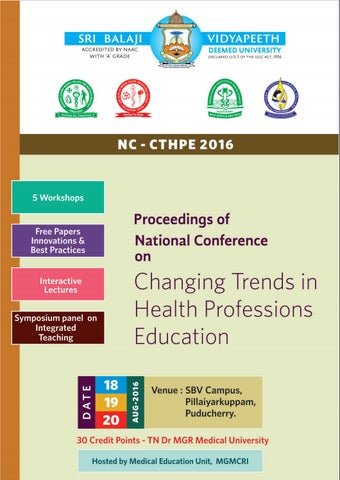
National Conference on Changing Trends in Health Professions Education Chief Patron
Shri MK Rajagopalan Chairman, Sri Balaji Educational and Charitable Public Trust
Patrons Prof. P Rajaram Chancellor, Sri Balaji Vidyapeeth
Prof. KR Sethuraman Vice-Chancellor, Sri Balaji Vidyapeeth
Advisors Prof. N Ananthakrishnan, Dean- Research and AHS, SBV Prof. M Ravishankar, Dean, MGMC & RI Prof. Carounanidy Usha, Dean, IGIDS Prof. K Renuka, Dean, KGNC Prof. AR Srinivasan, Registrar, SBV Prof. Nirmal Coumare, MS, MGMCRI
Organizing Chairman
Dr.Balachandra V Adkoli Prof. of Medical Education, MGMCRI
Organizing Secretary
Dr SeeteshGhosh Coordinator, MEU, MGMCRI
Treasurer
Dr.VN Mahalakshmi, Vice Principal (Curriculum), MGMCRI
Core Committee Members Dr.K.A.Narayan Dr.Partha Nandi Dr.Jagan Mohan Dr.R.Kannan Dr.A.N.Uma Dr.Ganesh Babu Mrs. Asha Suresh Babu Mr. Kannan Iyer
NC-CTHPE 2016
2
National Conference on Changing Trends in Health Professions Education
Index
S.No
Content
Page No.
1.
Messages
2.
From the desk of the Organising Chairman
16
3.
From the desk of the Organising Secretary
17
4.
National Conference on Changing Trends in Health Professions Education - NC-CTHPE 2016 – A Curtain Raiser - Dr B.V. Adkoli.
18
5.
About Medical Education Unit of MGMCRI - Dr Seetesh Ghose& Dr B.V. Adkoli.
24
6.
Innovative Programs in Health Professions Education - Prof K A Narayan
32
7.
Scientific programmes
42
8.
Resume and Abstracts of invited talk
46
9.
Abstracts of Free paper sessions
84
10.
Workshop Materials [Attached in separate folder]
NC-CTHPE 2016
4
108
3
National Conference on Changing Trends in Health Professions Education
Messages
NC-CTHPE 2016
4
National Conference on Changing Trends in Health Professions Education
MESSAGE FROM THE HONORABLE CHAIRMAN
I am indeed delighted to note that our Mahatma Gandhi Medical College & Research Institute (MGMCRI) and our Indira Ganndhi Institute of Dental Sciences (IGIDS), have joined together in hosting this National Conference on Changing Trends in Health Professions Education from 18th to 20th August 2016. It is a matter of pride for Shri Balaji Vidyapeeth to host this conference because of two reasons. The theme of the Conference is Faculty Development and Innovations in Education which together are critical factors for our SBV Mission of producing doctors, dentists, nurses and allied health professionals of high caliber, to face the challenges of future. Secondly, this conference is led by the key academic leaders from MCI, DCI and a galaxy of experts gathered from various centres of excellence in India, with whom we can mutually share our experience. I wish the Conference every success and hope that it will serve as an important mile stone in our journey towards excellence.
Shri M.K. Rajagopalan, Chairman, SBECT
NC-CTHPE 2016
5
National Conference on Changing Trends in Health Professions Education
MESSAGE FROM MESSAGE FROM HON’BLE CHANCELLOR Faculty Development Program (FDP), indeed, is an essential component for the growth of an institution. Faculty, besides executing the laid down curriculum, are also expected to bring out their hidden ability in producing physicians of tomorrow with leadership qualities having ethical values. At SBV, we have excellent infrastructure with various in-house plans, from human resource development to social welfare programs including counselling for carrying out jobs meticulously. Therefore, faculty of SBVU are in a position to share ideas with others and to emerge as leaders. However new ideas must be explored to prevent intellectual decay in medical profession plaguing the medical education. Prospective younger professionals should be identified to become model teachers and researchers, holding frequent conferences involving the faculty from rural institutions. Stress should be laid on leadership and self-development besides curriculum implementation and on the need to serve the community in preventive and promotive medicine. Emphasis on research and harnessing of information technology for the benefit of people coming from far-flung institutions through video conferencing are other areas to be looked seriously. Faculty development is a process by which the profession grows systematically. Educational skills that they learn will help them become effective leaders with intellectual ability to promote profession. The teacher-taught relationship and ethical aspects of patient care will improve. A teacher must always be enthusiastic to learn and teach only to learn. He should stress communication skills, mannerism and physician’s obligations towards patient’s rights. Teaching and training must include tools and technology for advanced patient care. A teacher must have vibrant ideas to share with colleagues and students that will contribute towards the development of the institution. The overall aim should be, developing a culture of co-operation and confidence. The Management has recognized the importance of faculty development program. Let the current faculty sow the seeds for the tree to grow and bear fruits that will ultimately benefit the community in preventive, promotive, curative and rehabilitative medicine. I wish the conference a grand success.
Prof. Rajaram Pagadala, MD (ObGyn), DSS (Surg. Onco., Vienna), PhD (Pop. Studies), WHO Dip. (Hlth.Econom. Thailand)
Chancellor
NC-CTHPE 2016
6
National Conference on Changing Trends in Health Professions Education
MESSAGE FROM THE VICE CHANCELLOR
Having been a key resource person trying to nurture Health Professions Education here at Sri Balaji Vidyapeeth (SBV) since 2013, I am personally delighted that the Faculties of Medicine, Dentistry and Allied Health Sciences are jointly conducting the ‘National Conference on “Changing Trends in Health Professions Education” (NC-CTHPE)’ at SBV from 18th to 20th of August, 2016. It is especially heart-warming to note the Dental Council of India (DCI) as well as the Medical Council of India (MCI) have permitted senior officials to be here at this rural health sciences Varsity to participate in this event and share the Vision of DCI and MCI, which will greatly help and guide the medical and dental institutions on ushering in relevant and meaningful changes envisaged by the Councils for the betterment of healthcare outcomes in India and rest of the Globe. It is equally heart-warming to note that several senior and well-known educationists of India have accepted our invitation to be resource persons and facilitators to share their experiences through key-note talks and hands-on workshops. The organising teams of both the segments of NC-CTHPE (viz., Dental education & Medical education teams) have worked tirelessly to make the 3-day event a reality. They deserve appreciation. I wish NC-CTHPE, a 3-day extravaganza in health professions education a successful outcome in terms of further improving the health-professions education and practice in India. Prof. K. R. Sethuraman. MD, PGDHE. Vice Chancellor – SBV
NC-CTHPE 2016
7
National Conference on Changing Trends in Health Professions Education
MESSAGE FROM THE REGISTRAR It is a pleasure to learn that the Medical Education Unit, MGMCRI, along with Dental Education Unit, IGIDS, are jointly organizing ‘National Conference on “Changing Trends in Health Professions Education” (NC-CTHPE)’ at SBV from 18th to 20th of August, 2016. This conference is extremely important for Sri Balaji Vidyapeeth in our mission of producing high caliber health professionals in Medical, Dental, Nursing and Allied Health Sciences. The UGC and NAAC have strongly recommended Choice Based Credits System (CBCS) as a major reform in higher Education, which our new programs in Health Professions Education have introduced successfully. The UGC is also working on the concept of introducing MASSIVE ONLINE OPEN COURSES (MOOC) and SBV is keen to emerge as a National MOOC Center in carrying forward these initiatives. The Changing Trends in Health Professions Education which this conference is expected to deliberate are therefore in perfect harmony with the mission and vision of SBV. I wish the conference a grand success. Prof. AR Srinivasan Registrar Sri Balaji Vidyapeeth
NC-CTHPE 2016
8
National Conference on Changing Trends in Health Professions Education
MESSAGE FROM THE DEAN RESEARCH AND AHS
Sri Balaji Vidyapeeth has consistently been in the forefront in keeping pace with advances in Medical education both at the Undergraduate and Postgraduate levels. In pursuance of this policy, several innovative measures have been taken, such as, bringing about integration in undergraduate teaching early exposure of undergraduates to the community and to elements of research, introducing Yoga in the undergraduate medical and nursing curriculum, introducing a competency based curriculum for Postgraduates for the first time in the country and starting courses in Health Professions Education on an inter- disciplinary basis such as the Postgraduate Diploma in Health Professions Education, the M.Phil degree and Doctorate in Health Professions education. Simultaneously, the University has focused attention on recent advances and changing trends in medical education. The first such conference was held in the year 2013 on Recent Advances in Medical education and the second on Changing Trends in Health Professions Education is being held during 18th -20th August, 2016. Leading experts in the fields from all over the country will be visiting SBV to participate in this programme and share their experiences with SBV and the audience. SBV is also projecting its own endeavors in this field. I am sure the deliberations of this three day programme, the first day being devoted to dental education and the second and third days to medical education, will go a long way in highlighting important issues which every institution training medical Undergraduates and Postgraduates must take cognizance. I am sure all participants will find the programme very useful and relevant. Prof. N. Ananthakrishnan, MS., DNBE, FRCS (Eng. Edin., Glasg.) FAMS, FICS. FACS.FACG.FIMSA. Dean - [Research & Allied Health Sciences] Sri Balaji Vidyapeeth
NC-CTHPE 2016
9
National Conference on Changing Trends in Health Professions Education
MESSAGE FROM THE DEAN
Curriculum for health profession needs to focus on the requirements of the community of the 21st century. Enormous development that has taken place in the understanding of the mechanism of disease production and modalities of treatment has not been matched with change in curriculum. Faculty Development Programs (FDPs) have been recognized as a major instrument for bringing about this change. In a vast country like India, the ideas need to be shared, discussed and debated for a meaningful implementation of the desirable changes.
I am happy that Sri Balaji Vidyapeeth has organized a National Conference on Changing Trends in Health Professions Education (NC-CTHPE 2016) from 18th to 20th August 2016. I am quite certain that the national level faculty in both Dental education and Medical education will deliberate on issues of importance and teach the faculty on the modalities of bringing about these changes that are essential.
I wish the conference all the success.
Prof. M Ravishankar, MD, DA., FRCP Dean MGMC&RI
NC-CTHPE 2016
10
National Conference on Changing Trends in Health Professions Education
MESSAGE FROM THE MEDICAL SUPERINTENDENT I am happy to note that our Medical Education Unit and Dental Education Unit under the aegis of Sri Balaji Vidyapeeth have joined together in hosting the National Conference on Changing Trends in Health Professions Education. While education, patient care and research constitute a trinity of our mission, it is difficult to say which is more important than the other. We can’t achieve high quality patient care unless we recruit and retain teachers of high caliber. Because, teachers are instrumental in training health professionals who are competent and committed to deliver patient care of high quality. With hospital systems becoming more complex and interdependent, we need to train our health manpower in a different manner to develop a competent professional who is oriented to ‘high tech’ as well as ‘high touch’ aspects of medicine. This necessitates a clarion call from the academicians to identify the changing trends in education and selectively imbibe the best practices that contribute to patient care and quality services. In this context the National Conference on Changing Trends in Health Professions Education is a most welcome initiative to move further. I wish the Conference every success. Prof. V Nirmal Coumare Medical Superintendent, MGMC&RI
NC-CTHPE 2016
11
National Conference on Changing Trends in Health Professions Education
MESSAGE FROM THE DEAN DENTAL Improvement in quality of health care delivery, by way of relevant and effective health professions education, has been the focus of interest since the turn of the 20th century. Beginning with the popular Flexner’s report in 1910, numerous committees, both at the international and national level, have addressed various issues in medical education, at varied time periods. These exhaustive reports have indeed changed the way this profession is being learnt and practiced. Some of the issues that repeatedly appeared almost in every report are implementation of the need based/ competence based curriculum and integration of basic and clinical knowledge. Acquiring professionalism had also been one of the steady goals in health professions education since yesteryears. However, despite such constant efforts, chasm continues to exist between the patient service and health professions education. Currently it seems to be deepening and widening. Ironically, this might be due to knowledge explosion and rapid–paced technological advancements in all health professional subjects. Distilling appropriate knowledge from facts and translating them into patient service skills, without getting lost in professional silos, is the current challenge for both teachers and learners. ICT in education, which has changed the instructional methods and media, is yet another force to reckon with. Increased life span and changing life styles have changed the needs/ wants and preferences of health care of public. Such changes and challenges, therefore mandates that Health professions education system also transforms accordingly and dynamically, so as to bridge the gap between service and education. It is heartening to note that the transformation has already begun; a beginning that is promising a major revolution in HPE in the immediate future. This conference on health professions education focusing on changing trends, is a standing proof for such process. The conference also reiterates the point that education system is an open and conducive system and one has to constantly update, upgrade and evolve in educational technology in order to keep pace with the environmental changes outside the system. I am very happy and proud to be part of this educational endeavour of Sri Balaji Vidyapeeth. I am sure every delegate will take home some fond memories, knowledge and skill; but most of all they are sure to become a part of the change that they wish to see in HPE! Dr. Carounanidy Usha Dean, Faculty of Dentistry Sri Balaji Vidyapeeth
NC-CTHPE 2016
12
National Conference on Changing Trends in Health Professions Education MESSAGE FROM CHAIRMAN, ACADEMIC COMMITTEE
NC-CTHPE 2016
13
National Conference on Changing Trends in Health Professions Education
MESSAGE FROM THE PRESIDENT, SOUTH EAST ASIAN REGIONAL ASSOCIATION FOR MEDICAL EDUCATION (SEARAME)
Greetings from SEARAME It gives me great pleasure to learn that Sri Balaji Vidyapeeth, Puducherry is organizing a National Conference on “Changing Trends in Health Professions Education� from 18th - 20th, August 2016. We at SEARAME are concerned and committed to make medical education more responsive to the needs of South East Asian Region. At the same time, we need to align with the international trends in the field through our partnerships with WHO, World Federation for Medical Education (WFME) and National networks of health professions education of the member countries. In this context, the above theme chosen for the conference is timely and appropriate. Faculty Development has been recognized as a key instrument in bringing about desirable changes in the curriculum. It is heartening to note Sri Balaji Vidyapeeth has taken a bold step in this direction, by launching new programs and synergizing the activities of medical, dental and nursing colleges. This move can meaningfully contribute towards inter-professional education, which is an important and effective step towards development of human resources for health to meet the health care needs of the populations. I am sure, the leaders and the delegates participating in this conference will be able to make a great stride in their march towards quality and excellence in health professions education. I wish the conference a great success.
Dr Rita Sood President, SEARAME
NC-CTHPE 2016
14
National Conference on Changing Trends in Health Professions Education
MESSAGE FROM THE SEARAME SECRETARIATE
SEARAME is happy that Sri Balaji Vidyapeeth University is playing a leadership role in facilitating the improvement in the quality of medical education by hosting this National Conference on “Changing Trends in Health Professions Education� (NCCTHPE 2016) as well as provide opportunities for capacity building through workshops on topics that are relevant and addresses the capacity-building needs of faculty in India. This is in line with the mandate with which SEARAME as an organization was formed. As you all know, SEARAME is a regional non-government organization interested in enhancing the quality of Medical Education by promoting the highest Standards in Medical Education among the member countries of the South-East Asia Region of the World Health Organization (WHO) with which it is in strategic partnership to achieve the above mentioned purpose. The parent Organization of SEARAME is the World Federation for Medical Education (WFME) with the mission of quality improvement in Medical Education met through the development of standards in medical education, by the facilitating accreditation of National Accreditation bodies that do accreditation of medical schools, with the development of databases on resource persons for medical education, through projects on the future of medicine and medical education, and through other publications and partnerships. We are sure that the program laid out by the organizing committee will achieve its intended purpose and also contribute to building the community of practice of Health Professions Educators in the region. Best Wishes Thomas V Chacko Secretary-General, SEARAME
NC-CTHPE 2016
15
National Conference on Changing Trends in Health Professions Education
FROM THE DESK OF THE ORGANIZING CHAIRMAN
Medical education in our country is confronted with several issues which are quite complex and at times complicated. The need to train right type of doctors at right place, to strike a balance between quality and quantity, to selectively assimilate various innovations in to the curriculum in the backdrop of burgeoning information – all these point out to a single most important instrument, viz., faculty development. A lot of emphasis is being laid on introducing competency based education, integrated teaching, developing professionalism and ethics, encouraging transformative learning, and stimulating inter-professional education. All these issues can be successfully implemented provided we have a faculty development mechanism in place. The National Conference on Changing Trends in Health Professions Education hopefully provides a platform for some of the best brains in the country to collectively deliberate on these issues. Thanks to the initiatives taken by the MCI, Regional and Nodal Centres, FAIMER Regional Centres, NTTCs and other leading centres of medical education in India, we are witnessing significant progress in this area in recent years. In line with these trends, Sri Balaji Vidyapeeth has also taken some initiatives for launching curricular reforms in the undergraduate and postgraduate programs. By starting a new forum called SBV Academy for Health Professions Education and Development, popularly called SBV AHEAD, it has also launched some innovative courses in Health Profession Education based on the Choice Based Credit System (CBCS) recommended by the UGC and at par with the advanced programs like FAIMER or FIME introduced by the MCI. However, in a vast country like India, the ideas need to be discussed, debated and shared extensively for facilitating smooth implementation of the best practices. It is my pleasure and privilege to be a part of this August Gathering which is an important mile stone for SBV AHEAD to really move ahead with commitment and confidence. Prof. B.V. Adkoli Organizing Chairman, NC-CTHPE
NC-CTHPE 2016
16
National Conference on Changing Trends in Health Professions Education
FROM THE DESK OF THE ORGANIZING SECRETARY
Medical education in our country is faced with the challenges of producing a right type of doctors who can meet the future challenges of rising expectations of patients, in the backdrop of globalization, market forces and changing technologies. With the realization that effective health delivery is possible only with a team work and inter-professional education, the emphasis has been laid on a broader concept of Health Professions Education with an aim to prepare practicing professionals in medicine, nursing , dentistry, public health, and allied health sciences who can serve as an educational leaders. This conference is an attempt to address the issues in health professions education as a whole, through lectures, panel discussions and workshops conducted by the stalwarts in the field of health professions education from all over the India . It gives me immense pleasure to be a part of organizing team and conducting this National Conference on Changing Trend in Health Professional Education. I wish this conference will help all the delegates in gaining insight into the health professions education for their continuing professional development. Dr.Seetesh Ghose Organizing Secretary NC-CTHPE
NC-CTHPE 2016
17
National Conference on Changing Trends in Health Professions Education National Conference on Changing Trends in Health Professions Education- NC-CTHPE 2016 – A Curtain Raiser
Dr B.V. Adkoli, Professor, Dept., of Medical Education, MGMC& RI The Genesis The quality of health care delivery depends largely on the quality of training which in turn is linked with the competence and the commitment of the faculty to facilitate the implementation of expected reforms. The last decade has witnessed an unprecedented growth in the enrolment of students in health professions at the same time shortage of faculty to cope with this demand. New curricular strategies have been identified, and new modalities of learning have been explored. However, what is needed is a consensus on how we can address various innovations and mould our Faculty Development Programs (FDPs) to meet the challenges of implementing the curricular reforms mooted by the MCI, UGC and other decision making Bodies. The National Conference on Changing Trends in Health Professions Education (NC-CTHPE 2016) is an attempt to address innovations and best practices in education and the modalities of bringing about changes through sustained faculty development efforts. Background Faculty Development Program (FDP) in Medical Education has a long history, though the importance attached to it has reached a new height only recently. Thanks to initiatives taken by NTTCs in 1980s, and later by other Centres of Medical Education in India, followed by the formation of Indian Consortium of Medical Institutes during 1990’s a ground work had been already laid for faculty development to take off. The establishment of three FAIMER Regional Centres at CMC Ludhiana, Seth GS Medical College Mumbai, and PSG Institute of Medical Sciences & Research at Coimbatore provided a new wave of enthusiasm to engage in Fellowship programs including International Fellowship in Medical Education (IFME). Several advanced Centres such as Maharashtra University of Health Sciences (MUHS), KLE University, Belgaum, Manipal University also introduced advanced programs in medical education. The real impetus for the FDPs came from the combined effect of two initiatives taken the MCI since 2009. The first one was the recommendation to establish Medical Education Units (MEUs) in each medical college to run Basic Course Workshops for sensitizing all faculty, as a mandatory requirement, supported by the establishment of a network of Regional Centres and Nodal Centres to prepare faculty for leading FDPs through advanced courses and a Fellowship program in Medical Education (FIME) on a more organized basis. This was indeed, a fall-out of MCI Regulations of 1997 which were based on the work of the Consortium of Medical Institutes.
