 2,000 CCRCs in operation throughout the U.S, finding a facility that fits your lifestyle, needs and budget will require some legwork. Here are some steps that can help you proceed.
• Make a list: To find CCRCs in the area you want to live go to “MyLifeSite.net” and “Caring.com,” which provide online lists. Once you’ve located a few, call them to find out if they have any vacancies,
what they charge and if they provide the types of services you want.
• Take a tour: Many CCRCs encourage potential residents to stay overnight and have a few meals in their dining hall. During your visit, notice the upkeep of the facility and talk to the current residents to see how they like living there. Also, check out the assisted living and nursing facilities, and find out how decisions are made to move residents from one level of care to another.
• Do some research: While on your tour, find out who owns the CCRC and get a copy of their most recently audited financial statement and review it. Also find out their occupancy rate. Unless it’s a newer community filling up, occupancy below 80 percent can be a red flag that the facility is having financial or management problems.
To investigate the CCRC’s longterm care services call your state long-term care ombudsman (see “LTCombudsman.org” — type “New York” in the search menu) who can tell you if the assisted living and nursing care services had any complaints or problems. You can also use Medicare’s nursing home compare tool at “Medicare.gov/care-compare.”
• Understand the contract and fees: Most CCRCs offer three types of contracts: life-care, or type A contracts, which have the highest entry fee but covers all levels of long-term care as needed; type B, or modified contracts that have lower entry fees but limits long-term care services in the initial fee; and type C, or fee-forservice contracts, which offer the lowest entrance fees but requires you to pay extra for long-term care if you need it.
You also need to find out what yearly price increases you can expect? How much of your entry fee is refundable to you if you move or die? And what happens if you outlive your financial resources?

Walk-ins welcome
555 French Rd., Building 2 in New Hartford
To help you sort through all this, consult with your financial adviser or lawyer before committing. When you need lab work, we’re in New Hartford

Send your senior questions to: Savvy Senior, P.O. Box 5443, Norman, OK 73070, or visit SavvySenior. org. Jim Miller is a contributor to the NBC Today show and author of “The Savvy Senior” book.
Open Monday through Friday, 7:30 a.m. to 4 p.m.
Prompt, courteous and no appointment needed. Learn more at laboratoryalliance.com

We thank our nurses at Upstate Caring Partners for their continuous support and for positively impacting the lives of individuals every single day.

It allows doctor to change the prescription of a lens that’s been already placed inside your eye
By Barbara Pierce“It’s remarkable! Remarkable technology!” is how Alexander Harris, ophthalmologist and president of Slocum-Dickson Medical Group, describes the lens that recently became available to correct cataracts.
What’s so remarkable is that there is now a lens implant that allows eye doctors to customize a patient’s vision after cataract surgery. The doctor can change the prescription of a lens that’s been placed inside your eye. It’s state-of-the-art vision correction.
“In traditional cataract surgery, we gave it our best guess which lens to implant,” Harris explained.
In traditional cataract surgery, the lens with the cataract is removed and replaced with an artificial lens. These lenses reverse the effects of cataracts and improve vision. The lenses come in different focusing powers, just like prescription eye glasses. But
before the surgery, the eye surgeon had to guess at the focusing power for the new lenses, according to Harris.
That resulted in the fact that most who received these standard lenses, with the focusing power that the doctor guessed at, still needed glasses or contacts to read or correct astigmatism. Once implanted those lenses can’t be changed; they’re what’s known as ‘”fixed.”
The new adjustable lens is the first and only adjustable lens that can be customized to refine your vision after cataract surgery.
“The lenses we implant now are like fitting a suit to your specific body,” Harris said. “You test drive your new lens after surgery, see how it works for you. For example, you might want one eye for reading, the other for distance. It’s the best of both worlds!”
After your cataract surgery, to-

