
















Monitor.

The new health secretary – the third this year – faced criticism almost immediately after her appointment for her views and voting record on abortion.

Then only a week later, Thérèse Coffey angered some in the health service by sending round an email urging staff to be positive and avoid using Oxford commas. There is no doubt Coffey has a lot on her plate already with Covid backlogs and staff shortages. Though she has not been in the role long, it is hoped she will get to work immediately on addressing these problems ahead of what is set to be one of the toughest winters ever for the NHS.
This issue examines the Government Property Strategy and how the NHS can save money on its estate, as well as taking a look at some of the Green Plans in place across the NHS.




We also cover the Women’s Health Strategy and look at some of the problems women face when accessing healthcare.

Finally, the technology section includes a look at the government’s Digital Health and Care Plan and an article on robotic-assisted surgery.

 Polly Jones, editor
Polly Jones, editor

EICR testing and remedials. Thermography – nonintrusive testing of the distribution boards. Our advanced camera’s will indicate any faults within the db’s as a heat source, not visual to the eye.

We supply and install quality energy saving lighting which are maintenance free and backed by our industry leading warranties. Due to our experience within this sector, we can advise and source lighting to suit any environment.


We o er a complete turnkey electrical installation service, from electrical design to a complete building installation. Our load monitoring machines can be installed nationally, these measure a sites power usage and rating.
Our skilled team will complete site surveys, including load monitoring to validate the power availability of a site. We can then supply and install the best suited electric car chargers along with any infrastructure requirements. Back-end software can be added allowing clients to manage the chargers and generate revenue.
Our highly skilled team are fully employed by TCS and further training is regularly undertaken in our inhouse training academy. We utilise the latest innovative technologies such as augmented reality glasses to reduce our carbon footprint which also improves our quality and speed of service to our clients.
Thérèse Coffey appointed health secretary; NHS Scotland announces winter plans; and Genetic testing service to provide rapid, life-saving checks for children
With a staffing crisis in the NHS, the REC looks at what Trusts and the government can do to address this problem
Crown Commercial Services launched its Permanent Recruitment 2 framework earlier this year. Health Business recaps what it’s all about
At a challenging time for the sector, Debra Gers, employment lawyer at Blake Morgan, and Jordan Cummins, health director at the CBI discuss what can be done to improve the wellbeing of staff working in health and social care
The government has recently published its Government Property Strategy, which aims to make savings by selling off government property and making government buildings more efficient. Health Business examines the strategy and how it will work in practice in the NHS

The North of England Commercial Procurement Collaborative has a freeto-access Hard FM Framework known as Estates, Maintenance and Engineering Services (Hard FM) (NOE.0289)


Gonzalo Vargas del Carpio, head of healthcare at TODD Architects looks at rehabilitation service design
All NHS Trusts now have a Green Plan, Health Business takes a look at some of them
The updated Women’s Health Strategy for England was launched in August 2022, with the previous version launched in July then withdrawn in August. HB takes a look at the strategy and talks to those working in women’s healthcare


Social prescribing offers many benefits to the NHS and its patients and has become more popular and more frequently used over recent years, HB looks at how it is being used in the health service and the benefits it offers
15&16 November 2022: Online Conference
The Medical Imaging Convention offers a comprehensive programme on the latest innovations in imaging diagnosis and treatment. Attended by hundreds of medical imaging professionals and senior management teams for 2 days of online education, innovation, and collaboration
Heriot-Watt University in Edinburgh is developing cutting-edge manufacturing techniques that may lower the cost of medical equipment and devices for the NHS, freeing up money that trusts can then invest in supporting members of staff and improving outcomes for patients. Professor Robert Thomson and Professor Duncan Hand explain
South Yorkshire Integrated Stroke Delivery Network and Yorkshire Ambulance Service tell us about their telehealthcare
The Association of British HealthTech Industries (ABHI) has launched a white paper: Robotic Assisted Surgery and New Models of Surgical Care, which sets out the case for a national multi-stakeholder strategy for Robotic Assisted Surgery to support its uptake across the NHS.
Dr Lloyd Humphreys examines the government’s Digital Health and Care Plan, which was released in June
At 07:00 BST on the 4 August 2022 – NHS IT provider, Advanced, identified they had been compromised by a ransomware attack and immediately started responding to contain the hackers. They issued a statement to address the growing concern.
For Cyber Security Month, Mike Fell, NHS Digital’s executive director of national cyber security operations laid out his top security tips for health and social care workers

With tens of thousands of dormant medical devices set to be connected to IT networks in the next 2-3 years, potentially exposing our healthcare systems to thousands of vulnerabilities, how can hospitals and healthcare settings mitigate risk to patient safety and care?


Thérèse Coffey has been appointed health secretary by new prime minister Liz Truss.
She replaces Stephen Barclay, who had been in the role for two months.
The MP for Suffolk Coastal since 2010 has previously served as work and pensions secretary, environment minister, Commons deputy leader and assistant whip.
Her appointment as health secretary has been criticised by abortion charities, due to her record on abortion rights.
When asked about her views on abortion following the US Supreme Court ruling, she said the law was not going to change in the UK, though she would prefer people not to have abortions.
She has previously voted against
extending access to abortion care and recently voted against making at-home abortion pills permanently available in England and Wales. In 2010, as a backbencher, she introduced a motion in Parliament, which called for mental health assessments for women seeking an abortion. She also voted against extending abortion rights to women in Northern Ireland.
Upon her appointment, Coffey said: “I am honoured to be asked to serve as SoS for Health and Social Care. Patients are my top priority, as we focus on ABCD - ambulances, backlogs, care, doctors and dentists.”
NHS workers took part in the Queen’s funeral last month.
May Parsons, a modern matron at University Hospital in Coventry, who delivered the first Covid vaccination, joined members of the Civilian Services Contingent, with some marching with the Queen’s coffin and others in the congregation.
Ms Parsons accepted the George Cross from the Queen in July on behalf of the health service. Volunteers from St John Ambulance also took part in the funeral procession.

Dr Henrietta Hughes, the first ever patient safety commissioner for England, began the role in September.
In her new position, Dr Hughes will be an independent point of contact for patients. The intention of the role is to use patients’ insight to help the government and healthcare system in England listen to and act on patient’s views. This will be used to promote patient safety particularly in regard to medicines and medical devices.
The patient safety commissioner can be contacted at commissioner@ patientsafetycommissioner.org.uk.




More than a thousand GP assistants are set to be recruited to practices in an attempt to free up doctors’ time to see more patients.
The GP assistants will offer more admin support, do blood pressure checks, heart rate and blood tests and arrange appointments, referrals and follow-up care for patients.
Up to 1,250 digital and transformation leads will also be recruited to improve patient access to primary care.

Each primary care network will have a digital lead, who will ensure practices are using the latest technology, offer more telephone lines and offer support with the NHS app.
Dr Amanda Doyle, national director of primary and community care, said: “Giving patients timely and convenient access to GPs and primary care is vital, especially during winter, which is why we are introducing brand new roles and giving GPs more
flexibility to create teams that best meet the needs of their local population.
“NHS staff have worked incredibly hard to deliver record numbers of GP appointments for patients, with 11 million more this year so far than the same period last year, and more than four in five people who book an appointment seen within two weeks, including two fifths who are seen on the same day.
“The introduction of GP assistants can reduce the time doctors spend on correspondence by up to 85 per cent, while also carrying out basic clinical tasks such as taking patients’ blood pressure and heart rate, meaning doctors have more time to do what they care about most –treating patients – while digital leads will help practices use the latest technology to manage demand and capacity”.


Scottish health Secretary Humza Yousaf has set out measures for the NHS over the coming months to support the health and care system over the winter.
The measures include the recruitment of 1,000 additional staff over the winter, with £8 million of funding to recruit up to 750 nurses, midwives and allied health professionals from overseas and 250 support staff across acute, primary care and mental health; £45 million for the Scottish Ambulance Service to support on-going recruitment, service development and winter planning; and £124 million to assist health and social care partnerships expand care at-home capacity.
The Social Care Staff Support Fund will also be extended to 31 March 2023, so staff receive full pay in Covid isolation.
GPs will be contacted to underline the expectation that pre-bookable appointments are available in every practice, as well as sameday, face-to-face and remote appointments.


Yousaf said: “NHS Scotland’s staffing and funding is already at historically high levels, but as we approach the winter period it is crucial that we look to maximise, and enhance where we can, the capacity of the NHS. Given the scale of the escalating cost of living crisis, combined with the continued uncertainty posed by COVID and a possible resurgence of Flu, this winter will be one of the most challenging our NHS has ever faced.
“These measures will support winter resilience across our health and care system, ensuring people get the right care they need at the right time and in the most appropriate setting. We will also expand our workforce, particularly registered nurses to assist with the expected increase in workload. We have jointly agreed a number of overarching priorities with Cosla which will help guide our services this winter. We are on course to double our virtual capacity this year and so far have avoided or saved bed days equivalent to adding a large district general hospital.
“We have published the first update on our NHS Recovery Plan which highlights just how much progress we have made in the past year, I am determined to build on this and we will report on progress annually.
“Our NHS and social care staff have shown remarkable resilience in the face of sustained pressure on services and I would like to thank them for their continued commitment and hard work. As we approach the Winter period their efforts will be vital in ensuring we deliver high quality care for the public.
“To help relieve pressure on services, people should continue to consider whether their condition is an emergency before going to A&E. Local GPs and pharmacies can be contacted during the day for non-critical care, NHS 24 is also available on 111 for nonemergencies.”
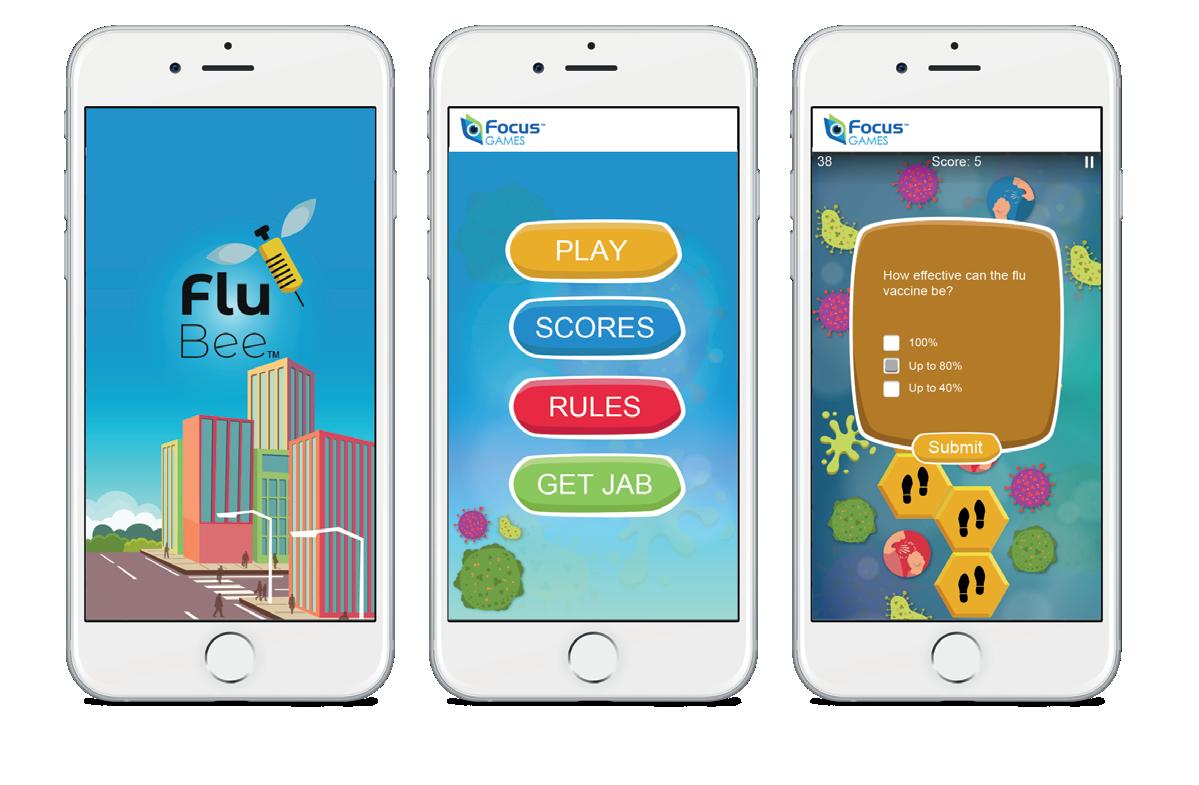
The UK Health Security Agency (UKHSA) has urged those eligible for a free flu vaccine and Covid booster to get the jabs as soon as possible.
The agency has warned that this will be a difficult winter with wide circulation of respiratory viruses.
Covid restrictions last winter meant more people worked from home and mixed a lot less, so many people were protected from flu. However, it also means there is less natural immunity in the population.

In 2021 and 2022, there was record uptake of the flu jab in people over 65. However, there was lower uptake among those in clinical risk groups and pregnant people. These groups are being particularly encouraged to come forward this year.

This year, all primary school children and some secondary school children are eligible
for the flu nasal spray. This is usually given at school. Two and three-year-olds are also being invited to GP surgeries for the nasal spray vaccination.
Covid rates are already starting to rise ahead of winter and statistics show that those who catch flu and Covid at the same time are almost twice as likely to die compared to those who only have Covid.
Dr Susan Hopkins, Chief Medical Advisor at UKHSA, said: “Flu and COVID-19 are unpredictable but there are strong indications we could be facing the threat of widely circulating flu, lower levels of natural immunity due to less exposure over the last three winters and an increase in COVID-19 circulating with lots of variants that can evade the immune response. This combination poses a serious risk to our health, particularly those in high-risk groups.
“The H3N2 flu strain can cause particularly severe illness. If you are elderly or vulnerable because of other conditions you are at greater risk, so getting the flu jab is a sensible, potentially life-saving thing to do.
“We are extremely fortunate to have vaccines against these two diseases. Most eligible groups have been selected because they are at higher risk of severe illness.
“Younger children are unlikely to have built up any natural immunity to flu and therefore it is particularly important they take the nasal spray vaccine this year. So, if you are offered a jab, please come forward to protect yourself and help reduce the burden on our health services.”
You deserve to work with a team that can help you choose when you work, at the tap of a button.
that can offer you a job searching experience that combines the power of technology, with that human touch. That is made up of specialist recruitment consultants who offer you more choice, more often.
Randstad Nursing and let us be more than just your recruiter.
career is at the heart of what we do.
We work by focusing on you: your career aims, goals, and needs. Our wide scope of experience and our large client base means that we can offer you temporary or fixed-term nursing jobs in both the NHS and private healthcare sector, nationwide and free of charge for you.

Thousands of severely ill children and babies are set to benefit from a national genetic testing service launched by the NHS.

The new service is able to rapidly process DNA samples from children and babies, who are seriously ill in hospital or are born with a rare disease. This means a diagnosis can be reached within days rather than weeks, potentially saving lives.
Children in intensive care often have to undergo several tests, the results of which take weeks to come back. With the new service, they will just need a blood test, for which the results will take days.
Whole genome sequencing works by looking for changes in genes in DNA.



The service will be based in Exeter and was launched as part of the NHS Genomics Strategy at the inaugural Genomics Healthcare Summit in London.

Amanda Pritchard, NHS chief executive, said: “This global first is an incredible moment for the NHS and will be revolutionary in helping us to rapidly diagnose the illnesses of thousands
of seriously ill children and babies — saving countless lives in the years to come.
“I have seen how these simple blood tests can change the lives of babies and their families and being able to expand this further, is wonderful for children and their families.
“When a child comes to intensive care, timing is everything, so finding the right diagnosis and treatment as quickly as possible is absolutely vital, and I am delighted that the pioneering work of the NHS’ Genomic Medicine Service is transforming the way we diagnose and treat patients in England.
“The NHS is recognised worldwide as a world leader in genomics, and this new service proves just that — it also builds on our Long Term Plan commitment to deliver the most medically advanced services possible for all our patients — boosting the life chances of thousands across the country”.
The UK Health Security Agency (UKHSA) has issued a warning to parents and guardians on the dangers of children missing routine vaccinations.
The agency has urged parents and guardians to ensure children are up to date with all routine childhood immunisations. This includes polio, and measles, mumps and rubella vaccinations.
The warning comes as recent data shows that vaccine coverage for young children decreased last year, across almost all programmes. Vaccination rates have been falling for several years, with the pandemic likely to have contributed to this.
The WHO recommends vaccination coverage of 95 per cent to prevent the spread of serious diseases such as measles and polio. However, the latest stats from UKHSA and NHS Digital show that only 89.2 per cent of two year olds had had their first MMR dose.
Dr Vanessa Saliba, consultant epidemiologist at UKHSA, said: “Measles is highly contagious and can be dangerous, and it is extremely worrying that we are seeing levels of uptake of the MMR vaccine falling among young children. It is also vitally important that children get their polio vaccinations to help prevent the risk of paralysis.
“I would urge parents to check that all children are up to date with their vaccines, and if not to get them booked in as soon as possible to make sure they have maximum protection against what can be terrible diseases.
“Childhood vaccines also boost population immunity levels, helping prevent outbreaks, so by taking up all vaccinations for our children, we play our part in keeping these diseases confined to the past.”
Local authorities are set to receive funding for research into health inequalities in their local area.
£50 million is being invested to improve health outcomes across the country.
13 local authorities will receive the funding, which will be used to set up Health Determinants Research Collaborations (HDRCs) with experts and academics addressing knowledge gaps in local areas.
The areas set to receive funding include Tower Hamlets Council, Newcastle City Council, Doncaster Council, Aberdeen City Council, City of Bradford Metropolitan District Council, Plymouth City Council, Gateshead Council, Blackpool Council, Coventry City Council, Middlesbrough Council and Redcar & Cleveland Council, The London Borough of Lambeth, Medway Council and Islington Council.
Research will be conducted into the local challenges affecting people’s health in areas such as childhood obesity, Covid recovery, mental wellbeing and drug use.
The funding is part of the government’s Plan for Patients which aims to support people to stay well and in the community with the intention to ease pressure on health and care services.
This is the first time local authorities will receive funding for research into health disparities.
Minister of State for Health, Robert Jenrick, said: “The pandemic shone a light on the stark health inequalities that exist across the country – we are committed to levelling up the health of the nation.
“This funding will drive progress to address health challenges locally, particularly in the places and communities most affected by ill health such as high
levels of obesity, drug use and poor mental health.
“Everyone should be able to live long, healthy lives regardless of their background and where they live, and this new research will help us deliver on our ambition.”
Professor Jim McManus, President of the UK Association of Directors of Public Health, said: “We know that health inequalities are one of the major barriers facing communities the length and breadth of the country, especially for disadvantaged groups and areas.
“HDRCs will help drive the research culture within local government, building on the local knowledge that authorities already have and enable what is being done to be more readily researched and evaluated to make a difference to local people.
UKHSA warns parents about dangers of missing vaccines

Designed with infection control in mind, Vepps Hygen is a rigid and stable system that’s impervious to water and easy to clean and maintain. Its seamless design, manufactured from one piece of Solid Grade Laminate (SGL), has flush-fitting hinged and lockable access doors that minimise dirt traps. It’s a simple, easy-click wall system with concealed fixing channels for a quick yet sturdy, long-lasting installation. From basins and WCs to scrub-up troughs and showers, we’re proud to now offer more than 120 variations as well as multi-panel units to choose from when writing your healthcare specifications.


our team to discuss your healthcare project requirements.

In June, more than 100,000 patients were seen by their high-street pharmacist, an increase of more than four-fifths on June 2021.
118,123 people were treated for minor illnesses including sore throat or constipation, after calling NHS 111 or their GP practice.
NHS England has also announced expanded roles for community pharmacies ahead of winter. NHS 111 online will now be able to directly refer people to high street pharmacist for a same-day consultation, instead of patients needing to call the phone line.
Amanda Pritchard, NHS chief executive, said: “Our local pharmacies ensure hundreds

Scottish First Minister Nicola Sturgeon has announced that new Rapid Cancer Diagnostic Services will be established in NHS Lanarkshire and NHS Borders.

£600,000 of funding will support the new services, with the aim of getting faster cancer diagnoses through a fast-track primary care route for patients with non-specific symptoms, including weight loss, fatigue and nausea.
There are already three Rapid Cancer Diagnostic Services in NHS Ayrshire & Arran, Fife, and Dumfries & Galloway, which were established in Spring 2021.
A new pathway will be established which aims for patients to receive an outcome within 21 days of referral.
Sturgeon said: “The best chance of surviving cancer remains early detection and treatment.
Over the past year, we have established three new rapid cancer diagnostic services - in Ayrshire & Arran, Dumfries & Galloway and Fife. They have already supported hundreds of patients.
“More than one in seven of people referred to a fast track service were found to have cancer. Around half of them were from the poorest parts of the country - so these services are helping tackle health inequality too.
“I’m delighted to confirm today that two more services will open next year - one in the Borders and one in Lanarkshire. And by the end of this Parliament there will be a Rapid Cancer Diagnostic Service in every heath board in Scotland.”
of thousands of people every week get the support and medication they need and today’s figures show that in just one month, over 100,000 patients have also had consultations with their local pharmacist for minor illnesses – this means patients are getting the care they need quickly but also in a convenient way that can fit in with their busy lives.
“We are committed to making access to NHS services as easy as possible for our patients –from this week, people can be referred for a consultation with their local pharmacy through the touch of a button through NHS 111 online and from tomorrow, a new pilot will mean
people can register for a local GP practice online within minutes.