NC-CTHPE 2016
18
National Conference on Changing Trends in Health Professions Education
Closely associated with this initiative is the Vision 2015 document prepared by the MCI and the MCI Regulations of 2012 which made some important recommendations such as the concept of Indian Medical Graduate, introduction of foundation courses during the first year of MBBS, early clinical exposure, the role of Attitudes and Communication Skills through a modular approach (popularly called ATCOM Modules), integrated teaching, impetus to clerkship experience and structured internship. It was recognized that successful implementation of these reforms required a strong faculty development program in place. MCI soon revised the basic course and the Regional Centres are presently engaged in sensitizing the faculty with the Revised Basic Course Workshops and one day sensitization workshop for integrating ATCOM modules in to the curriculum of MBBS. Initiative by Sri Balaji Vidyapeeth One of South India’s premier healthcare academic and research institutions, Sri Balaji Vidyapeeth (SBV) has been at the forefront of health professions education, healthcare delivery and research ever since its inception in 2008. Sri Balaji Vidyapeeth is accredited by India's National Assessment and Accreditation Council (NAAC) with 'A' Grade and is ranked among top eight Medical Universities in India by NIRF. The vision of SBV is to be in the forefront of higher education in order to give the country high calibre manpower. The Mission statement envisages collegiate education that culminates in post doctoral programmes, to produce knowledgeable professionals in various aspects of health science with a high concern for providing and organizing appropriate health services including health education and policy, to provide service to the underprivileged, to impart specialized skills, to be successful in their endeavours and to set a high standard of professional conduct and ethics for staff and students alike. The Medical Education Unit, being upgraded as Dept of Medical Education, has made significant strides in launching several innovations in UG and PG Education. Faculty development activities are not limited to the sensitization of faculty alone, but include a variety of high quality programs/workshops for the Postgraduate students, Interns and Undergraduate students. Thanks to the collaborative arrangements made between SBV and the Partners Medical International (PMI) Harvard, a new wave of activities have been organized in the recent past including Competency Based approach to PG Medical Education besides integrated teaching, sensitization of faculty on ATCOM Modules, exploring the use of Standardized patients for developing communication skills, orientation of junior faculty to Research Methodology, and addressing problems of Students Needing Additional Curricular Support (SNACS). These initiatives are being discussed elsewhere. More exciting development has been establishment of a separate interdisciplinary forum called Academy for Health Professions Education and Academic Development (SBV- AHEAD) established by Sri Balaji Vidyapeeth, to bring together and support all health professionals to achieve academic excellence through training and research in educational science and technology. With the presence of medical, dental
NC-CTHPE 2016
19
National Conference on Changing Trends in Health Professions Education
and nursing institutes in one campus, the University is uniquely placed to launch innovative programs in health professions education. Sri Balaji Vidyapeeth, as a part of the innovative initiatives, launched a one year Post Graduate Diploma in Health Professions Education (PGDHPE) in 2014, to cater to the needs of medical and nursing faculty of SBV, who aspire to develop as educators and leaders in their field. Inspired by the success of this course, and to provide a new pathway for the aspiring teachers across the health profession, it has recently launched a credit based program with following options: a) Pursue Certificate Courses of three months duration (total four courses of 8 Credit points, each), with options for exit after any course, thus obtaining a course completion certificate b) Obtain PGDHPE after successful completion of comprehensive examination, based on Four Courses of study, and completing a mini-project and portfolio (32+4=36 Credits). Again there is an option to exit or continue further. c) Continue further to M. Phil program of one year (36 Credits), subject to the candidates’ holding a Master’s Degree. This program eventually leads to Ph D Program in Health Professions Education.
4 Certificates (32 Credits)
PGDHPE (36 Cr)
M. Phil (36 Cr)
Ph D
FIGURE 1: CAREER PATHWAY IN HPE The major highlight of the new programs is adoption of Credit Based Choice System (CBCS) recommended by the NAAC and UGC as a major reform in higher education. As a corollary to this system, a competency based approach has been proposed for the new program. The model proposed by the SBV needs to be examined, and evaluated for its possibility of adoption at a national level. The NC-CTHPE 2016 : Agenda and the Themes National Conference on “Changing Trends in Health Professions Education (NCCTHPE 2016) is an attempt to bring together, key decision makers and medical / health professions educators to deliberate on the strategies for implementing various innovations and best practices in faculty development that can impact quality of medical/health professions education.
NC-CTHPE 2016
20
National Conference on Changing Trends in Health Professions Education Objectives of National Conference (NC-CTHPE 2016)
1. To survey and assess the global trends in medical/health profession education vis-Ă -vis, national context and local needs 2. To identify innovations that can be carried out within the existing regulatory frame work with reference to a) Undergraduate education, b) Postgraduate Training c) Faculty Development Programs 3. To compile best practices in Faculty Development that have bearing on improving quality of medical / health professions education The scope of Health Profession Education includes medical education, dental education, nursing and allied health sciences which together constitute the essential health manpower for the country. Unfortunately the sectarian approach to development although contributed to the development of specialties, actually hampered the optimum training and utilization of the health manpower in tune with the requirements at various levels. One of the major developments in response to this malady has been the emerging concept of inter-professional education (integration among medical, dental, nursing and allied health professions) and trans-professional education (integration among health, and other disciplines such as education, biomedical engineering, economics, humanities, law and ethics). Discussion Themes While the first day of the conference is exclusively devoted to Undergraduate Dental education, the deliberations of the main conference will address three major themes: Undergraduate Medical Education, Postgraduate Education and Faculty Development Programs. Levels of Education Undergraduate Education
Themes and sub-themes Innovations in teaching: Integrated teaching, focus on critical thinking, problem solving, clinical skills and soft skills training (Communication, Professionalism and Ethical behavior), mentoring and feedback, Problem Learners or Students Needing Academic and Curricular Support (SNACS) Postgraduate Education Competency Based PG Medical Education Defining Competencies (Entrustable Professional Activities - EPAs); linking EPAs with Multi-Source Feedback and Portfolio approach Faculty Development Best practices in FDPs; Choice Based Credit Programs System (CBCS), blended learning, networking and scholarship development; linking FDPs with career advancement; Transformative learning, Inter-professional education
NC-CTHPE 2016
21
National Conference on Changing Trends in Health Professions Education
The program The program includes key note addresses by the speakers, panel discussions and free paper sessions by the selected participants on the innovations and best practices carried out by them in their own settings. Five Hands on Workshops have been planned as follows: Professionalism Leading and managing changes Problem Learners Clinical skills in a digital era Mentoring and Feedback Expected outcome (Participants’ level)
Increase in the awareness of participants about the changing trends in curriculum planning and implementation Skill enhancement in interactive teaching and training, conducting a comprehensive assessment using Multiple Source Feedback (MSF) and 360○ Assessment Networking with their professional colleagues to stimulate Continuous Professional Development (CPD) and scholarship in medical education Expected outcome (Organizational level)
Dissemination of the proceedings across all participating institutes resulting in the increased awareness of medical colleges about the current trends in medical education and the need to introduce innovations in teaching and assessment. Impetus for other medical colleges to carry forward such activities with added strength and vigor. Questions to ponder The NC-CTHPE will provide a forum for discussing some of the questions that haunt our teachers and academicians for a long term action and intervention:
How can we look assessment in a new perspective to address vital elements such as professionalism, ethics, communication skills and patient safety within the curricular frame work recommended by the regulatory bodies? What are the innovations and best practices that can be implemented at the Undergraduate and Postgraduate level? How to bring about integration both horizontal and vertical across the MBBS course? What are the pro’s and con’s of competency based approach which involves: o Redesigning our approach to teaching learning and assessment? E.g., redefining the professional competencies in to Entrustable Professional Activities (EPAs) o Use of interactive methods, e-learning, and Learning Management Systems (LMS) combined with steps to strengthening clinical teaching in a digital era o Extensive use of mentoring and feedback for addressing the needs of all students and special innovations for the Students Needing Additional Curricular support
NC-CTHPE 2016
22
National Conference on Changing Trends in Health Professions Education
o Application of a wide range of techniques and modalities such as portfolio or eportfolios to document, monitor and assess the students’ progress, using evidence from multiple sources (360○) It may not be possible to find out clear-cut answers for these highly loaded questions within a time frame of two or three days. However, what is expected is that the participants try to discuss these issues threadbare and find out their own solutions in their institutes, departments and class rooms. In conclusion, the success of NCCTHPE depends upon every participant and his/her active participation in the discussions and deliberations to be led by the renowned speakers and local facilitators. As the experience has shown, no governments, no policy makers, and no regulations have succeeded alone in bringing about desirable changes, unless they are backed by active participation of the end user. The end user in this game is the faculty member. But he or she has the responsibility and accountability to reach the benefits to improve the health care delivery of the country, which is the ultimate goal. Acknowledgments: The Management of SBV, Vice Chancellor, Dean, (Research & Allied Health Sciences), Dean, MGMCRI, Resource Faculty, and the Organizing Committee of NC-CTHPE 2016
NC-CTHPE 2016
23
National Conference on Changing Trends in Health Professions Education
Medical Education Unit
Mahatma Gandhi Medical College & Research Institute Dr Seetesh Ghose, Coordinator, MEU& Dr B.V. Adkoli, Professor, Dept., of Medical Education, MGMC& RI Background Information Medical teachers are the architects and builders of students’ competence. Though the curriculum of medical education is decided by the competent bodies, the way in which the curriculum is transacted depends largely upon the competence of the faculty and their preparedness to deliver the curriculum including ‘hidden curriculum’. Thus, it is well accepted that faculty development is a potential instrument for maintaining and enhancing quality of education, which ultimately influences the quality of health manpower and the quality of health care delivery. Realizing this felt need, the Medical Council of India (MCI) recommended the establishment of Medical Education Unit (MEU) in each medical college to sensitize every faculty member in medical education technology. While the faculty in challenge important
focus of most medical colleges in India is on sensitizing and training of harnessing educational technology, the MEU at MGMCRI took up the of going beyond this issue and trying to address the needs of other stakeholders, viz., the residents, interns and the undergraduate students.
Keeping in mind the need to address capacity building of all health professionals, one of the foremost missions, SBV, established a joint forum called Academy for Health Professions Education and Academic Development (SBV-AHEAD) which encompass the whole spectrum of health professions education. It is gratifying to note that the NAAC team during their visit appreciated the vision of SBV to address the whole range of health professions, and SBV’s initiative to launch new innovative programs for preparing educational leaders, rather than medical education experts. This has seen fruition in the form recent launching of PG Diploma in Health Professions Education (PGD-HPE) and M.Phil programs based on the Choice Based Credit System (CBCS) recommended by the UGC as a major instrument for reforming the higher education system in India. Learning from the experience of others, especially from our collaboration with Partners Management Institute (PMI), Harvard, we are charting our own course of action. With the result, MEU has been upgraded as a Department of Medical Education, which is a stepping stone towards our dream of full-fledged Department of Health Professions Education possibly for the first time India.
NC-CTHPE 2016
24
National Conference on Changing Trends in Health Professions Education Vision
The vision of Medical Education Unit is to develop as a Centre of excellence committed to develop faculty as future leaders in medical and health professions education. 1. To organize faculty development programs in medical education technology for the faculty of MGMCRI and others 2. To organize MCI Basic Workshops Courses for the faculty as well as advanced courses for the faculty, leading to higher degree in health professions education, in collaboration with SBV AHEAD 3. To organize sensitization programs for the post-graduate students and interns to enrich their professional growth. 4. To facilitate ongoing quality assurance and maintenance of standards in courses run by MGMCRI 5. To promote inter-professional education in collaboration with dental and nursing education at the SBV. 6. To promote educational research and facilitate partnership with national and international organizations and networks. 7. To explore new frontiers of blended learning for the pursuit of self-directed, lifelong learning of health professionals The Scope of Activities of MEU The scope of activities of MEU has been extended from faculty to address other important stakeholders, viz., PG Students, Interns and even undergraduate students, who are the ultimate beneficiaries of the system.
Faculty
PG students
Interns
ATCOM sensitization
Research Methodology
Competency Based PG ME
Protocol + Dissetration
Induction Program
FDP Workshop Series
Orientation Program
Pedagogy Workshps
UG Students Communication Training Counselling Services
NC-CTHPE 2016
PGDHPE and M.Phil. Progran
25
National Conference on Changing Trends in Health Professions Education
Recent initiatives
The MEU has added a few programs this year including Pedagogy Workshop for the PG students, orientation program for the Basic Sciences Faculty (teaching MBBS first year) and a Workshop series on Research Methodology for the junior faculty of MGMCRI. Another experiment carried out last year has been training and utilization of Standardized Patients for the training of the undergraduates in certain aspects of clinical training, such as history taking and communication skills. The MCI has laid a lot of stress on the teaching of attitudes and communication skills through a modular approach utilizing ATCOM modules. Our MEU has taken this initiative forward not only by sensitizing our faculty through Regional Centres, but also starting sensitization of mid level faculty and the Heads of the Departments to facilitate smooth implementation of the ATCOM modules. The introduction of Competency Based Medical Education prompted MEU to organize sensitization workshops for the faculty to take up this new challenge. Constitution of MEU and the expertise available: The organization structure of MEU is in conformity with the Regulating Body, viz., MCI. However, it captures expertise from several corners and different angles that make MEU a unique set up. As per the MCI norms, the Unit is under the direct charge of Dean (Prof M Ravishankar), assisted by a Vice Principal Curriculum (Prof Mahalakshmi) and coordinated by a senior faculty member of the institute (Prof Seetesh Ghose). The core team of MEU however, includes eminent faculty with more than three decades of experience gained in medical education in India and overseas. Some notable names are Prof K.R. Sethuraman, Vice Chancellor of SBV, Prof N Ananthakrishnan, Dean, Research & Allied Health Sciences and Prof K Narayan, Professor of Community Medicine and Prof B.V. Adkoli who has joined as Full time Professor with long experience at NTTC, JIPMER and AIIMS, New Delhi. The SBV University established collaboration with Partners Medical International (PMI), an affiliate of Harvard Medical School, Boston, for knowledge and technology transfer for curricular reforms and Faculty Development. This has resulted in a new wave of changes in both Undergraduate and Postgraduate Medical Education enabling MEU to move on a fast track of development. Many faculty members of MGMCRI have joined the MEU bandwagon in its activities that are likely to impact the quality of education. • • • • • • •
Officer-in Charge: Dr. M. Ravisankar, Dean, MGMCRI. Dr V.N. Mahalakshmi, Vice Principal, MGMCRI Coordinator Dr.Seetesh Ghose, Professor, Obst & Gynaecology Core Committee Dr.K.R.Sethuraman, Vice-Chancellor, SBV Dr.N.Ananthakrishnan, Dean, Research and Allied Health Sciences Dr.B.V.Adkoli, Professor, Health Professions Education Dr.K.A.Narayan, Professor, Community Medicine.
NC-CTHPE 2016
26
• • • • • • 1. 2. 3. 4. 5.
National Conference on Changing Trends in Health Professions Education
Dr. C.P.Ganeshbabu, Professor, Surgery. Dr.Sunita Samal,Professor, Obst & Gyn. Dr.Manoj Karthik, Assoc. Professor, Surgery. Dr.R.Kannan,Assoc Professor, Surgery. Dr.P.Pallavee, Assoc. Professor,Obs& Gyn. Dr.G.Niranjan, Assoc.Professor, Biochemistry. Academic Support Staff (Technical and Administrative Staff) Mrs. Rama. S ( Student Counselor) Mrs. Prabavathi. R ( Tutor) Mrs. Senbagame. P (Department Secretary) Mr. Kumar (Artist) Mr. Velmurugan ( Photographer) Resources and Facilities Infrastructure available and facilities provided by the MEU
Infrastructure available (Total 6000 sq ft area) Lecture Hall Seminar Hall Small group discussion rooms (Four) Access to a comprehensive Skills lab AV aids including black/white boards, flip charts, overhead projectors, LCD projector, computers with printers, photocopier and internet connection In-house Library with essential books in Medical Education besides access to e-books and other resources through central library
Facilities provided by the MEU Venue for all workshops conducted by MEU for Faculty, Residents, Interns and UG students Venue for PGDHPE program Venue for assessment and evaluation work Training site for counselling workshops and venue for Individual and Group counselling. Venue for developing resources for standard patients including training of standard patients. Venue for seminars, small group sessions and other activities as requisitioned by various constituent colleges of SBV.
Brief Description of various programs 1. Programs for the Faculty of MGMCRI 1. A)Faculty Development Programs (FDP) Faculty Development Programs are held periodically to enable the faculty for performing their diverse roles as competent and effective teacher, mentor, assessor, administrator, researcher and a complete professional. Some of the topics discussed are as follows:
NC-CTHPE 2016
27
National Conference on Changing Trends in Health Professions Education
Educational Objectives & Blooms Taxonomy Teaching Learning Principles & Lesson Planning Teaching Learning Methods Microteaching Teachers role as a Student Counsellor
Microteaching workshops are organized regularly to enable the teachers to hone their teaching skills by obtaining feedback from the peers, students and faculty supervisors. 1. B) New FDP series As a follow up of the collaborative arrangements with PMI Harvard, the mid level faculty are sensitized in some of the key educational issues through a workshop series conducted by senior faculty. In organizing this series, each senior faculty involves another mid-level faculty in a spirit of hand-holding so that the mid-level faculty is encouraged and empowered for transformative learning. The FDP series addresses topics like Adult Learning Principles, Integrated Teaching, Engaging Large Group, Feedback, Problem Learners, Problem Based Learning & Case Based Learning. Besides these, occasional sessions are also organized by the external experts on relevant topics such as “The Management of Curricular Changes - The Challenges and the Way Forward” (Dr Krishna Seshadri) 1. C) Faculty Development for Competency Based PG Medical Education Another exciting development is MEUs effort to implement a Competency Based PG Medical Education from the current batch of PG training. Learning from the experience of PMI Harvard, MGMCRI initiated a new approach to the training of PGs based on the Competency Based model. This involved extensive preparation of faculty on the concept and modalities of CBME besides, introducing a learning management system and e-portfolio which become the main vehicle for monitoring progress and internal assessment. We started with the step of sensitizing the Heads of the Departments and mid-level faculty to identify the Entrustable Professional Activities (EPAs) in each subject, the mile stones to be achieved and the entry level expected of a PG student. This enabled mapping of the EPA in terms of five levels, viz., able to observe, perform under strict supervision, perform under loose supervision, perform independently and teach others. A detailed e-portfolio developed through in-house IT initiative (Garuda) as a part of the Learning Management System (LMS) helps in capturing all the learning experiences, which can be monitored and mentored by the faculty. Though we are in a beginning stage of introducing such a model for internal assessment, this has a far reaching implicationfor introducing such a model on a nationwide basis. 1. D) Attitude and Communications Skills (ATCOM) Sensitization Program for the Faculty of MGMCRI Attitude and Communication Skills are receiving increased emphasis in the undergraduate teaching. The Medical Council of India has prescribed a
NC-CTHPE 2016
28
National Conference on Changing Trends in Health Professions Education
comprehensive module called ATCOM for introducing these elements in the undergraduate curriculum. However, the sensitization of the faculty goes a long way in successful implementation of the module. In response to this, the Medical Education Unit (MEU) has launched a sensitization program for the senior faculty of MGMCRI. The Program is conducted through three afternoon session workshops including brief presentations, in depth review of ATCOM document prepared by the M.C.I, discussion on case scenarios, role play exercise and other modalities of teaching and assessment. The sensitization is followed by another workshop for the various Heads of the Departments to design a strategy for implementing the ATCOM modules in the UG curriculum. The meeting addresses the roles and responsibilities at various levels for ensuring proper implementation of the ATCOM Modules. 1. E) Research Methodology series A recent addition to the Faculty Workshop series is an orientation workshop for the first year faculty and another series of workshops on Research Methodology for the junior faculty conducted by the MEU and biostatistics department. 2. Workshop for Resident Doctors 2. A) ‘PG Protocol Writing’ Workshop Post-graduate students are the prospective teachers and researchers. Hence their preparation for future career requires development of competency related to research methodology. In response to this felt need, MEU of MGMCRI conducts a two days workshop on Protocol writing for all the first year PG students. The issues addressed during this workshop are: An overview of research methodology, how to identify a research problem, writing a research question, skills in literature search and the role of ethics in the research. The workshop includes extensive interactive methods including brief presentation by the faculty, Group tasks followed by plenary sessions. Evaluation of the program has revealed that the participants find this program highly relevant, useful and timely intervention for crystallizing their dissertation topics. 2.B) PG Dissertation workshop The postgraduate training heavily relies on the grounding of students in the art and science of writing dissertation in particular and scientific articles in general. In order to train the PG residents in this area, the MEU of MGMCRI organizes a five half days workshop for the Final year PG students on “Dissertation- Write up” to enable them to submit high quality dissertations. The issues addressed during the workshop are: use of IMRAD structure in writing a paper, writing an abstract, using statistical formulae, constructing tables, figures and other tools of data representation, how to manage bibliographical references
NC-CTHPE 2016
29
National Conference on Changing Trends in Health Professions Education
using software and finally ethics of scientific writing, code of conduct including plagiarism checks. The workshop makes extensive use of interactive techniques including brief presentations and group tasks, followed by plenary sessions. Program Evaluation questionnaire reveals that the program is highly relevant and useful to the participants. 2.C) PG Pedagogy Workshop This workshop has been added from the current year to cater to the needs of PG students to develop teaching and communication skills for their future role as teachers. 3. Orientation Programs for the Interns 3.A) Interns’ Induction Programme Part I Proper induction of the Interns and their sensitization to various aspects of internship training is crucial for the effective training of interns as well smooth functioning of the hospital services. A one day induction program is held to familiarize the new interns regarding the infrastructure, hospital functioning, working hours and code of conduct for the interns during duty hours. 3.B) Interns’ Orientation Programme Part II The objectives of this program are to enable the interns to prevent errors, develop good communication skills, both verbal and written, be aware of the psychosocial needs of the patients, appreciate the principles in rational drug therapy, develop and refine the skills of requisitions for diagnostic tests, appropriate techniques for collection and transport of samples for laboratory test, appreciate the ethical issues involved in patient care, common medico-legal issues, their role in a multidisciplinary team and how to deal with the medical representatives. The program is highly structured with interactive lectures, group tasks, role play by students and faculty and discussion of ethical and medico-legal case scenarios. Evaluation of the program is done by using the feedback questionnaire. 4. Program for UGs A White Coat ceremony for second year MBBS students. Facilitating integrated teaching, imparting communications skills training during 3rd semester, regular counseling support for the needy students are some of the activities in which MEU provides input to the institute. Strategies used by MEU Most of the activities conducted by the MEU are based on Workshop format, in order to facilitate interactivity and hands on experience.
