50 Years of IAOMS
The Development of the Specialty
Written by Paul J.W. Stoelinga & John Ll. WilliamsInternational Association of Oral and Maxillofacial Surgeons
Library of Congress Cataloging-in-Publication Data
Authors: Stoelinga, Paul J.W. and Williams, John Ll.
50 Years of IAOMS — The Development of the Specialty ISBN 978-0-615-59136-0 (hardcover)
© 2012 International Association of Oral and Maxillofacial Surgeons 17 W. 220 22nd Street, Suite 420 Oakbrook Terrace, Illinois 60181 United States of America www.iaoms.org
All rights reserved. This book or any part thereof may not be reproduced, stored in a retrieval system, or transmitted in any form by any means, electronic, mechanical, photocopying, or otherwise, without prior written permission of the publisher.
Interior designed by Arc Group Ltd, Chicago
Printed in Canada by Friesens Corporation
Introduction
The authors were asked by the Executive Committee of the IAOMS to compose a book to commemorate the organization’s 50th anniversary. We were given a free hand to insert any information that we found relevant to the history of the IAOMS.
It soon became very clear that the emergence of the specialty was intimately related to the development of national, regional and international organizations of the profession. This is the reason why room has been made for a relatively large chapter on the development of the specialty that precedes the chapters on the history of IAOMS. It was clearly necessary in the context of the emergence of the International Association.
It was also obvious that the establishment of the international organization was preceded, in most instances by national organizations, although in some instances the International Association became the catalyst for establishing a national association. The role these national associations play and their particular history is well represented by the individual national accounts and was thought to be of interest for the international reader. The same is more or less true for the regional associations that are invaluable since they are the bodies that have significant impact on the daily practice of individual surgeons.
Both authors have witnessed the emergence and development of national and regional associations, as well as the International Association but, above all, the tremendous development of the specialty since the early 1960s. They have also been active clinicians, involved in education and training. That made them well equipped to reflect on it and to describe this development within the political environment in which both of them were active.

We seek forgiveness for any sins of omission but in a book of limited size, harsh decisions had to be made. We are very grateful to the various contributors who have made this venture possible, as well as to Kerry Spaedy and Susan Nowicki for their assistance in the production of this book.
J.W. Stoelinga The book’s authors at work. Left to right: John Williams and Paul Stoelinga. Paul John Ll. WilliamsTable of Contents
Introduction 3
Paul J.W. Stoelinga and John Ll. Williams
Foreword 6 Larry W. Nissen, President, 2010–2011 and Kishore P. Nayak, President 2012–2013
Chapter 1 The Development of the Specialty 9
Introduction
The emergence of the journals The subspecialties
Dentoalveolar surgery Infectious diseases Trauma Clinical pathology
Oncology
Preprosthetic surgery Surgery of the temporomandibular joint Orthognathic surgery Cleft lip and palate and craniofacial surgery Epilogue References
Chapter 2 The International Association of Oral Surgeons (1962–1986) 61
The beginning (1962–1971) 1962: The 1st ICOS, London 1965: The 2nd ICOS, Copenhagen News Sheet begins 1968: The 3rd ICOS, New York 1971: The 4th ICOS, Amsterdam Consolidation and expansion (1971–1986)
1974: The 5th ICOS, Madrid 1977: The 6th ICOS, Sydney 1980: The 7th ICOS, Dublin 1983: The 8th ICOS, West Berlin 1986: The 9th ICOMS, Vancouver References
Chapter 3 The International Association of Oral and Maxillofacial Surgeons (1986–1999) 75
A wind of change
The Tenerife and Bermuda conferences (1987–1988)
The governance of IAOMS 1989: The 10th ICOMS, Jerusalem 1992: The 11th ICOMS, Buenos Aires 1995: The 12th ICOMS, Budapest
1997: The 13th ICOMS, Kyoto 1999: The 14th ICOMS, Washington, D.C. Budget and membership fee Epilogue References
Chapter 4
The International Association of Oral and Maxillofacial Surgeons (1999–2012) 87
Modern times
The headquarters
A new era of governance 2001: The 15th ICOMS, Durban
First IAOMS-sponsored educational course 2003: The 16th ICOMS, Athens 2005: The 17th ICOMS, Vienna
Futures Summit I 2007: The 18th ICOMS, Bangalore 2009: The 19th ICOMS, Shanghai 2011: The 20th ICOMS, Santiago Epilogue References
Chapter 5 The Foundation 105
Financial challenges
Structural changes Educational projects
African service Scholarships established
Strengthening the Journal Change in publisher
Albania Argentina Austria Azerbaijan, Republic of Bangladesh Belarus Belgium Bolivia Brazil Bulgaria Canada Chile Columbia Costa Rica Croatia Cuba Czech Republic Denmark Dominican Republic East Africa
Ecuador Egypt Estonia Finland France Georgia, Republic of Germany Ghana Greece Hong Kong Hungary India Indonesia Iran Ireland Israel Italy Japan Kazakhstan, Republic of Korea
Content expansion Epilogue
Latvia Lithuania Malaysia Mexico Moldova, Republic of Mongolia The Netherlands Nigeria Norway Pakistan Panama Paraguay
People’s Republic of China Peru The Philippines Poland Portugal Romania Serbia
Africa Asia Europe Latin America North America Oceania
The Affiliated National Oral and Maxillofacial Surgeon Associations
Timeline for National OMS Association Affiliations with IAOMS
IAOMS Presidents
Honorary and Distinguished Fellows of the IAOMS
IAOMS Award Recipients
International Conferences and Executive Committee Members Report on Workshop on Training of the Oral Surgeon Throughout the World (1974) Report of Education Committee (1980)
International Guidelines for Specialty Training and Education in Oral and Maxillofacial Surgery (Durban, 2001)
Seychelles Singapore Slovakia Slovenia South Africa Spain Sri Lanka Sweden Switzerland Taipei — China Thailand Turkey Ukraine United Kingdom United States of America Uruguay Venezuela Epilogue
This chronicle of the 50 year history of the International Association of Oral and Maxillofacial Surgeons is dedicated to the founding fathers who recognized the need for an association of oral and maxillofacial surgeons and specialty organizations around the world, as well as those next leaders who continued to carry the torch, lighting the way for the specialty to flourish. These pioneers always understood the need to work together and that collectively, goals could be more easily achieved on a global basis.
It took the foresight of Fred Henny, of the American Association and Sir Terence Ward, of the British Association, who in 1962, while together at a meeting in London, began the construction on the foundation of a truly international organization. This international organization would prosper for years, but also see many challenges, some of which would threaten its very existence. The first such challenge was a lack of mutual understanding centering on the debate over whether medical qualification as well as dental qualification was required prior to surgical training. Unfortunately, it took most of the first 40 years sparring on this issue within the Association before a resolution was reached.
In 2001, it was finally decided through acceptance of the International Guidelines for Training and Education in Oral and Maxillofacial Surgery that regional differences in training existed and were acceptable. This document stated that the actual surgical training in the oral and maxillofacial region was what qualified one to become an oral and maxillofacial surgeon, regardless of whether one had dental and/or medical qualification. Despite these early differences, the International Journal of Oral and Maxillofacial Surgery was established and quickly became the well-respected flagship publication of the Association. The IAOMS Foundation was chartered to fund much needed educational programs and projects to enhance the specialty.
The history of the first 40 years provides a backdrop that underscores how maturation of an international organization made of diverse members sharing a common cause can be slow to develop but once achieved, great progress can result and move forward to great effect.
The past ten years have shown the Association has flourished in many areas. Numerous courses on the basics of the specialty have been provided in developing areas of the world that otherwise lack formalized training programs. This has expanded the knowledge base by bringing education to those who need it most.
Surgical interest groups (SIGs) were established and fellowship training programs developed to further expand the surgical expertise of the specialty. The Association’s membership has seen a dramatic increase, now approaching 5,500 and much of that is a result of the IAOMS website and the Association’s ever-expanding presence in social media. Information must be readily accessible, precise and timely; and the Association is focused on providing such information.
The International Conference on Oral and Maxillofacial Surgery (ICOMS) is held every two years and the recently concluded 20th edition of the event was held in Santiago, Chile, and proved to be one the most successful attracting more than 2,100 participants. The ICOMS is undoubtedly the flagship event of the IAOMS and is growing from strength to strength with member countries vying and competing with each other to host the event with great emphasis on scientific and social content. The next three meetings of the ICOMS are scheduled to be held in Barcelona, Spain; Melbourne, Australia and Seoul, Korea, respectively.
Future endeavors of the IAOMS are likely to include development of an international accreditation process and a board certification process for programs and practitioners who may not otherwise have access to these opportunities. An internationally organized humanitarian aid and disaster relief effort is also being investigated. These and other programs of the Association are dependent upon the many volunteers who for 50 years have dedicated themselves to the mission of creating a better specialty worldwide. Many of them are mentioned in this work but unfortunately, in a brief document such as this, some dedicated individuals will go unnamed. Our thanks go to everyone who has participated in the activities of the IAOMS since 1962.
This publication would not have been possible without the timeless dedication of Paul Stoelinga and John Williams. Their endless hours of research, securing of photographs, reminding regional reporters of deadlines and mind-numbing editorial review are tasks that few of us can appreciate. Without their diligence and adherence to strict timetables, this work might never have been finished. The IAOMS owes them a huge debt of gratitude for their efforts.
The next 50 years will surely see great achievements by the IAOMS. We know future generations will rise to the challenge and continue to strive for excellence in the specialty of oral and maxillofacial surgery and this Association.
2010–2011 President, 2012–2013
Larry W. Nissen K ishore P. Nayak President,Chapter 1
The Development of the Specialty
Introduction
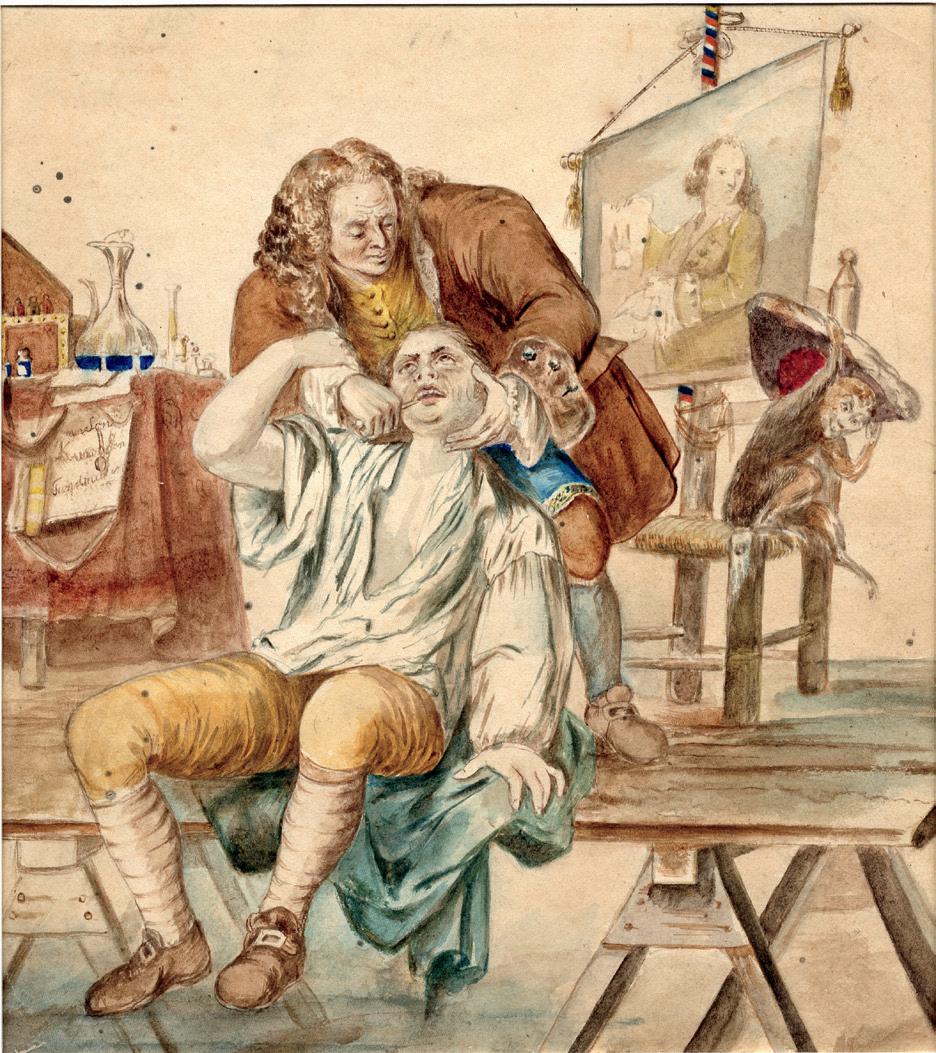
There is ample evidence that the Egyptians and later the Greeks dealt with fractures of the mandible and even dislocation of the jaw. Hippocrates (400 BC), in particular, is credited with describing a bandage to support the chin which would stabilize the mandible in cases of fracture. Several illustrations are proof of the fact that in many ancient civilizations in both Asia as well as Europe, teeth were “pulled.” Throughout the 16th to 18th century, artists in Europe made paintings of traveling barber-surgeons, or charlatans, pulling teeth in the open air (Ring, 1985). It is, however, safe to assume that these treatments were not widely available for the general public.
It is really hard to point towards the true beginning of the development of the specialty, because there are anecdotal reports of oral surgery in most countries of the world that go back to medieval times or even earlier. A detailed description of the development of the specialty in ancient times is presented by Hoffman-Axthelm (1995). With the Renaissance, however, a new era of medicine began which started with some important discoveries in anatomy, which, in large part, were carried out in Italy. Preceding the true development of our specialty, however, which really began in the second half of the 19th century, three surgeons paved the way for its emergence.
Artwork depicting a tooth puller. This painting was made during the 19th century in the Netherlands using a mirror picture from a copper etching made by F. Maggiotto. On loan from the Utrect University Museum, Medical-Dental collection, but in possession of the Dutch Dental Association. Reproduced with permission.
The Frenchman Ambroise Paré (1515–1590) is generally considered to be the father of modern surgery and the first to have published about oral surgery in a book called “A Treatise on Surgery.” As a military surgeon he became famous for the way he treated gunshot wounds. Contrary to the then current method of using hot oil, he dressed the wounds with “an unguent of egg whites, oil of roses and turpentine.” This practice was widely copied after his publication, probably much to the relief of the wounded soldiers. He also described the treatment of mandibular fractures for which he recommended manual reposition and wiring to the neighboring teeth, supported by a bandage around the chin, similar to the description by Hippocrates. His book also presents illustrations of instruments to elevate teeth from their sockets.

Another French surgeon, Pierre Fauchard (1678–1761), is considered to be the father of dentistry. He published the first comprehensive book on dentistry in 1728, “Le chirurgien dentiste, ou, traité des dentes” (The Surgeon-Dentist or Treatise on the Teeth). This book became the authoritative text for a century to come and was translated into German, which meant that it spread over most of the European continent. He settled in Paris and devoted his entire career to dentistry. He covered the whole field of dentistry, including oral surgery, for instance, extractions, re-implantation of avulsed teeth and homologous tooth transplantations.

The third person who was instrumental to dentistry and oral surgery alike was a Scotsman, John Hunter (1728–1793). Trained as a surgeon, he is seen as the founder of a scientific approach to the subject. He became interested in dentistry early in his career and wrote the classic, “Natural History of the Human Teeth” in 1771, in which he explained their structure, use, formation, growth and diseases. He introduced the nomenclature of teeth still used today and made observations about caries, periodontal disease

and inflammation around affected teeth. This book became a main reference for many practitioners in Europe as it was translated into German, Dutch, Italian and Latin.
Seminal discoveries
Advances in surgery have generally been by a process of gradual evolution but by the end of the 18th and throughout the 19th centuries, several seminal discoveries were made which had a profound influence on medicine as a whole. Louis Pasteur (1822–1895) recognized the role of bacteria as the cause of infection and Joseph Lister (1827–1912) developed the concept of antisepsis and applied these techniques to surgery through his carbolic spray.
The development of general anesthetic agents started with Horace Wells, who, in 1845, first carried out a painless dental extraction under nitrous oxide anesthesia at Massachusetts General Hospital. This work was followed by T.G. Morton (1846), using ether and, in Edinburgh, James Young Simpson, using chloroform, all of which changed treatments dramatically.


Carl Thiersch (1874) adapted the technique described by Louis Léopold Ollier (1872) and using the principles of Lister, introduced the split skin graft for reconstruction, which revolutionized this aspect of surgery. Additionally, Wilhelm Conrad Röntgen (1895), a physicist, demonstrated the use of x-rays in the diagnosis and management of fracture care.
New interest in mouth surgery brings breakthrough
As previously mentioned, the real breakthrough came in the second half of the 19th century when general surgeons with a special interest in surgery of the mouth and related structures began to practice oral and facial surgery. This happened particularly in the U.S.A. and in the Germanspeaking areas of Europe but also in many other countries, as appears from the various reports of the affiliated national associations (see chapter 7)
This development came relatively late considering the development of surgery in general. This may be explained by the lack of knowledge about dentistry, which is of great importance when working in the orofacial area. It is, therefore, not surprising that the first pioneers are
to be found in the U.S.A. where dentistry had become an academic profession with the establishment in 1867 of Harvard Dental School, which was soon followed by several state universities. Before that time, however, there were already dental colleges where dentistry was taught, with Baltimore College of Dental Surgery, established in 1840, being the first.
James E. Garretson (1825–1895) is rightly considered by the American Association of Oral of Maxillofacial Surgeons (AAOMS) as the father of oral surgery. Garretson, a general surgeon with a formal dental degree, published in 1873 a book entitled: “A System of Oral Surgery: A Consideration of the Diseases and Surgery of the Mouth, Jaws and Associated Parts.” Almost 140 years later, one can only admire the vision this man must have had about the specialty considering the title of his book. He truly can be considered the father of oral and maxillofacial surgery worldwide, although colleagues in other parts of the globe had no knowledge of his work.


Probably the first surgeon who exclusively limited his practice to OMF surgery was Simon Hullihen (1810–1857). He also was a general surgeon who later received an honorary dental degree from Baltimore College of Dental Surgery. Despite his lack of formal dental training, he performed a wide spectrum of surgical procedures in the oral and maxillofacial area and is particularly known for the first mandibular, subapical, segmental set-back osteotomy, which was carried out in 1849.

There were several American colleagues at this time who held medical and dental degrees and who were specialized in oral surgery but a man who really stood out is Truman W. Brophy (1848–1929). In 1883, he established the Chicago Dental College and became a professor in oral surgery at that institution. He gained a tremendous reputation, particularly for his skills in cleft surgery. His major contribution to the specialty, however, was his 1916 book, “Oral Surgery: A
Treatise on Diseases, Injuries and Malformations of the Mouth and Associated Parts.”
It is also striking to note that in those days, Brophy, just like Garretson before him, had a wider vision of the specialty than just the mouth. One can only be deeply impressed by the quality of this two-volume book, which not only covered oral surgery in its widest sense, it also covered the treatment of fractures, tumors and congenital deformities. It is the color anatomy figures, in particular, of the mouth and related structures in color that impresses the reader today.
He was also instrumental in establishing the first U.S.A. association of oral surgery in 1921. Originally, the membership consisted of surgeons with both medical and dental degrees but two years later, membership was opened up to include those with a single degree, either medical or dental. Some well-known names that are either linked to surgical procedures or instruments, such as Cryer, Ivy, Risdon, Waldron and Lyons, joined this association. It is of interest to note that this association became the American Association of Plastic Surgery in 1941, after it had changed its name in 1933 to Oral and Plastic Surgery (Randall et al., 1996). From 1931 on, the membership of this association was only open to colleagues with a medical degree. Disciples of Brophy continued to advance the specialty and wrote another excellent comprehensive book, “Essentials of Oral Surgery” (Blair, Ivy & Brown), which first appeared in 1923, with updated reprints in 1936 and 1944.
Specialty grows in Germany
The early history of the specialty in Europe is largely defined by the activities of surgeons in the German-speaking countries, although there were also pioneers in other countries, such as France, England and elsewhere (see chapter 7). Similar to the specialty’s American beginnings, but somewhat later, it was general surgeons who began to develop an interest in the surgery of the mouth and face.
What were probably the first books in the German language, which dealt with what is now called oral and maxillofacial surgery, stemmed from general surgeons and were published in 1907 by Perthes and in 1913 by Bruns, Garré and Küttner. The German involvement in the 1870–1871 Franco-Prussian War and World War I apparently initiated some original thinking on how to treat soldiers with facial wounds and fractures. The use of arch bars, fixed to bands around the molar teeth, provided anchorage for intermaxillary fixation. This was often supported by a bandage around the chin. The use of splints, made of vulcanite, both for dentate as well as edentulous patients, was already known to surgeons of this period.
It is particularly interesting to read what these surgeons did for those poor young men who were missing parts of their mandible due to gunshot wounds. Extraoral pin fixation and devices that gradually repositioned the stumps in the desired position were fabricated, using very ingenious techniques. It is also fascinating to read about the first attempts to graft defects of the jaws with autogenous bone from various donor sites, including the mandible, tibia and even metatarsal bones, in times when no antimicrobial treatment existed. These first attempts date back to the very beginning of the 20th century in the German-speaking area and were used especially to treat large defects as a result of war injuries during and after World War I (Bruhn et al. 1915, Misch & Rumpel, 1916, Klapp & Schröder, 1917).
Very much the same discussions took place in Germany as those held in the U.S.A. regarding the need for oral surgeons to possess a dental education. Texts on oral and maxillofacial surgery from this period were written by general surgeons with an interest in the field (Sontag & Rosenthal, 1930). It was Martin Wassmund (1892–1956), however, who was one of the strongest supporters of the double degree. As a dentist with a keen interest in oral surgery and very much an autodidactic, Wassmund later studied medicine and became the leading surgeon at Rudolf-Virchow Hospital in Berlin. It is only fair to say that he probably wrote the first comprehensive book on oral and maxillofacial surgery (1935, 1939) which contained surgical procedures that are still widely practiced today. His name, of course, is also linked to the subapical anterior maxillary set-back osteotomy.
Georg Axhausen (1877–1960) also deserves special recognition. He was a general surgeon, departmental chair and professor at the University of Berlin in oral and maxillofacial surgery (Zahn-, Mund- und Kieferheilkunde), whose 1940 book presents some very impressive and still valid thoughts on free autogenous bone grafts and soft tissue transplantations. It also includes the description of a vestibuloplasty in the symphyseal area of the mandible, using a free skin graft.


If we regard the Huntarian period of English surgery, the years preceding this, comprising the 17th and 18th centuries, were marked by repeated wars in Europe. Military
surgeons wrote individual vivid accounts of severe facial injuries, particularly those resulting from gunshot injuries. Treatment consisted of suturing skin to mucosa and later, making good the anatomical defects with prosthetic shields made from silver.
These meticulous descriptions are exemplified by those of Richard Wiseman, who, in the 17th century, was probably the most advanced thinker of the age. A naval surgeon, he wrote up some 600 cases which accurately described the signs and symptoms of bone fractures and the nature of jaw fractures from gunshot wounds and assaults. His writeups included shrewd observations of a middle third fracture in a child, including the posterior displacement. He went on to describe the digital reduction of this displacement and the problems associated with retaining it in a forward position. He was also the first person to emphasize the need for early removal of facial sutures to reduce the scar from the continuous suture itself.

During this period, any surgery was carried out by general surgeons, but in the late 18th and early 19th centuries, there was an increased influence from dental surgery. These were individual contributions which each added significantly to the practice of the specialty although no single one was responsible for any major breakthrough. The consequence of this greater awareness of the dentition meant that the treatment of fractures of the jaws advanced side by side with improvements in prosthetic techniques and later, in orthodontic techniques, so that at last, someone attempted to effect a cure other than by simple ligation of adjacent teeth and the provision of a submental bandage.
The first dental splint was probably made in 1780. Over the next 100 years it underwent significant modification to improve its ability to stabilize the jaw fragments. For instance, Naysmith, a dentist, working with Robert Liston, describes the use of a metal cap splint to prevent displacement of the jaw following resection for a tumor. With the exception of this case, the majority of reports were of extensive gunshot wounds and the subsequent replacement of missing parts by ingenious devices constructed of silver.
Lessons then poured in from the American Civil War, which resulted in significant developments in the dental splint. The very nature of trench warfare and the increased power of munitions all tended to increase the severity of facial injuries in particular. The introduction of anti-gas gangrene serum, the copious irrigation of soft tissue wounds
with hypochlorite solution, and the introduction of the tube pedicle by Harold Gillies and at the same time, but independently, by Filatov in Russia, together with bone grafting, greatly facilitated the management of these injuries.
Against this background, the U.K recognized the need for special centers within which this type of reparative surgery could be carried out. The first such center was at Queen Mary’s, Sidcup, where Major Harold Gillies, Captain Kelsey Fry and Captain Fraser worked together, aided by many noteworthy surgeons of the time including Kilner (U.K.), Blair, Ivy, Kazanjian and Curtis (U.S.A.), Valadier (France) and Pickerell (New Zealand), among many others.
Between the wars, iliac crest bone became firmly established as the site of choice for the reconstruction of jaw defects. An improved form of eyelet wiring was described by Ivy (1920) and Gillies, Kilner and Stone (1927) described the temporal approach to the zygomatic arch.
The British government at that time established a special task force charged with ensuring that in the event of further hostilities, the injured service men and women would be assured of far better care than ever before. From the maxillofacial point of view, Harold Gillies (later, Sir Harold Gillies) was charged with the task. It established the concept of a team of surgeons, dedicated to the management of facial injuries, who would work together in frontline hospitals, evacuate the injured after primary stabilization to rear positions, often to the U.K., when it was the most practical thing to do. The surgeons involved in these teams would be general surgeons, some of whom were already trained in reconstruction, and would be known as plastic surgeons, together with ENT and dental surgeons. It must be remembered that, at that time, the treatment of jaw fractures was largely by the use of cast silver cap splints, for which dental expertise was essential.
The development in France was slightly different and can only be understood when realizing that dentistry was not considered an academic profession until quite recently. Instead, a medical specialty called “Stomatologie” existed. Stomatologists would carry out dentistry but some specialized in maxillofacial surgery. There were, however, other specialists, such as general and plastic surgeons and ear, nose and throat surgeons who could attain a “competence” in maxillofacial surgery.
A French surgeon who contributed a lot to our understanding of maxillary fracture patterns was

Rene Le Fort (1869–1951). His classic studies were carried out in 1901, when he was still a young doctor in the military (Pons et al., 1988). One of the most renowned surgeons of his time was Victor Veau (1869–1951), a general surgeon who published his seminal work on the treatment of cleft lip and palate in 1938. There were several other French pioneers who contributed to the development of the specialty in France. Guillaume Dupuytren (1777–1875), for instance, was probably the first surgeon who described the typical signs and symptoms of a jaw cyst including crepitation of the thin overlying bone shell. He also called these lesions cysts but had no idea about their origin.

An excellent account of the early French contributions is presented by Dechaume and Huard (1977). One cannot escape the impression, however, that much published in German or English never penetrated into the French literature but that is also probably true the other way around. There is a French book on oral surgery that reflects the state of the art in France in the 1930s (Chompret, Dechaume & Richard, 1935). It is limited to pure oral procedures and is less comprehensive than the German or American books of the same period.
One of the factors that defined this early period, apart from the daring character that all of these pioneers must have had, was the fact that they were almost certainly unaware of what was going on in other countries, let alone in the transatlantic world, the one exception being Truman Brophy, who quotes Perthes (1907) in his book. For this reason, some operations or techniques were invented several times in different countries without the inventors knowing of each other. The reason for this was the limited number of journals available and the inability of most professionals to read each other’s language. Most medical and dental journals were also rather parochial as they had limited distribution. The event which changed this completely was World War II. Not only did this war profoundly change the profession due to the new developments caused by the need to take care of large numbers of wounded soldiers but soon afterwards, the world opened and English became the main language for scientific publications.

The specialty has benefited enormously from general advances in medicine and surgery that were made during the war. Probably the most important one relates to the discovery of Penicillin by Fleming in 1941. This enabled surgeons to begin exposing jaw bones more safely and to carry out procedures, including open reductions of fractures and osteotomies, in a predictable manner. This was certainly not common practice before and, for instance, Brophy warns in his book that, “this procedure, which should be the last resort, etc.” He was referring here to open reduction of some mandibular fractures and to applying a wire osteosynthesis. Also, inflammatory diseases caused by the teeth were no longer as life threatening as before, while specific infections, such as actinomycosis, could be adequately tackled.
The emergence of the journals
Another factor that contributed to the rapid spread of knowledge worldwide was the establishment of journals solely devoted to oral surgery. The AAOS began their journal in 1943, which appeared quarterly in the early years. It was later published every two months and became a monthly journal only in 1965. Although this journal was meant especially for the American colleagues, there were many subscribers from overseas but few contributions from abroad. The other American journal that appeared first in 1958, also quarterly, was called Oral Surgery, Oral Medicine and Oral Pathology. This journal, from the beginning, had a somewhat broader vision in that it aimed to attract international contributions and even had international editors. This probably had to do with the fact that its first
H. tH o maIn the first issue of the “Triple O,” Thoma writes a remarkable and extensive editorial, introducing the new journal: “The material will include advances in clinical procedures as well as information about new developments in the basic sciences. The latter are fundamental, since they furnish the foundation needed for the thorough understanding of disease processes and the application of correct treatment, be it medicinal or surgical in nature. Let us not forget that the true art of medicine and surgery is based on a thorough concept of the basic medical sciences, which include anatomy, physiology, biochemistry, bacteriology, pathology and pharmodynamics and that the clinician depends on investigation and research for progress. Yet, truly, the clinic is the proving ground for discoveries made in laboratories.”
He then goes on to mention the names of various pioneers, such as Pasteur, Semmelweis, Lister, Morton and several others in medicine and surgery who applied basic ideas to the development of an important discovery. This introduction led to the following narrative. “Today, we definitely accept organized investigations as the most promising method for success in the revelation of new scientific facts. We no longer wait for a genius to appear, for a lucky discovery to come along. The great wonder of organized progress is made by an army of patient investigators, by groups working together with leadership from within. Discoveries in modern times are made by cooperation and by the cumulative effort and therefore, it is necessary for investigators to study the accumulated scientific knowledge which has increased in an amazing manner, as highly trained specialists added fact upon fact by the sweat of their brow.”
Thoma then describes the passing of knowledge in ancient times as it was based by word of mouth and often went lost, contrary to the present time. “It was the advent of the printing press which facilitated the distribution of knowledge and today man is to a great degree educated by published material. Periodicals are published constantly to keep the reader informed of the most recent accomplishments of his contemporaries,” he wrote. He then continues to promise the reader to provide the best original articles, including all aspects of the profession and “Quarterly Reviews of the Literature.” He had appointed corresponding editors in many countries to report on the development outside the U.S.A.; “because the world is small and there should be complete cooperation, especially in the medical and dental professions, for the benefit of all.”
The reader, almost 60 years later, could not agree more with these wise and highly relevant words. Apart from his phenomenal accomplishments and broad knowledge of the pathology and surgery of his time, this man had a vision that has proved to be right until today.
Paul J.W. Stoelinga
editor, Kurt H. Thoma, who was born in Switzerland, was brought up speaking both German and French. American OMF surgeons were hitherto sporadically publishing in either dental or surgical journals.
The German-speaking countries had their Fortschritte der Mund,-Kiefer,- und Gesichtschirurgie from 1954, which was not so much a real journal and was certainly not peer reviewed but rather was an accumulation of the papers presented at their annual meeting, edited by one of their leading professors. Nevertheless, it contained some very useful information and gave the reader a sense of where the specialty was heading.
The British established their journal in 1963, which only appeared twice a year and later, in 1980, three times a year. The IAOMS published its first journal in 1972, followed by the European association in 1976. Both journals started out by appearing six times a year.
It is of interest to note that French stomatologists had their journal from 1899, called La Revue de la Stomatologie. This journal, however, did not exclusively publish on oral and maxillofacial surgery but also on common dental issues. The same was true for the Acta Stomatologica Belgica, which first appeared in 1902.
In order to gain an impression of the scope and armamentarium of the OMF surgeon in those days, it is quite revealing to read the journals of these years. There were a lot of case reports and experienced based papers written by authors who were leaders in the specialty. This is well illustrated when comparing the 12 issues of the American Journal of 1963 and 1964 with the four issues of the British Journal from 1963–1965 (see table below)
The British Journal in those years appeared only twice a year, the American Journal six times a year. The contents
were quite comparable. Case reports, mainly pathology, made up about one third of the contents. Reviews and experience based articles filled about one third to one quarter, the remainder were technical notes and papers about anesthesia, the latter were only present in the American journal for obvious reasons. Of 225 published articles, altogether there were only 11 papers that could be classified as research and these were mainly clinical retrospective studies.
It is also of interest to note that in 1965, Fred Henny, the editor-in-chief of the Journal of Oral Surgery, wrote an editorial in a special issue of that journal which was completely devoted to research. He stressed the importance of research and, in fact, became very directive in indicating the areas that should be explored.
The subspecialties
Around 1960, it was possible to define nine specific areas of clinical practice. They will be discussed here in three time frames that are somewhat arbitrarily chosen, although some major trends mark the selected dates.
The period before 1960 is characterized by post-war recovery and the establishment of oral and maxillofacial surgery as a specialty in most western countries, as well as several others. In most countries, the development was still mainly orientated towards the national interests and based on historical customs, with very little awareness of what was happening in other countries. This changed in the period 1960–1990, largely as a result of the appearance of journals that were purely devoted to the specialty. They were read worldwide and caused a growing sense of international dependency on ideas brought forwards by various clinicians and researchers.
t h e e m e r g e n c e o f t h e j ou r n a l s
Type of Ar ticle
British Journal of Oral Surger y (19 63 –19 65) 4 issues
Journal of Oral Surger y (19 63) 6 issues
Journal of Oral Surger y (19 64) 6 issues
Opinion 8 4 14
Review 20 15 18
Research — 5 6
Anesthesia — 14 4
New Te chnique 9 9 3
Case Repor t 19 35 32
Total 66 82 77
This was also the time that elective surgery began to emerge, including orthognathic and preprosthetic surgery. These two subspecialties would flourish in this period and expand the scope of OMF surgeons enormously. The period 1990–2010 brought many new technologies into the specialty and also a growing awareness that the treatments chosen needed to be valid and preferably evidence based. For this, several mechanisms became available but not the least of which was the “Parameters of Care: Clinical Practice Guidelines for Oral and Maxillofacial Surgeons,” as proposed by AAOMS and endorsed by the IAOMS and many affiliated, national associations.
In the following sections, the development of these specific areas will be described in the three periods mentioned. It was not the intention of the authors to describe a detailed or complete history of all aspects of the specialty but rather to present a bird’s eye view, with an emphasis on the reasons why and when we arrived at the present situation. When studying the literature of the past, the sheer number of articles on procedures that are no longer carried out and also the number of papers that are repetitive as they emphasize points previously made,
is striking. We inevitably had to be selective to illustrate the points made. In some sections, strong beliefs and even conclusions were postulated by various authors which later had to be reversed. Some of these conclusions were wrong and had to be changed dramatically. In that sense, the history is quite revealing and worth studying as it may happen again.
It is also acknowledged that the development is described from the perspective of “westerners,” with an emphasis on English literature and, to a lesser degree, on German and French literature. When reading the contributions of the affiliated associations from different parts of the world, it appears that important developments also took place in the non-English, non-German and non-French speaking world. However, it was not possible to get access to written documents from these countries, let alone that it would have been necessary to translate them.
Apart from many articles on specific items, it was most instructive to read the textbooks as they appeared over the years. They are listed in a separate column at the end of this chapter since many are quoted through all nine sections.
researc HFred Henny wrote an introduction in
of
Journal of
Surgery of June 1965, which was completely devoted
research and
of a research summit, which had taken place at Henry Ford Hospital in Detroit in September of the previous year. This was an initiative of the American Board in conjunction with the leadership of AAOS at that time. He writes a lengthy introduction in which he stresses the importance of research as part of the training of residents. This column contains his main message and one cannot escape being impressed with the vision of this man who was the first president of this association. Everything he says would apply to the current situation and his warning is just as timely today as it was in 1965.
“Education and research are welded together in an unbreakable band and it is a basic truth that a high quality of training service in any of the health sciences cannot be developed or maintained without this combination,” he wrote. “Strength in a clinical science, such as oral surgery, is built like a Russian troika: three powerful forces all pulling equally together: clinical care, education and research. If one force gets out of balance, obviously the pace of progress must slacken and the overall result becomes less desirable.
“Although formal education provides the foundation for a capable specialty in the health sciences, it is research that keeps it moving forward at a vigorous pace. In the present day of rapidly expanding scientific technology, it is virtually impossible for a branch of health sciences to keep pace with others around it unless it is fed by a steady diet of imaginative, well-conceived and productive research. Oral surgery cannot be an exception to this principle and obviously it must conform or eventually be relegated to a minor professional position that could almost be considered a craft.”
He also outlines 11 areas where he foresees that research is very much needed so as to improve patient care. These include: growth and development, neoplasia, aging process, trauma, the painful temporomandibular joint, focal infection, neurological state, wound healing, anesthesia, vascular changes and speech. It would not be difficult to update this list so as to make it more applicable for the present time but how appropriate this message was in 1965 and how much did we benefit from research in all these areas.
Paul J.W. StoelingaDentoalveolar surgery
Before 1960
Dentoalveolar surgery had been carried out in many countries for about 150 years before the 1960s on a more or less regular basis. Exodontia, in particular, was most often performed, using various forceps and elevators. It was John Tomes, however, a surgeon who practiced dentistry, who in 1841 proposed a logical design for forceps that would fit the contour of the cervices of the various teeth. Since that time, extraction forceps exist until today with few variations, something which is particularly notable when comparing European forceps with those commonly used in the U.S.A.
It is not surprising that in the two countries where oral surgery began, i.e. the United States and the German speaking area that the first written instructions appear. There are even monographs, solidly devoted to exodontia, which were published at the beginning of the 20th century (Mayrhofer, 1922, Winter, 1926, Berger, 1929 and Sicher, 1937). The latter emigrated to the U.S.A. and became widely known for his contributions to oral anatomy.
It is of interest to note that the techniques described entail the complete removal of all teeth and their roots, without any attempt to split them. This is even illustrated when removing deeply impacted third molars in the mandible. The removal of bone was largely done by chisel, although Adolf Berger recommended the use of a dental bur as an alternative, apparently against the then prevailing opinion, as he remarked: “The use of the bur is not regarded favorably by those who scoff at the dental engine as a surgical instrument. It will be found, however, that this method is satisfactory from the surgical and from the patient’s standpoint. Furthermore, it often has several advantages over the chisel technique. The bone can be cut accurately, quickly and safely; the tissue destruction is minimal; and the trauma and postoperative pains are mild.”
Berger was ahead of his time and would not have found much opposition today. It is needless to mention that large amounts of bone had to be removed to expose impacted teeth and to be able to remove them in one piece. This practice was still advocated by Wassmund (1935), although he used burs to remove the bone around impacted teeth.


Just before, during or shortly after the war, several textbooks on oral surgery appeared, again, mostly written by American and German-speaking authors. From most of these books, several new editions appeared with updates
on techniques or new developments, sometimes changing the titles slightly. (Archer, 1952, Pichler & Trauner, 1940, Mead, 1933, Thoma, 1948, and Rheinwald 1958). Some of them had updated editions until the 1970s.
There is one French book written by Chopret, Dechaume and Richard (1935) that reflects the state of the art in France at that time. The chapters dealing with dentoalveolar surgery, however, hardly changed and most advocated the use of burs to remove the necessary bone and to split impacted teeth and remove them in pieces. This probably had to do with the development of drills that had evolved from simple engines, driven by foot pedals, to electrically powered machines. The burs also had evolved into various designs suitable for the removal of bone or to cut through the teeth in the desired fashion. The techniques described in these books have not changed much and probably served as a basis for many manuals published in many countries in different languages.
There is one exception that needs further explanation. It concerns the “lingual split” technique as was previously practiced widely in the U.K. According to Ward (1956), this technique was introduced by Kelsey Fry but never written up until the publication of Terence Ward. The rationale for this technique is beautifully described by Killey and Kay (1965): “When a chisel is preferred for 3rd molar surgery, use should be made of the fact that the buccal bone is relatively thick by comparison with the thin shelf of lingual plate and that when the latter is split off, the main bony support to the tooth is eliminated and with it the resistance to effective delivery. It also reduces the size of the residual socket and, therefore, the blood clot.” This author (PS) learned this technique in 1971 in East Grinstead and has used it ever since in selected cases, particularly distally tilted molars, very much to his satisfaction.
Apicectomies, with the intention of treating an apical cyst or granuloma and to save the tooth, also have a long history. According to Wassmund (1935), it was Partsch (1896) who introduced the principle of surgical endodontics, but Thoma (1948) refers to Farrar (1876). From the beginning, removal of approximately one-third of the root was recommended to include the apical inflammatory tissues along with the ”necrotic” cementum (Wassmund, 1935, Mead, 1940, Thoma, 1948, Archer, 1952), or even to resect to the deepest level of the bony defect so as to avoid any dead space behind the root (Rheinwald, 1958).
To illustrate the way of thinking of that time, it is revealing to quote Thoma in 1948 “…consists of the apex of the tooth because it harbors bacteria in the dentinal canals and the lacunae of the cementum which are not accessible to ordinary methods of sterilization. The apex of tooth undergoes necrosis, but, unlike bone, it is not sequestrated although resorptive processes are frequently present.” What did he see that we presently are not aware of?

All mentioned authors describe only an orthograde filling technique, apart from Pichler & Trauner (1940) and Rheinwald (1958), who also described retrograde fillings using amalgam. Most authors were also rather hesitant to embark on multi-rooted teeth such as molars and bicuspids. They warn of perforation of the sinus membrane with possible sinusitis as a result, or damage to the inferior alveolar nerve. Louis Grossman (1965) described the operation in a step-by-step version with simultaneous root canal filling. It is obvious at this stage that knowledge of the detailed anatomy of the dental root canals was lacking, while also the advances made in conventional endodontic treatment had not yet become apparent. The theories on which the treatment was based,
along with the subsequent recommendations, were all based on experience and assumptions rather than evidence, as we know it now.
A procedure that had certainly fascinated clinicians for a long time was tooth transplantation, be it autogenous or allogenic. It was already known, at this time, that allogenic transplantations did not result in long-lasting success. A very good description of autogenous tooth transplantation is found in the book of Georg Axhausen (1940), who describes the importance of maintaining the periodontal membrane and, thus, the need for atraumatic removal of the tooth used for re-implantation or transplantation. He had done animal experiments, without being specific about it, that showed replacement resorption occurring soon if the periodontal membrane is not preserved. He also showed some very good results in his book. This technique became very popular in the succeeding years.
There are, of course, other procedures that could be mentioned in this section but they will be dealt with in the specific sections, such as pathology and preprosthetic surgery. One exception has to be made; it concerns the handling of oro-antral perforations. In the second volume of Wassmund (1939), almost all methods used during this time to close an open antrum are beautifully presented with extreme detail, including excellent illustrations. There has been very little new published, in this respect, ever since. It also becomes very obvious when reading the American textbooks, that they had no knowledge about the things Wassmund had written about and vice versa and certainly not about this topic.
1960–1990
Exodontia had not developed further during this period, apart probably from some better drills to free retained roots or impacted teeth. All textbooks or monographs written in this period [Killey & Kay, (1980), Tetsch & Wagner, (1982), Laskin, (1985)], or adapted from earlier versions of published books and reprinted, show pretty much the same techniques. There was, however, more concern about the possible complications associated with removal of impacted mandibular third molars. This had largely to do with some follow-up studies that were done during this period. It became obvious that temporary or even permanent disturbance of sensitivity of the inferior alveolar and lingual nerve was a serious problem and occurred with a frequency of between 5–12 percent. The majority of cases, however, recovered spontaneously.
The issue of alveolitis was also addressed during this period, and with it came the discussion whether or not to use antimicrobial drugs as a prophylactic measure. The studies of Birn (1973), however, threw some light
on the etiology of alveolitis, pointing towards fibrinolysis as the causative factor rather than primary infection. In retrospect, it is surprising that there was no doubt about the recommendation of prophylactic removal of all impacted third molars, despite the absence of any evidence to support this notion, apart from personal anecdotal experience. The National Institute of Health in the U.S.A. even came out with a statement in 1979 saying:
• A ll third molars are pathological.
• T hey cause crowding over the years.
• R emoval at a young age causes fewer complications.
At present, this would be called level V evidence, the lowest level possible, based on a consensus of “experts.” At that stage no information was available on any longitudinal study supporting the statements they made.
The practice of apicectomies was still carried out according to the principles as laid out by the authors of the mentioned texts but some nuance was introduced, probably because of the progress endodontics had made over the years. Gerstein, writing the chapter on apicoectomies in Laskin’s book (1985), writes: “It is usually not necessary to remove the portion of the root that lies within the bony lesion, except for access to the area of pathosis.” Most current practitioners would agree with this statement in the light of the current knowledge of minimal exposure of accessory canals. There is also no hesitation anymore in treating posterior teeth.
The biggest progress in this period was made in the area of tooth transplantations and re-implantations. Research in this field had resulted in fairly predictable outcomes, particularly when teeth were transplanted with wide open apical foramina. One of the pioneers in this field was Shullman, who also wrote a chapter in Laskin’s book (1985) about tooth re-implantation and transplantation, for a large part based on his own research. He emphasized the advantages of transplanting teeth at a young age, when the apical foramen is still wide open, so as to facilitate survival of pulp vasculature. He preferred auto-transplanted teeth to implants, because erupting transplanted teeth stimulate growth of the alveolar process, contrary to implants. He also wrote: “Survival depends on maintained viability of the periodontal ligament and cementum on the surface of the donor tooth.”
This is pretty much in line with what Axhausen had said some 45 years previously. Considering the many articles in various journals on this topic, this technique was enormously popular. The ultimate book on tooth transplantation and re-implantation is written by Andreasen (1991), another pioneer in this area. It provides
the science behind the technique but also serves as a step-by-step atlas, demonstrating the procedures in detail. He also advocates transplantation of developing bicuspids into sockets of avulsed front teeth in growing children, as opposed to implants.
1990–2010
As stated before, dentoalveolar surgery did not change much during this period, apart from the improvement of instruments used and better imaging. Numerous manuals in various languages appeared but two classic books stand out, one from Sailer and Pajarola (1996) and the other from Andreasen, Kølsen, Petersen and Laskin (1997). In both texts, up-to-date information is provided about the currently used techniques, the preoperative preparation of patients and their aftercare.
In this period, the third molar issue came prominently into play, initiated by two thought-provoking articles (Mercier & Precious, 1992 and Shepherd, 1993). They questioned the routine prophylactic removal of asymptomatic third molars in the light of the morbidity associated with it and the cost effectiveness. This discussion prompted some research that in part is still going on but is notoriously difficult, because the necessary long-term, longitudinal studies are still not present. There are, however, some well-designed studies that, for the time being, are helpful in making up one’s mind.
Kugelberg et al. (1991–1993) from Norway did some excellent work on the healing capacity of the periodontium distal to the second molar and found that this was almost 100 percent when the patients were younger than 25 years. Beyond that age, the chances are that irreparable damage will occur, leading to loss of septal height distal to the remaining second molar, with subsequent problems. Ventä et al. (2004) found in a group of dental students that over a period of 18 years seemingly deeply impacted third molars in the mandible could still change their position and even erupt. Last, but not least, the assumption that third molars contribute to the crowding of the lower front teeth is seriously questioned by orthodontists as well as OMF surgeons, based on some rather convincing clinical research (Lindauer et al., 2007).
This would certainly be one reason less for contemplating prophylactic removal. The overriding argument, however, to question this policy is the fact that from several studies, it became apparent that only in some three percent is there serious pathology involved, including cysts and tumors, associated with impacted third molars (Eliason et al.,1989, Güven et al., 2000). It will probably take some time until this issue is settled, based on evidence rather than speculation or anecdotal information.
The AAOMS currently has a research project underway that should provide clinical and biological data to support effective third molar treatment (White, 2007). The Cochrane Group, however, has come out with a recommendation based on currently available information (Mettes et al., 2005): “Asymptomatic bony impactions and even third molars completely covered by soft tissues should not be removed, while only partially erupted wisdom teeth should be removed, preferably before the age of 25 years.”
There is no doubt, however, that there is another side of the coin. Removal of third molars at a later age, because of inflammatory disease or otherwise, particularly when elderly people are involved, leads to more morbidity. (Kunkel, et al., 2007). The longitudinal study that is currently underway, sponsored by the AAOMS, should establish whether hard data exist to support established practice.

Another issue in which much progress has been made concerns the avoidance and the repair of damaged branches of the trigeminal nerve after mandibular third molar surgery. Excellent studies have appeared on the anatomical variation of the lingual nerve position, which enables the prudent surgeon to avoid its damage (Pogrel et al., 1995). Three dimensional imaging allows for exact assessment of the relationship between the inferior alveolar nerve and the roots of a third molar to avoid traumatic injury of this nerve. It is thanks to Hillerup and coworkers (2007, 2008), that objective criteria have been established upon which to base the seriousness of the damage and a protocol for micro-surgical repair with subsequent follow-up.
The development of endodontics has narrowed the indications for surgical endodontic treatment (apicoectomies) considerably. Modern techniques to find and open obliterated canals, or to remove metal posts in previously treated canals, have eliminated the need for surgery. In addition, the current practice of conventional endodontic treatment has improved the outcome of the treatment in such a way that there is less need for surgical solutions. Yet, there are still indications for surgical endodontic treatment and the techniques as described above are still valid.
Infectious diseases
Before 1960
Infectious disease must have been very prominent in the old days as there was no emphasis on oral hygiene and both periodontal and pulpal infections must have abounded.
There are many illustrations made in the 17th and 18th centuries and even before that time, which show individuals suffering from a swollen cheek with a bandage around their heads. This probably was the main reason why general surgeons were called upon, since some of these conditions were life-threatening.
In the beginning of the 19th century, these surgeons had no idea what the cause was of the severe abscesses and indurations that they saw. This is well illustrated by the description of “an inflammation in the anterior part of the neck with an emphasis on the submandibular regions” by Friedrich von Ludwig in 1836. He describes that he favored a conservative approach, which in most cases would result in death. He also commented that in some cases, foul smelling, reddish-brown fluid escaped via the mouth. He had, however, no idea what the cause could be and suggested an “erysipelitic process probably related to a poor general condition or a weak nervous system.”

Contemporary surgeons such as Dupuytren in Paris, shared his approach (Hoffmann-Axthelm, 1995). It took some time before the link was made to the role of bacteria and the dentition.
A complete and accurate description of the often dramatic and rather quick development of a phlegmone of the floor of the mouth (Ludwig’s angina) is presented by Mickulicz and Kümmel in 1898. They recognized the delicate anatomical structure and the proximity to the throat as the main reason why the patients had difficulty swallowing and breathing. They also mentioned difficulty in inspecting the mouth because of trismus and the swollen tongue and realized that this condition had, of course, nothing to do with an inflammation of the throat. They also described the often fatal course of events, despite surgical intervention, such as incision and drainage and particularly emphasized that death might be a matter of days if the patient does not respond to the surgical treatment. Thoma, in 1948, added: “The clinical course might be mild but it may suddenly change and assume an alarming character. Deglutition is hindered, speech is difficult and saliva may run from the mouth since swallowing causes pain. There is a rapidly extending edema, which causes respiratory difficulties (angina). The larynx itself may be involved suddenly in the rapidly progressing edema and may become obstructed.” Today, one cannot think of a better description. It is only after the introduction of penicillin that the prognosis of this condition changed, as Thoma rightly noticed in 1948.
Textbooks in German and English from the first half of 20th century all mention the necessity of treating abscesses in and around the mouth by incision and drainage, recognizing that the cause of these inflammatory conditions in most instances were decayed teeth which, therefore, had to be extracted as well. The better knowledge of head and neck anatomy also led to the recognition of the stereotype appearance of deep space infections.
Osteomyelitis was another condition that gave rise to major concern in the days before antimicrobial agents were available. It was in particular, the acute form that worried the clinicians. One has to keep in mind that most of them had a general surgery background and were, therefore, inclined to compare the disease in the mandible with the often dramatic course of events in the long bones. Surgeons like Axhausen and Wassmund, but also others, were hesitant to go into the bone to remove sequestra, fearing uncontrollable spread of the inflammatory process.
A much feared complication was thrombophlebitis with hematologic spread to other bones, resulting in certain death. These considerations still played a role in the 1950s. For instance, Archer writes in the late 1950s and early 1960s that sequestrectomy should only be carried out “when the sequestra are freely movable.” There apparently was still this fear of manipulation in the infected bone with the idea in mind of metastatic spread despite “the use of massive doses of penicillin.”
Last but not least, specific infections were apparently a widespread problem. Tuberculosis, syphilis, gonorrhea and actinomycosis presented frequently in the orofacial area and also affected the jaw bones. The old German textbooks are full of case reports and describe drastic surgical approaches with often negative results. When reading, for instance, how clinicians struggled when treating patients with actinomycosis, one can only utter a sigh of relief that we live in a different era. Brophy (1918) quite flatly states “that spreading usually takes place in the soft part of the neck and even mediastinum and that there is no cure!” Wassmund (1935) mentions also that there is a high mortality rate associated with actinomycosis but recommends irradiation on top of rinsing with potassium-iodine. This therapy was followed by many German clinicians until the 1950s as they all quote Wassmund as the proponent of irradiation (Pichler & Trauner, 1948). Even in 1952, Hofer and Reichenbach still mention potassium-iodine rinsing in combination with irradiation, although they also mention the use of penicillin and aureomycin.
1960–1990
As mentioned previously, the introduction of antimicrobial agents changed the approach to infectious disease drastically
although the principles of incision and drainage remained valid and the old adage “ubi pus ubi evacue” the mainstay of proper management of an abscess. Textbooks written in this period all deal with odontogenic infections and emphasize the elimination of the cause by either extraction of the causative teeth or proper endodontic treatment (Thoma, Archer, Laskin, etc.).
Another factor that played an important role in the improved management of infectious disease was the introduction of better imaging as compared to the hitherto used plain radiographs. The orthopantomogram, CT scan, MRI and scintigraphy all contributed to the diagnostic capacity of the clinician. Most important were also the advances made in microbiology, in that better determination of the bacteria involved was possible. This had major consequences because the antimicrobial therapy could be directed specifically to the microorganisms involved. This was particularly important for deep space infections in which anaerobic bacteria are often involved.
Recommendations for the treatment of osteomyelitis and particularly the acute form included much more aggressive procedures than in the preceding period, including decortications and removal of sequestra along with proper antimicrobial treatment (Topazian, Goldberg 1981, Laskin, 1985). It is somewhat remarkable that there are relatively few papers written in this period on the subject of acute osteomyelitis.
In the early 1970s, the first reports appear on a special entity that was called chronic sclerosing osteomyelitis. It was Jacobsson et al. (1978) who emphasized the use of scintigraphy in the diagnosis of this therapy resistant lesion. Further diagnostic improvement was reported in 1984, also by Jacobsson, while the adjunct diffuse was added to the description of the condition. It is of interest to note that surgeons applied the techniques, as known from the suppurative form of osteomyelitis, including decortication and long term use of antimicrobials but with poor results (Montonen et al. 1990). There simply was no causative agent to be detected in most instances, which eventually changed the thoughts about this lesion and, consequently, the treatment.
The improved medication against tuberculosis, syphilis and other specific infections resulted in the fact that orofacial manifestations were hardly mentioned anymore in the world literature. That does not imply that these infections did not occur but probably not in the developed world as much as they used to. It is likely that in the developing world, this was still a problem, but there were simply no OMF surgeons in many of these countries who were prepared to write about these diseases. A condition which had not disappeared is actinomycosis. Early recognition and proper antimicrobial treatment had, however, changed the picture
completely. Cervico-facial actinomycosis used to be a killer in the old days, posing enormous dilemmas for the surgeons involved. The days of surgical exploration and rinsing with potassium-iodine and/or sulfanilamide were definitely gone.
An excellent book on the management of infections of the oral and maxillofacial regions was presented by Topazian and Goldberg (1981), who described the state of the art in the early 1980s.
1990–2010
The fundamentals of the management of infectious diseases had not changed in this period but some new conditions occurred as a result of immune suppression, be it acquired or drug induced and because of the side effects of biphosphonates. Clinicians are also more alert to bacterial resistance to the commonly used antimicrobials because of overuse of these drugs over the years. Plain penicillin, for instance, used to be the drug of choice for any odontogenic infection because streptococci always used to be sensitive to this drug. In many countries that is no longer the case.
Patients with AIDS or persons carrying the HIV virus became a giant problem for healthcare providers and certainly caused the OMFS profession to be alert to the typical oral manifestations. In addition to that, these individuals are very sensitive to infections, including specific infections such as tuberculosis.
The surprise of this period was undoubtedly the discovery that biphosphonates cause osteonecrosis of the jaw bones (Marx 2003). Since this publication, a large number of cases have been reported, cautioning the profession to be alert. Infection is only secondary to the primary problem but long-term antimicrobial treatment is certainly important in the treatment, along with surgical debridement of all necrotic bone and tension-free primary closure of the overlying mucosa (Williamson 2010). This is similar to the treatment of osteoradionecrosis.
The debate about chronic diffuse sclerosing osteomyelitis went on and several new suggestions were made about its etiology and treatment. Van Merkesteyn et al. (1990) introduced the concept that the condition should be considered a tendo-periostitis because of overuse of the masseteric muscles. This idea was not unequivocally followed and probably rightly so, because promising results had been achieved by influencing the bone metabolism using calcitonin (Jones et al., 2005) and biphosphonates (Yamazaki et al., 2007 and Kuijpers et al., 2011). If these treatments appear to be successful in the long run, then this condition should no longer be considered an infectious disease.
As mentioned in the previous section, specific infections in the oro-facial area are rare but currently an interesting
phenomenon can be observed. Tuberculosis is emerging again since there is increasing global resistance to antituberculous drugs (Kakisi et al., 2010). It presents itself mostly in the soft tissues and lymph nodes, of course, but apparently also in the maxilla and mandible and even the TMJ.
In the last ten years, several case reports of tuberculous osteomyelitis affecting the mandible have been described, especially by authors from developing countries and often in the pediatric and radiological literature. It often concerns extrapulmonary presentations of the disease and frequently occurs in HIV patients (Bendick et al., 2002). In the developed world, it remains a rare phenomenon and, in particular, the bones are rarely affected (Chaudlary et al., 2004) but the migration of people means that even in the western world, every once in a while, a surprise finding occurs (Heibling et al., 2010). Actinomycosis, of course, is still around but is usually diagnosed at an early stage and, therefore, easily treated. It may also still involve the jaw bones (Finley and Beeson, 2010).
Despite the improved dental care in many parts of the world, odontogenic infections are still relatively frequently encountered. The present generation of clinicians, however, has the tools to deal adequately with them. Yet, danger lies around the corner and a certain degree of alertness is warranted, because the course of events may still run out of control.
The most dramatic example is the evolution of a seemingly simple odontogenic infection into a fulminant necrotizing fasciitis. Although the first reports of this often fatal condition were described in the ENT literature in the late 1970s, because of pharyngeal infections, it soon appeared that odontogenic infections could also cause this dramatic spread, which is mostly based on a mixed infection.
It is particularly during the last two decades that numerous case reports have appeared in OMFS literature. The most frightening observation is that, recently, cases have been reported caused by staphylococcus resistant to methicillin (Zhang et al. 2010). Apart from this unusual but potentially fatal condition, resistance against the currently known antimicrobials is increasing and will, therefore, play a more prominent role in the future.
The massive number of AIDS and HIV infected patients in the developing world who are not adequately treated to control the underlying condition, still pose an enormous problem. Although better drugs are on the market, they are often not available for patients in the developing world (Bendick et al. 2002). Hence, it might be expected that unusual infections that were thought to be eliminated will appear again and even present in the developed world because of the migration of people.
Trauma
Before 1960
Although trauma has been with us since the dawn of time, it is only relatively recently that we have been able to approach it scientifically. For this reason, the reports of treatment do not necessarily follow any logical pattern, really amounting to a series of case reports contained within the literature from the earliest pre-Christian times to Egypt in 2000 B.C. when a dislocation of the mandible is described as well as a fractured mandible. Hippocrates, described reduction and fixation of mandibular fractures with strips of calico glued to the skin immediately adjacent to the fracture and laced together over the scalp. The ancient physicians of Alexandria and Rome also mention the ligation of teeth using fine gold wire or Carthugian leather strips glued to the skin. The principles laid down by Hippocrates really extended through the literature as far as the turn of the first millennium.
It was probably Salicetti in 1474, in Bologna, who first described the simple expedient of ligating the teeth of the lower jaw to the corresponding teeth of the upper jaw to effect immobilization of a fracture. Previously, it had been recognized that within three weeks, union of jaw fractures was complete.
The 16th and 17th centuries saw the introduction of gunpowder and the first reports of gunshot wounds. It was Ambroise Paré to whom we must attribute the first significant change in the management of facial wounds through copious irrigation of wounds and the application of balms rather than cauteries. His particular care to facial injuries and his application of what he described as “a dry suture” facilitated secondary healing of facial wounds, particularly compound injuries.
The next milestone was with Richard Wiseman, a surgeon in the latter part of the 17th century who described the management of maxillofacial injuries. As well as describing the signs and symptoms of a fracture, he also described many individual cases, including a child with a comminuted fracture of the cribiform plate of the Ethmoid. He also described the disturbance in occlusion and related protrusion or recession of the lower jaw and the destruction of soft tissues in association with these injuries (Rowe, 1971). These astute clinical observations were added to those studies of anatomy and physiology at the Italian schools of Bologna and Padua as the eighteenth century arrived. Together they laid the foundation for serious advances in the systematic management of jaw injuries.
Chopart and Desault (1780) were the first to describe a different type of approach by introducing the concept of a dental splint which consisted of a shallow trough of iron, inverted over the occlusal surface of the lower teeth, which
they protected with cork on lead plates. A bar projected from the front in the incisor region, being bent at right angles and fastened by thumbscrews to a submandibular plate of sheet iron. Movement of the fragments was thus prevented by compression between the occlusal surface of the teeth and the lower border of the mandible.
Variations of this principle were employed during the next 100 years being introduced into Germany by Rütenick in 1799, who further stabilized the fracture by using a head harness, in England by Lonsdale in 1833 and the Netherlands by Hartigs and Grebber (1840) but each was a modification of the original principle which still found employment even after World War II for the fixation of some epithelial inlay splints in the edentulous mandible (Rowe, 1971). Different forms of supportive bandaging were introduced, accompanied by wedges of cork between the occlusal surfaces of the teeth to maintain the teeth apart and facilitate feeding. Slightly earlier than this, in 1825, Naysmith, co-operated with Robert Liston by providing a cast gold cap splint. This was soldered together and affixed to the teeth, where they had the effect of preventing displacement of the mandible in a mandibulectomy case, until the majority of the forces of soft tissue contraction had dissipated.
The advent of ether anesthesia in 1846 and chloroform a year later saw a significant increase in the scope for treating jaw injuries when Fouchard in France and Buck in the U.S.A. began to use direct intraosseous silver wires. Results were very variable due to the development of sepsis and consequently sequestration. A variation by Wheelhouse, involved driving silver pins through each piece of bone and winding silk thread around each pin in a figure eight to approximate the bone ends.
War has always provided opportunity for development in surgery and so it was with the American Civil War of 1861–1865 and the Franco-Prussian War of 1870–1871, in quick succession, a large proportion of mandibular fractures arising from horse-kicks or falls onto the chin as well as gunshot wounds.
In 1861, Gunning produced his splint, although he was probably unaware that it followed the same principle as the one developed by Naysmith in 1825. From dental impressions, a monobloc construction was produced and bound to the jaws by a bandage passing under the chin and over the vertex of the skull. Teeth in the line of fracture were extracted. Later in the war (1864) Bean, who treated many fractures, made a significant advance by sectioning dental models of the jaws and carefully realigning them before constructing a Gunning type of splint (Rowe, 1971).
The first reports of swaged metal splints appear simultaneously by Allport in America and Hayward in London. Allport’s gold splints were swaged so as to leave
the occlusal and incisal edges free and having correctly aligned them, the splints were soldered together. Soft gutta-percha was used to attach them to the teeth. Hayward covered the occlusal surfaces of the teeth and also used soft gutta-percha for attachment. A separate sub-mental, gutta-percha splint was placed in position and a bandage or rubber bands used to connect it to two arms projecting from the splint and curving backwards around the commissures of the mouth. Despite further modifications by Kingsley, all these splints are essentially modifications of that original splint of Chopart and Desault of 1780 (Rowe, 1971).
The inherent weakness in all these splints was the lack of secure fixation to the jaws and various attempts now begin to appear to overcome this. Hamilton Adams in 1871 used fine nuts and bolts passing through the interdental spaces. Some three years later, Moon, in London used fine inter-dental wires to achieve the same result. It was at about this time that Woodward, in the U.S.A., melted down silver coins (silver & copper) to produce open cast metal cap splints, attached to the crowns of the teeth by small screws. The two splints were located to one another by lugs and through the means of eyelets soldered to them the jaws could be wired together, thus giving mandibular, maxillary or inter-maxillary fixation (Rowe, 1971). Although a significant advance, the very complicated
nature of the process and the lack of a cementing medium for attaching the splints to the teeth meant that they did not catch on rapidly. However, attention is now shifting to the improved accuracy of reduction provided by focusing on the occlusion.
During the Franco-Prussian War, Hammond described using arch bars on both the lingual and buccal aspects fixed to the teeth by fine inter-dental eyelet wires. This was adapted in both the wiring of arch bars and the continuous loop method. At the same time, Suerson, in Berlin, was chiefly employing the Gunning principles, but, when treating malunions, conceived the idea of separate splints for each section and by driving wedges of hickory wood of ever increasing thickness between these, gradually realigned the arches. This seems to be the first account of an attempt at realignment of displaced arches.
In 1887, Gilmer returned to an almost forgotten technique, the direct wiring of teeth. This resurrection of an old principle, suitably modified, was a significant advance and became increasingly important as orthodontic techniques became adapted by surgeons to the treatment of fractures. Angle applied his principles of fixed anchorage points and individual bands cemented to selected teeth in each jaw as a means for restoring a correctly aligned dentition (Hoffman-Axthelm, 1985).
So now, for the first time, we see science being applied to the management of these injuries. This, together with the huge advances in surgery, occasioned by the introduction of anesthesia, the institution of antiseptic and later aseptic techniques and the introduction of x-rays for clinical purposes by Röntgen in 1895, changed the scene dramatically.
Other significant advances which followed at that time included the reconstructive work of Abbe, Estlander and Thiersch; the treatment firstly of fractured zygomas by Matas (1896) and then a middle third by Bouvet in 1901 and the surgical approaches to the zygoma of Lothrop (1906), Keen (1909) and Manwaring (1913), coupled with the description of fracture lines by Rene le Fort in 1901, meant that by the onset of World War I, surgeons were in a position to consider treating the mutilating injuries resulting from trench warfare. The scale of these injuries, 26 million casualties of the 56 million involved in armed conflict, was due largely to trench warfare and the destructive nature of the high energy explosives which rendered the face prone to more severe injuries than had previously been seen.
However, the sound principles laid down at the turn of the century did not undergo any radical change rather there were a series of refinements in techniques, often following the application of orthodontic principles to splint construction. Circumferential wires were used in

some cases, Gunning’s type splints in others, especially edentulous cases and both open and closed cast silver cap splints in dentate patients were used to a greater extent than previously. Fresh cases were treated by sectioning the models, restoring the occlusion in the laboratory and forcing the segments into the splints at the time of reduction and immobilization. In cases where treatment was delayed, reduction was effected using orthodontic techniques. The use of interdental eyelet wires was demonstrated by Ivy (1914) to be an effective way of providing intermaxillary fixation in the dentate patient and was increasingly practiced.
Quite independently, the same sort of development took place in the German-speaking part of Europe and in France. Splints, arch bars and the principles of traction to reduce displaced fragments also were used, as presented by Hoffman-Axthelm (1995). The name of Claude Martin from Lyon should be mentioned in this context, but also those of Bruhn, Hauptmeyer, Kuhl and Lindemann, (1915), Misch & Rumpel (1916) and Klapp & Schröder (1917), who devoted monographs to the treatment of the facial injuries of the military.
Replacement of both hard and soft tissues had reached a remarkable degree of sophistication with surgeons developing ingenious techniques to achieve outstanding results but sepsis, leading to gangrene, hospital-based infection as well as other general infections, all contributed to the high level of morbidity and mortality of that time. There followed certain specific improvements in the surgical care of facial fractures. Notable among these was the development at East Grinstead of sectional splints, one for each segment, linked together by intraorally located locking plates, which underwent later modification to be located extraorally. Middle third fracture management also underwent improvement where cheek-wires, first developed by Federspiel, were used to fix the posterior part of the maxilla to the plaster of Paris head cap (Rowe & Killey (1955).
The use of circumferential wiring, prosthetic replacement of soft tissues, the general management of soft tissue injuries, including the lavage with hypochlorite solution, all helped to keep down infection. However, the description of the use of the tube pedicle by Gillies (1917) and Faltrow (1917), the precision techniques of Kazanjian (1949), brought forward from World War I and improvements in bone grafting also demonstrated the need for special centers where reparative surgery could be carried out. It also saw the union of different like-minded surgeons from a variety of backgrounds resulting in improvements in patient care through a team approach.
In England, the first such center at the Queen’s Hospital in Sidcup was established under the leadership of Major Harold Gillies, who assisted in the care of jaw
injuries by Kelsey Fry and Fraser. However, many other notable names were involved, including Kilner from the British Forces, Blair, Ivy, Kazanjian and Curtis from the American forces, Pickerill from New Zealand and Valadier working in France.

Both sides in the conflict adopted a principle of establishing field hospitals where teams of surgeons would work together providing stabilization of the injuries before evacuating the casualties to rear positions. In the case of the British and American forces, this often meant to the U.K. It was the need for rapid stabilization that led Adams (1942) to introduce his internal suspension techniques. The rate of evacuation was slow by comparison with the process in 2000 since air evacuation had not yet been developed.
By 1945, the end of World War II, there was an increasing realization that when bone ends are brought into close proximity with one another, more rapid healing occurs. With the advent of antimicrobials at the same time, a greater use of direct approaches to the fracture sites led to the advent of direct interosseous bone wiring or osteosynthesis. Such wires were generally applied to either the upper or the lower borders of the mandible and the fronto-zygomatic suture, all solid pieces of bone.
During this war pin fixation was used, particularly in the treatment of compound, comminuted and frequently
infected jaw fractures. Despite a reduction in their use, the concept was retained and used by Fordyce in the “Boxframe” technique. A variety of pins were used from the fine threaded Clouston-Walker pin, modified for the East Grinstead pattern and MacGregor pins to the coarse threaded, tapered Moule pin. It was not until the Vietnam War that the American forces came to use biphasic pin fixation, popularized by Morris (1949), that external pin fixation was again to become the treatment method of choice. In France, Ginestet (1958), working in the military hospital of Val de Grace, also favored percutaneous pins with fixation by an extraoral bar, fixed to these pins with screws.
The vast experience of the American, British and German surgeons with the treatment of injuries and the increase in traffic accidents led to the first comprehensive books on maxillofacial trauma written by Rowe and Killey (1955, 1968), Kazanjian and Converse, (1949, 1959, 1974), Dingman and Natvig (1964) and Reichenbach (1969).
1960–1990
With the advent of antimicrobials, recognition of the value of direct fixation became widely accepted in orthopedic practice and was adapted for maxillofacial purposes. Initially, direct bone wiring was used to control the edentulous posterior fragment in the mandible. Grossly comminuted mandibular fragments also were wired together.
Although the use of bone plates had previously been attempted, [Konig, (1905), Lambourne (1907), Lane, (1914) and Sherman, (1924)], it was not until Roberts (1964), Battersby (1967), Snell (1969) and Michelet et al. (1971) introduced stainless steel or vitallium mini-plates, fixed with monocortical screws, that the present vogue for use in the OMF sphere of surgery was established. The lack of malleability in these initial mini-plates limited their usefulness, for they broke just as soon as any attempt was made to bend them.
The introduction, initially of malleable stainless steel, followed by titanium, enabled Champy et al. (1976) to prepare a scientific basis for the application of mini-plates in the treatment of mandibular fractures through an intraoral route, although Michelet et al. (1973) had also recommended an intraoral approach. Inevitably, numerous clinicians and manufacturers provided their own modifications but the principles of application, as laid down by Champy et al., remained
unchanged. Use of micro-plates has a particular role in the treatment of fractures in children.
Bioresorbable plates made initially of polylactic acid and more recently of a combination of this with other suitable materials, have been developed by Bos, (1983), Rozema, (1991) and Suuronen, (1992), using poly-L-lactide. The biodegradation tends to be accompanied by significant collection of fluid beneath the skin, probably caused by a foreign body, inflammatory reaction.
The compression osteosynthesis techniques of orthopedic surgeons were translated to maxillofacial surgery by Spiessl (1969), Luhr (1968, 1972) and Becker & Machtens (1970). The use of specially designed taps and matching screws allowed both cortices to be engaged, which, when combined with the specially designed plates, produced firm apposition of the fractured bone ends under a degree of compression. This results in primary bone healing by direct osteoblastic activity within the fracture, as opposed to the secondary bone healing through callus formation.
Intra-medullary pinning, the use of titanium as well as non-metallic mesh, particularly in the treatment of malunions and fractures of the edentulous mandible, all have a place. Williams (1994) developed a modification of the circlage principle in the management of fractures of the severely atrophic edentulous mandible.
Detailed descriptions of all these techniques were published in a textbook by Rowe and Williams, “Maxillofacial Injuries” (1985).
1990–2010
One of the most significant developments in the management of trauma in recent years has been the evolution of immediate care as proposed in the U.S.A. with the introduction of the principles of “Advanced Trauma Life Support.” These principles have been advanced even further into the immediate management of injured military personnel:
• T heir extremely rapid evacuation by helicopter to highly equipped and staffed field hospitals where intensive care facilities are provided;
• T he almost immediate air evacuation to specialist units in the home countries by teams of intensivists who can ensure a continuity of care throughout the whole procedure.
It is, in many respects, developments around resuscitation and immediate care that have improved the outcomes for all patients, including those with maxillofacial injuries, rather than any single surgical technique developed within the specialty.
However, the consequence of an earlier presentation of resuscitated patients and the move towards earlier surgery by trauma teams has meant that facial injuries are being tackled at an earlier stage. This led to a different approach with early exposure of fracture sites, direct plating of them and reconstruction of the facial skeleton from the cranial base downwards (Gruss & Mackinnon, 1986). This direct approach has greatly facilitated the rehabilitation of facial appearance but unless adequate attention is paid to the occlusion, function can be prejudiced.
With the move to shorter hospital stays and earlier mobilization of the injured, this development is in keeping with the overall modern philosophy of trauma management. There is always a risk that patients may be seen as being over-treated when simpler techniques may be more appropriate. This is a tendency to be avoided in the face of over-enthusiasm. Management of civilian injuries has always followed those acquired in armed conflict and the recent conflicts, both in Iraq and Afghanistan, have resulted in these principles of resuscitation and early intervention being taken forward into civilian practice.
Despite these advances, there remain controversies over the treatment of specific injuries and in some instances lessons of the past seem to have been forgotten. One notable example among these is those associated with fractures of the mandibular condyle both in children and adults (Izuka et al., 1991). There are many proponents of open reduction and rigid fixation of condylar fractures and several techniques have become available (Eckelt and Loukota, 2010). It is claimed that better functional results are achieved with these methods as compared to non-surgical treatment. Double-blind, randomized studies, however, are lacking and one cannot escape the impression that there is a tendency towards overtreatment.
Where children are concerned, Rowe, as long ago as 1968, urged caution and a conservative approach, a view shared by Walker (1994) and a lesson which was reiterated by Hovinga et al. (1999). In an almost identical series treated operatively with a wide exposure, Izuka et al. (1998) had later problems with all his cases. In adults Smets et al. (2003), in a retrospective analysis, concluded that only in cases of shortening of the ascending ramus by 8mm or more or where there was considerable displacement of the condylar fragment, was surgical intervention indicated. This was in keeping with recommendations formulated by Silvennoinen et al. (1992).
Ellis (1999) noted significant positional changes in the condylar fragment during conservative treatment and concluded that care needed to be exercised before basing treatment decisions on the degree of displacement. So, the fact that open operation and internal fixation is clinically
feasible through a variety of approaches and techniques does not mean that condylar fractures should always be treated in this way.
Enormous improvements in technology have resulted in better diagnosis of the detail of severe injuries, yet even with that degree of sophistication, there remain areas where application of reconstructive surgery fails to produce the expected outcome. A good example of this is with orbital fractures. Here the use of axial tomography by Koorneef & Zonneveld (1987) demonstrated not only the exact location of injury but also the soft tissue damage caused by the trauma. Development of their techniques enabled the estimation of orbital volumes and the construction of grafts of appropriate volume for use in reconstructive surgery. Further refinement of this technique became possible with the introduction of 3D computed models.
Studies on unaffected orbits might be helpful in creating pre-shaped implants particularly for the posterior portion of the medial wall and floor of the orbit (Kamer et al., 2010). Although various forms of allografts have provided a means for restoring orbital volumes, the conical nature of the orbit is very difficult to mimic, thus good results are not reliably achieved.
The developments in resuscitation, CT scanning, wide open reduction, internal fixation, immediate bone grafting and soft tissue handling have revolutionized the potential for restoring the pre-injury appearance and function of patients, sustaining pan-facial fractures. The facial buttresses remain the key to satisfactory reconstruction, a feature stressed by others in previous years, notably Sicher & Tandler (1928), Rowe & Killey (1955) and Merville (1974). The use of bone plating, coupled with a wide exposure of the buttress fracture sites will produce a rigid fixation but, as shown by Ellis and Walker (1996), absolute rigidity is not always consistent with optimum healing and can easily produce a malalignment of the dentition, a feature not usually seen where the correct establishment of the occlusion was one of the basic requirements for satisfactory restoration of function.
Drawing all these developments together, there has emerged a drive in the U.S.A. to establish major treatment centers capable of providing the full range of treatments for these patients. A similar move in the U.K. by the Royal College of Surgeons (2010) has recognized the value of such an approach but, in line with many European countries, recognized the local geography as well as the distribution of the population makes such centers impractical. However, a system of networking can provide the same type of clinical expertise.
Clinical pathology
Before 1960
It is virtually impossible, within the scope of this section, to provide a complete overview of the development of this branch of OMF surgery since the space allotted is limited. For this reason, a choice had to be made of those lesions that appear to occur with enough frequency to warrant a historical description. The authors acknowledge that this may lead to an arbitrary description of the course of events in clinical pathology and that some rare but interesting lesions are left out but the main aim is to emphasize particularly those topics that had a significant impact on the daily practice of surgeons.
At this stage, terms as we know them today, with regard to the pathology that may occur in the oral cavity and the jaws, were, for a large part, already known for more than a century. Particularly the etiology and pathogenesis of odontogenic cysts but also many odontogenic and non-odontogenic tumors were described in the period before World War II. For the sake of understanding the development in the periods to be described, it is necessary to go briefly over the early development, especially of cysts and odontogenic tumors.
It was the Frenchman Magitot (1872), who first recognized that all cysts of the jaws had to do with teeth: “tout kyste spontanité des machoires est de nature essentiellement et exclusivement dentaire.” He also coined the term “follicular cyst,” instead of dentigerous cyst, realizing that the cyst originated from the tooth follicle. The term dentigerous still exists today but only points towards the fact that a tooth is inside the cyst. Most importantly, however, he recognized the epithelial lining as an essential part of the lesion.
Before this time there were several theories of which the so-called “mesoblastic origin” prevailed, particularly in the Anglo-Saxon world. Malassez (1885) described the epithelial islands as found in the periodontium of teeth. He was at that time not aware of their origin, despite the fact that Hertwig (1874) had already discovered the epithelial sheath in amphibians that is essential for root formation. Malassez (1885) did, however, link his finding to the origin of radicular cysts, a name that he ascribed to Aguilhon de Sarran (1884). It was von Brunn (1874) who discovered the epithelial sheath in the developing human tooth, while Partsch (1892) finally formulated the presently accepted theory about radicular cysts that these cysts originate on the basis of epithelial proliferation in an apical granuloma.
This non-intentional French-German cooperation completely escaped the English-speaking world until Turner (1898) also discovered epithelial islands in the wall of cysts and disregarded the “mesoblastic origin” of
cysts. It illustrates again the ignorance that existed, mainly because of the language barrier and the handicap of not being able to communicate in one scientific language.
More importantly, it was also Partsch (1892), who came up with a rational treatment that is still currently valid. He advocated what we today would call marsupialisation and to keep the opening patent until the defect was shallow enough to allow for easy cleansing. In 1910, he recommended enucleation and primary closure for small cysts. Apart from these two odontogenic cysts other, rarer types were described over time; naso-labial (Klestadt, 1913), naso-palatine duct (Meyer, 1914), lateral periodontal (Bauer, 1927) and primordial (Kronfeld 1933).
The first attempt at classifying odontogenic cysts and tumors stems from Broca (1866). He also introduced the term odontoma, which was used later by several clinicians for various odontogenic tumors in a very confusing manner. For instance, Axhausen (1940) describes clearly an ameloblastic fibroma but calls it a soft tissue “odontoma.” The term “ameloblastoma,” instead of adamantinoma as it was called before, was suggested by Ivy and Churchill (1930). The term adamantinoma, however, suggests the presence of enamel and was, therefore, less desirable.
Thoma & Goldman (1946) finally presented the first useful classification based on a differentiation between epithelial, mesenchyemal and mixed tumors. They reserved the term “odontoma” for the types we presently know but also recognized soft tissue odontomas. In the course of time, many classifications would follow.
Most other tumors that occur in the mouth or jaws were described in books on general pathology, or were written up as case reports in various dental or surgical journals. A major turnaround came with the publication of the first edition of Thoma’s “Oral Pathology” (1941). In retrospect, one can only have the greatest admiration for this giant in both oral surgery and pathology alike. This very comprehensive text contained all diseases and pathological conditions of the mouth and jaws known at that time, including oral manifestations of metabolic and other general diseases.
Thoma had already written a book in 1934 entitled: “Clinical Pathology of the Jaws.” Born and educated in Switzerland, he understood both German and French, something that becomes very obvious when reading his texts as he frequently refers to German and French sources. In the introduction he writes: “This textbook on pathology not only covers the histological study of oral disease, but also endeavors to correlate the microscopic picture with the roentgen and clinical findings, thereby demonstrating the value of pathology as a vital part of clinical practice.” He was the right person to make this statement since he was unique in combining the two disciplines, which nobody
after him would ever be able to copy. His book had four editions during this period and served worldwide as the “bible” of oral pathology. In 1960, the fifth edition appeared written together with Goldman.

