










Your specialist for medical devices in


Tracheostomy tubes with an excellent realtionship between inner and outer diameter


Halberstadt M edizintechnik GmbH Straße des 20. Juli 1 D - 38820 Halberstadt Tel. 0049 (0) 3941 - 668 6 Fax. 0049 (0) 3941 - 245 65 www.primed-halberstadt.de primed@primed-halberstadt.de

interact with us
Steve Barclay is back for his second stint as health secretary after a very short spell earlier this year. Meanwhile two recent health secretaries have announced they will not be standing for reelection.
At the same time, the NHS is facing unprecedented challenges, with record backlogs and staff shortages. This is expected to be the toughest winter on record for the NHS, with the threat of a “twindemic” and already freezing temperatures and large amounts of snow. Calls for a pay rise and concerns about patient safety have also led to the largest nurses strike in NHS history.
This issue of Health Business magazine has lots of information on how to prepare for and deal with the cold weather from a facilities management point of view, as well as informative articles on recruitment and how volunteers can contribute to the NHS.

We also have a look at medical equipment, how it can help tackle the backlog and the advancement in home testing. Finally, we look at the pros and cons of digital transformation and the cyberthreat to the NHS.

 Polly Jones, editor
Polly Jones, editor
© 2022 Public Sector Information Limited. No part of this publication can be reproduced, stored in a retrieval system or transmitted in any form or by any other means (electronic, mechanical, photocopying, recording or otherwise) without the prior written permission of the publisher. Whilst every care has been taken to ensure the accuracy of the editorial content the publisher cannot be held responsible for errors or omissions. The views expressed are not necessarily those of the publisher.ISSN 1478-7687
Health Business is a member of the Independent Press Standards Organisation (which regulates the UK’s magazine and newspaper industry). We abide by the Editors’ Code of Practice and are committed to upholding the highest standards of journalism. If you think that we have not met those standards and want to make a complaint please contact Polly Jones or Angela Pisanu on 0208 532 0055. If we are unable to resolve your complaint, or if you would like more information about IPSO or the Editors’ Code, contact IPSO on 0300 123 2220 or visit www.ipso.co.uk

EICR testing and remedials. Thermography – nonintrusive testing of the distribution boards. Our advanced camera’s will indicate any faults within the db’s as a heat source, not visual to the eye.
We supply and install quality energy saving lighting which are maintenance free and backed by our industry leading warranties. Due to our experience within this sector, we can advise and source lighting to suit any environment.


We o er a complete turnkey electrical installation service, from electrical design to a complete building installation. Our load monitoring machines can be installed nationally, these measure a sites power usage and rating.
Our skilled team will complete site surveys, including load monitoring to validate the power availability of a site. We can then supply and install the best suited electric car chargers along with any infrastructure requirements. Back-end software can be added allowing clients to manage the chargers and generate revenue.
Our highly skilled team are fully employed by TCS and further training is regularly undertaken in our inhouse training academy. We utilise the latest innovative technologies such as augmented reality glasses to reduce our carbon footprint which also improves our quality and speed of service to our clients.
Funding packages are available for all works.

T: 0845 5009006 E: nhs@tcsukltd.com W: www.tcsukltd.com

Chancellor delivers Autumn Statement; NHS marks two years since first Covid jab; and Government announces independent review of Integrated Care Systems 15
With winter now well underway, with cold weather, rain and even snow, there is lots of facilities management work you can do to protect your properties. HB shares ten top tips for facilities management prep for winter
In this issue’s Expert Panel, Benedict Wallner, general manager and Regina von Campe, quality assurance manager at preOx.RS GmbH discuss The European Union Medical Device Regulation - Regulation (EU) 2017/745 (EU MDR) and how it affects SMEs

35
With winter well under way, road maintenance is more important than ever. With large hospital sites having a surprising amount of mileage, it’s a good idea to get ahead before the cold weather gets worse 25

Signage can bring real benefit to your organisation and it is a very cost-efficient way to do so. HB looks at the benefits of good signage 31
Will Lloyd, technical manager at the Fire Industry Association discusses the importance of fire safety in hospitals
Richard Hipkiss, development director of the Modular and Portable Building Association (MPBA) makes a case for volumetric manufactured buildings in shaping a net zero future 39

Recruiting talent to the public sector is not easy, but here are some tips to help 43
Maeve Hully, director of volunteering, Helpforce explains the benefits of volunteering for patients, the workforce and the health service as a whole 47
Barbara Harpham, chair of the Medical Technology Group explains how medical technology can help clear the backlog
Valerie Phillips, healthcare expert at PA Consulting discusses the advancement and benefits of at-home testing
Tim Morris, vice president, clinical solutions, Elsevier Health has a look at the pros and cons of digitised healthcare
Join the diverse UK digital health community for the ultimate learning and networking experience at London’s Business Design Centre, 14-15 March. Digital Health Rewired is for anyone wanting to make a difference in UK digital health including NHS and social care, private healthcare, suppliers, start-ups, innovators, policy makers and patients
Cybersecurity will always be needed for the NHS, but what is the current threat level and what can be done to mitigate these threats?


Phil Howe, chief technology officer at Core to Cloud examines the cyberthreat to the NHS from nation state actors and cyber criminals
In this article, Barbara Harpham, chair of the Medical Technology Group, looks at regional variation in healthcare and how regions and hospitals can learn from each other to improve care


Dr Helen Davies, NHS general practitioner, population health/digital lead and Cegedim Healthcare Solutions’ Clinical Advisory Board member, lays bare Population Health Management and steps for NHS organisations to achieve it

Chancellor Jeremy Hunt has delivered his long-awaited Autumn Statement in the House of Commons.
Hunt began his speech by acknowledging that the UK is in a recession and that things will get worse before they improve.
Among the measures announced is a reduction in the threshold for when the highest earners start paying the top rate of tax, and a windfall tax on the energy industry.
Hunt has confirmed the government departments can expect a squeeze and that they will have to make “tough decisions to deal with inflationary pressures in the next two years”. He did say that overall spending on
The government is setting up an Elective Recovery Taskforce intended to help the NHS meet waiting list targets.
The aims are to eliminate 18-month waits by April 2023 and waits of over a year by March 2025.
The Taskforce will be chaired by Health Minister Will Quince and feature academics and experts from the NHS and independent sector to advise the government on ways to help the NHS recovery from the pandemic, and reduce waiting times.
The Taskforce will deliver a series of recommendations to the government early next year.
One topic of focus will be how the NHS can utilise existing capacity in the independent sector to cut the backlog.
Health and social care secretary Steve Barclay said: “The NHS is facing an unprecedented challenge to tackle covid backlogs.

“Hardworking staff have made strong progress but I want to turbocharge our current plans to bust the backlog and help patients get the treatment they need.
“The taskforce will look at sensible steps to utilise all existing capacity to slash waiting lists while ensuring the NHS always remains free at the point of use.”
Patients will also be able to access treatment and diagnostic tests closer to home, with the approval of 19 new one-stop shops for tests, checks and scans.
Diagnostic centres will be set up across the country including in football stadiums and shopping centres and will provide MRI, CT and x-rays. 91 centres are already in operation.
public services will rise for the next five years after accounting for inflation.
According to the chancellor, the health budget will be protected. However, he has called on the NHS to “join all public services in tackling waste and inefficiency. He said:
“That doesn’t mean asking people on the frontline to work harder, but rather asking challenging questions on how to reform all public services for the better.” Hunt has announced that the NHS budget will be increased by £3.3 billion in each of the next two years.
The chancellor also included an extra £1.5bn for the Scottish government, 31.2bn
for the Welsh government and £650m for the Northern Ireland executive to tackle pressures on schools and the NHS.
NHS chief executive Amanda Pritchard has responded to the chancellor’s autumn statement. Pritchard said: “While I am under no illusions that NHS staff face very testing times ahead, particularly over winter, this settlement should provide sufficient funding for the NHS to fulfil its key priorities. As ever, we will act with determination to ensure every penny of investment delivers for patients.”
He continued: “An efficient system addresses bottlenecks that delay patient care by designing new journeys for patients that avoid those delays.
“Because quicker – and therefore earlier treatment – will lead to better patient outcomes whether that is from earlier cancer diagnoses, with the announcement a couple of weeks ago on direct access for GPs, or on antibiotics – getting the right antibiotic first time, rather than the third or fourth time. Obviously bringing significant patient benefits, but it is also efficient in terms of cost.
“So an efficient system will get better treatment to the patient and improvement patient outcomes, but in doing so, it will also unlock value for money.”
The health secretary called for a move to more personalised care, with previous examples including at-home Covid tests and the Women’s Health Strategy.
Barclay began by highlighting the £6.6 billion of extra funding for the NHS over the next two years, as well as increased funding for social care that was announced in the Autumn Statement.
Barclay listed priorities including pandemic backlogs, operations, access to GPs, urgent and emergency care, ambulance handovers and delayed discharge.
Barclay put the focus on efficiency: “Now, efficiency within the NHS is often seen through the lens of finance.
“So, the case I want to make today is that efficiency is not just a finance priority – it’s a patient priority too.
“Because efficiency is an indicator of wider system health.”



He also urged senior clinicians to lead change and shared his pleasure that Professor Sir Tim Briggs has taken up the role of clinical lead for the Elective Recovery Programme. Barclay called for innovation and technology to tackle challenges such as cancer and GP pressures.
He concluded his speech by saying: “Covid is still with us. And so in particular are its consequences, in the form of pandemic backlogs.
“So we must continue to embrace the pace and risk appetite of the pandemic when it comes to innovating at pace and at scale, and better assessing how risk is scored when we do so.
“That is what I believe the British people rightly expect us to do, and if we are to confront the scale of challenges facing the NHS, that is what we need to do.”

a recruiter.
You deserve to work with a team that can help you choose when you work, at the tap of a button.
One that can offer you a job searching experience that combines the power of technology, with that human touch. That is made up of specialist recruitment consultants who offer you more choice, more often.
Choose Randstad Nursing and let us be more than just your recruiter.

your career is at the heart of what we do.
We work by focusing on you: your career aims, goals, and needs. Our wide scope of experience and our large client base means that we can offer you temporary or fixed-term nursing jobs in both the NHS and private healthcare sector, nationwide and free of charge for you.
If you are ready to explore new career opportunities, pick up extra shifts, or simply have a conversation with our team, reach out today:
randstad.co.uk/nursing 0161 245 3633
apply@randstad.co.uk
you are #morethananurse we are more than
Health secretary Steve Barclay has set out plans to amend NHS pension rules in order to retain more experienced NHS clinicians and remove barriers to staff returning from retirement.
The changes to pension rules will apply to all NHS staff, including senior doctors and are intended to support staff to remain in work for longer and boost the NHS workforce.
The changes include introducing flexibilities to allow retired and partially retired staff to return to work or increase their working hours without having payments to their pension reduced or suspended, meaning staff can claim a



portion or all of their pension benefits but continue working and contributing to their pension.
Health and social secretary, Steve Barclay, said: “The generous NHS Pension Scheme is one of the best in the country, but it’s not working as it should for everyone.
“We need a system where our most experienced clinicians don’t feel they have to reduce their workload or take early retirement because of financial worries. I also want to make it easier for staff that want to return to work to support the NHS to be able to do so without penalties.
“These proposed changes will help open up extra appointments so patients can see their GP and consultants more quickly. With record numbers of doctors and nurses working in the NHS alongside record funding, I’m focused on giving people the security of knowing the NHS will be there for them when they need it.”
A consultation on the changes has been launched and will be open for eight weeks. Any changes are likely to be implemented in Spring 2023.
The NHS has marked two years since the world’s first Covid jab by urging the public to get boosted before Christmas.
143 million doses of the vaccine have been delivered since the start of the campaign two years ago.
With cases rising again and more mixing over the festive period, the NHS is urging those eligible to come forward.
NHS chief executive Amanda Pritchard said: “The unparalleled success of the life-saving NHS Covid-19 vaccination programme, which began exactly two years ago when the NHS
administered the first covid vaccine in the world outside a clinical trial, has been the single most important reason we have been able to get back to a pre-pandemic way of life.
“The determination and dedication of NHS staff and volunteers up and down the country to respond with extraordinary speed and precision to rollout the vaccine is something we can all look back on with great pride – delivering more than 143 million doses so far – and staff are continuing to give hundreds of thousands of covid and flu jabs every single day to protect us all from serious illness.
“The health service is currently facing huge pressure from all angles – and while covid may feel like a thing of the past – we continue to deal with thousands of covid hospitalisations as well as the resurgence of flu and other respiratory viruses. Just as it was two years ago, the best thing you can do to avoid serious illness and hospitalisation is to make sure you are up to date with your covid and flu jabs.”
The government has announced a VaccineTaskforce-style approach to tackle public health challenges.
£113 million will be used to fund research into four healthcare missions: cancer, obesity, mental health and addiction, with the aim to “unlock the next generation of medicines and diagnostics to save lives, transform patient care and ensure UK patients are the first to benefit from medical breakthroughs”.

The government said the Vaccine Taskforce model will be used to harness world-leading research expertise, remove unnecessary bureaucracy, and strengthen partnerships.
It is hoped that tackling these healthcare challenges can save the NHS money, with the estimated cost of obesity to the NHS currently at £6.1 billion a year.
The prime minister Rishi Sunak, health and social care secretary Steve Barclay and business secretary Grant Shapps will meet with industry figures including NHS leaders and industry experts at the Life Sciences Council to discuss delivering innovations and improving NHS efficiency.
Sunak said: “The NHS faces real pressures, which is why we are investing over £100 million
in the technologies and medicines of the future to address some of the biggest public health challenges facing our country.
“This funding will improve outcomes for patients, ease existing pressures on the system and ensure that we are amongst the first to benefit from medical breakthroughs. Importantly it will also help save the NHS millions of pounds that could otherwise be spent on patient carefor example by tackling obesity which costs the health service over £6 billion annually.
“It is hugely welcome too that the highly successful Vaccine Taskforce, which procured millions of life-saving vaccines in record time during the pandemic, will now become a blueprint for how we harness the best talent and expertise from around the world and drive investment in research and development.”
£22.5 million will be spent on cancer research to develop immune-based cancer therapies such as vaccines which are targeted to a specific cancer.
£40.3 million will be invested in mental health to develop and introduce digital technologies, such as technology to monitor mental health at home.
£20 million is to be used for obesity, to trial how best to deliver new medicines and technologies for those living with obesity, particularly in deprived areas.
Finally, £30.5 million will be spent on addiction, to accelerate the development of new technologies to prevent deaths from overdoses.
Barclay said: “Conditions such as cancer and obesity prevent people leading long, healthy lives and cost the NHS billions of pounds every year.
“We’re leading the way in cutting-edge research which can find new ways to speed up diagnosis, enhance treatments and ensure a better quality of life for patients - both now and in the future.
“By harnessing the same spirit of innovation that delivered the vaccine rollout and working hand in hand with the NHS, industry and healthcare experts.
“We’re building a stronger, healthier NHS with record numbers of staff and record funding, to give people the security of knowing it will be there for them when they need it.”







Paid-for resources include RCN Leadership programmes, RCN Infection Prevention and Control, RCN Leadership in Sustainability, the RCN Cultural Ambassador Programmes, RCN Leadership in Physical and Mental Health Outcomes, and RCNi products.
General secretary & chief executive Pat Cullen said: “This is an exciting new development in our commitment to providing the very best evidence-based learning resources for nursing staff.
The Royal College of Nursing has launched a new learning hub for the nursing profession.

RCN Learn enables access to quality-assured educational resources to support clinical and professional development.
The content sits behind a secure log-in. According to which category a person is in, they may have limited access to specific resources.
Registered users can access free core resources including standards and frameworks, while RCN members can access hundreds of clinical and non-clinical learning resources. NMC registrants can access a purpose-built tool to help build, store and track their evidence for revalidation quickly.
The government has announced an independent review of Integrated Care Systems (ICSs) to improve health outcomes across the country.
The review into oversight of ICSs intends to reduce disparities and boost efficiency, financial accountability and autonomy. It will explore how to empower local leaders to focus on improving outcomes for their populations.
Possible measures include giving local leaders more control and also making them more accountable for performance and spending. National targets will be reduced with an attempt to make the healthcare system more transparent.
The review is to be led by Patricia Hewitt, former health secretary and current chair of NHS Norfolk & Waveney Integrated Care Board.
As of 1 July, there are 42 ICSs across England.
Hewitt said: “I am delighted to have been asked to lead this review of how Integrated Care Systems can best be empowered and supported to succeed.
“By bringing together local government, the NHS and the voluntary, community and social enterprise sector, ICSs provide the biggest opportunity in a generation to improve health outcomes, transform health and care services and reduce health inequalities. Despite the many challenges we face, I am excited by how much has already been achieved in many different systems, including in Norfolk and Waveney, and optimistic about what our partnerships can do in future as we respond to
the different needs of our own communities.
“This review will focus on how national policy and regulation can most effectively support and enable local systems to solve problems locally. It will build on the welcome work already done by NHS England to develop a new operating model.
“I look forward to working with colleagues from all 42 ICSs as well as DHSC, NHSE, colleagues in local government and others as we respond to the Health Secretary’s and the Chancellor’s invitation to help create a system of regulation and accountability based on the principle that change should be locally led and nationally enabled.”
Health and social care secretary Steve Barclay said: “I’m focused on supporting the health and care system through what we know will be a challenging winter but also crucially making the changes that will better prepare us for the future.
“Rather than a one-size-fits-all approach dictated from a ministerial office, local leaders are best placed to make decisions about their local populations and I want to empower them to find innovative solutions to tackle problems and improve care for patients.
“Fewer top-down national targets and greater transparency will help us deliver this aim and I am grateful to Patricia Hewitt for agreeing to lead this vital review to help us |get this right. I look forward to reviewing her findings.”
“For nursing to keep advancing, the true potential in every one of us must be reached. RCN Learn will help support members to realise that potential and attain their career goals. I hope it will empower nursing staff to embed an education and learning culture within their care delivery.”
According to a report by Health Education England, digital technologies will play a vital role in helping the NHS workforce cope with demands on the system in the future.
Demand for the NHS and social care workforce will continue to grow over the next decade and by maximising digital technologies, the transformation of workforce planning and supply, education and training, clinical decisionmaking and delivery of personalised healthcare services will be enabled.
The report expands on the legacy of the Topol Review, chaired by digital leader, cardiologist, and geneticist Professor Eric Topol, and looks further into how to ensure the health and care workforce is digitally ready for the future.