gether with Harris, you will have the ability to adjust the lens and optimize your vision based on your unique preferences and lifestyle requirements.
Cataract surgery is the mostperformed procedure in the U.S., according to JohnHopkinsMedicine. org. The majority of us will develop cataracts by age 75. If left untreated, they can cause blindness. Cataracts form when the proteins and fibers in your eye’s natural lens begin to break down, causing hazy or cloudy vision. Once begun, cataracts only worsen until surgery is necessary. They impair vision and make everyday activities increasingly difficult.
Symptoms of cataracts include clouded, blurred or dim vision, trouble seeing at night, need for brighter light for close activities, seeing halos around lights, double vision in one eye, sensitivity to light and glare.
If you have cataracts in both eyes, each eye is usually done on separate days. Typically, cataract surgery is performed while you are awake, though not until numbing eye drops have taken effect so that you don’t feel discomfort.
Cataract surgery has advanced over the years and the new lenses used by Harris are a big step for-

ward, according to the doctor. Called RxSight Light Adjustable Lens, they have been approved by the FDA. Initially approved in 2017, modifications were approved in 2021.
“They allow me to provide my patients the most precise outcome from cataract surgery,” said Harris. “With these lenses, I can administer a more customized treatment to match my patient’s individual needs.”
The prescription can be adjusted after it is implanted, helping patients achieve the clearest far, near and intermediate vision possible.
During the month after cataract surgery, Harris works with his patients until they’re satisfied that they’ve achieved the best possible vision.
“It requires a few extra visits, but these are the fun visits while we’re modifying and refining your vision. “It requires three extra visits to Harris lasting only a few minutes, he added.
The new lenses are adjusted through targeted ultraviolet light treatments which are totally painless and take only a few minutes. The RxSight Light Adjustable Lens is made of special photosensitive silicone material that undergoes subtle changes in lens power and shape when exposed to carefully dosed ultraviolet light. This technology lets your Harris adjust your lens power and curvature to better address myopia, hyperopia and even astigmatism.
These subtle changes can impact the sharpness of your vision at various distances. Following each UV light treatment, Harris will ask for feedback after you’ve lived with the vision “tweak” for a couple of days to see if it improves your visual experience.
Sadly, for those who have already had cataract surgery, there’s no going back for the new lenses.
“Once you’ve had cataract surgery, you’re set,” said Harris.
Medicare and insurances do not cover the new lenses at this time.
“Hopefully they’ll be covered in the future,” added Harris.
Harris is the only surgeon in Oneida County to offer the Light Adjustable Lens to patients.












The Community Memorial

Hospital (CMH) announced it has hired Jackie Ireland, a certified physician assistant (PA-C) who will work alongside physician Kamaljeet Banga in both the outpatient and operating room settings. Ireland joins the CMH team with over a decade of experience, with specialized support in orthopedic spine surgery. She holds certifications with the National Commission on Certifications of Physician Assistants, and is professionally affiliated with the American Academy of Physician Associates (AAPA) and the NYS Society of Physician Assistants (NYSSPA).
Graduating from Le Moyne College with a Bachelor of Science in biology and also a Master of Science in physician assistant studies, Ireland has worked in Central New York in a busy orthopedics and spine surgery setting..
“I chose to join the Community Memorial network because of the close feel of the hospital and orthopedics group. I look forward to providing collaborative care with a practice that offers a variety of sub-specialties and superior orthopedic care,” she said.
Ireland comes to the CMH family as a new location for the orthopedic practice was just opened. Situated on the hospital campus as the new Center for Specialty Services building, the Center for Orthopedic Services moved in early 2024 to fit