It is not surprising that oral pathology had its roots in the U.S.A. A whole generation of well-known oral pathologists was educated in the U.S.A. where this was a dental specialty from 1950. The Academy of Oral Pathologists was established in 1947. This academy was also one of the co-founders of the first journal on Oral Surgery, Oral Medicine and Oral Pathology in 1958, with Thoma as editor-in-chief. The first volumes of this journal are full of case reports of all sorts of pathological conditions, with an emphasis on cysts, tumors and other conditions that typically arise in the mouth and jaws.
Oral pathology was, thus, a well-organized and respected specialty in the U.S.A. with some outstanding clinicians who have contributed substantially to the current knowledge. Among them are Shafer, Hine and Levy, who published another classic text in 1958: “A Textbook of Oral Pathology.” This book was also upgraded and reworked over the years and eventually four editions appeared, the last one in 1983. A handy atlas that many surgeons had at reach when doing clinics was Bhaskar’s “Synopsis of Oral Pathology,” which first appeared in 1961 and had five subsequent updated editions.
Despite the American dominance in oral pathology, some European colleagues also made a significant contribution during this period. Particularly the group around Pindborg in Copenhagen, Denmark, who were very successful in discovering some novelties. Philipsen (1956) first used the term “Keratocyst” and described the typical histology in the Danish dental journal. Before that time, this cyst was often called a cholesteatoma.
Pindborg & Hansen (1963) first mention the high recurrence rate, up to 60 percent, of these cysts. This was soon followed in several European follow-up studies with a substantial number of cases (Panders & Hadders, 1969 and Browne, 1970). It is somewhat surprising, given the number of oral pathologists in the U.S.A., that it took approximately ten years before American studies appeared (Payne, 1972 and Donoff et al., 1972), showing the same tendency. Another novelty was the first description of the odontogenic calcifying tumor by Pindborg (1958), followed by the description of the calcifying odontogenic cyst by Gorlin et al. (1962). Lucas, finally, published the first British book on “Pathology of Tumours of the Oral Tissues” in 1964.
A key paper with great impact on the surgical management of ameloblastomas appeared in 1958. Small and Waldron recognized the infiltrative growth of ameloblastoma and as a consequence, advocated resection
of at least 1cm of healthy looking bone beyond the apparent radiological margins. This paradigm is still valid and followed by many surgeons today.
The publication of the first edition of “Syndromes of the Head and Neck” by Gorlin and Pindborg (1964) was an eye opener for most clinicians. It had an enormous impact on the day-to-day practice of many surgeons and made them realize that solitary findings in and around the oral cavity could be signs of systemic conditions. This book can be considered the beginning of the serious study of dysmorphology within the head and neck area.
1960–1990
During the next period many new discoveries were made and further refinement of the existing classifications of cysts and (odontogenic) tumors was carried out (Pindborg & Kramer, 1971). Since the clinical implications are particularly important, the discussion will be limited to those topics with implications for surgery.
Cysts of the jaw received much interest and several monographs appeared on this topic, with recommendations on their treatment (Killey & Kay, 1966, Shear, 1976). A German text, (Harnisch, 1971), completely ignores the findings of Gorlin and Pindborg and largely refers to old German literature, not paying much attention to the importance of the histology. The two items that were of clinical importance are the unicystic ameloblastoma and the odontogenic keratocyst simply because of their potential aggressiveness.
In a key paper, written by Vickers and Gorlin in 1970, they describe early histopathological features of neoplasma in cysts, unequivocally proving that ameloblastomas can originate from cysts. The term “unicystic ameloblastoma” stems from Robinson and Martinez (1977), who emphasized the differences from the solid or multicystic variant. Ackerman et al. (1988) reclassified this entity in three subtypes with diagnostic and therapeutic significance. Since that time, numerous studies have appeared that either are pro- or contra-aggressive treatment of these unicystic ameloblastomas. This dispute lasted throughout this whole period and would, more or less, be settled some 20 years later (Lau & Samman, 2006).
The story of the odontogenic keratocyst (OKC) is no less interesting or complex. Numerous retrospective studies also have appeared about this condition, focusing on the clinical, radiographic or histological features and, above all, showing a high recurrence rate varying from 10-60 percent
depending on the follow-up period and the way the followup was organized. Stoelinga (1971) and Stoelinga and Peters (1973) showed that the possibility existed for epithelial islands, located in the mucosa overlying these cysts and probably derived from the basal layer of the mucosa, to play a role in the origin and tendency for recurrence. The ultimate proof of this hypothesis would come in the next period. The multiple occurrences of OKC’s in the “Multiple Basal Cell Naevi Syndrome” (Gorlin & Goltz, 1960) also drew a lot of attention and many colleagues found that this syndrome is not rare at all.
One more lesion that deserves attention in this context is the “Central Giant Cell Granuloma” (CGCG). A key paper was written by Chuong et al. in 1985. They emphasized the difference between aggressive and non-aggressive lesions. In those days curettage or curettage with peripheral ostectomy was common practice (Eisenbrud et al., 1988). No mention was made of any recurring or aggressively growing lesion after therapy, as is currently known.
Two more editions (1976, 1990) of “Syndromes of the Head and Neck” appeared during this period with Gorlin as first author. Each new edition contained a considerable extension of new syndromes, which meant that the clinicians had access to the wealth of knowledge of these authors and their contributors.
Under the auspices of the World Health Organization (WHO), two publications appeared that were also of interest to the OMF Surgeon: “Histological Typing of Oral and Oropharyngeal Tumours” (1971), and “Odontogenic Tumours, Jaw Cysts and Allied Lesions” (1971). Both of these books contained up-to-date information of the growing knowledge about these lesions and subsequent editions, appearing in the next period, would attest to the increased insight into these conditions, largely gathered in this period. This is especially true for the non-neoplastic bone lesions such as, among others, cemento-osseo-fibrous dysplasia. The clinical implications, however, were somewhat limited because, for surgeons, the overriding factor is whether the tumor needs to be resected with a wide margin or whether enucleation is sufficient. One very relevant clinical change included the name change of “adenoameloblastoma” into “adenomatoid odontogenic tumor,” which put it in the benign non-aggressive category.
1990–2010
Further progress was made with regard to the understanding of the clinical presentation and pathological behavior of various tumors, both odontogenic and non-odontogenic, mainly through analysis of large case series. For instance, Reichart et al. (1995) presented a biological profile of 3,677 cases of ameloblastoma and revealed that more than
50 percent of recurrences occurred in the first five years postoperatively. Strong support was given for resection of these tumors with margins up to 2 cm into healthy bone by MacIntosh (1991) and Williams (1993).
Gortzak et al. (2006) however, on the basis of growth characteristics of large mandibular ameloblastomas, made a plea for a more conservative approach. They discovered that small tumor nests were found in the cancellous bone but none further away than 4 mm. They did not find any invasion into the subcutaneous tissues either and found the periosteum to be a good barrier. They also suggested, following the recommendation of Nakamura et al. (2001), saving the inferior alveolar nerve, where possible, since in none of their specimens was the nerve invaded, nor in the specimens from Nakamura et al.
A thorough overview of a large number of unicystic ameloblastomas was presented by Philipsen and Reichart (1997). They concluded that those cysts with intramural proliferations must be treated radically. The ongoing discussion on the preferred treatment of unicystic ameloblastoma was well illustrated in a paper from Lau & Samman (2006). Enucleation and treatment with Carnoy’s solution came out favorably in their systemic review, second best after resection but much better than enucleation alone. This was also the case with cysts with intramural proliferations reaching to the periphery of the cyst wall. Considering the morbidity that goes along with resections, in their opinion, the second option is to be preferred.
There were also some case series reported on rare but aggressive tumors, such as odontogenic myxoma, that give insight into the clinical presentation of these lesions (Simon et al., 2004). The other odontogenic tumors are extremely rare, apart from odontoma and usually completely benign. The most updated WHO classification is from 2005. This issue also contains a section on non-odontogenic tumors and bone-related lesions, with brief recommendations for treatment. Since most of these tumors are benign, simple excision is often the method of choice, the exception being the central giant cell granuloma (CGCG) and some aggressive fibrous dysplasias.
Various new approaches to the treatment of CGCG came to the surface during this period. It began with intralumin injections of corticosteroids (Jacoway et al., 1988), followed by calcitonin therapy (Harris, 1993). Both therapies appear to have limited value and are certainly not the solution in all cases (de Lange et al., 2006). Kaban et al. (2002) introduced the concept of inhibiting the angiogenesis in some aggressive CGCG’s by treating them with interferon alpha.
The cystic lesions of the jaws, still representing the bulk of the pathology seen in an OMFS practice, underwent a reclassification again as two new entities were incorporated;
the glandular odontogenic cyst (GOC) and the botryoid cyst. Both are to be considered aggressive in that they have a strong tendency to recur after simple enucleation or curettage. The GOC was described in 1987 by Padayachy and van Wyk but they used the term sialo-odontogenic cyst. Gardner et al. (1988) introduced the term “GOC” and that is the name used in the WHO classification from 1993. The term “botryoid cyst,” although mentioned by Weathers and Waldron (1973), came into fashion during the late 1980s, but reports of case series appear in the 1990s and later (Gurol et al.,1995 and Ramer & Valauri, 2005) This multilocular lesion has a strong predilection for the body of the mandible. In other words, the differential diagnosis of cysts had substantially expanded over the years, with important clinical implications.
The story of the OKCs came to a surprising apotheosis. An extensive report of all the recent research can be found in “Cysts of the Oral and Maxillofacial Regions” from Shear and Speight (2005). The WHO experts from 2005, as well as the authors of the aforementioned book acknowledge that the origin of some keratocysts is located in the overlying mucosa as a result of offshoots of the basal layer of the mucosal epithelium. This is in accordance with the theory as proposed by Stoelinga in 1971 and 1973 and repeatedly mentioned in subsequent studies.
A prospective study on 82 keratocysts revealed that the epithelial islands often found, were almost always located in the area where the cyst is connected with the mucosa (Stoelinga, 2001). This has serious implications for the surgical treatment of these lesions. Last but not least, the experts of the WHO renamed the lesion “Odontogenic Keratocystic Tumor,” which also correctly identifies the role of the epithelial clusters so often found in the wall of these cysts.
During this period, several new textbooks on oral and maxillofacial pathology appeared in many languages, among them Cawson et al. (1996). It is simply not possible to mention them all but it certainly reflects the importance of clinical pathology for the average OMF surgeon. An exception will be made for the book of Marx and Stern (2003), because it has the advantage that recommendations for the surgical management are emphasized. It was also provided to the participants of the 17th ICOMS in Bangalore as a gift from the organizing committee. What a generous gift it was!
In summary, clinical pathology underwent an enormous evolution and is probably still developing. The more we seem to understand, the more questions arise. The more

sophisticated techniques with which to investigate tumors and other lesions has led to a refinement in the diagnostic practice that 50 years ago was unthinkable. Yet, the words of Thoma (1941) are still valid; “surgeons need to have a thorough understanding of pathology in order to make rational decisions.”
Oncology
Before 1960
The early origins of the management of carcinoma of the head and neck follow much the same pattern as for other areas of the body, simply because of the lack of any obvious means with which to treat the disease. The lack of understanding of the pathophysiology and the spread of cancer was only resolved by the works of the early anatomists, as reviewed by Subramanian et al. (2006), notably Gaspar Asellius (1622), Antony Nuck (1692) and Paolo Mascagni, who published the first description of the lymphatic network in 1787.
A little later, several authors reported their studies on the functional anatomy of the lymphatic system. Astley Cooper (1840) reported the presence of breast cancer cells in the lymphatics, thereby demonstrating spread through these channels and Virchow (1860) showed that lymph nodes formed a barrier to arrest further dissemination of these cancer cells.
It was these studies that led Warren (1847) to perform an experimental dissection of carcinoma in the neck and Kocher (1880) excised a carcinoma of the tongue with an incontinuity dissection of the regional lymph nodes.
Butlin (1885), Jawdynski (1888) and Regulskiy (1894) all removed tumors and their associated lymphatics for oral carcinomas but the major breakthrough came in 1906 when Crile published his paper on the technique of radical neck dissection. Although the technique seems very similar to that of Jawdynski, the fact that it received much wider publicity meant that his ideas spread rapidly.
In essence, he believed that head and neck cancer was a local disease and, therefore, that each case should be curable by a complete excision. This theory was built on the observation that in less than one percent of cases was there any evidence of secondary cancer in distant organs. He believed, therefore, that the logical technique was that of a “block dissection” of the regional lymphatic system, as well as the primary lesion and that such a dissection was indicated whether the nodes were palpable or not. He also believed that the handling of the carcinomatous tissue should be strictly avoided as long as the lymphatic channels remained intact, thereby avoiding further dissemination of the growth.
The limits of Crile’s resections were: the clavicle, the strap muscles and the posterior border of sternocleidomastoid muscle. He removed the sternocleidomastoid muscle, the posterior belly of the digastric muscle, internal jugular vein and the accessory nerve, leaving the platysma intact. In this way, he believed that cases of carcinoma of the head and neck should yield better results than for any other portion of the body!
In parallel with these surgical developments, Röntgen (1895) discovered X-rays and Leopold Freund (1897) successfully treated a young girl with a superficial “naevus” by using them (Heilmann, 1996), while others reported similar success, notably with lupus. Initially, treatments focused on superficial lesions but by 1889, other sources of radiation, such as thorium and uranium as well as radium were recognized. The use of radiation to treat deeper tumors was some time in coming about and only in 1912 did Coutard, in France, develop treatment for head and neck tumors with fractionated, low-dose radiotherapy. He used one or two low-dose fractions per day, extended over at least two weeks and longer for larger tumors, which provided significantly less oedema and necrosis than with single-dose treatments (Jungling, 1924). This was the period when hyperfractionation was first discovered as well as the relationship between single-dose treatments and late complications.
The use of applicators which contained buried sources of radium, usually as needles, were also introduced at this time, largely for treatment of lesions of the cervix. These delivered beta particles, very effectively over shorter distances but lacking deeper penetration.
Progress between these early observations and 1960 was focused on the one hand on the use of radiation and how to use it to the greatest effect without causing excessive oedema and necrosis. On the other hand, the surgical approaches necessary to effectively eliminate the disease were balanced with the feasibility of successful restoration of function following excision of the primary lesion.
Both the radiotherapists and surgeons were involved in the evolution of training but, unfortunately, there was singular lack of exchange of results or ideas between them. The development of fractionation and rotational therapy were significant advances, yet both were surrounded by controversy. Wintz (1937) argued for single-dose therapy on the basis that the cells of the body were endowed with variable radio-sensitivity and capacity to recover from radiation damage, depending on their cellular metabolism. Furthermore, in a rapidly growing tumor, cells recover more rapidly than do adjacent connective tissue cells with their slower metabolism. Therefore, the difference in response will favor the tumor cells if the cancericidal dose is not given in the first instance.
Counter to this was the biological argument that in the same tumor, there would be cells of different sensitivity, depending on what stage of the division cycle in which they were found. For this reason, it was more logical to use smaller daily doses to catch the most advantageous time for irradiation. In 1924, the Roentgen was introduced as a unit and provided a major step in determining the exact dose of radiation.
By the 1930s, it became evident that high energy photons were advantageous in radiotherapy. The Siemens Company developed tubes capable of delivering up to 1000mV and gamma rays were used in radiotherapy, while the possible use of neutrons was first mentioned. Subsequently, the therapeutic use of these megavoltage machines was developed and in addition to the Betatron, linear accelerators were being built (Heilmann, 1996).
From the point of view of head and neck specialties, the introduction of electrons was important in developing techniques for focusing more precisely on the primary site than was feasible with gamma radiation. This fundamental development in treatment reduced oedema and necrosis significantly.
It was also during the 1950s that attention was turned to the possible use of chemotherapy. Unfortunately, solid tumors of the region were found to be resistant to each of the commonly used agents. Nevertheless, there was a strong belief that this form of therapy would find a solution to the systemic management of cancer and research into their use persisted. It took a further decade before methotrexate and, subsequently, bleomycin, were seen to have beneficial effect, particularly on premalignant, superficial lesions.
In an attempt to flood the tumors with higher doses of the therapeutic agents, intra-arterial regional perfusion was attempted, similar to that tried in the limbs for the treatment of melanomas. Unfortunately, this was unsuccessful and simply produced a series of patients with green faces caused by the methylene blue dye used to define the anatomical area supplied by the artery involved!
The parallel surgical developments during this time are best reviewed from the point of view of the regional lymphatics and the primary lesion. It is true to say that surgical reconstruction of orofacial defects was very much in its infancy and the available techniques were more appropriate for traumatic or congenital defects than for those produced by cancer surgery.
During this time, however, surgery to the neck nodes made significant progress. The standard, set by Crile, served until 1951 when Hayes Martin contended that a routine prophylactic radical neck dissection was not practical in the management of cancer of the tongue and lips (Carlson et al., 2006). This was drawn from an extensive review of almost 1,500 radical neck dissections carried out between
1928 and 1950; his statistics being drawn from some 655 operations on 599 patients. He concluded that prophylactic radical neck dissection was illogical and unacceptable for cancer of the oral cavity. He also contended that no one could carry out prophylactic radical neck dissections to a degree sufficient to effect significant improvements in cure rate; the radical neck dissection was too radical a technique for the N0 neck.
This paved the way for the development of several modifications of the radical neck dissection which, while retaining oncological safety, reduced the significant morbidity which was so prevalent with the radical procedure. These modifications sought to retain the sternocleidomastoid muscle, spinal accessory nerve and internal jugular vein or at least one or two of those vital structures.
Surgical reconstruction of primary lesions during this same period was still very limited to simple bone grafting and the use of split skin grafts. The techniques of soft tissue transfer were being developed but it was really in the period after 1960 that so much change occurred.
Although salivary gland tumors were recognized long before 1960, their pathophysiology was poorly understood and consequently, their clinical management was inadequate. Broca (1866) assumed that the most common tumor of the salivary glands was of a mixed epithelial and mesenchymal origin. This long-standing assumption continued with clinicians and pathologists alike until halfway through the 20th century. This lack of understanding can be explained on the basis that these tumors are relatively rare and often treated by clinicians from different disciplines. Consequently, it was some time before sufficient cases existed as a series from which conclusions could be drawn.
One of the earliest authorities in this area was Rauch (1959), who published his experience of some 4,245 cases of pleomorphic adenomas, clearly stating that this was an epithelial tumor presenting with a variety of histological patterns. Surgery of the salivary glands at this time tended to be reported in an anecdotal fashion and benign tumors, including pleomorphic adenomas, were enucleated or treated with a wedge excision.
It is obvious that clinicians struggled with the assumed multifocal presentation of pleomorphic adenomas, since high recurrence rates were published, as was illustrated in papers by McFarland (1941,1943), who recommended radiotherapy for these tumors, since the high recurrence rates were attributed to their multifocal character. The approach changed with the results presented by Bailey (1941), who emphasized the need to remove the whole superficial lobe of the parotid with preservation of the facial nerve. This set the standard for years to come, with surgery and radiotherapy being advocated. Even so, the
recurrence rate was still 15 percent (Corcoran et al., 1983). These same authors proposed the use of radiotherapy followed by surgery for all parotid tumors but their survival rate was only 30 percent (Gallegos et al., 1991). 1960–1990
The significant improvements in the treatment of cancer of the mouth and associated structures, as seen during this period, are well recorded by Loré (1962) as well as in his subsequent books. This theme was taken up by Soutar and Tiwari (1994), who demonstrated not only the value of systematic excision but also the use of osseomyocutaneous flaps in reconstruction.
In the U.S.A., the importance of specialization was seen at the Memorial Sloan-Kettering Cancer Center, where Shah collated their results in his publications (1996).
During this period, through several review articles and monographs, the specific pathology of salivary gland tumors became much better understood, particularly with reference to the pseudo-encapsulation of the pleomorphic adenoma (Eneroth, 1964, 1971, Thackray, 1972, 1974). This in turn led to a rational approach to parotid and other major salivary gland tumors, as well as to those of the minor salivary glands which, although much less common, were more frequently malignant when they did occur.
Removal of the superficial lobe of the parotid was standard treatment, the facial nerve being preserved. Frozen sections were recommended for appropriate diagnosis on the spot and if necessary, the deep lobe was removed when the tumor was found to be located within it. Malignant tumors were often treated with additional neck dissection and/or radiotherapy (Rankow & Polayes, 1976). Tumors of the submandibular and sublingual glands were approached with great caution because of their propensity to be malignant lesions. Rankow and Polayes recommended complete removal of these glands with preservation of the lingual and hypoglossal nerves, resulting in excision biopsies, to avoid the seeding of malignant cells into the wound bed.
The work of Thackray et al. (1972, 1974) laid the foundation for all classifications of these tumors in the years to come. This included all the benign as well as all of the malignant tumors, including the well-known adenoid cystic and adeno-carcinomas, together with the mucoepidermoid tumors and the great variety of histologically different tumors that may occur in both the major and minor salivary glands, with differing prognoses that tended to confuse the clinician.
The first tissue flaps to be used extensively were those classified as axial pattern flaps, marked by having their own arterial blood supply and, in use, they were transposition flaps, which meant dependence on this blood supply until
vessels grew in from the periphery. It is not the purpose of this book neither to evaluate each variety nor to explore the full scope but some of the commonly used ones are worthy of mention because of their position in the specialty’s evolution. The first and most commonly used flap was the lateral forehead flap, based on the anterior branch of the superficial temporal artery, which forms a midline corkscrew anastomosis with the matching artery on the opposite side. This allowed use of the entire forehead skin, from one zygomatic arch to the other. The donor site was made good with a thick split skin graft. This was a true “workhorse” flap of that period, which, in addition to surface coverage use, could readily be inserted intraorally for lining use or doubled on itself to provide both.
The second major flap was the deltopectoral flap, developed by Bakamjian and Poole (1977). Based on the perforating vessels of the internal mammary artery. This large and versatile flap could be extended out to the shoulder, providing a large amount of tissue for closure of extensive defects but, additionally, it could also be folded on itself to provide lining as well as coverage for through and through defects.
Further axial pattern, transpositional flaps were developed, notably the pectorals major myocutaneous flap, based on the thoracoacromial branches of the axillary vessels, the latissimus dorsi flap which, as well as being supplied by the thoracodorsal branches of the subscapular vessels, also received multiple vascular pedicles on its deeper surface. This flap could also include a pedicled muscle and bone flap of serratus anterior and subjacent rib, which could be used to reconstruct the mandible.
Finally, where facilities and expertise existed for major reconstruction, microvascular anastomoses allowed for the development of free flaps, the first and most important of which was the radial forearm free flap (known as the Chinese flap), Yang et al. (1981) This flap has been extensively used, including the split radius to reconstruct lost parts of the mandible (Vaughan,1990). It still has its place in reconstructive surgery but other types of flaps have largely replaced its use.
Although many have been described, those most used include the latissimus dorsi flap (Bailey & Godfrey, 1982); the dorsalis pedis flap with its long pedicle of larger vessels (McLeod & Robinson, 1982); the SCIA groin flap (O’Brien et al.,1979), based on the superficial circumflex iliac vessels and the DCIA flap, based on the deep circumflex iliac vessels and providing a compound bone and skin flap with a long vascular pedicle (Saunders & Mayou, 1979, Taylor & Townend, 1979). Where bone grafting was not indicated, a titanium implant could be fitted to the lingual aspect of the mandible to retain its overall shape (Bowerman & Conroy, 1969).
It is timely to reflect on surgery to the neck nodes during this period. Bocca and Pignatano (1967) published their work on a more conservative functional neck dissection, where only the lymphatic tissue of the neck was removed, rendering it a more appropriate operation for the N0 neck. Recurrence rates for these dissections, both for N0 and neck positive patients were low at 8.1 percent and Calearo and Teatino (1983) achieved 3.5 percent, thereby justifying such a treatment as against the radical neck dissection for these patients.
Research by Woolgar (1988) demonstrated that upon serial sectioning of material from block dissection specimens, micro-metastases could be demonstrated in previously described, pathologically negative specimens. Furthermore, there could be “skip” areas between such deposits.
In 1991, Robbins et al. recommended a standardized classification of all neck dissections, dividing the neck into levels I–V depending on the anatomical location of the nodes. This facilitated discussion on management as well as pathology. The supra-omohyoid neck dissection had attracted attention as a possible means for staging in the management of the N0 neck associated with oral carcinomas. This involves removal of levels I–III of the lymph nodes, preserving the other structures, but it is no replacement for elective neck dissection, although it does help to address the issue of occult disease.
What was ascertained in this period was the need for combining techniques but in that process, never to compromise the full therapy of one mode in the mistaken belief that two types of treatment reinforced one another and hence, demanded less than the full regime of either. For the majority of head and neck lesions, surgery and radiotherapy produce the standard against which any alternatives should be measured.
1990–2010
The improved histopathological investigation of neck dissection specimens demonstrated by Woolgar (1997, 1999) came in association with what might be seen as the next era and be referred to as “super-selective neck dissection.” This approach, originally developed for melanoma patients, specifically analyses lymphoscintigraphy guided biopsies of sentinel nodes. Meticulous examination of these specimens showed that even microscopic extracapsular spread had a profound influence on the progress of the disease and such detail is likely to be mandatory if progress is to be made. Immunohistochemical analysis has been shown to be a feasible way of examining this pathological material, as have other molecular techniques. Elsheikh et al. (2006) concluded that molecular analysis is exquisitely sensitive in detecting very small cancer deposits within lymph nodes.
With the emphasis on unraveling of the sequences of the human genome, it was to be hoped that new avenues of treatment might be open to the management of oral squamous cell carcinoma. Unfortunately, the genome of oral cancer has proven to be extremely complicated. Progress along this route is consequently much slower than had been hoped (Fernandez, 2011).
Surgically, the potential for the development of endoscopic neck dissection has been demonstrated clinically by Weiner et al. (2004) but it will take some time before the oncological value of such an approach can be assessed.
When it comes to the primary lesion, the experience gained with the use of microvascular surgery has led to the use of various flaps with successful incorporation of bone grafts, suitable for the placement of implants, both for the mandible and maxilla (Urken et al., 1997, Chan et al.,1997, Bak et al., 2010, Bianchi et al., 2010). Whether this has led to a higher patient satisfaction, however, remains to be seen (Schliephake & Jamil, 2002).
As a consequence of the enormous success of microvascular grafts for the reconstruction, particularly of lost parts of the face, the first successful human allograft of facial tissue, for replacement of cheeks and lips, was carried out by Devauchelle et al. (2005). Further developments in tissue transfer include the use of double flaps for extended composite defects, particularly of the chin area (Gaggl et al., 2007). Tissue engineering, of course, holds promise, but has certainly not achieved a stage where it will replace currently used methods (Terheyden et al., 2004, Warnke et al., 2006, Suuronen, 2010).
The WHO Classification of salivary gland tumors (Eveson et al., 2005) has further refined the terminology within these neoplasms. In clinical practice, only five salivary gland carcinomas are likely to be encountered (Speight & Barrett, 2009). These authors also considered clinical staging, histological grading and perineural invasion important prognostic factors in malignant salivary gland tumors, pointing out that T1 and T2 tumors less than 4cm in size generally do well, regardless of other features.
Fine needle aspiration biopsies and cytology have been used, but the variability of histology within a single tumor makes this an unreliable diagnostic test. This is controversial with the American Head and Neck Society recommending that it is only useful where the tumor is likely to be metastatic in nature, while the Scottish Intercollegiate Guidelines recommend that it should always be used. As a result, Kieran et al. (2010) concluded that FNA should be performed on all those aged 60 years or over. Where it is practiced, success depends on the establishment of a very close working relationship between surgeon and pathologist, who must also be an experienced cytologist.
In their study of salivary gland cancer in younger patients, Rutt et al. (2011) found mucoepidermoid carcinomas to be those most frequently encountered but in young adults this changes to adenoidcystic carcinomas and there is a female predominance (Chomette et al., 1982). Ryan et al. (2010) noted that patients who received radiation therapy for these lesions were more likely to suffer a recurrence and Jenson et al. (2010) found that control using conventional radiotherapy required a very high dose and consequently favored the use of intensity modulated radiation therapy (IMRT) to achieve better local control. IMRT also avoids high dose radiation in areas where implants are to be inserted, particularly in the symphyseal area of the mandible and is preferably used for oropharyngeal cancer. (Lee et al., 2007, Verdonck et al., 2010).
In a randomized controlled trial of IMRT versus conventional radiotherapy, Nutting et al. (2011) showed that sparing the parotid glands with IMRT significantly reduced the incidence of xerostomia and leads to recovery of salivary secretion and improvements in associated quality of life. This strongly supports a role for IMRT in squamous cell carcinoma of the head and neck. Cryotherapy with liquid nitrogen is also effective because of the propensity for some salivary gland tumors to spread along tissue planes, which also explains why poorly focused radiotherapy is not always the most effective mode of treatment. Even with intense freezing, the neural sheaths remain intact and regeneration of neural tissue is, therefore, possible.
Looking at parotid squamous cell carcinoma, Bhide et al. (2009) noted that in general, five year loco-regional control was better for patients who had definitive surgery and post-operative radiotherapy (82 percent compared to 21 percent for those who had radiotherapy alone).
However, analysis of publications by Brown (2011) on the survival data for oral squamous cell carcinoma, covering 7,786 patients, throws doubt on the value of post-operative radiotherapy, especially when the increased morbidity associated with this therapy is taken into account. He makes a plea, which has frequently been made by others, for prospective randomized trials and better audit of outcome data.
One of the most important trends is the regular involvement of multidisciplinary teams in the management of head and neck oncology patients, meeting together and making joint decisions on the best course of treatment for each individual. This extends to outcome audit and Quality of Life Assessment (Rogers et al., 1999). Internationally agreed outcome parameters are, however, necessary to be able to compare results (Rogers et al., 2010)
This whole development has proved to be a very long road and yet despite this, the survival rates for head and neck cancer remain stubbornly unchanged. Consequently,
there remains much work still to be done, which includes a re-examination of long held dogmas on protocols and management of this disease.
Preprosthetic surgery
Before 1960
Some of the techniques used in preprosthetic surgery were developed before but mostly just after World War II in the German-speaking part of Europe. The split skin graft was described by Thiersch in 1874. It is, therefore, somewhat surprising that the real spread of preprosthetic surgery only took place in the 1970s. This had largely to do with the earlier mentioned language barrier that existed between the Anglo-Saxon world and continental Europe where German used to be the most important language for medical publications. There simply was very little crossover or exchange of information until about half way through the 1960s, when the influence of the journals became apparent.
This is borne out by the description of simple preprosthetic measures in most American textbooks during this period which only mention procedures such as: alveoloplasties to remove bony irregularities or correct alveolar prognathism, and vestibuloplasties followed by secondary epithelialization and other rather minor procedures.
Techniques such as vestibuloplasties with lowering of the floor of the mouth and split skin grafting evolved over the years through the input of several pioneers in the German-speaking area but were almost unnoticed on the other side of the Atlantic (Pichler & Trauner, 1930, Trauner, 1952, Schuchardt 1952, Rehrman, 1953, Obwegeser, 1963). Axhausen (1940) shows in his book an excellent example of a vestibuloplasty at the anterior mandible covered with a skin graft. A detailed description of the history of the development of these techniques is described by Davis and Davis in the book of Fonseca and Davis (1986).
The only novelty in this area, stemming from the U.S.A., is the description of the lip switch technique by Kazanjian (1924). He also described in the same paper a technique for increasing the depth of the anterior lingual fold. The lip switch was later modified by Edlan and Mejchar (1963). Worth mentioning also is the mylohyoid ridge reduction technique without grafting, as described almost simultaneously by Brown (1953) and Downton (1953) and independently by Caldwell in 1955. The latter
demonstrated that some Americans, at that time, did not even read British publications.
Preprosthetic surgery in the maxilla was almost exclusively limited to alveoloplasties until Celesnik (1954) introduced the tuberoplasty and Obwegeser (1959), the submucous vestibuloplasty, although Schuchardt (1952) had already described the vestibuloplasty in the maxilla, covered by split skin grafts.
Bone augmentations using bone grafts or alloplastic material were not performed during this period, except for a German pioneer, Clementschisch (1948), who described autogenous rib onlay grafts to augment atrophic mandibles.

The real breakthrough came after the publication of the paper of MacIntosh and Obwegeser in 1963. Obwegeser had also presented his work on maxillary vestibuloplasties at the first ICOS in London in 1962. Preprosthetic surgery was to take off in the years to come, not only in the U.S.A. but also in other, non-German-speaking countries. 1960–1990
The rapid spread of preprosthetic surgery during this period had probably, not only to do with the introduction of new techniques, but also with the growing affluence of the developed world. This certainly was elective surgery, meant for a group of patients who had lost their teeth at a fairly early age. For a large part, this was the result of poor dental care, which was not the highest priority in times of war or the immediate post-war period. In other words, there was a large contingent of people who were potential candidates for this type of surgery.
There were four new developments during this period that had an enormous impact. The first was the introduction of the mucosal graft as suggested by Propper (1964) and later popularized by Steinhauser (1969) and Tideman (1972). The use of mucosal grafts circumvented the need for taking skin grafts, with its inherent and unavoidable donor site morbidity and visible scar formation. The area to be grafted was smaller than was possible with skin but this was turned into an advantage, because in this way less damage was done to the mental nerves.
Follow-up studies on vestibuloplasties pointed toward a lack of appreciation of a numb lip and chin as a result of freeing of the mental nerve (de Koomen, 1977). Patients’ appreciation improved substantially when care was taken, not to extend the graft beyond the mental foramen (Huybers et al. 1985). In general, the two major disadvantages of these vestibuloplasties, including nerve dysaethesias and sagging chins, could be avoided by careful planning and limiting the extent of the surgery (Stoelinga, 1992).
The second introduction was the absolute heightening of the severely atrophic mandible and maxilla. The pioneers were Härle (1975) and Schettler (1976), who independently
developed the visor and sandwich osteotomies. It is only fair to mention here that Barros Saint-Pasteur had already described a sandwich technique in 1966. This was an important improvement over the rib onlay technique (Terry et al., 1974), which, again in a follow-up study, had been shown to be highly unreliable in that rapid resorption occurred, almost to 100 percent, in a matter of two years (Fazili et al., 1978). The two techniques were further refined by various clinicians and widely used over a 20-year period.
Although these methods were much better than the onlay technique, there were also drawbacks, such as nerve dysesthesias and unwanted resorption under a mucosally borne denture (Stoelinga et al. 1983). For the maxilla, the sandwich principle resulted in a Le Fort I osteotomy with interposed grafting, bringing the maxilla downward and forward (Bell et al., 1977). This principle stood the test of time, since it is currently still used when implants are planned for severely resorbed maxillae.
The third development concerned the introduction of hydroxylapatite in both a solid as well as particulate form. It was the particulate form that caught the attention of the profession, since it had the potential to augment the jaws in a stable fashion, since resorption was not very likely (Kent et al., 1982). Mixing it with particulate autogenous bone made it an ideal graft material, because the hydroxylapatite grains acted as a scaffold, preventing graft resorption (Fonseca 1986). In a follow-up study this was proven, in that very little resorption was observed after the first year, in the areas posterior to the mental foramina, where the mixture was deposited. (Satow et al. 1997).The main drawback was the difficulty both in application and containment of the particles, whereas additionally mucositis tended to occur because of the thin mucosa overlying the layer of hydroxylapatite. This, of course, was not a problem when it was used to fill a flabby ridge in the maxilla (Terry, 1983).
The fourth introduction that really brought about a revolution into preprosthetic surgery was, of course, the titanium implants of Brånemark et al. (1977). Before this time several implants had been tried, including subperiosteal implants made of chrome-cobaltmolybdenum alloys, implants that were screwed into the jaws and so called blade implants. They all failed, sooner or later, since the materials used were not biocompatible as was titanium, or better to say titanium oxide and also allowed downgrowth of epithelium, which resulted in extrusion. Brånemark and his group coined the term osseointegration which meant that the bone really attached
to the surface of the implants, which was the major breakthrough in the application of implants in general.
The publication of Adell et al. in 1981 opened the eyes of many clinicians and from then on implant dentistry developed. In retrospect, it is somewhat amazing that it took so long before the profession and dentistry as a whole jumped at this opportunity. This probably had to do with a hesitation that was fed by the frustrating experiences associated with older types of implants. The major developments with regard to implant surgery and preimplant surgery in particular, took place in the next period.
In this period several monographs solidly devoted to preprosthetic surgery appeared, illustrating the enormous popularity this branch of surgery had achieved (Starshak & Sanders, 1980, Fonseca & Davis, 1986, Hopkins, 1987, Härle, 1987). The publication of these books was preceded by a publication of a Consensus Conference, organized by the IAOMS in 1983 in Berlin (Stoelinga, 1984). This was a unique event, because the prosthodontists, who looked critically at the results that surgeons tended to present in a more positive way, were also present.
From this event biennial conferences evolved where surgeons and prosthodontists came together to discuss matters of mutual interest, resulting in consensus statements, published in the International Journal. This conference took place alternately in the U.S.A. and Europe and lasted until 2008.

A publication that has had a significant impact on the way of thinking in reconstructive preprosthetic and pre-implant surgery alike was presented by Cawood and Howell (1988). They proposed a classification of resorption patterns, based on studies of dry skulls. This classification is, at present, the gold standard when discussing treatment options for patients who are candidates for pre-implant surgery, because it facilitates the interdisciplinary cooperation, using a terminology that is universally understood. Before that time, terms such as knife-edge ridge or severe resorption etc. were used, leaving much to the imagination of the readers.
1990–2010
It is fair to mention that, by now, conventional preprosthetic surgery had almost ceased to exist. It had become apparent that the term “reconstructive preprosthetic surgery” had to be replaced by “pre-implant surgery,” because implants had changed the scene profoundly. Yet the techniques, as employed in the previous period, served as the basis for modern pre-implant surgery. This is well described by Cawood et al. (2007).
The profession had become heavily involved in implant dentistry and so had several other dental disciplines. The number of implant systems had exploded
and various improvements were also introduced, making implant dentistry a reliable and popular adjunct in the armamentarium of the dental profession. Implant dentistry has made it possible to truly rehabilitate the edentulous and partially dentate patient to an extent that hitherto was unthinkable.
Pre-implant surgery, however, still has a place because enough bone volume needs to be present in the strategic areas where implants are planned to be inserted. For this reason, sinus floor augmentation was soon introduced by Boyne and James (1980) and Tatum (1986), but only widely applied in the 1990s and at the present time. A modified Le Fort I osteotomy with bone grafts in the floor of the sinus and nasal aperture and simultaneous implant insertion was proposed by Sailer (1989). This was soon followed and modified by several others.
The increased knowledge about the healing of bone grafts has contributed significantly to the success of various grafting techniques. It is particularly the reports of the Swiss-Austrian working group on the healing of fractures (Arbeitsgemeinschaft für Osteosynthesen Frage), that improved the understanding of this healing process. They introduced the concept of primary fracture healing as a result of rigid fixation. It was Spiessl (1969) who introduced this principle in oral and maxillofacial surgery. This concept is currently widely used in trauma surgery but it also applies, to a certain extent, to the healing of bone grafts, in that rigid fixation is mandatory for these grafts to take. The grafted bone heals by creeping substitution, which implies that all grafted bone resorbs but will be replaced by new bone (Fonseca et al., 1980).
This explains why onlay grafting with corticocancellous blocks became successful, provided rigid fixation is present, be it through implants or plates and screws. Several techniques have recently been described for augmenting alveolar ridges with cortico-cancellous block grafts, either simultaneously with the insertion of implants or as a single procedure, followed by implant placement at a later stage.
Another technique for increasing bone volume, in limited sized defects, was introduced by Buser et al. (1990). They favor the use of guided tissue regeneration using a membrane to protect the graft from ingrowth of fibroblasts. This technique also has many followers and seems to serve its purpose in selected cases.
Last, but not least, a true “hype” has crept into this branch of the profession called “distraction osteogenesis.” Several preliminary results have been presented on the results of augmentation of the symphysis of the mandible and even local augmentation of the deficient alveolar process. As promising as the results may appear, until
now little evidence exists that this technique will provide better and more reliable results than bone onlay grafting and it is questionable whether the method, in general, is more patient friendly, considering the cumbersome device that has to be inserted. There are, however, certain indications where this technique may prevail.
Unlike, for instance, orthognathic surgery, little evidence-based practice is employed in pre-implant surgery (Blackburn, et al. 2008). The literature is replete with recommendations based on case series or, at best, follow-up studies with limited value because of insufficient followup or other confounding factors. Properly designed and prospectively carried out studies are rare and, thus, solid conclusions cannot easily be drawn.
Surgery of the temporomandibular joint
Before 1960 Surgery of the temporomandibular joint (TMJ) has a relatively long history. Both American and German literature contain early reports of treatment of ankylosed joints in the second half of the 19th century but according to Merrill (1986), the first surgery described in English literature concerns a condylectomy for a patient with arthritis, carried out by Humphrey of Cambridge, England, in 1856.
In those days, before antimicrobial treatment was available, inflammatory diseases affected the joints more often than is currently seen and even specific infections, such as gonorrhea, were not uncommon (Axhausen, 1940 and Thoma, 1948). This would sometimes result in ankylosis and require a surgical intervention to allow the patient to function again. Ankylosis was, thus, far more frequently seen than is the case today, at least in the developed world. The treatment ranged from various ostectomies in the ascending ramus to allow for free movement of the main body of the jaw with or without interposition of alloplastic material and true condylectomies.
A detailed description of all these techniques written by German- and English-speaking colleagues is to be found in the book of Hoffmann-Axthelm (1995). A chapter written by Stiebitz summarizes all techniques known until 1950. Apart from ankylosis and arthritis, conditions that are currently called internal derangements were already known in the late 1800s and sometimes surgically treated with rather drastic means. The chapter in the first edition of Thoma’s “Oral Surgery” describes all possible procedures that were performed in those days (Thoma, 1948).
It strikes the reader that few new procedures have been introduced since then, apart from some technical advances in both instruments and implants. Fundamentally, however, the procedures described have hardly changed.
What has changed, however, are the means of establishing a proper diagnosis and the better understanding of the pathology of some of the conditions involved.
Annandale (1887) is generally credited with the first surgical reposition of displaced disks, whereas Lanz (1909) first described a meniscectomy for a painful joint, followed by many other authors. Even condylectomy was suggested by Ireland (1951) to treat a “clicking jaw.” It is not particularly clear who described the first joint transplantation but in the book of Klapp and Schröder (1917), several case reports are described of metatarsal joint transplantations to restore function in patients who had lost their joint and ascending ramus because of gunshots. This was long before Dingman and Grabb (1966) introduced this technique in the English literature. It was Axhausen (1933) who described the first case of chondromatosis of the TMJ.
The understanding of the pathophysiology of a painful joint received a great boost by the publication of Costen (1934) in which he pointed out the importance of dental occlusion and vertical dimension. The term “TMJ pain dysfunction syndrome,” however, stems from Schwartz (1956) He emphasized that the pain was often located in the masticatory muscles. His theory dominated the thoughts about the pathophysiology of TMJ dysfunction for almost 20 years. Drastic surgery for TMJ dysfunction became less popular and was replaced by more subtle procedures, such as high condylectomy (Baldridge & Henny 1957) and eminectomy (Myrhaug, 1951 and Irby, 1957).
A novel technique to treat chronic dislocating joints was introduced by LeClerc and Girard (1943) and later refined by Deautrey (1974). It entailed down fracturing of the zygomatic arch as to prevent dislocation of the condyle out of the fossa. An alternative technique had been used by Sutton Tayler since the late 1950’s, which involved simple subperiosteal bone graft augmentation of the articular eminence (Williams, personal communication).
The dental profession and particularly the prosthodontists, however, began to show interest in the non-surgical treatment of the pain dysfunction syndrome, which also contributed to a more conservative approach for a while. By the end of this period, TMJ surgery was carried out for ankylosis, arthritis, chronic dislocations and what was then called a painful joint not responding to conservative treatment. Refinement of the diagnosis of TMJ dysfunction was advanced during the next periods. 1960–1990
The treatment of ankylosis followed the patterns as laid out in the preceding period. Gap arthroplasties, with or without interposition of autogenous grafts, i.e. dermis, muscles or alloplastic material e.g. silastic, were still the gold standard. Large studies are lacking but there are plenty
of case reports and small case series that recommend these procedures. Textbooks which were published in this period also favor these techniques.
The same is true for the treatment of chronic dislocations of the TMJ. Both eminectomies and down fracturing of the zygomatic arch were successfully carried out. Several case series attested to the validity of these techniques.
Surgery for tumors and conditions, such as chondromatosis and synovial cysts, is also reported in this period, where the usual pre-auricular approach is utilized. These conditions often went unnoticed for several years because diagnostic means were lacking until the introduction of magnetic resonance imaging (MRI).
An important development in these years is the introduction of growth center transplants using rib grafts. It soon became obvious that costochondral grafts were the best choice to adapt to the mandibular growth pattern. The intention was to insert a graft with the potential to grow with the individual (Ware & Taylor, 1965, Ware, 1966). This was taken on by many surgeons as a means for treating children with asymmetric growth because of ankylosed joints, or who suffered from hemifacial microsomia (MacIntosh & Henny, 1977, Rowe, 1982, Mulliken et al., 1989). It also became clear that these grafts were still somewhat unpredictable as undergrowth as well as overgrowth occurred at times.
Contrary to the concept of replacing the condyle with an autogenous graft, the idea of an alloplastic joint prosthesis was put forward by several authors in the 1960s and 1970s, among them the most popular from Christensen (1971) and Kent et al. (1983). They were mainly used to replace the condyle in cases of ankylosis, or after resections for tumors, although so-called reconstructions, including fossa and condyle, were advocated after failed, multiple attempts to surgically treat degenerative arthritis.
An excellent and complete account of these early developments is presented by Driemel et al. (2009). They describe the developments in the English, German and French speaking areas, including the serious problems that were associated with the Vitek® joint systems that had such a negative impact on the further introduction and development of alternative systems for quite a while.
The term “pain dysfunction syndrome” was slightly modified to “myofascial pain dysfunction syndrome” as suggested by Laskin (1969) with an emphasis on the psycho-physiological factors that contributed to the muscle pain. This concept had to be revised, however, when new imaging techniques were introduced that made the relation between the disc and condylar head visible. It concerned arthrograms and later MRI. As a result, the term “internal derangement” was introduced (Farrar & McCarty, 1979).
The definition is defined differently by various authors but basically it refers to a condition whereby the disc is not in its proper anatomical position, either at closed and/or open position of the mandible and most often anteriorly displaced. It caused a new wave in open TMJ surgery, particularly in the U.S.A., with procedures such as repositioning of the anteriorly displaced disc with simultaneous reduction of the elongated posterior ligament (McCarty & Farrar, 1979) and disc removal with or without replacement with an autogenous graft, i.e. cartilage (Hall & Link,1989) or alloplastic material, i.e. silastic sheets (Wilkes, 1991).
The long-term results of all these procedures were not unequivocally positive, although Wilkes (1991) claimed successes of over 90 percent in a long-term retrospective study. It is of interest to note that another technique for treating a painful joint, as suggested by Ward (1961), went almost unnoticed. It entailed a condylotomy carried out
1990–2010
The debate about whether an autogenous graft or alloplastic joint replacement is preferable for cases of ankylosis in adult patients, or otherwise severely deformed joints, went on. The introduction of CAD-CAM produced models, on which custom-made prosthesis could be made, had brought about a revolution when considering major joint reconstruction. The idea of an alloplastic joint prosthesis came from the successful application of these prostheses in orthopedic surgery. The review, as presented by Driemel et al. (2009), provides a complete overview of the development of these devices since 1950. The three major players in this area are the TMJ Concept® prostheses, that have a reasonable track record (Mercuri 1998), TMJ implant ® to which the name of Christensen is attached (1971) and the Biomet ® total TMJ prosthesis. The latter is not custom made but consists of fixed sizes and shapes that are available off the shelf.
with a Gigli saw in a blind fashion. The idea was to shorten the ramus with minimal change of the position of the condylar head. Banks and MacKenzie (1975), however, reported good results on a group of 211 patients treated over a rather long period.
An authoritative and complete review of the then existing techniques is presented by Merrill (1986). He admits that surgery of the TMJ is rapidly changing. This was largely because of the better understanding of the pathophysiology and better imaging methods. (Bronstein et al. 1981, De Bont et al. 1986, Holmlund & Hellsing 1989)
Another novelty concerned the introduction of the arthroscope for examination of the TMJ (Onishi 1975). This application enabled surgeons to examine the joint spaces and to eliminate adhesions so as to improve mobility of the disc. There were also surgeons who claimed that disc repositioning was possible using an arthroscopic approach (Murakami & Takatoki, 1986, Moses & Poker, 1989, McCain et al., 1992).The sheer number of patients treated makes one wonder what the criteria were that made these surgeons decide to do this kind of surgery.
Westermark (2010) presented a long-term follow-up on these, reporting good results after a maximum of eight years. Guarda-Nardini et al. (2008) concluded, after a study of the pertinent literature over a period of 16 years, that the findings on all three systems were promising but that multi-center trials are necessary, taking into account inter-operator variability. Contrary to the proponents of alloplastic prostheses, several colleagues still favor the use of an autogenous graft, mainly costochondral in nature, to replace a condyle and part of the ascending ramus (Perrot et al., 1994, Peterson et al., 1998, Zhi et al. 2009). Yet, comparative studies reveal a tendency for re-ankylosis in some patients (Saeed et al., 2002).
Dimitroulis (2005), however, rightly made the point that alloplastic TMJ prostheses tend to be placed in relatively young patients, as compared to hip and knee prostheses. The life expectancy of these patients is in the order of 30 to 40 years instead of 10 to 15 years, as is often the case for patients with hip and knee prostheses. It remains to be seen, therefore, whether these TMJ prostheses will stand the test of time, or whether placement of a new prosthesis will be necessary over the years. The treatment of ankylosis in growing individuals still remains
“There probably is no other branch of our profession where opinions differ so much about indications and surgical approaches as there are for diseases and abnormalities of the TMJ.”
a challenge and in these cases, costochondral grafts appear still to be favored in combination with covering the fossa with either the original disc or a temporalis muscle flap (Peterson et al., 1992, Kaban et al., 2009).
A novelty worth mentioning is the miniplate eminoplasty for the treatment of recurring dislocation of the TMJ, as suggested by Puelacher and Waldhardt (1993). This simple but very effective technique, makes clever use of the introduction of miniplates in the armamentarium of the oral and maxillofacial surgeons by blocking the condyle on its way to dislocate out of the fossa with a plate that is bent to do just that. Excellent results are reported by Kutenberger and Hardt (2003) on 20 patients followed for three to seven years. This procedure appears to be less unpredictable than the earlier mentioned eminectomies and downfracturing of the zygomatic arch and certainly produces less irreversible damage.
Treatment and diagnosis of the painful and dysfunctional joint underwent a reappraisal mainly because of a paper by Nitzan et al. in 1991. They reported on the results of simple lavage of the joint spaces, without the need for arthroscopy. Several follow-up studies showed good results, even in cases of closed lock.
This observation casts some doubt upon the mechanical theories of disc displacement as a result of muscle traction caused by habits and/or occlusal or articular malfunction. Soon a new theory was proposed by Nitzan and Marmary (1998) and Nitzan and Etsion (2002), which they called the “anchored disc phenomenon,” which might cause the adhesion of the disc to the fossa and/or eminence. It is suggested that the lubrication by phospholipids that are protected by hyaluronic acid, is impaired. This is caused by reactive oxygen species that degrade hyaluronic acid and are released as a result of overloading of the joint. Whatever the truth may be, this theory explains the successful results of simple lavage of the upper joint space in various stages of disc displacement. The use of arthroscopy gradually went out of fashion because of the successes achieved with arthrocentesis (Brennan & Ilankovan, 2006).
There probably is no other branch of our profession where opinions differ so much about indications and surgical approaches as there are for diseases and abnormalities of the TMJ. This is particularly true for the conditions that were previously described as pain dysfunction of the TMJ, but that over the years had several name tags attached to it which are not necessarily overlapping. Terms used in various publications, such as internal derangement, non-reducing disc displacement, painful TMJ hypomobility, chronic locking of the TMJ, closed lock, osteoarthritis and osteoarthrosis, already point towards descriptive diagnoses that leave much to the imagination of both the authors of these articles as well as the readers.
One cannot escape the impression that, when reading the various papers on the treatment of these conditions, apples were compared with pears. The results of the many clinical studies where certain modes of treatment are discussed are often contradictory. This comes through loud and clear when reading the reviews of Dimitroulis (2005) in which he critically assesses the role of surgery in the management of disorders of the TMJ. Procedures that were carried out in the 1970s and 1980s with high success rates claimed, turned out to be less recommendable. Thousands of patients, particularly in the U.S.A., had multiple operations performed without the desired result. In retrospect, one can only wonder about the course of events, but certainly the lack of a proper, less descriptive, diagnosis was part of the reason. Dimitroulis remains optimistic on the grounds that he expects that molecular biology might offer the tools to better diagnose the conditions we used to treat by universal means. It might lead to more specific treatment geared to the state of the condition to be treated. Only the future will tell, but there certainly is a need for some evidence-based treatment in TMJ surgery before the profession jumps on the next bandwagon.
Orthognathic surgery
Before 1960
Not surprisingly, oral and maxillofacial surgeons were challenged from the beginning to attempt to correct dentofacial deformities as there were plenty of patients who needed corrective surgery. As widely assumed, Hullihen (1849) was the first surgeon who performed an osteotomy of the mandible. It concerned a subapical, segmental osteotomy to close an anterior open bite. Both in the U.S.A. and in continental Europe, however, several surgeons had designed and developed techniques for sectioning mandibles in order to set back or advance the jaw, as early as the late 1800s and at the beginning of the 20th century. It was Blair (1907), who probably carried out the first mandibular setback by a body ostectomy in 1897 but also an advancement osteotomy in the ascending ramus ten years later.
Detailed descriptions of all the techniques used in the German-speaking area can be found in Wassmund’s book from 1935, which pays attention to every single name that had contributed to the slightest alterations in a given operation. To a lesser extent, this was also true for France (Dechaume et al., 1977). In the U.S.A., similar procedures are described in the various textbooks on oral surgery that appeared before, during or immediately after World War II.
It is only fair to note that most of the procedures currently used were designed in the period after the war. In the maxilla, the exception was the subapical anterior
maxillary osteotomy, according to Wassmund (1926) and the Le Fort I osteotomy, thought to be designed first by von Langenbeck (1859), according to Drommer (1986). The first real Le Fort I osteotomy, including separation of the pterygo-maxillary junction was, however, probably carried out by Schuchardt (1942). In the mandible, the subapical, anterior alveolar osteotomy, as suggested by Hullihen (1849), but popularized by Hofer (1942), still has some application.
After the war, elective corrective surgery became very popular, certainly helped by the availability of adequate antimicrobial drugs. The popularity of the Le Fort I osteotomy was further enhanced by publications of Gillies and Rowe (1954) and Obwegeser (1965, 1969). Wunderer (1962) reported on a modification of the subapical anterior maxillary osteotomy, completely relying on the buccal mucoperiosteal pedicle. This method facilitated the intrusion of this segment, as compared with the Wassmund procedure. Kufner (1960) described the quadrangular osteotomy to advance the middle third of the face.
The publications of Trauner and Obwegeser (1959) on the sagittal split osteotomy, however, caused a complete revolution in the approach to mandibular corrective surgery. Most previously suggested methods, carried out in the horizontal or vertical ramus, were abandoned, including the low condylar osteotomy as proposed by Kostecka (1931). The only exception was the vertical osteotomy of the ascending ramus as designed by Robinson (1956). Obwegeser presented a paper on the versatility of the sagittal split osteotomy at the 3rd ICOS in New York in 1968, where it made quite an impact. From then on, the sagittal split osteotomy would replace most other types of mandibular osteotomies in the U.S.A. and elsewhere.

1960–1990
The further development of orthognathic surgery was, for a large part, due to the input of orthodontists. It was particularly the American orthodontists who saw the opportunities but also paid attention to some of the drawbacks, such as relapse (Profitt & White, 1970 and Poulton & Ware, 1971). They also provided the tools for proper clinical and radiological follow-up. They advocated the preoperative and postoperative orthodontic alignment of teeth, assuring a stable occlusion, which in turn would contribute to the stability of the results. Tricks, such as the use of an acrylic splint (wafer) to
stabilize temporarily the occlusion, or leveling of a deep curve of Spee postoperatively, to increase lower facial height, were certainly the result of their input.
This aspect of a coordinated approach, working as a team, was lacking in all papers that had come from the European mainland. West and McNeill worded this very well in 1977: “Joint diagnosis and treatment planning and analysis of longitudinal treatment responses, based on traditional orthodontic principles, have contributed to the continuing advancement of knowledge and improvement in standards of care.”
It is particularly the follow-up with standardized cephalometric radiographs that opened the eyes of many clinicians. It soon appeared that even during intermaxillary fixation in case of advancement of the mandible using a bilateral sagittal split osteotomy, the mandible was slipping back (McNeill et al., 1973). The wire osteosyntheses simply were not rigid enough to prevent this movement. The impact of this coordinated approach soon became visible in the literature, with numerous papers accompanied by a plethora of suggestions on how to prevent or minimize relapse. Surgical over-correction, particularly for advancement of the mandible and various different wiring techniques were suggested. The sagittal split technique also underwent some modification, as the suggestions of Dal Pont (1958), Hunsuck (1968) and later Epker (1977), were incorporated into the standard procedure. The upper border wiring probably became the standard, instead of the circumferential wire, until lower border wiring came in fashion, just before rigid fixation was widely used (Booth, 1981). An article from Hinds and Kent (1969) on the versatility of the horizontal chin osteotomy made this a popular way for improving the chin contour, instead of silastic implants that were hitherto widely used, particularly among plastic surgeons.
Maxillary surgery, particularly segmental surgery, was also popular, particularly in the late 1960s and early 1970s. Bell et al. (1969, 1971, 1973)had performed experimental research on monkeys, proving that Le Fort I and anterior and posterior maxillary segmental osteotomies were safe with regard to blood supply. He showed that fast revascularization and bone healing occurred, provided the mucoperiosteal pedicles were intact. Although the posterior segmental maxillary osteotomy was introduced by Schuchardt in 1954, as a two-staged procedure, this technique only became popular after the modification by West and Epker (1972). They recommended this procedure, performed bilaterally, for closure of an anterior open bite. This is a valid option today, if one wants to circumvent too much rotation of the maxilla, leading to a backwards rotation of the anterior teeth with subsequent flattening of the naso-labial angle.
The Le Fort I osteotomy, however, as described before, became the workhorse for corrections of the middle third of the face. Not only were advancements possible, for which it was originally described but also vertical movements, including extrusion with interposed bone grafts and intrusion, as reported by various authors (Schendel et al., 1976, Bell & Bride, 1977). Patients with a short or long face could be well treated by vertical lengthening or shortening of the maxilla. This made it possible to really affect the appearance of the middle face.
It became particularly useful for treatment of the cleft lip and palate patient, who often had severe maxillary hypolasia in all three dimensions. It also appeared possible to tilt the maxilla over a horizontal axis, by posterior intrusion, to close an anterior open bite, or the other way around, to bring the anterior part downwards.
This canting of the maxilla was mandatory when treating patients with some types of anterior open bite (Epker & Fish, 1977). Research was also carried out with regard to the split from the pterygoid plate. Several authors had shown that the original technique, making use of the heavy curved chisel, would sometimes cause unwanted bleeding from the venous plexus in this area, or even fractures of the skull base (Wikkeling & Koppendraaier, 1973 and Lanigan, 1987). Trimble et al. (1983) suggested, therefore, splitting the tuberosity distal of the 2nd molar, while Precious (1991) just fractured the maxilla down, without splitting the maxilla from the pterygoid plate.
Last but not least, the surgically assisted orthodontic expansion or distraction, as it presently is called, came in vogue as a means for facilitating the preoperative coordination of the dental arches. This technique came from orthodontics as well, because Dirchsweiler (1956) recommended palatal expansion in young individuals by opening the mid palatal suture, without surgical intervention. This technique also gained popularity and appeared to be very useful indeed for selected patients (Bell & Epker 1977).
It did not take long before surgeons were beginning to do bimaxillary procedures to correct more precisely the imbalance between maxilla and mandible. Obwegeser
(1970) is probably the first to have published about this possibility, describing a case of maxillary hypoplasia combined with mandibular hyperplasia treated by a bimaxillary osteotomy. The 1970s and early 1980s were really the boom times for this type of surgery, with lots of articles appearing that presented follow-up studies and suggestions for improved techniques.

Another novelty introduced during this period, was the maxillary osteotomy following the lines of the Le Fort II pattern (Henderson & Jackson, 1972). The extracranial Le Fort III osteotomy had already been introduced by Gillies and Harrison (1950). These procedures, although not often necessary, completed the scope of the surgeon who was doing orthognathic surgery.
Although Hinds and Kent (1972) had published the first monograph on orthognathic surgery, the appearance of the book of Bell, Proffit and White (1980) finally caused surgeons and orthodontists to work together all over the world; the message being that a coordinated surgical-orthodontic approach would provide superior results. This was the first book on the subject that presented orthognathic surgery in a comprehensive way, emphasizing how diagnostic tools and properly coordinated treatment lead to the best results, both from a functional as well as esthetic point of view.

Another means of fixation that had already quite a history finally came to the surface in this period. Surgeons had been struggling with wire osteosynthesis for years, neglecting the developments in trauma surgery, or at least, not considering them fit for this type of surgery. Spiessl has to be credited for his pioneering work in this area. He advocated lag screws to fix the fragments in cases of sagittal split osteotomies in 1974, applying the principles of rigid fixation. It took quite a while before this was followed by others (Paulus & Steinhauser, 1982).
It soon became clear that positional screws were a better choice because these would not squeeze the nerve between the fragments (Jeter at al 1984), while stability was achieved with less relapse than was seen with wire osteosynthesis (Van Sickels et al., 1986).The evolution of small plates, as proposed by Champy et al. (1976), also made it possible to fix the fragments of the sagittal split osteotomy (McDonald et al., 1987, Rubens et al., 1988). This also was true for maxillary surgery, where mini- and later micro-plates replaced the wire osteosyntheses. It was especially beneficial for the extrusion le Fort I osteotomy
to use plate fixation, since late relapse, up to 50 percent, often occurred when using wires (Quejada et al., 1987). The introduction of all these techniques made the surgery more reliable and predictable since the relapse tendency was further diminished
It is safe to state at this point that the input of orthodontists and experimental and clinical research brought orthognathic surgery to the next level of development, something that was augmented by the introduction of rigid fixation. The time of pioneering was over; further refinements would come from technology that would be introduced in the next period. A detailed review of the historical development of orthognathic surgery, up to this period, is presented by Steinhauser (1996).
1990–2010
In the late 1980s, a new indication for orthognathic surgery began to emerge, which came to its full expression in the next decade. It is particularly Riley, Guilleminault and Powell (1989 &1993) who laid the foundation for the wide application of mandibular advancement, along with the hyoid with or without the maxilla, for patients with sleep apnea. Their research prompted many colleagues from all over the world to participate in teams in the treatment of patients with severe sleep disorders.
Currently, it seems that maxillo-mandibular advancement may be the best solution to increase posterior pharyngeal space in most cases (Prinsell 1999). It also caused the profession to look into the possible effects of mandibular set-back surgery on the posterior airway space (Hochban et al., 1996, and Tselnik & Pogrel, 2000). Caution appeared to be warranted in certain patient groups with other risk factors.
The search for maximum stability continued during this period, resulting in several retrospective and even prospective studies, showing that both the bicortical screws and plates fixed with monocortical screws were equally stable for mandibular advancement surgery using the sagittal split technique (Dolce et al., 2000, Borstlap et al. 2004, and Joss & Vassalli, 2009). The choice of the method of fixation became mainly a preference of the surgeon and the patient. These considerations are also valid for set-back procedures using the sagittal split method, although there are less known studies which refer to the hyperplastic mandible. This may also be attributed to the fact that many surgeons still prefer the vertical ramus osteotomy (Robinson 1956) for this purpose.
In Le Fort I osteotomies, stability with plate osteosynthesis did not appear to make much of a difference, for understandable reasons (Haers et al., 1999), except, of course, for the extrusion osteotomy. Micro-plates were particularly favored because of ease of application. This,
of course, is also applicable for the high level maxillary osteotomies, where stability with wire osteosyntheses is difficult to achieve and certainly for all sorts of segmental osteotomies, including genioplasty.
During this period, much more attention was paid to possible complications and side effects of the various osteotomies that were routinely carried out. For the mandible, it mainly concerned nerve dysesthesia and progressive condylar resorption. Permanent nerve dysesthesia, occurring in approximately 15 percent of cases when using the sagittal split osteotomy, is probably related to several factors, such as age, the need for dissecting the nerve out of its canal and the stretching of the nerve (Borstlap et al., 2004). Teerijoki-Oksa et al. (2002), however, made it quite clear that holding a medial tunnel retractor in place may knick the nerve, particularly when this stays in place for quite a while. There is certainly a need to bring the number of permanent nerve deficits down further and many surgeons would prefer the vertical ramus osteotomy, to set the mandible back for that reason alone (Zaytoun et al.,1986).
Although some case reports have been presented in the time that wire osteosyntheses were widely used, progressive condylar resorption (PCR), as it is currently called, was first well described by Arnett and Tamborello (1990). Since this publication, several clinicians have recognized this problem and have come up with suggestions about its etiology. It is likely that this only came to the surface when rigid fixation was used, because before that time all relapse was thought to be caused by backwards slippage of the wired distal fragment. One simply did not look at the change in morphology of the condyle. In any event, this is an awkward condition that seems to occur particularly in women with a high mandibular plane angle and often in patients that have an open bite as well (Hoppenreijs et al., 1998). Recommendations for treatment vary from redo operations to replacement of the condylar unit (Hoppenreijs et al., 1999 & Troulis et al., 2007).
An excellent account of all possible complications is to be found in “Risks and Benefits of Orthognathic Surgery,” edited by Precious and Lanigan (1997). It goes beyond the scope of this section to deal with all of them, but it certainly deserves a lot of attention from all surgeons who like to perform elective orthognathic surgery.
A new technique that made its “grand entrée” in this arena is called osteodistraction. It was McCarthy et al. (1992) who introduced this concept in maxillofacial surgery and they soon got a long list of followers. The profession quickly focused its research on developing intraoral devices, instead of the extraoral pins that caused awkward scars. This became extremely successful and currently there are
many devices available for applications in both mandible and maxilla (Wangerin & Grob, 1994 and Chin & Toth, 1996). At present, the principle of distraction osteogenesis is widely used for all sorts of procedures. The main advantage of this technique being that bone grafts are not necessary in cases where distances have to be bridged. For this reason, the method is extremely suitable for patients with maxillary hypoplasia, including patients with cleft lip and palate but also for patients with hemifacial microsomia. There is ongoing dispute as to whether conventional osteotomies are to be preferred in preference to distraction in straightforward cases, or the other way around. It looks like a pendulum that will go back and forth as time goes by.
Another new technique, that has already made inroads in many branches of surgery, is minimally invasive surgery, making use of endoscopic instruments. An excellent review of its current and possible future applications is presented by Resnick et al. (2009). The use of resorbable osteosyntheses has also made its way into orthognathic surgery, although they were already frequently used in trauma surgery and are dealt with in that section.
development of the specialty as a whole, which includes facial esthetic surgery. Many colleagues are, nowadays, carrying out adjunctive esthetic procedures in conjunction with orthognathic surgery, such as liposuction and cosmetic rhinoplasties. It is to be expected that this development will continue.
Cleft lip and palate and craniofacial surgery
Before 1960
It is not surprising that children born with cleft lip and palate have drawn the attention of surgeons for a long time. This is probably true for many parts of the world but in Europe several 16th, 17th and 18th century surgeons attempted to close lips, among them Paré, as illustrated in his well-known book. They all confined surgery to the lips, as the cleft sides were pared and brought together and fixed in a straight manner. The latter was done with a pin that was stuck through both sides, around which a figure of eight thread was wrapped. Alternatively, a triangular needle was used to suture the skin and lip mucosa together. In the 19th century, curved full thickness incisions
There is, of course, another technical advance that needs to be mentioned and that is the 3-D imaging technique. This has brought about a revolution in many ways, as 3-D models can be prepared for studying complicated reconstructive cases but also for mimicking the operations to assess the best possible solution for the patient. This technique will also allow for circumventing the need for cast models by producing virtual models and constructing real, intermediate splints, purely based on proper 3-D imaging (Xia et al., 2000, Swennen et al., 2007, Choi et al., 2009). Last, but not least, it provides a means for the documentation and study of changes brought about by corrective surgery in a three-dimensional fashion that was hitherto was not possible (Khambay et al., 2002).
The development of orthognathic surgery has gone from simple surgical techniques to correct gross facial deformity, that were developed decades ago, to a highly sophisticated specialty, that has the tools to correct all possible deformities with a high degree of accuracy at the present time. This is well illustrated in the book of Reyneke (2003). There currently is much more emphasis on the esthetic component, which is in keeping with the
came in fashion, which allowed for lengthening of the lip but still created a straight lip closure Rose (1891). The history of the development of cleft lip and palate treatment over the centuries is described in detail by Stiebitz in the book of Hoffman-Axthelm (1995) and by Millard (1976 and 1977).
It was French surgeons, in particular, who took the initiative to improve the techniques for closure of cleft lips. The name of Malgaigne (1843) is attached to a “cheiloplasty” in which the surgery tried to circumvent a straight closure and to avoid a whistling deformity. He pared the upper part of the cleft sides combined with a horizontal relaxing incision, which allowed for lip lengthening. Later the name of Merault (1871) became known for his using the same technique with a slight modification. In Germany, von Bruns (1844) claimed to be the first to use this type of closure. It is interesting to learn that two great names in cleft surgery, Veau and Blair, practiced the Merault technique, with modifications, for unilateral cleft lip up until the beginning of the 20th century.
There were several other pioneers, including von Langenbeck and Hagedorn (1884), who tried to improve
“It was French surgeons, in particular, who took the initiative to improve the techniques for closure of cleft lips.”
on the existing techniques of lip closure. The latter introduced the principle of a Z-plasty, avoiding a straight scar and at the same time providing lengthening of the lip. This principle was later refined by LeMesurier and even Millard.
The closure of the alveolar cleft posed a more complicated challenge, particularly when a complete bilateral cleft was involved. It was common practice in the first part of the 19th century to remove the premaxilla (Roux, Dieffenbach), while some would reduce it (Fergusson) and others forcefully set it back (von Bruns, Langenbeck). Bringing both sides together by compression of the cheeks was also attempted, using various extraoral types of apparatus, the best known being the “Hainby’s truss” as recommended by Fergusson in 1864.
One has to realize that all these operations were carried out on babies or young children, without the use of general anesthesia. This was not without risk, as appears from reports of Billroth and Krönlein. In the years between 1860 and 1867, Billroth reported 18.7 percent mortality, whereas Krönlein mentioned as much as 43 percent from the Langenbeck clinic in Berlin (HoffmanAxthelm, 1995)
Graefe (1816) and Roux (1819) were the first to attempt to close the soft palate, soon followed by several others, among them Gustav Passavant, known from the cushion in the posterior pharyngeal wall that is named after him. He cleverly predicted: “since early closure of the lip-alveolus is the most important factor in achieving spontaneous narrowing of the anterior palatal cleft, it might be expected that early closure of the soft palate will result in narrowing of the posterior palatal cleft.” He reported on the successful operation on five children varying in age from 6 weeks to 2.7 years, all operated upon without general anesthesia! It also is not clear from these descriptions whether attempts were made to align the palatine muscles.
The story about closure of the cleft of the hard palate began with attempts to mobilize only the mucosa. Several surgeons in Germany, England and the U.S.A. experimented along these lines, among them Dieffenbach, Passavant, Fergusson, Pollock and Warren. The breakthrough, however, came with von Langenbeck, who in 1862 and 1863 presented the results of successfully closed palates of patients varying in age from 7 to 59 years, using mucoperiosteal flaps. Again, all these operations were carried out without the use of general anesthesia. Until that time, surgeons were afraid of including the periosteum in the flaps, fearing that the underlying bone would become necrotic. His method was soon adopted by surgeons from all parts of the world (Hoffmann-Axthelm, 1995).
The introduction of chloroform anesthesia meant that early operations were carried out on children in the second half of the 19th century. This was also the period when obturators were introduced to take advantage of the action of the split pharyngeal constrictor muscle. The names of Kingsley from the U.S.A. and Schiltsky from Germany became widely known in relation to these devices (Hoffmann-Axthelm, 1995).
In the U.S.A., Truman Brophy (1916) dominated the art of cleft surgery for many years. When reading his text, in which he devotes 230 pages to the treatment of cleft lip and palate, he shows little modesty. He obviously was a self-confident man, very much aware of what was going on in Europe but quite convinced of his methods being right, considering his comments in the book directed to his colleagues.
He would stick to a strategy that was completely against the then common practice by propagating a reversed sequence: “The lips should not be operated on until after the bones have been approximated and united.” His technique looks rather gruesome nowadays, including introducing silver wires through the maxilla, cranial of the palate, to hold the approximated fragments in place. In cases of bilateral cleft, he first brought the premaxilla backwards after a wedge excision in the vomer and carried it back and fixed it by means of silver sutures. The palatal shelves were approximated as described before, trying to achieve bony union. Lips were closed six weeks to three months later. He also advocated operating early, since the bone would still be soft and malleable. It took years before it was realized that this treatment had a detrimental effect on the growth of the maxillofacial complex. His disciples, Blair and Ivy (1923) did not follow their master’s example but adapted the strategy of Victor Veau.
A true new era in the treatment of children with cleft lip and palate began with the introduction of the double layer closure of clefts by Victor Veau (1882–1949), using the nasal mucosa, both from the lateral side and the vomer. He simultaneously freed the alar base and turned it across the cleft just inside the entrance to the nostril. He also emphasized the need to approximate the muscles using wires, in fact creating a three-layer closure and closed the anterior palate simultaneously. He was, at the same time, aware that he was operating on growing individuals in which growth could be impaired by early surgery.

He published his work in two monographs in 1933 and 1938. It is astonishing to read the detailed descriptions of both the classification and surgical treatment of cleft lip and palate, particularly in his standard text “Bec de Lievre.” He devoted his life not only to the treatment but also to the study of the embryology related to cleft lip and palate. Even today, it is worthwhile studying his observations. His work had a great influence on his contemporaries as is borne out in the books of Wassmund (1939) and Axhausen (1940) but also by publications in English, for instance, Blair, Ivy and Brown (1923, 1936, 1944) and Kilner (1937).

Other major forward steps were the first attempts at improving speech by carrying out pharyngoplasties. Rosenthal (1924) presented a caudally pedicled posterior pharyngeal flap to insert into the velum, while Sanvenero-Rosselli (1932) used a cranially based flap. Various modifications have since been published but almost all are based on these two principles.
In the period from roughly 1940 to 1960, numerous wellknown surgeons came up with suggestions for improving the esthetics of the lip and nose, including lengthening of the lip, creating a Cupids bow and avoiding the notching of the upper lip. Those names include, although no completeness is claimed, Le Mesurier, Tenisson, Limberg and Trauner.
Last but not least, primary bone grafting of the alveolo-palatal cleft was carried out by several surgeons, most of whom were European. According to Stellmach (1973), this procedure was performed in 1914 by Drachter but also by Kazanjian (1951) and Axhausen (1952). However, it was particularly Schmid (1964), who in the 1950s advocated this procedure. Conversely, Stellmach (1973), based on a review of the then existing literature and on his own long term experience, pointed towards the disappointing results with regard to growth inhibition, which led to cross bites and maxillary hypoplasia.
Although the principles of primary cleft lip and palate surgery by the end of this period were known, little was understood about the impact on growth, although there was a growing awareness that because of surgery, growth retardation did occur. Schweckendieck (1973), in a paper in a year book of the German Society, mentions this as a general feeling among German surgeons (although not a single non-German author is mentioned!!) and specifically points to the advantages of early closure of the soft palate (nine months) followed by lip and naso-alveolar closure two to three weeks later, limited to the soft tissues only.
His father began to follow this protocol in 1944 and reported good results also with little growth retardation in the long run (Schweckendieck 1955 &1958).
1960–1990
There were five important and noticeable developments during this period which would fundamentally change the treatment of patients with cleft lip and palate, whereas other breakthroughs occurred that opened the pathway to craniofacial surgery.
First, the introduction of cephalometrics made it possible to register and monitor growth and development of the jaws of the growing child and thus, to quantify the amount of growth impairment. It was particularly orthodontists who made these observations and became the “watchdogs” in the cleft lip and palate teams, as the impact of certain techniques on growth could be objectively documented.
Evaluation of dismorphic growth in both operated as well as non-operated patients contributed enormously to the improvement in techniques with which to approach cleft lip and palate patients and patients with craniofacial syndromes. There is no doubt that Pruzansky (1920–1984), the founding director of what is probably the first cleft lip and palate and craniofacial team in the world, at the University of Illinois, was the leading authority in this area. In a series of articles during his professional life, he produced invaluable and groundbreaking information that paved the way for a more rational approach to the treatment of clefts as well as to craniofacial deformities (Cohen & Rollnick, 1985). His information had a particular impact on timing of the surgical interventions.
Another pioneer who promoted the team approach and also stressed the importance of keeping careful records, including casts, cephalometric radiographs, photographs etc., in order to gain knowledge but also to assess critically one’s own results, was Berkowitz. In an authoritative publication, he reviewed the then-existing literature on orofacial growth in cleft lip and palate patients and suggested future studies to improve treatment (Berkowitz, 1977). At the end of his career he presented a multi-authored book on the state of the art of cleft lip and palate management (Berkowitz, 2006).
As a result of cephalometric studies, one of the most important discoveries of this particular time period was the observation that individuals with unoperated clefts had almost normal facial growth (Dejesus, 1959, OrtizMonasterio et al., 1966, Bishara et al., 1976, 1986). This observation has been repeatedly confirmed by various studies until today. This led to the conclusion that almost all growth impairment had to be attributed to the effects of surgery. This in turn led to a treatment protocol that limited
the surgical interventions and modified the sequencing, including the postponement of the closure of the hard palate, as previously recommended by Schweckendieck (1955).
An original idea to allow the palatal shelves to grow and to facilitate the feeding of babies, while postponing the closure of the hard palate, was introduced by Hotz in the early 1960s (Hotz & Gnoiski, 1978). They recommended the use of an acrylic plate to obturate the cleft, soon after birth. This early orthopedic treatment, actively guiding the fragments into the desired position by selective grinding of the acrylic plate, was widely adopted, particularly in Europe, despite the fact that it required frequent followup and often the fabrication of new plates to catch up with growth.
Second, teams of specialists of various origin began to work together to approach the complex problems in a rational way, based on growing evidence that growth, speech and psychological development of the child were intimately related to each other. The possible problems with regard to dysfunction of the eustachian tube were also recognized and heralded expertise from the ENT discipline (Soudijn & Huffstadt, 1972). It was Pruzansky (1955), who became the initiator and great promoter of this idea. He emphasized not only the clinical advantages but also the need to carry out research to improve results.
His example was soon followed in several places all over the world, acknowledging the importance of a multidisciplinary approach in which next to the cleft surgeons, orthodontists, ENT surgeons, speech pathologists, pediatricians, dentists and disciplines providing psychological and social support, were equally important. This philosophy came through loud and clear with the introduction of the Cleft Palate Journal in 1962.
Third, the introduction of secondary bone grafting of the alveolo-palatal cleft. This grafting was done in order to promote the eruption of the canine in the cleft, which in turn would improve the dental arch form. This so-called early secondary bone grafting was introduced by Nordin and Johanson in 1955 and, as seen in German literature (Stellmach, 1973), was followed by many clinicians.
It was Boyne and Sands (1972), however, who pointed towards the proper timing (between nine and 11 years) to allow the canine to erupt through the grafted bone. It is of interest to note that Freitag and Fallenstein (1984) adapted the timing of the grafting in cases where a lateral incisor could be brought into the arch. This brought about a revolution in the treatment of the dental arches because, depending on the number of missing teeth, in many cases, an uninterrupted dental arch could be achieved through adequate orthodontic treatment. This in turn facilitated the surgical advancement of the hypoplastic maxilla when
such a procedure was indicated. Several studies were subsequently published to attest to the validity of this technique using various donor sites for the bone graft, including anterior iliac crest, rib and chin but also calvarium and tibia (Abyholm et al., 1981, Bergland et al., 1986, Sindet-Pedersen & Enemark, 1988, Witsenburg & Freihofer, 1990, and Borstlap et al., 1990).
Fourth, development in orthognathic surgery made it possible to treat the under-developed maxilla and restore the vertical and anterior-posterior position, combined with adequate orthodontic treatment. This concept was initiated by Obwegeser (1971) in the 1960s. Simultaneous grafting of the cleft and osteotomy of the maxilla was suggested by Henderson and Jackson (1975). The concept of segmental advancement and aligning the segments, along with simultaneous bone grafting of the alveolo-palatal cleft was introduced by Tideman et al. (1980).