The report examines how digital technology is being used to develop a continuous learning environment and enable new ways of working. It also looks at how improved technology can help to organise health and care services and deliver them more efficiently.
The report also reveals that the use of digital technology will enable the NHS to widen access and participation for healthcare training and education, as well as promote diversity and inclusion.
Patrick Mitchell, director of innovation, digital and transformation at Health Education England said: “This report highlights how HEE’s approach to using current and emerging innovative technologies in educating and training future and current health professionals.
Earlier this year, Radar Healthcare launched its new podcast, What the HealthTech? The podcast, aimed at health and social care professionals, provides a platform for staying upto-date on the industry’s latest topics, challenges, ideas and innovation.
With a new episode out every Thursday, What the HealthTech? hosts a diverse range of well-known guest speakers in health and social care, engaging in open and honest conversations about some of the most important issues. Topics covered in the 32 episodes so far have included: Bridging the gender gap, Learning from Patient Safety Events, Mental Health Awareness, Learning from Tragedy and Caring about Care
This wide range of topics has already drawn guests from all over the UK, including Peter Walsh from AvMA (Actions Against Medical Accidents), Lee Davies and Lottie Moore from Public Policy Projects, Judy Walker from iTS Leadership, and many others, all of whom are doing outstanding work in health and social care.
The vision for the podcast came from Radar Healthcare’s head of marketing, Hayley Levene, who wanted to connect with audiences in a different way and create a space for healthcare professionals to be open and have honest conversations. “I wanted to inspire people with what we do,
because we’re a company that is inspirational, our product is different, and our people are different,” Hayley said of the inspiration, which grew out of a passion for Steven Bartlett’s podcast “Diary of a CEO.”
Only eight months since the launch, What The HealthTech? has attracted over 1400 listeners, 900 downloads and nearly 2,000 views on YouTube. One of the most popular episodes is ‘ The Road to Patient Safety,’ with Marcos Manhaes of NHS Improvement and Paul Ewers of Milton Keynes University Hospitals NHS Trust about the journey from NRLS to LFPSE and the future benefits for the NHS.
With some fantastic guests and topics on the horizon, What the HealthTech? is one to watch in 2023 - you can listen on all major podcast platforms or on the Radar Healthcare YouTube channel. Watch the most recent episode here

Want to be a guest? Reach out! Are you a health or social care worker who wants your voice to be heard, or an organisation that wants to talk about the work you’re doing? Radar Healthcare would love to hear from you – get in touch by emailing whatthehealthtech@ radarhealthcare.com
Visit www.radarhealthcare.com to learn more about Radar Healthcare and how they can help you make a difference.
www.radarhealthcare.com

The UK Health Security Agency (UKHSA) has published data on the take up of the flu vaccine among two to three year olds, and expressed concern at the low vaccination rates and the high rates of under fives hospitalised with flu.
According to the data, between 14 and 20 November, it is estimated that 200 children under five were hospitalised with serious complications caused by flu. Hospitalisation rates for flu are highest in the under fives.
The uptake of the flu vaccine is 30.9 per cent among two year olds and 32.9 per cent among 3 year olds. This rate has dropped by around 11 per cent compared to the last two years.
The UKHSA said: “Flu is now circulating at higher levels than recent winter seasons and young children are particularly vulnerable



A £3 million investment has been announced for accelerated treatment for lung cancer in Scotland, with new diagnostic services to ensure patients receive faster access to treatment.
Lung cancer is the most common cancer in Scotland.
It is hoped the new services will ensure a faster process, reduce patient anxiety, reduce the risk of the cancer growing or spreading and reduce the risk of patients being unfit for effective treatment.
The new services will set timeframes for each step, with diagnosis set for 21 days after referral and treatment for most set at day 42.
Health boards will receive funding to realign services, so patients can receive multiple tests at the same time and reduce their trips to hospital.
Led by the Centre for Sustainable Delivery, the nationally developed lung cancer pathway is the first to be developed in Scotland. It will be funded by the Scottish Government’s Detect Cancer Earlier Programme.
Health Secretary Humza Yousaf said: “Lung cancer is the most common cancer in Scotland with around 5,500 cases diagnosed each year. The number of new cases is predicted to increase by 29 per cent for women and 12 per cent for men by 2027. That’s why we have to do as much as we can to tackle this disease.
“This redesign means faster and more efficient treatment for lung cancer patients. Even in advanced disease, newer treatments have improved patient outcomes but are highly dependent upon the patient remaining fit enough to receive those treatments.”
and can become seriously unwell. Due to coronavirus (COVID-19) restrictions in the past couple of years most young children will not have ever encountered flu. This means they will not have built up any natural immunity to this virus, so it is particularly important for them to take up the flu vaccine this year.”
GP practices are inviting those aged two and three for the nasal spray vaccination. Those who haven’t heard from their practice should contact them directly to make an appointment.
All primary school children and some secondary school children are also eligible for the nasal spray vaccine, which is usually given at school.
Dr Conall Watson, Consultant Epidemiologist at UKHSA, said: “Young children are particularly vulnerable to becoming very poorly
from flu. For the third week running we have seen hospitalisation rates among children under 5 jump up, with a 70 per cent increase in just the last week. Over 200 children were hospitalised because of flu in one week.
“Flu is now circulating at higher levels than recent years and because of the pandemic restrictions most young children will not have encountered flu before. This means they will have no natural immunity and are therefore at even greater risk this year.
“Two and 3 year olds can get protection with a free nasal spray vaccine from the NHS. Nobody wants their child to get sick so I strongly urge parents to book the vaccine at their GP surgery as soon as possible.”
The government has announced a £175 million fund for genomics research intended to save lives and improve health outcomes.
£105 million will be spent on a research study lead by Genomics England in partnership with the NHS. The study will explore the effectiveness of using whole genome sequencing to find and treat rare genetic diseases in newborn babies.
The Newborn Genomes Programme is intended to support vital healthcare research to enable better diagnostics and treatments to be developed and explore the potential benefits of safely and securely storing a patient’s genome on record to help predict, diagnose and treat future illnesses through their lifetime. The current NHS heel prick blood test is used to detect nine health conditions in babies, but it is believed genome sequencing can detect hundreds more.
£26 million will be spent on a cancer programme to evaluate genomic sequencing technology to improve the accuracy and speed of diagnosis for cancer patients and use artificial intelligence to analyse a person’s DNA, alongside other information such as routine scans.


There will also be £22 million for a programme to sequence the genomes of up to
25,000 research participants of non-European ancestry, who are under-represented in genomic research to improve understanding of DNA and its impact on health outcomes. The intention is to reduce health inequalities and improve patient outcomes.
Health and social care secretary Steve Barclay said: “We’ve made advancements in so many areas to improve people’s health – from ensuring ground-breaking new medicines get to patients faster to bolstering the NHS workforce to ensure we have record numbersand this plan, backed by £175 million, sets out how we will use the latest genomic technology to go further.
“The potential for genomics to revolutionise the way we deliver health care is great – if we can detect treatable illnesses earlier and ensure patients access potentially lifesaving treatment faster, we could improve people’s lives across the county, including thousands of babies through this new pilot.
“The NHS is a world leader in genomics and by investing in this cutting-edge research we’re cementing our status as a life sciences superpower.”

With winter now well underway, with cold weather, rain and even snow, there is lots of facilities management work you can do to protect your properties. HB shares ten top tips for facilities management prep for winter

Over the winter, weather can be unpredictable, snow, ice, rain and wind can all pose significant risk to buildings and you need to be prepared. Buildings themselves can tend be the main area of focus, and pre-emptive maintenance is a must to try to avoid any nasty surprises. However, management of the site is also important, making sure it is safe and access remains clear. This is especially important in the health service, with vulnerable service users.
Below are ten areas to focus on for the winter.
Perhaps the most obvious thing to check is water supply. A burst pipe can cause a lot of problems very quickly. You should check the mains, pipes and taps for any signs of damage and make sure taps are turned off properly to prevent pipes from freezing. It should be noted that vacant properties

Power is essential for the running of any organisation and extreme weather can have an effect on this. It may be worth investigating generators or other alternative power supplies such as solar panels, if your power supply is cut off, or even to combat the energy crisis.
If you do have an alternate power supply, ensure it is properly maintained and make sure you have a plan if power does go out.
Perform an energy survey and audit and identify where savings can be made. Make sure unused electrical items are switched off if the building is closed over Christmas.
Though you may not have used your heating for a while,
Ensure your boiler is serviced regularly, and make sure the heating is scheduled to come on if the building is to be empty over Christmas to avoid the aforementioned burst pipe.
To ensure your power and heating are used as efficiently as possible, make sure all your windows and doors are working properly and there are no draughts. This can also prevent mould. Some handles and catches may become stiff during the winter months, so it is important these are maintained and any issues are identified before they become a problem and you can’t shut the door properly.
Cleaning and hygiene Virus circulation is
pipestheCheckmains, and taps for any signs of damage and make sure taps are turned off properly to prevent pipes from freezing





The colder weather also means people are less likely to make use of natural ventilation – opening a window – giving airborne viruses more chance to spread.
Another part of cleaning is keeping buildings free of visible dirt. Wetter weather and fallen leaves mean dirt, mud, leaves etc can be brought into the building and spread, making it look unclean. Wet leaves and water also present a slip hazard.
The best ways to prevent dirt spreading are a good doormat and regular cleaning.
Though it may not seem obvious or easy, it is critical to check the roof of your building before winter. Roof maintenance is essential to protect against cold and wet weather. Check for missing, loose or cracked tiles before they get worse and check for leaks. You should also check for pooling water on flat rooves and any signs of damage on ceilings on the inside.
Following on from the above, make sure to check your gutters and downpipes for leaks and blockages. Ice and snow can make problems worse and a damaged gutter or downpipe can cause water to get inside the building.

Make sure to clear leaves from drains and the surrounding area to make sure they are not blocking drains ahead of any heavy rain. A blocked drain in a storm can become overwhelmed very quickly and cause access problems as well as flood damage to a property.
Fallen leaves can be a slip hazard, so it is important to clear them to ensure your
paths and walkways are safe, especially if your facility caters for vulnerable users.
Snow and ice are the biggest issues to face walkways and roads in the winter months. Be prepared for snow clearance and removal and make sure you have

a good supply of grit. It is important to grit surfaces before the ice hits. If you have plants, it is important to look after them too, so they survive the winter and provide a nicer place to work and visit. E

Make sure to check your gutters and downpipes for leaks and blockages. Ice and snow can make problems worse and a damaged gutter or downpipe can cause water to get inside the building




Outside lighting is essential to keep staff and services users safe, especially if a building is not in a public area with already provided street lights. It will be dark by the time most people leave work now and even when some people arrive. Good lighting reduces the likelihood of accidents, such as trips and vehicle collisions. It also acts as a deterrent for crime and makes those using the facilities feel safer. Check your wiring and lamps, and make sure any breakages are fixed. Ensure any timers and motion sensors are working.
Security is critical if your building is going to be shut over Christmas and as the days get shorter. Make sure your lights and alarm are working properly. You should adjust the timers on your lights as it gets darker sooner and get your alarm serviced. Dark nights and empty buildings are attractive for potential criminals.

NHS SBS’s Hard Facilities Management 2 (Hard FM Framework) offers a range of Hard FM facilities management products and services, including a range of estates and maintenance specialisms such as painting and decorating; kitchen equipment maintenance, plumbing services and building management systems.
The framework agreement has been specifically designed for the NHS and healthcare sector, with inputs from NHS
Security is critical if your building is going to be shut over Christmas and as the days get shorter. Make sure your lights and alarm are working properly





With winter well under way, road maintenance is more important than ever. With large hospital sites having a surprising amount of mileage, it’s a good idea to get ahead before the cold weather gets worse
In order to ensure proper resilience from your roads, it is a good idea to perform maintenance before the wet and cold weather properly sets in. As the old saying goes, “failing to plan is planning to fail” – leaving your road network vulnerable to the cold will cause more problems and prove more costly in the long run.

In the health service, road maintenance is particularly important. Ambulances need to be able to travel safely and quickly. Service users may be vulnerable or have mobility issues and it is important that they have a safe and easily accessible route to your door.
We all know that in cold weather, water gets into cracks in the road and freezes and expands, damaging the road surfaces. This combined with heavy traffic means potholes are formed and they only get worse.
Charity IAM RoadSmart reports that 79 per cent of the 2000 motorists surveyed in February believe that potholes are a bigger issue for them than three years ago. 90 per cent of those polled had been affected by potholes in the last year, 32 per cent said they had changed route to avoid them and 16 per cent said they had reported a pothole to the authorities.
Due to funding restrictions, there tends to be a shortterm approach to road maintenance, with reactive rather than proactive treatments, though authorities are doing what they can – ALARM
reports that 1.7 million potholes were filled last year – one every 19 seconds. However, it is much more expensive to repair individual potholes than to surface dress and maintain a road for ten years. Regular proactive maintenance of roads and paths is more sustainable and cost effective than letting roads and paths deteriorate, and then needing reactive repairs.
Many surface treatments are available, such as surface dressing and these treatments are quick to apply, generate minimum waste, lower the carbon footprint of roads and generate savings for local authorities. E
itHowever, is much more expensive to repair potholesindividual than to surface dress and maintain a road for ten years






It is not only cost benefits that can come from road maintenance – safety is also an important factor. Improved road surfaces mean better texture and better skid resistance – both of which are particularly important for the winter. It means that drivers won’t be swerving to avoid potholes, potentially endangering themselves and other road and pavement users. Again, this is more dangerous in winter, when the roads and paths may be icy.
Once the pre-emptive road maintenance is taken care of, you should plan for any adverse weather conditions. This means making sure that your gritters and snow ploughs are well maintained and you have a good supply of grit. You should also make sure the drivers are trained and accustomed to their routes. Make sure you keep up to date with short and long-term weather forecasts and ensure you have duty rotas to cover 24 hours in the case of extreme weather or sudden weather changes.
Of course, you should have winter maintenance plans, in coordination with any partners. These should monitor road surface conditions and the weather. Make sure systems are in place that means decision makers and implementors are able to make decisions and react appropriately.
Make sure you have enough grit supplies and a gritting plan before you need it, so you are ready to go before it gets icy or snowy. Identify priority areas. Grit should be laid before the ice forms. It is also good practice to keep a record of what has been gritted and when.
Share information with service users on your winter plan and let them know which
roads and paths have been gritted and if any roads or paths should be avoided. You can also share information with local residents on how they can help themselves and their neighbours. This could include removing snow when it is fresh, instead of after it has been compacted by footfall and traffic; never use water to clear snow and ice as this can refreeze and form black ice and look out for vulnerable neighbours if you are able.
Winter road maintenance is a big task, but forward planning can make a big difference in protecting your roads, improving safety, saving money and making a big difference for your service users. L

Share information with service users on your winter plan and let them know which roads and paths have been gritted and if any roads or paths should be avoided





Signage can bring real benefit to your organisation and it is a very cost-efficient way to do so. HB looks at the benefits of good signage
There are many different types of sign that your organisation may need: external to highlight where you are located, wayfinding signs to direct people to where they need to be, health and safety information, fire exits etc.
Signage is one of the first things people see when they visit your organisation. It is important for your signs to be clear, as this gives a good impression of your organisation. Clear and concise signage makes your organisation look trustworthy and legitimate, whereas misleading or unclear signage can be confusing and produce a negative impression. As the saying
goes, you never get a second chance to make a first impression and good signage shows you care about your staff and visitors.
Signs make it easy for people to visit. Clear and concise signage makes the visitor experience easier. In the health service, visitors from the general public maybe be unfamiliar or, depending on the nature of your organisation,
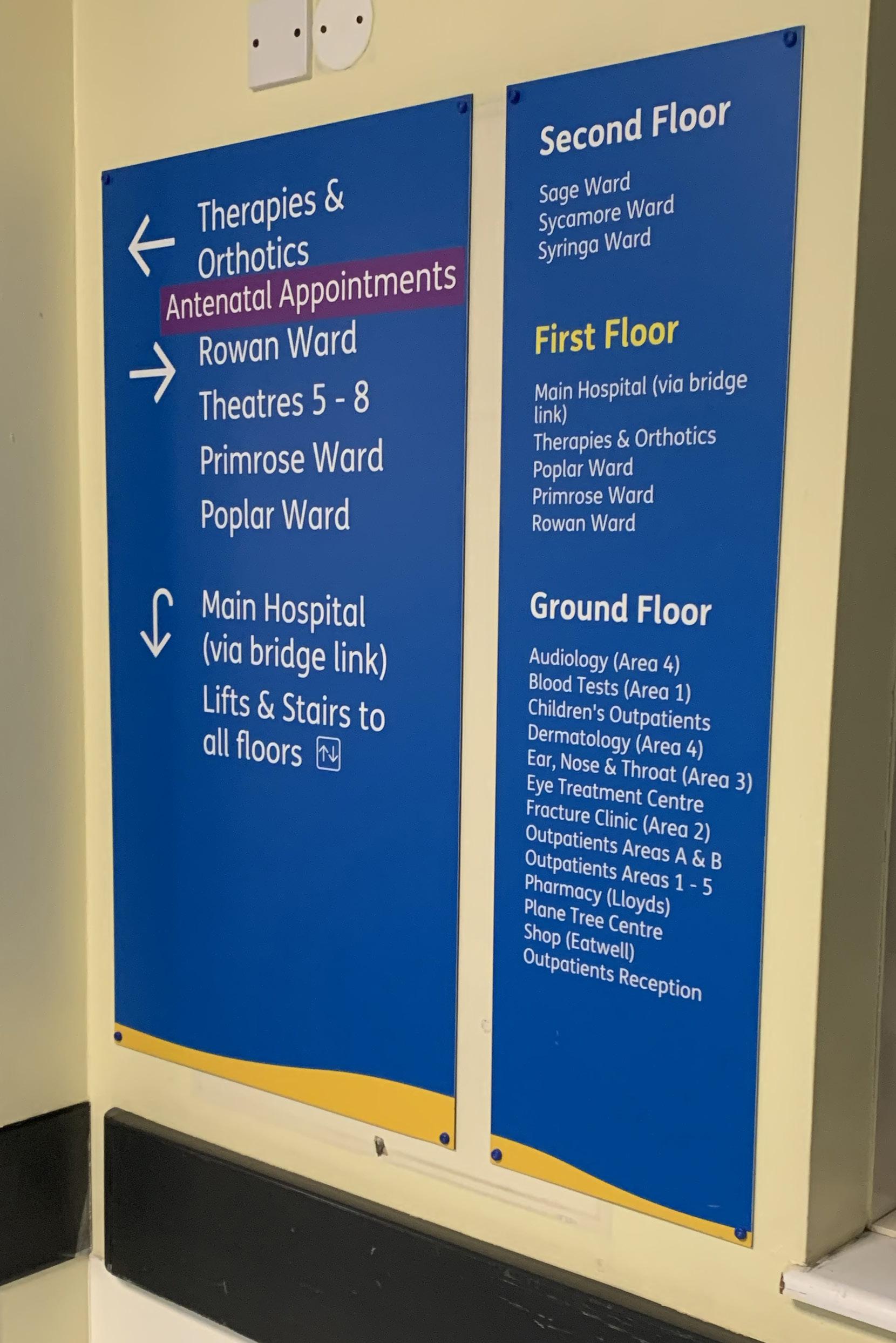

already uncomfortable visiting your office or location and a good sign can help reduce some of this stress. If the signs are easy to follow, visitors will feel more relaxed. If you are already stressed, difficulty navigating an unfamiliar building is not helpful.