“It is likely that we will face a busy and challenging winter and while we have already announced plans to boost capacity across our services, I am delighted that hardworking pharmacy teams are playing an even greater role.
“It is vital that the public continue to use the NHS as they normally would if they are unwell so people should continue to use NHS 111 and as ever if it is life-threatening, call 999”.
Bowel cancer home testing in Wales is to be available to more people as the screening age is lowered to 55.
As a result, 172,000 people will have access to at-home kits that test for the early stages of bowel cancer.
It is intended for the screening age to be lowered to 50 by October 2024.
From 5th October, those aged 55-57 will be invited for screening and will receive kits in the post. The screening will be rolled out to the newly eligible over the next year.
The use of at-home testing kits has improved the screening rate to 65 per cent.
Minister for health and social services, Eluned Morgan said: “It is great to see the next phase of our plan to widen access to bowel cancer screening come into effect.
“We have previously introduced the more user-friendly test and started inviting those aged 58-59. This next phase of the programme widens access to those aged 55-57.
“This move will help us to identify more bowel cancer cases early and support improvement in survival rates.
“I’m also pleased to see that more people are taking part in the programme and that the uptake rate now meets the expected standard.
“In future, we plan to continue to optimise the programme by lowering the age range to 50 and increasing the sensitivity of the test until we come into line with UK recommendations.”
Genevieve Edwards, chief executive at Bowel Cancer UK says: “This is a step in the right direction towards screening from 50 in Wales, which we’ve long campaigned for. Screening is one of the best ways to diagnose bowel cancer early, or in some cases prevent it from developing in the first place, and so inviting more people to take part is welcomed.
“Offering the home test to more people is just one of the ways to improve bowel screening, however, the biggest barrier to improving early diagnosis, and offering a world-class screening programme, is the long-standing workforce shortage in endoscopy and pathology services. We now urgently need to address this through a comprehensive workforce plan that can support the bowel cancer screening programme in Wales to achieve its full potential.”
Saloon style doorfor wider openings

Only 9mm thick
Fibreglass coated, giving a durable finish


Crib 7 fire rating and waterproof Fire-resistant and Biosafe
Load release magnets stitched and welded into the hinge
SafeArt
Lightweight, soft and flexible Fire-resistant and Biosafe
Load release magnets stitched into anti-tamper pockets Swap which SafeArt is displayed on each mounting plate
sizes available

According to a report for MPs, women should be invited for a menopause check-up when they turn 45.
The report follows a year-long inquiry. The Menopause All-Party Parliamentary Group heard women’s experiences, such as difficulties getting a diagnosis and accessing hormonereplacement therapy (HRT), as well as long waits. Some were also offered antidepressants which is against guidelines.
The group calls for action to improve the situation for those going through menopause and others affected by it, such as families, friends and colleagues.
The report recommends a health check for all women in their mid-40s, as this should ensure they get the necessary support and care as early as possible.
Also mentioned in the report, is a socioeconomic divide, with people missing out in the


postcode lottery and not having the financial ability to get treatment elsewhere.
Carolyn Harris MP, chair of the group, said: “We are beginning to feel the tide of change but the taboo around the menopause still prevails in all corners of society – in workplaces, within families and among friends, in education, and in the medical profession. Access to HRT remains a postcode lottery for women in the UK and there is a stark divide between those who can afford to seek treatment elsewhere, and those who cannot.
“The consequences for those suffering with menopause symptoms who can’t get the right treatment can be severe – leading to the break down of personal relationships and jeopardising careers, with women being forced to take additional days off or leave work all together, putting their financial situations at risk.

“Whilst the development of a Women’s
Health Strategy was an opportunity to revolutionise access to menopause support and treatment for all, in its current form it has failed to address the multiple issues that women in the UK are facing. Change is vital and we urge the new Minister and Government to give the menopause the attention it is due and take forward the recommendations in our report for the sake of women across the country.”
importance of confidence and support when quitting.
Jordan said: “I consider myself a confident person in most areas of my life, but have always faltered with smoking, so thought I wouldn’t be able to quit. I smoked for 27 years. My quitting journey has shown me that I am more capable than I thought, thanks to the support of my own family and friends and the professional help I sought.
“Quitting smoking can improve your health, quality of life and save you money. I am so glad I took this step and had the chance to speak to the brilliant experts to give myself and others the confidence that quitting smoking, even if you’ve been smoking for decades, is possible.
This year’s Stoptober campaign has been launched in England, with the aim to empower people to give up smoking during October.
Smoking is currently the single biggest cause of preventable illness and death in England, with the latest statistics showing smoking costs the NHS £2.4 billion a year. Smoking is known to cause at least 15 types of cancer.
Smoking rates have declined, though there are still six million adults in England who still smoke. It is believed smoking costs society around £17 billion a year.
Stoptober provides free quitting tools, including the NHS Quit Smoking app, online communities and daily emails and texts. An online Personal Quit Plan is also available, alongside advice on stop smoking aids and vaping, and expert support from local Stop Smoking Services.
This is Stoptober’s eleventh year and statistics show that people are five times more likely to quit for good if they complete 28 days smoke free.
Research shows that most smokers want to stop and more than a third have tried to quit in the last year.

Research has shown that self-confidence is an important factor in successful attempts to quit, with the focus of this year’s campaign on encouraging people to take steps to build their confidences and get support from friends and family as well as professional help.
As part of this year’s campaign, a film featuring ex-Strictly Coming Dancing professional James Jordan has been released. During the film, he talks about his quitting journey, after smoking for 27 years. He also talks to NHS psychiatrist Max Pemberton, who is also a former smoker, and stop smoking professional Louise Ross about the
Emeritus Professor Behaviour Scientist at UCL Prof. Robert West said: “What is really interesting is just how much of an impact self-efficacy, that sense of self-belief and confidence, has on quitting success. That confidence is something we can really help to influence. It really does show the power of the mind – self-belief when combined with other quitting aids such as vapes or NRT effectively equip people in giving up.
“What people considering quitting this Stoptober should also bear in mind is that even if you’ve tried to quit before and not managed it, that doesn’t mean it won’t work this time. You will have learnt something from your previous attempts: think of each quit attempt as a stepping stone to becoming smoke free for life.”

The Out-patient Antimicrobial Therapy (OPAT) has saved 45,000 hospital bed stays over the last year and is now set to be rolled out further across Scotland.
The new service enables people to be treated at home or in out-patient settings and reduces the need for hospital admission and long stays.
Intravenous antimicrobial therapy and other complex antibiotic treatment will be available to patients in out-patient clinics at a convenient time. In some cases, these treatments will be available at home.

The service is part of the right care in the right place initiative along with other programmes which aim to reduce pressures on the rest of the system.
Scottish cabinet secretary for health and social care Humza Yousaf said: “I am pleased to see the roll-out of the Out-patient Antimicrobial Therapy service. We know that our accident and emergency departments continue to be under significant pressure, and that is why we are working at pace to deliver this scheme, and others like it, to provide more care in the community while reducing pressure on hospitals.
“We know there is a real benefit to treating people at home where possible. We are determined to build on this success and want to see this approach adopted across as many health boards as possible.”
Dr Andrew Seaton, chair of the scottish antimicrobial prescribing group and consultant
in infectious diseases, said: “Hospitals are under significant pressure as we try to recover from the effects of the COVID pandemic and there is a real need for initiatives to support recovery and promote different ways of caring for our patients traditionally managed in hospitals.
“OPAT is an excellent example of how nurses, pharmacists and doctors can work together to provide high quality patient centred care without the need for a hospital bed. The focus now on further developing virtual capacity and new ways of working with support across Scotland for initiatives like ours is very welcome”.
Giant inflatable lungs and specialist teams of volunteers are to tour England’s lung cancer hotspots with the hope of catching more cancers early.
The Let’s Talk Lung Cancer Roadshow is being run in collaboration with the Roy Castle Lung Cancer Foundation.
The 12-foot-high lungs are expected to reach thousands of people in supermarkets, shopping centres and high streets across the UK.
People will be urged straightaway to check if they have any signs or symptoms.
Visitors can step inside the lungs and learn about lung structure, lung health and the effects of smoking.
Community engagement teams and volunteers will be talking to the public and encouraging people with symptoms to visit their GP.
The roadshow will visit 26 locations including Blackpool, Sunderland, Bradford, Dudley and London. Data shows that these areas have significantly higher rates of lung cancer.
In a recent survey, only 55 per cent of those surveyed said they would contact their GP if they had a cough for three weeks or more, though this is a key symptom of lung cancer.
The number of people being treated for lung cancer is now back at pre-pandemic levels, as is the number of people coming forward for lung cancer checks.
NHS National cancer director, Dame Cally Palmer, said: “A life-saving diagnosis can begin with a simple conversation, and the NHS is doing everything it can to bring lung cancer to the forefront of people’s minds.
“Our targeted campaigns have been extremely successful in the past, catching hundreds of cancers early in communities which traditionally are less likely to come forward for checks. This novel scheme will no doubt raise eyebrows, but it will also raise awareness of early cancer detection, ultimately meaning better chance of successful treatment for those coming forward.
“So if you have had a persistent cough for three weeks or more, feel aches or pains when breathing or coughing, or show any of the other symptoms of lung cancer, help us help you and please come forward for care.”
The website provides five questions, when they are answered, people can get a personalised Mind Plan, which gives them tips to deal with stress and anxiety, boost their mood, and sleep better.

The Office for Health Improvement and Disparites (OHID) has launched a Better HealthEvery Mind Matters campaign urging the public to “be kind to your mind”.
The campaign coincides with World Mental Health Day on Monday 10 October.
Research commissioned by OHID shows that 70 per cent of the UK report regularly experiencing the “Sunday Scaries”.
The campaign calls on the public to do small things to make a big difference to their wellbeing. It also provides free tips and advice.
Secretary of state for halth and social care, Thérèse Coffey, said: “My focus is on making sure people can get the care they need, when they need it - and that includes for their mental wellbeing.
“The Every Mind Matters tool is a great way to build your mental resilience and help ward off the anxiety many of us feel on a Sunday.”
The campaign is backed by BBC Radio 1 host Vick Hope, TV personality Scarlett Moffatt and pop star Tom Grennan, as well as leading psychologist Kimberley Wilson.
Psychologist, Kimberley Wilson, said: “Many people experience a feeling of heightened anticipatory anxiety on a Sunday, otherwise



known as the ‘Sunday Scaries’. Often when people feel sad or anxious, they spend time trying to distract themselves, by binge watching TV or spending hours scrolling on social media, for example. But these ‘distraction’ habits can actually exacerbate the problem.
“It’s so important to enjoy every last minute of your weekend and start the week in the best frame of mind. So, if you experience the Sunday Scaries like clockwork every week or feel sad or anxious, try getting active, which can help you to burn off nervous energy, writing down or keeping a diary of what you are doing and how you feel at different times to help identify what’s causing anxiety and what you need to do to help manage it. Small things can make a big difference to our mental wellbeing.”


With a staffing crisis in the NHS, the REC looks at what Trusts and the government can do to address this problem
“The greatest workforce crisis in the history of the NHS and social care.”
This is how the Health and Social Care Select Committee’s report on workforce described the current staffing situation in the sector. And the Recruitment and Employment Confederation (REC) agrees. We have a large number of long-serving, experienced and dedicated recruiters who have been working with medical professionals, NHS Trusts, local authorities and care home providers for decades. They all say that the level of staff shortages we are seeing now is very alarming..
The numbers support this too. As of September 2021, there were 99,460 vacancies in the NHS and a further 105,000 vacancies in social care. What’s even more worrying is the industry’s future. Research says that almost a million more healthcare workers are needed by the early 2030s due to the growing demand for services. This is striking. The question on many lips is – where is the future workforce strategy?
To help think this through for this sector and others, the REC has published a new report Overcoming Shortages – How to create a sustainable labour market. The report finds that not addressing labour shortages across the economy could cost the UK economy £39 billion a year. To put into context, the total cost of NHS staff in 2019/2020 was £56.1 billion. Included in the report are a set of recommendations for governments and businesses to deal with labour and skills shortages. Central for all is putting the people at the heart of the agenda. For governments and policy makers they should create specific home within the Cabinet Office or with an independent commission for creating a future workforce strategy. This builds on from the REC’s call for governments and departments to deliver a long-term workforce planning. We are glad that there is now more talk of doing this for the health and social care sector but we must see action too.
“People stuff” Employers also need to play their part, by putting the “people
stuff” first and meet the needs of their workforce. Employers need to engage their workforce to improve working conditions and give tailored workplace support. This means many things, from flexible working arrangements to mental health support. In August 2021 alone, the NHS lost half a million full-time equivalent days due to mental health issues. The staff burnout and resilience in healthcare is not a new issue, hence the Health and Social Care Select Committee’s 66-page report on the issue.
What we are hearing on the ground backs this up. Recruiters tell us the main reason NHS workers are leaving their permanent posts is the lack of flexibility and worklife-balance. Flexibility at workplaces is becoming increasingly important. But this is even more distinct in the healthcare sector where flexibility isn’t always guaranteed. More needs to be done on this and Trusts must look at how to improve the working conditions for frontline workers.
Working via agencies or bank is a popular alternative. But to create a more sustainable labour market, Trusts and care home providers need to borrow the insights, experience and expertise of agencies who are already successfully responding to workers’ asks. This important collaboration will help more permanent frontline staff enjoy a similar level of flexibility. Equality, diversity and inclusion (ED&I) should also be at the core of any people plan. There has been abundant evidence on how a more diverse workforce is a more productive and more efficient workforce. According to the NHS Workforce Statistics 2020, 22.1 per cent of NHS staff were from ethnic monitory background. This is within the context of a 15.2 per cent non-white population across England and Wales. However, only 55.5 per cent of NHS staff feel that there are equal opportunities for all. 7.8 per cent of NHS staff said that they have experienced discrimination in the last 12 months from patients or members of the public while 9.1 per cent said they had such experience from colleagues. This is a distressing truth about ED&I at the heart of the NHS. No colleague should ever go through negative experiences based on their ethnic background – especially within a sector where international recruitment is active.
International recruitment Speaking on international recruitment, the REC urges government to have policies
is industry’sthe
around immigration that stimulate growth and allows access to medical talent from abroad. While we fully support homegrown talent strategies, we need an immigration system that meets the labour market needs of the UK and supports the growth and innovation that the sector seeks to deliver well for patients.
The costs, the bureaucracy and the duration of the visa process are frequently cited as challenges for both workers and employers. But not being able to bring extended family members (such as parents) and uncertainty of their future career at the end of the first visa also play a big part. This goes further for care workers and care assistants who have been added to the Shortages Occupation List on a temporary basis. Workers need greater certainty and job security before they pick up their lives and start over across seas. For these social care roles in particular, the minimum salary requirement is also a huge blocker. The immigration point is one for policy makers. But without the pressure from employers and the industry, we are less likely to achieve changes.
Another key point around overcoming shortages in healthcare is the need to view skills as an investment, not a cost. Increasing investment and funding is critical and necessary for growth, progress and innovation. Governments must think about how to support added funding for training for medical professionals while employers think about how to provide adequate and equal
opportunities to train for both permanent and temporary staff. People still need to pay their bills and put food on the table when they go back to training. So, in-work training and adequate financial assistance is important. Not all recommendations from our Overcoming Shortages report are short-term and most require a series of discussions and actions from more than one party including governments. But staff shortages in the industry are bringing some services to breaking point. More and more workers are leaving their permanent jobs and often leaving the industry all together. Agencies are here, in many cases as a safety net, catching the leavers – who would have otherwise left the industry all together – and bringing them back in.
There are plenty of examples where agencies are providing tailored, individual support with a focus on ensuring the optimal working arrangement for each worker. Some agencies have a robust staff engagement strategy and NHS Trusts and care home providers should be doing the same.
What’s important for the industry is a genuine partnership and collaboration where agencies’ expertise and technology meet employers’ resource and hiring needs. Achieving this true partnership model is a critical step in the right direction to manage staff shortages, where the industry can strategically marry the strength that both permanent and temporary staff placements have to offer to support our healthcare system.
About the REC
The REC is the voice of the recruitment industry, speaking up for great recruiters. We drive standards and empower recruitment businesses to build better futures for great candidates and themselves. We are champions of an industry which is fundamental to the strength of the UK economy. L
Find out more about the Recruitment & Employment Confederation at www.rec.uk.com.
What’s important for the industry is a genuine partnership and collaboration where agencies’ expertise and technology meet employers’ resource and hiring needs
Our proven methodology encompasses seamless, workflow driven candidate acquisition strategies that deliver the right talent, quickly and effectively, wherever it is needed.

Design and execute overseas marketing campaigns to develop skilled talent pools.
Screening every candidate from our UK Head Office ensuring eligibility for the role & sponsorship. We do not use land based agents.
Support candidates through their visa application - handholding them throughout the process.


Coordinate travel arrangements for candidates helping them book flights and confirm arrival dates.

Collect candidates from the airport and provide transport to their new place of work.



Source suitable accommodation for candidates, local to their place of work, ensuring no modern slavery concerns.

Crown Commercial Services launched its Permanent Recruitment 2 framework earlier this year. Health Business recaps what it’s all about
Crown Commercial Services (CCS)’ Permanent Recruitment 2 framework enables all public sector organisations to access recruitment services to hire permanent, fixed-term and internal secondment roles through recruitment agencies. Organisations are able to access general recruitment services to search for and hire candidates for a specific role or job. The framework applies to England, Scotland, Wales and Northern Ireland.
The framework will also provide a way to hire clinical roles through the general recruitment service.
The new framework replaces the current Permanent Recruitment Solutions framework which is due to expire in November 2022.
Recruiters will compete to find a suitable candidate and will only get paid if they successfully fill the role – general recruitment is a non-exclusive contingency model service. The recruitment agencies will help public sector organisations to recruit one or more candidates for clinical and non-clinical roles.
Suppliers need not be able to provide on a national basis, but should be able to provide recruitment services in and outside of London and the south east, as well as where civil service and public servants are located throughout the UK – this is not restricted to large cities. The Supplier Capability Matrix provides information on the locations that suppliers are able to provide services for. All suppliers are able to attend virtual meetings.
The new framework will provide access to individual candidate placements for clinical and non-clinical roles. Services are available in a modular format if required. The framework is not to be used for hiring temporary labour. This should be done through other CCS agreements.
The Permanent Recruitment 2 framework is part of the Workforce Alliance portfolio, which provides an additional access route to the framework for the NHS. A partnership between CCS and NHS Procurement in Partnership, the Workforce Alliance brings together a range of procurement and commercial expertise
with the intention of benefitting the NHS.
The Workforce Alliance claims: “Nobody is better placed to help you meet the challenges of NHS staffing. As a team of health workforce experts, we are motivated by a genuine desire to make the NHS better. You can trust us to act in the best interests of the NHS – always putting patient care first.”
The core services of the Permanent Recruitment 2 framework include search services, to allow organisations to find applicants, tools for the evaluation of applicants and the ability to appoint an applicant to the role.
Non-core services of the Permanent Recruitment 2 framework include services for strategy and planning to help organisations plan for recruitment gaps and help them ensure they have the right people with the right skills. This is essential at the moment, with employers struggling to fill roles and a well-documented digital skills gap Non-core services of the framework also include services for talent development with the intention of helping organisations develop a talent pool of potential applicants with the needed skillset. Public sector organisations will be able to access all core and non-core services and will have the flexibility to choose which services to add to their call offs. The new agreement will run for two years and has the option to extend for up to two years if necessary. Under the agreement, there is no maximum length for a call off contract, though CCS is recommending that it should not be any longer than four years.
CCS has listed a number of potential benefits of the new framework. One such benefit is that hiring managers and departments have the ability to choose who they engage with from the supplier list and how they do this. With 157 suppliers listed,


organisations will have a large choice.
CCS has also claimed that those hiring will be able to access capable suppliers, leading to increased fill rates. This will also avoid repeated campaign costs.
The ability to direct award could save organisations time and money, by avoiding a long and costly recruitment process.
Capped maximum costs are intended to protect contracting authorities from market price increases. This is important with the current inflation rate and the cost-of-living crisis.
The framework also boasts no hidden costs as everything is included in the cost of the service. This includes methods of attracting candidates including social media, digital campaigns and job boards. This also includes the cost of travel, subsistence and lodging; document or report reproduction; shipping; desktop or office equipment costs; network or data interchange costs or other telecommunications charges; and costs incurred prior to the commencement of any call-off contract.
As suppliers are obliged to work towards civil service diversity and inclusion requirements, contracting authorities should, as a result, be further on the way to achieving their own diversity and inclusion requirements.
Listed suppliers must also develop an employer value proposition (EVP) to ensure candidates want to work for the contracting authority’s organisation. An EVP includes any benefits that the candidate will receive for their work, including pay, learning and development opportunities and the culture of the organisation.
The framework also includes discounts for hiring more than one supplier. Finally, the framework provides a compliant route to candidates for permanent roles via recruitment agencies. The terms and conditions will also stay consistent. For those looking to hire on a permanent basis, the Permanent Recruitment 2 framework is the place to start. L
Further information on the framework is available on the Crown Commercial Services website
The willframework also providea way to hire clinicalroles through thegeneralservicerecruitment






At a challenging time for the sector, Debra Gers, employment lawyer at Blake Morgan, and Jordan Cummins, health director at the CBI discuss what can be done to improve the wellbeing of staff working in health and social care
There’s no question that the last few years have led to unprecedented pressure on the health and social care sector, with the Covid-19 pandemic and its residual effects, and now the cost-ofliving crisis creating fresh challenges.

