




7 Laguna Honda At Risk: SFMMS Meets with the Centers for Medicare and Medicaid Services About Certification of Laguna Honda Hospital
12 The Many Benefits of Laguna Honda
Victoria Sweet, MD
SPECIAL SECTION: ENVIRONMENTAL HEALTH
10 Healthier Humans, Healthier Planet: 20 Years of CHE
Steve Heilig, MPH and Michael Lerner, PhD
12 Two Decades of Progress in Environmental Health and Science Communication
Pete Myers, PhD
13 A Story of Health: Narrative in Medical and Public Health Training and Practice
Ted Schettler, MD
14 Impacting US Chemical Policy and Environmental Health
Tracey Woodruff, PhD and Swati Rayasam, MSc
15 Past and Future of Environmental Health Research
Linda S. Birnbaum, PhD
16 Cancer and Chemicals
Margaret Kripke, PhD
17 The Collaborative on Health and the Environment (CHE)
Jerry Heindel, PhD
18 A Perspective from Alaska Pamela Miller
19 Because Health
Karen Wong, PhD, MSc
20 Generation X-Y-Z: Bridging the Gap Between Then and Now
Julia Varshavsky, PhD, MPH
21 Climate Health Activism: Twenty Years Out and Counting
Robert M. Gould, MD
22 CHE at 20: Celebration, Reflection and Renewal
Kristin Schafer
July/August/September 2022
Volume 95, Number 3
23 Post Roe: Women Still Have the Right to Emergency Medical Treatment
Maria C. Raven, MD, MPH
24 The No Surprises Act: A Welcome Trojan Horse of Healthcare Legislation
Jonathan Kaplan, MD and Senator Bill Cassidy, MD
26 Strengthening the FDA Proposed Rule on Menthol-Flavored Products
John Maa, MD and Jeffrey Wigand, PhD
28 Physician Wellness is Complicated and It's Simple Jessie Mahoney, MD
2 Membership Matters
5 President's Message: Violence Against Health Care Workers Must Stop Michael Schrader, MD, PhD
6 Executive Memo: Laguna Honda Closure Lays Bare Our Delicate Ecosystem of Care Conrad Amenta
COMMUNITY NEWS
31 Kaiser News Maria Ansari, MD
31 Kaiser Permanente San Rafael Naveen Kumar, MD
34 Advertiser Index
Editorial and Advertising Offices: San Francisco Marin Medical Society 312 Sutter, Suite 608 SF, CA 94108
Phone: (415) 561-0850
Web: www.sfmms.org
CMAdocs.org – Sept. 14
A bill that will reform prior authorization for Medicare man aged care plans has unanimously passed out of the U.S. House of Representatives on a voice vote. The legislation – the Improving Seniors’ Timely Access to Care Act of 2022 (HR 3173) – will streamline Medicare Advantage prior authorization for rou tinely-approved services, ensure plans adhere to evidence-based guidelines developed by physicians, mandate public reporting of prior authorization decisions and timeframes, and implement an electronic process to reduce physician administrative burdens. The California Medical Association (CMA) strongly supports this bill and is working to pass the bill before Congress adjourns in December. CMA thanks the California Members of Congress for moving the bill and we urge the Senate to act swiftly to get it across the finish line.
The American Medical Association and three other major health groups warned Thursday patients across the nation could suffer “irreparable harm” due to the shattered legal landscape left in the wake of the Supreme Court’s decision to overturn Roe v. Wade.
In a statement, co-authored with the American Pharmacists Asso ciation, the American Society of Health-Systems Pharmacists and the National Community Pharmacists Association, the groups said they were deeply concerned by state efforts to limit access to medically necessary medicine. Ongoing questions about state laws are already impacting patients, and language in newly enacted rules is “vague,” “unclear” and “disrupting care,” they said.
https://www.ama-assn.org/press-center/press-releases/state ment-state-laws-impacting-patient-access-necessary-medicine
Rotacare Bay Area Free Clinic in San Rafael is Seeking Physician Volunteers

Rotacare Bay Area is a volunteer alliance of medical profes sionals, organizations, and community members, dedicated to providing free primary quality healthcare services to uninsured families and individuals with limited ability to pay for medical care. Rotacare Bay Area is a non-profit 501(c) (3) public benefit corpo ration supported solely through locally based philanthropies. This organization was formed in 1989 by a Rotarian who identified the needs of many residents who had limited access to primary care services in the Bay Area.
Rotacare Bay Area Free Clinic is seeking physician volunteers of any specialty to donate their time to help with this underserved population.

Among SFMMS' highest priorities is an unerring dedication to reducing the consumption of tobacco products, particularly by young people and underrepresented communities targeted by these companies' marketing practices.
This week, Juul, whose headquarters was once located in San Francisco, settled a multi-state inquiry that began in San Fran cisco and California thanks, in part, to the physician leadership at SFMMS. The settlement is another victory following years of advocacy by organized medicine, which also resulted in SB 793, a 2020 bill that would ban the sale of flavored tobacco products in California. This fall, California voters will be asked to vote on Ballot Proposition 31, a referendum on whether to uphold SB 793's ban on flavored tobacco.

As part of SFMMS' Physician Wellness efforts, we host quarterly a book club for our members! Join your colleagues as we read and discuss Atlas of the Heart: Mapping Meaningful Connection and the Language of Human Experience" by Brené Brown.
SFMMS members who register for this session receive a copy of the author's book.
When: November 3rd at 6:45pm
Since April 2022, SFMMS Retired Members have been meeting up in Greenbrae on the third Thursday of every month for casual conversation, connection, & coffee. Thank you to retired SFMMS Member, Joan Saxton, MD, for her efforts to start this group and her continued coordination to gather our retired SFMMS Members each month. If you would like to attend, please RSVP to Joan Saxton, MD at jsaxton6505@gmail.com.
Scan this code using your smartphone to view the Slate of Candidates for the upcoming 2022 SFMMS Election

Voting begins on 10/31/22 and ends at 5pm on 11/14/22. Electronic ballots will be available at this link the day voting begins.
You can also find the information our website: sfmms.org/advocacy/leadership-opportunities

Effectively transitioning your practice for your patients, staff, and family requires careful planning and sufficient time to accomplish. During this 1-hour, free evening webinar, Deb Phairas, President of Practice & Liability Consultants, LLC, will discuss creative strategies to help you accomplish your goals, including: bringing in an associate, recruiting, selling the practice, or closing the practice.
Special thanks to our sponsor Cooperative of American Physicians (CAP)!

The Marin County COVID-19 vaccine success has gained the attention of the federal government. The partnerships forged locally are held as a model for building trust and reducing barriers to access to vaccines in our most vulnerable communities.
On September 22, Dr. Willis will be presenting Marin’s vaccine equity strategy to the National Vaccine Advisory Committee (NVAC) in Washington DC. The presentation will be broadcast live for the public. Visit NVAC’s website for the meeting agenda and webcast link.
CMA bill to provide more eRx flexibility for low volume prescribers passes state legislature
A CMA-sponsored bill to provide exemptions to e-pre scribing requirements for low volume prescribers has passed the state legislature. Assembly Bill 852 will also provide exemptions for practices affected by federal, state or local emergencies or disasters. The bill passed the State Senate by a vote of 32 to 2 and is now on Governor Newsom’s desk.
Volume 95, Number 3
Editor Gordon L. Fung, MD, PhD, FACC, FACP Managing Editor Steve Heilig, MPH Production Maureen Erwin
President Michael C. Schrader, MD, PhD, FACP
President-elect Heyman Oo, MD, MPH
Secretary Jason Nau, MD
Treasurer Dennis Song, MD
Immediate Past President Monique Schaulis, MD, MPH
SFMMS STAFF
Executive Director Conrad Amenta
Associate Executive Director, Public Health and Education Steve Heilig, MPH Director of Operations and Governance Ian Knox Director of Engagement Molly Baldridge, MPH
2022 SFMMS BOARD OF DIRECTORS
Edward Alfrey, MD Melinda Aquino, MD Ayanna Bennett, MD Julie Bokser, MD Kristina Casadei, MD Anne Cummings, MD Manal Elkarra, MD Mihal Emberton, MD Beth Griffiths, MD
Robert A. Harvey, MD Harrison Hines, MD Ian McLachlan, MD
Jason R. Nau, MD Heyman Oo, MD Sarita Satpathy, MD Monique Schaulis, MD Michael C. Schrader, MD Yalda Shahram, MD Neeru Singh, MD Dennis Song, MD Kristen Swann, MD Kenneth Tai, MD Melanie Thompson, DO Matthew D. Willis, MD, MPH Joseph W. Woo, MD Andrea Yeung, MD
Cover Art: “Rewilding” by Cynthia Fletcher, 20x16, oil on panel, 2021, from her Coronavirus series.


Physicians suffer violent attacks by patients with increasing frequency. These violent assaults often occur in emergency departments. One of our colleagues at St Francis ED told me she has been attacked by patients many times over the years. Most recently she was punched in the face by a patient she was caring for which resulted in her having double vision.
These assaults were reported to the police. Under California law an assault that does not involve a deadly weapon or result in serious bodily injury is classified as a misdemeanor assault. Offenders may be cited and released. This was what occurred in the above incident. The assailant was released and did not show up in court. Although the physician followed up and pursued the case with the district attorney’s office, ultimately the assailant was not penalized.
According to a 2018 survey by the American College of Emer gency Physicians, 47% of ED physicians report being assaulted at work. The US Bureau of Labor Statistics has published that healthcare workers are 5 times more likely to suffer a workplace violence injury than workers overall.
Physicians and nurses are protected from violent acts under Section 241(c) of the California penal code if they are providing medical aid in an emergency setting outside of a hospital. An assault under these circumstances doubles the potential fine and imprisonment term. But an assault against a physician or healthcare worker in an emergency department, hospital, or clinic carries no increased penalty.
Other states have felony statutes against assaulting phy sicians and healthcare workers performing their duties in a healthcare setting. Nationally there are two similar bills H.R. 1195 and S.4182 both entitled “Workplace Violence Preven tion for Health Care and Social Service Workers Act” that are progressing through the House and Senate respectively. These bills would both direct the Secretary of Labor to issue an occu pational safety and health standard that requires covered employers within the health care and social service industries to develop and implement a comprehensive workplace violence prevention plan. This includes hospitals and clinics that operate within a hospital license.
Reproductive clinics are frequently subject to harassment and occasionally to violence. On March 19, 2022, the Women’s Reproductive Clinic at Zuckerberg San Francisco General was forcibly invaded. While there was aggressive intimidation there was no physical assault. The San Francisco DA did press charges for unlawful trespass. Although no one suffered bodily injury, the threat of violence and the fear it created left a lasting impact on the providers.
SFMMS Delegation District VII submitted a resolution to the CMA about healthcare worker violence. Authored by Drs. ManKit-Leung and Roger Eng, the resolution “Protection of Health care Workers Against Physical and Verbal Violence,” called for CMA support for legislating equivalent sentences for assaults against healthcare workers whether these incidents occur inside or outside of a healthcare facility. In addition the resolution called for CMA to support legislation that bans online “doxing” of all healthcare workers. It proposes:
“To decrease the prevalence of violence against physicians and healthcare workers and to mitigate threats of violence, We propose that the California penal code be modified to include hospitals, emergency departments, and clinics as well as emergency aid sites under Section 241(c). This would create deterrence but also allow repeat violent perpetrators to face maximal penalties.”
In addition, I propose that the maximal penalties be levied under existing laws. We need to encourage the police to arrest and the DA to fully prosecute those who attack physicians and healthcare workers at their workplaces.
It’s a start. No doubt there is more we can do, including in some of our own hospitals and other clinical settings. No one should be afraid in the workplace. No one should be beaten at work.
Dr. Schrader practices internal medicine at Dignity Health, is President of the SFMMS, and co-chairs the SFMMS delegation to the CMA.