Signs are important for the smooth running of an organisation – if people know where to go, they are unlikely to go the wrong way, stand in the wrong queue, cause crowding in a lobby or need to ask for help. Signs can also help people get the help they need more quickly, once they are where they need to be – signs near a queue or in a waiting room can provide people with the information of what they need when it is their turn to be seen – for example if they need photo ID or an appointment letter.
Of course, signs are designed to be helpful, so don’t provide too many. Think about what information a visitor would need and where the best place to display it would be. It is important not to overload your visitors. E
As the saying goes, you never get a second chance to make a first impression and good signage shows you care about your staff and visitors
Every hospital doctor’s fingers touch 33,000 things a week. Every touch transfers bacteria and risks an HCAI outbreak and possible hospital closure. Hygenius furniture helps you cut this risk.
Thoughtful design eliminates dirt traps that harbour infection. Smooth, seamless surfaces are easier to clean and better withstand the knocks of hard-working healthcare environments. Robust construction keeps wards safer for years.
Find out more about fighting infection at hygenius.healthcare or call us on 01738 633184.
The furniture that helps you fight infection
It is important not to provide too many signs, but it is also important not to provide too much information on your signs, as visitors need to be able to pick out what they need to know quickly. Don’t put any information that isn’t necessary on your signs.
Signage helps in advertising, if visitors and service users know where you are located ahead of their needs, this can help them should they ever need to visit. Depending on the nature of your organisation, signs that display your services can bring potential users towards you ahead of a competitor.
Good signage with a recognisable brand can differentiate you from the competition. Branding is important as it shows what you are about. Pay attention to your branding including logo, font size and style and colour. To provide information, generally, the simpler the better. There’s no point using a fancy font you think looks good, if it is not easy to read.
The signs you use must be appropriate for your audience as well, don’t use small fonts in areas frequented by elderly visitors and don’t use complicated language where children are. Be alert to the colours you are using – for example, we know that
a yellow sign is warning us to be careful or watch out for a hazard.
Consistency is also important, to provide a seamless experience to your visitors and avoid confusion. It also creates a uniform idea, that visitors will come to recognise.
Signage isn’t just about advertising, it is also important to keep people safe. It is crucial to indicate fire exits and safety equipment to keep staff and visitors safe and provide assistance in an emergency.

Signage should always be part of health and safety strategies, and can protect against accidents like trips or falls. As well as keeping people safe, it can protect against lawsuits in the event an accident should happen.
Signage relating to health and safety should be more prominent and clear than any other signage you have on display.
Health and safety signage for example on fire escapes or Covid can reassure staff and visitors that their safety is taken seriously.
A safety sign should be up-to-date and compliant with regulations (for example fire exits signs should be green with white text). As with any signs, they should be clear and readable and in a good state of repair.
One of the major benefits of signage is that it is a cost-effective and long-term way to achieve all of the above. Once a sign is installed, it is yours to keep, requires no maintenance and lasts a long time.
Particularly from an advertising and health and safety perspective, signage is one of the most cost-effective things you can do.
Overall, good signage provides a better experience for staff and visitors and is a very simple and cost-efficient way to do this. L
Signage should always be part of health and safety strategies, and can protect against accidents like trips or falls
By continuously improving solutions for ecological transformation, additional resources can be identified and recovered for hospitals across the UK.

This is where Veolia comes in. We specialise in helping hospitals run big, complex, and energy-hungry facilities and can help meet the NHS Net Zero targets. We have increased the sustainability of the healthcare sector by saving over 120,000 tonnes of CO₂ emissions annually.
To discuss our extensive range of decarbonisation and FM services visit: www.veolia.co.uk
Follow us on LinkedIn: VeoliaUK

With deficit levels at their highest in NHS history, now more than ever, hospitals must strike the right balance between managing costs and efficiencies while providing a high level of patient care. Healthcare authorities are under a lot of pressure to achieve cost savings and recognise their responsibility in delivering excellent patient care and the impact of its activities on the social, economic and environmental well-being of the local communities
This is where Veolia comes in. Unlike any other sector such as manufacturing, healthcare is unique as its focus and purpose is based on people, not products. It is the backbone of our country. As the population is ageing and the demands of NHS trusts are changing, ensuring patients get the services they need from hospitals is more crucial than ever. We specialise in helping hospitals run big, complex, and energy-hungry facilities enabling the NHS to become more sustainable, helping to focus budgets on patient care-enhancing facilities and directly improving healthcare.
How could a partnership with Veolia benefit your trust?
A partnership that prioritises patient care. Veolia provides secure on-site energy, Facilities Management (FM) and waste services to over 230 UK hospitals. By implementing site-wide decarbonisation strategies, we are at the forefront of delivering significant cost and carbon reductions using proven energy-efficient technology, and best practice optimisation, supported by a whole building approach. We currently provide energy services for over 100 hospitals that support the care of patients across 43,000 UK hospital beds. These supply the energy requirements for around 8.1 million inpatients each year and increase the sustainability of the healthcare sector by saving over 120,000 tonnes of CO₂ emissions annually.
Unlock your potential - What solutions can Veolia offer?
For hospitals, ensuring that services are running efficiently and that equipment is well-maintained are key priorities. When patients’ lives and well-being are at stake, the security and stability of their surroundings are crucial. With tight budgets to adhere to, and other pressures in the form of an ageing population and workforce. Veolia’s FM team offers a full range of core services such as; cleaning, fabric maintenance, and electrical engineering. However, we know that hospital requirements often go beyond the typical boundaries of what many would consider FM. Managing supplies of medical gas, installing ramps or fire doors, and even installing hand sanitiser stations. These are all examples of the type of extra work our FM team undertakes. This agile approach ensures that hospitals can keep functioning efficiently, even in the face of unexpected circumstances - for example, during the pandemic we responded quickly to a hospital’s urgent requirement for more oxygen. With engineering support from Veolia’s IFM team, we ensured a reliable oxygen supply at bedsides and there were no disruptions to the vital services the hospital provides. For hospitals under pressure to continuously provide high standards of customer care, knowing that equipment and critical assets are being maintained to the
same high level of compliance delivers much-needed peace of mind. With around £5 billion of backlog maintenance in the NHS currently, we can help sites carry out necessary improvements, and support them to be more sustainable. With hospitals gradually moving towards a ‘smart hospital’ model, we can help you give patients a better experience by creating more modern, user-friendly facilities.
By inspiring partnerships across the UK, Veolia is now at the forefront of innovation and delivering the circular economy. The real demonstration of what we can achieve lies in the results we deliver to our customers, and how we can help them to become more resource-efficient, more sustainable, and save money. From helping Rotherham NHS Foundation Trust save money and cut carbon emissions, to enhancing biodiversity at the Broadgreen Hospital Community Garden in Liverpool providing a space for hospital staff, patients, along with members of the local community, to find a moment of peace and enjoy the outdoors. These are just a few great examples of how we can help our customers take the lead and show how we can cut emissions to help mitigate climate change and preserve precious resources for future generations. Explore our bespoke, immersive and interactive VR experienceashowcasing the impactful work we do at Veolia: http://app.1stepnorth.com/iheem/
With the NHS responsible for 25 per cent of public sector emissions in England, the healthcare sector needs to act now to meet net zero targets. We can work with trusts to assess the existing infrastructure of hospitals, and can then make suggestions for optimising equipment. We can identify the projects that will work with your hospital, and design and build the right solutions that will help you meet your net zero goals. By continuously improving solutions for ecological transformation, additional resources can be identified and recovered for hospitals across the UK. L

Gain the knowledge you need to excel in our industry. Designed especially for you by our in-house expert team, we offer a wide range of industry focused CPDs hosted every fortnight. Scan to register online!


Effective fire safety in any environment depends on a combination of physical fire precautions and a robust system of effective management. Fire safety in the healthcare environment is particularly challenging, since many healthcare building occupants will require some degree of assistance from trained staff to ensure their safety in the event of a fire evacuation.
Even in primary care environments, the proportion of building occupants that may require some assistance to quickly escape the effects of a fire is likely to be greater than that which would be expected from a cross-section of the general population.
While physical fire precautions within a building are intended to provide protection to building occupants, effective fire safety management ensures that the incidence of fire is minimised, the physical fire precautions are maintained in an operational state, the organisation is able to respond effectively should a fire occur, and that the impact of a fire incident is minimised.

The current legislation in the form of the Regulatory Reform (Fire Safety) Order 2005 (equivalent legislation applies in Scotland and Northern Ireland) requires a managed risk

approach to fire safety. The process of fire risk assessment, mitigation and review requires a robust system of management capable of identifying hazards, qualifying their impact, devising appropriate mitigation, and continual monitoring.
The presence of a robust system of fire safety management is a key influence in fire risk assessment and in many healthcare environments it is the determining factor in evaluating the level of fire risk.

The increasing prevalence of building fire strategies for healthcare premises which contain fire-engineered design solutions, are likely to intensify the need for enhanced fire safety management.
These solutions may require enhanced fire safety management procedures to be applied holistically or simply as a specific component of a fireengineered solution.
Risk mitigation In a healthcare environment with very high dependency patients, it is unlikely that any amount of physical fire precautions on their own can reduce fire risks to an acceptable level. Adequate risk mitigation can only be achieved with the provision of a sufficient number of suitably trained staff, an environment in which the fire precautions are well maintained, and effective emergency action plans that have been sufficiently E
Even in primary proportionenvironments,carethe of building occupants that may require some assistance to quickly escape the effects of a fire is likely to be greater than that which would be expected from a cross- section of the populationgeneral











rehearsed. It is the non-physical elements of these fire precautions that are provided as a function of fire safety management.
Another way to significantly improve fire safety in hospitals and other healthcare facilities is to minimise the number of false alarms and unwanted fire alarm signals (UFAS). An UFAS is a false alarm from an automatic fire detection and fire alarm system that has been passed on to the fire and rescue service. For example, a typical cause of a false alarm in a hospital/care setting might be from the burning of toast (the NHS runs on toast). Instances of UFAS impact upon the treatment and care of patients and can result in the loss of appointments, disruption to care and treatment regimes, and can significantly affect staff morale. In addition to this, unwanted fire alarm signals have a serious impact on the fire and rescue service, diverting firefighters from other genuine emergencies and potentially life-saving activity.

In order to identify incidents of false alarms correctly, it is necessary to define the sources of fire detection and alarm system activations.
The causes of fire detection and alarm system activations can be broadly classed as one of two incident types: fire; or false alarm. These incidents can be defined as follows: Fire – a fire can be regarded as an incident resulting in the uncontrolled emission of heat and/or smoke or false alarm – activation of the fire detection and alarm system resulting from a cause other than fire.
In accordance with the National Fire Chiefs Council (NFCC) policy, a false alarm becomes an unwanted fire signal at the point the fireand-rescue service is requested to attend.
The false alarms may be subdivided into four categories as defined in BS 5839. Firstly, equipment false alarms, in which the false alarm has resulted from a fault in the system. The most serious of the categories as well as the one where fast action can bring significant
improvement to fire safety is an alarm caused by faulty equipment. Reducing false alarms begins when designing the equipment.

Article 18 of the Regulatory Reform (Fire Safety) Order 2005 (RRO) requires the Responsible Person to ‘appoint one or more competent persons to assist in undertaking the preventive and protective measures’. Where the protective measures include a fire alarm and fire detection system, a proper service and maintenance programme is essential to ensure the fire alarm and detection system works when it is needed most.
British Standards recommend that the number of service visits per annum should be a minimum of twice a year (with the actual number dictated by a suitable and sufficient risk assessment).
Secondly, unwanted alarms, in which a system has responded, either as designed or as the technology may reasonably be expected to respond, to any of the following: (i) a fire-like phenomenon or environmental influence (for example smoke from a nearby bonfire, dust or insects, processes that produce smoke or flame, or environmental effects that can render certain types of detector unstable, such as rapid airflow); (ii) accidental damage; (iii) inappropriate human action (for example operation of the system for test or maintenance purposes without prior warning to building occupants and/or an alarm receiving centre). This could also be malicious false alarms, in which a person operates a manual call point or causes a fire detector to initiate a fire signal, whilst knowing that there is no fire. There are also
false alarms with good intent, in which a person operates a manual call point or otherwise initiates a fire signal in the belief that there is a fire, when no fire actually exists. In order for an organisation to adequately address the issue, accurate records of all false alarms should be maintained. The healthcare organisation should set in place a mechanism to review the organisation’s false alarm performance, and arrangements to mitigate such incidents.
In tackling the issue of false alarms, it is important to involve the appropriate stakeholders. These may include fire safety manager fire safety advisor (where appointed), staff representative, fire detection and fire alarm system maintainer, fire detection and fire alarm system manufacturer; local fire service representative, estates manager, staff residences representative, planning department officer, and contractors (as appropriate). This list is not exhaustive; other stakeholders may be required depending on the nature of false alarms experienced and their causes. For example, it may be necessary to include the local authority pest control officer if a number of false alarms are attributable to insect infestations. It is not expected that all stakeholders will attend every meeting, as the attendance at each meeting should be tailored to the main reported causes of false alarms in the organisation. L
www.fia.uk.com
The healthcare organisation should set in place a mechanism to review the organisation’s false alarm performance, and arrangements to mitigate such incidents
It has been more than two years under the pandemic, and our lives have changed forever, especially in terms of how we work. Companies and institutions that recognised the benefits of flexible workplaces and WFH were quick to implement these new ways of working with great success in productivity and improved well-being for their workforce. Solutions such as video conferences rendered distances long or short irrelevant and removed communication barriers. The healthcare sector equally underwent those changes with, amongst others, the introduction of flexible workstations. Working on a laptop that hooks up to a monitor, keyboard, and mouse has increasingly become the new normal at doctor’s surgeries and hospitals.
This year, Philips monitors brought three new displays to market, which were conceptualised from the ground-up for flexible working. The new B1U models from the Philips monitors’ business portfolio combine high-resolution webcams, USB-C connectivity and a KVM switch to instantly create an individualised workspace by connecting a laptop with just a single cable.
In the extensive Philips monitors portfolio, the Philips 24B1U5301H, a 23.8” display with a colour-accurate IPS panel is the most compact variant of this new line-up. It features Full HD resolution and a 75 Hz refresh rate, with 105 per cent sRGB gamut coverage, making it proficient in displaying accurate colours and sharp text.

The 24B1U5301H comes with a noisecancelling microphone and a 5 MP webcam, which also supports Windows HelloTM. This enables medical staff to log in to a Windows PC by just looking at the camera, without entering a password, increasing security, and allowing the team to unlock their PC when their hands are full or contaminated. To ensure patients’ privacy,
the webcam also has a shutter to physically block the camera view. Thanks to the clear sound of the microphone and the high resolution of the webcam, a more natural conversation is ensured via video call.
Furthermore, this monitor offers an integrated USB-C docking station, complete with a KVM switch. This means that a laptop, which is connected to the monitor’s USB-C port, can access the ports on the monitor (4x USB 3.2 and RJ-45). Users can choose to extend or mirror their notebook’s display to the monitor via USB DP-Alt Mode, all the while the laptop is being charged or powered (up to 90 W). Thanks to the DisplayPort output, a second display can be easily connected alongside the 24B1U5301H - extending the screen real estate whilst keeping the workstation clutter-free. A separate desktop system can also be attached at the same time as a second input source. Switching between the two devices is a doddle with the KVM switch on the monitor and without the need to make any further adjustments to the monitor, keyboard, and mouse setup.
In a real-world scenario, a doctor can bring their work laptop to the flexible work desk at their office/hospital and simply connect it to the monitor via USB-C. It will have a fast and secure access to the local network (thanks to the monitor’s RJ-45 port), as well as to the keyboard and mouse or a printer (connected to the monitor’s USB hub), creating an ergonomic, clean working desk in an instant.
For a sharper display and larger screen area, the Philips 27B1U5601H offers a step-up with the same webcam, but with a 27” display and QHD resolution (2560x1440).
Fit for administration purposes, the Philips 34B1U5600CH features a curved 34” display with 3440x1440 pixels, including the same full docking station
as its smaller siblings: a USB-C docking station with 100W power delivery, 5 MP Windows Hello webcam with a noisecancelling microphone, and an RJ-45 input with Gigabit Ethernet support. Thanks to its 21:9 aspect ratio, it can easily replace dual-monitor setups. With a sleek, futuristic design, it perfectly matches the interior design of the reception area at doctors’ offices and hospitals.
Both the 27B1U5601H and 34B1U5600CH also support up to 100W power delivery via USB-C so they can operate and charge laptops and similar devices with higher electricity consumption. The large display makes working with long texts, wide spreadsheets and detailed images so much easier.
Sustainable working with sustainable products
Finally, the three B1U models are shipped in 100 per cent recyclable packaging material and are certified with EnergyStar 8.0 and EPEAT. All models also meet the TÜV Rheinland Eye Comfort standard, as they offer an ideal viewing experience even when used for long hours thanks to FlickerFree and LowBlue light technologies. Due to the PowerSensor with infrared detection, the display can reduce brightness when the user is away, saving energy costs of up to 70 per cent.
For health institutions that need to take the next step in their IT infrastructure, Philips monitors offer the ideal technology for productivity. L
Philips monitors’ portfolio offers a wide range of features to help healthcare workers whilst also providing security
Recognising and finding ways to meet the requirements of changing regulations and policy demands is crucial in reshaping our approach to sustainability. The ecological clock is ticking, and we must take urgent action to mitigate the impact of global warming. Here Richard Hipkiss, development director of the Modular and Portable Building Association (MPBA) makes a case for volumetric manufactured buildings in shaping a net zero future
Identifying a route to net zero emissions for a complex system as large as the NHS is particularly challenging. On 1 July 2022, the NHS became the first health system to embed net zero into legislation, through the Health and Care Act 2022. The Delivering a Net Zero National Health Service report is now issued as statutory guidance.
So, what is net zero? Put simply net zero is a target of negating the amount of greenhouse gases we produce by reducing emissions and implementing methods of absorbing carbon dioxide from the atmosphere.
The emphasis with net zero construction is quite rightly focused on the environment but through a more sustainable approach to designing and developing buildings, those
operating in the healthcare sector will reap the benefits for many generations to come.
Energy costs are now not only having a major impact on household budgets but also NHS Estate resources. There is significant evidence that traditionally constructed buildings do not produce structures that perform as well as design expectations and there is a great void between anticipated and actual in-use performance. Findings from studies such as PROBE (Post Occupancy Review of Buildings and their Engineering) reveal that actual energy consumption in buildings is often as much as twice of that predicted at the design stage. With great challenges come opportunities.
We have a proud legacy of innovation and many of our members in the volumetric modular and portable building sectors are setting out road maps to deliver structures that will be net zero in operation and highly energy efficient.
At the forefront of offsite approaches, it is now established that volumetric modular technology is a game changer for the construction industry – reducing build times by an impressive 50-60 per cent whilst increasing quality, productivity and safety. Volumetric modular buildings however are less susceptible to poorly specified products as time can be taken upfront to validate the correct specification of materials.
At the core of module manufacture, Design for Manufacture and Assembly (DfMA) protocols and Building Information Modelling (BIM) technology empower optimal configuration of the offsite solution by digitally connecting multi-discipline teams from the beginning of the concept design right through to the development process and beyond. E

nowcostsEnergyare not only having a major impact on household budgets but also NHS resourcesEstate
financial windfalls 25 2090

alysis
is Contact us on 0344 225 2090

iew of ver ising ted Our Health Checks are carried out on a NO RECOVERY – NO FEE basis.







s

ing the review of t also recover Teams, utilising d unbudgeted
the review of so recover ms, utilising nbudgeted
nalysis
covery Auditing, involving t o identify anomalies but als ers on behalf of Clients s’ Finance and/or Audit Team rate often unknown and un al windfalls

Analy C t us on 0344 225 2090

DfMA means buildings are conceived for offsite manufacture and assembly onsite. BIM facilitates early design detail and three-dimensional design information, minimising the risk of errors by eliminating the time-consuming process of translating engineers’ information into cutting lists and assembly drawings. BIM also facilitates the optimising and testing of designs in virtual and pre-production environments which means modules are digitally constructed and virtually tested before they move onto the manufacturing phase.
Factory manufactured modular buildings are highly accurate, well insulated and airtight, with air permeability with 1.5-3 m3 @50PA being the norm. A key advantage of modular construction is the quality benefits which come from working in a controlled environment. By producing buildings in a factory setting, the quality of elements such as insulation can be better assured. Predictability of in-use performance is a substantial benefit in not only achieving net zero goals but reducing primary energy requirements and in-use operational emissions during the lifetime of the building. This manufacturing method also allows better control over optimising material use. The surplus materials are recycled or reused for future projects, reducing construction waste that ends up in landfill. Materials are protected from moisture and extreme weather conditions, reducing the risk of disposal through water ingress and damage. It is widely recognised that modular has the potential to reduce overall construction programmes, but it is not often acknowledged this approach can reduce up to 90 per cent
of the waste generated when compared with traditional construction methods.
The volumetric modular way limits the amount of concrete in the ground and eco-friendly materials are often specified and each individual component can be selected specifically for its performance characteristics, tailoring every inch of a volumetric modular build.
With volumetric manufactured buildings, all construction data can be validated and coordinated as part of a structured process, which helps provide accurate and reliable information for clients at the point of handover. Volumetric construction helps ensure client satisfaction and product assurances through the certainty and quality embedded into the manufacturing process.
Many MPBA members are accredited under a number of modular building frameworks, including NHS Shared Business Services Framework, LHC, Crown Commercial Service and NHS Commercial Solutions. These frameworks help NHS trusts and other public sector clients improve the speed and cost-efficiency of procurement to support world-class patient care.