Another useful osteotomy for treatment of a midface hypoplasia, often as a result of cleft lip and palate, concerned the quadrangular osteotomy, as first described by Kufner (1971). This osteotomy had its drawbacks because the infraorbital nerve was often damaged but produced satisfying esthetic results, particularly when extended into the zygomatic bone (Obwegeser, 1969, Souyris, 1973).
Last, but not least, the introduction of the subcranial Le Fort III, in the early 1940s (Gillies, & Harrison, 1950), (Gilles & Rowe, 1956) and the Le Fort II (Henderson & Jackson, 1973) osteotomy made it possible to correct deformities of all areas of the midface as sometimes seen in this patient group but also in some syndromic patients. Again, Obwegeser (1969) pointed to the usefulness of this osteotomy in some cleft patients, combining it with a Le Fort I osteotomy so as to allow for differential advancement of the midface and the tooth bearing part of the maxilla. The results of the Zurich experience were presented by Obwegeser (1973) and Freihofer (1973), followed by many others both in Europe and the U.S.A.
Secondary surgery on the adult cleft lip and palate patient also became more sophisticated and particularly the closure of secondary palatal fistulae using intraoral tissues, including tongue flaps and bone grafting, became the standard (Jackson, 1972). Lip revisions and corrections of the nose were often necessary, particularly in the adult patient group, initially operated upon by less experienced surgeons or being subjected to less advanced techniques.
The above-mentioned developments took place almost simultaneously, beginning in the early 1960s and extending over the whole of this period. Further improvement in surgical techniques primarily for closure of the lip, however, were also reported. The two most important improvements, which had many followers, were the wave line of Pfeifer (1970), and the advancement rotation flap of Millard (1959, 1964). These techniques were applied to both unilateral as well as bilateral cleft lips, although in the latter case, staged procedures were often used depending on the position of the premaxilla.
The management of the protruded or extruded premaxilla was subject to a lot of debate. A review of the then existing literature is presented by Eppley et al. (1986), in which they concluded that “secondary reconstruction should be directed towards proper skeletal positioning of the premaxilla.” This should be done after orthodontic alignment and after the age of 8 years. It would entail an osteotomy of the vomer and nasal septum, bone grafting of the defects and proper mucosal coverage with either rotational flaps from the vestibule or tongue flaps.
Fifth, probably the most exciting and revolutionary development in this period was the emergence of craniofacial surgery, including intracranial access to the midface and the treatment of craniosynostosis at an early age so as to promote the normal development of the brain in patients with one of the craniosynostotic syndromes. It also allowed for correction of the position of the orbits and the reduction of telecanthus.
The pioneer in this field, without any doubt, is Tessier, who first published in 1967 the intracranial approach to the orbits to treat hypertelorism. He showed that if the orbital contents were circumferentially mobilized, the eye itself could be moved permanently in any direction without affecting the vision. He also demonstrated that simultaneous intracranial and extracranial surgery was possible. This brought about a revolution in the treatment of patients with Apert and Crouzon syndromes and all other syndromes caused by craniosynostosis (Tessier, 1967). It is somewhat beyond the scope of this book to go into detail but this was the basis for further development and refinement of techniques for treating these complicated and often rare syndromes. The progress made in these years is well illustrated in a standard text written by authors from Europe and the U.S.A. (Stricker et al. 1990).
Apart from these daring procedures, the history of which is well recorded by Ortiz-Monasterio in the book of Jackson et al. (1982), Tessier also showed that extensive areas of the craniofacial skeleton could be completely devascuralized, repositioned and still somehow healed. This trick became very useful in the context of access surgery to the brain and orbital content.
1990–2010
By this time, the general consensus was to try to reduce the iatrogenic growth impairment as much as possible by limiting the number of surgical procedures and by postponing the closure of the hard palate. Lips are closed first by most surgeons at an age varying from six to nine months, depending on the weight of the baby and the soft palate is closed about a year later. Pharyngoplasties, if necessary, are carried out at around six years.
The timing of hard palate closure varies from two to 11 years between the different teams. The development of speech is a decisive factor when deciding to close the hard palate early but it clashes with the idea of postponing the surgical closure in order not to disturb the maxillary growth. Various retrospective studies, however, are not conclusive whether delaying hard palate closure until the early teens is of any benefit (Novarraz et al., 1993, Stein et al., 2007). When postponing from nine to 11 years, it can be done simultaneously with the grafting of the alveolopalatal cleft. There is currently no consensus as to what should prevail and, thus, teams differ in the timing of this procedure.
The above-mentioned approach would result in a minimum of three operations before the age of 16, at which possible secondary corrections on lip and nose can be done. Where maxillary hypoplasia is developing, an osteotomy might be planned, which implies that no orthodontic compensation for the skeletal deformity should be carried out. Despite all efforts to promote adequate growth of the maxilla, advancement surgery of the maxilla is still needed in about 25 percent of cases (DeLuke et al., 1997, Steinberg et al., 1999).
In this context, it is only fair to quote the work of Delaire (1977), who in a series of articles in the 1970s pointed towards the roles the nasal septum and vomer play in the growth of the maxilla. He also emphasized the need to restore the normal anatomy of the muscles of the lip and soft palate, if normal development is to be achieved. This was largely published in French and did not initially receive the attention it deserved but subsequent publications in English in the late 1980s and early 1990s spread his philosophy about cleft lip and palate repair with special attention to the proper attachments of the nasolabial muscles (Delaire & Precious, 1986, Markus, Delaire & Smith, 1992).
This surgery is preferably carried out at the age of six months simultaneously with the closure of the soft palate. The hard palate is then closed about a year later using

only the fibro-mucosa. His ideas have had great influence among many cleft surgeons. It is particularly the idea of using limited sized flaps to close the hard palate and not to denude the palatal bone that has gained acceptance among many surgeons.
The main emphasis during this period is on monitoring growth and several, mostly retrospective, studies are published on the supposed effects of certain modifications of treatment on maxillary growth. A pioneer in this arena is Ross (1987), who in a series of seven papers, published on the effects of certain modes of treatment on maxillary growth. Many others followed in the subsequent years (Semb & Shaw, 1990, Noverraz et al., 1993, Liao et al., 2006, Friede, 2007, Geraedts et al., 2007). In general, however, the current studies are retrospective in nature and not randomized, which makes it difficult to arrive at evidence-based conclusions.
A randomized, prospective study revealed that no advantages are to be expected from early orthopedics in UCLP patients (Bongaarts et al., 2009). This outcome study was certainly surprising and a blow for those who had adopted the original ideas of Hotz.
Orthognathic surgery for cleft lip and palate patients underwent further refinement, as is nicely presented by Posnick and Tiwana (2006). It was particularly orthodontic input that improved results, as the surgery was already known about in the years preceding this period. As mentioned in the orthognathic section, distraction osteogenesis has made its inroads into this type of surgery and certainly in relation to the treatment of CLP and patients with craniofacial anomalies. Numerous reports have appeared that advocate distraction versus osteotomy and bone grafting as the method of choice. Particularly for the high-level midface osteotomies this seems to be a sensible way of doing things (Figueroa et al., 2004, Cheung et al., 2005).
Another novelty in the treatment of the CLP patient is the placement of implants in the grafted alveolar cleft area to replace missing teeth (Kearns et al., 1997, Takahashi et al.,2008). Timing of this procedure is important since most of these grafts are placed in still growing individuals.
Today, the art of cleft lip and palate repair has become a multidisciplinary endeavor, requiring the expertise of many specialists. Future prospective studies, preferably of a randomized nature, have to be carried out to make further progress. This will take time since outcome studies, per definition, will need to have a follow-up of, at least, 16 years.
Craniofacial surgery also made major progress during this period. The advent of CT scans with accurate 3-D models made the diagnosis of some rare anomalies possible and the planning of the operations easier. Special procedures
were developed by several craniofacial surgeons to approach the anomalies caused by the synostosis of the various cranial sutures (Zöller et al., 2002). The introduction of distraction osteogenesis reduced the morbidity and even mortality of, for instance, the monobloc advancement, including the fronto-orbital skeleton with the maxilla on the Le Fort III level (Arnaud et al., 2007).
The latest development in craniofacial surgery concerns the endoscopic, minimally invasive, release of the synostosis. The existing skull malformation is gradually molded with the help of a helmet, allowing for expansion in recessed areas and compression in areas of compensated growth. A prerequisite for success is timely surgery, that is to say, around three months of age. The first results of this technique look very promising and the authors report few and no disastrous complications (Jimenez, Barone, 2007).
An excellent account on the development of craniofacial surgery from the days of Tessier until today is presented by Arnaud (2010). Several pioneers in craniofacial surgery are interviewed and answers to the questions raised are literally printed in this article.
Epilogue
At this stage, the profession has moved away from dogmatic statements by individuals, based on personal experience, to properly constructed outcome audits, which in turn have fueled research projects along many fronts, frequently involving multidisciplinary teams of workers. Together with advances produced with industry and various emerging technologies, such as nano technology and tissue engineering, it has constantly broadened the scope for surgical advances and continues to do so.
Abyholm FE, Bergland O, Semb G. Secondary bone grafting of alveolar clefts. Scand J Plast Reconstr Surg 1981; 15:127–40.
Ackermann GL, Altini M, Shear M. The unicystic ameloblastoma: a clinicopathological study of 57 cases. J Oral Pathol 1988; 17:541–46.
Adell R, Lekholm U, Rochler B, Brånemark PI. A fifteen year study of osseointegrated implants in the treatment of the edentulous jaw. Int J Oral Surg 1981; 10:387–416.
Allport WW. The use of plates in combination with Gutta-Percha in treatment of fractures of the lower jaw. Chicago Med J 1858; 15:514.
American Head and Neck Society. Practice guidelines; Parotid http://www. headandneckcancer.org/clinicalresources/docs/parotid php (April 2010).
Andreasen JO. Atlas of replantation and transplantation of teeth. Fribourg Mediglobe, 1991.
Andreasen JO, Kølsen Petersen, Laskin DM. Textbook and Color Atlas of Tooth Impactions. Munksgaard, Copenhagen, 1997.
Angle E H. A new method for treatment of fractures of the maxillae. Int Dent J 1890;11:330.
Annandale T. On displacement of the interarticular cartilage of the lower jaw and its treatment by operation. Lancet 1887;1:411.
Arnaud E, Marchac D, Renier D. Reduction of morbidity of the frontofacial monobloc advancement in children by the use of internal distraction. Plast Reconstr Surg 2007;120:1009–26.
Arnaud E. L’innovation en chirurgie craniofaciale: depuis Tessier jusqu’aux perspectives futures. D’apres les témoignages de F. Ortiz-Monasterio, D Marchac, F Firmin et T. Wolfe. Ann Chir Plast Esthet 2010; 55:363–83.
Axhausen G. Pathologie und Therapie des Kiefergelenkes. Fortschr Zahnheilk 1933;9:171–86.
Bailey BN, Godfrey AM. Latissimus dorsi free flaps. Br J Plast Surg 1982;35:47–52.
Bailey H The treatment of tumours of the parotid gland with special reference to total parotidectomy. Br J Surg 1941; 28:337–46.
Bak M, Jacobson AS, Buchbinder D, Urken ML. Contemporary reconstruction of the mandible. Oral Oncol 2010;46:71–76.
Bakamjian VJ, Poole M Maxillofacial and palatal reconstructions with the deltopectoral flap. Br J Plast Surg 1977; 30:17–37.
Baldridge OL, Henny F A. Condylectomy for the persistently painful TMJ. J Oral Surg 1957; 15:24–31.
Banks P, Mackenzie I. Condylotomy: A clinical and experimental appraisal of a surgical technique. J Max–fac Surg 1975; 3:170–81.
Barros Saint-Pasteur, J. Plastia restauradora de la creuesta alveolar de la mandibula. Acta Odont Venez 1966; 4:3.
Battersby T.G. The plating of mandibular fractures. Br J Oral Surg 1967; 4:194–201.
Bauer W. Über zystische Bildungen im Kiefer. Z Stomat 1927; 25:205–69.
Becker R, Machtens E. Druckplattenosteosynthese zur Frakturbehandlung bei Orthopaedisch–Chirurgischen Massnahmen am Gesichtsschädel. OSTEO–NEWS 1973 19; 2.
Bell WH. Revascularisation and bone healing after anterior maxillary osteotomy: a study using rhesus monkeys. J Oral Surg 1969; 27:249–55.
Bell WH, Levy BM. Revascularisation and bone healing after posterior maxillary osteotomy. J Oral Surg 1971; 29:313–20.
Bell WH. Biological basis for maxillary oteotomies. Am J Phys Antropol 1973:38:279–88.
Bell WH, Epker BN. Surgical-orthodontic expansion of the maxilla. Am J Orthod 1976;70:517–28.
Bell WH, McBride KL. Correction of the long face syndrome by Le Fort I osteotomy. Oral Surg Oral Med Oral Pathol 1977; 44:493–520.
Bell W, Proffit W, White R. Surgical correction of dentofacial deformities. Volumes I,II and III, W B Saunders, Philadelphia, 1980.
Bendick C, Scheifele C, Reichart PA. Oral manifestations in 101 Cambodians with HIV and Aids. J Oral Pathol Med 2002; 31:1–4.
Berger A. The Principles and Technique of the Removal of Teeth. Dental Items of Interest Publishing Co. Brooklyn, NewYork, 1929.
Bergland O, Semb G, Abyholm FE. Elimination of the residual alveolar cleft by secondary bone grafting and subsequent orthodontic treatment. Cleft Palate J 1986; 23:175–205.
Berkowitz S. Orofacial growth and dentistry. Cleft Palate J 1977; 14:288–301.
Berkowitz S. Cleft Lip and Palate. Diagnosis and Management. Springer Verlag, Berlin, Heidelberg, New York, 2006.
Bhide SA, Miah A, Barbachano Y et al. Radical radiotherapy for treatment of malignant parotid tumours: A single centre experience 1995–2005. Br J Oral Maxillofac Surg 2009; 47:284–89.
Bianchi B, Ferri A, Ferrari S et al. Iliac crest free flap for maxillary reconstruction. J Oral Maxillofac Surg 2010;68:2706–13.
Birn H. Etiology and pathogenesis of fybrinolytic alveolitis (“dry socket”), doctorate thesis Arhus. Int J Oral Surg 1973; 2:211–63.
Bishara SE, Krause CJ, Olin WH et al. Facial and dental relationships of individuals with unoperated clefts of the lip and/or palate. Cleft Palate J 1976; 13:238–58.
Bishara SE, Jakobsen JR, Krause JC et al. Cephalometric comparisons of individuals from India and Mexico with unoperated cleft lip and palate. Cleft Palate J 1986;23:116–25.
Blackburn T, Cawood JI, Stoelinga PJW, Lowe D. What is the quality of the evidence base for pre–implant surgery of the atrophic jaw? Int J Oral Maxillofac Surg 2008;37:1073–79.
Blair VP. Operations on the jaw bone and face. Surg Gynec Obstet 1907;4:67–78.
Blair VP, Brown JB. Mirault operation for single harelip. Surg Gyn Obst 1930;51:81–98.
Bocca E, Pignataro O. A conservation technique in radical neck dissection. Ann Otol Rhinol Laryngol 1967;76:975–87.
Bongaarts CA, Prahl-Andersen B,Bronkhorst EM et al. Infant orthopedics and facial growth in complete unilateral cleft lip and palate until six years of age (Dutchcleft). Cleft Palate Craniofac J 2009;46:654–63.
Bont de LGM, Boering G, Liem R et al. Osteoarthritis and internal derangement of the temporomandibular joint. A light microscopic study. J Oral Maxillofac Surg 1986;44:634–43.
Borstlap WA, Heidbuchel KL, Freihofer HPM et al. Early secondary bone grafting of alveolar cleft defects: a comparison between chin and rib grafts. J Cranio- Maxillofac Surg 1990;18:201–05.
Borstlap WA, Stoelinga PJW, Hoppenreijs TJM, Van ’t Hof MA. Stabilisation of sagittal split advancement osteotomies with miniplates: a prospective, multicentre study with two-year follow-up Part I &II. Int J Oral Maxillofacial Surg 2004;33:433–41 & 535–42.
Bos R M. Poly (l-lactide) osteosynthesis, development of bioresorbable plates and screws. Ph.D.Thesis 1989, University, Groningen.
Bouvet J. An Appliance for double fracture of the superior maxillae. Dent Cosmos 1901;43:251–64.
Bowerman JE, Conroy BA. Universal kit in titanium for immediate replacement of the resected mandible. Br J Oral Surg 1969 6:223–28.
Boyne PJ, Sands NR. Bone grafting of alveolar clefts. J Oral Maxillofac Surg 1972;39:874–77.
Brånemark PI, Hansson BO, Adell R et al. Osseointegrated implants in the treatment of the edentulous jaw. Scand J Plast Reconstr Surg. 1977;11(Suppl).
Brennan PA, Ilankovan V. Arthrocentesis for temporomandibular pain dysfunction syndrome. J Oral Maxillofac Surg 2006;63:949–51.
References (continue
d)
Bro c a P. Traite d es Tume ur s. P. A sse lin, Par is, 1866
Brons tein SL , Tomase t ti BJ, R yan DE. Inte r nal d e range me nt s of the te mp oromandibular joint : cor re lation w ith ar thrograp hy w ith surgic al fi nding s. J O ral Surg 19 81; 39:57 2– 8 4
Brow ne RM. T he o dontoge nic ke rato c ys t . Br D e nt J 1970;128:2 25– 30
Br uhn C , Hauptme ye r F, Kuhl M, L ind e mann A . Die ge ge nwar tige B e handlung s we ge d e r K ie f e r sc huss ve r le t zunge n. JF B e rgman Ve r lag, W iesbad e n, 1915
Br unn von A . Üb e r die ausd e hnung d es Schme lzorganes und seine B e d e utung f ür die Z ahnbildung. A rc h Mikrosk A nat 18 87;29: 367 – 83
Buse r D, Bragge r U, L ang NP, Nyman S. Re ge ne ration and e nlarge me nt of jaw b one using guid e d tisue re ge ne ration. Clin O ral Implant s Res 199 0;1:2 2– 3 2
Butlin HT. Diseases of the tongue. London, Casse ll & Co. 18 85
Butlin HT. The results of operations for carcinoma of the tongue BMJ 1905; (i): 1–10
Calearo C V, Teatini G . Func tional ne ck disse c tion. A natomic al grounds, surgic al te c hnique , clinic al obse r vations. A nn O tol Rhinol L ar yngol 19 83;92:215–2 2
Car lson ER , Che ung A , Smith B , P fobl C . Ne ck disse c tions for oral/head and ne ck c ance r : 19 0 6 –20 0 6. J O ral Ma xillof ac Surg 20 0 6;64 : 4 –11
Cawo o d JI, Howe ll R A . A classifi c ation of the e d e ntulous jaw s. Int J O ral Ma xillof ac Surg 19 8 8;17 :23 2– 36
Cawo o d JI, Sto e linga PJW, Black bur n TK . T he Evolution of preimplant surge r y f rom pre pros the tic surge r y. Int J O ral Ma xillof ac Surg 20 07; 36: 37 7 – 85
Ce lesnik F. Die Tub e r plas tik . O es t Z Stomat 19 5 4 ;51:5 8 4
Champy M, Lo d d e J, Jae ge r JH, W ilk A . Os te os ynthèsis mandibulares se lon la te c hniques d e Mic he le t . I Bases biomé c haniques. II Prese nt ation d’un nouveau mate r ial. Result at s. Rev Stomatol 1976;7 7 :569 –76; 57 7 – 5 82
Chan MF, Hay te r JP, Cawo o d JI, Howe ll R A . O ral re habilit ation w ith implant–re t aine d pros thesis follow ing ablative surge r y and re cons tr uc tion w ith f re e flaps. Int J O ral Ma xillof ac Implant s 1997;12:820 –27
Chaudhar y S , K aira N, Gomb e r S. Tub e rculous os te omye litis of the mandible: a c ase re p or t in a 4 – year old c hild. O ral Surg 20 04 ;97 :6 03 – 0 6
Che ung LK , Chua HDP, Hagg MB. A me t a – analysis of cle f t ma xillar y os te otomy and dis trac tion os te oge nesis. Int J O ral Ma xillof ac Surg 20 0 5; 35:14 –2 4
Chin M, Toth BA . Dis trac tion os te oge nesis in ma xillof acial surge r y using inte r nal d evices – revie w of fi ve c ases. J O ral Ma xillof ac Surg 199 6;5 4 : 45– 5 3
Choi JY, Song KG , Bae k SH. V ir tual mo d e l surge r y and waf e r f abr ic ation for or thognathic surge r y. Int J O ral Ma xillof ac Surg 20 0 9; 38:130 6 –10
Chome t te G , Aur iol M, Te reau Y,Vaillant JM. Muco e pid e r moid tumour s of minor salivar y glands. Clinic al and pathologic al cor re lations. His to e nz ymic and ultras tr uc tural s tudies. A nn Pathol 19 82;2:29 –40
Chr is te nse n RW. T he te mp oromandibular joint pros thesis e leve n year s late r O ral Implant 197 1;2:125– 33
Chuong R , K aban LB , Kozke w ic h H, Pe re z- At ayd e A . Ce ntral Giant Ce ll L esions of the Jaws: A Clinicopathologic al Stud y. J O ral Ma xillof ac Surg 19 86; 4 4 :70 8 –13
Cle me nt sc hisc h F. In: Pic hle r H & Traune r R , e ds: Mund - und K ie f e r Chir urgie 19 4 8 p 5 2 4
Cohe n MM Jr, Rollnick BR . Craniof acial D ysmor p holog y. Studies in Honor of Samue l Pr uzansk y. A lan R L iss. Inc , Ne w Yor k ,19 85
Corcoran MO, Co ok HP, Hobsle y M. Radic al surge r y follow ing radiothe rapy for advance d parotid c arcinoma . Br J Surg 19 83;70:261– 63
Cos te n J B. A s yndrome of ear and sinus s ymptoms d e p e nd e nt up on dis tur b e d f unc tion of the te mp e romandibular joint . A nn O tol Rhinol L ar yng. 193 4 ; 4 8: 499
Cout ard H. Die Rönt ge nb e handlung d e r e pithe liale n K re b es d e n Tonsille nge ge nd. Strahle nthe rapie 1929; 33:2 49 – 5 2
Cr ile G . E xcision of c ance r of the head and ne ck . JAMA 19 0 6; 47 :1786 – 8 8
Dal Pont G. L’osteotomia retromolare per la correzione della progeny. Minerva Chir 1958;1:3–10.
Deautrey J. Reflexions sur la chirurgie de l’articulation temporomandibulaire. Acta Stomatol Belg 1974;72:577–81.
Dejesus JA. Comparative cephalometric analysis of nonoperated cleft palate adults and normal adults. Am J Orthod 1959;45:61–62.
Delaire J. Comment le septum nasal influence–t–il la croissance premaxilaire et maxilaire. Rev Stomat Chir Maxillo–Fac 1977;78:241–254.
Delaire J. Precious D. Influence of the nasal septum on maxillonasal growth in patients with congenital labiomaxillary cleft. Cleft Palate J 1986;23:270–77.
DeLuke DM, Marchand A, Robles EC et al. Facial growth and the need for orthognathic surgery after cleft palate repair: Literature review and report of 28 cases. J Oral Maxillofac Surg 1997;55:694–97.
Devauchelle B, Badet L, Lengelé et al. First human face allograft: early report. Lancet 2006;368:203–09.
Dierichsweiler H. Die Gaumennahterweiterung. Carl Hanser Verlag, München, 1956.
Dimitroulis G. The role of surgery in the management of disorders of the temporomandibular joint; a critical review of the literature. Part I and II. Int J Oral Maxillofac Surg 2005;34:107–13;231–37.
Dingman RO, Natvig P. Surgery of facial fractures. WB Saunders, Philadelphia, London, 1964.
Dingman RO, Grabb WC. Intracapsular temperomandibular joint arthroplasty. Plast Reconstruct Surg 1966;38:179–85.
Dolce C, Van Sickels JE, Bays RA, Rugh JD. Skeletal stability after mandibular advancement with rigid versus wire fixation. J Oral Maxillofac Surg 2000;58:1219–27.
Driemel O, Braun S, Müller-Richter A et al. Historical development of alloplastic temporomandibular joint replacement after 1945 and state of the art. Int J Oral Maxillofac Surg 2009;38:909–20.
Drommer RB. The history of the Le Fort I osteotomy. J Max–fac Surg 1986;14:119–22.
Eckelt U, Loukota R A. Fractures of the Mandibular Condyle — Approaches and Osteosynthesis. Eberl Medien GmbH & Co, Immenstadt in Allgäu, 2010.
Edlan A, Mejchar B. Plastic Surgery of the vestibulum in periodontal surgery for better denture service. Int Dent J 1963; 13:593–96.
Eisenbud L, Stern M, Rothberg M, Sachs SA. Central Giant Cell Granuloma of the Jaws: experiences in the management of thirty–seven cases. J Oral Maxillofac Surg 1988; 46;376–88.
Eliason S, Heimdahl A, Nordenram A. Pathological changes related to longterm impaction of third molars. Int J Oral Maxillofac Surg 1989; 18:210–12.
El-Belasy FA, Dolwick MF. Arthrocenthesis for the treatment of temporomandibular joint closed lock: a review article. Int J Oral Maxillofac Surg 2007; 36:773–82.
Ellis E, Walker L. Treatment of mandibular angle fractures using two non–compression miniplates. J Oral Maxillofac Surg 1996; 54:846–71.
Ellis E. Further displacement of condylar process fractures after closed treatment. J Oral Maxillofac Surg 1999; 57:1307–16.
Eneroth CM. Histological and clinical aspects of parotid tumours. Acta Otolaringol (Suppl) 1964; 191:1–99.
Eneroth CM. Salivary gland tumours in the parotid gland, submandibular gland and the palate region. Cancer 1971;27:1415–18.
Epker BN. Modifications in the sagittal osteotomy of the mandible. J Oral Surg 1977; 35:157–60.
Eppley BL, Sclaroff A, Delfino JJ. Secondary management of the premaxilla in bilateral cleft lip and palate patients. J Oral Maxillofac Surg 1986; 44:987–98.
Eveson JW, Auclair P, Gnepp DR, El Naggar AK. Tumours of the salivary glands. In: Barnes L, Eveson JW, Reichart P, Sidranski D eds: WHO Classification Tumours: Pathology & Genetics of Head and Neck Tumours. Lyon: IARC 2005:212–15.
Farrar WB, McCarty WL. Inferior joint space arthrography and characteristics of condylar paths in internal derangements of the TMJ. Prosth Dent 1979; 41:548–55.
Faltrow (1917). Cited by Rowe (1971).
Fauchard P. Le chirurgien dentiste, ou, traité des dentes, Jean Mariette, Paris, 1725.
Fernandes R. Oral and maxillofacial surgery in the treatment of oral squamous cell cancer. The American perspective. BAOMS Symposium Nice 2011.
Figueroa AA, Polley JW, Friede H et al. Long–term skeletal stability after maxillary advancement using a rigid external distraction device in cleft maxillary deformities. Plast Reconstr Surg 2004; 114:1382–92.
Fonseca RJ, Dark PJ, Jefferson-Burkes E, Baker RD. Revascularisation and healing of onlay particulate autologous bone grafts in primates. J Oral Surg 1980; 38:572–77.
Fonseca RJ, Davis WH. Reconstructive Preprosthetic Oral and Maxillofacial Surgery. W B Saunders Company, Philadelphia, London, Toronto, 1986.
Fordyce G.L. L’ embrochage transmaxillaire seul ou associé dans 16 cas de fracture de la mâchoire supérieure. Rev Stomatol 1960; 61:542–44.
Fouchard M. Sur un nouvel appareil dans un cas difficile de fracture de la machoire inferieure. J Chir 1826 p327.
Freihofer HPM. The results after midface-osteotomies. J Max-fac Surg,1973; 1:30–36.
Freitag V, Fallenstein G. Über die sekundäre Osteoplastiek im Wechselgebiss bei Lippen-Kiefer-Gaumen-Spalten. Dtsch Z Mund-Kiefer-Gesichts-Chir 1983;8:343–59.
Friede H. Maxillary growth controversies after two–stage palatal repair with delayed hard palate closure in unilateral cleft lip and palate patients: perspectives from literature and personal experience. Cleft Palate Craniofac J 2007;44:129–35.
Gaggl H, Bürger H, Müller E, Chiari FM. A combined anterolateral flap and vascularized iliac crest flap in the reconstruction of extended composite defects of the anterior mandible. Int J Oral Maxillofac Surg 2007;36:849–53.
Gardner DA. A pathologist’s approach to the treatment of ameloblastoma. J Oral Maxillofac Surg 1984;42:161–66.
Gardner DG, Kessler HP, Morency R, Schaffner DL. The glandular odontogenic cyst: an apparent entity. J Oral Pathol 1988; 17:359–66.
Geraedts CTM, Borstlap WA et al. Long-term evaluation of bilateral cleft lip and palate patients after early secondary closure of premaxilla and repositioning. Int J Oral Maxillofac Surg 2007; 788:96.
Gillies H. Fractures of the malar–zygomatic compound, with a description of a new X–ray position. Br J Surg 1927; 14:651–56.
Gillies HG, Harrison SH. Operative correction by osteotomy of recessed malar maxillary compound in a case of oxycephaly. Brit J Plast Surg 1950; 2:123–127.
Gillies H, Rowe NL. L’ostéotomie du maxillaire supérieur evisagée essentiellement dans les cas de bec-de-lièvre totale. Rev Stomat 1956; 55:545–52.
Gilmer T L. A case of fracture of the lower jaw with remarks on treatment. Arch Dent 1887; 4:388–90.
Ginestet G. Le traitement des fractures maxilaire inférieur par fixateur externe. Schweiz Monatschr Zahnheilk 1958; 68:226–35.
Gorlin RJ. Potentialities of oral epithelium manifest by mandibular dentigerous cysts. Oral Surg Oral Med Oral Pathol 1957; 10:271–84.
Gorlin RJ, Goltz RW. Multiple nevoid basal cell epithelioma, jaw cysts and bifid rib. A Syndrome. New Eng J Med 1960; 262:908–11.
Gorlin RJ, Pindborg JJ. Syndromes of the Head and Neck. McGraw-Hill Book Comp, New York, 1964.
Gorlin RJ, Pindborg JJ, Cohen M M. Syndromes of the Head and Neck. 2nd ed, McGraw-Hill Book Comp, New York, 1976.
Gorlin RJ,Cohen MM, Levy LS. Syndromes of the Head and Neck.3rd ed., Oxford University Press, New York, Oxford, 1990.
Gortzak RATh, Latief BS, Lekkas C, Slootweg PJ. Growth characteristics of large mandibular ameloblastomas: report of 5 cases with implications for the approach of surgery. Int J Oral Maxillofac Surg 2001; 35:691–95.
Grossman L I. Endodontic Practice. 6th edition. Lea & Febiger, Philadelphia, 1965.
Gruss J S, Mackinnon SE. Complex maxillary fractures: role of buttress reconstruction and immediate bone grafts. Plast Reconstr Surg 1986; 78:9–22.
Guarda–Nardini L, Manfredini D, Ferronato G. Temporomandibular joint total replacement prosthesis: current knowledge and considerations for the future. Int J Oral Maxillofac Surg 2008; 37:103–10.
Gunning T B. The treatment of fractures of the lower jaw by Inter-dental splints. NY Med J 1866; 3:433.
Gurol ME, Burkes J, Jacoway J. Botryoid odontogenic cyst: an analysis of 33 cases. J Period; 1995:1069–73.
Güven O, Ikeslin U, Akal K. Incidence of cysts and tumors around impacted third molars. Int J Oral Maxillofac Surg 2000; 29:131–35.
Haers PE, Oechslin C, Sailer HF. Is wire osteosynthesis obsolete for fixation of Le Fort I osteotomies? Oral Surg Oral Med Oral Pathol 1999; 88:391–94.
Hagedorn W H. Über eine Modification der Hasenschartenoperation. Zentralbl Chir 1884; 11:756–58.
Hall HD, Link JL. Diskectomy alone and with ear cartilage interposition grafts in joint reconstruction. Oral Maxillofac Surg Clin North Am 1994; 6:287–94.
Härle F. Visor osteotomy to increase absolute height of the atrophied mandible A preliminary study. J Max-fac Surg 1975; 3:257–60.
Härle F.Atlas der Präprothetischen Operationen. Carl Hanser Verlag, München, Wien, 1987.
Harnisch H. Klinik und Therapie der Kieferzysten. Die Quintessenz Verlag, Berlin, 1971.
Heilmann H P. Radiation Oncology. Int J Rad Oncol Biol Phys, 1996; 35:207–17.
Henderson D, Jackson IT. Naso-maxilary hypoplasia- the Le Fort II osteotomy. Br J Oral Surg 1973; 2:77–93.
Henderson D, Jackson IT. Combined cleft lip revision, anterior fistula closure and maxillary osteotomy; a one–stage procedure. Brit J Oral Surg1975; 13:33–39.
Hertwig O. Über das Zahnsystem der Amphibien und seine Bedeutung für die Genese des Skelets der Mundhöhle. Arch Mikrosk Anat Suppl 1874; 11:98–100.
Hillerup S, Stolze A. Lingual nerve injury after third molar surgery I. Observations on sensory recovery with spontaneous healing. Int J Oral Maxillofac Surg 2007; 36:884–89.
Hillerup S Iatrogenic injury to the inferior alveolar nerve: etiology, signs and symptoms and observations on recovery. Int J Oral Maxillofac Surg 2008; 37:704–43.
Hinds E, Kent J. Genioplasty; The versatility of horizontal osteotomy. J Oral Surg 1969; 27:690–700.
Hinds E, Kent J. Surgical treatment of developmental jaw deformities. The CV Mosby Comp. St Louis, 1972.
Hochban W, Schuurmann R, Brandenburg U etc. Obstructive sleep apnea syndrome following surgery for mandibular prognathism. Int J Oral Maxillofac Surg 1996; 25:333–38.
Hofer O. Die operative Behandlung der alveolären Retraktion des Unterkiefers und ihre Anwendungsmöglichkeit für Prognathie und Mikrogenie. Zahn Mund Kieferheilkd 1942; 9:121–32.
Hofer O, Reichenbach E, Spreter von Kreudenstein T, Wannenbacher E. Lehrbuch der Klinischen Zahnheikunde. Band 1, Johan Ambrosius Barth Verlag, Leipzig, 1952.
Holmlund A, Hellsing G. Arthroscopy of the temporomandibular joint. A comparative study of arthroscopic and tomographic findings. Int J Oral Maxillofac Surg 1989; 17:128–33.
References (continue d)
Hopkins R . A Colour Atlas of Pre pros the tic O ral Surge r y. Wolf e Me dic al Publishe r s Ltd, 19 87
Hopp e nreijs T hJM, Freihof e r HPM, Sto e linga PJW e t al. Cond ylar re mo d e lling af te r L e For t I and bima xillar y os te otomies in patie nt s w ith ante r ior op e n bite A clinic al and radiologic al s tud y. Int J O ral Ma xillof ac Surg 199 8; 27 :81– 91
Hopp e nreijs T hJM, Sto e linga PJW, Grace KL , Robb e n CMG . Long– te r m evaluation of patie nt s w ith progressive cond ylar resor ption follow ing or thognathic surge r y. Int J O ral Ma xillof ac Surg 1999; 28: 411–18
Hot z MM, Gnoiski WM, Nussbaume r H e t al. Ear ly ma xillar y or thopae dic s in CLP c ases: guid e lines for surge r y. Cle f t Palate J 1978; 15: 40 5–11
Hovinga J, Boering G, Stegenga B Long-term results of nonsurgical management of cond ylar f rac tures in c hildre n. Int J O ral Ma xillof ac Surg 1999; 28: 4 29 –40
Hullihe n SP. A c ase of e longation of the und e r jaw. A m J D Sc 18 49; 9:157 – 65
Hunsuck E. A mo difi e d intraoral sagit t al split ting te chnique for cor re c tion of mandibular prognathism. J O ral Surg 19 68; 26:2 49 – 5 2
Hunte r J. Natural His tor y of the Human Te e th. J Johnson, London,17 7 1 Hu yb e r s TJ, Sto e linga PJW, d e Ko ome n HA , T id e man H. Mandibular ves tibuloplas tiy using f re e mucosal graf t . A 2–7 year evaluation. Int J O ral Surg 19 85; 14 :11–15
Iizuka T, L indqvis t C , Haillikane n D e t al. Seve re b one resor ption and os te oar throsis af te r miniplate fi xation of high cond ylar f rac tures. O ral Surg O ral Me d O ral Pathol 1991; 7 2: 40 0 – 07
Ire land VE. T he proble m of the clicking jaw. Pro c Roy So c Me d 19 51; 4 4 : 363 –74
Ir by W B. Surgic al cor re c tion of c hronic dislo c ation of the TMJ not resp onsive to conse r vative the rapy. J O ral Surg 19 57; 15: 307 –12
Iv y RH, Churc hill HR . T he ne e d of a s t andardize d surgic al and pathologic al classifi c ation of the tumour s and anomalies of d e nt al or igin. Trans A m D e nt A ss 1930; 7 :2 40
Iv y RH. B one graf ting for res toration of d e f e c t s of the mandible. Plas t Re cons tr Surg 19 51; 7 : 333 –41
Jack son IT, Munro IR , Salye r KE, W hit acke r L A . Atlas of Cranioma xillof acial Surge r y. T he C V Mosby Comp, St Louis, Toronto, London, 19 82
Jacobsson S , Holle nd e r L , L indb e rg S , L ar sson A . Chronic scle rosing os te omye litis of the mandible. Scintigrap hic and radiograp hic fi nding s. O ral Surg 1978; 45:167 –74
Jacobsson S. Dif f use scle rosing os te omye litis of the mandible. Int J O ral Surg 19 8 4 ; 13: 363 – 85
Jacoway JR , Howe ll F V, Te r r y BC . Ce ntral giant ce ll granuloma — an alte r native to surgic al the rapy. O ral Surg 19 8 8; 66;57 2
Jawd ynski FI Pr z ypad e k raka pie r wotne go s y zi. T z. raka skr ze lowe go Volkmanns W ycie cie nowot wor u w ra z z re ze ke yja te tnic g szjow ej i z yly szjowej we w ne tr znej. W y zdrow ie neie Ga z L e k 18 8 8; 28:5 30 – 35
Je nse n AD, Nikoghos yan A , W ind e muth - K iese lbac h e t al. Combine d treatme nt of malignant salivar y gland tumour s w ith inte nsit y – mo dulate d radiation the rapy (IMR T ) and c ar b on ions; COSMIC BMC . Cance r 2010; 10:5 46 – 50
Jime ne z DF, Barone CM. Ear ly treatme nt of c alvar ial cranios ynos tosis using e ndoscopic– assis te d minimally invasive te c hniques. Childs Ne r v Sys t 20 07; 23:1411–19
Je te r T S , Van Sicke ls JE, D olw ick MF. Mo difi e d te c hniques for inte r nal fi xation of sagit t al ramus os te otomies. J O ral Ma xillof ac Surg 19 8 4 ; 4 2:270 –7 2
Jones J, A mess TR , Robinson PD. Treatme nt of c hronic scle rosing os te omye litis of the mandible w ith c alcitonin: a re p or t of t wo c ases. Br J O ral Ma xillof ac Surg 20 0 5; 43: 17 3 –76
Joss U, Vasalli IM. St abilit y af te r bilate ral sagit t al split os te otomy advance me nt surge r y w ith r igid inte r nal fi xation: A s ys te matic revie w. J O ral Ma xillof ac Surg 20 0 9; 67 : 301–13
Jungling O Ro e nt ge nthe rapie c hir urgisc he r K rank heite n, L eipzig, 192 4 , p 237
Kaban L, Troulis et al. Antiangiogenic therapy with interferon alpha for giant cell lesions of the jaws. J Oral Maxillofac Surg 2002; 60:1103–11.
Kaban LB, Bouchard C, Troulis MJ. A protocol for management of temporomandibular joint ankylosis in children. J Oral Maxillofac Surg 2009; 67:1966–78.
Kakisi OK, Kechagia AS, Kakisis IK et al. Tuberculosis of the oral cavity: a systematic review. Eur J Oral Sci. 2010; 118:103–09.
Kamer L, Noser H, Schramm A, Hammer B. Orbital form analysis: problems with design and positioning of precontoured orbital implants. A serial study post–processed clinical CT data in unaffected orbits. Int J Oral Maxillofac Surg 2010; 39:666–72.
Kazanjian V H. Surgical operations as related to satisfactory dentures. Dental Cosmos 1924; 66:387–95.
Kazanjian VH, Converse JM. Surgical Treatment of Facial Injuries. Vol I & II. The Willliams &Wilkins Comp., Baltimore,1949,1959,1974.
Kearns G, Perrot DH, Sharma A et al. Placement of endosseous implants in grafted alveolar clefts. Cleft Palate Craniofac Surg,1997; 34:520–25.
Keen W D(1864). Cited by Rowe(1971)
Kent JN, Quin JH, Zide MF et al. Correction of alveolar ridge deficiencies with nonresorbable hydroxylapatite. J Am Dent Assoc 1982; 105:993–1001.
Kent JN, Misiek DJ, Akin RK et al. Temporomandibular joint condylar prosthesis: a ten–year report. J Oral Maxillofac Surg 1983; 41:245–54.
Khambay B, Nebel JC, Bowman J et al. 3D stereophoto–grammetric image superimposition onto 3D CT scan images: the future of orthognathic surgery. A pilot study. Int J Adult Orthod Orthogn Surg 2002; 17:219–26.
Kieran SM, McKusker M, Keogh I, Timon C. Selective fine needle aspiration of parotid masses. FNA should be performed in all patients older than 60 years. J Laryng Otol 2010; 124:975–79.
Killey HC, Kay L. Benign cystic lesions of the jaws. E & E Livingstone, Edinburgh, 1966.
Killey HC, Seward G R, Kay L W. An outline of Oral Surgery Part I&II. John Wright & Sons Ltd. Bristol, 1971.
Kilner TP. Cleft lip and palate repair technique. St Thomas Hosp Rep. 1937; 2:127.
Kingsley N W. A Treatise on Oral Deformities. H.K.Lewis, London 1880.
Klapp R, Schröder H. Die Unterkieferschussbrüche. Verlag von Hermann Meuser, Berlin 1917.
Klestadt W. Gesichtsspalten Zysten. Zbl Chir 1913; 38:1489.
Kocher T. Über Radicalheilung des Krebses. Dtsch Z Chir 1880; 13:134–66.
Konig F. Über die Berechtigung frühzeitiger blutiger Eingriffe bei subcutanen Knochenbruchen. Arch Klin Chir. 1905; 76: 23.
Koomen de HA. A prosthetic view on vestibuloplasty of the mandible. J Oral Surg 1977; 6:38–41.
Koorneef L, Zonneveld F W. The role of direct multiplane high resolution CT in the assessment and management of orbital trauma. Radiol Clin N Am 1987; 25:753–66.
Kostecka F. Die chirurgische Therapie der Progenie. Zahnärztl Rdsch 1931; 16.
Kronfeld R. Histopathology of the teeth and their surrounding structures. Lea & Febiger, Philadelphia, 1933.
Kufner J. Nove metody chirurgickeko leceni otevreneho skusu. Cs Stomatol 1960; 60:387–94.
Kugelberg C F, Ahlström U, Ericson S et al. Periodontal healing after impacted lower third molar surgery in adolescents and adults: a prospective study. Int J Oral Maxillofac Surg 1991; 20:18–24.
Kuijpers SC, de Jong E, Hamdy NA, van Merkesteyn JP. Initial results of the treatment of diffuse sclerosing osteomyelitis of the mandible with biphosphonates. J Cranio–Maxillofac Surg 2011;39: 65–68.
Kunkel M, Kleis W, Morbach T, Wagner W. Severe third molar complications including death–lessons from 100 cases requiring hospitalization. J Oral Maxillfac Surg 2007; 65:1700–06.
Kuttenberger JJ, Hardt N. Long–term results following miniplate eminoplasty for the treatment of recurrent dislocation and habitual luxation of the temporomandibular joint. Int J Oral Maxillofac Surg 2003; 32:474–79.
Lambourne A. L’intervention operatoire dans les fractures. Malcine, Paris, 1907.
Lane W.A. The Operative treatment of Fractures. Medical Publishing Co, London, 1914.
Lange de J, Akker van de HP, Veldhuijzen van Zanten HA et al. Calcitonin therapy in central giant cell granuloma of the jaw: a randomized double blind placebo-controled study. Int J Oral Maxillfac Surg 2006; 35:791–95.
Lansdale E F. Instrument for treating fractures of the jaw. London Med. Gaz,1833;7:565.
Laskin DM The etiology of the myofacial pain dysfunction syndrome. JADA 1969;79:147–53.
Lanz W. Discitis mandibularis. Zentralbl Chir 1909; 36:289.
Lau SL, Samman N. Recurrence related to treatment modalities of unicystic ameloblastoma: a systematic review. Int J Oral Maxillofac Surg 2006; 35:681–90.
LeClerc G, Girard G. Un nouveau procédé de butée dans le traitment chirugical de la luxation récidivante de la mânchoire inférieure. Mém Acad Chir 1943; 69:457.
Lee N, Puri DR, Blanco AL, Chao KS. Intensity-modulated radiation therapy in head and neck cancers: an update. Head Neck 2007; 29:387–400.
Le Fort R. Etude expérimental sur les fractures de la mâchoire supérieure. Rev Chir 1901; 23:208–227, 360–379, 479–507.
Liao YF, Cole TJ, Mars M. Hard palate repair timing and facial growth in unilateral cleft lip and palate: A longitudinal study. Cleft Palate Craniofac J 2006; 43:547–58.
Lindauer SJ, Laskin DN, Tüfekci E et al. Orthodontists and surgeons opinions on the role of third molars as a cause of dental crowding. Am J Orthod Dentofacial Orthop 2007; 132:43–48.
Lizuka T, Lindqvist C, Hallikainen D, Mikkonen P, Paukka P, Oral Surg. 1991; 72,400–407.
Lore JM. An Atlas of Head and Neck Surgery WB Saunders Company, 1962.
Luhr HG. (1968) “Zur stabilen Osteosynthese bei Unterkieferfracturen. Dtsch Zahnärztl Z 1968; 23:754.
Luhr HG. Die Kompressionosteosynthese bei Unterkieferfracturen. Hauser Verlag, München, 1972.
Lucas RB, Pathology of Tumours of the Oral Tissues. J & A Churchill Ltd, London,1964.
MacIntosh RB, Obwegeser HL. Preprosthetic surgery: a scheme for its effective employment. J Oral Surg 1963; 25:397–413.
MacIntosh RB, Henny FA. A spectrum of application of autogenous costochondral grafts. J Maxillofac Surg 1977; 5:257–67.
MacIntosh RB. Aggressive surgical management of ameloblastoma. In: Assael LA, ed. Benign Lesions of the Jaws Vol III. Oral and Maxillofacial Surgery Clinics of North America 1991:73–97.
Magitot E. Mémoire sur les kystes des mâchoires. Arch Gén Méd 1872; 2:399–414 & 681–99.
Malassez L. Sur l’existence d’amas épithelieux autour de la racine des dents chez l’homme adults et l’état normal. Arch Physiol 1885; 17:29–49.
Malassez L. Sur le role debris epitheliaux paradentaires. Arch Physiol 1885; 17:129–48.
Manwaring JGR Replacing depressed fractures of the malar bone. JAMA 1913; 60: 278–79.
Markus AF, Delaire J, Smith WP. Facial balance in cleft lip and palate I Normal development and cleft palate. II Cleft lip and palate and secondary deformities. Br J Oral Maxillofac Surg, 1992; 30:287–95 & 296–304.
Markx RE. Pamidronate (Aredia) and Zoledronate (Zometa) induced avascular necrosis of the jaws: a growing epidemic. J Oral Maxillofac Surg. 2003; 61:1115–17.
Martin HE, Del Valle B, Ehrlich H, Cahan WG. Neck Dissection. Cancer 1951; 4:441–99.
Matas R. Fracture of the zygomatic arch. New Orleans Med Surg J 1896; 48:139.
Mayrhofer B. Die Praxis der Zahnextraction einschlieslich der örtlichen Schmerzbetäubung. J.F.Bergman Verlag, München and Wiesbaden, 1922.
McCain JP, Sanders B, Koslin et al. Temporomandibular joint arthroscopy — a 6-year multicenter retrospective study of 4831 joints. J Oral Maxillofac Surg 1992; 50:926–30.
McCarty W L, Farrar W B. Surgery for internal derangements of the temporomandibular joint. J Prosth Dent 1979; 42:191–96.
McFarland J. The treatment of Mixed Tumours of the salivary glands by Roentgen rays and Radium. Am. J Roent Rad Therapy 1941; 45:506–508.
McFarland J. The mysterious mixed tumours of the salivary glands. Surg. Gynec. & Obst. 1943;76: 23–24.
McLeod AM, Robinson DW. Reconstruction of defects involving the mandible and floor of the mouth by free osseocutaneous flaps derived from the foot. Br J Plast Surg 1982; 35:239–46.
McNeill RW, Hooley JR, Sundberg RI. Skeletal relapse during intermaxillary fixation. J Oral Surg. 1973; 31:212–27.
Mercier P, Precious D. Risks and benefits of removal of impacted third molars. Int J Oral Maxillfac Surg 1991; 21:21–27.
Mercuri LG. Alloplastic temporomandibular joint reconstruction. Oral Surg 1998; 85:631–37.
Merkesteyn van JH, Groot RH, Bras J et al. Diffuse sclerosing osteomyelitis of the mandible: a new concept of its etiology. Oral Surg 1990; 70:414–19.
Merrill R G. Historical perspectives and comparisons of TMJ surgery for internal disk derangements and arthroplasty. J Craniomand Pract 1986; 4:74–84.
Merville L. Multiple dislocations of the facial skeleton. J.Max–fac Surg1974; 2:187–200.
Mettes TG, Nienhuis MEI, Sanden WJM van der et al. Interventions for treating asymptomatic impacted wisdom teeth in adolescents and adults. Cochrane Database Syst Rev 2005; 18:2.
Meyer AW, Median anterior maxillary cysts. JADA 1931; 18:1851–77.
Michelet F V, Deymes J, Dessus B. Osteosynthesis with miniaturized screwed plates in maxillofacial surgery. J Max–fac Surg 1973; 1:79–84.
Mickulicz J, Kümmel W. Krankheiten des Mundes. Verlag von Gustav Fischer, Jena, 1898.
Millard DR. A radical rotation in single harelip. Am J Surg 1959; 95:318–22.
Millard DR. Rotation-advancement principle in cleft lip closure. Cleft Palate J 1964; 1:246–52.
Misch J, Rumpel C. Die Kriegsverletzungen der Kiefer und die angrenzenden Teile. Hermann Meusser Verlag, Berlin, 1916.
Moloney F. Internal derangements of the temporomandibular joint. A review. Ann Roy Austr Coll Dent Surg 1984; 8:106–26.
Montonen M, Iizuka T, Hallikainen D, Lindquist C. Decortication in the treatment of diffuse sclerosing osteomyelitis of the mandible. Retrospective analysis of 41cases between 1969 and 1990. Oral Surg 1993; 75:5–11.
Moon H (1874). Cited by Rowe (1971).
Morris J H. Biphase connector, external splint for reduction and fixation of mandibular fractures. Oral Surg 1949; 2:1382–98.
References (continue d)
Moses JJ, Poke r I. TMJ ar hroscopic surge r y : an analysis of 237 patie nt s. J O ral Ma xillof ac Surg 19 89; 47 :79 0 – 9 4
Mullike n JB , Fe r raro NF, Ve nto AR . A re trosp e c tive analysis of grow th of the cons tr uc te d cond yle – ramus in c hildre n w ith he mif acial microsomia . Cle f t Palate J 19 89; 26: 312–17
Murakami K , Takatoki O. Te mp oromandibular joint ar throscopy by inf e rolate ral approac h. Int J O ral Surg 19 86; 15: 410 –17
Myr haug H. Ne w me tho d of op e ration for habitual dislo c ation of mandible A c t a O dontol Sc and 19 51; 9:2 47 – 61
Nakamura N, Higuc hi Y, Mit su yasu T e t al. Grow th c harac te r is tic s of ame loblas toma involving the alve olar ne r ve: A clinic al and his tologic al s tud y O ral Surg O ral Me d O ral Pathol 20 01; 91:557 – 62
Nit zan DW, Dolwick MF, Mar tinez GA Temporomandibular joint ar throcenthesis: a simplifi e d treatme nt for seve re , limite d mouth op e ning. J O ral Ma xillof ac Surg 1991; 49:1163 – 67
Nit zan DW, Mar mar y Y. T he “anc hore d disc p he nome non”: a prop ose d e tiolog y for sud d e n onse t , seve re and p e r sis te nt close d lo ck of the TMJ J O ral Ma xillof ac Surg 1997; 55:797 – 8 02
Nit zan DW, Et sion I. A dhesive force: the und e r lying c ause of disc anc horage to the fossa and/or e mine nce in the te mp oromandibular joint — a ne w conce pt Int J O ral Ma xillof ac Surg 20 02; 31:9 4 – 99
Nordin K E, Johanson B. Freie K no c he ntransplant ation b ei D e f e k te n im A lve olar kamm nac h kie f e ror thopädisc he r eins te llung d e r Ma xilla b ei L ipp e n - K ie f e r- Gaume nspalte n. In: For t schr it te d e r K ie f e r- und Gesic ht sChir urgie. Sc huc hardt K , e ditor. T hie me Ve r lag, Stut t gar t 19 55; 1:168:7 1
Nove r ra z AEM, Kuijp e r s- Jag tman AM, Mar s M e t al. T iming of hard palate closure and d e nt al arc h re lationship in unilate ral cle f t lip and palate patie nt s: a mixe d - longitudinal s tud y. Cle f t Palate Craniof ac J 1993; 30: 391– 9 6
Nut ting CM, Morden JP, Harring ton KJ et al Parotid –sparing intensit y modulated ve r sus conve ntional radiothe rapy in head and ne ck c ance r PA SP OR T ): a p hase 3 multice ntre randomize d controlle d tr ial. L ance t/O ncolog y 2011;12:127 – 36
O’Br ie n BM, MacL e o d AM, Hay hur s t JW, Mor r ison WA . Successf ul transf e r of a large island flap f rom the groin to the fo ot by microvascular anas tomosis. Plas t Re cons tr Surg 197 3; 5 2:27 1–78
O bwe gese r HL . Die tot ale Mundb o d e nplas tik . Sc hweiz Monat schr Z ahnheilk 19 63; 3:565–7 1
O bwe gese r HL . Eingr if f e am O b e r kie f e r zur Kor re k tuur d es proge ne n Zus t andbild es. Sc hweiz Monat sc hr Z ahnme d 19 65; 75: 365–74
O bwe gese r HL . Surgic al cor re c tion of the small and re tro displace d ma xillae Plas t Re cons tr Surg 19 69; 43: 351– 59
Obwegeser HL Die einseitige Vorb ewegung des Ob erkiefers und Rückb ewegung d es Unte r kie f e res zur kor re k tuur d e r e x tre me n proge nie. Sc hweiz Monat sc hr Z ahnheilk 1970; 8 0:5 47 – 56
O bwe gese r HL . Surgic al cor re c tion of ma xillar y d e for mities. In Cle f t L ip and Palate — Surgic al, D e nt al and Sp e e ch A sp e c t s. Grabb WC , Rose ns tein S W, Bzo ch KR , e ditor s. Fir s t e dition L it tle , Brow n, B os ton,197 1:515– 56
O bwe gese r HL . Cor re c tion of jaw p osition in an adult cle f t patie nt . D t sc h Z ahnär t zl Z ,197 3; 28:68 8 – 9 4
O hnishi M. A r throscopy of the te mp oromandibular joint . J Jpn Stomatol So c 1975; 4 2:207 –13
O r tiz– Monas te r io F Se r rano A Bar re ra G . A s tud y of untreate d adult cle f t palate patie nt s. J Plas t Re cons tr Surg 19 66; 38: 36 –41
Paré A mbroise. Dix livres d e c hir ugie ( Te n b o ok s on surge r y) 1863
Padayac he e A , van W ijk C W. Two c ys tic lesions w ith f eatures of b oth the b otr yoid o dontoge nic c ys t and the ce tral muco e pid e r moid tumour : sialo –o dontoge nic c ys t? J O ral Pathol 19 87; 16: 499 – 504
Pand e r s AK , Had d e r s HN. Solit ar y ke rato c ys t s of the jaw s. J O ral Surg 19 69; 27 :931– 38
Par t sc h C . Üb e r K ie f e rc ys te n. D t sc h Msc hr Z ahnheilk 1892; 7 :27 1– 304
Partsch C Zur Behandlung der Kiefercysten. Dtsch Mschr Zahnheilk 1910; 28:252–60.
Paulus GW, Steinhauser EW. A comparative study of wire osteosynthesis versus bone screws in the treatment of mandibular prognathism. Oral Surg Oral Med Oral Pathol 1952; 54:2–6.
Perrott DH, Umeda H, Kaban LB. Costochondral graft construction/reconstruction of the ramus/condyle unit: long–term follow–up. Int J Oral Maxillofac Surg 1994; 23:321–28.
Pfeifer G. Über ein entwicklungsgeschichtlch begründetes Verfahren des Verschlusses von Lippenspalten. Dtsch Zahn-Mund-Kieferheilk.1970; 54:69–77.
Philipsen HP. Om keratocyster (kolesteatomer) i kaeberne. Tandlaegebladet 1956; 60:963–80.
Philipsen HP. Keratocystic odontogenic tumor. In: Barnes L, Eveson JW, Reichart P, Sidransky D ,eds. Head and Neck Tumours, WHO Classification of Tumours. IARC Press, Lyon, 2005,pp 306–07.
Philipsen HP, Reichart PA. Unicystic ameloblastoma. A review of 193 cases from the literature. Oral Oncol 1998; 34:317–25.
Pichler H, Trauner R. Die alveolarkammplastik. Öst Zeitschr Stomatol 1930; 28:675.
Pindborg JJ. A calcifying epithelial odontogenic tumour. Cancer 1958; 11:838–43.
Pindborg JJ, HansenJ. Studies on odontogenic cyst epithelium. Acta Path Microbiol Scand 1963; 58:383–94.
Pindborg JJ, Kramer IRH. Histological Typing of Odontogenic Tumours, Jaw Cysts, and Allied Lesions. World Health Organisation. Springer Verlag, Berlin etc, 1971.
Pogrel MA, Renaut A, Schmidt B, Ammar A. The relationship of the lingual nerve to the mandibular third molar region: An anatomic study. J Oral Maxillofac Surg 1995; 53:1178–81.
Pogrel MA. Biphosphonates and bone necrosis. J Oral Maxillofac Surg 2004; 62:391–92.
Pons J, Duboscq JC, Sadaia JB. René Le Fort, de Lille. Ann Chir Plast Esthet 1988; 33:199–200.
Posnick JC, Tiwana PS. Cleft-Orthognatic Surgery. In: Cleft Lip and Palate, Berkowitz S editor Springer Verlag, Berlin, Heidelberg, New York, 2006.
Poulton DR, Ware WH. Surgical-othodontic treatment of severe mandibular retrusion. Am J Orthod 1971; 59:244–65.
Precious DS, Lanigan DT, editors. Risks and Benefits of Orthognathic Surgery. Oral and Maxillofacial Surgery Clinics of North America. WB Saunders Company, Philadelphia, London, Toronto, 1997.
Prinsell JR. Maxillomandibular advancement surgery in a site-specific treatment approach for obstructive sleep apnea in 50 consecutive patients. Chest 1999; 116:1519–29.
Profitt WR,White RP. Treatment of severe malocclusions by correlated orthodontic–surgical procedures. Angle Orthod 1970; 40:1–10.
Profitt WR, Philips C, Turvey TA. Stability following superior repositioning of the maxilla by Le Fort I osteotomy. Am J Orthod Dentofacial Orthop 1991; 6:211–25.
Propper RH. Simplified ridge extension using free mucosal grafts. J Oral Surg 1964; 2:469–74.
Pruzansky S. The multi–discipline approach to the treatment of cleft palate in children: Integration of multi–professional resources through a program of basic research. J Int College Surg. 1955; 24:827–51.
Puelacher WC, Waldhart E. Miniplate eminoplasty: a new surgical treatment for TMJ-dislocation. J Cranio-Maxillofac Surg 1993; 21:176–78.
Ramer M, Valauri D. Multicystic lateral periodontal cyst and botryoid odontogenic cyst. Multifactorial analysis of previously unreported series and review of the literature. New Y St Dent J 2005; 71:47–51.
Randall P, McCarty JG, Wray RC. History of the American Association of Plastic Surgeons. Plast Reconstr Surg 1996; 97:1254–92.
Rankow RM, Polayes IM. Diseases of the salivary glands. WB Saunders, Philadelphia, 1976.
Rauch S. Die Speichseldrusen des Menschen. Georg Thieme, Stuttgart, 1959.
Rehrman A. Beitrag zur alveolarkammplastik am Unterkiefer. Zahnärztl Rdsch 1953; 62:505.
Reichenbach E. Traumatologie im Kiefer-Gesichts-Bereich. Johan Ambrosius Barth, Leipzig, 1969.
Regulskiy M. Statistics and clinical features of cancer of the lip Dissertation Moscow 1894.
Resnick CM, Kaban L, Troulis MJ. Minimally invasive orthognathic surgery. Facial Plast Surg 2009; 25:49–62.
Rheinwald U. Zahnärztliche Chirurgie. Johann Ambrosius Barth, München, 1958.
Riley RW, Powell NB, Guileminault C. Inferior mandibular osteotomy and hyoid myotomy suspension for obstructive sleep apnea: A review of 555 patients. J Oral Maxillofac surg 1984; 47:159–64.
Riley RW, Powell RB, Guileminault C. Obstructive apnea syndrome; surgical protocol for dynamic upper airway reconstruction. J Oral Maxillofac Surg 1993; 51:742–72.
Ring ME. Dentistry an illustrated history. Abradale Press Harry N Abrams, inc, New York, 1985.
Robbins KT, Medina JE, Wolfe GT et al. Standardised neck dissection terminology. Official report of the Academy’s committee for head and neck surgery and oncology. Arch Otolaryngol Head Neck Surg 1991; 117:601–05.
Roberts W R. The case for mandibular plating. Br J Oral Surg 1964; 1:200–04.
Robinson L, Martinez MG. Unicystic ameloblastoma; A prognostically distinct entity. Cancer 1977; 40:2278–85.
Robinson M. Prognathism corrected by open vertical condylotomy. J S California Dent Ass 1956;24:22–26.
Rogers SN, Lowe D, Brown JS, Vaughan ED. A prospective quality of life study for patients treated with primary surgery for oral cancer. Head Neck 1999; 21:394–401.
Rogers SN, Forgie S Lowe L et al. Development of the international classification of functioning, disability and health as a brief head and neck cancer patient questionnaire. Int J Oral Maxillofac Surg 2010; 39:975–82.
Röntgen WC. Eine neue Art von Strahlen. Sitsungsberichte der Wurzburger Physic–medic Dec 28.1895.
Ross RB. Treatment variables affecting facial growth in complete unilateral cleft lip and palate. Part 5: Timing of palatal repair. Cleft Palate J 1987: 24:54:63.
Roychoudhury A, Parkash H, Trikha A. Functional restoration by gap arthroplasty in temporomandibular joint ankylosis: a report of 50 cases. Oral Surg 2001; 91:388–89.
Rowe N L. The history of the treatment of maxilla-facial trauma. Ann Roy Coll Surg Engl 1971; 49:329–49.
Rowe NL. Ankylosis of the temporomandibular joint. J Roy Coll Surg Edinb 1982; 27:209–11.
Rowe NL, Killey HC. Fractures of the Facial Skeleton. First and second edition, Churchill Livingstone, Edinburgh, London, 1955, 1968.
Rozema FR. Resorbable Poly (L-lactide) bone plates and screws Ph.D.Thesis, 1991, University of Groningen.
Rutt AL, Hawkshaw MJ, Lurie D, Sataloff RT Ear Nose Throat J 2011; 90:174–84.
Ryan JT, El–Naggar AK, Huh W et al. Primary surgery in the management of mucoepidermoid carcinoma in children. Head Neck 2011(Epub ahead of print).
Quejada JG, Bell WH, Kawamura H et al. Skeletal stability after inferior maxillary repositioning. Int J Adult Orthod Orthogn Surg 1987; 2:67–74.
Sailer H F, Parajola GF. Orale Chirurgie. Georg Thieme Verlag, Stuttgart, New York, 1996.
Satow S, Slagter AP, Stoelinga PJW, Habets LL. Interposed bone grafts to accomodate endosteal implants for retaining mandibular overdentures. A 1–7 years follow-up study. Int J Oral Maxillofac Surg 1997; 26:358–64.
Saunders R, Mayou BJ. A new vascularised bone graft transferred by microvascular anastomosis as a free flap. Br J Surg 1979; 66:787–88.
Schendel SA, Eisenfeld JH, Bell WH, Epker BN. Superior repositioning of the maxilla: Stability and soft tissue osseous relations. Am J Orthod 1976; 70:663–74.
Schettler D. Sandwich technique with cartilage transplant for raising the alveolar process in the lower jaw. Fortschr Mund Kiefer Gesichtschirurgie 1976; 20:61–63.
Schliephake H, Jamil MU. Prospective evaluation of quality of life after oncologic surgery for oral cancer. Int J Oral Maxillfac Surg 2002; 31:427–33.
Schmid E. Die Osteoplastik bei Lippen-Kiefer-Gaumenspalten. Langenbecks Arch Klin Chir, 1960; 295:868–76.
Schuchardt K. Ein beitrag zur chirugischen Kieferorthpädie unter Berücksichtigung ihrer Beteutung für die Behandlung angeborener und erworbener Kieferdeformitäten bei Soldaten. Dtsch Zahn-Mund-Kieferheilk 1942; 9:73–??.
Schuchardt K. Die Epidermistransplantation bei der Mundvorhofplastik. Dtsch Zahnärztl Zeitschr 1952; 7:364–369.
Schwartz L. A temporomandibular joint pain-dysfunction syndrome. J Chron Dis 1956; 3:284–93.
Schweckendiek H. Zur zweiphasischen Gaumenspaltoperation bei primärem Velumvecschluss. In Fortschritte der Kiefer-und Geschtschirurgie, vol 1, Schuchardt K and Wassmund W, editors, Thieme Verlag, Stuttgart, 1955;73.
Schweckendiek H. Ergebnisse bei Lippen-Kiefer-Gaumenspalt-operationen mit der primären Veloplastiek. In: Fortschritte der Kiefer-und Geschtschirurgie, vol 4, Schuchardt K editor, Thieme Verlag, Stuttgart, 1958;167.
Schweckendiek W. Die zweizeitige Gaumenplastiek. In Fortschritte der Kiefer-und Geschtschirurgie, vol 16–17 Schuchardt K , Steinhardt G, Schwezer N, editors, Thieme Verlag, Stuttgart,1973;140–144.
Scottish Intercollegiate Guidelines Network. Diagnosis and management of Head and Neck Cancer, Edinburgh, 2006:8.
Semb G. A study of facial growth in patients with bilateral cleft lip an palate treated by the Oslo CLP team. Cleft Palate Craniofac J 1991; 28:22–39.
Semb G, Shaw WC. Pharyngeal flap and facial growth. Cleft Palate J,1990; 27:217–24.
Shah JP. Head and Neck Surgery.2nd. Ed. Mosby-Wolfe Baltimore, London, 1996.
Shear M. Cysts of the Oral Regions. John Wright & Sons Ltd, Oxford, 1976, 1983, 1992.
Shear M, Speight PM. Cysts of the Oral and Maxillofacial Regions. Blackwell, Munksgaard, Copenhagen, 2007.
Shepherd JP. The third molar epidemic. Br Dent J 1993; 174:85.
Sherman L O. Poor Functional Results in the Treatment of Fractures. Transactions of the section of Orthopaedic Surgery of the American Medical Association, 1922 p71.
Sicher H, Tandler J . Anatomie fur Zahnärzte. Springer Verlag, Wien, 1928.
Sicher H. Über das Zahnziehen. Urban & Schwarzenberg, Berlin and Wien, 1937.
Silvennoinen U, Iizuka T, Lindquist C, Oikarinen K. Different patterns of condylar fractures: an analysis of 382 patients in a 3-year period. J Oral Maxillofac Surg 1992; 50:1032–37.
Simon ENM, Merkx MAW, Vuhula E et al. Odontogenic myxoma: a clinicopathological study of 33 cases. Int J Oral maxillofac Surg 2004; 33:333–37.
Small IA, Waldron CA. Ameloblastomas of the jaw. Oral Surg Oral Med Oral Pathol 1955; 8:281–97.
Smets L M H, van Damme P A, Stoelinga PJW. Non-surgical treatment of condylar fractures in adults: a retrospective analysis. J Cranio-Maxillofac Surg 2003; 31:162–67.
Snell JA, Dott WA. Internal fixation of certain fractures of the mandible by bone plating. Plast Reconstr Surg 1969; 43:281–86.
References (continue d)
Solis Cohe n J T he surgic al treatme nt of lar yngeal c ance r. Trans A m L ar yngol A sso c 19 01; 2 2:75– 87
Soudijn ER , Huf f s t adt AJC . Cle f t palates and mid dle ear e f f usions in babies Cle f t Palate J 1975; 2 29 – 33
Sou yr is F, Carave l JB , Re ynaud JP. Os té otomies inte r mé diaires d e l’e t age moye n d e la f ace. A nn Chir Plas t ,197 3; 18:149 – 5 4
Sout ar DS , T iwar i R . E xcision and Re cons tr uc tion in Head and Ne ck Cance r, Churchill L iving s tone , Edinburgh & London, 199 4
Sp eight PM, Bar re t t AW Prognos tic f ac tor s in malignant tumour s of the salivar y glands Br J O ral Ma xillof ac Surg 20 0 9; 47 :5 87 – 93
Spiessl B. Er f ahr unge n mit d e m AO - B es te ck b ei K ie f e r br uc hb e handlunge n Sc hweiz Msc hr Z ahnme d 19 69; 79:112–13
Spiessl B. Os te os ynthese b ei sagit t ale r Os te otomie nach O bwe gese r- Dal Pont For t sc hr, K ie f e r– und Gesic ht sc hir 1974 ; 18:12 4 – 37
St andish SM, Shaf e r WG . T he late ral p e r io dont al c ys t . J Pe r io d 19 5 8; 29:27 – 33
St ar shak T hJ, Sand e r s B. Pre pros the tic O ral and Ma xillof acial Surge r y. T he C V Mosby Comp. St Louis, Toronto, London, 19 8 0
Stein S , D unsc he A , Claudius- Ge llr ic h N e t al. O ne or t wo -s t age palate closure in patie nt s w ith unilate ral cle f t lip and palate: Compar ing ce p halome tr ic and o cclusal outcomes. Cle f t Palate Craniof ac J 20 07; 4 4 :13 –2 2
Steinb e rg B , Pad wa BL , B oyne Ph, K aban L . St ate of the ar t in oral and ma xillof acial surge r y : Treatme nt of ma xillar y hyp oplasia and ante r ior palat al and alve olar cle f t s. Cle f t Palate Craniof ac J 1999; 36:283 – 91
Steinhause r E W. His tor ic al d eve lopme nt of or thognathic surge r y. J CranioMa xillof ac Surg 199 6; 25:185–204
Ste llmach R . Von d e r Id e e d e r pr imäre n Os te oplas tik b ei L ipp e n - K ie f e rGaume n -Spalte n zur Realit ät nac h A blauf eines Jahr ze hnt s. In:For t sc hr it te d e r K ie f e r- und Gesichtc hir urgie , vol16 –17 Scuc hardt K , Steinhardt G , Sc hwe nze r N, e ditor s, T hie me Ve r lag, Stut t gar t , 197 3; 83 – 86
Sto e linga PJW. Re cur re nces and multiplicit y of c ys t s. In: K ay LW, e d Transac tions 4th ICOS , 197 1, Munk sgaard, Cop e nhage n 197 3 pp 7 7 – 8 0
Sto e linga PJW, Pe te r s JH. A note on the or igin of ke rato c ys t s of the jaw s Int J O ral Surg 197 3; 2: 37 –4 4
Sto e linga PJW, d e Ko ome n HA , T id e man H, Hu yb e r s TJ. A reappraisal of the inte r p ose d b one graf t augme nt ation of the atrop hic mandible. J Ma x-f ac Surg 19 83; 11:107 –12
Sto e linga PJW e d. Pro ce e ding s Conse nsus Conf e re nce: T he re lative roles of ves tibuloplas t y and r idge augme nt ation in the manage me nt of the atrop hic mandible. Q uintesse nce Publishing Co ,Inc . Chic ago, B e r lin, Rio d e Janeiro, Tok yo, 19 8 4
Sto e linga PJW. Pre pros the tic re cons tr uc tive surge r y. In Pe t te r son LJ, e d Pr inciples of oral and ma xillof acial surge r y, vol 2 L ippincot t W illiams and W ilkins, Philad e lp hia, 1992 p 1169 –207
Sto e linga PJW. Long- te r m follow - up on ke rato c ys t s treate d according to a d e fi ne d proto col. Int J O ral Ma xillof ac Surg 20 01; 30:14 –20
Stricker M, van der Meulen JC, Raphael B, Mazzaola R Craniofacial Malformations Churchill L iving s tone , Edinburg, London, Me lb our ne and Ne w Yor k , 199 0
Subramanian S ,Chiesa F, Lyubaev V e t al. T he evolution of surge r y in the manage me nt of ne ck me t as t ases A c t a O tolar yng It al 20 0 6; 26; 30 9 –16
Suurone n R . Bio d e grad eable , se lf – reinforce d p olylac tid e plates and scre w s in the fi xation of os te otomies. Ph D. T hesis, 1992, Unive r sit y of He lsinki
Suurone n R . Pe r sonal communic ation, 2010
Swe nne n GRJ, Bar th EL , Eulze r C , Sc hut yse r F. T he use of a ne w 3D splint and double C T sc an pro ce dure to ob t ain an accurate anatomic vir tual augme nte d mo d e l of the skull. Int J O ral Ma xillof ac Surg 20 07; 36:146 – 5 2
Takahashi T, Inai T, Ko c hi S e t al. Long– te r m follow – up on d e nt al implant s place d in a graf te d alve olar cle f t : evaluation of alve olar b one height . O ral Surg O ral Pathol O ral Me d O ral Radiol 20 0 8; 10 5:297 – 302
Taylor GI, Townend P. Composite free flap and tendon transfer. Br J Plast Surg 32; 170–83.
Terheyden H, Menzel C, Wang H et al. Prefabrication of vascularised bone grafts using recombinant human osteogenic protein-1:part 3:dosage of rhOP-1, the use of external and internal scaffolds. Int J Oral Maxillofac Surg 2004; 33:164–72.
Terry BC, Albright JE, Baker RD. Alveolar ridge augmentation in the edentulous maxilla with use of autogenous ribs. J Oral Surg 1974; 32:429–34.
Terry BC. Personal communication 1983.
Tessier P, Guiot G, Rougerie J et al. Osteotomies cranio-naso-orbital faciales. Hypertelorisme. Ann Chir Plast 1967; 12:103–18.
Tessier P. Ostéotomies totales de la face: Syndrom de Cruzon, syndrom d’Apert; oxycéphalies, turricéphalies. Ann Chir Plast 1967; 12:273–78.
Tetsch P, Wagner W. Die operatieve Weisheitszahnentfernung. Carl Hanser Verlag, Munchen, Wien, 1982, 1985.
Thackray AC, Sobin LH. Histological typing of salivary gland tumours. Int classification of Tumours. No.7 WHO, Geneva, 1972.
Thackray AC, Lucas RB. Tumours of the major salivary glands. Atlas of Tumour Pathology. Second series. Fascicle 10. Washington DC, Armed Institute of Pathology, 1974.
Thiersch C. Über die feineren anatomischen Veranderungen bei aufheilung von Haut auf Granulationen. Arch Klin Chir 1874.
Tideman H. A technique of vestibuloplasty using a free mucosal graft from the cheek. Int J Oral Surg 1972; 1:76–80.
Thoma KH, Goldman HM. Odontogenic Tumors, a classification based on observations of the epithelial, mesenchymal and mixed varieties. Am J Pathol 1946;22:433–71.
Tomes J. On the reconstruction and application of forceps for extracting teeth. London Med.Gaz 1841;2: 424–30.
Topazian R G, Goldberg M H. Management of Infections of the Oral and Maxillofacial Regions. W B Saunders Comp, Philadelphia, 1981.
Trauner R. Alveoloplasty with ridge extensions on the lingual side of the lower jaw to solve the problem of a lower dental prosthesis. Oral Surg 1952; 5:340–46.
Trauner R, Obwegeser HL. The surgical correction of mandibular prognathism and retrognathia with consideration of genioplasty. Part I Surgical procedures to correct mandibular prognathism and reshaping of chin. Oral Surg Oral Med Oral Pathol 1957; 10:677–89.
Trauner R, Obwegeser HL. The surgical correction of mandibular prognathism and retrognathia with consideration of genioplasy. Part II. Operating methods for micrognathia and distocclusion. Oral Surg Oral Med Oral Pathol 1957; 10:899–909.
Troulis MJ, Tayebaty FF, Papedaki M et al. Condylectomy and costochondral reconstruction for treatment of active idiopatic condylar resorption. J Oral Maxillofac Surg 2007; 36:1193–97.
Tselnik M, Pogrel A. Assessment of the pharyngeal airway space after mandibular setback surgery. J Oral Maxillofac Surg 2000; 58:282–85.
Turner JG. Dental cysts. Brit Dent J 1898; 19:711–32.
Urken ML, Buchbinder D, Constantino PD et al. Oromandibular reconstruction using microvascular composite flaps: report of 210 cases. Arch Otolaryngol Head Neck Surg 1998; 124:46–55.
Van Sickels JE, Larsen AJ, Thrash WJ. Relapse after fixation of mandibular advancement. J Oral Maxillofac Surg 1986; 44:698–702.
Vaughan ED. The radial forearm flap in orofacial reconstruction. J CranioMaxillofac Surg 1990; 18:2–7.
Veau V. Division Palatine. Masson et Co, Paris,1931.
Veau V. Bec de Lievre. Masson et Co, Paris, 1938.
Ventä I,Ylipaavalniemi P, Turtola L. Clinical outcome of third molars in adults followed during 18 years. J Oral Maxillofac Surg 2004; 62:182–85.
Verdonck HWD, Jong de J, Granzier M et al. Intensity-modulated therapy for oropharyngeal cancer: radiation dosage constraint at the anterior mandible. Oral Oncology 2009;45:511–14.
Vickers RA, Gorlin RJ. Ameloblastoma: delineation of early histopathologic features of neoplasma. Cancer 1970; 26:699–710.
Wangerin K, Grob H. Die enorale Zugang bei der Ilizarov-Kallusdistraktion am Unterkiefer. Dtsch Z Mund Kiefer Gesichtschir 1995; 19:303–07.
Ward TG, Surgery of the mandibular joint. Ann Roy Coll Surg 1961; 28:139–52.
Ware WH, Taylor RC. Cartilaginous growth centers transplanted to replace mandibular condyles in rhesus monkeys. J Oral Surg 1966; 24:33–43.
Ware, WH, Growth centre transplantation to replace damaged mandibular condyles. JADA 1966;73:128–137.
Warnke PH, Springer IN, Wiltfang J et al. Growth and transplantation of a custom vascularised bone graft in a man. Lancet 2004;364:766–70.
Warren JC. Surgical observations on tumours with cases and operations. Crocker & Brewster, Boston, 1837.
Weiner JA, Sapundzhiev NR, Teymoortash A, Dunne AA, Behr T, Folz BJ. Endoscopic sentinel lymphadenectomy as a new diagnosyic approach in the NO neck. European Archives of Oto-Rhino-Laryngology 2004; 261/9, 463–468.
West R A, McNeill RW. Diagnosis and treatment planning: a coordinated effort between oral and maxillofacial surgery and orthodontics. J Oral Surgery 1977;39:809–16.
Westermark A. Total reconstruction of the temporomandibular joint. Up to 8 years of follow–up of patients treated with Biomet® total joint prostheses. Int J Oral Maxillofac Surg 2010;39:951–55.
White RP. Progress report on third molar clinical trials. J Oral Maxillofac Surg 2007;65:377–83.
Wilkes CH. Surgical treatment of internal derangements of the temporomandibular joint: A long term study. Arch Otolaryngology Head Neck Surg 1991;117:64–72.
Williams J Ll. In Rowe & Williams “Maxillofacial Injuries” 2nd. Edition Churchill Livingstone, Edinburgh, London,1994.
Williams ThP. Management of ameloblastoma: a changing perspective. J Oral Maxillofac Surg 1993;51:1064–70.
Williams WB, Kaban B. Condylectomy and costochondral reconstruction for treatment of active idiopathic condylar resorption. J Oral Maxillofac Surg 2007;58:282–85.
Williamson RA. Surgical management of biphosphonate induced osteonecrosis of the jaws. Int J Oral Maxillofac Surg 2010;39:251–55.
Wintz H. Die Einzeitbestrahlung. Strahlentherapie 1937;58:545–51.
Wiseman R “Several Chirurgical Treatises “,London, In Rowe & Killey, Fractures of the Facial Skeleton p867. E&S Livingstone Ltd, Edinburgh, London,1955.
Witsenburg B, Freihofer HPM. Autogenous rib graft for reconstruction of alveolar bone defects in cleft patients. J Cranio-Maxillofac Surg 1990;18:55–62.
Woolgar JA. Bierne JC, Vaughan ED, Lewis Jones HG. An audit of one surgeons experience of oral squamous cell carcinoma. Am J Surg 1988;156:286–89.
Woolgar JA. Detailed topography of cervical lymph-node metastases from oral squamous cell carcinoma. Int J Oral Maxillofac Surg 1997;26:3–9.
Woolgar JA. Pathology of the N0 neck Br J Oral Maxillofac Surg 1999;37:205–09.
Woolgar JA. Micrometastasis in oral/oropharyngeal squamous cell carcinoma: Incidence, histopathological features and clinical implications. Br J Oral Maxillofac Surg1999; 37: 181–86.
Wunderer S. Die Prognathieoperation mittels frontal gestieltem Maxillafragment. Oest Z Stomatol 1962; 59: 98–102.
Xia J HH, Samman N, Wang D et al. Computer-assisted three-dimensional surgical planning and simulation: 3D virtual osteotomy. Int J Oral Maxillofac Surg 2000;29:11–17.
Yamazaki Y, Satoh C , Ishikawa M et al Remarkable response of juvenile sclerosing os te omye litis of mandible to pamidronate. O ral Surg 20 07;104 :67 –7 1
Yang G , Che n B , Gao Y, L iu X e t al. Forear m f re e skin flap transp osition. Nat Me d J China 19 81; 61:139
Z ay toun HR , Philips C , Te r r y BC . Long te r m ne urose nsor y d e fi cit s follow ing transoral ver tical ramus and sagit tal split osteotomies for mandibular prognatism J O ral Ma xillof ac Surg 19 86; 4 4 :193 – 9 6
Zhang WJ,Cai X Y, Yang C , e t al. Ce r vic al ne crotising f asciitis due to me thicillinresis t ant s t ap hylo co ccus aure us: a c ase re p or t . Int J O ral Ma xillof ac Surg 2010; 39:830 – 3 4
Zhi K , Re n W, Zhou H e t al. Manage me nt of te mp oromandibular joint ank ylosis: 11 year s clinic al e xp e r ie nce. O ral Surg 20 0 9; 10 8:687 – 92
Zölle r JE, Küble r AC , Lor b e r WD, Mühling JFH. K raniof a ziale Chir urgie. Ge org T hie me Ve r lag, Stut t gar t , Ne w Yor k , 20 02
General Tex tbook s
A x hause n G . Die A lge meine Chir urgie in d e r Z ahn -, Mund - und K ie f e r heilkund e JF L e hmanns Ve r lag, Munche n - B e r lin, 19 40
A rc he r W A . O ral Surge r y A s te p by s te p atlas of op e rative te chniques W B Saund e r s Company, Philad e lp hia and London, 19 5 2, 19 56, 19 61, 19 66, 1975
Bhaskar SN. Synopsis of O ral Patholog y. T he C V Mosby Comp, St Louis, 19 61, 19 65 , 19 69
Blair VP, Iv y RH, Brow n JB. Esse ntials of O ral Surge r y. T he C V Mosby Company, St Louis, 1923 , 1936 and 19 4 4
Brop hy T W. O ral Surge r y : a treatise on the diseases, injur ies and malfor mations of the mouth and asso ciate d par t s. He nr i K impton, 1916 Br uns von P, Gar ré C , Küt tne r H. Chir urgie d es Kopf es 4 e Edition Band I Fe rdinand Enke Ve r lag, B e r lin, 1916 Caw son R A , L angdon JD, Eveson JW. Surgic al patholog y of the mouth and jaw s Wr ight , 199 6
Chompre t J, D e c haume M, Richard. Te c hnique Chir urgale Bucco D e nt aire Masson e t C ie , Edite ur s Par is, 1935 D e c haume M, Huard P. L’ar t D e nt aire , Stomatologie e t O dontologie. L’Edite ur s Roge r Dacos t a, Par is, 197 7
Garre t son J E A System of Oral Surger y : a consideration of diseases and surger y of the mouth, jaw s and asso ciate d par t s. JB L ippincot t & Co, Philad e lp hia, 187 3
Hof f man - A x the lm W. Die Gesc hic hte d e r Mund -, K ie f e r- und Gesic ht schir urgie Q uintesse nz Ve r lag- GmbH, B e r lin, 199 5
Kruger GO Te x tbook of Oral and Ma xillof acial Surger y T he C V Mosby Company St Louis, Toronto, London, 19 59 , 19 64 , 19 68 , 1974 , 1979
L angdon JD, Patel MF Operative Ma xillofacial Surger y Chapman & Hall Medical, London, 1992
L askin D N. O ral and Ma xillof acial Surge r y. Vol. I & II, T he C V Mosby Company, St Louis, Toronto, Pr ince tow n, 19 85
Mar x RE, Ste r n D, O ral and Ma xillof acial Patholog y. A rationale for Diagnosis and Treatme nt . Q uitesse nce Publishing Co, Inc , Chic ago, B e r lin e tc , 20 03
Mead S V. O ral Surge r y. T he C V Mosby Company, St Louis. 193 4 , 19 40 , 19 4 4
Pe r thes G . Die Ve r le t zunge n und K rank heite n d e r K ie f e r. Ve r lag von Fe rdinand Enke , Stut t gar t , 19 07
Pe te r son L J, Indressano A ,T h,Marciani R D, Rose r St M. Pr inciples of O ral and ma xillof acial Surge r y Vol I,II,III, JB L ippingcot t Comp, Philad e lp hia, 1992
Pe te r son LJ, Ellis E, Hupp JR , Tucke r MR . Conte mp orar y O ral and Ma xillof acial Surge r y. JB L ippingcot t Comp, Philad e lp hia, 199 8
Pic hle r H, Traune r R . Mund - und K ie f e rc hir urgie. Ur ban & Sc hwar ze nb e rg B e r lin, W ie n, 19 4 2
Shaf e r WG , Hine MK , L ev y BM. A Te x tb o ok of O ral Patholog y. WB Saund e r s Comp, Philad e lp hia, London, 19 5 8 , 19 63 , 1974 , 19 83
Sont ag E, Rose nthal W. L e hr buc h d e r Mund – und K ie f e rc hir urgie , Ge org T hie me Ve r lag, L eipzig, 1930
Traune r R . K ie f e r– und Gesic ht sc hir urgie. Ur ban & Sc hwar ze nb e rg. B e r lin, Münc he n, W ie n. 197 3
T homa KH, O ral Surge r y. C V Mosby Company, St Louis, 19 4 8 , 19 5 2, 19 5 8 , 19 63 , 19 69
T homa KH, O ral Patholog y. C V Mosby Comp, St Louis, 19 41, 19 4 2, 19 50 , 19 5 4
T homa KH, Goldman HM. O ral Patholog y. C V Mosby Comp. St Louis 19 6 0 Ward B o oth P. Sc he nd e l S. Hausane n JE. Ma xillof acial Surge r y Vol. 1 & 2, 20 0 6
Wassmund M, L e hr buc h d e r prak tisc he n Chir urgie d es Mund es und d e r K ie f e r, band 1 & 2 “ Ve r lag von A mbrosius Bar th, L eipzig, 1935 , 1939
Chapter 2
The International Association of Oral Surgeons (1962–1986)
The beginning (1962–1971)
There is no doubt that the very first steps in establishing an international association of oral surgeons were taken by Fred Henny. He was an oral surgeon and chief of the departments of dentistry and oral surgery at Henry Ford Hospital in Detroit and in 1960, president of the American Society of Oral Surgeons (ASOS). He was also the editor-in-chief of the Journal of Oral Surgery. He attended a meeting of the American Dental Society of Europe in 1959 in Stockholm, where he came into contact with Gerry Leatherman, a British dental surgeon, who at that time was secretary general of the FDI.
While at the meeting, he made inquiries about the possibility of holding an international conference of oral surgeons with European colleagues. Leatherman advised him to make contact with Terence Ward, a consultant oral surgeon in East Grinstead, U.K. Fred and Lyall Bishop (the incoming president of ASOS) subsequently made a trip to London to meet with Terry Ward and some of Terry’s colleagues from the Oral Surgery Club of Great Britain. From this meeting emerged the idea of having a conference in London, to be organized by the British under the leadership of Terry Ward.
The first International Conference on Oral Surgery (ICOS) took place at the Royal College of Surgeons of England on July 1-5, 1962. It was attended by 750 delegates and accompanying persons from over 40 countries. The particulars of this meeting were very well described by Bob Walker, one of the American attendees and one obviously very much impressed

At first glance, it may look like a sheer coincidence that Fred Henny met Gerry Leatherman at the conference in Stockholm and made inquiries about the possibility of organizing an international conference on oral surgery. In retrospect, however, one can safely assume that the time was ripe. Europe had more or less recovered from the damage done by World War II and Americans were anxious to know how oral surgery had developed in Europe. The development of the airline industry made it possible to cross the ocean comfortably in a reasonable period of time, while the means of communication also had improved a lot. Yet, the development of the specialty on both sides of the ocean and indeed in all other parts of the world had progressed without much input from abroad. In fact, the world at that time was not familiar with the term “Globalization.”

In 1962, there were two journals in the U.S.A. dealing with oral surgery; the Journal of Oral Surgery, which was launched in 1943, and Oral Surgery, Oral Pathology, Oral Medicine which first appeared in 1957. Since 1955 the Germans had their Fortschritte der Kiefer-und Gesichts-Chirurgie, which were transactions of their yearly conferences, whereas the French had the Revue de Stomatologie since 1899.
It is safe to say that neither of these journals was read much outside the language area they represented. One can be fairly sure, therefore, that a great deal of ignorance existed about the state of the art of oral surgery on both sides of the Atlantic. The language barrier was huge and thus, it is understandable that Fred Henny sought to contact a British colleague. Although separated by a common language, they, at least, understood each other.
If Fred Henny had not taken the initiative, it surely would not have taken long before somebody else had. Yet the IAOMS thanks its inception to this visionary man.
Paul J.W. Stoelingaby the meeting’s pomp and grandeur. The conference sparked enough enthusiasm among participants to consider the foundation of an international association of oral surgery.
The person who had an enormous impact on the early years of the International Association of Oral Surgeons (IAOS) was Terry Ward. Fred Henny probably could not have found a better person to set up an international association. Terry Ward was the prototype of an English gentleman, at least in the eyes of non-Englishmen. He was a very self confident, headstrong person with a touch of arrogance, to put it mildly, an excellent speaker and writer of impeccable English, who had a healthy mistrust in anything foreign to him. He was also a very good organizer who was determined to make the IAOS a success. This is borne out by many notes in the minutes of meetings that most of the time he chaired himself but, above all, by his deeds.
The organization of the first ICOS was a great success thanks to his leadership and the support he had from his colleagues in the British oral surgery club. Terry was in his prime years in the British hierarchy, being the Dean of the dental faculty of the Royal College of Surgeons of England and also the first president of the British association, which was established in the same week as the first ICOS. At the London conference, he was asked to write the constitution of the International Association of Oral Surgeons (IAOS) during a meeting that was attended by Lyall Bishop, president of ASOS; Fred Henny; Jørgen Rud of Denmark and Martin Hut, at that time the president of the Dutch Association. Colleagues attending the conference were asked to join the to be established IAOS and apparently this campaign was very successful as the IAOS membership by June 1963 had already grown to 516.
The fellowship fee in those days was $15, or £5 per annum, an amount that would not change until 1990. One could also become a life member by paying a one-time fee of $300.
The draft of the constitution was sent back and forth to selected oral surgeons worldwide and, according to Walker and Rud (1996), was accepted on April 22, 1964 by the initial executive committee which was appointed by Terry Ward. The committee consisted of Fred Henny as chairman; Lyall Bishop; Pierre Cernea of France; Jørgen Rud as chairman of the 2nd ICOS in Copenhagen and Terry Ward as secretary general.




The constitution laid down the principles of the rules and regulations of the IAOS that for a large part are still valid today:
• T he IAOS should consist of individual fellows.
Fellows present at the ICOS formed the “General Assembly.”
• National associations could affiliate to the IAOS.
• R epresentatives from affiliated national associations and the members of the executive committee would form the “Council,” the ultimate decision-making body of the IAOS.
• T he executive committee would be responsible for the conduct of the IAOS and answerable to council.
• T he day-to-day work would be done by the secretary general.
Fred A. Henny was the first dedicated internationalist in American oral and maxillofacial surgery. Certainly, World War II exposed American military surgeons in the specialty to surgical practice in both Europe and the Pacific, but under less than expansive or otherwise ideal circumstances. Fred Henny, excused from that conflict by his responsibilities at Henry Ford Hospital in Detroit, one of America’s most dynamic wartime medical facilities, became attuned to matters European in the decades immediately following the war through his consultative relationships with military surgeons, his affiliations in veterans affairs and his enthusiasm for the developing kinship between professionals of English-speaking nations. These latter relationships, most notably with Dutch, Scandinavian and English colleagues, resonated in his binding friendship with Sir Terence Ward, their founding of the IAOS in 1962 and his role as its first president.
The decades of the first and second world wars were the time of the slow maturing of the American specialty but only occasionally in those years was it represented in more expansive surgical arenas. It was in this milieu, however, that Fred Henny developed as a surgeon learning from whomever he could, daring when he had to, and by the 1950s, becoming a master in cleft, temporomandibular joint and malignant disease surgery. Among the Henry Ford Hospital staff of internationally recognized general surgeons, Henny was acknowledged to be the premier head and neck surgeon of the group.
The attributes which carried Fred Henny to prominence in America were chiefly four:
• His consummate surgical facility
• His admirable decorum
• His political and organizational senses
• His totally unselfish encouragement of his protégés and all young surgeons
He was able to keep his goals in focus with an indifference to ancillary considerations and those goals remained throughout his career the integrity and growth of his specialty. The much broader vistas of American oral and maxillofacial surgery today reflect Henny’s personal skills and teaching but, perhaps, more importantly, his tireless encouragement and aggressive incorporation of things international into training and practice everywhere.
Fred Henny’s surgical accomplishments elevated him to the presidencies of both the American Association of Oral Surgeons and the American Board of Oral Surgery, as it was called in those days. He served 13 years as editor of the Journal of Oral Surgery, he was honored as an outstanding alumnus of the University of Michigan at that institution’s sesquicentennial celebration and he was elected a fellow of the Royal College of Surgeons of England. In no role did he take more satisfaction, however, than in his service to the International Association of Oral Surgeons. Fred A. Henny was the paladin of American oral and maxillofacial surgery for his time and stands today as an international icon for all time. He left a legacy of truly worldwide proportion for his beloved specialty when he moved on to the better world in the early morning hours of January 10, 1989.

1965: The 2nd ICOS, Copenhagen
The 2nd ICOS took place in Copenhagen on June 19–24, 1965. It was organized by the Danes under the chairmanship of Jørgen Rud, who incidentally missed the whole event because of acute appendicitis. This again was a very successful conference attended by 212 fellows of the IAOS, 189 non-fellows and 239 associates and guests. Forty percent came from the U.S.A., the remainder largely from Europe, 39 countries in all were represented.
A detailed report of this conference was written by Jørgen Rud which included particulars of the opening ceremony, scientific program, exhibition, banquet, transactions and various other items. The report probably served as the basis of the “ICOMS Rules and Regulations” for many years thereafter. Of particular note is the fact that a golf tournament was organized in which only 20 people participated. The report mentions that it became a loss to the organization! Other noteworthy facts are that Terry
Ward was reimbursed for nine trips to Copenhagen and that the total profit of the meeting amounted to $600. Apart from an interesting scientific program and apparently a highly appreciated social program, the main thing about this conference was that the IAOS was now officially established as the general assembly approved the constitution. At this point, the IAOS had 567 fellows with six or seven affiliated associations, notably the American, British, Dutch, French, Israel and Scandinavian associations and probably Australia-New Zealand. More importantly, the international association was now on a solid footing with a “chosen” executive committee and a formal council. The initial executive committee did not change, however, with the exception that Fred Henny was now called “President.”
News Sheet begins
In the period before the third meeting in New York, Terry Ward began to send around a publication named News Sheet each year. The first appeared in 1965 and he continued to publish them until 1968. These issues contained very detailed information on the development of the IAOS in the early years, including the growth of the membership, the activities of the affiliated nations, changes made to the constitution and news about the upcoming ICOS.