One area which has been adversely affected is the physical and mental wellbeing of those working in the NHS and wider health and social care organisations. The backlog of appointments, on-going demand for services, and staff shortages has added extra pressure to an already squeezed workforce, which has had little to no respite following an intense few years.
Many are suffering from unprecedented levels of poor mental health, including
stress, anxiety, depression and PTSD, and organisations are experiencing higher volumes of sickness absence. With the cost-of-living crisis deepening, financial concerns are also rising. Improving the wellbeing of those working within the sector has never been more important.
The health and social care sector must put this at the centre of its value proposition and work to improve job design and satisfaction to protect the workforce from ongoing challenges.
The NHS has a strategy for improving the wellbeing of its staff, and is investing in initiatives including supporting the new Integrated
Care Systems to develop and pilot locallyowned health and wellbeing offers for their workforce. Other organisations and businesses across the sector need to follow suit and make proactive investment in the wellbeing of workers.


Long working hours and high workload has been a challenge in the sector for many years, leading to burnout for staff. Reducing these this is an obvious first step. While a longer-term approach is needed to combat the strain on resources, there are structural changes which can be implemented now to ease pressures on individual staff members. These include creating better shift patterns to give employees greater flexibility, ensuring better training, and putting E
One areawhich has beenadversely affectedis the physical andmental wellbeingof those workingin the NHS

We provide a variety of furnishings including lounge chairs, high back armchairs and more which are great for a wide range of users.


With our wide range of styles and colours we can help you create the right atmosphere for your care home without compromising on comfort or safety and all our upholstered furniture is available in a range of easy to clean and hygienic fabrics or faux leathers

Please browse to see our full range or contact our sales team to discuss your requirements further

All healthcare chair orders placed before 30th Nov 2022*

Rosehill’s bestselling The Hamilton Patient & Visitor Chairs are a high quality and durable choice for your ward or waiting room. The chairs have a profiled seat for maximum comfort and an ergonomically designed back rest with a removable seat to help for easy cleaning. Optional extras include wheels, variable seat depth cushions to ensure the correct posture for multi-patient use, armpads and filled in sides.

in place initiatives such as shared workloads to ensure those on the frontline do not feel unnecessary burdens.
Organisations should also prioritise mid-level management, putting more people in these positions and giving them the training needed to ease the pressure on more junior workers.
For employees who are experiencing poor mental health, creating a more open culture where staff feel able to talk about their concerns is crucial, and support is key.

The NHS’s People Plan, the workforce strategy for delivering its Long Term Plan, sets out the ambition for every staff member to have regular conversations focused on health and wellbeing with their line manager, including discussion of flexible working requirements and matters related to equality, diversity and inclusion. The NHS has also set up 40 staff mental health and wellbeing confidential hubs to provide colleagues with free-of-charge rapid access to assessment and local evidence-based mental health services and support, such as talking therapy and counselling.
Across wider organisations, mid-level management should be trained to better spot the signs of poor mental health and be able to proactively address these, and guidance should be given to individual staff members on how and where to ask for help. Employers may wish to refer to the measures set out in guidance from the Covid Trauma Response Working Group which, while
designed to support early-stage responses to the pandemic, also apply to the longer-term effects of the crisis, and new challenges too.
Where possible, health and social care organisations should also implement homebased and remote working to ensure a better work-life balance, although it must be noted that for some, remote working can have an adverse impact on their mental wellbeing because of increased feelings of loneliness.
Smaller measures should also be put in place to improve the day-to-day lives of employees. Research from the Nuffield Trust has coined this ‘hygiene factors’ and includes ensuring employees have access to amenities such as rest areas and car parking, as well as the correct equipment. These can help to mitigate problems in the short-term, easing overall pressure on the workforce.
It is also important that leaders foster an inclusive, compassionate and cooperate environment which creates a sense of belonging among employees, making them feel valued and giving them a sense they have a stake in their work. This is
particularly effective in the health and social care sector, where workers are motivated by a sense of public service.
With the cost-of-living crisis deepening, financial concerns are increasing for much of the workforce, particularly those on lower wages. The sector must consider how it can adapt for this challenging period, and introduce measures which support employees. These could include subsidised meals at work, tax-free vouchers for rising bills, or even loans for public transport.
Improving – and maintaining – staff wellbeing is a priority, but there is no magic fix. The onus should be on continued investment into these initiatives over a longer period. L
Debra Gers and Jordan Cummins will be discussing the challenge of workplace wellbeing within the health and social care sector as part of the upcoming Future Health Conference which is being run by Blake Morgan and taking place in November.
https://www.blakemorgan.co.uk/ future-health-conference/
It is also important that leaders foster an inclusive, compassionate and cooperate environment which creates a sense of belonging among employees, making them feel valued and giving them a sense they have a stake in their work.
By monitoring procedure-level costing. Proper inventory management solutions gives NHS organisations valuable insights into procedures’ tariff-to-cost ratios, costly procedures, the impact of different medical equipment on procedure delivery costs, time spent on procedures and resource allocation.


How NHS trusts help ease the growing cost pressures and financial crises affecting the NHS?
The NHS has been dealing with funding challenges for more than a decade now, and experts predict more funding crises will continue and get worse over the foreseeable future. A 2020 report by the BBC reveals that we spent more than £156 billion on the NHS in 2019 – approximately 12 times more than we spent 70 years ago. Notably, healthcare costs are rising, increasing the size of the NHS budget, with an average increase of 1.4 per cent per year from 2009 to 2019
professionals. Besides making cost-efficient items and equipment available, NHS organisations should also recommend that healthcare professionals use them instead of cost-inefficient alternatives, reducing cost pressures and increasing cost benefits.
In this article, we will discuss how NHS organisations’ inefficiency when tracking procedure-level and patient-level costing makes NHS trusts incur avoidable financial losses. We will also propose an efficient and practical solution: utilising inventory management to track and manage costs.

Many NHS organisations don’t understand procedure-level costing
Unfortunately, many NHS organisations don’t know how much they spend on delivering healthcare procedures such as surgery. Some organisations unnecessarily spend more on a procedure than others because of adopting inefficient policies and practices or using inefficient healthcare equipment.
NHS organisations’ inefficiency when tracking and determining procedure delivery costs results in avoidable financial losses for their respective trusts. NHS trusts pay a fixed tariff for every procedure delivered. However, the inability to track costs means that trusts could be losing money on every procedure, adding to the cost pressure and funding crises.
Fortunately, NHS trusts can help ease the growing cost pressures and financial crises affecting the NHS by monitoring and managing procedure-level costing. Proper inventory management is one of the best ways to do this, as it can give NHS organisations valuable insights into the following factors.
The tariff-to-cost ratio refers to a comparison
of the tariff paid and the cost incurred for each procedure. Proper inventory management can provide valuable insights into which procedures cost less to deliver than the tariff paid, enabling NHS trusts to capitalise on them.
Some procedures cause unavoidable cost pressures, essentially making cost-control solutions useless. Fortunately, proper inventory management can also help NHS organisations identify procedures that are simply a cost pressure and manage them accordingly, such as allocating more tariffs or reducing the number of procedure deliveries.
Surgeons and other healthcare professionals can choose to use varying interchangeable medical equipment and items to conduct their procedures. Variations in the type of equipment and items used can mean that some surgeons spend more on procedure delivery than others, essentially causing cost pressures.
Fortunately, there is a simple solution to this problem: providing healthcare professionals with cost-efficient medical equipment and items.
Facilitating constructive discussions around procurement and product rationalisation can help convert cost pressures into cost benefits. Product rationalisation entails identifying and eliminating items that negatively impact the organisation’s strategic goals, such as reducing costs and losses.
The goal is to identify cost-effective items and make them available to healthcare
Time spent on procedures Ideally, NHS healthcare facilities should attend to patients within four hours of arrival. Unfortunately, the summer of 2015 is the last time that the NHS in England met this target – many patients wait considerably longer than four hours to get seen in most NHS hospitals, adding to the organisation’s inefficiencies and cost pressures. Proper inventory tracking can enable NHS organisations to measure the amount of time spent on delivering different procedure types. It can also enable reviews on why some surgeons spend more time on procedure delivery than others.
NHS organisations can then use these insights to facilitate the sharing of knowledge of time-efficient practices between surgeons, reducing procedure delivery times for all surgeons and procedure types. Ultimately, this can help reduce patient waiting times to reduce cost pressures and improve throughput rates to create more cost benefits.
As explained, proper inventory management can help NHS organisations determine different procedure types’ tariff-to-cost ratios. The organisations can then use these insights to make informed decisions on how and where to allocate resources for larger positive cost impacts. A more prudent resource allocation plan can enable organisations to reduce waiting times and increase procedure through put while reducing the potential burden of costs over budget sizes.
Proper inventory management can help NHS organisations reduce cost pressures and increase cost benefits for procedure deliveries.
The Scan4Safety program is based on GS1 standards and can help improve inventory management and supply chain management.

The government has recently published its Government Property Strategy, which aims to make savings by selling off government property and making government buildings more efficient. Health Business examines the strategy and how it will work in practice in the NHS
The pandemic has highlighted the need for buildings to be flexible, with lockdowns leading to more people working from home and social distancing and health requirements meaning buildings need to be adaptable. NHS buildings were already ahead of the rest of the public sector with regards to infection control and cleaning, though the pandemic highlighted the need for this to be as easy and manageable as possible.
The recent heatwave and drought have demonstrated the impact of global warming and underlined the need to cut carbon emissions – with such a large estate, the NHS is well placed to make big savings. The heatwave highlighted the need for temperature control in hospitals, with

buildings designed to be cooler, money can be saved in air conditioning, for example, and patients will be more comfortable and have improved health outcomes.
Furthermore, the cost-ofliving and energy crisis has highlighted the need for the NHS to make savings to free up funds to spend elsewhere.

Published at the end of August, the Government Property Strategy is expected to save the government more
than £2 billion through property sales and efficiencies. Though the strategy applies to the public sector as a whole and is at this stage, quite general, it does also apply to the NHS.
The government estate is made up of hundreds of thousands of properties which includes hospitals, administrative offices, and much more. The NHS alone has around 130,000 buildings covering a combined floor space of around 42 billion square feet.
The Government Property Strategy has an “achievements” section which shows the changes already made by the government including reducing the size of the central general purpose estate by 30 per cent since 2010 and reducing emissions by 57 per cent in 2020-2021 compared to 2009-10. An estimated 38 per cent of this reduction is due to improved management of the estate.

Launching the strategy, Jacob Rees-Mogg, then-minister for brexit opportunities and government efficiency said: “The public estate is a singular resource, with a significant impact. Its location, cost and effectiveness all have a direct relationship to the quality of public services and contribute to communities and places, driving economic growth throughout the UK.”
Part of the strategy includes selling £1.5 billion worth of E
With such alarge estate, theNHS is well placedto make savingsbig



i n m a i n t e n a n c e , s e r v i c e a n d i n s t a l l a t i o n o f H e a t i n g V e n t i l a t i o n a n d A i r C o n d i t i o n i n g s y s t e m s i n :
• H e a l t h c a r e • S c h o o l s • O f f i c e s • H o t e l s a n d h o s p i t a l i t y • C r i t i c a l e n v i r o n m e n t s
E c o m e c h a s b e e n n a m e d a s a s u p p l i e r o n N H S S h a r e d B u s i n e s s S e r v i c e s ' H a r d F a c i l i t i e s M a n a g e m e n t f r a m e w o r k a g r e e m e n t f o r L o t 5 . 1 V e n t i l a t i o n a n d A i r C o n d i t i o n i n g
H O U S E T E A M O F M O B I L E E N G I N E E R S L O C A T E D I N L O N D O N , S O U T H E A S T A N D
O U T H E R N E N G L A N D
government property assets over the next three years. However, it seems this goal is less achievable for the NHS than for other public sector organisations, who may have more unused space.
The plan also intends to make £500 million of savings by reducing operating costs, cutting spend on leases, and using modern building materials and energy sources. With its net zero ambitions, the NHS is already ahead in many of these areas. With such a large estate and workforce, the NHS is in an excellent place to make these savings and lead the way in the public sector on reducing operating costs.
The Government Property Strategy has three missions. Mission One is to transform places and services. Mission Two is to create a smaller, better and greener public estate. Mission Three is to improve professional excellence and insight.
Mission One is to transform places and services and commits to maximise on opportunities to exit from properties or colocate services within existing properties. Though as previously mentioned, this goal is better met by other public sector organisations, such as central and local government, rather than the NHS which does need a lot of space to operate effectively and provide appropriate care. Virtual ward trials are currently running, meaning people can be treated at home rather than in hospital wards and this could be one area where the NHS can make space and building savings.
The One Public Estate programme brings public sector partners together to make the best use of public sector land and property in order to deliver efficiencies, local economic growth and more integrated customer services. Over three years, the programme is expected to make over £400 million capital receipts, £80 million running cost savings and provide land for over 10,000 homes and around 30,000 jobs.
The mission also intends to improve access and interoperability across the public sector to enable space to be shared between services and organisation. Some administrative and management organisations within the NHS could potentially co-locate in office spaces with other local public sector organisations, which could save property costs.
Mission One also includes a commitment to invest £300 million in locally led grant funding, including the Brownfield Land Release Fund, which aims to unlock smaller brownfield sites across England for housing through the One Public Estate (OPE) programme.
The mission also commits to embed flexibility in estate design and construction to future proof the public estate. This includes uncertainty about future requirements being built into design for new buildings, for example through specification of flexible space which can be used for multiple purposes, through separation of shell and core from fit out or design to allow expansion and contraction without complex redesign. We don’t know what the NHS will need in 10, 20 or even 50 years, though the buildings should still be fit for purpose at this time.

Unforeseen events, such as pandemics and extreme weather events could happen and NHS property needs to be ready for this and fit for purpose. Heatwaves are only going to become more frequent and we need to ensure that the NHS can continue to work at full capacity during these times. The recent shutdown of Guy’s and St Thomas’ during the heatwave highlights this. This means that services and technology in particular, need to be able to run and the temperature inside NHS facilities needs to be manageable for
staff and comfortable and safe for patients. Success in Mission One will be measured against the Places for Growth targets, by looking at the property footprint in each region and by assessing the cost savings.
Mission Two is to create a smaller, better and greener estate. The aim is for a smaller, more flexible estate, which reflects the requirements of modern public services. The estate should be more flexible and adaptable to meet E
Part of the strategy includes selling £1.5 billion worth of government property assets over the next three years


changing demands and needs for property.
Mission Two commits to making £500 million of cumulative resource savings from the operating costs of the government estate.
To reduce the size of the estate, organisations will take a whole portfolio view of their assets and look at the potential value to other government priorities from repurposing or disposal. Costly, poor-quality properties should be prioritised for disposal.
A pipeline of disposals will be developed, which aims to generate gross capital receipts of £500m per annum, to fund investment in the estate which is to be kept.
For the estate to be fit for purpose and in a good condition to meet the needs of a modern Health Service, organisations will develop accessible and responsive spaces which enable delivery of flexible and inclusive services in supportive workplaces,
enabled by FM professionals with the required skills and capabilities, who are supported by effective standards, tools, technology and organisation.

The strategy commits to improve the quality of estates across a number of departments including hospitals.
Feedback will be collected from customers on the quality of public buildings and this will be acted on. Quality and condition will be embedded
in budget prioritisation and property investment decisions. This means patients will be able to provide their feedback on NHS properties and facilities, and trusts will listen to this and make changes where possible.
Mission Two also commits to deliver the Greening Government Commitments E
Unforeseen events, such as pandemics and extreme weather events could happen and NHS property needs to be ready for this and fit for purpose
HTM 06-01
and











Power Control
CPC
Agreement
emergency power
other healthcare
maintenance services.
and 25 Year Environment Plan goals on net zero, adaptation, natural capital and resource efficiency.
The Greening Government Commitments set out actions that UK government departments and their agencies will take to reduce their impact on the environment from 2021 to 2025. These include targets for reducing water consumption, reducing greenhouse gas emissions and minimising waste and promoting resource efficiency.
To make the estate greener, an adaptation framework will be developed and embedded to enable consistent high standards in development and use of Adaptation Risk Assessment and Action Plan methodologies. Biodiversity and natural capital guidance will be developed and embedded for estate teams, including guidance to maximise the impact of interventions in constrained urban sites. Sustainability requirements and standards for the whole lifecycle of the property will be built upon, from procurement, to construction to end of life.
The KPIs of Mission Two will be the size and annual running cost, capital value, land disposed, exits from central London offices, utilisation targets; resource savings and capital release; estate condition and customer satisfaction.
Success will also be measured against Greening Government Commitments.
Organisations should develop property strategies setting objectives that take into account their individual business drivers and that are informed by the principles of the Strategy. Where property asset types are used by multiple organisations, portfolio strategies will be developed, setting objectives that take into account future cross-government demand, condition, sustainability and affordability for each asset class. These portfolio strategies should be in place by March 2023.
The NHS is already leading the way in the public sector with regards to reducing emissions and greening the estate, with every NHS Trust now having a green plan in place and an aspiration to be the world’s first net zero health service by 2040. This ambition includes reduced emissions from services, buildings and vehicles by 80 per cent compared to a 1990 baseline by 2030. 212 trusts have a green plan, accounting for more than 1,000 hospitals and
healthcare facilities. It is hoped these plans will save more than 1 million tonnes of carbon over three years – the equivalent of taking 520,000 cars of the road. These plans will also help improve patient care and reduce costs and waste.

The NHS accounts for around 40 per cent of public sector emissions, so the NHS is in a good position to make a big difference. As well as this, nine in ten NHS staff support a net zero NHS, seeing the benefits it brings to the organisation, patients’ health and the impact it can have on the wider environment.
The NHS Delivering a ‘Net Zero’ National Health Service report identifies a core carbon footprint as well as a ‘NHS Carbon Footprint Plus’. The core footprint includes emissions from NHS facilities including fuel used for heating, electricity use, water consumption, waste management and treatment, medical gases and fuel used in fleet vehicles. NHS success stories in net zero include a solar-powered “field of dreams” in Hull, E

Feedback will be collected from customers on the quality of public buildings and this will be acted on








which is able to provide enough power to meet the entire daytime needs of Castle Hill hospital. This is saving Hull University Teaching Hospitals Trust between £250,000 and £300,000 a month. It is hoped other trusts will be able to make similar changes, to contribute to net zero, as well as reducing operating costs. With the cost of energy so high at the moment, installing solar panels on the property and using this energy across the site is a great way to save money, as well as help the environment.
Dr Nick Watts, chief sustainability officer of the NHS, recently wrote about the NHS’s net zero ambitions for Health Business Magazine. He said: “I was fortunate enough to visit Manchester University NHS Foundation Trust Hospital recently to meet

some of the staff behind their ambitious green plan. I was humbled by the passion and commitment of people like Frank, who works on the adult stroke rehabilitation unit. Frank has poured his heart into creating a green space that benefits both patients and the environment. I was inspired by the drive and commitment of consultant anaethetist Cliff, who is championing greener care at Wythenshaw Hospital because of the benefits it brings his patients.
“With the announcement of 212 NHS green plans, there is no doubt that the NHS has signed sealed and is on the way to delivering the world’s first net zero health service.”

Speaking about the Government Property Strategy, Rees-Mogg said:
“We will transform the public estate to enable the updating of public services. The public estate has the potential to be at the vanguard of improving society, through helping to make our streets safer, supporting the NHS and educating children and adults.”
With the NHS having such a large property portfolio, it is in a great position to make a real difference to public sector spending on property and at the same time reduce carbon emissions. However, the NHS is already leading the way in the public sector in financial and carbon savings with several innovative projects and trials already underway with Green Plans across every single NHS trust. The NHS can be used as an example for other public sector organisations to follow to see how they can also make property and emission savings. L
Further information on KPIs, relevant departments and organisations within the government and related property programmes is available on the gov.uk website.