The benefits of volumetric manufactured buildings begin in the factory, continue on to the construction site and last through the lifetime of the building. We understand the challenges facing healthcare providers – from changing patient demographics, new medical technologies and treatment strategies, the Covid-19 pandemic and highly constrained budgets, to increasing demands for carbon and waste reductions. L
The MPBA plays a key role in the connecting of sectors in the modular and portable building industry. The association collaborates with specialist technical advisors to enhance innovation in the design and manufacture of volumetric modular buildings. These can be designed and manufactured from timber or steel in any size and shape to meet individual client needs while ensuring full compliance with Building Regulations. To discover how volumetric modular technology can benefit healthcare construction projects go to: www.mpba.biz
FURTHER INFORMATION www.mpba.biz
With volumetric manufactured buildings, all construction data can be validated and coordinated as part of a structured process, which helps provide accurate and reliable information for clients at the point of handover
Anderson Quigley (AQ) are a specialist executive search, interim management and advisory consultancy, supporting organisations that focus on society and social development. We are driven by our core values - integrity, diversity and hands-on project ownership, using our decades of knowledge and expertise to deliver leadership recruitment in health and social care, education, charities, cultural organisations, the arts and government
Consulting on highly complex public and third sector leadership assignments, we continually present gender-balanced, diverse, high-quality shortlists in both executive and non-executive recruitment. We challenge our clients to take positive action to promote diverse appointments and to think more creatively on cross sector hires - ensuring candidates are seen for more than just their skillset.
Our highly experienced team are dedicated to the advancement of social development with a real enthusiasm for their respective sectors. Above all, we are a responsible business, focused on individual and collective development. We ensure our people work in a respectful, diverse environment, where every effort is made to support continual learning. We always act responsibly towards our clients and candidates, guaranteeing them fair, honest, and objective advice. These are the fundamentals of our culture. They are the foundation upon which our business continues to grow and thrive.
Sector Insight – having worked with many NHS Trusts, professional regulators, and National Health organisations, we have a strong understanding and perspective on the market. We are also able to work closely with clients to identify the key challenges and opportunities and hone those to establish a clear candidate proposition.
Candidate Engagement – when managing senior level appointments, most candidates will have at least two to three conversations with a head-hunter. We understand the importance of this relationship and that we are acting as your ambassadors. Candidates look to us for an honest appraisal of their skills and experience. We want to present to you a strong list of candidates that absolutely have the credentials, experience, and values to make a lasting contribution to the role.
Partner-Led Model – established in 2017, Anderson Quigley is a purpose-led

organisation founded and driven by a core values set of diversity, integrity and hands-on project ownership. As such, each assignment will be partner-led, with a senior member of our team taking personal responsibility for the delivery of your campaign.
Diversity – AQ is committed to diversity and was created to support clients and candidates in the public services. With a deep belief in equality, diversity and fairness, these values are at the heart of our business. Our role is to seek out talent in all its forms, identify future talent and challenge assumptions –we do this by having an open mind about sources of talent and we see it as our duty to actively challenge assumptions about what outstanding talent looks like.
Small is Beautiful – agile, fleet of foot, AQ’s size is our strength. We have your best interests at heart and can freely and independently search for the right candidates and work in the best interests of your organisation to produce a quality, results-led process that will result in the presentation of an outstanding shortlist.
Track Record – since our inception, AQ have worked with a variety of different organisations on executive and nonexecutive appointments. These have included in the past twelve months alone: Northern Care Alliance NHS Foundation Trust, South Western Ambulance Service NHS Foundation Trust, Herefordshire & Worcestershire Integrated Care System, Queen Victoria Hospital NHS Foundation Trust, Birmingham Women’s & Children’s Hospital NHS Foundation Trust, Northamptonshire Healthcare NHS Foundation Trust, Care Dorset, Camphill
Village Trust, General Dental Council, Innovate HealthCare Services, and Coventry & Warwickshire Integrated Care Board.
Helene Usherwood, AQ
Partner, Health & Social Care
With over 20 years’ headhunting experience, Helene has appointed to senior roles within the arts, health and education fields as well as central and local government.
Joining Anderson Quigley in 2018, Helene has established and continues her work specialising in the appointment of executive and non-executive directors in the NHS covering acute, ambulance service, primary care, mental health and regulatory bodies as well as national organisations and Royal Colleges.
In addition to her work with NHS Trusts, Helene has developed Anderson Quigley’s Board Practice, working across all sectors to appoint chairs and non-executive directors. She has developed excellent networks across the public and private sectors to encourage greater levels of diversity around the boardroom table. As well as providing bespoke services, advice and guidance to her clients and candidates, Helene is highly motivated to provide careers advice and guidance to individuals, especially to those who have not previously considered a non-executive opportunity before but whom have unique insights and skills to offer the role. L
www.andersonquigley.com helene@andersonquigley.com
Recruiting talent to the public sector is not easy, but here are some tips to help

Public sector recruitment is hard at the moment, with funding cuts and budget squeezes meaning there are likely fewer positions available and fewer resources available to fill vacant positions.
The pandemic has led to people retiring earlier than expected and Brexit has caused a shortage of employees. Coupled with the pressures of working in the health service, the NHS has been hit particularly hard hit. These problems are universal across the job market so there is also competition for the top talent, with the private sector often able to provide higher salaries and better benefits.
Before you start your candidate search, think about what you want to achieve. Do you want to hire someone for a vacant position on the same job description as the person who left or could you shuffle some responsibilities? Would it be better to hire two people to share a role or to fill a vacant position internally? Look at how your organisation works and see if you could benefit from redefining some job descriptions or reallocating some roles or responsibilities to make your organisation run more smoothly.
Identifying and attracting potential applicants
Firstly, write attractive adverts and job descriptions. Public sector positions can sometimes be uninviting for those looking for a new job or a career move. Make sure your job ads are personable and enthusiastic and make the job look enjoyable. Try not to use overly formal language that could put people off.
Highlight what is good about working in the public sector, that may be different from the private sector, for example job security and having a positive impact on society. Emphasise the importance of the public sector and the essential services you provide. Think about the benefits you can offer that won’t cost any money, such as working from home and flexible hours. Despite the pandemic, a lot of private sector organisations still don’t offer these benefits, even though a lot of workers want them, it doesn’t cost a penny and can in fact improve employee satisfaction and therefore productivity
as well. It can also widen your candidate pool, for example to parents with schoolage or younger children, who may not have been able to take a full-time job before.
You can also provide benefits such as training and mentorship which are littleto-no cost and will actually benefit your organisation in the long run, by improving the skills and confidence of your new hire.
Young hires can also reverse mentor their senior colleagues by providing guidance on things like social media, cybersecurity and software implementation.
Don’t be afraid to advertise your open positions outside of traditional NHS job boards, for example if you are hiring for an admin role, post your job ad on an admin job website.
It does not hurt to invest in technology – an efficient, easy-to-use and well-run application platform can make you more inviting to potential applicants and increase the number of applications. Good technology can reduce your costs elsewhere in the long run. Also updating the technology you use for day-to-day operations can make you more attractive to applicants.
Social media is a great place to advertise for local positions and can help you attract young people who may not have considered a career in the public sector or others who are looking for a career change.
Think about your brand. If you are a local hospital for example, make sure the local residents know what you do. If local residents have a good perception and awareness of what the hospital does and a positive attitude towards it, then they are more likely to want to work there. E search,youryouBeforestartcandidate
think about what you want to achieve

Make sure you have policies and strategies in place to help you evaluate the best candidates. Consider assessment tools such as AI, which can save the hiring team money as well as help you find the most qualified candidate. Draft appropriate and informative interview questions and avoid the old classics like “Where do you see yourself in five years’ time?” and “What is your biggest weakness?” Assess the interest of the applicant in the vacant position, those who are genuinely interested in the role are more likely to be successful and stick around for longer. When interviewing a candidate, create a positive and welcoming environment. Be friendly and approachable and start with some small talk and general chit-chat before launching into the interview. Acknowledge and respond to their answers and don’t just move from one question to another. If someone is coming into the office for an interview, make sure you are prepared, you have a room set up and the place looks friendly and welcoming, as well as clean and in good repair. This can be the difference between a candidate accepting a position or deciding to go somewhere else.
Be prepared for the questions a candidate might ask, and have an answer ready. You can also use this opportunity to share the pros of working for your organisation. For example, they may ask about benefits or career advancement. Public sector organisations tend to have well defined and clear career progression opportunities that may not be available in the private sector.
You should always keep an open mind, if your admin assistant has retired after 30 years in the same role, don’t assume that the perfect candidate is a similar person. It might be the perfect position
for a recent school-leaver rather than someone with years of experience.
Make sure you follow all guidelines and regulations, whether these be legally enforceable or at your organisation level. Note that some NHS organisations have very strict regulations and you need to make sure you follow these.
Think about the criteria that are necessary for the role. Does someone need experience or could you hire someone inexperienced and train them up? Is a degree really necessary? This can be a barrier for applicants from lowersocioeconomic backgrounds, who could do the job just as well as someone with a degree.
Make sure you have a flexible recruitment process and get back to candidates quickly, acknowledge receipt of their application, thank them for coming in for an interview etc.
If a candidate doesn’t make the shortlist, or doesn’t make it past the interview, let them know. This creates a good impression in their mind and they are more likely to remember you as an employer. If they have to wait a long time to hear back from an interview, they may already have taken another job. If they never hear back from you, they are unlikely to want to apply for another job
in your organisation, even if they may be a good candidate. Remember word-ofmouth is important, particularly if you are a large local employer such as a hospital.

Make sure to check references before offering your candidate the job.
Remember, there is no guarantee your chosen candidate will say yes.
When making a job offer, your chosen candidate should receive all the information they need to make an informed decision. If there is information missing, this may lead to them leaving the role prematurely if something unexpected happens once they start the job. A job offer should include the candidate’s name, the job title, the salary and start date. It should also include terms and conditions, benefits and requests for any required legal documents, such as proof of right to work in the UK.
Once a candidate has accepted a job offer, make sure a contract is sent promptly. This should already be prepared.
Your organisation should already have templated offer letters and contracts, but make sure everything is approved by the relevant team or manager and the legal department or representative.
The chosen candidate may have questions, make sure these are answered promptly. L
If someone is coming into the office for an interview, make sure you are prepared, you have a room set up and the place looks friendly and welcoming, as well as clean and in good repair
















Keeping in touch Your support makes a life-changing difference to people in crisis. We write to our supporters to update you about the work of the British Red Cross, and how you can help and donate in other ways. You can change the way we contact you at any time by visiting redcross.org.uk/keepingintouch or calling Freephone 0800 2800 491.
Privacy statement The British Red Cross is committed to privacy and will use personal data for the purpose it was collected or other legitimate purposes we tell you about: for example, to provide goods, services or information you have requested or to administer donations or services we provide. We may also analyse data we collect to better understand the people who support us or those who use or deliver our services. Sometimes this means us combining that data with information from reliable public sources. Our research allows us to tailor communications and services in a more focused and cost-effective way, as well as better meeting your needs and the needs of others like you. However, we will never do this in a way that intrudes on personal privacy and will not use your data for a purpose that conflicts with previously expressed privacy preferences. For full details about how we use personal data, our legal basis for doing so and your privacy rights, please see our privacy notice online at redcross.org.uk/privacy.
The DEC Ukraine Humanitarian Appeal will support people in areas currently affected and those potentially affected in the future by the crisis. In the unlikely event that we raise more money than can be reasonably and efficiently spent, any surplus funds will be used to help us prepare for and respond to other humanitarian disasters anywhere in the world. For more information visit https://donate. redcross.org.uk/appeal/disaster-fund



*Texts cost £10 +1 standard message (we receive 100%). For full T&Cs visit redcross.org.uk/mobile, must be 16+.











The British Red Cross Society, incorporated by Royal Charter 1908, is a charity registered in England and Wales (220949), Scotland (SC037738), Isle of Man (0752) and Jersey (430).





Nobody can be under any illusion about the scale of the challenges that face the NHS and social care. Millions of people are waiting for treatment they desperately need, and A&E and ambulances services are overwhelmed. Meanwhile, millions of vacancies remain unfilled, impeding the treatment and support available to some of society’s most vulnerable people. In a recent survey for NHS Confederation, 99 per cent of healthcare leaders agreed there is a social care workforce crisis in their area and almost all said it is worse now than it was 12 months ago.
Thérèse Coffey, the previous health and social care secretary, set out a new plan for patients. This included a call for a ‘national endeavour’ to support the health and social care system, encouraging the one million volunteers who stepped up during the pandemic to support the NHS to come forward again.
The power of volunteering
We have already seen the huge power of volunteering throughout the pandemic, when local residents organised to support elderly or vulnerable neighbours. We also saw thousands of volunteers support the vaccination programme. Now we must unlock that power to combat exceptional challenges ahead and build the resilience and connectivity of our communities. However, there is no point in calling people to volunteer without effective roles ready for them. These challenges are complex and require multiple solutions, but harnessing the power of volunteering is an essential part of the answer. To maximise volunteering, we need government, local
authorities, health and care leaders and community organisations to unite to put in place well-designed and properly managed volunteer initiatives.
Helpforce, which exists to maximise volunteering to its full potential, has been working with health and care leaders to harness the power of volunteering for the benefit of patients for many years. We are seeing first-hand the measurable improvements in the delivery of care that volunteers bring for staff and patients.
It is a little-known fact that volunteers are already playing a vital role in supporting people at home as they wait for NHS care at a time of record waiting lists. For example, E
We thealreadyhaveseen huge power of volunteering throughout the pandemic, when local residents organised to support elderly or vulnerable neighbours




we are supporting five Waiting Well pilots across England, helping to connect volunteers with patients to provide a range of services to make their wait more comfortable – from therapeutic wellbeing and health coaching to nutrition support and falls prevention.
Currently, four out of every five patients do not receive any support while they wait for treatment – which can mean the need for more complicated surgery, worse outcomes, increased used of medication and increased anxiety. Waiting Well volunteers are vital in reducing pressures on GPs and social care.
Volunteers can provide practical and emotional support to people on waiting lists, minimising anxiety and providing companionship to people who are concerned about their treatment. With more than six million people currently on waiting lists, and delays causing heightened patient worry and the need for more complex surgery, there is a huge potential for volunteers to help.
Volunteering can assist pressures at every stage of the patient journey. In hospitals too, volunteers working alongside
medical staff, can provide additional support to make treatment more effective, efficient and personalised, and can even reduce the need for treatment. There are a wide range of volunteer roles already available to tackle urgent concerns.

Helpforce’s research shows that volunteers can free up almost 30 minutes per nurse per day and can speed up patient discharge. One of the most developed parts of our volunteering support are those response volunteers within hospital. Examples of their work include pharmacy runs for clinicians or nurses and admin activity which can be a huge time saver.
NHS staff consistently tell us that they value the contribution of volunteers. 79 per cent of staff strongly agree that volunteers support them in their work. The vast majority of patients who receive volunteer support say they are shown excellent care and compassion.
An emerging growth area is the work to support patients after they are discharged to reduce the risk of readmission. Helpforce is working to roll out a discharge call service, where volunteers call patients within 72 hours of being discharged to check they are OK and provide signposting to community services where needed. This has increased understanding about what might be behind readmissions with issues identified such as gaps in appropriate aftercare, missed discharged medical advice leaflets or wellbeing checks to advise on recovery needs. Once the volunteers find out what is needed, they can pass on requests/ next steps to the community so that the care for patients is fully integrated. But while there are some great examples of volunteers being used to improve outcomes for patients and staff, volunteering still isn’t being prioritised or properly integrated anywhere near enough in NHS trusts or community settings. This is a major missed opportunity.
Volunteering must become a priority in every health and care organisation. It should be seen as an essential component of health and care, not a ‘nice to have’. We need to ensure that there are highimpact roles for volunteers across the UK. There should be a more joined-up approach which integrates volunteers across trusts and community services, to ensure that volunteers can support people before they come to hospital and after they leave.
The volunteer response to the pandemic and the vaccination programme demonstrated that there is an extensive resource of skills in our communities. Helpforce’s hope is that the success of these projects will help to demonstrate the power of volunteering and that they can be scaled up across the UK. We cannot afford to squander that potential. We must unlock the huge power of volunteering to combat exceptional challenges ahead. L
Helpforce is a national charity which partners with health and care organisations to transform how they deliver volunteer services. Find out more at: https://helpforce.community/

But while there are some great examples of volunteers being used to improve outcomes for patients and staff, volunteering still isn’t being prioritised or properly integrated anywhere near enough in NHS trusts or community settings.
Fast and accurate measurement of C-reactive protein (CRP) supports treatment decision making in the management of respiratory infections in different healthcare settings. CRP point of care (POC) testing increases diagnostic certainty and optimizes antibiotic prescribing. Accurate and rapid diagnostics play an important role in decreasing antibiotic overuse – a key factor in fighting against antimicrobial resistance (AMR).
QuikRead go® test system includes a selection of different accurate, precise, and ready-to-use CRP POC

Etests for healthcare professionals. Just a small sample is enough to get laboratory quality results at the point of care site. Results are available within 2 minutes already during the patient’s visit and instrument read results ensure objective result interpretation. Traceability of test results ensures high quality and reliability.