The News Sheets were also a testimony to Terry’s commitment to the cause. They provided the fellows of IAOS with a feeling of belonging to an association which was clearly meeting a demand. The three years between international conferences were without any real activities but Terry made it sound as if a lot was going on. For
instance, he reported on the major jump in membership right after the second ICOS to 662 fellows. The sheer fact that membership kept growing, albeit minimally, to 673 in 1968 and that four more national associations joined, attest to the vitality of IAOS at that time. The associations that joined were from Spain (1967), Canada (1968), Argentina (1967), and Cuba (1968).
1968: The 3rd ICOS, New York
The third ICOS in New York in October 1968 was deliberately scheduled to take place simultaneously with the 50th anniversary meeting of the ASOS. This was a well-attended meeting by both Americans and Europeans but it was difficult to tell how many were there as fellows of the IAOS. This also was the meeting where Hugo Obwegeser introduced the sagittal split osteotomy to a large audience, signaling the beginning of a new era in orthognathic surgery.
The meeting again produced a boost in membership to 793 and the decision was made to use the first funds on scholarships that would allow trainees to work in selected centers abroad. It is not clear whether this was actually put into effect.
This was also the first time that the president wore a badge suspended from a crimson ribbon. This badge has been replaced by the current one but it resembles very much the first badge in that the IAOS symbols were also in gold on red enamel. The golden chain came in 1971 and was a gift from Andrew Linz.

An important change in the constitution was made regarding the executive committee. From now on, the president would serve another three years as immediate past president on the executive committee. The officers of the IAOS in New York also changed with Terry Ward becoming president, Norman Rowe, the secretary general and Willem (Bill) A.M. van der Kwast came on board as chairman of the fourth ICOS, to be organized in Amsterdam.
It is of interest to note that three committees were set up: education, finance and research. They were chaired respectively by Norman Rowe, Elmer Bear and Bob Walker. There was apparently already a sense that the international association had a mission to fulfill as an initiator of guidelines for education and training. The following years will see this to be a constant issue in the discussions of the executive committee and council. Not unexpectedly, the first honorary member — Fred Henny — was chosen at this meeting.

In 1960, when Fred Henny first met Terry Ward, Terry Ward probably knew more about Fred Henny than Fred Henny did about Terry Ward. Terry Ward had achieved eminence in the United Kingdom via an unusual and, in many ways, quite remarkable career path. His was not a privileged background. The son of a teacher in Edinburgh, he aspired to become a dental surgeon. Of modest means, he earned entry to the profession apprenticing as a dental mechanic. From there, it was his academic ability that secured his entry into Edinburgh University and it was through his skill as a dental mechanic that he was able to support himself through his student years. In 1928, he qualified in both medicine and dentistry and joined a dental practice in the south of England in Hastings.
It was World War II that changed his life. The British government established a number of Emergency Medical Service Hospitals at the beginning of the war, one of which was at East Grinstead, a small town south of London. It was here that Archibald McIndoe and Kelsey-Fry (both later knighted for their work) established what became an internationally acclaimed burns and maxillofacial center. For Terry Ward, who already had a special interest in surgical dentistry, this was an opportunity. East Grinstead was not far from Hastings, so he went to see Kelsey-Fry and a relationship was established which was based on mutual respect and which continued until Kelsey’s death many years later.
general, 1963–1968 and 1971–1974
In 1940, Ward joined the Royal Air Force and served as a specialist dental officer until the end of hostilities. By that time, he had an established reputation as an innovative and brilliant oral surgeon. Kelsey-Fry saw him as his natural successor at East Grinstead, where he became head of the then dental department in 1948. Despite its wartime reputation, the Queen Victoria Hospital at East Grinstead was a small regional hospital with none of the facilities and academic ambience of a teaching hospital in a major city. But Terence Ward was unusual because he was one of the first genuine specialist oral surgeons. As a result, trainees competed vigorously for his attention and the new Ministry of Health rapidly came to appreciate his political skill. He became a consultant adviser to the government and played a leading role in the early development of hospital dentistry within a new nationalized health service.
In his professional life, Terry Ward had two great loves: the Queen Victoria Hospital at East Grinstead and the Royal College of Surgeons of England. He ran his hospital department as an ever-expanding family. Surgical trainees came from all over the world to obtain experience at his hands, while he himself was invited far and wide to operate and lecture. He never appeared to treat one patient differently from another and was equally at home with kings, dictators and the internationally famous as he was with the day-to-day problems of his outpatients at home.
He had an equally charming disregard for the value and quality of the many gifts he received, such that garish diplomas and executive toys sat side-by-side on his desk with exquisitely crafted statuettes and other “objets d’art,” for he never threw anything away.
In his hospital, he was a tireless worker and his staff had to rise early to get round the wards before him. He had equal time for the problems of all levels of staff, from secretary to the senior trainee and he inspired a particular kind of loyalty.
Ward was a man of mischief, and would spend as much time organizing a practical joke on a colleague as he would in preparation for an important meeting with the Minister of Health. One new trainee in the 1960s, intent on making an impression, invited “the boss” for dinner and was immediately asked whether dress should be formal. “Oh no sir, quite casual,” came the innocent reply, only to find that his distinguished patron had delegated his clinical responsibilities and spent most of the day with the full-time assistance of his secretary in obtaining a long-haired wig and a flowing robe with bells attached (appropriate to the post-Beatles, hippy generation), in order to arrive in “casual” dress for dinner.
From the point of view of the modern international oral and maxillofacial surgeon, it is important to see Terence Ward in a proper historical perspective. He was trained essentially as a dentist, albeit with a double degree, which, in those days, was mainly a passport to a fashionable dental practice. He was fortunate (if that is the right word) to gain experience in wartime. He then used his skills, experience and political ability, along with a few others of like mind, to establish oral surgery as a specialty in United Kingdom hospitals open to dental surgeons, enjoying the same salary and status as their medical colleagues.
It was perhaps because of this battle on behalf of dentistry that he resisted making the double degree a requirement, never realizing that in Europe, it was the only route into basic surgical training, which was to become essential to the development of oral and maxillofacial surgery in the 21st century. Unusually, however, in 1960, he was one of the very few with a truly international perspective and realized the importance of uniting oral surgeons both at national and international level, a perspective which he fortunately shared with Fred Henny. These two men will always enjoy a special place in the history of IAOMS.
 Banks
Banks
general, 1968–1971
Norman Rowe kept the secretariat at the Royal College of Surgeons of England. The IAOS was recognized as a charity and, therefore, exempt from paying taxes. He continued to send the News Sheets to the fellows at the same frequency of one a year until 1971. After that year, the International Journal of Oral Surgery was thought to be the vehicle for messages to the fellows.
It is noteworthy to mention here the liaison the IAOS had with the FDI (now known as the World Dental Federation). The IAOS officially affiliated with the FDI and from the available minutes of executive committee meetings from this period, it appears that subsequent executive committees were very concerned that oral surgery be represented at FDI meetings. This stance was followed until 1986.
There was no question about the association’s vitality at this stage. The leadership of the IAOS was in the firm hands of Terry Ward, who single-handedly picked Bill van der Kwast as the chairman of the next organizing committee. His appointment, without consulting with the Dutch association, raised some eyebrows and Bill had some explaining to do at their business meeting. Yet, he received full support from his Dutch colleagues but he was closely and frequently monitored by Sir Terence, as were the Danes in the years before.
One of the most important decisions that this executive committee made was to begin an International Journal of Oral Surgery. This was a highly appropriate move at this stage of the association’s development as it was difficult for colleagues from non-English speaking areas to publish in peer-reviewed journals.
They found an eminent scientist in the person of Jens Pindborg, a world-renowned oral pathologist from Copenhagen, to take on the job of editor. Pindborg was recommended by Jørgen Rud, who had also made contact with Munksgaard publishers in Copenhagen. One may wonder whether the selection of Pindborg was a wise decision given the fact that he was by no means a surgeon. However, given the circumstances, i.e. the necessary frequent contacts with the publisher and the lack of a suitable candidate on the European continent who was a surgeon with a reasonable command of English, it was a sensible decision at that time.
The period between the third and the fourth conferences went without further activities. It is, therefore, somewhat surprising that despite this, the
membership grew quite substantially from 793 just after the New York meeting to 843 in the year before the fourth ICOS.
1971: The 4th ICOS, Amsterdam

The Amsterdam conference, held from May 17 to 21, 1971, was again a great success with approximately 800 attendees, including accompanying persons. The conference was opened by H.R.H. Prince Bernhard of the Netherlands. Those attending probably remember most especially the reception offered by the Dutch government, at the “Rijksmuseum” where drinks were served literally under the eyes of Rembrandt’s “De Nachtwacht.” One cannot imagine this happening today.

During the conference, Prince Bernhard of the Netherlands became the second honorary member of the IAOS. At this meeting one more national association became affiliated: the Brazilian “Collegio.” It was also recognized that fellows not represented by a national association would be represented by two council members

Membership as a result of this meeting rose to 938. Jørgen Rud was chosen president and Terry Ward again became the secretary general. He wouldn’t let go! Victor Sada from Spain was named chairman of the fifth ICOS, to be organized in Madrid in 1974.
It is probably fair to state that at this time the IAOS had achieved a very respectable status and already had considerable impact on the development of oral surgery throughout the world. If one looks at the years that national associations were founded in the various corners of the globe (see addendum), it is tempting to assume that oral surgeons who came from countries with no national association, attended one or more of the four ICOS and returned home to take local initiatives and assist in founding their own national associations. Additionally, after nine years, the organization had outgrown its teething problems with a membership that had almost doubled and the affiliation of 12 national associations.
The IAOS was ready to consolidate and further expand. It was no coincidence that the further evolution of the organization followed the boost the specialty received from two relatively new directions in oral surgery: pre-prosthetic and orthognathic surgery (see chapter 1) These developments created an enormous expansion of scope for the specialty and thus, a demand for manpower and not just in the countries where oral surgery was already established. During this time period, it seemed clear that the absolute number of oral surgeons had grown and was continuing to grow worldwide.
Consolidation and expansion (1971–1986)
1972’s major event was the launch of the International Journal of Oral Surgery in June of that year. The Journal appeared six times annually and had an “International News” section. It is interesting to note that the leading article in the first issue was written by Terry Ward. The

that “there might be subjects not fitted for publication in a journal but only to fellows.” For this reason, in 1974, the decision was made to reinstate a News Sheet now called the Newsletter, which would appear twice a year from then on. Given the association’s growth, it became clear that more steering was needed between meetings, especially as initiatives began to emerge regarding the organization of a workshop about education in Madrid. For these reasons, council and the general assembly agreed to set aside funds for annual executive committee meetings. This proved to be a big step forwards as a growing organization, such as the IAOS, required a structured way of conducting business, particularly since real business had entered the organization with the introduction of the Journal.
1974: The 5th ICOS, Madrid

The fifth ICOS in Madrid (from April 21–25, 1974), was also very successful, although its main event, a workshop on “Training in Oral Surgery” chaired by Terence Ward, could hardly be called a success as it caused a clash between colleagues with medical degrees and those with dental backgrounds. The report on the workshop that was sent to all fellows six months later (see addendum) was written in very diplomatic language, particularly in its statement that the IAOS was not the organization to impose any specific training program on any country.

The Newsletter’s coverage of the event reported that: “It is not to be expected that results from discussions where oral surgeons from so many countries meet for the first time will satisfy everyone.” No one expected this. The value of such worldwide discussions on a subject which is of great importance to us all is, first of all that everyone is confronted with views from other environments which may stimulate discussion of national training programs. The present workshop document should, therefore, not be looked upon as the official IAOS recommendation, but regarded as a basis for further discussion.” These lines are presumably from Terry Ward. Those fellows who were involved in the Tenerife and Bermuda conferences and with the final discussions about the “Guidelines” could not have agreed more with this introduction.
The meeting was well attended and three new national associations joined: Hungary, Mexico and Venezuela. The executive committee for the first time had a new face as president: Alton D. “Sandy” MacAlister from New Zealand. Jørgen Rud became secretary general, while Terry Ward stayed on as past president and “chose” Andrew Linz as representative of ASOS in the executive committee. Sydney was chosen as the new venue for the 6th ICOS with Frank Helmore as chairman of the organizing committee. This was certainly a right choice as the Association of Australian and New Zealand Oral Surgeons (ANZOS) was one of the founding associations of the IAOS. For the first time, however, mention is made of a competition between cities of different countries to be candidates for the organization of an ICOS.
H.R.H. Prince Juan Carlos of Spain and Sir Terry Ward were appointed honorary fellows. As a result of this meeting, the secretariat moved to Copenhagen. The membership, as reported in the autumn issue of the Newsletter of 1974, had risen to 1,048.


Very little happened in the years between 1974 and 1977, the year the sixth ICOS was to be held, apart from
the appointment of Erik Hjørting Hansen, in 1976, as the new editor-in-chief of the Journal. He had been working very closely with Jens Pindborg, which guaranteed a smooth transition. He would hold this position until 1988.
1977: The 6th ICOS, Sydney
The sixth ICOS in Sydney almost turned into a fiasco because of a strike of air traffic controllers which ended just before the meeting. Frank Helmore and his organizing committee must have drawn a sigh of relief when the strike was called off. The attendance, as could be expected, was less than in previous years but still totaled 557 delegates, including accompanying persons, with 28 countries represented.
Everyone enjoyed the hospitality of the Australian and New Zealand colleagues. The highlight of this meeting was the reception in the Sydney Opera House foyer overlooking the Sydney harbor. At this meeting, a golf tournament was also organized, as had occurred at previous conferences.
From an organizational point of view, an important change in the regulations was in order, given that Council now consisted of 21 national associations representing 96 percent of the membership. This implied that the actual power was in the council rather than in the general assembly. Consequently, in Dublin three years later, it was decided “that decisions taken by Council shall not require approval from the General Assembly.” This regulation still exists today.
Another item that was decided in Sydney was the re-introduction of life membership, something that had been instituted from the inception of the IAOS but had been discontinued for unknown reasons. For $300, one could become a life member of IAOS. The idea behind this was that the bulk money would generate interest and thus, predictable income. In reality it did,
however, treasurers to come would consider this money as not suitable for covering the running expenses of the association but rather to cover special events.
Although it was decided in Sydney to hold educational symposia between ICOS, this did not actually happen because of time constraints but also because of financial limitations. The IAOS, however, took the initiative to hold a workshop on European oral and maxillofacial surgery in 1977 in Copenhagen, which was attended by 19

colleagues from Belgium, Denmark, France, Israel, Great Britain, Spain, Switzerland, the Netherlands and West Germany. There were also two observers from the U.S.A.
This meeting exposed the fundamental differences between various continental European countries and the Anglo-Saxon world at that time. The “double-degree” issue was prominent and caused a split among the participants. In 1980, the education committee, under the chairmanship of David Gutman from Israel, produced a report containing “Guidelines for the Education and Training of the Oral and Maxillofacial Surgeon.” This report was based on the outcome of the workshop in Madrid in 1974 and the meeting in Copenhagen in 1977. It was published in English, German, French and Spanish in the fall 1980 Newsletter (see addendum)

1980: The 7th ICOS, Dublin
In the period leading up to the seventh ICOS in 1980 in Dublin, there were again very few activities reported except that the Newsletters in those days provided excellent information on the activities of affiliated associations but also reports on the membership and the financial situation of IAOS.
The president of this period, Bill van der Kwast, traveled to various parts of the world to make contacts with colleagues from affiliated but also non-affiliated associations. He mentions in his report, which is the only one available for his period, that he visited India twice and even went to the AAOS and ANZOS meetings and the Philippines, apart from various visits to European meetings. He took his representative task very seriously but there are no signs of truly governing an international association as we know it now. Mention is only made of one executive committee meeting in East Grinstead to prepare for the Dublin meeting. One can hardly imagine that the “retired” Terry Ward was not involved in this meeting.

As usual, the ICOS in Dublin was the main event of IAOS in this period and was again very well organized by the organizing committee under the chairmanship of Ian Findlay. The president of Ireland, Dr. Patrick J. Hillary, opened the conference in the St. Patrick’s Cathedral; as a result, an honorary membership of the IAOS was conferred upon him. The conference attracted 900 attendees, 548 of whom were delegates, certainly a good attendance, which resulted in a modest profit for the meeting. According

The official opening of the 7th ICOS in Dublin took place, not surprisingly in Catholic Ireland, in St. Patrick’s Cathedral in the presence of Dr. Patrick Hillary, the president of the Irish Republic. According to Catholic tradition, it is the privilege of the Bishop to enter the church first. For this reason, the dignitaries of IAOS had to wait in the back of the cathedral for him to arrive. When he entered the church, he was followed by the boy’s choir who would sing during the opening ceremony. President Bill van der Kwast and Sir Terence Ward followed behind the boys, leading Sir Terence to remark to van der Kwast, “William, it must be a sign of age to have to run after the choir boys.”



 Bill van der Kwast
Bill van der Kwast
to the official report, it was particularly the symposia led by Norman Rowe and David Poswillo that made the meeting a successful scientific event.
The executive committee following this ICOS underwent a profound change as several new faces from various countries came on board. Geoffrey Howe became the new president, while Bill van der Kwast became the new secretary general. Jørgen Rud, who had been present from the very beginning with Terry Ward, finally retired from the executive committee and was rightly made an IAOS honorary member. The chairman of the organizing committee for the eighth ICOS in Berlin was Wilfried Schilli.
Despite the strong representation of European members in the executive committee during the ensuing period, very little progress was made in the effort to bring together the different opinions regarding the building of the specialty. This probably had to do with the fact that the president was located in Hong Kong. Consequently, there simply is not any documentation of any activity during this period of time, apart from the organization of the Berlin meeting.
1983: The 8th ICOS, West Berlin
The Berlin meeting introduced a novelty with a “Consensus Conference” on “The relative roles of vestibuloplasty and ridge augmentation in the management of the atrophic mandible,” chaired by Paul Stoelinga. It was held one day before the official opening and was a great success, at least that was the opinion of all of the panel members, who had gone out of their way to bring their prosthodontists to the event. However, there was only one person in attendance: the incoming president, Daniel Laskin. Unfortunately, the organization had not included this symposium in the ICOS program announcements, although it was announced in the Newsletter. The proceedings subsequently were published and had quite an impact among interested colleagues. Most surgeons
and prosthodontists who were involved became lifelong friends and had many contacts afterwards.
The 8th ICOS had a modest attendance given the location and the fact that the German-speaking area was the cradle of European oral and maxillofacial surgery.
There were 567 delegates and 230 accompanying persons. Unfortunately, there is no report available about this meeting but the organization was excellent and the ambiance left little to desire. It was not a financial success, as the organization took a loss. The new executive committee, however, under the presidency of Dan Laskin, made some important decisions that had far-reaching effects.
• First, and most importantly, the much desired name change came about. From 1984 on, the association’s name was to be “International Association of Oral and Maxillofacial Surgeons (IAOMS).” The journal name change followed only in 1987.
• Second, this executive committee found it necessary to meet between the triennial meetings and, in fact did, contrary to previous committees.
T hird, the secretariat moved from Amsterdam to London, as David Poswillo took over as secretary general.


• Fourth, this committee recognized the importance of communication so as to involve the membership in the business of the IAOMS. For this reason, the Newsletter underwent a facelift with David McGowan appointed as editor. Each issue would have reports from the president and the secretary general, along with pertinent information of the IAOMS’ state of affairs, such as finances and membership details, including the names of new members. The Newsletter also encouraged national associations to publish announcements of their meetings and to report on their activities. In addition, the publication announced the new affiliated national associations.
While the revised Newsletter was meant to appear twice a year, in actual fact, it would appear only once a year until 1989.
It became clear from the preceding nine years that the IAOMS had been struggling with its position. On the one hand, it had achieved a respectable status, whereas on the other hand, there was a demand for further action that was frustrated by the limited funds available. The financial position did not allow for a professional secretariat as had been discussed several times in previous years.
The secretaries general used local secretarial staff to run the administration and at the same time served as association’s treasurers. The income was limited
indeed and hardly enough to conduct day-to-day business. The ICOS were not particularly profitable either, with rather small profits in Sydney and Dublin and a loss from the conference in Berlin. Most importantly, however, the association was led by busy clinicians who simply did not have enough time to put in more managerial professionalism. There were, for instance, no executive committee meetings between the conferences, despite an earlier decision to set aside money for these meetings to happen.
The new executive committee in Berlin made a start bringing about some changes and certainly made a correct analysis when Dan Laskin formulated the goals for his term of office “to improve communications, to expand our educational activities and to increase the involvement of the fellowship.” Those goals could have been written today.
It is of interest to learn that a meeting was organized in 1984 between the executive committee of the European Association of Maxillofacial Surgery (EAMFS) and representatives of the IAOMS executive committee.

David Poswillo, the secretary general at that time, writes, “There was an obvious interest on both sides in maintaining regular contact between the associations with a view to closer ties, possibly federation and in the long term, to a World Federation of Specialist Associations.” It was also decided that a liaison committee be set up to report back to their respective executive committees. Sadly, this never occurred, but how close these thoughts were to the recommendations of the Tenerife and Bermuda conferences!

This executive committee was also the first to write guidelines for governing international conferences. This document underwent several corrections and extensions over the years but the sheer fact that it existed was important and it was a move in the right direction.
1986: The 9th ICOMS, Vancouver
The apotheosis of this period was the 9th ICOMS in Vancouver organized by our Canadian colleagues under the capable chairmanship of Alva Swanson. Vancouver, at that time, was also hosting a World Exhibition, which formed a real attraction for those who attended. This was the first really big meeting with 795 delegates and 263 accompanying persons from 39 countries.
The scientific meeting was excellent and included three symposia and several limited attendance clinics and
Dan Laskin presents Bill van der Kwast with a pin for his service as secretary general from 1980–1983.

no less than 254 oral presentations. It is worthy of note to read the titles of these symposia as they still would be relevant in the present day: “The maintenance of stability in facial advancement procedures; Tissue transfer in consideration of maxillofacial repairs and alveolar ridge replacement with alloplastic materials.”
The social program was also memorable, particularly the ladies’ program, as they were very well looked after by a special ladies committee.
Three new honorary fellowships were awarded: Bill van der Kwast and Norman Rowe received their distinction at the meeting but Gerry Leatherman, the person who brought Fred Henny into contact with Terry Ward, was awarded his designation in 1987 at an executive meeting in London at the Royal College of Surgeons. He was then in his late 80s and wrote to the secretary general these memorable words: “As an old man with a listening heart rather than a listening head, I am really very conscious of the honor offered to me and which is totally unexpected. One is more
The executive committee and councilors at the 9th ICOMS in Vancouver. Front row from left to right: Al Swanson, Geert Boering, David Gutman, Wilfried Schilli, David Poswillo, Dan Laskin, Jean-Marie Vaillant and Basilo Arienza.
forgotten than remembered at my time of life. Naturally I am delighted to accept when your Executive next meets in London.”
At the Council meeting in Vancouver, it was decided to terminate the official affiliation with the FDI, which had existed from the beginning.
The membership had grown in this period from 1,074 to 1,737 and there were 25 affiliated national associations by the end of 1986. The French had two affiliated associations but one councilor, whereas the five Scandinavian countries were represented by one councilor.

References
Kwast van der, WAM, personal communication.
Minutes of Executive Committee and Council meetings 1965–1986. Newsletters, 1976–1986.
Rowe NL, News Sheets of IAOS, 5–7, 1968–1971.
Stoelinga PJW, Editor, Proceedings Consensus Conference: The Relative Roles of Vestibuloplasty and Ridge Augmentation in the Management of the Atrophic Mandible. (8th International Conference on Oral Surgery).Quintessence Publishing Co., Inc. Berlin, 1984.

Walker RV, Rud J. History of the International Association of Oral Surgeons 1962–1986 and International Association of Oral and Maxillofacial Surgeons 1986–1996. Int J Oral Maxillofac Surg 1996: 25 254–63.
Ward TG, News Sheets of IAOS, 1–4, 1965–1968.
Chapter 3
The International Association of Oral and Maxillofacial Surgeons (1986–1999)
A wind of change
As mentioned in the previous chapter, the IAOMS had outgrown its teething problems but had not been able to assume its coordinating function largely because of the lack of funding to create a professional organization with a permanent headquarters and an executive staff. The coming 14 years would turn out to be crucial as progress was made to achieve such an organization. A series of devoted, strong-willed presidents with a clear vision, assisted by other members of the executive committee, worked steadily towards a better organization that would meet the requirements of a changing time. Another factor that contributed to the rapidly changing professional world was the collapse of the “Iron Curtain.” Several East European nations became independent and established national associations of OMF surgery that subsequently joined the IAOMS. Oral and maxillofacial surgery also grew in other parts of the world, which is reflected by the enormous increase of affiliated national associations during this period. The event that had the most impact during this period, however, was the introduction of the “Guidelines for Education and Training.”
As described in the previous chapter, the lack of a common pathway for training and education in OMF surgery had split the profession for many years. Previous attempts to achieve a consensus had failed and had even deepened the divide between the various educators and trainers. The keys to a change in attitude were the invitational conferences in Tenerife and Bermuda.
The Tenerife and Bermuda conferences (1987–1988)
The persons to be credited for taking the initiative for the Tenerife and Bermuda conferences were Wilfried Schilli, who became president of the IAOMS in 1986 after the Vancouver meeting and Rudi Fries, at that time president-elect of the European Association for Cranio-Maxillo-Facial Surgery. These two colleagues had a vision to break the deadlock that existed between the supporters of the double degree and those who stuck to the single dental or medical degree, by organizing invitational meetings with leaders of the specialty from all corners of the world.
There was no consensus within the executive committee of the IAOMS about this plan and, therefore, it was organized as a private enterprise by these two gentlemen and four former presidents of AAOMS, including Jack Gamble, Dan Laskin, Charles “Scotty” McCallum and Bob Walker. Wilfried Schilli had assured himself beforehand of the backing of his German colleagues. He had also built up a good understanding with several American colleagues, because he had been teaching throughout the U.S.A. about rigid fixation according to the AO principles.

The first invitational conference was held in Tenerife from April 26 to 29, 1987. The planning committee had invited 87 selected OMF surgeons from 36 countries, who were considered to be the leaders in the specialty in their own countries. A total of 53 attendees showed up from
• A model of professional education and surgical training for future OMF surgeons.
• International organizational unity.
The participants also agreed on a vertical structure in which the continental organizations would determine the delegates to the IAOMS council based on the percentage of the continental members. Members of the national associations would automatically be members of the continental organization and the IAOMS for a fee.
It is of interest to note that a strong suggestion was made on the governance of the IAOMS. There was a detailed recommendation on how the executive committee should be put together along with a roster of succession. There was also a pertinent statement about the desired management of the IAOMS: “The unanimous position of
24 countries and all came at their own expense. There were representatives from Asia, Australia, North and South America, and Europe. The surprise was the attendance of György Szabó, who managed to get the permission of the then existing regime of Hungary, in spite of the strict restrictions on travel. The purpose of the meeting was to review and deliberate:
First, the education of the oral and maxillofacial surgeon and the scope of oral and maxillofacial surgery.
• Second, the status of organized oral and maxillofacial surgery internationally and how to improve cooperation and more effective communication among countries to create a strong international oral and maxillofacial surgery organization and to enable the specialty to speak with one voice internationally.
There were very lively discussions but the participants agreed fairly easily on the following:
• T he scope of the specialty and the factors that might influence the scope.
• T he professional education.
T he surgical training (five years) of which two years of core surgical training and three years of concentrated OMF surgical experience, or alternatively one year and four years.
the Tenerife Conference was that the administrative operations of the IAOMS be conducted by a full-time, salaried and experienced administrator at a permanent IAOMS headquarters, with an additional full-time staff of at least two. The site of the IAOMS permanent headquarters preferably to be located in Europe.”
A report was drawn up which served as a working paper for the subsequent meeting a year later. This conference was held from April 28 to May 1, 1988 at the Princess Hotel in Hamilton, Bermuda. The attendance at this meeting differed slightly from the first meeting
“We should stop the fighting in our backyards if we are to make progress.”Shown in an off-duty moment at the Tenerife conference from left to right: Drs. György Szabó (Budapest, Hungary), Mikko Altonen (Oulu, Finland), Alekso Pisceric (Belgrad, Yugoslavia), Victor M. Sada (Madrid, Spain).
As mentioned before, the success of the Tenerife and Bermuda conferences was, in part, due to the fact that the leaders of the various national associations were invited on a personal note, instead of the representatives of the national and regional executive committees. This caused some frustration and outspoken criticism. David Poswillo, the secretary general of IAOMS, apparently had no part in these discussions. According to Wilfried Schilli, he was against this meeting for unknown reasons. He vented his anger in the secretary general’s column in the first Newsletter of 1988.
“What is not widely known is that the original invitation, which was sent only to selected people, came from the address of the headquarters of the AAOMS on specially printed paper which listed the names of several senior officers of the IAOMS. It is not surprising that without any clarification or other effort of communication, great confusion should have arisen. It is even more bewildering to read in the report of the Tenerife Conference that 18 months were spent in the planning phase. During this ‘planning period,’ there were numerous meetings, all official, of the General Assembly at Vancouver and many other opportunities for those involved in the planning committee to inform their colleagues on the Executive Committee and/or Council of the preparations and the ideas behind the proposed conference and to communicate these matters globally through the lines of communication already established by the IAOMS. That senior officers, all bearing the responsibilities of trustees of the association, should have acted without communicating on any official occasion associated with the IAOMS is bewildering in the extreme. It is this bewilderment which caused the anxiety and aggravation referred above.”
It is obvious that David was left out of the plot. It may not have been all that elegant, but it was certainly effective.
Paul J.W. Stoelingaas 54 attendees were present again from 24 countries. The participants came again at their own expense. Some attendees from the first meeting did not show up and there were some new faces.
The meeting began with presentations from various colleagues providing feedback from the different national associations on the report from the first meeting. The participants were subsequently divided in four groups to discuss scope, education and training and international organization. From the reports of these workshops, a draft report was put together that was called: “Final summary of deliberations of the first and second invitational conferences on oral and maxillofacial surgery.” It differed very little from the report of the first meeting. This report was submitted to the IAOMS and served as a draft for the “International Guidelines for Specialty Training and Education in Oral and Maxillofacial Surgery.”
In retrospect, one only can admit that the procedure followed had the desired effect. The sheer fact that individual, influential colleagues were invited instead of official representatives of national and regional associations was the key to the success of both meetings. However, this was a mixed blessing, since some associations were not 100 percent supporters of the meetings. It was, therefore, difficult to implement the proceedings of the meetings.
Yet, there was an ambiance of genuine desire to come up with something constructive. As one of the participants stated: “We should stop the fighting in our backyards if we are to make progress.”
The agreement in principle on the scope of the specialty was the deciding factor in the formulation of a sensible report that turned out to be instrumental for the development of the specialty, particularly in the countries where OMF surgery was just developing. The final document has been very helpful in many countries by convincing local health authorities to recognize the education and training of OMF surgeons. It has also served as the basis for regional documents geared to the needs of the region.
The governance of IAOMS
The selection of officers of the executive committee in the past had largely been through recommendation of the existing officers. This practice was still in place, certainly at the beginning of this period. Wilfried Schilli, for instance, was asked by Bill van de Kwast to join the executive committee in 1983 by telling him: “Wilfried, you are the first German president of the IAOMS.” These candidates were subsequently voted in by council without much
dispute. This was not necessarily bad and reflects the spirit of the time but had little to do with democracy.
At any rate, the series of presidents who came in this period and with them the other members of the executive committees, had a strong feeling that things had to be changed in order to make the IAOMS a true coordinating organization. One of the major differences, as compared to the previous period, was the regular, yearly meetings of the executive committee, which provided the much desired continuity in the governance of the association.
Wilfried Schilli spent most of his energy on the Tenerife and Bermuda conferences in order to create harmony among OMF surgeons worldwide. He also initiated the change of the editor-in-chief of the Journal. The Journal suffered from a low circulation and from a low impact on the profession. The appointment in 1988 of Paul Stoelinga turned this around. The executive committee decided to make the Journal compulsory for the regular members as of 1990, whereas the new editorial policy, with clear sections in the Journal, made the Journal a lot more attractive (see chapter 6)
W the e X e cuti V e committee W o rkedThe Executive Committee in this period met at least once a year; once in conjunction with the ICOMS and during the other years, in various places of the globe. The attending members were reimbursed for their travel expenses on the basis of an economy fare, while they received a daily allowance that covered room and boarding for three days. This was not the case when meetings took place at an ICOMS. It was assumed that all members then paid their own fares, because they attended the ICOMS anyway.
Contrary to what a lot of IAOMS Fellows thought, these meetings were no pleasure trips, even though some attractive cities were chosen as meeting places, mainly because they had hub airports. The meetings would last for two full days and required a lot of attention from the members of the committee, since the agendas were typically quite ambitious. The common denominator of all these meetings, however, was that half of the committee members had a jet lag of at least six hours. It was, therefore, not unusual to see some people with closed eyes while discussions took place.
The agendas contained items such as reports from the president and secretary general, which included the financial statement and budget for the next year. These were based on rather vague accounts and presented in a casual manner, certainly at the beginning of this period. They definitely would not be considered adequate in present times but the association was much smaller in those days and professional personnel were lacking.
A lot of time was spent on the upcoming ICOMS with all its implications, both regarding its scientific content, as well as financial matters. The meetings also had reports from the editors of the Newsletter and the Journal, including the financial implications but above all the distribution of the Journal to its members. This was a consistent source for concern, since the membership administration could not keep up with the changes that occurred and did not manage to coordinate its administration with that of the publisher.
There was usually a report of the chairman of the Education Committee, which commonly caused quite a bit of discussion. The chairmen of the other committees were only present at ICOMS meetings and usually had little to report. The remaining part of the meetings would be used on topics such as discussions on the desirability to create a fund that could sponsor educational activities and the establishment of a permanent office. The latter was a constant issue and gained in actuality towards the end of this period.
These meetings were conducted — and still are — in an American fashion, which is rather unusual for non-Americans, to say the least. There was and still is, a lot to learn for newcomers. The president chairs the meeting and allows for free discussions to take place. So far, quite understandable.
When he senses that a consensus or majority is in the making, he then asks whether there will be a motion on the table. He cannot do that himself. One of the committee members has to formulate this motion, after which it needs to be seconded by another member. Then follows a ritual that probably stems from the early days of the American constitution. The president asks: “All in favor, say ‘yea’,” followed by: “All against, say ‘nay.’” Without counting the votes, he then inquires about members abstaining. This all happens very quickly and I am quite sure that many non-American members of the executive committee must have wondered when they were laying in bed after a long day of meeting, fighting their insomnia because of jet lag, what had taken place and what they had voted for. Considering the adopted policies over the years, however, they had not been sleeping all the way.
Paul J.W. Stoelinga1989: The 10th ICOMS, Jerusalem
Wilfried Schilli’s presidency ended in 1989 in Jerusalem, where the 10th ICOMS was held. Unfortunately, the appointed chairman, Jacob Epstein, had passed away the year before the meeting. He was replaced by E. Rorien, who, with his committee, did a wonderful job. The conference was again very well organized but poorly attended because of the political situation. A total of 439 participants were present, of whom only 224 were members of IAOMS, and 108 were accompanying persons.
Together with the president, David Poswillo stepped down as secretary-general, a position he had occupied for six consecutive years. During his period of stewardship, the financial standing of IAOMS — despite the crash of October 1987 — had remained strong and quite undamaged by the collapse of the international markets. Yet, the funds available were not sufficient to create a permanent office with a professional staff, a wish of all the executive committees of the coming years. It is also rather tragic that this great contributor to the specialty was somewhat bitter about the invitational conferences held in Tenerife and Bermuda. He personally was not invited because he did not agree with the strategy of organizing these meetings outside the context of the IAOMS.


Bob Walker followed through, emphasizing the need for visibility of the IAOMS, by proposing educational meetings between ICOMS meetings and by stressing the importance of the Newsletter. The usual membership, education and scientific committees were revived by appointing new members and chairmen. Dan Laskin, the past president of the period 1980–1983, took the position of secretary general. David McGowan, a professor of oral surgery in Glasgow, was appointed editor of the Newsletter in 1986. He changed the Newsletter into a very informative format but it

still appeared only once a year. He was followed by Professor John Frame from Birmingham, U.K., in 1989, who planned to increase the frequency to twice a year but also found it difficult to put that into effect.
The Executive Committee in this three-year period was very busy creating support for the “Guidelines” that were to be discussed and hopefully accepted at the next council meeting in 1992 in Buenos Aires. For this reason, Bob Walker wrote personal letters to all presidents of all national associations to pave the way for an open forum discussion at the ICOMS in Buenos Aires.

The Education Committee, under the guidance of John Helfrick, scrutinized the wording of the Bermuda document and put together the final version. The “Guidelines” were extensively discussed in Buenos Aires, where it became apparent that some opposition against the formulation of the preface existed, in which it was stated: “It is most desirable for this training to be formalized and that the oral and maxillofacial surgeon possesses both the D.D.S. or D.M.D. degree, or equivalent and the M.D. degree, or equivalent.” Yet, the “Guidelines” were accepted by a vast majority of council members and were printed in the International Journal in 1992.
The recommendations regarding the organizational structure of international OMF surgery were never published and unfortunately did not receive the attention that they deserved.
Another important change was proposed and accepted whereby it was decided to hold an ICOMS every two years instead of three years. It had long been felt that the impetus after an ICOMS was easily lost in the years between these meetings, where little activity took place. This change became effective in 1995.
1992: The 11th ICOMS, Buenos Aires
The 11th ICOMS in Buenos Aires in April 1992 was a great success, thanks to the outstanding organization of the Argentinean committee, chaired by José “Pino” Ferreria, with a record attendance of 920 registrants, of whom 460 were members, 355 were trainees and 105 were accompanying persons.

The next president was Bob Cook from Australia who was seconded by Dan Laskin as the secretary general. Bob had been a very active council member since 1983 and was well known in the professional world. He was to be the last president to serve a three-year period. During his presidency, the association really started to grow and the various committees, such as education, scientific and membership, were given clear instructions on what was to be expected. One of the important decisions made was that the education committee was asked to conduct a survey of educational and training policies in affiliated nations. The result of this survey then served as the basis for the education conference at the ICOMS in Budapest

Most importantly, the Executive Committee discussed the necessity of establishing a Foundation in order to assist in educational activities worldwide. Once the decision was made to form the Foundation, Bob really went out of his way to find funding and succeeded in securing a commitment from Mr. Walter Lorenz of $250,000.
During his presidency, again, extensive discussions took place regarding the possibility of establishing a permanent central office and an executive secretary. It was thought that the donation of Walter Lorenz would provide the money necessary for establishing such an office and employing an executive secretary. Plans were put on paper, including the financial consequences, which
resulted in the appointment of a part-time executive director, assisted by an executive secretary. The position was taken by Dan Laskin, a former president and previous secretary general, assisted by Ellie Coyne, a part-time secretary. Council also approved a change in the organizational structure that better reflected the importance of the various regions in the world, whereby from then on, the Executive Committee would include members representing the regional associations.
1995: The 12th ICOMS, Budapest
The 12th ICOMS took place in Budapest in 1995, organized by György Szabó and his staff. Some 900 participants from all parts of the world attended the meeting. Financially, it also turned out to be successful. The IAOMS received a substantial profit, which was necessary to continue with their ambitious plans.

Several novelties were introduced at this meeting, including an educational conference at which Alastair Goss presented the results of the survey on education and training policies in the various affiliated national associations. This document provided invaluable information previously unknown to the profession.
At this conference, a lively discussion also took place regarding a proposed wording change in the preface of the document on education and training, as accepted in Buenos Aires. The council finally agreed on this change, but the wording would continue to be a topic for discussion for the coming years and would finally be resolved in 2001 in Durban.
There were two occasions when a potential crisis arose, necessitating meetings of senior members of various organizations in order to retain the structure and policies of the IAOMS.
The first of these occurred following the publication of the “IAOMS Guidelines on Education and Training,” which had been developed and agreed upon during the council meeting in Buenos Aires in the autumn of 1992. The wording used in the document was seen by some as dogmatic and based very much on the practice throughout Europe. However, both the North American and Scandinavian associations, together with the Japanese, felt severely disadvantaged by the wording in relation to the need for a full medical qualification and threatened to resign from the association unless this section was replaced.
The Americans argued that their extensive training in anesthesiology equipped them with more than adequate knowledge and experience to satisfy the requirements for the general care of the patient under critical clinical circumstances. Equally adamant were those members from European countries for whom a fully registerable qualification in both medicine and dentistry was the only way that a person could satisfy the requirements of both the IAOMS and the European Medical Board for recognition as an OMS specialist in the EEC. Scandinavia was outside the EEC at that time.
The EACMFS and the AAOMS were charged with resolving their very significant differences, yet not disrupting the overall attempt at harmonization proposed by the Buenos Aires agreement, to which over 70 countries had been signatories, including the contentious parties.
Accordingly, the following individuals arranged a summit meeting at a neutral venue of a small city on the south coast of England, Chichester:
• Professor Daniel Lew, president of the AAOMS,
• Dr. John Helfrick, president of the IAOMS,
• Dr. Paul Stoelinga, president of the EACMFS, and
• Dr. John Williams, secretary general of the EACMFS
Basically, they were told to lock the door and throw away the key until such a time as they were able to send a cloud of white smoke through the chimney.
The solution came in the concept of “regionalization.” The guidelines were standards, which were the same wherever you trained or worked. However, how you achieved these inviolable standards was entirely a matter for regional or national trainers and registering bodies to resolve.
Qualifications were equally a regional or national responsibility and once the concept of regionalization was introduced were both superfluous to the guidelines and potentially, inflammatory. As such, they should be eliminated from the document.
These recommended changes enabled everyone to maintain their own positions and formed the basis of the modifications in the education and training document put to the council and ratified in Budapest in 1995.
Everyone thought they could breathe again but despite this approach, there remained dogmatic individuals who, instead of seeing this as a true breakthrough, continued to try to force their own point of view, failing in the process to recognize that there was more than one way to achieve the same outcome. People had to be able to achieve a common approach, yet in different ways, as appropriate to their own needs and circumstances.
All present were able to return, satisfied, to their own councils with no one having to give one iota on their principles.
Ll. WilliamsAt the request of the Executive Committee, the Scientific Committee, under the chairmanship of Kursheed Moos, organized a consensus conference on condylar fractures. This was one of the highlights of the meeting, with excellent speakers and it was attended by a large crowd. The proceedings of this conference were published in the Journal
It was also the first meeting at which the president invited a speaker to present the “Presidential Lecture.” Hermann Sailer from Zürich had the honor to be the first such speaker.
The next Executive Committee was chaired by Rudi Fries, a former president of the European Association for Cranio-Maxillo-Facial Surgery (EACMFS) and one of the driving forces behind the Tenerife and Bermuda conferences. Rudi had many contacts in East Europe with colleagues who had been totally unaware of the development of the specialty in the world. He had several contacts in the Arab world and in some African countries. He was very much committed to promoting the involvement of Eastern European colleagues in the EACMFS and in the IAOMS and in advancing the specialty in the less privileged world.


As a result of his numerous trips, he knew the key persons in the various countries and was, therefore, the right person in the right place at this crucial time in the history of the IAOMS. It was particularly the establishment of the Foundation in 1996, under the chairmanship of past-president Bob Cook that would enable the IAOMS to eventually become active as an initiator of educational programs in the developing world. The members of the Executive Committee, after a long discussion, decided to install a board of trustees for the Foundation, separate from the executive committee of IAOMS. It is of interest to note that this decision was reversed some ten years later (see chapter 5)


The “Bylaws” and “Rules and Regulations” underwent several adjustments and additions because of the changes that took place during this period, including the ruling that members of the Executive Committee could vote at council meetings. The past president would also get a vote in the Executive Committee but the most important
change involved the inclusion of regional representatives so as to have proper representation of all parts of the world on the Executive Committee.
This implied a considerable extension of the number of members on the Executive Committee but the decision really improved the committee’s communication with the regional associations. North and Latin America, Europe and Asia, including Oceania, from then on were permanently represented on the executive committee of IAOMS. This decision was fully in line with the recommendations as expressed by the participants of the invitational conferences in Tenerife and Bermuda.
Last, but not least, an important decision was taken about the governance of the IAOMS, which included moving the IAOMS headquarters to Chicago in 1998 and the appointment of a full-time executive secretary.
1997: The 13th ICOMS, Kyoto
The 13th ICOMS took place in Kyoto, Japan and was organized by Kenichi Seto and his organizing and scientific committees. Because of the large number of Japanese attendees, this became one of the best attended ICOMS in the history of the IAOMS. Again, several novelties were introduced, of which the invitational
participants discussed items such as:
• Helping underdeveloped countries improve services.
• Establishing uniform accreditation standards and developing methods of outcome assessment.
Financing educational opportunities.
• Promoting an expanded scope of capabilities.
• Establishing the OMS’ ultimate area of expertise.
• Preparing oral and maxillofacial surgeons to meet competition from other specialties.
Increasing the scope and participation at the ICOMS.
• Increasing IAOMS membership among fellows and trainees.
The proceedings of this conference were distributed among the representatives of national and regional associations. This conference set a trend for many years to come, as from this ICOMS on, invitational conferences were held covering various subjects of interest for national and regional leaders in the specialty. Another policy for future ICOMS was the publication of abstracts of the free papers in a supplemental issue of the Journal so as to make them accessible to the international readership.
Another new event introduced at this meeting was the “Great Debate.” In the future, this would be a fixed part of the scientific program, dealing with topics prone to evoke controversy. Each topic was introduced by two speakers; one for and one against, after which a rebuttal occurred, followed by an audience vote. At this ICOMS, the topics were: “Odontogenic Keratocysts” and “Disc Replacement after Discectomy.”
In hindsight, this was also a very successful meeting not only because of the excellent Japanese organization but also because it demonstrated the growing sense of
international cohesion. It certainly attracted more Asian attendees than ever before and, thus, made the IAOMS a true international coordinating organization to which many national associations turned for advice and assistance.
The last president of this period was Peter Banks, who much to his chagrin, served only for eighteen months, the shortest period ever for a president. This had to do with the fact that the Kyoto meeting was in September 1997, whereas the next ICOMS in Washington took place in April 1999. During his tenure, however, the final steps were set in place to create a permanent office and to attract a full-time executive secretary. The AAOMS generously offered a small space for a reasonable rent at their new headquarters in Rosemont, Illinois.

The Executive Committee held its first meeting in the AAOMS building in December 1998. Peter, along with John Helfrick, spent much time, selecting a candidate for the position of executive secretary. In January 1999, Lynne Sayler became the first executive secretary. This, in retrospect, may be called a milestone in the history of the IAOMS. A dream of many previous presidents and members of the executive committees had come through. How right a decision this turned out to be!

There were, however, further developments that made this a true transitional period. The presence of regional representatives at the Executive Committee meetings allowed for direct information about regional matters of interest. For the first time in the history of IAOMS a real worldwide representation was present that appeared to be very useful, particularly in the way relevant information was exchanged. It also promoted the camaraderie among

delegates from around the world. Most importantly, it helped to establish well-functioning regional associations along the lines of the structure of IAOMS, notably in Asia and Latin America.
Another very important change introduced during this period was the appointment of a treasurer and a Finance Committee who would prepare and approve the budget and a yearly financial statement, checked by a certified accountant. Kent Cohenour was chosen as the first treasurer of IAOMS. This was thought to be necessary in the context of a new job description for the appointment of a new executive director, since Dan Laskin had announced his resignation as of the end of 1998. Victor Moncarz was suggested for this position, which was confirmed by council at the Washington meeting in April 1999.
Last but not least, the search for a new Journal editorin-chief resulted in the appointment of Piet Haers as the successor of Paul Stoelinga. After 12 years, Paul resigned from his post, leaving the Journal in a very healthy condition.

Probably the most time-consuming effort of Peter Banks was the drastic and thorough revision of the bylaws and rules and regulations. The many changes in the association’s governance, along with the various decisions taken on different subjects over the past several years made these changes necessary. It took an eloquent Englishman to do this job and in that sense, he qualified perfectly well.
1999: The 14th ICOMS, Washington, D.C.
The 1990s ended with the 14th ICOMS in Washington D.C. Unfortunately, this was not a well-attended meeting, despite the president’s efforts to attract the attention of his American colleagues for the event. The event’s organization was largely done by the AAOMS’ professional staff and lacked the personal touch that was the hallmark of previous ICOMS.



The theme for the invitational conference was: “Harmonization of education and training in oral and maxillofacial surgery worldwide.” This very relevant topic gave rise to lively discussions on how to establish centers of excellence in developing countries. The conclusions of this conference were summarized and sent to all participants and councilors. The following recommendations were made:
• T here is a need for the receiving country to organize the training for oral and maxillofacial surgery. For that reason a local, national association will be necessary to serve as a partner when discussing possible assistance from the IAOMS or regional association.
• W hen planning a training center that would be a candidate for international assistance, the presence of a local OMF-surgeon to act as a liaison person is mandatory.
• If possible, conceptual and financial support from the country in which the training center will be located should be received.
• Cooperation between IAOMS and the regional and national associations is necessary for the center to be successful. The IAOMS will assume a coordinating function in that all activities should be made known to the IAOMS secretariat.
• T he IAOMS will remain active with regard to harmonization of training and education, whereby the education committee will produce a working paper on how this can be achieved based on the draft of “Basic program of training in oral and maxillofacial surgery,” as circulated at the meeting.
•
It was felt that there is a need for certified programs following the guidelines from IAOMS. The IAOMS will provide a template against which national associations can match their programs.
Continuity in support was felt to be of paramount importance. For that reason, only a limited number of training centers, strategically positioned in the various regions, can be supported. The various regions were asked to come up with suggestions, particularly our African colleagues.
When reading these very sensible recommendations, one can only wonder why this has not been implemented in full. At present, the IAOMS still lacks the pertinent information necessary to play a role as overseer of all activities, while cooperation with some regional associations still leaves much to be desired.
On this occasion, Bob Cook was honored as a “Distinguished Fellow of IAOMS.” He was the first to receive this award, since the category of “Honorary Fellow” had been changed by the executive committee to apply to individuals who were not oral and maxillofacial surgeons but had made special contributions to the specialty. Bob had been involved for many years in the governance of IAOMS and was the first chairman of the IAOMS Foundation.


Budget and membership fee
Since the inception of the IAOMS, the membership fee was $15, an amount that went unchanged until 1990. From the beginning, with a short interruption, members also had the option to be a life fellow, which implied a one-time fee of $300. This fee was raised to $500 in 1990. The rationale behind the “life fellow” idea was to build up a corpus of money that would generate income from interest and dividends.
Considering the fact, that in the beginning, membership only grew on a modest scale from around 500 to 1,000 members, it is not surprising that the lack of funds kept many executive committees from expanding their activities. The situation became slightly better in the second half of the 1980s, mainly because of the considerable profit made at the 9th ICOMS in Vancouver, which was very well-handled by David Poswillo. He transferred the money into British pounds and made a handsome profit by changing the money back again into US dollars some years later, due to a more favorable exchange rate.
The growth of the membership in these years also accelerated, which further contributed to a more stable financial situation. However, the yearly budgets in these years still did not allow for needed initiatives to be financially supported. It is, therefore, not surprising that
it was decided in 1990 to increase the membership fee to $85. This went along with the decision to make the Journal compulsory for Fellows.
Since that time, the fees have increased to keep pace with inflation rates, while additional income has been generated by institutional and individual subscriptions to the Journal. The category of life fellowship was discontinued in 1993. Until this book’s publication date, there were some 400 life fellows but this number will gradually become less and less and finally disappear altogether. Modest profits from ICOMS’ in the ensuing years and the donation from Walter Lorenz also improved the financial situation considerably.
An important change in the dues structure was decided upon in 1997. After many discussions about the need to adapt the dues for the less privileged world and to create an attractive vertical membership for national associations which joined with all their members, these policies were finally implemented in 1998.
Reduced membership fees were offered to members from countries with a GDP of less than $7,500 per capita, based on the data presented by the United Nations Human Development Index. It made the administration of membership somewhat more complicated but has served its purpose well until now. This change made it more attractive for colleagues from less developed countries in Africa, Asia, East Europe and South America to join. In fact, this did happen as membership of these countries increased. The first association to adopt vertical membership was the Dutch, soon followed by the Argentineans, the Swiss and later the Hong Kong association.
Until 1999, the IAOMS’ financial matters were dealt with by the secretary general, who was assisted by Andrew Linz, a former
IAOS executive committee member (1974–1980) and loyal supporter of IAOMS, who mainly advised on investments. A formal treasurer was finally appointed in 1999, which turned out to be a very good decision, since real expertise in these matters proved to be quite beneficial for the association (see chapter 4)
Epilogue
During the period 1986–1999, the IAOMS gained tremendously in terms of importance and professional status. The more than doubling of the membership from 1,737 to 3,778 and the growth in the number of affiliated associations from 25 to 52, also signaled the association’s growing impact worldwide. It was particularly the concept of regionalization that appeared to be instrumental in achieving global approval for the “Guidelines of Education and Training” but also for other activities, as will become evident in the next chapter.
Another major step forwards was the establishment of the Foundation. Bob Cook’s plan to establish the Foundation was amended and agreed upon at the ICOMS in Budapest. The further development of the Foundation will be described in chapter 5.
The tireless efforts of all presidents during this period paid off, since many contacts were made that had paved the way for better relations among colleagues worldwide. The weight of the presidential job had grown enormously and the position had become crucial for the success of the IAOMS.
Presidents not only visited national association meetings in different parts of the world, they also attended regional conferences, meeting with much larger groups of colleagues than ever before. Invariably, they were received with due respect, which increased the visibility of the association. These regional meetings were often also used as opportunities to informally meet with members of the executive committee that lived in those areas. In short, the association gained in its professional conduct and was ready to make the next jump.
References
Banks P., Personal communication.
Cook R., Personal communication.
Fries R., Personal communication.
Schilli W., Personal communication.
Walker R., Personal communication.
Editorials, International Journal of Oral and Maxillofacial Surgery, 1988–2000.
Final Summary of the Deliberations of the First and Second Invitational Conferences on Oral and Maxillofacial Surgery. Planning Committee: Rudolph Fries, Jack W. Gamble, Dan M. Laskin, Charles A. McCallum, Wilfried Schilli and Robert Walker, 1988.
the lost chain
The chain, a rather valuable ornament donated by Andy Linz in 1971, was a precious thing to travel with but also a matter of great concern to all presidents. From the beginning of the tenure, a decision had to be made as to where to store it when not in use. There was the possibility to store it in a safe at a bank, or to keep it at home in a safe place where potential burglars would not find it. Both options had their advantages and disadvantages, as many presidents experienced. In case an official trip had to be made, a visit to the bank had to be made when it was stored in a safe, which was time consuming and a bit of a nuisance. Keeping it at home was more user-friendly, but a constant reason for some worry. Each president made a choice and so did Bob Walker. On one occasion when Bob needed the chain, a truly nervous search was made at the Walker home. The chain, however, appeared non-findable and Bob took its loss as a real gentleman, not planning on losing face. He simply had a new one made at his own expense. The story would have gone untold if the lost chain had not eventually turned up. The matter of the fact is, however, that it did turn up when Emily (Bob’s wife) decided on a real cleaning exercise, including various cupboards and closets. Sure enough, it turned up behind a stack of cloths or sheets. Apparently, Bob or Emily had hidden it away too well so as to hide it from the eyes of unwanted guests. In hindsight, it was a good investment, but Bob was left with an attractive but pretty useless, trophy. Where it is currently hidden is unknown.
 Paul J.W. Stoelinga
Paul J.W. Stoelinga
International Guidelines for Specialty Training in Oral and Maxillofacial Surgery.
International J Oral Maxillofacial Surg. 1992: 21; 130–32.
Leadership Conference Compendium of all contributions. Kyoto 1997. Editor: PJW Stoelinga.
Minutes of the Ex. Committee meetings of the period, 1986–1999.
Minutes of Council meetings of the period, 1986–1999
Newsletters , 1986–1999. McGowan D., until 1989, Frame J., until 1999.
Report on the First Invitational Conference on Oral and Maxillofacial Surgery, Tenerife, 1987.
Chapter 4
The International Association of Oral and Maxillofacial Surgeons
(1999–2012)
Modern times
With the introduction of new methods of communication and, above all, with the emergence of a new generation of leaders in the profession, a new era had begun. The IAOMS had grown into a large organization with global representation and needed to be managed accordingly.
The newly structured executive committee with energetic presidents, who had gained managerial experience in national and/or regional associations, pushed the organization further forwards. Computers and websites facilitated communication but at the same time, the issues to be tackled became increasingly more complicated and certainly involved huge financial input. On top of that a new generation of baby-boomers and generation X’ers were not used to the old fashioned, rather direct approaches from previous executive committees. The style of governance gradually changed, driven by the rapidly “globalizing” world with a generation that had different priorities as compared to past generations.
The headquarters

The IAOMS literally used to be run from a cardboard box. The lack of a permanent office and a less than up-todate membership administration did not do any good to the association’s reputation. The move to Rosemont, Illinois, therefore, was like a breath of fresh air. Lynne Sayler settled nicely in a rather small office that was soon filled with all sorts of boxes and other items that needed to be filed.
The purchase of a computer and printer were the first steps to a professional
organization. Lynne was wholeheartedly received by her colleagues from AAOMS and in fact took advantage of their experiences on how to run a large organization. The board of AAOMS generously let the IAOMS executive committee use their splendid board room for the meetings that usually took place during weekends.
The first priority was to set up a better membership organization. With the help of Patrick MacGinnis, this was done in such a way that finally there was control of who had paid their dues and who had not and who received Journals and had paid for them. In previous years, this had been a major cause of frustration for both the executive committees as well as the membership. The next step was trying to set up a website, which turned out

to be a harder nut to crack. Again, Patrick spent a lot of time getting this working but not being on the spot made it difficult for him to be effective. Alexis Olsson, the new assistant executive director, also worked very hard to produce the website, which went “live” in 2000.
Despite the generous hospitality from AAOMS, it soon became obvious that the office space was too small. The search for another space in the Chicago area was, therefore, begun. The burst of the IT bubble made it somewhat easier to find a nice space for a reasonable rent.
After many discussions and visits to two selected options, the board decided on the new location in Oak Brook, Illinois. Two thousand square feet appeared to be perfect for the rapidly expanding secretariat. This move
The second crisis leading to another high-level Chichester meeting occurred a few years later, just as we were thinking that “Regionalization” had been implemented and no problem existed.
Again, the vexed parties were the Americans on one side and the Europeans on the other side, although there also was a side issue with the Scandinavians. The Americans did not feel their interests had been adequately addressed, even though the ratification by the IAOMS council in Budapest should have settled the matter. The Scandinavians, largely led by the Swedes, did not feel that they had been accepted adequately within Europe, a view for which they sought support from the Japanese association.
The players around the table this time were only slightly different from the first Chichester meeting, although they were wearing different hats. The only newcomer was Don Booth, president of AAOMS, and John Helfrick, past president of IAOMS, who this time were joined by Paul Stoelinga as IAOMS president, and John Williams, who continued to represent the EACMFS, except that this time it was as its president.
The issue boiled down to a lack of understanding of what was happening in relationship to “Regionalization.” The Scandinavian association and, in particular, Sweden, felt they were being severely disadvantaged in terms of being able to achieve full membership in EACMFS and consequently, they believed the European association was in default of the IAOMS guidelines on regionalization, despite reassurances to the contrary from the officers of the EACMFS. The European association subsequently had to amend their “Rules and Regulations”, always a lengthy process, to satisfy the IAOMS concept while at the same time fulfilling the needs of the European association regarding the majority practice in Europe where both medical and dental qualifications were essential pre-requisites for the specialty. This requirement was clearly laid down by the EEC within the “Directive on Monospecialities.” At that time, the Scandinavian countries were not members of the EEC.
The reasons for the discord, together with the explanation, were accepted by the Americans at the meeting but it was not until an open confrontation at the council meeting in Vienna that the Scandinavians were shown to be at fault in their promoting an incorrect picture of the situation. At that point, the Japanese association accepted the fact that they had been misled and the issue was resolved once and for all.
As a result, the American association was again firmly on board and remained able to continue their stance on the role of both medicine and dentistry in relation to fulfilling the educational and training guidelines of the IAOMS. Honor was satisfied on all sides and there was no blood on the carpet. Chichester as a neutral venue had once again proved its value. Perhaps it was the ambiance, or maybe it was the food or beer!
John Ll. Williams
turned out to be one of the best initiatives of IAOMS, because the opportunity existed to expand when it was needed and the current office offers a nice meeting room for the board and separate offices for the executive director and the president. All secretarial staff had desks with plenty of filing space.
The office was opened on February 3, 2003. The first board meeting was held in the new space in March of that year and was followed by an open house reception attended by our former hosts, the AAOMS board of directors. In short, the space could not be better.

During this period, it appeared necessary to expand the office space to accommodate a new person on the staff, who would be responsible for marketing the association and development and fundraising for the Foundation. Kerry Spaedy was chosen for this position and began working at the IAOMS in July 2006.


A new era of governance
With John Helfrick at the reigns, a true new era had begun. One of the first moves, under his governance, was to have the executive committee really assess the role of the IAOMS in this global world. Two very special sessions were organized under the guidance of an expert mediator, Russell Massaro, one in Chicago in 1999 and one a year later in Amsterdam. Both sessions focused on an analysis of the strengths, weaknesses and opportunities of IAOMS and how the association should proceed to address the various problems that lay ahead.
The result was a clear mission statement and the formulation of a vision. These were later implemented in the bylaws of the IAOMS. From these sessions, a strategic plan evolved with specific aims to be achieved within well-defined time frames. After ample discussions within the executive committee, the plan was modified and brought to the invitational conference in Durban in 2001. There it was discussed at length and changes were suggested that were implemented in the next version. The plan was meant to serve as a guideline until 2007 with periodic progress assessments and, if necessary, adjustments at each meeting of the board or executive committee.
Discussions during these two special sessions also centered on the “International Guidelines for Specialty Training and Education” as accepted in Buenos Aires in 1992 and later modified in Budapest in 1995. As there was no consensus within the executive committee with regard to the desired degrees before OMS training could begin, a serious confrontation threatened to take place again between mainly Europeans on one side and Americans and Japanese on the other.
The enormous cohesion that existed after Tenerife and Bermuda had disappeared, as had the spirit that went along with it. An emergency meeting was organized between IAOMS president John Helfrick; the president of AAOMS, Dan Lew; the president of EACMFS, John Williams; and Paul Stoelinga, IAOMS president-elect and a former EACMFS president. This meeting took place in July 2000 in Bosham, near Chichester in the south of England.
Eventually, after long discussions, a compromise was reached on the wording of the document’s preface. It took a lot of convincing to finally get this modification

final document, however, was agreed upon again, much to the relief of everyone involved (see addendum)
A practical change in the governance of the association was also introduced by John Helfrick. The executive committee had expanded so much it was now too large to be efficient. Additionally, it was also rather expensive to meet every year with a group of almost 20 people from all over the globe. Nonetheless, a lot of daily work needed to be done, preferably by a relatively small group of people.
For this reason, a new table of organization was proposed and accepted by the executive committee and later by council. A small group of officers would form the board, which would, along with the executive director and assistant executive director, take care of the daily affairs. The board would consist of the president, the presidentelect, the past-president and the treasurer. This made the running of the association a lot more practical and efficient. This board would also meet more frequently, often taking advantage of regional association meetings to convene. When urgent decisions had to be made by the executive committee, this was done either by mail or postponed until the next ICOMS.
Apart from these major issues, some less catching but certainly important issues were tackled:
• T he 2000 edition of the “Parameters and Pathways: Clinical Practice Guidelines for Oral and Maxillofacial Surgery,” as prepared by AAOMS, was endorsed by the IAOMS. Many affiliated associations followed this good example.
• T he manual for preparing an ICOMS was thoroughly revised so as to meet the changing demands of the IAOMS and to accommodate a much larger attendance.
• T he education committee, under the leadership of Alastair Goss, was restructured to include all chairmen of regional educational committees. This was done not only to improve international cooperation but also, above all, to improve understanding among the regions.
The education committee was asked to review the “International Guidelines for Specialty Training and Education in Oral and Maxillofacial Surgery” again and to formulate a core curriculum for developing countries with the idea in mind of commencing educational programs in these countries. They were also to come up with a plan for certification of trainees from these
countries. Unfortunately, their proposals were not accepted by the executive committee for various reasons. Core programs proved difficult to define because the regions differed in their needs, while IAOMS was hesitant to provide certificates simply because the IAOMS is not an accrediting body. It was generally felt that this was a national or regional responsibility.
At the same time a communications and technology committee was established as it was thought that this would be important in times where new technologies were overwhelming the specialty. This committee had a promising start but never became productive.
A very important and far reaching decision was the change of the Journal’s publisher, preparations for which were already completed by the previous executive committee. It had become obvious that the Journal was losing money instead of being a source of income. After consultation with the association’s legal counsel and the evaluation of several proposals from various publishers, including one from Munksgaard, Harcourt Brace (later taken over by Elsevier) was chosen for its acceptable offer. The transition became effective in 2001. This move turned out to be beneficial to IAOMS with regard to the profitability of the Journal. As a result of the change in publishers, for the first time in its 29-year history, the main asset of the association, the Journal, became profitable.

chairmanship of Patrick Uys, organized the first ICOMS on the African continent. This meeting, again, had a very special flavor because of the personal touch of the organizers. The attendance was somewhat disappointing — 539 registrants with 127 accompanying persons but the organization and hospitality were unsurpassed.
The conference featured a special trainees’ session that was very well attended as a number of trainees were

iaoms organization chart
Board of Directors and Budget & Finance Committee
• President
• President-Elect
• Past-President
• Treasurer
Three At-Large Regional Members
Foundation Board of Trustees Regional Representatives
• Africa
• A sia
• Europe
• L atin America
• North America
• Oceania
sponsored by their national benefactors, while a few were supported by the IAOMS Foundation. The biggest event was the Invitational Conference, to which all national presidents were invited, along with all IAOMS councilors. As mentioned before, the topic was the draft strategic plan, which received lots of comments and suggestions for improvement. A revised version would later be sent to all councilors, who approved the new version in 2003 in Athens, after which it was published in the Newsletter, including an accompanying budget.
Leonard Kaban was the Presidential Lecturer, and he talked about the biomedical technology revolution and the opportunities and challenges that we are facing.
The executive committee also approved a motion to accept Oceania as a new region. A lot of discussion within
Non-Voting Members
• Journal Editor
• Education Committee Chairman
• HADR Committee Chairman
• ICOMS Committee Chairman
• IT Advisory Committee Chairman
• Research Committee Chairman
the Asian association had preceded this move but eventually both sides agreed to split up.
A novelty in Durban was the Foundation luncheon where Philip Tobias, an internationally acclaimed paleoanthropologist, presented a brilliant talk on “The hominid fossils of Africa with special emphasis on their facial and dental features.” The lunch raised money for the Foundation and this event would become a tradition for each ICOMS to come.
Three members of the executive committee, Peter Banks, Kent Cohenour and Jürgen Reuther completed their tour of duty. Peter especially had been instrumental in bringing about the changes in the governance of IAOMS. His particular sense of humor often caused a much needed tension break during meetings of the executive committee.
Kent’s input, too, can hardly be overestimated. He was responsible for a thorough analysis of the financial situation and subsequently for the proper budgeting and yearly financial statements that were approved by a registered accountant. Today these activities sound like an open door but these processes were lacking in previous years when General Secretaries were also the treasurers. Jürgen had played an important role in the discussions about the infamous “Guidelines.”
At the gala dinner Rudi Fries received a rightly deserved Distinguished Fellowship. He was the second oral and maxillofacial surgeon to receive this award. The role Rudi Fries had played in the policies of the specialty both in Europe and worldwide would be hard to be fully recognized. Special credit should be given to his tireless efforts to make contacts with first the Eastern European colleagues and later also with several African colleagues. This was almost always done at his own expense.
Thanks to Rudi Fries, many openings were made and the current educational programs in different parts of the world were largely initiated because of his constant pleas. He is a true icon of our specialty, not bothered by self image.

Another person who needs to be mentioned here is Alastair Goss. He stepped down after six years as chairman of the education committee and ex officio member of the executive committee. Alastair made the education committee work, unlike all previous committees. The inventory made in 1994 about the status of training worldwide, under his chairmanship, was truly a major effort and proved the importance of this committee for the governance of the association.
He was also responsible for the report on “The international growth and development of the surgical specialty of oral and maxillofacial surgery in the nineties,” which was the result of a follow-up survey, carried out in 2001. Questionnaires were sent to 54 national associations with a response of 41. It showed a marked shift towards a longer training period, as compared to the survey from 1992. Most likely the influence of the “Guidelines on Education and Training” as first published in 1992 and amended in Budapest, in 1995 and Durban, in 2001. This report also showed the wide scope of practice that exists worldwide.
His efforts to produce a core curriculum for less developed countries was equally important but appeared to be difficult to achieve for reasons mentioned before. He was followed in his role as Chairman of the educational
committee by Nabil Samman, who would continue on the same route, while also becoming heavily involved in IAOMS initiated and sponsored educational programs. The last person to be mentioned is John Frame who was the editor of the Newsletter from 1990 to 2001. He also retired and was replaced by Alexis Olsson, the assistant executive director.
The presidency was taken over by Paul Stoelinga with a new executive committee, because several new members had been voted in. The most important change was the appointment of John Williams as the new treasurer, since the board would now be in charge of the association’s daily affairs. John found himself thrown in deep waters despite his previous experience in both national and European affairs. American bookkeeping differs from European book keeping and even the terminology used is different in the two regions. Nevertheless, a decent three-year rolling budget was presented at the first board meeting. The finances were in proper shape supported by a handsome profit that was made by the South Africans on the XVth ICOMS in Durban. The aim was to run the association with the money received from the dues and to spend the dividends and interests on special activities as outlined in the strategic plan.
First IAOMS-sponsored educational course
One of the main things initiated during the period that Paul Stoelinga was president was the first IAOMSsponsored educational program in Hat Yai, Thailand. This program officially began on 17 March 2002 but was preceded by two years of preparation, including negotiations with the Thai Association of Oral and Maxillofacial Surgeons and officials of the Prince of Songkla University in Hat Yai and, of course, the IAOMS Foundation under its new Chairman Marsden Bell. The location in the south of Thailand was chosen so as to facilitate participation by trainees from other, neighboring, countries, in particular Indonesia. Henk Tideman, who was familiar with the region and the leaders of the Thai association, played an important role in making the program happen.
The success of this project, completed in 2005, exceeded all expectations. Some 150 very enthusiastic young colleagues of Thailand and seven neighboring countries attended and the teachers, from Europe, Asia, Argentina and the United States did an outstanding job. The “Thai project” became an example of how educational projects should be organized and was successfully transplanted

later to Peru, Indonesia and East Africa in versions adapted to the local needs. The European association used this model for a similar program in Iasi, Romania.
The IAOMS had finally fulfilled one aspect of its mission statement i.e. “The mission of the International Association of Oral and Maxillofacial Surgeons is to elevate the quality of healthcare worldwide through the advancement of the art and science of oral and maxillofacial surgery.” The dissemination of knowledge to less privileged countries would from now on be a constant issue in the policies of the IAOMS.
In this context it is important to mention the efforts to assist Africa as the last region to link up with IAOMS. Paul Stoelinga had made contacts in Durban to initiate the establishment of an African association and to seek their representation on the executive committee of the IAOMS. There were two further African associations at that time, apart from South Africa. Egypt and Nigeria representing the north and the west but the east was lacking. Through contacts in Kenya and Tanzania it was possible to create an East African association that represented nine East African nations. Professor Symon Guthua from Kenya became its first president.

At its founding meeting there were only 15 registered oral and maxillofacial surgeons, all trained outside their countries but as a result of newly established training programs in Nairobi (2001) and Dar es Salaam (2005) and with the help of the IAOMS supported educational program, a rapid increase of locally trained colleagues has occurred. In 2003, at the ICOMS in Athens, it was decided by the Africans present at that meeting, that a Pan African association should be established. It was for the next president, José (Pino) Ferreria, to attend their first meeting in 2005.
The governance of the association became more demanding because of the ambitious strategic plan, which implied all sorts of initiatives. The Executive Secretary was overwhelmed with work and the executive director simply could not physically keep up with the demands. Victor Moncarz was a non-salaried executive director and could only spend a limited amount of time on IAOMS business.
The Board, therefore, suggested the hiring of a salaried part-time executive director, who would physically be present in the office and could guide the expanding staff in coping with the growing work load. The executive committee agreed with this plan after
approving the job description drawn up by the board. This, for the time being, was the final step in the process of changing the governance of IAOMS into a true professional organization. John Helfrick expressed his willingness to take the job and was appointed in Athens.
2003: The 16th ICOMS, Athens
The XVIth ICOMS took place in Athens, Greece, in May 2003. The change to Athens was made, after a site visit by Peter Banks in 1999 when it became clear, that the original location, Corfu, did not have a hotel that could accommodate a meeting of the size of an ICOMS. The promised venue, at the time the choice was made by Council, simply had not materialized.
The organization of the conference was chaired by Angelo Angelopoulos assisted by his local committees and a Congress organizer represented by a rather shrewd lady. She promised a reception at the Acropolis and several other unique events, when a delegation of the Executive Committee went for a site visit. Unfortunately several of her promises did not come through but the conference turned out to be excellent thanks to the hard work of the Organizing and Scientific Committees. Much to the chagrin of the Executive Committee, however, no profit was made on this conference. The Iraq war and an outbreak of SARS made many Americans cancel their trip to Greece. The attendance was, therefore, somewhat disappointing (approximately 800 participants) but the ambiance of Athens made up for this drawback.
Again, an invitational conference was held this time on a very ambitious topic: “Standardizing and Advancing of Quality of Care in Oral and Maxillofacial Surgery.” It drew some 130 participants from all regions of the world and was preceded by four introductions from John Helfrick, Nabil Samman, Henning Schliephake and Alexis Olsson. They addressed the following sub-topics:
• R ole of practice guidelines.
• Clinical pathways.
• Education and training.
• R esearch and communication.
The full report of this conference was published in the Newsletter of March 2004. It appeared that the five participating regions had different priorities but all agreed on the need to promote “evidence-based practice” while admitting that this was insufficiently available in the current practice. The participants agreed, however, on the need for improving the website so as to promote education and communication. This was a desire that was soon to be met.
The Foundation luncheon in Athens was extremely well attended and the guest speaker, Professor Stefanos Geroulanos, entertained the participants with an outstanding lecture on “Ancient Medical Practice: What else could you expect in a country that was the home of Hippocrates? The presidential lecture was presented by Henk Tideman, the topic being “Vita brevis est longa art,” translated from Hippocrates: Life is short, the art is long. He presented his view on the development of the specialty mixed with his personal experience, which made an impressive talk.
An unforgettable boat trip through the Aegean Sea with visits to some small islands was the highlight of the social program, organized as a half-day break away from the scientific program. This was a much appreciated novelty in the organization of an ICOMS.
At the usual Gala Dinner, John Frame, the editor of the Newsletter from 1990–2001, received the IAOMS Distinguished Service Award for his outstanding service during this period. This award had been established two years previously. José (Pino) Ferreria took over the presidency. John Williams became president-elect and Don Booth became the new treasurer.



The inauguration of Pino in Athens was enthusiastically welcomed by a large delegation of Argentineans who were present at the gala dinner. The first president from Latin America gave an impressive introductory speech.
The new board of directors set off in the new headquarters in Oak Brook making use of new electronic means of communication, such as all correspondence and minutes of meetings sent by e-mail. The Newsletter sent by e-mail but on popular demand, as the new executive director called it, this was turned around in 2005.
Alexis Olsson, the new editor of the Newsletter met the target of distributing at least two Newsletters It also contained relevant information including a yearly report in 2003, which was very informative for the membership. An executive director that was physically present at the office and who could guide the growing staff really made the difference. Meetings of the Board
and Executive Committee were much better prepared and initiatives to further improve the governance were plentiful. There was also time for some highly necessary updates on documents that were often consulted, such as a policy on co-sponsoring meetings and above all the guidelines for organizing an ICOMS. The latter needed constant updates because of the expanding IAOMS activities that had to take place during these conferences and also because of the increasing financial implications. The times were long gone that an ICOMS was just a meeting of a few hundred colleagues.
Another important activity was the questionnaire that was sent to all national associations to assess the profile of the specialty of Oral and Maxillofacial Surgery. The results of this survey were quite revealing in that there appeared to be a large emphasis on dentoalveolar surgery but a growing expansion into the full scope of the specialty. Unfortunately, the response was somewhat disappointing, which made the outcome less representative.
The work of the new treasurer, Don Booth, in this period was impressive. Don clearly had a feel for investments because the assets of the association grew at an incredible rate, freeing money for some upcoming events that would benefit the leadership of all national associations but also was put to use for some projects that were included in the strategic plan. It was quite reassuring for the Executive Committee to realize that the finances were in good order, firmly in the hands of a very capable person.
Pino, in the meantime, represented the IAOMS all over the world. The growing number of affiliated nations and members coupled with an increasing interest in international cooperation caused him to visit Asian countries in particular, aside from the usual regional conferences and meetings in Latin America. The most rewarding of all was his visit to Nairobi in Kenya, where he represented the IAOMS at the founding meeting of the African Association of Oral and Maxillofacial Surgery (AfOMFS). The African colleagues, from then on, took their well-deserved seat in the Executive Committee, which would contribute to better communication with this continent.
Although there are still many problems within this large continent, with many countries of different cultural backgrounds, a modest start had been made. The IAOMS literally sponsored this historical event.
The Education Committee under the chairmanship of Nabil Samman was very busy indeed with the increasing requests for educational programs, in particular from Asian and Latin American countries. He managed to mobilize enough teachers to cope with this demand.
The IAOMS had also established a Research Committee to encourage and facilitate research activities within the IAOMS by serving as a forum that brings senior researchers and surgeons together to develop an environment to initiate basic, translational and clinical investigations. The committee was co-chaired by Stephen Feinberg and Henning Schliephake.


2005: The 17th ICOMS, Vienna

The organization of the XVIIth ICOMS in Vienna was in the hands of Rolf Ewers and his very capable staff. He, unfortunately, received little backing from the Austrian association, despite the original bid from this association but without any hesitation, took the risk himself to organize this congress in the superb setting of Vienna. He was not disappointed as a record number of delegates (1,400) came to the meeting. Apart from the excellent scientific program, the social program was superb, blessed by magnificent weather. The whole conference took place in the “Hofburg Palace,” the original residence of the Habsburgs and was dedicated to Rudi Fries, a well-deserved honor and unique in the history so far of the IAOMS. The opening ceremony in the well-known “Redoutensaal” was a very special event, enlightened by music from Richard Strauss. It would be hard to find a better experience, sitting in that room of splendor, listening to his music.
The invitational conference for this ICOMS focused on “Using Technology to Advance the Specialty.” The topic was very appropriate in the quickly changing times where modern technology tends to bring about a revolution in communication. Not surprisingly, the event drew a large attendance from all over the world.
A novelty of this ICOMS was the first research symposium, which was organized by Stephen Feinberg and Henning Schliephake. More than 30 colleagues from all around the globe expressed their interest in actively participating in research interest groups.
Another highlight of the conference was certainly the presidential lecture by Michael Cohen Jr. on the topic: “Some disorders of bone.”
The Foundation enjoyed a very successful luncheon with its speaker, Christoph Wagner-Trenkwitz, who spoke on “Music in Vienna; Quotation of Mozart: the best place in the world for my profession.” There was not one attendee who doubted that statement!
The whole conference will always be remembered by those who attended as one of the best ever organized, particularly under the charming but also very capable leadership of Gabriele Millesi, who was in charge of the daily affairs with her committee.
At the gala dinner, Wilfred Schilli received the award of Distinguished Fellow. At last, a well-deserved recognition for his pioneering work and far-reaching vision. At the end of the meeting the presidential chain was handed over to John Williams.
Futures Summit I
In his inaugural speech, John mentioned two important strengths of our specialty; “We are big enough to be taken notice of and small enough to be able to launch pilot programs, should that be deemed necessary.” How true this prophecy would turn out to be. He also described several obvious problems that seemed to have been ignored, particularly by those in government responsible for any sort of healthcare manpower planning and not just in the OMFS specialty.
On this basis, the new president welcomed OMFS leaders from around the world to attend a conference in Chicago in April 2006 to address issues of this nature the “Futures Summit I.” John told his audience that he trusted that those in attendance would bring some very serious thoughts regarding the need to involve the younger generation in decisions that would affect their future. It was the success of the Vienna conference that made it possible for the Board to even contemplate such a major event as the Summit for a non-ICOMS year.
The Summit was also seen as a natural follow-up to the strategic plan of 2004, a “re-thinking” of how the association could move forwards in order to satisfy the
needs of the emerging generations of X, Y and beyond. The Summit convened with an essential element, a group of some 90 IAOMS members who were as representative as possible of the future leadership of all six regions. A “futurist,” Ed Barlow, served as the event’s coordinator, assisted by Breda Bover, a psychologist and professor in adult learning. Between them, they facilitated the two-day conference that was subtitled, “Aligning the IAOMS with Continuous Change.”
The whole meeting will be remembered by the many participants, who came from all corners of the world, as an eye-opening experience. As a result of this meeting, it became obvious that the association and the specialty itself needed a very different approach in order to reach future participants, the emerging generations.
The principal outcome of this first meeting was to establish a task force, which was charged with exploring emerging trends and issues which affect the OMFS profession and making particular recommendations to ensure the provision of an adequate workforce for the future needs of the global population. (see sidebar below)
Another issue which emerged from the Summit was the need to develop a new website for the facilitation of better communication and educational opportunities. From the proposals submitted, after extensive discussion and planning meetings on the part of the Board and Executive Committee, an Indian company, EDC, was chosen on the basis of its very competitive bid. Several months later, the resulting redesigned website was launched during the 19th ICOMS in Bangalore.
The key message, however, that came out of the “futures” event was the association’s need to increase its flexibility in governance in order to embrace the upcoming generations of leaders and members. For instance, while the association’s finances had gradually been brought into a structured format by recent treasurers, which enabled developments like the Summit and new website to be afforded, additional financial problems were developing. During the period from 2003 to 2007, the association’s administrative expenses had risen by 65 percent. While it was clearly time to check this trend in order to grow and expand its capabilities, association leadership voted in a six percent increase in membership dues over the next five years.
The IAOMS Foundation also sought additional means of generating funds during this period due to the commitments the IAOMS had made for educational programs in developing countries, the most significant of which was an educational program in East Africa where there was extensive political change. In this region, a governmental model reflecting almost exactly what had transpired in the European Region had been formed where nine countries had established an economic community with the declaration that there was to be freedom of movement, freedom to reside in any of the countries and to work there.
The IAOMS educational program in East Africa began in September 2006 with some 20 attendees. John Williams, accompanied by Paul Stoelinga, who had done all the initial work, and Julio Acero, attended the launch
first task force formed to study future specialty
At the Futures Summit I, a “Task Force” on the future of the profession of oral and maxillofacial surgery was established with Gabriele Millesi serving as the chair. The task force’s work focused on six issues covering all the main struggles of the profession and of IAOMS members, from young to old:
• Collaboration with and integration of professions related to emerging science and technology (multidisciplinary).
• E xtending the productive work life of the retirement-eligible members of the profession.
• Establishing the profession as a great place to work (image and awareness building).
• Earn and learn approach to education/training and development of future members of the profession.
• Alternative approaches to work environment and work process (project work, etc.).
• Maintaining knowledge and competency among the practicing professionals.
The task force’s first step was to design two questionnaires, one for members of IAOMS and one for trainees only. Both were designed to give the task force and the association a tremendous amount of potentially important feedback. Results of the surveys were disseminated at the Bangalore ICOMS in November, 2007.
of this program in Nairobi where the letter of agreement was signed by all involved, including the vice chancellor of the University. A similar document was later signed in Dar es Salaam, Tanzania, where half the courses would be held.
Another milestone for the association’s finances, which would have far-reaching effects in the organization’s future, came in the form of a proposal from 18th ICOMS chair, Kishore Nayak. This fundamental proposal concerned the reimbursement by the national OMFS association host to the IAOMS for the work done on behalf of each ICOMS on the development of congresses, which entailed 10 percent of registration revenue and 20 percent of exhibition revenue being returned to the IAOMS to compensate them for the work done centrally.

2007: The 18th ICOMS, Bangalore
The Bangalore conference was an enormous success with another record attendance of 1,780 delegates, including 590 trainees and 148 accompanying persons attending a colorful social scene in magnificent surroundings. A generous donation of two recent textbooks “Oral & Maxillofacial Pathology” by Marx and Stern and “Essentials of Orthognathic Surgery” by Reyneke, allowed every delegate to receive their own copies. Trainees had a separate symposium on trauma, followed by a huge
A reintroduction, to the delight of many, was a golf tournament in aid of Foundation funds and the Foundation Luncheon was also totally sold out. This was the second ICOMS with a larger than expected turnout, so much so that improvised lecture rooms had to be erected to create
installed as President. He introduced a different emphasis on work to be addressed with the introduction of Special Interest Groups (SIGs). He nominated two starter topics — cleft/facial deformities and head and neck cancer/ reconstruction — and appointed two small committees, led by Tim Turvey and Moni Kuriakose, respectively, to advance the projects. Each group was to draw up draft SIG guidelines together with a governance structure. Although the groups were self-financed, scholarships were sought from industry to enable selected candidates access to Fellowship programs linked between different centers around the world.


Two important changes were also made to the governance structure of the association. In order to address the issue of appropriate timings for conferences in different regions of the world, it was decided that the presidency

outcome audit of task force surveys
The priorities demonstrated in answers to the questions differ between the six regions. The general conclusions drawn, however, may be summarized as follows:
1 A need to have core surgical skills which should include:
• Dentoalveolar surgery;
• Management of clinical pathology, including infections; and
• Trauma, as an integral part of a trauma team and aspects of implantology related to the need for pre-implant surgery or reconstructive surgery following ablation.
2 Education and training must be appropriate to the desired clinical practice and tailored to save time. Double qualification should not be seen as a threat.
3 Ability to deal with emerging technologies:
• T issue engineering and regenerative medicine;
• Nanotechnology;
• Improved 3-D imaging; and
• Intra-uterine surgery.
4 Both members and trainees considered that the image of the specialty should be improved amongst the general public.
5 The general recommendation was that each national or regional association should analyze their individual situation and deal with it.
January 1st of the appropriate year. Secondly, the issue of reimbursement to the association regarding ICOMS income, as proposed by Kishore Nayak, was formally adopted.
Nabil carried on with efforts to promote educational programs in various Asian countries. He travelled extensively, not only in Asia but also in the other continents as a means of increasing the visibility of the IAOMS. He put steps in place to develop an electronic platform that would augment the educational value of IAOMS’ programs, which would enhance the reach of the association’s educational programs. He also aimed to facilitate advanced training in the areas traditionally regarded as subspecialties, namely cleft lip and palate/craniofacial deformities and head and neck cancer. Under the SIGs concept, advanced training fellowships were planned throughout the world.
At this time, membership numbers showed an increase from 1,000 in 1963 to almost 5,000 in 2008. A further reflection of the growth in membership resulted in the appointment of a membership associate at IAOMS headquarters. Additionally, the increasing workload for the IJOMS editor-in-chief prompted Piet Haers to propose a structure with three assistant editors to improve the workings of the Journal. He would remain as editor-inchief, responsible for overseeing each edition and also for the overall policy of the Journal
A second “Futures Summit” followed in 2008 where the results of the workforce survey were examined, together with the progress made in the preceding two years plus the survey results communicated at the invitational conference in Bangalore.