NC-CTHPE 2016
30
National Conference on Changing Trends in Health Professions Education
Brief presentations and Video clippings Individual and Group Tasks based on case scenarios Buzz sessions Participants’ presentation to the whole group Role Plays Brain Storming Mini Quiz Assignments and projects Program Evaluation
Every program of MEU involves extensive program evaluation. While some programs have pre-test and post-test components, others would have a system of obtaining feedback from the participants in the form of Daily Evaluation and Program Evaluation Questionnaires. Full participation of the participants is a mandatory requirement for issuing Certificate of participation at the end of the program. Short Term Outcomes Though it is difficult to assess the outcome of activities of MEU, in short span of seven years, it is possible to identify some short term outcomes in the form of certain changes that have occurred cumulatively over the years. The MEU workshops for the faculty have been received well as evident by the feedback received from the participants. We are receiving more and more queries by the faculty to undergo such programs. Some of the participants have initiated research study and enrolment in the higher degree programs launched by the SBV. The workshops for the PG students have also been perceived as highly useful by the participants. There are informal reports from the senior faculty and examiners on the enhancement in the quality of dissertations submitted by PG candidates. Happily there is substantial increase in the number of research projects approved for intra-mural and extra-mural grants for research. Future plans Considering that the changing trends in medical education are pointing towards a wider role for the MEUs, we have started visualizing our future activities in terms of introducing courses and programs with blended learning approach to facilitate a larger number of professionals who would like to emerge as educational leaders. This implies that we need to look at the quality issues, inter-professional education and moving education to a higher level of research, networking and dissemination of information, on par with the international standards. This will also mean development of robust learning management systems with e-learning Learning capabilities. In the ultimate analysis, MEU dreams to emerge as one of the Centre of excellence in medical education which strives towards linking of education systems with medical practice and health care delivery system.
NC-CTHPE 2016
31
National Conference on Changing Trends in Health Professions Education
Innovative Programs in Health Professions Education
Prof K A Narayan, Professor of Community Medicine & Academic Training and Development Consultant The Rationale Availability of competent and committed teachers and trainers has been recognized as a key factor for the development of health manpower in the country. The infrastructure for training of doctors, dentists and nurses existed for decades. There is rapid expansion of other health professional courses such as physiotherapists, occupational therapists, physician assistants, optometrists etc. While the training of doctors, nurses and dental professionals has been largely governed by the respective Professional Councils, there is a need to develop a cadre of health profession educators under a common umbrella, to leverage an integrated and team approach for training for delivery of health care services. This is all the more essential, in view of the rapid expansion of health professional infrastructure in the country leading to imbalance in production and acute shortage of educators in quality and quantity, across the health professions. There is also an urgent need to revamp the existing approaches to training of teachers in health profession, in the light of changing needs of the health profession, in the wake of a move towards competency based education, new information technology and digital India revolutionising the brick and mortar of education. The system should also respond to the globalization and market forces that are likely to influence the quality as well as the quantity of the health professionals. SBV AHEAD initiative The Academy for Health Professions Education and Academic Development (SBV- AHEAD) was established by Sri Balaji Vidyapeeth, to bring together and support all health professionals to achieve academic excellence through training and research in educational science and technology. With the presence of medical, dental and nursing institutes in one campus, the University is uniquely placed to launch innovative programs in health professions education. The establishment of a Deanery for Research & Allied Health Sciences has provided an executive machinery for designing and running innovative courses within the ambit of Regulations enforced by the UGC from time to time. Taking off on the experience of a training programme for dental educators of the University, Sri Balaji Vidyapeeth, launched a one year Post Graduate Diploma in Health Professions Education (PGDHPE) in 2014, as a part of its innovative initiatives, to cater to the needs of medical, dental and nursing faculty , who aspire to develop as educators and leaders in their field.
NC-CTHPE 2016
32
National Conference on Changing Trends in Health Professions Education
The introduction of Choice Based Credit System (CBCS) is one of the major recommendations made by the UGC for reforming higher education to make the system highly flexible, transparent and yet quality driven initiative. Inspired by the success of the PGHDHPE course, and to provide a new pathway for the aspiring teachers across the health profession, the course has been re-designed as a credit based program. Programmes in Educational Sciences – The SBV initiative. The Career Pathway The new Programs are structured to provide a continuous journey of learning with multiple entry exit options to suit the needs of diverse learners. Apart from restructuring the programme as a Credit Based one the PGDHPE has been reorganised as four certificate programmes leading to PG Diploma (PGDHPE/one year). This can be followed up by M. Phil. Program of another year, thus making them eligible for Ph D program being offered under the Faculty of Allied Health Sciences. Those having done equivalent programmes to the PGDHPE can enter directly to the M.Phil programme. Figure.1 summarises the Career pathway.
4 Certificates (32 Credits) Lateral Exit
PGDHPE (36 Cr)
Lateral Exit
Lateral Entry
M. Phil (36 Cr)
Lateral Entry
Lateral Exit
PhD
NC-CTHPE 2016
33
National Conference on Changing Trends in Health Professions Education Figure 2: Career Pathway in HPE
Thus, the candidates will be able to: Pursue Certificate Courses of three months duration (total four courses of 8 Credit points, each), with options for exit after any course, thus obtaining a course completion certificate Appear for PGDHPE comprehensive examination, based on Four Courses of study (36 Credits) Continue further to M. Phil program of one year, subject to the candidates’ holding a Master’s Degree. This program eventually leads to Ph D Program in Health Professions Education. The major highlight of the new programs is adoption of Choice Based Credit System (CBCS) recommended by the NAAC and UGC as a major reform in higher education. As a corollary to this system, a competency based approach has been proposed for the new programs.
Advantages of the Credit System To the Focus from teacher-centric to learner-centric education learners Flexibility to choose courses according to their interest Flexibility to work according to their own pace and style of learning Facilitates learners’ mobility across the courses, programs, institutes It accounts for the self-learning efforts made by the student Linked with Grading, which is fair to the students, compared with marks To the Provides scope for fixing, and assessing learning Institutes outcomes in an objective and transparent manner. Credit calculations are based on competencies and linked with study hours, rather than routine time table approach. Possibility to optimize the teaching workload, and respect teachers’ expertise, interest and preference Twinning mechanisms can be developed with other institutes, to allow credit transfers To the To ensure uniformity in standards across the States, System, nation Parents, Facilitates issues of recognition and accreditation Society To move towards international standards Ultimately, it promotes quality assurance to the society
NC-CTHPE 2016
34
National Conference on Changing Trends in Health Professions Education
Competency Based Approach
Competency based approach is the hall mark of a progressive curriculum. Knowledge and skills are of no significance, unless they are used by the professionals for the benefit of communities.
Considering the present scenario of health professions education in the country and based on future projections it is possible to identify the following core competencies, expected out of the future health professions educators. This is shown in figure 2. Figure 2. Core Competencies expected at the end of Health Professions Education Programs
Teachers Mentors Facilitators
Critical Thinkers Researchers Innovators
Ethical, Learner Oriented, Quality Conscious, Professionals
Leaders Managers Communicators Team Workers
Curriculum Planners Instructional Designers ICT users The courses chosen for the program also reflect a gradual movement. The PGDHPE comprises of four core courses. Two of these can be chosen as elective courses along-with a core course on research methodology, along-with a comprehensive project leading to Dissertation for the M.Phil.
NC-CTHPE 2016
35
National Conference on Changing Trends in Health Professions Education
Eligibility for HPE Courses
Postgraduates in Medical/Dentistry/Nursing/Public Health are eligible for entry to PGDHPE or M. Phil (2 years course). Graduates in above specialities with two years academic work experience are eligible for PGDHPE. Graduates in Allied Health Science recognized by the UGC with two years academic work experience are also eligible for PGDHPE. Those who have completed FAIMER or FIME (MCI) are eligible for M.Phil directly, provided they have a PG Degree. The Program Structure The PGDHPE program is a cluster of Four Certificate Courses in health professions covering the broad domains of Principles of education, Teaching and Learning, Assessment in education, and Management of Education. These courses are designed to assist participants to develop a broad understanding of fundamental principles, concepts, trends and issues related to health Professions education. Further, it would provide opportunity to participants to understand, appreciate and acquire skills in teaching, evaluation, curriculum development and implementation, maintenance of standards and accreditation of educational programs relevant to their discipline. Each certificate course will be spread over 12 weeks. The content delivery involves a unique combination of faculty led seminars, and self-directed learning, assignments, mentoring, portfolio and web-based discussions. Each course would have two “in-class” sessions of 2 ½ hrs/ day for 2 classes per week (5hrs/wk). These would run on a “Heutagogy” model facilitated by experienced faculty providing modelling, coaching and scaffolding experience to the participants. Practical component of the program will be in the campus/participants’ work places. Certification will be by formative and summative assessments of the theory and practical. Each program will have eight 8 credits. After successful completion of the four certificate courses, participants can complete an education project, submit teaching and learning portfolios and appear for the University examination consisting of four papers and practicals to gain the PGDHPE. The certifacte programmes and the credits assigned are summarized in Table 1. Marks of Final Examination for each course are converted in to Grade Points and CGPA is computed for the whole year as per UGC norms. Evaluation Participant evaluation is done by a mix of tools for formative and summative assessment. Formative assessment is based on a portfolio, project, peer and faculty appraisal. The summative evaluation is done by theory and practical examinations. Portfolio Each student is required to maintain a portfolio (electronic or printed) of his/her activities during the course. The portfolio will have both teaching and learning elements and is assigned 2 credits
NC-CTHPE 2016
36
National Conference on Changing Trends in Health Professions Education
The Teaching portfolio will contain
A personal statement describing teaching goals for the academic year and for each session. A reflective “teaching statement” describing ones personal teaching philosophy, strategies, and objectives. The Learning portfolio will contain a purposeful collection of the participants’ work that exhibits a learning effort, and a reflective description of progress, achievements and competencies gained during the course Table 1: Outline of PGDHPE Program with Credit Hours Course 1
Course 2
Course 3
Course 4
July – Sept
Oct – Dec
April-June
Principles of Education for Health Professions (CPEHPE)
Teaching and Learning in Health Professions Education (CTLHPE)
Jan – March Certificate in Assessment of Educational Process (CAEP)
2 Seminars of 2.5hrs/wk x12 wks 60 hrs*
2 Seminars of 2.5hrs/wk x12 wks 60 hrs* 4 Cr
2 Seminars of 2.5hrs/wk x12 wks 60 hrs* 4 Cr
2 Seminars of 2.5hrs/wk x12 wks 60 hrs* 4 Cr
Self learning 10 hrs/ wk x 12 wks = 120 hrs 4 Cr
Self-learning 10 hrs/ wk x 12 wks = 120 hrs
4 Cr
Self learning 10 hrs/ wk x 12 wks = 120 hrs 4 Cr
Total = 8
Total = 8
Total = 8
Total = 8
4 Cr
Self learning 10 hrs/ wk x 12 wks = 120 hrs
NC-CTHPE 2016
Certificate in Health Professions Education– Management (CHPEMR)
4 Cr
Final Examination Written 4 Papers 4x100=400 Internal Assessment = 50 Miniteaching=50 Portfolio =50 60 hrs (2 credits) Project =50 60 hrs (2 credits)
Total=600 Total Credits=36
37
National Conference on Changing Trends in Health Professions Education
Project
Every candidate is expected to complete a Project based on the problem encountered in his/her routine teaching and suggest the modification for rectifying the same. The submission of project report is a mandatory requirement. The project is assigned 2 credits FINAL EXAMINATION The final examination consists of four theory papers with 100 marks each. The practicals consist of a mini teaching session. Weightage is accorded to the internal assessment, portfolio and project. The final examination marks are converted in to Grade Points and CGPA is arrived for a total of 36 Credits.
M. PHIL PROGRAM IN HEALTH PROFESSIONS EDUCATION Course duration One Academic Year covering 48 weeks of study. Objectives: The participants shall be able to 1) Critically evaluate the theoretical and practical advances in selected areas of health professions education. 2) Demonstrate an ability to apply these advances in their work environment. 3) Demonstrate leadership in bringing about change in their respective work environment THE PROGRAM STRUCTURE M. Phil. program broadly consists of the following:
One core course on Research Methodology, which is linked with extensive research project work culminating in the submission of a dissertation (12 Credits) Two elective courses/areas, to be chosen from amongst the four core courses of PGDHPE program for in-depth study (each carrying a weight of 8 credits) culminating in a monogram on the chosen field (2 credits each). Submission of a comprehensive portfolio capturing the work done during the whole year (60 Hours = 2 credits) Regular teaching sessions embedded during the course (60 Hours = 2 credits). The examination consists of one theory paper from core subject of 100 marks, two theory papers of 100 marks each (based on the electives), Dissertation based on the project work (100 marks), Viva (100 marks), internal assessment (50 marks) and portfolio (50 marks). The internal assessment marks break up is: Faculty/Peer evaluation (30), Student evaluation (20). The total marks for the final examination is 600.
NC-CTHPE 2016
38
National Conference on Changing Trends in Health Professions Education
The marks secured in the examination are converted in to letter grades. Grade points are calculated for each course and final CGPA is arrived as per the norms of UGC. The content delivery in M.Phil.program involves a combination of extensive mentoring by the faculty, and self-directed learning/self-learning pursued through practice teaching/mini-teaching, assignments, portfolio and web-based discussions. The students will be connected with each other, as well as with their faculty mentors, peers and mentees (PGDHPE students) using learning management systems (LMS), aided by web-technology such as Google group or forum. Outline of M.Phil. HPE program indicating credit hours Course 1 Elective 1 July – Sept Weekly Mentoring 2.5 hrs/wk for 12 wks (30 Hrs) 2 Credits Self study leading to a monogram 2 h/day for 90 days = 180 Hours 6 Credits
Course 2 Elective 2 Oct – Dec Weekly Mentoring 2.5 hrs/wk for 12 wks (30 Hrs) 2 Credits
Total Credits 8
Total Credits 8
=
Self study leading to a monogram 2 h/day for 90 days = 180 Hours 6 Credits
=
Core Courses 3 and 4 Research Methodology July – September Initial workshop series and grounding in theoretical foundations of research 30 Hours (2 Credits) January to June Identification, designing, implementation of an educational project, leading to the submission of dissertation: Self-study of 2.5 h/day under a Guide for 168 days. 420 hours = 14 Credits Total Credits for Research = 16 Maintaining portfolio for the whole year and regular teaching planning and practice = 60+60=120 Hours = 4 Credits
Total Credits = 36; The final examination marks are converted in to Grade Points and CGPA is arrived for a total of 36 Credits. *20 Marks are allotted for Monograms, and are assessed internally.
NC-CTHPE 2016
Final Examination Paper 1: Elective 80 + 20 Marks* Paper 2: Elective 80 + 20 Marks* Paper 3: Core 80 + 20 Marks* Dissertation and Viva (100 + 100) Portfolio = 50 Internal Assessment =50 (This Includes, Faculty/Peer (30) Student evaluation(20)
Total = Marks
600
39
National Conference on Changing Trends in Health Professions Education
Why attend the course?
Listen to what participants have to say
Suganya. M. Asst. Professor, Paedodotics, IGIDS, Pondicherry
Two key elements I learnt through this course is ‘how to be a life long learner’ and ‘thinking about thinking’ (metacognition). My advice to anyone regarding this course would be “Carpe Diem!” (“Seize the day!”) It is sure to make a big difference in your career as an educator! This is a "highly practical" and "must know” subject for any health professional. Learning to be professional in building knowledge, sharing, working as a team, being responsible and accountable, is woven into the curriculum which makes it to be unique. I was a poor organizer thinking till the last moment of what to speak in the class. This course had taught me how to organize myself and be prepared... The best thing of this course is that you learn at your own pace, learning by yourself and most importantly with all the guidance you need Why join PGDHPE in SBV? "To experience a blissful journey of experiential learning along with the stalwarts by your side...who can sculpt anyone, as highly motivated lifelong learner and perfectly handle all avatars of a teacher in a holistic approach".... We liked the way how our teachers dealt with the ‘why, how, when and where’ of what they teach... PGDHPE has drastically changed me from just a teacher to a facilitator. It made me realize that I am one among those responsible for moulding students and act as "CHANGE AGENT" in my profession.
Manoj Karthik S Associate Professor,Surgery, MGMCRI, Pondicherry
If you perceive yourself as a medical educationist, this course gives a new meaning to you. Your attitude changes from "Why should I learn all these?" to "Why haven't I used all these?"
David Livingstone, Professor, Prosthodontics, IGIDS, Pondicherry P. S. Manoharan Professor & Head of Prosthodontics, IGIDS, Pondicherry Vikneshan.M, Asst. Professor, Public Health Dentistry, IGIDS, Pondicherry
M. Shivasakthy, Associate Professor, Prosthodontics, IGIDS, Pondicherry
NC-CTHPE 2016
40
National Conference on Changing Trends in Health Professions Education Senthil. M, Assoc. Professor, Public Health Dentistry, IGIDS, Pondicherry
NC-CTHPE 2016
I consider myself as lucky and fortunate to be under the mentorship of legends in Health Professional Education in India. PGDHPE is a joyful, pleasant and remarkable journey, it made me to explore my self as an effective teacher and academician. The course is one of its kind which has created a spirit of life long learning, for me it is a nostalgic experience which i am going to treasure throughout my life.
41
National Conference on Changing Trends in Health Professions Education
Scientific programmes Day one Aug 18, Dental Conference Aug 19, 2016
8.30 9.00 am
Registration
9.00 to 9.45 am
Is everything Objective Reliable?
Dr Tejinder Singh, Pediatrics and Medical Education Director CMCL - FAIMER Regional Institute CMC Ludhiana
9.45 to 10.30 am
Competency Based PGME – The Nuts and Bolts
Dr N. Ananthakrishnan &AHS), SBV
10.30 to 10.45 am
Dean (Research
Tea Inaugural Program Keynote Address - Prof Ved Prakash Mishra, Chief Guest, Chairman, Academic Committee, MCI Welcome Address
Presidential Address 10.45 am to 12.15 pm
Dr. N. Ananthakrishnan, Dean – Research & AHS, SBV
Dr. KR. Sethuraman, Vice Chancellor, SBV
Current Trends in HPE - The SBV initiatives
HPE courses
Assessment reforms
NC-CTHPE 2016
Dr. K.A. Narayan Coordinator, PGDHPE courses, SBV
Dr. V. N. Mahalakshmi Vice Principal (Curriculum), MGMCRI
42
National Conference on Changing Trends in Health Professions Education MEU Activities
Dr. Seetesh Ghose MEU Coordinator, MGMCRI
DEU Activities
Dr. Carunanidy Usha Dean, Faculty of Dentistry, SBV
Introduction of the Chief Guest
Key Note Address
Dr. BV. Adkoli Organising Chairman, NC- CTHPE Dr. Ved Prakash Mishra, Chairman, Academic Committee, MCI
Releases of Conf Shri. MK. Rajagopalan, Proceedings/ Honoring Chairman, SBECPT the Chief Guest
12.15 to 1.00 pm 1.00 2.00 2.00 2.30
to pm to pm
Vote of Thanks
Dr. Seetesh Ghose Organising Secretary, NC-CTHPe
Inter-professional Education - A Myth or reality?
Dr K. R. Sethuraman, VC, SBV lunch
Assemble in the venue for workshops Work Shop 1 Problem Learners
2.30 to 5.00 pm
2.00 to 5.00 pm
Dr N.Ananthakrishnan
Dean (Research & AHS), SBV & Dr Shivasakthy Reader, Prosthodontics, IGIDS
Work Shop 2 Professionalism Dr Tejinder Singh, Director - Regional FAIMER Institute, CMC Ludhiana & Dr.Anshu, Prof. of Pathology, MGIMS, Sevagram
Workshop 5 – Leading Change in Medical Education Dr. Krishna G Seshadri Head of Endocrinology and Diabetes, Sri Ramachandra University, Chennai
Concurrent Thematic Free Paper - Session 1
NC-CTHPE 2016
43
National Conference on Changing Trends in Health Professions Education
Scientific programmes Day Two Aug 20, 2016
8.30 to 9.00 am 9.00 to 9.45 am
9.45 to 10.30 am
Registration Transformative learning
Dr Rita Sood, Professor of Medicine AIIMS New Delhi
Evolution of Medical Education in India
Dr D.K. Srinivas, Former Dean, JIPMER & Curriculum Consultant, RGUHS
10.30 to 10.45 am
Tea Symposium Forum Integrated Teaching : A SWOC Analysis of Perspectives
10.45 to 1.00 am
NC-CTHPE 2016
Why Integration?