Fast CRP POC testing before antibiotic prescribing is one effective way to guide prudent and sustainable use of antibiotics and prevent the development of AMR.


CRP point of care testing aids in the prevention of Antimicrobial Resistance
At a time of crisis for the health service, the MTG’s flagship event Medical Technology Awareness Week may have been our most important yet. This year’s theme ‘Futureproofing the NHS’ brought together MPs, NHS leaders, industry groups and patients to showcase the best of NHS innovation in tackling the backlog, improving the quality of care and relieving pressure on the workforce. It was a milestone in our ongoing campaign to make the case for medical technology as the solution to many of the NHS’s future challenges.

We have long believed that uptake of medical technology must be a priority if the health service is to face these challenges. In recent years, there has been some improvement with

the MedTech Funding Mandate and a greater drive by the NHS Innovation Accelerator to adopt the right technology. But as our series of reports on regional inequality in the NHS show, there is still a long way to go in ensuring timely and equitable access to the best medical technology and innovation on the NHS for every patient.
For Government, NHS leaders and even local NHS bodies, the need to embrace medical technology as the solution is becoming more urgent by the day. There are challenges that sit clearly on the horizon: an ageing population, a backlog that predates the pandemic, as well as the need to upgrade our diagnostic and surgical capacity. There is also a transition to a ‘population health’ model of care under the Integrated Care Systems, much of which rests upon the use of medical and data technology E
uptakebelievedhaveWelongthat of medical technology must be a priority if the health service is to face these challenges

to assist prevention and management of chronic illness long term in the community. Despite the challenges of the pandemic, many regions of the NHS have relied on innovation and medical technology to cope with the unprecedented pressure on health services. The sorts of same day surgery techniques we highlighted in our manifesto can now be widely found in surgical hubs across the country. In our latest report, we showcased those regions that had used examples of innovation and technology to recover from the pandemic. The variety of our case studies reflect both innovation in leadership and management structures, but also the effective use of data and medical technology. Broadly, their positive impact can be broken down into three key areas: managing longterm conditions; improving surgery times and patient experience; and supporting the NHS in its workforce challenges.
In NHS Wakefield, now part of the West Yorkshire ICS, using SystmOne software the hospital set up a ‘Shared Referral Pathway’,


allowing clinicians to communicate with each other between primary and secondary care as the patients moved through the pathway. As the chief executive of the Hospital Trust, Len Hutton, said, this was not an overnight transition but ‘two years of trial and tribulation’. In fact, the theme of longer-term transition emerged from other case studies, and highlights the important role hospital executives have in facilitating the effective uptake of innovation. When we talk of ‘futureproofing’, the NHS, there is no magic wand to wave with regards to a piece
of technology that will. Rather it’s dependent on how the leadership teams deploy such technology, one which requires them to occasionally make bold, often brave decisions. One significant example of this was the work done in NHS Northumbria under the stewardship of Sir James Mackay. The utilisation of data, particularly the effective development of live dashboards and information on the changing needs of the patient was crucial to the effective allocation of resources as the trust looked to recover from the pandemic. This use of E
In NHS Wakefield, now part of the West Yorkshire ICS, using SystmOne software, the hospital set up a ‘Shared Referral Pathway’, allowing clinicians to communicate with each other between primary and secondary care as the patients moved through the pathway
The modular QualityMix-system provides a continuous and precise mixture of medical Air and Oxygen for infants, children and adults. High-Flow/Low-Flow variants are available configured according to your requirements. Expandable with monitor and various flowmeters.



And we don’t stop at mixing Oxygen and Air! Nitrous Oxide and Carbon Dioxide blender are also available. For these gases too, we offer a large number of variants.


At least we don’t stop at mechanical devices! Blending gases goes electronic with the QualityMix PRO gas mixer - an O2/Air gas mixer of the latest generation. Integrated flow control, Oxygen monitoring and SpO2-measuring! Operated by the touchscreen, with network capabilities and much more. Not enough? As a specialist for medical gas and mechanics, we offer more! For example our Demand Valve for emergency ventilation.

data can also be seen in Maidstone and Tunbridge Wells NHS Trust, where a ‘mission control’ style room, used to allocate beds and staff, has seen them slash waiting times.


Though the pandemic has been devastating for our health service, these examples of innovation forged through crisis now need to be the bedrock for the future vision of the NHS. There is also work for NICE, and other centralised NHS bodies to do in this respect. During our Medical Technology Awareness Week, we showcased a number of technologies that have contributed to clearing the backlog, particularly a variety of minimally invasive surgery techniques which have had successful records in reducing surgical times and patient stays in hospital. Continuing to invest in these minimally invasive procedures will allow the government to extend the use of surgical hubs and intensive surgery clinics. The use of this technology should therefore
become not just a means to clear the backlog, but also increase the NHS’s surgical capacity, reduce hospital stays and prevent readmission.
The last point we made to NHS leaders and politicians gathered at our reception was one around health spending. To fully harness the benefits of medical technology and futureproof not just our NHS, but also our economy, we must increasingly see each pound spent on the health service as an investment in our economy. There are plenty of examples where long-term investment in medical technology assisted surgery sees improvements to our economy. Total Hip Replacement is a way of tackling the cost of osteoarthritis - which amounts to roughly one percent of Gross National Product (GNP) per year with 40 per cent of people with musculoskeletal disease of working age unable to work. The procedure sees 97 per cent of patients report improvements in their condition. With up to
2.5 million people economically inactive due to long-term sickness, futureproofing our health service also means investing in the NHS to ensure we return as many people as possible back to work and their normal lives. Ensuring the NHS is sustainable is no easy task. It requires brave and bold decisions by local NHS leadership teams as well as a willingness to see the value of investment beyond short-term benefits to the health service. There is, however, a lot to be optimistic about. The pandemic has forced us to adopt innovation to overcome its challenges, and in doing so we now have working models of how to increase diagnostic capacity, improve patient outcomes and manage workforce pressures only in pockets of our NHS. Our Medtech Week is a chance to convince the Government, NHS England and local NHS bodies to increase the spread and uptake of innovation, and regard the investment in medical technology as a benefit both to the future of our health service and our economy.
L
Barbara Harpham is chair of the Medical Technology Group (www.mtg.org.uk), a notfor-profit coalition of patient groups, research charities and medical device manufacturers working together to improve patient access to effective medical technologies.
FURTHER INFORMATION www.mtg.org.uk
The pandemic has forced us to adopt innovation to overcome its challenges, and in doing so we now have working models of how to increase diagnostic capacity, improve patient outcomes and manage workforce pressures only in pockets of our NHS

In 2021, a quiet revolution happened in the world of diagnostics. Billions of COVID 19 tests were undertaken independently across the globe by people of all ages, in their homes. For the first time ever, it was demonstrated on a global scale that lay people can effectively perform independent diagnostic self-tests. Self-testing became the norm. Clinical terms such as “antigen”, “lateral flow”, “time to result” and “infectious levels” became part of everyday life. Along with this came empowerment. Citizens were able to make informed decisions – to leave the house or stay in, to isolate or socialize safely, or to visit an elderly relative. Now that
the pandemic era has ended, the question remains whether this global experience in self-testing can be built upon. Can selftesting be used in non-pandemic situations, and outside of infectious disease control, to enable meaningful health outcomes?

What are the key factors which will support self-testing in the future?
Prior to COVID, diagnostics were very much viewed as being firmly in the domain of health care professionals, with expert training required to undertake professional testing. Because professional testing capacity could

not be ramped up to cater for the demand of COVID testing, self-testing at mass scale was developed and over a period of time, lateral flow devices evolved to provide enhanced usability for lay users. Buffer vials were prealiquoted, test packs became smaller for home use, components required for one test were assembled together, visual aids were printed on instructions for use, and digital readers were developed to improve the accuracy of results reading and reporting. This product development evolution demonstrates that there is potential for other diagnostic products to be designed around lay persons to enhance usability, provide clear guidance, and reduce human error in sample taking, the operation of tests and reading of results. User-centric design will be a key driving factor in enabling lay person self-testing across multiple indications outside of pandemic conditions.
Historically, not many diagnostic tests gained regulatory approval for use as selftests, given the lack of clinical and usability evidence. Regulators had not seen many self-tests, designed with the lay user in mind from the outset, and the supporting clinical and usability studies to evidence that self-testing can be adequately undertaken by a range of users of various ages and demographic profiles. Designing and undertaking self-test studies which meet and surpass regulatory requirements will be a key factor in providing robust evidence and reducing any regulatory and clinical concerns about potential end user risk. This is a key factor in creating trust amongst clinicians and acceptance into clinical pathways.
Given the wide range of health conditions and user needs, future self-tests will need to recognise various requirements across disease pathways and be offered accordingly. E
For the first time ever, it demonstratedwas on a global scale that lay people can effectively performdiagnosticindependent self-tests








This will require a diversified portfolio approach with self-tests being offered for a range of conditions, incorporating a variety of appropriate sampling techniques and chemistries. For example, respiratory diseases (nasal sampling – lateral flow), kidney diseases (urine sampling – dip stick and/or lateral flow), and biomarker testing (blood sampling – finger pinprick testing). Moreover, pre COVID, the most widely used sampling techniques for self-testing were blood pinpricks and urine. However, there is now mass acceptance of nasal and throat sampling which has resulted in public acceptance of and engagement in additional sampling techniques. This has opened the market to wider use cases ranging from acute infection diagnosis to chronic condition care to recognizing potential health concerns and supporting preventive care.

The uptake and adoption of self-testing will depend very much on the healthcare system’s ability to recognise, accept and incorporate self-reported results into care pathways, leading to clinical action and meaningful clinical outcomes. Self-reported results could enable targeted population health management at scale, at risk monitoring, cohort triage, primary care access levers, the enablement of self-care through targeted patient information and qualified routes to HCP in-person appointments, as required. This is an area which is largely underdeveloped but has enormous potential to enable new care models and triaged access to in-person clinical interventions, supported by data and evidence. The desire and drive from the health system to incorporate self-reported results into established care pathways will be a key determining factor for the extent to which self-testing will be adopted at scale.
There is no doubt that self-testing is convenient and enables patient empowerment, and there
are currently many self-testing products on offer to those who can afford them. However, unless self-testing products are affordable and offered at scale across the system to ensure equal access, then the take-up may remain in the hands of the few who can afford it. Affordable, accessible selftesting has the potential to remove health inequalities at scale as it can overcome access barriers, including location, depravation and regional/local capacity constraints. To realise this will require a fresh perspective, a new approach to health provision and a willingness across the healthcare landscape to change the way healthcare is accessed and delivered. We are likely to see several markets emerge in parallel; affordable retail self-pay products for self-care, wellness and prevention. Government-funded products for vulnerable sections of the population to enable timely and accurate intervention; and insurer provided offerings to enable self-care and a detailed patient cohort view, underpinned by data.
So, what is the outlook for self-testing as we enter the post-pandemic era?

To effectively extend self-testing into new disease areas will require collaboration from a whole host of players across the eco-system. Innovators will need to design
user-centric tests which are intuitive and reduce potential human errors. Test manufacturers will need to consult with regulators and take on board their input to design and undertake clinical and usability studies which provide the evidence basis required. Crucially, health systems will need to incorporate self-testing into clinical pathways and enable results integration and actionability. Tests will need to be affordable and made available to a wide range of users, whether this be via the high street and online self-pay, insurers or Government-provided schemes. What we have learned from COVID is that lay users are eager and ready to engage. Behaviours have been modified at scale. There is appetite amongst the public to self-test and self-manage. Crucially, health systems now appear eager to incorporate self-testing, given the pressure on health systems to provide care with fewer resources. To bring about change at scale across multiple conditions will require extensive collaboration between multiple parties. There is growing consensus amongst these parties as to the potential upsides and improved patient outcomes. L
FURTHER INFORMATION www.paconsulting.com
Tests will need to be affordable and made available to a wide range of users, whether this be via the high street and online self-pay, insurers or Governmentprovided schemes


Benedict Wallner has 35 years’ experience in the medical device industry, having started in 1987 as a sales representative for laparoscopic surgery at WISAP where he played a major role in developing minimal invasive surgery in the early nineties. In 1993, he made the switch to single-use medical devices as a sales manager. Since 2001, Benedict has been a partner at preOx.RS GmbH and since 2015, has been general manager. In his current role, he is responsible for sales marketing and product development.
Regulation (EU) 2017/745 is an EU regulation on the clinical investigation and sale of medical devices for human use. The regulation came into force on 25 May 2017, with previously approved medical devices having a transition time of three years to meet the new requirements (up to 26 May 2021).
The regulation replaced Directive 90/385/ EEC, Directive 93/42/EEC. In comparison to the previous Medical Device Directive (MDD), noticeable differences include changes in device classification and device scope, stricter oversight of manufacturers by Notified Bodies, the introduction of
Regina von Campe has 32 years’ experience in the medical device industry, having started as a product manager in 1990 at Sherwood Davis & Geck GmbH. Regina became the regulatory affairs manager at preOx. RS GmbH in 2006. In her current role, she is responsible for quality assurance and regulatory affairs.

the “Person Responsible for Regulatory Compliance” (PRRC), and increased post-market surveillance activities..
With the new regulation now in place, we discuss the effect it has had on the medical device industry. preOx.RS GmbH has been developing, manufacturing and marketing innovative medical products since 1998 with a focus on single-use medical devices
We know that medical devices are incredibly important and are indispensable in any health service, by improving patient
care, reducing costs and saving time. We began by asking our panellists about the importance of medical devices. Benedict says: “Medical devices are used in many diverse settings, for example, by laypersons at home and clinicians in hospitals as well as by healthcare professionals in medical facilities. Medical devices play a very important role in the prevention of health problems with the screening, diagnosis and finally treatment of illness. Medical devices are irreplaceable tools to drive healthcare systems all over the world. They keep us alive, if necessary, and help us to recover. Without medical devices, the survival of E
humankind is challenged. Without medical devices, only the fittest will survive.”

With the introduction of any new regulation, it can always seem more difficult for SMEs to get to grips with it, as they don’t have the workforce, money or legal teams that a large corporation has.
Benedict says: “SMEs often cover niche markets with niche products. The MDR requirements for niche products are the same as for products that sell millions, and so the cost is also the same. The turnover with niche products is smaller so the challenge is to establish a price level which enables SMEs to invest in MDR transition.”
Benedict continued: “The biggest challenge is personnel resources. To support their own Regulatory Affairs, SMEs must look to consultancy. Consultants are rare and expensive, and everyone is looking for one. In the end, MDR is the highest financial risk for SMEs ever and many companies will close.”
On the topic of cost implications of MDR for SMEs, Benedict says: “The cost of MDR is higher than before. Additional regulatory work leads to a cost increase. Depending on the product portfolio of a company, the cost increase could cause a
company to put a stop to products with a low margin or low turnover. SMEs often have low-turnover niche products. These products run the risk of discontinuation.”
Because of this, our experts warn that there will be a negative effect on health care and health services. Regina says: “Devices will vanish from the market, simply because it doesn’t pay off. The availability of products, especially of niche products for treatments which are not regularly used, will get worse.”
In order to prepare for MDR, SMEs face the same process and regulatory journey to approval. Benedict says: “It is very hard for small companies to cover all the necessary regulatory fields and to finance the expenditure. To prepare for MDR, small companies must follow the same ways as big players, so the effort is the same. The major difference is the manpower SMEs can put into the transition. In many SMEs, you have only one person responsible for Regulatory Affairs who must cover the transition to MDR. A regulatory affairs manager needs support from IT solutions. There are many on the market to help companies in the transition but the challenge for SMEs is to find a solution which covers their needs, with easy handling, and minimal cost.”
However, hope is not lost for SMEs in the medical device field. Our experts have some advice for SMEs navigating MDR. Benedict says: “SMEs must build networks and cooperations with each other to bundle experience and know how. Now is the time to share and leave old competitiveness behind. If SMEs take this path, the MDR barrier can be overcome. We are already working in a network, but taking the step to share more for the benefit of all is difficult as there are too many concerns.”
On that note, is there anything that regulators could do to help SMEs with MDR? Of course, it would be in their best interest to do so, as this can only lead to the approval of more medical devices which could be beneficial to population health. Our experts believe that more could be done to help SMEs. Regina says: “The actual situation is that from the 80 former notified bodies, only 34 are newly certified and ready for MDR. If a company like us lose their notified body because they are not certified yet, there is no chance of getting a new notified body. If you have a certified notified body, the time for recertification of products takes more than 18 months. Regulators must accept that the timeframe for changing to MDR is not realistic. The argument that we
had a five-year transfer period and medical device companies did not use this time to prepare for MDR occludes the reality. The reality is that we have too few Notified Bodies for too many companies and medical products. This leads to an overload in the system of certification and finally to the collapse of medical device allocation.”

Regina says that taking all of this into account, there are several actions that regulators can take to help SMEs. This includes expanding the transition time from the previous MDD to the current MDR by a minimum of an additional three years and establishing a scope of action for how to transfer existing products to MDR.
Regina calls for the focus to be on high-risk products to be prioritised and for niche and existing products with a low-risk classification to be excluded from immediate re-certification.
Regina is also calling for the certification of new Notified Bodies to be sped up. At the end of our conversation, we asked our panellists if there was anything they would like to add. Benedict cited Chapter 2 of the Medical Device Regulation, which reads: “This Regulation aims to ensure the smooth functioning of the internal market as regards medical devices, taking as a base a high level of protection of
health for patients and users, and taking into account the small- and medium-sized enterprises that are active in this sector. At the same time, this Regulation sets high standards of quality and safety for medical devices in order to meet common safety concerns as regards such products.”
However Benedict disagrees with this statement, saying: “This 2nd chapter of the MDR illustrates how unrealistic the claim of the new regulation is. It demonstrates an attitude against all medical device companies and implies that medical devices were not safe and had no high standards before MDR. It also implies that there are public concerns about the safety of medical devices and the reliability of medical device manufacturers.”
Benedict continues: “Based on chapter 2, SMEs must ask the question what the intention was with “taking into account the small- and medium-sized enterprises”. Was the intention to eliminate them?
“In the end, MDR overregulates the medical device market in Europe without achieving more safety and patient benefits than before.”
Though MDR has been in effect for a while now, it is clear there are still barriers for SMEs in achieving accreditation. The result of this may be a reduction in the production and invention of medical devices, the closure of medical device companies and therefore a negative effect on healthcare and health services. L
“This Regulation aims to ensure the smooth functioning of the internal market as regards medical devices, taking as a base a high level of protection of health for patients and users, and taking into account the small- and mediumsized enterprises that are active in this sector.”
With
Each year, NHS England releases a report highlighting the number and types of “Never Events” that have occurred across healthcare provider organisations in England.