2009: The 19th ICOMS, Shanghai
The Conference in Shanghai was another huge success with a massive attendance of 1,503 delegates from 76 countries. It is of particular interest to note that the meeting was organized by the Chinese and Hong Kong associations together. Their excellent cooperation had resulted in a superb and well organized meeting. Not surprisingly, the majority of the attendees came from Asia, with the Chinese being the largest contingent.
The Foundation Luncheon was again completely sold out with a lecture and practical demonstration on Tai Chi that had all participants actively involved! An innovation was the Past-Presidents Luncheon, held on the top floor of the Trade Centre with commanding views over the whole of Shanghai that was attended by 11 past presidents and their wives as well as the president-elect.
The prestigious Presidential Lecture at this event was presented by Ghali E. Ghali, who talked about the evolution, current status and future of maxillofacial surgery.
In the run up to the congress, the association and the foundation had been very busy in Dar es Salaam where, thanks to a generous donation, two operating theatres and their associated facilities had been built and equipped. The new facilities would enable trainees, in particular, to gain additional surgical experience.
January 2010 was the first occasion when the presidency changed hands with the New Year. The Board marked the occasion with a meeting in Hong Kong that was attended by members of the Shanghai organizing committee as a small “thank you” celebration. Larry
Nissen was now in the driver’s seat and was immediately faced with challenges over the organization of the next congress in Santiago. This led to the Board appointing a permanent conference organizer to assist with future ICOMS. Additionally, the increasing use of IT in all aspects of the specialty led the Board to establish an IT Advisory Committee, not for the first time!
For some time, the issue of the IAOMS acting as an accrediting body had been sought by many national OMS associations. This need was becoming greater, predominantly in countries where no such mechanism was available. In 2010, the Board established a group to look into the practicalities of performing this function when it was requested.

The occurrence of a series of natural disasters around the world raised the question in 2010 of what IAOMS could do to provide oral and maxillofacial surgical assistance when needed. Don Booth, past treasurer and North American representative, was asked to investigate an IAOMS disaster relief team. As a result of his efforts, the IAOMS Humanitarian Aid and Disaster Relief (HADR) Committee was formed to look in to this and make recommendations. Its first action was a credentialing course that was held immediately prior to the Santiago ICOMS.
Members began to easily and quickly stay on top of news related to the specialty when the association began offering the IAOMS Weekly e-News Bulletin in 2010. These brief missives provided short encapsulations of pertinent news items from around the world and quickly became a member favorite.
In an effort to attract the future leadership of the IAOMS, during the fall of 2010, Council voted for free membership for all OMFS trainees with options for either printed or electronic IJOMS subscriptions for a nominal fee. As a result, by the summer of 2011, IAOMS trainee members had ballooned from 2010’s count of 110 to nearly 600!
In 2011, IAOMS leadership continued with its quest to attract and keep trainee members through several new ventures including the formation of a separate trainees association, the International Association of Oral and Maxillofacial Surgeon Trainees (IAOMST), which was rolled out during the 20th ICOMS in Santiago.



E-learning opportunities that began in 2009 with the web-lecture series “ProjecTrain” (initiated and managed by OMS trainee Satheesh Prabu) expanded in 2011 and will continue into 2012 with regular online clinic-pathology conferences and live online debates between specialty leaders on current controversies. A member from Vanderbilt University in the U.S.A., Steven Press, (with collaboration from his colleagues in North Carolina) provided the next steps in unique trainee and
member benefits with two programs. The first program was a histopathological series for viewing on any Internet connection in the world. The series included a written didactic component and copies of digitally scanned histopathology slides that would allow viewers, essentially, to turn their computers into microscopes using free software to view the slides and take snapshots.
Steven Press second shared project focuses on trauma and reconstructive surgery and involves the sharing of medical modeling technology with members worldwide.
Finally, OMFS trainees worldwide were treated to a long-time AAOMS trainee benefit, an online manual of familiar OMFS terminologies, medications and procedures. Done in cooperation with AAOMS, under IT committee chair Alexis Olsson’s supervision, the manual was revealed to trainee members at the Santiago ICOMS and rolled out to all trainee members by the end of 2011.
The research committee continued its outreach to the six regions of IAOMS by offering research symposia at national and regional OMS conferences. The committee also received co-sponsorship from the IAOMS for the Research Summits hosted by AAOMS in 2009 and 2011.

2011: The 20th ICOMS, Santiago
The enormous growth of the number of attendees to the ICOMS that had begun in Vienna in 2003 reached its height in Santiago. For the first time in the history of IAOMS, more than 2,000 participants were registered, including accompanying persons. There was a massive merica; in particular, Brazil and Chile but Asia, Europe and U.S.A. were also
The Invitational Conference was about technology, information and the future of IAOMS. There were many speakers addressing the advantages of the new technology to communicate, with particular emphasis on its use for education. This technology opens new avenues, particularly for the lessdeveloped world in that interactive teaching via the web becomes available for them. E-learning in general will take off and will probably replace conventional teaching to a large extent. Later in the conference, a special symposium was held on: “Training of Oral and Maxillofacial Surgeons: Leveraging Technology.” The faculty represented each of the six regions.
At the opening ceremony, Luis Quevedo announced that the 20th ICOMS was dedicated to Bob Walker. He had passed away unexpectedly in July, 2011. In attendance were Bob’s wife Emily and his three children. The dedication received a standing ovation from the audience.

A special feature of the conference was the reformation of the International Association of Oral and Maxillofacial Surgeons in Training (IAOMST), an effort spearheaded by Bob Woodwards (U.K.) and Piet Haers (U.K.) who were both active in the original IAMFST which had been founded in 1989. More than 100 enthusiastic trainees attended the formation meeting, where plans were made to begin by forming six regional groups to explore its potential.
The scientific content was superb, with four major symposia on topics such as: Facial reconstruction, complications in orthognathic surgery, new developments in research, and the role of implants in OMF reconstructive surgery. In addition, another 16 symposia and more than 40 free paper sessions completed the program.
Jay Malmquist (U.S.A.) gave the Presidential Lecture: “Education, Research, Technology, and Innovation: The Foundation of an Exceptional Specialty.”
The chain is a fairly heavy and expensive ornament since it is made of pure gold, with a medallion of the IAOMS logo set in the center. Most presidents would pack it in their carry-on luggage when boarding planes for formal visits to national or regional meetings, so as to make sure it did not get lost at some airport. This meant that the chain’s heavy metal would set off the alarm at security check-ins, which often caused quite an upheaval before boarding. Presidents frequently had to explain why they were carrying such a valuable chain and what it represented.
As security people are probably not selected because of their scholarly performances, an explanation, such as being the president of the International Association of Oral and Maxillofacial Surgeons, was generally not well understood. This often lead to some embarrassing moments where a senior security officer had to be consulted, while a long line of impatient passengers were staring at you.
I learned quickly to carry the chain in the velvet bag that I inherited from my predecessor, John Helfrick and put it in my pocket. This avoided hand searching my carry-on luggage and having to have a long discussion with the person checking me. This bag, by the way, used to envelop a fancy whisky bottle and the rumor goes that Peter Banks had introduced this means of carrying the chain.
Once approaching security, I would put it in front of them and tell them I was representing an international group of surgeons. This would reduce the time wasted considerably but still the chain could cause a lot of excitement at various borders in all continents. At one of these borders, the person who checked me suggested it was a chain worn by a mayor of a big city. Half sleepingly, I nodded yes, and much to my surprise, I was waved through. This appeared to be luminous thought and I have since boarded planes many times as the mayor of the very little town where I live. No questions asked anymore!
Paul J.W. StoelingaLuis and his committees had done a wonderful job and added the much-appreciated local touch, exemplified by a beautiful opening ceremony, featuring dance and music of Chile and a Chilean Evening. They can be rightly proud of their achievement, because Latin America has made a distinct footprint in the IAOMS.
Leadership positions at IAOMS went through significant changes, starting with the resignation of Piet Haers editor-in-chief and the appointment of his replacement, Nabil Samman. After many years of service, John Helfrick stepped down as executive director. He received a well-deserved Distinguished Fellowship at the Gala Dinner.
Nabil Samman was presented with a “Distinguished Service” award for his many years of service to IAOMS. Don Booth received an “Outstanding Committee Member” award for his pioneering work on the newest IAOMS committee, the Humanitarian A ssistance and Disaster Relief Committee.
At the meeting, the new Executive Director, Barbara Morrison, was introduced. She will be present full-time in the IAOMS office and brings with her the management skills appropriate for the fast growing association.

Of course, a new president, Kishore Nayak, took over at the end of the 2011 calendar year with Piet Haers as the presidentelect. The beginning of 2012 also saw the launch of the redesigned website, which had been upgraded to better suit the technologies that had developed since the last site upgrade in 2007.

In addition, two new committees were established, notably the IT Technology Committee, chaired by Alexis Olsson and the Humanitarian Assistance and Disaster Relief Committee, chaired by Don Booth.
The affiliation of three national associations was approved: Seychelles, Bulgaria and Serbia. This brought the total number of affiliated national associations to 78.
Epilogue
When reflecting on the history of the IAOMS, as described in chapters 2, 3 and 4, there are several facts that catch the eye.
• First, the enormous expansion of the membership, from a mere 500 in 1962 to approximately 6,000 in 2012. This growing membership went along with a steady increase of affiliated national associations from the original seven to 78 (see addendum). This definitely reflects the growing understanding that the interests of the specialty are best served by a worldwide representation of oral and maxillofacial surgery.

• Second, considering the tremendous growth in numbers of attendees at the international conferences and particularly those from A sia, it becomes clear that the specialty has spread worldwide and will probably continue to do so. It seems to go along with a global trend in which Asia is becoming a major player, although, to a lesser extent, this also applies to Latin America and Africa.
• T hird, the positive effect that the concept of regionalization has had on the organization of the regional associations, notably Asia, Latin America and Africa. They all have restructured their loose organizations into firm regional associations with a structure compatible with that of the IAOMS.
• Fourth, the overriding impression one gets, when reading the decisions of the various Executive Committees, that a lot of these decisions were never implemented. It seems that some of them simply disappeared and were hidden in the drawers of filing cabinets, only to turn up again after several years and be debated as if no previous discussions had ever taken place.
• Fifth, the missed opportunity to create a truly harmonized professional specialty with a vertical structure of international organization, as was suggested by participants at the Tenerife and Bermuda conferences. This recommendation was simply ignored, probably because people were distracted by the enormous efforts that were necessary to get the education and training document accepted.
• Sixth, there is no doubt that the success of the Journal, with its prime position, has contributed to the growing interest in joining IAOMS.
• Seventh, the activities of the Foundation that has made educational programs possible in various parts of the world. This has contributed substantially to the popularity of IAOMS and could be considered an example of effective assistance to the developing world.
References
Ferreria J., Personal communication
Helfrick J., Personal communication
Samman N., Personal communication
Stoelinga P., Personal communication
Williams J., Personal communication
International Guidelines for specialty training in Oral and Maxillofacial Surgery. Final version as adapted in Durban, 2001.
Minutes of the Board meetings of the period 1999–2011
Minutes of the Executive Committee meetings of the period 1999–2011
Minutes of Council meetings of the period 1999–2011.
Newsletters, 1999–2011. Alexis Olsson and Kerry Spaedy.
The Foundation
The IAOMS Foundation was established in September 1996 with the first meeting of the board of trustees held on September 18th in Miami Beach, Florida. This final step was preceded by many discussions within the IAOMS Executive Committee. It was generally felt desirable to establish such a Foundation to support the educational activities initiated by IAOMS.
The Executive Committee decided to appoint an independent board of trustees, very much along the lines of the AAOMS board of trustees for their Foundation. There was some opposition to this model, notably from Rudi Fries, who favored a model in which officers of the Executive Committee would form the board of trustees, so as to be assured that the plans of IAOMS would not find opposition from an independent board. However, this proposal was rejected and the first board of trustees was formed, consisting of Bob Cook, Andrew Linz, Bob Walker and Dieter Pape, together with an independent lawyer from New York, Arthur Brill. This board formulated its own constitution and bylaws and chose Bob Cook to serve as its chairman. Andrew Linz was chosen as treasurer and Arthur Brill, vice chairman.
Financial challenges
To begin its operations, the Foundation received a loan from the IAOMS of $250,000. The intention was to tap other sources of money for a corpus of money from which the interest only would be used to support the educational activities. The first attempts at fundraising were very successful with several affiliated national associations providing generous donations and the donations of individual members surpassing all expectations. In a matter of just two years, almost $150,000 was received.
With the move to the first permanent office, however, the Foundation was expected to finance about 20 percent of the costs of the administrative services provided by the new office. This bled the Foundation coffers as the projected interest income of $20,000 on $400,000 in investments, was hardly enough to cover the 20 percent charge.
In 2000, Bob Cook wrote a rather bleak report on the future of the Foundation, noticing that the expenses needed to run the Foundation were significantly exceeding the Foundation’s income. While various suggestions were made for increasing the income, including approaching industry, it was felt that a tangible project needed to be defined before this could be done. By this time, Dieter Pape had retired and had been replaced by Marsden Bell, while Vic Moncarz had been added to the board as executive director.
The first Foundation Luncheon was held at the 14th ICOMS in Washington to raise funds for a “Foundation Fellowship.” This luncheon honored the founders of IAOMS, Fred Henny and Terence Ward. Bruce MacIntosh and Peter Banks, disciples of these great characters, presented details of the respective contributions of these former presidents.
Not too much happened in the years between 1999 and 2001, apart from incidental sponsoring of trainees from developing countries to attend the ICOMS in Durban, where a special trainee workshop was held. The sheer fact that the board of trustees met only once during this period illustrates the operational difficulties that were beginning to show.
Meetings for the board were expensive events and, thus, continually postponed to save money. As a result, decisions were not made, nor was there progress in sponsoring any
A check in the amount of $250,000 was presented by President Rudi Fries to Bob Cook, the Foundation chairman accompanied by John Helfrick, secretary general.

educational activities. At the 2001 ICOMS, Marsden Bell took over as chairman of the Foundation, while Peter Banks was added to the board to replace the deceased Andrew Linz.

The novelty of the Foundation Luncheon that Bob Cook introduced for the Washington meeting was altered to feature an invited speaker from the organizing country as an ongoing fundraising event. The luncheon was a huge success in Durban, due in large part to the impressive presentation of Professor Philip Tobias of Johannesburg, a paleoanthropologist who talked about the hominid fossils of Africa, with special emphasis on their facial and dental features. The luncheon was sponsored by a generous donation from Walter Lorenz Surgical, which would also sponsor several successive Foundation Luncheons. The purpose of raising a substantial amount of money was easily achieved.
Together with John Helfrick, Marsden Bell wrote an ambitious working paper on how the board should be structured to involve all areas of the world. The paper stressed the necessity of adopting the concept of “Regionalization,” as the IAOMS Executive Committee had already done for the association itself. Marsden also developed an attractive brochure to promote donations to the Foundation. Most importantly, however, an educational program in Thailand became the first tangible project, with intentions for the program to serve as a pilot for further activities.
This foray into producing educational programs appeared not only to be beneficial for all attendees, it was also fruitful money-wise for the Foundation as several companies sponsored part of the educational modules,
while many teachers donated their time and often also their air ticket expenses. This three-year educational project, with 10 modules each of one week covering essentially the whole scope of oral and maxillofacial surgery, was a huge success.
Participants came not only from Thailand; they also attended from neighboring countries such as Indonesia, Malaysia, Cambodia, the Philippines, Singapore and a few others. Between 100 and 120 very enthusiastic trainees, together with established colleagues, followed the whole course. Participants who attended 80 percent of all of the modules were eligible to take an exit test. The project set an example for the many courses to be held in the coming years in various parts of the world.
Structural changes
Within the Executive Committee of IAOMS, however, opposition was growing regarding the way the Foundation was managed. The IAOMS administration fee was particularly thought to be unreasonable and the disconnection between IAOMS Executive Committee and board of trustees additionally appeared to be a distinct disadvantage.
In February 2001, the Executive Committee accepted a motion to eventually regain control over the Foundation and to reorganize its management. It was also felt to be desirable to put the $250,000 loan back into the accounts of the IAOMS and the formulation of a business plan was recommended. Despite Marsden’s hard work and many attempts to organize money for the planned projects, little money had come through.
In the meantime, the assets of the Foundation were dwindling and the board of trustees was essentially paralyzed, as no meetings were being held in order to save travel expenses. For these reasons, it was decided in 2004 to change the structure whereby the Foundation would be run by the officers of the Executive Committee with the past-president normally serving as the chairman of the board of trustees. The main advantage of this change was the Foundation board from now on would meet in conjunction with the board of IAOMS, while the treasurer of IAOMS also would oversee the Foundation’s finances. This turned out to be a cost-saving maneuver and there was a direct link to the educational activities of IAOMS, which facilitated action. This is the situation as it currently exists. After all these years, Rudi Fries appeared to have been right when he opposed the original form of the Foundation’s establishment.
It is only fair to mention the very successful Foundation Luncheon held at the 15th ICOMS in Athens in 2003. The guest speaker was professor Stefanos Geroulanos, a professor of surgery and ancient medical history, who gave

a dramatic presentation on ancient medical practice in Greece. Again, this sponsored event raised a fair amount of money as it was completely sold out.
Paul Stoelinga took over as chairman of the Foundation in the spring of 2005 and would stay on until the 17th ICOMS in Bangalore in 2007. The assets of the Foundation needed a boost and an appeal was made again to the various national associations to consider yearly donations, whereas the Executive Committee also was asked to donate generously, thereby setting an example for the membership at large, which indeed was followed by many IAOMS fellows.
The IAOMS received its loan back but decided to donate $15,000 on an annual basis to the Foundation. Another move was the appeal to industry to apply for

Attendees of the final module of the Lima, Peru education program in 2006.

corporate membership. The first company to join was KLS-Martin/S.O.R.G., later followed by W. Lorenz Surgical. Their status would be changed into “Patrons” of the Foundation in 2007. Based on a reliable source of income, a proper budget could be prepared and the expenses could be matched against the planned income, without having to dig into the corpus of money. The bleeding had stopped!
Educational projects
As the years went by, several new projects emerged modeled on the Thai program. In his term as president, José Ferreria initiated a program in Peru, in conjunction with ALACIBU, and partially sponsored by the AAOMS Foundation, with voluntary support from mainly Spanish speakers. As with the Thai project, this again was highly successful and much appreciated by the participants.
At the initiation of John Williams during his presidency of the European association, EACMFS was instrumental in establishing a similar course in Iasi, Romania, which was subsequently led by John Lowry, the
Lima, Peru educational project.
From left to right: Carlos Abugattas, ASPECOM president, Mario Dominguez (Uruguay) lecturer; Horacio Sanchez (Uruguay) lecturer; Luis Quevedo (Chile) program coordinator and IAOMS education committee ALACIBU representative; José Luis Ferreria (Argentina) IAOMS president; Eduardo Rey (Argentina) ALACIBU president; Juan Enrique Bazan, Dean of Colegio Odontologico del Peru; Mario Hernandez, Dean of Universidad Inca Garcilazo de la Vega; Alejandro Cornejo, IAOMS councilor for Peru, Arturo Rodriguez, ASPECIME president.

EACMFS secretary general at that time. The EACMFS, however, took on the financial responsibility for these courses. Programs in Indonesia and Africa were then developed, both of which would apply for financial support from the IAOMS Foundation.
At the 16th ICOMS in Vienna in 2005, the guest speaker at the Foundation Luncheon was Christoph Wagner-Trenkwitz, assistant director of the “Vienna Volksoper,” who spoke on “Music in Vienna.” This again was a marvelous presentation on a topic perfectly fitting for “the Capital of Music.” Rolf Evers can be rightly proud of his choice of this speaker.
African service
Between the years 2003 and 2009, the attention of the IAOMS turned to Africa as one of the target areas for assistance. Under the presidency of Pino Ferreria, the African Regional Association was established. After that, the next step in assistance to this country was an appeal to the IAOMS membership for used analogue x-ray equipment, including Orthopantomogram machines and other equipment. The appeal was reasonably successful as several machines were shipped to both west and east African locations. The donations also included anesthetic equipment, dental chairs and generous gifts of surgical instruments. Generous though these gifts were, they were but a drop in the ocean as far as need was concerned.
As Africa is effectively a vast region where one type of assistance that is appropriate for one area may not be appropriate for another, the board of IAOMS decided that if it was going to have any effect at all, it needed to work with smaller areas of Africa. Nine countries, which were already united by their governments into a common East African Economic Community as well as an East




gave the Foundation scope within which to work.
John Williams, the president at that time and subsequently, the Foundation chairman made several trips to Nairobi and Dar es Salaam to help in the establishment of an East African training program that could serve for the whole East African region with centers in Nairobi and Dar es Salaam. The establishment of an East African Association of Oral and Maxillofacial Surgery facilitated this endeavor.
The starting point was the adoption of the “IAOMS Guidelines for Specialty Training and Education” as the basis for a common curriculum. Once achieved, the universities were encouraged to modify both the duration and content of their Masters’ courses towards a common pathway. This proved to be a major breakthrough as, in due course, the community governments decreed that there should be “Freedom of Movement and Freedom to Work” for all people in the East African Community.
This demanded harmonization of training for all medical specialties and it was decided that this should be set for all at five years duration. To help with this process, an educational program was developed, similar to the Thai and Peru programs but adapted to the needs of East Africa. A major plan also was launched to support the OMFS department in Dar es Salaam which was desperately in need of improvement both of equipment and other facilities. The plan was to enhance the conditions there in order to accommodate the much wanted expansion of manpower in the area, as well as complementing a planned expansion by the University of Nairobi.


The Foundation was fortunate in securing a valuable donation from the Nina Harris Pebley Charity with which to build two operating facilities, including an immediate
recovery area and two changing rooms. Donations from individuals secured sufficient funds for the equipment to make these facilities functional.
The first module of the East African educational project, with Mark Chindia as the host and supported by Fawzia Butt, was an eye-opening experience for both the attendees from various East African countries and for the teachers from Europe. The original intent was to hold the course in Dar es Salaam and Nairobi on a rotational basis, but because of political unrest in Kenya, the courses for the most part were held mainly in Dar es Salaam under supervision of Elison Simon, the department chairman. IAOMS had surely made an impact in this part of the world, where the need for basic oral and maxillofacial surgery in very high indeed.
Julio Acero, the Education Committee chair for the period 2005–2012, was largely responsible for the detailed content and organization of speakers for the East African region. This was a huge task, as it often was difficult to find the right people who were available to teach at the right time. During this period, Nabil Samman, the former Education Committee chair, continued the Foundation’s Asian project
with a few advanced courses that were held at a lower frequency, while he also initiated plans to begin a similar course in Indonesia, which came into effect in April 2007.
Needless to say that all the above mentioned activities were costly and required heavy support from the Foundation. Fortunately, assistance was given notably from the AAOMS for the Peruvian project and also by generous support from the Spanish association, which sponsored the travel expenses of the many Spanish teachers. Yet, while the Foundation reached its financial limits, it did not draw down any of its assets in this period.
It is fair to say that the Foundation at this stage had outgrown its teething problems and was ready to face the challenges that lay ahead. The IAOMS had engaged itself in educational projects in all corners of the globe, which would require ever more resources in order for the association to live up to worldwide expectations.
training. The East African College of Surgeons now entered the scene again and declared their intent on taking a lead with accreditation. In so doing, they demanded that the two-year period be a structured time, at the end of which the College would be responsible for undertaking an appraisal of the surgeons before they were appointed to outside hospital appointments anywhere within the Economic Community.
Additionally, work focused on the West African part of the African region, where an initial survey had been conducted in an attempt to ascertain the area’s needs and shortcomings. The fact emerged that, whereas five of the countries are Anglophone, there also are Francophone-, Spanish- and Portuguese-speaking countries and the specialty in these countries had been founded on totally different backgrounds. This meant that the IAOMS could not devise and support any one single aid project.
The Foundation luncheon at the 17th ICOMS in Bangalore in November 2007 was again a fascinating event. Thimappa Hedge, a neurosurgeon, talked about ancient Indian medicine. This luncheon was sold out, as usual, and sponsored by Biomet Microfixation, formerly known as W.Lorenz Surgical. A novelty was the golf tournament which had not been run for many years. This was great fun and also provided money for the Foundation. There was an overwhelming interest in the event, which was sponsored by ABN-AMRO Bank and Franklin Templeton. It was definitely an example which, it is hoped, will be followed for future ICOMS.
At this meeting, the chairmanship of the Foundation was handed over to John Williams. Much of his time as chairman was occupied by the many aspects of the East African project, which have already been described. It was inevitable that support for East Africa would be needed for many years to come.
A large stride was made in linking together the basic training period leading up to the acquisition of the Master’s degree and the final accreditation of these doctors as fully trained surgeons. Previously, the post Master’s degree period was served in the training center for two years, with essentially unstructured and largely unsupervised
Furthermore, a significant number of countries were in a state of unrest or open warfare. The outcome was that only Ghana and Nigeria were candidates for any sort of collaborative project. This would materialize in the period of 2011–2012.
Scholarships established
Under Nabil Samman as president, attention turned to “Special Interest Groups,” (SIGs) particularly in oral oncology and craniofacial deformities, in particular cleft lip and palate. The SIGs developed two initial scholarship schemes to support trainees. The first of these took place during the academic year of 2010–2011 and supported:
• Two fellowships in oral and maxillofacial oncology and reconstructive surgery. The locations for these fellowships were the Ninth People’s Hospital in Shanghai, China, and the Peking University School and Hospital of Stomatology in Beijing, China. For the academic year of 2011–2012, a third fellowship in oral oncology also was held at Mazumdar-Shaw Cancer Center, Narayana Hrudayalaya Health City in Bangalore, India.
“The objectives of the Foundation are to financially assist IAOMS programs in education and communication to eliminate the many imbalances which exist today.”
•
A single fellowship in cleft lip and palate and craniofacial surgery. The locations for this fellowship was split throughout the academic year between Arnold Palmer Children’s Hospital in Orlando, Florida, U.S.A.; Dr. Hasan Sadikin Hospital in Bandung, Indonesia; and the University of Pretoria in Pretoria, South Africa.

Although the fellowships were originally conceived as self-funding, the Foundation succeeded in gaining financial support from the healthcare industry, specifically Biomet Microfixation and Synthes, for the first two years of the program.
So, within the period described, the rather loose but, nevertheless, entirely laudable concept of a charitable Foundation to support the initiatives of the IAOMS Board, has evolved into a structured and well-financed body which works jointly with the association to demonstrate determination, both to develop concrete projects and to see them through to fruition.
From the successive presidents’ perspectives, IAOMS presidents are able to conceive a scheme for Foundation activities during their time as present-elect, see the plan initiated during their presidential years and then secured in all respects during their terms as past-president and
chairman of the Foundation. Not only does this indicate just how long these projects can take, it also shows the value of the challenges made to the administrative structure of the Foundation at the turn of this century.
At the 20th ICOMS in Santiago, Chile, the speaker at the foundation Luncheon was Francisco Mûnoz Thomson, an oral and maxillofacial surgeon and an experienced mountaineer. He presented an overview of the Chilean landscape and its original inhabitants, followed by a fascinating account of the difficulties encountered when climbing steep and barely accessible mountains. He compared the planning and execution of mountaineering with the same measures required for surgery and life. The philosophy behind it was that the satisfaction does not lie in reaching the summit, but in the collaboration within the team that allows everyone to come back alive — a statement that could be related to the daily lives of everyone in the audience.
International Journal of Oral and Maxillofacial Surgery

As mentioned in chapter 2, the Journal was established in 1972 under the leadership of Jens Pindborg, a renowned oral pathologist from Denmark. In the first years, the publication contained mainly case reports on clinical pathology and some, mainly Scandinavian, clinical followup studies on dentoalveolar surgery. Pindborg held this position until 1976 when Erik Hjørting Hansen took over.


The format of the Journal in those days was smaller and contained far less papers than currently is the case but it certainly served its purpose in giving colleagues from outside the U.S.A. access to a journal that they could feel was theirs. Erik invested an enormous amount of time in making the Journal a success during the 13 years he was in charge. However, he was only partially successful for reasons that were not completely in his power.
First, the Journal of Oral Surgery remained the main vehicle for non-Americans to publish their research because they knew this journal had the widest distribution. Secondly, the Europeans introduced their journal almost at the same time, while the British had also just come out with their national journal in 1962. In other words competition abounded. Another obstacle was the very limited spread Journal because of the limited number of members that actually subscribed to it.
In February 1987, the new executive committee met at Guy’s Hospital, London, under the presidency of Wilfried Schilli. High on the agenda was the need to appoint a new editorin-chief of the International Journal, to replace Erik Hjørting Hansen, who had just completed his contract. The choice seemed difficult, particularly to achieve a balance of language skills, academic expertise, clinical experience and geographic location. One name stood out, Paul Stoelinga, of the Netherlands. The executive committee was unanimous; he should be invited to fill the vacancy. At that time, the executive committee only met once a year and it was considered urgent to finalize an appointment as the association’s arrangements with the publisher were presenting problems and the position of editor was critical to the discussions with Munksgaard in Copenhagen.
The secretary general, David Poswillo, suggested the executive committee telephone the Netherlands and offer Dr. Stoelinga the position immediately. It was Saturday morning and by midday, he had tentatively accepted the position, subject to contractual arrangements. After some discussion, it was mutually agreed that the editor-in-chief should become an ex-officio member of the executive committee and he should have the authority to appoint his own editorial board. Thus began an association between the executive committee and the editor-in-chief of the Journal, an association which persists today.
Paul Stoelinga chaired the editorial board for 12 years, during which time it expanded dramatically in stature and circulation. His direction and guidance were monumental in laying the foundations to place the Journal at the forefront of scientific journals in the field.

At present, one could not imagine that an appointment for such a crucial position would be decided in a matter of one day. It reflects, however, the stage of the IAOMS at that time: it had just left behind its embryonic development and began its path to adulthood.
Strengthening the Journal
The time was ripe for a change and the executive committee at that time, desperate to strengthen the future of the Journal, appointed Paul Stoelinga in 1988 as the new editor-in-chief. They gave him freedom and the means to bring success to the Journal. The first thing Paul oversaw was the change to a more attractive format and the addition of color. In the year preceding the appointment of the new editor-in-chief, the name had already been changed to Journal of Oral and Maxillofacial Surgery.
The most important change, however, was the concept of dividing the Journal into different sections and attracting active clinicians in the midst of their careers to become section editors. The new approach demonstrated its success through the subsequent increase in circulation and number of submitted papers. An important boost to the popularity of the Journal was the implementation in 1990 of a compulsory subscription for IAOMS fellows. In a matter of only a few years, the circulation rose dramatically from 1,000 subscribers to 2,500.
Another factor that contributed to the Journal’s success was the increasing importance of the impact factor, as published by the Institute for Scientific Information (ISI). The ISI, a private enterprise, publishes Journal Citation Reports on a yearly basis. The impact factor is calculated by dividing the number of citations to articles of the two preceding years by the number of published articles in a given year. This impact factor has since become a means for assessing the success of a journal but more importantly a means “to measure one’s scientific contribution.” Universities and other institutions all over the world use this system to assess the output of their scientific workers.

The ISI turned out to be a blessing and a curse for the Journal. In his yearly reports, Paul proudly presented a steady increase in the impact factor from 0.32 in 1987 to 1.18 in 1994. The Journal had achieved the number one position among its competitors and, thus, had gained tremendously in prestige.
The next year, however, when the ISI reported the 1995 results, the impact factor had dropped to almost zero. It appeared the ISI had mistakenly added the citations to our Journal to the account of the International Journal of Oral and Maxillofacial Implants as their system could not differentiate between the two abbreviations that they used for these two journals in the process of counting the citations in the various journals. So much for the reputation and professionalism of that institution that has so much impact on the world of science! They did come up with a very meager excuse but no official rectification. Fortunately, the next year the impact factor bounced back to a reasonable level, which saved its standing and, to a certain extent, its survival as a respectable scientific journal.
Paul Stoelinga stepped down as editor-in-chief at the end of 1999 after 12 years at the helm of the Journal. The circulation had increased to approximately 3,000, which included members and institutional subscribers and the number of published articles per year went up by roughly 30 percent. It truly had become one of the IAOMS’s major assets.

Change in publisher
Piet Haers, already appointed two years previously as assistant editor-in-chief, took over Paul’s role in the year 2000 and initially carried on with the staff of editors that he had inherited. His transition was not exactly made easy for him as during the previous year, the executive committee had decided to change publishers. Despite its 28-year history with the IAOMS, Munksgaard in Copenhagen was not delivering enough benefits for the IAOMS even with the Journal’s significant growth in recent years.
Harcourt Brace was chosen from several other bidders and in 2001, took over as publisher. (Two years later, Harcourt would be taken over by Elsevier.) As a result of this monumental change, Piet had to cope with working with new people at the publishing house, more specifically, with the frequently changing editorial managers for his journal. On top of that, he was in the midst of overseeing the change towards electronic submitting and editing which made his transition to editor-in-chief even more complicated. Only after Elsevier had complete control of the Journal, some three years later and a new manager had been appointed, who turned out to be a blessing, did the turmoil end.

Content expansion
Piet’s main goal was the inclusion of more review and research papers. This objective proved to be very successful as interest in the Journal and its impact factor rose substantially. The amount of submitted papers grew from about 300 to close to 800 by the end of his term, which also caused him gradually to expand his editorial staff and the number of reviewers. The number of sections also had to be increased and with that, the number of section editors who were responsible for the papers in their section.

The Journal went from six sections to 17 and the number of reviewers and editors grew to nearly 200 individuals. This number did not take into account the incidental expertise that also was solicited, which brought the total to about 250 experts. At this point, it is only fair to mention the invaluable help that both Paul and Piet received from all the volunteers who spend so much time making the Journal a success. Some of these editors stayed on board for more than ten years, with particular appreciation going to
John Cawood, who chaired his section for 18 years and Joe Piecuch, who stayed with Piet until the very end for a total of 24 years. Both were instrumental in making the Journal endeavor a huge success.
The enormous growth of the by the increase of the number of printed pages and articles published per issue. This happened gradually, of course, over Piet’s 12-year tenure. While it was still published six times a year, the Journal went from 96 pages per issue to
Jørgen Rud, the president in 1972 when the International Journal of Oral and Maxillofacial Surgery (IJOMS) was launched, wrote a letter from the president as a foreword in the first issue. It is of interest to read this some 40 years later as it provides insight into the state of oral surgery at that time and the perceived need for international communication.
“In the past, the science of oral surgery has to a great extent been practiced within localized areas determined by tradition and language barriers. This segregation must not be upheld if we want to attain the highest degree of progress. It will be necessary to make all qualified scientific material on oral surgery from all over the world easily accessible to the interested. Too often valuable papers are actually wasted because they are published in a national dental journal and either do not reach surgeons in other countries or are written in a language not understood outside that particular country. At present, specialized journals on oral surgery exist in the U.S., England and Germany.”
Here he is slightly wrong because he overlooks the Japanese and French journals, but he is right in emphasizing the parochial view most clinicians must have had, doing their own thing, not being aware of developments outside their own circle. In the following section he also makes an important point! “Although these journals do accept contributions from oral surgeons in other countries, they reflect mainly the tradition in their own countries and their editorial boards are national. The growing interest in oral surgery in other countries will result in increased research and development activity and a need for more space in a specialized journal.”
Although his analysis of the situation was right, he overlooked the efforts of Kurt Thoma, editor-in-chief of Oral Surgery, Oral Pathology and Oral Medicine, who had made it a policy to have an international flavor with consultants from different countries. He continued on to present Jens Pindborg, a renowned oral pathologist, as the editor-in-chief, assisted by oral surgeons and editors from 19 countries.

Looking back one can only admit that the right decision was made at the right time. The journal has indeed achieved the standard that Jørgen Rud foresaw.
Paul J.W. Stoelinga120 pages per issue. It then increased its frequency and size, first to eight issues a year at 96 pages per issue, then to 12 issues per year with 100 pages per issue. The number of published articles also increased at roughly the same rate, going from approximately 90 articles to 210 per year. The acceptance rate, on the other hand, has stayed at a 35 percent rate.
With the introduction of the digital version of the Journal, the exact circulation is difficult to estimate. What is known, however, is the number of copies sent monthly to IAOMS members. At the publication of this book, roughly 4,000 members now receive the Journal. With the launch of the digital version, the number of institutions that subscribed to the analogue version went down considerably and may go down even further as most libraries nowadays limit their journal subscriptions to digital versions, which are often sold to them in packages by the publisher.
Our Journal’s status as a real asset may be illustrated by the increase over the past several years in the number of article downloads. When this service became available in 2005 it recorded 4,000 article downloads per month. In 2010, the number of downloads had grown to 45,000 per month. This spectacular growth truly is the result of the professionalism of the current editorial board. It is, therefore, no wonder that the impact factor has stabilized at around 1.5 which means the Journal is number one among its competitors.
In view of these figures, it should not be surprising to learn that the job of editor-in-chief in the digital age had become a true challenge that could hardly be achieved by a full-time clinician or academician. For this reason, three
associate editors-in-chief had to be appointed to help relieve the editor-in-chief from this enormous burden. If the Journal continues its rapid growth pattern, it may become even more desirable for the association to hire a full-time editor-inchief. The job description of that individual, however, would need thorough consideration as today an all-around clinician is difficult to find, particularly someone with a talent and willingness to be a supervising editor and leader at the same time.
The IAOMS, recognizing the merits of Piet Haers, rightly gave him a distinguished service award at the ICOMS in Bangalore in 2005. Piet stepped down at the end of 2011 after 12 years of service. At the 20th ICOMS in Santiago, Chile, Nabil Samman was appointed editorin-chief of the Journal beginning in 2012.

Epilogue
The enormous evolution of the Journal over the years and particularly its scientific impact is best demonstrated when comparing the different categories of articles in the Journal in the first year, at the beginning of the editorship of Paul Stoelinga (1988), at the beginning of Piet Hears’ editorship (2000) and at nearly the end of his term (2010) as shown in the table on the previous page. This illustrates the growing realization that evidence is the basis for further development. It also shows the growth of the number of papers published, which more than doubled since 2000.
The Affiliated National Associations
This chapter contains the reports of the affiliated national associations, with an emphasis on their histories and origins. They also contain relevant information about the current situation, including membership, organization of training and education and the number of training institutions involved.
All councilors to IAOMS were asked during 2010–2011 to submit their abstracts and 63 of the 75 affiliated associations responded.
The common thread throughout the stories of the formation of national associations is the struggle to gain recognition from within the generality of surgery. The need for special dental skills became apparent and with this, progressive mobilization of interested dental surgeons to take care of these patients with oral and maxillofacial injuries and pathologies. The background of these individuals varied throughout the world. Some came from a single degree either in dentistry or medicine, while others held qualifications in both disciplines. Similarly, the need for further education and training, both to gain acceptance by the medical and dental professions as well as governments and regulatory bodies, was essential for the provision of support for the fledgling organizations. The guidelines on education and training, developed by IAOMS, greatly facilitated the accomplishment of these objectives.
Albania
Albanian Association of Oral and Maxillofacial Surgery
Oral and maxillofacial surgery is a rather young specialty in Albania. At the beginning, maxillofacial work was carried out by ENT surgeons in the 1930s, more precisely by Professor Besim Zyma, who was an obstetrician-gynecologist surgeon trained in Austria and Turkey, as well as an ENT surgeon. During World War II, Professor Zyma and Dr. Xhevdet Asllani covered all maxillofacial work in Tirana Civil Hospital.
In 1959, the University of Tirana opened for the first time and the dental school was created. In 1964, part of the ENT ward (10 beds) was used for maxillofacial patients and Albanian maxillofacial specialists, who were trained abroad, served there. Samedin Gjini and Dhori Pojani, who had their training in Sofia, Bulgaria, as well as Isuf Kasapi
and Ago Shametaj, who were both trained in Bucarest, Romania, all served there.
In 1971, the first maxillofacial postgraduate training course started. In the beginning this was a one-year course and the specialists were professionals who had dental degrees.
At present, maxillofacial training is a four-year course and the trainees come from medical schools and have medical degrees.
In 1976, the first maxillofacial ward opened within Tirana’s University Hospital Centre and was comprised of 15 beds and four consultants.
In 1998, the new dental school opened and part of the oral surgery work is carried out there.
In the Albanian territory with a population of nearly three million inhabitants, apart from our unit which is in the French hospital “Claude Barnard,” part of Tirana’s University Hospital Centre there are two other active hospital centers (one in Durres and the other in Vlora), where maxillofacial work is performed.
Recent years have been very positive for our unit as we have established very close relations with other maxillofacial centers in Europe, more precisely with the maxillofacial units of Dresden, Germany headed by Uwe Eckelt; the unit of University Hospital Centre of Gallway in Ireland, headed by Patrick McCann and Jack McCann of the plastic surgery department.
This cooperation has proved very positive as we have now expanded our knowledge and improved our work in important areas such as orthognathic, reconstructive and cleft surgery.
The Albanian Association of Oral and Maxillofacial Surgeons was established in 1993. It has some 70 members, 16 of whom cover the public sector throughout the country, the rest work only in the private sector.
Andis QendroArgentina Argentine Society of Oral and Maxillofacial Surgery and Traumatology Sociedad Argentina de Cirugia y Traumatologia Bucomaxilofacial

The Argentine Society of Oral and Maxillofacial Surgery found its roots in the establishment of a section of oral surgery and traumatology within the Argentine Dentistry Association in 1958. The founding fathers were Enrique Müller, Esteban Biolcati and Noberto Costoyas. The first years were characterized by attempting to increase the membership but in 1964, the first scientific meeting took place. In that year, the society was also one of the founding associations of ALACIBU. The society joined IAOMS in 1967.


During these early years, severe opposition was encountered, particularly from head and neck surgeons. Thanks to the steadfast attitude of Basilio Arienza and his colleagues Michael and Müller, who set up departments of oral surgery in three hospitals where they trained several new colleagues, the battle was won. These colleagues really can be considered the pioneers of OMF surgery in Argentina. Enrique Müller was also Vice President of IAOMS during the years 1989–1992.
In 1972, under the presidency of Hermes Becerra, the bylaws of the society were modified so as to incorporate the definition as used by the IAOS at that time. The society also improved their relationship with plastic and head and neck surgeons. The name change to Argentine Society of Oral and Maxillofacial Surgery and Traumatology came about in 1974.
A milestone in the history of the society, under the presidency of Pezza, was the recognition of the specialist certificate, as given by the society, by the Ministry of Public Health in 1978. This was followed by recognition of a voluntary recertification every five years, as suggested by
the society. This was promoted by the then-president, Roberto Blanco.
A true highlight in the history of the society was the XIth ICOMS in Buenos Aires in 1992, so elegantly organized by José Ferreria and his committee. It drew a record participation and exposed Latin America to the international brotherhood of OMF surgery.
The society has steadily grown into a membership of approximately 500. They serve a population of about 40 million people. The training and education of OMF surgeons falls under the auspices of the society and includes a four-year full-time course. They are taught the full scope of the specialty along the guidelines of IAOMS. There are four accredited training institutions where currently 120 trainees are employed but several hospitals take part in the training of residents. Rotations in medicine, surgery and anesthesiology are common but not mandatory.
The society is optimistic about its future and counts on further development and growth. The biannual meetings are attended by about 900 participants, not only from Argentina but also from neighboring countries.
Adrian BenciniAustria
Austrian Association for Oral and Maxillofacial Surgery

Österreichische Gesellschaft für Mund-, Kiefer- und Gesichtschirurgie
Austria, without any doubt, can be considered the cradle of modern oral and maxillofacial surgery on the continent of Europe. It all began with Hans Pichler, born in 1877 in Vienna as the son of a dentist. He studied medicine in Freiburg, Prague and Vienna, at that time the capital of the Austrian-Hungarian monarchy. He began a residency in general surgery, with Anton von Eiselsberg, at the famous department of general surgery of the University of Vienna, where Billroth had earned his reputation. Due to an allergic reaction to carbolic, he had to stop his training. Instead, he went to dental school in Vienna and later attended dental school in Chicago at Northwestern University. He became familiar with G.V. Black and translated his famous book on “Operative Dentistry” into German. He began a dental practice in Vienna in 1903 and became a consultant for the general surgery department, where his former teacher Anton von Eiselsberg was still in charge. The latter mentions in his memoirs the cooperation with Pichler that became effective as of 1903.
As in many countries throughout Europe, World War I became the “raison d’être” for the establishment of units to treat the wounded military, including maxillofacial trauma. Hans Pichler became the first chairman of such a
Surgery department. Among his pupils was Richard Trauner, with whom he would later write a standard text on Oral and Maxillofacial Surgery In 1923, he became the head of the dental clinic as well.
One has to realize that dentistry in Austria in those days was considered to be a specialty of medicine. Dentists went to medical school first and then specialized in dentistry. This only changed in 2000, when Austria had already joined the European Union, as a result of European regulations on the free movement of professionals. Since that time, dental schools have been established.
It is of special interest to mention Pichler’s intervention with the ailment of another famous Austrian; Sigmund Freud. He suffered from a squamous cell carcinoma of the hard palate and was treated by Pichler in 1923. He did a partial maxillectomy and marginal mandibulectomy along with a submandibular lymph node dissection. Freud survived but needed an obturator, which apparently caused some trouble because he had a total of 12 of these prostheses made, including eight made by Pichler, three by Kazanijan and one by Schröder.


World War II caused another upheaval in the profession as again there was a need for the treatment of the wounded. Several military units to treat maxillofacial trauma were set up and many colleagues gained experience with these casualties, among them Rudolf Ullik, who became the successor of Hans Pichler in 1949. During his leadership the department became independent from the general surgery department in 1962. He ultimately became a full professor in maxillofacial surgery in 1967.
Ullik was followed by another well-known colleague, Siegfried Wunderer, particularly known for his approach to the anterior maxillary segmental osteotomy. The Vienna clinic trained several well-known colleagues who took on prestigious positions in other clinics throughout Austria, among them Rudi Fries, who went to Linz and Helene Matras in Salzburg.
In 1989, Rolf Ewers, who received his training from Wilfred Schilli in Freiburg and later from Franz Härle in Kiel, took the chair in Vienna until the present day. His energetic approach to the specialty resulted in several innovations, among which was the world’s first tongue transplantation in 2003; the procedure drew global attention.
Currently, the department covers the full scope of the profession and carries on the reputation which it had gained over more than one hundred years. A special mention, however, is warranted about the very successful organization of the XVII ICOMS in Vienna in 2005 in which all members of the department were involved.
In Vienna, three other small maxillofacial units are located in city hospitals. They are situated in the Danube Hospital (Ingeborg Watzke), in Hospital Hietzing (Werner Millesi) and in the Evangelic Hospital (Kurt Vinzenz).
Although Vienna was the nucleus of the specialty in Austria, over the years some eight departments were established in this country with a little over eight million inhabitants. During World War I. Franz Trauner became the chairman of the department in Graz and kept this position until 1937. Graz is the seat of the second medical school of Austria. He was followed by Hermann Mathis until 1947.
The next chairman was Richard Trauner, a son of Franz and a pupil of Pichler. He became a well-known cleft surgeon and above all the trainer of two well-known colleagues, Hugo Obwegeser and Heinz Köle. Köle eventually succeeded Trauner in 1971. He became known for his contributions to orthognathic surgery and was the inventor of the anterior mandibular segmental osteotomy to close an anterior open bite with interposed grafting, using chin bone. The current chairman in Graz is Hans Kärcher, who followed Köle in 1989 and who can be considered the pioneer in microvascular surgery in Austria.

Hugo Obwegeser went to Zürich, Switzerland in 1954, to become the chairman of the new department. He became full professor in 1964 and chaired his department until 1987, when he retired. His pioneering work on preprosthetic, orthognathic and craniofacial surgery is well known throughout the world. His name is attached to many innovative procedures of which many are still practiced. He is also one of the initiators of the establishment of the European Association for Cranio-Maxillofacial Surgery and a former president of the Swiss and German Associations of Oral and Maxillofacial Surgery.
At the third medical school in Innsbruck, a dental clinic was established in 1909 with a small department of oral and maxillofacial surgery. This clinic was chaired by Bernhard Mayerhofer. This department expanded during WWI for obvious reasons.
Mayerhofer was followed by Wilhelm Bauer in 1933 but he had to leave the country for political reasons in 1938. Georg Riha became the new chief but after WWII, Karl Häupl took over. He had an interesting career being involved with Andresen in Oslo, to co-author a book on functional orthodontics and also during WWII he was heavily involved in the treatment of war casualties in Berlin. While in Innsbruck, he reorganized the dental clinic and the department of oral and maxillofacial surgery.

Häupl left to become chairman in Düsseldorf, Germany and was succeeded by Otto Preissecker, who had trained with Pichler in Vienna. His chair was taken

by Hans Wunderer, a cousin of Siegfried Wunderer, after Preissecker passed away in 1964. The department of oral and maxillofacial surgery had no chairman at that time but Hans Mehnert and Otto Hofer were the surgeons. The latter became known for the anterior mandibular osteotomy that was widely practiced in the days before orthodontics became involved in orthognathic surgery.
In 1971, however, Ernst Waldhart became the chairman. He was trained in Innsbruck but had also done a fellowship in plastic surgery in Galveston, Texas, U.S.A. He managed to develop a full blown department as part of a “Head Clinic” and led this until 2003. His successor is Michael Rasse who trained in Klagenfurt and Vienna. He is known for his work on TMJ surgery but also has a reputation as an oncologic and reconstructive surgeon as well as a craniofacial and cleft surgeon. The department in Innsbruck is particularly recognized for its experience in trauma surgery, mostly related to accidents associated with skiing.
In Linz, an OMFS department was established in 1947 with Otto Hofer as its first chairman. He retired in 1964 and was briefly succeeded by Heinz Köle before he went to Graz again. In 1971, Rudi Fries became the chairman and would hold this position until 1989 when he retired. His special interest was tumor surgery and reconstructive surgery, the field to which he contributed a lot. His successor was Bernd Gattinger, who would also keep this position for 20 years. Gattinger made his name in craniofacial surgery and is considered the pioneer in Austria in that specialty. At present, Michael Malik has served as chairman since 2009.
In Wels, also in upper Austria, a department was established in 1977. The successive chairmen were Heinz-Peter Müller-Schenken, Michael Rasse, Günther Schultes and presently Gert Santler. The “Klinikum Wels-Griesskirchen” is a regional hospital in which this department is located.
In Salzburg, WW II also precipitated activities in oral and maxillofacial surgery but in a different way. An outpatient department was set up in 1940 within the department of ENT with Karl Czerwenka as a consultant dentist, who also treated maxillofacial trauma. A separate department of OMFS was finally established in 1947, headed by Franz Clementschitsch, known for his pioneering work in the field of pre-prosthetic surgery. He was also a disciple of Pichler and under his chairmanship the department flourished. He retired in 1977 and was briefly followed by Gerhard Zisser, who unfortunately passed away soon after.
Helene Matras, also trained in Vienna, became the successor and further developed this department. She was very active and a great team leader and made her
name by the introduction of fibrin glue in reconstructive surgery. She also organized many international meetings, particularly about cleft lip and palate surgery. She was succeeded by Christian Krenkel, who was already a longstanding member of her staff. He became internationally known for his pioneering work in distraction osteogenesis and the application of osteosynthesis. In 2003, a private medical school was established in Salzburg and the city hospital with its department of OMFS became part of it. Krenkel retired in 2010 and was succeeded by Alexander Gaggl, who trained in Graz.
In three other hospitals departments of OMFS have been established: one in Klagenfurt since 1974, one in St. Pölten since 1976 and one in Feldkirch since 1985. All evolved over the years into complete units where the whole scope of the specialty is practiced. The current heads of the departments are Friedrich Chiari in Klagenfurt, Franz Watzinger in St. Pölten and Oliver Ploder in Feldkirch.
There are 11 departments of OMFS in Austria that are all involved in the training of residents. There is no national structured program and the training period, therefore, differs from place to place and also per individual. There is also no fixed number of trainees to be accepted per year but each year some 10 to 12 candidates apply for the final exit examination to achieve official specialist status.
The Austrian association was founded in 1967. Rudi Fries and Rudolf Ullik were the initiators with the idea in mind to structure the training programs and to promote interdisciplinary communication and relations with other disciplines. Ullik became its first president. The current president of the association is Ingeborg Watzke. Only in 1994 did the specialty receive an official status as a medical and dental specialty. There are currently 184 active members. The majority of them work in a hospital setting, often combined with part-time private practice. A few are private practitioners, combining oral and maxillofacial surgery with dentistry. Private practitioners can have a contract with the social insurance companies for dentistry but no contract exists for oral and maxillofacial surgery in Austria.
As a pioneer in our specialty, Rudi Fries needs to be credited for his outstanding contributions to the IAOMS. He not only was one of our founding fathers but also served as one of our former presidents as well as president of the German association, the European Association for Cranio-Maxillofacial Surgery and the IAOMS. On top of that he initiated the establishment of the GermanAustrian-Swiss working group on oral oncology (Doesak), which, until the present day, is a very active multinational scientific organization.
Werner MillesiAzerbaijan, Republic of
No report received. Bangladesh Bangladesh Association of Oral and Maxillofacial Surgeons
The first initiatives to develop oral surgery in Bangladesh took place in the early 1980s at Dhaka Dental College by Monjurul Haque. These initiatives mainly concerned dentoalveolar surgery.
The true development of oral and maxillofacial surgery, including the treatment of trauma, benign and malignant tumors and cleft lip and palate repair, was begun by Molla and his staff, including Rafique, Shaheed and Altaf, in 1987. Under the most difficult of circumstances, with a lack of sufficient and adequate instruments and materials and even with poor anesthetic equipment, these colleagues managed to provide Dhaka with some service in the field of oral and maxillofacial surgery. They were the true pioneers.
The year 1990 was the turning point for Bangladesh oral and maxillofacial surgery because of the foundation of the Joint Australian-Bangladesh Oral and Maxillofacial Surgery Project. The founding chairmen were Molla and Barry Fitzpatrick, later followed by John Arvier. This turned out to be the catalyst for the Bangladeshi colleagues since a fair number of Australian colleagues came over in the years 1991–2001 to instruct them and also to donate instruments. On top of that, OR nurses and young colleagues were trained in Australia for a short period of time. This project also initiated the establishment of post graduate training which resulted in an official master degree in OMF surgery in 1994.

Another important development was the initiative in 1996 of Omar F. Rahman who, along with the help of the Japanese Cleft Palate Foundation, began visiting Dhaka to provide treatment for cleft lip and palate patients with the assistance of Japanese colleagues.
In 1998, Molla was transferred to Shaheed Suhrawardy General Hospital where he managed to set up a new department with operating facilities and beds to admit his patients. By 2004, Bangabandhu Sheikh Mujib Medical University (BSMMU) was also able to provide an advanced OMF surgery service. Including Dhaka Dental College, where Rezaul Haque chaired the department of OMF surgery and Mohiudin is the current head. These three centers are now responsible for the education and training of students and they provide OMF surgical service for the 160 million people residing in Bangladesh.
The education and training of OMF surgeons in Bangladesh is currently based on a MS degree, which is a three-year, full-time course, followed by two years of advanced training in the above-mentioned hospitals.
At present, there is the beginning of a true OMF community with 35 qualified OMF surgeons and 90 trainees. Most of the colleagues work in Dhaka with the exception of a few who work in some other cities.
The Bangladesh Association of Oral and Maxillofacial Surgeons was established in 1993. The first successful international conference was held in 1995 with delegates from India, Japan, Nepal and some other countries. The association holds yearly conferences but also organizes free dental, cleft lip and palate and oral cancer screening clinics in the rural areas of the country. We are very interested in international exchange and treasure our association’s affiliation with the IAOMS.

 Motiur Rahman Molla
Motiur Rahman Molla
Belarus
No report received.
Belgium
Royal Belgium Society of Stomatology and Maxillofacial Surgery
Société Royale Belge de Stomatologie et Chirurgie Maxillofaciale Koninklijke Vereniging voor Stomatologie en Mond-Kaak-en Aangezichtschirurgie
The evolution of oral and maxillofacial surgery in Belgium is rather unusual and, to a certain degree, comparable to that of France in that initially there were colleagues with a medical degree who practiced dentistry and who, in 1900, organized themselves and established the “Société Odontologique des docteurs en médecine de Belgique.” Some of these had some formal dental training abroad but all of them practiced dentistry, some along with general medical practice. These “pioneers” were, thus, not surgeons but medical doctors with some dental education. Four years later they renamed the society “Société Belge de Stomatologie.” As of 1903, they published a quarterly journal that was later called Acta Stomatologica Belgica.
The first chair in stomatology was established in Louvain, in 1905 and occupied by Auguste van Mosuenk. This was soon followed by similar appointments at the Universities of Gent, Brussels and Liege.
Dentistry became an academic study in 1929, but its scope was limited to the treatment of teeth and their supporting tissues. As of 1934, the practice of dentistry was reserved for people with a dental degree and for medical doctors with additional dental training. In 1956, stomatology became an official medical specialty based on a medical degree with four years of dentistry and stomatology training. Many of these stomatologists still mainly practiced dentistry but some sought further training in maxillofacial surgery, particularly in France and Germany.
A major supporter of the profession and a tireless fighter for the status of the stomatologists was Robert Peiffer. He was instrumental in the expansion of the scope of the specialty into maxillofacial surgery and in 1982 the “competence” of oral and maxillofacial surgery was officially recognized by the health authorities and the criteria for achieving this “competence” were precisely described. Some 37 stomatologists, almost equally divided among the French- and Dutch-speaking colleagues, received this competence, which could be achieved by an additional two years of training after the stomatology training.



The last step in this evolution is the formal recognition that candidates for training in oral and maxillofacial surgery needed to have a medical degree (six years) and a dental degree (three or four years, depending on the policy of the University involved), followed by a four-year training in one of the six medical schools, including Louvain (a Flemish and a French), Brussels, Gent and Antwerp. Part of the
training is provided by some large training hospitals, where several consultants are practicing the full scope of OMFS. The content and quality of the training is supervised by special accreditation committees. The training includes the full scope of the specialty with a growing emphasis on esthetic surgery of the face. It also includes oncological surgery but colleagues interested in that part of the profession often follow a fellowship to gain expertise. In actual fact this scenario is rather similar to most European countries where dual degrees are required but in this country the origin of the profession stems from stomatology which is still reflected in the name of the society. The adjunct “Royal” was granted in 1973 by the King.
The society has currently some 250 members and some 10 trainees per year are accepted. Almost all members are also members of the European association and many of the IAOMS. The society holds two meetings a year and has a board with a president that alternates from the French and Dutch speaking regions. The doyen of OMFS in Flanders is Luc Neyt who was the first to really begin a full-scope practice in Bruges, in the early 1970s. The same is true for Hervé Reychler but for the Walloons, who chairs the University department in Brussels and who trained many colleagues from the French-speaking area. Another pioneer and specialist in head and neck surgery is Eric Fossion`, who is both nationally and internationally recognized as an expert oncological surgeon.
The highlights of the society were the jubilee congresses in 1975 and 2000, both in Brussels, where many guests

from abroad were present and the two European meetings, in Brussels (1990) and in Bruges (2010), organized by the then presidents of the EACMFS, Robert Peiffer and Maurice Mommaerts.
Constantinus
Bolivia
Politis• To stimulate the training and education of specialists in recognized centers.
• To promote the exchange of knowledge and experience among national and international centers and specialists in OMFS.
• To stimulate research related to OMFS and to assist in publishing these studies.
Bolivian
Society of Oral and Maxillofacial Surgery Sociedad Boliviana de Cirugia
The Bolivian Society of Oral Surgery was founded in 1944 by Luis Palza Veintenillas, a professor in oral surgery at the University Mayor of San Andrés. It happened at a meeting held at his home with Raúl Chavez Ayoroa, Jorge Rios Moscoso and Hugo Perez Salmon, all staff members at the same university.

In 1969, because of the development of the specialty and following the same tendency as adopted by Argentina, Brazil, Mexico, Chile and other Latin American countries, the society changed its name and became the Bolivian Society of Oral and Maxillofacial Surgery.

Thanks to the efforts of Eduardo Alandia Borda, in 1981, the Minister of Health created a section of oral and maxillofacial surgery at the department, directed by an oral and maxillofacial surgeon.
A training program was established in 1997 by Jorge Rios Jordan, who is still in charge of this three-year program. It is a program similar to other medical specialties and is spread over several hospitals. It is a full-time commitment and only one trainee a year is accepted. It is still the only program in the country recognized by the university, the Ministry of Health and the Medical and Dental associations.
The objectives of the society are:
• To promote the development of the specialty.
• To create centers or services of oral and maxillofacial surgery in hospitals or health centers where there is a need.
• To improve the working conditions of the OMF specialists.
To seek the cooperation of public and private, national and international institutions to help achieve our objectives.
The society has 25 full members and 50 associate members. The latter group consists of dentists with a surgical interest. Bolivia has a population of almost 10 million inhabitants. The society actively participates in the meetings of ALACIBU and of the group countries of the south part of Latin America.
Jorge Rios Jórdan BrazilBrazilian College of Oral and Maxillofacial Surgeons Colégio Brasileiro de Cirurgia e Traumatologia Buco-Maxilo-Facial

As was the case in many countries, in Brazil the need for oral surgery was first recognized by the military. This happened at the end of the 19th century and it was especially the Navy that was in need of oral surgeons because they made long journeys in order to guard the long coast of the country. In 1931, this resulted in a federal act making the practice of oral surgery official in the military. It was not, however, until 1966 that the Federal Council of Odontology formalized oral and maxillofacial surgery as a specialty.
Four years later, in July 1970, a group of about 350 surgeons gathered in the capital Brasília for the 1st Brazilian Congress of Oral and Maxillofacial Surgery

and decided to start an association. The meeting, which was the beginning of the Colégio Brasileiro de Cirurgia e Traumatologia Buco-Maxilo-Facial, was presided over by Gustavo Demerval da Fonseca and was attended by foreign colleagues including Harry Archer (U.S.A.), Norman Rowe (U.K.), Guillermo Ries Centeno (Argentina), Hirokichi Sato (Japan) and Chavez Jaramillo (Ecuador). The thenpresident of Brazil, Emílio Médici, participated in the opening ceremony. The event itself and the creation of the association were on the cover pages of some of the most important Brazilian newspapers in July, 1970.
In the following year, the “founding members” gathered again in Porto Alegre, for a second meeting. During its first three years, the association was presided over by João Jorge de Barros, a nationally renowned surgeon from São Paulo. Subsequently, the college members elected each new president for a period of two years during the “Congresso Brasileiro de Cirurgia Buco-Maxilo-Facial” (COBRAC).

During the last 40 years, the “Colégio” has undergone a dramatic evolution. The number of members has reached almost 1,400, which makes it the second largest association affiliated to the IAOMS and the largest in ALACIBU. The growing number of regional meetings and the current magnitude of the Brazilian congresses (1,800 participants are expected for the 22nd edition in 2013, in Rio de Janeiro), are reflections of the success of the association. Besides, even though this was not the original intention, the “Colégio” is now the formal consulting group of the Federal Council of Odontology with regard to the regulation and practice of OMFS. Being a member of the “Colégio” has become of significant value for Brazilian colleagues, both for their practices and for their patients.
There are currently 57 training programs in Brazil with approximately 334 residents in training (average of 5.8 residents per institution). The Federal Council of Odontology is the supervising body and sets the minimal requirements, such as the subjects to be taught and the training format. Basic disciplines of anatomy, physiology, pathology, pharmacology and medicine are taught during the first year. Programs have to offer at least 2,000 hours of training and the hospitals in which they take place must be fully equipped. Training in general takes a minimum of three years but each program has its specific priorities, such as trauma, orthognathic or reconstructive surgery.
The full scope of OMFS is practiced in Brazil, except for malignancies as they are treated by head and neck surgeons. Some colleagues participate in the head and neck team. In recent years, there has been an increase in the number of surgeons who have considered attending medical school after their residencies. As we still do not have an integrated residency program, including medical school, an MD degree takes at least six years to complete.
Considering the size of the Brazilian territory (8.5 million km2) and its population (184 million people in 5,560 cities), the “Colégio” currently has 14 regional chapters. One coordinator heads each of these branches with the goal of promoting the specialty, gathering more colleagues and organizing meetings. Partly due to the Brazilian dimensions, there are still many professionals registered as OMFS specialists in the Federal Council of Odontology who do not take part in the association.
The “Colégio” is very proud of its history and aware of its evolving role, not only of representing OMFS as a specialty in Brazil but also helping to establish training guidelines and standards of patient care.
Paolo RodriguesBulgaria
Society of Oral and Maxillofacial Surgeons in Bulgaria
The Society of Oral and Maxillofacial Surgeons in Bulgaria was founded in 2009. It officially became a national affiliate of IAOMS in 2011 during the 20th ICOMS in Santiago, Chile. At that time, the Society had 60 members while the total number of oral and maxillofacial surgeons in the country was 54.
Nikolay YanevCanada
Canadian Association of Oral and Maxillofacial Surgeons

Oral surgery was the first specialty of dentistry, the “raison d’être” being necessity and public welfare. Specialists in oral surgery were located in the larger population centers across Canada early in the 20th century, with the exception of Newfoundland and the central prairie region. It is fitting to recall the names of some of these self-reliant pioneers: Johnson and Cox of Vancouver; Henniger of Halifax; Roger McMahon in Montreal; E.W. Paul in Toronto; George Everett in Hamilton; Roy Beer in Winnipeg and Doug Coupland in Ottawa.
Those who nourished the flame of oral surgery in our teaching institutions during the early days merit grateful recognition. There were not many dental schools in Canada at that time and Dr. Henniger at Dalhousie, Beers and
McMahon at McGill and Henderson and Paul at Toronto must be held in grateful and respected memory. The latter served his confreres in a teaching capacity for four decades.
The concept of the formation of a Canadian Society of Oral Surgeons started with discussion among some of the members of the Ontario Society of Oral Surgeons. The activating group decided that the most opportune time to organize would be at the time of the joint meeting of the CDA and the Montreal Fall Clinic in Montreal in the fall of 1953. Notice of such a meeting was publicized as widely as possible through personal letters and notices in the journals. Pro tem officers were elected and a committee to draft a constitution was set up.
For the previous few decades, Canadian colleagues had relied heavily on the American Society of Oral Surgeons (ASOS) for their continuing education. Many of them, of course, had taken their training in the U.S.A. and so there was a natural connection via their training centers, chiefs of service and fellow residents. The ASOS, a much older and larger organization, had also developed its meetings to a high degree of excellence, offering the very best in speakers and programs. Many Canadian colleagues were also members of the AAOMS and, indeed, in the 1960s and 1970s, the ASOS allowed for a Canadian delegate to sit in their legislative arm, the House of Delegates, as a voting member.
However, our American colleagues perceived that, with the passage of time, the CSOS should develop into a strong entity unto itself, independent of the ASOS. In 1969, with this constructive motive to foster this goal, the ASOS negotiated a gradual separation of the Canadian section of their House so that when the time came that the number of Canadian Active Members of the ASOS fell below 25, there would cease to be any delegates from Canada.
This was looked upon variably by our Canadian colleagues; some thought it was unfair and discriminatory,
while others thought it might have a salutary effect by serving as a stimulus for growth and development of the fledgling CSOS. Influential leaders within the ASOS, such as Jim Hayward and Fred Henny, privately confided that this latter reason was the real basis for this decision, hoping that the move would stimulate the CSOS “to stand on its own two feet.” Indeed, this proved to be so and in retrospect, was one of the best things that could have happened to our national specialty association. Canadian oral and maxillofacial surgeons, formerly active members of the ASOS, were invited to remain as affiliate members under the new legislation.
As mentioned earlier, education and training of the early Canadian oral surgeons necessarily occurred offshore, principally in the United States. It was only natural, therefore, that standards of training of oral surgeons in Canada be modeled after those of our American confreres. With the achievement of section status within the specialties grouping of the CDA, the CSOS became a partner with the national dental association in nurturing its goals and objectives. To this end, the Council on Education of the CDA, at its 1971 annual meeting, was directed to seek the collaboration of the section in developing acceptable standards for the graduate and postgraduate educational programs in oral surgery. In response to this invitation, the CSOS produced a document entitled “Guidelines for Graduate and Postgraduate Programs in Oral Surgery.”
Canada currently supports six graduate training programs in oral and maxillofacial surgery: Dalhousie, Laval, McGill, Toronto, Manitoba and Western Ontario. Although these programs commenced as three-year requirements, consistent with accreditation demands of the day, expanded scope and elevated standards have necessitated an increase in the length of training to accommodate these changes. At present, there are 66 residents in training, of whom 53 are in Canada and 13 are in the U.S.A.
The history of the Canadian association would be incomplete if some mention were not made of the advent of the Royal College of Dentists of Canada and the interaction between that institution and the CSOS. This is particularly so in view of the significant contribution which our colleagues made and continue to make, to this esteemed establishment. Memorable surgeons of our past, such as Gerard De Montigny of Montreal, James Coupland of Ottawa, and Frank Smith of Vancouver, should be cited as major contributors to the genesis of the RCDC and its official launch on March 18, 1965.
The scope of practice of our specialty has undergone a metamorphosis over the years as well. Our European colleagues were quite influential in this regard and as their clinicians visited North America on speaking tours and our residents and fellows extended their training exposure

in Europe, the “oral” part of our designation as a specialty was seen as being patently inadequate to describe the full profile of our daily practice. Following the example of the U.S.A. colleagues, the CDA Board of Governors granted official approval of the name change to “Canadian Association of Oral and Maxillofacial Surgeons (CAOMS)” in 1977.

The steady growth and success of the association is due largely to the initiative, self-sacrifice and dedication of successive executive councils. The load has always been heavy but has progressively increased with the growth of the association. There are currently some 300 active members of whom 85 are life members. They serve a population of 34 million people.
Continued progress in oral and maxillofacial surgery depends upon constant renewal by younger oral and maxillofacial surgeons emanating from unassailable teaching programs. It also relies on the vigilance of the Canadian Association of Oral and Maxillofacial Surgeons in continually pressing for higher standards in the profession. Thus far, the success of the organization has more than fulfilled the dreams of its founders.
Al Swanson ChileChilean Society of Oral and Maxillofacial Surgery Sociedad De Cirugia y Traumatologia Bucal y Maxilofacial de Chile
As in many other countries, the practice of oral and maxillofacial surgery, as it is called today, was initially carried out by general surgeons. At first, in the colonial period (1540–1810), they were Spanish but in the years of the struggle for independence (1810–1818), there was a strong French and British influence. The first dentists arrived in 1828 but there is no evidence of their involvement in any oral and maxillofacial surgery.
With the foundation of the University of Chile in 1842, its faculty of medicine became the entity that regulated the practice and teaching of health sciences and the Dean authorized the entry of an increasing number of foreign dentists, especially from Europe. In 1889, the first dental school was established in Santiago. This new generation of dentists began to develop an interest in surgery and some worked together with general surgeons who had been in the practice of oral and maxillofacial surgery.
Two of these general surgeons in particular became the founders of the specialty in Chile. Italo Alessandrini and Alberto Rahaussen can be considered the pioneers. These strong characters had the vision to involve dentists in the surgery of the mouth and jaws and trained the first
generation of oral surgeons, notably Manuel Ramírez, Mario Salcedo, Horacio Rivera, Juan Rojas, Leopoldo Panat, Luis Cobos, Rodolfo Villaseca, René Loubel and Antonio Kokic. This generation became instrumental in the foundation of the Chilean Society of Stomatological Surgery in 1950. The evolution of the specialty into oral and maxillofacial surgery took place gradually and in 1991 this resulted in a name change “Sociedad de Cirugía y Traumatología Bucal y Maxilofacial de Chile”. The society has currently over 200 members spread over the whole country and is the official body that represents the specialty in Latin America and globally. The recognition of oral and maxillofacial surgery as a dental specialty was obtained in 1957 and from this time on, all public and private health institutions consider these specialists to be part of the surgical teams.

The society participates in the National Committee for Certification of Dental Specialties in collaboration with the universities and the College of Surgeon Dentists and has a say in the programs for education and training of oral and maxillofacial surgeons in Chile that are attached to the Universities. The aim of the society is to promote the development of oral and maxillofacial surgery in Chile.
There are five training programs in Chile, two in Santiago and one in Valparaíso, Concepción and Antofagasta. Each year there are 15 to 20 training positions available for which 150 candidates apply. The duration of the program is three years with full-time dedication to academic activities and hospital practice. At the end of the training program, the specialist is capable of dealing with the whole scope of the specialty, as described in the guidelines endorsed by IAOMS, with the exception of malignancies, that are dealt with by head and neck surgeons in cooperation with oral and maxillofacial surgeons.
Hernan Ramirez, Edwin Valencia and Julio CifuentesColombia
Colombian Association of Oral and Maxillofacial Surgery

Asociacion Colombiana de Cirugia Oral y Maxilofacial
The pioneers of Colombian oral and maxillofacial surgery can be traced back to the early 1940s with the names of Alfredo Barcenas and Vincente Plata. In those years the first dental school was established at the National University of Colombia in Bogota. The person who really made the difference was Waldemar Wilhelm, a German-trained oral and maxillofacial surgeon who served as a professor at the University for 20 years. He taught a whole generation of colleagues the art of oral and maxillofacial surgery, which had a tremendous impact on the level of practice in the country. He also served as president of ALACIBU for the years 1972–1976.
Another outstanding person who contributed to the Colombian OMFS community is Tomas Garcia. He trained in the U.S.A. from 1957 to 1959 and returned to Colombia in 1962 to become chairman of the department at the central military hospital. He would hold that position until 1971 after which he became Dean of the dental school at Pontificia University Javeriana in Bogota.
The Colombian Society of “Dentomaxillofacial Surgery” was established in 1958 through the initiative of four founding fathers in Medellin. The years to come would be characterized by rivalry between the two dental schools in Bogota and Medellin but in 1984 an agreement was achieved and from then on a uniform training program was established for both schools. Two individuals deserve credit for their tireless efforts to enhance the specialty:

Enrique Amador, who trained with Waldemar Wilhelm, became the chairman of the department at the University in Bogota. He developed international contacts by inviting several leading authorities from Europe and the U.S.A. to come and lecture. He also served as president of ALACIBU from 1994 to 1997.
Luis Campos, who did his postgraduate training in the U.S.A., worked with Thomas Garcia and became an outstanding clinician and academician.
In the late 1980s, Chirivi became the editor of the society’s journal Odontologica Maxillofacial, which was later renamed Revista Colombiana de Cirugia Oral y Maxilofacial.
During the 1990s, it became necessary to hold several meetings with representatives of neighboring specialties and health officials from the government to both defend the specialty and also to set up authorized training programs in the various hospitals. This battle ended with the establishment of recognized “oral health” departments in several hospitals, including entrée to the emergency rooms. During this period, the society changed its name to the Colombian Association of Oral and Maxillofacial Surgery.
The framework laid down in the 1990s has led to uniform training in seven university departments, along with the affiliated hospitals. There are five training programs in Bogota and two in Medellin, all of them recognized by the Ministry of Health. At this point, the training capacity appears to be somewhat redundant since the number of graduates is exceeding the demand. Nevertheless, several Latin American countries are benefiting from the excess of oral and maxillofacial surgeons in Colombia.
At present, Colombian oral and maxillofacial surgery meets the international standards and the association is very active in stimulating scientific work. The association currently has 223 full members and 83 trainee members.
Daniel Alfonso Rey VásquezAsociación Costarricense de Cirurgia Oral y Maxilofacial (ACCOM)
The idea of creating the Costa Rican Academy of Oral and Maxillofacial Surgery stems from 2003, when nine colleagues came together at the ALACIBU meeting in Panama. A draft of the bylaws was made there and the academy was officially established in the same year. Oscar Reiche Fischel was its first President and also became the first Costa Rican Councilor to the IAOMS. Today, the membership has grown to 16. It is likely that this number will grow since the population of the country is about 4.6 million.

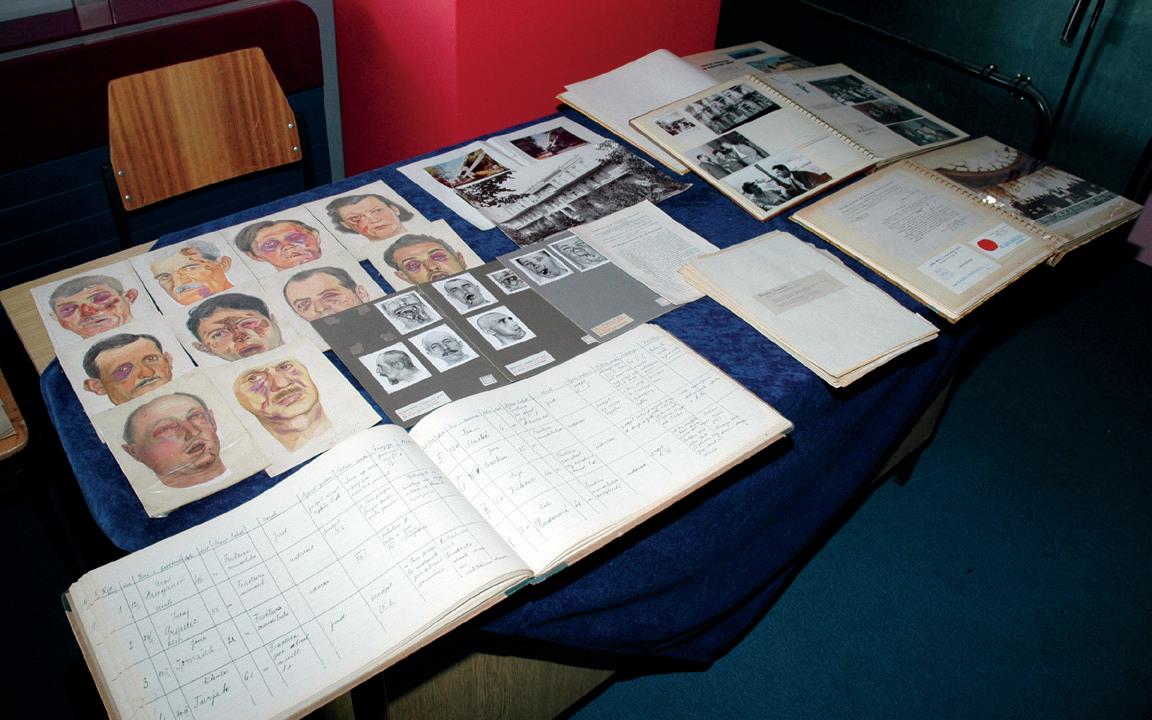
Since there is no training institution in Costa Rica for OMFS surgery, trainees go abroad for their education. Most of them train in Latin American countries. After their training they are registered as OMF surgeons. Oral and maxillofacial surgery is a fully recognized specialty in the country by government authorities.
The ACCOM provides guidance and continuing education for its members to practice the full scope of the specialty.
Oscar Reiche FischelCroatia
Croatian Society of Maxillofacial, Plastic and Reconstructive Head and Neck Surgery

Hrvatsko Društvo Za Maksilofacijalnu, Plasti čnu I Rekonstrukcijsku Kirurgiju Glave I Vrata
The Croatian Society of Maxillofacial, Plastic and Reconstructive Head and Neck Surgery was founded in 1954 as a branch of the Croatian Medical Association under the name “Croatian Society for Maxillofacial and Plastic Surgery.” The founder and first president of the society was Ivo Čupar. At that time, the society included also Croatian plastic surgeons.
In November 1954, the first scientific meeting of the society was held. During that meeting, it was decided to publish a journal, Chirugia Maxillofacialis & Plastica, and in 1955 the first issue was published. The second scientific meeting of the society was held in 1956, the third in 1959 and one every year after that.
The Croatian society members initiated the first Congress of the Yugoslavian Association of Maxillofacial and Plastic Surgeons, which was held in Opatija in 1960.
In 1968, during the third Congress of the Yugoslavian association, Celesnik mentioned the initiative of some European maxillofacial surgeons to establish the European association, which was founded in Zurich in 1970. The representative from Croatia on the founding assembly was Branka Pilar. Four members of the Croatian Society (Čupar, Barlović , Pilar and Korda) participated in the first Congress of the European Association for CranioMaxillofacial Surgery.
On the occasion of the 15th anniversary of the society in 1969, a scientific meeting was organized in Zagreb on “Head and Neck Traumatology.”
In 1973, Ivo Čupar retired and the next president of the society was Herbert Klemenč ić , a plastic surgeon. At that time there were 33 members.
In 1981, Vladimir Mikolji became the president and under his leadership, with assistance from Mišo Virag, several meetings took place with renowned foreign speakers. The society also organized thematic symposia on current topics, such as: “Rigid fixation in maxillofacial surgery,” and “Oral cancer treatment.” In 1990, the society organized an international meeting in Zagreb with more than 100 participants and invited lecturers.
In 1993, the Croatian society, together with the American Academy of Facial Plastic and Reconstructive Surgery (AAFPRS), organized and participated in the project: “Operation Second Chance – America Cares for Croatia.”
In 1997, after 42 years, the Croatian plastic surgeons withdrew from the society and established their own association. In 1988, during the general assembly of the society, the name changed to the Croatian Society of Maxillofacial, Plastic and Reconstructive Head and Neck Surgery. Mišo Virag was elected as president. The society presently has 45 active members and about 12 trainee members but also a large number of associate members, such as oral surgeons, otolaryngologists and other related specialists. The population of Croatia is approximately 4.5 million.
Education and training of maxillofacial surgeons is provided by four university clinics in Zagreb, Split, Rijeka, and Osijek. It takes at least five and a half years to complete maxillofacial training and a medical degree is required. In the training period, residents rotate through all dental disciplines for a total of one year. All residents of the four institutions will spend at least half a year at the University Hospital Dubrava in Zagreb.
Oral surgery can be done after achieving a dental degree and training takes three years. There are about 150 oral surgeons who often work together with the maxillofacial surgeons in the local clinics. They often join the society as associate members.
From 1999 until today, the society has organized meetings every year in different Croatian cities. The society also organized the 4th International Danubius Conference on Maxillofacial and Oral Surgery, in 2002 in Rovinj.
Since 2001, the Best Trainee Presentation, the “Dr. Vladimir Mikolji Award” has been given at the annual meeting.
In 2004, at the 50th anniversary of the Croatian Society, the society became affiliated to the IAOMS.
For the period 2010–2012, Professor Virag served as the president of EACMFS with Dubrovnik the venue of the 21st EACMFS Congress.
Naranda Ratkovic and Mi š o Virag
Cuba
No report received. Czech Republic
No report received.
Denmark
Danish Association of Oral and Maxillofacial Surgeons
Maxillofacial surgery began in Denmark in 1943–1944 when the first Professor in “Jaw Surgery,” Erik Husted, was appointed at the Copenhagen University Hospital “Rigshospitalet” in Copenhagen. At the same time, the
Royal Danish College of Dentistry was established in new buildings in Copenhagen.
The close neighbor, Rigshospitalet, had their first dentist employed in 1910. In 1917, Husted was succeeded by Otto Bjerrum, still known for his thesis on mandibular fractures written in 1934. Bjerrum was the chief of the Dental Clinic at Rigshospitalet until 1952, when he was succeeded by Jens Jorgen Pindborg. During the years 1960–1970, a number of dental clinics were opened at the various Danish county hospitals, and a close teaching and scientific collaboration between the Royal Dental College (later School of Dentistry) and Rigshospitalet proved fruitful over the years.

The establishment of the Danish Association of Oral & Maxillofacial Surgeons followed in 1953. Jørgen Rud, Herluf Baggesen and Jens Pindborg were the pioneers at the time, which moved the development forward from “dentists interested in surgery” towards the establishment of a formal specialist training based on a dental degree. It was accepted by the Danish Dental Association in 1964 and later (in 1976) authorized by the National Board of Health (Sundhedsstyrelsen). In the beginning, the dental consultants at the hospitals treated toothaches and jaw fractures, mainly non-surgically. The first two resident-intraining positions were created in 1964 at Rigshospitalet, comprising of a three-year training curriculum.
In those years (1965), the Scandinavian Association of Oral & Maxillofacial Surgeons was also founded with Erik Husted as the first president. In the following years, an extensive exchange took place between the Scandinavian countries regarding standardization, content of training and compliance with international trends. Another pioneer from the 1970s until recently was Erik Hjørting Hansen, who solidified the specialty in Denmark.
In 1972, the Danes became members of the European Union. It took until 1976 when the specialist training curriculum in “Hospital Dentistry” was officially authorized by the Danish National Board of Health. Denmark has two recognized dental specialties: oral and maxillofacial surgery and orthodontics. A five-year OMFS training curriculum including 1½ years of core medical training was formulated in 1986 under the auspices of the National Board of Health. However, it took another five years until the updated curriculum became formalized in 1991.
Departments of oral and maxillofacial surgery, mainly one-man units, appeared at almost every large county hospital in Denmark from 1980 on until recently but because of a major restructuring of the provincial governments in 2007, 15 counties were reduced to five and the hospital services also had to merge. As a result we have, at present, seven departments of OMFS surgery and four trauma centers, serving a population of 5.6 million, including Greenland. There are 45 active members of the association, with three trainees admitted per year.
The current specialist training in Denmark is based on a dental degree and takes five years to complete. Two years of general dentistry are obligatory before the beginning of training. The training includes general surgery and medicine, ENT, anesthesiology, plastic surgery, neurosurgery and oncology for 1½ years and 3½ years of oral and maxillofacial surgery. Danish specialists have appreciated international collaboration and after finishing training many have further developed their skills by working one or several years outside Denmark.
Many Danish OMFS have been pushing to open the option of double-degree based OMFS training (DDS + MD) in Denmark to comply with European and global trends. However, there is still a way to go before this wish may be implemented in Denmark.
The scope of oral and maxillofacial surgery has changed considerably over time in Denmark. From taking care of toothaches and wiring jaw fractures together, the specialty now covers orthognathic surgery, pre-implant and pre-prosthetic reconstructive surgery, secondary cleft surgery, maxillofacial traumatology and a fair share of maxillofacial and craniofacial reconstruction. This development has been conveyed by a growing understanding of the importance of collaboration with other medical specialties. The multidisciplinary collaboration involves a significant part of oral cancer diagnosis, treatment and rehabilitation, oral medicine, treatment of osteonecrosis and craniofacial anomalies and the units for treatment of rare diseases.
Major contributors to the international literature of OMF surgery were Jens Pindborg on oral medicine and oral pathology, Jens Andreasen on dental trauma and Erik Hjørting Hansen on bone biology and bone augmentation techniques.
We feel privileged to be a part of the international scene of OMF surgeons, which is essential in the global world of today. We are also proud of the role one of the Danish pioneers, Jørgen Rud, played in the early years of the IAOMS. The successful second ICOS, held in Copenhagen in 1965, was in fact the real start of the International association.(see chapter 2)
Morten SchiodtDominican Republic
No report received.
East Africa
Eastern Africa
Association of Oral and Maxillofacial Surgery
The Eastern Africa Association of Oral and Maxillofacial Surgery was established in February 2002 in the presence of the then President of IAOMS, Paul Stoelinga. The association was accepted as an affiliated association in 2003 at the ICOMS in Athens. For this affiliation, the IAOMS bent the rules a little bit as normally associations of single countries apply for affiliation and not regional associations. The situation in Eastern Africa, however, warranted this exceptional decision because despite the enormous size of this region, with an estimated population of over 220 million people, there were only a handful qualified OMF surgeons in this part of Africa. The countries involved in its establishment were Botswana, Burundi, Ethiopia, Kenya, Malawi, Mozambique, Rwanda, Somalia, Sudan, Tanzania, Uganda, Zambia and Zimbabwe.