Dr. M. Ravishankar, Dean, Faculty of Medicine, SBV,(Moderator)
MCI Perspectives
Dr. P. Vijayaraghavan, Dean Education, Convener, MCI Nodal Center, SRMC, Chennai
Students' Perspectives
Dr. Latha Ravichandran CoConvener, MCI Nodal Center, SRMC, Chennai
Teachers' Perspectives
Dr. Gitanjali Padmanabane Convener, MCI Regional Center, JIPMER, Pondicherry
Curriculum Perspectives
Dr. V. N. Mahalakshmi Vice Principal (Curriculum), MGMCRI
Assessment Perspectives
Dr. Himanshu Pandya Convener, MCI Nodal Center, PSMC, Karamsad, Gujarat
44
National Conference on Changing Trends in Health Professions Education
1.00 - 2.00
Lunch
2.00-2.30 pm
Assemble in the venue for workshops Work Shop 3 - Teaching Work Shop 4 - Mentoring & Clinical Skills in the Feedback digital era
2.30 - 5.00
2.00-5.00
NC-CTHPE 2016
Dr Avinash Supe, Dean, SGMC & KEM Hospital, Dr Anshu, Professor of Pathology, Mumbai & Dr Rita Sood, Sevagram Professor of Medicine, AIMS, New Delhi Concurrent Thematic Free Paper - Session 2
45
National Conference on Changing Trends in Health Professions Education
Resumes & Abstracts of invited talks
NC-CTHPE 2016
46
National Conference on Changing Trends in Health Professions Education
1. Dr. Vedprakash Mishra
Chairman, Academic Committee, Medical Council of India, New Delhi Honorary Chancellor, Krishna Institute of Medical Sciences (Deemed University), Karad, District Satara, Maharashtra Pro-Chancellor-cum-Chief Advisor, Datta Meghe Institute of Medical Sciences (Deemed University) Nagpur (NAAC Accredited with Grade ‘A’ and Conferred ‘A’ Grade Status by the Ministry of Human Resource and Development, Govt. of India) Chairman, Advisory Board, R.T.M. Nagpur University, Nagpur Honorary Director, Centre for Health Policy planning and Education Research, Datta Meghe Institute of Medical Sciences (Deemed University), Nagpur Honorary Advisor to National Secretary General(Headquarters), New Delhi Vice President, Management Committee, Education Promotion Society for India, New Delhi. Member, Board of Management, D. Y. Patil University, Kolhapur Member, Academic Council, Yenepoya University, Managalore, Karnataka Member, Advisory Board, BhartiVidyapeeth, Deemed University, Pune Special Invitee on Board of Management, Dr. D. Y. Patil University, Pune Professor Emeritus, DattaMeghe Institute of Medical Sciences (Deemed University), Nagpur Professor Emeritus, TeerthankerMahaveer Medical College & Research Centre, Moradabad, U.P. Professor Emeritus, Kalinga Institute of Industrial Technology (KIITS), Deemed University, Bhubaneswar, Odisha Professor Emeritus, Sharda University, Noida, Uttar Pradesh Professor Emeritus, Himalaya Institute of Medical Sciences Deemed University, Deharadun, Uttarakhand Life Member, B.C. Roy Memorial National Endowment Fund, New Delhi Co-Convener Multi Country Expert Group for registration and Licensing for South East Asia Region countries and Member, Multi Country Expert Group for accreditation of medical schools for South East Asia Region
NC-CTHPE 2016
47
National Conference on Changing Trends in Health Professions Education
countries and Member, Multi Country Expert Group for competency based medical education model for South East Asia Region countries Member, Governing Council Kasturba Health Society, Sewagram, Wardha which manages Mahatma Gandhi Institute of Medical Sciences, Sewagram. Former Chairman, Postgraduate Medical Education Committee, Medical Council of India, New Delhi Former Member of Executive Council of Medical Council of India, New Delhi Former Vice Chancellor, DattaMeghe Institute of Medical Sciences (Deemed University), Nagpur Former, Dean, Faculty of Medicine, R.T.M. Nagpur University, Nagpur Former Member of the Management Council, Academic Council, Senate of R.T.M. Nagpur University, Nagpur Former Member of Management Council, Academic Council, Senate Maharashtra University of Health Sciences, Nashik Former Member, Board of Management (Hon'ble Chancellors Nominee), Chhattisgarh University of Health Sciences, Raipur Former, Dean, Faculty of Medicine, R.T.M. Nagpur University, Nagpur Former Member of the Management Council, Academic Council, Senate of R.T.M. Nagpur University, Nagpur Former Member of Management Council, Academic Council, Senate Maharashtra University of Health Sciences, Nashik Former Member, Board of Management (Hon'ble Chancellors Nominee), Chhattisgarh University of Health Sciences, Raipur .
INAUGURAL ADDRESS Dr. Vedprakash Mishra, Chairman, Academic Committee, MCI, New Delhi The inaugural session would highlight the importance of the theme identified for the conference, viz., the changing trends in health professions education across the globe, especially medical education, and how innovations and best practices in Faculty Development can play a major role in the implementation of desirable changes in the curriculum. The key note address will engage the delegates in asking pertinent questions such as what is the role of regulating agencies such as MCI in maintaining standards in education, vis-à-vis, role of the faculty in implementing the curriculum? How can it be played effectively through a concerted efforts from faculty, managements and the governments with a collective voice from the civil society to launch innovative practices in education backed by continuous faculty development
NC-CTHPE 2016
48
National Conference on Changing Trends in Health Professions Education
2. Professor K.R. Sethuraman. MD, PGDHE
Professor K.R. Sethuraman is the Vice Chancellor of Sri BalajiVidyapeeth, Pondicherry, since April 2013. Prior to this, he was the Dean of Faculty of Medicine and Deputy VC (Academic & International Affairs) of AIMST University, Malaysia for 7 years - from 2006 to 2013. Prior to that, he was in the department of Medicine at JIPMER (www.jipmer.edu) for 25 years (1981 to 2006) in various capacities and became HOD and Director-Professor in 2003. During this period, he was also the coordinator of the National Teacher Training Centre (NTTC) and he headed the Department of Medical Education & NTTC during 1996-2006. He has guided 48 PG dissertations and is currently guiding 7 PhD scholars. He has been consultant in the Taskforce of JPT on Medical Education in Malaysia; a Training consultant for Training of Trainers for the World Bank aided Health Systems Projects of Andhra Pradesh (APVVP), Karnataka State (KHSDP) and Orissa State; a Temporary advisor to WHO for the bi-regional HRH meet at Cape town, South Africa (2004), Psycho-social Issues meet at Bangkok (2005) and First South Asian Conference on PG medical education in Colombo (2005). He has authored 33 Pubmed Referenced papers, 40 invited papers, 60 presentations in conferences or workshops in India, Malaysia, USA, South Africa, Srilanka, Thailand and Nepal. He has authored or co-authored 9 books including the well known “Trick or Treat – a survival guide to healthcare” & its Tamil version “Post Mortem”. His multimedia creations include "Push, Promote or Educate", a WHO aided video, "Doctor-Patient Dyads", a video on common communication problems, "Patient Personality Types", a video on how to handle different patients, "Oral Examination", part-4 of a video on DNB Examination, "Album of Clinical Cases", a collection of interesting & unique cases and a PPT based self-learning module on ECG for medicos.
NC-CTHPE 2016
49
National Conference on Changing Trends in Health Professions Education INTER-PROFESSIONAL EDUCATION IN HEALTH SCIENCES Prof K.R. Sethuraman. VC, SBV “The health care we want to provide for the people we serve—safe, high-quality, accessible, person centered—must be a team effort. No single health profession can achieve this goal alone”. -- Carol Aschenbrener, M.D. Executive Vice President Association of American Medical Colleges Inter-professional education can be defined simply as: "Occasion when two or more professions learn with, from and about each other to improve collaboration and quality of care." (The Center for Advancement of Inter-professional Education (CAIPE), 1997) India is not a stranger to team based Inter-professional Health care. During early 1900's, there were mission hospitals in India that sent out teams of physicians, nurses, and auxiliaries to remote communities. An article published in 1915 advocated a team of doctor, educator, and social worker. (Baldwin D. 1996) "The Logic of Interdisciplinary Studies," an exhaustive 1997 research report, found broad consensus among dozens of researchers as to what the report called the "positive educational outcomes" for students in an integratedstudies program: o Increased understanding, retention, and application of general concepts. o Better overall comprehension of global interdependencies, along with the development of multiple perspectives and points of view, as well as values. o Increased ability to make decisions, think critically and creatively, and synthesize knowledge beyond the disciplines. o Enhanced ability to identify, assess, and transfer significant information needed for solving novel problems. o Promotion of cooperative learning and a better attitude toward oneself as a learner and as a meaningful member of a community. o Increased motivation. My own epiphany (‘eureka’ moment) was during a WHO funded workshop on "Society and Medicine" in 1991. Primary care practice in Sweden was compared with that in Sri Lanka by Goran Tomson (Medicine) and Lisbeth Sachs (Anthropology). Their observations were remarkable: Medically 80% of Sri Lankan practice was irrational and 80% of Swedish practice was rational, while Anthropologically ≥90% of Sri Lankan practice was commendable and only around 10% of Swedish practice was acceptable. The take home message was that one group needed to learn how to practice rationally, while the other group needed to learn how to practice humanistic Medicine. "It is also important to state what inter-professional collaboration is and is not. It is about taking responsibility for your own area of practice and coordinating it effectively, and with others, as you make decisions about patient management. It does not mean that we are being cross-trained to perform others’ roles. Nor is it necessarily about developing a team consensus or about thinking alike." (McMurty A 2007)
NC-CTHPE 2016
50
National Conference on Changing Trends in Health Professions Education
Current Scenario is disheartening and is in dire need of improvements. I have discussed with nearly 700 PG students, during 1994-2005, a case of "paralyzed-butaware-patient on operating table" who wiggled his toes, noted by the OT nurse, who indicated it to the OT team but was ignored as "reflex movements". Later the patient sued the hospital for negligence. Only two PGs out of 700+ suggested that perhaps the operating surgeon could have been more receptive to the warning by the nurse. (Personal notes of NTTC workshops for PGs 1994-2005 ) Triple aim for IP Education are to achieve, o better patient centered care (Sach's view in anecdote above) o better health (outcomes) (Tomson's view in the anecdote above) o efficient and affordable educational and health care systems Desirable Inter-professional Behaviors o Communicates with members of other health professions in a way they can understand, without using profession-specific jargon. o Demonstrates confidence, without arrogance, while working with members of other health professions. o Places patient/client needs above own needs and those of other health professionals. o Contributes to decisions about patient care regardless of hierarchy/ professionbased boundaries. o Reports or addresses unprofessional and unethical behaviors when working in a team. Many educators are uncomfortable with Inter-professional teaching because they do not know what to expect with learners of other professions. The enabling technologies for teaching Inter-professionally may be unfamiliar to some educators, thus causing the educators greater apprehension about engaging in IPE activities. To overcome these challenges, a major investment in faculty development is necessary. Three major barriers to the maturation of Inter-professional education (IPE) and collaborative practice: 1. Lack of alignment between education and practice 2. Lack of a standardized model of IPE across the education continuum , and 3. Significant gaps in the evidence linking IPE to collaborative practice and patient outcomes Thibault has offered six lessons. 1. 2. 3. 4. 5. 6.
The lessons are:
Leadership from the top is essential. Extensive planning is necessary for rigorous experiences. Experiences need to be repeated throughout the educational continuum. IPE must accomplish better outcomes; it is not an end in itself. New technologies can assist in accomplishing goals. A major commitment to faculty development is required.
NC-CTHPE 2016
51
National Conference on Changing Trends in Health Professions Education
Models which are effective for IP Education (Colorado Univ) o o o o
Traditional model of the facilitated discussion Group projects Problem-based learning Michaelson’s team-based learning model Summing up Students who gain a better understanding and appreciation of one anothers' roles in the provision of health care services, and who learn to respect and value the input of other disciplines in the team decision making process, will be better prepared for Inter-professional collaboration following graduation. Therefore we are committed to providing high quality Inter-professional experiences to health professional students during their education. (http://piper.mcmaster.ca/about_intro.html ) References
1. Baldwin D. Some historical notes on interdisciplinary and Inter-professional education and practice in health care in the U.S.A. J Interprof Care. 1996;10:187– 201 2. Inter-professional Education & Core Competencies - CIHC. (Download via Google) 3. McMurty A. Reinterpreting interdisciplinary health teams from a complexity science perspective. U Alberta Health Sci J. 2007;4:33–42 4. The Logic of Interdisciplinary Studies. http://www.albany.edu/cela/reports/mathisonlogic12004.pdf 5. WHO Framework for action on Inter-professional education and collaborative practice. (download from www.who.int )
3. Dr. N. Ananthakrishnan, Dean, Research & AHS
Presently the Dean, Research and Allied Health Sciences, Sri Balaji Vidyapeeth, Pondicherry. During his long tenure in JIPMER, Pondicherry, he has extensively contributed to innovations in teaching as well as teacher training. He has the rare distinction of serving as Faculty member of the National Teachers
NC-CTHPE 2016
52
National Conference on Changing Trends in Health Professions Education
Training Centre, JIPMER for 26 years, participating in 50 National Courses resulting in the training of over 2500 medical teachers all over the country. He has worked as a key member of the consortium group of medical colleges which revised the MBBS curriculum which formed the basis of the 1997 MBBS guidelines of the MCI. Innovations in teaching Introduced First aid training, clinical clerkship, problem oriented symposia, video assisted teaching of operative surgery and modular teaching for undergraduates. Introduced total objective multidimensional internal assessment, log books, research methodology and pedagogy training for postgraduates. Author and Editor of one of the the most sought out book “Medical Education, Principles and Practice” and also another popular book “Medical Postgraduate Dissertations – a step by step approach.” Devised the first Objective method of evaluation of dissertations which is now used by several medical universities in India. Teachers Training Besides his rich contribution to the NTTC courses, he also participated in several onsite and offsite workshops on different areas of educational science. Participated in training of trainers for the states of Tamil Nadu, Andhra Pradesh and Karnataka Faculty member of the Society of educators for rational drug use in training medical graduates and practitioners in “The concept of essential drugs and rationalized therapy”. Faculty member of WHO sponsored workshops on Essential Drug Concept
COMPETENCY BASED POSTGRADUATE MEDICAL EDUCATION N. Ananthakrishnan , Dean, Research and Allied Health Sciences, SBV, Pondicherry Postgraduate medical education involves not only a thorough exposure to in depth knowledge relevant to the concerned specialties, but even more important than this is acquisition of skills and attitude required to perform independently as specialists in the concerned discipline. The current system of postgraduate training in India does not ensure a uniform quality of output since there is no continuous assessment and the final evaluation is confined to a single University examination at the end of the course. Here a disproportionately large amount of time is spent on testing of theory. Testing of various skills is limited to the very short contact period between the candidate and the examiners and is confined to a few skills with the vast majority remaining untested. Attitude is not tested at all.
NC-CTHPE 2016
53
National Conference on Changing Trends in Health Professions Education
Most Western Countries have tried to overcome this by switching to a competency based system of postgraduate education in the recent past. SBV is the first University in India to launch a comprehensive competency based postgraduate medical education programme for all their Postgraduates from this year. The essential aspects of the competency based postgraduate medical education programme include the following: 1 A comprehensive list is drawn up for all competencies required to be present and certified for each postgraduate in each medical specialty at the end of the course. 2 These competencies are converted to measurable activities called “ENTRUSTABLE PROFESSIONAL ACTIVITIES” (EPAs). This implies that the outgoing graduates should be certified to possess all these EPAs at the end of the programme at the desired level to be able to function as independent Specialists. 3 These EPAs are assessed on a continuous basis throughout the course using appropriate tools to ensure the performance status at various stages of the course. The desired levels at various stages called the “mile stones” are prescribed for each EPA in each subject. 4 It is the aim of the Postgraduate training programme to ensure that all candidates reach a level of four as per the milestone classification (the ability of the candidate to be able to perform the skill independently without need for supervisions) at the end of the course, for the prescribed EPAs. 5 The progress of the training is ensured at regular intervals by supervisors who score the candidate as to the level of mile stone achieved at every stage when compared to the target. Individual feedback is given to the candidate and corrective measures are taken when it is found that a particular candidate has not reached the desired “mile stone”. 6. For Entrustable activities which involves communication, team work, relationship with other health care personal, attitude etc., feedback is taken from other health care professionals, patients, relatives, peers, etc., This is called Multi Source Feedback. Till now, these aspects were totally missing in the Postgraduate curriculum. 7. Provisions is also made in the system for the candidate to reflect ON his goals, his targets, his strengths and weaknesses, the issues he has with the learning process etc., This is recorded by him in a portfolio, which is discussed at regular intervals with the supervisors for specific corrective measures. The whole process of postgraduate teaching and learning activities including academic work, clinical work, laboratory work, research, co-curricular activities, continued medical education, attendances in conferences, presentation of research papers etc., are recorded in an e-portfolio which is monitored regularly by the supervisors. 8. The whole aim of this system is to ensure that 100% of the all postgraduate acquire 100% of the EPAs at the appropriate level by the end of the course.
NC-CTHPE 2016
54
National Conference on Changing Trends in Health Professions Education
4. Dr. M. Ravishankar, Dean, MGMCRI
Dr. M. Ravishankar is one of the eminent anesthesiologists in India and currently, the Dean, Professor of Anesthesiology, Director, Medical Simulation centre, Chairman, Quality control and Patient safety, ITC coordinator of AHA at Mahatma Gandhi Medical College and Research Institute (MGMCRI) His achievements include upgrading the Department of Cardio-thoracic Anaesthesia and establishment of Critical Care Unit at JIPMER, Puducherry. He was appointed as Inspector by the National Board for the accreditation of hospitals for starting DNB program. Dr Ravishankar has been honored with 10 awards including a Life time achievement award for his outstanding contribution to the specialty of Anesthesiology. He organized 10 conferences or CMEs and served as a Resource Person for 67 programs all over the country. He has published 56 papers and completed 36 research projects.
WHY INTEGRATION ?
Dr. M. Ravishankar, Dean, MGMCRI The term integration in education means coordination of teaching learning activities across various departments, to provide holistic approach to the learning. The traditional medical curriculum in our country is largely disciplinary and taught by many departments in silos. This has resulted in a situation where the students are expected to learn a huge quantum of information in a disjointed manner without addressing the disease or the patient as a whole. Lack of integrated approach not only makes the teaching dull and boring, but also results in a huge wastage of faculty time in covering the entire curriculum in a piece-meal manner. At times the concepts taught are even contradictory, creating more confusion for the students. Important topics such as Tuberculosis are dealt by seven departments engaging the students for more than 60 hours during the entire course. Does it make any sense? The Medical Council of India, therefore, recommended implementation of integrated teaching as a major element of the curriculum, as early in 1997 regulations, even
NC-CTHPE 2016
55
National Conference on Changing Trends in Health Professions Education
stating the elements in each subject area which can be integrated. Unfortunately, the concept of integration has not been understood fully, partly because of the lack of sensitization and partly because of the ‘mind- set’ of the teachers to feel safe in their territorial zones. As a result, it has been implemented in varying degrees in different colleges. It is therefore necessary to discuss this concept from different perspectives to facilitate its smooth implementation.
5.Dr. Krishna Seshadri, Head of Endocrinology and Diabetes at
Sri Ramachandra University, Chennai.
Dr Krishna Seshadri is currently a Senior Consultant, Endocrinology Diabetes and Metabolism at the Fortis Malar Hospital. He is also a Visiting Professor of Endocrinology and Medical Education & Member Board of Management Sri Balaji Vidyapeeth. Dr Krishna Seshadri served as the Head of Endocrinology and Diabetes at Sri Ramachandra University, Chennai for a long tenure. He is an American Board certified professional in Internal Medicine, Endocrinology, Diabetes and metabolism. He is a member of several academic bodies including American College of Physicians, The Endocrine Society and American Diabetes Association. He is also the recipient of several prestigious awards. Having associated with Partners Medical International (PMI), Harvard Medical School, Dr Seshadri has been instrumental in enabling SBV-PMI initiative. His areas of interest include integrated teaching, communication skills, humanistic approach to medicine, leadership and change management. Dr Krishna Seshadri is an astute physician, excellent communicator and an inspiring leader. He is conducting a workshop on Leading change in medical education.
NC-CTHPE 2016
56
National Conference on Changing Trends in Health Professions Education
6. Dr. P.V. Vijayaraghavan
Dr. P.V. Vijayaraghavan is presently the Director (Academic Administration) and Dean Education at Sri Ramachandra University. Basically he is a Professor of Orthopaedics. He took interest in Medical Education since 1997 when he attended the NTTC Programme at JIPMER. Following this he became a Member of Medical Education Unit at SRMC. Participated as Resource Person in Teachers Training Programmes.Collaborated closely as Coordinator of MEU at SRMC with Harvard Medical International in evolving and implementing an integrated MBBS curriculum under the aegis of Medical Council of India. Has been taking keen interest in competency development and assessment of competencies in postgraduate orthopaedic education. Completed FAIMER Fellowship in 2012 at CMC Ludhiana and also Fulbright Scholarship for Health Profession Education Administration in 2015. As Dean-Education of SRU, the Medical Council of India has appointed him as Convener of Nodal Centre on Medical Education since 2010. Has been responsible for the successful conduct of FIME and Basic Course workshop on MET.
MCI PERSPECTIVES ON INTEGRATION IN MEDICAL EDUCATION Dr. P.V. Vijayaraghavan, Director (Academic Administration), Dean Education, and Professor of Orthopaedics, SRU, Chennai. Integration in Medical Education is the organization of teaching/learning matter to interrelate or unify subjects frequently taught in separate departments. It occurs when relevant components of the curriculum are connected and related in meaningful ways by both the students and the facilitators.
NC-CTHPE 2016
57
National Conference on Changing Trends in Health Professions Education
The first formal attempt by the Medical Council of India in formalizing and structuring the MBBS curriculum happened in the 1960s and later a formal document was produced in 1981 which was completely subject based in a phase wise distribution. It was the 1997 regulations which in its written document included integrated elements under each subject correlating basic science with clinical subjects and vice versa. The guidelines also provided for examination questions to formally include clinical correlation questions in basic science and vice versa but this was really dormant as a document in the shelves of the Deans and the MEU coordinators. Vision 2015 document while addressing the issue of creating doctors as physician of first contact, writes about improving quality of training and introducing newer teaching elements in which horizontal and vertical integration has been included and the rationale is to develop a student knowledge base that is relevant to practice, rational and promotes stepwise acquisition and application of knowledge and skills. The proposed stress in integration is given in each phase as in figure principles of integration were clearly understood and it was really felt that there was a
problem with implementation of the 1997 regulations due to lack of faculty training and faculty development. Since 2009 MCI understood the value of seamless integration between faculty development and curriculum development and gave a lot of stress on educating faculty in newer technologies in Medical Education through creation of Regional centres and Nodal centres and authenticating Basic and Advanced courses in Medical Education. This has yielded good results and the curriculum implementation support programme (CISP) in the basic workshop provided for nearly an hour of discussion on Integration in MBBS curriculum. Nearly 20000 faculties across the country have been sensitized toward this principle. What started of as a Board of Governors initiative in 2010, as a Graduate Medical Regulation document of 2012 has been carried forward by the present academic committee over the past 4 years and developed as a “competency based curriculum� which is awaiting final stamp of approval by the Ministry.
NC-CTHPE 2016
58
National Conference on Changing Trends in Health Professions Education
7. Dr. Avinash Nivritti Supe, MS, FCPS, FICS, DNBE, PGDME, DHA, FMAS, FAIS, FAIGES, MHPE (UIC)
Director, Medical Education and Major Hospitals, MCGM Professor of Surgical Gastroenterology, Seth G S Medical College Dean, KEM Hospital, Ex-Dean- Sion Hospital Past President Indian Chapter of Indian Association of Hepatobiliary Pancreatic Association; President of Academy of Health Professions Educators of India, Secretary elect- Asia Pacific Hepato Biliary Association. Academic Council /BOS member MUHS, Chairman, Medical Education Board, MUHS Director, GSMC FAIMER regional Institute, Chairman – MCI reconciliation Board, Expert group Editorial Board – Medical Education, Journal of Post Graduate Medicine Associate Editor, The Clinical Teacher Chairman- GI surgery – National Board of Examinations Member – National committees- Ministry of Health and Family welfare Recipient of over 33 national and international awards and medals. Recipient of International College of Surgeons fellowship Trained at Memorial Sloan Kettering Cancer Center – New York and Hamburg FAIMER Fellow 2002, International Fellowship in Medical Education 2007 Master in Health Professions Education – University of Illinois, Chicago- USA Visiting Faculty, Tata Institute of Social Sciences Prestigious Dr GM Phadke, Network, Bangalore, Dr Dholakia and AMASI orations; Publications in National and International journals – 247 (Pubmed 108); 4 books, Faculty and speaker all over the world - more than 360 presentations Wild life, Nature and Medical Photography. Awarded Honorary Membership of Photographic Society of India. Centurion Donor Award – Govt. of India – donated blood – 111 times Marathi Book – Arogya Sampada , regular articles in weekly.