Described as “patient safety incidents that are wholly preventable where guidance or safety recommendations that provide strong systemic protective barriers are available at a national level and have been implemented by healthcare providers”, hundreds of incidents arise across the NHS annually.
From 1 April 2021 to 31 March 2022, 407 Never Events were reported across the NHS, including a range of safety incidents including wrong implant/prosthesis and medication administration via the wrong route.
The Healthcare Safety Investigation Branch (HSIB) is responsible for conducting
independent safety investigations of such incidents in NHS-funded care. Its purpose is “to improve patient safety by carrying out independent and effective investigations without apportioning blame or liability”. Since launching in 2017, the HSIB has completed and published 76 reports based on national investigations and has made 215 improvement recommendations for improvement. Ten of these reports have concerned Never Events and the learning from these was aggregated in a National Learning Report on the subject1
National drivers for traceability Many Never Events do not result in significant patient harm, it is the repercussions that are often more wide-reaching. However, when such patient safety incidents are occurring and recurring, then the importance and effectively addressing them is clear.
Take the parallels of the 2011 PIP breast implant scandal versus the 2013 horsemeat scandal. In both cases, substandard products were identified as a risk to population health. However, due the widespread use of GS1 standards for product identification, contaminated horsemeat products were removed from retail shelves within two hours. In contrast, to this day, it is estimated that many of the 47,000 patients with faulty PIP implants, are still living with them2
Fast-forward to 2020, and the Independent Medicines and Medical Devices Safety Review (IMMDSR)3, chaired by Baroness Julia Cumberlege, reflects these same challenges.
The IMMDSR explained how the lack of standardised data capture and sharing, made it difficult to monitor trends for adverse events and to then trace these reports back to affected patients. This prompted a central strategy to develop a
national patient-identifiable database to improve traceability. The foundations of which would rely on the effective capture of accurate data, at the point of care, and associating it with the correct patient.
Used for the unique identification of people, products and places, GS1 standards would enable data to captured directly at the point of care via through the scanning of a GS1 barcode – a process known as Scan4Safety4

The Cumberlege Review highlights the benefits of Scan4Safety implementation with reference also noted in some HSIB report findings.
In 2017, the HSIB investigated an incident where a patient received an incompatible hip prosthesis during surgery5. “The error was identified when data from the procedure was recorded in the National Joint Registry several days later.”
As part of the recommendations, it was suggested that “an interim basic scanning system [could be developed and implemented] to identify wrong prostheses prior to implantation”, and for “the Department of Health and Social Care to expand the remit of the working group which includes University Hospitals of Derby and Burton’s Scan4Safety programme.”
Dr Sean Weaver, deputy medical director at HSIB explains, “Different people do things differently. A barcode scanning system could standardise the selection and identification of equipment to prevent errors”.
Scan4Safety
traceability across the NHS
So, how can technology be used to improve patient care? For Leeds Teaching Hospitals NHS Trust, implementing Scan4Safety has provided a wealth of data to help mitigate the risk of errors at the point of care. Medical director of operations, Mr Stephen Bush explains, “Using Scan4Safety has helped us to track activity and inform our decisionmaking around patient care and flow. We now have better and more rapid access to data which has allowed us to improve our ability to care for patients across our organisation”. Leeds have implemented GS1 standards to uniquely identify patients, products, and places across multiple trust sites. Mr Bush continued, “Barcodes and GS1 standards are the key to enable clinicians to reduce patient harm”. The traceability benefits also go a long way. ‘‘Real-time scanning of devices used in patient care ensures that the right product is rapidly identified for that patient and assures us that we have the correct stock levels to care for future patients.’’
To improve patient safety across healthcare systems, introducing system-wide effective risk management strategies are crucial. Dr Weaver explains, “Investigations should be done to maximise learning to make it as safe as possible”. Scan4Safety has been proven to reduce errors and decrease the risk of Never Events.
To deliver better patient care, Scan4Safety should be made commonplace for all


healthcare provider organisations. The tools exist. As Mr Stephen Bush said, “Make the easy thing the right thing and it will work.”L
Credits to: Dr Sean Weaver, deputy medical director, HSIB, and Mr Stephen Bush, medical director operations, Leeds Teaching Hospitals NHS Trust
www.gs1uk.org/industries/healthcare healthcare@gs1uk.org
References:
1. Never events: analysis of HSIB’s national investigations 2. https://www.nhs.uk/ conditions/pip-implants/ 3. https://www.immdsreview.org.uk/ downloads/IMMDSReview_Web.pdf 4. https://healthcare.gs1uk. org/scan4safety/ 5. https://www.hsib.org.uk/ investigations-and-reports/ implantation-of-wrong-prosthesesduring-joint-replacement-surgery/
The UK healthcare system is currently under huge strain. Nearly 20,000 people a day are waiting at least four hours in A&E, while 7.1 million people in England are waiting for elective hospital treatment, up from 4.4 million before the Covid-19 pandemic. The target time patients should wait for cancer therapy in the UK is 62 days, however, the total number of people waiting longer than this period has exceeded 69,000 in England, Northern Ireland and Scotland, and doubled since 2017-2018
The frontline is facing unprecedented pressure to reduce the number of patients waiting for services whilst significantly understaffed.
Recent analysis of NHS figures shows 4.8 million patients waited more than six weeks for a test or scan from Sept 2021 to Aug 2022, which is a 12-fold increase on figures before the pandemic. This is coupled with the reality that there are more than 130,000 vacancies to fill across the NHS, and the effects of this shortfall are exacerbated by the current cost-of-living crisis
A poll of more than 2000 adults by the UK Council for Psychotherapy and YouGov found that almost one in two feel the cost-of-living crisis is affecting their mental health. NHS therapy services won’t be able to manage the increased demand driven by the crisis as they are already thousands of therapists short. Moreover, the significant lack of available social care also means many patients who are fit for discharge are unable to leave hospital as they have nowhere else to go. As many as one in three hospital beds in parts of England are occupied by patients who
are medically fit to leave, but appropriate care services either in patients’ homes, placements in care homes, or NHS-funded aftercare, are lacking.
Increasingly dependent population in the UK
In the UK, we are already facing an ageing population with a growing number of people living with long-term chronic conditions.
The number of Brits over the age of 85 is predicted to double to 2.6 million in the next 25 years, and as such, the population that is dependent on continuous care will also significantly grow. There is also a growing number of younger patients presenting with comorbidities and obesity-related diseases, while it is now estimated that a third of middle-aged adults in the UK have at least two chronic health issues. These groups will continue to contribute to the healthcare burden as they age, presenting challenges when planning health and care services.
The 2022 Elsevier Health Clinician of the Future report explored global trends and changes that are expected to impact the future of healthcare through a global survey of nearly 3,000 clinicians from 111 countries. The report revealed that clinicians believe the increasingly dependent population is driving change across the global healthcare landscape, with 94 per cent believing the rise of chronic health issues will be a key driver of change in healthcare over the next 10 years. Data also showed that 71 per cent of clinicians agree the increase in comorbidities in younger patients will also play a pivotal role in the changing healthcare landscape.
The report suggests a shift to preventive care could potentially reduce the burden of
chronic illness and, in the longer term, result in people visiting healthcare facilities less often. However, findings show that 79 per cent of clinicians believe there is currently not enough being done on preventive care, and 84 per cent agreed that patients with ageassociated diseases will make up the majority of the patient population in 10 years’ time.

The use of digital technology is everincreasing, as clinicians continue to use innovative tools to support interactions and communication with patients. The movement towards more digital appointments, especially in primary care, was accelerated by the pandemic. The Clinician of the Future report highlighted that doctors and nurses believe there is great potential in a digital-first future. Of those surveyed, 70 per cent of clinicians believe the widespread use of digital health technologies will enable the positive transformation of healthcare, in fact, 63 per cent expect most consultations in 10 years’ time will be remote rather than face-to-face.
If digital health technologies are designed with clinicians and patients in mind, wellintegrated, and supported by sufficient training, they have the potential to provide many benefits. Digital technology could save clinicians time spent on administration, enabling them to spend more time with patients, either remotely or face-to-face.
Furthermore, using technology to improve processes around patient records and transitions throughout the care pathway could also free up the frontline from maintaining electronic medical records (EMRs).
A shift to remote may have the potential to empower patients to take on a more active role and become equal partners in the management of their long-term care, however, we must also acknowledge that the evolution to a digital-first will not come without its own challenges. This is also recognised by clinicians themselves. The Clinician of the Future report showed that 69 per cent of clinicians agreed digital health technologies will be a challenging burden, and a further 64 per cent agreed
Tim Morris, vice president, clinical solutions, Elsevier Health has a look at the pros and cons of digitised healthcarelacktheMoreover,significant of available social care also means many patients who are fit for discharge are unable to leave hospital as they have nowhere else to go
the impact of health inequalities will be exacerbated by digital tech.
With primary care activities being pushed to online support and teleconsultation, we risk excluding vulnerable and older adults without digital skills from accessing important health information. According to NHS Digital, it is predicted that by 2030, 4.5m people in the UK, totalling around 8 per cent of the population, will remain digitally disengaged
The reality of the shift to digital-first health services has a huge impact on the well-being of vulnerable patients and places challenges on access to care, I’ve had to manage the consequences of this with my own parents. Both my mother and father have physical and social health needs,
health issues and lives with cataracts and macular degeneration. Though there was adequate online support for respiratory breathing exercises, the ability to assess her condition was significantly more complex when she was unable to travel to the place of care. Further to this, having to book appointments online with impaired vision poses significant challenges.
Digital solutions as the future enabler of clinical care priorities As clinicians continue to face an increasingly dependent patient population, digital transformation has the potential to empower patients to take an active role in their care. This can help reduce the time clinicians spend on administration so they

complex and continuous needs. It is vital that we ensure digital health technologies should be co-developed with clinicians and patients, to ensure they are fit for purpose.
With a shift to digital-first care, healthcare organisations must support clinicians with sufficient training on new technology and processes so that they are implemented and used to full effect. As a company committed to improving patient outcomes, Elsevier Health will continue to listen to and partner with clinicians, so that we can better understand the challenges they are facing and help to address their evolving needs to best support the dependent population. L
Much has happened since Getinge was founded in 1904 in the small town of Getinge, Sweden. Now with operations in 39 countries, sales in more than 125 countries and more than 10,800 employees worldwide, the company has transitioned from selling products to a trusted partner with customer focused solutions that contribute to quality enhancements and cost efficiencies for healthcare systems in the UK, Ireland and the world
Five years ago, this family of healthcare and life science brands – including Maquet, Lancer, Atrium, Pulsion, Datascope, Steritec, Stericool, Trans and others – were merged into one single Getinge brand.
“Our solutions are designed to help healthcare providers improve patient outcomes, drive efficiency, and maximise their return on investment,” says Avril Forde, president North Europe and managing director of Getinge UK & Ireland.
Avril continues: “With a global network of experts and 25,000 customers across 120 countries, we can offer our partners valuable insights from all over the world – and our local teams are always ready to help anytime, anywhere, with a deep understanding of the market and the unique needs of each customer’s facilities.”
Getinge has grown considerably, mainly through acquisitions, over the last two decades. In 2000, the acquisition of Maquet enabled the Swedish-based enterprise to start provisioning operating theatres, and the expansion continued with the integration of several companies within OR equipment and critical care. Since 2008, Getinge has also contributed to clinical progress in the field of cardiology with acquisitions such as Datascope and Atrium.
The recent acquisition of Applikon Biotechnology in 2020 strengthens the offering of advanced bioreactor systems from research to production within the Life Science area.
“We have an extensive brand portfolio with products, solutions and services for intensive care, operating theatres, sterile reprocessing, cardiovascular procedures and life science. Our purpose is as true today as it has always been – we want to empower our customers with the knowledge, expertise, technology and resources to save lives. Our brand promise of ‘Passion for Life’ is not just words, it’s at the heart of everything we do,” says Zah Hussain, director marketing and communications North Europe.
Combining industry-leading solutions into a holistic offering Getinge’s intensive care portfolio includes innovative life-supporting products and solutions for ICUs and intensive care transport that can improve clinicians’ ability to save more lives and reduce long-term complications.
The operating room offering features advanced life-saving therapies and equipment, digital patient management, and the design and implementation of both standard and hybrid operating rooms made to handle a broad range of procedures and patient needs.

Getinge has been working with sterile reprocessing since the early 1930s, and presently the company offers customised and flexible solutions for the complete CSSD, including equipment, consumables and software that can enable hospitals to increase throughput of sterile instruments with the highest level of infection control.
Within cardiovascular surgery, there are solutions for open-heart surgery, advanced monitoring technologies and minimally invasive therapies that help clinicians to conduct successful surgeries as well as to enhance visibility and awareness of patient status.
Finally, the life science business area covers a complete range of sterilisation equipment and transfer systems for pharmaceutical production and medical research institutes, customisable and designed for end-to-end contamination free processes and workflows.
“Our vision is to become the world’s most respected and trusted medtech company, and the ability to combine all our industry-leading
solutions into one holistic offering, which can be individually tailored for the customer, is one of strongest assets,” Zah Hussain explains.
By using EcoDesign principles to design products with special consideration for the environmental impact during their entire lifecycle, Getinge proactively minimizes the use of materials, ensures that products are recyclable and helps customers reduce their consumption of energy, water and other consumables.
“Our sustainability work is an integral part of our passion for life. We are committed to conducting business that is socially, ethically and environmentally sound across the entire value chain. By respecting our customers, employees and the planet in everything we do, we make a positive impact on society, today and in the future,” Zah continues.
Helping hospitals to catch up with the backlog of surgeries in the aftermath of the COVID-19 pandemic has been an important focus area for Getinge.
Research by the NIHR Global Health Research Unit on Global Surgery shows that 50 million operations globally were cancelled in the first pandemic wave –and that a restart has only been partially successful due to lack of capacity.
In the UK, the NHS has expedited its digitisation plans as a point of necessity throughout the pandemic, with the aim to use additional digital tools in order to realise the full efficiency potential, encouraging staff to work smarter, not harder.
“Our global expertise and significant legacy in operating theatres has enabled us to develop several successful solutions for supporting hospitals in their efforts to reduce the backlog of patients waiting for an operation,” Amy Rothwell, general manager healthcare UK & Ireland says.
Getinge’s Torin OptimalQ and Torin OR Management are designed to help hospitals utilize their surgical capacity in the best possible way.
Torin OptimalQ was launched in the summer of 2020 as a direct result of the acute situation during the pandemic. The service is scalable, easy to deploy, and delivers quick results for staff and patients.
By merging statistics in different areas, such as surgical times and best planning practices, with the customer’s own waiting list data, the tool can calculate the best way to prioritise the surgeries and propose a schedule for the upcoming weeks.
In addition, Getinge’s Patient Flow system INSIGHT gives a hospital complete control over the patient flow from arrival to discharge. It supports the highest standards of care by allowing staff to plan, prioritise and take action to manage patients and beds with a clear overview across the hospital.

As data is shared in real-time, INSIGHT enables better decision-making on all levels, from the individual caregiver to the hospital management.
Both Torin and INSIGHT can be connected with existing systems and deliver a simple and intuitive way of working. These solutions can be implemented separately or deployed in conjunction with each other.
“Successful implementation has been seen across hospitals worldwide and from across all types and sizes of sites. These software solutions can deliver efficiencies and operational improvements across hospital disciplines, which in turn deliver significant savings, improve working environments and ultimately help reduce the NHS elective backlog,” Avril Forde explains.
Partnership is the key to success Getinge’s new technologies and new approaches have demonstrated results, from increased throughput to decreases in average length of stay and reducing non-contact clinical time for staff, all helping to reduce waiting lists and improve patient outcomes.
None of this would have been achievable without the partnership approach, where both the hospital and Getinge work together, sharing best practice, and delivering solutions to agreed common goals.
Flexible commercial solutions, which improve efficiency and productivity while minimizing financial and operational risks are vital components in Getinge’s partnerships with healthcare organizations in the UK and Ireland.
Solutions are designed to meet each hospital’s individual needs, and they come with the flexibility to make changes at any time.
“We guarantee that the chosen solution performs as well on the last day of the contract as on day one. This means that we maintain all equipment to guaranteed availability, so you can plan your work flow with confidence. We also carry out safety-related updates and improvements at no extra cost,” says Getinge’s service programme manager Bob Allen, who has been with company for 20 years.
Bob continues: “As a Getinge partner, all your needs for planning, maintenance and support go through one single source, saving you time and resources. Customers can choose from a variety of preventive service plans and rely on our certified technicians to resolve any issue.”
Education and training Getinge’s education and training solutions bring together healthcare professionals from all over the world, empowering them with advanced clinical and technical programs.
Participants can benefit from technical and operational training, to maximize the use of Getinge equipment. There are also opportunities to gain insights and clinical know-how for implementing new options for improved treatment, including skills needed to operate a new software solution efficiently. L

Join the diverse UK digital health community for the ultimate learning and networking experience at London’s Business Design Centre, 14-15 March. Digital Health Rewired is for anyone wanting to make a difference in UK digital health including NHS and social care, private healthcare, suppliers, start-ups, innovators, policy makers and patients

Explore eight stages of CPD-accredited educational content featuring the latest direction on national policy, pioneering work by local health IT teams and the new innovations making waves across health services.
What does Rewired offer? Rewired 2023 offers two-days of networking, collaboration and in-person learning
during two days of educational conference sessions, exhibition and meetings.
What topics are covered? Topics include National Policy, Digital Transformation, Integrated Care, AI, Data and Analytics, Cyber Security, Digital Nursing, and Smart Heath. Rewired will also showcase a fantastic array of latest best practice, case studies and experience
from all parts of the NHS. The joint headline sponsors are System C and TPP.
The event’s latest keynote is the author of ‘Better, Broader, Safer’, the review into better using health data for research and analysis published in April 2022.
Professor Ben Goldacre will share his views on how the NHS should safely E


and efficiently use its powerful datasets to improve healthcare outcomes.
Other confirmed Digital Health Rewired 2023 keynotes include deputy CEO of NHS Providers, Saffron Cordery, and NHS England director of transformation Dr Tim Ferris.
Drawing on experiences from NHS Providers’ digital board programme, Saffron will outline the next steps for delivering digital at trust-level against the backdrop of political structural reform. Dr Ferris will be speaking at a key moment following the merger of NHS Digital into NHS England, with major changes in priorities and programmes.
Other speakers include Dom Cushnan, director of AI, imaging and deployment for NHS AI Lab; Lisa Emery, chief transformation, innovation and digital officer for NHS Sussex Integrated Care System, and chair of the CIO Network; Dr Natasha Phillips, CNIO at NHS England; Rob Webster, CEO of West Yorkshire Health and Care Partnership and Ruth May, CNO, NHS England.
The event will also be running the popular Rewired Pitchfest – a competition which provides a platform for young and innovative ventures to scale in the NHS. The 2023 contest, which closed for applications on 8 December, has added a new category for scale ups.



The live final will take place at Rewired 2023 with finalists pitching to win an NHS test bed site. Start-ups and scale ups can apply by completing a short entry form at digitalhealthrewired. com/rewired-pitchfest-2023
Rewired is free to attend for NHS, public sector, non-for-profit and third sector providers, charitable sectors, academics and researchers. L








Cybersecurity will always be needed for the NHS, but what is the current threat level and what can be done to mitigate these threats?
Cybersecurity is always a hot topic in the NHS, with huge amounts of personal data possibly at risk. The WannaCry cyberattack in May 2017 was an example of the risk faced by the NHS.
A report from the Department of Health and Social Care revealed that the attack led to the cancellation of 19,000 appointments, with an estimated 1 per cent of care disrupted. While this might not seem like a lot, it is estimated this cost the NHS around £19 million in lost output. The estimated cost of IT support during and after the attack amounts to £73 million pounds. With record backlogs, the NHS cannot afford to cancel appointments on a large scale. Nor can it afford millions of pounds of unexpected IT costs.
80 hospital trusts and 8 per cent of GP practices were disrupted after ransomware locked users out of digital systems and medical devices. The attack was brought to an end by a cyber researcher activating a kill switch.
A National Audit Office investigation into the attack looked into the impact on the NHS and its patients; why some parts of the NHS
were affected; and how the Department and NHS national bodies responded to the attack. The report found that the Department was warned about the risks of cyber attacks on the NHS a year before WannaCry and though work was underway, it did not formally respond with a written report until July 2017.
So what is the current cyber risk to the NHS now and what can be done about it?
NHS Digital says: “Cyber threats are constantly evolving and always present, so digital health and care organisations must remain prepared and ready to respond. We provide a range of specialist services that help NHS organisations manage cyber risk and to recover in the event of an incident.”