Since its establishment, things have progressed nicely because the capacity for training has increased. In addition to Nairobi, Dar es Salaam also has become a training center for the region. The Eastern African association has agreed on a mutual training program that will be valid for the whole region, which is adapted to the needs of the countries involved. The IAOMS sponsored educational program, that ran from 2006 to 2011 and was held alternately in Nairobi and Dar es Salaam, has been instrumental in bringing expertise and the necessary means to spread the information needed.
Since its inception, several associations’ meetings have been held in Nairobi, which is the association’s headquarters. The association also joined the African association along
with West and South Africa and the Egyptian association in 2003. With new maxillofacial surgeons qualifying every year from the two training centers, the number of members of the association is expected to slowly but steadily increase. The current numbers are 35 members (25 from Kenya and 10 from Tanzania) and 15 trainees; 10 in Nairobi and five in Dar es Salaam.
Further growth of the association is to be expected since many young trainees from several of the nations involved have enrolled in the two existing training programs. Since the inception of the joint IAOMS-sponsored courses in Dar es Salaam and Nairobi, young maxillofacial surgeons and trainees have benefited from knowledge offered by experienced local and international experts in the fields of biomedical sciences, oral maxillofacial surgery, surgical orthodontics, oral medicine and oral pathology.
With assistance from the IAOMS, the Dar es Salaam center renovated its operating rooms. When fully functional, they will increase the capacity for handling surgical cases and hence greatly reduce the waiting period of referred cases, while at the same time providing room for more exposure to practical maxillofacial surgery for trainees.
Elison SimonEcuador
Ecuador Association of Oral and Maxillofacial Surgeons Asociación Ecuatoriana de Cirugia Bucomaxilofacial
Oral and maxillofacial surgery emerged in Ecuador in the mid-1950s through Pamina and Oswaldo who, after some training in Argentina, returned home to establish the first oral and maxillofacial surgery service in Quito. Pamina and Chavez subsequently taught at the Faculty of Dentistry of the Central University of Ecuador. Before this period, oral and maxillofacial surgery was performed by trauma surgeons, oncologists, otolaryngologists and plastic surgeons.
The first real specialist was Diaz, who acquired this status in 1970 in San Pablo, the Philippines. He worked in the Pasaje Military Hospital and later founded the Maxillofacial Surgery Service of the Armed Forces General Hospital, where he served for 30 years. It is fair to say that Chavez and Diaz were the real pioneers of the art of oral and maxillofacial surgery in Ecuador.
Another important person in our history is Cabezas, who completed his specialization at the University of Chile. For eight years, his work at the Hospital Eugenio Espejo was dedicated to people with limited financial resources. From 1988 until the present time, Chavez served as head of maxillofacial surgery at this hospital.

A pivotal role in the development of OMF surgery was played by Fernando Sandoval, who trained in Mexico and the United Kingdom and worked for 13 years in the
Military Hospital. Later he joined the Quito Metropolitan Hospital where he was appointed head of the department of maxillofacial surgery, a position he has held until the present time. He strove to create the Institute of Postgraduate Studies at the “Universidad Central del Ecuador.” Through agreements with hospitals and with the help of foreign universities, the first graduate courses began in 1998. Currently, there are two universities that offer a specialized program in maxillofacial surgery: “Universidad San Francisco de Quito” and “Universidad Central del Ecuador.”
In the following years, many trainees finished their education and training and settled throughout the country. Many regional hospitals now have oral and maxillofacial surgery services.
The Ecuadorian Association of Oral & Maxillofacial Surgery and Traumatology is a founding member of ALACIBU and in 1986, hosted the ALACIBU Congress. Lyn Blanco Pérez and Fernando Sandoval Portilla
Egypt
Egyptian Association of Oral and Maxillofacial Surgeons
The Egyptian Association of Oral and Maxillofacial Surgeons (EAOMS) was established in 2000 and was accepted as a member of the International Association of Oral and Maxillofacial Surgeons in 2001. During the 3rd International Conference of EAOMS held in Cairo in 2004, the African Regional Association was established.

In 2005, EAOMS organized a scientific conference in Cairo, Egypt to celebrate the 500th anniversary of the Royal College of Surgeons of Edinburgh.
The mission of EAOMS is to improve the quality and safety of healthcare through the advancement of patient care, education and research in oral and maxillofacial surgery. Toward this aim, EAOMS organizes a biannual International Conference in which eminent international speakers participate. These conferences include training courses in recent advances and in technologies in the
commercial exhibit. EAOMS also organizes seminars in different cities in Egypt.

In 2004, EAOMS, in association with Ain Shams University, Al-Azhar University, Glasgow University and Cork University presented a research proposal entitled: “New curriculum for management of maxillofacial deformities” to the European Union and were granted a Tempus Joint European Project “2004–2009.”

In 2010, the Egyptian Association of Oral and Maxillofacial Surgeons is launching its scientific journal, The Egyptian Journal of Oral and Maxillofacial Surgery.
Sherif El-MoftyEstonia
Estonian Society of Oral and Maxillofacial Surgery
The development of the specialty in Estonia began before World War II. The teaching of oral and maxillofacial surgery, however, started in 1936 at the University of Tartu.
The pioneer of maxillofacial surgery in Estonia was Valter Hiie (1902–1963), who graduated from the Medical Faculty of the University of Tartu in 1927. He did his specialty training in Vienna, at that time one of the prime centers of Europe. He became a well-known and much respected maxillofacial surgeon, who developed reconstructive surgery in the maxillofacial region, cleft lip and palate treatment and orthognathic surgery. It was a major step forwards for the patients in Estonia who suffered from maxillofacial diseases, deformities and trauma.
In 1938, the Department of Oral and Dental Disease (as it was called in those days) was founded at the Faculty of Medicine, University of Tartu. Valter Hiie established the Department of Maxillofacial Surgery at Tartu University Hospital in 1945 and was appointed as a full professor and head of the department. His commitment was to teach both dental and medical students. Until 1944, training in dentistry could only begin after having obtained a six-year medical training (MD degree), followed by three years in dentistry.
at the Medical Faculty, University of Tartu and in 1945, the departments of surgical stomatology, oral and dental diseases and prosthetic dentistry.
Valter Hiie established the Estonian Society of Stomatologists in 1938 and chaired the department of maxillofacial surgery until 1963, when he passed away. Maie Lövi-Kalnin became the head of the department of stomatology, Faculty of Medicine between 1982 and 1992. Edvitar Leibur was the head between 1992 and 2003 and from 2003 until the present time, Mare Saag.
Teaching has been based on the concept of training in both medicine and dentistry, being the essential prerequisites for the practice of maxillofacial surgery. The specialty evolved very much from a medical background on the basis of a mono-specialty of stomatology.
It is realized that the dental skills to practice oral and maxillofacial surgery are necessary but that training in dentistry could be combined with training in surgery. The IAOMS International Guidelines for Specialty Training and Education in Oral and Maxillofacial Surgery have been taken into account and this document has provided guidance for the advanced training program.
A certificate of specialty is issued after the completion of training and the passing of a final examination.
Until 1992, the graduates of the department of stomatology at the Faculty of Medicine at the University of Tartu were awarded medical degrees. The accreditation process was created with an appropriate curriculum. Up until 1992, all oral and maxillofacial surgeons belonged to the Estonian Scientific Society of Stomatologists.
The Estonian Society of Oral and Maxillofacial Surgery has a written constitution and was established in 1992. At the same time, the Baltic Association of Maxillofacial and Plastic Surgery was founded and since then, regular congresses have been held biennially. The presidents of Estonian Society have been:

• 1992–1995 — Siiri-Mai Hanstein
• 1996–1999 — Edvitar Leibur
2 000–Present — Marianne Soots
Membership of the society has grown to 23 registered members and four residents. The increasing number of young oral and maxillofacial surgeons in training is welcome and we hope that by the time they take over, our efforts will have started to yield fruit.
The Estonian Society of Oral and Maxillofacial Surgery was officially affiliated with the IAOMS in 1996, with Edvitar Leibur and Tiia Tamme serving as councilors of the Estonian Society of OMFS to the IAOMS from 1996 to 2004 and from 2005 to present respectively.

At present, 23 full members of the Estonian Society of Oral and Maxillofacial Surgery serve a population of 1.3 million. There is one university department for undergraduate and postgraduate training, including a five-year program for oral and maxillofacial surgery. Two hospitals, Tartu University Hospital and the NorthEstonian Regional Hospital in Tallinn, are involved in the training. A principal goal of the Estonian Society of Oral and Maxillofacial Surgery is to improve the specialty and the care provided to patients through the improvement of training programs.
 Tiia Tamme
Tiia Tamme
Finland
Finnish Association of Oral and Maxillofacial Surgeons Suomen Suu-ja Leukakirurgiyhdistys ry
The early beginnings of the Finnish association can be traced back to 1951 when Juuso Kivimaki, a professor of oral surgery, formed a Club of Stomatology. He was a general surgeon but also a specialist in maxillofacial and oral surgery. The establishment of the association, however, occurred in 1966, initiated by Mikko Altonen, who was trained in Hamburg by Schuchardt. Of the founding members, two-thirds had a medical as well as dental degree, whereas one third had a single dental degree. The first president was Ingmar Virtanen, who was a professor of oral surgery at Helsinki University. The association was officially registered in 1968 and the logo for the new association was designed by Arvi Tasanen.
It was in 1892 that Matti Ayrapaa began a school of dentistry at the University of Helsinki. Before that time dentists received their education in Germany, Sweden or Russia. There were several reasons which led to the demand for a specialty that combined medical and dental knowledge, including the war circumstances, increase in
facial trauma and diseases together with the development of anesthesiology. Up until the 1960s, there were three different kinds of specialists with both dental and medical basic degrees, including specialists of oral diseases, specialists of oral surgery and specialists of maxillofacial surgery.
The next step was that medical and dental specialists received separate education and became single-qualified either oral surgeons or maxillofacial surgeons, although the latter usually also had a dental degree. In 1975, the first single-qualified dental specialists were approved. Since 1984, education and training of specialists has taken place at the universities.
From the beginning of 1999, the training program for oral and maxillofacial surgery was adapted to European and international recommendations. The two former specialties were united as one specialty of oral and maxillofacial surgery. Either a dental or medical basic degree is needed to start training in a specialty program. The official training period is six years and it is open for dentists and physicians.
Double qualification is not an official requirement for completion of the training. It appears, however, that all colleagues with a medical degree also have a dental degree. Dentists have to do complementary studies in medicine. The residents do their clinical service at several hospitals across Finland. Currently, three universities, including Helsinki, Turku and Oulu, are entitled to provide a specialist certificate. In 2009, seven new certificates were handed out.
The trainees keep a logbook, which indicates a minimum number of different kinds of treatment in which the candidate has shown proficiency and they must pass a national exit exam before graduating. The license to work as an OMFS specialist is granted by the National Supervisory Authority for Welfare and Health. The specialist training is supervised by the Ministry of Education and Culture which is the highest authority in Finland.
At present, the Finnish association has 164 members, for a population of 5.5 million. Colleagues with completed
have been added to the membership roster. In 1970, Norman L. Rowe from London, and in 1992, Hermann Sailer from Zürich were invited as corresponding members. The membership of the Finnish association has been very active in the Scandinavian Association of Oral and Maxillofacial Surgeons (SFOMK) from the very beginning. Since the foundation of the Scandinavian association in 1965, there have been seven Finnish presidents.
The cooperation with the European Association for Cranio-Maxillofacial Surgery (EACMFS) brought the conference to Helsinki, Finland in 1998 with Christian Lindqvist acting as president. Since the year 1978, the Scandinavian councilor for EACMFS has been from Finland.
In the beginning, a councilor for the International Association of Oral and Maxillofacial Surgeons (IAOMS) was appointed through the Scandinavian association. Since 1995, the Finnish association has had its own representative. Irja Venta
France
French Society of Stomatology and Maxillofacial Surgery Société Francaise de Stomatologie et Chirurgie Maxillo-Faciale

French oral and maxillofacial surgery derived from a medical specialty called stomatology. Its origin goes back to the year 1883, when some colleagues with a medical degree but practicing oral medicine and dentistry, organized themselves in a “Society of Stomatology of Paris.”
In 1895, the first chair in stomatology was created in Lille, which was occupied by Redier, while during the previous year the Revue de Stomatologie was introduced. A person who was instrumental in introducing proper training was Paul Cires. He went to the U.S.A. to orient himself on the education and training of dentists and stayed for two years in Philadelphia where he acquired a formal degree in dentistry. On his return to France, he became the main promoter of the establishment of a School of Stomatology in Paris, which was eventually
Board of the French Society of Stomatology and Maxillofacial Surgery, from left to right: Doctors Dujarric, F. Boutault (president-elect 2013), L. Ben Slama (president 2012), X. Pouyat, F. Cheynet, Joel Ferri (president 2011), P. Sabin, D. Pouit, J.P. Fusari, P. Blanchard and P. Breton (Secretary General).

It is of interest to note that the International Association of Stomatology was established in 1907 consisting of members from more than 20 nations, particularly from the south and east of Europe. As in other countries involved in World War I, the demand for treating the wounded created a need to organize their transport behind the front lines. For this reason special centers for the treatment of maxillofacial trauma were created, notably in Paris (Val de Grâce) but also in Lyon and Bordeaux.
In 1920, another important step in the development of stomatology occurred in that Chompret was appointed to chair the stomatology department at the medical faculty of the University of Paris. Over the years, several other schools of stomatology were established throughout France, notably in Bordeaux, Lille, Lyon, Nancy and Nantes. In 1943, the Society of Stomatology of Paris changed their name into the French Society of Stomatology.
In 1949, an official recognition of stomatology as a medical specialty was received. Subsequently the specialty gradually developed into a surgical specialty under the guidance of some key pioneers, such as, Pierre Cernea in Paris, Maurice Gosserez in Nancy, Freidel in Lyon and Georges Ginestet, who was a general in the military service. As of 1953, the society was called the “French Society of Stomatology and Maxillofacial Surgery.” However, it took another 20 years before the first congress was held in Paris in 1973. It was Pierre Cernea, the president at that time, who organized it and this congress marked the beginning of the true development of maxillofacial surgery in France. Members of the society gradually lost their interest in dentistry and this went along with the establishment of national dental schools, which was made possible by law in 1965, in accordance with the practice in other European Community member states. The teaching of dentistry, at that time, however, remained the responsibility of the stomatologists in the medical schools. It was only after the “revolution” of 1968 that dentistry became completely separate from the medical schools.

Oral and maxillofacial surgery in France, despite its different background, has contributed substantially to the profession. The names of Dechaume, Delaire, Merville and Champy do not need any further explanation but there are many more that should be recognized. The work of Paul Tessier, although not a stomatologist, also does not need any reiteration. The specialty has also developed into a true regional specialty in that the whole face is included in the scope of the profession. This is exemplified by the world’s first facial transplant, carried out by Bernard Devauchelle and his team in Amiens.
At present, the training of stomatology and maxillofacial surgery takes a full five years and includes one and a half years of general surgery, two years of maxillofacial surgery and one and a half years minimum in plastic, neuro, or ENT surgery. One year, but often it will be two years, needs to be spent in a university department of stomatology and maxillofacial surgery. There are approximately 30 new trainees accepted each year, spread over the country, which implies that some 150 trainees are educated.
There are currently about 1,200 registered colleagues but some of them may be retired. The French Society organizes national meetings every year.
Joël FerriGeorgia, Republic of Republic of Georgian Association of Stomatology
and Maxillofacial Surgery
The Georgian Association of Stomatology and Maxillofacial Surgery was established in 1991. Before that time, a Georgian society of dentists and maxillofacial surgeons existed. The first president of that association was Professor Omari Nemsadze. The association had about 300 members.
In 1997, Zurab Chichua attended the 4th Congress of Oral and Maxillofacial Surgery of the Mediterranean Sea countries, which was held in Antalya, Turkey. It was there that he met Rudi Fries, who was instrumental in the efforts of the association to join the international scene. Professor Fries was subsequently invited to attend a meeting of dentists and maxillofacial surgeons of the Black Sea countries and it was there that an application for membership of the IAOMS was agreed upon. The association eventually joined IAOMS at the Kyoto ICOMS in 1997.
Over the past several years, colleagues, particularly from Germany, have visited Georgia to hold workshops for trainees and young colleagues. In 1998, the association

also became involved with the European Association for Cranio-Maxillofacial Surgery and sent a councilor to the Helsinki Congress.
The Georgian association is responsible for the training of OMFS surgeons. It consists of four years of hands-on training in oral and maxillofacial surgery based on a degree in stomatology (dentistry). There are three training institutions that accept a total of six trainees per year. The specialty is officially recognized by the Ministry of Health.

There are currently approximately 30 OMFS surgeons in Georgia for a population of 4.6 million people. The association is keen to send some young colleagues to western countries to expand the scope of OMFS in Georgia.
Zurab ChichuaGermany
The German Society of Oral and Maxillofacial Surgery
Deutsche Gesellschaft für Mund-, Kieferund Gesichts-chirurgie (DGMKG)
The German profession has two organizations representing oral and maxillofacial surgery. Both organizations are affiliated with the IAOMS but are represented by one councilor.

The history of the German Society of Oral and Maxillofacial Surgery is tightly linked to the development of the specialty during the two World Wars. Hugo Ganzer and Christian Bruhn were the protagonists in the field at that time. They ran army hospitals for oral and maxillofacial surgery during World War I in Berlin and Düsseldorf. The department in Düsseldorf was later named West German Department of Oral and Maxillofacial Surgery and was the first department of this specialty at that time in Germany.
Already after World War I, a board certification for oral and maxillofacial surgery (“zahn-, mund- und kieferkrankheiten”) was established. From 1924 onwards, a three-year residency was mandatory to become a specialist.
In 1950, the professional “Union of German Oral and Maxillofacial Surgeons” (“Verband der Fachärzte für Zahn-, Mund- und Kieferkrankheiten”) was established. The members of this association founded the precursor of the German Society of Oral and Maxillofacial Surgery in 1951. Martin Waßmund was elected the first chairman of the society. The reason for the establishment of a new society was the need for a scientific representation of the specialty in the council of the German Medical Association.
The society started with 52 members and adopted the name “The German Society of Maxillofacial Surgery.” Karl Schuchardt became chairman of the society in 1953 and held this post until 1964. His successors included names of such well-known authorities as Rehrmann, Schröder, Steinhardt, Stellmach, Spiessl, Scheunemann, Pfeifer, Becker, Schilli, Schwenzer, Fries, Obwegeser, Machtens and Hausamen. The current chairman of the society is Henning Schliephake. In 1972, the term “oral” (“mund”) was included in the name of the society. From 1976 on, the specialty was officially called “oral and maxillofacial surgery.”

Between 1948 and 1990, oral and maxillofacial surgery took a separate course in East and West Germany. With the German reunification, the East German Society was integrated in the German Society.
The professional Union of German Oral and Maxillofacial Surgeons (“Bundesverband Deutscher Ärzte für Mund-, Kiefer- und Gesichtschirurgie”) represented the specialty and the professional interests of more than 1,000 oral and maxillofacial surgeons of 17 regional associations. In 2000, however, the professional Union of German Oral and Maxillofacial Surgeons and the German Society of Oral and Maxillofacial Surgery merged and formed the new German Society of Oral and Maxillofacial Surgery (Deutsche Gesellschaft für Mund-, Kiefer- und Gesichtschirurgie).
Today, the executive board consists of the president, vice president, treasurer and four additional board members, who represent the whole breadth of the specialty of oral and maxillofacial surgery, both with regard to patient care as well as research. The board is supported by

an executive’s office and special departments for quality assurance, scientific guidelines, esthetic surgery, pain therapy, implantology and continuing education. The current active membership is 1,600 for a population of 82 million.
The training and education for oral and maxillofacial surgery takes five years according to the current regulations for board certification. Board certification can only be achieved when the candidate has a medical as well as dental degree. Twelve months of the training can be done in general surgery, anesthesiology, otorhinolaryngology or neurosurgery. The sub-specialization “plastic operations” takes an additional two years.
The training in oral and maxillofacial surgery includes the acquisition of knowledge, experience and skills in the specialty as well as the performance of a defined number of operations (logbook) in traumatology, tumor surgery, surgery of malformations, orthognathic and TMJ surgery, dentoalveolar surgery, preprosthetic surgery and implantology, surgery of peripheral facial nerves, septic surgery and plastic and reconstructive and esthetic surgery. There are currently 79 hospital-based departments that are accredited to be a training institution. The number of trainees is not limited but at present, there are approximately 100 trainees in Germany.
In the bylaws of the German Society of Oral and Maxillofacial Surgery, it is written that it is the mission of the society to promote, protect and advance oral and maxillofacial surgery scientifically as well as on a professional level, to assure excellence in the field and to support its members in practicing their specialty through education, research and advocacy.
One of the major activities of the society was the patronage of the German-Swiss-Austrian Working Group on Maxillofacial Tumors (DOESAK, “Deutsch-

Österreichisch-Schweizerischen Arbeitskreis für Tumoren im Kiefer- und Gesichtsbereich”) that was established in 1971 and was dedicated to a systematic documentation of all tumors in the oral and maxillofacial region. Along the same lines, the German Cleft Palate and Craniofacial Association (“Deutschen interdisziplinären Arbeitskreises für Lippen-Kiefer-Gaumenspalten/kraniofaziale Anomalien”) was founded in 1982. Both associations run annual congresses that are well established and attended by members of the DGMKG. The DOESAK has become an independent association since 2006.
A major activity of the German Society of Oral and Maxillofacial Surgery is the establishment of guidelines for diagnosis and treatment of diseases in the field of oral and maxillofacial surgery.
The Academy for Oral and Maxillofacial Surgery was founded in 2004 and aims at securing continuing education (e.g. in esthetic facial surgery and implantology). For this reason the Academy holds annual spring and fall meetings.
Publications of the German Society of Oral and Maxillofacial Surgery and the Federal Association of German Specialists in Oral and Maxillofacial Surgery were made in Fortschritte der Kiefer- und Gesichts-Chirurgie (Proceedings in Maxillofacial Surgery) from 1955 to 1996 and from 1977 to 1996 in the Deutsche Zeitschrift für Mund-, Kieferund Gesichtschirurgie (German Journal for Oral and Maxillofacial Surgery). After the merger of the two organizations the new journal Mund-, Kiefer- und Gesichtschirurgie was established and replaced its two predecessors. Mund-, Kiefer- und Gesichtschirurgie is also the official journal of the Austrian, Hungarian and Swiss Societies of Oral and Maxillofacial Surgery. In 2008, the journal changed its name to Oral and Maxillofacial Surgery and is now published online in English. The journal Der MKG-Chirurg was also launched in 2008 and is focused on continuing education. On top of this, the Journal of Cranio-Maxillofacial Surgery is also an official journal of the German Society of Oral and Maxillofacial Surgery.
The annual conference of the German Society of Oral and Maxillofacial Surgery is held each year in May at various places. From 1981 onwards, the conference has been run by an elected congress president. Joint congresses have been held in 1968 in Philadelphia and in 1993 in Orlando and in 1997 in Hamburg with the American partner societies and in 1993 with the Dutch association. The annual conference is always dedicated to one or two main and two minor topics. There is always a symposium on military medicine and the “Day of the Academy.” Since 1958, the Waßmund award is conferred annually on a member of the specialty for outstanding scientific achievements. The winner is chosen by a jury of five members of the society.
Oral and maxillofacial surgery is one of the surgical specialties of the head and neck region. As it requires
a dental and medical qualification, it will remain an irreplaceable link between medicine and dentistry. The engagement in the IAOMS is seen as an important activity in order to keep up with developments in the field and to represent the professional interests of the specialty on an international level.
Emeka NkenkeGermany
German Academy of Oral and Maxillofacial Surgery

Arbeitsgemeinschaft für Kieferchirurgie
In the 1920s, a board certification for oral and maxillofacial surgery was established in Germany that required double qualification. From 1924 onwards, a three-year residency became mandatory. Detailed regulations for training in oral and maxillofacial surgery were established in 1935. Consequently, the predecessor of the Academy of Oral and Maxillofacial Surgery (Arbeitsgemeinschaft für Kieferchirurgie) had already been founded in 1932 by Georg Axhausen, who was the head of the department of oral and maxillofacial surgery in Berlin at that time, Wolfgang Rosenthal (1882–1972), who became the head of this department in 1950 and Christian Bruhn (1869–1942), who was the head of the West German Department of Oral and Maxillofacial Surgery (Westdeutsche Kieferklinik) in Düsseldorf. They named it “German Society for Stomatology.” In 1935, the name was changed to “Arbeitsgemeinschaft für Kieferchirurgie” (Academy of Oral and Maxillofacial Surgery).
The Academy of Oral and Maxillofacial Surgery aimed to bring together oral and maxillofacial surgeons with double qualifications and dentists interested in surgical aspects in their field, because Axhausen felt that there was need for establishing regulations for a board certification in oral surgery. The bylaws stated that it was the mission of the Academy of Oral and Maxillofacial Surgery “to give a clear definition of the specialty “oral and maxillofacial surgery” for doctors as well as dentists, who intended to practice in this field. Eligible members of the academy are surgeons as well as dentists who have proven their dedication to oral and maxillofacial surgery either “scientifically or on a professional basis.”
In the early years, the meetings of the Academy of Oral and Maxillofacial Surgery were included in the annual conventions of the German Society of Dental, Oral and Craniomandibular Sciences (Deutsche Gesellschaft für Zahn-, Mund- und Kieferheilkunde). The first separate conference of the academy was held in 1938 in Berlin with the main topic of “oral surgery.” From that time on, an annual conference was established.
In 1945, the short history of the Academy of Oral and Maxillofacial Surgery came to a temporary end. However, in 1951, it was re-established by Walter Sauvélet and 10 colleagues, as a reaction to the foundation of the Professional Union of Oral and Maxillofacial Surgeons (“Verband der Fachärzte für Zahn-, Mund- und Kieferkrankheiten”).


In 1950, Sauvelet and Axhausen, the honorary chairmen of the new Academy of Oral and Maxillofacial Surgery, feared that if oral and maxillofacial surgery was only represented by the Professional Union of Oral and Maxillofacial Surgeons of Germany, the aspect of dentistry in the field would lose its central role, although dentistry was supposed to be of utmost importance in oral and maxillofacial surgery. Again, it was the aim of the Academy of Oral and Maxillofacial Surgery to support the development of the specialty in a symbiosis of surgery and dentistry.
At the first conference of the new academy in 1952, it was emphasized again in the bylaws that “it is the mission of the academy to create a clear and consistent vision of the role of dentists practicing in the field of oral and maxillofacial surgery.”
In 1958, the Academy of Oral and Maxillofacial Surgery concluded an agreement with the Professional Union of Oral and Maxillofacial Surgeons of Germany in a way that the union would be responsible for the advocacy of professional interests of the specialty, while the academy would take care of the scientific progress in the field. From that time on, the different orientations of the two organizations were clearly defined. A comparable agreement was made with the Professional Association of German Oral Surgeons (“Berufsverband Deutscher Oralchirurgen”) in 1988.
One of the major activities of the Academy of Oral and Maxillofacial Surgery, together with the German Society of Oral and Maxillofacial Surgery, was the patronage for the foundation of the German-Swiss-Austrian Group on Maxillofacial Tumors (DOESAK, “Deutsch-
Österreichisch-Schweizerischen Arbeitskreis für Tumoren
im Kiefer- und Gesichtsbereich“) that was established in 1969 and was dedicated to a systematic documentation of all tumors in the field.
The annual conference of the Academy of Oral and Maxillofacial Surgery gives life to scientific, practice oriented and social activities of the members. From 1963 on, it has been held in Bad Homburg with only few interruptions until today. The conference traditionally takes place around Ascension Day. Today, the audience does have the opportunity to attend scientific lectures and practical hands-on workshops as well as a program dedicated to continuing education in oral surgery.
The Academy of Oral and Maxillofacial Surgery has been involved in joint conferences starting in 1962 when the German Society of Dental, Oral and Craniomandibular Sciences held the congress of the FDI. In 1971, the academy organized a joint conference together with the International Association for Dental and Maxillofacial Radiology. In 1977, the Academy affiliated with the IAOMS and held the 8th ICOMS in Berlin in 1983 in order to underline its interest in international relations.
Today, the Academy of Oral and Maxillofacial Surgery is one of the two major representatives of oral and maxillofacial surgery in Germany with the mission of securing the scientific and practice-oriented development of the specialty. In this context, it has achieved a central role in the development of scientific guidelines in the field and runs one of the most important annual conferences on oral and maxillofacial surgery.
Emeka NkenkeGhana
Ghana Association of Oral and Maxillofacial Surgeons
The Ghana Association of Oral and Maxillofacial Surgeons (GAOMS) had its first meeting on 24th June 2005 but was inaugurated on 27th June 2008. Twelve members form the association, which currently has a president, secretary and treasurer as officers.

The aims of the association are:
To improve the healthcare of the population of Ghana by improvement in the delivery of oral and maxillofacial surgery (OMFS).
• To foster relations with other nations of West Africa.
• To agree on common grounds of basic education, standards of delivering patient care and strategy of collaborative research
• To forge links with other African countries.
• To achieve international accreditation of the training programs and establish centers of excellence for education in Ghana.
The association has an annual meeting in June but has not organized itself well enough to start scientific meetings on an annual basis. However, it joins the Ghana Dental Association for annual scientific meetings, where there are presentations on subjects relating to oral and maxillofacial surgery. One such presentation was by the president on the topic, “Common Oral Tumors in Ghana.”
The officers of the association are: president, Grace Parkins; general secretary, Emmanuel Kofi Amponsah and treasurer, Eric Ngyedu. The association sought affiliation with the International Association of Oral and Maxillofacial Surgeons in March 2009. This was agreed in Shanghai.
Grace Parkins GreeceHellenic Association of Oral and Maxillofacial Surgery
The Hellenic Association of Oral and Maxillofacial Surgery was founded in March 1959 as “The Hellenic Association of Oral Surgery,” following the suggestion of Theo Mavrogordatos, professor of oral surgery in the dental school of the University of Athens. He was also the first president and remained president until 1972.

In 1960, the association began its activities organizing meetings with the participation of leading Greek and foreign specialists. In 1969, to mark the first decade of the HAOS, the first Assembly in Oral Surgery took place. It was followed by the second, third and fourth assemblies in 1979, 1983 and 1986 respectively.
In 1986, in accordance with the evolution of oral and maxillofacial surgery into a specialty with a broader
spectrum, the title of the association was changed to “The Hellenic Association of Oral and Maxillofacial Surgery.” The HAOMS became an affiliated association of the IAOMS and of the European Association for Cranio-Maxillofacial Surgery (EACMFS). The HAOMS has councilors in both associations. In the same year, in co-operation with the publishing company of LATTERE, The Greek Journal of Oral and Maxillofacial Surgery was launched. This journal appeared four times a year, until 2000.
In 1988, the 8th Congress of the EACMFS took place in Athens, while Professor Christos Martis was president of the EACMFS.
Beginning in 1989, the year of the 5th Assembly on Oral and Maxillofacial Surgery, it was decided that there be yearly congresses of the HAOMS instead of the assemblies that were held once in three years. In the same year, the specialty of oral and maxillofacial surgery was officially recognized in Greece. A change in the rules and regulations of the HAOMS was made, implying that only qualified oral and maxillofacial surgeons could become full members.
From 1989 until 2010, 25 Pan-Hellenic Conferences of the HAOMS have been organized. The number of

president of HAOMS, George Panos. This meeting will be well remembered by those who participated.
From 2000, the HAOMS has published the bilingual Greek-English journal, “Hellenic Archives of Oral and Maxillofacial Surgery” and began a web site: www.haoms. org with George Panos being the present editor.




For the past 50 years, the Hellenic Association of Oral and Maxillofacial Surgery has contributed to the progress of the specialty in Greece and abroad. It has also helped educate medical doctors, dentists and oral and maxillofacial surgeons and is sure to play a significant role in the future.
The Greek requirements for entry into specialist training begin with examinations after the acquirement of both medical and dental degrees. Specialist training is a continuum lasting five years with an exit examination taken towards the completion of specialist training. It consists of six months General Surgery, 48 months Oral and Maxillofacial Surgery and 6 months of Plastic, ENT , or other relevant surgical specialty.
George Panos
The development of the specialty started relatively late in Hong Kong, during the 1950s. The then colonial government ran a dental service mainly for its civil servants. The dentists in charge were educated overseas. Walter Allwright was the first dental specialist in charge of the service, who would also run an operating list in Queen
In the 1960s, dental officers with an interest and some experience in oral surgery were sent to centers overseas for further training. On their return they were deployed in various hospitals. The appointment of Eric Fung as the
first consultant oral surgeon was a milestone because it denoted the recognition of oral surgery as a specialty. This was gradually followed by appointments of other colleagues in some other hospitals.
An important event happened in 1980 with the establishment of a dental school at the University of Hong Kong. This also included a department of oral surgery and oral medicine. At the same time, some specialists, trained abroad, returned to Hong Kong and began practicing more advanced surgery, such as orthognathic surgery. Bill Yan and Nigel Clark are among these pioneers.
Things really changed with the arrival of Henk Tideman in 1988, who was appointed the new chairman of the department at the university. Under his leadership, the postgraduate training was structured and enhanced but above all, he was instrumental in advancing orthognathic and reconstructive surgery to meet international standards. The name of the department also changed to “oral and maxillofacial surgery.”
In 1990, Henk Tideman and some other surgeons from the department and private sector came together and founded the Hong Kong Association of Oral and Maxillofacial Surgeons. With the establishment of the Hong Kong College of Dental Surgeons as a constituent college of the Hong Kong Academy of Medicine in 1993, oral and maxillofacial surgery training programs were set up at the university and other major hospitals. The specialty was subsequently recognized as a specialty by the Hong Kong Academy of Medicine.

To qualify as a specialist, one has to undergo six years of postgraduate education and training divided into three years of basic and three years of higher surgical training. In the first part the emphasis is on pre- and post-operative patient assessment and management, including modern modes of imaging, sedation and pain treatment but also on oral diagnosis and surgery. An intermediate examination is conducted at the end of the first three years, which is
Edinburgh. In the following three years, the full scope of the specialty is taught with an emphasis on orthognathic and reconstructive surgery, including pre-implant and implant surgery. At the end of the sixth year, candidates have to sit for an exit examination. When passed, the candidates will receive a FCDSHK (OMS), after which one can be registered by the Hong Kong Dental Council as a specialist in oral and maxillofacial surgery.
In the first decade of this century, two special events took place. In 2006, the Hong Kong Association of OMFS was delighted to host the 7th Asian Congress on Oral and Maxillofacial Surgery. The 19th ICOMS, which was held in Shanghai in 2009, was organized in conjunction with the membership’s Chinese colleagues, with whom we maintain a cordial relationship. The membership is also proud of the positions held by two of their members. First, Nabil Samman served as the president of the Asian Association from 2004–2006, as president of the IAOMS from 2007–2009 and as chairman of the IAOMS Foundation from 2009–2011. He also participated in the editorial board for both associations’ journals and was selected as the editor-in-chief for the International Journal of Oral and Maxillofacial Surgery in 2012. Lim Cheung also served in various capacities in both aforementioned associations.
With the increasing number of qualified specialists, currently 48 for a population of 4.5 million, many of our members have entered private practice but still play an active role in the association. Despite the relatively short history of our association, it has grown into a robust and coherent group, which is friendly within and outside the association. We are proud to have a nationally recognized training program and accreditation and certification processes independent from other countries. This achievement could not have materialized without the pioneering vision of our forbearers and the continuing efforts of all our current members.
Ben Chow and Jason ChengHungary Hungarian Association of Oral and Maxillofacial Surgery

As in most continental European countries, oral and maxillofacial surgery began with general surgeons being faced with war victims. The first person to become known to have practiced oral and maxillofacial surgery is János Balassa, a general surgeon in charge of the treatment of gunshot wounds during the Austro-Hungarian War of 1848–1849. The St. Rokus Hospital, built in the 18th century in Pest, was the hospital where all wounded military were treated. Dr. Balassa’s claim to fame was also various types of labioplasties and the surgical treatment of cleft lip and palate. He became the physician of the court.
At the end of the 19th century, one of the most modern medical university complexes in Europe was built in Budapest. The University Stomatological Department was also planned at that time but it was completed only in 1908, with József Árkövy as the first director. After working as a surgeon in Hungary, Árkövy went to London to study dentistry. On returning home, he founded first a private and then the university dental school and in the early years of the 20th century, dentistry was officially included in the medical curriculum.
The Stomatological Clinic had one of the first inpatient wards. World War I led to further advances in the care of facial injuries. The Stomatological Clinic was rapidly filled and it was necessary to convert other treatment rooms into wards and operating theaters. As a result of the tremendous need for treatment of large numbers of patients with facial injuries, the importance of oral surgery became clear not only in Budapest but also in other hospitals throughout the country.
Árkövy retired in 1920 and died as a lonely and somewhat forgotten man in 1922. He was succeeded by
József Szabó, who renewed the internal structure of the clinic and broadened the education in maxillofacial surgery. It was thanks to Szabó and his successors and colleagues (Károly Balogh, Ferenc Skaloud and Sándor Orsós) that a national network of units providing oral and maxillofacial surgical care, was built up. By the end of World War II, practically every large county hospital had a ward for oral surgical inpatients.
From the beginning of the 20th century there was an active exchange of science, as related to oral and maxillofacial surgery in Hungary. In recognition of this, the then International Society of Stomatology (L’Association Stomatologique Internationale) organized its congresses in 1908 and 1931 in Budapest.
Books in Hungarian on oral surgery were translated into English, German and Russian. In spite of the post-war hardships, a new lecture room was built at the oral and maxillofacial and stomatology department in Budapest in 1946. This gave a possibility for Károly Balogh, the head of the department, to hold scientific sessions on a regular basis, attended by colleagues from all over the country.
Dental education in the new Dental Faculty began in Budapest in the 1950s and later in the university cities of Szeged (1960), Pécs and Debrecen in the 1970s.
Forming the Hungarian association, Béla Berényi and Imre Vámos from Budapest and Károly Tóth from Szeged were the first professors from behind the Iron Curtain to take an active part in the congresses of the International Association of Oral and Maxillofacial Surgeons. Hungary became affiliated with the IAOMS in 1974.

In 1971, it became officially possible to specialize in oral and maxillofacial surgery in Hungary. At the beginning of the 21st century, the Hungarian specialization system was recognized by the UEMS, the board representing the medical professions in the European Union. The Hungarian association of Oral and Maxillofacial Surgeons, as an independent organization, had been established at the beginning of 1996, its first president being György Szabó. Before that time, it had functioned only as one of the sections of the Hungarian Association of Dentistry, under independent leadership but not with an independent budget. The next presidents of the association were: Adam Kovács, Jozsef Barabás and Lajos Olasz.
The Hungarian association has been very active internationally. Its national congress is held annually, attended by some 200 members. Since 1991, the Danubius Congress is held biannually, in conjunction with all countries through which the Danube flows. It has been held nine times in the subsequent 18 years. These events are recognized and co-sponsored both by the IAOMS and by the European Association for Cranio-Maxillofacial Surgery.
It was one of the great achievements of the Hungarian Association of Oral and Maxillofacial Surgeons to win the bid to organize the 12th ICOMS in Budapest in 1995. Together with the IAOMS, it succeeded in putting on a highly successful congress. It was a remarkable achievement so shortly after the lifting of the Iron Curtain and the organizing committee received many compliments afterwards.
At present, hospital units providing oral and maxillofacial surgery service are functioning in every region of Hungary. Their number is less than it was 15 years ago but they are headed by outstanding specialists with medical and dental qualifications. Both outpatient and inpatient care is available at the four medical universities in Hungary.
As a result of the present severe financial restrictions, only five to six maxillofacial residents receive training each year, though there are many more applicants. The duration of training is six years and the universities are responsible for the training programs.
The six-year maxillofacial training program begins with a compulsory two-year period of dental study; the trainees participate in this together with the undergraduate students. Many of them take advantage of the possibility of extending this two-year period with a further two years in order to also obtain a dental diploma. Unfortunately, these additional two years are no longer financed by the state. Double-qualified maxillofacial and single-qualified oral surgeons are members of the Hungarian association. Training in dentoalveolar surgery is also the responsibility of the universities. The training lasts three years after acquisition of the dental diploma, six months of which must be spent in a university inpatient unit. The ratio of maxillofacial to oral surgeons is 1:5 and at present, there are about 50 maxillofacial surgeons and 250 oral surgeons for a population of around 10 million.
The leadership of the association has so far succeeded in avoiding the separation of these professions.
Very significant roles have been played in the recent developments in oral and maxillofacial surgery in Hungary by the professors at the four university clinics: György Szabó and József Barabás in Budapest, Ádám Kovács and József Piffkó in Szeged, Pál Redl in Debrecen, and Lajos Olasz in Pécs.
Joszek Barabas and György SzabóIndia
Association of Oral and Maxillofacial Surgeons of India

Mino S. Ginwalla is generally considered as the father of Oral and Maxillofacial Surgery in India. He returned to India in the early 1950s after training as an oral surgeon
at McGill University in Canada. Oral surgery was a late specialty in India as it did not have the advantage of wartrained oral surgeons as did Europe and America. Most surgery in the maxillofacial region before the 1950s was being done by general surgeons with an interest in oral surgery.
Ginwalla joined the Nair Hospital Dental College in Bombay (now Mumbai) as professor and head of the department. It was an exciting phase when plastic surgery was also in its infancy. Doyens such as Benjamin Rank (Melbourne) were establishing plastic surgery as a specialty in India under the Colombo Plan. Ginwalla, even in those days, had worked with the pioneer plastic surgeons and encouraged the participation of oral surgeons (as they were then called) in cleft rehabilitation. He started the first post graduate course in oral surgery in the early 1960s; the first generation of oral surgeons in India were mostly his students.
The early oral surgeons were united under a common banner with the formation of the Association of Oral Surgeons of India in 1969. The founding group included the late Mino Ginwalla, C. Dhanasekharan, C. Raju, K. Ramachandran, S. Khera and A. Chitre. Almost all of them had a dental background. Even today oral and maxillofacial surgery is a specialization of dentistry and 95 percent of all maxillofacial surgeons only have a dental qualification.
The association was formally affiliated to the IAOMS in 1977 at the Sydney ICOMS when a few of the members attended the International Congress. By the mid-1970s postgraduate programs were started in most of the main dental colleges including GDC Mumbai, Madras (Chennai), Bangalore, Trivandrum, Hyderabad, Calcutta (Kolkota), Manipal, etc. The AOSI was renamed “Association of Oral and Maxillofacial Surgery (AOMSI)” in 1985.
Today, the AOMSI is a registered organization and admits qualified oral and maxillofacial surgeons as life or annual members. It currently has 1,300 members,

most of whom are lifetime members. The association is committed to the promotion of the specialty through its scientific meetings and social causes. The journal is called The Journal of Maxillofacial and Oral Surgery and is the official publication of the association. It is published four times a year from its office in Chennai (changing with the residence of the editor).
The association has two major conventions every year. The annual conference is held in November/December in pre-determined venues around the country. The mid-term conference is focused on postgraduate students and trainees and is a two-day conference held in June/July every year. In addition, the AOMSI officially participates in continuing education programs held by its members in different parts of the country.
The executive committee meets three or four times every year and is the official decision-making body. The AOMSI is officially affiliated to the IAOMS and the AAOMS (Asian Association) and has cordial relationship with all national associations.
The AOMSI has recently promoted an Independent Board to further excellence in oral and maxillofacial surgery by conducting examinations and awarding board certification. The primary collegium of senior surgeons was selected through a point system and admission to the board is through an annually conducted examination.
The 19th ICOMS was held in Bangalore and was a huge success with almost 1,600 delegates from around the world. The AOMSI held a joint conference with the British association in November 2009 at Kochi.
Kishore Nayak is serving as the IAOMS president for the period of 2012–2014. He is the first Indian to be elected to this prestigious post.
The secretariat of the association is located at the place of residence of the Hon. General Secretary of the AOMSI and is presently situated in Madurai, Tamilnadu.
George PaulIndonesia
Indonesian Association of Oral and Maxillofacial Surgeons
Persatuan Ahli Bedah Mulut dan Maksilofacial Indonesia
The Indonesian Association of Oral Surgeons was founded in 1973 after 11 oral surgeons came together in Jakarta. These pioneers were already established oral surgeons long before this date: Soedarmadi from Surabaya, Moerniyati from Jogyakarta, Soeriasoemantri, Tet Soeparwadi from Bandung, Pranoto, Subekti, Hendarmin, Eddy Aulia Fatah and Ilyas Darmawan from Jakarta and Geri Panjaitan and Lukito Handriyo from the military.
Education and training hardly existed and was based on an apprenticeship since 1971 in only one center in Bandung.
Since 1975, the military had an established training center, which only served their needs. The first national congress took place in 1975 in Jakarta.
It took some years, until 1984, before the government began to see the need for an oral surgery service and formally opened four centers for training at four universities in Surabaya, Jakarta, Bandung and Yogyakarta. In the beginning, there was no uniform training pathway for these centers but currently there is. Training is based on a dental degree but the first two years of the total of five years in training are largely devoted to medicine. The following three years are solidly spent on oral and maxillofacial surgery. The programs are still localized in the four big centers and the total number of trainees is around 120.

The programs are recognized by the Indonesian Medical and Dental Council. The College of Oral and Maxillofacial Surgery keeps an eye on the programs and is responsible for the national examinations and standardization of the curricula in each center.
At the end of the training period, they all have to pass an exit examination that consists of two parts. First, they have to write a paper, which is assessed by two examiners from the College. Second, they have to do an oral examination at which a representative of another surgical specialty is present.
During the last three years, the demand for newly trained OMF surgeons has increased tremendously because of a change in government policy. Each of the 26 provinces is now responsible for its healthcare, which implies that they have to pay for the training of the young doctors in their own district hospitals. This policy is aimed at improving the spread of manpower over this huge country with 1,000 islands and a population of 250 million. The current number of 300 OMF surgeons is mainly concentrated in the large cities, whereas in the rural areas and remote islands, hardly any OMFS service is available.
In order to raise professional standards, there is a need for international exchange and fellowships. Some but not enough colleagues did gain additional expertise in Japan, Germany, France, Scandinavia, China and several in the Netherlands but we need a lot more input from more advanced countries to raise the level of care in Indonesia. There is a large number of patients with untreated pathology and congenital deformities who badly need adequate care. There is also a need to begin to develop some research projects, as research is the basis for education. We hope to be able to do that with international collaboration.
Benny LatiefIran
No report received.
Ireland Irish Association of Oral and Maxillofacial Surgeons
The development of oral and maxillofacial surgery in Ireland has had a hesitant start and a somewhat checkered history.
Prior to the establishment of “recognized” oral surgery units in Belfast and Dublin, dentoalveolar surgery was carried out by interested dentists, while facial trauma and head and neck oncology was managed by other specialties. The first oral surgery units on the island of Ireland were established in the Royal Victoria Hospital in Belfast, Altnagelvin Hospital, Derry, Dr. Steevens’ Hospital, Dublin and the Dublin Dental Hospital in the years following the second World War.
Notable figures in those days were Roy Whitlock, John Gorman and Robert Boyd in the north and Ian Findlay, Niall Hogan, Hugh Barry and Frank Allen in Dublin.
These units catered for injuries sustained during the “troubles” of the 1970s and 1980s and the Belfast unit established an international reputation in the management of severe gunshot and bomb blast injuries.
In 1979, Frank Brady was appointed to Dr. Steeven’s Hospital in Dublin as an oral and maxillofacial surgeon, following a period of training in the United States.
In 1984, a training program was established with David Ryan being the first trainer, although he completed his senior registrar training in the United Kingdom. Cliff Beirne and Kumara Ekanayke were subsequent trainees. Following Hugh Brady’s appointment, there were no further appointments at consultant level until 1989, when David Ryan replaced Professor Ian Findlay at the Dublin Dental Hospital and the Mater Hospital.
While the units in Belfast and Derry have thrived with consultant appointments and active training units in both cities, the situation in the Republic of Ireland has
not been as fruitful due mostly to the lack of funding and leadership. The OMFS training program was withdrawn from the National Maxillofacial Unit in 2001. Currently, those interested in OMFS careers are required to train in the United Kingdom and United States.
A significant development in recent years, however, was the establishment of a chair in oral and maxillofacial surgery at Trinity College, Dublin in 2003. The current holder of that chair is Leo Stassen. He also heads up the National Maxillofacial Unit at St. James’s Hospital (formerly at Dr. Steeven’s Hospital) with fellow consultants Gerry Kearns, Padraig O’Callaigh, Kumara Ekanayeke and David Ryan. This is a developing unit, covering all aspects of maxillofacial practice, with a doubling of consultant numbers and the imminent re-establishment of a training program backed by the RCSI through its training committee.
Activity of the Irish Association of Oral and Maxillofacial Surgeons lapsed since the heady days of 1980 when the International Association visited Ireland but has resurrected itself with a new group of surgeons from both North and South, involving those who are interested in developing the specialty.
Currently there are eight oral and maxillofacial surgeons in the North of Ireland, four in Belfast and four in Derry. In the Republic of Ireland there are 10 health service appointments, five in Dublin, two in Cork, two in Limerick and one in Galway. The plan is to have 21 hospital appointed oral and maxillofacial surgeons in order to adequately cover the Irish population of 6.2 million, including Northern Ireland.
David RyanIsrael Israeli Association of Oral and Maxillofacial

Surgery
The development of the specialty in Israel began in the mid-1950s, carrying the name of “oral surgery” but as the specialty progressed, it turned into “oral and maxillofacial surgery.” The founding fathers were Jacob Lewin-Epstein, David Gutman and Yochanan Ramon.
Jacob Lewin-Epstein graduated from the Dental School at the University of Pennsylvania in 1944. He completed his postgraduate education in oral surgery at the University of Columbia in New York in 1953. At the establishment of the Faculty of Dental Medicine at the Hebrew UniversityHadassah in Jerusalem, he was appointed as the head of the department of oral surgery. He served in this capacity from 1955 to 1985. In the years 1969–1973, he served as Dean of the Faculty of Dental Medicine of the Hebrew University-Hadassah.
During Lewin-Epstein’s tenure as head of the department, he had to compete with the disciplines of plastic surgery and ENT for the privileges of the overlapping surgical procedures. The head of surgery, Zaltz, made the “verdict” that all the overlapping surgical procedures with ENT, plastic surgery and general surgery should be performed by those who have skills and most experience. As a result, maxillofacial trauma, orthognathic surgery, salivary glands pathologies, benign and malignant maxillofacial tumors were performed by the staff of OMF surgery. Lewin-Epstein looked also into further training of the younger staff at different centers outside of Israel.

Azaz spent one year in 1963 as a Fellow at Queen Victoria Hospital-East Grinstead, U.K.; Shohat spent a year as fellow at Cleveland Hospital in 1963 and Arie Shteyer spent his last year of his residency program at the University of Kentucky in 1967. Badry Azaz followed Lewin-Epstein as head of the department for the period 1985–1995 and Arie Shteyer from 1995 to 2003. Both of them also served as deans of the Faculty of Dental Medicine at the Hebrew University.
David Gutman completed his residency in oral surgery in Pittsburgh, Pennsylvania, U.S.A. in 1953. In 1955, he founded the unit of OMFS at Rambam Medical Center in Haifa as part of the department of ENT. A few years later, his department became independent, performing all kinds of surgical procedures. Gutman served in the late 1980s as dean of the Faculty of Medicine at the Technion in Haifa. The following head of the department was Dov Laufer between the years 1980 to 2001. He spent two years as a fellow with Hugo Obwegeser in Zurich in the years 1967–1969. As of 2001, Micha Peled has acted as head of the department.
Yochanan Ramon, who was also a general surgeon, founded the department of OMFS at Sheba Medical Center in the late 1950s. He was followed by Shlomo Taicher as of 1986. He completed his residency at the Hadassah Medical Center in 1976 and continued for two years as fellow at NYU in New York.


The association was established in 1964 by the aforementioned pioneers but unfortunately, the exact date is not to be traced. However, it has to be before 1965 since the Israeli association was one of the six associations that affiliated with IAOMS at the 2nd ICOS in Copenhagen in 1965.
As the specialty developed, several other centers were established throughout the country. In 1969, Andre Edlan, who was able to leave Czechoslovakia and to immigrate to Israel, opened a new unit of OMFS within the department of ENT in Beilinson Medical Center in Petach-Tikva. He was followed by Shlomo Kalderon, who completed a fellowship in Miami, Florida.

Daniel Temkin opened a unit of OMFS at Poria Medical Center, near Tiberias, in 1972, within the department of ENT as a single staff member. Temkin had his training in OMFS at Queen Victoria Hospital, East Grinstead and U.K. and completed it at Rambam Medical Center in Haifa. He was head until 2001 and was followed by Zvi Laster, who also spent two years as a fellow at Queen Victoria Hospital, East Grinstead, U.K. Amos Neder completed his residency program in 1966 at Rambam Medical Center in Haifa. Following that, he gained more experience by practicing in Africa for two years. Upon his return, he opened a unit of OMFS at the Barzilai Medical Center, Ashkelon, serving as head until 1996. He was followed by Oded Nahlieli, who has served as head from 1995 until the present time.
Itzhak Horowitz, completed his residency program at Hadassah Medical Center in Jerusalem in 1968 and did an ENT residency at Sheba Medical Center. He opened an OMFS Unit at Ichilow Medical Center in Tel Aviv, in the mid-1970s, within the department of ENT. He was followed as head of the unit by Gabriel Chausho and later by Benjamin Shlomi.
Now there are seven departments of OMFS in Israel that are accredited to provide training and education in the specialty, including, Poria Medical Center, Tiberias, Rambam Medical Center, Haifa, Beilonson Medical
Center, Petach-Tikva, Sheba Medical Center, Tel Hashomer, Ichilow Medical Center, Tel Aviv, Barzilai Medical Center, Ashkelon and Hadassah Medical Center, Jerusalem. On top of that, several small units have been established throughout the country in order to serve the whole population.
The training program of OMFS was the first in the field of dental medicine in Israel. Until the mid-1980s, the residency lasted three years. As the specialty grew, the program was extended to five years. In 1978, the Ministry of Health acknowledged specialties in other fields of dental medicine, which is controlled by the Scientific Council of the Israel Dental Association. All the residency programs are governed by this Council and controlled by the different boards, in our case the board of OMFS. The five-year program of OMFS consists of rotations in general surgery (six months), plastic surgery or otolaryngology (three months), general anesthesia (three months) and pathology (three months). The actual training in OMFS lasts 3½ years, whereas three months are reserved for research activities.
Upon completion of the program, the resident is entitled to take his final written and oral examination, controlled by the Board of Examiners in Oral & Maxillofacial Surgery. Those who pass the examinations are entitled to a specialty certificate in oral and maxillofacial surgery, which is provided by the Ministry of Health. The holders of the specialty certificate in oral and maxillofacial surgery, which is provided by the Ministry of Health. The holders of the specialty certificate may apply for membership of the Israeli Association of Oral and Maxillofacial Surgeons.
At present, the Israeli association has over 50 full members, for a population of seven million. There are 35 residents in the training programs and approximately seven residents graduate each year.
Ofer MardingerItaly
Italian Society of Maxillofacial Surgery
Società Italiana di Chirurgia Maxillo-Facciale (SICMF)

The first signs of Italian maxillofacial surgery can be traced back to the beginning of the 20th century, coinciding with World War I, when Arturo Beretta established a center for treating soldiers with facial injuries in Bologna (Beretta Institute). This task was entrusted to a general surgeon, Cesare Cavina, who gained considerable experience, using novel techniques that were particularly innovative for that time.

Among Cavina’s disciples, Giuseppe Maccaferri stood out but he left Bologna and moved to Parma University. In 1935, Natale Calabrò succeeded Cavina, continuing his work while expanding the scope of maxillofacial surgery. In 1966, Guido Stea took over the department of Calabrò, moving from the Beretta Institute to Rizzoli Hospital in 1977.

Bologna had been the center where many young surgeons, eager to enhance their experience and training in oral and maxillofacial surgery, were educated and trained and then they spread their work throughout the country. Some of them became chiefs of centers of maxillofacial surgery that gradually developed in northeastern and central Italy. Among them were Giuseppe Rossi in Venice and Camillo Curioni in Vicenza. Other schools in nonuniversity hospitals were those of Giuseppe Ferrari Parabita in Brescia, Franco Torrielli in Genua and Enrico Panzoni in Florence.
During these years, oral and maxillofacial surgery became part of the medical curriculum, mainly thanks to pioneers such as Giosué Giardino and Bernardo Roccia, from the Universities of Naples and Turin and stomatology also developed as a medical specialty in Italy.
Later on, a new generation of pioneers began to establish themselves in other Italian universities, such as Cesare Enrico Pini in Milan, and Giuseppe Maccaferri, followed by Luigi Rusconi in Parma. The next generation developed the specialty further, also thanks to experience gained in renowned foreign centers. As a result, other schools developed, such as that of Remo Modica in Turin, Paolo Gotte in Verona, Constantino Giardino in Naples, Roberto Brusati, who was first in Parma and later in Milan and, finally, Giorgio Iannetti in Rome.
Constantino Giardino created the first official training program in maxillofacial surgery at the University of Naples in 1977. His example was gradually followed by the Universities of Milan Turin, Parma, Verona and Rome. Many students of these universities would occupy new positions that were being gradually built throughout the country, following the evolution of maxillofacial surgery.
At that time, many maxillofacial surgeons had a background in stomatology, a medical specialty before dentistry was introduced as an academic study in Italy in 1980.
The enthusiasm of that period led to the birth of two scientific associations; on the one hand there was the ASCMFOI (Association of Italian Hospital Stomatologists and Maxillo-Facial Surgeons), founded in 1965 and formed by surgeons working in non-university hospitals), while the other was the AICMF (Italian Association of MaxilloFacial Surgeons), founded in 1977 and formed by academic practitioners. Both societies organized scientific and cultural events separate from each other, even though their meetings addressed the same problems and developments of maxillofacial surgery. The members of both societies, however, began to feel the lack of mutual contacts and the need for a fruitful cooperation, which would be beneficial for all maxillofacial surgeons.
As a result, during the first congress of the AICMF, held in Naples in June 1978 and during the congress of the European Association for Cranio-Maxillofacial Surgery, held in Venice during the same year when Curioni was president of the European association, Giardino, Curioni and Arlotta began to negotiate the possibility of creating a single scientific society, bringing together all Italian maxillofacial surgeons, both academic and non-academic. In the end, Modica organized the first joint congress of AICMF and ASCMFOI in Saint Vincent in 1979.
Following the joint conferences of 1983 in Gardone Riviera and of 1985 in Ancona, between 1987 and 1989, Constantino Giardino and Pio Arlotta, presidents of the two separate scientific societies, decided to prepare the bylaws of what would later become the Italian Society of Maxillofacial Surgery (SICMF).
In 1989, the sixth National Congress of Maxillofacial Surgery was organized in Genua by Enrico Righi. This actually may be considered the first official Congress of SICMF where both Arlotta and Giardino were copresidents. Since then, the SICMF organizes its national congress every other year on topics of scientific and clinical interest but also dealing with the organizational evolution of specialist training in Italy and the European Union, in collaboration with the UEMS. The SICMF also organizes two thematic and practical training courses per year that are targeted at young colleagues and trainees. At present, SICMF has 307 active members serving a population of about 60 million people.
The SICMF also promotes the publication of its official journal, the Italian Journal of Maxillofacial Surgery, which is published in English. It also published a multiauthored handbook Patologia Chirurgica Maxillo Facciale (Maxillo-Facial Surgical Pathology) in 2007, written by Italy’s leading experts. This book is a reference manual

for all those who want to study maxillofacial surgery, both at the medical schools and at the training programs.
During the past 70 years, maxillofacial surgery has grown both in scope as well as in the number of practicing surgeons. At present, there are departments of maxillofacial surgery in many general and academic hospitals throughout the country, while there are 10 post-doctoral training programs for a total of 33 to 35 new residents each year. The duration of the training is five years and includes 2,000 hours of dentistry, as agreed within the oral-maxillofacial surgery section of the UEMS. Only those who have earned a master’s degree in medicine and surgery, which takes six years, may apply.
Since the formation of the European Union in 1993 and because of the treaty of Rome, the recommendation is the promotion of freedom of movement for professionals among the European countries. Thus, there remains one hurdle for Italian OMF surgeons: in most European countries, a master’s degree in medicine and dentistry is a prerequisite for achieving a license to practice OMF surgery, of course after proper training. This precludes the free movement of Italian OMF surgeons to other European countries. The SICMF will continue to work to overcome these problems.
Paolo RonchiJapan
Japanese Society of Oral and Maxillofacial Surgeons (JSOMS)

Dentists gained legal independence from medical doctors in Japan in 1906 when the Physicians and Dentists Laws were published separately. Until then, diseases of the oral cavity had been treated by stomatologists for approximately 1,300 years since the dawn of medicine in ancient Japan. The establishment of the Faculty of Dental Science in Baltimore University in 1840 inspired Einosuke Obata to declare in 1875 that “dental science” should be independent from “medical science.” When the first qualified dentists came on the market, the old-fashioned stomatologists gradually disappeared. Soon, “oral surgery” emerged as a specialty of dentistry.
The Japanese Association of Oral Surgery was established in 1933. From the beginning, the specialty degree “oral surgery” could be achieved via either dentistry or
medicine but the great majority was via dentistry.
The history of the JSOMS has been characterized by debate regarding licensing because of major changes in the education system before and after World War II.
Before World War II, there was much debate about the scope of medical practice by dentists. But when military medical doctors became scarce during the war, dentists, who followed a condensed medical course, were sent to the battle fields. This was the origin of the double qualification in Japan.

After the war, under the rules of the government of the occupational forces, dentistry became an academic profession and the study was prolonged to six full years, the same as that of a medical university. Programs in oral surgery sprung up throughout the country in both faculties of dentistry and medicine. The JSOMS arose from its post-war dormancy in 1956 with its journal re-named as the Journal of the Society of Oral and Maxillofacial Surgery and has been vigorously active in society since then. Under the administration of the Occupational Forces, dentists were deprived of their right to write a certificate of death but five years later, that right was legally restored and continues to the present.
The specialist system of the JSOMS started in 1973. In the beginning, the JSOMS certified senior specialists and accredits training institutions. To become a senior specialist certified by the JSOMS, applicants must perform surgery as a chief surgeon in a total of at least 100 cases in the categories of dentoalveolar surgery, maxillofacial trauma surgery, orthognathic surgery, temporomandibular
joint related surgery, preprosthetic surgery, cleft lip and palate surgery, reconstructive surgery, implant surgery and surgery for cancer. The examination for the specialists has been carried out every year since 1980.
The JSOS came to participate in the activities of the IAOMS in the early 1980s and its name was changed to the Japanese Society of Oral and Maxillofacial Surgeons in 1984. The JSOMS expanded its international activities by establishing the Asian Association of Oral and Maxillofacial Surgeons in cooperation with Korea and Taiwan in 1989. The Asian Association of OMFS came to include the Thai, Philippine, Malaysian and Chinese associations.


One of the central concerns of the AAOMS was the issue of licensing. This issue was resolved in a new formulation in Durban in 2001, where the pre-training qualification was left to the agreement of the regional associations. During this period, the JSOMS had the proud honor to be the first Asian nation to host a conference of the IAOMS: the 13th ICOMS, held in Kyoto in 1997.
More recently, there have been two significant developments in the history of the JSOMS. In 2003, the JSOMS was allowed by the government to officially provide certificates for “oral surgery,” the scope of which includes the treatment of malignancies and major reconstructive surgery. The Japanese Board of Cancer Therapy was established for high level treatment of malignant tumors in all fields of medicine in Japan and in 2009 dentally based oral and maxillofacial surgeons were officially permitted to treat malignant tumors.
The current membership of the society is 9,266, including 1,755 registered specialists and 792 senior specialists who are responsible for the accredited training institutes and officially qualified to educate trainees. At present, the percentage of OMFS surgeons with both a dental and medical qualification is less than four percent. Both dentists and medical doctors, with at the least six
years of postgraduate training, can take the surgical skill test in certain surgical cases as well as oral and written examinations. They have, however, to be trained in an accredited institution. This examination is rather difficult and includes a logbook of operations performed. There are currently 248 accredited training institutions and each year about 160 trainees pass the examination.
Jinichi Fukuta
Kazakhstan, Republic of No report received.
Korea, Republic of Korean Association of Oral and Maxillofacial Surgeons
The first evidence that patients were treated for diseases of the oral and maxillofacial area stems from the year 1915. Dr. Seok-Tae, along with some others, was responsible for this. The American evangelist and dentist JL Boots and another dentist, McAnlis, began to work in the dental department of Severance Hospital in Seoul in 1921 and they also carried out oral surgery.
The first dental school was established in Korea in 1922 but it was only after World War II that oral surgery was taught at Seoul National University by Professor ChunGeon Lee and his staff. They began a Master’s course in

1952 and the first students graduated in 1956. From 1959 onwards, the dental curriculum was extended to six years.
The Korean Association of Oral Surgeons was established in June 1959. Oral surgeons from the U.S. army, such as Alling, Shira and Cooksey and some Japanese colleagues participated in scientific meetings and contributed considerably to the advancement of the specialty in Korea.

In the early 1970s, the deans of the then three dental schools met several times and set the standards for education and training of oral surgeons. The association also published a journal from 1975, which is currently published bimonthly.
The association was renamed the “Korean Association of Oral and Maxillofacial Surgeons (KAOMS)” in 1984. A committee of chair professors of departments of OMF surgery of the then 10 dental schools once again formulated guidelines for training and education of OMF surgeons in 1987. They also published a translation of the “Textbook of Oral and Maxillofacial Surgery” from Kruger into the Korean language. This book became the standard text for residents in training.
At present, the training is based on a dental degree and takes four years. Residents in training receive additional medical education and training in the first year. The whole scope of the specialty, including the treatment of malignancies and their reconstruction, much along the lines of the Guidelines of the IAOMS, is covered during the training. There are currently 48 institutions involved with the training of 71 residents.
The association has about 750 active members, spread all over the country. They serve a population of 48.5 million people. The 50th anniversary of the KAOMS was celebrated in 2009 in Seoul with a scientific congress. The KAOMS is determined to further advance and promote the specialty in Korea but also in Asia and beyond. Thanks to the vision and inspiration of the pioneers of KAOMS, the specialty has gained the current status and position.
 Kyung-Wook Kim Latvia
Kyung-Wook Kim Latvia
Latvian Association of Oral and Maxillofacial Surgery
The Latvian Association of Oral and Maxillofacial Surgery was established in 1995 by 19 stomatologists, who had different backgrounds. Most of them had acquired their training in surgical stomatology in either Moscow, St. Petersburg or Kiev. Since 2000, however, the specialization is based on a dual degree and five years of postgraduate training. This is in accordance with the recommendations of the EACMFS and implemented with the support of Rudi Fries, former president of the EACMFS and IAOMS. The first president was Andrejs Skagers.
Historically, Latvia and particularly Riga, have played an important role in the development of oral and maxillofacial surgery. Early pioneers in the 19th century were Alphonius von Szymanowski and Nikolay Pirogoff, the latter well known for his rhinoplasties.
The academic education in the specialty was introduced in 1920 when the University of Latvia was founded, including a medical school which also had an Institute of Stomatology. The department of surgical stomatology was established in 1944, with Ilja Leja as its first chairwoman. She was followed by successively Vladimir Aronson, Astra Linare, Indulis Bakulis and finally Andrejs Skagers, who has served in that position since 1978.
Currently, the Paul Stradins University in Riga provides the undergraduate and postgraduate training of OMF surgeons. The department of oral and maxillofacial surgery is responsible for this training. It also entails rotations at the Latvian Cleft Centre and the Latvian Oncology Centre. Residents also have the opportunity to rotate through centers outside Latvia such as Cardiff in Wales, Helsinki, Gothenburg, Rostock, Oslo and Lyon.
The Latvian Association has 35 active members serving a population of 2.2 million people. There are six residents in training. All members of the association are also members of the Baltic Association of Maxillofacial and Plastic surgery and some are members of the EACMFS and/or the IAOMS. The main activities of the association include certification and recertification of specialists, the latter every five years. There are regular meetings held and the association has an advisory voice both to the Latvian Medical Association and to the Ministry of Health.
 Andrejs Skagers
Andrejs Skagers
Lithuania Lithuanian Association of Maxillofacial Surgery

The Lithuanian Association was established in 1995 and Pranas Tercijonas became its first president, a position he still holds. Many of the members are also members of the Baltic Association of Plastic and Maxillofacial Surgery and the European Association for Cranio-Maxillofacial Surgery, while LAMFS became affiliated with IAOMS in 1995.

LAMFS has honorary, associate and affiliate members and candidate members; the latter category is for trainees. Full members are those who are registered maxillofacial surgeons, while oral surgeons are associate members. They have voting rights and count for 50 percent of the total membership. Affiliate members can be physicians working in the same field but who are not registered maxillofacial or oral surgeons.
Lithuania, with a population of 3.6 million, has two training centers, one at Kaunas Medical University and one at Vilnius Medical University. A dual degree is necessary to become a maxillofacial surgeon. If dentistry has been done first, he or she has to do medicine first before the training can begin, which lasts three years. If medicine is the first diploma, dentistry is included in the training period, which will then take five years. Oral surgery can be done after achieving a dental diploma and requires three years of training. There are currently 29 maxillofacial surgeons and 20 oral surgeons. Each year, four to six oral surgery trainees are accepted and two to four maxillofacial trainees.
The association is quite active with the organization of three scientific meetings a year. The board of LAMFS is supported by a council that has executive power.
Danius RazukeviciusMalaysia
Malaysian Association of Oral and Maxillofacial Surgeons (MAOMS)

The idea of forming a Malaysian association of oral surgeons began with discussions among colleagues at the Ministry of Health and the University of Malaya, Kuala Lumpur. It was deemed necessary to establish such an association so as to have a forum for discussions related to the specialty, and to promote its development and progress. The formal meeting to approve the idea was held in December 1995, although the official registration did not take place until March, 1996.

The first general assembly and scientific meeting took place in December, 1996 in Kuala Lumpur. At this meeting the constitution was drafted and later approved. At that time, some 15 members were present.
Since that first meeting, scientific meetings were held each year along with general assemblies. Speakers from the region, Europe and the U.S.A. were invited to present the newest developments in the field of oral and maxillofacial surgery. Several courses and symposia were also organized with the intention of educating our membership. A highlight was the international symposium on craniofacial distraction osteogenesis, which was held in 1998 on the island of Langkawi. Several leading international clinicians were invited and it was a huge success.
The association has currently some 120 members, the vast majority having a dental degree only but there are 11 dually-degreed colleagues and their number will increase as some are in the process of acquiring a medical degree. Training of new specialists was traditionally based on sending them overseas, notably to the U.K. This has now largely been replaced by national training centers, one at the University of Malaya in Kuala Lumpur and one at the University Sains in Kelantan.
The training is organized along the lines of a master’s degree and takes four years. Each trainee has already worked for three years as a general practitioner, as required by
the government. After that he or she can sit an entrance examination to the master’s program. This entails basic sciences, a research component and medical rotations in anesthesia, ENT and plastic surgery. The OMFS part covers the full scope of the specialty but after the master’s degree, additional training has to be done for at least six months, under supervision but can be prolonged as deemed necessary. At present, some three to four trainees finish the program each year but soon that number will increase to seven or eight.
An important event took place in 2001 when the Malaysian Journal of Oral and Maxillofacial Surgery was launched. It is the aim of the association to elevate the quality of patient care and to promote the advancement of practice and education by this publication.
Since its establishment, the association has seen a dramatic improvement in the scope of the specialty. This is well demonstrated by the microsurgery course that was presented in 2007 by Zhang Chen-Ping and his staff from Shanghai Jiao Tong University. It was particularly directed towards better reconstruction possibilities for patients with oral cancer.
The MAOMS hosted the 9th Asian Conference on Oral and Maxillofacial Surgery at the end of 2010. This was the second time that this honor was granted to the MAOMS.

As our membership gradually increased, some members became actively involved in charity work not only within the country but also overseas, notably in Cambodia, Sri Lanka and Bangladesh.
The growth and success of the association has largely been due to the initiatives, self-sacrifice and dedication of the successive executive committees headed by the presidents
Mexico
Mexican Association of Oral and Maxillofacial Surgeons Asociacion Mexicana de Cirugia Bucal y Maxilofacial

In the 1940s, orthopaedic surgeon Zimbron was the first to perform surgery on patients with facial injuries. Learning from the experience of this surgeon, two dentists, Gomez and Lugo, assisted by Lavalle, began to teach these skills at the National School of Dentistry. Early beneficiaries of this training were doctors Miranda, Obregon and Oliva. From there, Obregon took charge of the dental and dentomaxillary service at the National Medical Centre. This led to the start of a residency program with two initial trainees. Other hospitals gradually developed training programs throughout the period of 1965–1975.
The first professor and departmental head appointed at the 20th of November Hospital was Soto. He subsequently moved on to the pediatric unit at the Centro Medico Naciaonal and later to be Chief of the Hospital Service de la Raza. He appointed Tavara to develop a residency program at the 20th of November Hospital ISSSTE, where from 1966–1986, he was Chief of OMFS and Professor of the Postgraduate Course in OMFS, a position he held until 1976, when he was succeeded by Mogel (1976–2003). Romero currently holds the chair and the program director is Pacheco.
Another important figure in the development of the specialty was Vidal, who, as well as being National Coordinator of Education in Dentistry, also served as the president of the Federal District Dental Association and president of the Mexican Dental Association.
This was a time of development of various training programs, notable amongst them being the one led by Torres in the Hospital Juarez. Here, despite only having a dental qualification, he was involved in teaching residents of orthopaedics and trauma about the management of facial injuries, as well as being responsible for the treatment of these cases.
Torres, without the advantage of modern means of communication, achieved a very significant advance in the management of maxillofacial injuries in Mexico. He created a renowned school both for his own trainees but also for all the programs in Mexico. He was a pioneer in the publication of modern techniques and wrote more than 50 articles. He was the pillar of union of all departments and responsible for the formation of the Council of the Mexican Association of OMFS.
Several new training programs were established at this time and in 1996, an agreement was signed between the three institutions to ensure that henceforth, these institutional programs would carry the recognition of the Universidad Nacional Autonoma de Mexico. This agreement was signed by the authorities of each of the Institutions and also by the government of the university. Rodriguez was appointed as the general coordinator of the training programs.
Orthognathic surgery was started at the National Medical Centre by Palomera and Fujikami. This was expanded to the creation of a cleft center with the appointment of Padilla.
Throughout this period of development of the specialty in Mexico, significant use was made of overseas speakers during annual national congresses, with many of the notable world authorities contributing. Most importantly, from 1989 onwards, a close integration with the Spanish society developed, which enabled teaching programs and workshops to be held; accomplishments which not only


have greatly enhanced training, they also linked them with the outside world and all in the shared language of Spanish.

In 1994, an important change of status occurred when, after many years of the association being based within the capital of Mexico City, the association’s name and operating mode were changed to that of a national association under the presidency of Valenzuela. This meant that both the Chairman and Board members could come from anywhere in the country. In 2002, under the administration of Garcia, the name was changed from association to college and regulations were implemented which still stand.
A further link of importance was established when Garcia was president and Pino Ferreria president of the IAOMS. Garcia was also prominent within Mexico as head of department at the Medical Specialties Centre of the Government of Veracruz, which included the State cleft lip and palate service.
The association maintained partnerships for regulation and standards in compliance with the General Secretary Professions and consequently achieved the Federal Government’s recognition of the Mexican College of Oral and Maxillofacial Surgery, officially representing the entire professional guild. Additionally, there is a Mexican Council of OMFS, which is a civil partnership whose function is to improve the teaching practice in Mexico. Its main purpose for our specialty is to certify foreigners who wish to practice in Mexico. The association has, thus, gained recognition for the specialty at the highest possible level within Mexico.
Cesar VillalpandoMoldova, Republic of No report received.
Mongolia
Mongolian Association of Oral and Maxillofacial Surgeons

Oral and maxillofacial surgery was first recognized as a medical specialty and approved by the Minister of Health, on August 24th, 1971. The first oral and maxillofacial surgery department was officially opened in the Central Hospital in the capital, Ulaanbaatar. Since that time the specialty has evolved and great advances have been made in the last 28 years.
The pioneers of Mongolian OMF Surgery are doctors Selee, Tseren and Natsagdorj. They received great help from former USSR consultants doctors B. Pavlov 1962–1965, F. Saifullin 1964–1967, I. Fediyaw 1969–1971, A. Rukovishnikov 1982–1983, and K. Zamiyatin 1985–1989, who trained Mongolian colleagues.
At present, there are three major departments located in the Central Hospital, Maternal and Child research center
and Central Oncology Hospital in Ulaanbaatar. In addition, there are several private practitioners. The new generation of Mongolian oral and maxillofacial surgeons is largely trained in Korea, Japan, Russia and the U.S.A.
In 1998, the Mongolian Association was established with a clear mission statement. The first president was Natsagdorj and first general secretary Dolgorsuren. Since 2009, Khentii is the president of MAOMS and Gantumur the general secretary.
Mongolia is a vast country that is sparsely populated (approximately 3 million). The majority of the people live in the capital and only about 1 million live in the rural areas. That is the reason why OMF surgery is concentrated in Ulaanbaatar.
Currently, the training and education is based on a dental degree. Candidates have to sit an entrance examination and must have two years of practical dental experience. There is only one training center located in Ulaanbaatar. The training period is one year but preparations are underway to expand this period.
In 2009, MAOMS was officially affiliated with IAOMS and sent delegates of MAOMS to international and regional congresses. MAOMS organized its first national congress in October 2009, discussing its future.
The MAOMS is determined to maintain the high standards of oral and maxillofacial surgery in Mongolia and to support the training of our members abroad.
Gantumur Tsegmed
The Netherlands
Dutch Association of Oral and Maxillofacial Surgery Nederlandse Vereniging voor Mondziekten, Kaak-en Aangezichtschirurgie (NVMKA)
The development of the specialty began relatively late in the Netherlands. That had largely to do with the fact that the Netherlands was not involved in World War I and, thus, there was no need for the care of wounded soldiers as in most other European countries. World War I gave
an enormous impetus to the specialty, in that there was a great need for treatment of soldiers with facial gunshot wounds, including fractures of the maxillofacial skeleton.
In this context, it is of interest that the pioneer of Dutch oral and maxillofacial surgery was Johannes Esser, who had a medical degree from the University of Leiden and a degree in dentistry from Utrecht Dental School. He trained in general surgery in Utrecht and followed a course in “war surgery” in Paris in 1914. He offered his service to France and England but was turned down by both countries, which was reason for him to turn to the Austro-Hungarian monarchy, where he was accepted as an army surgeon.

Esser became a well-known and much respected maxillofacial surgeon, who developed pedicled flaps, based on feeding arteries, to cover defects in the face. This way he was able to treat large defects in the face with, for those days, exceptional good results. He deserved an honorary doctorate at the University of Berlin because of his groundbreaking work in the field of reconstructive surgery. After the war he established a surgical practice in Berlin but the economic downturn forced him to return to the
Netherlands. Despite his widely known reputation, he did not succeed in finding a suitable job in the surgical world. He finally emigrated to the U.S.A. in 1940, where he lost all his money and died in 1946 as a poor and forgotten man.
The first head of a department of oral surgery and diseases as it was called in those days was H. de Groot, an ENT surgeon. He passed away at a relatively young age and was followed by Jeramiah Tjebbes, who was appointed an associate professor in 1932. He had training in general surgery and was educated in dentistry at the school in Utrecht. It was his responsibility to teach dental students at the only dental school in the Netherlands at that time.
The further development of the specialty was severely hampered by the German occupation. Tjebbes worked under the most difficult circumstances with a minimum of staff. Dental students were not allowed to study anymore and the university hospital was hardly operational during the last years of the war. Yet, Tjebbes had established himself very well and became an expert in cleft-lip and palate surgery. Immediately after the war, he was appointed full professor and became head of a department of oral and maxillofacial surgery. He would chair this department until 1973.
The person who would be instrumental in the establishment of the Dutch association was Martin Hut. He was a dentist with an affinity to oral surgery and worked in the general surgery department of the University of Groningen. During the war he and a group of influential dentists had prepared a memorandum for the post-war Dutch government that suggested giving dentistry an academic status. The recommendations of this group were accepted and in 1947, the law was changed so as to make dentistry an academic profession. This also had an enormous impact on the scope of dentistry, which from then on also included oral surgery in its broadest sense.

Hut began a department of oral surgery at the University of Groningen, which had also acquired a new school of dentistry, to combat the dramatic shortage of dentists that existed after the war. He also began a training program in oral surgery. From the beginning of his activities, there were frictions with stomatologists, who at that time were medical specialists. Their register had been closed, however, by the Dutch Medical Association, because of the new dental specialty. The Dutch Medical Association tried to bring together the two pioneers with a different background, Tjebbes and Hut, but that initiative failed for unknown reasons. Hut, frustrated by the battles he had to fight, established the Dutch Association of Oral Surgery in 1956 and became its first president.
From the beginning the association fared well, despite the fact that its members came from different schools. Its membership grew within a few years from a handful to more

than 50 full members. The training capacity was expanded along with the opening of three more dental schools in Nijmegen (1959) and two in Amsterdam (1960 and 1968). This caused an enormous increase in the number of dentists but also an increased demand for specialists. The Dutch population after the war also doubled in a matter of 40 years, which explains, in part, the growing needs. The increased motorized traffic and the demand for elective surgery, for instance preprosthetic and orthognathic surgery, also contributed to the fast growing demand for OMF surgeons.
In the early 1970s, some members of the association began to worry about the pressure from some medical, neighboring specialists, who tried to limit our activities to the oral cavity. At about the same time, the UEMS section on stomatology and oral and maxillofacial surgery began its meetings in Brussels to try to harmonize the education and training in the different European countries. It soon became clear that Dutch colleagues would become isolated if they would not adopt the mainstream European training pathway, which required a medical and a dental degree.
In the meantime several oral surgeons, as they were called until 1986, had begun their medical studies and indeed received medical degrees. With the arrival of Peter Egyedi and later Hans Peter Freihofer, the departments in Utrecht and Nijmegen pushed for a “double degree.” This course of events made the time ripe for a fundamental change in the education and training of oral and maxillofacial surgeons in the Netherlands. The “Guidelines,” as formulated by the IAOMS in 1992, were instrumental in receiving official permission from the Dutch government to require a medical and dental degree before one could be registered as a specialist oral and maxillofacial surgeon. Officially this became effective in 2000, but most trainees had already done their medical and dental studies before that time.
At present, the Dutch association has more than 200 full members, for a population of 16.6 million. There are eight university departments with training capacity, whereas eight general hospitals are also involved in the training of approximately 12 residents each year. The official training period is four years and follows a rather strict protocol. In general the programs follow a stepwise learning curve, covering all aspects of the profession. The trainees keep a logbook that needs to meet the minimum demands as laid down in a document produced by the association.
In the first year a surgical examination, organized by the Dutch College of Surgeons, needs to be taken, which is required for all surgical specialties. The training can only be continued when the trainee passes this examination. In the following three years they have to follow two-day
courses, twice a year, which deal with special topics. These courses are organized nationwide and are followed by examinations that also need to be successfully completed. There is no exit examination but the European board examinations are highly recommended if one wants to make an academic career.
When the trainee wants to incorporate oncology in his or her armamentarium, another two years will be required. Oncology of the oro-facial area is limited to the eight university hospitals and some of the large regional hospitals. The surgeons who carry out the surgery need to be recognized as oncologic surgeons.
In general, the Dutch association is fairly active in that scientific meetings are held twice a year, while every five years this is done in conjunction with associations of neighboring countries. The universities are not only the principal institutions responsible for training but are also supposed to encourage research. This is often done either before training has begun but may also be done afterwards. The Dutch colleagues have contributed substantially to research in various areas of OMF surgery, particularly in the last 25 years.
The association became affiliated with the IAOMS from the early beginning and went “vertical” in 1998. There were two Dutch presidents of IAOMS; Bill van der Kwast (1977–1980) and Paul Stoelinga (2001–2003), whereas Geert Boering and Isaac van der Waal have been long-term councilors of the Dutch association to the IAOMS.
Membership in the European Association for CranioMaxillofacial Surgery is also encouraged.
Paul StoelingaNigeria Nigerian Association of Oral and Maxillofacial Surgeons

In the period before independence there was hardly any specialization in medicine or dentistry. Things changed for the better with the founding of the University of Ibadan (UCH) in 1948. It started as an affiliated College of the University of London. With the establishment of UCH, many medical experts were deployed from the U.K. to Nigeria. One of the lecturers in surgery was Horatious Oritsejolomi Thomas, a Nigerian, who showed a keen interest in maxillofacial surgery and operated on cases coming from all parts of the country at UCH, between 1952 and 1962. Thomas moved to Lagos in 1962 and became the founding Dean of the College of Medicine of the University of Lagos, where he was largely responsible for maxillofacial surgery.
The first appointment of a trained maxillofacial surgeon was that of Akinosi, as a lecturer in surgery and a
consultant maxillofacial surgeon at the UCH in 1966. He established a maxillofacial unit in Ibadan, which became well known all over the country.
When the civil war broke out in 1968, the Federal Government of Nigeria, in response to the large numbers of casualties with hideous facial and jaw injuries, established an emergency maxillofacial surgery unit in the Military Hospital in Kaduna. This unit was set up by a tripartite arrangement of the Ministry of Overseas Development of Britain, the Royal Air Force and the Nigerian Armed Forces Medical Services. It was later ceded to Ahmadu Bello University. Experts were recruited from the U.K. and they came for short periods. Among the experts were: Terence Ward, Michael Awty and Peter Banks. Adekeye was the Nigerian counterpart for this program. By the end of the war, he continued to carry out maxillofacial surgery and trained many maxillofacial surgeons in this center.
Since 1962, several dental schools have been established and this has resulted in increased possibilities for the training of oral and maxillofacial surgeons. Today, training of OMF surgeons is available in nine teaching hospitals in the country. The training takes at least six years and begins with one-and-a-half years of basic medical science. This is followed by a primary examination by one of the two colleges. The candidate then has to rotate through departments of medicine, surgery, anesthesia, ENT and the emergency department for a period of one and half years. He or she then has to pass part one of the college examination, which consists of written, clinical and oral parts.
The actual OMF surgery training takes three years and covers the full scope of the specialty. This is concluded by part two of the college examination. There are two colleges involved, one is the West African College of Surgeons, and the other is the National Postgraduate Medical College of Nigeria. The candidate may choose the college he or she prefers. Both certificates are recognized by the health authorities. The number of trainees depends on the capacity
of the training institution and is not consistent. At present, there are some 30 residents in various stages of training.
After a series of meetings and consultations, spearheaded by Arotiba, the Nigerian Association of Oral and Maxillofacial Surgeons (NAOMS) was formed in Lagos at the School of Dental Sciences, College of Medicine, University of Lagos on October 31, 1993. Election of the executive officers, amendment and ratification of the constitution were conducted in Ibadan on April 16, 1994. There were, at that time, about 40 members. Today, we have 75 members serving a population of approximately 100 million people. In 1995, the NAOMFS became affiliated with the IAOMS.
The activities of the association were curtailed by lack of funds in the turbulent political years of 1993–1998.The inaugural conference and the first scientific conference was held at the Lagos University Teaching Hospital in 2004. Since then, the scientific conference is held biannually. The association hosted the third conference of the African Association of Oral and Maxillofacial Surgeons in Abuja, in 2008. The immediate past president of the IAOMS, Nabil Samman, Paul Stoelinga and other international speakers were in attendance. Since becoming affiliated, the NAOMS has always been well represented at IAOMS conferences. Gwenba
 Ogunlewe
Ogunlewe
Norway Norwegian Association of Oral and Maxillofacial Surgeons
The Norwegian situation is rather complicated since there is a medical and a dental specialty dealing with the same field. There are, of course, historical reasons for this that date back to the beginning of the 20th century. A pioneer of Norwegian OMF surgery is Sophus Lossius, who had an American dental degree and a Norwegian medical degree. He initiated a medical specialty called “dental and maxillofacial surgery,” later called “maxillofacial surgery and oral diseases.” The Norwegian Dental Association, in 1952, decided to recognize two dental specialties, including
dental surgery and orthodontics. Sophus Lossius opposed this move despite the fact that he was the first chairman of the department of maxillofacial surgery at Ullevål University Hospital until 1949 and professor at the dental school in Oslo until 1961.