With the cost of energy so high at the moment, installing solar panels on the property and using this energy across the site is a great way to save money, as well as help the environment
There are unique challenges and considerations that go into carrying out work for healthcare contract clients. Everything from the site induction to waste disposal has to be carefully planned and accurately executed. Client expectations are always very high, timescales are usually very tight, and contractors work is highly visible
After many years and thousands of successful contracts working in healthcare, Novus knows that these types of contracts are very different from your run-of-the-mill property maintenance or refurbishments. Firstly, an extremely comprehensive site induction is always needed due to the complexity of the site and the work involved. Uniquely, certain areas within healthcare settings are no-go areas due to biological hazards, radiation hazards, asbestos etc. These areas require either separate inductions and/or special permits to work. Site inductions within healthcare environments also need to include any specific details regarding the work area with emphasis that we are always working within a live environment and potentially near patients in-situ. Some of those patients may be seriously ill and each team member must be mindful and considerate of this at all times.
One of Novus’ overarching considerations in healthcare settings is the need to ensure dignity and compassion is demonstrated as much as possible. Any works within a live environment will, by nature, impact on the day-to-day running of that department/ ward. Our job is to minimise this impact. Dialogue with the ward manager, confirming what works are being undertaken, is vital as often what is planned by others doesn’t necessarily suit what the ward is looking for. Extensive planning and preparation are required when carrying out hot works or potentially dusty works. Control measures may be required to isolate or change fire detection which then requires permits, thorough communication etc.
Novus operatives may have to adopt the hospital’s fire and emergency procedures for each specific department if the works are not in isolated construction areas. Areas of work need to be kept clean at all times to ensure there will be no build-up of rubbish and that fire escapes from the surrounding buildings are clear at all times. We take a flexible approach when planning and are also aware that as we are working in a live environment, works sometimes have to be delayed or even postponed due to the needs of the patients and staff. Most hospitals operate a permit-to-work system with specific lead-in times before tasks can be undertaken. This needs to be factored in when programming works. Notifications of works also need to be in place to ensure the wider hospital trust staff and relevant departments are aware. This again can impact a programme if not planned effectively. Electrical and mechanical isolations on general construction sites can be easily managed. On sites such as a hospital however, accidently turning off power within certain areas could potentially cause massive disruption - especially considering surgical departments and areas where expensive medical equipment may be running, which may not be covered by essential supplies. Extreme care must be taken in the planning stage prior to any electrical isolations.
Logistics and waste disposal requirements are also different in healthcare settings. The roads around hospitals are constantly busy with private, commercial and public transport, and the management of waste
disposal and deliveries to the site areas need to be planned, authorised, and carried out in a safe manner and in accordance with the infection control requirements. In addition, traffic management needs to ensure that the primary function or operational requirements of the hospital are not disturbed. Novus aims to minimise the dust generated during construction activity and prevent dust infiltration into adjacent patient areas. Housekeeping whilst working in live environments is key. We mustn’t lose site of the fact that not only can we carry infection onto wards, but we can also pick up infection whilst on the wards and potentially pass this on to work colleagues and family members. On a typical construction/refurbishment project, the workforce normally come into contact with people or situations they see on a day-to-day basis. In healthcare however, the workforce may enter some areas such as children’s wards, palliative care wards, end of life wards, A&E etc. where they may encounter distressing scenes which can upset even seasoned healthcare staff. This kind of information needs to be communicated, managed and monitored regularly to address any issues. We have established relationships working with some of the largest names within the healthcare sector. Our extensive experience includes longstanding Measured Term Contracts with many of the country’s largest NHS Trusts, and we are a member of several healthcare frameworks. To learn more about how Novus’ dedicated healthcare service can deliver your property’s needs, visit our website. L
The North of England Commercial Procurement Collaborative has a free-to-access Hard FM Framework known as Estates, Maintenance and Engineering Services (Hard FM) (NOE.0289)
NHS North of England Commercial Procurement Collaborative (NOE CPC) is wholly owned by the NHS and provides collaborative and bespoke procurement solutions for the NHS and other public sector organisations. Through category expertise and harnessing its collective buying power, NOE CPC aims to deliver comprehensive, compliant and innovative procurement solutions which save the NHS money.
The framework enables contracting authorities to procure specialist services such as asbestos removal, air conditioning, electrical works, fire risk assessments and water system maintenance and has been designed to help NHS trusts and public sector organisations successfully manage their estate requirements.
The framework enables users to address maintenance backlogs and set up Planned Preventative Maintenance (PPM) programmes to reduce the breakdown of equipment and increase operational efficiencies.

Developed for the NHS
It has been specifically developed for the NHS and the healthcare sector’s FM requirements, utilising input and expertise from NHS stakeholders, so the needs of the NHS have been taken into account.
The framework offers an efficient, FTScompliant process. A detailed procurement exercise has been carried out, ensuring that suppliers meet all legislative requirements; suppliers are prequalified, which saves valuable time and money in the procurement process.
NOE CPC’s procurement team meets regularly with suppliers to ensure that the products and services they provide are compliant with its policies and
guidelines. These meetings also enable the sharing of knowledge, expertise and market innovation and offer the opportunity to look for further ways to improve collaboration for the benefit of the customers.
The framework offers several other benefits including a fully managed service, which offers the option to award one supplier to perform all services offered within the scope of the Framework Agreement or two or more services.
Direct Award is a key component of the framework, meaning Participating Authorities have the ability to choose in certain circumstances to award to a specific supplier from within the agreement, without going through a long procurement process, provided this is in accordance with the procurement regulations.
The framework has a Measured Terms Contract (MTC) option available for reactive and planned maintenance of buildings, and electrical and mechanical works.
Pricing is capped during the framework, to support budgeting and calculation of benefits realised by Participating Authorities. Mini-competitions can be undertaken to meet the bespoke
requirement of each customer and are encouraged to support the delivery of best value to participating authorities.
The framework offers a mix of suppliers including large national providers, as well as a number of regional SMEs currently utilised by the NHS to be more reactive to local needs.
The agreement offers NHS organisations the option of using locally based suppliers with demonstratable experience of working in the healthcare environment and membership of professional bodies.
Bradford Teaching Hospitals used the framework to appoint a provider under Lot 12 for fire risk assessments.
Wendy Stanley, estates administrator at Bradford Teaching Hospitals NHS Foundation Trust, said: “I would definitely recommend NOE CPC to other trusts. They have always provided a reliable service and the teams are very knowledgeable about their categories.
They are always available to support us with any issues we encounter and guidance on procurement matters and we have benefitted hugely from working with NOE CPC.”
The NHS has one of the largest property portfolios of any organisation in the world. In England alone, it owns more than 130,000 buildings with a combined floor space of approximately 42 billion sq ft. The maintenance backlog is a growing problem for all public service organisations
In the NHS, it’s estimated that there is a £5 billion shortfall in maintenance spending across trusts and primary care sites. These facilities are continuing to age and new challenges have been created by the emergence of digital technology. The maintenance and estate issues that are plagued by the NHS are not unique to the organisation as many buildings across the public estate are facing similar challenges.
The NHS Estates Strategy is the centrepiece of NHS England’s approach to facilities management and the operation of the estate. The strategy outlines the role of the NHS in the delivery of its buildings and infrastructure, and how the different partners work together. The strategy, which is implemented across England, is a response to the challenges posed to the NHS by the rising number of people, the ageing population, and the growth in digital technology. The government recently announced their 2022-2030 property strategy which looks at how to create a more efficient, effective, and sustainable public estate. The strategy outlined three missions including: transforming places and services, a smaller, better and greener public estate and improving professional excellence and insight. Both strategies are designed to support an NHS and public estate that is fit for the future, and to be the blueprint for how organisations will operate their estate.
Smart Buildings refer to buildings that are designed, built, operated and connected in order to reduce the cost of operations, minimise the risk of disruption, and lower carbon emissions. NHS England has been working with the Department of Health and Social Care, the NHS Trust Development Authority, NHS Improvement, the Health and Safety Executive and others to develop the NHS Smart Building Framework. This is a set of objectives that will be used to drive forward the transformation of the health estate into smarter buildings that will deliver these benefits. The framework will be used to assess and award buildings that are designed to meet the highest standards in terms of performance, health, safety and sustainability. These will then be used as a model for the
transformation of the health estate. The framework includes a set of 25 health, safety, and sustainability outcomes for buildings, 10 service delivery objectives, and five design and construction objectives. Smart Buildings are not only being trialled at the NHS but across the public sector, the Crown Commercial Service, a strategic partner at Smart 2022, has dedicated Smart solutions frameworks to help organisations make the transition.
Sustainable design and construction – as well as operation, maintenance, and decommissioning – is at the heart of the NHS estates strategy. It is important, as this will ensure that assets are fit for the future with a longer lifecycle, as well as reduce the energy required to provide the same level of services. Healthcare facilities are complex and interdependent environments, and they need to be designed and managed according to the specific needs of the healthcare setting. However, it is important to understand that sustainable design is not merely an aesthetic choice. Sustainable design practices are a means of reducing costs and improving efficiency and performance, whilst also reducing the environmental impact of NHS facilities. The adoption of sustainable design and building practices can be expected to have a significant impact on the maintenance backlog, as well as future performance, operations, and sustainability of NHS facilities.
Whilst sustainable design will directly impact upon the maintenance backlog, the emergence of digital technology heralds a new wave of challenges and opportunities in NHS Facilities Management. As the NHS has already committed to reducing the amount of CO2 produced by its activities, it is therefore developing strategies and targets of how it will reduce the amount of electricity it uses. One of the key methods to reduce the amount of electricity being used is by increasing the energy efficiency of the buildings that house vital equipment and assets. For example, the rise of smart meters in electrical infrastructure has
created new opportunities to improve energy efficiency. As a large institution, the NHS is uniquely positioned to demonstrate leadership on this issue. It can show the rest of the world how to reduce the amount of CO2 produced by electricity and set an example of how important it is to reduce our dependence on fossil fuels. Another conversation that spans across the entire public sector is the use of PropTech and how this can aid with property performance to reduce costs and reach sustainability targets. It can help with analysis for smarter decisions and modernising property management. This engaging conversation at Smart 2022 will feature Christopher King of NHS Property Services, to share not only what the NHS is doing, but understand what else is available and already utilised across other sectors.
CAD/CIM - Computer Aided Design and Computer Aided Manufacturing are essential tools for developing and managing the design process of a building. It allows engineers to design the building in a virtual environment and identify and address any potential issues with the building before construction begins. This will ensure that the finished building will be fit for purpose and meet the specific requirements of the health service with regards to design, functionality, and energy efficiency.
BIM - Building Information Modelling is another key tool for managing and

maintaining the estate. BIM can be used to manage all aspects of the design, supply chain, construction, commissioning, and lifecycle of the building. It will also enable better collaboration, as all the stakeholders can share the same information about the building online and use the tools available to check and amend the information.
The adoption of digital technology in NHS facilities and across the public sector will require careful management, as the integration of innovative technologies can be challenging, and responsible interoperability is essential. However, the adoption of digital technology in facilities management offers a significant opportunity to improve efficiency, reduce costs and create better working environments for staff.
In addition to managing the backlog of maintenance work, the NHS and other public sector organisations also have a significant challenge in recruiting enough staff to manage the high-level operational requirements of the estate. This is particularly true in relation to facilities management. NHS England recently published a 10-year plan to accelerate the transformation of the facilities management function across the health estate. The 10-year plan aims to increase the number of facilities managers in the NHS from 10,000 to 25,000. This will be achieved through a combination of recruiting new staff, changing working practices and increasing productivity.
The NHS estates strategy is designed to address the challenges posed to the NHS by the rising number of people, the ageing population, and the growth in digital technology. The NHS Long Term Plan sets out its strategy for managing and investing in the health estate over the next 10 to 15 years. The NHS is not alone in feeling the pressures in estate and facilities management, asset and estate managers across the entire public sector are facing challenging goals and pressures to meet targets and decrease backlogs. At Smart Estates we feature a stream looking at the facilities management backlog, where you can gain
cross-government department learnings. Our panellists will discuss ways of improving efficiency, building a more productive workforce, and ‘building back better’.
Learn more about the NHS Estate and the Public Estate at the Smart Asset & Estate Management Conference on 8th December at the prestigious QEII Centre, London. Smart 2022 is the ideal place for all public sector property professionals to get the latest policy updates and discover new initiatives around estate management, sustainable buildings, smarter working, and the technology that enables them. The conference boasts an agenda packed with case studies, expert insight and inspiring practical takeaways that will help you accelerate change.

Our interactive session formats enable you to network with likeminded peers, share resources and rethink estates
& property management in the digital age. Speakers confirmed include Christopher King, NHS Open Space Lead and Principal Strategic Asset Manager at NHS Property Services; Mark Chivers, Government Chief Property Officer at Office for Government Property; Louisa LeRoux, Net Zero Programme Manager at Government Property Agency; Angela Harrowing, Deputy Director, Property Programme at the Cabinet Office; Dr Janet Young, Government Head of Property Profession at Office of Government Property. Tickets are available now, public sector members
an exclusive 30% discount, using
register your place today.
In
health and social care secretary
Rt Hon Matt Hancock,
the launch of the Health Infrastructure Plan
regeneration plan of more than 40 hospital building projects to transform
NHS
of the plan
infrastructure for the NHS
With a vision to develop a more modern and efficient NHS infrastructure, part of the HIP plan included a new hospital building programme – a £2.8 billion investment, later increased to £3.7 billion, apportioned to a selection of hospitals to transform estates and facilities.
One area of focus centres on the digitisation of building infrastructure to enable greater management of the estate, but to make this viable for all, processes and build plans need to be standardised in order to drive development. One way this can be supported is by the implementation of GS1 Global Location Numbers (GLNs).
GLNs enable the unique identification of any locations across the NHS estate. These include locations from the highest level, such as whole NHS organisations, down to lower levels such as a ward, bed bay, or even a particular shelf.
A GLN is more than just a number. It is the data that is the key, and this is where the advantages are gleaned.
The benefits of implementing GLNs are three-fold: easier differentiation between locations, greater traceability of products and assets, and improved patient management.
By attributing these unique identifiers to every location it becomes easier to distinguish separate organisations within an Integrated Care System (ICS) from one another, or to better identify individual sites that make up an NHS trust.
One, this will enable vital medical equipment to be tracked directly to storage locations or points of use to allow for more efficient resource planning and asset management, preventing delays to patient care. Equipment can then be located quickly and sourced for use as and when needed, ensuring it is in the right place, at the right time, every time, and two, patient management.
With an appropriate patient identifier (such as a GS1 barcoded patient wristband) in place, GLNs can be used to help to

monitor a patient’s movement throughout a site. Doing so would provide an accurate picture of where a particular patient has been – particularly important for infection prevention and minimising spread. Sites that are at risk can be swiftly identified and appropriate measures taken to minimise risks to patients and staff.
In context, Leeds Teaching Hospitals NHS Trust has more than 26,000 rooms which have been updated with a GLN locator. These are added into their property register (or estates management system) with each GLN allocated so they can be managed and tracked centrally. The GLN information is then shared via the national NHS GLN registry, LocationManager so details can be communicated with suppliers to manage deliveries into goods in bays.
The trust has also implemented GLN extensions to scan to bed level, in order to understand where patient beds are. The GLN extensions are printed onto plaques and allocated to each bed space.
The GS1 patient wristband is scanned to positively identify the patient before the wall plaque is scanned to capture the location information. It is then updated in the electronic patient record (EPR). This updates the patient administration system (PAS) and the ward’s electronic whiteboard so staff can efficiently track where the patient has been. During the pandemic, this had particular benefits when it came to infection monitoring and prevention.
If a patient moves beds, or is transferred to another ward or location, it updates in real time each time the new GLN is scanned. This makes it much easier to identify which beds are occupied to facilitate bed allocation planning and speeds up the transfer process preventing any delay to patient care.
During the pandemic, the visibility of available inventory and assets across NHS estates heightened the wider system’s traceability challenges. Many trusts found difficulty tracking where vital products or equipment were located. However, for those using GS1 standards, this process became simpler.
For University Hospitals Plymouth NHS Trust, using GS1 standards was instrumental in helping to manage supplies and resources during the pandemic –supplies of personal protective equipment (PPE), and the supply of consumables required on the intensive care unit.
to develop a
Head of supply chain and e-procurement, Peter Sewell explains, “We receive an item, we scan it in, and then as we consume it we scan it out. We can look at how much PPE we’ve got, how much we’ve used, and how many days’ worth of stock we’ve got left. We went from 35 ICU beds to 250, so we created 10 extra ICU locations. But because we had an ICU that was already barcoded, we just replicated that in all those other 10 locations.”
Senior IM&T procurement manager and lead for Scan4Safety at the trust, Richard Price, added, “Using GS1 standards has given us the visibility we needed over our stock and our equipment. This has made a real difference throughout the pandemic so we can spend less time looking for items and counting stock, and more time where it is needed most.”
Making GLNs a critical part of NHS infrastructure has the potential to drastically improve both efficiency and patient safety. Not only do they streamline purchase to pay (P2P) processes to make procurement more efficient for all stakeholders, when used in tandem with unique product identifiers such as GS1 Global Trade Item Numbers (GTINs), they also facilitate e-procurement to ensure the right products are available whenever and wherever they are needed. Products can then be seamlessly tracked and traced from the point of manufacture or supply, through to the appropriate delivery location, point of care, or point of use to enable end-to-end product traceability. Staff can quickly and easily scan GLN barcodes to track where products are delivered to or where care is administered. This enables them to manage their inventory far more efficiently, saving time and money, while developing a clearer picture of the patient pathway. The ability to identify every location across NHS trusts provides certainty, not only regarding what was delivered and where, but also in the identification and removal of recalled products and the truth of who did what to who – when, where and why. L

Whilst a fundamental element of the acute care pathway, rehabilitation has found itself undeservedly neglected as part of the healthcare system, often undervalued and living in the shadow of other higher profile and immediate life-saving treatments. However, addressing unmet rehabilitation needs is fast becoming a recognised global priority. According to a 2017 research paper on the Global Need for Physical Rehabilitation, aging populations and the high survival rate of people with severe health conditions has seen the physical rehabilitation needs of the global population increasing exponentially since the 1990s, even in high-level income countries.
The Covid-19 pandemic has undoubtedly added further to that demand. Whilst we await further quantifiable data on the pandemic’s impact on physical rehabilitation need, initial studies give some indication
of possible ramifications. Researchers at the University of Michigan, for instance, found the global prevalence of Long Covid in those diagnosed with the virus to be around 43 per cent and, whilst most Long Covid symptoms are treatable and selfmanaged at home, it is clear that many more patients may require rehabilitation for ongoing physical, psychological, and cognitive difficulties following infection.
It’s not only the increased numbers of patients requiring treatment, but also the disruption to existing rehabilitation services and the impact it may have on frontline healthcare systems further down the line. A study published in early 2021 on cardiac rehabilitation during the COVID19 pandemic, for instance, concluded that programme suspensions and access for high-risk patients to these services might have an impact on longterm hospital admissions. It’s true that continuing pressure from rehabilitation charities
and professionals on the importance of rehabilitation has seen some progress made in recent years, particularly following the World Health Organizations’ Rehabilitation 2030 call for action. We have also seen Governments commit to a number of highprofile, landmark developments such as the National Rehabilitation Hospital (NRH) in Dublin and the recently green-lit National Rehabilitation Centre at Stanford Hall in Nottinghamshire which will combine clinical rehabilitation, R&D, training and education under one roof. However, a more coordinated approach for the rehabilitation of people with long-term conditions is required, particularly at a local level.
Further research on the impact of Covid-19 on diverse rehabilitation programs is required for the appropriate planning of resources, services and facilities for rehabilitation. This is especially important now, post pandemic, before planning decisions around health service recovery and resilience get locked in and opportunities to optimise the delivery of rehabilitation are lost.
Throughout Europe, many governments are planning to address the backlogs built up during the pandemic and tackle long waits for care by building dozens more community diagnostic centres to expand capacity for checks, scans and treatments. However, there is not much discussion on rehabilitation, or mental health provision for that matter.
The latter is important because physical rehabilitation is often accompanied by mental health issues. Yet towards the end of last year, NHS England estimated that a staggering 1.6 million people were waiting for treatment from mental health services, with the Royal College of Psychiatrists warning that the unprecedented impact of the pandemic will wipe out years of hard-won progress in mental health unless there is sustained investment. E
However, addressing unmet rehabilitation needsis fast becoming arecognisedpriorityglobal
would have been like without technology to underpin the vaccines?
Today, though, we’re facing up to a different kind of storm. Much like Covid, no one is totally immune to cost of living increases and a looming recession. And of course it’s not just individuals and families affected.