NC-CTHPE 2016
59
National Conference on Changing Trends in Health Professions Education 8.Dr. D.K. Srinivas
D. K. Srinivas, MBBS, MD, has Postgraduate Diploma in Distance Education, undergone special training in Medical Education under a WHO Fellowship at the Regional Teacher Training Centres, in Sri Lanka and Thailand. Teaching experience: He is a Public Health specialist. He has taught Community Medicine in Maulana Azad Medical College, New Delhi, Goa Medical College, Panjim and JIPMER, Pondicherry. He retired as Dean of Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER), Pondicherry in 1996. Contribution to Medical Education: Dr DK Srinivas is one of the pioneers in the development of Medical and Health Professional education in India. He was one of the founding members of the first National Teacher Training Centre (NTTC) at JIPMER, Pondicherry, established by Ministry of Health & Family Welfare, Government of India in 1976, and contributed to Training of Teachers in Educational Science & Technology. He has the distinction of conducting the highest number of Teacher’s Training programs in India. After retirement, he was invited by the first Vice Chancellor of RGUHS, Dr. S. Kantha to help newly established Rajiv Gandhi University of Health Sciences (RGUHS), Bangalore, as Consultant, Curriculum Development. He made pioneering effort in development of undergraduate and postgraduate curricula for various faculties like medical, dental, nursing, pharmacy, AYUSH at RGUHS. He also introduced teaching of Ethics in all Curricula and system of Synopsis Review during his tenure at RGUHS. He retired from there in 2006. He has been training consultant to medical education centres across the country and for WHO (World Health Organization), and World Bank. Publications & Books: He has contributed to four books on medical education and published 97 papers in peer reviewed national and international scientific journals in addition to Key Note addresses and Orations. His jointly edited book
NC-CTHPE 2016
60
National Conference on Changing Trends in Health Professions Education
-“What is Not Taught in Medical Colleges” – was published by Rajiv Gandhi University of Health Sciences, Bangalore, in June 2011. Positions: Till recently, he was Consultant to the Health Portfolio of the Sir Ratan Tata Trust for Human Resources and Health Systems Development and Member Board of Management, Sri Devaraj University, Tamaka, Kolar. He is a member of Planning & Monitoring Board, KLE University, Belgaum, Member of Academic Council of Yenepoya University, Mangalore and Member Advisory Board of RGUHS for Development of MPH (Hon) course, member of Ethics Committee of FRHS. He is a freelance trainer.
Evolution of Medical Education in India D.K. Srinivas
Dean (Retired), Jawaharlal Institute of Medical Education and Research, Pondicherry, Former Project Officer, National Teacher Training Centre, JIPMER, Pondicherry, Former Consultant, Curriculum Development, Rajiv Gandhi University of Health Sciences, Karnataka, Bangalore Introduction In my presentation I would like to dwell first on understanding the term evolution and some general principles of evolution of life and try to fit these principles to the evolution of health professional education including medical education. Since evolution is a process over generations, I propose to view medical education in four periods, the Ancient period, Moghul period, Colonial era and the period of Independent India - 1947 to 2000 respectively. I shall conclude by flagging some concerns and questions for you to ponder. Understanding the term Evolution According to dictionary evolution means: expanding, gradual development. A brief study of essays on evolution provides more insight. Evolution is the process of change in all forms of life over generations. Evolution is not a random process. It is gradual development, a development from simple to a complex state. Evolution is an inevitable result of imperfectly copying, self-replicating organisms reproducing over years under the selective pressure of the environment. The outcome of evolution is not a perfectly designed organism The environment determines probability of change or success. It is regulated and systematic series of movements. Let me try to apply above principles to Evolution of Medical Education in India
Evolution is an inevitable process of change.
NC-CTHPE 2016
61
National Conference on Changing Trends in Health Professions Education
Traditional systems of health care in India
Ayurveda all over India and Siddha, particularly in some parts of South India, were the principle systems of health and medical care practiced in India. Training was essentially based on ‘Gurukula’ method. Unani medicine arrived in India around 12th-13th Century with establishment of Delhi Sultanate. The royal hakeems practiced a hybrid Muslim version of Greek (Yunani or Unani) which came to be known as Tibbi medicine. Initially medicine was mainly transmitted from father to son. Training collectively as is done now started with establishment of a Tibbi medical school known as Madrasah Tibba in 1882 in Delhi1. Homeopathy in India took roots in by Royal patronage of Maharaja Ranjit Singh when a German homeopath treated the Maharaja in 1836. First Homeopathy College was established at Calcutta in 1835 by a group of intellectuals. Colonial Era Training of locals and establishment of medical outposts was essentially to treat the natives. Portuguese introduced the European medicine to India. The French established ‘Ecole de Médicine de Pondichéry’ in 1823 in Pondicherry, granting a diploma called Médicin Locale that allowed them to practice medicine in the colonial territories. With the de jure transfer of Pondicherry to India it became a full-fledged medical college, Dhanvantri Medical College. It was later upgraded to a postgraduate institute and was named after Jawaharlal Nehru in 1964 which is the present JIPMER. The Portuguese established ‘Escola Medico Cirurgica da Goa’ in 1842 at Panjim, renamed as Goa Medical College in 1963. British Era: The greatest influence on medical education in India was during the British rule in 19th century. In the ‘Native Medical Institution’ (NMI) established at Calcutta in 1822, medical teaching was imparted in vernacular. Treatises on anatomy, medicine, and surgery were translated from European languages for the benefit of the students. It is interesting to note that medical education provided by the colonial state at this stage involved parallel instructions in western and indigenous medical systems. From 1826 onwards, classes on Unani and Ayurvedic medicine were held respectively at the Calcutta madrasah and the Sanskrit college. NMI was closed and ‘Medical College, Bengal’ (the present Calcutta Medical College) said to be the first to teach European medicine in Asia was started in an old building of Petty Court Jail in Calcutta in 1835. Teaching was in English. It is so even now in all medical colleges in India. Around the same time Madras Medical College was also
NC-CTHPE 2016
62
National Conference on Changing Trends in Health Professions Education
started. The latter admitted women so that they could treat the female population who shied away from male doctors. An exclusive medical school for women ‘Women's Christian Medical College’ was established in Ludhiana, Punjab in 1894. Fifteen more medical colleges were started until 1947. During the colonial era in about 120 years just 18 colleges were established! Most of them were government run. Post Indian Independent Era (1947-2000) Evolution is development from simple to complex state. Growth of Medical Colleges: One of the strengths of medical education in our country is the rapid increase in the number of medical colleges after independence in general and with the entry of private sector in particular. From 15 medical colleges at the time of independence (Keswani1) the number has gone up to 400+ in just about over six decades. Recommendations of particularly three committees popularly known as Bhore Committee2 , Mudliar Committee3 and Srivastava Committee4 appointed by Government of India influenced the development of medical education. Let us have bird’s eye view of these recommendations. Bhore Committee (1946) made some significant recommendations. Among them few notable and interesting were coining a name to the type of doctor for the first time and establishing AIIMS. The type of doctor needed for the country is to be a ‘Social Physician’. Training methods should “encourage to learn himself, think, observe and draw conclusions.” Medical Colleges should “stress and encourage research by students and teachers”. There should be One year Internship after completing MBBS. Establishment of Primary Health Centres in rural areas and Starting of an All India Institute of Medical Sciences (AIIMS) to meet with shortage of specialists and teachers so that postgraduate training is done in India. Mudliar Committee (1962) laid following norms: One doctor for 3000-3500 population One medical college for every 5 million population To establish by 1971 at least 100 medical Colleges with 100 admissions. Establishment of PG courses Establishment of 6 Regional Institutes like AIIMS Full time teachers in medical colleges with uniform designation: Professor, Reader/Assistant Professor, Lecturer and Registrar
NC-CTHPE 2016
63
National Conference on Changing Trends in Health Professions Education
Srivastava Committee (1975) recommended health needs of rural people: Involvement of medical colleges in the health care of community by adopting three selected Primary health centres Establishment of Referral Services Complex to provide “efficient, accessible refferal system to higher centres” Reorientation of Medical Education Application of “Educational science” in educational process In spite of far reaching recommendations, between1999-2008, 80% of the colleges established were in private sector and nearly half of them (40) were in top 100 cities. Nearly two thirds of the colleges are in south India. Many more are likely to be established. Needless to say the quality of training has suffered. Medical education has become expensive and critics say that it is ‘commodified’. Faculty Development movement in India: Bhore Committee recognized the need for training of medical teachers as early as in 1946 and made recommendations. Nearly, three decades later, faculty development began in India. Its progress may be categorized into six initiatives: (i) NTTCs: Govt. of India established three NTTCs. This was also part of WHO’s global initiative. First Teacher Training course at national level was conducted by NTTC, JIPMER in March 1976. A seed was sown for training of teachers (ToT) and faculty development programs in India. (ii) CMET: K.L. Wig Centre for Medical Education and Technology was established at All India Institute of Medical Sciences, New Delhi in 1989-90. The Centre has contributed to the development of educational specialists and leaders. It also coordinated consortium activities and brought out two valuable documents5,6 pertaining to curricular changes in MBBS course. (iii) Consortium of Medical Institutions (1989-95): Initially four leading medical institutions and the Department of Medical Education College of Medicine at Chicago, University of Illinois, US and later by twinning with 16 colleges a Consortium was formed that undertook “Inquiry Driven Strategies for Innovations in Medical Education” under a WHO project. The consortium prepared a national consensus curriculum document. Medical Council of India incorporated many of the ideas and suggestions from this document in the MBBS Regulations of 1997. The Consortium project came to halt as the WHO support was stopped. (iv) Medical/ Health Sciences and Deemed to be Universities (1986) were formed to promote high standards of education, faculty development and research. These
NC-CTHPE 2016
64
National Conference on Changing Trends in Health Professions Education
universities offer courses in Medical, Indian systems of medicine (AYUSH), Dentistry, Nursing, Pharmacy, Physiotherapy, and Allied health sciences. Although different faculties have come together under one umbrella the expected or desired interdisciplinary integration is yet to take place. (v) Medical Education units (MEUs) in medical colleges was made mandatory by Medical Council of India in 1999. It also made teacher training essential for all medical teachers. (vi) FAIMER (2001) (Foundation for Advancement in International Medical Education and Research, Philadelphia) through three Regional centres has supported faculty development through two-year part time fellowship program designed to develop managerial and leadership skills, in order to promote changes in medical education through networking. It has become popular. Journals & Books: Credit must be given to Indian Association for Advancement of Medical Education for bringing out what can be considered the first Indian journal ‘Indian Journal of Medical Education’ as early as 1961 exclusively devoted to improvement of medical education. The Association held annual conferences on various themes. Unfortunately, both the Association and the Journal are defunct now. ‘Trends in Medical Education’ was another journal started by the Consortium of Medical Institutions. Many of the past and present day stalwarts in medical education contributed articles. With the end of the consortium project the journal had to be discontinued due to lack of funds. In the seventies, World Health Organization’s publications on medical education were the main source for teacher training. In 1990s many books on medical education were published; first by NTTC, JIPMER (1995), followed by CMET, AIIMS, (1995), Indian Academy of Paediatric Education Centre (1997) and MET cell of Seth GS Medical College, Mumbai, besides a much needed Trainer’s Manual was brought out by NTTC, Pondicherry (1997). These books helped in enhancing knowledge of medical teachers in educational science and served as resource material for conducting teacher training courses in the pre IT era. Concerns The evolution is regulated by systematic series of movements.The outcome of evolution is not a perfectly designed organism. There are about 1200 colleges related to health sciences which include 400+ conventional Medical, 280+ Dental, 500 + Ayurvedic, Homoeopathy, Siddha and Unani (AYUSH) colleges bringing out nearly 65,000 doctors of different systems annually, perhaps highest number in the world. There is concern about uneven
NC-CTHPE 2016
65
National Conference on Changing Trends in Health Professions Education
distribution of the colleges. The standards and quality have not kept pace with the quantitative increase. There is not only inequity in health care delivery but also widening gap between health care and medical education. The situation has been well summarised7 and I quote “… from Bhore Committee (1946) report to that of the Bajaj committee (1991) report in India or from Flexner’s original report (1910) to the latest papers on ‘One hundred years after Flexner’s report’ have expressed concern, if not dissatisfaction, about medical education. In other words, the malady existed and still exists all over the world! The Edinburgh Declaration in 1988 during the World Conference on medical education lamented that “..aim of medical education is to produce doctors who will promote the health of all the people and that aim is not being realized in many places. The individual patient … expects a doctor trained as an attentive listener, a careful observer, a sensitive communicator and an effective clinician.” Though medical colleges are regulated by Medical council of India on the basis of ‘stringent’ criteria, academic growth has not been systematic. In 180 years of existence of medical colleges in India only duration of MBBS course has been changing but hardly any change methods of teaching or assessment. Flexnerian influence is still strong! Questions to Ponder As I said in the introduction let me raise few questions to ponder. Should we go on expanding at this rate to reach the target of 1 doctor per 1000 population envisaged by Ministry of Health & FW, Govt. of India? Should we have one type of doctor with an integrated training of Indian system and modern system as a means to overcome shortage and poor utilization? How do we improve the quality of medical education on one hand and on the other bridge the gap between medical education and health care? Should we still base our delivery of health care and health systems on Primary Health Centres established on the recommendations made by Bhore Committee in 1946? Is it the only solution? Should innovative methods be tried? PPP model of health care has put considerable strain on people due to the mounting out of pocket expenses for medical service. What other methods should we try to provide Universal Health Care? These concerns have to be addressed. It is our social responsibility. The ‘social physician’ envisaged by the Bhore Committee or the ‘pluripotent doctor’ visualized by Prof. Ramalingaswamy has not emerged from our medical colleges. I would look forward to discussion over these issues and would be most happy either here (iha) or there (para) if through evolution or revolution the ‘pluripotent’ doctor* dreamt by Prof V. Ramalingaswamy becomes a reality.
NC-CTHPE 2016
66
National Conference on Changing Trends in Health Professions Education The doctor we need* “Call it by whatever name, the need is for a new breed of physician who has broad understanding of human biology, is imbued with ingredients of rural & peri-urban societies & their way of life, who can communicate effectively with patient’s family, who will be effective leader of health workers, and who will use his knowledge to stimulate other community building programs. We need in effect a social biologist.” V. Ramalingaswamy, 1968 (Prof. Ramalingaswamy, noted medical educationist, was former Director of AIIMS, New Delhi and Director General of ICMR, New Delhi)
References 1. Keswani N H. Medical Education in India since Ancient times, in O’Malley C (Ed.).The History of Medical Education, UCLA Forum Med. Sci. No. 18, Uni. Of California Press, Los Angeles, 1970. P 329-366. 2. Bhore. J. Report of the Health Survey and Development Committee, Simla: Government of India Press, Government of India; 1946 3. Mudaliar A.L., Report of the Health Survey and Planning Committee, New Delhi: Ministry of Health, Government of India; 1962. 4. Shrivastav J.B, Health Services and Medical Education – A programme for immediate action; Report of the group on medical education and support manpower, New Delhi: Ministry of Health and Family Planning, Government of India; 1975 5. Verma K, D'Monte B, Adkoli BV, Nayar U, editors. Inquiry Driven Strategies for innovations in medical education in India, The Consortium of Medical Institutions, New Delhi: All India Institute of Medical Sciences. 1992. 6. Verma K, Nayar U, Adkoli BV (editors). Inquiry Driven Strategies for Innovations in medical education in India, Currricular Reforms. The Consortium of Medical Institutions, New Delhi: All India Institute of Medical Sciences; 1995. 7. Shekar K.S., Srinivas D.K., Editors. What is not taught in medical colleges. Bangalore: Prasaranga, Rajiv Gandhi University of Health Sciences; 2011. P iiii. DKS/14.08.2016
NC-CTHPE 2016
67
National Conference on Changing Trends in Health Professions Education
9. Dr.Tejinder Singh
Dr. Tejinder Singh is Professor of Pediatrics and Medical Education and Vice Principal at CMC Ludhiana. He is also the founder Director of CMCL-FAIMER Regional Institute and National Convener of Fellowship in Medical Education program of the MCI. Recently he has been conferred with B.C. Roy National Award as eminent medical teacher. As a prolific writer, Dr Tejinder Singh has authored 3 books, 50 chapters and 220 papers. His landmark book “Principles of Medical Education” is now updated in 4th edition. His articles cover wide range of topics such as student assessment, competency based medical education, work-place based assessment, professionalism, feedback and mentoring. He is passionate about student assessment, and feels the need for making a new breaking ground in this field.
IS EVERYTHING OBJECTIVE RELIABLE? Dr. Tejinder Singh, Professor of Pediatrics and Medical Education and Vice Principal, CMC Ludhiana
There is a common belief that for reliable results, only ‘objective’ assessment should be used. A fallout of this belief is that anything which cannot be objectively assessed is ignored. Competencies like communication, professionalism, inter-personal relations and ethics are the sufferers of this belief. There is enough data accumulating that this is not necessarily true. Objective assessments have their advantage that they allow a large sample to be tested in a relatively short span of time but they use a norm referenced approach and work in a limited domain with lower level of simulation. Subjective assessments, on the other hand work with a criterion referenced approach at a higher level of simulation. Objective assessments require well-structured standard problems but in actual practice, most of the times, the physicians encounter non structured
NC-CTHPE 2016
68
National Conference on Changing Trends in Health Professions Education
problems. They thus limit the ability of the student to deal with variability of clinical practice. Very commonly, reliability is seen as a measurement issue and is often limited to reproducibility of the results. In its true sense, reliability should be a decision making issue. A truly reliable assessment is one, which can be relied upon. This reliance can come only with an adequate sample size of domain, tasks and assessors. The major threat to reliability comes from inadequate sample rather than from marker variability. In a true sense, there is nothing like objectivity in assessment because all assessments are colored by the values, beliefs and philosophy of the assessor and the institution. All we do is to prepare assessments subjectively but try to measure them objectively. This has been called as ‘objectification’ and hardly contributes to reliability. Expert subjective judgment, on the other hand, deals with real life situation, exposing the students to variability of clinical practice. In that sense, it is more valid than purely objective assessments. It also helps us to assess a number of competencies which are essential to the practice of medicine. They encourage students to engage in deep learning contrasted to superficial learning promoted by objective assessments. Subjective ratings are not less reliable has been shown repeatedly by many studies. While objective assessments can be used for selection type of assessment, for better learning, subjective ratings hold the key. Subjectivity is not synonymous with bias and we would be well advised to start viewing reliability as consistency of performance rather than as consistency of marking.
10. Dr.Rita Sood, MD, MMEd, FAMS, FRCP
Rita Sood is a Professor of Medicine and practicing internist at the All India Institute of Medical Sciences (AIIMS), New Delhi. She has been teaching undergraduate and postgraduate students for more than 30 years. She has
NC-CTHPE 2016
69
National Conference on Changing Trends in Health Professions Education
been an adjunct faculty at the Centre for Medical Education and Technology at her institute since 1990 and was heading the Centre from 2005 to 2009. She has been actively involved in the faculty development programs in medical education for the last two decades and has worked with National bodies in her country and with WHO and UNICEF for issues pertaining to medical education. She has edited two books in medical education, published more than 90 papers, written 26 book chapters, and is on the review board of many national and international journals. She was a fellow of FAIMER (Foundation for Advancement of Medical Education and Research) Institute, Philadelphia (2005-2007) and a faculty for all the three regional FAIMER institutes in India. She is the President of the South-East Asian Regional Association for Medical Education (SEARAME) and is an executive council member of the World Federation for Medical Education. She was also the founder President of the Academy of Health Professions Education in India.
TRANSFORMATIVE LEARNING Rita Sood, Professor of Medicine AIIMS, New Delhi. Transformative learning (TL) is an adult education theory that states individuals must critically reflect on life events in order to change their beliefs or behaviors. It involves helping adults to elaborate, create and transform their meaning schemes i.e. beliefs, feelings, interpretations and decisions, through reflection on their content, the process by which they were learned and their premises (Mezirow, 1991, 2000). The core of TL is the uncovering of distorted assumptions or errors in learning. Beyond transmitting content, TL develops skills for ongoing autonomous thinking. Mezirow named steps or stages leading to transformation starting with a disorienting dilemma and ending with restored equilibrium. As the health care systems become more complex with increasing sophistication in technology, working in it will require better understanding and manipulation of information rather than just acquiring it. Lancet Global Commission (2010) on reforms in health professions education for the 21st century strongly proposes transformative educational reforms that will empower the individual (learner) to think as an autonomous agent in a collaborative context rather than to uncritically act on the received ideas and judgment of others. Transformative learning is about developing leadership attributes; its purpose is to produce enlightened change agents. Empowerment of learners is both a goal and a condition for transformative learning. An empowered learner is able to participate fully and freely in critical discourse and the resulting action. Critical reflection is a key concept in transformative learning theory. How can educators promote and support transformative learning. Most importantly, the educators need to take a reformist perspective, rather than a subject-centred perspective. Here the educator is a co-learner and provocateur;
NC-CTHPE 2016
70
National Conference on Changing Trends in Health Professions Education
they challenge, stimulate and provoke critical thinking. They need to create an environment that encourages and rewards intellectual openness. Teaching strategies making intentional use of transformative learning theory directed towards each process involved in TL could include the following: -
The activating event (triggering students to examine their thinking);
-
identifying current assumptions (critical questioning techniques);
-
encouraging critical reflection (students privately examine their current assumptions);
-
encouraging critical discourse (creating opportunities for students to reflect through conversation); and
-
giving students an opportunity to test a new paradigm or perspective (opportunities to students to apply new knowledge). All through for transformative learning to occur, the instructor or the educator must strike a careful balance between support and challenge. The key step to implementing educational reforms to promote transformative learning is the faculty development. Faculty development programs need to be designed in such a way so as to use the above techniques promoting transformative change in the educators first thus empowering them to innovate with the student learning.