In April 2022, federal regulators decertified Laguna Honda Hospital and Rehabilitation Center in San Francisco following inspections from 2021-2022. The decertification ended Medicare and Medicaid payments, requiring closure of the hos pital and the transfer of approximately 700 medically fragile patients, sending shockwaves throughout the community of care in San Francisco and laying bare just how fragile our ecosystem can be.
For those unfamiliar, Laguna Honda has a long and storied history dating back to its founding in 1866, two years before the San Francisco Medical Society, when it was referred to as “the Almshouse.” It was a place of refuge for the chronically ill or impoverished with nowhere else to go. In the 20th Century, Laguna Honda housed a cancer research center and provided occupational therapy. In 1963, it was accredited as a hospital, and today is a hospital specializing in skilled nursing and reha bilitation.
Laguna Honda serves the most medically fragile and complex members of our community, many of whom simply have no place else to go, and as a publicly funded hospital, owned by the City and County of San Francisco and operated by the San Francisco Department of Public Health, Laguna Honda is a glowing but all-too-rare example of how a city can invest in care for its com munity’s most vulnerable.
When the Centers for Medicare & Medicaid Services (CMS) decertified the Hospital in April and ordered that its patients must be transferred, it set off a frantic search by the Hospital’s staff to find alternative beds. Thousands of phone calls were made. There were simply no beds to be found. Approximately fifty patients out of 700 were transferred to facilities in Contra Costa and San Mateo counties. Some patients landed in homeless shelters in San Francisco. At least four patients died following the transfers, leading to an outcry from community stakeholders and regulators agreeing to a pause in transfers.
San Francisco has been given a brief, nightmarish glimpse of what it would look like if the publicly funded hospital respon sible for the most vulnerable patients were to disappear. Patients paid for this perspective with their lives. We must learn from it.
The physician community is already contending with the COVID-19 pandemic, an epidemic of opioid and heroin over doses, a public health emergency due to monkeypox, all of which are exacerbated by a chronically inadequate housing supply. Vulnerable and complex patients cycle through our emergency medicine departments and criminal justice system, neither of which are designed to link these patients to social services. Many of these patients had been transferred to Laguna Honda Hospital. If you remove the hospital of last resort, failures cas cade through the system, and it threatens collapse.
The Medical Society has collaborated with our partners in the community to communicate these and other concerns to CMS and will continue to do so until Laguna Honda is recertified. As of this writing, patient transfers remain paused and the federal payments upon which the hospital relies have resumed. But even if Laguna Honda returns to full capacity in a permanent fashion, we must look at the reality of our health systems squarely. We now know what a world without Laguna Honda looks like, and we cannot allow that to happen again.
On August 29th, 2022, the San Francisco Marin Medical Society (SFMMS) met with the Centers for Medicare & Med icaid Services (CMS) regarding ongoing issues related to the certification of the Laguna Honda Hospital and Rehabilitation Center (LHH), the deadline for which is now November, 2022. Approximately 700 patients with complex care needs receive care at LHH. It has long served an essential purpose in our community, serving as a care site for some of our most vul nerable citizens, most with no other options.

Of particular concern to SFMMS is that in order to attain cer tification, LHH must either expand its capacity to house patients or reduce the number of beds by approximately 120 before the November 2022 deadline for certification. Further deadline extensions or continuance of federal payments without certifica tion are unlikely. Should LHH fail to attain certification, federal payments will cease, and the remainder of LHH patients would require transfer.
It is unclear how LHH can fund the transfer of patients should payments cease. There are insufficient beds in San Francisco, the Bay Area, or California to accommodate either 120 or 700 long-term patients, and their transfer may have drastic, negative effects that will ripple throughout San Francisco’s health care systems.
“We understand that the standard for certification is a matter of statute, and CMS’ responsibility is to issue certification based on whether a hospital meets that standard. Those standards exist in order to ensure the safety of patients and quality of care,”said SFMMS President, Michael Schrader, MD.
“However, in order for LHH to meet those standards, it may be required to transfer patients on such a short timeline that it will result in harm to those patients. The removal of this hos pital of last resort may also create failures that will cascade throughout the health care system.”
In April 2022, federal CMS decertified LHH following inspec tions from 2021-2022. The decertification ended Medicare and Medicaid payments, which constitute the vast majority of LHH’s revenue, requiring closure of the hospital and the transfer of approximately 700 medically fragile patients.
Patient transfers began in June 2022, following which, at least four patients died. Some of these medically fragile patients found themselves in homeless shelters. After outcry from the community, patient transfers were paused, payments resumed, and the deadline for certification was extended until November 2022.
The initial attempt to transfer patients from LHH laid bare the gaps in San Francisco’s delicate ecosystem of care and the devastating effects of transfers on some of the most complex patients in our community. Lack of access to LHH beds causes further gridlock in transferring appropriate patients out of our community hospitals, with adverse impacts for all concerned.
SFMMS is deeply concerned that it is not possible for LHH to attain certification without resuming transfer of patients that will again result in patient harm or deaths. SFMMS com municated these concerns to CMS, along with anecdotes col lected from dozens of SFMMS’ physician members about the importance of LHH to their practice, their patients, and their community. We cannot let the “cure” become worse than the problem itself.
The following quotations from doctors who have taken care of LHH patients are especially notable for their emphasis on the bilateral benefits of LHH. First, simply to the hospital system as a whole of San Francisco, because these patients are the most complex patients you can imagine, many of them acutely chronic, as it were, and if they don't go to LHH, then they jam up the acute hospitals, as one of these doctors notes. And jamming up other hos pitals is terrible for all of us, especially as citi zens and potential patients.
Then of course the second issue is to the humanity of the patients themselves and therefore to our own humanity.
And last perhaps, as I have often tried to emphasize, in the end the kind of care LHH gives that keeps these incred ibly sick and complicated patients out of the acute hospital is cheaper. Think of a patient like the patient I called Terry Becker in “God's Hotel,” who had 28 admissions to the General fol
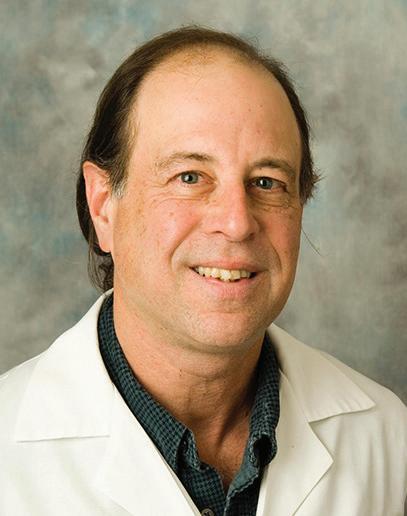
 Victoria Sweet, MD
Victoria Sweet, MD
lowing her transverse myelitis, including three failed skin grafts, although she took two and a half years to completely heal at LHH- she eventually did heal, and was never admitted to a hospital again as far as I know. So in the end LHH was—and is—not only better but cheaper.
We are all suffering today across the country because of the lack of institutions that formerly provided places for people to go—state mental institutions, county hospitals, and almshouses like Laguna Honda.
Victoria Sweet, MD is an Associate Clinical Professor of Medicine at the University of Cal ifornia, San Francisco, and a prize-winning historian with a Ph.D. in history. She practiced medicine for over twenty years at Laguna Honda Hospital in San Francisco, where she began writing her book “God’s Hotel: A Doctor, a Hospital, and a Pilgrimage to the Heart of Medicine,” a highly-lauded bestseller.

As a resident physician in San Francisco, I have cared for patients who are residents of Laguna Honda Hospital as well as patients who have benefited from their services while recovering from illness requiring hospital stays. This is particularly important for patients who are members of vulnerable populations, such as those who are elderly, have complex medical needs due to rare or debilitating medical conditions, or those who struggle with substance use or psychiatric disorders. For these patients, Laguna Honda has provided a place they can receive care outside of a general hospital setting, giving them the opportunity to lead a life outside of our hospital system.
When I have cared for patients who are residents of Laguna Honda, I am consistently struck by the complexity of their care and admiring of the Laguna Honda staff's ability to take care of them. When I am sending a patient to Laguna Honda to recover from illness, I feel confident that they are going to a place that gives them excellent support to continue their journey to recovery. Laguna Honda has become a haven for these folks, and its closing renders them without a place to go in a city that historically and presently struggles to house its citizens.
It is essential to the health of the people of San Francisco that Laguna Honda Hospital remains open. As a resident physician in San Francisco, I have seen firsthand the benefit that Laguna Honda has on our patients. I cared for a gentleman early on in my first year of residency who presented after being found down in his home for many days, unable to care for himself and with no other options for places to go. He had no support network. Every other skilled nursing facility declined to accept him because of his substance use history and social vulnerability. Laguna Honda accepted him and our team as a whole felt so much relief, as the alternate was discharging him back home to continue to fail in the community.
I have also cared for many patients brought into the hospital from Laguna Honda with acute medical needs. One patient was entirely dependent on others to care for him 24/7, requiring a feeding tube and hourly turning due to prior devastating spinal cord injuries. This patient was incredibly medically complex and many other SNFs in the area would have been unable to provide him with adequate care. LHH was a safe place for him to be. Oth erwise, he would have remained in the hospital indefinitely, likely acquiring an infection or other adverse event that we know is so common for our vulnerable patients.
I hope that Laguna Honda will remain open so that our patients can continue to receive care that they otherwise would not.
Finally, the health of everyone in San Francisco is contingent on LHH remaining open. Often times we admit patients to the hospital who are too medically complex or whose families do not have sufficient funds to pay for a full time caregiver and they are not accepted at many other area SNFs. LHH provides a safe dis charge option for these patients. If LHH closes, these patients will remain in the hospital, taking up valuable space in San Francis co's hospital for other acutely ill patients to receive medical care. It is essential that LHH remains open, for the health and safety of everyone in this city.
During a month of UCSF Parnassus medicine wards, I took care of a Laguna Honda Hospital resident who showed me how much she loved her living place. As a younger woman, she had attempted suicide and had been left paraplegic and wheelchair-bound. Now in her older age, without family support, she lived happily at Laguna Honda for many years with nursing support and loving caregivers—such that she did not develop any of the pressure sores so characteristic of bed-bound nursing home patients. Her hair was clean, her clothes were tidy, and she appeared well-fed; a stark contrast to similar patients coming from home or other facilities. Her hospitalization at Parnassus had unfortunately resulted in a tracheostomy placement which required frequent suctioning that was a barrier to discharging her back to Laguna Honda. Her number one goal was to get back to the place she loved and the place she felt safe—Laguna Hondao we worked with her every day to figure out how we could care for her tra cheostomy more effectively. Laguna Honda meant everything to her, and it really showed me how much of an impact a place like LHH can have for vulnerable members of our community with challenging medical needs. If anything, we need MORE places like Laguna Honda to help those in need—prolong life, promote well-being for the chronically ill, and provide a secure, healing environment for people like my patient.
As a medical provider in San Francisco for the last 5 years, I often care for Laguna Honda patients in the hospital. I am always amazed at the complexity of Laguna Honda patients—all have several medical comorbidities—and marvel at the incredible job that Laguna Honda providers do. I remember having a patient with dementia who was non-verbal, on 18 medications, who's family remarked how cared for he was at LHH and how well his wounds were healing and weight was maintained. When I called his LHH provider they knew so much about his medical problems but also so much about him as a person.
When Laguna Honda is closed for any given reason, it is ALWAYS a disaster in the hospital. People live in the hospital for months or even years and it prevents us from caring for patients with acute needs. It is impossible to discharge patients in this city that already has so little housing for our elders. When Laguna Honda is open, we feel confident that our patients have a safe place to go.
We are failing our elderly patients already. Please do not take away 780 beds. Keeping Laguna Honda open will allow us to pro vider better care for our community as a whole.
The last patient I took care of from LHH came to the hospital because she was having some issues with her heart (heart failure exacerbation). She was a lady also who needed assistance in transferring herself, cleaning herself and performing all the activities of daily living and then more recently, with a decline in mental status causing her to not be able to verbalize her wishes or preferences. She is also someone who was disconnected from her family and thus did not have a place to go to if she otherwise didn't have LHH to return to. During her hospital stay we needed to have a goals of care discussion regarding the next steps of her care and unfortunately was not able to have this conversa tion with the patient herself given her mental status. Thank fully her LHH doctor (who was the only person who has seen her consistently in the last 3 years as she had no close family) was able to advocate for what she was like as a person including her values and what she would want at the end of life. Thankfully, the patient was also able to return to LHH; it would have otherwise been very difficult to find her a new home as she had significant needs medically and nursing-wise. I wish there were more places like LHH that can take our most socially and medically vulner able patients and provide an excellent continuity of care. For this reason it would be disastrous to go in the opposite direction and transfer patients out of LHH to an alternative place. I can't imagine this same patient surviving a transfer out of LHH as she would have lost the doctor that knew her values (prior to her mental status decline who could advocate for her) as well as the excellent nursing care provided at LHH.
I took care of an elderly woman who was a long-term LHH resident while she was hospitalized for respiratory distress. She slowly recovered to the point of being able to leave the hospital but unsafe to go home. Her son, her primary caregiver, was incredibly dedicated and at bedside daily advocating for his mother. He spoke of visiting his mother daily at LHH, knowing the staff there on a first name basis, and being actively engaged in her care while she resided at LHH. When this patient discharged back to LHH, we were confident as a medical team that this would be the best place for her care. Not only would she continue to receive excellent care from the LHH medical team that knew her well, but she would receive the additional loving support from her son who we were confident would remain actively involved in the care of his mother due to the collaborative spirit of the LHH staff.
forfacilitatingthesequotesfromtrainees.
Some people identify as clinicians, some as environmen talists, some as scientists, some as people affected by dis eases thought to be at least partly related to environmental factors such as industrial or other chemicals, and some who are any combination of these identities. Twenty years ago, some of us decided that all these diverse people might ben efit from talking with each other more—and by working for a healthier future as well. And so in 2002 we convened a group of leaders in all these fields at the San Francisco Medical Society to plan what might be most useful.
That inaugural meeting led to the creation of the Collabora tive on Health and the Environment (CHE), which we formally launched at a large conference at UCSF medical center co-chaired by the late great former UCSF Chancellor Philip R. Lee, MD.