Businesses, too – including those in private healthcare – are grappling with increased risk and challenges. With firms and individuals poised to reduce spending, even if your business has a full order book, it is probable that this won’t last. It pays, then, to not only be fully tapped into every digital opportunity but also to have a diversified customer base. And this means targeting public sector tenders.
How can private healthcare businesses navigate economic turbulence?
Sandy Boxall investigates
I just used my phone to order up a repeat prescription. It’s the sort of action that was unthinkable even a decade ago but is now so commonplace it barely merits mentioning.
Thanks to the relentless tide of digital advances, patients no longer have to rely on traditional routes to healthcare – thank goodness. Can you imagine what the pandemic

Although media reports suggest that the chancellor is hunting for spending cuts, the government sector nonetheless enjoys some big advantages.
For example, its budgets are committed for the future, sometimes for years in advance, and it cannot go bankrupt. Government must also pay on time – with plenty of avenues available to complain if for some reason it doesn’t.
And it’s also important to remember that much government spending is non-
discretionary. It is going to happen – regardless of external pressures – regardless of the political stripe of the incumbent administration.
That all said, it’s important to remember switching to public sector tenders won’t address every economic challenge in one fell swoop.
Companies need to continue to prioritise digital business while understanding that public sector work doesn’t happen overnight. Suppliers need to invest in the market, build relationships, and bid for the right tender and win it. First time entrants should look to make a minimum three to six month commitment. This means that now is the time to begin pivoting your business – there’s no time to waste. If you need any advice, Contract Finder Pro is here to help. Don’t hesitate to get in touch. L
Sandy Boxall is director of Contract Finder Pro.
Of course, remote technology will have a role to play in the future of rehabilitation programme provision and, as the authors of the above report on cardiac rehabilitation found, the rapid adoption of technology into standard practice has improved services provision and patient access. However, the research also highlights issues regarding limited uptake of technology by patients over 65, safety concerns and reduced patient experience due to lack of social interaction. It is clear, therefore, that whilst technology can assist, it is not a solution in its own right. It is well understood that rehabilitation should commence as soon as possible, requiring access to services in a timely manner to provide early intervention. Given that physical rehabilitation should also be accompanied by counselling, an integrated care system needs to be promoted where co-location of services closer to the community can speed up the journey through diagnosis, physical and mental
treatment and rehabilitation. Co-location of services can also allow critical care, acute medical and specialist rehabilitation teams to work closely together to develop better rehabilitation pathways for patients.
This is particualry important in rural or semi-remote urban locations, where the colocation of healthcare services can maximise resources, improve the patient pathway and address health inequalities. Commonly referred to as Health and Well Being Centres or Community Treatment and Care Centres, these ‘one-stop shop’ facilities typically include GPs, consulting and treatment suites, physiotherapy, paediatrics, dentistry, occupational and speech therapy together with social services such as homecare, primary mental health teams and outsourcing centres. The design of these environments has, at its core, ‘simple-to-access’ healthcare making it easier for patients to get tests closer to home and reducing the number of visits by delivering multiple tests and consultations in a single appointment and location.
TODD Architects has been widely involved in this model of care in Northern Ireland, including the award-winning Omagh Hospital & Primary Care Complex, which includes a range of hospital and community healthcare services together in one place and was heralded as a unique and new ‘model of care’ and ‘environment for healing’. In Dublin, too, the Finglas Primary Care Centre will also co-locate physio and occupational therapy spaces with mental health services, alongside General Practitioners services.

Rehabilitation is an important part of the treatment process, reintegrating patients back to their normal lives and improving their quality of living, whilst also relieving pressure on other areas of health service provision. To deliver effective rehabilitation to the people who need it, evidence-based planning is required and co-location of services in accessible, welcoming and flexible facilities is a sensible proposition to meet the rising demand. L
Gonzalo Vargas del Carpio was the clinical design lead for the Defence and National Rehabilitation Centre (DNRC) in Loughborough.
Further information is available here
Co-location of services can also allow critical care, acute medical and specialist rehabilitation teams to work closely together to develop better rehabilitation pathways for patients








All NHS Trusts now have a Green Plan, Health Business takes a look at some of them
The NHS has the goal of becoming the first net zero health service in the world – it’s ambitious but not unachievable. A major milestone has been ticked off, with every NHS Trust now having its own Green Plan, hoping to contribute to this goal.


Devon Partnership NHS Trust has a Green Plan, which was published in January. In their foreword, they say: “Devon Partnership NHS Trust (DPT) recognises how important it is for us to make sure we are committed to sustainability in everything we do. Our Strategic Aims include: to make a positive contribution to our environment and make the best use of resources. We are committed to playing our part in Delivering a Net Zero National Health Service, recognising that, left unabated, climate change will disrupt care, with poor environmental health contributing to major diseases and economic disruption.”
DPT’s Green Plan sets out how the Trust will improve how resources are used, to cause the least harm to the environment and benefit staff and those who use the
services. The Plan includes a commitment to update it regularly in line with changes in national requirements and local experience.
The Trust also commits to further developing a culture which has sustainability at the heart.
The Leeds Teaching Hospitals NHS Trust has already reduced its carbon emissions by 33 per cent compared to 2014, with a vision to become one of the greenest NHS Trusts in the UK. The key focus areas of their Green Plan include: embedding sustainability across the Trust; making buildings more energy efficient; promoting active travel such as cycling, lift sharing and public transport; innovative approaches to care; sustainable medicines; reducing plastic use; waste management; sustainable
catering and improving biodiversity and green spaces across sites.
The Trust can boast that it is the first Carbon Literate NHS Hospital Trust and has already invested over £20 million in energy-saving projects. Furthermore, all general waste is converted into energy and none is sent to landfill.
100 per cent green renewable energy
Leeds and York NHS Foundation Trust said: “Global warming affects everyone. If we don’t take immediate action, the adverse effects of rising global temperatures will worsen, leading to the most vulnerable groups within society, who are least able to cope, being most affected.”
NHS Trusthas already reducedits carbon emissionsby 33 per comparedcent to 2014
The Trust aims to become carbon neutral by 2028 and the Green Plan was created to reduce the carbon emissions produced by the Trust.
The Plan includes a commitment to become carbon neutral and for staff to be a part of this, to sustainably recycle waste and develop environmentally efficient care services.
The Trust already sources energy for its owned and leased properties from 100 per cent green renewable energy and over 60 per cent of the fleet is electric.
Wirral University Teaching Hospital NHS Foundation Trust said: “The Trust vision is ‘Together we will deliver the best quality and safest care to the communities we serve’, an important factor in ensuring that we can deliver the safest care is recognising the responsibility that we have as a health care organisation to reduce our impact on the environment as the link between climate and the NHS ambitions in becoming the world’s first net zero national health service.” E

The foreword to the Trust’s Green Plan highlights the climate change effects that have already been felt in the region such as higher temperatures in summer and longer dry spells, wetter winters and more frequent storms and floods. Matthew Swanborough, Director of Strategy & Partnerships said: “As a coastal peninsular, it’s imperative that we work with our system partners to ensure a combined approach not only in reducing our carbon footprint, but also adapting to the changes that are already happening.”
The Green Plan commits to resource consumption and greenhouse gas emission reductions in line with NHS net zero targets. The Trust will also reduce the environmental impact of its activities and build the groundwork for becoming a climate-change-resilient organisation.
The climate emergency is a health emergency West London NHS Trust has the aspiration of becoming one of the greenest Trusts in London and even in the UK. They say: “The climate emergency is a health emergency. Climate change threatens the foundations of good health, with direct and immediate consequences for our patients, the public and the NHS. As a Trust, we recognise the enormous challenge that the issues of climate change, air pollution, flooding, extreme heat and waste present to West London and the impact that these issues have on our patients, colleagues and communities. The environment is changing and the pace of change is accelerating.”
Their plan has seven areas of action which each have a nominated lead responsible for setting, reviewing and updating the objectives. The seven areas of action are energy, transport, people, buildings, waste, investment and digital.
In the energy category, for example, is the goal to transition to low or zero carbon solutions for the provision of energy services, by reducing consumption, introducing new technology and utilising on-site generation.
Imperial College Healthcare NHS Trust said: “As one of the largest NHS trusts serving some of the poorest communities in London, we recognise the important role we have to play in helping to reduce emissions and improve sustainability overall.”

Their plan sets out how the Trust will reduce the impact of climate change on health, reduce reliance on unsustainable services and medicines and embrace green learning and innovation.
This Trust’s Green Plan has 12 green goals covering: cleaner air, reduced energy usage, smarter travel, innovative water use, better waste management,
reduced plastics, sustainable medicines, innovative care, sustainable catering, greener facilities, sustainability research and redeveloped hospitals.
Through sustainable catering, the Trust commits to a food and retail transformation programme, mapping sustainability from farm to plate. This will include reviewing supply chains, and increasing plant-based packaging and locally sourced products.
Though the above is just a brief summary of the Green Plans from only six of the 219 NHS Trusts in England, all are detailed, comprehensive and well planned. The Green Plans are a good indication of what is to come and we can look forward to the changes they implement and the benefits they bring. The plans are convincing and with patients and staff on board, the NHS is well on the way to becoming the world’s first net-zero health service.
Further information can be found
Through sustainable catering, the Trust commits to a food and retail transformation programme, mapping sustainability from farm to plate
The updated Women’s Health Strategy for England was launched in August 2022, with the previous version launched in July then withdrawn in August. HB takes a look at the strategy and talks to those working in women’s healthcare Goals


When the Women’s Health Strategy for England was launched, then secretary of state for health and social care Steve Barclay and then minister of state for health Maria Caulfield said: “This country’s health and care system belongs to us all, and it must serve us all. However, sadly, 51 per cent of the population faces obstacles when it comes to getting the care they need.
“Although women in the UK on average live longer than men, women spend a significantly greater proportion of their lives in ill health and disability when compared with men. Not enough focus is placed on women-specific issues like miscarriage or menopause, and women are under-represented when it comes to important clinical trials. This has meant that not enough is known about conditions that only affect women, or about how conditions that affect both men and women impact them in different ways.”
In the ministerial foreword, they highlighted disparities in women’s health across the country, including a smoking during pregnancy rate of 1.8 per cent in Kensington compared to 21.4 per cent in Blackpool.
They also said that women’s voices are not listened to and in the call for evidence, 84 per cent of respondents felt this was the case.
The Women’s Health Strategy for England is the first of its kind and aims to set out how to improve the way in which the health and care system listens to women’s voices and boost health outcomes for women and girls.
The Strategy has used the call for evidence, which was published last year and received almost 100,000 responses, as it base.
The Strategy covers a period of 10 years and includes commitments to improve the health of women – these include a plan to transform women’s health content on the NHS website, a definition of trauma-informed practice for the health sector and plans to increase female participation in research.
Women’s health ambassador
Professor Dame Lesley Regan has also been announced as the women’s health ambassador for England. Through this role, she will support the implementation of the strategy.
Dame Lesley said: “I am honoured to be taking up the position as the first Women’s Health Ambassador for England. Having spent my career working with and caring for women, I see this newly created role as a unique opportunity to ‘get it right’ for women and girls.
“In the 2014 chief medical officer’s annual report ‘The health of the 51 per cent: women’, we
identified the widening disparities for girls and women during their adolescent, reproductive and post-reproductive years. The issues raised then remain relevant today, and in some cases health disparities have widened and been further exaggerated by the pandemic. The Better for Women report published in 2019 by the Royal College of Obstetricians and Gynaecologists highlighted the need to adopt a life course approach, emphasising the importance of preventative health interventions, instead of focussing on the treatment of established disease.
“This first Women’s Health Strategy for England is the next step on the journey to reset the dial on women’s health. The call for evidence, which informs the ambitions of the strategy, reiterates what I hear repeatedly from women: that our healthcare systems are failing them because NHS services are not designed to meet women’s day-to-day needs.”
Dame Lesley said that her priorities will be to tackle health issues that affect most women for long periods of their lives, this includes menstruation, contraception, pregnancy, miscarriage and menopause.
Though these health issues affect trans, non-binary and other gender diverse people, only the term “women” is mentioned in the strategy.
According to the document: “While women in the UK on average live longer than men, women spend a significantly greater proportion of their lives in ill health and disability when compared with men. And while women make up 51 per cent of the population, historically the health and care system has been designed by men for men.”
This means there are gaps in data and evidence, and not enough is known about conditions that only affect people with uteruses, such as menopause and endometriosis. It also means that we don’t know enough about how conditions that affect all genders, affect different genders in different ways, such as cardiovascular disease or dementia. The Strategy has the ambition that within the next 10 years, the strategy will have boosted health outcomes for all women and girls and radically improved the way in which the health and care system engages and listens to all women and girls. This will be achieved by taking a life
51per cent ofthe facespopulation obstacleswhen it comes togetting the carethey need
course approach, focusing on women’s health policy and services throughout their lives, embedding hybrid and wrap-around services as best practice and boosting the representation of women’s voices and experiences in policy-making and at all levels of the health and care system.
The strategy has a six-point long-term plan for transformation change, which as stated in the document is as follows: “Ensuring women’s voices are heard – tackling taboos and stigmas, ensuring women are listened to by healthcare professionals, and increasing representation of women at all levels of the health and care system.
“Improving access to services – ensuring women can access services that meet their reproductive health needs across their lives, and prioritising services for women’s conditions such as endometriosis. Ensuring conditions that affect both men and women, such as autism or dementia, consider women’s needs by default, and
being clear on how conditions affect men and women differently.
“Addressing disparities in outcomes among women –ensuring that a woman’s age, ethnicity, sexuality, disability or where she is from does not impact upon her ability to access services, or the treatment she receives.
“Better information and education –enabling women and wider society to easily equip themselves with accurate information about women’s health, and healthcare professionals to have the initial and ongoing training they need to treat their patients knowledgably and empathetically.
“Greater understanding of how women’s health affects their experience in the workplace – normalising conversations on taboo topics, such as periods and the menopause, to ensure women can remain productive and be supported in the workplace, and highlighting the many examples of good practice by employers.
“Supporting more research, improving the evidence base and spearheading the drive for better data – addressing the lack of research into women’s health conditions, improving the representation of women of all demographics in research, and plugging the data gap and ensuring existing data is broken down by sex.” E
The strategy has a six-point long-term plan for transformation change
Reception
Following the launch of the Women’s Health Strategy for England and the appointment of Dame Lesley Regan as Women’s Health Ambassador, we asked those who work in women’s health or connected industries what needs to be done to tackle the gender health gap.

Bloody Good Period, a charity that campaigns for menstrual equity and provides period products to those who can’t afford them and menstrual education to those less likely to access it, said: “There is a significant gender health gap around menstruation. Rising numbers of women and people who menstruate are unable to access period products, and strong shame and stigma continue to surround this entirely normal bodily function - with huge consequences. This is entirely missed by the Women’s Health Strategy, which only discusses menstruation as it relates to medical conditions. It talks about endometriosis, fibroids, and heavy menstrual bleeding - all of which of course are vital to recognise and address. But the strategy doesn’t consider the everyday, wide-ranging impact of menstruation - on education, employment, finance, activity, inclusion and much more.
“It also fails to acknowledge the growing issue of period poverty. One in eight feel it’s likely they won’t be able to afford period products in the next year. BGP is seeing a 150
per cent higher demand for period products than this time last year. The cost-of-living crisis will only make this worse - yet period poverty is hardly mentioned in the strategy.
“For the people we work with, navigating the ever-increasing cost of period products (which have risen 57 per cent in price in recent months), as well as balancing the shame, stigma and taboo society places on menstruation, is a monthly reality. The system is rigged against those who menstruate. Without acknowledging this, we cannot hope to overcome the gender health gap.
But the strategy doesn’t consider the everyday, wide-ranging impact of menstruation - on education, employment, finance, activity, inclusion and much more
“At Bloody Good Period, we believe the following steps need to be taken in order to ensure that menstrual equity is achieved: “Universal, free period product provision. Currently, those who menstruate are being taxed because of a normal bodily function. The current measures put in place by the government (school’s provision program, removing VAT on period products, free products via the NHS) are failing to meet the huge levels of need The Women’s Health Strategy needs to address this, with clear deliverables.
“Increase the quantity and quality of menstrual education. This is something which the Women’s Health Strategy set out to achieve - but only focuses again
on menstrual health conditions rather than the basics of menstruation. We need everyone in society to understand the reality and impact of periods, so we can develop policies to support the needs of women and people who menstruate.
“Eradicate shame, stigma and taboo. This is something activist organisations such as Bloody Good Period have already been doing, without a budget or governmental support, for years. We know there is both need and appetite for periods to be seen as completely normal. Ensuring that employers and educational institutions play a role in this normalisation will be key to its success.
“In 2019, the UK Government made a commitment to ending period poverty and shame by 2025. The Women’s Health Strategy should have been its action plan for delivering this commitment, and while commendable in many ways, it ultimately falls short. We urge the UK Government to acknowledge growing period poverty as a serious issue, and to recommit to its vision for 2025, with the right resources, community engagement and deliverables also in place.”

Endometriosis UK is a charity that campaigns to ensure those with endometriosis get access to the right care at the right time. Head of Campaigns and Communications Faye Farthing said: “The New Women’s Health Strategy for England is long awaited and much needed for the endometriosis community. There is much to be welcomed in the Strategy, but there are also notable gaps.
“We welcome the commitment within the Strategy to reduce the time it takes to get a diagnosis of endometriosis. It currently takes an average of 8 years to get a diagnosis of endometriosis in the UK – a statistic that shockingly hasn’t changed in a decade. The new women’s health hubs mentioned in the plan could help contribute to turning this around. Another investment area the government has promised are new Integrated Care Systems (ICSs), a promising opportunity to provide integrated pathways for those with endometriosis. However, the Government has lacked ambition in its commitment to reducing diagnosis times. We are disappointed that a timeframe has not been committed to, unlike the Scottish Government’s Women’s Health Plan, which took up our recommendation target of less than a year, by 2026. The new ICSs are also only ‘recommended’ rather than mandated, leaving it up to individual NHS Trusts to incorporate these within service plan strategies. This could lead to varying degrees of implementation and therefore service quality across England. E
It currently takes an average of 8 years to get a diagnosis of endometriosis in the UK – a statistic that shockingly hasn’t changed in a decade
“We are also pleased that the Government has called on NICE to update its guideline on endometriosis – a guideline which, if updated to address the gaps within it such as ensuring those with endometriosis outside the pelvic cavity have access to the right care, and all those with the disease can access mental health support if needed, could, if properly implemented by healthcare practitioners, improve care for the 1.5 million women and those assigned female at birth with the disease.

“A glaring omission from the Strategy is a lack of dedicated funding on how to ensure there is the right resources and capacity to deliver the plan. We know that there are geographical disparities in how endometriosis care is provided, which has become even more prevalent since the pandemic began. The NHS continues to be under huge pressure, and the Government have a responsibility to ensure that the capacity is there to ensure those with endometriosis are not left behind, and that the NHS has the resource it needs.
“Inclusivity is also vital. It is widely recognised that transgender and nonbinary people, as well as other minoritised groups, experience additional barriers to accessing healthcare. Endometriosis UK is disappointed in the use of noninclusive language, and endometriosis services must always be welcoming to those who were assigned female at birth but who do not identify as a woman.
“We would also have liked to have seen a commitment to invest in endometriosis research. For the 1.5million women and those assigned female at birth with endometriosis, research is vital to improving all aspects of living with the disease. There are huge barriers in accessing care due to a lack of government investment into endometriosis research. We do not know the cause of the disease, treatment options are limited, and there is currently no cure. Investment in research is vital to turning this around.
“To summarise, the Women’s Health Strategy for England is a step forward. It comes at a critical time when waiting times are soaring, and the average diagnosis time remains a shocking 8 years. We now look forward to working with the Government and Dame Lesley Regan to ensure that all those with endometriosis or suspected endometriosis receive the right care at the right time. “
Stowe Family Law Gemma Davidson, a senior associate at Stowe Family Law, who also has a masters degree in medical ethics said: “The government’s strategy on women’s health acknowledged that there is a significant data gap. Historically medical research has
not adequately considered the different health needs of men and women and crucially women’s reproductive health. In years gone by topics such as miscarriage, infertility, abortion, endometritis, and the
menopause were taboo; partly due to social stigma and because our health system did not understand women’s needs. In addition women’s health needs have evolved over time, partly as a reflection of social and economic change but also due to advances in assisted reproductive technology providing women with a greater perceived choice of options. Our health system however has not kept pace with such changes, consequently the day-to-day experience of women receiving health care services now requires investment and improvement.
Historically medical research has not adequately considered the different health needs of men and women and crucially women’s reproductive health
“The government’s strategy focuses upon the need for research, investment and change in our health care system. However, I am not a medical professional, nor am I a politician instead I see this from the viewpoint of a lawyer and a woman. I have over 15 years of experience practicing as a family solicitor, have a Masters in Medical Ethics and specialise in surrogacy and fertility law.
“I advise and support an increasing number of people who have started or are now looking to have a child via surrogacy, IVF, donor conception, as a single parent by choice or
with a platonic co-parenting arrangement. A keystone of our laws on health care is the concept of consent and respect for the autonomy of individuals. The law does so in the context of a right to a private family life. There is a tension between our reproductive laws and the impact that has upon a person’s options for starting their family.
“The repeal of Roe v Wade in America sent shockwaves across the pond and consequently our own abortion laws were discussed in the House of Commons and across the media placing a spotlight on reproductive health law. This act is now over 50 years old and therefore not without the need for review considering medical advancement and societal change. The Human Fertilisation and Embryology Act 2008 and the Surrogacy Arrangements Act 1985 are now over 20 years old, which in the landscape of important medical advancement in recent years is significant. Consequently, when these issues go before the Court, the law can be insufficient leading to complicated case law and more calls for reform. The Law Commission’s consultation paper on surrogacy laws to protect surrogates, intended parents and the child commenced in 2019, but the draft bill is still awaited and is now expected in autumn this year. It is anticipated that the changes will include the intended parents being the legal parents at birth, rather than the surrogate. Legal parenthood across reproductive and fertility laws is particularly complex, with relationship status and method of conception impacting upon who is recognised as a legal parent. For example, while the strategy comments on removing costs barriers to artificial insemination for same sex female couples if such a couple avoids the costs of a fertility clinic via artificial insemination at home they must be married or in a civil partnership for the woman who does not carry the child to be recognised as the legal parent at birth.
“The tension between our laws and our private life creates an intrusion. Many people do choose to seek advice and they are wise to do so in such a complicated area of the law. In other circumstances people seek advice when things unfortunately go wrong, for example when an intended mother who (unlike the surrogate) is biologically linked to a child cannot obtain a parental order which would legally recognise her as the child’s mother because she did not meet the law’s criteria or a same sex female couple who find that only one mother is legally recognised due to their relationship status and method of conception.
“The strategy is a start, but it is not the full picture.”
While the Women’s Health Strategy for England is a step in the right direction, it is clear there is still much to be done to reduce the gender health gap and ensure women and those assigned female at birth get access to the healthcare they need. L

The Women’s Health Strategy can be viewed here:
The strategy is a start, but it is not the full picture
Social prescribing offers many benefits to the NHS and its patients and has become more popular and more frequently used over recent years, HB looks at how it is being used in the health service and the benefits it offers
Social prescribing enables healthcare professionals to prescribe non-clinical services to patients. The aim of social prescribing is to address health needs in a holistic way and empower people to take greater control of their own health.