11. Dr. K.A.Narayan
Dr K.A. Narayan is the Professor of Community Medicine & Academic Training and Development Consultant with long experience in Health Professions Education, with special interest in curriculum planning, program evaluation and Disaster Management training. Before joining MGMCRI, Dr Narayan had long experience at JIPMER, besides 7 years stint at AIMST University, Malaysia.
NC-CTHPE 2016
71
National Conference on Changing Trends in Health Professions Education
He is the program coordinator for the PGDHPE program of SBV and a resource person for the MEU. It is difficult to get in one person a rich diversity of expertise which Dr Narayan possesses, such as epidemiology, biostatistics, medical informatics, ethics, disaster management, disease surveillance, quality assurance & accreditation, assessment, program evaluation, research methodology including both quantitative and qualitative techniques.
Dr Narayan has to his credit 50 peer reviewed articles in journals of high impact, and he has authored 7 books or chapters besides technical papers and PBL modules. Email:narayan.ka@gmail.com, Skype id: narayan_ka
INTER- PROFESSIONAL APPROACH TO CAPACITY BUILDING IN EDUCATIONAL SCIENCES – The SBVU Innovation in launching Innovative Programs in Health Professions Education
Dr. K.A.Narayan, Professor, Dept. of Community Medicine Rapid expansion of Health Professions Education in the country has created a need for preparing a new generation of health professions educators, who would serve as educational leaders, irrespective of their background in medicine, dental, nursing or allied health sciences. The expansion has also led to a shortfall in trained and competent teachers. This shortfall is partially met by training programmes mandated by the regulatory bodies. However, most of the available training programs are short term and uni-disciplinary. Rapid strides have been made in pedagogical sciences. Growth of knowledge management systems and information technology have added new challenges to health professions education. Identifying this gap, The Sri Balaji Vidyapeeth implemented an inter professional capacity building programme starting with dental educators in 2013. Following this a full-fledged University level Postgraduate Diploma in Heath Professions Education (PGDHPE) was implemented in 2014. The duration of the course was for one year. Based on the successful experience, the programme has been restructured as a Credit Based Program of one year, incorporating 4 certificates programmes. Further, a one year MPhil programme has been designed for those completing the PG Diploma or any other equivalent programmes. The university also offers Ph D in Health Professions Education. Thus, the University has achieved the unique distinction of providing a full range of courses in educational sciences for health professionals.
NC-CTHPE 2016
72
National Conference on Changing Trends in Health Professions Education
12. Usha Carounanidy
Dr Usha Carounanidy completed Bachelor of Dental Surgery from Madras Dental College, Chennai in 1989 and Master of Dental Surgery from Conservative Dentistry and Endodontics, from BHU, Varanasi, UP in 1991. She gained additional qualification PGDHPE from Sri Balaji Vidyapeeth, Puducherry in 2015.She has 21 years of experience as a passionate teacher in her field serving tenure in BDCH, Davangere, MGPGI, Puducherry and RMDCH, Annamalai University since 1992. Her passion for teaching won her the Best Teacher Award from Annamalai University in 2007. She has numerous publications to her credit in the journals and chapters in books in conservative Dentistry and Endodontics. She has co-authored a hand book for endodontic practice, by Jaypee publishers. She is the co-director for a dental education website, onlinedentallearning.com, in which she has published numerous case reports, articles, procedural videos along with her husband Prof. Dr.R. Sathyanarayanan. She has been invited for more than100 guest lectures by various institutions and national/ regional associations. Currently she is associated with Sri Balaji Vidyapeeth, as the Dean, Faculty of Dentistry, and Principal, Indira Gandhi Institute of Dental Sciences. She is an active member of the Dental education unit of the institute.
SBV INITIATIVE – DENTAL EDUCATION UNIT Dr. Usha Carounanidy, Dean, IGIDS, Pondicherry One of the maiden activities of SBV-AHEAD (Academy of Health Professions Education and Academic Development) is the Capacity Building program for the faculty of Indira Gandhi Institute of Dental Sciences, on educational technology. The program was of 8 months duration commencing from June 2013 to January 2014. The sessions were held fortnightly and covered topics in educational system, objectives, TL methods and media, evaluation and assessment. All 40 faculty were certified at the end of the course. Pretest and posttest had shown a significant difference indicating the success of the program. Formation of a Dental Education Unit with 9 volunteers is the major outcome of this inter-professional capacity development program.
NC-CTHPE 2016
73
National Conference on Changing Trends in Health Professions Education
The young unit under the tutelage of the mentors from AHEAD, started the Training of the Trainers program, for the dental educators. The duration and course content varies as per need of the institutions from 2 days, 4 days or 6 days. Around 50 senior and junior teaching faculty from 4 neighboring dental institutes have undergone this course. In 2016, external consultancy was extended to 25 faculty in a dental institute in Chennai. Internal faculty development program for the other newly recruited faculty was also done by the DEU. The satisfactory program feedbacks and the statistically significant difference in the pre-test and post-test score indicates the effectiveness of all the program. Dental education unit has also expanded to a 13 member team in 2016. Recently efforts have commenced in analyzing the outcome of the programs at the Kirkpatrick’s levels.
13.Dr.Anshu, MBBS, MD, DNB, MNAMS, MHPE
Dr Anshu is a graduate and postgraduate from Government Medical College, Nagpur. In 2002-03, she trained in Oncopathology and Cytology at the Tata Memorial Hospital in Mumbai. She was awarded a Commonwealth Academic Staff Fellowship in 2007 at Guy’s Hospital and St. Thomas’ Hospital in London, United Kingdom to train in cervical cancer screening and liquid based cytology. Dr.Anshu is a key member of the MGIMS medical education unit. She has been awarded a CMCL-FAIMER Fellowship from Ludhiana (2007) and a Foundation for Advancement of International Medical Education and Research (FAIMER) Institute Fellowship from Philadelphia (2009). She is a faculty member and resource person at all three Indian FAIMER Regional Institutes—CMCLFAIMER, Ludhiana; GSMC-FAIMER, Mumbai; and PSG-FAIMER, Coimbatore. She has been invited as global faculty for the FAIMER-Institute at Philadelphia in 2011-12. Dr.Anshu is also a resource person for the advanced medical education workshops conducted each year by the Medical Education Department of the Maharashtra University of Health Sciences (MUHS), Pune. She is on the Board of Studies for Medical Education at MUHS. She has also written three WFMEFAIMER distance learning modules for the Open University Centre for Education in Medicine (OUCEM), UK. She has edited a book along with Dr Tejinder Singh titled ‘Principles of Assessment in Medical Education’. She has been invited as guest speaker and resource person for several national and regional medical education conferences and workshops. In 2012, Dr Anshu was
NC-CTHPE 2016
74
National Conference on Changing Trends in Health Professions Education
awarded the International Fellowship in Medical Education (IFME) from FAIMER, USA. The award allowed her to pursue her Masters in Health Professions Education (MHPE) from Maastricht University, which she completed with distinction in 2014. She also organized the National Conference in Health Professions Education in 2014.
14. Dr.Himanshu Pandya
Dr.Himanshu Pandya is Professor of Medicine and Medical Education at Pramukhswami Medical College, Karamsad, Gujarat. Dr.Pandya is convener of MCI Nodal Centre for National Faculty Development Program at Pramukhswami Medical College. He is Dean of Faculty of Medicine at Sardar Patel University, Vallabh Vidyanagar. Dr.Pandya is a member of expert group for revision of Basic Course Workshop under MCI National Faculty Development Program. He is national consultant for MCI Fellowship in Medical Education (FIME), He has been a resource faculty at National Conference in Health Profession Education (NCHPE) and at GSMCFAIMER Regional Institute. He is a member of executive committee of National Academy of Health Profession Education. His areas of interest are faculty development and educational research.
INTEGRATED ASSESSMENT Dr.Himanshu Pandya, Professor of Medicine & Medical Education at Pramukhswami Medical College, Karamsad, Gujarat Integrated assessment refers to assessment of mastery of curriculum content in manner that is closest to the way in which any learning is applied in practice. The content of different disciplines is assessed at a single examination instead of assessing individual disciplines separately. If the curriculum model is integrated, the written curriculum should define integrated outcomes and the assessment system blue printed on to these curriculum outcomes. A curriculum must have coherence and the same model or approach throughout. One common mistake is to develop individual discipline-based questions and then include them within the same examination. If individual questions can be answered without drawing on the content of different disciplines, then students
NC-CTHPE 2016
75
National Conference on Changing Trends in Health Professions Education
are not driven to learn curriculum content of different disciplines in an integrated manner. One of the common problems mentioned with regards to integrated assessment is students passing examinations with wide gaps in knowledge. In truly integrated assessment questions, it is not possible to do well in one discipline while not doing well in the other. It is a problem when the assessment is poorly written or not properly integrated. The problems related to integrated assessment can be avoided by developing properly planned and blueprinted assessments that have truly integrated different contributory disciplines in a given question. All examination question setters need to master the skills of getting integrated questions before writing items. The most common assessments formats are MCQ, structured assay questions and the clinical examination.
15. Dr.Gitanjali Batmanabane, MD, PhD
Gitanjali Batmanabane did her undergraduate and postgraduate training from the Jawaharlal Institute of Postgraduate Medical Education & Research (JIPMER), Puducherry and her PhD from Pondicherry University. She is Professor and Head of Pharmacology at JIPMER. She was Technical Officer, Essential Medicines & Other Drugs, at the World Health Organization, South East Asia Regional Office, New Delhi for two years (from 2010 to 2012) and coordinated the Better Medicines for Children project in India. She is Section Editor for Clinical Pharmacology, for the Journal of Pharmacology and Pharmacotherapeutics. She is a member of the NTTC core-group at JIPMER and was Head of the Dept. of Medical Education at JIPMER (2013-2016). She is a member of the World Health Organization’s (WHO) Expert Committee on the Selection and Use of Essential Medicines and is also a member of the WHO Expert Advisory Panel on Drug Evaluation. She heads the WHO Collaborating Centre for Research and Training in Essential Medicines and Rational Use of Medicines at JIPMER. She also is the Nodal Officer for JIPMER and is Faculty (Finance). She has conducted many workshops on Elementary Biomedical Statistics, Research Methodology and Biomedical Communications all over India. Her area of interest is essential medicines and their rational use and medical education. She has many publications in national and international journals
NC-CTHPE 2016
76
National Conference on Changing Trends in Health Professions Education INTEGRATED TEACHING: TEACHERS’ PERSPECTIVES Dr.Gitanjali Batmanabane
Professor & Head, Dept. of Pharmacology, JIPMER Teachers are the most important stakeholders in the successful implementation of the integrated teaching. Unless they cooperate in a spirit of team teaching, one can’t expect good results. In the Indian context, the teachers in general are not tuned to the concept of integrated teaching. They have been trained in a traditional approach, in which the departmental affiliation is very strong. Lack of awareness of the information dealt by other departments makes them feel uncomfortable. What they have learnt and have been teaching for a long time is the only correct approach, according to them. An artificial barrier between, basic sciences and clinical departments also creates a hurdle for gaining new knowledge which the other discipline offers. However, once the teachers engage in such activity by chance or by choice, they tend to accept it more and become part of the change process. Many medical colleges have overcome the problems mostly by dynamic leadership on part of the Dean, and active role played by the Medical Education Units, and sometimes by enforcing measures such as compliance of requirement for recognition by the MCI. The experience shows that the training and involvement of the faculty in the implantation process goes a long way in successful implementation. The recent initiatives like competency based medical education (CBME), and representation of MEU faculty in the Curriculum committees, and general enthusiasm of the faculty in attending higher courses such as NTTCS, FAIMER, FIME or Advanced Courses are likely to push greater participation of the faculty in integrated teaching and assessment activities.
16. Dr.Latha Ravichandran
Dr Latha Ravichandran is Professor of Paediatrics, Sri Ramachandra Medical College and Research Institute, Senior consultant, Sri Ramachandra Medical Centre, President, AHA, IAP Chennai City, Co-convener, MCI Basic Workshop on Medical Education technologies, Faculty, Department of Medical Education , at MCI Nodal
NC-CTHPE 2016
77
National Conference on Changing Trends in Health Professions Education
Centre at SRMC and NATIONAL Consultant, MCI Advanced course for Faculty Development. Dr Latha’s main area of interest is adolescent health. She has established the Adolescent Clinic at Sri Ramachandra Medical College and Research Institute in 1999. She has organized a large number of programs in this area during the last ten years, presented and published papers.
INTEGRATED TEACHING – STUDENTS PERSPECTIVE Dr.Latha Ravichandran Professor of Paediatrics, Sri Ramachandra Medical College and Research Institute, The terms traditional and integrated curriculum represent two extremes of the spectrum of the integration ladder as described by Harden from discipline based teaching (isolation) at one end to full integration at the other (transdisciplinary) . Whether it is traditional or integrated learning, students are the stakeholders. Sharing an experience from Sri Ramachandra medical college and Research institute.The institution introduced an integrated curriculum for MBBS in 2006. The organ system block was the dominant mode of instruction in first two phases while traditional discipline based instruction dominated phase III with a small proportion of newer methods including problem solving, clinical skills and Professional development (PRODEV). By design, phase I had tighter integration than in subsequent phases. The integration was introduced phase wise as the students moved from first to third phase. An intense orientation program at the beginning of each phase prepared the students for the change. Horizontal and vertical integration through Organ system blocks , Anchoring lecture, experiential learning , linking cases, problem solving sessions in small groups, integrated projects, hybrid Problem based learning, and clinical skills sessions were some of the learning methods adopted . The students were supported by faculty mentors, provision of learning resources and modifications in infrastructure. A meticulous Formative evaluation system was introduced. The final assessment was however disciple based as per MCI norms .The effectiveness of the curriculum was evaluated through the student perception and the performance of the students A stakeholder feed- back on five point Likert scale was collected at end of each phase for three successive batches from 2006. There was a positive impact of integrated education on learning and growth of students. Higher impact noted in Phase 1 demonstrated effectiveness of tighter integration in enhancing learning and personal growth.The performance of students was analysed and compared with previous batches in traditional curriculum. Students who learnt in an integrated system did
NC-CTHPE 2016
78
National Conference on Changing Trends in Health Professions Education
not perform worse in discipline based assessments. Observation of a higher pass percentage was heartening. Key words , Student feed- back , Integrated Teaching
17. Dr. V. N. Mahalakshmi
Dr. V.N.Mahalakshmi did her MS (General Surgery) from Jawaharlal Institute of Postgraduate Medical Education & Research (JIPMER), Pondicherry and MCh (Paediatric Surgery) from Madras Medical College, Chennai. She also has a One year certificate course in Hospital Management from National Institute of Health and Family Welfare, New Delhi and Honorary Fellow of The Royal College of Surgeons, Glasgow). Currently she is pursuing PhD in medical education under Sri Balaji Vidyapeeth University, Pondicherry. She is currently Vice Principal Curriculum from May 2015 onwards and Member of Core Team SBV collaborations with Partners Medical International (associated with Harvard Medical School) – to bring about Curricular reforms. She has to her credit 10 publication in Book Chapters and has organized four conferences. She has taken keen interest in activities of medical education unit and other activities related to curriculum reforms at SBV. Her diverse areas of interest are Quality Assurance in Healthcare and Patient Safety, Process control and Ergonomics, Healthcare leadership, Computerisation and Standardisation of the evaluation system, Post validation of learning outcomes and curriculum mapping, Curriculum development and Developing PBL cases.
SETTING STANDARDS AND INNOVATIONS Dr. V. N. Mahalakshmi, Vice Principal (Curriculum), MGMCRI Introduction As a part of the quality initiatives involving Teaching-Learning-Evaluation systems, the Exam division of Sri Balaji Vidyapeeth University, under the able guidance of our honorable Vice-Chancellor, Prof. K.R. Sethuraman, an educationalist par excellence, has taken initiatives to benchmark standards and innovations in the evaluation process.
NC-CTHPE 2016
79
National Conference on Changing Trends in Health Professions Education
Innovations in the exam process
The process of standardization started with an analysis of the strengths and weaknesses of the existing system and search for technically and logistically viable options. Once the analysis of the strengths and weaknesses of the existing system was complete, the following innovations/ standardizations are introduced in the exam process. UG exams 1. Eliminating Ambiguity in questions - As a part of the quality initiatives, the SBVU exam division is set about eliminating ambiguity in questions. The question papers pattern is changed to include very short objective questions, focused short answers and structured essay questions. SBVU-AHEAD, the Academy Of Health Education And Development, organized and conducted workshops on “Question paper setting and validation” to all faculty of the constituent colleges. As a follow-up of this work shop, all the Departments prepared the blue print guidelines of question papers based on the specific learning objectives (SLO) in mind. This is used as a template for the question paper setters. The paper setters are given elaborate blue print guidelines specific to the learning objectives of the subject being evaluated and also weight-age for various systems. They are asked to fill in an item card analyzing the distribution of questions and marks across systems, level of difficulty and type of knowledge being tested – recall, understanding or application. They are also asked to submit a relevant answer key covering the key points to be discussed in the answer. The paper setters are asked to frame specific and relevant questions, without ambiguity. 2. Vetting of the question papers -The question paper received from the examiners are subjected to a 3 stages vetting process involving, Matching against the blue print guidelines & Looking for grammatical errors, errors in the framing of questions and repetition – to be done by COE’s office. Checking for relevance and validity by the concerned subject expert. All question papers are subject to scrutiny and approval by the Vice- Chancellor, for their global relevance and applicability to the student population being tested. A checklist encompassing these details is evolved and is being filled by the exam division. 3. The actual conduct of exams Secure online transmission and printing of question papers to off campus institutions in secure, encrypted form ½ an hour before the start of exams. 4. Redesign of Answer Booklets - To expedite the exam process, OMR coding of answer books is introduced to code student and exam information. Each booklet has an unique barcode to tag examinee information and valuation. 5. The answer booklets are subjected to central evaluation. To eliminate ‘examiner bias’, each examiner is asked to correct the same question in all the answer booklets – Item Marking.
NC-CTHPE 2016
80
National Conference on Changing Trends in Health Professions Education
6. Post validation of learning outcomes is done through Evaluation of the group performance by plotting of the marks scored by all the students in the group to total marks awarded for each question. This process can identify the potential faults in the evaluation tool i.e., the question themselves or the evaluation process (examiners). This also helps in the need for moderation of the group score if there are flaws in the system / tools. Also, the triple feedback loop helps the curriculum planners to evaluate the validity of the learning process. Though this system has been used extensively in many Universities & Colleges across India, our evaluation is unique, that it allows analysis of marks awarded to individual questions. This robust system was conceived and developed by Dr.Mahalakshmi under the able guidance of our Vice- Chancellor, Prof.K.R. Sethuraman, in collaboration with the Department of Information Technology to suit our local needs and has an error free rate of six sigma. Practical / Clinical exams Having restructured the theory exams and systemized the exam process, we set out to objectivise the practical /clinical / oral exams. This is by introducing OSCE / OSPE and structured viva in the exams. A series of workshops on Objectivising the clinical /practical /Oral exams on OSCE / OSPE for faculty of the constituent colleges planned for in Feb-June 2014 and robust OSCE / OSPE blueprints and subject wise question banks developed. A national level, nodal meeting was held to present the SBV’s plan to align with MCI and seek experts opinion on the project, in May 2014. The model blueprints with the expert groups’ comments have been submitted to MCI for approval. Oral Exams The oral / viva-voce exams for UG students have been restructured as ‘Structured Viva’ examinations, which follow a definitive blue print and specific mark allocation pattern for different topics. The successful introduction of changes in the MBBS exams has helped us to carry forward the changes in the UG Dental & Nursing courses. PG exam reforms The following innovations/changes were brought about in the PG exam process. I. II. III. IV.
To eliminate ambiguity in the setting up of question papers, detailed blue printing of the question papers has been done and is followed. The long essay type questions are replaced by ’10 Brief Essay’ questions, to improve the sampling. To eliminate bias, all answer sheets of all students are being evaluated by all the examiners (4 times valuated) The evaluations of PG dissertations have been made more objective by using a designing checklist for examiners to evaluate the dissertations. The data from the evaluators is shared with the subsequent batch of PG students in the ‘Dissertation Writing’ workshops, so that such shortfalls can be minimized and eliminated.
NC-CTHPE 2016
81
National Conference on Changing Trends in Health Professions Education THE INTEGRATED CURRICULUM Dr. V. N. Mahalakshmi, Vice Principal (Curriculum), MGMCRI
“The integrated curriculum is like getting a new pair of lenses that make teaching a lot more exciting and help us look forward into the next century. It is helping students take control of their own learning.” - M. Markus, teacher. “I'm learning more in this course, and I'm doing better than I used to do when the subjects were taught separately”.- Student. This teacher and student express an increasingly widespread enthusiasm for curriculum integration, a new way of looking at teaching. Curriculum integration has received a great deal of attention in educational settings.
Definitions Shoemaker defines an integrated curriculum as ...”education that is organized in such a way that it cuts across subject-matter lines, bringing together various aspects of the curriculum into meaningful association to focus upon broad areas of study. It views learning and teaching in a holistic way and reflects the real world, which is interactive”. Dressel's definition goes beyond the linking of subject areas to the creation of new models for understanding the world: “In the integrative curriculum, the planned learning experiences not only provide the learners with a unified view of commonly held knowledge (by learning the existing models, systems, and structures) but also motivate and develop learners' power to perceive new relationships and thus to create new models, systems, and structures” These definitions support the view that integrated curriculum is an educational approach that prepares the medical students for lifelong learning. There is a strong belief that medical schools must look at education as a process for developing abilities required by life in the twenty first century, rather than discrete, departmentalized subject matter.