CHE was focused on two fundamental questions: 1) Given the increasing prevalence of chronic diseases and disabilities, what do we know from the science about the role of environmental expo sures? and 2) How can we make the emerging environmental health science more accessible to researchers, health profes sionals, health-affected groups, and the general public in order to press for upstream prevention of these major health concerns? It seemed to us that the more people who are experiencing health problems understood the environmental exposures and diseases, from conception to senior ages, then the groundswell of demand for cleaner air and water, healthier foods, safer products, and healthier homes, schools and workplaces would be immeasurably strengthened. In turn, not only would we have a healthier planet, but we would be healthier, too.
CHE has fostered numerous interdisciplinary collaborations that have advanced disease prevention and health promotion, including these:
• Establishing, with a major international conference, the first major academic program in the United States on reproductive health and the environment (housed at the University of California, San Francisco – UCSF).
• Creating an award-winning eBook on multiple contributors to specific health concerns with continuing education credits for health professionals available from the Centers for Disease Control and Prevention.
• Engaging the President’s Cancer Panel in the first major review of the scientific literature on links between toxic exposures and cancer
• Educating national learning and developmental disabilities organizations about the emerging science and empowering them to become influential voices in reducing exposures to toxic chemicals through chemical policy reform initiatives and market campaigns.

• Producing more than 60 publications, for researchers, health professionals, and lay constituencies to better understand new research and how it can be applied in “real world” ways.
• Developing scientific consensus statements that have advanced research on environmental links to a wide range of diseases and disabilities.
, a consumer-oriented resource
And, from the beginning, presenting hundreds of open on the full range of environmental health science, policies, and other
We now embark on a new era for CHE, with an excellent new director, Kristin Schafer. Through the years CHE has had well over a dozen great staff, expert advisors, scores of leading scientists and others lending their brains and voices to our forums; some generous funders who’ve made it all possible; and again, thou sands of CHE partners who have come along with us.
Legendary biologist Rachel Carson’s landmark 1962 book Silent Spring focused on the impact of pesticides and other chemi cals on birds and other species, helping launch a moderniza tion of environmentalism. But humans are hardly immune to such impacts as well. When CHE began, we figured giving the new effort a five-year “trial incubation” period might be a smart approach to start, and that if it thrived, it might be spun off of Commonweal to become its own independent entity. Two decades later, CHE is an effort with wide impact. One could say, for better and worse, it is needed even more than two decades ago.
This special section presents brief reflections from some of CHE’s founding and other loyal leaders, from leading figures in the field to students CHE has nurtured, and concluding with our new Executive Director. We are proud of this onetime “startup” and know it will continue to make significant contributions to the broad field of environmental human health.

Steve Heilig is with the SFMMS and Common weal.

Michael Lerner is the President of Common weal. They were among the small group of CHE co-founders and are still actively involved.

 Pete Myers, PhD
Pete Myers, PhD
After Theo Colborn, Dianne Dumanoski and I published Our Stolen Future in 1996, we got “slapped” by one of the most prominent science journalists of the day, Gina Kolata writing for the New York Times. Among her criti cisms was that one chemical can’t cause a plethora of dis eases. It was one chemical, one disease, like asbestos and meso thelioma.
Talk about progress. That ‘paradigm’ is so broken now it’s hard to imagine how any science editor who has been following advances in the environmental health sciences, including endo crine disruption, would allow an argument like that to pass the editorial laugh test. Yes, there are examples other than asbestos that do follow that pattern, but especially in endocrine disrup tion, they are the exception, not the rule.
As Thomas Kuhn wrote in The Structure of Scientific Revo lutions (1962), current scientific paradigms have enormous inertia. This is still true. And that’s even without the active dis sembling focused on resisting change funded purposefully and heavily by vested interests, a fact of life in work on the environ mental health consequences of chemical exposures.

Despite strong and wily opposition, the environmental health science community using science and communication over the past 2 decades has shattered multiple paradigms that for decades if not centuries medicine had held dear, preventing its practitioners from embracing the opportunities to prevent diseases by reducing exposures, instead of merely treating them (usually with pharmaceutical chemicals).
Some of my favorite broken paradigms? “The dose makes the poison.” We now know that high dose exposures do not pre dict low dose impacts. “Nature vs. Nurture” becomes “Nature and Nurture.” “Those statistically significant adverse effects are not toxicologically relevant because they aren’t the same in both sexes.” Actually, for endocrine disrupting compounds, the default expectation now is that there will be differences between how the sexes respond to exposure. And then there’s the still ubiquitous practice among regulatory agencies of testing chemicals one at a time, instead of in the mixtures in which they always occur.
The CHE community has played a pivotal role over the last two decades in breaking down these outdated para digms. How? It has created, purposefully and steadfastly, multiple real and virtual safe spaces where new ideas and results can be examined, dis cussed and debated, not just by people throwing bricks at the old paradigms, but by thoughtful scientists willing to listen to new ideas, new data, new hypotheses that challenge some of their most cherished notions. More, these spaces by design have welcomed advocates with serious commitments to carry the discussions into the real world, to share this ongoing thunder of scientific understand ings with the media, policy advocates, and even, provocateurs. Those safe spaces have been immeasurably valuable for prog ress. They might not be the flashiest new shiny objects on the block, but they have helped us get beyond old, outdated and sometimes even harmful ideas.
CHE has done all that as waves of new scientific results have been published and as the media landscape has changed enor mously. The CHE community has embraced the new results and adapted to sweeping revolutions in communication challenges and opportunities.
And that’s what the next 2 decades of environmental health science and communication needs more of, turbocharged.
Pete Myers is Chief Scientist and Board Chair of Environmental Health Sciences, which he founded 2 decades ago, and Board Chair of the Science Communication Network. He is also a board member and founder (with Terry Collins) of Sudoc, a start-up chemical company commercializing a family of cata lysts invented by Terry Collins that bio-mimic peroxidase enzymes, part of human body chemistry, to oxidize haz ardous chemicals. In 1996, along with Theo Colborn and Dianne Dumanoski, he co-authored Our Stolen Future, a book for the general public about endocrine disruption.
 Ted Schettler, MD
Ted Schettler, MD

Story telling has a long history in medical training and practice. Narratives describe a patient’s experience of illness, a clinician’s experience caring for them, or both. Yet, contemporary medical practice tends to deemphasize narratives in favor of facts and find ings gleaned from laboratory tests, imaging studies, and brief hospital or office visits.
Resisting this trend, a few medical schools offer courses in narrative medicine, encour aging students to tell and closely listen to unique stories of illness. They use literature, philosophy and the creative arts to help cli nicians-in-training better understand their patient’s experience and their own response. Public health training and practice also use stories showing how epidemiologic data play out in the lives of individuals, fami lies and communities. This can be tricky because the relation ship between a story teller and the people in the story raises questions of consent, framing and content. People generally do not appreciate being unable to participate in how to tell their story. But a skillful narrative can drive effective public health interventions.
Ten years ago, several colleagues and I began a project that grew into six fictional stories of health and illness published as a free, online multi-media eBook featuring graphics, illustra tions, short videos and links to outside resources. We wanted to tell realistic stories of people and their families. We were joined by a gifted graphic designer, a specialist in medical communica tion from the CDC as well as a talented agency illustrator. As the stories developed, we enlisted additional content experts. Each chapter went through external peer review, including health professionals at the CDC, before being certified for continuing education (CE) credits.
We created a realistic personal, family, community, envi ronmental, social, and cultural context for each story. Then we developed fictional characters, families and neighborhoods to tell stories illustrating how these multi-level variables can interact to influence the risk of illness, its prevention, and response to treatment. The storylines include rural, suburban, and city settings and people of different ethnicities. They are collected in A Story of Health—A Multi-media eBook1. Protago nists are Brett, a boy with asthma; Amelia, a girl with a devel opmental disability; Stephen, a toddler with leukemia; Toshio
and Reiko, a young couple struggling with infertility; Sam, an older man with cognitive decline; and Sofia and her family who face threats from wildfires.
The response has been overwhelmingly favorable—more than 20,000 registrations for CE credits for health professionals for one or more of the six chapters and countless others who have downloaded chapters without seeking certification. Readers surveyed ini tially and three months after CE completion found the chapters not only highly informa tive and useful for their work but many also described the storylines, interactive features, graphics and videos as particularly engaging. Respondents repeatedly confirmed the value of story-based learning and were drawn to the unique eco-social framework in each chapter. Their responses suggest that if clinicians, com munity-based organizations, advocates, and people adversely affected by social and environmental hazards were to join more frequently in telling their unique stories it could inspire improvements in personal and public health where they live.
Ted Schettler MD, MPH is Science Director of the Science and Environmental Health Net work. (www.sehn.org) He also serves as Sci ence Advisor to Health Care Without Harm and is a founding member of the Collabora tive on Health and the Environment.
1. Miller M, Schettler T, Tencza B, Valenti M (concept and origi nal authors), et al. A Story of Health—A Multi-media eBook Available at: https://tinyurl.com/538s62e6 Accessed Aug 15, 2022.
The 2007 CHE/UCSF Summit brought together 400+ scientists, clinicians, policy makers, media, NGO/community groups to set a visionary agenda for addressing environmental threats to health. The “Shaping our Legacy” plan developed there over 20 years ago still guides our work today – creating research to answer pressing environmental health questions, translating science into improved clinical care, and supporting policy that addresses health and health equity. The summit also launched our organization, The UCSF Program on Reproductive Health and the Environment (PRHE). CHE was and still is an integral connector those of us in the scientific/clinical/health environmental space working to transition from a society that treats chronic disease to one that prevents it.
Chemical pollution threatens the health of our planet and everyone who lives on it. Despite this, the manufac ture and production of chemi cals has continued to increase, 350,000+chemicals and chemical mixtures registered worldwide have led to extensive and dispro portionate exposures, and gen erations of children being born pre-polluted.
In the United States, the 1976 Toxic Substances Control Act (TSCA), called “one of the most important pieces of 'preventive medicine' legislation" ever passed by Congress, was the primary legal authority to reduce harmful chemical exposures. Unfortunately, the law and its implementation was ineffective, causing state and local jurisdictions to create a patchwork of gap-filling regulations. This set up the most recent significant shift for our work in US chemical policy, the 2016 amendments to TSCA via the Frank Lautenberg Chemical Safety for the 21stCentury Act. In the 40 years between enactment of TSCA and its 2016 amendments, EPA regulated fewer than 10 of the 86,000+ chemicals on the market; amended TSCA promised an immense opportunity to fix the mistakes of the past and protect the public’s health.