Also known as community referral, the use of social prescribing recognises that people’s health is determined by a range of social, economic and environmental factors and that addressing these factors can improve a person’s health.
The activities prescribed are generally provided by voluntary and community sector organisations and include activities such as volunteering, arts activities, group learning, gardening, befriending, cookery, healthy eating advice and sports.
Social prescribing is part of the NHS Long Term Plan to make personalised care part of the health and care system. This is so people have choice and control over the way their care is planned and delivered.
Local agencies such as general practice, local authorities, pharmacies, multidisciplinary teams, hospital discharge teams and allied health professionals, as well as the fire service, police, job centres, social care services, housing associations and voluntary, community and social enterprise (VCSE) organisations are able to refer people to a link worker. Link workers then connect people to community groups and agencies for practical and emotional support and collaborate with local partners to make community groups accessible and sustainable.
The benefits of social prescribing are numerous and include improving outcomes by giving people more choice and control over their lives and giving them an improved sense of belonging when they are involved in community groups.
It is also effective at improving health inequalities, for example, by helping with debt, unemployment, and housing or improving health literacy.
Social prescribing can be beneficial for people who need support with their mental health, have one or more longterm conditions, are lonely or isolated or have complex social needs that affect their wellbeing. Social prescribing can help people
with non-clinical needs, such as support on things like debt, unemployment, and housing issues, which can in turn improve their mental health. Building social connections through local community groups, like walking, singing and gardening groups can help people suffering from loneliness. There is also evidence to suggest that social prescribing reduces pressure on the NHS by directing people to more appropriate services and groups and supporting people early on, before they need more help from the health service.
Social prescribing hubs NHS Property Services (NHSPS) has recently announced the delivery of over 50 buildings and outdoor spaces that are being used as social prescribing hubs around the country.
Over the last three years, NHSPS has identified, converted and made available 54 tailor-made social prescribing hubs, where people are able to access non-clinical services, including outdoor gyms; sensory gardens, suicide prevention counselling, breastfeeding advisory sessions and ‘toy libraries’.
When using the hubs, people are encouraged to take more control of their own health and their wellbeing.
NHS England announced earlier this year the planned recruitment of 2,000 link workers to ease the demand on primary care over the winter and the hubs are also a key component in reducing pressures on clinical and acute services. It is hoped the hubs will help the NHS to remain resilient as winter pressures are expected to be the worst on record.
Since the start of the hub project in 2019, figures suggest that around 35,000 people have been able to access social prescribing services. Those benefitting from the hubs include patients experiencing physical and mental health issues, including People with Special Educational Needs (SEN)/Learning Difficulties and Disabilities (LDD), people with physical and mental health issues, young carers, asylum seekers and refugees, expectant parents, and adult offenders.
Rhea Horlock, Head of Corporate and Social Responsibility (CSR) for NHSPS said: “Passing the 50-hub milestone is important progress in our efforts to support NHSE in meeting its targets for 900,000 people to be referred to social prescribing by 2023/24. We are committed to continue to grow our social prescribing programme to bring this valuable support to more local communities.”
“With the NHS Long Term Plan expecting to be refreshed over the coming months, nonclinical interventions such as social prescribing are expected to feature as a core focus for innovation given their proven results to reduce the pressures on primary and acute care. NHS Property Services will continue to support the development of hubs across the NHS estate to support this growing ambition.”
The Listening Place in London, in a space delivered by NHSPS, has been set up to provide face-to-face support from professionally supervised volunteers to people with chronic suicidal feelings.
The Listening Place CEO Sarah Anderson
CBE said: “Although The Listening Place was only established five and a half years ago, with a second full time premises opened in partnership with NHSPS, and even more volunteers trained, we are now receiving and responding to more than 500 referrals a month.”
“The Listening Place is currently on course to open a third full time facility in West London in the next few months and is already looking to East London for more premises - we have been fortunate to find funders and partners who have supported our growth so far, and we hope to continue to grow across London, and beyond. We have doubled our capacity over the last few years and need to double it again over the next few years if we are to meet the demand for support for those who feel life is no longer worth living.”
Lucy Patterson, visitor support manager at The Listening Place added: “We are offering some 100 appointments a day, with currently over 1,100 suicidal visitors receiving ongoing support for the time they need from our Listening Volunteers.”
“We have received over 11,000 referrals in five and a half years. We need to provide a warm listener, and a safe and welcoming place, and give our visitors the opportunity to talk confidentially about their feelings and their thoughts of suicide.”
The benefits of social prescribing are clear, as these services and activities offer help to people struggling with issues such as
debt and loneliness and therefore having a positive effect on their physical and mental health and reduce the pressure on the NHS. With the new social prescribing hubs delivered by NHSPS, it is hoped many people will be able to access these services and help the NHS as we head into winter. L

https://listeningplace.org.uk








Our family of healthcare and life science brands – including Maquet, Lancer, Atrium, Pulsion, Datascope, Steritec, Stericool, Trans and others
unifying as Getinge.
As our company has grown over the years, Getinge has become a global market leader in healthcare and life science. By unifying all our brands into one, we can combine decades of scientific and technical knowledge, and commit even more to investing in new innovations, helping to pioneer therapies and build a more sustainable healthcare for the future.

Heriot-Watt University in Edinburgh is developing
cutting-edge manufacturing techniques that may lower the cost of medical equipment and devices for the NHS, freeing up money that trusts can then invest in supporting members of staff and improving outcomes for patients. Professor Robert Thomson and Professor Duncan Hand, Heriot-Watt University explain
FROM the outside, the Medical Devices Manufacturing Centre (MDMC) at Heriot-Watt University on the outskirts of Edinburgh may look like just another corridor in just another building. Yet, appearances can be deceptive.
Inside the unassuming centre, engineers are working with clinicians to develop medical equipment that will not only save NHS Trusts money but will also improve treatment for patients. Heriot-Watt University, which last year [2021] celebrated its 200th anniversary, has a long history of engineering innovation, and the institution is now bringing the skills and experience of its staff to bear on the medical device sector.
One of the university’s most far-reaching achievements has come in the field of lasers. A team has developed a way to change the shape of a laser beam, which makes it quicker and cheaper to produce pieces of medical equipment that could be used during keyhole surgery and while performing biopsies.
The laser beam can now be used more efficiently and effectively to create tiny optical components for the ends of the fibre-optics
used by doctors during keyhole procedures. Manufacturing techniques that used to take hours have now been slashed to just a matter of minutes using the new method.
Moving from scalpels to lasers Surgery once revolved around scalpels and forceps, creating an incision to give specialists access to the body to repair damage or remove problems. Yet patients then had to recover from the impacts of the surgery itself, alongside the underlying condition that necessitated the treatment.
Keyhole surgery revolutionised operations. Instead of making large incisions, surgeons were able to make smaller cuts and then use long and thin tools to slip inside the body, leaving smaller and less invasive wounds behind, which reduced the risk of infection and sped up the recovery time.
Fibre-optic cables and tools sit at the heart of the success of keyhole surgery – tiny lights and cameras at the end of flexible tubes can give surgeons a view from within the body, while smaller surgical instruments can be used to make
cuts and then stop bleeding. Operations that would have involved long, expensive stays in hospital as an in-patient can now be performed quicker and cheaper, allowing patients to be treated as day cases and sent home to recover. Only decades ago, few doctors could have imagined the transformation that would be brought about by keyhole surgery. Now, cutting-edge techniques are set to elevate the procedures onto a whole new level.
Engineers have developed thinner and more flexible optical devices to help with diagnosing and treating conditions, ranging from detecting cancer through to laser surgery. Yet these devices are built with micro-optics such as lenses, mirrors, and prisms – in a similar way to a tiny microscope – at their tips, called distal-end microsystems, which can take a long time to build and so are very expensive to buy, limiting their uptake in medical devices. Heriot-Watt University’s breakthrough in changing the shape of laser beams will E






make it quicker and therefore cheaper to produce these distal-end microsystems, which will make them more readily available for diagnosing and treating patients. The University’s innovation gives the engineers making the microsystems more control over the laser, allowing them to use the energy more efficiently from the pulses of light.
The same team has also built its own microoptic systems for future use in precision endoscopic surgery. Its systems send ultrafast pulses of laser light down hollow core fibres, which were developed at the University of Bath.


Following on from the success of the laser shaping breakthrough, Heriot-Watt has expanded its work in the healthcare field by creating the Medical Device Manufacturing Centre (MDMC), based at Heriot-Watt University and in partnership with Edinburgh, Glasgow and Robert Gordon universities. The centre is not only working on further advances to improve surgery but is also helping entrepreneurs to develop devices and tools that can be used on hospital wards and even in patients’ homes.
Bringing innovations to the wards One in every 400 people who undergo surgery in the UK have a stoma, an opening created in their abdomen to collect waste. The technique is used to treat a wide variety of conditions, including Crohn’s disease, several types of cancer, and bowel incontinence.
A bag is attached to the stoma to collect waste and needs to be changed at regular intervals. Often the bag will leak though, causing embarrassment for the patient and denting their confidence to carry on leading a normal life.
In hospitals, leaking stoma bags cost the NHS significant time and money. Changing a soiled bed sheet is a 38-step process, tying up nursing and auxiliary staff.
If a bag leaks on the operating table then the area must be sterilised again before surgery can proceed. Elderly patients cannot
be discharged if their stoma bags are leaking, which in turn ties up beds and puts increasing pressure on hospitals and their staff.
The MDMC is working with Confidence Plus, a company that has designed the ConfiPlus, a cover that absorbs stoma bag leaks and draws them away from the skin to reduce irritation and give people the chance to change their bags without embarrassment.
Anne Inch created the prototype for the device on a sewing machine in her attic using an old bedsheet after the stoma bag being worn in hospital by her husband, Iain, leaked nine times in a single day.
At the moment, ConfiPlus is only available over the counter, but the MDMC is working with Confidence Plus to put the device through its clinical evaluations, so that it will be available on prescription. ConfiPlus is unique, so it cannot be benchmarked against existing products, highlighting the need to harness the expertise within the centre to help win approval for the product.
While NHS regulations are complex in order to protect patients, the process of navigating the regulatory system is burdensome for small companies, which can stifle innovation. The MDMC offers a free service to small and medium-sized enterprises (SMEs) in Scotland and beyond to help get their devices approved for use in clinics and hospitals, and available on prescription.
Back in the operating theatre, Heriot-Watt’s engineers are not only harnessing the power of lasers but are also developing technologies that can help surgeons for robot-assisted minimally-invasive surgeries. As well as the MDMC, the university is also home to the new National Robotarium, the most advanced robotics and AI centre of its kind in the UK.
One of its flagship projects involves developing a probe that will give surgeons more information about the tissues they are examining during robot-assisted surgery. The new probe is equipped with sensors that can take mechanical measurements of a cancerous tumour and the surrounding region, allowing surgeons to judge how much of a surgical margin to remove along with the tumour.
The probe is also linked to and enhanced with a computer-based modelling strategy. This can detect the presence of the cancerous tissue and help surgeons optimise the surgical margin. The system can give the surgeon extra insight, helping them to judge the right size of surgical margin.
This is supplemented by other research to develop computer vision technologies for intraoperative assistance to surgeons and higher precision surgical robotic manipulators using laser-based manufacturing techniques.
Through the work of facilities such as the MDMC and the National Robotarium, engineers at Heriot-Watt University are at the forefront of medical device innovation.
By working together with clinicians and entrepreneurs, these advances will help to save money for the NHS and improve outcomes for patients. L
About the Authors:
Prof. Robert R. Thomson is Professor of Physics at Heriot Watt University. He obtained his BSc in Physics from Heriot Watt in 2000, the MSc in Optoelectronics and Laser Devices from the University of St Andrews in 2001, and the PhD in Physics from Heriot Watt University in 2006.
From 2010-15 he was an STFC Advanced Fellow developing photonic technologies for astronomy. He is Principal Investigator of the £6M “U-Care” EPSRC Programme Grant (u-care.ac.uk) which is aimed at developing advanced healthcare technologies based on the unique properties of deep UV light. He has been awarded ~£35M in funding since 2009 (~£11M as PI and £24M as Co-I). He co-founded Optoscribe Ltd in 2010.
Prof. Duncan Hand is Professor of Applied Photonics at Heriot-Watt University. He became fascinated by the science and engineering of photonics whilst studying for a degree in Physics at the University of St Andrews in the mid 1980s and his passion for this technology continues to drive his academic career today. Following his first degree he studied for a PhD in optical fibres at the University of Southampton before moving to Heriot-Watt in 1991. Photonics is an enabling technology that he has applied to a diverse range of applications, with the aerospace and defence industry; ship building and ship engine manufacturing; medical device manufacturers; plant biology; and medical practitioners including surgeons. His current key focus is on manufacturing of medical devices, and he is Director of the £3.6M Medical Device Manufacturing Centre (MDMC) and the £1.3M EPSRC Platform Grant on Multimodal Medical Device Manufacturing (4MD).







Radar Healthcare, a provider of risk, quality, and compliance software, has taken partnership working to a new level. By taking a collaborative approach and always placing their partners at the heart of their product and service, they’re able to adapt and evolve their offering to suit their partner’s current needs and objectives, whilst focusing on the shared goal of improving patient outcomes.
In their video, ‘Your Journey with Radar Healthcare’, the teams express how their service is so unique. From business development to customer experience to product, developers, and support, everyone shares the same values and a strong desire to make a difference in safer healthcare.
Radar Healthcare’s commitment to its partners is reflected in a 96% customer retention rate and the customer experience awards they have been shortlisted for this year, including three UK Customer Experience Awards 2022. They have also launched a podcast ‘What the HealthTech?’ and in episode 10 ‘People and Partnerships,’ Radar Healthcare’s Customer Success Lead, Mark Harrison discusses the importance of collaboration and what organisations should look for in a supplier when considering a true partnership.
“Our sales process is truly a transparent process. Everything that we offer is around understanding the needs and the requirements of what our partners wish to achieve. And then we go ahead and plan and execute a strategy that’s
going to be their requirements,” says Simon Qasir, Head of Sales at Radar Healthcare.
With the help of its Product team, Radar Healthcare has also been able to ensure that the software is innovative and constantly meeting the needs of its partners. Part of this process is listening to what is needed and when, which is why having a flexible product is so important in an everchanging health and social care market.

“29% of our development suggestions on our community forums have been delivered,” says Radar Healthcare’s Product Owner, Ellie Jordan. “We want to be able to have a system that makes a real impact on our partners.”
Chloe Weatherhead, Head of Customer Experience at Radar Healthcare, further supports this:
“There is something very heart-warming about working for an organisation where everyone is completely engaged in the mission to improve patient safety and to improve outcomes for patients. You can’t help but feel proud of working for an organisation that is so focused on that approach.”
Radar Healthcare is here to help you make a real difference, now and in the future. Watch the video here to discover more about how they collaborate with their partners, or listen to their podcast, What the HealthTech? for updates, opinions, and insights on all things healthcare.

South Yorkshire Integrated Stroke Delivery Network and Yorkshire Ambulance Service tells us about their telehealthcare
Stroke within South Yorkshire Stroke strikes every five minutes and is a leading cause of death and disability in the UK. It’s vital that those with stroke symptoms seek urgent help and dial 999. This ensures urgent treatment is received in the correct stroke specialist centres.

South Yorkshire has a population of approximately 1.4 million, made up of 32 neighbourhoods, four Local Authorities and eight acute and NHS Hospital Trusts. The South Yorkshire region is predominantly urban and has relatively high levels of deprivation and health inequalities, in comparison with the rest of the country. Recent reviews of data have shown a strong social gradient and there are significantly more stroke admissions from the most deprived neighbourhoods across the region. The prevalence of stroke in the region is 2.1 per cent and there are around 33,115 people living with stroke or transient ischaemic attack. In 2021/22,
Unit’s (HASUs), and are in the areas of Sheffield and Doncaster, with some patients receiving treatment in Wakefield. Treatments offered here include the ‘clot retrieval’ treatment, Thrombectomy, and the ‘clot busting’ treatment, Thrombolysis. These centres are supported by the South Yorkshire Integrated Stroke Delivery Network (SY ISDN). ISDNs are the key vehicle for transforming stroke care across the country, working with partners from across the region to help prevent stroke and improve access to treatment. Since 2020, the South Yorkshire Integrated Stroke Delivery Network (SY ISDN) has been working with partners to improve the quality of stroke care with the aim of improving clinical outcomes, patient experience and patient safety.
improving the prehospital pathway and how we can ensure that the right patients, arrive at the right place and at the right time. The use of technology such as video triage to modernise and improve the prehospital pathway is advocated for in key national guidance.
These include: Carter Review (September 2018) recommendations, Stroke GIRFT (Getting It Right First Time) National Speciality Report (April 2022) and National Stroke Service Model: Integrated Stroke Delivery Networks (May 2021).
The South Yorkshire ISDN are continuously looking for innovative solutions that can benefit patients, solve problems and transform pathways of care.
Of particular interest has been
An opportunity to bid for some NHS England funding to implement a Stroke Video Triage Pilot presented itself in March 2022. The South Yorkshire ISDN seized this opportunity and brought key partners together to develop a collaborative bid which was successful. In total, eight pilot sites across England are striving to implement and evaluate stroke patients through video triage.
To support the funding bid, the South Yorkshire ISDN Stroke Survivor and Carer Panel were consulted and strongly supported this being taken forwards. The Panel was developed to allow those who are living with stroke or caring for someone with stroke to share their views and help shape stroke services across the region. E



Connecting without boundaries in telemedicine, tele-ICU and live surgery broadcasts all over the world.







Three NHS Trusts; Yorkshire Ambulance Service NHS Foundation Trust, Sheffield Teaching Hospitals NHS Foundation Trust and Doncaster and Bassetlaw Teaching Hospitals NHS Foundation Trust, committed to delivering the pilot with the assistance of GoodSAM providing the technology.
As well as being a platform used nationally to alert NHS Volunteers to help those who need support, GoodSAM provides advanced video technology to the 999 and 111 services, revolutionising how care can be given.