NHS Digital regularly publishes cyber alerts, with recent alerts including “OpenSSL Vulnerabilities Impact Multiple Cisco Products” and “AliveCor KardiaMobile Vulnerabilities”, as well as several security update announcements.
Threat intelligence bulletins are issued to users registered on the respond to an NHS cyber alert service when a threat is assessed as high-severity or weekly via email. Cyberattacks are of course still a real threat, especially with even more reliance on digital systems and technology. Cyberattacks can cause low to serious disruption to patient care and services and also present a serious risk to patient data. Several things are needed to improve cyber resilience, including tools, organisations and people and none can be used in isolation.
NHS SBS’s Cyber Security Services
Framework provides a range of external support services to help NHS organisations manage cyber risks and recover in the event of a cyber security. The Framework runs from 12 May 2020 - 11 May 2024 and can be used by the NHS, Local Authorities, Emergency Services, Educational sector and all Public Sector Organisations located across the UK. E
In May 2017 a global ransomware attack known as WannaCry affected more than 300,000 computers in at least 100 countries, which in the UK particularly affected the NHS.

According to NHS England, the WannaCry ransomware affected at least 80 out of the 236 trusts across England, because they were either infected by the ransomware or turned off their devices or systems as a precaution. A further 603 primary care and other NHS organisations were also infected, including 595 GP practices. It was estimated to cost the NHS £92 million after 19,000 appointments were cancelled as a result of the attack.


Reduce the risk of this happening again and book a Vulnerability Assessment today from only £29 per user! Its not a matter of IF you get hacked, but WHEN…
The Framework has three lots: 1, Emergency Cyber Incident Management; 2, Cyber Security Consultancy Services and Lot 3 Security Personnel.
The Framework offers several benefits, including that it is supported and approved by NHS Digital who provide detailed input into specification and evaluation. Lot 1 Emergency Cyber Incident Management offers specialised suppliers with the option to offer time-critical response 24 hours a day. It also offers the opportunity to appoint providers on a regional or national basis. There are 25 suppliers on the framework, including SME specialists and multi-national providers. The framework offers the ability to direct award, providing a quick route to market to meet requirements. It also offers mini-competition, which can help drive competitive pricing. The fixed public sector framework pricing offers competitive rate.
On top of this, all appointed suppliers have mandatory certifications, including Cyber Essentials Plus or equivalent.
Lot 1 Emergency Cyber Incident Management includes the provision of urgent incident response capability for large-scale or local incidents.
Lot 2 Cyber Consultancy Services provides the specialist support needed to enhance an organisation’s cyber credentials. This could include Data Security On-Site Assessments, Security Testing, Technical Assurance, Forensics and Investigations, Policy Development, Awareness and Training. This could be useful for an organisation with a requirement to access

ad-hoc or ongoing advisory support. Lot 3 Security Personnel enables the supply of specialist personnel to support existing in-house capability. The aim of this lot is to support organisations to reduce their exposure to threats, improve security defences and provide resource support to respond to cyber incidents.
Aside from services, tools and personnel that you can source, they are ways you can improve cyber security at an organisation level. For Cyber Security Month, Mike Fell, NHS Digital’s executive director of national cyber security operations laid out his top security tips for health and social care workers. He said: “From email and social media to online banking and shopping, it has never been so crucial to take vital cyber security steps to prevent criminals getting hold of data, devices and accounts.
“Here in the NHS, getting cyber security wrong has the potential to cause significant impacts across the health and care system.
“If a GP can’t access their system, they may not be able to share life-saving prescriptions with pharmacies or critical information with hospitals. Similarly, cyber attacks can cause
cancelled appointments and surgeries, possibly resulting in care diversion to other hospitals.
“Cyber security is as important as health and safety, and in just the same way it’s the responsibility of every person in the NHS to understand security risks and what they can do to reduce them. Fortunately there are a few simple steps we can all take to ensure we stay cyber resilient at home and work.”
Regularly sharing information and tips with your colleagues is a great way to improve your cyber security.
Fell’s top tips include using a strong password as a more complex password is more difficult to crack and make sure you always lock your computer or mobile device when you are away from them. He also warned people to be aware of phishing scams which can attempt to steal information and are getting more sophisticated.
Fell also pointed out that it is important to keep up to date with data training, as well as to make use of the resources that are available to promote and improve cyber security. L FURTHER
“If a GP can’t access their system, they may not be able to share life-saving prescriptions with pharmacies or critical information with hospitals.”

Since October, the UK Government has been on ‘high alert’ - preparing for a new wave of potentially devastating Nation State-led cyber-attacks towards our critical infrastructure. With cybercrime rising around the world, costs are set to reach $10.5 trillion a year by 2025, with the health sector being a specific target for cyber criminals due to the sheer amount of data it harvests and stores.
According to U.S. government data, cybersecurity vendors have seen a sharp increase in data breaches targeted at the healthcare industry during the first five months of 2022. Supporting this, a 2021 study by Critical Insight using HHS (U.S. Department of Health and Human
Services) information found that between 2018 and 2021, there was an 84 per cent increase in the number of data breaches against healthcare organisations. When it came to the number of victims impacted by these breaches, the figures jumped from 14 million in 2018 to 44.9 million in 2021.
While the increase in these figures is shocking, what’s important is that we recognise that the form of many of these attacks is changing. Some threat actors are stealing and ransoming data, but others are encrypting entire networks and disrupting urgent medical care. As a result of the type, impact, and frequency of cyberattacks evolving so rapidly, many organisations are left struggling

to stay one step ahead of the battle to keep their organisation, patients and data safe.
The explosion in cyber threats against the medical industry is being fuelled by the increasing use of medical IoT. The medical IoT industry produces all manner of equipment, from heart monitors to infusion pumps that administer crucial drugs. All this is changing the face of many healthcare services around the world by increasing medical accuracy and patient satisfaction rates, thanks to its ability to facilitate remote treatment and monitoring.
Over time, gathering vast amounts of patient data upon specific illnesses improves patient treatment and advances the future of care for the betterment of everyone. But gathering this data requires such medical devices to be connected to networks or the internet. With more than 75 per cent of all medical devices now linked to a network, these devices increase the attack surface, thereby increasing the number of potential routes in for cyber criminals.
Despite the inherent benefits of connected medical devices, many hospitals’ devices are over a decade old and have never been patched. This is particularly problematic for healthcare settings which use extremely sensitive pieces of technology, for example, highly targeted radiological cancer equipment. It’s also been reported by the Interim CIO at NHSX that 21 million items of malicious activity get blocked every month within the NHS, which can only emphasise the criticality and urgency of the issue.
The rapid growth of these connected devices also means that the supply chain for many healthcare providers has widened. With rising third parties involved in the chain, from software suppliers to the device manufacturing companies, cybercriminals look for ways to E
The explosion in cyber againstthreats the medical industry is being fuelled by the increasing use of medical IoT
We are a UK based Veteran owned IT Security Consultancy, specialising in the technical aspects of Cyber Security. We provide a broad consultative approach to all of our customers in order to support their drive to improve their security posture, we achieve this through recommending/implementing the appropriate levels of security controls and also general security hardening.

























































Our team are adept at providing specialist knowledge at all levels within a Security Operations Center (SOC), Vulnerability Management Team, Endpoint Security or even guiding and securing Infrastructure and Cloud technologies. What’s more, all of our team members have hands on experience across multiple technology stacks, not just the theory.
While we primarily provide consultancy services, we have aligned with some vendors that we believe offer the best value for money to prospective customers. Our chosen partners, Microsoft, Tenable, Juniper and Palo Alto are used by us or would be used by us if we had a particular requirement for them, we won’t promote a vendor just for a sale.








“We have worked with Planned Link for the past 5 years. As we have grown and evolved, what I have valued most about our relationship is that Planned Link understand us, our business and where we are going.”

To contact us by Email Click here To view our website Click here
































compromise these businesses as a way to gain access to confidential information on the medical organisations that they serve.
With 60 per cent of incidents reported as the result of a third-party partner with stolen , these cyber criminals are targeting the smaller suppliers and service providers, knowing that their cyber security measures may present a weak spot, and an opportunity to attack further up the supply chain. A recent example of this was seen in the UK in August 2022, when the NHS 111 suffered an attack by cybercriminals which impacted one of their suppliersthe software vendor, Advanced. This led to specific NHS services being rendered unusable for certain parts of the country.
To safeguard against attacks through the supply chain, healthcare organisations should ensure that supply chain partners comply with their own cyber security and data management policies.
To increase supply chain resiliency, hospital leaders should insist that your suppliers have simple but standard processes in place like having Multi Factor Authentication (MFA) as standard and not as an exception.

Ensure that any new suppliers complete an information security questionnaire which will allow healthcare organisations to understand and enforce best practices when it comes to cybersecurity measures.
Create new contingency plans that address serious, long-term disruptions, such as forming coalitions with other hospitals to ensure they can share scarce resources (as appropriate).
Automate and update enterprise resource planning (ERP) and materials management information systems (MMIS). While healthcare was initially a leader in implementing ERP and MMIS, the industry has fallen far behind
other industries when it comes to supply chain management. Many hospitals haven’t upgraded their systems or transitioned to automated processes. Doing so will enable easier tracking and analysis of data, for example, data related to inventory will allow for a much quicker response to shortages and use fewer resources to remedy.

Implement AI-based analytics and demand forecasting that incorporates supply chain disruption into their algorithms. A February 2020 survey of 100 hospital and supply chain leaders by Sage Growth Partners indicates there is a significant need for hospitals to adopt these technologies. Only 12 per cent of survey respondents said they use AI or predictive analytics to optimise the supply chain. AI and demand forecasting technologies will help ensure that hospitals have enough critical supplies and devices during the next significant supply chain disruption. In addition to securing their supply chain, healthcare organisations must also increase their vigilance and implement
extra cybersecurity measures if they wish to remain one step ahead of the continual threats from cyber-attackers.
In the 2022 Data Breach Investigations Report, it’s been found that 82 per cent of breaches involved a human element. Whether it’s the result of using poor credentials, a lack of good network management or education among staffbelow are the key steps healthcare trusts can take to better protect themselves against any impending cyber-attacks:

















With numerous devices accessing any one network together with the boom in the Internet of Medical Things (IoMT), it’s crucial for organisations to have clear visibility of what is connected, from where and by whom. Currently, many connected devices are largely unmanaged, and healthcare E

With 60 per cent of incidents reported as the result of a third-party partner with stolen access privileges, these cyber criminals are targeting the smaller suppliers and service providers, knowing that their cyber security measures may present a weak spot, and an opportunity to attack further up the supply chain

staff don’t have enough visibility of what these pieces of equipment are doing in real time. Understanding how these devices are communicating to the network is paramount to ensuring the security of any device and minimising the chance of an attack.
Proper access management
Access to data, systems and services needs to be protected, which often involves restricting employees only to the information they need to do their job, and always having some level of verification in place for every user. As a result, it’s imperative for an organisation to consider how it establishes identity and to incorporate appropriate methods that will establish and prove the identity of users, devices, or systems, making it increasingly harder for attackers to pretend to be legitimate. Identity and access management policies should be put into operation to account for who has access and under what circumstances.
The people employed by an organisation need to be front and centre of every cybersecurity strategy. As they’re often on the frontline of patient care and safety, they are well positioned to be one of the most effective resources in preventing incidents or detecting when one has occurred. However, this is only possible if they are properly educated on the potential cybersecurity risks and vulnerabilities, and trained in how to reduce these as well as respond in the event of an emergency.


To better guard themselves against the ongoing attacks from cybercriminal gangs, the healthcare sector needs to take steps to defend itself from the outside by ensuring robust supply chain security, but also from the inside. This entails proper cybersecurity management, access, and training of staff on how to detect, minimise and react to breaches. However, doing this will require better tools to enhance visibility of networks, monitor access and risks, and mobilise staff through ongoing training to keep them one step ahead of these ever-changing cyber-attacks. L
Phil Howe is the chief technology officer (CTO), appointed 2020, at Core to Cloud. Phil is a highly experienced, multi-skilled senior IT manager with a hands-on understanding of building new technologies inside significant and critical IT infrastructures, having spent over 18 years working in the NHS. Before joining Core to Cloud, Phil was an IT specialist for
Ehealth at NHS Dumfries & Galloway and later joined the Bolton NHS Foundation Trust as a senior system & network technician and was appointed as deputy chief technology officer. Here he oversaw the third line and projects team, responsible for technical strategy and programme management, planning, funding, and delivering major IT projects and systems to support IT security and patient care delivery in a large and complex organisation.
Phil also has extensive experience working in the private sector, where he worked as a senior technical project expert and engineer with Northgate Information Solutions for almost four years. As a member of the Core to Cloud team, he will now assist the company in expanding and progressing to the next stage of its rapid development.
FURTHER INFORMATION www.coretocloud.co.uk
Access to data, systems and services needs to be protected, which often involves restricting employees only to the information they need to do their job, and always having some level of verification in place for every user
From important meetings, and vital training sessions to life-saving MDTs and remote consultations, videoconferencing technology is a vital tool for healthcare providers these days.
In recent years, many organisations have moved to the Microsoft Teams platform, which provides substantial advantages over traditional videoconferencing systems such as scale, easy connectivity with meeting rooms, laptops, smart phones and tablets and it is very intuitive to use. Teams has transformed the way many health sector organisations communicate and collaborate, resulting in high efficiencies and improved service delivery.

Interoperability - the challenge
Unfortunately Teams does not work natively with traditional VC solutions. Third party Cloud Video Interoperability (CVI) services came to the rescue and allowed standards-based VC systems to work with the Teams platform via the CVI Service.
A major benefit to organisations that had previously invested in traditional VC environments, CVI ensured they could continue to use those technologies alongside their new Teams ecosystem.
NHS Digital who provides all NHS organisations with a CVI service retired the service on 28th October 2022. See the official notification here
For those organisations that have a hybrid environment of Teams and traditional VC, this change has created a disruptive communication pathway. Today, meetings are just as likely to be held online as they are in-person, transitioning to a communication strategy empowered by Microsoft Teams Rooms has never been more relevant.
An abundance of experience Here at Visavvi, we have over five decades of experience designing and delivering AV and communication and collaboration solutions for NHS organisations. We are highly certified and have long-held, senior, trusted relationships with Microsoft, Poly, Logitech, Crestron, and Lenovo.

As industry collaboration experts, in 2015, we were selected by Microsoft to be a launch partner for the groundbreaking Microsoft Surface Hub and have remained a trusted partner ever since.
From consultation to design, installation, and support, we are trusted by NHS trusts, large government departments and global businesses, to provide technology solutions that empower their employees to collaborate and communicate.
Our highly experienced account managers, solution architects, and
engineers are supported by a team of trained communication and collaboration specialists who are industry-leading experts when it comes to Microsoft Teams.
In partnership with Microsoft and to help organisations overcome this new interoperability challenge, we offer a free site survey of videoconferencing environments along with recommendations to Teams and a detailed communication, collaboration, and audio-visual consultancy report. One of our specialist digital workplace consultants will undertake a full strategic assessment of your current and future operational needs across your entire estate.
Carefully listening to your needs and gaining a detailed understanding of your IT and Microsoft environment will allow our specialists to specify the right solution for your organisation.
Commisioning a full consultancy report including a network and MS Teams readiness assessment, will allow for a smooth transition to a Teams-based communication strategy for the future, bringing enhanced operational benefits for healthcare professionals and patients alike.
South Tees NHS “Visavvi have changed the way we work. They are professional, they answer any questions, they are happy to carry out demonstrations, nothing seems too much trouble for them and that makes a big difference when you are the customer.” L
To find out more, visit www.visavvi.com/ healthbusiness or scan the code. 0370 606 1100
With an ever-increasing need for videoconferencing technology in the NHS, Visavvi can help with a transition to Microsoft Teams
For many years organisations have relied on videoconferencing technology to allow healthcare teams to communicate, collaborate and to deliver vital services to patients
In this article, Barbara Harpham, chair of the Medical Technology Group, looks at regional variation in healthcare and how regions and hospitals can learn from each other to improve care

A new report by the Medical Technology Group reveals that high performing hospitals are treating up to three times as many patients as consistently poor performing ones in London and the Midlands. Despite proof that the ‘postcode lottery of care’ has been entrenched by the pressures of the pandemic, this variation should now be seen as an opportunity to learn from the best.
If you want urgent treatment, the data from our latest report suggests you should probably move to Wakefield. This was the highest performing region during our eightmonth investigation into where you could find the best NHS care in England. Looking at NHS patient referral to treatment data, we found that some areas of the country perform consistently better than others. Amid an ongoing crisis in resourcing, staffing and provision of care, it’s important we find out why this is the case. Since 2019, we’ve been campaigning to raise awareness of the fact that all too often in the
NHS, your level of treatment is dependent on where you live rather than what you need. However, a lot has changed since our original campaign in 2019. The health service is going through its worst ever crisis in the wake of Covid-19 at a time when it has transitioned to the Integrated Care System. Rather than frame regional variation as a problem, we wanted to champion and highlight those regions and hospitals that were succeeding against the odds. In analysing their success, we wanted to present their level of care as a benchmark all hospitals in the NHS are capable of achieving.
Our data analysis period was significant for a number of reasons. July 2021 to March 2022 saw hospitals begin to work in earnest through the backlog of care, tackle the spread of the Omicron
variant, and work out the impact of the pandemic on an overworked, and all too often under-rewarded workforce. This was the re-emergence of the NHS from the pandemic before it fully transitioned into the integrated care model that in some regions had already been in operation. This all added a layer of complexity to our analysis of the regions. It’s fair to say there are a number of factors that need to be considered when comparing different regions, such as varying levels of population density, different health population needs and the varying spread of Covid-19. To address this, we focused not just on those that performed consistently well, but also those that managed to improve their ranking during our data period. Some CCGs, for example Bury, rose dramatically while others marked consistently high performance E
If you want treatment,urgent the data from our latest report suggests you should probably move to Wakefield

With our wide range of styles and colours we can help you create the right atmosphere for your care home without compromising on comfort or safety and all our upholstered furniture is available in a range of easy to clean and hygienic fabrics or faux leathers




Please browse to see our full range or contact our sales team to discuss your requirements further

Rosehill’s bestselling The Hamilton Patient & Visitor Chairs are a high quality and durable choice for your ward or waiting room. The chairs have a profiled seat for maximum comfort and an ergonomically designed back rest with a removable seat to help for easy cleaning. Optional extras include wheels, variable seat depth cushions to ensure the correct posture for multi-patient use, armpads and filled in sides.

where their neighbours continued to decline. What was at play in these hospitals? We decided to investigate.