Amended TSCA requires EPA: evaluate chemicals on a spe cific schedule, account for risks to “potentially exposed or sus ceptible subpopulations” like children, pregnant people, and workers, use the “best available” science, and determine if a chemical poses an “unreasonable risk” without considering cost. However, the 2016 law preempts states from taking action on chemicals evaluated by EPA and leaves many decisions related to the specifics of implementing up to EPA, leaving it vulnerable to political interference and scientific integrity concerns. For example, under amended TSCA, the industry is not required to provide data on the health effects for chemicals already on the market, and new chemicals have limited review. This is unlike the European Union, where every chemical on the market must
provide a minimum data set of health effects information order to stay on the market.
Following the goals laid out in the CHE/UCSF Summit, PRHE has been engaged in the imple mentation amended TSCA as the primary public policy that influences exposures to toxic chemicals. We have submitting dozens of scientific public com ments with hundreds of col lective signatures, publishing manuscripts analyzing the law and its impacts and developing actionable recommendations for EPA. As such, we have five scientific principles for hazard and risk assessment to guide our work to make chemical policy incorporate the most up to date science and account for real-world risks and protect public health for years to come.
To do this Decision-makers must:
1. Make manufacturers pay for data collection on the chemicals they currently or will produce
2. Stop treating a lack of data like a lack of hazard, exposure, or risk
3. Better identify and protect populations disproportionately exposed and/or more susceptible to harmful chemicals
4. Not assume a “safe” or “no-risk” level of chemical exposure in the diverse general population
5. Evaluate and account for conflicts of interest in risk and hazard assessments
The goals of environmental laws and policies like amended TSCA often aspire to protect health, but to date it has fallen short of ensuring equitable, socially just safeguards. If EPA fails to cor rect its mistakes, it will continue to underestimate risk, recre ating the same inefficiencies as the original law and continuing to endanger our health and our environment for years to come.
We deeply value our collaboration with CHE and other partners to support using the best science to protect communities dispro portionately exposed to toxic chemicals and ensure that we can all live our healthiest lives.
Tracey Woodruff, PhD, MPH is a leading sci entist who has produced seminal research on how harmful chemicals and pollutants impact health, pregnancy, and child development, including the first international study to docu ment the effects of air pollution and preterm birth and the first to document toxic chemicals in pregnant women and newborns. A national expert in chemical and regulatory policy, Dr. Woodruff was a senior scientist and policy advisor for the U.S. EPA’s Office of Policy prior to joining UCSF.
Swati Rayasam, MSc is a Science Associate on the Science & Policy team at PRHE. She has been one of the leads on the team for PRHE’s work to ensure EPA’s implementation of the Toxic Substances Control Act protects the health of communities disproportionately impacted by toxic chemical pollution such as incarcerated people, people with disabilities, and BIPOC com munities. She has expertise in federal and international policy, exposure science, community-guided science, science translation/ communication, toxics, infectious disease, and water, sanitation, and hygiene (WASH).


While the potential impact of the environment on our health has been recognized for thousands of years, the need to use a multi- and trans- disciplinary approach has only been rec ognized relatively recently. Exposures must be broadly defined and inclusive – the environment includes social and economic factors, as well as natural stressors, pollutants, infectious agents, and nutrition. The newspaper story of environmental health includes the who, what, when, where, why, and how of exposures and populations. Another key understanding is that noncommu nicable, chronic disease – notwithstanding the recent focus on the COVID pandemic – pose the greatest threat to human health throughout the world. Cancer, heart disease, obesity, and type 2 diabetes have increased dramatically and are impacted by our environment. Neurodevelopmental disorders such as autism spectrum and ADHD are on the rise.
Both our environment and our genes determine our health. Air pollution is the greatest environmental cause of morbidity and mortality, but pollution of water and soil also have sig nificant impacts. And pollution can impact ever organ and tissue in our body and at every life stage. The vulnerability of the developing organism has been recognized within the past twenty years – but there are multiple developmental stages, ranging from preconception through aging. The key role of epigenetics controlling gene expression and its malleability has only been recognized relatively recently. The key role of the microbiome and the role of stem cells are under intense investigation. The realization that effects can occur at very low doses when the endocrine system is perturbed has led us to understand that environmental impacts can occur within the general population. And that many exposures can have long term effects which may not be known for many years, and some can impact future generations.
Key disciplines in environmental health include toxicology, exposure science, and epidemiology. There is a need to better link these fields. New approaches are transforming toxicology, such as the use of new approach methodologies (e.g., cell-based, computational, etc.) which will reduce the use of experimental animals as models for human health – although when effects are seen in multiple species in multiple tissues and at various ages, it is unlikely that at least some humans are not also susceptible. Exposure science is being transformed by exposomics, the totality of exposure over a lifetime. Environmental sensors can measure external exposures, and internal exposures are being monitored by increased use of biomonitoring, both agnostic and targeted. Metabolomics, proteomics, lipidomics, and glycomics all provide insight into impacts of various exposures. The recognition that exposures are always to multiple stressors – chemical, physical, social, economic, and of course climate - is transforming how we view cumulative exposures.
Systematic review allows evidence integration from human, animal, and mechanistic studies. The use of key characteristics is helping to predict adverse effects by looking at key bioactivity profiles of stressors. Key characteristics involves pattern recogni tion, something at which people are very good, and allows a more holistic use of mechanistic understanding in predicting disease. Accurate prediction can lead to preventionof environmentally related disease, always preferable than treatment and cures.
Linda S.Burnbaum is the former Director of the National Institute of Environmental Health Sciences and the National Toxicology Program. She was granted Scientist Emeritus Status at NIH when she retired and is also a Scholar in Residence at the Nicholas School of the Environment, Duke University.

Like most cancer researchers, I was initially quite skeptical of the importance of envi ronmental factors in causing cancer. But several years ago, the President’s Cancer Panel, of which I was a member, did a year-long study of this issue, which dramatically changed my outlook. Through testimony from scientists, clinicians, advo cates, and public health officials, I discovered that contrary to my assumptions, most chemi cals were not tested for cancer causing activity before being put on the market. Even more con cerning, chemicals banned in other countries because of their cancer inducing potential were freely available in the U.S. The main reason for this is because we have adopted the reactionary approach to chemical safety, which means that we only regu late substances after there is evidence that they are harmful. In contrast, other countries use a precautionary approach, which requires proof of safety prior to release to the public. One conse quence of the reactionary approach is that we now live in a vir tual ocean of chemicals in our air, water, homes, and workplaces.
These findings led us to wonder what the impact of all these chemicals could be on human health. Could they be responsible for the continual rise in the incidence of cancer in children and adolescents over the past 50 years, or the fact that more than 80% of women diagnosed with breast cancer have no family history of the disease? We wrote in our report that the common estimate of the contribution of chemicals in causing cancer (around 6%) was likely to be way too low. In the years since the Panel’s report, new information on the mechanisms of cancer development and increasing evidence of the cancer-causing activity of environmental chemicals have served to strengthen this conclusion.
On the positive side, these advances highlight the potential that exists to decrease the enormous burden of cancer, but we need to identify and reduce exposure to agents that contribute to cancer induction. Unfortunately, relatively little attention or funding has been devoted to the area of cancer prevention. The vast majority of cancer research is focused on treating cancer, which is understandable—we all want better, less toxic treat ments for cancer. But preventing cancer is also important: it has the potential to affect large numbers of people and has the added benefit of sparing people from the physical, emotional, and financial consequences of a cancer diagnosis.
There are many reasons why prevention research has lagged behind. It takes a long time to see the impact of preventive measures. Also, prevention is not personal. Cancer treatment
 Margaret Kripke, PhD
Margaret Kripke, PhD
deals with real, identifiable people. Patients and survivors have a voice and a face. Treating someone with cancer is a part nership, and curing cancer is a personal triumph. In con trast, prevention has no face. We never know whose cancer was prevented. The impact occurs at the population level, not the individual level. Health insurance providers have been reluctant to support preventive measures, and funding agencies want more immediate results. Pharmaceutical industry incentives are aligned with treating cancer, not preventing it. Therefore, most of the focus and funding for cancer research has been devoted to cures, rather than prevention.
The medical and scientific communities have an important role to play here, both in appreciating the power of prevention, and in helping to educate the public on the role of environmental causes of cancer. We need to help people realize that no one is protecting us from many toxic exposures—not the government, and certainly not industry. Therefore, reducing the incidence of cancer by identifying harmful substances in our environment and decreasing exposure to them must be more urgent research and public health goals.
Dr. Kripke is Professor Emerita at the Univer sity of Texas M. D. Anderson Cancer Center and the U. T. Graduate School of Biomedical Sciences. She served as a member of The Pres ident’s Cancer Panel from 2003-2011.

References
1. “Reducing environmental cancer risk: What we can do now”. Report of the President’s Cancer Panel, USDHHS, NIH, NCI, Washington, DC, 2010.
My fondest memories of CHE are of Alison Carlson. The most enthusiastic, dedicated, focused and charismatic facilitator of the CHE Fertility/Pregnancy Com promise Working Group and Senior Fellow at Commonweal Health and Environment Pro gram. To me, her name became synonymous with CHE. Her pas sion came from her years as an infertility patient, which led to her awareness that society was ignoring the effects of toxic chemicals on fertility.
My first memory is of the 2005 Fertility Workshop on Envi ronmental Contaminants and Fertility Compromise organized by Alison. It was held at a Catholic Retreat Center, and we stayed in rooms used by the nuns, small and bleak and sparsely deco rated. There were 45 scientists, doctors, fertility and reproduc tive health patient groups, environmental advocates and CHE representatives. An eclectic but high-powered and enthusiastic group. This was my first meeting with such diverse attendees, and it made for a fascinating and fruitful discussion. There were discussions of anogenital distance (AGD) and body parts some participants were not used to hearing about. I remember dis tinctly at the end of the meeting, everyone sitting in a big circle, and we all had to say something we were going to do to help improve fertility as a result of the workshop. The result was the Vallombrosa Consensus Statement on Environmental Contami nants and Human Fertility Compromise, which summarized the science and identified critical scientific gaps for the first time. It was groundbreaking, thanks to Alison.
Next up was the 2007 UCSF-CHE Summit on Reproductive Health and the Environment, attended by 400 attendees world wide. This was a pioneering, multidiscipline, environmental reproductive health conference attended by health profes sionals, basic and clinical researchers, public health profes sionals, policymakers, advocates, funds and community health leaders: notice the similarity to Vallombrosa? Inclusiveness became the middle name of CHE, especially when Alison Carlson was involved, in this case, a co-chair with Linda Giudice of UCSF and Philip Lee, former US Assistant Secretary of Health Educa
tion and Welfare. This Summit included innovative sessions such as, Conversations on Stage (pairing clinicians, reproductive health advocates, federal regula tors, policymakers and funders) discussing how to work together effectively, and Breakout Groups focused on transdisciplinary dis cussions around reproductive health questions and issues that could help shape follow-up ini tiatives. Never before had there been a meeting of the minds and sharing of ideas between attendees from such diverse fields.
I am so thankful for what CHE has done in Reproductive Health and the Environment. I am particularly grateful that Alison Carlson showed up at the right time and made CHE the center of Reproductive Health. In my work today with HEEDS, I use Alison’s model; this fall we are bringing together a diverse group of obesity scientists, obesogen researchers, and NGOs at a workshop to get them in the same room in hopes of bringing obesogen science into mainstream obesity work. I hope we can use these lessons learned from Alison for many years to come.
Jerry Heindel PhD is Director, Healthy Envi ronment and Endocrine Disruptor Strate gies (HEEDS), a program of Environmental Health Sciences (EHS).