Preparations for the pilot commenced in May 2022 and it was officially launched on 15 August 2022, with successful calls being made that day.
The key to the successful implementation
Video triage will explore four key areas to monitor the success of the pilot, these include: Improved Assessment - enhance the existing ‘pre alert’ triage assessment and enable earlier access to stroke specialist assessment and treatment; better use of technology - effectively use ambulance and clinical resources, reduce pressure on Emergency Departments by using technology to reduce in-hospital assessment times and reduce handover times, releasing crews sooner to assist further calls; and improved outcomes - increase equity of access to urgent stoke care, improve patient outcomes by ensuring that the right patients, arrive at the right place and at the right time, reduce the
throughout ambulance crews, as well as through the 1:1 training provided by the project team.
Despite some early connectivity challenges, positive outcomes have already been seen. The pilot has provided more opportunities for education and training for clinical staff increasing their awareness of stroke. The communication and engagement plan developed to support the project has also ensured the pilot mobilised at pace and collaboratively across the whole region. The impact of the pilot will be continuously monitored, and a final evaluation completed. We are already sharing learning across the community of practice that has been established for the pilot sites.
Our vision is that if the pilot is successful, in the future, all stroke patients within the region will benefit from the introduction of stroke video triage and have improved outcomes should they suffer from a stroke. L
The
of technology onto
crew
was
resolved

CLEO Systems developed its electronic prescribing solution CLEO SOLO EPS initially as a response to the Covid-19 pandemic and to give clinicians instant prescribing capability in remote settings, without the need for any systems integration. CLEO SOLO EPS is now accredited by NHS Digital and available to health organisations across the country after having been successfully piloted in the prominent Midlands Partnership NHS Foundation Trust (MPFT), where it is delivering key cost-saving and patient safety benefits
which meant less time with their patient. Now at the touch of a button, CLEO SOLO EPS has transformed clinicians’ work, modernising how healthcare professionals prescribe medication in a timely and efficient manner.
A consultant at MPFT says, “It is not too dramatic to state that EPS has revolutionised my practice. I can now write and deliver prescriptions in five minutes compared to the time and effort it took to handwrite a prescription from scratch, arrange for it to be collected by the service user or a member of the team, or otherwise hand deliver it to a pharmacy. A huge time saving with inbuilt safeguards to enable safe prescribing.”
One service user says, “So happy with this new service, I don’t drive so I would have to catch a taxi to collect my prescription which was very costly, so having it sent straight to the pharmacy is going to save me money.”
Community pharmacy: “No issues, everything has worked well and the patients have been happy with the service.”
As an instant electronic prescribing solution, CLEO SOLO EPS enables quick, seamless, clinically safe prescribing which provides improvements in efficiency and sustainability while significantly reducing the need for paper prescriptions. The solution can be used in a wide range of outpatient secondary care settings – from community pharmacies and mental health to secondary care, enabling patients’ prescriptions to be entered and sent electronically to a nominated community pharmacy of the patient’s choice.
CLEO Systems worked collaboratively with MPFT and NHS Digital to deploy CLEO SOLO EPS in a successful First of Type pilot culminating in accreditation from NHS Digital. The successful pilot has delivered key benefits across the Trust, including a move away from hand-writing prescriptions, meaning that patients’ prescriptions are now sent electronically to their nominated pharmacy, freeing-up time for busy clinicians, enhancing patient safety and increasing data security.
With handwritten prescriptions sometimes being illegible, this can have an impact on clinical safety as prescriptions can be incorrectly interpreted or time can be
wasted phoning the hospital to check the prescription details with the clinician. Before the pilot at MPFT, patients often needed to travel to the hospital to collect prescriptions. Since the implementation of CLEO SOLO EPS, prescriptions are now sent electronically to the pharmacy of choice, freeing up time for patients, reducing cost while adding convenience by enabling collection from the pharmacy.
Areas of estimated cost savings during the pilot have included a reduction in stationery and first-class postage, as well as mileage and travel time costs for clinicians. Future cost and efficiency savings are also being identified as the trial expands.
The solution has a robust and innovative method of search functionality which means that patient search errors are minimised and the correct medications can be seamlessly prescribed. It also enables excellent governance and reporting.
Feedback from the successful pilot at MPFT has been impressive, with evidence of cost and time savings for clinicians, solution users and patients. Before the CLEO SOLO EPS pilot, the legacy process was hand-writing prescriptions before posting or delivering them physically,
David Brown, managing director, CLEO Systems says, “As the first provider to launch a product of this type into the sector, the clinical and patient benefits associated with the successful launch and pilot of CLEO SOLO EPS are evident. CLEO SOLO EPS aligns with the NHS agenda, supporting the NHS England focus on digitisation and electronic prescribing as set out in the NHS Long Term Plan (www. longtermplan.nhs.uk/publication/nhs-longterm-plan/), while improving efficiency and enhancing the patient pathway.”
CLEO Systems is a leading provider of digital health software solutions in Acute, Outpatient, Urgent and Community settings. As a social enterprise - and with a suite of interoperable solutions already under its belt - when Covid-19 hit, CLEO Systems was well placed to be agile and to provide solutions to support the NHS in unprecedented times.L

The Association of British HealthTech Industries (ABHI) has launched a white paper: Robotic Assisted Surgery and New Models of Surgical Care, which sets out the case for a national multi-stakeholder strategy for Robotic Assisted Surgery to support its uptake across the NHS. In this article for Health Business Magazine, ABHI’s Robotic Assisted Surgery Group Vice Chair, Chris Gray, explains the thinking behind the paper
The benefits of Robotic Assisted Surgery (RAS) versus manual surgery are increasingly well catalogued. Reduced trauma to patients that can lead to quicker recovery and better experience, fewer days spent in hospital freeing up much needed capacity including Intensive Care Units and High Dependency Units, less physical stress on surgeons, potentially extending their working life, and procedures being performed on high-risk patients or patients with complex conditions where open surgery would not be an option, as well as the capacity to track and measure surgery, far more than has ever been achievable with manual approaches. The use of RAS is increasing in abdominal, thoracic and orthopaedic surgical specialities and the benefits of using these systems are
beginning to resonate across the NHS.
The NHS is reforming, some of it planned, some of it driven by necessity. The expected changes are in part, a response to the underlying challenge the NHS faces - ensuring healthcare remains accessible and free at the point of need - despite an ageing population, rising demands and cost pressures, and a fatigued NHS workforce facing an endemic challenge of recruitment and retention. In parallel, the
The use ofRAS is increasingin abdominal, thoracicand orthopaedic surgicalspecialities and thebenefits of using thesesystems are beginningto resonate acrossthe NHS
NHS will, for the foreseeable future, deal with the elective surgery backlog. In England, a move to integrated care with regional strategies directing future investment, could lead to different models of elective surgery emerging to address local/regional requirements and objectives. This could be an opportunity to recognise RAS, in a similar way to how Scotland and Wales have recognised the role of RAS in their national planning. With this in mind, we at the E












Association of British HealthTech Industries (ABHI) have launched a white paper: Robotic-Assisted-Surgery and New Models of Surgical Care, which sets out the case for a national multi-stakeholder strategy for RAS to support its uptake across the NHS.
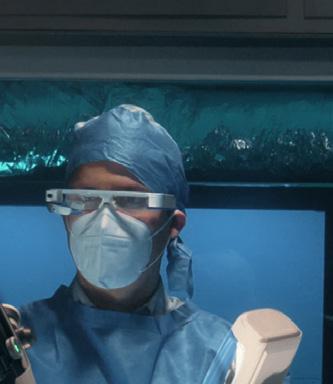


The paper has been spearheaded by ABHI’s dedicated Robotic Assisted Surgery Group, which sits within the Association, and brings together HealthTech companies, the clinical community and other relevant organisations who have a strong interest in furthering the use of RAS.
The timing of this paper is important. The NHS in England is at a significant juncture, with political decisions about how the healthcare system is structured and what is prioritised post-Covid all to be made in the coming months. This will set the direction and course of the NHS for a generation.
The document recognises the common themes and challenges across the environment for providers, clinicians and industry, in supporting the adoption of RAS, and makes a series of recommendations across the key areas of regulation, policy, evidence, awareness and training.
We have also identified building blocks that we view as crucial for the sustainable growth of RAS including:
Enable the efficient evaluation of clinical and economic value of RAS through the utilisation of real-world evidence
The capacity to generate, capture and analyse data can drive a revolution in our ability to understand more quickly the safety, effectiveness and value of new digitally enabled technologies.
However, this capacity and the potential benefits it can offer, also needs to be accompanied by clarity in thinking on what data needs to be captured, for what purpose, how will it be used to inform decisions and by whom.
The move in England to population-based healthcare strategies delivered by integrated care systems and providers could pave the way
for understanding the benefits of technologies beyond the setting in which they were utilised.
Whilst RAS has well-reported benefits supporting patients to recover quicker and leave hospital sooner following surgery, how this benefit is maintained and enables them to return to normal life, is less understood. Demonstrating the potential ‘ripple effect’ of RAS through perioperative care, is one area that requires further attention.
Support the development of professional education, training, and expanding the knowledge of RAS to non-surgical NHS staff RAS is a revolution and a significant leap forward from how surgery was performed even 20 years ago. Nevertheless, whilst the technology can significantly enhance the skills of the surgeon and their team, it still requires surgical competency, knowledge and understanding to deliver outcomes safely and efficiently.
As Robotic Assisted Surgery becomes more widely adopted, the need to train surgeons and NHS staff at scale will continue to grow.
The HealthTech industry recognises that training will necessarily vary because of the different RAS platforms specialties they are being used for. Ensuring high standards in training and access to continuous professional development, therefore, will be critically important.
Improve the general understanding of RAS and its benefits, to positively inform the development of patient pathways and integrated care strategies
Equity of access to minimally-invasivesurgery, let alone RAS, remains a problem in the NHS. This can have serious implications for the patient, their treatment choices, and their overall wellbeing and recovery.
The patient benefits of RAS, including reduced trauma leading to quicker recovery, are not always recognised beyond the surgeon and their team. Raising awareness of RAS
and demonstrating its benefits to those supporting patients through their treatment journey will be important for them to make informed choices about their treatment.
More pressing is the need to address the surgical backlog that has grown significantly since the start of the COVID-19 pandemic.
Greater awareness amongst NHS planners of RAS, especially its positive impact on reducing length of stay of patients and reliance on Intensive Care Units and High Dependency Units, could help alleviate the burden on capacity that some Trusts are facing.
Lack of payment for RAS procedures can also be a disincentive for Trust investment in robotic surgery. Block contracts do not support uptake of RAS due to a lack of legacy payment mechanisms for such technologies outside urology.
Recognise RAS when formulating policy, for example, in response to the current backlog of elective surgeries and in future life sciences strategy
For the UK to take a leading role in research and development of digitally enabled technologies such as RAS, it needs to positively and proactively recognise it in key policies and strategies.
This recognition would provide a welcome signal that the Government and NHS sees value in nurturing this fast-growing sector. An active partnership with industry is needed to demonstrate the value it can bring to patients and improved efficiencies in health delivery.
In Conclusion Ensuring that the NHS and patients can realise the benefits from RAS is a key motivation behind this paper. It is our view that RAS should be viewed strategically, and given key consideration when looking at future surgical care configuration and patient pathway design.
The opportunities that further RAS adoption presents will only be delivered safely, effectively and efficiently through collaboration across industry, the NHS, Government, and patients.
Fundamentally though, collaboration will be key to realising the benefits of RAS, and through the ABHI group, we will be using the paper as an engagement tool to inform future work and partnering opportunities. L
The report can be downloaded at www.abhi.org.uk.
An active partnership with industry is needed to demonstrate the value it can bring to patients and improved efficiencies in health delivery

MIRACL, the world’s only single-step multifactor authentication, has created a new partnership with Birmingham Women’s and Children’s NHS Foundation Trust. With a recent directive from NHS Digital to ensure multi-factor authentication (MFA) across IT services within the NHS, MIRACL was perfectly placed to deploy their single-step MFA system in these world-renowned hospitals.

Time is precious for all those working in the NHS, so finding a MFA solution that was efficient yet provided the additional layer of security that was now required and, at a cost that met the tight NHS budget, was a challenge. Medical records are highly sought by cyber criminals so any data held by the hospital is always incredibly vulnerable and must be well protected on every level.
David Marshall, Head of ICT at Birmingham Women’s and Children’s NHS Foundation Trust comments: “Numerous staff throughout our sites are having to access NHS IT on a daily basis, but time is always of the essence and it is essential that not only is all data kept safe and private, but staff who need to access information can do so instantly and securely. It was no surprise when we were required to add multi-factor authentication to our systems but finding a solution that would fit our needs was a challenge. MIRACL has provided a single-step MFA that does not require a password and has integrated into our systems seamlessly.”
MIRACL was able to integrate their singlestep MFA codelessly, in just fifteen minutes - minimising disruption to services during the implementation phase, yet providing an added layer of IT security across the organisation. With thousands of users within the Trust accessing IT services on a daily basis, the transfer happened seamlessly and without any unwanted hiccups.
Furthermore, as a passwordless solution, staff weren’t tasked with having to remember yet another password or have to share biometric data. A simple four-digit PIN is all that is requiredthe patented tech does the rest.
Rob Griffin, CEO at MIRACL adds: “When we were advised that NHS Digital were
directing hospitals to install MFA, we knew our solution was perfect. MIRACL provides MFA, yet requiring just a singlestep to use, means that staff can access the IT services as they were before and without the need to remember another password or have a second device at hand to authenticate by SMS. We all know that staff are often working at a high pace across the NHS, so sourcing a solution that did not waste precious time authenticating was really important.”
Since deployment of the service in midApril, there have been a total of over 150,000 authentications and only 283 failures or a failure rate* of only 0.18 per cent.
Michael Tanaka, Chief Commercial Officer at MIRACL said: “Healthcare professionals, quite rightly, prioritise the care of their patients above all else. IT and the security of its systems will always be important, but understandably unlikely to be the main focus - until systems collapse like we saw in 2017. The NHS was brutally hit by a Wannacry attack, bringing services to a standstill for several days. So, using secure systems that provide an additional layer of security, but do not compromise the work of the healthcare professionals is the ideal solution. Which is what we have seen here in Birmingham work so successfully.”
MIRACL is the world’s only single-step multi-factor authentication provider. It can easily be integrated into current company
and NHS platforms and is a low-cost verification option but with banking-level security. It boasts clients such as Experian, Domino’s and Cashfac and has been licensed by big tech names such as Google and Microsoft. It really is a login you’ll love.
MIRACL creates a positive user experience and cost savings by removing the barriers to secure authentication. With a near faultless login success rate of over 99.6 per cent,
MIRACL reclaims the 15 per cent of traffic that’s lost to poor login experiences caused by insecure passwords, expensive SMS texts and complex authenticator apps. The single-step, two-second login also decreases support costs by 30 per cent+ while saving significant time for both consumers and staff.
MIRACL Trust is a PSD2 compliant multifactor solution for both authentication and transaction signing that runs natively on any device without downloads. It’s GDPR friendly since no user data is stored or needed to integrate with any other identity or service platform. MIRACL’s global portfolio of clients include Credit Agricole, Cashfac, Experian and Domino’s Pizza.
MIRACL’s technology is licensed to the US Government, Intel, Google and Microsoft.
more about the world’s fastest MFA, how you can integrate MIRACL into your Trusts’ IT systems or watch a demo or contact us below.

Dr Lloyd Humphreys examines the government’s Digital Health and Care Plan, which was released in June

At the end of June, poised to launch his long-awaited Digital Health and Care Plan, then health secretary Savid Javid told an audience that: “We can combine valuable lessons from the pandemic with incredible new technology and innovative ways of working... It’s a small window of time where we can make a big difference.”
He was right. Now is the time to capitalise on the momentum achieved by digital health during the pandemic. ORCHA research published by the British Medical Journal noted a striking 343 per cent increase in recommendations of digital tools by healthcare professionals during the first months of lockdown.
Whilst a new secretary of state finds her feet, it’s up to those of us in the health tech sector to make sure Javid’s laudable plan makes its mark.
If you look at the big picture, the spirit of this plan is as important as its individual parts. We want its very existence to propel digital to the forefront of minds. Digital tools are already being activated across the NHS to help tackle the elective backlog. One app has the potential to save 1.7m hours of nursing time if
deployed for use in eye services alone. Another reduces the need for pre-operative assessment appointments in MSK by 60 per cent.
In various parts of the health system, there are different modalities of intervention. In some areas there will be pharmacotherapy, where patients will be prescribed medicines, in others you may be given physiotherapy, speech and language therapy or talking therapies. All these are embedded in pathways – and now we need to add digital health.
So much potential is literally at our fingertips. I look forward to the day when all this incredible tech is par for the course –utterly embedded in our healthcare systems and considered to be merely a different modality for a health intervention. This is already happening successfully in mental health. Patients going into step
two IAPT services might have talking therapies prescribed (on the telephone, online or in a group) or might be given a digital intervention. This is one area of healthcare where digital health is fully integrated and has parity of esteem.
Looking now at the detail of the plan: it describes how the government intends to scale digital health. It takes existing schemes and approaches and builds upon them in a way that drives the sector forward. The new EVA – the early value assessment for digital health products –makes sense (test and perfect a new product before rolling it out at scale). The NHS Innovation Accelerator Programme has been doing excellent work on this front, but a fresh approach should boost the profile of innovation still further and is a way to formalise the process using NICE.
It’s noteworthy that the original scheme was set up because it takes up to 17 years to get an innovation working within the E
Nowis the timeto capitalise onthe achievedmomentum by digitalhealth during thepandemic





NHS. So, the new EVA is laudable and will hopefully give developers a boost.
Additionally, the plan flags that digital products with strong evidence for clinical and cost effectiveness will potentially be commissioned nationally, building on what NICE has done with the Rapid Uptake Programme and the Accelerated Access Collaborative with the Innovation Technology Tariff/Payment schemes. If this can be scaled then this is a significant and positive change away from the previous locally commissioned model and mirrors approaches elsewhere, for example in Germany.
The challenge, though, is that evidence can be hard to measure. If you run a mole-tracking device, it could be straightforward to track its impact as it can speed up identifying a tumour. But what if you provide an educational and signposting app, how do you measure the effectiveness of that technology?
Finally, it appears that some further work will be done on the regulatory approvals developers need to meet, such as the Digital Technology Assessment Criteria (DTAC).
The DTAC has had a solid start, with many ORCHA clients having passed its tough benchmarking criteria. Some developments are needed, as would be the case with any new standard. A key issue is that aspects of the DTAC are interpretive rather than objective. Any developer asked to self-certify an app will, naturally, look at it very positively.
Javid’s plan flags the issue of privacy and ethics in digital health and rightly so as there’s a hill to climb. ORCHA’s recent report into period tracking apps found that 84 per cent share data with third parties.

Period tracking apps have made headlines recently, yet the privacy issues flagged in this case are not distinct to this case, they apply across the board.
The government makes more than a hundred commitments to make better use of data whilst maintaining privacy and ethics standards –and developers must take responsibility here, too. There’s an industry-wide issue with where and when users are asked for their permission to share their data. This often comes at the beginning of the app registration process, with new users being asked to tick overall consent to Terms and Conditions and the Privacy Policy.
Having signed away control of their personal data within minutes of downloading a new app, it can then become hard to regain control. It would be best practice for an app to have a ‘consent’ page that’s easily accessed from the main menu. Each individual permission could then be ticked or unticked at any time. This is an area where developers can lead the charge, recognising their ethical responsibilities.
A welcome addition to the plan is the focus on digital inclusion and the grass roots approach of working through local connections and existing programmes to uncover and address fears about using digital health products.
The plan says that ‘lack of trust in the security and reliability of digital technologies can be a barrier to their uptake’. However, independent surveys commissioned by ORCHA have found overwhelming support from the public for the introduction of digital tools. Sixty-one per cent of respondents questioned earlier this year supported the introduction of digital tools to help the NHS.
Yet the same research found that healthcare professionals are recommending just a small percentage of the health apps being used. We expect to see the number of referrals increase as access to digital health training improves and doctors and nurses become more familiar with the technologies now available. NHS providers such as the Greater Manchester Mental Health Foundation Trust and the Chelsea and Westminster Hospital Foundation Trust (through its charity arm, CW+) are at the forefront of
digital health adoption, having commissioned digital health libraries so their staff can safely find and recommend the best apps. Other frontline workers wanting to improve their digital skills can take advantage of the country’s first online digital health training academy, freely available to all via the Health Education England learning hub.
To conclude, let’s return to the big picture. The government has commissioned and published its first ever digital health and care plan for the NHS and this is a landmark statement of intent in terms of digitising healthcare. There may be details to iron out, but the potential offered by these digital tools is revolutionary and our NHS needs nothing short of a revolution. L
Dr Lloyd Humphreys is a clinical psychologist and managing director of ORCHA, the Organisation for the Review of Care and Health Apps: www.orchahealth.com
A welcome addition to the plan is the focus on digital inclusion and the grass roots approach of working through local connections and existing programmes to uncover and address fears about using digital health products