The case is often made for the uptake of medical and data technology in the abstract - faster operations, more efficient use of staffing resources, better patient outcomes. It was refreshing to see it in action in places like Bury, who slashed their waiting lists using same-day, highly specialised surgical clinics that treated record numbers of patients. In Wakefield, data technology created a ‘shared referral pathway’, allowing doctors to communicate with each other often across primary and secondary care as the patient completed their pathway. In examining the use of medical and data technology, something we’ve written extensively about in our reports, another factor also emerged: the leadership strategies and implementation of this technology which accounted for its varying degrees of success across the system. Put simply, management, human resourcing and clinical practices, despite NICE guidance, vary heavily from region to region. The use of medical and data technology was often only as good as the way in which it was utilised by management. In many instances, this best practice was years in the making and accountable to long-term health initiatives planned around specific treatments areas such as cardiology, orthopaedics and gynaecology.
Learning from the best This all brings us to the question. How can we ensure that what is working best in the system is scaled out and replicated across the health service? The solution is quite clearly not a simple one. It rests on a degree of cooperation, but also understanding across different stakeholders that best practice can not be replicated overnight, but is often built
into the ‘culture’ of one particular hospital or region. That said, strategies to level up, or even in some instances ‘raise up’ specific areas of the NHS which are chronically struggling, must be based upon this best practice. Observing what works well in the system and communicated effectively by fellow NHS professionals is tangible and not built on the abstract. It transforms the promises of the ICS: innovation, integration and population health into tangible management structures and procurement of technology. We need strategies built around this, with targeted funding for those regions to implement them.
For this to happen, there is work for all three tiers of NHS management to do. Firstly, the Government must develop a national strategy to implement best practice backed up by a meaningful recourse to funding and action for those ICSs that continue to perform poorly. Our report and our case studies may serve as a start for determining this best practice, but if the government is going to continue to pump money into the NHS to recover from the backlog and deal with the workforce crisis, time must be spent ensuring it is being spent on proven solutions. Secondly, NHS England must work in conjunction with this strategy by developing better pathways to spread innovation. This is a particular priority given the new ICS model risks devolved health regions siloed on particular
population health data. We should continue to believe that what works well in one part of the country should work well in another. Lastly, local NHS bodies and leaders must continue to procure and encourage proven medical technology and innovative practices, as well as champion best practice they find in their region. NHS variation is not just a regional one, but also a local one too, with hospitals barely ten miles apart treating twice as many patients in some instances.
As we prepare for another winter of misery, we must continue to believe that the NHS is capable of delivering a worldclass quality of care. Indeed, there are many regions and hospitals that continue to fulfil this thanks to the endeavour and innovation of their staff. In a crisis, ways of working more efficiently and making the best use of resources have been forged. It is now essential that we back this innovation with appropriate funding, policy and commitment across all levels of the NHS. L
Barbara Harpham is chair of the Medical Technology Group (www.mtg.org.uk), a notfor-profit coalition of patient groups, research charities and medical device manufacturers working together to improve patient access to effective medical technologies.
www.mtg.org.uk
Firstly, the Government must develop a national strategy to implement best practice backed up by a meaningful recourse to funding and action for those ICSs that continue to perform poorly
Dr Helen Davies, NHS general practitioner, population health/digital lead and Cegedim Healthcare Solutions’ Clinical Advisory Board member, lays bare Population Health Management and steps for NHS organisations to achieve it
What is Population Health Management?
It is sometimes described in vague terms that make it sound like public health, or - what we have always done as clinicians - attempting to do evidence-based, patientcentred practice. What it is actually about is a radical shift in care delivery that starts with the needs of a population, not the capability and configuration of a string of isolated providers. It is a model for the planning and delivery of proactive, anticipatory care to achieve maximum impact within collective resources. It is an exercise in service design for the whole population, one cohort at a time, using data and analytics to guide us.
So, why is it so important now? There is an increasing body of evidence internationally that healthcare is delivered best, if it’s done as an integrated care system across various health and care providers, with person-centred care at its centre. The data also tells us it is multi-morbidity which is currently driving demand and cost within the NHS: more than one in four of the adult population in England currently lives with two or more conditions. Living with numerous and often complex health problems is becoming the norm for older people and those from disadvantaged communities. Some conditions cluster together and people can experience many different combinations of conditions, the impact of which can also vary.
Yet, despite considerable diversity in their disease profile and circumstances, people with multiple conditions frequently share common problems. They may have reduced mobility, chronic pain, shrinking social networks, incapacity to engage with work, and lower mental wellbeing. To date, these problems have not been well-addressed by services or research.
We tend to organise services around single conditions; doctors train in specialties; and research and decision support tends to be organised one disease at a time. This siloed way of thinking about morbidity doesn’t reflect the real world. People with multiple conditions want greater service integration, more person-centred, holistic care, and better support for mental wellbeing. To address this, innovative ways of intervening are needed; a Population Health Management approach is needed. Here is how we can succeed in its delivery.
Population health management laid bare

There is an overlap with Population Health (public health) which the Faculty of Public Health defines as “the science and art of preventing disease, prolonging life and promoting health and wellbeing, through the organised efforts of society”. Population Health Management (PHM) focuses on groups of people with shared characteristics (a cohort) and the design and delivery of holistic care of that cohort and each person within it. In this it links public health with direct patient care. This proven approach uses datadriven planning (quantitative and qualitative) and includes segmentation, stratification and ‘impactability modelling’ to identify which specific ‘at risk’ cohorts to target. The concepts of integration are key to this redesigned service and the concept of working closely with users and communities themselves. The PHM approach is anticipatory and proactive to achieve maximum impact and uses collective system resources to address wider factors such as environment, e.g. housing, transport, green space, as well as social factors such as education, employment, isolation, and safety – and behaviours, e.g. smoking, diet, and alcohol – all of which we know are important determinants of health and wellbeing.
It is about using data, insights and evidence of best practice to co-design and deliver integrated models of care working with health, social, community, voluntary and private sector and the public themselves.
The implementation of the 2021 Health and Care Act puts in place enablers to make it easier for health and care organisations to deliver joined-up care for people who rely on multiple services. These include enablers such as engaged leadership with aligned incentives, joined-up data and IT, facilitative decisionmaking processes, lines of accountability and information governance in place.
Equally important as these structures and processes, we must not forget that the workforce aspects to this change are key. People are the ones who are both delivering and receiving care, so we must ensure that we take people with us, that they are involved in and feel part of the journey.
People often wonder where and how to start, but I often say to simply start where you are with what you have. We cannot use PHM to address the needs of the whole population in one go.

Step one: is to prioritise, use data analysis or community stories to find priority areas - i.e. an area of unwarranted high cost or high demand, or unmet need or inequality of care. The wider and richer the linked system data, the more informed this decision making can be, but you need to get on with it with what you have –using your ‘best available insights’. This can be cross referenced to compare against similar practices/areas for example, fingertips data and Joint Strategic Needs Assessment (JSNA).
Step two: is the cohort. Use data analysis (stratification and impactability modelling) to identify a cohort within your priority area for whom there is the best opportunity to improve the quality, efficiency or equity of care. This may include a particular condition(s), or more likely a group of conditions or just “comorbidity” or “complex needs”, within a geographic area, a particular demographic (age, ethnicity) or those at risk of a hospital or care home admission.
Step three: use a wide lens to include the broadest range of available existing insights and include the patient’s and carer voice to understand your cohort. Seeing it from the patient/citizen side will address wider determinants of health and consider health inequalities. Use this broad view to get a clear picture of the existing resources and services.
Step four: designing. In designing a new model of care to deliver better outcomes, ask questions such as: What are the needs of the cohort? What outcomes do you need to see in order to meet these needs? What activities do you need to do to achieve the outcomes?
What resources and skills do you need to invest to do those activities?
Step five in delivering PHM is implementation: the ‘how’, ‘who’ and ‘what’ involved in making it happen. You need to ensure necessary buy-in from system leadership and stakeholder organisations for the support, co-operation and IG processes to deliver the plan. From the outset, plan how you will measure the outputs and outcomes including both care provider and patient/user feedback. Keep the process agile, adapt as you learn. Finally, Step six is about evaluation and expansion. You need to evaluate the process and the outcomes, including: Did you reach the target group? Did you achieve the intended outcomes/outputs? What worked well and what can you improve? Do you need to make any changes based on your evaluation? How can you scale up/share your plan? Trust in the process. Involve all relevant stakeholders and the patient/citizen at every stage from information gathering, planning and designing to delivery and evaluation. Make sure to combine best laid plans with pragmatic delivery.
The increasing pressure on the NHS makes it a clear necessity to do things differently if it is to endure. In the past the NHS has
worked in silos of care where success is judged by the success of the institutions within it, measured by individual organisation activity and financial balance sheets. This has resulted in perverse incentives, gaps and overlaps, and inefficient and disjointed care. Instead the health and care system needs to collectively manage and be measured by the health and wellbeing outcomes of the population being served, moving from reactive to proactive and anticipatory care, targeting care to meet the requirements of different groups and personalising care to the individual needs, which will require a cultural shift for healthcare professionals and patients. Our care system needs to rise to the challenge of ensuring that integrated care is a success. Population Health Management is key to enable the delivery of Integrated Care Systems and needs to become embedded in the day-to-day as the way we do things, to target care appropriately, effectively and efficiently. L
www.cegedim-healthcare.co.uk/ blog/clinical-advisory-board
www.linkedin.com/in/helendavies-0b490a120/
In the past the NHS has worked in silos of care where success is judged by the success of the institutions within it, measured by individual organisation activity and financial balance sheets.

Chris Bennett, head of behaviour change and engagement at Sustrans explores the pros of social prescribing and what is needed to really reap the benefits

It was recently announced that walking, wheeling and cycling have been included as part of social prescribing, within an upcoming NHS pilot due to be delivered as a year-long scheme in 11 areas throughout England.

Yet, social prescribing has existed for years as advised activity from GPs for patients to attend social activities in their community, which can range from attending classes, group meetings, as well as simply meeting friends and family.
Sustrans, the UK’s largest walking and cycling charity, is excited to welcome this, but what does this pilot aim to achieve?
The addition of active travel may seem selfevident, but research continues to show its benefits. The University of Edinburgh suggests that walking and cycling at current recommended levels can achieve risk reductions in premature mortality of 11 per cent and 10 per cent respectively.
There are obviously many benefits of active travel on health, but this is most easily achieved when incorporating the physical activity into our everyday lifestyles.
Walking and cycling reduce risk factors for diseases such as cardiovascular disease, some cancers, and Type II diabetes. According to Diabetes UK, physically active people have a 33-50 per cent lower risk of developing Type II diabetes compared to inactive people, whilst Cancer Research UK highlights that keeping active could help to prevent more than 3,000 UK cancer cases every year.
This pilot, entwining social prescribing with walking and cycling, aims to provide a boost to the overall health of patients, to the benefit of mental wellbeing and combating a range of medical conditions.
Just as Covid lockdowns decreased social occasions, opportunities for physical activity were also reduced, especially for travelling actively. With
the restrictions, we weren’t able to walk to the café at the corner of the road to buy a coffee, or to commute into work by cycle, or simply enjoy a day out shopping and seeing friends on high streets.
Cycling levels did increase during lockdown, and whilst this shows a reliance on present cycling infrastructure, there were still many who did not engage with cycling or, particularly, walking throughout the pandemic.
Car-dependency is a primary cause of inactivity in the UK, which can have hugely negative consequences for our health, our economy, and our NHS. Sustrans is therefore excited to welcome this pilot and to see the positive results enjoyed and will be supporting those looking for advice on getting started with active travel.
Currently, 27.2 per cent of adults do less than 30 minutes physical activity a week, whilst around 40 per cent of adults do less than 10 minutes brisk walking a month. This is a real risk to their physical and mental health.
The impact of reduced social and physical activity on the health and wellbeing of thousands up and down the UK was realised, with some feeling unable to revert to pre-Covid social and physical habits, to the detriment of their mental health.
From this, the Government is targeting prescribed social activities as a support to the recovery of many ailments; depression, anxiety, and many other complex mental health conditions, but notably loneliness - which is a present threat to the UK public’s health.
This is a growing issue in our communities, and health professionals have pushed for social prescribing to the point of this pilot scheme being initiated between this year and 2025.
According to the Mental Health Foundation, physical activity can be as effective as medication and counselling, whilst E
The addition of active travel may seem self- evident, but research continues to show its benefits
the NHS says regular exercise can help combat mild to moderate depression.

Many are unaware of the positive impact that in-person social activity can have on physical and mental health, just as they may not know that isolation and other severe mental health trauma are a profoundly important factor in feeling depressed, which in turn affects physical health.
An appetite for active travel
We expect this pilot will also be welcomed by a great majority of the public, as we know that opportunity for travelling actively is in great demand, as was made evident during the pandemic.
Our Paths for Everyone – Three Years On report found that 89 per cent of users felt that improving their wellbeing was a factor in using the National Cycle Network. The Network spans 12,619 miles throughout the UK, with approximately 50 per cent of people living within one mile of it, and over a third living within a 10-minute walk.
At the height of pandemic in 2020, the Network carried 4.9 million users over 764.8 million trips, showing massive public reliance on walking and cycling infrastructure. 72 per cent of users said it was their best option for transport, with 95 per cent using it for exercise.
We all know that health and community services are extremely stretched at the moment, so they need support to be able to implement this, which is where the Network is of great importance to the hopes of this pilot.
The appetite for active travel is clearly strong, but it also holds an importance essential to the UK’s social and economic development, as well for the health of ourselves and our planet.
Sustrans’ Walking and Cycling Index, showed that in 2021 walking, wheeling and cycling created £36.5 billion of economic benefit across the UK.
This research also found that physically active people take 27 per cent fewer sick days each year than their colleagues.
The base of this solution, for mental and physical health, is people travelling actively to enjoy being together.
We should also remember that physical inactivity costs the NHS up £1 billion per year, with further indirect costs calculated at a startling £8.2 billion.
What is needed to make this work?
Ultimately, humans are meant to be together. Once we were tribes and now we are communities, and we’re supposed
to be physically active on a very regular basis. This pilot and these prescriptions are to encourage the behaviour change towards more walking and cycling, which must be long-term and cannot be achieved quickly – especially as people will need support from organisations such as Sustrans to start and maintain this vital change.
If social prescribing with elements of active travel is to be effective, then UK walking, wheeling and cycling infrastructure must see continued investment and development, so the public feel safe and confident in fulfilling their GP’s advice to improve their health.
Walking, wheeling and cycling are essentially opportunities. They are opportunities to exercise, to enjoy outdoors and hopefully green spaces, to meet our neighbours, and to engage with our communities. It is all the things our very nature as humans expects us to do.
L
www.sustrans.org.uk
The appetite for active travel is clearly strong, but it also holds an importance essential to the UK’s social and economic development, as well for the health of ourselves and our planet
4C Strategies is an independent ICT consultancy specialising in technology and infrastructure projects.

The company covers all aspects of technology and infrastructure in the enterprise environment, with consultants showing demonstrable experience in helping clients to procure new technologies to meet their business requirements, providing endto-end support on ICT projects by delivering a portfolio of consultancy services to meet client requirements, from audit and strategy through to procurement, implementation and resourcing.
4C Strategies has been assisting organisations in the healthcare industry for over 20 years. Expertise covers
all aspects of IT technology and infrastructure, including: digital strategy, IT and technology strategy, data centres, servers and storage, patient data security, desktop telephony, Microsoft Teams and wide area networks.
Trevor Nelms, Director from West London Mental Health Trust, said: “4C Strategies has assisted in a range of complex ICT projects, from inception through to deployment, and demonstrated a rare ability to bring together technical expertise with business acumen and tight project management skills.”
Contact one of 4C Strategies’ qualified healthcare technology consultants today.
Tel: 01858 438938 nhs@4c.co.uk www.4c.co.uk
G-Cloud 13 which goes live at the end of November 2022.
Working alongside the NHS, DadPad has developed a package of physical and digital resources that have been specifically written for men, to give them the knowledge and practical skills necessary to support themselves, their partner, and baby, as they transition to fatherhood. At the same time, the healthcare professionals working with new dads will have the opportunity to build a full picture of the family dynamic, equipping them to give that new family unit the utmost in personalised support. Our DadPad areas in the UK use a mixture of our ‘essential guide’ DadPad and the ‘baby basics’ quick read hardcopy guidebooks to engage, empower and aid assessment of each
dad’s knowledge, skills and preparedness for fatherhood, alongside the DadPad app, which provides an accessible, personalised, safe space for dad to explore information and interact with peers and health professionals alike. With this ‘fatherhood-at-your-fingertips’ app, each dad will be empowered to take ownership of his parenting journey. At the very heart of our offer is the opportunity to learn, develop and implement strategies for new fathers, so that Integrated Care Systems can provide a ‘whole family’ approach in supporting new families to parenthood. L
FURTHER INFORMATION
www.thedadpad.co.uk

max20 (established 2001) is a specialist supplier of IT & digital skills and services to the NHS. In 2017, we created max20 Project Solutions.

max20 Project Solutions was established to provide fully outsourced IT & digital projects and highly skilled subject matter experts. Unlike max20 which continues to provide IT contract staff via the Government framework, RM6160, max20 Project Solutions conducts its public sector business via G-Cloud and DOS (Digital Outcomes & Specialists). All three frameworks are government operated by Crown Commercial Service.
The company is now the leading supplier of IT & Digital services to the NHS under G-Cloud 12 and has secured a place on
During 2021/2022, we had the opportunity to work alongside some of the top suppliers of Electronic Patient Record (EPR) systems including Altera (Allscripts), Cerner, Meditech, TPP SystmOne, SystemC and EMIS Health. Using this valuable experience, we created five EPR Support Services which cover each stage of delivery of a new EPR system. These will be officially launched in January 2023. These five services are Initiation, Implementation, Cut Over, Optimisation & Closure. We have the capability and experience to deliver all the above services either individually or collectively. L
Email ps@max20.com quoting EPR Services in the subject line.
In high-risk settings, curtains are commonly used as a ligature whilst curtain tracks are often removed and used as a weapon, creating a need for a safe alternative.
The new K2500 reducedligature curtain track is designed for areas where there is a risk of violence and ligature. The track fits flush to the wall and cannot be removed without spealised equipment, meaning it can’t be used as a weapon.
Yewdale supplies the track with two types of anti-ligature gliders as standard. The grey heavy duty gliders support a load of up to 20kg, whereas the white low weight gliders support 10kg. The standard installation uses a mixture of the two gliders,
achieving a 15kg release weight. The gliders easily slot into the curtain track during installation and can’t be removed. The curtain separates from the gliders if a downward force is exerted, preventing ligature. The smooth operation of the anti-ligature gliders ensures ease of use and reduces the chance of the curtain being pulled down due to heavy manual handling.
Reattaching the curtain to the gliders is quick and easy, making this curtain track ideal for hospitals, mental health units, prisons and other high-risk settings. L
FURTHER INFORMATION www.yewdale.co.uk
skills and services