Scan this code using your smartphone or visit sfmms.org/advocacy/leadership-opportunities to view the Slate of Candidates for the upcoming 2022 SFMMS Election
Voting begins on 10/31/22 and ends at 5pm on 11/14/22. Electronic ballots will be available at this link the day voting begins.

 Pamela Miller
Pamela Miller
In the early years of CHE, the staff of Alaska Community Action on Toxics (ACAT) would eagerly join the monthly teleconferences and huddle together around the conference speaker phone in the early morning darkness of Alaska. It is no exaggeration to say that these calls inspired our work and left us feeling that we were part of an international community, members of civil society working together to advance scientific understanding and motivated by a passion to protect public health and the environment with which we are inextricably connected. The teleconferences provided a much-needed remedy to alleviate the isolation we experienced as environmental health and justice researchers and advocates in Alaska. CHE continues to provide inspiration and enlightenment that informs our daily work for environmental health and justice.
After expressing interest in forming a regional partnership of CHE, I was invited to Commonweal to join a meeting of core staff and advisors. I remember a conversation with Michael Lerner in which he suggested that CHE-Alaska could be a “window to the Arctic.” Michael’s foresight guided the develop ment of CHE-Alaska as well as our research and advocacy work. In the intervening 20 years, it has become apparent that the Arctic is a hemispheric sink for persistent industrial chemicals that are transported on atmospheric and oceanic currents from lower latitudes through global distillation. Arctic Indigenous Peoples have some of the highest levels of persistent pollutants of any population on earth. These problems are exacerbated by the rapid pace and magnitude of climate change in the Arctic which is now known to be warming at a much faster rate than earlier studies predicted—at least four times faster than the planet as a whole. Melting of sea ice, permafrost, and glaciers is mobilizing sequestered chemical contaminants and micro plastics, threatening the health of our oceans, fish, wildlife, and peoples of the north. With the support of CHE National, the Alaska regional partnership (CHE-AK) has hosted more than 170 seminars, with an emphasis on environmental health sci ence and policy concerning the Arctic and many drawing over two hundred people. We see growing awareness of the Arctic as a place of vulnerability and an increasing interest in concerted action to protect the health and well-being of this region, its wildlife and peoples.
CHE is a vital resource for those who are most directly affected by chemical exposures and burdens of disease. We recently taught a college-cred ited Community-Based Environ mental Health Research Institute in Nome, Alaska with students from Alaska Native communities throughout the Norton Sound region of the Alaskan Arctic. The students used CHE resources such as fact sheets, the Toxi cant and Disease Database, con sensus statements, and webinar recordings in seeking information to address environmental health disparities in their own communities.
Over the past twenty years, CHE has expanded our under standing of emerging science, including endocrine disruption, developmental and reproductive health, epigenetics, obesogens, and climate change. CHE is fostering a sea change in awareness and engagement among scientists, health care providers, stu dents, and policymakers that is necessary to create positive and protective environmental health and justice policies from local to international levels. May CHE continue to encourage our col lective actions toward primary prevention and transformative change that protects the health of all.
Pamela Miller founded Alaska Community Action on Toxics (ACAT) in 1997 and serves as Executive Director. Since 2016, she has served as Co-Chair of the International Pollutants Elimination Network (IPEN), a network of more than six hundred environmental health and justice organizations working in more than 120 countries. She is a Principal Inves tigator for community-based participatory research projects in the Arctic supported by the National Institute of Environmental Health Sciences.

The public’s knowledge of environmental health issues has changed tremendously over the past few decades, with CHE playing a critical role. In 2018, while I was Director of CHE, we launched Because Health, an environ mental health educational cam paign for the general public. Because Health is now a part of the Center for Environmental Health, a nonprofit leading the nationwide effort to protect people from toxic chemicals. Because Health successfully brought younger voices into the environmental health conversation and played a crucial role in educating mainstream audiences about environmental health issues. Because Health’s specialty was distilling complex envi ronmental health concepts into actionable steps that people can take to build a healthier future for all. When Because Health merged with the Center for Environmental Health, the website had more than 400 pieces of educational environmental health content and averaged 40,000 users a month with more than 1 million page views a year. Because Health also organically built an engaged community of over 70,000 users on Instagram.

Quality educational forums and resources are particu larly critical at this time because current political forces are threatening to undermine decades of public health and envi ronmental protections. CHE’s role in this context as a trusted evidence-based resource and forum for sharing emerging envi ronmental health science in easily accessible and engaging formats is extremely important. When I was at CHE, I was able to launch Because Health by leveraging CHE’s rich network of environmental health scientists and advocates. By translating the science and communicating it in ways that were appealing, we reached a new audience of millennials. Because Health focused on reaching millennials because many of them are having children or are preparing to enter the phase of their lives where they are rethinking their environment, their con sumption, and the impact of their purchasing. Because Health sparked an interest in environmental health in a new genera tion by creating environmental health education that was acces sible, curated, relevant, and shareable, while still being strongly rooted in the latest science.
Karen Wang, PhD MSc
By educating the public and engaging citizens of all ages in the environmental health con versation, we helped build a groundswell of demand for poli cies, as well as economic and legal structures, that prioritize preventative actions to pro tect public health. Millennials have upwards of $200 billion in annual buying power and are trendsetters across all industries from fashion to food. More and more, millennials are taking on higher leadership and manage ment positions in the workforce and are at the forefront of innovation in many sectors. I hope that by getting millennials engaged with limiting exposure to toxic chemicals, individuals will apply their talents to incorporate environmental health principles and the precautionary principle in their personal lives and careers. In order to face the current and future chal lenges of toxic chemical pollution, we need all hands on deck.
Karen Wang, PhD, MSc is an expert science educator with deep knowledge in environ mental health, data analysis, and research methodology. She is currently a healthy building environmental consultant. She is the former director of the Collaborative on Health and the Environment at Commonweal, and the founder of Because Health, an envi ronmental health website and social media campaign. Karen has a PhD in Applied Economics from the University of Washington and also holds a MSc in Earth Systems and a BA in Economics from Stanford University.
My passion for environmental health and justice took hold twenty years ago in college at the University of California, Berkeley, where I learned of the disproportionate health prob lems faced by communities that have been historically mar ginalized – many of which included low-income residents, immigrants, black, indigenous, or people of color.
The more I learned, the more hooked I became. My favorite book in college was Our Stolen Future, the groundbreakingwork on endocrine disrupting chemicals. I was fortunate to work for GAIA (Global Alliance for Incinerator Alternatives), which was run by Annie Leonard, who created the Story of Stuff and is now at Greenpeace, and as a junior scientist in an ecotoxicology lab at UCB, helping develop a microarray to detect metals in water. These experiences led me to change my major from pre-med to molecular environmental biology, and to do my senior thesis on the bioremediation of dioxin, highlighting incinerators as a key source of dioxin. They also led me to CHE.
As the program associate and fertility/reproductive health coordinator for CHE between 2005 to 2010, I learned about scientific rigor and effective communication from leading researchers and environmental health communicators such as Pete Myers, Ted Schettler, Michael Lerner, Sharyle Patton, Steve Heilig, and Charlotte Brody. As the CHE-Fertility coordi nator, I also had the opportunity to work with leading scientists, including Tracey Woodruff and Lou Guillette, to organize a con sensus workshop of interdisciplinary researchers on women’s reproductive health and the environment, which resulted in a published white paper and Girl, Disrupted, a lay translation report that I co-authored. This led me to pursue an MPH and PhD in environmental health science with Rachel Morello-Frosch at UC Berkeley and then a post-doc at UCSF’s Program on Repro ductive Health and the Environment (PRHE), both academic experiences that shaped my current research agenda.
Since my time at CHE, environmental health science has grown tremendously. It has been especially exciting to watch the science shift from studying individual chemicals to evalu ating chemical groups, such as phthalates and PFAS, with current efforts to assess and regulate them as chemical classes and eval uate their cumulative impacts (across the life course and in com bination with other exogenous and endogenous compounds). For PFAS alone, we’ve seen the number of studies conducted since 2010 grow almost exponentially. We’ve also established phthal ates as reproductive toxicants in laboratory studies and have even shown through predictive mixture toxicology experiments how they can have greater (additive) effects on reproductive health in combination than they can individually. These effects have now been well documented in humans as well, and scien
tists are beginning to leverage multiple epidemiologic cohorts to get better answers to other exposure-outcome questions.
Advancements in statistical mixture modeling techniques and our ability to measure the exposome has also become a reality over the past twenty years. We have devised methods to assess the combined effects of chemical and non-chemical or social stressors, including structural racism and poverty, with new conceptual models for researchers to consider, such as the socio-exposome.
But we still have so much more work to do. Chemicals policy in the United States remains fragmented and inadequate, and risk assessment methods often fail to account for groups with increased susceptibility due to multiple internal (biological) and external factors, including social stressors and/or exposure to multiple environmental health hazards. We also have more work to do to understand biological mechanisms and standardize mixture modeling techniques to examine the combined effects of exposures across the life span, including during puberty and preconception, during and after pregnancy, and even as we age. We also need more intervention studies to understand sources and how to mitigate harmful exposures, with a sharper focus on upstream solutions to identify safer alternatives and develop opportunities for climate change mitigation and adap tion. We also need our decision-makers to use evidence-based systematic review methods to evaluate the explosion of scientific knowledge over the past 20 years. And finally, we need more community-engaged research, including report-back studies, to better address the needs of highly impacted communities. Recruiting and retaining student and researcher voices of color in scientific and public discourse is also critical for the future of environmental health and justice science.
As an assistant professor of environmental health at North eastern University (with a joint appointment in health sciences and civil and environmental engineering), I seek to bridge disci plines in ways that will promote solution-oriented research. I also hope to bridge the past and present generations of environmental health, by remembering how far we have come standing on the shoulders of giants in the field while inspiring the next generation of environmental health scientists and problem solvers.
Julia Varshavsky, PhD, MPH (she/her) is Assistant Professor of Environmental Health, Department of Health Sciences and Depart ment of Civil and Environmental Engineering Social Science Environmental Health Research Institute, Northeastern University.

The dawn of CHE came at a cusp of our environmental health movement, when health professionals moved beyond efforts to reduce pol lution emanating from the healthcare sector, toward transforming healthcare to respond to our climate crisis.