Components of the integrated curriculum In general, all of the definitions of integrated curriculum include: Relationships among concepts (curricular links) Thematic units as organizing principles enrichment or enhancement activities with a cross-curricular focus assessment activities that are also cross-curricular in nature Flexible schedules Flexible student groupings. The basis of developing the integrated curriculum The "explosion" of knowledge, the increase of state mandates related to myriad issues, fragmented teaching schedules, concerns about curriculum relevancy, and a lack of connections and relationships among disciplines have all been cited as reasons for a move towards an integrated curriculum. These forces in contemporary education, along with
NC-CTHPE 2016
82
National Conference on Changing Trends in Health Professions Education
the trends towards global interdependence and the interconnectedness of complex healthcare systems, the increase in pace and complexity of the twenty-first century, the expanding body of knowledge, and the need for healthcare workers to have the ability to draw from many fields and solve problems that involve interrelated factors are compelling reasons to integrate the curriculum. Educational theories also support the fact that Curriculum integration is a way of making education more meaningful. Learning is believed to occur faster and more thoroughly when it is presented in meaningful contexts, with an experiential component. Learning is best accomplished when information is presented in meaningful, connected patterns. Finally, the movement toward a global economy and international connections, as well as the rapid changes in technology, are pushing education toward integration. The ability to make connections to solve problems by looking at multiple perspectives, and to incorporate information from different fields, will be an essential ingredient for success in the future. An enduring argument for integration is that it represents a way to avoid the fragmented and irrelevant acquisition of isolated facts, transforming knowledge into personally useful tools for learning new information.
Research findings support the positive effects of curriculum integration Integrated curriculum helps students apply skills. An integrated knowledge base leads to faster retrieval of information. Multiple perspectives lead to a more integrated knowledge base. Integrated curriculum encourages depth and breadth in learning. Integrated curriculum promotes positive attitudes in students. Integrated curriculum provides for more quality time for curriculum exploration. Factors that need to be considered in an integrated curriculum are Common definitions of terms (such as theme, strand, or outcome) Available resources Flexibility in scheduling Support services including e-learning tools Subjects and concepts that will be integrated Links between integration and broader outcomes Curricular scope and sequence How evaluation will occur Parent and community support Themes that promote the transfer of learning and connections (curricular strands) Team planning time that is used to exchange information about content, students, special areas of teacher expertise, and teaching methods.
NC-CTHPE 2016
83
National Conference on Changing Trends in Health Professions Education
Abstracts of free paper session
NC-CTHPE 2016
84
National Conference on Changing Trends in Health Professions Education 1. FREE PAPER SESSION Author Name: Designation : Institute : Email : Mobile :
Ananda Balayogi Bhavanani Deputy Director CYTER Sri Balaji Vidyapeeth, Pondicherry yoga@mgmcri.ac.in 9842311433
SecondAuthor: Designation : Institute :
Madanmohan Director CYTER and Head, Dept of Physiology, MGMCRI Sri Balaji Vidyapeeth, Pondicherry
Abstract Title: RESTORING HUMAN VALUES IN MEDICINE: ROLE OF YOGA Recent developments showcased through social media highlight a lack of human values in modern medical professionals. Compassion, empathy and a sincere desire to relieve suffering are found lacking and this seemingly becomes even rarer as qualifications increase. Exploitation of trust with kidney rackets, unnecessary surgeries, lab referral commissions and inflated bills are commonly bemoaned and even recently medical students in Chennai threw a poor dog off their rooftop with glee. This paper suggests a view that introduction of Yoga in medical education may help stem the rot and restore values. Why yoga? Yoga is an ancient cultural heritage of India spreading rapidly and being practiced by millions across the globe. It offers a broader perspective of life and refines the personality thus enabling practitioners to attain their inherent potential in a holistic manner. Yoga is not just a system of exercise but is a way of life. It stresses the importance of social and personal values through the yama (restraints of subhuman tendencies such as violence, stealing and greed etc) and the niyama (humane observances including cleanliness, contentment, self-introspection and dispassionate discipline). The inculcation of these universal values in medical students at the start of their professional career can help them be more humane in their life and profession. Suggested mechanisms Numerous physical and mental techniques of Yoga such as asana, pranayama, dharana and dhyana enable the attainment of physical, mental and emotional fitness. This facilitates a skillful and efficient management of omnipresent stressors. Inculcation of a broader ‘worldview’ leads to the performance of one’s duty in a spirit of nishkama karma (non-attachment to results of actions) thus preventing unhealthy “Me first”, “Make the most money”, “Who cares as long as I am safe” type of attitudes. Healthier connection with one’s inner being creates a cheerful, strong and compassionate countenance with empathy towards the suffering.
NC-CTHPE 2016
85
National Conference on Changing Trends in Health Professions Education
Conclusion
Introduction of Yoga as a holistic way of life with stress on its astha anga (eight components) in the medical curriculum will inculcate a compassionate sense of selfless service (karuna and seva) towards our human brethren. We need to understand that illness becomes wellness when we consciously move from the limited sense of “I” to a broader inclusive “WE". Such an understanding will motivate young doctors to be vehicles of change thus restoring once again the much extolled nobility of our medical profession. 2. FREE PAPER SESSION Author Name: Designation : Institute : Email : Mobile:
Carounanidy Usha Principal Indira Gandhi Institute of Dental Sciences, Sri Balaji Vidyapeeth principal@igids.ac.in 09843184039
Abstract Title: MULTISOURCE POSTGRADUATION
FEEDBACK
IN
DENTAL
Introduction Workplace based assessments are effective tools to assess professionalism. Multisource feedback is one of such assessment methods. It can also be used as formative assessment in postgraduation. This study was done to assess the intention-to-change towards better professionalism among dental postgraduates of Indira Gandhi Institute of Dental Sciences after exposing them to MSF process.. Methodology Colleague assessment questionnaire was used to obtain feedback from 7 colleagues for each clinical postgraduate. Patient assessment questionnaire was used to obtain feedback from 15 patients for each postgraduate. Selfassessment questionnaire was designed with similar elements. The feedbacks were shared with the postgraduates in a private session comparing with selfassessment. After 24 hours reflection, feedback was obtained from them, on the influence of MSF procedure on their attitude and behaviour as well on feasibility of implementation. Results All the postgraduates agreed that MSF can improve upon their communication skills and attitude, if used as a formative assessment tool. An intention-tochange at Kirkpatrick’s level 2a was evident from their feedback. Thus if MSF is implemented in dental postgraduation, a definite improvement in professional behaviour can be expected.
NC-CTHPE 2016
86
National Conference on Changing Trends in Health Professions Education
3. FREE PAPER SESSION Author Name: Designation : Institute : Email : Mobile :
Daynidy G Lecturer CYTER Sri Balaji Vidyapeeth, Pondicherry dayanidy@gmail.com 9789210593
SecondAuthor: Designation : Institute :
Ananda Balayogi Bhavanani Deputy Director CYTER Sri Balaji Vidyapeeth, Pondicherry
ThirdAuthor: Designation : Institute :
Madanmohan Director CYTER and Head, Dept of Physiology Sri Balaji Vidyapeeth
Abstract Title: PSYCHOPHYSIOLOGICAL BENEFITS OF YOGA TRAINING IN PHYSIOTHERAPY STUDENTS AT PONDICHERRY Introduction Yoga is primarily a spiritual science and a healthy life and worldview is a byproduct of its practice. It is essential that paramedics are physically, mentally and spiritually healthy and hence an invite to conduct 12-weeks of Yoga training for undergraduate physiotherapy students of MTPG & RIHS was taken up and also utilized to study various psycho-physiological parameters for the purpose of scientifically validating such training. Materials and methods Integrated Yoga sessions comprising of a combination of jathis (loosening practices), kriyas (breath-body coordination practices) along with asana, pranayama, contemplation and relaxation were conducted for 12 female and 3 male students twice weekly for three months. Anthropometric, cardiovascular, heart rate variability (HRV), reaction time and psychological parameters were measured before and after training period and statistical analysis done using Students t (paired) test. Results There was a significant reduction in weight and BMI, as well as hip and waist circumference following training. All resting cardiovascular parameters reduced significantly with significant shortening of auditory and visual reaction time. Improvements were noted in all HRV parameters and there was enhancement of quality of life index (QOL) scores and retrospective wellness scores. Discussion The above mentioned improvements in psychophysiological parameters suggest normalization of cardiac autonomic function with improved central neuronal processing. Improvements in anthropometric, cardiovascular and neurological
NC-CTHPE 2016
87
National Conference on Changing Trends in Health Professions Education
parameters, coupled with positive changes in HRV and QOL indices signify a healthier state of body and mind. Conclusion
Our study gives preliminary evidence of positive psychophysiological benefits of Yoga training in a graduate student population. We suggest the inclusion of Yoga in paramedical collegiate education and recommend further controlled studies to validate such training.
4. FREE PAPER SESSION Author_Name: Designation : Institute : Email : Mobile :
Dr Mahalakshmi VN VP Curriculum MGMCRI vp@mgmcri.ac.in 9244436037
Second Author: Designation : Institute :
Dr Ravishankar M Dean MGMCRI
Third Author: Designation : Institute :
Dr Partha Nandi Vice Principal Students MGMCRI
Abstract Title: CHALLENGES OF STUDENTS - A UNIQUE SOLUTION
CLINICAL
POSTING
FOR
250
The challenges before faculty when they handle a very large group of students such as 250 of them are to ensure that students receive effective clinical skills education through both teaching and assessment of clinical skills. However, these numbers project a huge problem by themselves especially in semester 3, wherein they have to be split into just 4 departments. This paper elaborates on our experience of effective handling of 237 students into semester 3 using a novel approach. An integrated approach to clinical teaching was undertaken, the philosophy, process and outcome of which is detailed in the presentation.
5. FREE PAPER SESSION Author Name: Designation : Institute : Email :
NC-CTHPE 2016
Dr. Partha Nandi Professor of Community Medicine MGMCRI Pondicherry nandipartha13@gmail.com 88
National Conference on Changing Trends in Health Professions Education
Mobile
:
9994017873
Second Author: Designation : Institute :
Dr. D.R. Bharati Associate Professor of Community Medicine IGIMS, Patna
ThirdAuthor: Designation : Institute :
Dr. K. A. Narayan Professor of Community Medicine MGMCRI
Abstract Title: VALUE OF OBJECTIVE STRUCTURED CLINICAL EXAMINATION IN THE FORMATIVE ASSESSMENTOF CLINICAL POSTING IN COMMUNITY MEDICINE GRADUATE TRAINING PROGRAMME Background Objective structured clinical examination (OSCE) was designed to improve reliability of the clinical examination. Objective of the study was to find the effectiveness of OCSE in comparison with the conventional method this study was con-ducted in Community Medicine end-posting examination. Methods An educational interventional study was conducted among the 7th semester students to find the effectiveness of OCSE in comparison with the conventional method of ‘end-posting examination’ using stations and checklists as a part of formative assessment at the end of their clinical posting in the department of Community Medicine. Results The mean score obtained by the students in group one by conventional method was lesser than OSCE method; this difference was statistically significant. By OSCE method, maximum number of student had provided improved performance. Conclusions Performance by students in the applying OSCE in the formative assessment was found to be significantly better in comparison with the conventional method. Maximum number of students performed above average in the OSCE compared to the conventional pattern of assessment.
6. FREE PAPER SESSION Author Name: Designation : Institute : Email : Mobile :
NC-CTHPE 2016
Jayshree Kharche Assistant Professor Bharati Vidyapeeth Deemed University Medical College jskharche@gmail.com 9823535324 89
National Conference on Changing Trends in Health Professions Education
SecondAuthor: Designation : Institute :
Asmita Phadke Associate Professor Bharati Vidyapeeth Deemed University Medical College
ThirdAuthor: Designation : Institute :
S M Vaidya Professor & HOD Bharati Vidyapeeth Deemed University Medical College
Abstract Title: STUDENTS
ASSESSMENT
OF
HEALTH
AWARENESS
IN
I
MBBS
Background Medical student is the future doctor and one should be aware of own health status. Therefore, this study to assess heath status in medical students was carried out. Objectives To assess health awareness of I MBBS students. Methodology: Total 148 students were present for the health checkup (Boys= 69, Girls=79). Detailed medical history was obtained from each student and thorough general and systemic examination and physical fitness tests were performed in all the students. Results The Boys (16 %) had BMI ≥25 Kg/m2. 10 % of boys were found obese having BMI ≥ 30kg/m2 whereas the girls (17 %) had BMI ≥25 Kg/m2 and 10 % were obese. Only 10 % of boys and 20 % girls were underweight as evidenced by BMI <18Kg/m2. In all 68 % of students were immunized for hepatitis B and 69 % of students were immunized for tetanus. Majority of them had no knowledge of dangers of hepatitis-B or tetanus and protection offered by vaccination. Half (50%) of the students had no knowledge about pubertal changes and association between personal hygiene and skin diseases. Family history of hypertension was present in 26 % of students and that of diabetes in 43 % of students. Only 3 % of girls were found to have borderline hypertension and were referred to physician. Interestingly, 70% of the students were not aware of the future risks posed by family history of diabetes mellitus and hypertension. Conclusion It is important to maintain optimum health for every medical student to avoid future risk of various life style related diseases.
NC-CTHPE 2016
90
National Conference on Changing Trends in Health Professions Education
7. FREE PAPER SESSION
Jyothi.V1,Rajesh Kumar Konduru 2,Kalaiselvi 3, Zile Singh4 1. Junior Resident, Department of Community Medicine, Pondicherry Institute of Medical Sciences, 2 .Associate Professor, Dept Of Community Medicine, PIMS, 3. Assistant Professor, Dept. Of Community Medicine, PIMS, 4.Prof and HOD, Dept. of Community Medicine, PIMS, Pondicherry.Phone :0413-2656068, Mobile â&#x20AC;&#x201C; 09443843304,E-mail:dr.jyothivasudevan@gmail.com Abstract Title:PRACTICAL APPROACH TO LEARN RESEARCH THROUGH ROME- OUR EXPERIENCE Introduction Engaging students in active learning lies at the heart of effective education. The Medical Council has recommended that learning outcomes for all medical graduates should include research skills to enable them to obtain insight into scientific and research methods. Keeping in mind this recommendation, the Dept. Of Community Medicine, PIMS has introduced a month long ROME (Reorientation of Medical Education) posting for the students of the Sixth Semester, to give them a firsthand practical experience of research methodology. Methodology he entire batch was divided into four groups, each group closely monitored by and guided by two faculty and one PG student. Their classes were rescheduled for one month. Our group developed a protocol to assess the morbidity pattern and quality of life of the elderly population in a rural area of Tamil Nadu. The students collected data by going on house to house visits. Each proforma was cross checked for validity by the PG and Faculty. Data entry and analysis was done subsequently. Intervention was done by providing health education using IEC materials developed by the students. At the end of the posting, a detailed report was written by students and the findings presented in the PIMS Scientific Society Meet. Results Positive feedback was obtained from students who felt it improved interpersonal relationships, communication skills besides igniting their interest in research. Conclusions It was found that the ROME posting for undergraduates helped to a great extent in acquisition of skills like teamwork, time management, improving critical thinking and fostering positive attitudes toward science and scientific methodology. Similar activities can be carried out in other medical schools which will be of immense benefit to the undergraduates.
NC-CTHPE 2016
91
National Conference on Changing Trends in Health Professions Education 8. FREE PAPER SESSION Author Name: Designation : Institute : Email : Mobile :
DR. K. HENRI BALRAJ Professor MGMCRI - Pondicherry drhenribalrajk@gmail.com 9003547417
Abstract Title: A JOURNEY TOWARDS MULTIMODAL APPROACH IN TEACHING/LEARNING. A journey is an exploration which throws up challenges and opportunities. The journey in my teaching/learning experience of 20 plus years got enriched due to me being sensitive to the changing needs of students and the environment. I present this journey of my under-graduate teaching, which has aided me in my professional development. As I commenced my post-graduate course as a demonstrator, I realized that if I did some crucial time management; I could collect the students for brief discussions both in the practical and in the theory of the day. I noticed that it was soon a win win situation for both. Because of these discussions, later after demonstrator-ship, lectures were inter-active and I started to use verbal/non-verbal cues and body language. Simultaneously I realized the need for mentoring and hand holding the students for supporting their learning by empathizing, motivating, explaining, illustrating and recapitulating the concepts. I added the means of putting-up instructional objectives and communicating, and there was uniform benefit to the taught. Soon the level of the order in the taxonomy for these objectives rose. I then got the opportunity of using the interactive panel where the students see real time text and drawings projected along with the talk of the lecture. Exposure to faculty development program got me to initiate problem oriented learning. Relating to students thus became easier. Through-out this journey I learnt that we should create new opportunities and consider â&#x20AC;&#x2DC;problems as challenges.â&#x20AC;&#x2122;
9. FREE PAPER SESSION Author Name: Designation : Institute : Email : Mobile :
Dr. M. Shivasakthy Associate Professor, Dept of Prosthodontics Indira Gandhi Institute of Dental Sciences shivasakthym@igids.ac.in 9940724320
Second Author: Designation : Institute :
Prof. K.R. Sethuraman Vice Chancellor Sri Balaji Vidyapeeth
NC-CTHPE 2016
92
National Conference on Changing Trends in Health Professions Education
Third Author: Designation : Institute :
Prof. Carounanidy Usha Dean, Faculty of Dentistry Indira Gandhi Institute of Dental Sciences
Abstract Title: ASTROLOGY TO PREDICT THE FUTURE OF STUDENTS NEEDING ADDITIONAL CURRICULAR SUPPORT (SNACS) Referring to weak students as slow learners or low achievers is considered as pejorative term. Hence, it is replaced by the term Students Needing Additional Curricular Support (SNACS). The management of SNACS group students remain as nightmare for all educators irrespective of their profession and specialty. The ultimate pass percentage of any batch is adversely affected by the performance of this group. Providing remedial coaching for such students after they fail in the final exams is like ‘justice delayed’. Steps should be taken to prevent them from losing any subject within the same academic year. The undergraduate dental student’s performance in their internal exam and university exam was compared and the results suggest a strong relation. This paper throws light on identifying SNACS by predicting their future earlier, which provides sufficient time to implement the remedial measures.
10.
FREE PAPER SESSION
Author Name: Designation : Institute : Email : Mobile :
M.I.GLAD MOHESH Assistant Professor,Department of Physiology, Shri Sathya Sai Medical College & Research Institute, gladmohesh@gmail.com 9176282179
SecondAuthor: Designation : Institute :
Semmal Syed Meerasa Professor & Head,Department of Physiology, Shri Sathya Sai Medical College & Research Institute,
Abstract Title: PERCEPTIONS ON M-LEARNING THROUGH WHATSAPP APPLICATION: A PILOT STUDY ON FIRST YEAR MEDICAL STUDENTS Introduction In this era of digital learning, Medical education blended with technology will enhance a medical student to learn anything, anywhere, anytime. Mobile learning (M-learning) through the smartphones is one of the technological tool to achieve this concept. Objectives To determine the perceptions on M-learning platform for physiology by first year medical students. Methods I MBBS students who were on their study leave participated in this study(106). Students were assisted to revise the content of practical physiology from three different books in a WhatsApp
NC-CTHPE 2016
93
National Conference on Changing Trends in Health Professions Education
group,“SmartPhysio2015-16”. Optimal practical viva voce questions were posted every evening by the group admin. Feedback on this learning methodology was sought through a questionnaire designed with google forms. The results were reported in percentages of the total responses. Results M-learning of physiology happened on the go(96%). Most of them graded the method Good (88.31%). Students expected the messages to be posted anytime (45.45%), however 32.47% expected it to be posted in the evening. Students preferred reading the messages whenever they get time. They found it to be time saving as the content from 3 books are delivered into their mobiles. Conclusions
Students use Smartphone for communication and leisurely activities. Incorporating these devices as a learning tool will promote learning anywhere anytime. Students of this generation are at ease with this M-learning which is going to be a promising tool of medical teaching in the near future. Keywords : M-learning, Medical education, Physiology.
11.
FREE PAPER SESSION
Author Name: Designation : Institute: Email : Mobile:
Dr Mahalakshmi VN VP Curriculum MGMCRI vp@mgmcri.ac.in 9244436037
Abstract Title: TOOL
STRUCTURED VIVA AS A SUMMATIVE ASSESSMENT
Introduction The Viva-voce/Oral examination is an important element of summative and formative assessments in medical education. It is helpful in assessing the students’ knowledge of the subject and their ability to express it clearly. However, it tends to be highly subjective and examiner-dependent. By structuring the viva examination with regard to the specific content being evaluated and the time allotted for each student, objectivity of this form of assessment can be improved. Materials & Methods The viva examination for the summative university evaluation of I-MBBS course was structured with regard to time duration and the coverage of topics. Feedback was collected from the students and the examiners alike on this format of examination.
NC-CTHPE 2016
94
National Conference on Changing Trends in Health Professions Education
Results
The feedback form of students indicated that they were very satisfied/satisfied with this format of examination(93.7%).The major contributory factors were reduction in anxiety/stress level of facing the examiner, uniformity of time allotted for all students, preparation time given and question similar difficulty level asked to all students. The examiners were also satisfied with the uniform coverage of topics and wider sampling made possible by this method. Conclusion Structured viva examination can serve as a good tool for summative assessment. However, assigning clear system weightage, blueprinting of the process and developing a robust question bank are pre-requisites to enhance the quality of assessment. Keywords Structured viva, structured oral examination, assessment tool, medical education.
12.
FREE PAPER SESSION
Author Name: Designation : Institute : Email : Mobile :
Meena Ramanathan Cordinator-cum-Yoga therapist CYTER Sri Balaji Vidyapeeth, Pondicherry saineema@yahoo.com 9790582999
Second Author: Designation : Institute :
Ananda Balayogi Bhavanani Deputy Director CYTER Sri Balaji Vidyapeeth, Pondicherry
Third Author: Designation : Institute :
Renuka K Dean, Faculty of Nursing Sciences Sri Balaji Vidyapeeth
Abstract Title: YOGA FOR PSYCHOPHYSICAL BENEFITS
NURSING
STUDENTS:
RATIONALE
AND
Introduction Health professionals, especially of the nursing cadre, are constantly under extreme pressure from patients, caregivers, doctors and hospital authorities. They require high levels of professional competency, resilience, as well as ethical and compassionate behavior. Yoga has the potential to facilitate all aspects of human development and hence can help develop these attributes through attainment of physical, mental, emotional and spiritual wellbeing.