the need for expanded patient care space along with a growing team of providers.
“Our medical staff welcomes Jackie Ireland as an esteemed member of our team, bringing expertise and a passion for orthopedic care,” said Michael Walsh, chief medical officer. “She provides a great skill set in education and knowledge with the goal of collaborative community-based care.”
Slocum-Dickson Medical Group’s podiatrists Kimberly Hurley and Christopher Powers are now conducting minimally invasive bunion surgery.
This innovative approach to correcting bunion deformities, provides faster recovery time, less pain and minimal scarring.
Bunions form at the joint of the base of the big toe. There are various ways to ease the pain from bunions, however, the most successful fix for painful bunions is surgical. Traditional bunion surgery involves a large incision and a lengthy recovery time. Minimally invasive bunion surgery requires tiny incisions and offers faster bone healing and a quicker return to activities.
“By offering minimally invasive bunion surgery, patients are returning to their normal lifestyle faster,” said Hurley. “They experience significantly less pain and recover much faster.”
“The smaller incisions in minimally invasive bunion surgery provides faster recovery and minimal scarring, all while improving patient mobility,” said Powers.


Representatives from Excellus BlueCross BlueShield recently visited On Point for College in Utica to present a $2,500 Health and Wellness Award. The funds will be used for the program’s Mental Health Support in Safe Spaces for First-Generation College Students program, which provides mental health workshops
for college students and quarterly trainings for front-line advising staff to improve their empathy, advocacy, and listening skills as well as their understanding of mental health issues. The program will also provide Safe Space and NARCAN training to the entire staff, to serve students’ needs.

Hybrid Nurse Aide Training Program
ELEMENTAL MANAGEMENT GROUP
Hybrid Nurse Aide Training Program ELEMENTAL MANAGEMENT GROUP
Hybrid Nurse Aide Training Program ELEMENTAL MANAGEMENT GROUP
ELEMENTAL MANAGEMENT ROUP






Hybrid Nurse Aide Training Program ELEMENTAL MANAGEMENT GROUP



Equip your facility with our unstoppable HYBRID CNA program, empower your team to deliver top-notch care with the strength of a champion.
Equip your facility with our unstoppable HYBRID CNA program, empower your team to deliver top-notch care with the strength of a champion.
Equip your facility with our unstoppable HYBRID CNA program, empower your team to deliver top-notch care with the strength of a champion.
Are you looking for an innovative way to attract CNA students? We have your answer
Equip your facility with our unstoppable HYBRID CNA program, empower your team to deliver top-notch care with the strength of a champion.
Are you looking for an innovative way to attract CNA students? We have your answer
Are you looking for an innovative way to attract CNA students? We have your answer
Are you looking to minimize and most importantly eliminate agency use? We have your solution
Are you looking to minimize and most importantly eliminate agency use? We have your solution
Are you looking for an innovative way to attract CNA students? We have your answer
Are you looking to minimize and most importantly eliminate agency use? We have your solution
Are you looking to improve morale by increasing your direct care PPD? Reach out to us to hear more
Are you looking to improve morale by increasing your direct care PPD? Reach out to us to hear more
Are you looking to minimize and most importantly eliminate agency use? We have your solution
Are you looking to improve morale by increasing your direct care PPD? Reach out to us to hear more
Are you looking to improve morale by increasing your direct care PPD? Reach out to us to hear more
Are you looking to captivate and motivate the newer generation by offering unique and rewarding training opportunities? Look no further contact us today
Are you looking to captivate and motivate the newer generation by offering unique and rewarding training opportunities? Look no further contact us today
Are you looking to captivate and motivate the newer generation by offering unique and rewarding training opportunities? Look no further contact us today
CONTACT:
CONTACT:

Peg Reith BSN, RN
Peg Reith BSN, RN
Phone: 315-529-3267
Phone: 315-529-3267
CONTACT:
Email: CNA_Training@elementalmgt.com
Email: CNA_Training@elementalmgt.com
Peg Reith BSN, RN
Phone: 315-529-3267
CONTACT:
Peg Reith BSN, RN
Email: CNA_Training@elementalmgt.com
Phone: 315-529-3267
Email: CNA_Training@elementalmgt.com
Are you looking to captivate and motivate the newer generation by offering unique and rewarding training opportunities? Look no further contact us today