Since the founding of Health Care Without Harm in 1996, many of us had focused on working with our colleagues within California Medical Asso ciation (CMA) to support policies such as eliminating mercury from our hospital systems, and to stop the incineration of med ical waste, curbing toxic streams that were poisoning our most dumped-on, and poorest communities, mostly of color.
In 2002, CMA’s adoption of two resolutions, “Air Pollution, Energy, and Health,” and “Climate Change and Human Health,” signaled a remarkable sea-change of climate health activism among committed health professionals increasingly propelled by younger colleagues. Over the past 20 years, working in spe cialty societies, county, and national health professional asso ciations, and in health systems across the country, policies ranging from institutionalizing climate-health curriculum to healthcare sector divestment from fossil fuels have now gained national traction.
Emblematic of this welcome transformation was the unprec edented coordination of over 200 worldwide medical and health journals in the publication of an editorial in 2021 declaring the anticipated rise in global temperatures to be “the greatest threat to global public health,” and calling for our governments to urgently cooperate in investing adequately to redress our environmental crisis to avoid risking “catastrophic harm to health that will be impossible to reverse.”
Unfortunately, this revolution of consciousness has crashed up against the global disruptions posed by COVID and unabated militarism exemplified by the brutal war in Ukraine. Beyond the already horrific costs of human lives and uprooting of millions, we now face heightened dangers of nuclear weapons use, and the risk of a catastrophic radiation release from nuclear reactors operating in the conflict zone.
Our government and its allies have responded to war-induced energy disruptions by promoting increased production of oil and gas. This, coupled with “false solutions” to our energy and cli mate crisis, exemplified by accel erated support for nuclear power and unproven “carbon capture” proposals, will delay us from making the rapid transformation to the truly clean energy systems we need to survive.
In the wake of vastly increased U.S. military and nuclear weapons budgets, the recently passed Inflation Reduction Act (IRA), while providing significant sup port for promising green technologies, simultaneously perpetu ates fossil fuel extraction.The IRA has been largely stripped of the original “Build Back Better” programs that our most over burdened communities were promised to enable their full par ticipation in a “Just Transition” to a green future.
To fully support the health of our patients and our com munities, we will need to redouble our efforts to help build an intersectional movement that is local, national, and global in its vision, and capable of developing the political power to trans form our world so we can protect and restore our web of life to survive as one species among many.
Robert M. Gould, MD, is an Associate Adjunct Professor with UCSF's Program on Reproduc tive Health and the Environment (PRHE), a member of the Santa Clara County Medical Association, and long-time President of SF Bay Physicians for Social Responsibility.
What an interesting moment it’s been to step into leadership at the Collaborative on Health and the Environment (CHE). This 20th anniversary year offers opportunities for celebration, reflection and renewal—all of which are well underway.

CHE has made significant contributions to the environ mental health field over the years, from co-launching the first academic program in the country on reproductive health and the environment, to cre ating an award-winning ebook on environmental determi nants of health, to building a Toxicant and Disease Database for researchers and the Because Health website for consumers. Details of each of these accomplishments are described in other articles in this compilation.
What’s struck me as I’ve learned more about CHE’s his tory is how often we’ve played the role of incubator or catalyst, sparking and nurturing efforts that have gone on to have incred ible impact in the field of environmental health. This catalytic role is the result, I believe, of CHE’s commitment to connecting across disciplines to create space for collaboration and mean ingful partnerships. You never know what will emerge when you bring together committed, creative people from diverse back grounds to tackle tough problems—but very often, it’s some thing important and good.
We’ll celebrate CHE’s legacy and future this fall with a series of CHE Cafes, bringing back a past format of informal, online conversations with leading “thinkers and doers” working for environmental health and justice. On Saturday, November 12 we’ll gather at Commonweal for a hybrid in-person/online event to share stories of CHE’s work over the years and plan for what’s ahead.
Addressing threats to health from environmental risks is more relevant and urgent than ever before. Science now sug gests that the human health harms caused by chemical contami nation is a global crisis commensurate with climate change and biodiversity loss. Addressing these interlinked crises urgently, effectively and equitably is the challenge before us.
Kristin SchaferThis anniversary year has spurred us to reflect on how we can most usefully meet this critical moment, supporting environmental health and jus tice today and into the future. We’ve interviewed and sur veyed thousands of members of the CHE community to find out what people appreciated most, and where we might change and grow.
While our signature webi nars with partners will con tinue, we’re exploring new strategies to help meet the urgent needs of today’s world. We’ll focus particularly at the intersec tion of chemicals, climate and health (including plastics and pesticides), with additional work promoting cancer prevention and children’s environmental health. Within these areas, we’ll collaborate with partners to host in-depth webinar series and workshops, develop and amplify existing ‘science to policy’ tools, and highlight solutions rooted in environmental justice. I look forward to working with this vibrant, dedicated community of environmental health scientists, advocates and policymakers as we move forward into CHE’s next 20 years.
Kristin Schafer, CHE’s new director, brings over three decades of experience in the field of environmental health and justice. After working at EPA and the World Resources Institute in Washington, DC, she moved back to Northern California where she held vari ous roles — including Executive Director — over her 25-year tenure at Pesticide Action Network (PAN) North America. Kristin holds a Masters in Social Change and Development from Johns Hopkins School of Advanced International Studies.

 Dr. Maria C. Raven, MD, MPH
Dr. Maria C. Raven, MD, MPH

The recent overturn of Roe v. Wade took away a woman’s constitutional right to abortion. But it didn’t take away her right to life-preserving health care, or my right as a physician to pro vide that care. Pregnancy is a medical condition. As an emergency room phy sician, I see medical complications that women endure throughout their pregnancies including serious and lifethreatening bleeding and ruptured ectopic pregnancies, as well complica tions around childbirth like high blood pressure, seizures, heart problems and infections, all of which can pose serious threats to a woman’s life. Pregnancy can also result in lost work and pay for women when complications force them to remain on bed rest, unable to go to work let alone care for other family members.
By taking away a woman’s right to choose to terminate a pregnancy, our country is not only forcing women who may not want or be able to bear a child to do so — we are putting those same women at risk of pregnancy-related medical problems whose consequences can range from lost wages to death. The U.S. has the highest maternal mortality rate of any developed country, more than double that of most other high-income coun tries. Non-Hispanic Black women have three times this risk, and women over age 40 have almost 8 times the risk of women who are under 25. Maternal death rates in the U.S. have been rising since 2018, and it is within this context that our country will now also become the only country to restrict, not increase, access to abortion apart from Nicaragua.
Fortunately, one thing all women do have a right to under federal law is to seek emergency medical treatment. The federal emergency medical treatment and labor act (EMTALA) means that all people — including pregnant women — have the right to a medical screening exam, which includes stabilizing treatment, in an emergency department. Our job as physicians is to provide the highest quality emergency care for all of our patients, and in this age of restricted access to abortion, we anticipate that more women will come to us not only with complications stemming from illegal abortions, but also seeking care after unprotected intercourse, sexual assault and to evaluate early pregnancies.
Patients should have a right to privacy when undergoing medical treatment based on the Health Insurance Portability and Accountability Act of 1996 (HIPAA), which is supposed to protect sensitive patient health information from disclosure without the patient’s consent. Yet, since Roe v. Wade was over turned, pregnant women – in states that have allowed trigger
laws to take effect have been forced to con tinue their pregnancies even when their lives have been in grave danger. Disturb ingly, the doctors’ determination that their patient was facing a life-threatening situa tion wasn’t good enough for their laws to permit termination — instead, the opin ions of hospital administrators and law makers uninvolved with the patient’s care were sought out, seemingly in violation of HIPAA’s patient privacy laws.
On July 11, the Centers for Medicare & Medicaid Services (CMS) clarified that EMTALA overrides state laws related to the medical screening examination, stabilizing treatment and transfer requirements. Under EMTALA, if a physi cian believes that an abortion is needed to stabilize a patient with an emergency medical condition, this treatment must be provided regardless of state law. It also states that the physician or other qualified medical personnel determines what is and is not an emergency medical condition. EMTALA also protects physicians who perform an abortion in order to treat a pregnant woman’s emergency medical condition from legal action by the state. Unfor tunately, EMTALA does not protect against a hospital or physician being sued, and in the state of Texas, a lawsuit has already been filedthat challenges EMTALA’s protections for abortion care.
To be sure, emergency physicians are not abortion providers, and we will rely on our OB/GYN colleagues to work with us when the life of a pregnant woman is in danger. Physicians and their hospitals must fight to assure that EMTALA continues to offer the protections it was designed to provide. For politicians and lawmakers who propose to deny care for gravely ill pregnant women in need of emergency abortions, or who try to persecute treating physicians who are simply doing their job, the courts must make it clear that EMTALA is pre-emptive over state laws that may be more restrictive.
Patients have a right to privacy under HIPAA, and physicians have not only a right, but an obligation, to provide unrestricted emergency medical care under EMTALA. If you’d like to weigh in further, go to medical school.
Dr. Maria C. Raven (MD, MPH, MS, FACEP) is a practicing emergency physician and the chief of emergency medicine at UCSF Medical Center. She is professor and vice chair in the UCSF Depart ment of Emergency Medicine. She researches the intersection of medical, behavioral and social needs in the emergency department.
The No Surprises Act1, a bipartisan effort to reduce the number of surprise medical bills, went into effect on Jan uary 1. As significant as this legislation is—surprise bills are one of the biggest drivers of medical bankruptcy in America—the act is still being overlooked.
This legislation remains unfa miliar to those it affects most, specifically patients, doctors and outpatient surgery centers. But it has the potential to drastically reshape the economics of health care in America. Those who have heard about it likely know it makes surprise bills rarer—but more importantly, it aims to make transparency a routine part of American health care.
In addition to minimizing surprise bills after a trip to the emergency room, the No Surprises Act (NSA) also minimizes surprise bills in non-emergency settings. It requires a level of price transparency for both insurance and self-pay health care services that will affect Americans and the medical establish ment far more than previous price transparency rules imposed on hospitals. In many ways, this bill affects the day-to-day rou tine of providers even more than the Affordable Care Act did. And yet, many consumers and providers are unaware of it.
“The No Surprises Act aims to reduce uncertainty over med ical costs by:

• Outlawing out-of-network bills in emergency situations, except for ground ambulances
• Requiring financial consent and out-of-network cost sharing estimates in the non-emergent setting
• Requiring a Good Faith Estimate for uninsured/self-pay individuals, including those undergoing multi-session or multi-provider counseling, therapy or aesthetic services”
The aspect of the law garnering the most attention addresses patients who receive treatment in an emergency setting. While insurance may cover much of their "in-network" care, patients can get surprise bills from other providers in the facility, such as a radiologist who reads a patient's x-rays but are not within their insurance network. Depending on the patient's coverage, these medical bills from out-of-network (OON) providers may not be covered at all, or only partially covered, requiring the patient to shoulder a greater share of the cost.
With implementation of the NSA, the radiologist's bill in that scenario would be switched to a lower in-network rate and covered by the patient's insur ance. What that in-network rate should be is the basis for litigation by several parties against the Center for Medicare Services (CMS), the agency responsible for the regulations implementing the NSA. Amid the litigation, CMS is rewriting regulations pertaining to what the new in-network rate should be and it appears it will take into account several factors including, but not limited to, the median in-network rate, complexity of case, historic reimbursement and dominance of payors in the community.
The NSA also protects patients from getting surprise bills when they receive OON treatment at an in-network facility during non-emergency treatment. Consider a woman who delivers a baby at an in-network hospital, with care from an innetwork ObGyn—but an anesthesiologist who is out-of-network. That could result in a surprise bill that is not covered by the patient's in-network benefits. With the NSA, this surprise bill would be covered at the in-network rate as eventually deter mined by forthcoming CMS regulations.
The most transformative aspect of the NSA is its require ment for price transparency in two situations: 1) when a patient chooses to receive care from an OON provider in a non-emer gency situation and 2) if a patient is paying for care without insurance.
In the case of a patient choosing to receive non-emergency care from an OON provider, he or she must consent and accept the higher OON charge from the doctor. But that consent has to be informed. The patient must be told how much their out-ofpocket cost will be.
That's not the same as what the doctor will charge, however. Providers must now give patients an estimate of what their out-of-pocket expense will be. Knowing their actual out-ofpocket cost for the care provided by an out-of-network doctor allows patients to make informed financial decisions. This level of transparency was not a guarantee prior to the NSA.
While consent for a balance bill can be given for an out-ofnetwork provider in a non-emergency situation, that is not always allowed. Whether it is for emergent or non-emergent care, the NSA strives to minimize surprise bills when the patient is unable to choose their provider. For example, choosing a pro vider is not practical in an emergency setting, so no provider can obtain consent for balance billing. Even if it is a non-emergent situation, the consumer would not normally have the oppor tunity to choose their radiologist, pathologist, anesthesiolo gist, hospitalist, assistant surgeon or neonatologist, and for this reason, the Center for Medicare and Medicaid Services (CMS) disallows these providers from obtaining consent for balance billing – even in a non-emergent setting.
In the case of uninsured or self-paying patients, NSA requires that patients receive a Good Faith Estimate (GFE) up front. The GFE is required even for those patients who have insurance but are choosing not to utilize it—for instance, if the cash rate is less than the insurance rate because a consumer hasn't met their deductible yet.
Similar to the estimate a doctor must provide a patient seeking out-of-network care, the Good Faith Estimate (GFE) must include the expected costs associated with a procedure. But unlike the OON estimate, there are no cost-sharing calculations since the patient doesn't have or is not using their insurance.
The GFE also differs from the OON estimate in a more sig nificant way. For the former, a provider must include all charges that would be reasonably expected in the patient's episode of multi-session or multi-provider care. That includes not only the doctor, but also the anesthesiology and operating room fee as well as any ancillary fees such as, but not limited to, lab work, radiological or pathological studies.
A GFE must also be provided when patients are receiving multi-session care. In the case of mental health, physical therapy, counseling sessions or even multi-session laser hair removal, a patient must receive an estimate of the cumulative costs of all sessions over a time period not exceeding a year. An updated GFE is required each year but not for each individual session.2 On top of that high degree of transparency, patients have a right
to dispute any charges that are $400 greater than the GFE. To avoid these disputes, doctors are incentivized to ensure accurate pricing up front, and when appropriate, overestimate additional charges. Not only does this ensure that possible charges match actual charges, but it addresses the original purpose of the NSA: avoiding surprise bills after a procedure.
And while minimizing surprise bills may capture the head lines, the integration of price transparency into the daily routine of the health care establishment is the real news here. Prior to the NSA, health care was immune to basic market forces such as up-front pricing seen in other sectors of the economy. But now, just as a consumer can determine the cost of a car or house prior to buying, it's possible to know their costs prior to receiving care, thanks to one transformative Congressional act.
Dr. Jonathan Kaplan is a board-certified plastic surgeon based in San Francisco, CA and founder/CEO of BuildMyHealth3, a price transparency-lead generation platform.

Dr. William Cassidy is Louisiana's senior US Senator and co-author of the No Surprises Act with US Senator Maggie Hassan (D-NH).

1. NoSurprisesAct.com
2. https://www.buildmybod.com/blog/cms-faqs-about-con solidated-appropriations-act-2021-implementation-goodfaith-estimates-gfe-for-uninsured-or-self-pay-individualspart-2/
3. www.buildmyhealth.com
We applaud the recent action by the Biden administration to restrict the sales of menthol cigarettes and flavored cigars. In this article, we review the ratio nale for a ban and offer recommen dations on ways to make the Food and Drug Administration’s (FDA’s) proposed rule stronger.

Menthol is used extensively in health care products due to its anesthetic and antimicrobial effects. The substance is also intentionally added by tobacco manufacturers to a tobacco blend of burley, flue-cured, and ori ental tobacco with additional ingredients. Menthol reduces the irritating nature of tobacco smoke aerosol on the airways, thus promoting greater inhalation of the smoke mixture of nicotine and combustion byproducts.
Tobacco products in the marketplace are categorized into two distinct types: non-menthol cigarettes and menthol ciga rettes (for example, Newport, Kool, and Salem). While the mar keting of cigarettes as either menthol or non-menthol might lead some smokers to believe that these are two distinct tobacco products, the reality is that menthol is used in all tobacco prod ucts. When menthol is added at a higher concentration of 5–9 percent weight/weight (w/w) basis the product is marketed as a menthol product, whereas when menthol is added at a lower concentration (generally less than 1 percent w/w), the product is referred to as non-menthol. (The term “weight/weight basis” means that the percentage of various components in a whole is determined by weight, with volume disregarded.) The proposed FDA product rule will prohibit the industry’s use of higher levels of menthol as a characterizing flavor but allow the continued use of menthol as an additive at lower levels in the remaining cigarettes.
A tobacco blend goes through several manufacturing steps before menthol is sprayed on the blend. Casing operations use additives such as licorice, honey, and chocolate to smooth out the harshness of the finished product. In 1986, the Federal Cig arette Labeling and Advertising Act required tobacco manu facturers to submit annually to the Department of Health and Human Services all the additives they use in tobacco manu facturing. The listing of all the additives (600 plus) from each
manufacturer are collated and presented together (in past years by the law firm Covington and Burling) to protect any proprietary information that give indi vidual brands their dis tinctive flavor and aroma. Many of these additives are considered generally recog nized as safe for use in food and cosmetics, although they undergo pyrolysis in a cigarette that may change their chemical structure and toxicity, and the possible health hazards afterwards remain unresolved. The Flavor and Extract Manufacturers Association supplies organic-based flavors to manufacturers that are used in final tobacco blends, but in very low concentrations.
The proposed FDA ban is also supported in extensive tobacco industry internal documents produced in tobacco litigation by the states’ attorneys general and in individual product liability suits, which reveal that the industry worked for decades to opti mize menthol delivery and yields, resulting in numerous patent applications since the 1960s. The tobacco industry also har nesses the characteristic effects of menthol in novel ways other than as an intentional additive to the tobacco blend. A recent innovation is a crushable capsule containing menthol that is imbedded in the tobacco column (high menthol delivery on demand); other approaches include menthol coating of pack aging components and in the cellulose acetate filters. Menthol then migrates into the tobacco rod via mass transfer. The inten tion behind all these methods to increase delivery of menthol is severalfold: to permit an increased puff volume and deeper inhalation into the lungs; to enhance and strengthen nicotine addiction; to facilitate the ease of initiation by children; to com plicate tobacco cessation; and to allow manufacturers to use cheaper, lower-quality tobacco. Menthol does not undergo any chemical modifications in the aerosol delivery to the smoker in a combustible product and acts an independent chemical in all other types of tobacco and medical products.
The industry has used menthol’s attributes to target “at risk” groups, such as African Americans, women, children, and LGBTQ individuals. The science of menthol in tobacco products serves as a strong foundation for the proposed FDA ban, which has been awaited since 2011, when the FDA Tobacco Products Sci entific Advisory Committee (TPSAC) concluded that “Removal of menthol cigarettes from the marketplace would benefit public health in the United States.” The World Health Organization’s Framework Convention on Tobacco Control, the world’s first global public health treaty, recommended banning menthol tobacco products. The World Health Organization’s Framework Convention on Tobacco Control, the world’s first global public health treaty. Numerous entities—first Brazil in 2012, then the European Parliament, then Ethiopia, Moldova, Turkey, and seven provinces in Canada—moved forward with a menthol ban. The EU legislation prohibits the use of menthol as a characterizing flavor at the higher concentration but allows its continued use as an additive in lower concentration in cigarettes. The Canadian legislation is the most comprehensive, prohibiting menthol’s use at any concentration as an additive in cigarettes, most cigars, papers, and filters.
In 2016, a Federal Appeals Court ruled against a tobacco industry challenge to the FDA TPSAC recommendation, opening the door for menthol to be banned as a cigarette additive in the US. Since then, a wave of menthol bans have been adopted in cities and states around the nation, championed by the African American Tobacco Control Leadership Council. The state of Mas sachusetts passed a statewide menthol ban in 2019, followed by California in 2020.
First, the proposal does not address menthol use in e-ciga rettes or vapor products that have great appeal to youth. Second, even if the proposed rule is adopted, a menthol cigarette smoker who wishes to continue can readily construct their own men thol products by mixing bulk cans of tobacco with commercially available United States Pharmacopeia (USP) menthol (often available as crystals). The proposed FDA rule will prohibit the manufacture, distribution, and sale of commercially available menthol drops, capsules, filter tips, or cards that can be added to roll your own tobacco. We would recommend that USP menthol marketed to be added to bulk tobacco also be included in this prohibition.
Third, evidence in Canada suggests that going further and also removing menthol as an additive at any level—not just at high-enough levels in which menthol becomes a “characterizing flavor—could be a more effective smoking cessation strategy and help smokers to quit rather than switch to “non-menthol” ciga rettes that still contain menthol at a lower concentration. With this approach, menthol smokers in Ontario were more likely to make a quit attempt, be successful at quitting for six months, and did not significantly switch to other flavored tobacco products, e-cigarettes, or to contraband menthol cigarettes. Finally, the proposed FDA rule does not have a consistent approach to all uses of mentholated tobacco products—it does not disturb the agency’s previous grant of an exemption for menthol-flavored “heat not burn” products and does not include vaping devices that are still undergoing premarket tobacco product application and review. The complete ban of menthol (both as an additive and a characterizing flavor) would resolve these inconsistencies and encompass all menthol tobacco products.
John Maa, MD, is a general surgeon in San Francisco, California, and was the 2018 president of the San Francisco Marin Med ical Society and previous chair of the Uni versity of California Office of the President Tobacco Related Research Program. He is on the board of directors of the American Heart Association Western States Affiliate, which supports the proposed menthol rule.

Jeffrey Wigand, PhD, is a medical biochemist and former vice president of research and development and environmental affairs at Brown & Williamson Tobacco Corporation based in Louisville, Kentucky, who worked on the development of reduced-harm cigarettes and in 1996 blew the whistle on tobacco tam pering at the company.

Voting begins on 10/31/22 and ends at 5pm on 11/14/22. Electronic ballots will be available at this link the day voting begins.

The system is broken and needs fixing. We must change the culture to treat physicians and anyone working in health care as humans not superheroes. When we acknowledge our humanity, we enhance relationships, communication, quality and caring, we bring back the art of medicine as well as joy, meaning, purpose, passion, and fun.
As your fearless wellness warrior, this quarter I am opting to share a number of recent podcasts and YouTube videos on Physician Wellness. I hope you enjoy the opportunity to LISTEN and WATCH, as well as READ.
The Super Hero Cape Causes Harm: Healthy Physicians Are Humans Healing Humans
The vision of physicians as heroes was shared prominently during the covid pandemic. The cape analogy causes harm to many physicians.
Appreciation for our hard work is welcome but physicians, and nurses, and everyone who works in healthcare are humans first.
There should be human expectations of us and we need to have human expectations of ourselves.
Anythingotherthanthisisarecipeforburnout,exhaus tion, and long-term disaster to our healthcare system.
We are stronger when we recognize our common humanity.
We are stronger when we acknowledge our fallibility.
We are stronger when we are a team and not expecting to hold back locomotives.
We are stronger when we see our lives as one without victims, villains, or superheroes.
The hero cape actually is a heavy burden for many.
The hero cape leads to isolation and pressure to control things out of our control.
We can do everything right and things will still go wrong because we, and our patients, are humans.
Take a listen to this Mindful Healers Podcast Episode to learn more by scanning the QR code with your smartphone:
What if you dropped the cape?
What thought patterns and habits do you practice that you were taught during training, but don't serve you anymore?
Many helpful well-being lessons can be learned from indus tries outside healthcare.
Perspectives outside of medicine are integral to solving the complex problem of physician burnout and creating a sustain able practice of medicine in the United States.
In this Mindful Healers Podcast episode, we share lessons from artificial intelligence, the military, interior design, virtual reality, photo-journalism, yoga, art, and nature about how to bring more sustainability and wellness into the practice of medicine.
Included are many insights from the Mindful MD/Teravana Foundation's Think Tank on Physician Well-Being held in June 2022. Take a listen to this Mindful Healers Podcast Episode by scanning the QR code with your smartphone:



The harm we do to ourselves as physicians is unintentional. It is done in the name of serving others. And it is harmful none theless.
Caregiver wellness is a cultural problem in medicine and beyond. The pandemic has brought it to a crisis level.
Burnout is super costly financially.
It impacts quality, access and service.
If caregivers are not healthy, we can’t provide great care.
Even if we can hold for a while, it's not sustainable for a long time.
Our broken system is a big part of the problem.
Our medical training, our expectations of ourselves and others, and our societal culture are also a part of the problem.
We are also part of the problem.
Our underlying thought patterns and natural tendencies, the exact ones that helped us successfully get through training and professional school make burnout worse.
Then we are trained to think and behave in certain ways, in the name of service and care. We are told if we don’t do it this way, we don’t care about patients.
Take a listen to this talk I gave to my 1997 UCSF medical school class at our virtual reunion to learn more.
On Sunday, August 28th, SFMMS Physi cian Wellness Com mittee Chair, Dr. Jessie Mahoney led yoga and community building in the Celebration Garden of the San Francisco Botanical Garden in Golden Gate Park. Yoga was followed by social izing and community building between SFMMS physician colleagues. Special thanks to Dr. Mahoney for leading this event and the SF Botanical Garden for hosting SFMMS members.