NC-CTHPE 2016
95
National Conference on Changing Trends in Health Professions Education
Materials and Methods
In collaboration with KGNC, biweekly Yoga training (60 min /session) was imparted to 60 students enrolled in BSc Nursing course for 6 months. Introduction to theoretical aspects of Yoga, its philosophy and practices was given along with practice sessions comprising of jathis (loosening practices), kriyas (breath-body coordination practices), suryanamaskar (sun salutation), asanas (postures), pranayamas (energy techniques) and relaxation. Selected biochemical and hematological parameters were recorded along with Ferrans and Powers QoL index before and after training period. Due to inability to have separate control group, changes were correlated with subjects´ frequency of attendance. Results and discussion Post-intervention statistical analysis (repeated measures of ANOVA) revealed highly significant and beneficial changes in most hematological and biochemical parameters. Major findings were enhanced bone marrow function, reduced allergic tendency, alkalization of urine, metabolic reconditioning (with special emphasis on liver function) and improvement in QoL indices. All changes correlated positively with subjects´ frequency of attendance, as evidenced by Pearson’s linear correlation testing. Significant improvements that also correlated positively with attendance were found in QoL index and subscales, at mid and post training. Conclusion The present pilot study provides evidence of beneficial psychophysical effects of Yoga training amongst nursing students. We suggest that Yoga be made an integral part of nursing education as being done at Sri Balaji Vidyapeeth.
13.
FREE PAPER SESSION
Author_Name: Designation : Institute : Email : Mobile :
Dr. N. Asha Rani Assistant Professor Adichunchanagiri Institute of Medical Sciences ashanellore@gmail.com 9448957069
SecondAuthor: Designation : Institute :
Dr Aliya Nusrath Professor & Head Adichunchanagiri Institute of Medical Sciences
ThirdAuthor: Designation : Institute :
Dr. Dhanalakshmi T A Associate Professor Adichunchanagiri Institute of Medical Sciences
NC-CTHPE 2016
96
National Conference on Changing Trends in Health Professions Education
Abstract Title : MEDICAL PROFESSION AS CAREER - PRESSURE OR PASSION: A CROSS SECTIONAL SURVEY AMONG UNDERGRADUATE MEDICAL STUDENTS. Background
To become an eminent doctor one has to work hard, endure lengthier periods of training both at undergraduate and postgraduate level, compromise personal and family time, and dedication for lifelong learning. In spite of these many shortcomings, in India we find lakhs of students are still eager to pursue medical profession. Hence the present study was designed to assess the probable factors influencing the students to choose medical profession as career Method A questionnaire based survey was carried out among 126 1st MBBS students to document motives for choosing medical profession, career aspiration on completion of a medical degree and willingness to serve in rural area immediately after completion of degree. Results Out of 126 students, 79 (62.69%) were females and 47 (37.30%) were males. Passion(41.26%) was the major motivational factor for choosing medical profession as career. 50%had decided to join medical profession before 10th standard and proportion was more among females (63%). Nearly 80% and 96% students planned to do rural service and post-graduation respectively. Majority of females opted for Obstetrics and Gynecology and males preferred surgical specialty as their post-graduation subjects. Conclusion The present study revealed that these students were early deciders and passion was their major motivational factor. There is a traditional gender based choices in choosing post-graduation specialty among males and females. So educational polices and career counselling seminars should be formulated to guide and encourage them to pursue career fields in medicine which are most needed.
14.
FREE PAPER SESSION
Author_Name: Designation : Institute : Email : Mobile :
Pranita Ashok Assistant Professor ,Dept of Physiology Bharati Vidyapeeth Deemed University Medical college pranita76@gmail.com 9850062612
SecondAuthor: Designation : Institute :
Jayashree Kharche Assistant Professor Bharati Vidyapeeth Deemed university Medical college
NC-CTHPE 2016
97
National Conference on Changing Trends in Health Professions Education
ThirdAuthor: Designation : Institute :
S M Vaidya Professor Bharati Vidyapeeth Deemed university Medical college
Abstract Title : METABOLIC EQUIVALENT TASK ASSESSMENT FOR PHYSICAL ACTIVITY IN MEDICAL STUDENTS
(MET)
Background The ability to assess energy expenditure (EE) and estimate physical activity (PA) in free-living individuals is extremely important in the global context of noncommunicable diseases including malnutrition, over nutrition (obesity) and diabetes. MET is used as a means of expressing the intensity and energy expenditure of activities Objective So the study was undertaken to assess the physical activity as Metabolic Equivalent Task (MET) using subjective questionnaire i.e. IPAQ. Material and Methods: TIt was a cross sectional study conducted on 87(29 males and 58 females) medical students aged between 18-25 years took part in the study. Detailed history of physical activity was taken so as to find out the type and quality of physical activity they were engaged in. In IPAQ (short) questionnaire information is asked about three specific types of activity such as walking, moderate-intensity activities and vigorous-intensity activities. Metabolic Equivalent Task (MET) is calculated by IPAQ evaluation which is one of the easiest methods for recording of the intensity of a physical activity. Results It was found that, as per MET score calculated from IPAQ, 40%, 47%and 13% students fall in low, moderate and high physical activity groups respectively. Conclusion : Mets utilization provides a convenient method to describe the functional capacity or exercise tolerance of an individual. Healthy habits among medical students are even more important as they are future physicians who personally ignore adopting healthy lifestyle are more likely to fail to establish health promotion opportunities for their patients.
15.
FREE PAPER SESSION
Author_Name:R. Ramesh, HOD. Dept., of Biochemistry, MGMCRI, Pondicherry Abstract Title RELATIONSHIP BETWEEN NONCOGNITIVE SCORES AND ACADEMIC PERFORMANCE AMONG STUDENTS REQUIRING ADDITIONAL CURRICULAR SUPPORT
NC-CTHPE 2016
98
National Conference on Changing Trends in Health Professions Education
Introduction
The concept of Noncognitive skills was introduced by sociologists Bowelâ&#x20AC;&#x2122;s and Critis (1976) to focus on scores other than those measured by cognitive tests and it mostly and it mostly reflects Stenbergâ&#x20AC;&#x2122;s contextual and experiential intelligence. Scores on Noncognitive variables have shown validity for a wide range of students in many fields (Bandales and Sedlacek 1989), It is also believed that Noncognitive rather than cognitive factor are more important elements. It is also believed that Non cognitive rather than cognitive factor are more important elements of success at both academics and work(Bowles& Grintis,2002). Noncognitve attributes and skills may play an important role in reversing or limiting delays or deficiencies in cognitive development and academic achievement, and they may complement direct efforts to improve academic learning. As little work has been done under Indian scenario regarding Noncognitive variables our study was focussed on establishing the relationship between Noncognitive scores and academic performance among students requiring additional curricular support.AIM: To study the relationship between Noncognitive scores and Academic performance among students requiring additional curricular support . Methodology Validated questionnaire was applied for assessing 12 the Noncognitive variables was administered to the students at the end of 6 months. Students who scored less than 40 marks in three consecutive formative assessments were included in the study as SNACs Group. Correlation analysis and logistic regression were performed to establish any relationship between Noncognitive variables and academic scores. Results Non cognitive variables like realistic self appraisal, Positive self concept, strong support system, Emotional intelligence, Expected involvement with faculty and academic support and study methods and involvement showed statistically significant correlation with academic scores among students requiring additional curricular support.
16.
FREE PAPER SESSION
Authors: SathishbabuM,Niranjan G, Ramesh R.Institution and address: Department of Biochemistry, Mahatma Gandhi Medical College and Research Institute, Sri BalajiVidyapeeth, Pillayarkuppam,Puducherry - 607 403, India. Corresponding Authors email: dr.msathishthemetropolis@gmail.com Abstract Title :SUPPLEMENTINGOPEN BOOK EXERCISES DURING AND AFTER LECTURE CAN BE AN ALTERNATE TEACHING LEARNING STYLE ON UNDERGRADUATE MEDICAL STUDENT
NC-CTHPE 2016
99
National Conference on Changing Trends in Health Professions Education
Background
Didactic lectures were often teacher centered. So far much work had been done to involve students during the lecture or after lecture for effective teaching and learning (TL).So, our aim was to study the efficacy of open book teaching and learning by group discussion among undergraduate medical students. Methodology Study topic was on ‘’Basics of Nutrition’’. Out of250students,187were enrolledin the study during the year 2014-15. Pre-lecture test was conducted to check prior knowledge by MCQsfollowedby open book teaching, post lecture test and open book exam with small group discussion. Task templates for small group discussion and questions were peer validated and instructions about the session plan were given one week prior the lecture. Statistical test
Data were expressed as mean ± SD. Gain score was calculated by the formulae: Post exercise test – Pre lecture test. For group comparison ANOVA test was performed. A Likert five scale score was used for pre-validated questionnaire for student’s feedback. A ‘p’ value of <0.05 was considered significant. Microsoft Excel 2010 and Graph pad software were used for analysis of data. Results The average marks had increased from basal test 2.8+ 4.2 to Post lecture test 10.8 + 5.7 and post exercise test 15.9 + 1.4. It wascomparatively more effective among group of slow achievers. Open book teaching and learning using standard text book significantly improved and helped in better understanding of subject. Difficulty index had decreased after the open book teaching andexercise. Student’s perceptions on this teaching module were positive. Conclusion Allowing student to bring text book during lecture and involve them to read and write as group exercise can be effective mode of teaching and learning method among different group of First year undergraduate medical student in this topic of Biochemistry.
17.
FREE PAPER SESSION
Author_Name: Designation : Institute: Email : Mobile :
Dr Shilpashree Y D Assistant professor Adichunchanagiri Institute of Medical Sciences dr.shilpashree.yd@gmail.com 07259138112
SecondAuthor: Designation : Institute :
Dr Aliya Nusrath Professor & Head Adichunchanagiri Institute of Medical Sciences
NC-CTHPE 2016
100
National Conference on Changing Trends in Health Professions Education
ThirdAuthor: Designation : Institute :
Dr Prathibha K Assistant Professor Adichunchanagiri Institute of Medical Sciences
Abstract Title: EFFECTIVENESS OF A MICROTEACHING WORKSHOP DESIGNED TO IMPROVE THE TEACHING PERFORMANCE OF POSTGRADUATE MEDICAL STUDENTS Objectives Microteaching helps in professional development in prospective professional teachers. The objectives of the present study were to know whether such a microteaching training / workshop programme conducted at our setting helped the participants to improve their teaching skills and also to know what are changes that can be implemented to make such workshop more effective and useful. Methodology In all 54 postgraduate students participated in the workshop. It was a three-day workshop programme conducted by medical education unit. At the end of the 3rd day feedback form was given to participants to know their perception on the effectiveness of the workshop. Results: 100% of the participants felt the workshop was useful. They also felt that feedback given during the session was most useful to improve their teaching skills. Conclusion Present study shows that postgraduates perceived the workshop to be beneficial to improve their teaching skills and to build their self-confidence. Conducting such workshops at regular interval will definitely benefit them to improve their teaching process.
18.
FREE PAPER SESSION
Authors: Stalin P1and Thomas Alexander2 1Associate
Professor, Department of Community Medicine
2Associate
Professor, Dept. of Gastroenterology and Dean, Medical Education
Unit,
Pondicherry Institute of Medical Sciences, Puducherry, India – 605014 Abstract Title:"MEDICAL STUDENTS’ PERCEPTIONS ABOUT COMMISSIONS – A MIXED METHODS RESEARCH"
NC-CTHPE 2016
101
National Conference on Changing Trends in Health Professions Education
Background
Among Indian medical practitioners, the unethical practices of accepting commissions for investigations, seems to be increasing exponentially. No studies were found that assessed the reasons for this specific form of unethical practice related to accepting commissions. Therefore, it would be useful to identify factors that promote or impede this practice of accepting commissions. Methods A mixed method study was conducted among a group of 140 first year medical students. A before-after study design was used to assess the change in perception of students about the practice of accepting commissions after the session on Medical Council of India (MCI) code. Analysis was done for only 132 students who responded both before and after the session. Focus Group Discussions (FGD) were conducted to identify the factors that influenced their perception and decision using a FGD guide which consisted of domains such as reasons for their initial decision, reasons for the change in their decision and others. Qualitative data was analyzed using thematic approach. Institutional Ethics Committee clearance was obtained. Results The number of students who refused to take commissions in the beginning (n=46) had doubled after the session (n=96). Monetary supremacy, high living costs and vying with others were identified as some of the reasons for accepting commissions. Reasons for refusing commissions were conscience and parental education. Fear of punishment was the main reason for their change in decision from acceptance to refuse commissions. Conclusion The key internal factor that promoted ethical behavior was conscience while the supremacy awarded to money was the main reason for the opposite. Key words: Medical Ethics, Conflict of Interests, Physician Self-Referral
19.
FREE PAPER SESSION
Author_Name: Designation : Institute : Email : Mobile :
Dr.Varsha Murthy Professor Indira Gandhi Institute of Dental Sciences, MGMCRI,Pondicherry drvarshamurthy@gmail.com 7708364959
Abstract Title: PERCEPTION OF DENTAL STUDENTS REGARDING THEIR BEHAVIORAL SKILL, COMMUNICATION SKILL AND INTERPERSONAL RELATIONSHIP COMPETENCE - A CROSS SECTIONAL STUDY
NC-CTHPE 2016
102
National Conference on Changing Trends in Health Professions Education
Introduction
The aim of this cross-sectional study was to assess the perception regarding the competence of communication and behavioral skill achieved during the undergraduate course, among alumni dental students of Indira Gandhi Institute of Dental Sciences, SBV, Pondicherry , India. Methods The alumni students were approached through alumni association of the dental college (‘’The Guild’’) and personally and were requested to participate in the study. They were sent a questionnaire through online link and their perception was assessed with the 35-item self administered questionnaire in English language. Results Majority (more than 75%) of the students, opinion was that these skills are important and should be taught .Around half of them felt, that they were competent to some extent in dealing with patients in their practice. However, more than 75% of them felt that they were lacking in various components of communication and interpersonal skills such as dealing with difficult and dissatisfied patients and breaking bad news. Conclusion The findings from this study suggested a possible need to attention in developing need based Communication Skill and Interpersonal Relationship training in individual specialties of dentistry.
20.
FREE PAPER SESSION
Author: Dr. Prakash SS, MD DNB, Dr. Anand R, MD DNB, Department of Biochemistry, Christian Medical College, Vellore, Abstract Title: NEED FOR CURRICULAR PROFESSIONS EDUCATION – A PROPOSAL
INNOVATIONS
IN
HEALTH
Background The model of medical education comprises of undergraduate degree followed by postgraduate degree and subsequently further sub-specializations if desired. The current regulation sees the undergraduate medical education as an end in itself whose products can deliver health care to the community. However, most medical graduates prefer to specialize in a particular field after graduation. Even patients demand such specialist care.
NC-CTHPE 2016
103
National Conference on Changing Trends in Health Professions Education
What we tried?
We devised a model of medical education based on our perceptions and experiences in the field of medical education as students and teachers. We came up with this model which could befit the requirements of medical graduates of this generation as well as the patients. In the proposed curricular model, both undergraduate and postgraduate medical education is delivered as a continuum. In this model, the end point of medical education will be graduates passing out as a specialist in a broad medical specialty. The choice of specialty can be made either at joining or midway during the course. What were the lessons learned? We rationalized as to why this model would be of use to all stakeholders. We also realised the challenges in implementing this model of education. It is our hope that this model would help mitigate the need for specialists in different areas of medical education. We learned that more than the ratio of doctor: population being less, it is the specialists in various fields who are inadequate. We hope that this would relieve the students from the constraints of long duration of medical education and the stress involved in clearing the postgraduate medical entrance examinations. It would also help refine the training requirements at every stage of education from first year till passing out as a specialist. It might help reduce redundancy in the medical education since the students would learn only those things which are directly involved in their practice. Conclusion Instead of increasing the number of medical colleges and seats in undergraduate medical education, it is important to address the disproportionate numbers of specialists in various fields which is a major concern in health care delivery. The curricular model proposed by us gives a framework to work upon, which would help bridge the existing gap in the numbers of specialists in various fields. Since the ultimate goal of medical education is to improve the health status of the community, the model proposed here might be one of the strategies which could help achieve that. 21.
FREE PAPER SESSION
Author_Name: Designation : Institute: Email : Mobile:
Dr.P.Vaithiyanathan Assistant Professor Mahatma Gandhi Medical College & Research Institute vaithibh@gmail.com 9994476834
Second Author: Designation : Institute:
Dr. N. Seetharaman Professor & Head Mahatma Gandhi Medical College & Research Institute
Third Author: Designation : Institute :
Dr. K. A. Narayan Professor Mahatma Gandhi Medical College & Research Institue
NC-CTHPE 2016
104
National Conference on Changing Trends in Health Professions Education
Abstract Title: TECHNIQUES”
“THE HEART MODULE - HEALTH ASSESSMENT BY RAPID
Background: Research in the Medical field has been growing exponentially over the past decades and has contributed significantly in the betterment of human health. However, because of the increasingly complex nature of the matters being researched, there has been a rather unwanted outcome - the realm of the practising Doctor is becoming increasingly detached from the realms of Scientific Research. Current systems of Medical Education world-over are predominantly hospital oriented and our medical graduates are educated based only on a very narrow, disease-centric approach to health. What we really need are teaching/learning approaches that equip medical graduates with a scientific temper, teach them to empathize with the people’s needs and comprehend the multi-dimensional nature of health, ultimately providing healthcare with a humanistic touch. Considering these, the HeART Module (Health Assessment by Rapid Techniques) was designed as an innovative community-based experiential learning opportunity for first year undergraduate medical students of MGMC&RI. It envisions two broad goals: 1) To expose students to the Biopsychosocial dimensions of health and disease – beyond the usual diseasecentric hospital-based learning. 2) To demystify ‘research’ by orienting students to the basics of Health Research Methodology. Methodology: This 2 week programme was organised for the first year MBBS students (2015 batch; 250 students) in August, 2015. The programme was divided into three components- An initial training on research methods, followed by field data collection and finally, data analysis & presentation. During the first phase, the students were given training on basic qualitative research methodology and were oriented to different tools of rapid appraisal such as transect walk, social and resource mapping, seasonal and 24 hour calendars, etc. After the initial training, the students were split into 6 groups namely green, red, blue, pink, yellow & brown and were allotted specific tasks / tools for each group. The group worked out the methods for collecting information pertaining to the particular task / tool. In the second phase, the students were taken to the village named Bahour in Pondicherry for the field experience. The students used ‘transect walk’ to identify the resources, features and facilities in the community and ‘social mapping’ to mark the health facilities available in the village. ‘Key informant interviews’ were done to elicit historical events, local festivals, customs & beliefs in the community. The ‘24 hour calendar’ was used by the students to identify the usual activities of housewives, working men & women, adolescent girls, geriatric group and so on in a typical day. The ‘seasonal calendar’ method was used to know the disease patterns & agricultural activities. In the Third phase the students compiled and analysed the data. Students prepared charts, posters and banners, in addition to oral and PowerPoint presentations detailing their findings and presented to all the faculty of the University. At the end of the programme feedback was obtained from all the stakeholders.
Results: At the students developed the following competencies Obtain health related data about social and cultural environments, growth and development factors, needs and interests
NC-CTHPE 2016
105
National Conference on Changing Trends in Health Professions Education
Analyse social, cultural, economic and political factors that influence health. Apply principles of community organization in planning programs. Communicating health and health education needs, concerns and resources. Demonstrate both proficiency and accuracy in oral and written presentations. Apply appropriate research principles and methods in community diagnosis. Assess the merits and limitations of qualitative and quantitative research methods Lessons learned
Managing 250 young and enthusiastic students in the field at one time and ensuring uniform level of involvement from all students in various group activities were extremely challenging. Conclusion The current module was a unique community based experiential learning for the students and unique learning experience for the organising team. Based on the feedback from all the stakeholders the programme will be up scaled and fine-tuned and will be implemented for the upcoming undergraduate students in future. 22.
FREE PAPER SESSION
Author_Name: Designation : Institute: Email : Mobile:
Dr Shubhangi Baviskar Assistant Director Central Leprosy Teaching & Research Institute Chengalpattu TN shubhangi.baviskar@gmail.com 9445458979
SecondAuthor Designation : Institute :
:Dr. Vijay Bhagat Assistant Director Central Leprosy Teaching & Research Institute Chengalpattu TN
ThirdAuthor: Designation : Institute :
Dr. M.K.Showkath Ali Director Central Leprosy Teaching & Research Institute Chengalpattu TN
Abstract_Title: EFFECT OF ROLE PLAY FOR QUALITATIVE IMPROVEMENT IN COUNSELING OF LEPROSY PATIENTS Introduction Persons with leprosy are often victimized to various participation restrictions at home, in the communities and at workplace which leads to emotional breakdown, social ostracism, defaulting from treatment and economic loss as well. Role play is widely used as an educational tool for learning about communication in health professional education. Role play is used as a training tool to acquire knowledge, attitudes and skills in a range of disciplines, with learners of different ages, cross cultural values and with applications in varied human resources.
NC-CTHPE 2016
106
National Conference on Changing Trends in Health Professions Education
Objectives:
To enhance quality of counseling of persons affected with leprosy by health staff. Methodology: Role play was incorporated as a teaching method for health care staff to deal with counseling issues of persons affected with leprosy. Step wise approach followed for training of health personnel for counseling of leprosy patients. The contents, methodology in detail, dealing with specific issues etc were incorporated in the training material. Pre-post test assessment on qualitative contents was carried out with structured proforma. Feedback was collected for further improvement. Results Overall 80 % improvement was noted in the quality of counseling among the health workers. The role play was appreciated and advised to incorporate in training programmes at all levels for counseling of persons with leprosy. Inadequate time for counseling was identified as constraint, but due to less number of patients per health worker the constraint was resolved. Conclusion: Role play was noted to be effective in improving quality of counseling.
NC-CTHPE 2016
107