A second dental school was opened in 1962 in Bergen and a third one in Tromsø in 2004. At these dental schools, departments of dental and oral surgery were also established.
Many Norwegian specialists, both single- and double-qualified, have had part of their training abroad, particularly in the U.S.A. and the U.K. There has also been a lot of interaction with the other Scandinavian countries, while the Scandinavian Association has had connections and combined meetings with the British, Dutch and German associations.
The teaching, training and supervision of dentally based specialists are confined to the three university departments but obligatory hospital experience of at least one year is required. This implies that the three university hospitals with OMFS departments (two in Oslo and one in Bergen) are responsible for this part of the training. These departments are often led by medical specialists. In the past, several chairmen of the OMFS departments at the university hospitals were also chair professors at the dental schools. That facilitated the rotations in the hospitals for the trainees with a dental degree.
In Bergen, formal arrangements were made in 1973 to secure these hospital rotations. The actual training consists of a five-year, full-time program, including medical education, which also entails rotations through departments of ENT, plastic surgery, general surgery and anesthesiology. Certification will be granted after final examination and a written paper.
Training and education for the medical specialty “maxillofacial surgery and oral diseases” is only available in Oslo at Ullevål Hospital. It includes a four-year program at a department of maxillofacial surgery and two years of rotations through ENT, plastic surgery and neurosurgery. A dental degree is no longer mandatory but will be recognized for a maximum of one year in each part of the training.
At present, some 10 departments of OMF surgery exist in so-called county hospitals. Cities like Ålesund, Arendal, Molde, Bodø and Stavanger now have this service.
The foundation of the current association is largely thanks to Olaf Grythe, who was a member of the committee that decided on the two dental specialties in 1952. He was the first president of the association that at that time only had four members. The name change from dental surgery to oral surgery took place in 1970 and to oral surgery and oral medicine in 1997. Presently, the association has 60 active members and 17 trainee members. The Norwegian Association of Maxillofacial Surgeons has 12 ordinary members; some of them are member of both associations. All together, they serve a population of 4.6 million Like anywhere else, the scope of the specialty has expanded, which in part explains the need for more specialists. Single-qualified colleagues in hospitals often work together with colleagues from ENT, plastic surgery, neurosurgery and orthodontics in cases of cancer surgery, trauma, reconstructions or treatment of cleft lip and palate. A special topic in Norway is auto-transplantation of teeth, which has a long tradition Since the 1960s, about 1,500 tooth transplantations have been carried out in Oslo.

Despite its relative small size, the association is fairly active and holds yearly meetings. This comes on top of the yearly Scandinavian meeting that also attracts many Norwegian participants.
Arne Groenningsaeter
Pakistan Pakistan Association of Oral and Maxillofacial Surgeons
The Pakistan Association of Oral & Maxillofacial Surgeons (PAOMS) was founded in Karachi in 1994 by four OMF surgeons: Ajaz Aqeel, Mervyn Hosein, Mahmood Haider and Mansur Ahmed. Today, its membership is still limited to approximately 70 members. The association has been affiliated with the IAOMS since 2003.

The specialty of OMFS is typically dentally based in Pakistan. Specialist training consists of a structured four-year program followed by a fellowship examination. Some universities in the country also offer MDS and MSc courses in oral surgery.
With a population of 160 million, Pakistan is a large country with a dentist-to-population ratio of 1:26,000. There are plenty of patients with oral diseases, trauma, jaw pathologies, developmental defects and infections to be dealt with by the profession.
The specialty only took off in the early 1990s and most of the practicing surgeons are foreign trained, however, there is a new breed of specialists that are trained in Pakistan and their numbers are rapidly increasing. Overall, there are four training centers offering a residency in OMF surgery at various institutions. At present, the overall number of trainees may not have reached more than a couple of hundred but the quality of training is of a certain standard.
The PAOMS is entrusted to promote the cause of the specialty through its role in training, research and development of the profession and to protect the interests of its members. Seeking to broaden its membership base, PAOMS is also trying to promote itself on the international stage and affiliation with the IAOMS was our first step in that direction.
The first and second annual meetings were held in Karachi in 2003 and 2004. These were well organized and attended events but subsequent meetings have not been held apart from local meetings. The PAOMS, however, plans to develop a larger membership base, arrange regular annual events and regional meetings and to have a website. We would also like to have more representation in national, regional and international platforms.

We are happy to be part of the bigger picture and hope to learn and contribute to the development of the specialty on a global basis.
Mahmood HaiderPanamanian Society of Oral and Maxillofacial Surgeons
No report received.
Paraguay
Paraguayan Association of Oral and Maxillofacial Surgeons Sociedad Paraguaya de Cirugia Buco Maxilofacial


Oral surgery in Paraguay began earlier than 1958 but the first records regarding oral surgery are from this year, specifically from June 13, when the local Circle of Paraguay Dentists founded the Paraguayan Society of Oral Surgery, whose initials were SOPAC, as a subsidiary of the local Circle of Paraguay Dentists. The foundation charter was signed by doctors Guido Ciotti, Victor Boettner, Anthony Solomon, Norman Zavala, Fernando Gonzalez, Nicolas Pangrazio, Reinaldo Mayans, Miguel Barreiro, Juan Rios, Bittar Carin Ruben Ditore, Victor R. Vera V., Bianchi and Pierpont Insfran Homer.
Days later, the first board of directors was assembled with Pierpont Insfran (1958) installed as president and reelected in 1962. During his tenure, training sessions, institutional initiatives and scientific relations were all instituted with other countries. Insfran was succeeded as president of SOPAC by Artemio Salerno Netto in 1966.
In 1967, the society was partially renewed under the vice presidency of Reinaldo Mayans, when the association changed its name to the Paraguayan Society of Oral Surgery, SOPACIBU. In January 1968, a note from the Latin American Association of Oral Surgery mentions the draft of statutes by the society with the appointment of Caesar Franco and Antonio Nicolas Pangrazio as the authors. No further meetings took place until 1969.
In May 1968, Enrique Müller invited local oral surgeons to a five-day didactic and practical course. It was the first course of its kind in the area and it was duly recorded at the local Circle of Dentists in Paraguay along with the installation of the first dental team.
In 1969, Artemio Salerno Netto was again elected president.
From the aforementioned dates, a continued relationship with the Latin American Association of Oral Surgery was verified.
In 1973, Guido Ciotti, president of SOPACIBU, appointed Antonio Nicolas Pangrazio as the representative of the Paraguayan Society of Oral Surgery to ALACIBU. Months later, Pangrazio distinguished himself through his participation in the ALACIBU Congress. At that time, preparations were being made to integrate the words, “maxillofacial and traumatology” into the name of the specialty.

In 1975, President Guido Ciotti reported that ALACIBU appointed SOPACIBU as a member of the Arbitrator Tribunal, which included Venezuela and Mexico.
In 1976, Nicholas Pangrazio assumed the presidency. The minutes for this period reflect the significant scientific activities going on, including the number of oral and maxillofacial surgeons from Paraguay who completed their training abroad in countries like Argentina and France. During this time, Enrique Müller of Argentina, a former ALACIBU president, was appointed an honorary member of the society for his continued contributions and support of the specialty in Paraguay.
In 1979, Pierpont Infran is elected president at a time when many society members become more involved in both national and international scientific courses and congresses.
Victor Raul Vera Verci was elected president in 1981 of the now named Paraguayan Society of Oral & Maxillofacial Surgery. Vera Vierci, who had already distinguished himself
Auxilios Hospital, laid down the foundation for what is now the surgical service of oral and maxillofacial traumatology in the Medical Emergency Center, under the Ministry of Public Health and Welfare.
From 1988 to 1998, Ezequiel Gomez Ocampo served as the society’s president, overseeing the very successful Cono Sur Americano Congress in Paraguay.
From 2006 until the present day, Carlos Mallorquín has served as president, focusing on drafting the statutes of the specialty, with daily practice parameters, as well as conforming to applicable national laws. The society also voted through the name of the Paraguayan Society of Oral Surgery and Oral and Maxillofacial Traumatology. Under Mallorquin’s direction, in 2009 and 2010, several very successful educational extension courses in oral and maxillofacial surgery, sponsored by the IAOMS and endorsed by ALACIBU took place, featuring educators from around the world.
Carlos Mallorquin BueyPeople’s Republic of China Chinese Society of Oral and Maxillofacial Surgery
The Chinese Society of Oral and Maxillofacial Surgery (CSOMFS) was established in December 1986 at the initiation of Qiu-Wei Liu. Before that time there was a professional group of oral and maxillofacial surgeons who were part of the stomatology branch of the Chinese Medical Association. The first Chinese national congress was held in 1981 in Hang-Zhou. From the beginnings of the association and, in fact, also before that time, the Chinese colleagues have maintained a cordial relationship. The structure of its organization evolved as its membership grew.

At present, the CSOMFS has approximately 1,000 members and has a permanent office in Shanghai, with one executive vice-president and two secretaries dealing with the daily affairs under the guidance of the board of the CSOMFS led by the president. There are also several regional societies of oral and maxillofacial surgery in this vast country. The society has six special interest groups including, oro-maxillofacial and head and neck oncology, orthognathic surgery, salivary gland diseases, traumatology, cleft lip and palate and vascular malformations. Each of these groups (divisions) has about 30 members with one chairman and four vice chairmen.
The society is responsible for the continuing education of its members and organizes, therefore, several hands-on training courses. It has published the official journal called China Journal of Oral and Maxillofacial Surgery since 2002. Each member of the society receives a copy of this journal.

The scope of oral and maxillofacial surgery has evolved over the years from mainly oral surgery to all branches of the specialty as described in the “Guidelines” of the IAOMS. It is particularly oncology and reconstructive surgery in all its facets that deserves a lot of attention not only from the specialty but also, among other topics, from orthognathic surgery, implants, cleft lip and palate, trauma, TMJ disorders, salivary gland diseases and the new developments such as distraction osteogenesis, minimally invasive and navigation surgery.
A prerequisite for training in OMF surgery is a stomatology degree. There are about 30 schools of stomatology in China. The curriculum includes two years of basic sciences, one year of pure medical science and two years of dentistry. After a successful final examination, the student will be a bachelor in stomatology. Some of the key schools have a combined bachelor/master program,
It covers the full scope of OMF surgery, including oncology and cleft lip and palate. The resident has to keep a logbook with all procedures done in order to meet minimum requirements. A final written exit examination is required and also the candidate’s technical skills are assessed. When successfully passed, he or she will be a registered specialist. There are approximately 100 new residents accepted per year, divided among the 30 schools of stomatology.
The CSOMFS organizes a national congress every three years. It also has written training guidelines for the education and training of specialists, while consensus documents on diagnosis and treatment of various diseases and conditions were produced as well. Both documents were published in the Chinese Journal in 2006.


In 1999 the CSOMS joined IAOMS at the ICOMS in Washington DC. It had the privilege to organize the 19th ICOMS in Shanghai in association with the Hong

Peru
Peruvian Association of Oral and Maxillofacial Surgeons

Asociación Peruana de Cirugia Bucal y Maxilofacial (ASPECIBUM)
As in many other countries, it was the military which saw the need for oral surgery and they established the first service at the end of the 1940s in Peru. The department was headed by a dentist with a special interest in surgery and was located in the old San Bartolome Hospital in Lima.
It is, however, Felipe Plaza, who can be considered the pioneer of Peruvian oral and maxillofacial surgery. He was a dually qualified surgeon who was appointed in the 1960s, as a professor in oral surgery at San Marcos University. He was a very much respected colleague, who became president of the National Academy of Surgeons in the period 1994–1996.
A further boost to the development of the specialty came from some colleagues who trained abroad in Argentina, United States, Great Britain and Germany. Persons to mention include Yoel, who trained several colleagues at the Hospital Rawson in Argentina. After training overseas, doctors Guillermo Velezmoro, Adolfo Merino, Guillermo Cuadros, Segudo Hidalgo and Gilmer Rubio returned to Peru and began to develop the specialty of oral and maxillofacial surgery. It is of interest to note that the first bilateral sagittal split osteotomy in Peru was performed by Hidalgo in 1974.

In the 1960s, the specialty had difficulties in gaining access to the operating theaters as neighboring specialties tried to prevent them. Thanks to Apolinar Trevejo, the groundwork was done to change that. He was also a duallydegreed surgeon and could not be refused the right to operate upon his patients in a hospital. Another pivotal moment was the arrival of Carlos Abugattas Heredia in 1982, who had been trained in New York and who began to teach at Cayetano Heredia University in Lima. This evolved into the first formal training program in 1990, with doctors Delgado, Rojas and Trevejo in charge.
The second training program is located at San Marcos University, also in Lima and has been under the leadership of Hosting Barria since 1994. Both programs run a four-year residency program. The content differs somewhat between both centers as at Cayetano Heredia University, the medical rotations are limited to one year, whereas at San Marcos, they amount to almost two years. Both programs offer a broad scope of practice but are not involved in oncological surgery, although the residents do go through a rotation in head and neck oncology. The programs together graduate five to seven trainees per year. Since 2005, the specialty has earned official recognition from the national health authorities.
A tremendous jump in the development of the specialty resulted from the IAOMS supported educational course in Lima, as initiated by José Ferreria, who was president of IAOMS at that time. The program was run with the help of Eduardo Rey, as representative from ALACIBU and Samuel Allen as the local liaison. This three year course with several modules was a huge success and attended by many colleagues from the whole of Latin America. It definitely improved the level of the specialty in Peru but also elsewhere in South America.
The Peruvian association was established in 1976 with Oscar Lopez Zapata as its first president. Despite an enthusiastic beginning, this association was essentially dormant for several years. Only in 1997, when a group of colleagues formed a new association with Segundo Hidalgo as its president, did it become active again. In 1999 another group formed a second association with Freddy Gutierrez as president. The two associations, after many discussions, decided in 2010 to merge, recognizing that this would be in the interest of everybody involved. The new association has about 70 active members serving a population of 29.5 million people.

Both associations were affiliated with IAOMS in 2003 but the councilors rotated. This is no longer the case since the merger became effective. The current president of the association is Queneth del Aguila.
Samuel Allen
The Philippines College of Philippine Oral and Maxillofacial Surgeons


Doctors Ocampo Arenas de los Reyes and Nazareno were the pioneers who led the efforts to establish the Philippine College of Oral Surgeons, as it was called in the early days. Since no formal training existed in the Philippines, candidates for fellowship had to prove that they had followed postgraduate courses abroad. The constitution was finally approved in 1960 and the inaugural meeting was held in December 1960. There were 15 fellows accepted at that time.
In 1977, during its 17th anniversary, the presidential badge was introduced by then president Hilario. In the same year the PCOS was accepted as an affiliated association to the IAOMS. The association was honored by repeated visits from IAOMS presidents Bill van der Kwast and Geoffrey Howe in the following years.
In 1987, the name change into oral and maxillofacial surgery took place and a qualifying examination was introduced for those who wanted to be accepted as fellows, including a written examination and case presentations. An important event in the same year was the establishment of the Asian Association of Oral and Maxillofacial Surgeons. Its first meeting was held in Manila and not only attracted Asian participants but also surgeons from the U.S.A. and Europe. The revenues of this meeting were used to establish a Philippine Foundation, which would allow for assistance in the training of residents and rendering free service for underprivileged people, provided they were referred by members of the Philippine Dental Association. The close cooperation between the Asian associations opened pathways for the Philippine association to boost their expertise in that fellowships to renowned centers in neighboring countries became available. This resulted, for instance, in a sisterhood agreement with the Republic of China Association of Taiwan in 1990.
In 1997, Rudi Fries came to our national meeting as a guest speaker but also as president of the IAOMS.
The formal training in OMF surgery was established in 2004. There is presently only one center, located in
Quezon City that takes one resident per year. Following the “Guidelines,” as formulated by the Asian association, the training consists of a four-year program, including rotations in the department of medicine. Senior residents spend six months at the Taichung Veterans Hospital in Taiwan thanks to the generosity of Daniel Wong and Chan Man Yee.
The PCOMS, with currently 40 full members, organizes yearly national meetings and seminars for continuing education of their members but also for general practitioners. It also plays an important role in the Philippine Dental Association as an affiliate association.
Mario EsquilloPoland
Polish Association for Oral and Maxillofacial Surgery Polskie Towarzystwo Chirurgii Jamy Ustnej i Chirurgii Szcz ę kowo-Twarzowej (PTCHjU)

The Polish Association for Oral and Maxillofacial Surgery was founded in September 1997, independent from the Polish Dental Society.
The founders of the association were Leszek Kryst, from Warsaw Medical University, Stanislaw Bartkowski from Jagiellonian University, Krakow and Sylwester Kowalik, from Pomeranian Medical University in Szczecin. The Polish Association became affiliated to the IAOMS in 2005 and the EACMFS in 1997. Stefan Flieger was the first councilor for EACMFS, serving until 2002. He was followed by Leszek Kryst, serving until 2005 and Hubert Wanyura, until the present time.
Since 1997, every two years the Polish association organizes a congress and since then seven have been held, the majority of them had international input. Presidents are elected for a period of two years and the following persons have been in office: Leszek Kryst (Warsaw), Stanislaw Bartkowski (Krakow), Sylwester Kowalik (Szczecin), Zyta Grabowska (Bialystok), Tomasz Tomaszewski (Lublin), Jan

All past presidents are affiliated with medical schools in Poland and were heads of the oral and maxillofacial surgery departments.
Andrzej Wojtowicz, past president, is an oral surgeon and president of the Polish Association of Dental Implantology.
The subjects of special interest are the application of piezosurgery in orthognathic surgery; implants in relation to orthognathic surgery and fixed epiphysis, application of stem cells, growth factors and bone augmentation. These topics are also the aim of many studies and international projects.
The number of maxillofacial surgeons is about 300 and the number of oral surgeons is about 800, while there are 1,000 implantologists.
The 7th Congress of the Polish association was held in 2010. The main topics were: “Transplants in oral and maxillofacial surgery,” “Congenital defects and disorders,” “Orthognathic surgery,” “Implantology,” “Oncology and reconstruction, including microsurgery.” This congress was a great success in which important scientific results were reported.
Maciek Jakgielak and Andrzej WojtowiczPortugal
No report received. Romania
Romanian Society of Oral and Maxillofacial Surgery

The development of oral and maxillofacial surgery in Romania is very much linked to the development of dentistry. The first professional dental association was established in 1923. The first dental school was founded in 1929 in Bucharest, at Coltea Hospital, with Mina Minovici as the first director. This institution played an important role in the evolution of oral and maxillofacial surgery. Minovici was succeeded by Iacob Iacobovici, who established the first department of oral and maxillofacial surgery, chaired by Dan Theodeorescu, in 1935. In 1938, the professional dental association changed its name to: “Romanian Society of Stomatology (RSS),” with Dan Theodeorescu as president, and Iacob Iacobovici as honorary president.

During World War II, the department of OMFS moved to a new building in the Colintina Hospital, where most of the wounded military were treated. After the war, academic education in dentistry was established at the universities, beginning in Bucharest in 1949, and the
following years in Cluj-Napoca, Iasi, Timisura, Targu
In Bucharest, Valerian Popescu had taken over from Theodeorescu and it was he who pushed for the proper teaching of oral surgery for dentists. Popescu became very actively involved in international affairs despite the problems associated with the Iron Curtain. He was a member of the committee of IAMFS that issued the regulations of that organization and a vice president of that association. He also organized its congress in 1967 in Bucharest.
Of particular interest is the fact that Popescu was also one of the founding members of the European Association for Cranio-Maxillofacial Surgery, in 1972. It was thanks to him and his successors that a national network of units providing oral and maxillofacial surgical care was built up.
The Romanian Association of Oral and Maxillofacial Surgery (RAOMFS) was established in 1991, just after the regime change, with Corneliu Burlibasa as its first president. This association became affiliated with the EACMFS and with the IAOMS.
The current president is Professor Alexandru Bucur. A national congress is held once every three years.

The members of the association are both medically and dentally qualified oral and maxillofacial surgeons as well as dentally qualified oral surgeons.
At present, OMFS departments are functioning in most county capitals of Romania. There are 260 members for a population of 22 million people, 140 of them are OMF surgeons, while 120 are oral surgeons mainly doing dentoalveolar surgery. Several of them work in hospitals that are not involved in training or private practice.
The training of specialists is provided by the departments at the nine universities and takes five years. This training includes three years of compulsory medical education for dental graduates and four years of dental education for medical graduates. This is not financed by the government.
The training of oral surgeons is also the responsibility of the universities. The training lasts three years after
acquisition of the dental diploma, three months of which must be spent in a university inpatient unit.
The EACMFS, particularly anxious to offer help to the impoverished Eastern European countries, were presented with a unique opportunity to assist with a program of courses in Iasi. Working with Dan Gogaluieceaniu, the Romanian councilor for the European association, EACMFS organized and funded a three-year rolling educational program, along the lines of the Thai IAOMS project.
Very significant roles have been played in the recent developments in oral and maxillofacial surgery in Romania by the chairmen at the university departments: Alexandru Bucur in Bucharest, Grigore B ăciuţ in Cluj-Napoca, Mihai Surpăţeanu in Craiova, Carmen Vicol in Ia şi, Dezideriu Kovacs in Târgu Mureş, lecturer Marius Pop in Timi şoara, and lecturer Adrian Creangă in Constanţ a.

Alexandru Bucur
Serbia
Serbian Association of Maxillofacial Surgeons
The Serbian Association of Maxillofacial Surgeons was founded in 1965 and it became a national affiliate of IAOMS in 2011 during the 20th ICOMS in Santiago, Chile. The Association has 80 members, which includes all oral and maxillofacial surgeons in Serbia.
Saša Jovi ć
Seychelles
Maxillofacial Surgeons Association of Seychelles
The Maxillofacial Surgeons Association of Seychelles was established in 2010 and it became affiliated with the IAOMS in 2011 during the 20th IOMS in Santiago, Chile. There are currently 11 members while there are a total of 16 oral maxillofacial surgeons in the country.
Faiz Mohamed TanveerSingapore, Republic of Association of Oral and Maxillofacial Surgeons Singapore (AOMSS)
The Association of Oral and Maxillofacial Surgeons Singapore was officially established in 1991 with only 16 members and held its inaugural general meeting on the 11th of January, 1992. The pioneers instrumental in accomplishing this were N. Ravindranathan (president), Loh Fun Chee (honorary secretary), Chew Swee Chiok (honorary treasurer), Teh Luan Yook, Myra Elliott and Lewis Lee, all of whom continue to be active members and still contribute significantly to the development of OMFS in Singapore.

There are currently some 57 members in the association, serving a population of approximately 4.5 million. Between two and three residents are accepted into training positions every year.
The dental faculty at the National University of Singapore and the National Dental Centre Singapore jointly carry out training in oral and maxillofacial surgery. Selected residents undergo a rigorous three-year basic specialty training program, with rotations to anesthesia, general surgery and plastic surgery. This cumulates in a Master’s degree. They then spend an additional three years in advanced specialty training at approved local or overseas hospitals to hone their surgical skills. A logbook of all their surgical cases is kept and exposure to the various sub-specialties is a requirement. An exit interview is then conducted to assess competency before entry into the specialist register is granted. To further develop their surgical skills, the Ministry of Health sponsors one young surgeon every year to take up a fellowship in his/her area of interest, at an overseas hospital of his/her choosing, under the Health Manpower Development Program. This has proved to be very effective in broadening the scope of practice of maxillofacial surgery in Singapore, with some even venturing into facial cosmetic surgery, once an exclusive domain of plastic surgeons.
The recognition of the specialty came relatively late in Singapore and the specialist dental register was only established by the Singapore Dental Council in 2008. With the Dental Specialist Accreditation Board and the
Dental Specialist Accreditation Committee (OMS) working in tandem, a proper and formalized training framework and pathway was quickly put in place and serves as a guide for the training of all future oral and maxillofacial surgeons in Singapore.
The association meets yearly for its annual general meeting where members discuss controversial issues, plans are drawn for the new year and the new executive committee for the incoming year is elected. It also organizes educational symposia, hands-on courses and journal clubs throughout the year to facilitate continuing dental education for both its members and the general dental population. Eminent local and overseas speakers are often invited to lecture at these events. Occasional social events provide interaction amongst the members.
The association is affiliated with both the International Association of Oral and Maxillofacial Surgeons as well as the Asian Association of Oral and Maxillofacial Surgeons and members are encouraged to attend their meetings. It also has close ties with the Hong Kong Association of Oral & Maxillofacial Surgeons. An inaugural joint symposium was held in Hong Kong on January 2011, with speakers from both countries sharing their research and experiences. Following its success, henceforth, it is to be held biennially.
The association celebrated its 20th Anniversary in 2011. With this milestone, it must continue to strive to reinvent itself to meet the challenges of the new millennium. Staying relevant in this ever-changing world is the only way to ensure the continued progress of the specialty in Singapore.
Shyong
Siak GohSlovakia
Slovak Association for Oral and Maxillofacial Surgery (SAOMFS)

The SAOMFS was established in 1998 as a branch of the Slovak Medical Association. Before that time, maxillofacial and oral surgery was a “sub-branch” of the Slovak Medical Association within the Slovak Stomatological Association, similar to that of prosthodontics, restorative dentistry, orthodontics, and oral medicine. The initiators were Ivan Satko, Eugen Kurill, Dusan Poruban, Jozef Mracna, Andrej Jenca and Peter Stanko.

The current number of the SAOMFS members is 73 including 14 trainees. The president is Ivan Satko. Slovakia has a population of about five million. The education and
one in Bratislawa (Comenius University) and one in Koscice (Safarik University).
There are three pathways to becoming an officially recognized OMF surgeon. First, after acquiring a medical degree, one has to do two years dentistry followed by one year of medical rotations including, intensive care/ anesthesia (one month), general surgery/ trauma (six months), neurosurgery (two months), plastic surgery (three months), otolaryngology (two months) and oncology (one month). This is followed by three years of training in maxillofacial surgery.
Second, a person may do general surgery for three years and take a board examination and then go into training for maxillofacial surgery. He or she will still have to do two years of dentistry and three years of maxillofacial surgery.
Third, the most popular route starts from a dental degree. This person usually starts by doing two years of oral surgery and will receive a certificate that acknowledges his specialization. If they want to continue, they must do the same medical rotations and then the training of three years in maxillofacial surgery. One has to realize that dentists in Slovakia have, to a certain degree, a common curriculum with their medical colleagues. There is no special dental school, but dentistry is considered a branch of medicine.
All candidates have to sit an exit examination that includes a written paper on an assigned subject and an oral examination. They also have to keep a logbook and must have performed a given number of operations. On top of that they have to perform two operations, supervised by members of the board that is responsible for the whole exit examination.
The scope of OMFS in Slovakia covers the whole spectrum of the specialty. In summary, there are 14 residents in various stages of their training that varies from four to six years.
The SAOMFS has a close relationship and cooperation with the Czech and Polish associations. These three associations hold combined scientific symposia each year.

Slovenia
Slovenian Society for Maxillofacial and Oral Surgery Združenje za maksilofacialno in oralno kirurgijo Slovenije
The Slovenian Society for Maxillofacial and Oral Surgery in its present form was established in 1996 but the roots of the society go back to 1956. In that year, the Slovenian Section of Plastic and Maxillofacial Surgery was established as a part of the Slovenian Medical Association and it was Torol Skoog, a plastic surgeon from Uppsala, Sweden, who suggested the formation of this new section. The section was active as part of an Association of Plastic and Maxillofacial Surgery of Yugoslavia, which was also established in 1956. Bi-annual meetings were organized, each time in one of the republics of former Yugoslavia. The first president of the Yugoslavian Association of Plastic and Maxillofacial Surgery was Ivo Čupar from Zagreb.
In Slovenia, it was Jože Rant who began to perform maxillofacial surgery in 1933. After World War II, a Medical School was established as well as a Dental Clinic, which was later transferred into a Dental School. In 1949, Jože Rant passed the leadership of the division of oral and maxillofacial elešnik. At that time, the division was part of the general surgery department, chaired by Božidar Lavrič
In 1958, a new department of oral and maxillofacial surgery was established and Franc Čelešnik became the director. He had close connections with surgeons from Graz, Prague, Zurich, Paris, Dusseldorf, Lyon and Stuttgart. In 1970, the European Association for Cranio-Maxillofacial Surgery was founded in Zurich and the first Congress of the association was held in Ljubljana, under the presidency of Franc Č elešnik
Slovenia became independent in 1991 and the Slovenian Society for Maxillofacial and Oral Surgery was founded in 1996, a few years after the Society for Plastic and Maxillofacial Surgery had stopped functioning. The first president was Borut Sotošek, who also initiated the formation of the new society.
The main goals of the society today are to set the standards and to promote and maintain the high quality of oral and maxillofacial surgery in Slovenia, as well as tending to the professional interests. The society, whose activities have been increasing over the years, prepares and holds seminars and courses for specialists and for general dentists. It has also prepared informative brochures for patients and guidelines on certain procedures for the
professionals. At least two meetings per year are organized for members of the society, at which scientific and professional issues are discussed.
In Slovenia, it is possible to enter the specialty of maxillofacial surgery after obtaining a medical or dental diploma, while specialization in oral surgery can only be done by dentists. The specialist training takes six years to complete for maxillofacial surgery and four years for oral surgery. Trainees with a medical or dental degree have four years of the specialization in common, while two years are devoted to obtaining dental or medical knowledge respectively, depending on the degree with which one began.
Maxillofacial surgeons cover the whole scope of the specialty, while oral surgeons deal mostly with dentoalveolar pathology. Currently, there is only one active maxillofacial surgeon in Slovenia with a medical and dental degree. There is only one training center for maxillofacial surgery and oral surgery at the University Medical Center in Ljubljana but part of the specialization can be completed in different departments in Slovenia.
Slovenia has a population of 2 million and at present there are 17 active maxillofacial surgeons, 20 oral surgeons and 10 trainees (seven for maxillofacial surgery and three for oral surgery).
The Slovenian Society for Maxillofacial and Oral Surgery has close connections with the department of oral and maxillofacial surgery at the University Medical Center in Ljubljana, with the faculty of medicine and with members of similar societies and associations in neighboring countries. Members often meet with Croatian colleagues to exchange knowledge and ideas and also to socialize. Colleagues from other countries are often invited to our seminars to present their work.
In the future, the Slovenian Society will continue to spread knowledge by organizing seminars and courses and will also try to organize international courses on specific topics. It will try to connect with other associations in Europe and from other parts of the world.
David DovšakSouth Africa
South African Society of Oral and Maxillofacial Surgery
Maxillofacial and oral surgery was one of various branches of surgery that evolved following the outbreak of World War I but it was World War II that introduced oral surgery to South Africa when Brenthurst, the residence of Sir Ernest Oppenheimer, was placed at the disposal of soldiers for the treatment of plastic and maxillofacial and oral surgery injuries. This unit was established by

• A plastic surgeon
Major Jack Penn (a plastic surgeon) and Captain Lester Brown (a dentist).
The South African unit was based on the British pattern that recognized that a dental background was essential for the training and practice of maxillofacial and oral surgery. These units were all known as plastic maxillofacial and oral surgery units and included at least the following members:

• A dentist/maxillofacial and oral surgeon
• A n anesthetist
• A dental technician
The South African unit performed a mammoth task that was on par with work done by similar units in the United Kingdom and U.S.A. When Penn and Brown found the Rodger Anderson extra-oral splint to be ineffective for the treatment of facial fractures, they developed an entirely different splint and called it the Brenthurst-splint (after the residence Brenthurst where the unit was accommodated). These splints were manufactured to exceptionally high engineering standards by the technical division of the South African Railways and Harbors and compared favorably with global standards at that time.
When the war came to an end, both maxillofacial and oral surgery and plastic surgery were well established and by 1948, recognized as separate specialties by the South African Medical and Dental Council. The institution of a maxillofacial and oral surgery register was announced in the Government Gazette on September 9th,1950. While the scope of maxillofacial and oral surgery was being
designed, fierce disagreements arose between the plastic surgeons and the maxillofacial and oral surgeons. This continued for a number of years until a new generation of specialists saw the futility of these differences resulting in a better understanding and collegiate acceptance of the merit of each specialty.
The name “maxillofacial and oral surgery” was changed by the South African Medical and Dental Council in 1972 to “maxillofacial and oral surgery (dental)” because the former name could supposedly mislead the public! For the first decade after inception of a specialist register for maxillofacial and oral surgeons, only 10 individuals were registered, many of whom were not active.
Tribute is due to a number of people who were involved during the formation of the specialty. The brothers Lester and Jack Brown were pioneers and both worked in Johannesburg. Lester should be regarded as the founder of the profession, contributing greatly to both professional and technical aspects and who fought like a tiger to get a good dispensation for maxillofacial and oral surgery. He qualified in dentistry at Guys Hospital in London and then worked as a postgraduate with a number of British and continental European surgeons of note, before spending time in the U.S.A. and eventually, returning to South Africa in 1949, as chief of the Johannesburg group of hospitals. Honored by the Royal College of Surgeons of England, he was largely responsible for the development of maxillofacial and oral surgery in South Africa.
In Pretoria, Harry Goldin also contributed greatly to the specialty of maxillofacial and oral surgery. Chris Snijman started work as a miner on the Witwatersrand before he decided to study dentistry at the Witwatersrand University where he qualified in 1950. Two years later, he was appointed as lecturer in the department of pathology and histopathology of the oral cavity and oral surgery at the dental school of the University of Pretoria. Recognizing the need for qualified postgraduate teachers in maxillofacial and oral surgery, Chris Snijman resigned from his post and left for the United Kingdom in 1956 to attend postgraduate courses at this own expense.
After two years working in the major units in the U.K. and elsewhere in Europe, he returned to Pretoria, where the experience he had gained enabled him not only to master techniques that were up to then unknown in South Africa but also to demonstrate and introduce them to his home country. Chris Snijman was the first Afrikaans-speaking maxillofacial and oral surgeon to be registered with the South African Medical and Dental Council. When the South African Society of Maxillofacial and Oral Surgeons was established shortly thereafter, he deservedly became the first elected president.

With the establishment of the first dental school for the Cape Province at the University of Stellenbosch, Manie Breytenbach was appointed as head of the maxillofacial and oral surgery department in 1973. A year later, he was promoted to dean of the newly established dental school at the University of the Western Cape and was succeeded by Frans Grotepass at Stellenbosch, who started the training program for specialist maxillofacial and oral surgeons at this institution in 1976.

Subsequent training units were established at the University of the Western Cape (1973) and the Medical University of South Africa (MEDUNSA) near Pretoria (1986), where the first maxillofacial and oral surgeons qualified shortly afterwards under the mentorship of Lionel Miles and Bernie Jordaan respectively.
Recognizing an international trend towards dual dental and medical qualifications in the late 1980s, various training models were introduced by individual departments at the universities of the Witwatersrand, Pretoria and Stellenbosch. Since the early 1990s, dual medical and dental courses have been offered for maxillofacial and oral surgery training in a two-tier system, which runs parallel to the single dental qualification courses. Lack of political support, economic as well as practical issues make a mandatory dual degree qualification unlikely in the near future.
Since 1973, the South African College of Medicine has contributed nationally to the development and setting of standards for examination and evaluation of specialists in dentistry. A faculty of dentistry within the parent college was established during 1973 and this allowed for assessment of postgraduate students parallel to but independent of South African universities.
In 1978, the first candidate entered the FFD Part I in maxillofacial and oral surgery with success and two years later, in 1980, the college conferred the first two fellowships in maxillofacial and oral surgery. By 1995, 20 FFD(SA)MFOS fellowships had been conferred and a further 10
before a separate constituent College of Maxillofacial and Oral Surgery was established within the greater College of Medicine on 23 April 1998. This was achieved largely as a result of the efforts and vision of John Lownie, who deservedly became the first president of the new College of Maxillofacial and Oral Surgery. To date, 22 FCMFOS(SA) fellowships have been conferred.
From humble beginnings in 1964, the South African Society of Maxillofacial and Oral Surgeons has grown to a membership of about 100. The society has been affiliated to the IAOMS from the early days. To date, two South Africans have served on the executive council of the IAOMS; Pat Uys as convener of the 15th ICOMS, from 1999–2001 and Conrad Masureik as member-at-large, from 2003–2005.

In conclusion, maxillofacial and oral surgery is recognized as a specialist discipline of dentistry in South Africa, with established training centers in Johannesburg, Pretoria and Cape Town.
Albert van der Westhuizen Spain
Spanish Association of Oral and Maxillofacial Surgery
Sociedad Española de Cirugía Oral y Maxilofacial (Secom)

Dentistry was introduced in Spain in 1901. The need to expand the knowledge of undergraduate students meant that the specific studies in dentistry were modified and broadened in 1910. It was at this time that Bernardino Landete Aragó emerged as the founder of oral and maxillofacial surgery in Spain. It was he who created the stomatology concept and was responsible for this philosophy being incorporated within the dental curriculum. His tireless efforts to promote stomatology and oral and maxillofacial surgery were rewarded many years later when both were recognized as medical specialties.
During World War I, surgeons required the help of dentists to treat maxillofacial fractures. In fact, dentists with certain surgical skills were obliged, as pointed out by García Palao, “to take on more and more surgical tasks, as a result of which they developed surgical skills for treating the injured to such a point that these tasks were soon
When the Civil War ended, the dental department at the University of Madrid suffered an enormous upheaval as Florestán Aguilar had fallen from grace and died in 1934, while Bernardino Landete had been politically ousted. During this time, the dental faculty was inaugurated in the University of Madrid in 1945, while stomatology was
approved as a medical specialty, the medical-stomatology degree created and the dentistry degree eliminated.
From 1952 on, following the new Seguro Obligatorio de Enfermedades (Compulsory Health Insurance), health authorities were obliged to institutionalize the provision of a series of surgical specialties within the system. These slowly start appearing in the Instituto de Medicina, Higiene y Seguridad del Trabajador (Institute of Workers’ Medicine, Hygiene and Insurance) and gave rise to the National Centre of Surgical Specialties. The department of maxillofacial surgery was first created in 1954. Victor Sada Tejero was put in charge of the department and he was aided by José Alonso del Hoyo and Ramón Castillo Escandón y Sierra. Whereas Bernardino Landete had founded the specialty, it was Victor Sada who saw that the specialty was recognized and extended across the whole country. The transition of the existing departments of dentistry and stomatology began and maxillofacial surgery was incorporated into the surgical group. In 1956, José Alonso del Hoyo became section head and together they were able to change the name of the department to maxillofacial surgery.
Another important event in the history of the specialty took place in 1964 when the Hospital Complex La Paz, the flagship of the SOE insurance network, started operating
but with two independent departments, stomatology and maxillofacial surgery. Victor Sada was named head of the maxillofacial department in La Paz and José Alonso del Hoyo moved to become head of the Gran Hospital de la Beneficencia del Estado, which today is known as Hospital de la Princesa. From this point on, departments were created in the specialty in all the important Spanish cities.
The residents in oral and maxillofacial surgery who trained from 1966 onwards were not recognized until a Royal Decree was passed in April 1977, when oral and maxillofacial surgery was recognized as a medical specialty.
Under a law passed in 1986, which created the degree in dentistry, the roles of these different specialties were defined. Dentists would carry out prevention, diagnosis and treatment related to anomalies and diseases of the teeth mouth jaws and adjacent tissues. They would be able to prescribe medicines, prostheses and health products corresponding to the area of their professional practice. This law in no way limited the professional scope of doctors and in particular, of specialists in stomatology and maxillofacial surgery, who would continue with their normal clinical responsibilities.
The Spanish association (SECOM) was established in 1965 thanks to a group of colleagues who worked in La Paz Hospital and the Gran Hospital de la Beneficencia del Estado in Madrid. There were 26 founder members. Victor Sada Tejero was elected president and he organized the first national congress, which was held in Madrid, in 1967.

From 1966 onwards, despite still not being recognized as a specialty, the training of residents in maxillofacial surgery commenced, in order to obtain the medical stomatology degree. The training period was three years in addition to the two previous years in stomatology. The new hospitals started training residents who were chosen through interviews, which was in the hands of the committees of the hospitals themselves. The public health service depended on the Ministerio de Trabajo but

more especially on the Instituto Nacional de Prevision, that gave the residents their certificates once their training periods were completed.
As previously mentioned, the oral and maxillofacial specialty was formed as a result of a Royal Decree in 1977. This official recognition of the specialty was the result of intense negotiations by the SECOM, in particular of its first three presidents, Victor Sada, García Palao and José Alonso del Hoyo. The latter was president of the SECOM when our specialty was recognized.
In 1978, a Royal Decree was issued that signified an important change in the regulations governing the training of medical specialists. Maxillofacial surgery and stomatology were then recognized as specialties. An important fact was the disappearance of the word “oral” from the name of the specialty and it will not be until many years later, in 2003, that the specialty regained its original name.
The Royal decree of January, 1984, which regulated specialized medical training and obtaining the degree of medical specialist, gave rise to a new list of medical specialties, which included maxillofacial surgery. There are currently 31 institutions involved in the training of oral and maxillofacial surgeons
According to the rules and regulations of SECOM, which were approved in May, 2004, the society is a scientific and professional organization. Its aim is to promote oral and maxillofacial surgery nationally as well as internationally and to offer services to its members as well as to defend their interests.
Spain, with a population of about 40 million, has 735 registered OMFS and 138 trainees who are members of SECOM.
In 1974, the first international scientific event took place regarding Spanish oral and maxillofacial surgery, organized by Victor Sada, which was the 5th ICOS.
In 1978, the fifth national congress of the specialty was held, which was presided over by Alvaro García Perla. It was the first Latin American congress. The transatlantic relationship of the society with ALACIBU is still maintained. During this congress, the first issue of the Revista Ibero-Americana de Cirugía Oral y Maxillofacial (Latin-American Journal of Oral and Maxillofacial Surgery) was presented, which years later would change its name to the Revista Española de Cirugía Oral y Maxilofacial (Spanish Journal of Oral and Maxillofacial Surgery).
In 1982, José Alonso del Hoyo was named presidentelect of the European Association for Cranio-Maxillofacial Surgery, which involved hosting the 1986 European Congress in Madrid. He was the first Spaniard to hold such a high position at an international level.
In 1980 in Palma de Mallorca, Guillermo Raspall organized the sixth national congress in conjunction with
the American Association of Oral and Maxillofacial Surgeons. Guillermo Raspall was particularly keen to promote the society internationally. He was elected president of the European Association for Cranio-Maxillofacial Surgery for the period 2004 to 2006 and in 2006 he organized the 25th congress of the EACMFS in Barcelona.
Carlos Navarro Vila became chairman of the oral and maxillofacial surgery section of the UEMS between 1988 and 1994, subsequently becoming president of the European Board of Maxillofacial Surgery (EBOMFS) from 1994 to 1999. During these years, Clavero, who later took over as president of the SECOM, became president of the scientific committee of the board. Carlos Navarro was again made president of this prestigious body for the period of 2007 to 2011.
Julio Acero is currently one of the Spanish professionals with the most international influence. He is chairman of the educational committees of the EACMFS and the IAOMS.
At the 18th ICOMS held in Bangalore, Barcelona was chosen as the venue for the 21st ICOMS, to be held in 2013.
Javier Lagunas-GonzalezSri Lanka
Sri Lanka Association of Oral and Maxillofacial Surgeons (SLAOMFS)
The Sri Lanka Association of Oral and Maxillofacial Surgeons (SLAOMFS) was founded in 1998 with about six members joining and from that humble beginning it has grown into a substantial membership. Prior to the formation of SLAOMFS, all professional and academic activities related to oral and maxillofacial surgery were undertaken by an umbrella organization by the name of “College of Stomatology.” With the establishment of a Postgraduate Institute of Medicine and a diversification of training in several medical and dental specialties, the need for the foundation of SLAOMFS was felt.
A Japanese grant, to improve the training facilities in oral and maxillofacial surgery in Sri Lanka had been received around this time and this proved to be instrumental in the development of oral and maxillofacial surgery in Sri Lanka. Japanese oral and maxillofacial surgeons, who were involved in the training of local surgeons, drew our attention to the need to affiliate with the IAOMS and helped us to obtain this in 1998. Our founding president, N. A. de S. Amaratunge, attended the congress of the IAOMS that was held in Washington in 2000 and presented a paper on the prospects of our center, at the Faculty of Dental Science in Peradeniya, to develop as a training center for the region. Since then, SLAOMFS had been represented at every international congress of the IAOMS and also at regional

Asian meetings. Our members have presented papers at these meetings and participated at educational conferences.
Presently, SLAOMFS engages in training programs, scientific conferences and research activities. Sri Lanka has just entered a new era of peace, harmony and economic development. As the focus of economic development shifts towards Asia, our strategically placed country has the potential to grow into prosperity. As a result, quality of life and life expectancy should improve substantially. Oral and maxillofacial surgery likewise should expand both in scope as well as in the number of OMF surgeons needed to cope with the expected demand to improve the quality of life of the people. SLAOMFS will, thus, have a greater and more crucial role to play in the envisioned development of the health sector of Sri Lanka.

Postgraduate education and training in OMF surgery in Sri Lanka is organized along the lines of the fellowships as they exist in the U.K. Candidates with a dental degree follow a five-year course that will lead to a Master’s degree in OMF surgery. This course is being conducted by the Postgraduate institute of Medicine in Sri Lanka at the University of Colombo with the contribution of the staff of the faculty at Peradeniya and some other consultants.

The first three years of OMFS training in Sri Lanka includes about two years of training in pure medical science involving general medicine and surgery but also rotations through most other medical specialties. The OMF surgery part is mainly focused on oral diagnosis, dentoalveolar surgery, clefts and oral cancer including perioperative patient care. After the Master’s degree, two years of intensive training follows, which includes one year of training abroad. An official “Board Certification as a Specialist” is awarded after the successful completion of an exit examination. The Ministry of Health in Sri Lanka recognizes the Master’s degree qualification for the recruitment of consultants. Presently, only three to four candidates per year follow OMF surgery training.
There are five major hospitals where training facilities exist but the Dental Hospital in Peradeniya, the only dental school in the country, offers the main component of the
training. At present, there are approximately 40 qualified OMF surgeons who are members of the association and about 20 trainees in various stages of their training for a population of around 20 million people.
The Dental Faculty at Peradeniya University also offers various postgraduate courses in OMF surgery. The MSc OMF surgery course is oriented towards researchers. The courses in minor oral surgery, basic orthognathic surgery, cleft surgery, oral cancer treatment, using pedicled flaps and microvascular free flaps are designed for the practicing OMF surgeons to improve their knowledge and skills. Members of SLAOMFS are the main instructors of these courses.
Parakrama Wijekoorn
Sweden
Swedish Association of Oral and Maxillofacial Surgeons Svensk Käkkirurgisk Förening
The Swedish association was established in 1953 as a dentally based specialty. Its original name included the surgical treatment of the mouth and tooth-bearing region, which was changed in the mid-1980s to oral surgery. In the beginning of the 1990s the term “käkkirurgi,” which means “jaw surgery,” was introduced.” Pioneers of Swedish oral surgery were Åke Nordenram and Erik Jönsson. Although not an OMF surgeon, Per-Ingvar Brånemark is recognized worldwide as the “godfather” of modern implant dentistry.

During the first 23 years the association also included hospital dentists but in 1975 they separated and formed their own association. The name change came about in 1991 to “Oral and Maxillofacial Surgeons.” This name is not yet officially recognized by the Swedish National Board of Health and Welfare, in spite of diligent diplomacy by the association. If recognized by the health authorities, it would better reflect the content of the specialty.
The mission of the association is to promote education and science and the interaction of clinicians but also to
scholarships are given to young colleagues or trainees to broaden their scope in countries outside of Sweden.
The association has currently about 150 active members who are mainly hospital-based or work at the four dental schools. An increasing number are also active in private practice. About 50 percent of all colleagues have done research and received a doctorate (PhD). There are about 40 departments of oral and maxillofacial surgery, spread over the country, serving a population of approximately nine million people.
The training is provided by 16 departments that are all hospital based. Some five trainees are accepted per year. All trainees have to have two years of experience in general dentistry before they may apply. The program includes 18 months of rotations through medical departments, including anesthesia, internal medicine, ENT and surgery. There are various medical courses to be attended as well. This is followed by 30 months of training in OMF surgery. Recent discussions within the association have led to a planned change in the setup of the training program, so that it might be extended to six or seven years so as to include a medical degree but the specialty will remain a dental specialty.
Björn JohanssonSwitzerland
No report received.
Taipei — China Republic of China Association of Oral and Maxillofacial Surgeons
The beginnings of the association can be traced back to about 50 years ago. During the years 1960 to 1980, “oral surgeons” were practicing mainly in four major health care institutions, including the National Taiwan University Hospital, National Defense Medical College Hospital, Taipei-Veterans General Hospital and Kaishiung Medical College Hospital. The leaders and senior staff of these departments were not only involved in the training of residents but also lectured in oral anatomy, radiology and oral and maxillofacial surgery at the seven dental schools in Taiwan. They held joint conferences in Taipei for almost a decade.
In the early 1980s, the pioneer oral surgeons began to work on founding the professional society, which resulted in an official recognition by the government in 1986. The association held its first annual meeting in 1987. While the members of the association continued to expand the scope and practice of oral and maxillofacial surgery in Taiwan, many well-trained pioneer members were trying to promote international collaboration.


In 1989, more than 30 members of the association participated in the first Asian Congress of Oral & Maxillofacial Surgeons (ACOMS) in Manila. In 1993, the ROCAOMS successfully hosted the 2nd ACOMS at the Grand Hotel in Taipei, with General Chao CF as the congress president and Charles A McCallum as the honorary president. Being highly appreciated by other medical and dental specialists, oral and maxillofacial surgery was subsequently recognized in 1998 as the first specialty in dental medicine by the Ministry of Health.

The mission of the ROCAOMS is to provide a service to the public, to be responsible for the education and training of their trainees and to promote research.
The training of a new generation of OMF surgeons is provided by 18 hospitals that are spread over the country and are approved by the association. The four-year training period consists of a minimum of six and a maximum of twelve months of medical rotations, including general medicine, surgery and intensive care. The remaining three years are devoted to OMF surgery, which covers the whole scope, including cleft lip and palate surgery and the treatment of malignancies.
After the completion of training, the candidate must pass an examination, which includes documentation of cases in all categories of the profession, a written test and a final oral examination. When successful, the candidate will receive a certificate accredited by the minister of health. This certificate is subject for renewal every six years, depending on proven postgraduate continued education.
The association has continued to grow for more than 20 years due to the lasting endeavor of all members and the contribution of previous outstanding board members led by the presidents: doctors Matthew C.F. Chao, Nien-The Yin, Liang-Jiunn Hahn, Richard C.S. Chang, Hong-Rong Chen, Duen-Jeng Wang, Chia-Ning Tu, Ying-Shiung Kuo, Steven Lai, Yong-Kie Wong, Shyun-Yen Liu, Chung-Ho Chen and Tung-Yiu Wong.

Currently, the ROCAOMS has 270 members spread over the country. We are confident to be in an excellent position to grow further and to support the growth and development of other OMFS societies in Asia.
Shou-Yen KaoThailand
Thai Association of Oral and Maxillofacial Surgeons
Before 1940, oral and maxillofacial surgery was largely performed by general surgeons in Thailand. When the first faculty of dentistry was founded in 1940, a part of oral surgery came under the responsibility of dentists. The first postgraduate course in oral surgery was in 1963 but it was limited to dentoalveolar surgery and it took only one year to complete.
Chuachote Hansasuta can be considered the founder of oral and maxillofacial surgery in Thailand. He graduated in dentistry in 1957 and in medicine in 1962. He was trained in oral surgery at the University of Alabama at Birmingham, U.S.A., completing his training in 1969. He even took the American Board of Oral and Maxillofacial Surgery exam and by doing so he became the first foreigner to become a diplomate of the American Board of Oral and Maxillofacial Surgery. He set up the first training
program in oral and maxillofacial surgery at the Faculty of Dentistry, Chulalongkorn University, Bangkok, in 1974. It was a two-year program until 1992, when it was extended to a three-year program.
In 1992, the second training center was established at the oral and maxillofacial surgery unit at Cholburi General Hospital, which is located in the east of Thailand.
In 1994, when the Dental Council was established, the training programs came under the supervision of the Dental Council’s training subcommittee. The examination for certification by the Thai Board of Oral and Maxillofacial surgery was launched and the first diplomas were handed out in January 1998. In December of the same year, the Office of the Civil Service Commissioners officially recognized the oral and maxillofacial surgery qualifications of the diplomates. Beginning in 2006, all dental training programs fell under the supervision of the Royal College of Dentistry.

New training centers in oral and maxillofacial surgery were established in 1996 at Mahidol University, in 1998 at Police General Hospital, and in 2000 at Prince of Songkhla University and Hat Yai General Hospital.
At present, postgraduate training in Thailand consists of a three-year program but it has been decided to extend the training to four years. The program includes one year devoted to medicine, which includes rotations in internal medicine, general surgery, ENT and others; and a three-month rotation in general anesthesia, which is mandatory. The training centers in Thailand take a total of 16 new residents each year. There are currently more than 200 trained oral and maxillofacial surgeons for a population of 62 million people. As of next year, there will be another three training centers: one in the north and two in the northeast. Each center will take at least two residents. The number of new residents will, therefore, increase to a total of 22 each year.
Since 1978, a society of oral surgeons existed but the Thai Association of Oral and Maxillofacial Surgeons was founded in 1990. In 1998, it earned the patronage of His Majesty the King. It is a professional and scientific organization which is also responsible for the quality of education and training of the residents.
The association has organized several symposia and scientific meetings since its foundation.
The Thai association also hosted the first IAOMS sponsored, three-year modular course on oral and maxillofacial surgery, which began in 2001. This took place in Hat Yai, as this city was easily reachable for participants from neighboring countries, including Malaysia, Indonesia, Singapore, the Philippines, Vietnam, etc. The success of this course became legendary and the Thai hospitality will be remembered by all teachers and participants.
The association also organized the Asian Regional Seminar on Training Guidelines, which was held from December 13–14, 2003 at Chulaongkorn University, Bangkok. During the seminar it was agreed that the training should be extended to meet the international standards, as formulated in the document on education and training by the IAOMS. This implied that the training be extended to at least four years.
Recently, the Thai association had the honor to organize the 8th Asian Congress on Oral and Maxillofacial Surgery in November 2008, under the presidency of Vacharee Changsirivatanathamrong.
The Thai association organizes two scientific meetings a year and has grown substantially over the last 20 years, not only in numbers but also with regard to scope of practice.
Vacharee ChangsirivatanathamrongTurkey
Turkish Association of Oral and Maxillofacial Surgery (TAOMFS) Türk Oral ve Maksillofasiyal Cerrahi Dernegi

The Turkish association was established in 1985 by 13 pioneers of Turkish oral and maxillofacial surgery, including Professors Türker and Akça and the doctors Borcbakan, Asri, Selahattin, Demiralp, Ergen, Yücetas, Güngör, Araz, Tasar, Colon and Güven. From its beginning, about 100 members have joined the association. Its first general assembly was held on June 21, 1986.
The TAOMFS has since organized 14 national and nine international conferences.
Ferda Tasar
Ukraine
No report received.
United Kingdom
British Association of Oral and Maxillofacial


Surgeons
Before 1948 and the establishment of the National Health Service (NHS), consultant appointments to hospitals were determined locally and there were very few dentally qualified surgeons who held hospital appointments. Among those who were engaged, a significant number were also medically qualified. It was from this group that the first organization to produce a coordinated professional body arose in the guise of the Oral Surgery Club of Great Britain. It was, and still is today, a club which individuals are invited to join, provided they were deemed suitable by the committee members. Its numbers were strictly limited to a ceiling of 50 active surgeons. Run along the lines of a gentleman’s club of the 1930s, it was strictly “men only” and no women were expected to be seen at any time during their clinical meetings. The leaders had all served military appointments; hence the behavior of the Club’s committee was very much along military lines, resembling an officer’s mess. Rupert Sutton Taylor, qualified in both medicine and dentistry and a consultant at the Westminster Hospital, was its leading light. Nothing occurred without his approval and as a body, the members of the club were those who led the profession; nothing occurred without their initiation, either officially or unofficially and collectively, they were a true “tour de force.”
As a group, these early surgeons had become progressively more disillusioned by their colleagues within the British Association of Plastic Surgeons who, while encouraging them to attend their meetings as guests, failed to incorporate them into an active role within that association. The rapid development of the specialty, combined with an increasing number of capable and ambitious surgeons who were not prepared to be treated in this way, provided a catalyst for change.
Other developments also contributed to the timing of these events:
• T he actions of successive governments, starting with the formation of the National Health Service (NHS) in 1948 and the establishment of “Consultant Dental Surgeon” appointments which gave parity with all other medical specialties, a structured salary and a guaranteed superannuation, as well as admitting rights for dental consultants who were totally responsible for the care of their own inpatients.
• T he creation of the Faculty of Dental Surgery within the Royal College of Surgeons of England, who became responsible for inspection and accreditation of training posts and trainees within the NHS. Trainee standards were set and monitored through a process of regular inspections. The establishment of the Fellowship in Dental Surgery in 1948 was an essential part of this process, since the two elements, satisfactory completion of a training program and the successful passing of an examination, became a necessity. Despite changes in training, accreditation and the examinations over the years to meet the changing nature of the specialty, this principle has remained.
A lso in 1948, the British Dental Association was able to negotiate terms and conditions of service jointly
dental surgeons were concerned, this was 1 per 250,000 head of the population. There was, therefore, a tremendous need for recruitment and training to reach this figure.
Although these bodies were officially those involved, there is no doubt that it was the particular individuals concerned whose representation across the various committees provided the real driving force. They determined the need to combine together to ensure standards of conduct and ability; bring about further progress; keep pace with developments abroad both now and in the future and, even at that stage, bearing in mind the possibility that the U.K. could enter the Common Market, give an appropriate lead to young aspirants.
Two members of the Oral Surgery Club, John Hovell and Norman Rowe, decided to approach colleagues about the costs and feasibility of establishing a British Association of Oral Surgeons. They invited a small group to dinner at the Royal Society of Medicine on March 27, 1961 to form a working party. It was as a result of this that the decision was made to inaugurate a British Association of Oral Surgeons in 1962, some 25 years after the formation of the Oral Surgery Club. The steering group proposed Terence Ward CBE as the first president and he was elected unanimously.
In parallel with this and quite independently, another

and conferred a special honorary fellowship on the president of the American association, ex officio. The first clinical meeting of the new association was held at East Grinstead October 5–6, 1962.
At that stage, it was clear that there was no international association but, rather, a group of individuals who were determined to hold an international meeting on a threeyear basis. However, the conference was such a resounding success that even during the week there was a clamor to establish an international association of oral surgeons. They moved rapidly, for within the same journal containing the write up on the conference, an advertisement appeared for the IAOS, along with an application form for membership! In March 1963, the newly fledged international association determined that their next conference would be in Copenhagen in 1965.
Within the U.K., training programs were organized around the District General Hospitals, rather than the teaching hospitals, since this was where accidents were seen predominantly and trauma constituted the principal element of work at that time.
Today, the U.K. has 125 trainees in 15 rotational programs under the control of a central committee on higher surgical training and its OMFS subcommittee. This is constituted from within the Surgical Royal Colleges and the specialist associations. Training lasts for five years in common with other surgical specialties, as agreed between EU member states. The rotations enhance experience and rotations are inspected regularly to ensure conformity with agreed standards.
It is of interest to note that within the minutes of BAOS, the desirability of medical training is mentioned as early as 1966. At the meeting of March 19, 1977, a formal proposal was made for the adoption of a dual degree for all future trainees. It was, however, not until 1981 that this proposal was put to the full membership and a vote taken to make it mandatory within a period of 10 years for anyone aspiring to a consultant position. The result was a vote in favor by 128 to 96, as recorded in 1982.
The alteration in the name of the association to BAOMS came about in May 1984, when members voted this a more appropriate reflection of their activities and to counter aspirational claims of other specialties, such as ENT, who had added “head and neck surgeons” to their title.
In 1984, the Royal College of Surgeons of Edinburgh inaugurated an FRCS examination in OMFS and the first examination was held in 1985. It was this departure that led ultimately to the Intercollegiate Final Fellowship
Examinations in all surgical specialties as part of the restructuring of all surgical training and examinations.
Within the U.K. an increasing number of women have entered the profession. They have also entered leadership of BAOMS, with Moira Morten serving as the first female president.
Today, there are almost 500 consultant OMFS surgeons serving a population of over 60 million people through approximately 150 hospitals and there are 1,131 active members of the BAOMS.
 John Williams
John Williams
United States of America American Association of Oral and Maxillofacial Surgeons
Oral and maxillofacial surgery in the United States is defined by the American Dental Association as the specialty which includes “the diagnosis, surgical and adjunctive treatment of diseases, injuries and defects involving both the functional and esthetic aspects of the hard and soft tissues of the oral and maxillofacial region.”1
The roots of the specialty can be traced back to the Civil War, when William A. Carrington, the medical director for the Confederacy, commented that dentists “plugged, cleaned, and extracted teeth,” in addition to “adjusting fractures of the jaw and operating on the mouth.” Dentists such as Thomas Gunning and J.B. Bean made revolutionary advancements in the treatment of facial fractures for the Union and Confederacy respectively. The first American textbook devoted to oral surgery, “A System of Oral Surgery”, was published in the late 19th century.
By the early part of the 20th century, oral and maxillofacial surgeons were already pioneering cleft palate and other facial reconstructive surgery. However, the majority of practitioners were known as exodontists, or extraction specialists and were not recognized as a cohesive specialty. As a result, there was a lack of a common interest among exodontists; no dental school offered a postgraduate course in exodontia and exodontists were not recognized as specialists either within or outside of the dental profession. An article in the Journal of Oral and Maxillofacial Surgery titled “The Building of a Specialty: Oral and Maxillofacial Surgery in the United States 1918–1998”2 notes that when the U.S.A. entered World War I, exodontists were inducted into the army as private soldiers. Even the Red Cross did not recognize the specialty. Clearly it was time to organize and unify the specialty to benefit both the exodontists and the public.
Led by the efforts of Menifee Howard, 125 prominent dentists who specialized in extraction gathered in Chicago
1Definition of oral and maxillofacial surgery, Approved by the Council on Dental Education and Licensure, adopted October 1990.
2The building of a specialty: oral and maxillofacial surgery in the United States, 1918–1998. J Oral Maxillofac Surg; 1989; 56(suppl 3):70–132.
on August 9, 1918 for the charter meeting of the American Society of Exodontists (ASE). He was elected chairman. Early meetings of the new organization were characterized as “stormy,” as the members sought to establish policy and procedures for the fledgling group. In addition, there was opposition to the creation of the society from other dental organizations.
In 1919, the National Dental Association granted official recognition to the ASE and by the time the society met for its third annual meeting, the climate had improved to a point that it was possible to add educational programming to the meeting’s business sessions. The 1919 annual meeting was also significant for the House of Delegate’s decision to officially change the name of the association to the “American Society of Oral Surgeons and Exodontists (ASOSE).” This new name was reflected in the practice modalities addressed during the annual meetings. Topics presented during these meetings included: developments in anesthetics and advancements in anesthesia administration and monitoring; the treatment of complications resulting from extractions, facial fractures, oral surgery and plastic cases; impacted teeth and cleft lip and palate. These conditions and procedures continue to form the solid foundation of the specialty today.
In 1946, the word “exodontists,” which had been a point of contention for many members since the society’s earliest days, was eliminated. From 1946 until 1977, the organization was known as the American Society of Oral Surgeons (ASOS), however, beginning in 1961, it was evident this new, abbreviated name was not a comfortable fit.
The specialty was growing and its scope of practice was changing to the point that even the definition of “oral surgery” was a point of disagreement between the American Dental Association and the American Medical Association. At issue was the rise of orthognathic surgery as a major component of OMFS specialty practice and the increased involvement of oral surgeons in maxillofacial trauma care.
The first suggestion that the word “maxillofacial” be added to the association’s name occurred in 1968, after oral surgeons from the United States attended international meetings and symposia that were designated “maxillofacial.”
As debate over incorporating the word “maxillofacial” into the association’s name began to heat up, similar discussions were taking place between plastic surgeons and otolaryngologists regarding the use of the term in the context of performing “facial plastic surgery.” In the end, a study session on maxillofacial surgery held by the AMA was co-opted by the plastic surgery section, which, over the objections of the otolaryngologists, was ultimately expanded to include maxillofacial surgery.

Following many discussions that included advice from legal counsel, a meeting between the ASOS and the ADA Board of Trustees in 1973 resulted in the approval of a resolution by the ADA House of Delegates permitting ASOS members to announce themselves as practicing oral and maxillofacial surgeons. Subsequent changes were also made to the ASOS Principles of Ethics and the definition of the specialty. In 1977, the ASOS House of Delegates changed the name of the organization to the American Association of Oral and Maxillofacial Surgeons and the name of the association’s journal to The Journal of Oral and Maxillofacial Surgery.

Throughout the 20th century, oral and maxillofacial surgeons were on the forefront in the development of oral and maxillofacial treatments and procedures that improved the outcomes and lives of their patients. Many current trauma techniques, for example, were developed by OMFS in combat hospitals in World War II, Korea, Vietnam, the Gulf Wars and the recent conflicts in Iraq and Afghanistan.
As we venture well into the second decade of the 21st century, the specialty of oral and maxillofacial surgery continues to be an exciting area of practice for the 9,500 oral and maxillofacial surgeons in the United States.
Oral and maxillofacial surgeons are respected and valued members of the U.S. healthcare team who maintain active staff privileges with local and regional hospitals in their communities and practice in a variety of settings, including private clinical practice, ambulatory surgical centers and hospitals. Other opportunities are available in academia, military service or in dental research and industry.

At present, there are 101 oral and maxillofacial surgery residency training programs in the United States providing the specialty with about 190 new surgeons each year. Following dental school, oral and maxillofacial surgery residents complete a hospital based surgical residency of at least four years. This includes a minimum of 30 months dedicated to oral and maxillofacial surgery, in addition to a core surgical year that includes rotations in medicine, general surgery, anesthesia and other services. All of our residents complete the same rotations with the same level of responsibility as medical residents.
Some oral and maxillofacial surgery residents earn medical degrees as an integrated component of their OMFS training but regardless of whether a resident decides to complete a residency with or without a medical degree, all training meets the accreditation standards and is, therefore, virtually identical. As a result, all oral and maxillofacial surgeons possess the knowledge and skills to perform the full scope of specialty practice.
Dentoalveolar procedures, including third molar and dental implant surgery, are a staple of the specialty but our surgeons also maintain a strong presence on the hospital staffs in their communities and routinely take trauma call. In fact, the American College of Surgeons’ guidelines for
optimal care require Level I trauma centers to have oral and maxillofacial surgeons on call to perform complex reconstruction of the maxillofacial and craniofacial complex.
In recent years, their skill in facial reconstruction, the same skills that enable OMFS to excel at orthognathic and cleft procedures, has led many oral and maxillofacial surgeons to expand into the elective facial cosmetic surgical area and several AAOMS members have limited their practice to the cosmetic surgery field. Another growing area of practice is oral pathology. Regrettably, we are seeing more young people present with malignancies relating to their use of tobacco and exposure to Human Papilloma Viruses.
Five years ago, oral and maxillofacial surgeons in the U.S.A. were among the first to identify a correlation between bisphosphonate drug therapy and a condition presenting as exposed, necrotic bone in the maxillofacial region, which has since been termed Bisphosphonate Related Osteonecrosis of the Jaw (BRONJ). While the condition remains difficult to cure, AAOMS fellows and members have published a white paper, conducted a webinar, published a BRONJ focused supplement to the Journal of Oral and Maxillofacial Surgery and generally performed an outstanding service to the dental and medical communities by alerting them to the condition, its symptoms, and ways to screen potential patients before they undergo oral surgical procedures.
As exciting as the specialty’s future is, there are some areas of concern. The AAOMS is particularly troubled by shortage of faculty in the OMFS programs. As academicians leave their posts in growing numbers for private practice,
there are not enough surgeons interested in filling their vacancies. In 2002, AAOMS established the Faculty Educator Development Award, which presents a three-year stipend to deserving young OMFS interested in working as an academician. Approximately four to five FEDAs are awarded each year and as of 2009, 33 individuals had been recognized.
Another concern is the effect of healthcare reform on our specialty. The bill signed into law in 2011 will not take effect until 2014 but there are a number of requirements that we must investigate further to determine how we may help our members comply. Further, we must determine what impact this bill will have on our abilities to continue to provide excellent oral and maxillofacial surgical care.
Overall, it is a privilege to be an oral and maxillofacial surgeon practicing in the United States today. OMFS enjoys a broad scope of practice that allows us to use the full range of our training and skill to save the faces and change the lives of our patients. It is truly an exciting time to be a member of this specialty.
Mark Tucker and John F. Helfrick
Uruguay
Uruguayan Society of Oral and Maxillofacial Surgery Sociedad Uruguaya de Cirugia Buco MaxiloFacial
The development of the specialty in Uruguay began in 1946, when a section of surgery was established by the Uruguayan Dental Association but it was not until 1955 that the constitution of the society was written. In 1972, the silver jubilee was celebrated and Ries Centeno was appointed as an honorary fellow.
The first scientific meeting of the society was held in 1974. In 1976, under the chairmanship of Leon Römer, the need for official recognition of the specialty by the health authorities was recognized and a commission established to advance this issue.
In 1985, Mario Scarrone became president of ALACIBU and the headquarters moved to Montevideo. The scientific congress was subsequently held in Montevideo in 1988, attended by Wilfred Schilli, the president of IAOMS. That also was the year that the society affiliated with IAOMS. A seminal event in the history of teaching in the specialty was the organization of the first training seminar, organized by the Uruguayan Society in Punta del Este.


On the occasion of the 50th anniversary of the society, a scientific meeting was held in Punta del Este in conjunction with the countries of the Southern Cone. At a meeting, at which participants of the MERCOSUR countries were present, the issue of regulation of the specialty was discussed. During the period 1995–2002, when Andres Migliorisi
was president, moves were made to have the specialty officially recognized by the health authorities, which was successfully accomplished.
In 2007, at the society’s national meeting, the dean of the dental school reported that the central board of the University of the Republic, had adopted the draft of “Specialization in Oral and Maxillofacial Surgery and Oral and Maxillofacial Trauma,” a move which had been long delayed and was important for the training of specialists. This became official in November 2008, when the board of the faculty of dentistry, supported by the University of the Republic, awarded the title of “Specialist Surgeon in Oral and Maxillofacial Traumatology and Surgery” to six senior members of the society.
The current training is organized through the University of the Republic in which teachers of the dental and medical school participate. Mario Escarrone is
In summary, since 1946, when the section of surgery of the Uruguayan Dental Association was founded, numerous efforts had been made to achieve the establishment of the Uruguayan Society of Oral and Maxillofacial Surgery and Traumatology.
Andres MigliorisiVenezuela
Venezuelan Society of Oral and Maxillofacial Surgeons

Sociedad Venezolana de Cirugia Buco-Maxilofacial
The pioneers in Venezuela were a group of surgeons who worked at the Red Cross Hospital, Dental Department, led by José Barros Saint-Pasteur. He was a dually qualified, self-trained maxillofacial surgeon, who performed a wide variety of surgical interventions, including oncologic surgery. Patients came from all corners of the country for dental extractions and treatment of oral-facial infections but also for reconstructive surgery and correction of facial deformities. For this purpose, hospital facilities were available. The members of the staff were mostly oral surgeons from Central University of Venezuela.
Raul Garcia Arocha, who trained at the University of Chicago, Illinois, was the initiator of the establishment of the Venezuelan Oral Surgery Society in 1957. He also became the first president, with José Barros Saint-Pasteur as his secretary. They organized seminars, wrote the bylaws and held a congress every two years. They also promoted strong ties with the AAOMS. The society grew and changed presidents every two years. The attendance at the meetings also increased steadily and international speakers were
always invited to stimulate the new generation and to elevate the level of the specialty. The second Latin American meeting (ALACIBU) was held in Caracas in 1967 under the presidency of José Barros Saint-Pasteur. The relations with the national associations of other Latin American countries were strengthened at that meeting.

The first training program for oral surgery in Venezuela was established by Raul Garcia-Arocha in 1978 at the Central University of Venezuela in Caracas. It was a two-year program that provided little hospital exposure. The other dental schools in the country copied this two-year training program. The society changed its name to “Oral and Maxillofacial Surgery” in 1983, following the AAOMS. The society has grown ever since and currently has 265 members. Altogether, society members serve a population of around 27 million people. The society has several regional sections in order to stimulate local activities and to provide information to all registered colleagues.
The practice of oral and maxillofacial surgery improved dramatically with the input of Olaf Sandner, trained in Hamburg, Germany; Cesar A. Guerrero, trained in Dallas, Texas; Esteban Papp, trained in Minnesota and Raul Garcia-Arocha, trained in Boston, Massachusetts. They introduced modern techniques and concepts to the country and brought a new vision to the specialty. In 2002, this all led to the opening of a four-year oral and maxillofacial surgery program in Caracas, based on the guidelines as supported by the IAOMS. Since that time, this program has been directed by Alberto Lander-Hoffman. There are two full OMFS training programs in the country. The second program is in Valencia directed by Ruben Muñoz. Together they take six new trainees every year. The first graduates are already in teaching positions and
a re helpi ng to f u r t her i mprove t he level of t ra i n i ng of OMFS t h roug hout t he cou nt r y. T hese t ra i n i ng prog ra ms comply w it h t he I AOMS st a nd a rd s , i nclud i ng med ica l rot at ion s , f u l l-t i me ded icat ion , emergenc y ca l ls , etc. T he societ y is a lso d isc u ssi ng t he need for cer t i ficat ion a nd re-cer t i ficat ion ever y 10 yea rs . A L ACIBU is con sider i ng i mplement i ng a n eva lu at ion prog ra m a nd pay i ng on-site v isit s to a ssess t he st ate of t he a r t i n L at i n A mer ica n educat ion a nd t ra i n i ng a nd to set u p a com m it tee to per ma nent ly su r vey t he d i f ferent t ra i n i ng prog ra ms a nd to of fer recom mend at ion s i n order to prov ide bet ter st a nd a rd s of ca re
Scient i fic meet i ngs of t he Venezuela n Societ y h ave been v isited by ma ny i nv ited i nter n at ion a l spea kers w it h great reputations A mong them have been: Hugo Obwegeser, Jen s Pi ndborg , R oy Eversole, R ober t Wa l ker, Wi l l ia m Bell, Philip Boyne, Per-Ing va r Brå nema rk a nd ma ny ot hers T hey a l l h ave cont r ibuted to t he i mprovement of t he st a nd a rd s of ou r profession
Venezuela a lso h a s cont r ibuted i nter n at ion a l ly w it h pioneer i ng work . In 19 67, José Ba r ros Sa i nt-Pa steu r descr ibed i nter posit ion a l bone g ra f t i ng for t he edent u lou s ma nd ible, wh ich wa s some fi ve yea rs before Schet t ler. In 19 6 8 , he a lso i nt roduced t he concept of t he orbic u la r is or is mu scle recon st r uct ion for bi latera l clef t l ips a nd i n 1970 , ma x i l la r y adva ncement u si ng a pa lat a l a pproach Cesa r Guer rero i n it iated i nt raora l d ist ract ion osteogenesis for w iden i ng a nd leng t hen i ng a s wel l a s bone t ra n spor t for ma nd ibu la r recon st r uct ion a nd a lveola r clef t s . He a lso d id some pioneer i ng work ut i l i zi ng z ygomat ic i mpla nt s a nd prei mpla nt su rger y for reh a bi l it at ion of ora l f u nct ion
Venezuela n textbook s h ave cont r ibuted to L at i n A mer ica OMFS . Ola f Sa nd ner ’s book s i n Spa n ish on temporoma ndibu la r joint surger y a nd ora l a nd ma xillofacia l su rger y h ave ser ved dent a l a nd postg radu ate st udent s i n L at i n A mer ica , a nd Cesa r A . G uer rero’s Dist ract ion Osteogenesis of t he Facia l Skeleton wa s t ra n slated i nto Spa n ish a nd Por t ug uese a f ter t he or ig i n a l version wa s publ ished i n Eng l ish . Zygoma Impla nt s: a n At la s of Su rger y a nd Prost hodont ics a lso wa s publ ished i n Eng l ish a nd Spa n ish
Cesa r G uer rero wa s president of A L ACIBU f rom 2 0 0 0 to 2 0 03 a nd du r i ng t h at per iod t he fi rst i ndex of su rgeon s i n Sout h A mer ica wa s i nt roduced . A n i mpor t a nt cont ract wa s sig ned at t h at t i me bet ween A AOMS , C AOMS (Ca nadia n A ssociation of Ora l a nd Ma x i l lofacia l Su rgeon s) a nd A L ACIBU to elevate t he level of t he specia lt y i n t h is cont i nent . A AOMS t ra n slated it s jou r n a l i nto Spa n ish i n Venezuela a nd a f ree issue wa s del ivered to ever y su rgeon of t he A L ACIBU membersh ip roster T he project , u n for t u n ately, d id not cont i nue becau se of
t he lack of i nterest f rom t he L at i n A mer ica n su rgeon s to subscr ibe, even for a d iscou nted fee. T he Venezuela n societ y is indebted to t he A AOMS for t heir help in tra ining so ma ny su rgeon s a nd for set t i ng t he ex a mple for t he development of t he specia lt y i n Venezuela Med ica l a nd dent a l ca re i n t he cou nt r y is c u r rent ly ba sed on gover n ment cl i n ics a nd hospit a ls where t he pat ient s a re t reated for f ree. T he Nat ion a l Hea lt h System eva luation, however, shows va st ly deteriorated insta l lations, poor a ssist a nce i n tech nolog y a nd major de ficiencies i n ava i la ble ph a r maceut ica ls . Ma ny med ica l specia lt ies h ave cea sed to ex ist i n t he hospit a ls a nd most of t he elect ive surger y is not performed in the government system anymore Elect ive su rger y is per for med i n pr ivate hospit a ls or a mbu lator y centers , w it h m i n i ma l i n su ra nce covera ge Cesar G u errero
Epilogue
T he cont r ibut ion s of 63 of t he 75 a f fi l iated n at ion a l ora l a nd ma x i l lofacia l su rgeon a ssociat ion s t h at subm it ted a n a bst ract , cont a i n a wea lt h of i n for mat ion i n t h at for t he fi rst t i me i n t he h istor y of t he specia lt y a nd of I AOMS , a rea son a bly acc u rate i mpression is ga i ned a bout t he tot a l nu mber of ora l a nd ma x i l lofacia l su rger y who a re operat i ng worldw ide
Considering that not a ll colleagues are members of their n at ion a l a ssociat ion a nd a lso t h at some cou nt r ies h ave not subm it ted a bst ract s , wh i le a lso some cou nt r ies a re not a f fi l iated to t he I AOMS , t he tota l nu mber of OMS shou ld be a rou nd 3 0 , 0 0 0 . T hese cont r ibut ion s a lso prov ide a good i n sig ht i nto how OMFS t ra i n i ng is orga n i zed i n t he d i f ferent pa r t s of t he world . Not on ly a re t here a nu mber
g l o ba l d i s t r i b u t i o n o f o m f s
Region Total Number of OMFS Africa 522
A sia 6, 45 4 Europ e 8 ,32 2
L atin America 2, 863 Nor th America 9 ,97 1 Oceania 20 0 Total 28 ,332
of similarities, it also is striking to see how over the last two decades, the various pathways of education and training have seemed to converge to a common denominator. There are, however, still many differences that are largely defined by historical and socioeconomic factors. It is obvious, however, that the “IAOMS’ Guidelines on Education and Training,” as they exist today (see addendum), has had an enormous impact on the emerging specialty in the various countries. It seems likely that the training of the new generation will be universally based on a sound medical and dental base, albeit that this may be arranged in different ways in the specific regions.
Another lesson to be learned is that the specialty has made an enormous progress over these 50 years. This took place worldwide and probably continues to do so. It
is heartwarming to see that many developing countries are catching up so quickly and are also participating in the academic setting by producing scientific articles in international literature. This is of great importance as Fred Henny pointed out in 1965; proper education and training is based on three pillars, education, patient care and research (see chapter 1). Let us hope that the content of this chapter will inspire even more educators to organize their education and training around these three fundamental aspects.
The Regional Associations
To facilitate communication and organization, the IAOMS decided to invite six geographical regions to represent their particular nations at the executive committee. This chapter contains the reports of these six regional associations, with an emphasis on their particular development and impact on the development of the specialty in the region they represent as well as globally.
Africa
African Association of Oral and Maxillofacial Surgeons
Development of oral and maxillofacial surgery on the continent of Africa has been rather slow and uneven among the various nations in the continent. The northern and southern parts of the continent are far ahead of west, east and central Africa in terms of the development of oral and maxillofacial surgery. While South Africa and Egypt can boast of fairly large numbers of oral and maxillofacial surgeons (OMS), Nigeria has just a little above 100 and the East African countries of Kenya, Tanzania and Uganda have less than 30 and Ghana has about 12. Figures in Francophone African countries are not easily available but are not significantly higher than in the other nations.
As far back as 1992, South Africa, with a thriving national association and a mandate from the International Association of Oral and Maxillofacial Surgeons, attempted to bring the continent’s OMFS specialists together in preparation for the hosting of the 11th ICOMS. Conrad Masureik made spirited efforts to achieve this. This effort failed to produce the desired result but probably was an ‘eye-opener’ and the necessary stimulus for a country like Nigeria to consider establishment of a national association, which came to be in 1993.
In 2003, Paul Stoelinga, as the president of the IAOMS, stressed the need for African oral and maxillofacial surgeons to come together at a meeting in Athens. This call became a reality in August 2005, when Pino Ferreria, then president of the IAOMS, assembled key colleagues from Egypt, Ghana, Kenya, Nigeria, Tanzania and South Africa in Nairobi, Kenya. At this meeting, extensive deliberation took place on the constitution, funding and structure of an African maxillofacial association. Discussion at this meeting gave birth
to the African Association of Oral and Maxillofacial Surgeons (AfAOMS) and election of its officers. The
this type is mainly in the East, South and Central Africa and Egypt. The other pathway is fellowship diploma, which is hospital-based and may last between four to six years. This is the pathway in the West African sub-region for both Anglo and Francophone countries. Individuals with qualifications from the U.K., continental Europe, the U.S.A., Canada, Australia or other regions of the world are found all over the African continent.
At the time of the AfAOMS’ affiliation with the International Association of Oral and Maxillofacial Surgeons, the IAOMS had individual national associations and societies as its affiliated national associations, with councilors representing each particular nation. The current arrangement recognizes regional representatives as members of the executive committee. AfAOMS is the 6th and the last region to place a regional representative on the IAOMS executive committee.

Guthua was elected the president of the association while Ademola Olaitan was elected as the secretary general.
As a young association, the activities of AfAOMS are anchored on the vigor, drive and enthusiasm of the executives. While some members of the executive committee have shown keen interest in the association’s affairs, the large size of the continent, relative communication handicaps and the non-availability of funds retarded the momentum at takeoff. The inability of nominated Kenya to raise funds for the hosting of the 2010 biennial scientific meeting is a typical case of the hindrance that the lack of funds can cause.
Eligibility for membership of the African Association of Oral and Maxillofacial Surgeons (AfAOMS) is based on membership of the national OMFS association in countries with such bodies. Individuals practicing in countries without national societies or associations are free to join the continental body. At the moment, members are drawn mainly from Anglophone countries. Francophone and Lusophone countries are yet to be fully involved in the activities of the association. Apart from Egypt, which is a founding member and Libya, which has shown keen interest in membership, other Arab-speaking nations have not.
Although there are African OMFS who are doubly qualified, dental qualification is the basic prerequisite for the practice of the specialty in most of the African countries. Two pathways are taken to qualify as an OMFS on the continent. One pathway is a university-based Master’s program, which lasts from three to four years. Training of
Despite the fact that AfAOMS is a very young regional association with its unique challenges of inadequate communication and lack of funds, it can boast of modest achievements. The first is the realization of the importance and benefits of coming together. Ghana inaugurated its national association in 2008 and formally became a full member of the IAOMS at the 19th ICOMS in Shanghai. Libya is in the process of establishing its national association. An ongoing IAOMS Foundation sponsored educational program in East Africa, initiated by John Williams and Paul Stoelinga has been of large benefit to the regional association. Communications and the exchange of ideas have commenced between Kurt Butow of South Africa, Vincent Ugboko and Ambrose Emeka Obiechina of Nigeria regarding the possibility of reciprocity and collaboration in the examinations and Fellowship Diplomas of the South African College of Oral and Maxillofacial Surgeons, West African College of Surgeons, Ghana College of Physicians and Surgeons and the National Postgraduate Medical College of Nigeria.

The African Association of Oral and Maxillofacial Surgeons is a fairly young association with challenges, modest achievements but with capability and potential to a great horizon. These capabilities and potentials can be reached with visionary leaders and recognition and with serious attention paid to challenges and sincere support, in all ramifications, from the established regional associations.

 Ademola Abayomi Olaitan
Ademola Abayomi Olaitan
Asia
Asian Association of Oral and Maxillofacial Surgeons
The Asian Association (AsianAOMS) was formed in Manila on March 16th, 1989. At the first congress, the founding president was E.M. Nazarino (Philippines), the chairman was Y. Uchida (Japan), the secretary general was Kanichi Seto (Japan), the publicity/social secretary was N. Ravindranathan and the chief editor was S. Enomoto (Japan). The first issue of the Asian Journal of Oral and Maxillofacial Surgery was published in October 1989.
The next congress was held in Taipei in 1993 with the congress chairman being Professor Chao, the organizing secretary Professor Chang and N. Ravindranathan was elected as the second president.