Listen to this podcast to enjoy a conversation about the inter section of beauty, space, nature, health and healing and optimal healing environments by scanning the QR code with your smart phone:

Jessie Mahoney is a Pediatrician, a certified life coach for physicians, and a yoga instruc tor. She is the Chair of the SFMMS Physician Wellness Task Force. She practiced Pediatrics and was a Physician Wellness leader at Kaiser Permanente for 17 years. She is the founder of Pause and Presence Coaching where she sup ports and empowers her physician colleagues using mindfulness tools and mindset coaching. She specializes in helping ease career transitions and burnout, parenting struggles, and relationship challenges. She is a leader of the Mindful Healthcare Collective and is co-host of the Mindful Healers Podcast. She teaches virtual weekly yoga to physicians and other healthcare providers and leads yoga, coaching, and wellness retreats in spectacular natural locations. You can read her blog at www.jessiemahoneymd.com. You can connect with her at jessie@jessiemahoneymd.com.
A quarterly weekend offering of free Mindful Yoga for Healers. This is specifically for SFMMS members to join their colleagues in order to heal, replenish, restore, and connect!

Sign up at https://mindfulyoga.jessiemahoneymd.com/ to be notified of class dates and times.
The fall SFMMS book club will feature our most popular SFMMS Summer Reads, "Atlas of the Heart: Mapping Meaningful Connection and the Language of Human Experience" by Brené Brown. To learn more and to register, visit our SFMMS Wellness page at www.sfmms.org/get-help/physician-wellness.
To learn more about upcoming wellness events or to view recordings of past events, visit the SFMMS Wellness Page at www.sfmms.org/get-help/physicianwellness.
Since 2016, the Nocturnists have uplifted the voices of over 350 healthcare workers through sold-out live performances and their acclaimed podcast. Their live performances help clinicians develop their stories for the stage, enabling them to speak publicly about the fears, doubts, joys, and passions that shape their personal and professional lives.

With the generous support of the Nocturnists, SFMMS Wellness raffled tickets to our membership to "TOGETHER AGAIN," their live performance on the evening of Friday, June 10th at the Brava Theater in San Francisco. Attendees heard from 8 wonderful sto rytellers, each with a unique spin on the theme.
A monthly weekend offering of free Mindful Yoga for Healers. This is specifically for SFMMS members to join their colleagues in order to heal, replenish, restore, and connect! Sign up at https://mindfulyoga.jessiemahoneymd.com/ to be notified of class dates and times.
Back by popular demand, SFMMS Wellness raffled sponsorship for our members to attend one of three one-day retreats at Pie Ranch on either Sunday, June 12th, Thursday, June 23rd or Saturday, September 24th. The Honoring Diastole Wellness Retreats are led by SFMMS Wellness Com mittee Chair, Dr. Jessie Mahoney and SCCMA Physician Wellness Leader, Dr. Gail Wright of SCVMC Pediatric Cardiology. You can sign up and learn more here: https://www.jessiemahoneymd.com/honoring-diastole

“I was initially skeptical about the value of a day-long retreat - but this day was deeply therapeutic.”
– Chief Infectious Disease, TPMG
“Thank you for the most soul (and belly) nourishing program. It was just what I needed. The location was incredibly special. Truly a magical day.”
– Marin Endocrinologist
What is physician coaching? Physician coaching is an evidence based intervention to decrease burnout and improve quality of life. (JAMA 2019) It is a safe space to explore your career and life frustrations, resentments, dreams and desires. It is preventive care for a sustainable and enjoyable career in medicine. It provides you with a toolbox of strategies to help you optimize your potential, productivity, and joy. It helps minimize stress and ease struggle. Professional athletes have coaches; physicians need them too.
SFMMS Wellness raffled 45 minute intro coaching sessions with local, certified physician coach to our membership in June. We plan on raffling more opportunities like this to our membership in Fall 2022. If you are interested in learning more, please email Molly Baldridge, SFMMS Director of Engagement at mbaldridge@sfmms.org.
To view recordings of past events or to register for upcoming events, visit the SFMMS Wellness Page at www.sfmms.org/gethelp/physician-wellness.
Our Physician Wellness Committee curated an SFMMS Summer Reads list of books for Summer 2022. In lieu of an SFMMS book club meeting this summer, members were randomly selected to receive the Summer Reads book of their choice. You can still enjoy the following curated list this summer:
"Can't We Talk about Something More Pleasant?: A Memoir" by Roz Chast

"The Conscious Parent: Transforming Ourselves, Empowering Our Children" by Dr. Shefali Tsabary
"The Menopause Manifesto: Own Your Health with Facts and Feminism" by Dr. Jen Gunter
"Things That Matter: Overcoming Distraction to Pursue a More Meaningful Life" by Joshua Becker
"An Invitation to Pause... again: musings from a mindfulness coach about life and dementia" by Janet Archer "Life's Messy, Live Happy: Things Don't Have to Be Perfect for You to Be Content" by Cy Wakeman

The past two years have been among the most difficult we’ve experienced in the history of modern health care, and our challenges have been intensified by the separation brought about by social distancing and remote work. Kaiser Permanente has been exploring ways to see each other in person, while maintaining safety protocols for social distancing. Just as we’ve missed those connections, our communities have missed the annual events that bring us together to celebrate what makes the Bay Area such a vibrant place to live and work.
That’s why we are excited to be participating in some of the community events that we’ve traditionally sponsored in the past.
After a two-year hiatus, the renowned SF LGBTQ+ Pride Parade and celebration will take place on June 25 and 26, commemorating the Bay Area’s LGBTQ+ communities and allies.
KPSF has a long history of involvement with the Pride Parade, the largest celebration of its kind in the country, which typically draws more than a million people from around the world. We’re proud to say that 2019 was our 25th consecutive year as one of the parade’s top sponsors, and equally proud that so many of our physicians and employees from Northern California participate and show their support.
At events such as these, we will be taking care of ourselves and our communities by making safety a top priority. All events sponsored by Kaiser Permanente will abide by city, county, and state COVID-19 guidelines. We will also take into consideration risk factors published by the CDC such as the number of COVID-19 cases in the community and whether the event is held outdoors.
Kaiser Permanente will also be sponsoring Carnaval, the two-day festival celebrating the diverse Latin American, Caribbean, and African Diasporic roots of the Mission District and the San Francisco Bay Area. Now in its 44th year, Carnaval has grown to be the largest multicultural celebration on the West Coast. This year’s theme, Colores de Amor: Inclusivity, Family, & Community, reminds us why its’s important for our communities to resume holding the events that strengthen our connections.

With so many Marin County residents entrusting Kaiser Permanente with their care, we were pleased to open the new San Rafael Park Medical Offices in July.
For more than 60 years, Kaiser Permanente San Rafael has been a part of Marin County, caring for our patients and promoting the health and well-being of our community. The new offices were designed with the community in mind, guided by our commitment to high-quality care, high levels of customer service, and convenience. San Rafael Park Medical Offices offer comprehensive primary care and onsite access to pharmacy, lab, rehabilitation therapies, imaging, endocrinology, and eye services—all under one roof.
The departments and services available at San Rafael Park Medical Offices: Adult and Family Medicine; Endocrinology; Health Education; Imaging; Lab; Ob-gyn; Ophthalmology; Optometry; Outpatient Eye Surgery Suite; Pediatrics; Pharmacy; Physical/Occupational Therapy; and Vision Essentials (includes Optical Sales).
“At this new technologically advanced building, our members can expect to receive the same high-quality, integrated, and industry-leading care they’ve come to depend on,” says Naveen Kumar, MD, Physician in Chief, San Rafael Medical Center. “I have tremendous gratitude for our care teams, whose clinical excellence is reflected in this beautiful new space.”
The project represents years of hard work and thoughtful collaboration with environmental stewardship top of mind. One example was the decision to repurpose an existing building instead of constructing one from the ground up. The three-story, 145,000 square-foot building has features like all LED lighting, electric vehicle charging stations, reclaimed water in the plumbing fixtures, and solar panels, which provide 100 percent of the building’s electrical needs. There are also bike racks and commuter showers to make it easy to leave the car at home.
The San Rafael Park Medical Offices was years in the making and is a testament to the San Rafael leadership team’s long and deep commitment to our community. We welcome the opportunity to serve the broader Marin County and surrounding communities in our spacious new building.!


The San Francisco Free Clinic was founded in 1993 by two CPMC physicians (Drs. Patricia and Richard Gibbs) to provide free medical care to people with no health insurance. SFFC would be grateful for volunteer help when needed for our uninsured patients. Volunteers can be involved in a variety of ways, including being available for phone con sults, donating 1 visit per month within your own clinic or seeing patients at SFFC. All specialties are welcome, and in particular we are seeking volun teer specialists from Dermatology, Endocrinology, Neurology and Urology. Volunteering is a great opportunity to be a part of an award-winning clinic providing much needed medical care to people who cannot find it elsewhere.
“This is why I went to medical school” – Dr. Ed Kersh, Volunteer Cardiologist.
“I can’t imagine not being a part of the SF Free Clinic. The physicians, staff, and volunteers all work together to provide outstanding, compassionate, evidence-based care.”
– Dr. Janice Hansen, Volunteer OB/GYN.
“The SF Free Clinic is among my most rewarding experiences.”
– Dr. Nina Schwartz, Volunteer Rheumatologist.
For more information on the SFFC, please visit our website at www.sffc.org. If you would consider volunteering one or two consults per month or donating resources, please contact Dr. Ian Nelligan at inelligan@sffc.org.
Scan this code using your smartphone or visit sfmms.org/advocacy/leadership-opportunities to view the Slate of Candidates for the upcoming 2022 SFMMS Election

Voting begins on 10/31/22 and ends at 5pm on 11/14/22. Electronic ballots will be available at this link the day voting begins.
870 square feet, first floor medical office right off lobby. Lots of natural light. Fully functioning surgery room; private restroom. Plenty of on-site parking. $3.50 per square foot + PG & E. Call Karen, 415-339-2222. First floor medical office at 900 S. Eliseo, Greenbrae, 1321 square feet consisting of four rooms, each with a garden patio waiting room; private bathroom. Great for therapy, chiropractic, massage therapy, rehab or psychi atric office. Plenty of on-site parking. $2.50 per square foot plus PG & E. Call Karen 415-339-2222.