At 07:00 BST on the 4 August 2022 – NHS IT provider, Advanced, identified they had been compromised by a ransomware attack and immediately started responding to contain the hackers. They issued a statement to address the growing concern, “We are rebuilding and restoring impacted systems in a separate and secure environment”. The NHS also responded with a statement “…the NHS has tried and tested contingency plans in place including robust defences to protect our own networks…”
Over two months later, chief executive of Oxford Health Foundation Trust, Nick Broughton, said problems were still ongoing, “One shouldn’t underestimate the impact this has had on our organisation… it is compromising our ability to deliver the quality of care that we would like to…”. Advanced had initially said that only a “small number of servers” had been affected and that it might be able to recover in a week.
This attack and 2017’s shocking WannaCry ransomware attack are two examples which remind us that defending the NHS is, despite best efforts, a very tall order.
The NHS is an enormous, complicated organisation with 1.22m full time employees, 219 separate trusts and over 8,000 suppliers within its supply chain.
It must fight on multiple competing fronts which include staffing, funding and the elective care backlog whilst trying to improve services, transform digitally and protect itself from increasingly sophisticated cyber criminals.
But why would someone target the health sector though? It could be that health services are often targeted because they have large vulnerable supply chains, plus their services are vital, so there is a good chance of extracting a ransom.
Of course, there is also a huge reservoir of potentially valuable data to harvest which can be monetised without anyone even being aware there’s been a breach.
According to Experian, stolen patient records on the dark web sell for between $250 and as much as $1,000. As a comparison, credit card numbers sell for around $5 each and Social Security numbers can be purchased for as little as $1 each. Patient records are way more
valuable because a credit card can be easily cancelled, whereas medical records contain lots of valuable persistent data, such as a patient’s medical health history, demographics, as well as their health insurance and contact information.
Once records are stolen, cybercriminals can harness the growing network on the dark web and connect with different criminal skill sets such as drug traffickers or money launders. They are eager to buy medical records for their own criminal activities, such as illegally obtaining prescription medications, false medical claims or using the patient’s identity to open credit cards and take out loans.
So, what is the way forward?
Well, it’s not easy, but lessons have been learned and there are some clear straightforward measures which can help. Ransomware attacks tend to be initiated using phishing emails, so it is important that all staff are aware of the dangers of clicking on suspicious links.
Of course, it’s also crucial to make sure that there are appropriate data back-up processes, and that strong disaster recovery and business continuity plans are prepared for ransomware attacks.
Other simple precautions include ensuring software is up to date, patched and, crucially, adopting a mindset that cyber security is everyone’s responsibility.
The idea that cyber security is everyone’s responsibility is one of the key drivers behind a major new cyber conference and expo - UK Cyber Week. It is a completely free event focused on levelling up the cyber security knowledge for cyber, IT and operational leadership teams. There are over 100 seminar sessions covering all aspects of cyber security and there really is something for everyone no matter how much they know about cyber.
The organisers have developed a unique rating system which grades each session on how technical it is, ranging from level 1 –“Absolute Beginner” to level 6 “Engineer/ Hacker” this allows attendees to self-select the content that’s the right level for their understanding of cyber issues. It also ensures that the speakers know what level to deliver their session. Everyone’s time is precious, so we wanted to make sure that if you do spend your valuable time with us at UK Cyber Week it is as efficiently used, and you will learn as much as possible. There is a definite image problem for cyber security in the world of those who aren’t cyber security experts – it can be seen as complicated, or a nuisance, a distress purchase. “How much will it cost to be safe?” is a somewhat impossible question to answer and of course anyone can be hacked, Sony, Apple, and the NHS. Also, you can’t buy a product and make the problem simply go away so it can be neglected, or the concern simply outsourced to a siloed IT team – let someone else worry about it all!
Fixing this image problem is one of the key missions of UK Cyber Week – how do you bring the subject to life for someone whose day job, isn’t cyber but they have influence over budgets or policy? How do you make it interesting, engaging, and educational. The organisers are particularly thrilled with one innovative session entitled “Confessions of a Hacker” – delivered by a real-life hacker. Back lit and speaking through a voice modulator off stage to protect their identity they will share insight into how they hack facilities including critical national infrastructure, airports, and casinos.
This is certainly one not to miss and their genuinely shocking insight into how it all works and how easily your own setting could fall to the techniques they use.
There is a fascinating live interview with Cecilie Fjellhøy, star of Netflix’s most watched documentary – The Tinder Swindler. Cecilie’s story is enough to scare anyone off dating apps, but we must be clear this is not about dating apps – it’s about fraud and deception.
There are opportunities to immerse yourself into the growing cyber community in the networking bars, the evening meet ups
Cecilie is an intelligent, professional woman and shows how criminals are increasingly sophisticated striking in unexpected ways.
High value NHS staff and leadership can represent tempting targets for fraudsters, and it is a genuinely shocking story.
Jayson E Street, somewhat of a rockstar in the hacking world, is jetting in from Austin, Texas to show how social engineering is used to trick people. By watching a bank robbery in real time (via a hidden camera) the audience will see that even in high security areas people can still be a victim of their assumptions. The audience will understand that while most people have biases, they may not even be aware of, they can be trained to spot suspicious behaviour. People will learn that untrained workers are a serious threat, yet workers educated in Security Awareness can be the biggest asset for a company’s security.
The content program also has lots of interesting speakers for the more technical audience too – speakers such as Google’s Chris John Riley exploring minimum standards in application security and Forescout’s Daniel Dos Santos who demonstrates a proof-of-concept malware that exploits IoT devices for initial
access, moves laterally on the IT network, and then holds OT devices hostage!
There is also a growing threat from outside the commercially motivated cyber criminals, these days, nation states and activists are a very clear and present danger. Someone who has had exposure to this offensive computer network exploitation is ex-US Department of Defence operative, Daniel Gericke. Daniel just doesn’t speak at conferences, so it is a real coup to be able to hear from him at UK Cyber Week.
The content program is hosted on a main keynote stage and 5 themed breakout theatres: Resilience Theatre - Covering organisations ability to prepare for, respond to and recover from cyber attacks Strategy Theatre - Focusing on the latest threat landscape and trends, and how to develop a robust cyber strategy in response to a changing world.
Culture Theatre - How to build a strong human based element to cyber security. Covering psychology, training, policies, leadership, recruitment, and retention Prevention Theatre - Arming you with the tools and thinking to prevent the next attack including monitoring, intelligence,
zero trust and vulnerability management

OT Security Theatre - Up to the minute expertise covering the risks and best practices in protecting physical processes and devices, industry, and critical national infrastructure Networking is also a key part of UK Cyber Week’s philosophy and there are opportunities to immerse yourself into the growing cyber community in the networking bars, the evening meet ups and at the big show party, organised in conjunction with Cyber House Party.
UK Cyber Week is completely free to attend event and if you would like to visit you can register through the website: https://www.ukcyberweek.co.uk/ Tell your network and bring your colleagues - Cyber security is all about people and there is no doubt we are all in this together. Protecting everyone in the health sector, staff, patients, and the supply chain is something we can certainly all get behind. Everyone here at UK Cyber Week hopes that you enjoy your visit and come away with actionable insight which you can use right away.

The healthcare sector is one of the most vulnerable to security attacks. The global COVID-19 pandemic brought the healthcare sector to the forefront of everyone’s minds, cyber adversaries included. Over the last couple of years, healthcare has become the sector hit by the highest increase of cyber attacks reported globally. Some security researchers posit that cyberattacks targeting healthcare organisations have spiked 45 per cent since November 2020,
to an overall 22 per cent increase
varying degrees of investigation and response. However, these systems should continue to be monitored and maintained. The best option for organisations that are looking to fortify their cyber security is internal network segmentation, or even micro segmentation. Separating production, non production and operational technology networks can prevent the malware in one section from affecting the other sections, essentially containing the issue.
5. Manage privileged access
Privileged access accounts are at the forefront of cyber attackers’ goals as they are the most valuable.
To mitigate the risk of cyber attack, healthcare organisations should review their security capabilities to ensure they are addressing the following five priority areas.
1. Plan ahead to recover from a disruptive attack
There are two main components of planning ahead for a disruptive attack; business continuity planning, and incident response planning.
For the former, organisations should identify systems and data sources that are required to maintain critical operations, develop plans so that these operations can be maintained even if systems become unavailable and plan for how to restore critical systems, including a priority scale. This also means having regularly updated backups that are protected from destruction. For the incident response, a clear understanding of key stakeholders, overall methodology and a high level work stream is required. To be better prepared, attack simulation exercises should be carried out and incident playbooks created and tested.
2. Defuse phishing emails
Phishing emails are the most common and effective form of attack used by cyber criminals. Healthcare organisations should use a number of methods to prevent themselves from being damaged by them. First of all, automated
filtering systems on email platforms are an effective first start. Secondly, proactive education of staff to enable them to identify, report and delete phishing emails can protect your team from harm to themselves and your organisation. In order to ensure a good grasp of both the dangers and solutions to phishing is a simulation service that can be used for improving awareness and training.
3. Identify and address software vulnerabilities
It is integral that you understand your technological shortcomings before an attacker does. Vulnerabilities are common across networks and applications. Organisations should regularly scan their networks, remediate any identified issues and ensure that they have a formal patching process that is adhered to. The team must implement mitigating controls and diligently monitor systems for suspicious activity. There are many instances in which breaches happen due to delays in patching smaller issues, so this should become a priority for your company.
4. Prevent malware from executing inside your network
Anti-malware technologies can be very useful in preventing or restricting ransomware execution. Every system in your organisations should have sufficient anti-malware technologies installed and configured to actively block malicious activity. This should also be regularly updated. The best method is to use an endpoint detection and response system, as they include more capabilities and allow for
The steps that organisations need to take are: allocate separate privileged access accounts to users and not allow them to be shared, provision privileged accounts with the minimum level of permissions required; and ensure that privileged access accounts are not used for daily activities, prohibit them from accessing the network remotely, ensure that they all require strong authentication and MFA to access, closely monitor use of these accounts, alert and investigate anything suspicious, harden systems (especially Active Directory), and review access controls regularly.
In conclusion, it is vital that healthcare organisations take cyber security extremely seriously. With so much personal information stored online, any breach can have long-term effects. Investment into preparation for disruptive attacks, whether it’s time or money, will help you feel secure against the threats of hackers and have confidence in the fact that your data is safe.

is a named supplier on Crown Commercial Service’s Cyber Security Services 3 framework and offers end-toend services covering every challenge throughout your cyber security journey.

For Cyber Security Month, Mike Fell, NHS Digital’s executive director of national cyber security operations laid out his top security tips for health and social care workers
Fell joined NHS Digital in April having previously worked in security at HMRC and the Foreign and Commonwealth Office.
He said: “From email and social media to online banking and shopping, it has never been so crucial to take vital cyber security steps to prevent criminals getting hold of data, devices and accounts.

“Here in the NHS, getting cyber security wrong has the potential to cause significant impacts across the health and care system.
“If a GP can’t access their system, they may not be able to share life-saving prescriptions with pharmacies or critical information with hospitals. Similarly, cyber attacks can cause cancelled appointments and surgeries, possibly resulting in care diversion to other hospitals.
“Cyber security is as important as health and safety, and in just the same way it’s the responsibility of every person in the NHS to understand security risks and what they can do to reduce them. Fortunately there are a few simple steps we can all take to ensure we stay cyber resilient at home and work.”
Strong password
Fell’s 8 top tips include using a strong password to make it difficult to crack. This means making it longer and more complex. It should be easy to remember but hard for someone else to guess.
He urged people to be aware of phishing scams which are getting cleverer and more realistic. Cyber criminals use email, websites and phone calls to steal information. Warning signs include spelling mistakes, incorrect branding, suspicious hyperlinks or urgent titles and requests. Suspicious emails should be reported to spamreports@nhs.net.
People should be mindful of what they share, for example by not wearing their ID pass out in public or sharing it on social media. Sharing information online means you are easier to socially engineer – this is when criminals use tricks or deception to manipulate people into giving them access to data or systems.
Fell warned staff to watch out for tailgaters who could gain unauthorised entry to protected areas. Tailgaters could follow a member of staff through a security barrier to an area they are not authorised
to be in. Staff are reminded to not be afraid to challenge or ask for ID.
Keep up to date with training NHS staff should keep up to date with data training. The more you know, the less the risk of service disruption. Data breaches can lead to reputational damage, fines and most importantly, service disruption.
Fell reminded healthcare workers to never leave computer or mobile devices unlocked – an unlocked device is an easy target.
People are reminded to stay safe when using public WiFi and be careful when connecting to public or unknown networks. Finally, Fell highlighted the resources that are available. NHS Digital’s Keep I.T. confidential campaign has an online security awareness toolkit. The toolkit includes practical steps for staff to implement in their everyday job such as those listed above including, secure passwords and keeping devices locked.
Fell concluded by saying: “I understand how busy everyone is across the NHS right now, but I would encourage everyone to make sure cyber security is a top priority.
“Once you start taking these small steps, they will become a natural part of your day-to-day work, which will in turn help to make a massive difference to protecting crucial information as well as the safety of patients.” L
Fell’s advice and further information on cyber security in the health sector is available here: https://digital.nhs.uk/
securityCyber is asimportant
and safety
With tens of thousands of dormant medical devices set to be connected to IT networks in the next 2-3 years, potentially exposing our healthcare systems to thousands of vulnerabilities, how can hospitals and healthcare settings mitigate risk to patient safety and care?

Our healthcare delivery system is automating. Through a process of digitalization and adoption of advanced technologies, this is something that has been ongoing for the past 20 years. We have moved from medical records maintained in manila files at each treatment location, to centralised electronic record keeping and full interoperability between discrete medical systems. This includes a long list of users from GPs to hospitals to pharmacies and to government aggregate population and public health systems. These changes have brought about a dramatic growth of medical devices. These now dominate hospital patient bedsides and act as nurse and monitor. Medical devices are growing at 20 per cent per year globally and at about 6 per cent per annum in the UK. Many of the medical devices found in NHS hospitals and clinics today are not currently connected to the network but are used in a standalone capacity. This however is about to change through interconnectivity and efficiency improvement goals. That means many more connected devices on healthcare networks.
Medical devices include X-Ray, CT and PET scanners, MRI and radiotherapy machines, to pharmacy robots that dispense medications, to Pyxis cabinets that secure those medications on hospital floors until they are needed, to simple connected infusion pumps and patient telemetry systems that report everything from O2 saturation levels and pulse rate, to automated blood pressure cuffs. They include diagnostic, treatment, patient management and monitoring systems and are ubiquitous across medical providers today.
Most of these are employed in hospitals and clinics, but an increasing number of traditional and wearable devices are sent home with patients following procedures allowing care teams to monitor patients remotely from their homes. Since the advent
of COVID-19, the numbers of remotely monitored patients has gone through the roof, and these systems are connected back to hospitals across the Internet. Together medical devices account for more than 75 per cent of connected endpoints at hospitals, and dwarf those devices managed by IT. Instead of being managed by IT and security, medical devices are usually managed by clinical engineering or biomed technicians, or a mixture of different vendors, many doing so remotely from outside of the hospital. Most of these technicians know little about cybersecurity and IT, and report outside of the IT department in health systems. So historically, there has been very little cybersecurity oversight of medical and other healthcare IoT (HIoT) devices. Nor has there been good cross-walking between teams, though this is changing rapidly. Unlike traditional IT systems such as workstations and laptops, medical and HIoT devices are quite different. They have very limited CPU, memory and storage capacity, so limited in fact that updated firmware and software that requires a larger footprint cannot be supported. So few are ever patched or updated. Many of these pose a security risk to healthcare networks because of the number of unpatched/unpatchable vulnerabilities that they carry.
Unlike a Windows workstation that has a useful lifespan of two to three years, many medical devices are expected to perform for 15 years or more before finally being retired and scrapped. They are in fact amortized in hospital finances to depreciate over this period so early retirement is usually not an option given the state of healthcare finances. Combined with this, few manufacturers are willing or good at providing timely patches against known CVEs and threats in the wild
that affect their systems, even when these systems will support a patch or update, nor have governments mandated that manufacturers do so.
The result is that healthcare suffers from growing cybersecurity risks that could result in another WannaCry cyberattack that takes down much of the NHS and other health systems.
Medical devices can easily be turned into footholds on the network by hackers looking to exfiltrate valuable data or by cyber extortionists spreading malware or ransomware. Medical devices are often attached on one side to the network and the other side to a patient. The patient is thus very thinly isolated from attack over the internet by perpetrators thousands of miles away. Medical devices such as ventilators are used to keep patients alive, yet security is often totally missing on these devices. Few of us would conduct our internet banking on an unpatched 15-year-old PC, yet we trust the health and wellbeing of our loved ones to old unpatched medical devices.
So, what can be done to reduce risks as existing HIoT systems are connected and to the growing number of new and other devices? The biggest issue is that traditional network vulnerability scanning will crash, break, or permanently damage fragile medical devices. Second, that hospitals generally have a really poor inventory of what devices they own, where they are located and what firmware and software levels each maybe running. And third, that patching devices is difficult even when patches are made available by manufacturers. We need tools that use advanced technologies like artificial intelligence to identify and profile inventory, and risk assess medical devices passively so as not to harm fragile systems yet still meet industry governance compliance standards. From that profile we can easily establish a baseline of ‘normal’ network activity for each device and quickly alert when anomalous traffic is attempted – perhaps a sign that a device is being compromised.
medicalManydevices found in NHShospitals/ clinics todayare not connected tothe network but areused in a capacitystandalone
We can also apply compensating security controls to highly vulnerable devices that cannot be patched using existing technologies already owned by trusts and built into their networks. Network Access Control can ‘enclave’ or ‘micro-segment’ all at-risk devices and thus provide an additional layer of protection. With the right tools this can be done easily with a simple click of a switch. This avoids having to ‘get nasty’ with manufacturers for security patches, or the need to strike manufacturers that do not support their devices with timely patches from the approved list of manufacturers for future purchases.
With compensating controls in place, providers can safely continue to use unpatched devices and still be compliant while operating at an acceptable level of risk against cyberattack. Patients are safe, the integrity of the healthcare network is safe, and hospitals don’t need to find millions of pounds to replace perfectly working devices that manufacturers are not providing patches for.
So, what should be done to ensure that devices currently being used in a standalone manner are safe to connect to the network? First, these devices need to be assessed for current versions and patched where patches are available. Second, all medical devices should be joined to separate firewalled network segments from PCs and everything else. This does not mean a simple separate VLAN (Virtual local Area Network) but a firewalled network zone. This will protect medical devices from critical HIT and vice versa. Third, security and clinical engineering/ biomed teams need to work together to reduce any risks as much as possible. Finally, NHS Trusts need to evaluate which manufacturers provide secure devices that are supported in a timely manner and remove all others from approved purchase lists.
Taking these steps will ensure that your healthcare setting is cyber
ready and mitigating against any risk that connected devices could have on patient safety and care. L


4C Strategies is an independent ICT consultancy specialising in technology and infrastructure projects.

The company covers all aspects of technology and infrastructure in the enterprise environment, with consultants showing demonstrable experience in helping clients to procure new technologies to meet their business requirements, providing endto-end support on ICT projects by delivering a portfolio of consultancy services to meet client requirements, from audit and strategy through to procurement, implementation and resourcing.
4C Strategies has been assisting organisations in the healthcare industry for over 20 years. Expertise covers
all aspects of IT technology and infrastructure, including: digital strategy, IT and technology strategy, data centres, servers and storage, patient data security, desktop telephony, Microsoft Teams and wide area networks.
Trevor Nelms, Director from West London Mental Health Trust, said: “4C Strategies has assisted in a range of complex ICT projects, from inception through to deployment, and demonstrated a rare ability to bring together technical expertise with business acumen and tight project management skills.”
Contact one of 4C Strategies’ qualified healthcare technology consultants today. L
Tel: 01858 438938 nhs@4c.co.uk www.4c.co.uk
NHS Trusts need to evaluate which manufacturers provide secure devices that are supported in a timely manner and remove all others from approved purchase listsRichard Staynings, Cylera chief strategist Richard is chief security strategist for Cylera and a globally renowned thought leader, author, public speaker, and international luminary for healthcare cybersecurity.
Yewdale has recently launched two new products which prevent suicide in high-risk environments. In mental health settings, most suicides occur in personal rooms. The en-suite provides privacy and enough time between checks to create a ligature point, often using a traditional en-suite door. SafeDoor 2 is Yewdale’s lifesaving antiligature en-suite door.
Designed to prevent the creation of ligature points, SafeDoor 2 has a Crib 7 fire rating. It’s waterproof, only 9mm thick and has gaps above and below the door to allow observational checks whilst maintaining privacy and dignity.
Introducing vibrant colours
and relaxing imagery can help create a therapeutic environment and reduce anxiety. With that in mind, Yewdale launched their anti-ligature artwork called SafeArt. Any high-resolution image can be printed on SafeArt, and Yewdale offer a selection of stunning nature photography images.
SafeDoor 2 and SafeArt utilise magnets which ensure the products fall safely under an excess load, preventing ligature. They are constructed from soft foam which poses minimal weapons risk once removed. The magnetic system provides a lifetime of trouble-free service because magnets take hundreds of years to lose their strength.L
www.yewdale.co.uk grant@yewdale.co.uk 01268 570900

temperatures that affect the stability of pharmaceuticals.
Tinytag data loggers
reliable devices for monitoring and validating temperatures of vaccines and pharmaceuticals in storage and transit.
Designed and manufactured in the UK by Gemini Data Loggers since 1984, Tinytag data loggers have provided economical temperature monitoring solutions to the NHS and healthcare professionals for over 35 years. With a compact and portable design, Tinytag data loggers can be situated inside vaccine fridges and freezers, in cold rooms and in temperature-controlled vehicles and packaging to continuously record the
Data loggers for vaccine monitoring include the costeffective Tinytag Talk 2 medical data logger, designed for use in vaccine fridges. The small data logger can be placed directly alongside vaccines in cold storage to precisely monitor the conditions that vaccines experience.
At the end of the monitoring period, recorded data can be viewed and assessed using easy-to-use data logging software.
For fuss-free, costeffective vaccine monitoring, Tinytag data loggers are the simple choice.

To find out more, please contact Gemini Data Loggers or visit the website below.
sales@tinytag.info 01243 813000 www.geminidataloggers.com

















Keeping in touch Your support makes a life-changing difference to people in crisis. We write to our supporters to update you about the work of the British Red Cross, and how you can help and donate in other ways. You can change the way we contact you at any time by visiting redcross.org.uk/keepingintouch or calling Freephone 0800 2800 491.
Privacy statement The British Red Cross is committed to privacy and will use personal data for the purpose it was collected or other legitimate purposes we tell you about: for example, to provide goods, services or information you have requested or to administer donations or services we provide. We may also analyse data we collect to better understand the people who support us or those who use or deliver our services. Sometimes this means us combining that data with information from reliable public sources. Our research allows us to tailor communications and services in a more focused and cost-effective way, as well as better meeting your needs and the needs of others like you. However, we will never do this in a way that intrudes on personal privacy and will not use your data for a purpose that conflicts with previously expressed privacy preferences. For full details about how we use personal data, our legal basis for doing so and your privacy rights, please see our privacy notice online at redcross.org.uk/privacy.
The DEC Ukraine Humanitarian Appeal will support people in areas currently affected and those potentially affected in the future by the crisis. In the unlikely event that we raise more money than can be reasonably and efficiently spent, any surplus funds will be used to help us prepare for and respond to other humanitarian disasters anywhere in the world. For more information visit https://donate. redcross.org.uk/appeal/disaster-fund



*Texts cost £10 +1 standard message (we receive 100%). For full T&Cs visit redcross.org.uk/mobile, must be 16+.











The British Red Cross Society, incorporated by Royal Charter 1908, is a charity registered in England and Wales (220949), Scotland (SC037738), Isle of Man (0752) and Jersey (430).