At the third congress, Professor Kim was elected president for the period 1997–2000. During the fourth congress in Korea, Jatinder Nath Khanna was elected president.
The next congress was held in conjunction with the 28th congress of the Association of Oral and Maxillofacial Surgeons of India (AOMSI), when the president also became the congress chairman. Khanna, therefore, became the chairman as well as president and Rajesh Dhirawani the organizing secretary. Hiroyasu Noma was elected as the next president and Kenichi Kurita became secretary general.
Four issues of the Asian JOMS were published in the period until 2002.
At the 6th congress in Tokyo, 2004, the Asian guidelines for training and education in the specialty were endorsed by the council and general assembly. However, at the next congress in Hong Kong, 2006, under the presidency of Nabil Samman, the constitution was revised to adopt the IAOMS’ recommendations. At this meeting, the Japanese association announced its

intention of joining the AsianAOMS, resulting in some 1,600 Japanese oral and maxillofacial surgeons forming a vertical type of agreement with the Asian Association. Vacharee Changsirivatanathamrong was elected as the seventh president.
The first educational program of the Asian Association, on the subject of orthognathic surgery, was held in Manila, Philippines in 2007 and included both lectures and live demonstrations.
The Asian Association found itself in a position in 2008 to donate $5,000 to the IAOMS Foundation and has continued to do so annually. The Japanese Society of Oral and Maxillofacial Surgeons (JSOMS) also decided that they would support the travel expenses of their members who were chosen to present papers at IAOMS and AsianAOMS congresses.
The 7th congress was held in Bangkok, 2008, at which Sharifah Fauziah Alhabshi was elected as the eighth president.
A second educational program was organized jointly by the Asian, Japanese and Malaysian associations in conjunction with the Oral Health Division, Ministry of Health, Malaysia in 2009. This three-day course on craniofacial distraction, headed by Lim Cheung, was attended by 69 participants and all 25 seats at the Hospital Selayang, Malaysia allocated for hands-on lectures were taken.
To facilitate education and training, the Asian Association established a Foundation in 2009 and utilizes up to $10,000 annually for up to two years for one trainee from each of two developing countries. A total of up to $40,000 is spent over each two-year period. So far, the Korean association has funded a Mongolian trainee on a two-year program and the Japanese association has funded a trainee from Bhutan on a one-year program. The budget for one year was
The number of papers submitted to the Asian JOMS has increased annually: 83 in 2007, 92 in 2008 and 114 in 2009. Acceptance rates were 37.3 percent in 2007, 48.9 percent in 2008 and in 2009, 23.7 percent. Delays in publication were caused by collapse of its publisher in 2010, which was resolved by Elsevier taking on the publishing.
As of March 2010, the total membership for the AsianAOMS was 2,116. Vertical membership arrangements exist for all accredited members of the JSOMS and those from Taiwan.
 Kenichi Kurita
Kenichi Kurita
Europe
European Association of Cranio-Maxillofacial Surgery

Established in 1970, the European Association of Maxillofacial Surgery was the brainchild of Hugo Obwegeser of Zurich. In the late 1960s, believing that the emerging specialty needed the support of a strong, professional body, he proposed the establishment of a European association to the German association, who rejected the idea. However, with the support of several like-minded individuals, in March 1970, he invited a group of 59 participants to a clinical meeting in Zurich and informed them of his resolve to establish a European association. The group, most of whom were qualified in medicine and dentistry, supported this move, as well as the suggestion that the requirements for membership should be a dual qualification and at least three years training in maxillofacial surgery. The suggestion that each person’s membership be based on their qualifications and not the membership of a national association was made by Hans Freihofer, a past president of the FDI. At the time, this was intended as a strong educational statement but changes in Europe, coupled with a history of diverse development of the specialty, resulted in this statement being appropriated by politicians and used for their own purposes.
It has to be remembered that Europe is a widely differing collection of nations and, as far as our specialty was concerned, was divided north-south and east-west in terms of its origins. In the north, the origins were from dentistry, while in the south they were medically based. In Eastern Europe, stomatology existed and was considered to be a medical specialty with little dentistry, a course which also was found in France, although here a true specialty existed on top of a medical degree. Only in Germany, Austria and Switzerland did the specialty develop from dual medical and dental training. Several countries, including the U.K. and the Netherlands, were to develop a training program that was similar to one developed by the Germans and others followed in the course of time. Just to complicate matters further, until 1989, the whole of Eastern Europe was isolated from the west by the Iron Curtain, created by the Soviet Union, which for 40 years prevented contact between surgeons on either side of it.
In 1957, the European Economic Community (EEC) was established and gradually expanded; as other countries joined later, it was renamed the European Union (EU). There was a need to take on this huge political force, since it would have a great influence on the specialty as harmonization was introduced as part of the process necessary to permit freedom of movement and freedom to work in any of the affiliated nations. It was against this background that the European association was established and the structure of the initial council reflected the divisions. The president was also the person responsible for the next conference and the other officers were the secretary general, treasurer and editor-in-chief.
The first president was Franc Celesnik of Yugoslavia and the first congress was held in Ljubljana in 1972. Eligibility for membership was a constant issue from the very outset, which bedeviled membership. An enormously successful congress was held in Zurich in 1974 under the presidency of Hugo Obwegeser, at the end of which Norman Rowe was installed as president and the third congress was scheduled for London in 1976. An unforgettable opening ceremony was held at the Royal College of Surgeons where the scientific program was also conducted. More than 550 delegates from 32 countries attended. It was at this meeting that Obwegeser was to be elected an Honorary Member of the association, which received unanimous support from the attendees. He would stay on council as editor-in-chief.
The 1978 congress in Venice, with Camillo Curioni as president, was followed by the first president from Eastern Europe: Stefan Knapik (1980). With the election of Gerhard Peiffer from Hamburg, the association demonstrated how attempts were made to rotate the presidency throughout Europe in order to encourage interest and further the
association’s membership. There were further changes among the officers after the first decade when Hermann Sailer became treasurer (1982) and Jacques Levignac was elected to the new post of education officer (1984), while Hans Peter Freihofer became editor-in-chief (1980).
It was at the Paris conference in 1984, with Jean Delaire as president that the first moves were made to change the name of the association. The move was proposed to recognize the full scope of clinical practice in the specialty which was feasible in some countries. The decision on the name change was deferred until the 1986 conference in Madrid, under the presidency of José Alonso del Hoyo. At that point, the association’s name became the “European Association for Cranio-Maxillofacial Surgery,” and with it came a name change to the Journal, to “The Journal of CranioMaxillofacial Surgery.” This meeting also saw Wolfgang Koberg forced to resign as secretary general due to ill health. John Sowray took his place and John Williams was elected as assistant secretary. Finally, the decision was made to hold the 1994 congress in The Hague with Paul Stoelinga as president, he, too, was elected to council.


Two years later in Athens (1988), the Bermuda and Tenerife meetings had taken place, and as a result, a proposal was made by council to make provision for senior singly qualified members to become eligible for full membership in the association. Following a heated debate in the general assembly, this was defeated by a single vote. However, the ballot had not been conducted under ideal circumstances, as the simultaneous translators had walked out at a critical moment in the proceedings. The vote was so unsettling for
two senior members of the executive committee that they spent the evening pacing the streets of Athens, seeking a way forwards.
The next six years saw presidents with significant roles in other international bodies and the influence of these positions affected the thinking of the EACMFS council. Under the presidency of Robert Pfeiffer, several pressing issues needed to be addressed: 1) trainee membership was introduced (Brussels, 1990); and 2) a forum of European leaders was necessary, in particular to provide advice on the specialty to the European Community on political and training issues. With this emphasis, it was important ideally to involve the presidents of all the European national OMFS associations. There also was an equal need for a European postgraduate educational college. Over the next few years, these issues were discussed and implemented in different ways. Additionally, for financial reasons, the publication of the journal was transferred from Thieme to Churchill-Livingstone.
By March 1991, the former East European association had been dissolved and as part of this, the EACMFS invited 44 European representatives to a meeting in Linz (December 1991) to examine a draft constitution for a Confederation of European National Associations, a body which was deemed necessary until such time as Europe could move forwards as a common front, ideally within the EACMFS. For the Bermuda/Tenerife proposals to work, this common approach was required. Almost at the same time, the section of stomatology and oral and maxillofacial surgery of the European Union of Medical Specialists (UEMS) decided to establish a European Board. The president, wearing his UEMS hat, found himself desperately in need of advice on the educational program from within Europe and council agreed that he should be supported in the formation of such a group by invitation.
Founding members of the European Association in Ljubljana, 1972. From left to right: L. Merville, France; M. Perko, Switzerland; G. Rossi, Italy; S. Knapic, Poland; J. Toman, Czechoslovakia; H. Obwegeser, Switzerland; F. Celesnik, Yugoslavia; M. Glahn, Denmark; C. Freidel, France; A. Rehrmann, Germany; W. Koberg, Germany.
The EACMFS was being consulted regarding political and educational issues for which it was inadequately prepared and the consequence was discord among its most senior members who still believed that the association was an entirely scientific one, without any other function. There was a clear need to strengthen the specialty’s links through the Confederation, thereby strengthening the association’s negotiating position. It was highly desirable that a common European response be prepared to counter any American attempts at downgrading the proposals which were on the table. As part of this process, council proposed changes to its constitution at its meeting in March 1992. A smaller, more flexible executive committee of five or six individuals would form the nucleus of the association and the council would be composed of representatives, ideally the presidents of all the national OMFS associations of the new, enlarged Europe.
presence also produced problems, some of which required the president to have to deal with immigration police in the middle of the night! A large number of late registrations for the social events was an unexpected issue, as was the presence of a film company which took a lot of money from delegates and then absconded with the proceeds. Despite all this, the conference made a profit.
The confederation was attended by 57 representatives of 27 nations, providing a much better representation of regional opinion than had been previously available. As a result of the changes voted in at the last general assembly regarding the constitution of council, this representation was also reflected in the EACMFS council, so the confederation had achieved its purpose and could now be disbanded.
The presidency now moved to Hermann Sailer and the conference to Zurich to celebrate the 25th anniversary of the founding of the association (1996). For the jubilee
A very successful congress was held in Innsbruck in 1992. At his final meeting as president, Rudi Fries announced, sadly, the deaths of two of the honorary members who had played large roles in the establishment of the association, Norman Rowe and Wolfgang Koberg. He also reported on the adoption of the IAOMS Guidelines on education and training, which would later serve as the blueprint for the EACMFS Guidelines. He proposed the need for the association to widen its membership while still complying with the standards that were already set, i.e., applicants for full membership should a) come from a country with a national OMFS association and b) such associations must have declared agreement with the EACMFS training principles and the IAOMS guidelines. Additionally, Emil Steinhauser would take over as editor-in-chief.
In his inaugural presidential address (1994), Paul Stoelinga announced that his prime objective was to follow up the many contacts and conduct a recruitment drive among East Europeans. Further, he was anxious to follow up on the association’s initial meetings with AAOMS by establishing a liaison committee to, hopefully, prevent any new misunderstandings, particularly over education and training. While the conference at The Hague succeeded in bringing a significant number of East Europeans, their
meeting, a significant effort was made to support Eastern Europeans who wished to attend the meeting, particularly by providing financial support. The first European board assessments were held in conjunction with the conference and the new education officer, Bernard Devauchelle, was officially invited to take part in the business of the Board. The executive committee held their first meeting in Midhurst (U.K.), combining this with an inspection of the office facilities which had become the organizational hub of the association (1995).
Christian Lindqvist was now the president (1998) and undertook the difficult task of taking the Scandinavian countries into the agreed common training program. It was at this time that the issue of representation on the IAOMS executive committee was raised. The difference in structure, particularly the fact that EACMFS members were there as individuals, plus the fact that the EACMFS did not have a mechanism for a national association to have membership, made the European association’s structure different from the established structure of IAOMS. However, in response to an invitation to send a representative to the executive committee, Hermann Sailer agreed to serve.
Also at this time, the journal’s editor-in-chief was facing an intolerable increase in workload. This provoked
“To facilitate communication and organization, the IAOMS decided to invite six geographic regions to represent their particular nations on the executive committee.”
a wide ranging discussion with the end result being a suggestion that sectional editors be appointed.
In his initial address to the executive committee as president, John Williams (2000) listed topics which he felt needed to be resolved by the association:
• h armonization of training;
• revalidation or reaccreditation of trained surgeons, which would be difficult to achieve in some of the major European countries, notably France and Germany;
• t he increased demand for accreditation of services, particularly from vociferous patient groups, but fueled by politicians across the EC; and
t he trainee membership and increasing difficulties in organizing any form of educational exchanges.
In addition, the financial state of the association had become critical as expenditure was exceeding income. Subscription rates had remained unchanged since formation of the association some 25 years earlier even as commitments continued to increase. During its period collecting membership dues, Churchill Livingstone had exposed a huge disparity between what was thought to be the membership (over 1,000) and what it really was in terms of who paid their dues (about 760). A new fees structure was approved at the Edinburgh meeting.
Increasing tension between the EACMFS, the IAOMS and AAOMS over the educational guidelines necessitated a second “summit” meeting which successfully resolved the differences once and for all (see chapter 4). The congress in Edinburgh was attended by more than 1,000 delegates and included a colorful opening ceremony where the dignitaries were led in by a piper in full regalia. The scientific meeting introduced early morning workshops aimed specifically at trainees.
This emphasis on trainees was continued by Ulrich Joos, the next president (2002), at his congress in Munster. The association was still in a quandary over educational guidelines, together with the thoughts of UEMS, the forthcoming IAOMS meeting in Durban and the need to present a position statement of European opinion on the issue. The lack of any increase in membership and the friction between the scientific role of the EACMFS and the political responsibilities also being asked of it resulted in further questions.
Following another successful congress, Bernard Devauchelle became president (2004) and was to organize


a conference in Tours. Irrespective of the ongoing financial situation, it was considered essential to support the development of an educational program in Iasi, Romania. The website, another financial priority, was now functional and provided enormous help to the educational program. The work that had been done over several years to establish a “Foundation” within EACMFS that would be particularly focused on education and training, was eventually brought to fruition in 2005. Despite being established as a scientific association, the political needs of Europe had been imposed on the membership and the latest was the “European Working Time Directive.” As it stood, it was unacceptable and interfered severely with training. This issue extended far beyond surgery and would take some years to resolve.
Guillermo Raspall became the new president in 2005 and as part of the process of resolution of the financial difficulties, was able to address the issue of the secretariat taking over collection of the membership dues. Political changes in the EU/UEMS workings were likely to have a significant effect on training because of a recently introduced “Bologna Agreement.” Just how this would affect OMFS training remained to be seen but a risk of the development of the specialty of oral surgery was concerning council. The executive committee, having worked on modification of the constitution, was supported by the general assembly who adopted all the amendments. This was an attempt at providing a mechanism of inclusiveness for all people in the specialty, irrespective of their qualifications.
Taking over the presidency in 2008, Luigi Clauser saw a desperate need to work closely with the European Commission on Harmonisation of Education and Training, which was chaired by Wolfgang Busch and covered extensively the evolving aspects of the specialty. The autumn of 2008 saw the sad and untimely death of John Lowry who had served the association both as assistant secretary and secretary general for ten years. Only the fourth person to hold this post since the inception of the association, he had been involved in many of its developments and was an absolute font of knowledge.
Following the Bologna congress, the presidency moved north again to Belgium and Maurice Mommaerts with Henri Thuau, acting as secretary general, before
being formally elected to the post. A résumé of training requirements across Europe demonstrated persisting great variation between nations, despite the attempts of the UEMS at achieving harmonization. The EACMFS was now working regularly with the UEMS through a series of joint committees. The meeting in charming Bruges was again a great success attended by a record number of colleagues. The presidency then moved to Mišo Virag, who will hold the next congress in 2012 in Dubrovnik, Croatia.
John WilliamsLatin America
Latin American Association of Oral and Maxillofacial Surgeons Asociacion Latino Americana de Cirugia y Traumatologia Buco Maxilo Facial

ALACIBU was established in 1962, in Bogota, Colombia, when an international group of Latin American oral surgeons and dentists with an interest in oral surgery met. It was decided that international congresses were to be held every three years and the location of the congress would alternate between the north and south of the Latin American continent in the following countries: Argentina, Bolivia, Brazil, Colombia, Costa Rica, Cuba, Chile, Ecuador, El Salvador, Guatemala, Haiti, Honduras, Mexico, Nicaragua, Panama, Paraguay, Peru, Dominican Republic, Uruguay and Venezuela.
The second meeting was held in Venezuela, in 1967, under the presidency of José Barros San Pasteur and the third in Buenos Aires, in 1970. The Buenos Aires congress was the first meeting attended by North American colleagues, among them Fred Henny, at that time a past president of the International Association of Oral Surgeons.
Subsequent meetings took place every three years in, respectively, Mexico (1973), Chile (1976), Honduras (1979), Brazil (1982) and Ecuador (1985). At these meetings, several well-known speakers from overseas and North America were invited to present the latest developments in oral and maxillofacial surgery.
A milestone in the history of ALACIBU occurred in 1985 when a formal document was signed between ALACIBU and AAOMS, together with CAOMS to promote cooperation in education and research in both North and South America. In this year, ALACIBU was also appointed as a member of the Latin American Dental Federation and it was decided to hold simultaneous scientific meetings. It is also of interest to note that at the general assembly in Ecuador, it was decided to improve the communication systems between the national associations so as to promote the professional exchange of ideas.
During the period 1985 and 1988, ALACIBU became involved in the infamous Tenerife and Bermuda conferences during which international guidelines on education and training were prepared. Several of Latin America’s most prominent members were invited to participate in this endeavor. These events had an enormous impact on the development of the specialty in this continent. One result was a seminar held in 1988 after the 9th scientific meeting in Uruguay, on the education and training of OMFS in Latin America. This seminar was held in Punta del Este and was preceded by a survey that was sent to all Latin American OMFS associations with the aim of learning each country’s current practice with regard to education and training. These preliminary discussions created a positive ambiance in which specialty leaders over the next 12 years were able to come up with a Latin American document on education and training.
At the meeting in Uruguay, it was also decided to establish a Latin American journal on oral and maxillofacial surgery. The first issue was published in 1989 with support from the Spanish society. Unfortunately, any further publications ceased due to a lack of funding.
At the next congress in Chile in 1991, the second seminar on education and training took place, at which the results about the scope of OMFS in Latin America were presented. It was agreed that the training in all Latin American countries would take a minimum of three full years. There were many European and North American colleagues present who gave their opinion under the leadership of former IAOMS president Robert Walker.
An important event for the specialty in Latin America took place in 1992 in Buenos Aires, the 11th ICOMS, held under the chairmanship of José Luis Ferreria. The conference was a huge success, not only because of the quality of the meeting but above all because it showed the involvement of South America in international affairs. The event also resulted in a boost for closer cooperation among Latin American associations, which was borne out at the next meeting in Cartagena, Columbia, in 1997, where new

regulations transformed ALACIBU from a society which organized scientific meetings every three years, to a true continental association with an executive committee.
As a result of those regulations, ALACIBU now has an executive committee, a council formed by all the national presidents and a general assembly. The president is now elected for a two-year period and each national association now pays a fee to ALACIBU for all their members. This means every OMFS, who is a member of his/her national association, is also a member of ALACIBU.
In 2000, in La Paz, Bolivia, a document on training and education for oral and maxillofacial surgeons in Latin America was finally approved by the general assembly. This document, based on the IAOMS education and training guidelines, was prepared in cooperation with AAOMS and CAOMS. At this meeting, a list of all registered oral and maxillofacial surgeons in Latin America was also presented. Former ALACIBU presidents Cesar Guerrero, Luis Quevedo and Eduardo Rey had all stressed education and training as their main objectives as president and this focus was borne out by the accomplishments of the 2000 general assembly.
The emphasis on education and training continued during the presidency of Edela Puricelli with a 2008 analysis of OMFS practice in Latin America and the proposal of a “core curriculum” in Foz de Iguazú in 2009.
In the period 2001–2011, further steps were taken to enhance professional standards in Latin America. These steps included the first IAOMS-sponsored educational course in Lima, Peru, which received generous assistance from AAOMS and SECOM and a second IAOMS educational program in Paraguay in 2009, the result of the successful course in Lima.
During the years 2003–2006, in addition to further improvements in the governance of ALACIBU, which required changes in the bylaws of the association, two important meetings took place in 2008 and 2009. The first “Latin American Forum on Professional Practice in OMF Surgery and Traumatology” occurred in 2008, under the auspices of the IAOMS and with the attendance of IAOMS president Nabil Samman and IAOMS educational committee chair, Julio Acero. The main purpose of this Forum was the selection of methodologies that would encourage the establishment of “Centers of Excellence” in Latin America and to enhance the training and education guidelines proposed by ALACIBU and the IAOMS.
At the second “Forum,” the focus was on a plan of action for the development of accreditation systems for OMFS training programs in Latin America, the adoption of common surgical protocols and favorable conditions for the establishment of guidelines that could be adopted as minimal curricular references in most Latin American
specialist training programs. Both meetings were attended by representatives of all of the Latin American national associations. At the second meeting, several invited guests from AAOMS shared their experiences in North America.
As of this book’s publishing date, ALACIBU had approved a Latin American Board to manage OMFS accreditation and certification policies.
In summary, ALACIBU has undergone a spectacular development in the last two decades and has progressed into a true professional organization in line with those on other continents.
Mario Scarrone and Edwin Valencia
North America
American Association of Oral and Maxillofacial Surgeons/ Canadian Association of Oral and Maxillofacial Surgeons

Oral and maxillofacial surgeons in the United States and Canada have always had a close collegial relationship. The training is virtually identical, as is the scope of practice. A large number of Canadian surgeons are members of the AAOMS and a significant number are American Board certified. Two joint association meetings have been held in Toronto. Therefore, when it was rumored that the IAOMS was going to regionalize, it was natural for the two associations to meet and discuss the formation of a North American association.
On September 19, 1996, a joint meeting was held at the Fontainebleau Hotel in Miami, Florida. Attending for the American association were John Helfrick, Daniel Laskin, and AAOMS staff member Barb Moles. The Canadian association was represented by Victor Moncarz and David Precious, with Moncarz serving as chair. Although invited, Dan Lew, Sam Kucey and Alva Swanson were unable to attend. The purpose of the meeting was to discuss the formation of an alliance between the AAOMS and CAOMS in order to form a regional affiliate of the IAOMS.
It was decided that all members of the AAOMS and CAOMS would comprise the membership of the North American Association. It was envisaged that there would be a board comprised of three members from each association and that the representative to the IAOMS executive committee would serve as chair of the board. The board would meet every other year, in the year in which there wasn’t an international conference (ICOMS). Because of the difference in size between the two associations, it was determined that the AAOMS would have a representative to the IAOMS for eight years and the CAOMS for two years in a ten-year cycle. Daniel Lew was appointed chair of the North American Association.

At the 1997 IAOMS meeting in Kyoto, the council approved the concept of regionalization of the association. Shortly after the meeting, Dan Lew stepped down from his position as North American Association chair and Kent Cohenour was appointed as the North American representative to the IAOMS executive committee. Kent Cohenour served in that position from 1998–2001. Don Booth was appointed as the representative in 2002 and
all states of Australia met and the society was conceived. Plans were put in place to develop a constitution, and it was agreed to meet in Perth in 1959, again concurrent with the next Australian Dental Congress. By then, New Zealand had joined and the first formal meeting was held under the presidency of Dr. Henderson. The executive consisted of the president, honorary secretary, treasurer and local councilor to run the association, with a broader council representing all states of Australia and New Zealand. The executive held office for two years and at the end of their term, a biennial scientific meeting was held and then affairs were passed on to the next executive.
IAOMS activities and international communication and cooperation has been facilitated by the regionalization. The AAOMS and CAOMS continue to support the concept of a North American regional association and of regional representation on the IAOMS executive committee.
John F. Helfrick and Dan LewOceania
Australia and New Zealand Association of Oral and Maxillofacial

Surgeons
Oral and maxillofacial surgery as it is known today did not exist in Australia and New Zealand in the first half of the 20th century. There were, however, several distinguished individuals working in isolation in their regional centers, either from a base in dentistry or from general surgery.
In both the first and second world wars, surgeons from Australasia made important contributions to the wartime reconstruction services in the United Kingdom. These include Percy Pickerill, Harold Gillies and Archibold McIndoe.
The first move to establish an Australian Society of Oral Surgeons occurred in Adelaide, concurrent with the Australian Dental Congress in 1957. Key individuals from

The honorary secretary was the key organizer for the association. The records were kept in cardboard boxes and one early secretary still vividly recalls receiving 20 cardboard boxes which were not marked or classified, at the start of his period of responsibility. The association’s affairs very much depended on the drive and enthusiasm, or sometimes lack of these skills, of the executive. Review of the records from those days show that there were recurrent themes: the membership and who was eligible; negotiation with state and federal governments in Australia and the national government in New Zealand as they all had different rules and regulations; the constitution and bylaws; helping members who got into professional difficulty and at times, prickly relations between dentistry and related medical specialties. The executive also had to arrange the scientific meetings and often more importantly, the social functions which went with the scientific meeting.
Membership decisions were always difficult in the early days as there was no agreed standard of training. Each dental school had its own master’s degree program which varied in length between one and three years. These were largely outpatient related and had variable research and coursework requirements. Graduates then commonly went to the United Kingdom for one or two years to obtain hospital experience and a United Kingdom fellowship. Some individuals went directly to the United Kingdom and bypassed any formal training and others obtained a medical degree. It was all very haphazard. In the early 1970s, an analysis of 23 consecutive successful applicants for membership showed that they had followed 22 different pathways of training which had taken between 1 and 22 years to complete and they ended up with one to six postgraduate qualifications!
Arising from this, the Australian and New Zealand Society of Oral Surgeons established an education committee of two young academicians, who subsequently became full professors, Frank Monsour of Brisbane and Alastair Goss of Adelaide. They presented a document entitled “Oral Surgery Training, A Plan for the 80s” to the 1979 ANZAOMS meeting in Sydney. The key steps
identified were a bi-national standardized curriculum, accreditation of training institutions and trainees, minimum requirements for the full scope as documented by log books and a national exit fellowship examination. A medical degree was not mandatory but considered desirable. The meeting presentation was fairly stormy and some dental school heads, who had not otherwise attended the national oral surgery conference, came in just for the afternoon to protect the independence of their school’s programs.
ANZAOMS supported the education committee’s initiatives and through the 1980s, the key steps were progressively put in place. Important educational courses besides the bi-annual scientific meetings were run under the chairmanship of Henk Tideman in Adelaide. He invited his European colleagues to update the profession in current maxillofacial surgery. These meetings were attended by about three quarters of the Australian and New Zealand membership and greatly broadened the horizons of members of the specialty.
At the end of the 1980s, the Australian and New Zealand Association of Oral and Maxillofacial Surgeons (ANZAOMS), as it became known, decided that the education and the examination components of the association would be better separated and put in the hands of the Royal Australasian College of Dental Surgeons. The College had established a diploma in oral surgery with the first examination held in 1973. Presentation to sit the exam was voluntary but many of the key leaders of the specialty presented for the searching examination, conducted under the chairmanship of John De Burg Norman.
In 1979 a section board in oral and maxillofacial surgery was established as part of the College under the chairmanship of Marsden Bell of New Zealand. The committee was largely comprised of heads of training units. This was supported by College representatives. This group had the drive, experience and authority to fully implement the training plans. Lateral entry into medical school for dental graduates training in oral and maxillofacial surgery was initiated in 1988 and lateral entry into dentistry for medical graduates was initiated in 1994. The academic teaching units, which are well embedded in each center’s major hospitals, covered the full scope of the specialty, including trauma, oncology and maxillofacial reconstruction.
Today, there is a fully functioning Board of Oral and Maxillofacial Surgery which sets the course and curriculum, accredits training units, selects advanced trainees and monitors their progress.
ANZAOMS has developed parallel to the College Board for all other aspects of oral and maxillofacial surgery. It has its own chief executive officer and a secretariat, thus the post of honorary secretary is no longer required.
The executive does not rotate through Australia and New Zealand but meets centrally and the officers are elected on merit. The research arm of the specialty was established in 1990 as the Australian and New Zealand Association of Oral and Maxillofacial Surgery Research and Education Foundation. This Foundation has established substantial funds from the membership and trade.

One of its first investments was to finance a series of workforce studies. The detailed information from this has greatly aided planning of the Board of Oral and Maxillofacial Surgery of the College and ANZAOMS. It has been an invaluable factual base to negotiate with government’s educational and funding bodies. Oral and maxillofacial surgery services are provided mainly in a private practice setting in which dentoalveolar surgery predominates but they also cover trauma, pathology, orthognathic surgery and implantology. Thus, in Australia and New Zealand today there is a strong specialty of oral and maxillofacial surgery which is well organized and comfortably meets as an equal with related surgical specialties and the medical and dental professions.
The Australian and New Zealand Association of Oral and Maxillofacial Surgeons were founding members of the international association. Marsden Bell of New Zealand was at the first meeting in London in 1962 and then attended every meeting of the international association until the Vienna meeting in 2003. He also served on the board of the IAOMS Foundation from 2000 until 2005, being chairman from 2001 until 2005.
7th Clinical meeting of ANZAOMS. Front row from left to right: Cliff Black, Jan Donaldsen, Bill MacKenzie, Sandy MacAlister (IAOMS president), Bruce Lindsay (ANZAOMS president), Paul Bramley (BAOMS president), Frank Helmore, Bob Cook, Berry Fitzpatrick, Paul Swinburn.

Australia and New Zealand has had two IAOMS presidents, Alton “Sandy” MacAlister of New Zealand and Robert Cook of Melbourne. David Poswillo, a New Zealander sometimes based in Australia but mainly in the United Kingdom, was the secretary general of the IAOMS in the days when the secretary was the key organizer. Alastair Goss was a long-serving member and chair of the education committee, as well as the first Oceania regional representative on the executive committee. He was followed by John Curtin and then Paul Sambrook.
In the mid-1990s representatives of regional associations were invited to join the executive committee of the IAOMS. These were North and South America, Europe and Asia. Australia and New Zealand were considered part of Asia, but as Oceania is a recognized continental grouping, it was later recognized as the 5th region. It is the second largest by area but the least populated. The dominant, well developed countries are Australia and New Zealand with the remaining over 40 countries being spread throughout the Pacific. These nations are all small, developing countries. Dental training can be achieved in some instances either in Australia or New Zealand or at the more recently developed regional dental schools at the University of the South Pacific in Fiji and at the University of Papua New Guinea in Port Moresby.
Australia and New Zealand have long been involved in providing aid at all levels within Oceania. The first formal major commitment of Australia and New Zealand to the development of health services was outside its region in Bangladesh. A full course in oral and maxillofacial surgery was set up under Australian mentorship and a number of senior Bangladeshi trainees spent time furthering their training on rotation through Australian schools.
Numerous education missions have been made to the Philippines, Indonesia, Fiji, Tonga, Samoa, East Timor and the Solomon Islands. Two courses for the Pacific region surgeons have been conducted under the auspices of the IAOMS and the leadership of John Curtin.
There remains much work to be done but the commitment of Australia and New Zealand to this important work in Oceania is in place and will continue.
The progress of the specialty has been based on the work of many but a few whose names are featured in this report were often stimulated by external competition from related surgical specialties and made giant steps. It’s in the hands of the new well trained young surgeons to take things further.
Alastair GossAlbania
Albanian Association of Oral and Maxillofacial Surgeons
Date Established 1993 Date Affiliated with the IAOMS 1995 Number of Members 70
Argentina
Sociedad Argentiana de Cirugia y Traumatologia Bucomaxillofacial
Date Established 1958 Date Affiliated with the IAOMS .......... 1971 Number of Members ............................ 50 0
Australia
Australian & New Zealand Association of Oral and Maxillofacial Surgeons (ANZAOMS)
Date Established 1957 Date Affiliated with the IAOMS 19 63 Number of Members 20 0
Austria
Austrian Association for Cranio-Maxillofacial Surgery
Date Established 1967 Date Affiliated with the IAOMS ......... 1990 Number of Members ............................. 184
Azerbaijan Republic
Azerbaijan Republic Association of Oral and Maxillofacial Surgeons
Date Established N/R Date Affiliated with the IAOMS 1998 Number of Members N/R
Bangladesh
Bangladesh Association of Oral and Maxillofacial Surgeons
Date Established 1993 Date Affiliated with the IAOMS 1997 Number of Members ............................. 125
Belarus
Belarus Association of Oral and Maxillofacial Surgery
Date Established N/R Date Affiliated with the IAOMS 1996 Number of Members N/R
Belgium
Societe Royale Belge de Stomatologie et Chirurgie Maxillofaciale
Date Established 19 00 Date Affiliated with the IAOMS 19 89 Number of Members ............................. 250
Bolivia
Sociedad Boliviana de Cirugia Bucomaxilofacial Date Established 19 69 Date Affiliated with the IAOMS 1993 Number of Members 25
Brazil
Colegio Brasileiro de Cirurgia e Traumatologia Buco-Maxilo-Facial
Date Established 1970 Date Affiliated with the IAOMS .......... 1971 Number of Members ......................... 1, 400
Bulgaria
Society of Oral and Maxillofacial Surgeons in Bulgaria
Date Established 20 09 Date Affiliated with the IAOMS 2011 Number of Members 60
Canada
Canadian Association of Oral & Maxillofacial Surgeons
Date Established 1953 Date Affiliated with the IAOMS 19 68 Number of Members ............................ 30 0
Chile
Sociedad De Cirugia y Traumatologia Bucal y Maxillofacial de Chile
Date Established 1950 Date Affiliated with the IAOMS 1991 Number of Members 20 0
Colombia
Asociacion Colombiana de Cirugia Oral y Maxilofacial Date Established 1958 Date Affiliated with the IAOMS 1993 Number of Members 30 6
Costa Rica
Costa Rica Asociacion Costarricense de Cirurgia Oral y Maxilofacial
Date Established 20 03 Date Affiliated with the IAOMS 20 06 Number of Members 19
Croatia
Croatian Society of Maxillofacial, Plastic & Reconstructive Head & Neck Surgery
Date Established 1954 Date Affiliated with the IAOMS 20 04 Number of Members ............................... 57
the affiliated national oral and maxillofacial Surgeon a S S o ciation S (continued)
Cuba
Sociedad Cubana De Cirugia Maxillofacial Date Established N/R Date Affiliated with the IAOMS 19 68 Number of Members N/R
Czech Republic
Czech Association of Maxillo-Facial Surgery Date Established N/A Date Affiliated with the IAOMS 1995 Number of Members 10 5
Denmark
Danish Association of Oral and Maxillofacial Surgeons
Date Established 1953 Date Affiliated with the IAOMS .......... 1993* Number of Members ............................... 45
Dominican Republic
Sociedad Dominicana de Cirugia Bucal Maxilo-Facial Date Established ................................... N/R Date Affiliated with the IAOMS 1993 Number of Members N/R
East Africa
Eastern African Association of Oral & Maxillofacial Surgeons
Date Established 20 02 Date Affiliated with the IAOMS 20 03 Number of Members 35
Ecuador
Asociacion Ecuatoriana De Cirugia y Traumatologia Oral y Maxilofacial Date Established 19 85 Date Affiliated with the IAOMS 20 03 Number of Members ...............................30
Egypt
Egypt Association of Oral & Maxillofacial Surgeons
Date Established .................................2000 Date Affiliated with the IAOMS ......... 2001 Number of Members 10 0
Estonia
Estonian Association of Oral and Maxillofacial Surgeons
Date Established 1992 Date Affiliated with the IAOMS 1996 Number of Members 23
Finland
Finnish Association of Oral and Maxillo-Facial Surgeons
Date Established 19 66 Date Affiliated with the IAOMS 1994* Number of Members 164
France
Societe Francaise De Stomatologie et Chirurgie Maxillo-Faciale
Date Established 1953 Date Affiliated with the IAOMS .......... 19 65 Number of Members ......................... 1, 200
Georgia, Republic of Georgian Association of Maxillofacial Surgery
Date Established .................................. 1991 Date Affiliated with the IAOMS 1997 Number of Members 30
Germany
Deutsche Gesellschaft fur Mund-Kieferund Gesichtschirurgie Date Established 1951 Date Affiliated with the IAOMS 1992 Number of Members 1,110
Germany
Arbeitsgemeinschaft fur Kieferchirurgie Date Established 1935 Date Affiliated with the IAOMS 1977
Ghana
Ghana Association of Oral and Maxillofacial Surgeons Date Established ................................. 20 08 Date Affiliated with the IAOMS ......... 20 09 Number of Members ............................... 12
Greece
Hellenic Association for Oral and Maxillofacial Surgery Date Established 1959 Date Affiliated with the IAOMS 1977 Number of Members 20 0
Hong Kong
Hong Kong Association of Oral and Maxillofacial Surgeons
Date Established 1990 Date Affiliated with the IAOMS 1993 Number of Members 48
*First became affiliated through the Scandinavian Association. Countries involved were Denmark, Finland, Iceland, Norway and Sweden. N/R — Not received
Hungary
Hungarian Association of Oral and Maxillofacial Surgeons
Date Established 1971 Date Affiliated with the IAOMS 1974 Number of Members 20 0 (150 of whom are oral surgeons)
India
Association of Oral and Maxillofacial Surgeons of India
Date Established 19 69 Date Affiliated with the IAOMS 1977 Number of Members .......................... 1,300
Indonesia
Indonesian Association of Oral and Maxillofacial Surgeons Date Established .................................. 1973 Date Affiliated with the IAOMS .......... 19 83 Number of Members 30 0
Iran
Iranian Society of Oral and Maxillofacial Surgeons
Date Established N/R Date Affiliated with the IAOMS 19 83 Number of Members N/R
Ireland
Irish Association of Oral and Maxillofacial Surgery Date Established 19 80 Date Affiliated with the IAOMS 19 89 Number of Members 21
Israel
Israeli Association of Oral and Maxillofacial Surgery
Date Established 19 64 Date Affiliated with the IAOMS 19 65 Number of Members ............................... 85
Italy
Societa Italiana Chirurgia Maxillo-Facciale
Date Established .................................. 19 89
Date Affiliated with the IAOMS ......... 20 02 Number of Members 30 9
Japan
Japanese Society of Oral and Maxillofacial Surgeons
Date Established 1933 Date Affiliated with the IAOMS 1977 Number of Members 1,755
Kazakhstan, Republic of Association of Oral and Maxillofacial Surgery of Republic Kazakhstan
Date Established N/R Date Affiliated with the IAOMS 1997 Number of Members N/R
Korea, Republic of Korean Association of Oral and Maxillofacial Surgeons Date Established 1959 Date Affiliated with the IAOMS .......... 19 89 Number of Members ............................. 750
Latvia
Latvian Association of Oral and Maxillofacial Surgeons Date Established .................................. 1995 Date Affiliated with the IAOMS 1995 Number of Members 35
Lithuania
Lithuanian Association of Maxillofacial Surgeons Date Established 1995 Date Affiliated with the IAOMS 1995 Number of Members 49 (20 of whom are oral surgeons)
Malaysia
Maylasian Association of Oral & Maxillofacial Surgeons Date Established 1996 Date Affiliated with the IAOMS 1998 Number of Members ............................. 120
Mexico
Asociacion Mexicana de Cirugia Bucal y Maxilofacial A.C. Date Established .................................. 1956 Date Affiliated with the IAOMS .......... 1974 Number of Members 150 (there are 600 OMFS in Mexico)
Moldova, Republic of Association of Cranio Maxillo-Facial Surgeons of Republic of Moldova
Date Established N/R Date Affiliated with the IAOMS 1995 Number of Members N/R
the affiliated national oral and maxillofacial Surgeon a S S o ciation S (continued)
Mongolia
Mongolian Association of Oral and Maxillofacial Surgeons
Date Established 1998 Date Affiliated with the IAOMS 20 09 Number of Members 85
The Netherlands
Nederlandse Vereniging voor Mondziekten Kaak-en Aangezichtschirurgie
Date Established 1956 Date Affiliated with the IAOMS 19 65 Number of Members .............................203
Nigeria
Nigerian Association of Oral and Maxillofacial Surgeons
Date Established .................................. 1993 Date Affiliated with the IAOMS .......... 1995 Number of Members 75
Norway
Norwegian Association of Oral Surgeons Date Established 1952 Date Affiliated with the IAOMS 1995* Number of Members 89
Pakistan
Pakistan Association of Oral & Maxillofacial Surgeons
Date Established 1994 Date Affiliated with the IAOMS 20 03 Number of Members 70
Panama, Republic of Panamanian Association of Oral and Maxillofacial Surgery
Date Established N/R Date Affiliated with the IAOMS 1997 Number of Members ............................ N/R
Paraguay
Sociedad Paraguaya de Cirugia Buco Maxilofacial Date Established .................................. 1958 Date Affiliated with the IAOMS ......... 2001 Number of Members N/R
People’s Republic of China
Chinese Society of Oral and Maxillofacial Surgery
Date Established 19 86 Date Affiliated with the IAOMS 1999 Number of Members 1,000
Peru
Asociacion Peruana de Medicina Estomatologica y Cirugia Bucomaxilofacial Date Established 1976 Date Affiliated with the IAOMS 20 03 Number of Members 70
Philippines
Philippine College of Oral and Maxillofacial Surgeons Date Established 19 60 Date Affiliated with the IAOMS 1977 Number of Members .............................. 40
Poland
Polish Society for Oral & Maxillofacial Surgery Date Established ................................... N/R Date Affiliated with the IAOMS .......... 1995 Number of Members 1,100 (800 of whom are oral surgeons)
Portugal
Associacao Portuguesa de Cirurgia Craniomaxilofacial Date Established N/R Date Affiliated with the IAOMS 20 03 Number of Members N/R
Romania
Societatea Romana de Ctururgie Orala of Maxilo Faciara Date Established 1991 Date Affiliated with the IAOMS 1995 Number of Members 260 (20 of whom are oral surgeons)
Serbia
Serbian Association of Maxillofacial Surgeons Date Established .................................. 19 65 Date Affiliated with the IAOMS .......... 2011 Number of Members 8 0
Seychelles
Maxillofacial Surgeons Association of Seychelles Date Established 2010 Date Affiliated with the IAOMS 2011 Number of Members 11
*First became affiliated through the Scandinavian Association. Countries involved were Denmark, Finland, Iceland, Norway and Sweden. N/R — Not received
Singapore, Republic of Singapore Association of Oral and Maxillofacial Surgeons
Date Established 1992 Date Affiliated with the IAOMS 1994 Number of Members 57
Slovakia
Slovak Association of the Oral and Maxillofacial Surgery Date Established 1988 Date Affiliated with the IAOMS 1995 Number of Members 59
Slovenia
Slovenian Society for Maxillofacial & Oral Surgery Date Established ................................. 1996 Date Affiliated with the IAOMS ......... 20 02 Number of Members 37 (20 of whom are oral surgeons)
South Africa
South African Society of Maxillofacial and Oral Surgeons Date Established 19 64 Date Affiliated with the IAOMS 1977 Number of Members 10 0
Spain
Sociedad Espanola de Cirugia Oral y Maxilofacial Date Established 19 65 Date Affiliated with the IAOMS 1967 Number of Members 7 35
Sri Lanka
Sri Lanka Association of Oral and Maxillofacial Surgeons Date Established 1998 Date Affiliated with the IAOMS .......... 1998 Number of Members .............................. 40
Sweden
Swedish Association of Oral and Maxillofacial Surgeons
Date Established .................................. 1953 Date Affiliated with the IAOMS 1993* Number of Members 150
Switzerland
Swiss Association of Maxillofacial Surgery Date Established N/R
Date Affiliated with the IAOMS 1994 Number of Members 63
Taiwan
Chinese-Taipei Association of Oral and Maxillofacial Surgeons Date Established 19 86 Date Affiliated with the IAOMS 1991 Number of Members 270
Thailand
Thai Association of Oral and Maxillofacial Surgery Date Established 1990 Date Affiliated with the IAOMS .......... 1997 Number of Members ............................ 20 0
Turkey
Turkish Association of Oral and Maxillofacial Surgery Date Established .................................. 19 85 Date Affiliated with the IAOMS 1990 Number of Members 10 0
Ukraine
Ukrainian Association of Cranio-Maxillofacial Surgery Date Established N/R Date Affiliated with the IAOMS 19 85 Number of Members N/R
United Kingdom
British Association of Oral and Maxillofacial Surgeons Date Established 19 62 Date Affiliated with the IAOMS 19 65 Number of Members 50 0
United States of America
American Association of Oral and Maxillofacial Surgeons Date Established .................................. 1918 Date Affiliated with the IAOMS .......... 19 65 Number of Members .......................... 7,929
Uruguay
Sociedad Uruguaya de Cirugia Buco Maxilo Facial Date Established 1955 Date Affiliated with the IAOMS 1990 Number of Members 35
Venezuela
Sociedad Venezolana de Cirugia Buco-Maxilofacial
Date Established 1957 Date Affiliated with the IAOMS 1974 Number of Members 265
1965 Spain, Argentina 1967 Canada, Cuba 1968 Brazil 1971 Hungary, Ireland, Mexico, Venezuela
Australia, France, Israel, The Netherlands, New Zealand, Scandinavia, United Kingdom, U.S.A.
1974 Germany — AGK, Greece, India, Japan, Philippines, South Africa
1977 Belgium 1980 Indondesia, Iran 1983 Republic of Korea 1989 Austria 1990 Taiwan, Chile 1991 Germany —DGMKG 1992
1993
Bolivia, Colombia, Dominican Republic, Hong Kong, Sweden*, Denmark*
Finland*, Republic of Singapore, Switzerland 1994
1995
Albania, Czech Republic, Latvia, Lithuania, Republic of Moldova, Nigeria, Norway*, Poland, Romania, Slovakia, Ukraine, Belarus, Estonia
1997
Bangladesh, Republic of Georgia, Republic of Kazakhstan, Republic of Panama, Thailand
1998 People’s Republic of China 1999 Egypt, Paraguay 2001 Italy, Slovenia 2002 East Africa, Ecuador, Peru, Portugal
Republic of Azerbaijan, Malaysia, Sri Lanka
2003 Croatia 2004 Ghana, Mongolia 2009 Bulgaria, Serbia, Seychelles 2011 *First became affiliated through the Scandinavian Association. Countries involved were Denmark, Finland, Iceland, Norway and Sweden.
Fred Henny U.S.A.

1962–1968 Netherlands 1977–1980
United Kingdom 1968–1971
Jørgen Rud Denmark 1971–1974





Alton D. MacAlister New Zealand 1974–1977



1989–1992
Geoffrey L. Howe Hong Kong 1980–1983



U.S.A. 1983–1986
1992–1995
Austria 1995–1997
Peter Banks United Kingdom 1997–1999
1999–2001
Netherlands 2001–2003
2003–2005
John Ll. Williams United Kingdom 2005–2007


Nabil Samman Hong Kong 2007–2009

Larry W. Nissen U.S.A. 2010–2011


Kishore Nayak India 2012–2013


Honorary Fellows*
Fred A. Henry
U.S.A., 1968
Fred Henny served as the Chairman of the Organizing Committee in the United States for that first historic conference in 1962. He served on the initial Executive Committee as its Chairman from 1962–1965 and then was President from 1965–1968.

His Royal Highness
Prince Bernhard The Netherlands, 1971

Prince Bernhard welcomed delegates to the 4th ICOS in 1971 and accepted Honorary Fellowship of the IAOS.
Terence G. Ward
United Kingdom, 1974
Terence Ward appointed to the first Executive Committee in 1964, served as Secretary-General from 1962–1968 and President from 1968–1971. He continued to serve on the Executive Committee as Past-President from 1974–1977.


His Majesty King Juan Carlos Spain, 1974

Prince Juan Carlos accepted Honorary Fellowship of the IAOMS in 1974 for his role in welcoming delegates to the 5th ICOS in Madrid.
Patrick J. Hillary
President of the Republic of Ireland, 1980
Patrick J. Hillary, was elected an Honorary Fellow in 1980 for his role in opening the 6th ICOS in Dublin.
Jørgen Rud


Denmark, 1980
Jørgen Rud was chairman of the 2nd ICOS Organizing Committee. In 1971, he took over as President, serving in that role until 1974 when he took on a six-year term as Secretary-General.

Bill van der Kwast
The Netherlands, 1986
Bill van der Kwast was Chairman of the 4th ICOS in Amsterdam and served on the IAOMS Executive Committee from 1971–1983, including holding the offices of President from 1977–1980 and Secretary-General from 1980–1983.
Norman Rowe
United Kingdom, 1986
During the years when Terence Ward was President of IAOMS, Norman L. Rowe fulfilled the role of Secretary-General (1968–1971). He also served on the Executive Committee from 1971–1977. He also received his award because of his professional stature.
Gerald H. Leatherman
United Kingdom, 1986
Gerald Leatherman was the Honorary Secretary General of the Federation Dentaire Internationale. He organized a dinner in London between Fred Henny and Lyall Bishop and leading British oral surgeons. He was a member of the first Organizing Committee.

David E. Poswillo
United Kingdom, 1992
David E. Poswillo began his long service with the IAOMS as a member of the Executive Committee from 1980–1983. He served as Secretary-General from 1983–1989.

Bernard Degen U.S.A., 1992
Bernie Degen was instrumental in developing international unity within the profession through education, organization and mutual understanding.
Robert V. Walker U.S.A., 1992
Bob Walker began serving on the IAOMS Executive Committee in 1986 and was elected President for the 1989–1992 term. He also was recognized as a pillar of the profession. The 20th ICOMS in Santiago was dedicated in his honor.

Daniel M. Laskin U.S.A., 1995
Daniel Laskin served on the Executive Committee from 1980–1983, as President from 1983–1986, Past President from 1986–1989 and then executive director from 1992–1999.


Distinguished Fellows*
Robert M. Cook Australia, 1999
Robert Cook was a member of the Executive Committee from 1986–1992 when he took over as President, serving until 1995. He then went on to serve as inaugural Chairman of the newly formed IAOMS Foundation, holding that position from 1995–2001.



Rudolph Fries Austria, 2001
Rudi Fries was Vice President from 1992–1995, President from 1995–1997. Past President from 1997–1999. He was particularly recognized for his tireless efforts in involving the eastern European countries and less developed nations in Asia and Africa. The 17th ICOMS in Vienna was dedicated in his honor.



Wilfried Schilli Germany, 2005
Wilfried Schilli served as Chairman of the organizing committee of the 8th ICOMS in Berlin; Vice President of the IAOMS from 1983–1986; President from 1986–1989 and Past-President from 1989–1992. He was particularly recognized for his unstinting attempts at unifying maxillofacial surgery education and training worldwide.
Paul J.W. Stoelinga
The Netherlands, 2007
Paul Stoelinga has had a long, distinguished career as a leader within the profession. He served as Editor-in-Chief of the International Journal of Oral and Maxillofacial Surgery from 1988–2000; PresidentElect from 1999–2001; President from 2001–2003; Past President from 2003–2005 during which he also became Chairman of the Foundation from 2003–2007.
György Szabó Hungary, 2007
György Szabó was chair of the organizing committee of the 12th ICOMS in Budapest. He also was a close link between the east European countries and IAOMS during the difficult Soviet period.
Qiu Wei-Liu People’s Republic of China, 2009
Qiu Wei-Liu was the chairman of the organizing committee of the 19th ICOMS in Shanghai. He is also recognized as the promoter of Chinese involvement in the international association.

John Helfrick U.S.A., 2011
John Helfrick was recognized for his distinguished service to the specialty internationally. Throughout his career he was in the forefront of IAOMS leadership serving as President-Elect from 1997–1999 and as President from 1999–2001. In 2003 he assumed the position of IAOMS Executive Director, serving in that post until 2011.
Distinguished Service Award
Andrew Linz
U.S.A., 1999
Honored for his service on the Executive Committee from 1977–1980. He was instrumental in developing a draft of the constitution and bylaws of the IAOMS Foundation.

Marsden Ball
New Zealand, 2001
Honored for his service as Vice Chairman of the inaugural Board of Trustees of the Foundation, subsequently serving as the Chairman during 2001.
John Frame


United Kingdom, 2003
Recognized for his service as the IAOMS Newsletter Editor from 1989–1999.
Piet Haers
United Kingdom, 2001
Recognized for his dedication and achievement in improving the scientific caliber of the International Journal of Oral and Maxillofacial Surger y, the official scientific publication of the IAOMS.
Donald F. Booth
U.S.A., 2009
Honored for his Board service in several important roles. Don Booth joined the Executive Committee in 2001 and served as Treasurer from 2003–2009. Under his leadership as treasurer, a sound financial basis for the association’s activities was established. He also received a Presidential Citation in 2009.

Nabil Samman
Hong Kong, 2011
Recognized for his service to the IAOMS in his role of organizing and overseeing the Fellowship programs in cleft/craniofacial and oncology reconstruction during their first two years. Professor Samman also helped secure funding for the Fellowship positions from corporate sponsors through the IAOMS Foundation. He also served as President-Elect, President and Past President.


i a o m S a w a r d r e c i p i e n t S (continue d)
Outstanding Committee Member Award
Patrick Magennis Unit e d Kingdom, 20 01
Re cognize d for his involvement in the development of a memb ership database
l Samman g Kong , 20 05 re d for his work and tion to the Education mmit te e
le Milesi , 20 05 nize d for her out standing utions to the 17 th ICOMS and her ser vice as 20 0 6 –20 0 8 Sp e cial Task Force Chair

Julio Acero


Sp ain, 20 0 9
Re cognize d for his out standing p er formance as Chair of the Education Commit te e during the p eriod 20 0 5–2011

Donald F. Booth
U S A , 2011
Re cognize d for his e xcellent p er formance as Chair of the Humanitarian Aid and Disaster Relief (HADR) Commit te e
Donald F. Booth U S A , 20 0 9
Provided ser vice above and beyond that ordinarily e xp e c te d of a Fellow as Treasurer of IAOMS.

Presidential Lecturers at ICOMS
Herman Sailer

Switzer land, 1995
“Biome dical te chnolog y revolution: oppor tunities and challenges for oral and ma xillof acial surgeons”
David Vaughan
Unit e d Kingdom, 1999
“Changing trends in the surgical management of head and ne ck cancer ”
e onard Bruce Kaban S A , 20 01
iome dical te chnolog y revolution: ppor tunities and challenges for ral and ma xillof acial surgeons”

Henk Tideman



Hong Kong , 20 03
“ Vita Brevis ES T, Longa ARS — Life is shor t , the ar t is long (Hippocrat es)”
Michael Cohen, Jr. Canad a, 20 05

“Some disorders of bone”
James Johnson
Unit e d Kingdom, 20 07
“Are Health Systems Converging Towards a World Health Polic y? ”
Ghali E . Ghali
U S A , 20 0 9
“Evolution, current status and future of oral and ma xillof acial surger y ”

Jay Malmquist

U S A , 2011
“Education, research, te chnolog y, innovation: the Foundation of an e xceptional sp e cialt y? A look at the past , present and future of an evolution”
1962 1963–1965 1965–1968
1st International Conference on Oral Surgery Royal College of Surgeons, London July 1–5, 1962



• Fred Henny (U.S.A.), Chairman
• Lyall Bishop (U.S.A)
• Pierre Cernea (France)
• Jørgen Rud (Denmark)
• Terence G. Ward (United Kingdom), Secretary-General
2nd International Conference on Oral Surgery Copenhagen, Denmark June 19–24, 1965
• Fred Henny (U.S.A.), Chairman
• Lyall Bishop (U.S.A.)
• Pierre Cernea (France)
• Jørgen Rud (Denmark), Chairman II ICOS Organizing Committee
• Terence G. Ward (United Kingdom), Secretary-General
• Fred Henny (U.S.A.), President
• Lyall Bishop (U.S.A.)
• Pierre Cernea (France)
• Jørgen Rud (Denmark)
• Terence G. Ward (United Kingdom), Secretary
1968–1971
4th International Conference on Oral Surgery Amsterdam, The Netherlands May 17–21, 1971
• Terence G. Ward (United Kingdom), President
• Lyall O. Bishop (U.S.A.)
• Pierre Cernea (France)
• Jørgen Rud (Denmark)
• W. A. M. van der Kwast (Netherlands), Chairman, IV ICOS Organizing Committee
• Fred A. Henny (U.S.A.), Past President
• Norman L. Rowe (United Kingdom), Secretary-General
1971–1974 1974–1977
5th International Conference on Oral Surgery Madrid, Spain April 21–25, 1974

• Jørgen Rud (Denmark), President
• Lyall O. Bishop (U.S.A.)
• W. A. M. van der Kwast (Netherlands)
• Norman L. Rowe (United Kingdom)
• Victor Sada (Spain), Chairman, V ICOS Organizing Committee
• Terence G. Ward (United Kingdom), Secretary-General
6th International Conference on Oral Surgery Sydney, Australia July 1–5, 1977


• A . D. MacAlister (New Zealand), President
• W. A. M. van der Kwast (Netherlands)
• Norman L. Rowe (United Kingdom)
• Victor Sada (Spain)
• Andrew M. Linz (U.S.A.)
• G. Buchanan (Australia), Chairman, VI ICOS Organizing Committee
• Terence G. Ward (United Kingdom), Past President
• Jørgen Rud (Denmark), Secretary-General
1977–1980 1980–1983
7th International Conference on Oral Surgery Dublin, Ireland June 23–26, 1980


• W. A. M. van der Kwast (Netherlands), President
• Geoffrey L. Howe (United Kingdom, Hong Kong), Vice President beginning 1978
• Andrew M. Linz (U.S.A.)
• Victor Sada (Spain)
• Wilfried G. Schilli (W. Germany)
• Ian A. Findlay (Ireland), Chairman, VII ICOS Organizing Committee
• A . D. MacAlister (New Zealand), Past President
• Jørgen Rud (Denmark), Secretary-General
1983–1986
8th International Conference on Oral Surgery West Berlin, Germany July 25–30, 1983

• Geoffrey L. Howe (Hong Kong), President
• F. Gordon Hardiman (United Kingdom), Vice President
• David E. Poswillo (United Kingdom)
• David Gutman (Israel)
• Jean-Marie Vaillant (France)
• Daniel M. Laskin (U.S.A.)
• Basilio Arienza (Argentina)
• Wilfried G. Schilli (West Germany), Chairman, VIII ICOS Organizing Committee
• W. A. M. van der Kwast (Netherlands), Secretary-General
• Daniel M. Laskin (U.S.A), President
• Wilfried G. Schilli (West Germany), Vice President
• David E. Poswillo (United Kingdom), Secretary-General
• Basilio Arienza (Argentina)
• David Gutman (Israel)
• Jean-Marie Vaillant (France)
• Geoffrey L. Howe (United Kingdom), Past President
• Alva E. Swanson (Canada), Chairman, IX ICOMS Organizing Committee
1986–1989
10th International Conference on Oral and Maxillofacial Surgery Jerusalem, Israel May 21–26, 1989

• Wilfried G. Schilli (West Germany), President
• David Gutman (Israel), Vice President
• David E. Poswillo (United Kingdom), Secretary-General
• Robert M. Cook (Australia)
• Enrique F. Muller (Argentina)
• Robert V. Walker (U.S.A.)
• Daniel M. Laskin (U.S.A.), Past President
• E. Rorien (Israel), Chairman, X ICOMS Organizing Committee
• Paul J.W. Stoelinga (Netherlands), Editor-in-Chief, IJOMS
11th International Conference on Oral and Maxillofacial Surgery Buenos Aires, Argentina August 8–12, 1992


• Robert V. Walker (U.S.A.), President
• Enrique E. Muller (Argentina), Vice President
• Daniel M. Laskin (U.S.A.), Secretary-General
• Robert M. Cook (Australia)
• H. Dieter Pape (West Germany)
• Wataru Yoshioka (Japan)
• Wilfried G. Schilli (West Germany), Past President
• José Luis Ferreria (Argentina), Chairman XI ICOMS Organizing Committee
• Paul J.W. Stoelinga (Netherlands), Editor-in-Chief, IJOMS
• John W. Frame (United Kingdom), Editor, Newsletter
• Robert M. Cook (Australia), President
• Rudolf Fries (Austria), Vice President
• Daniel M. Laskin (U.S.A.), Secretary-General
• Pe ter Banks (United Kingdom)
• H. Dieter Pape (West Germany)
• Wataru Yoshioka (Japan)
• José Luis Ferreria (Argentina)
• Robert V. Walker (U.S.A.), Past President
• György Szabó (Hungary), Chairman, XII ICOMS Organizing Committee
• Paul J.W. Stoelinga (Netherlands), Editor-in-Chief, IJOMS
• John W. Frame (United Kingdom), Editor, Newsletter
1995–1997
13th International Conference on Oral and Maxillofacial Surgery Kyoto, Japan October 20–24, 1997

• Rudolf Fries (Austria), President
• Pe ter Banks (United Kingdom), Vice President
• John F. Helfrick (U.S.A.), Secretary-General
• Robert M. Cook (Australia), Past President
• José Luis Ferreria (Argentina)
• Daniel Lew (U.S.A.)
• Victor Moncarz (Canada)
• Daniel M. Laskin (U.S.A.), Executive Director
• Kanichi Seto (Japan), Chairman, XIII ICOMS Organizing Committee
• Paul J.W. Stoelinga (Netherlands), Editor-in-Chief, IJOMS
• John W. Frame (United Kingdom), Editor, Newsletter
• Alastair Norman Goss (Australia), Chairman, Education Committee
• John P. Kelly (U.S.A.), Chairman, Scientific Committee
• Conrad Masureik (South Africa), Chairman, Membership Committee
• Robert M. Cook (Australia), Foundation Chairman
1997–1999
14th International Conference on Oral and Maxillofacial Surgery Washington, D.C., U.S.A. April 24–29, 1999

• Pe ter Banks (United Kingdom), President
• John F. Helfrick (U.S.A.), President-Elect
• Rudolf Fries (Austria), Past-President
• Luis R. Quevedo (Chile)
• José Luis Ferreria (Argentina)
• Victor Moncarz (Canada)
• Kanichi Seto (Japan)
• Herman F. Sailer (Switzerland)
• Kent Cohenour (U.S.A.)
• Anders Bo Holmlund (Sweden)
• Robert M. Cook (Australia), Foundation Chairman
• John W. Frame (United Kingdom), Editor, Newsletter
• Paul J.W. Stoelinga (Netherlands), Editor-in-Chief, IJOMS
• Daniel M. Laskin (U.S.A.), Executive Director; Chairman, XIV ICOMS
• Alastair Norman Goss (Australia), Chairman, Education Committee
15th International Conference on Oral and Maxillofacial Surgery
Durban, South Africa May 19–24, 2001
• John F. Helfrick (U.S.A.), President
• Paul J.W. Stoelinga (Netherlands), President-Elect
• Pe ter Banks (United Kingdom), Past-President
• Victor Moncarz (Canada), Executive Director
• Alexis Olsson (U.S.A.), Assistant Executive Director
• Kent Cohenour (U.S.A.), Treasurer
• José Luis Ferreria (Argentina)
• Anders Bo Holmlund (Sweden)
• Luis R. Quevedo (Chile)
• Jurgen Reuther (Germany)
• Herman F. Sailer (Switzerland)
• Kanichi Seto (Japan)
• John W. Frame (United Kingdom), Editor, Newsletter
• Patrick Bryan Uys (South Africa), Chairman, XV ICOMS Organizing Committee
• Piet E. Haers (United Kingdom), Editor-in-Chief, IJOMS
• Robert M. Cook (Australia), Foundation Chairman
• David Perrott (U.S.A.), Chairman, Technology & Communications Committee
• Herman Sailer (Switzerland), Chairman, Scientific Liaison Committee
• Alastair Norman Goss (Australia), Chairman, Education Committee
16th International Conference on Oral and Maxillofacial Surgery Athens, Greece May 14–20, 2003


• Paul J.W. Stoelinga (Netherlands), President
• José Luis Ferreria (Argentina), President-Elect
• John F. Helfrick (U.S.A.), Past-President
• Victor Moncarz (Canada), Executive Director
• Alexis Olsson (U.S.A.), Assistant Executive Director
• John Ll. Williams (United Kingdom), Treasurer
• Donald F. Booth (U.S.A.), North American Representative
• Edela Puricelli (Brazil), Latin American Representative
• Herman F. Sailer (Switzerland), European Representative
• Kanichi Seto (Japan), Asian Representative
• John Curtin (Australia), Oceania Representative
• Byoung Ouck Cho (Republic of Korea)
• Anders Holmlund (Sweden)
• Piet E. Haers (United Kingdom), Editor-in-Chief, IJOMS
• Marsden W. Bell (New Zealand) Foundation Chairman
• Angelos P. Angelopoulos (Greece), Chairman, XVI ICOMS Organizing Committee
• Nabil Samman (People’s Republic of China) Chairman, Education Committee
n
2003–2005 2005–2007
17th International Conference on Oral and Maxillofacial Surgery Vienna, Austria August 28–September 4, 2005


• José Luis Ferreria (Argentina), President
• John Ll. Williams (United Kingdom), President-Elect
• Paul J.W. Stoelinga (Netherlands), Past-President
• John F. Helfrick (U.S.A.), Executive Director
• Alexis Olsson (U.S.A.), Assistant Executive Director
• Donald F. Booth (U.S.A.), Treasurer, North American Representative
• Byung Ho Choi (Republic of Korea)
• Francis DiPlacido (U.S.A.)
• Kishore Pangal Nayak (India)
• Edwin Valencia Mundy (Chile), Latin American Representative
• John Lowry (United Kingdom), European Representative
• Kenichi Kurita (Japan), Asian Representative
• John Curtin (Australia), Oceania Representative
• Piet E. Haers (United Kingdom), Editor-in-Chief, IJOMS
• Marsden W. Bell (New Zealand), Foundation Chairman
• Nabil Samman (People’s Republic of China), Chairman, Education Committee
• Rolf Ewers (Austria), Chairman, XVII ICOMS Organizing Committee
• John Ll. Williams (United Kingdom), President
• Nabil Samman (People’s Republic of China), President-Elect
• José Luis Ferreria (Argentina), Past-President
• Paul J.W. Stoelinga (Netherlands), Foundation Chairman
• Donald F. Booth (U.S.A.), Treasurer, North American Representative
• John F. Helfrick (U.S.A.), Executive Director
• Alexis Olsson (U.S.A.), Assistant Executive Director, Newsletter Editor
• Gabriele A. Milesi (Austria), Task Force Chair
• Sanjiv C. Nadir (India), Member-at-Large
• Conrad Masureik (South Africa), Member-at-Large
• Henning Schliephake (Germany), Member-at-Large
• Edwin Valencia Mundy (Chile), Latin American Representative
• John Lowry (United Kingdom), European Representative
• Kenichi Kurita (Japan), Asian Representative
• John Curtin (Australia), Oceania Representative
• Ademola Abayomi Olaitan (Nigeria), African Representative
• Piet E. Haers (United Kingdom), Editor-in-Chief, IJOMS
• Julio Acero (Spain), Chair, Education Committee
• Stephen Feinberg (U.S.A.), Chair, Research Committee
• Kishore Pangal Nayak (India), Chair, XVII ICOMS Organizing Committee
19th International Conference on Oral and Maxillofacial Surgery

Shanghai, People’s Republic of China May 23–27, 2009
• Nabil Samman (Hong Kong), President
• L arry W. Nissen (U.S.A.), President-Elect
• John Ll. Williams (United Kingdom), Past-President Foundation Chair
• Donald F. Booth (U.S.A.), Treasurer
• John F. Helfrick (U.S.A.), Executive Director
• Alexis Olsson (U.S.A.), Assistant Executive Director
• Kishore P. Nayak (India), Member-at-Large
• Joseph F. Piecuch (U.S.A.), Member-at-Large
• Henning Schliephake (Germany), Member-at-Large
• Ademola Abayomi Olaitan (Nigeria), African Representative
• Kenichi Kurita (Japan), Asian Representative
• John Lowry (United Kingdom) & Henri Thuau (United Kingdom), European Representatives
• Edwin Valencia Mundy (Chile) & Luiz Fernando Lobo Leandro (Brazil), Latin American Representatives
• Boyd J. Tomasett (U.S.A.), North American Representative
• Paul Sambrook (Australia), Oceania Representative
• Piet E. Haers (United Kingdom), Editor-in-Chief, IJOMS
• Julio Acero Sanz (Spain), Chair, Education Committee
• Stephen Feinberg (U.S.A.), Chair, Research Committee
• Gabriele A. Millesi (Austria), Task Force Chair
• Steve Shen (People’s Republic of China), Chair, XIX ICOMS Organizing Committee
20th International Conference on Oral and Maxillofacial Surgery Santiago, Chile November 1–4, 2011

• L arry W. Nissen (U.S.A.), President
• Kishore Pangal Nayak (India), President-Elect
• Nabil Samman (Peoples Republic of China), Past-President, Foundation Chair
• Robert T. M. Woodwards (United Kingdom), Treasurer
• John F. Helfrick (U.S.A.), Executive Director
• Alexis Olsson (U.S.A.), Assistant Executive Director
• Gabriele A. Millesi (Austria), Member-at-Large
• Joseph F. Piecuch (U.S.A.), Member-at-Large
• Cesar A. Guerrero (Venezuela), Member-at-Large
• Ademola Abayomi Olaitan (Nigeria), African Representative
• Kenichi Kurita (Japan), Asian Representative
• Henri Thuau (United Kingdom), European Representative
• Luiz Fernando Lobo Leandro (Brazil), Latin American Representative
• Boyd J. Tomasetti (U.S.A.), North American Representative
• Paul Sambrook (Australia), Oceania Representative
• Piet E. Haers (United Kingdom), Editor-in-Chief, IJOMS
• Julio Acero (Spain), Chair, Education Committee
• Stephen Feinberg (U.S.A.), Chair, Research Committee
• Luis Quevedo R. (Chile), Chair, XX ICOMS Organizing Committee
Held in Madrid, April 1974 with comments by Sir Terence Ward, C.B.E., Chairman of the Workshop
Workshop Summary
The first world meeting of oral surgeons took place in London in 1962, and at that meeting, discussion was inevitable on the standards and training of young men entering the specialty.
The first world meeting of oral surgeons took place in London in 1962, and at that meeting, discussion was inevitable on the standards and training of young men entering the specialty.
Most of the senior men present were self-trained, in that no standard curriculum of postgraduate education was established in their own country, so they went to a country or environment of their own choice where they considered they could learn the science and art of their chosen profession.
There were exceptions. In the United States of America, training programs had been established, and state, national and American Society of Oral Surgeons’ Boards had been founded to assess the ability and proficiency of surgeons who had attended their prescribed programs.
In the United Kingdom, the Royal College of Surgeons of England had laid down a system of training and examination, at the end of which the trainee competed with others for an established consultant post in the National Health Service.
At all subsequent international meetings of oral surgeons some time was given to the consideration of training, but at Madrid, it was decided to establish a major exercise and investigate in depth the training of the oral surgeons.
The preliminary preparation for the workshop was immense. All national associations affiliated to the IAOS were contacted and they nominated a delegate or delegates to attend. Schemes of national training were obtained from each country and each delegate had in his possession before coming to Madrid, the documentation of all national training programs.
These national programs varied tremendously. In the United Kingdom, there is a minimum of eight years full-time training subsequent to the obtaining of a dental degree. In the United States, the training period was usually for three years, although some centers of excellence provided four-year training programs. Some countries left the length of training and the site of training to the judgment of the trainee, and in other countries the potential oral surgeon had to leave his own country to obtain training.
The intent of the workshop was to bring together for four days, senior clinicians who would discuss training programs, and perhaps at the conclusion, produce a document that would be presented to the international association.
Such a document should present a curriculum of training that could act as a model to all countries that had their training programs under review. Under no circumstances could such a document be considered mandatory. It would be an impertinence for the international association to impose a system of training on any country, because the context and pattern of training is the responsibility of each national association for application to its own graduates in its own country; if the I.A.O.S. could produce a document that would reflect the views of the delegate, it could be considered an advisory scheme, which countries might abstract from and modify for their own needs.
It was decided to work in modules. Two countries sat together with their national training programs and came to agreement on an acceptable program for their two countries. The groupings included:
• Denmark and Sweden
• Finland and Norway
• Netherlands and Israel
• Australia and Great Britain
• U.S.A. and Venezuela
• U.S.A. and Canada
• Argentina and Spain
• France and other countries
Next day, four countries met and considered the two documents from the four and produced one document acceptable to the four countries.
Then we had eight delegates with the two documents from each of the four countries, and each group of eight produced a document that went to the final session, where the 16 delegates came together for the first time.
Discussion was keen, never heated, and it meant a lot of give and take by all delegates. It was with regret that the Spanish delegation thought fit to withdraw after the penultimate session — a decision I believe related more to language and translation difficulties than disagreement, because I know the high objectives of the Spanish Oral Surgery do not differ from those in the rest of the world
Subsequent to agreeing on the format of the final document, the French delegation, in view of the political commitment to the European Economic Community, thought fit to withdraw — an action that I as Chairman could not understand, because they had made a major contribution through all stages of discussion and their presence had been appreciated by all.
The final document was presented to the general assembly of the IAOS and produced tremendous discussion and debate, and discussion and debate will continue whenever training is discussed in the future. Of overriding
importance was the general acceptance of the principle that a graduate may enter the specialty of oral and maxillofacial surgery with either a primary dental or a primary medical degree and that the ultimate result of training must be to produce a specialist of equal status and competence from either basic discipline. A number of the younger fellows desired that the title of IAOS be altered to include “Maxillo Facial” and, or the definition of oral surgery be changed, but the chairman ruled that these recommendations would have to be considered by a separate committee in the future.
Many men do not realize that the field of maxillofacial surgery is an extension of many disciplines and we could have specialties of “plastic and maxillofacial surgery” “oto-rhinology and maxillofacial surgery” “general and maxillofacial surgery” and “oral and maxillofacial surgery.”
If the oral surgeon extends his personal training to the requisite standard, there is nothing to prevent him assuming the title of oral and maxillofacial surgeon, if such a title is accepted by his national association. I think it is worthwhile stating the definition of our specialty —
“
O ral surgery is part of dental surgery which deals with the diagnosis, the surgical and adjunctive treatment of the diseases, injuries, defects of the human jaws and associated structures.”
You will see that this definition embraces the complete field in which we work. To generalize a definition leaves the spectrum wide open. To particularize has many dangers of strict adherence to the written word.
It became obvious during the workshop that there is no single road to excellence in training in our specialty and the international association has no intention to impose on any country, a rigid pattern of training. It is the right of any country to establish a regime of training for the specialists in its own domains, but we hope the workshop has produced patterns of training that can guide us in the future.
As chairman, I would like to express my personal thanks to all who gave up their valuable time and worked to make the workshop a success and to thanks Miss Pam Clarke and Miss Sheila Lawry; without their unselfish help and efficiency, the project would not have been completed.
Sir Terence G. Ward, C.B.E. Chairman of the WorkshopWorkshop Report – Final Stage
Oral surgery is practiced by specialist with differing training. However, in most parts of the world, the majority of this work is carried out by those who have a basic dental degree with additional medical and surgical training and experience.
It is felt that the definition of oral surgery should include the term maxillofacial. The reason for this is that like all fields in the health sciences the advances in knowledge and technology in our specialty are increasing rapidly and thus the scope of the specialty as we know it today is far different than it was twenty years ago. Therefore it is suggested that a new definition of our specialty be considered in the future.
The individuals entrusted with providing exemplary oral maxillofacial surgical care to their patients may have a dental degree and medical training or a medical degree and dental training. Some individuals have both the medical and dental degrees. Because of economy and the necessity of providing competent well trained individuals who will have the opportunity to serve for a significant period of time, the training and educational programs should not be prolonged unnecessarily. Excessive tenure in training difficult to justify in terms of the investment of money and manpower that a country might be willing to commit, whatever his basic educational background, the individual who enters into a postgraduate training and educational program in oral maxillofacial surgery must attain upon the completion of that training a minimal level of competency in the specialty. Each country must determine the best means of attesting to the quality of the educational and training experience in oral-maxillofacial surgery an appropriate certifying body in their country.
General objectives
Oral surgery for healthy patients and for those with systemic disease forms, with oral medicine, the bulk of the oral surgeon’s work in our countries. Maxillofacial injuries and major oral surgery are much smaller parts in terms of numbers of patients treated.
The oral surgeon should be broadly educated and widely experience as both clinician and diagnostician. He should have had a good basic training in all aspects of dentistry, but since the major part of his work involves oral surgery, he must have a sound knowledge and broad experience in this field.
A knowledge of general medicine and surgery is necessary because the physical state of an increasing number of patients is such that a decision on their correct management requires a detailed appreciation of problems that are not taught in the normal undergraduate training curriculum. For this reason it is essential for the oral surgeon to have acquired appropriate medical and surgical training during his postgraduate education.
Particular Training Objectives
An oral surgeon who has completed his training should ideally have acquired extensive knowledge of the basic biological and dental sciences and adequate competence in the following:
1. The relevant aspects of medicine and surgery and of general pathology microbiology, biochemistry, genetics, pharmacology, anesthesia, sedation techniques and local analgesia.
2. Preventive and restorative dentistry.
3. Oral medicine, oral pathology and therapeutics
4. Dentoalveolar surgery.
5. Management of maxillofacial injuries
6. Treatment of diseases, anomalies and functional disturbances of the teeth, jaws and salivary glands.
7. Applied statistics, research and teaching, administration, management and jurisprudence.
Considerable discussion took place regarding the time a postgraduate student should spend in specialist oral surgical training, and it was felt that a minimum period of four years would be desirable and should cover the particular training objectives outlined above. The importance of general hospital in-patient experience is stressed. In-service experience should always be supported by formal instruction. A suggested training program embracing the previous suggestions would be summarized as follows:
• Basic Degree in Dentistry
• Supplementary Basic Training
a. 1 year general surgery and medicine and 1 year on a rotational basis in some of the following departments:
i. General Anesthesia
ii. O to-rhinology-Laryngology
iii. Neurosurgery
iv. Traumatology
v. Plastic Surgery
vi. Orthopaedic Surgery
report of education committee (1980)
The Education Committee convened in Haifa, Israel October 17 to 21, 1977. In addition to the permanent members professors D. Laskin (U.S.A.), E. Machtens (West Germany, D. Gutman (Israel) and IAOS President Bill van der Kwast (the Netherlands), chairman participated in the meeting. Prof. A. Shersivan (Tel Aviv) served as educational consultant.
The committee reviewed all the documents accumulated by the previous education committee, especially the report on the Madrid workshop (April, 1974) and the summary of the seminar held in Copenhagen (February, 1977).
The committee believes, since educational systems vary so much from one country to another, that degree requirements and certification of training programs were not within the scope of this workshop. The document produced by the education committee that outlines the suggested education and training of the oral and maxillofacial surgeon should be considered as a guideline. It is a preliminary framework and if approved by the IAOS should be studied and detailed in each of its aspects through future workshops.
For the purpose of producing such a document the committee’s deliberations are based on the following definition of Oral Surgery: “Oral surgery is that part of surgery which deals with the diagnosis, the surgical and adjunctive treatment of the diseases, injuries and defects of the oral and maxillofacial region.” The term “oral surgery” in this document is used synonymously with the term “oral and maxillofacial surgery”.
IAOMS Newsletter, 1980
Guidelines for the Education and Training of the Oral and Maxillofacial Surgeon
The educational experience of the oral surgeon should include:
A. Basic Science Education which provides: Applicable knowledge in the basic preclinical sciences- anatomy, including, embryology, physiology, pathology, pharmacology, microbiology, immunology and genetics.
B. Basic Clinical Education which provides:
1. Skills in physical examination and proficiency with other diagnostic methods.
2. The capability to diagnose common dental and medical conditions, including knowledge of relevant pathophysiology.
3. Understanding and skills in the general management of these conditions.
C. Advanced Clinical Education which provides specific competence in the diagnosis, general and surgical management of the following conditions in the oral and maxillofacial region:
1. Diseases of the teeth, periodontal structures and oral mucosa.
2. Trauma of the soft and hard tissues.
3. Congenital, developmental and acquired deformities and defects.
4. Tumors and cysts.
5. Infections and inflammations.
6. Oro-facial pain.
The major portion of the basic science and basic clinical education should be obtained at the pre-doctoral (preapprobation) level. The advanced clinical education and skills and those aspects of the basic education not accomplished earlier, should be obtained in a teaching hospital.
Although the major portion of this phase of training should occur on the oral and maxillofacial service, some aspects of medicine and surgery can be learned by rotations on these services. The minimal time necessary to become didactically and clinically proficient as an oral surgeon, beginning with the pre-doctoral (pre-approbation) education at the college or university level and including the period up to board certification (when such situations are applicable in a particular country), is 10 years.
i n ternational guideline S for S p ecialty training and education in oral and maxillofacial S u rgery (durban, 2001)
Preface
The International Association of Oral and Maxillofacial Surgeons (IAOMS) is committed to quality patient care. The quality of care provided to patients by oral and maxillofacial surgeons is largely dependent upon the quality of their training in the specialty. In order to practice the full scope of the specialty, oral maxillofacial surgeons are unique in that they require education in dentistry, medicine and surgery, which should be formally recognized based on regional requirements.
The mission of IAOMS is to guide the regional or national development of oral and maxillofacial surgery worldwide. Although it is recognized that there are many social, economic, and political differences throughout the world which impact on the education of oral and maxillofacial surgeons, these international guidelines define the fundamental components which should be considered in the development of regional and national guidelines.
1.0 Components and Duration of Specialty Training
1.1 The specialty training in oral and maxillofacial surgery may be accomplished in a number of ways. The entry point for training may either be a dental degree or a medical degree.
1.2 The broad requirements for the component of training in oral and maxillofacial surgery are set out in these guidelines, particularly in sections 4.0 and 5.0. Precisely how this is accomplished and the required duration should be the subject of regional or national guidelines which assures the practice of the full scope of the specialty as defined in this document.
1.3 The maximum length of training following completion of the first degree should not be greater than eight years. Careful attention should be given to integrating components of dental, medical and clinical education so that an oral and maxillofacial surgeon may complete their training at an age which allows for a long and productive career.
2.0 Faculty
The advanced training program in oral and maxillofacial surgery should be directed by an oral and maxillofacial surgeon. It is the director`s responsibility to assure that individuals completing training meet the performance standards established for the program and for the practice of the specialty.
The faculty should have a strong interest in teaching and be willing to allocate the necessary time and effort to the educational program. The majority of the specialty instruction and supervision should be conducted by individuals who are educationally qualified in oral and maxillofacial surgery.
2.1 All training programs should be directed by a single responsible individual.
2.2 The program director should devote adequate time to the training program to ensure:
a. The development and implementation of a planned curriculum.
b. Ongoing evaluation of the program content, faculty teaching, and resident performance. c. Proper administration of the program.
d. Maintenance of records related to the educational program.
2.3 The size and time commitment of the teaching staff should be sufficient to ensure:
a. Continuity of instruction.
b. E xposure of trainees to a broad range of diagnostic and treatment modalities.
c. Faculty participation in teaching activities, including conferences and seminars.
d. Quality assurance and audit through the evaluation of complications and outcomes of cases treated by the trainees.
2.4 Faculty should be available for supervision and consultation for procedures completed in the operating room and outpatient departments.
2.5 The faculty should have a committed and demonstrated interest in teaching, personally provide the necessary time and effort to the educational process, and set an example for scholarly activities.
3.0 Facilities and Resources
Specialty training in oral and maxillofacial surgery requires both outpatient clinic and operating room experience. Facilities and resources should be adequate to provide the educational experiences and opportunities required to fulfill the needs of the educational program.
3.1 Clinical facilities should be properly equipped for performance of all ambulatory oral and maxillofacial surgery procedures.
4.0 Curriculum
4.1 The trainee should have extensive training in medicine which will provide the ability to evaluate the total patient and to assess the patient as a surgical and anaesthetic risk. This training in medicine should provide residents with an understanding of:
a. Systemic disease, including: (i) comprehensive knowledge of various organ systems with particular emphasis on cardiovascular, pulmonary, hepatic, renal and endocrine physiology and pathology. (ii) f amiliarity with diagnostic aids such as electrocardiography, general and maxillofacial imaging, and clinical laboratory diagnosis.
b. Patient evaluation, including additional experience in the art of history-taking and comprehensive physical examination.
c. Therapeutics, including knowledge of the accepted therapeutic agents employed in medical management and the pharmacologic action of agents used in the treatment of oral and maxillofacial surgery patients.
d. This core surgical experience should not be less than one year`s duration. This may be accomplished through formal medical education and/or during specialty training.
4.2 Fundamental to the training of an oral and maxillofacial surgeon is extensive experience in the areas of critical care of the seriously ill surgical patient and the team management of the severely injured patient.
4.3 The trainee should have training in dentistry as it is dental education which differentiates oral and maxillofacial surgeons from other surgical specialties.
4.4 The oral and maxillofacial surgery trainee should be exposed to the full scope of the specialty as defined in 5.0. The minimum time for this clinical oral and maxillofacial surgery training should be 30 months.
4.5 A minimum of 12 months of the time in oral and maxillofacial surgery training should be spent in a position of surgical responsibility (e.g. senior resident, senior registrar).
4.6 It is the regional or national responsibility to carefully review the curriculum as it relates to the local health needs. This review should commence with analysis of the entry point qualification to determine areas of deficiency which should then be addressed in accord with 4.1, 4.2 and 4.3.
5.0 Clinical Oral and Maxillofacial Surgery
Clinical training in oral and maxillofacial surgery should provide a complete, progressively graduated sequence of outpatient, inpatient, and emergency room experience. The trainee`s exposure to major and minor surgical procedures should be integrated throughout the duration of the training program. The trainee should be exposed to sufficient numbers of patients with a wide variety of problems to develop competence in the full scope of oral and maxillofacial surgery. The scope of oral and maxillofacial surgery includes, but it is not limited to:
a. Oral pathology/oral medicine, including management of diseases of oral and maxillofacial regions.
b. Dentolaveolar surgery and management of pain and anxiety.
c. Preprosthetic surgery including implantology.
d. Surgical and nonsurgical management of TMJ diseases and disorders.
e. Management of maxillofacial trauma (soft and hard tissues).
f. Management of benign and malignant tumors.
i n ternational training guideline S for S p ecialty training and education in oral and maxillofacial S urgery (durban, 2001) (continued)
g. Regional reconstructive surgery, including harvesting of hard and soft tissue grafts and microsurgery.
h. Orthognathic/orthopaedic facial surgery.
i. Aesthetic facial surgery.
j. Surgical treatment of congenital abnormalities, including cleft lip and cleft palate surgery.
k. Craniofacial surgery.
5.1 The trainee should receive extensive experience throughout the training program in all aspects of pain and anxiety control, including general and regional anaesthesia and other methods of pain control.
5.2 The trainee should receive a broad surgical experience by being primary surgeon on cases involving the full scope of oral and maxillofacial surgery, including major maxillofacial trauma, pathology, orthognathic surgery, and reconstructive maxillofacial surgery.
5.2.1 Fellowships, following specialty training, are one method for providing surgeons with additional surgical experience and for expansion of their scope of practice.
5.3 The trainee should have the opportunity of discussing treatment plans with members of other specialties in both medicine and dentistry.
5.4 Regularly scheduled seminars and conferences should be conducted to augment the clinical program.
5.4.1 Faculty and trainees should be encouraged to attend national, regional, and international scientific meetings.
6.0 Trainee Evaluation
There should be documentation of ongoing evaluation of the progress of each trainee. The trainee should receive formal periodic evaluation and should only be advanced to a position of higher responsibility on the basis of this evaluation and readiness for advancement.
Performance should be formally evaluated and documented in all the components of training as defined in sections 4.0, and 5.0 of this document by the responsible director as set out in section 2.1 and 2.2.
7.0 Research and Publication
The trainee is encouraged to participate in research and to publish.
7.1 Trainees should be encouraged to engage in an investigative project.
7.2 Training opportunities which incorporate a research qualification are strongly encouraged.
8.0 International Training Opportunities
The international exchange of trainees and faculties is to be encouraged.
8.1 International training opportunities for oral and maxillofacial surgeons and trainees expands educational options and improves international understanding within the specialty and is an important aspect of professional education in oral and maxillofacial surgery.
8.2 Each regional or national association should, in cooperation with the IAOMS, facilitate such educational opportunities.
9.0 Quality Assurance in Oral and Maxillofacial Surgery Education
It is recommended that each region and nation develop a standard of training document consistent with these International Guidelines. Mechanisms should be developed by each region and nation, to assure that the goals and objectives of its training document are met and recognized by the appropriate authorities.

